

Family Life

AAP Schedule of Well-Child Care Visits

Parents know who they should go to when their child is sick. But pediatrician visits are just as important for healthy children.
The Bright Futures /American Academy of Pediatrics (AAP) developed a set of comprehensive health guidelines for well-child care, known as the " periodicity schedule ." It is a schedule of screenings and assessments recommended at each well-child visit from infancy through adolescence.
Schedule of well-child visits
- The first week visit (3 to 5 days old)
- 1 month old
- 2 months old
- 4 months old
- 6 months old
- 9 months old
- 12 months old
- 15 months old
- 18 months old
- 2 years old (24 months)
- 2 ½ years old (30 months)
- 3 years old
- 4 years old
- 5 years old
- 6 years old
- 7 years old
- 8 years old
- 9 years old
- 10 years old
- 11 years old
- 12 years old
- 13 years old
- 14 years old
- 15 years old
- 16 years old
- 17 years old
- 18 years old
- 19 years old
- 20 years old
- 21 years old
The benefits of well-child visits
Prevention . Your child gets scheduled immunizations to prevent illness. You also can ask your pediatrician about nutrition and safety in the home and at school.
Tracking growth & development . See how much your child has grown in the time since your last visit, and talk with your doctor about your child's development. You can discuss your child's milestones, social behaviors and learning.
Raising any concerns . Make a list of topics you want to talk about with your child's pediatrician such as development, behavior, sleep, eating or getting along with other family members. Bring your top three to five questions or concerns with you to talk with your pediatrician at the start of the visit.
Team approach . Regular visits create strong, trustworthy relationships among pediatrician, parent and child. The AAP recommends well-child visits as a way for pediatricians and parents to serve the needs of children. This team approach helps develop optimal physical, mental and social health of a child.
More information
Back to School, Back to Doctor
Recommended Immunization Schedules
Milestones Matter: 10 to Watch for by Age 5
Your Child's Checkups
- Bright Futures/AAP Recommendations for Preventive Pediatric Health Care (periodicity schedule)

KATHERINE TURNER, MD
Am Fam Physician. 2018;98(6):347-353
Related letter: Well-Child Visits Provide Physicians Opportunity to Deliver Interconception Care to Mothers
Author disclosure: No relevant financial affiliations.
The well-child visit allows for comprehensive assessment of a child and the opportunity for further evaluation if abnormalities are detected. A complete history during the well-child visit includes information about birth history; prior screenings; diet; sleep; dental care; and medical, surgical, family, and social histories. A head-to-toe examination should be performed, including a review of growth. Immunizations should be reviewed and updated as appropriate. Screening for postpartum depression in mothers of infants up to six months of age is recommended. Based on expert opinion, the American Academy of Pediatrics recommends developmental surveillance at each visit, with formal developmental screening at nine, 18, and 30 months and autism-specific screening at 18 and 24 months; the U.S. Preventive Services Task Force found insufficient evidence to make a recommendation. Well-child visits provide the opportunity to answer parents' or caregivers' questions and to provide age-appropriate guidance. Car seats should remain rear facing until two years of age or until the height or weight limit for the seat is reached. Fluoride use, limiting or avoiding juice, and weaning to a cup by 12 months of age may improve dental health. A one-time vision screening between three and five years of age is recommended by the U.S. Preventive Services Task Force to detect amblyopia. The American Academy of Pediatrics guideline based on expert opinion recommends that screen time be avoided, with the exception of video chatting, in children younger than 18 months and limited to one hour per day for children two to five years of age. Cessation of breastfeeding before six months and transition to solid foods before six months are associated with childhood obesity. Juice and sugar-sweetened beverages should be avoided before one year of age and provided only in limited quantities for children older than one year.
Well-child visits for infants and young children (up to five years) provide opportunities for physicians to screen for medical problems (including psychosocial concerns), to provide anticipatory guidance, and to promote good health. The visits also allow the family physician to establish a relationship with the parents or caregivers. This article reviews the U.S. Preventive Services Task Force (USPSTF) and the American Academy of Pediatrics (AAP) guidelines for screenings and recommendations for infants and young children. Family physicians should prioritize interventions with the strongest evidence for patient-oriented outcomes, such as immunizations, postpartum depression screening, and vision screening.
Clinical Examination
The history should include a brief review of birth history; prematurity can be associated with complex medical conditions. 1 Evaluate breastfed infants for any feeding problems, 2 and assess formula-fed infants for type and quantity of iron-fortified formula being given. 3 For children eating solid foods, feeding history should include everything the child eats and drinks. Sleep, urination, defecation, nutrition, dental care, and child safety should be reviewed. Medical, surgical, family, and social histories should be reviewed and updated. For newborns, review the results of all newborn screening tests ( Table 1 4 – 7 ) and schedule follow-up visits as necessary. 2
PHYSICAL EXAMINATION
A comprehensive head-to-toe examination should be completed at each well-child visit. Interval growth should be reviewed by using appropriate age, sex, and gestational age growth charts for height, weight, head circumference, and body mass index if 24 months or older. The Centers for Disease Control and Prevention (CDC)-recommended growth charts can be found at https://www.cdc.gov/growthcharts/who_charts.htm#The%20WHO%20Growth%20Charts . Percentiles and observations of changes along the chart's curve should be assessed at every visit. Include assessment of parent/caregiver-child interactions and potential signs of abuse such as bruises on uncommonly injured areas, burns, human bite marks, bruises on nonmobile infants, or multiple injuries at different healing stages. 8
The USPSTF and AAP screening recommendations are outlined in Table 2 . 3 , 9 – 27 A summary of AAP recommendations can be found at https://www.aap.org/en-us/Documents/periodicity_schedule.pdf . The American Academy of Family Physicians (AAFP) generally adheres to USPSTF recommendations. 28
MATERNAL DEPRESSION
Prevalence of postpartum depression is around 12%, 22 and its presence can impair infant development. The USPSTF and AAP recommend using the Edinburgh Postnatal Depression Scale (available at https://www.aafp.org/afp/2010/1015/p926.html#afp20101015p926-f1 ) or the Patient Health Questionnaire-2 (available at https://www.aafp.org/afp/2012/0115/p139.html#afp20120115p139-t3 ) to screen for maternal depression. The USPSTF does not specify a screening schedule; however, based on expert opinion, the AAP recommends screening mothers at the one-, two-, four-, and six-month well-child visits, with further evaluation for positive results. 23 There are no recommendations to screen other caregivers if the mother is not present at the well-child visit.
PSYCHOSOCIAL
With nearly one-half of children in the United States living at or near the poverty level, assessing home safety, food security, and access to safe drinking water can improve awareness of psychosocial problems, with referrals to appropriate agencies for those with positive results. 29 The prevalence of mental health disorders (i.e., primarily anxiety, depression, behavioral disorders, attention-deficit/hyperactivity disorder) in preschool-aged children is around 6%. 30 Risk factors for these disorders include having a lower socioeconomic status, being a member of an ethnic minority, and having a non–English-speaking parent or primary caregiver. 25 The USPSTF found insufficient evidence regarding screening for depression in children up to 11 years of age. 24 Based on expert opinion, the AAP recommends that physicians consider screening, although screening in young children has not been validated or standardized. 25
DEVELOPMENT AND SURVEILLANCE
Based on expert opinion, the AAP recommends early identification of developmental delays 14 and autism 10 ; however, the USPSTF found insufficient evidence to recommend formal developmental screening 13 or autism-specific screening 9 if the parents/caregivers or physician have no concerns. If physicians choose to screen, developmental surveillance of language, communication, gross and fine movements, social/emotional development, and cognitive/problem-solving skills should occur at each visit by eliciting parental or caregiver concerns, obtaining interval developmental history, and observing the child. Any area of concern should be evaluated with a formal developmental screening tool, such as Ages and Stages Questionnaire, Parents' Evaluation of Developmental Status, Parents' Evaluation of Developmental Status-Developmental Milestones, or Survey of Well-Being of Young Children. These tools can be found at https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/Screening/Pages/Screening-Tools.aspx . If results are abnormal, consider intervention or referral to early intervention services. The AAP recommends completing the previously mentioned formal screening tools at nine-, 18-, and 30-month well-child visits. 14
The AAP also recommends autism-specific screening at 18 and 24 months. 10 The USPSTF recommends using the two-step Modified Checklist for Autism in Toddlers (M-CHAT) screening tool (available at https://m-chat.org/ ) if a physician chooses to screen a patient for autism. 10 The M-CHAT can be incorporated into the electronic medical record, with the possibility of the parent or caregiver completing the questionnaire through the patient portal before the office visit.
IRON DEFICIENCY
Multiple reports have associated iron deficiency with impaired neurodevelopment. Therefore, it is essential to ensure adequate iron intake. Based on expert opinion, the AAP recommends supplements for preterm infants beginning at one month of age and exclusively breastfed term infants at six months of age. 3 The USPSTF found insufficient evidence to recommend screening for iron deficiency in infants. 19 Based on expert opinion, the AAP recommends measuring a child's hemoglobin level at 12 months of age. 3
Lead poisoning and elevated lead blood levels are prevalent in young children. The AAP and CDC recommend a targeted screening approach. The AAP recommends screening for serum lead levels between six months and six years in high-risk children; high-risk children are identified by location-specific risk recommendations, enrollment in Medicaid, being foreign born, or personal screening. 21 The USPSTF does not recommend screening for lead poisoning in children at average risk who are asymptomatic. 20
The USPSTF recommends at least one vision screening to detect amblyopia between three and five years of age. Testing options include visual acuity, ocular alignment test, stereoacuity test, photoscreening, and autorefractors. The USPSTF found insufficient evidence to recommend screening before three years of age. 26 The AAP, American Academy of Ophthalmology, and the American Academy of Pediatric Ophthalmology and Strabismus recommend the use of an instrument-based screening (photoscreening or autorefractors) between 12 months and three years of age and annual visual acuity screening beginning at four years of age. 31
IMMUNIZATIONS
The AAFP recommends that all children be immunized. 32 Recommended vaccination schedules, endorsed by the AAP, the AAFP, and the Advisory Committee on Immunization Practices, are found at https://www.cdc.gov/vaccines/schedules/hcp/child-adolescent.html . Immunizations are usually administered at the two-, four-, six-, 12-, and 15- to 18-month well-child visits; the four- to six-year well-child visit; and annually during influenza season. Additional vaccinations may be necessary based on medical history. 33 Immunization history should be reviewed at each wellness visit.
Anticipatory Guidance
Injuries remain the leading cause of death among children, 34 and the AAP has made several recommendations to decrease the risk of injuries. 35 – 42 Appropriate use of child restraints minimizes morbidity and mortality associated with motor vehicle collisions. Infants need a rear-facing car safety seat until two years of age or until they reach the height or weight limit for the specific car seat. Children should then switch to a forward-facing car seat for as long as the seat allows, usually 65 to 80 lb (30 to 36 kg). 35 Children should never be unsupervised around cars, driveways, and streets. Young children should wear bicycle helmets while riding tricycles or bicycles. 37
Having functioning smoke detectors and an escape plan decreases the risk of fire- and smoke-related deaths. 36 Water heaters should be set to a maximum of 120°F (49°C) to prevent scald burns. 37 Infants and young children should be watched closely around any body of water, including water in bathtubs and toilets, to prevent drowning. Swimming pools and spas should be completely fenced with a self-closing, self-latching gate. 38
Infants should not be left alone on any high surface, and stairs should be secured by gates. 43 Infant walkers should be discouraged because they provide no benefit and they increase falls down stairs, even if stair gates are installed. 39 Window locks, screens, or limited-opening windows decrease injury and death from falling. 40 Parents or caregivers should also anchor furniture to a wall to prevent heavy pieces from toppling over. Firearms should be kept unloaded and locked. 41
Young children should be closely supervised at all times. Small objects are a choking hazard, especially for children younger than three years. Latex balloons, round objects, and food can cause life-threatening airway obstruction. 42 Long strings and cords can strangle children. 37
DENTAL CARE
Infants should never have a bottle in bed, and babies should be weaned to a cup by 12 months of age. 44 Juices should be avoided in infants younger than 12 months. 45 Fluoride use inhibits tooth demineralization and bacterial enzymes and also enhances remineralization. 11 The AAP and USPSTF recommend fluoride supplementation and the application of fluoride varnish for teeth if the water supply is insufficient. 11 , 12 Begin brushing teeth at tooth eruption with parents or caregivers supervising brushing until mastery. Children should visit a dentist regularly, and an assessment of dental health should occur at well-child visits. 44
SCREEN TIME
Hands-on exploration of their environment is essential to development in children younger than two years. Video chatting is acceptable for children younger than 18 months; otherwise digital media should be avoided. Parents and caregivers may use educational programs and applications with children 18 to 24 months of age. If screen time is used for children two to five years of age, the AAP recommends a maximum of one hour per day that occurs at least one hour before bedtime. Longer usage can cause sleep problems and increases the risk of obesity and social-emotional delays. 46
To decrease the risk of sudden infant death syndrome (SIDS), the AAP recommends that infants sleep on their backs on a firm mattress for the first year of life with no blankets or other soft objects in the crib. 45 Breastfeeding, pacifier use, and room sharing without bed sharing protect against SIDS; infant exposure to tobacco, alcohol, drugs, and sleeping in bed with parents or caregivers increases the risk of SIDS. 47
DIET AND ACTIVITY
The USPSTF, AAFP, and AAP all recommend breastfeeding until at least six months of age and ideally for the first 12 months. 48 Vitamin D 400 IU supplementation for the first year of life in exclusively breastfed infants is recommended to prevent vitamin D deficiency and rickets. 49 Based on expert opinion, the AAP recommends the introduction of certain foods at specific ages. Early transition to solid foods before six months is associated with higher consumption of fatty and sugary foods 50 and an increased risk of atopic disease. 51 Delayed transition to cow's milk until 12 months of age decreases the incidence of iron deficiency. 52 Introduction of highly allergenic foods, such as peanut-based foods and eggs, before one year decreases the likelihood that a child will develop food allergies. 53
With approximately 17% of children being obese, many strategies for obesity prevention have been proposed. 54 The USPSTF does not have a recommendation for screening or interventions to prevent obesity in children younger than six years. 54 The AAP has made several recommendations based on expert opinion to prevent obesity. Cessation of breastfeeding before six months and introduction of solid foods before six months are associated with childhood obesity and are not recommended. 55 Drinking juice should be avoided before one year of age, and, if given to older children, only 100% fruit juice should be provided in limited quantities: 4 ounces per day from one to three years of age and 4 to 6 ounces per day from four to six years of age. Intake of other sugar-sweetened beverages should be discouraged to help prevent obesity. 45 The AAFP and AAP recommend that children participate in at least 60 minutes of active free play per day. 55 , 56
Data Sources: Literature search was performed using the USPSTF published recommendations ( https://www.uspreventiveservicestaskforce.org/BrowseRec/Index/browse-recommendations ) and the AAP Periodicity table ( https://www.aap.org/en-us/Documents/periodicity_schedule.pdf ). PubMed searches were completed using the key terms pediatric, obesity prevention, and allergy prevention with search limits of infant less than 23 months or pediatric less than 18 years. The searches included systematic reviews, randomized controlled trials, clinical trials, and position statements. Essential Evidence Plus was also reviewed. Search dates: May through October 2017.
Gauer RL, Burket J, Horowitz E. Common questions about outpatient care of premature infants. Am Fam Physician. 2014;90(4):244-251.
American Academy of Pediatrics; Committee on Fetus and Newborn. Hospital stay for healthy term newborns. Pediatrics. 2010;125(2):405-409.
Baker RD, Greer FR Committee on Nutrition, American Academy of Pediatrics. Diagnosis and prevention of iron deficiency and iron-deficiency anemia in infants and young children (0–3 years of age). Pediatrics. 2010;126(5):1040-1050.
Mahle WT, Martin GR, Beekman RH, Morrow WR Section on Cardiology and Cardiac Surgery Executive Committee. Endorsement of Health and Human Services recommendation for pulse oximetry screening for critical congenital heart disease. Pediatrics. 2012;129(1):190-192.
American Academy of Pediatrics Newborn Screening Authoring Committee. Newborn screening expands: recommendations for pediatricians and medical homes—implications for the system. Pediatrics. 2008;121(1):192-217.
American Academy of Pediatrics, Joint Committee on Infant Hearing. Year 2007 position statement: principles and guidelines for early hearing detection and intervention programs. Pediatrics. 2007;120(4):898-921.
Maisels MJ, Bhutani VK, Bogen D, Newman TB, Stark AR, Watchko JF. Hyperbilirubinemia in the newborn infant > or = 35 weeks' gestation: an update with clarifications. Pediatrics. 2009;124(4):1193-1198.
Christian CW Committee on Child Abuse and Neglect, American Academy of Pediatrics. The evaluation of suspected child physical abuse [published correction appears in Pediatrics . 2015;136(3):583]. Pediatrics. 2015;135(5):e1337-e1354.
Siu AL, Bibbins-Domingo K, Grossman DC, et al. Screening for autism spectrum disorder in young children: U.S. Preventive Services Task Force recommendation statement. JAMA. 2016;315(7):691-696.
Johnson CP, Myers SM American Academy of Pediatrics Council on Children with Disabilities. Identification and evaluation of children with autism spectrum disorders. Pediatrics. 2007;120(5):1183-1215.
Moyer VA. Prevention of dental caries in children from birth through age 5 years: U.S. Preventive Services Task Force recommendation statement. Pediatrics. 2014;133(6):1102-1111.
Clark MB, Slayton RL American Academy of Pediatrics Section on Oral Health. Fluoride use in caries prevention in the primary care setting. Pediatrics. 2014;134(3):626-633.
Siu AL. Screening for speech and language delay and disorders in children aged 5 years and younger: U.S. Preventive Services Task Force recommendation statement. Pediatrics. 2015;136(2):e474-e481.
Council on Children with Disabilities, Section on Developmental Behavioral Pediatrics, Bright Futures Steering Committee, Medical Home Initiatives for Children with Special Needs Project Advisory Committee. Identifying infants and young children with developmental disorders in the medical home: an algorithm for developmental surveillance and screening [published correction appears in Pediatrics . 2006;118(4):1808–1809]. Pediatrics. 2006;118(1):405-420.
Bibbins-Domingo K, Grossman DC, Curry SJ, et al. Screening for lipid disorders in children and adolescents: U.S. Preventive Services Task Force recommendation statement. JAMA. 2016;316(6):625-633.
National Heart, Lung, and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents. October 2012. https://www.nhlbi.nih.gov/sites/default/files/media/docs/peds_guidelines_full.pdf . Accessed May 9, 2018.
Moyer VA. Screening for primary hypertension in children and adolescents: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2013;159(9):613-619.
Flynn JT, Kaelber DC, Baker-Smith CM, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents [published correction appears in Pediatrics . 2017;140(6):e20173035]. Pediatrics. 2017;140(3):e20171904.
Siu AL. Screening for iron deficiency anemia in young children: USPSTF recommendation statement. Pediatrics. 2015;136(4):746-752.
U.S. Preventive Services Task Force. Screening for elevated blood lead levels in children and pregnant women. Pediatrics. 2006;118(6):2514-2518.
Screening Young Children for Lead Poisoning: Guidance for State and Local Public Health Officials . Atlanta, Ga.: U.S. Public Health Service; Centers for Disease Control and Prevention; National Center for Environmental Health; 1997.
O'Connor E, Rossom RC, Henninger M, Groom HC, Burda BU. Primary care screening for and treatment of depression in pregnant and post-partum women: evidence report and systematic review for the U.S. Preventive Services Task Force. JAMA. 2016;315(4):388-406.
Earls MF Committee on Psychosocial Aspects of Child and Family Health, American Academy of Pediatrics. Incorporating recognition and management of perinatal and postpartum depression into pediatric practice. Pediatrics. 2010;126(5):1032-1039.
Siu AL. Screening for depression in children and adolescents: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2016;164(5):360-366.
Weitzman C, Wegner L American Academy of Pediatrics Section on Developmental and Behavioral Pediatrics; Committee on Psychosocial Aspects of Child and Family Health; Council on Early Childhood; Society for Developmental and Behavioral Pediatrics; American Academy of Pediatrics. Promoting optimal development: screening for behavioral and emotional problems [published correction appears in Pediatrics . 2015;135(5):946]. Pediatrics. 2015;135(2):384-395.
Grossman DC, Curry SJ, Owens DK, et al. Vision screening in children aged 6 months to 5 years: U.S. Preventive Services Task Force recommendation statement. JAMA. 2017;318(9):836-844.
Donahue SP, Nixon CN Committee on Practice and Ambulatory Medicine, Section on Ophthalmology, American Academy of Pediatrics; American Association of Certified Orthoptists, American Association for Pediatric Ophthalmology and Strabismus, American Academy of Ophthalmology. Visual system assessment in infants, children, and young adults by pediatricians. Pediatrics. 2016;137(1):28-30.
Lin KW. What to do at well-child visits: the AAFP's perspective. Am Fam Physician. 2015;91(6):362-364.
American Academy of Pediatrics Council on Community Pediatrics. Poverty and child health in the United States. Pediatrics. 2016;137(4):e20160339.
Lavigne JV, Lebailly SA, Hopkins J, Gouze KR, Binns HJ. The prevalence of ADHD, ODD, depression, and anxiety in a community sample of 4-year-olds. J Clin Child Adolesc Psychol. 2009;38(3):315-328.
American Academy of Pediatrics Committee on Practice and Ambulatory Medicine, Section on Ophthalmology, American Association of Certified Orthoptists, American Association for Pediatric Ophthalmology and Strabismus, American Academy of Ophthalmology. Visual system assessment of infants, children, and young adults by pediatricians. Pediatrics. 2016;137(1):28-30.
American Academy of Family Physicians. Clinical preventive service recommendation. Immunizations. http://www.aafp.org/patient-care/clinical-recommendations/all/immunizations.html . Accessed October 5, 2017.
Centers for Disease Control and Prevention. Recommended immunization schedule for children and adolescents aged 18 years or younger, United States, 2018. https://www.cdc.gov/vaccines/schedules/hcp/child-adolescent.html . Accessed May 9, 2018.
National Center for Injury Prevention and Control. 10 leading causes of death by age group, United States—2015. https://www.cdc.gov/injury/images/lc-charts/leading_causes_of_death_age_group_2015_1050w740h.gif . Accessed April 24, 2017.
Durbin DR American Academy of Pediatrics Committee on Injury, Violence, and Poison Prevention. Child passenger safety. Pediatrics. 2011;127(4):788-793.
American Academy of Pediatrics Committee on Injury and Poison Prevention. Reducing the number of deaths and injuries from residential fires. Pediatrics. 2000;105(6):1355-1357.
Gardner HG American Academy of Pediatrics Committee on Injury, Violence, and Poison Prevention. Office-based counseling for unintentional injury prevention. Pediatrics. 2007;119(1):202-206.
American Academy of Pediatrics Committee on Injury, Violence, and Poison Prevention. Prevention of drowning in infants, children, and adolescents. Pediatrics. 2003;112(2):437-439.
American Academy of Pediatrics Committee on Injury and Poison Prevention. Injuries associated with infant walkers. Pediatrics. 2001;108(3):790-792.
American Academy of Pediatrics Committee on Injury and Poison Prevention. Falls from heights: windows, roofs, and balconies. Pediatrics. 2001;107(5):1188-1191.
Dowd MD, Sege RD Council on Injury, Violence, and Poison Prevention Executive Committee; American Academy of Pediatrics. Firearm-related injuries affecting the pediatric population. Pediatrics. 2012;130(5):e1416-e1423.
American Academy of Pediatrics Committee on Injury, Violence, and Poison Prevention. Prevention of choking among children. Pediatrics. 2010;125(3):601-607.
Kendrick D, Young B, Mason-Jones AJ, et al. Home safety education and provision of safety equipment for injury prevention (review). Evid Based Child Health. 2013;8(3):761-939.
American Academy of Pediatrics Section on Oral Health. Maintaining and improving the oral health of young children. Pediatrics. 2014;134(6):1224-1229.
Heyman MB, Abrams SA American Academy of Pediatrics Section on Gastroenterology, Hepatology, and Nutrition Committee on Nutrition. Fruit juice in infants, children, and adolescents: current recommendations. Pediatrics. 2017;139(6):e20170967.
Council on Communications and Media. Media and young minds. Pediatrics. 2016;138(5):e20162591.
Moon RY Task Force on Sudden Infant Death Syndrome. SIDS and other sleep-related infant deaths: evidence base for 2016 updated recommendations for a safe infant sleeping environment. Pediatrics. 2016;138(5):e20162940.
American Academy of Pediatrics Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics. 2012;129(3):e827-e841.
Wagner CL, Greer FR American Academy of Pediatrics Section on Breastfeeding; Committee on Nutrition. Prevention of rickets and vitamin D deficiency in infants, children, and adolescents [published correction appears in Pediatrics . 2009;123(1):197]. Pediatrics. 2008;122(5):1142-1152.
Huh SY, Rifas-Shiman SL, Taveras EM, Oken E, Gillman MW. Timing of solid food introduction and risk of obesity in preschool-aged children. Pediatrics. 2011;127(3):e544-e551.
Greer FR, Sicherer SH, Burks AW American Academy of Pediatrics Committee on Nutrition; Section on Allergy and Immunology. Effects of early nutritional interventions on the development of atopic disease in infants and children: the role of maternal dietary restriction, breastfeeding, timing of introduction of complementary foods, and hydrolyzed formulas. Pediatrics. 2008;121(1):183-191.
American Academy of Pediatrics Committee on Nutrition. The use of whole cow's milk in infancy. Pediatrics. 1992;89(6 pt 1):1105-1109.
Fleischer DM, Spergel JM, Assa'ad AH, Pongracic JA. Primary prevention of allergic disease through nutritional interventions. J Allergy Clin Immunol Pract. 2013;1(1):29-36.
Grossman DC, Bibbins-Domingo K, Curry SJ, et al. Screening for obesity in children and adolescents: U.S. Preventive Services Task Force recommendation statement. JAMA. 2017;317(23):2417-2426.
Daniels SR, Hassink SG Committee on Nutrition. The role of the pediatrician in primary prevention of obesity. Pediatrics. 2015;136(1):e275-e292.
American Academy of Family Physicians. Physical activity in children. https://www.aafp.org/about/policies/all/physical-activity.html . Accessed January 1, 2018.
Continue Reading

More in AFP
More in pubmed.
Copyright © 2018 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
- Skip to main content
Child well visits, birth to 15 months
- Child well visit checklist
- Quiz: Child well-being and immunizations
Checking in: Questions to ask at your child's well visits
Welcoming a new child is exciting. But caring for a baby can also leave you with a lot of unanswered questions. Your baby’s care provider can help. From giving immunizations to offering you feeding tips, care providers help your baby grow up healthy. That includes making sure you have the answers and support you need.

A note about immunizations at child well visits
Your child’s care provider will give your baby immunizations during most visits. Immunizations work better and reduce the risk of infection by working with the body's natural defenses to help safely develop immunity to disease. Keeping your baby on schedule is also key, so don’t forget to schedule visits on time.
Learn what to ask at your child's well visits
Preparation is key for a stress-free appointment. Your baby should go to at least 8 child well visits before they are 15 months old. Knowing what will happen at each of these appointments can help you get ready. Knowing what to pack for your visit and questions you might ask when you get there can make your life easier. Watch the videos and view the questions below to get ready for each early child well visit.
Child Well Visits: Newborn
Video transcript.
Screen 1: What to expect at your baby’s appointment – Newborn
Screen 2: Your newborn will need a checkup before going home.
Screen 3: What to expect before you leave the hospital:
- Physical checkup (measurements, vitals).
- Screenings: Critical congenital heart defect, vision, hearing, newborn bilirubin, blood (check for disorders).
- Developmental and behavioral assessment.
- Immunizations: HepB.
Screen 4: Before you leave:
- Make sure your contact information is current.
- Schedule your next appointment.
Screen 5: In light of COVID-19, remember to practice social distancing at your well-child visits. Wash your hands often and wear a mask. Contact your care provider with questions about your visit.
Screen 6: UnitedHealthcare Logo
Your newborn will need a checkup before going home from the hospital. Watch the video to learn what screenings and immunizations you can expect at your child’s first appointment.
3 to 5-day visit
Child well visits: 3 to 5-day visit.
Screen 1: What to expect at your baby’s appointment – 3-5 Days
Screen 2: Early well-child visits and immunizations set your baby up for a healthy future.
Screen 3: What to expect at your child’s appointment:
- Physical checkup: Measurements, vitals.
- Umbilical cord examination.
- Screenings: Vision, hearing, blood (check for disorders).
- Review screenings done at birth.
Screen 4: You’ll also talk about if baby can:
- Suck to eat
- Grasp your finger
- React when startled
Screen 5: Before you leave:
Screen 6: In light of COVID-19, remember to practice social distancing at your well-child visits. Wash your hands often and wear a mask. Contact your care provider with questions about your visit.
UnitedHealthcare Logo
Watch the video to get an idea of what to expect at your appointment
In addition, here are some questions you may want to ask:
- How can I keep my baby comfortable and safe from seasonal weather?
- What can I do to make breastfeeding more comfortable for me and baby?
- When will my baby gain more weight?
- Should I always put my baby to sleep on their back?
- How do I care for my baby’s umbilical cord?
- How often should my baby get a bath?
- How do I calm and soothe my baby?
1-month visit
Child well visits: 1 month appointment.
Screen 1: What to expect at your baby’s appointment – 1 Month
- Immunizations: HepB.
- Postpartum depression screening (for mothers).
- Raise hands
- Focus on your face
Screen 7: UnitedHealthcare Logo
- When will my baby sleep through the night?
- What should I do for the peeling skin on my baby’s head?
- How do I care for my infant's skin?
- What is a normal number of wet or soiled diapers I should change every day?
- Are there programs to help me buy formula or breast pumps?
2-month visit
Child well visits: 2 month appointment.
Screen 1: What to expect at your baby’s appointment – 2 Months
- Physical checkup: (measurements, vitals).
- Screenings: Vision, hearing.
- Immunizations: DTaP, Hib, IPV, RV, HepB, PCV13.
- Developmental assessment.
- Turn and lift head
- Kick while laying on back
- Notice hands
- Follow objects with eyes
- How often should my baby be eating?
- Should I be using formula in addition to breastfeeding?
- How can I keep my baby comfortable after immunizations?
- How can I find childcare I can trust?
- When should I stop swaddling my baby?
- I’ve been feeling sad and anxious since delivering my baby. What should I do?
- What is “tummy time”?
4-month visit
Child well visits: 4 month appointment.
Screen 1: What to expect at your baby’s appointment – 4 Months
- Roll onto tummy
- Reach for objects
- Watch an object move
- Laugh and giggle
Screen 7: UnitedHealthcare Logo
- Is Tylenol safe to give my baby for a fever?
- How can I help my baby have healthy teeth?
- How can I soothe my baby during teething?
- How can we begin to create a sleeping routine?
- How long should my baby spend doing “tummy time” each day?
- How long should my baby nap each day?
6-month visit
Child well visits: 6 month appointment.
Screen 1: What to expect at your baby’s appointment – 6 Months
- Screenings: Vision, hearing, oral health.
- Immunizations: DTaP, Hib, IPV, RV, HepB, PCV13, IIV.
- Roll in both directions
- Play with toes
- Hold a bottle
- Sit with good head control
- When and how should I introduce foods other than breastmilk or formula?
- How can I wean my baby off night feedings?
- How long should my baby use a pacifier?
- Can my baby sleep with a favorite blanket or toy?
- When can my baby start drinking from a sippy cup?
9-month visit
Child well visits: 9 month appointment.
Screen 1: What to expect at your baby’s appointment – 9 Months
- Screenings: Vision, hearing, anemia, lead, oral health.
- Immunizations: IIV.
- Sit unassisted
- Crawl and pull up to stand
- Work to get toys that are out of reach
- I think my baby is behind in development (e.g., crawling). What can I do to help?
- What do I need to babyproof in my home once my baby can crawl?
- Should I be brushing my baby’s new teeth?
- How long should my baby be sleeping at night?
- How long should I let my baby cry at night?
12-month visit
Child well visits: 12 month appointment.
Screen 1: What to expect at your baby’s appointment – 12 Months
- Screenings: Vision, hearing, lead, oral health.
- Immunizations: MMR, HepA, Varicella, PCV13, IIV.
- Walk while holding onto something
- Use gestures to get things
- Eat solid foods with fingers
- Say more than one word
- Respond to name
- What should I do when baby pulls my hair or bites?
- Are my baby’s sleep patterns normal?
- How can I treat diaper rash?
- What can I do about sore arms and back from holding my baby?
- Should my baby nap at the same time each day?
- How do I keep my child safe as they learn to walk and explore?
15-month visit
Child well visits: 15 month appointment.
Screen 1: What to expect at your baby’s appointment – 15 Months
- Immunizations: DTaP, Hib, IIV.
- Walk and run
- Squat and stand back up
- Throw or kick a ball
- Point for things
- When should my baby switch from a crib to a bed?
- How much juice or milk should my baby be drinking?
- Should my baby have screen time?
- When should my baby go to the dentist?
- When should I switch to a front-facing car seat?
Wellness visits are also important for your child after 15 months
As your child grows, it’s important to continue to have regular checkups with your health care provider. You can view checklists for preventive care visits at every age, from 1 month to adulthood.
Looking for resources to help support you and your child?
- Most health insurance plans cover early child well visits or provide assistance. Call the number on your insurance card for more details.
- If you are a UnitedHealthcare Community Plan member, you may have access to our Healthy First Steps program , which can help you find a care provider, schedule well-child visits, connect with educational and community resources and more. To get started, call 1-800-599-5985 , TTY 711, Monday through Friday, from 8 a.m. to 5 p.m. 1
- If you need help getting to an appointment, or getting formula or healthy food, call the number on your insurance card.
- If you are having a hard time getting food or are experiencing unemployment, your care provider may be able to connect you with resources that can help.
Related content
- Preventive care
More like this:
- What’s preventive care and what’s covered?
- Children's health
Skip to content
Why Well-Child Visits Matter
Published on May 02, 2023
Primary Care Locations
Don't fall behind on your child's routine care — a minor issue today could become a major problem tomorrow.

Well-child visits allow your pediatrician to examine your child holistically, assess their physical and emotional needs, support their growth and development, and intervene quickly if any issues arise.
What are the risks of skipping well-child visits?
If your child is healthy, it can be easy to let well visits fall by the wayside. While those annual checkups may seem like just another thing to fit into your family’s hectic schedule, they play a crucial role in preventing future problems.
Find a CHOP Pediatrician
CHOP Primary Care practices, located throughout southeastern Pennsylvania and Southern New Jersey, provide convenient access to primary health and wellness services for children close to home.
Well visits are essential to ensure your child gets the required vaccinations to attend school, go to daycare and participate in sports. Visiting the pediatrician when your child is well also provides you with an opportunity to ask questions – and get expert answers – about your child’s health, development and well-being. Delaying these visits can put your child at greater risk of illness or delay needed interventions. For example, many common developmental delays are discovered during routine checkups with pediatricians – early intervention makes a big difference in getting your child the support they need before something small turns into a bigger issue.
What to expect at a well-child visit
During an annual wellness visit, your child's pediatrician will:
- Determine if your child is meeting growth and developmental milestones for their age.
- Evaluate your child's vision and hearing for anything out of the ordinary – it's important to catch these issues early.
- Ask about sudden changes in your child's usual activities, mood and overall health.
- Assess your child's mental health, and ask questions about how they are coping with school, friends, family and any other outside influences.
- Provide immunizations for childhood diseases and common conditions that affect children or young adults, such as measles and HPV.
- Give sports physicals to children who want to want to participate in competitive sports at school or in the community.
- Get to know your child: their diet, sleeping patterns, nutrition, social interactions, behavior and stress levels
- Help your child establish healthy habits and provide tips for families to reinforce these at home.
- Provide age- and behavior-based counseling for teens on topics such as driver safety, depression and drug or alcohol use.
- Check in on how your family is doing and identify any supportive resources or advice related to navigating daily life.
What are the ages for well-child visits?
A standard well-child visit schedule spans from infancy through adolescence, and includes checkups at the following ages:
- In your baby’s first year: Newborn visit (3-5 days after birth), at 1 month old, 2 months, 4 months, 6 months, 9 months, and at 12 months
- 11-14 years
- 15-17 years
- 18-21 years
Your pediatrician can be a trusted partner at every age and stage of your child’s development.
Contributed by: Lisa Biggs, MD
Stay in Touch
Are you looking for advice to keep your child healthy and happy? Do you have questions about common childhood illnesses and injuries? Subscribe to our Health Tips newsletter to receive health and wellness tips from the pediatric experts at Children's Hospital of Philadelphia, straight to your inbox. Read some recent tips .

With our patient portal you can schedule appointments, access records, see test results, ask your care provider questions, and more.

Subscribe to Health Tips
Subscribe to our Health Tips enewsletter to receive health and wellness tips from the pediatric experts at CHOP.
You Might Also Like

A Dose of Prevention
Learn why vaccinations are important for kids and the community, and what to do if you missed a vaccine and need to get back on track.

Preparing for an Annual Well Visit
Being properly prepared for annual well visits is a great way to get the most out of each appointment with your pediatrician.
How to Have a Productive Video Visit
If your child is scheduled for an online doctor’s appointment, read these tips to get the most out of your visit.
Internet Explorer Alert
It appears you are using Internet Explorer as your web browser. Please note, Internet Explorer is no longer up-to-date and can cause problems in how this website functions This site functions best using the latest versions of any of the following browsers: Edge, Firefox, Chrome, Opera, or Safari . You can find the latest versions of these browsers at https://browsehappy.com
- Publications
- HealthyChildren.org
Shopping cart
Order Subtotal
Your cart is empty.
Looks like you haven't added anything to your cart.
- Career Resources
- Philanthropy
- About the AAP
- Safe Administration of Medication in School: Policy Statement
- Policy Outlines Steps to Take When Students Need Medicine at School
- When Your Child Needs to Take Medication at School
- American Academy of Pediatrics Updates Guidance on Medication Administration In School
- News Releases
- Policy Collections
- The State of Children in 2020
- Healthy Children
- Secure Families
- Strong Communities
- A Leading Nation for Youth
- Transition Plan: Advancing Child Health in the Biden-Harris Administration
- Health Care Access & Coverage
- Immigrant Child Health
- Gun Violence Prevention
- Tobacco & E-Cigarettes
- Child Nutrition
- Assault Weapons Bans
- Childhood Immunizations
- E-Cigarette and Tobacco Products
- Children’s Health Care Coverage Fact Sheets
- Opioid Fact Sheets
- Advocacy Training Modules
- Subspecialty Advocacy Report
- AAP Washington Office Internship
- Online Courses
- Live and Virtual Activities
- National Conference and Exhibition
- Prep®- Pediatric Review and Education Programs
- Journals and Publications
- NRP LMS Login
- Patient Care
- Practice Management
- AAP Committees
- AAP Councils
- AAP Sections
- Volunteer Network
- Join a Chapter
- Chapter Websites
- Chapter Executive Directors
- District Map
- Create Account

- Materials & Tools
- Clinical Practice
- States & Communities
- Quality Improvement
- Implementation Stories
Well-Child Visits: Parent and Patient Education
The Bright Futures Parent and Patient Educational Handouts help guide anticipatory guidance and reinforce key messages (organized around the 5 priorities in each visit) for the family. Each educational handout is written in plain language to ensure the information is clear, concise, relevant, and easy to understand. Each educational handout is available in English and Spanish (in HTML and PDF format). Beginning at the 7 year visit , there is both a Parent and Patient education handout (in English and Spanish).
For the Bright Futures Parent Handouts for well-child visits up to 2 years of age , translations of 12 additional languages (PDF format) are made possible thanks to the generous support of members, staff, and businesses who donate to the AAP Friends of Children Fund . The 12 additional languages are Arabic, Bengali, Chinese, French, Haitian Creole, Hmong, Korean, Polish, Portuguese, Russian, Somali, and Vietnamese.
Reminder for Health Care Professionals: The Bright Futures Tool and Resource Kit, 2nd Edition is available as an online access product. For more detailed information about the Toolkit, visit shop.aap.org . To license the Toolkit to use the forms in practice and/or incorporate them into an Electronic Medical Record System, please contact AAP Sales .
Parent Educational Handouts
Infancy visits.

3 to 5 Day Visit
1 Month Visit
2 Month Visit
4 Month Visit
6 Month Visit
9 Month Visit
Early childhood visits.
12 Month Visit
15 Month Visit
18 Month Visit
2 Year Visit
2.5 Year Visit
3 Year Visit
4 Year Visit
Parent and patient educational handouts, middle childhood visits.
5-6 Year Visit
7-8 Year Visit
7-8 Year Visit - For Patients
9-10 Year Visit
9-10 Year Visit - For Patients
Adolescent visits.
11-14 Year Visit
11-14 Year Visit - For Patients
15-17 Year Visit

15-17 Year Visit - For Patients

18-21 Year Visit - For Patients
Last updated.
American Academy of Pediatrics
Doctor Visits
Make the Most of Your Teen’s Visit to the Doctor (Ages 15 to 17 Years)

Take Action
Teens ages 15 to 17 years need to go to the doctor or nurse for a “well-child visit” once a year.
A well-child visit is when you take your teen to the doctor to make sure they’re healthy and developing normally. This is different from other visits for sickness or injury.
At a well-child visit, the doctor or nurse can help catch any problems early, when they may be easier to treat.
Learn what to expect so you can make the most of each visit.
Child Development
How do i know if my teen is growing and developing on schedule.
Your teen’s doctor or nurse can help you identify “developmental milestones,” or signs to look for that show your teen is developing normally. This is an important part of the well-child visit.
Some developmental milestones are related to your teen’s behavior and learning, and others are about physical changes in your teen’s body.
See a complete list of developmental milestones for your teen .
Behavior Changes
What are some changes i might see in my teen’s behavior.
Developmental milestones for teens ages 15 to 17 years include:
- Spending less time with family and more time with friends
- Worrying more about the future (like going to college or finding a job)
- Thinking more about romantic relationships and sex
- Trying new things like new sports or hobbies — or possibly experimenting with tobacco, alcohol, or drugs
This is also a time when some teens may start showing signs of depression, anxiety, or eating disorders. That’s why it’s important to:
- Make sure the doctor screens your teen for depression
- Have your teen screened for anxiety
Physical Changes
What are some physical changes my teen is going through.
Teens ages 15 to 17 years may be nearing the end of puberty. Puberty is when a child’s body develops into an adult’s body.
- Get more information about puberty to share with your daughter
- Get more information about puberty to share with your son
Teens might not ask you questions about sex, their bodies, or relationships. That’s why it’s a good idea for you to start the conversation. You can also encourage your teen to ask the doctor or nurse any questions they have about body changes or other health concerns.
Learn how to talk with your teen about sex .
Take these steps to help you and your teen get the most out of well-child visits.
Gather important information.
Take any medical records you have to the appointment, including a record of vaccines (shots) your teen has received.
Make a list of any important changes in your teen’s life since the last visit, like a:
- New brother or sister
- Separation or divorce — or a parent spending time in jail or prison
- New school or a move to a new neighborhood
- Serious illness or death of a friend or family member
Use this tool to keep track of your teen’s family health history .

Help your teen get more involved in visits to the doctor.
The doctor will probably ask you to leave the room during part of the visit, usually the physical exam. This lets your teen develop a relationship with the doctor or nurse and ask questions in private. It’s an important step in teaching your teen to take control of their health care.
Your teen can also:
- Call to schedule appointments
- Help you fill out medical forms
- Write down questions for the doctor or nurse
For more ideas, check out these tips to help teens take charge of their health care . You can also share this list of questions for the doctor with your teen .
What about cost?
Under the Affordable Care Act, insurance plans must cover well-child visits. Depending on your insurance plan, you may be able to get well-child visits at no cost to you. Check with your insurance company to find out more.
Your teen may also qualify for free or low-cost health insurance through Medicaid or the Children’s Health Insurance Program (CHIP). Learn about coverage options for your family.
If you don’t have insurance, you may still be able to get free or low-cost well-child visits. Find a health center near you and ask about well-child visits.
To learn more, check out these resources:
- Free preventive care for children covered by the Affordable Care Act
- How the Affordable Care Act protects you and your family
- Understanding your health insurance and how to use it [PDF - 698 KB]
Ask Questions
Make a list of questions you want to ask the doctor..
Before the well-child visit, write down 3 to 5 questions you have. This visit is a great time to ask the doctor or nurse any questions about:
- A health condition your teen has (like acne or asthma)
- Changes in your teen’s behavior or mood
- Loss of interest in favorite activities
- Tobacco, alcohol, or drug use
- Problems at school (like learning challenges or not wanting to go to school)
Here are some questions you may want to ask:
- Is my teen up to date on vaccines?
- How can I make sure my teen is getting enough physical activity?
- How can I help my family eat healthy?
- How can I help my teen succeed at school?
- How can our family set rules more effectively?
- How can I help my teen become a safe driver?
- How can I talk with my teen about tobacco, alcohol, and drugs?
Take a notepad, smartphone, or tablet and write down the answers so you can remember them later.
Ask what to do if your teen gets sick.
Make sure you know how to get in touch with a doctor or nurse when the office is closed. Ask how to get hold of the doctor on call, or if there's a nurse information service you can call at night or on the weekend.
What to Expect
Know what to expect..
During each well-child visit, the doctor or nurse will ask you questions, do a physical exam, and update your teen’s medical history. You and your teen will also be able to ask your questions and discuss any problems.
The doctor or nurse will ask your teen questions.
The doctor or nurse may ask about:
- Behavior — Do you have trouble following directions at home or at school?
- Health — Do you often get headaches or have other kinds of pain?
- Safety — Do you always wear a seatbelt in the car? Do you and your friends use tobacco, alcohol, or drugs?
- School and activities — Do you look forward to going to school? What do you like to do after school?
- Family and friends — Have there been any changes in your family recently? Do you have close friends?
- Emotions — Do you often feel sad or bored? Do you often feel scared or very worried? Is there someone you trust who you can talk to about problems?
- Sexuality — Do you have any questions about your body? Have you talked with your parents about dating and sex? Are you dating anyone now?
- The future — Have you started to think about what you want to do after high school?
The answers to questions like these will help the doctor or nurse make sure your teen is healthy, safe, and developing normally.
Physical Exam
The doctor or nurse will also check your teen’s body..
To check your teen’s body, the doctor or nurse will:
- Measure height and weight and figure out your teen's body mass index (BMI)
- Check your teen’s blood pressure
- Check your teen's vision and hearing
- Check your teen’s body parts (called a physical exam)
- Decide if your teen needs any lab tests, like a blood test
- Give your teen vaccines they need
Behavior and Emotions
The doctor or nurse will pay special attention to signs of certain issues. .
The doctor or nurse will offer additional help if your teen may:
- Be depressed
- Have anxiety
- Struggle with an eating disorder
- Use tobacco, alcohol, or other drugs
- Experience any kind of violence
And if your teen may be having sex, the doctor or nurse will talk about preventing STIs (sexually transmitted infections) — also called STDs (sexually transmitted diseases) — and pregnancy. Learn how to talk with your teen about preventing STIs .
The doctor or nurse will make sure you and your teen have the resources you need.
This may include telling you and your teen about:
- Websites or apps that have helpful health information
- Organizations in your community where you can go for help
If needed, the doctor or nurse may also refer your teen to a specialist.
Content last updated February 16, 2024
Reviewer Information
This information on well-child visits was adapted from materials from the Centers for Disease Control and Prevention and the National Institutes of Health.
Reviewed by: Sara B. Kinsman, M.D., Ph.D. Director, Division of Child, Adolescent and Family Health Maternal and Child Health Bureau Health Resources and Services Administration
You may also be interested in:

Talk to Your Kids About Tobacco, Alcohol, and Drugs

Talk to Your Kids About Sex and Healthy Relationships

Get Your Teen Screened for Depression
The office of disease prevention and health promotion (odphp) cannot attest to the accuracy of a non-federal website..
Linking to a non-federal website does not constitute an endorsement by ODPHP or any of its employees of the sponsors or the information and products presented on the website.
You will be subject to the destination website's privacy policy when you follow the link.
Preventive Health Care Visits in Infants
Healthy infants should be seen by their doctor often during the first year of life. Preventive health care visits (also called well-child visits) typically take place within a few days after birth or by 2 weeks of age and at 1, 2, 4, 6, and 9 months of age. During these visits, the doctor uses age-specific guidelines to monitor the infant's growth and development and asks the parents questions about various developmental milestones (see table Developmental Milestones From Birth to Age 12 Months ). Tests are sometimes done, and during many visits, the doctor vaccinates the infant against various illnesses (see Childhood Vaccination Schedule ).
Health care visits also allow the doctor to educate the parents about eating, sleeping, behavior, child safety, nutrition, exercise, and good health habits. In addition, the doctor advises the parents what developmental changes to expect in their infant by the next visit.
Examination
The infant's length and height , weight , and head circumference are measured at every visit. The doctor examines the infant for various abnormalities, including signs of hereditary disorders or birth defects .
The eyes are examined, and vision is tested. Infants who were born very prematurely (before the completion of 32 weeks of development in the uterus) usually need more frequent eye examinations by an eye specialist to look for retinopathy of prematurity , which is an eye disease that occurs when infants are born before the blood vessels in their eyes are fully developed and may result in blindness, and for the development of refractive errors , which result in blurring of vision. These disorders are more common among infants who were born very prematurely.
The doctor checks the infant’s hips for signs that the hip joints are loose or dislocated ( developmental dysplasia of the hip ). The doctor checks the infant's teeth , if they are present, for cavities and the mouth for thrush , which is a common yeast infection among infants.
The doctor also examines the heart, lungs, abdomen, arms and legs, and genitals.
Screening tests are done to assess whether infants are at risk of certain disorders.
Blood tests are done to detect anemia , sickle cell disease , and exposure to lead .
Hearing tests are done shortly after birth to determine whether an infant has a hearing disorder or hearing loss (see Newborn Screening Tests ) and are repeated later if new concerns about the infant's hearing develop (see also Hearing Impairment in Children ).
Infants are screened for tuberculosis (TB) risk factors with a questionnaire at all well-child visits, usually beginning in infancy. Risk factors include exposure to TB, being born in or having traveled to areas of the world where TB is common (countries other than the United States, Canada, Australia, and New Zealand and Western and North European countries), having a family member with TB, and having parents or close contacts who are recent immigrants from an area where TB is common or who have recently been in jail. Those with risk factors usually have tuberculosis screening tests done.
At these visits, the doctor gives parents age-appropriate safety guidelines.
The following safety guidelines apply to infants from birth to age 12 months:
Use a rear-facing car seat and place it in the back seat of the vehicle.
Set the hot water heater to 120° F or less.
Prevent falls from changing tables and around stairs.
Place infants on their back to sleep on a firm, flat mattress for every sleep, do not share a bed, and do not place pillows, bumper pads, nonfitted sheets, stuffed animals or other toys, quilts, comforters, or weighted or loose blankets in the crib. (See also sidebar Safe to Sleep: Reducing the Risk of SIDS .)
Do not give infants foods and objects that can cause choking or be inhaled into the lungs.
Do not use baby walkers.
Place safety latches on cabinets and cover electrical outlets.
Remain alert when watching infants in the bathtub or near a pool or any body of water and when they are learning to walk.

Image courtesy of the Centers for Disease Control and Prevention (CDC), National Center for Injury Prevention and Control ( Transportation Safety Resources ). This guidance from the CDC is for the United States, and regulations may differ in other countries.

Nutrition and exercise
For infants, recommendations for nutrition are based on age. The doctor can help parents weigh the benefits of breastfeeding versus formula-feeding and give guidance regarding solid foods .
Parents should provide infants with a safe environment they can roam in and explore. Outdoor play should be encouraged from infancy.
Screen time (for example, television, video games, cell phones and other handheld devices, and noneducational computer time) may result in inactivity and obesity. Limits on the time a child spends using devices with screens should start at birth and be maintained throughout adolescence.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

- Health Topics
- Drugs & Supplements
- Medical Tests
- Medical Encyclopedia
- About MedlinePlus
- Customer Support
Well-child visits
Childhood is a time of rapid growth and change. Children have more well-child visits when they are younger. This is because development is faster during these years.
Each visit includes a complete physical exam. At this exam, the health care provider will check the child's growth and development in order to find or prevent problems.
The provider will record your child's height, weight, and other important information. Hearing, vision, and other screening tests will be part of some visits. So will immunizations.
Even if your child is healthy, well-child visits are a good time to focus on your child's wellness. Talking about ways to improve care and prevent problems helps keep your child healthy.
Information
At your well-child visits, you will get information on topics such as:
- Childhood diseases
- What to expect as your child grows
Write down your questions and concerns and bring them with you. This will help you get the most out of the visit.
Your provider will pay special attention to how your child is growing compared to normal developmental milestones. Your child's height, weight, and head circumference are recorded on a growth chart . This chart remains part of your child's medical record. Talking about your child's growth is a good place to begin a discussion about your child's general health. Ask your provider about the body mass index (BMI) curve, which is the most important tool for identifying and preventing obesity.
Your provider will also talk about other wellness topics such as family relationship issues, school, and access to community services.
There are several schedules for routine well-child visits. One schedule, recommended by the American Academy of Pediatrics, is given below.
PREVENTIVE HEALTH CARE SCHEDULE
A visit with a provider before the baby is born can be particularly important for:
- First-time parents.
- Parents with a high-risk pregnancy.
- Any parent who has questions about issues such as feeding, circumcision , and general child health issues.
After the baby is born, the next visit should be 2 to 3 days after bringing the baby home (for breastfed babies) or when the baby is 2 to 4 days old (for all babies who are released from a hospital before they are 2 days old). Some providers will delay the visit until the baby is 1 to 2 weeks old for parents who have had babies before.
After that, it is recommended that visits occur at the following ages (your provider may have you add or skip visits depending on your child's health or your parenting experience):
- 2 1/2 years
- Each year after that until age 21
Also, you should call or visit a provider any time your baby or child seems ill or whenever you are worried about your baby's health or development.
RELATED TOPICS
Elements of the physical exam:
- Auscultation (listening to heart, breath, and stomach sounds)
- Heart sounds
- Infantile reflexes and deep tendon reflexes as the child gets older
- Neonatal jaundice -- first few visits only
- Standard ophthalmic exam
- Temperature measurement (see also normal body temperature )
Immunization information:
- Immunizations -- general overview
- Babies and shots
- Diphtheria immunization (vaccine)
- DPT immunization (vaccine)
- Hepatitis A immunization (vaccine)
- Hepatitis B immunization (vaccine)
- Hib immunization (vaccine)
- Human papilloma virus (vaccine)
- Influenza immunization (vaccine)
- Meningococcal (meningitis) immunization (vaccine)
- MMR immunization (vaccine)
- Pertussis immunization (vaccine)
- Pneumococcal immunization (vaccine)
- Polio immunization (vaccine)
- Rotavirus immunization (vaccine)
- Tetanus immunization (vaccine)
- TdaP immunization (vaccine)
- Varicella (chickenpox) immunization (vaccine)
Nutrition advice:
- Appropriate diet for age -- balanced diet
- Breastfeeding
- Diet and intellectual development
- Fluoride in diet
- Infant formulas
- Obesity in children
Growth and development schedules:
- Infant -- newborn development
- Toddler development
- Preschooler development
- School-age child development
- Adolescent development
- Developmental milestones
- Developmental milestones record -- 2 months
- Developmental milestones record -- 4 months
- Developmental milestones record -- 6 months
- Developmental milestones record -- 9 months
- Developmental milestones record -- 12 months
- Developmental milestones record -- 18 months
- Developmental milestones record -- 2 years
- Developmental milestones record -- 3 years
- Developmental milestones record -- 4 years
- Developmental milestones record -- 5 years
Preparing a child for an office visit is similar to test and procedure preparation.
Preparation steps differ, depending on the child's age:
- Infant test/procedure preparation
- Toddler test/procedure preparation
- Preschooler test/procedure preparation
- School-age test/procedure preparation

Hagan JF Jr, Navsaria D. Maximizing children's health: screening, anticipatory guidance, and counseling. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics . 21st ed. Philadelphia, PA: Elsevier; 2020:chap 12.
Kelly DP, Natale MJ. Neurodevelopmental and executive function and dysfunction. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics . 21st ed. Philadelphia, PA: Elsevier; 2020:chap 48.
Kimmel SR, Ratliff-Schaub K. Growth and development. In: Rakel RE, Rakel DP, eds. Textbook of Family Medicine . 9th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 22.
Review Date 1/24/2023
Updated by: Neil K. Kaneshiro, MD, MHA, Clinical Professor of Pediatrics, University of Washington School of Medicine, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Related MedlinePlus Health Topics
- Baby Health Checkup
- Children's Health
- Health Checkup
An official website of the United States government
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
Preventive care benefits for children
Coverage for children’s preventive health services.
A fixed amount ($20, for example) you pay for a covered health care service after you've paid your deductible.
Refer to glossary for more details.
The percentage of costs of a covered health care service you pay (20%, for example) after you've paid your deductible.
The amount you pay for covered health care services before your insurance plan starts to pay. With a $2,000 deductible, for example, you pay the first $2,000 of covered services yourself.
- Alcohol, tobacco, and drug use assessments for adolescents
- Autism screening for children at 18 and 24 months
- Behavioral assessments for children: Age 0 to 11 months , 1 to 4 years , 5 to 10 years , 11 to 14 years , 15 to 17 years
You are leaving HealthCare.gov.
You're about to connect to a third-party site. Select CONTINUE to proceed or CANCEL to stay on this site.
Learn more about links to third-party sites .
- Blood pressure screening for children: Age 0 to 11 months , 1 to 4 years , 5 to 10 years , 11 to 14 years , 15 to 17 years
- Blood screening for newborns
- Depression screening for adolescents beginning routinely at age 12
- Developmental screening for children under age 3
- Fluoride supplements for children without fluoride in their water source
- Fluoride varnish for all infants and children as soon as teeth are present
- Gonorrhea preventive medication for the eyes of all newborns
- Hematocrit or hemoglobin screening for all children
- Hemoglobinopathies or sickle cell screening for newborns
- Hepatitis B screening for adolescents at higher risk
- HIV screening for adolescents at higher risk
- Hypothyroidism screening for newborns
- PrEP (pre-exposure prophylaxis) HIV prevention medication for HIV-negative adolescents at high risk for getting HIV through sex or injection drug use
- Chickenpox (Varicella)
- Diphtheria, tetanus, and pertussis (DTaP)
- Haemophilus influenza type b
- Hepatitis A
- Hepatitis B
- Human Papillomavirus (HPV)
- Inactivated Poliovirus
- Influenza (flu shot)
- Meningococcal
- Pneumococcal
- Obesity screening and counseling
- Phenylketonuria (PKU) screening for newborns
- Sexually transmitted infection (STI) prevention counseling and screening for adolescents at higher risk
- Tuberculin testing for children at higher risk of tuberculosis: Age 0 to 11 months , 1 to 4 years , 5 to 10 years , 11 to 14 years , 15 to 17 years
- Vision screening for all children
- Well-baby and well-child visits
More information about preventive services for children
- Preventive services for children age 0 to 11 months
- Preventive services for children age 1 to 4 years
- Preventive services for children age 5 to 10 years
- Preventive services for children age 11 to 14 years
- Preventive services for children age 15 to 17 years
More on prevention
- Learn more about preventive care from the CDC .
- See preventive services covered for adults and women .
- Learn more about what else Marketplace health insurance plans cover.
Your Guide to Well-Baby Visits
Medical review policy, latest update:, what are well-baby visits and why are they so important, when will my child's well-baby visits happen, read this next, what you can expect at well-baby visits, tips on making the most of well-baby visits, time it right, make a checklist, write down your questions, have some answers, too, dress baby for success.
What to Expect the First Year , 3rd edition, Heidi Murkoff. WhatToExpect.com, Your Baby's Vaccine Schedule: What Shots Should Your Child Get When? , January 2021. American Academy of Pediatrics, AAP Schedule of Well-Child Care Visits , September 2021. American Academy of Pediatrics, Checkup Checklist: 1 Month Old , September 2021. KidsHealth From Nemours, Your Child's Checkup: 1 Month , April 2021.
Go to Your Baby's Age
Trending on what to expect, the covid-19 vaccine for infants, toddlers and young children, how to create a night shift system when you have a newborn, ⚠️ you can't see this cool content because you have ad block enabled., when do babies start laughing, baby-led weaning, what happens in the ‘4th trimester’ (and is it a real thing).
Shop for Plans
Shop for your own coverage, plans through your employer.
Learn about the medical, dental, pharmacy, behavioral, and voluntary benefits your employer may offer.
Looking for Medicare coverage?
Well-child visits.
It's important for your child to have regularly scheduled checkups, often called well-child visits, beginning shortly after birth and lasting through the teen years.
These appointments allow your doctor to keep a close eye on your child's general health and development. Finding possible problems early gives your child the best chance for proper and successful treatment. Also, any concerns you have about your child can be discussed during these visits.
During these visits, the doctor examines your child and asks you questions about your child's development and behavior. Immunizations also are either given or scheduled at this time.
Your child's doctor will recommend a schedule for well-child visits. One example is for visits at ages: footnote 1
- 3 to 5 days old.
- By 1 month.
After age 3, well-child visits are usually scheduled yearly through the teen years.
Citations Bright Futures/American Academy of Pediatrics (2020). Recommendations for preventive pediatric health care. American Academy of Pediatrics . https://downloads.aap.org/AAP/PDF/periodicity_schedule.pdf. Accessed February 27, 2020.
Current as of: October 24, 2023
Author: Healthwise Staff
Clinical Review Board All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use . Learn how we develop our content .
To learn more about Healthwise, visit Healthwise.org .
© 1995-2024 Healthwise, Incorporated. Healthwise, Healthwise for every health decision, and the Healthwise logo are trademarks of Healthwise, Incorporated.
Related Links
Page footer, i want to..., secure member sites, the cigna group information.
Cigna. All rights reserved.
Individual and family medical and dental insurance plans are insured by Cigna Health and Life Insurance Company (CHLIC), Cigna HealthCare of Arizona, Inc., Cigna HealthCare of Illinois, Inc., Cigna HealthCare of Georgia, Inc., Cigna HealthCare of North Carolina, Inc., Cigna HealthCare of South Carolina, Inc., and Cigna HealthCare of Texas, Inc. Group health insurance and health benefit plans are insured or administered by CHLIC, Connecticut General Life Insurance Company (CGLIC), or their affiliates (see a listing of the legal entities that insure or administer group HMO, dental HMO, and other products or services in your state). Accidental Injury, Critical Illness, and Hospital Care plans or insurance policies are distributed exclusively by or through operating subsidiaries of Cigna Corporation, are administered by Cigna Health and Life Insurance Company, and are insured by either (i) Cigna Health and Life Insurance Company (Bloomfield, CT); (ii) Life Insurance Company of North America (“LINA”) (Philadelphia, PA); or (iii) New York Life Group Insurance Company of NY (“NYLGICNY”) (New York, NY), formerly known as Cigna Life Insurance Company of New York. The Cigna name, logo, and other Cigna marks are owned by Cigna Intellectual Property, Inc. LINA and NYLGICNY are not affiliates of Cigna.
All insurance policies and group benefit plans contain exclusions and limitations. For availability, costs and complete details of coverage, contact a licensed agent or Cigna sales representative. This website is not intended for residents of New Mexico.
Selecting these links will take you away from Cigna.com to another website, which may be a non-Cigna website. Cigna may not control the content or links of non-Cigna websites. Details

An official website of the United States government Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
Well-Child Care
Improving infant well-child visits.
High-quality well-child visits can improve children’s health, support caregivers’ behaviors to promote their children’s health, and prevent injury and harm. The American Academy of Pediatrics and Bright Futures recommend nine well-care visits by the time children turn 15 months of age. These visits should include a family-centered health history, physical examination, immunizations, vision and hearing screening, developmental and behavioral assessment, an oral health risk assessment, a social assessment, maternal depression screening, parenting education on a wide range of topics, and care coordination as needed. i When children receive the recommended number of high-quality visits, they are more likely to be up-to-date on immunizations, have developmental concerns recognized early, and are less likely to visit the emergency department. ii , iii , iv , v , vi , vii However, many infants do not receive the recommended number of infant well-child visits.
The Centers for Medicare & Medicaid Services (CMS) offers quality improvement (QI) technical assistance (TA) to help states increase the attendance and quality of well-child visits for Medicaid and Children’s Health Insurance Program (CHIP) beneficiaries ages 0 to 15 months.
QI TA resources , to help state Medicaid and CHIP staff and their QI partners get started improving the use of infant well-child visits for their beneficiaries
Improving Infant Well-Child Visit learning collaborative resources , to share different approaches to improving well-child visit care and state examples
For more information on these materials and other QI TA, please email [email protected] .
QI TA Resources
These resources can help states get started in developing their own infant well-child QI projects:
Getting Started on Quality Improvement Video . This video provides an overview of how Medicaid and CHIP agencies can start a QI project to improve the use of infant well-child visits. The Model for Improvement begins with small tests of change, enabling state teams to “learn their way” toward strong programs and policies.
Driver Diagram and Change Idea Table . A driver diagram is a visual display of what “drives” or contributes to improvements in infant well-child visits. This example of a driver diagram shows the relationship between the primary drivers (the high-level elements, processes, structures, or norms in the system that must change to use and quality of infant well-child visits) and the secondary drivers (the places, steps in a process, time-bound moments, or norms in which changes are made to spur improvement). The document also includes change idea tables, which contain examples of evidence-based or evidence-informed QI interventions to improve the use of infant well-child care. The change ideas were tailored for Medicaid and CHIP.
Measurement Strategy . This document provides examples of measures that can be used to monitor infant well-child care QI projects.
Improving Infant Well-Child Visits: Learning Collaborative Resources
Beginning in 2021, CMS facilitated the two year Infant Well-Child Visit learning collaborative to support state Medicaid and CHIP agencies’ efforts to improve the use of infant well-child visits from 0-15 months of age. The learning collaborative included a webinar series and an affinity group to support state Medicaid and agencies’ quality improvement efforts. The webinars, listed and linked to below, described approaches that states can use to improve attendance and quality of infant well-child visits.
California, Missouri, North Carolina, South Carolina, Texas and Virginia participated in the action-oriented affinity group where teams designed and implemented an infant well-child quality improvement (QI) project in their state with tailored TA from CMS. Learnings from participating states can be found in the state highlights brief.
Learning Collaborative Webinar Series
State Spotlights Webinar on Improving Infant-Well Child Care ( Video ) ( Transcript ). This 2024 webinar spotlighted several state QI projects from the affinity group, highlighting their strategies, partnerships, and lessons learned.
Using Payment, Policy and Partnerships to Improve Infant Well-Child Care ( Audio )( Transcript ). This August 2021 webinar focused on Medicaid and CHIP payment incentives, managed care contracts, and other strategies that can increase the use and quality of infant well-child visits and advance equity. Speakers from the CMS and Mathematica introduced CMS’ Maternal and Infant Health Initiative and shared the importance of high-quality well-child visits and the opportunities within Medicaid and CHIP to impact infant health. Speakers from Pennsylvania and Texas’ Medicaid and CHIP agencies described their efforts to expand and incentivize participation in infant well-child visits, such as through value-based purchasing, performance improvement projects, CHIP Health Services Initiatives (HSIs), and partnerships with aligned service providers like the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). State presenters offered insights into ways to incentivize efforts to close gaps in care, engage families, and improve performance on quality measures. During the Q&A session, presenters discussed the impact of the COVID-19 pandemic on well-child care, the potential of using telehealth or hybrid visits to increase access, and incentives for managed care entities, and addressing the social determinants of health in value-based payment strategies.
Improving Quality and Utilization of Infant Well-Child Visits ( Audio )( Transcript ). This September 2021 webinar focused on the characteristics of a high-performing system of well-child health care. CMS and Mathematica presenters shared the Maternal and Infant Health Initiative’s Theory of Change. Speakers from Washington and Arkansas Medicaid and CHIP agencies discussed how their states have achieved high rates of participation in infant well-child visits and how they use data to monitor performance and disparities and ensure access to services. Washington shared insights on leveraging collaborative performance improvement projects to identify and address barriers to care. Arkansas discussed the state’s per member per month incentives for performance and minimum performance measures for infant well-child visit rates. During the Q&A session, presenters highlighted efforts to improve health equity, engage parents and providers, and leverage performance measures and quality tools to improve attendance at infant well-child visits.
Models of Care that Drive Improvement in Infant Well-Child Visits ( Audio )( Transcript ). In this September 2021 webinar, three states—Oregon, Michigan, and North Carolina—shared approaches to designing and implementing models of care associated with improved infant well-child visit participation, including patient-centered medical homes (PCMHs) and home visiting. States offered insights on the importance of strategic alignment of policies, processes, and partnerships. Oregon discussed its home visiting program and quality incentive strategy for its coordinated care organizations. The state incentivizes progress on the HEDIS measures and other measures designed by the state’s Pediatric Improvement Partnership, including a measure of social-emotional health service capacity and access for infants and children. Michigan discussed how they requires MCOs to identify and publish disparities in well-child visit rates and how they encourage plans to reduce disparities. The state also uses an algorithm that automatically assigns members to MCOs based on MCOs’ performance and reimburses for maternal-infant health home visiting. North Carolina shared its Keeping Kids Well program, which aims to increase well-child visit and immunization rates and reduce disparities in those rates. The program offers coaches to practices to support their improvements, established an advisory board of key interested parties, and provides customized vaccination notices for practices to distribute to beneficiaries, in partnership with health systems and pharmaceutical companies. The state also used the Healthy Opportunities payment to incentivize the identification and redress of health-related social needs and provided the Health Equity Payment to providers serving areas with high poverty rates.
i 3 Hagan, J.F., J.S. Shaw, and P.M. Duncan (eds.). Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. 4th ed. Elk Grove Village, IL: American Academy of Pediatrics, 2017.
ii Gill, J.M., A. Saldarriaga, A.G. Mainous, and D. Unger. “Does Continuity Between Prenatal and Well-Child Care Improve Childhood Immunizations?” Family Medicine, vol. 34, no. 4, April 2002, pp. 274–280.
iii Buchholz, M., and A. Talmi. “What We Talked About at the Pediatrician’s Office: Exploring Differences Between Healthy Steps and Traditional Pediatric Primary Care Visits.” Infant Mental Health Journal, vol. 33, no. 4, 2012, pp. 430–436.
iv DeVoe, J.E., M. Hoopes, C.A. Nelson, et al. “Electronic Health Record Tools to Assist with Children’s Insurance Coverage: A Mixed Methods Study.” BMC Health Services Research, vol.18, no. 1, May 2018, p. 354–360.
v Coker, T.R., S. Chacon, M.N. Elliott, et al. “A Parent Coach Model for Well-Child Care Among Low-Income Children: A Randomized Controlled Trial.” Pediatrics, vol. 137, no. 3, March 2016, p. e20153013.
vi Flores, G., H. Lin, C. Walker, M. Lee, J. Currie, R. Allgeyer, M. Fierro, M. Henry, A. Portillo, and K. Massey. “Parent Mentoring Program Increases Coverage Rates for Uninsured Latino Children.” Health Affairs, vol. 37, no. 3, 2018, pp. 403–412.
vii Hakim, R.B., and D.S. Ronsaville. “Effect of Compliance with Health Supervision Guidelines Among US Infants on Emergency Department Visits.” Archives of Pediatrics & Adolescent Medicine, vol. 156, no. 10, October 2002, pp. 1015–1020.
The independent source for health policy research, polling, and news.
The Impact of the Pandemic on Well-Child Visits for Children Enrolled in Medicaid and CHIP
Elizabeth Williams , Alice Burns , Robin Rudowitz , and Patrick Drake Published: Mar 18, 2024
In Medicaid, states are required to cover all screening services as well as any services “necessary… to correct or ameliorate” a child’s physical or mental health condition under Medicaid’s Early and Periodic Screening, Diagnostic and Treatment (EPSDT) benefit (see Box 1). Many of these screening services along with immunizations are provided at well-child visits. These visits are a key part of comprehensive preventive health services designed to keep children healthy and to identify and treat health conditions in a timely manner. Various studies have also shown that children who forego their well-child visits have an increased chance of going to the emergency room or being hospitalized. Well-child visits are recommended once a year for children ages three to 21 and multiple times a year for children under age three according to the Bright Futures/American Academy of Pediatrics (AAP) periodicity schedule .
A recent Centers for Medicare and Medicaid Services (CMS) analysis shows that half of children under age 19 received a Medicaid or CHIP funded well-child visit in 2020. The onset of the pandemic in 2020 had a substantial impact on health and health care service utilization, but research has shown that many Medicaid-covered children were not receiving recommended screenings and services even before the pandemic. This issue brief examines well-child visit rates overall and for selected characteristics before and after the pandemic began and discusses recent state and federal policy changes that could impact children’s preventive care. The analysis uses Medicaid claims data which track the services enrollees use and may differ from survey data. In future years, claims data will be used to monitor adherence to recommended screenings. Key findings include:
- More than half (54%) of children under age 21 enrolled in Medicaid or CHIP received a well-child visit in 2019, but the share fell to 48% in 2020, the start of the COVID-19 pandemic.
- Despite having the highest well-child visit rates compared to other ethnic and racial groups, Hispanic and Asian children enrolled in Medicaid or CHIP saw the largest percentage point declines in well-child visit rates from 2019 to 2020.
- Children over age three enrolled in Medicaid or CHIP have lower rates of well-child visits and experienced larger declines in well-child visits during the pandemic than children under age three.
- Well-child visit rates are lower for Medicaid/CHIP children in rural areas, but rates in urban areas declined more during the pandemic.
How did use of well-child visits change during the pandemic?
More than half (54%) of children under 21 enrolled in Medicaid or CHIP received a well-child visit in 2019, but the share fell to 48% in 2020, the first year of the COVID-19 pandemic (Figure 1). Rates examined here use Medicaid claims data which differ substantially from survey data (see Box 2). While the vast majority of children in the analysis (91% in 2019 and 88% in 2020) used a least one Medicaid service, including preventive visits, sick visits, filling prescriptions, or hospital or emergency department visits, well-child visit rates remained low and are substantially below the CMS goal of at least 80%. One recent analysis found that 4 in 10 children enrolled in Medicaid or CHIP experienced at least one challenge when accessing health care. Barriers to Medicaid/CHIP children receiving needed care can include lack of transportation, language barriers, disabilities , and parents having difficulty finding childcare or taking time off for an appointment as well as the availability of and distance to primary care providers. Some states have seen a loss in Medicaid pediatric providers, and one recent story reported that families with Medicaid in California were traveling long distances and experiencing long wait times for primary care appointments. Data have also shown slight declines in the share of kindergarten children up to date on their routine vaccinations since the COVID-19 pandemic, which may, in part, be associated with the decline in well-child visits. The national measles, mumps, and rubella (MMR) vaccination rate is below the goal of at least 95%, and some states are now seeing measle outbreaks among children.
Despite having the highest well-child visit rates compared to other ethnic and racial groups, Hispanic and Asian children enrolled in Medicaid or CHIP saw the largest percentage point declines in well-child visit rates from 2019 to 2020 (Figure 2). Prior to the pandemic in 2019, about half or more of children across most racial and ethnic groups had a well-child visit, with rates highest for Hispanic (60%) and Asian (57%) children. The rate for American Indian and Alaska Native (AIAN) children lagged behind at just over one in three (36%), although this may reflect that some services received from Indian Health Service providers not being captured in the analysis (see Methods ). Between 2019 and 2020, the well-child visit rate fell for all racial and ethnic groups. Hispanic and Asian children experienced the largest percentage point declines in well-child rates (9 percentage points for both groups), but they still had higher rates compared to other groups as of 2020. Black, Native Hawaiian, and Other Pacific Islander (NHOPI), and AIAN children also experienced larger percentage point declines in their well-child visit rates compared with White children, and AIAN children had the largest relative decline on account of their lower starting rate. As of 2020, rates remained lowest for NHOPI (42%) and AIAN children (29%). Twenty-two states, including some states that are home to larger shares of AIAN and NHOPI children, were excluded from the race/ethnicity analysis due to data quality issues (see Methods ).
Children ages three and older have lower rates of well-child visits and experienced larger declines in well-child visits during the pandemic than children under age three (Figure 2). Well-child visit rates are highest when children are young because multiple well-child visits are recommended for children under age three. Although children under three have highest rates of a single well-child visit within the year, it is unknown whether the rates of adherence to recommended well-child screenings are higher or lower than that of other groups because this analysis only accounts for one well-child visit in a year. Well-child visit rates steadily decrease as children get older with the exception of the 10-14 age group, where somewhat higher rates may reflect school vaccination requirements .
Well-child visit rates are lower in rural areas than urban ones, but urban areas had larger declines during the first year of the pandemic (Figure 2). The share of Medicaid/CHIP children living in rural areas with a well-child visit declined from 47% in 2019 to 43% in 2020 while the share for urban areas fell from 56% in 2019 to 49% in 2020, narrowing the gap between Medicaid/CHIP well-child visit rates in rural and urban areas. Note that 18% of children in the analysis lived in a rural area, and three states were excluded from the geographic area analysis due to data quality issues (see Methods ). This analysis also examined changes for children by eligibility group, managed care status, sex, and presence of a chronic condition; data are not shown but well-child visit rates for Medicaid/CHIP children declined across all groups from 2019 to 2020.
What to watch?
Well-child visit rates for Medicaid/CHIP children overall fall below the goal rate, with larger gaps for AIAN, Black and NHOPI children as well as older children and children living in rural areas, highlighting the importance of outreach and other targeted initiatives to address disparities. Addressing access barriers and developing community partnerships have been shown to increase well-child visit rates and reduce disparities. It will be important to track, as data become available, the extent to which well-child visit rates as well as vaccination rates (often administered at well-child visits) rebounded during the pandemic recovery and where gaps remain.
Recent state and federal actions could help promote access, quality and coverage for children that could increase well-child visit rates. The Bipartisan Safer Communities Act included a number of Medicaid/CHIP provisions to ensure access to comprehensive health services and strengthen state implementation of the EPSDT benefit. CMS also released an updated school-based services claiming guide , and states have taken action to expand Medicaid coverage of school-based care in recent years. In 2024, it became mandatory for states to report the Child Core Set, a set of physical and mental health quality measures, with the goal of improving health outcomes for children. In addition, as of January 2024, all states are now required to provide 12-month continuous eligibility for Medicaid and CHIP children, which could help stabilize coverage and help children remain connected to care. Three states also recently received approval to extend continuous eligibility for children in Medicaid for multiple years, which could help children maintain coverage beyond one year. In the recently released FY 2025 budget, the Biden Administration proposes establishing the option for states to provide continuous eligibility in Medicaid and CHIP for children from birth to age six or for 36 month periods for children under 19.
Lastly, millions of children are losing Medicaid coverage during the unwinding of the continuous enrollment provision, which could have implications for access. Data up to March 2024 show that children’s net Medicaid enrollment has declined by over 4 million. In some cases, children dropped from Medicaid may have transitioned to other coverage, but they may also become uninsured, despite in many cases remaining eligible for Medicaid or CHIP. While people of color are more likely to be covered by Medicaid , data on disenrollment patterns by race and ethnicity are limited . KFF analysis shows individuals without insurance coverage have lower access to care and are more likely to delay or forgo care due to costs. A loss of coverage or gaps in coverage can be especially problematic for young children who are recommended to receive frequent screenings and check-ups.
- Children's Health Insurance Program (CHIP)
- Access to Care
Also of Interest
- Recent Trends in Children’s Poverty and Health Insurance as Pandemic-Era Programs Expire
- More Children are Losing Medicaid Coverage as Child Poverty Grows
- Medicaid Enrollment and Unwinding Tracker
- Headed Back To School in 2023: A Look at Children’s Routine Vaccination Trends
Security Alert May 17, 2024
Worldwide caution, update may 10, 2024, information for u.s. citizens in the middle east.
- Travel Advisories |
- Contact Us |
- MyTravelGov |
Find U.S. Embassies & Consulates
Travel.state.gov, congressional liaison, special issuance agency, u.s. passports, international travel, intercountry adoption, international parental child abduction, records and authentications, popular links, travel advisories, mytravelgov, stay connected, legal resources, legal information, info for u.s. law enforcement, replace or certify documents.
Get a Passport
Renew or Replace a Passport
Get My Passport Fast
Prepare to Apply
Passport Help
Legal Matters
Get a Passport Homepage
Share this page:
Apply for your First Adult Passport
Apply for a Child Under 16
Apply as a 16 or 17 Year Old
Get My Application Status
Get a Passport Card
Respond to a Letter or Email
- Both parents or guardians must approve that we can issue a passport to a child, and go with the child to apply in person.
- If one or both parents or guardians cannot apply with their child, you will need to show us more documents.
- You cannot renew your child's passport using Form DS-82.
- Passports for children under age 16 are only valid for 5 years.
Steps to Apply
1. fill out form ds-11 and print it.
Use our Form Filler tool to fill out your child's form on a desktop or laptop computer and then print it. If you are experiencing technical issues with the Form Filler, download a PDF .

Tips to complete your child's form :
- Do not sign your child's form until asked to do so by a passport acceptance agent or employee.
- You can apply for a passport book , a passport card , or both documents.
- You may ask for a larger passport book with more visa pages, at no extra cost, by checking the 'large book' box at the top of the DS-11.
2. Get Evidence of U.S. Citizenship (and a photocopy)
Your evidence must be an original or replacement copy. The document must have the official seal or stamp of the office which issued it. You must submit one of the following documents for your child:
- Issued by the city, county, or state of birth
- Lists applicant's full name, date of birth, and place of birth
- Lists the parent(s)' full names
- Has the date filed with registrar's office (must be within one year of birth)
- Has the registrar's signature
- Has the seal or stamp of the city, county, or state which issued it
- Consular Report of Birth Abroad or Certification of Birth
- Certificate of Citizenship
- Please note you must also provide a document, such as a birth certificate, that lists the parent(s) or legal guardian(s) of the child. Full validity means the document is or was valid for 10 years for adults and 5 years for children under 16.
If you cannot submit one of these documents, go to our Citizenship Evidence page for more information.
Paper only : You cannot submit digital evidence of U.S. citizenship such as a mobile or electronic birth certificate. You must submit physical evidence of U.S. citizenship and a photocopy of the document.
Returning your child's document : We will return your child's document in a separate mailing up to 8 weeks after you receive the new passport.
Tips for making a photocopy :
- Black and white (no color)
- Use 8.5 inch by 11 inch paper
- Use a single side of the paper
If you do not submit a photocopy, you must submit a second copy of your citizenship evidence. We will keep this copy for our records.

3. Show Your Relationship to Your Child
You must submit a document that lists the parent(s) or legal guardian(s) of the child. Examples include:
- U.S. birth certificate (also evidence of U.S. citizenship)
- Foreign birth certificate
- Adoption decree
- Divorce or custody decree
- A court order
Some documents, like a U.S. birth certificate, show both U.S. citizenship and parental relationship. These documents must be originals or certified copies (not photocopies).
You and your child may have different last names, as long as the document showing your relationship to your child lists your full name.
If your name is different than the one on the document showing your relationship to your child, submit proof of your legal name change.
4. Get a Photo ID (and a photocopy)
Both parents or guardians must bring a physical, photo ID and a photocopy of it. If your photo ID is from a different state than the state in which you are applying, bring a second photo ID.
You must show at least one of these photo IDs:
- Valid or expired, undamaged U.S. passport book or passport card
- In-state, fully valid driver's license or enhanced driver's license with photo
- Certificate of Naturalization
- Certificate of Citizenship
- Government employee ID (city, county, state, or federal)
- U.S. military or military dependent ID
- Current (valid) foreign passport
- Matricula Consular (Mexican Consular ID) used by a parent of a U.S. citizen child applicant
- U.S. Permanent Resident Card (Green Card) used by a parent of a U.S. citizen child applicant
- Trusted Traveler IDs (including valid Global Entry, FAST, SENTRI, and NEXUS cards)
- Enhanced Tribal Cards and Native American tribal photo IDs
- In-state, fully-valid learner's permit with photo
- In-state, fully-valid non-driver ID with photo
- Temporary driver's license with photo
If you do not have one of these photo IDs, go to our Identification page for more information.
5. Show More Documents (if both parents or guardians cannot apply)
- Both parents or guardians must approve that we can issue a passport to a child, and go with the child to apply in person.
- If one or both parents or guardians cannot apply in person with their child, you will need to show more documents.
Important : Submit Form DS-3053 and other notarized statements within three months of signing them.
6. Provide a Photo
You must provide one photo with your child's application. Go to our Passport Photo page for photo requirements and to see examples of photos.
- Do not attach or staple your child's photo to the form. The acceptance agent or passport employee will review the photo and staple it to your form.
- Some passport acceptance facilities
- A company which offers photo services
- Home. Ask your friend or family member to take your child's photo. Print it on glossy or matte photo quality paper.
7. Calculate Fees
When applying using Form DS-11, you will pay two separate fees - an application fee and an execution (acceptance) fee. You will pay the application fee to the U.S. Department of State, and the execution (acceptance) fee to the facility which takes your application.
- Add $60 to your application fee if you want expedited service .
- Add $19.53 to your application fee if you want us to ship your completed passport in 1-2 days after we issue it.
Child Applicants :
For more information on how to pay and a full list of fees, go to our Passport Fees page.
*How to fill out your check and pay the application fee to the U.S. Department of State. Please note you must pay a separate execution (acceptance) fee.
Families may write one check or money order to the U.S. Department of State if they are applying at the same time. The check or money order must include the name and date of birth of each applicant.
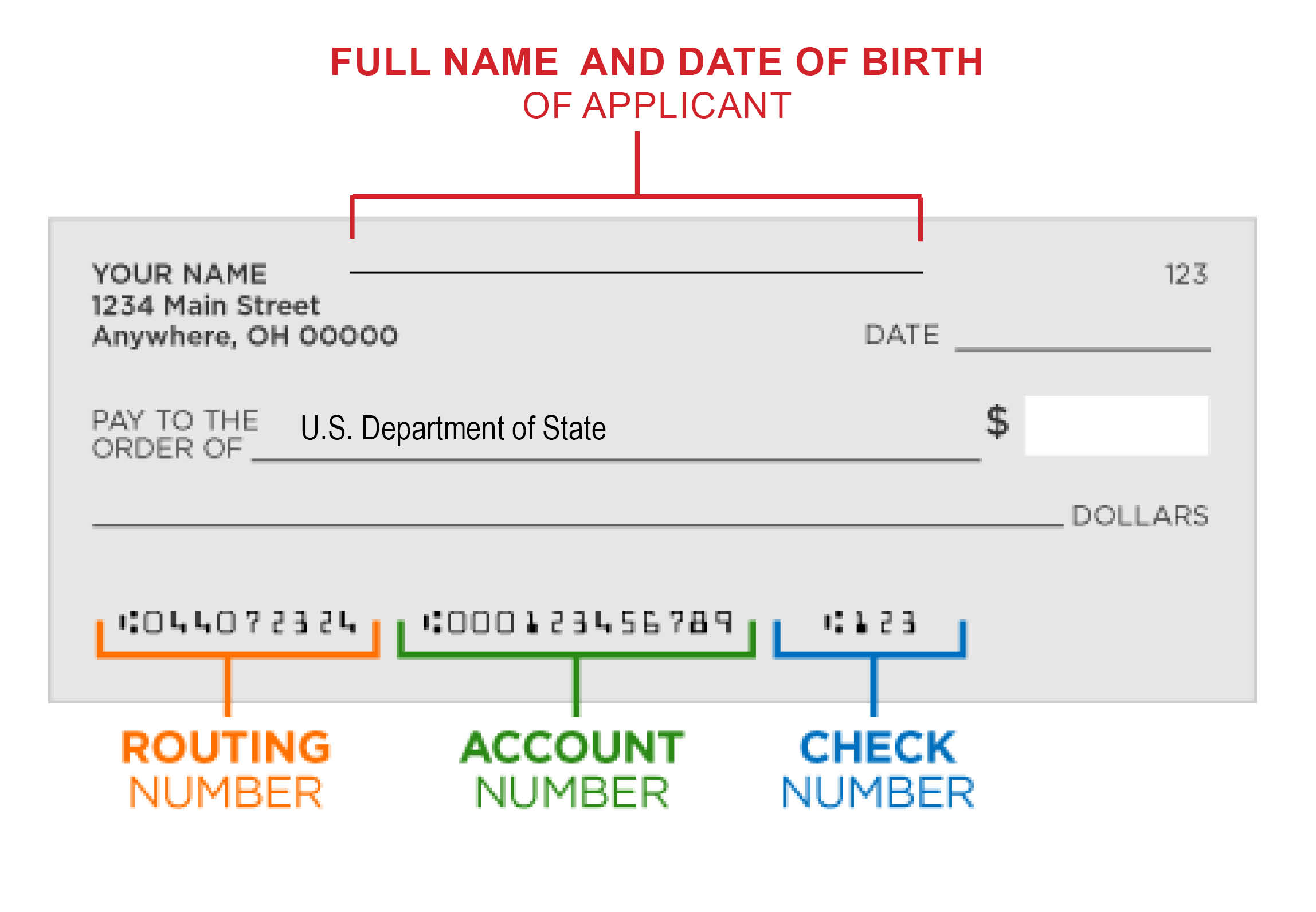
8. Find Location to Apply
In the United States:
- Traveling in more than 3 weeks? Go to a passport acceptance facility such as a post office, library, or local government office. Check with the facility to see if you need to make an appointment.
- Traveling in less than 3 weeks? Make an appointment to apply at a passport agency or center.
In another country:
- Contact your U.S. embassy or consulate .
9. Track Your Application Status
You can subscribe to email updates about your application status, and learn more about each status update .
It may take 2 weeks from the day you apply until your child's application status is “In Process.”
Frequently Asked Questions
How will you send my child's passport and supporting documents.
You will get multiple mailings. The number of mailings depends on what document(s) you asked for.
Passport Book : You may get your new passport and citizenship documents in two mailings. You may wait 8 weeks after getting your passport before you get a second mailing with your citizenship documents. We will return the passport book using a trackable delivery service.
Passport Card : You may get your new passport card and your citizenship documents in two mailings. You may wait 8 weeks after getting your passport before you get a second mailing with your citizenship documents. We only send the passport card via First Class Mail. We do not send cards using 1-2 day delivery services.
Both a Passport Book and Card : You may get three separate mailings:
- New passport book
- New passport card
- Citizenship documents
Contacting Us : If you have been waiting more than 8 weeks for your documents, call us at 1-877-487-2778 to report that you have not received your documents.
If you want us to reimburse you for a lost supporting document, you must contact us within 90 days of the date which we mailed your passport. You will also need to provide a receipt to show the cost of replacing the document.
Can I pay for faster delivery and return shipping?
Yes. You may choose one or both of the following shipment options:
- Delivering application to us : Pay for Priority Mail Express for faster shipping. The price for this service varies depending on the area of the country.
- Returning the passport to you : Pay $19.53 for 1-2 day delivery. This means you will receive your passport 1-2 days after we send it. Include this fee with your check or money order payable to the U.S. Department of State. Do not submit a return envelope to us with postage pre-paid.
You may receive your passport and supporting documents in separate mailings. If you are renewing a passport card, we will send it to you via First Class Mail. We do not use 1-2 day delivery services if you only applied for a passport card.
What countries require Form DS-3053 "Statement of Consent" to be notarized at an embassy or consulate?
In certain countries, a DS-3053 must be notarized at a U.S. embassy or consulate and cannot be notarized by a local notary public. Currently, these countries include:
Special Passport Fairs
Find a Special Passport Fair near you!
We're holding special passport fairs all across the United States to help you get your passport more easily. New events are added to our site every week.
Most events are for first-time applicants and children, (who use Form DS-11). If you can use Form DS-82, you can renew by mail at your convenience!
Processing Times
Routine: 6-8 weeks*
Expedited: 2-3 weeks and an extra $60*
*Consider the total time it will take to get a passport when you are booking travel. Processing times only include the time your application is at a passport agency or center.
- It may take up to 2 weeks for applications to arrive at a passport agency or center. It may take up to 2 weeks for you to receive a completed passport after we print it.
- Processing times + mailing times = total time to get a passport
Urgent Travel: See our Get my Passport Fast page.
How to Apply for your Child's Passport
Watch this video to learn how to apply in person for your child's U.S. passport!
External Link
You are about to leave travel.state.gov for an external website that is not maintained by the U.S. Department of State.
Links to external websites are provided as a convenience and should not be construed as an endorsement by the U.S. Department of State of the views or products contained therein. If you wish to remain on travel.state.gov, click the "cancel" message.
You are about to visit:
Official websites use .gov
A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
Getting Your COVID-19 Vaccine
Get an updated covid-19 vaccine.
To find COVID-19 vaccine locations near you: Search vaccines.gov , text your ZIP code to 438829, or call 1-800-232-0233.
- Ask your doctor, pharmacist, or community health center, or visit their website.
- Contact your state health department .
- Check your local pharmacy’s website to see if vaccination appointments are available. Some pharmacies may offer vaccines to those who walk-in without making an appointment ahead of time.
- Contact your healthcare provider or your state or local health department for information about getting a COVID-19 vaccine.
- In many states, you may also dial 211 to connect to essential community services.
- Call The Aging Network at 1-800-677-1116.
- Search for services by ZIP code with the Eldercare Locator .
- Contact the Disability Information and Access Line (DIAL) at 1-888-677-1199.
- Call the hotline for Medicare recipients at 1-800-633-4227 (TTY 1-877-486-2048).
Schedule Your Vaccination Appointment
Most vaccination providers schedule appointments online.

Visit a vaccine provider’s online scheduling services to schedule your COVID-19 vaccination appointment.
Contact the vaccination provider directly to verify, reschedule, or cancel or with any questions about your appointment. CDC cannot schedule, verify, reschedule, or cancel a vaccination appointment.
Getting a COVID-19 vaccine after having COVID-19
You should get an updated COVID-19 vaccine even if you already had COVID-19.
- Getting a COVID-19 vaccine after you recover from COVID-19 infection provides added protection against the virus that causes COVID-19.
- People who already had COVID-19 and do not get vaccinated after their recovery are more likely to get COVID-19 again than those who get vaccinated after their recovery.
If you recently had COVID-19, you still need to stay up to date with your vaccines, but you may consider delaying your vaccine dose by 3 months.
If you have COVID-19
People who have COVID-19 should wait to get vaccinated until after your complete your isolation period to avoid potentially exposing healthcare personnel and others during the vaccination visit.
If you have multisystem inflammatory syndrome
Children and adults who have (or have recently had) multisystem inflammatory syndrome (MIS) should wait to get vaccinated until :
- Recovering from being sick and
- It has been 90 days since the date of diagnosis of MIS-A or MIS-C.
Talk to your doctor if you have questions about getting a COVID-19 vaccine.
Before Your Vaccination Appointment
Get a covid-19 vaccine with your routine medical procedures and screenings.
You can combine most procedures, screenings, and vaccinations at the same appointment when you get your COVID-19 vaccination. Talk to your healthcare provider if you have questions.
Children, teens, and adults may get a COVID-19 vaccine and other vaccines, including a flu vaccine, at the same time .
Preparing children and teens for vaccination
The experience of getting a COVID-19 vaccine will be very similar to that of getting routine vaccines. Learn how you can support your child and talk to them before they get a vaccine about what to expect .
Requesting accommodations at COVID-19 vaccination sites
- When making an appointment or arriving for vaccination, you can let staff and/or volunteers know you or your child might need some accommodations.
- People with disabilities can use the COVID-19 Vaccine Disability Information and Access Line (DIAL) to get help with COVID-19 vaccinations.
If you have allergies related to vaccines
Talk to your doctor to learn if you should get a different type of COVID-19 vaccine if you:
- have had a severe allergic reactionto a previous COVID-19 vaccine dose.
- are allergic to an ingredient in a COVID-19 vaccine.
- had an immediate allergic reaction (a reaction that started within 4 hours of getting vaccinated) to a COVID-19 vaccine, but the reaction was not considered severe by a medical professional.
During The Vaccination Appointment
- You should receive a paper or electronic factsheet. The factsheet tells you more about the COVID-19 vaccine you or your child received. Each approved and authorized COVID-19 vaccine has its own fact sheet that contains information to help you understand the risks and benefits of that vaccine.
- Most people can get no-cost updated COVID-19 vaccines through their private health insurance, Medicare, and Medicaid plans.
- Adults without health insurance and adults whose insurance does not cover all vaccine costs can get no-cost updated COVID-19 vaccine at healthcare providers, federally supported health centers, and select pharmacy locations participating in CDC’s Bridge Access Program .
- CDC’s Vaccines for Children (VFC) program provides vaccines at no cost to eligible children through health care providers enrolled in the program.
After Getting a COVID-19 Vaccine

Possible Side Effects After Getting a COVID-19 Vaccine
Side effects after getting a COVID-19 vaccine can vary from person to person. Some people experience a little discomfort and can continue to go about their day. Others have side effects that affect their ability to do daily activities. Side effects generally go away in a few days and tend to be mild and temporary, like those experienced after routine vaccinations. Even if you don’t experience any side effects, your body is building protection against the virus that causes COVID-19.
Common side effects can include:
- Pain, swelling, and redness on the arm where the shot was given.
- Tiredness, headache, muscle pain
Relieve Common Side Effects
- It is not recommended to take pain relievers or medicines, such as ibuprofen, aspirin (only for people ages 18 years or older), or acetaminophen before vaccination to try to prevent side effects.
- Talk to your doctor about taking over-the-counter pain relievers after your vaccine.
- If possible, get some rest.
- Apply a clean, cool, wet washcloth over the area.
- Use or keep moving your arm.
- Drink plenty of fluids.
- Dress in comfortable clothes.
Talk to your child’s healthcare provider about giving your child a non-aspirin pain reliever and learn about other steps you can take at home to comfort your child after vaccination .
Call a doctor or healthcare provider about a side effect if:
- Redness or tenderness where the shot was given gets worse after 24 hours
- Side effects are worrying or do not seem to be going away after a few days
- After leaving a vaccination provider site, if you think you or your child might be having a severe allergic reaction, seek immediate medical care by calling 911.
Adverse events (serious health problems) after COVID-19 vaccination are rare
Adverse events after COVID-19 vaccination are rare, but can cause long-term health problems. They usually happen within six weeks of getting a vaccine. Learn more about the safety of COVID-19 vaccines.
Side effects and adverse events can be reported in Vaccine Adverse Event Reporting System (VAERS).
For Healthcare Workers
Use of COVID-19 Vaccines in the United States: Interim Clinical Considerations
To receive email updates about COVID-19, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- Skip to main content
- Keyboard shortcuts for audio player
Goats and Soda
- Infectious Disease
- Development
- Women & Girls
- Coronavirus FAQ
Are we doing better on child hunger? A sweeping UNICEF report weighs in
Fatma Tanis
1 in 4 children globally lives in severe child food poverty, UNICEF report says

A UNICEF report reveals more than 180 million children aren't getting anywhere near the nutrition they need. The problem is so severe, the report says, these kids suffer from the devastating effects of malnutrition. Some countries, however, have shown that it is possible to reduce what the report calls child food poverty . Discha-AS/Getty Images hide caption
We often hear that many children in the world aren't getting enough to eat. But what does that mean exactly and what does 'not enough' look like?
In parts of East Africa, it means babies are fed some breast milk and a porridge made of maize. In Yemen, a paste with just flour and water. And in conflict areas like Gaza, raw lemon and weeds.
A new report by UNICEF has pulled together these details and other data from 137 low and middle income countries to understand what young children are being fed and what that means for their growth, as well as the state of child development around the world.
And the results are alarming:
One in four children under the age of five are experiencing what study authors call “severe food poverty” which means kids are only being fed two or less food groups per day.
“It amounts to 181 million children who are deprived of the diets they need to survive,” says Harriet Torlesse, a nutrition specialist at UNICEF and the lead author on the report. “If you think about these diets, they really don't contain the range of vitamins and minerals and proteins that children need to grow and develop. “
Nutrition experts told NPR the numbers in the UNICEF report show the world is not making progress in tackling malnutrition and hunger. The covid-19 pandemic, the war in Ukraine, inflation and localized conflicts all added to food supply disruptions as well as an increase in food prices.
The report also highlights some good news: that several low-income countries have figured out how to get more and better food to children under 5.
Here are four takeaways from the report:
It’s not only that kids aren’t eating enough food, it’s that they’re eating the wrong foods
Richmond Aryeetey, Professor of nutrition and head of the department of Population, Family and Reproductive Health at the University of Ghana in Accra, describes the access to nutritious food across Africa as twofold:
“There are those who are not getting enough who would fall into the full poverty criteria. And then there are also those who potentially have the opportunity to get enough but are being fed unhealthy food.”
Experts say aggressive advertising of snacks and sugary beverages that often target children play a big role, and low-income countries have a harder time regulating those industries.
“One of the features of these snack foods is that they're often really cheap and they fill you up. And so, people are inclined to buy them,” says Deanna Olney, the Director of the Nutrition, Diets, and Health Unit at the International Food Policy Research Institute.
“But if they were more expensive because of taxes, you know, then maybe they'd be less inclined to choose those for their children, ” Olney says.
The abundance of ultra-processed foods is also a likely contributor to increasing rates of overweight and obesity in among children. Olney says that’s an issue that needs more attention.
In Gaza, extreme numbers underscore how conflict creates acute hunger for children
While conflict is not the biggest driver of child hunger across the globe, it does cause some of the worst cases, such as in Sudan, Somalia and Gaza.

Palestinian children who took refuge in Quds school wait in line to receive food distributed by charity organizations for their families in Rafah, Gaza on April 01, 2024. Abed Rahim Khatib/Anadolu via Getty Images/Anadolu hide caption
Data collected by UNICEF shows that since this past December, 9 out of 10 children in Gaza have experienced severe food insecurity.

There's already 'catastrophic' hunger in Gaza. Who decides when to call it a 'famine?'
“Children in Gaza at this point in time are barely eating any nutritious foods at all,” says Harriet Torlesse with UNICEF. “Before the war in Gaza, only 13% of children were living in severe food poverty.”
Experts say that since technological advances have made it possible to more accurately measure food intake in conflict zones, Gaza has experienced the highest rate of severe malnutrition documented.
Severe child food poverty is driving high rates of wasting and stunted growth
The stakes are high for the large numbers of children living in severe food poverty with far-reaching implications for overall global development.
UNICEF’s analysis shows these children are 50% more likely to suffer from wasting, when a child is too thin for their height, which is a sign of life-threatening malnutrition. More than 13 million children under 5 are suffering from the extreme form of this condition.
“We know that these children don't do well at school. They earn less income as adults, and they struggle to escape from income poverty. So not only do they suffer throughout the course of their life, their children, too, are likely to suffer from malnutrition,” says Harriet Torlesse.

A child is checked for malnutrition by a health worker at Kahda IDP camp near Mogadishu, Somalia. Most young kids arrive with severe malnutrition, and some die. Thousands of people have fled her home due to a long drought and armed conflict in the region Jonathan Torgovnik/Getty Images/Getty Images Europe hide caption
Malnutrition prevents children from reaching their full potential by not only stunting physical growth, but brain development as well. Even if they make it to adulthood their ability to fully contribute to their community and to the productivity of their country is limited compared to children who have had access to nutritious food.
“In 2016, there was a study that was commissioned to look at the cost of hunger in Ghana,” says Richmond Aryeetey. “The estimate was that Ghana was losing close to about $6.4 million annually because of children who are not being fed adequately. That's a lot of money being lost because we are not feeding our children well.”
The good news? There are solutions
Several low-income countries, such as Nepal and Burkina Faso, have managed to cut the rate of severe child food poverty in half. Rwanda has done so by a third. Experts say they all have several common factors that have led to success.
“The first being they've all made a real, deliberate effort to improve the supply of local nutritious foods. Be it pulses or vegetables or poultry,” says Harriet Torlesse. The less a country is reliant on imports for food, nutrition experts say, the better their chances of minimizing hunger.
Other countries are taking on the influx of ultra processed foods. In Peru for example, the government introduced legislation that processed foods and beverages must carry a warning label listing sugar, fat and salt content and they put a 25% tax on high sugar drinks.
“And we've seen in Nepal how a nationwide cash grant to poor families has increased their purchase of nutritious foods such as meat and pulses,” Torlesse says. “And then there's been a real effort within the health system to reach families with essential counseling and support so that caregivers know how best to feed their children using locally available, nutritious foods.”
Still, there needs to be a better broader approach to tackling child hunger, according to Richmond Aryeetey, “...we are sending people to the moon. We are doing all kinds of technologically advanced stuff, and yet we are not able to feed children. It's really a shame.”

IMAGES
VIDEO
COMMENTS
Parents know who they should go to when their child is sick. But pediatrician visits are just as important for healthy children. The Bright Futures/American Academy of Pediatrics (AAP) developed a set of comprehensive health guidelines for well-child care, known as the "periodicity schedule."It is a schedule of screenings and assessments recommended at each well-child visit from infancy ...
Take blood pressure. Measure oxygen levels. Listen to your child's lungs. Look at your child's eyes, ears, and throat. Press on your child's tummy to feel organs. Move your child's hips ...
Young children grow quickly, so they need to visit the doctor or nurse regularly to make sure they're healthy and developing normally. Children ages 1 to 4 need to see the doctor or nurse when they're: 12 months old. 15 months old (1 year and 3 months) 18 months old (1 year and 6 months) 24 months old (2 years) 30 months old (2 years and 6 ...
Immunizations are usually administered at the two-, four-, six-, 12-, and 15- to 18-month well-child visits; the four- to six-year well-child visit; and annually during influenza season ...
If you are a UnitedHealthcare Community Plan member, you may have access to our Healthy First Steps program, which can help you find a care provider, schedule well-child visits, connect with educational and community resources and more. To get started, call 1-800-599-5985, TTY 711, Monday through Friday, from 8 a.m. to 5 p.m.
The American Academy of Pediatrics recommends the following: Newborn: Checkup within five days of returning home from the hospital. HBV, if not given in the hospital. 2-4 weeks: Well-child check ...
It's important for your child to have regularly scheduled checkups, often called well-child visits, beginning shortly after birth and lasting through the teen years. ... After age 3, well-child visits are usually scheduled yearly through the teen years. Related Information. Growth and Development, Ages 11 to 14 Years; Growth and Development ...
Our well-child visit schedule for checkups lets you know how often kids should see a doctor, even when they're not sick. Read the articles below to find out what to expect at your child's next wellness checkup! Well-Child Visit: Newborn; Well-Child Visit: 3-5 Days; Well-Child Visit: 1 Month;
What are the ages for well-child visits? A standard well-child visit schedule spans from infancy through adolescence, and includes checkups at the following ages: In your baby's first year: Newborn visit (3-5 days after birth), at 1 month old, 2 months, 4 months, 6 months, 9 months, and at 12 months; 15 months; 18 months; 2 years;
Routine well-child visits. Early childhood is a time of rapid growth and change; physical and behavioral development is faster during these years and requires very close monitoring. That's why young children have more frequent check-ups, known as well-child visits. Our pediatricians follow the American Academy of Pediatrics (AAP) guidelines ...
Overview. Kids ages 11 to 14 years need to go to the doctor or nurse for a "well-child visit" once a year. A well-child visit is when you take your child to the doctor to make sure they're healthy and developing normally. This is different from other visits for sickness or injury. At a well-child visit, the doctor or nurse can help catch ...
Beginning at the 7 year visit, there is both a Parent and Patient education handout (in English and Spanish). For the Bright Futures Parent Handouts for well-child visits up to 2 years of age, translations of 12 additional languages (PDF format) are made possible thanks to the generous support of members, staff, and businesses who donate to the ...
Of course, visiting the pediatrician's office often early in your child's life gives you more opportunities to learn what to expect, ask questions, and help build your parenting skills. The American Academy of Pediatrics recommends the following well-check schedule for the first year of your child's life. 3 to 5 days.
How often should I schedule well-child visits? When you should come in for a well-child visit depends on your child's age. We follow guidelines set by the American Academy of Pediatrics. Well-child visits are recommended at the following ages for infants and toddlers: First-week visit (3-5 days old) 2 weeks old; 1 month old; 2 months old; 4 ...
Overview. Teens ages 15 to 17 years need to go to the doctor or nurse for a "well-child visit" once a year. A well-child visit is when you take your teen to the doctor to make sure they're healthy and developing normally. This is different from other visits for sickness or injury. At a well-child visit, the doctor or nurse can help catch ...
VIEW PROFESSIONAL VERSION. Healthy infants should be seen by their doctor often during the first year of life. Preventive health care visits (also called well-child visits) typically take place within a few days after birth or by 2 weeks of age and at 1, 2, 4, 6, and 9 months of age. During these visits, the doctor uses age-specific guidelines ...
Children have more well-child visits when they are younger. This is because development is faster during these years. Each visit includes a complete physical exam. At this exam, the health care provider will check the child's growth and development in order to find or prevent problems. The provider will record your child's height, weight, and ...
Sexually transmitted infection (STI) prevention counseling and screening for adolescents at higher risk. Tuberculin testing for children at higher risk of tuberculosis: Age 0 to 11 months , 1 to 4 years , 5 to 10 years , 11 to 14 years , 15 to 17 years. Vision screening for all children. Well-baby and well-child visits.
When will my child's well-baby visits happen? Your baby's first official checkup (and first immunization) will take place at the hospital. After that, well-baby visits are scheduled throughout the first two years at: The first week (usually a couple of days after you're discharged from the hospital) 1 month. 2 months.
During these visits, the doctor examines your child and asks you questions about your child's development and behavior. Immunizations also are either given or scheduled at this time. Your child's doctor will recommend a schedule for well-child visits. One example is for visits at ages: footnote 1. 3 to 5 days old. By 1 month. 2 months. 4 months.
Improving Infant Well-Child VisitsHigh-quality well-child visits can improve children's health, support caregivers' behaviors to promote their children's health, and prevent injury and harm. The American Academy of Pediatrics and Bright Futures recommend nine well-care visits by the time children turn 15 months of age.
Here's a look at what to expect at each stage of the well-child journey. Birth - 2 years old: It's recommended that children have six doctor visits within the first 15 months of life. 3 - 6 years old: Children at this age need a checkup once a year. 7 - 12 years old: Kids this age need a checkup at least once every two years.
child vaccine schedule Birth to 15 Months; Vaccine and other immunizing agents Birth 1 mo 2 mos 4 mos 6 mos 9 mos 12 mos 15 mos; Respiratory syncytial virus (RSV-mAb [Nirsevimab]) 1 dose depending on maternal RSV vaccination status, See notes: 1 dose (8 through 19 months), See notes: Hepatitis B (HepB) 1 st dose: ←2 nd dose→: ←3 rd dose ...
More than half (54%) of children under age 21 enrolled in Medicaid or CHIP received a well-child visit in 2019, but the share fell to 48% in 2020, the start of the COVID-19 pandemic. Despite ...
Apply for a Child Under 16. Both parents or guardians must approve that we can issue a passport to a child, and go with the child to apply in person. If one or both parents or guardians cannot apply with their child, you will need to show us more documents. You cannot renew your child's passport using Form DS-82.
Visit a vaccine provider's online scheduling services to schedule your COVID-19 vaccination appointment. Contact the vaccination provider directly to verify, reschedule, or cancel or with any questions about your appointment. ... Learn how you can support your child and talk to them before they get a vaccine about what to expect.
One in four children under the age of five are experiencing what study authors call "severe food poverty" which means kids are only being fed two or less food groups per day. "It amounts to ...