- Create Account
- Client Portal Login
- 866-211-7866
- Back to Blog page

Electronic medical records (EMRs) vs electronic health records (EHRs)
- May 31, 2024
- Medical , Medical Records , MRR Basics , MRR Security , Technology

Ready to get started with our medical record retrieval services? Choose one of the following options
What are electronic medical records (emrs).
Electronic Medical Records (EMRs) are digital versions of the traditional paper records that have been used in medical practices for decades. These records are created, gathered, managed, and consulted by licensed clinicians and staff from a single organization who are involved in the patient’s health and care. EMRs serve as a digital repository of a patient’s medical history, compiled from one healthcare provider’s interactions. Therefore, they are immensely useful in tracking patient data over time, recording all health-related details including symptoms, diagnoses, procedures, and outcomes within that particular practice or hospital.
The content of EMRs is exhaustive and includes comprehensive data about a patient’s medical history. This includes detailed records of past and current diagnoses, treatments received, and hospitalization records, ensuring that any healthcare provider accessing the record gets a thorough overview of the patient’s medical journey. Furthermore, EMRs contain demographic information such as age, ethnicity, and gender, which aids healthcare providers in tailoring their medical advice and treatments to the specific needs and risks of individual patients.
In addition to historical data, EMRs are crucial for ongoing care management. They contain detailed treatment plans customized for the patient, including prescribed medications, planned procedures, or ongoing therapies. These records ensure continuity of care by maintaining a structured and detailed timeline of the patient’s health status, interventions, and outcomes. This information is pivotal not only for the immediate treatment of acute conditions but also for long-term care management, particularly for chronic diseases.
EMRs are also designed to improve the overall quality of healthcare delivery. They help healthcare providers in identifying patients who are due for preventive screenings and check-ups, manage chronic diseases effectively, and monitor how patients measure up to certain health parameters like blood pressure and vaccination schedules. By enabling quick access to patient records, EMRs facilitate better and faster decision-making processes in clinical settings, enhancing both the efficiency and effectiveness of medical care provided.
What are Electronic Health Records (EHRs)?
Electronic Health Records (EHRs) represent a more integrated and comprehensive approach to managing patient health information compared to Electronic Medical Records (EMRs). EHRs encompass a digital version of a patient’s entire medical history that is maintained and updated by various healthcare providers over time. This system is designed to collect data from and share information across all the clinicians involved in a patient’s care, from general practitioners to specialists and hospital staff. The result is a holistic view of a patient’s health that supports high-quality healthcare delivery regardless of the location or provider.
EHRs are distinguished by their expansive content, which includes not only diagnoses and medications but also treatment plans, immunization dates, patient allergies, radiology images, and laboratory and test results. This comprehensive dataset ensures that every healthcare provider who accesses a patient’s EHR can obtain a full spectrum of the patient’s health data, which aids in making well-informed treatment decisions and managing the overall care more effectively. By consolidating all health-related information into one accessible record, EHRs make critical information readily available in emergencies or routine health checks.

Furthermore, the use of EHRs promotes better healthcare outcomes by enabling a unified, accurate, and up-to-date view of a patient’s medical history. For healthcare providers, the ability to access a complete set of health information supports better clinical decisions, reduces medical errors, and improves patient safety. For patients, EHRs simplify healthcare experiences, reduce redundant paperwork, and help ensure that their medical histories are accurately recorded and easily accessible to authorized clinicians, ultimately leading to better health management and more personalized care.
Key Differences Between EMRs and EHRs
Information source.
- These are sourced from a single provider.
- This means that the data in an EMR is collected and recorded by one specific healthcare provider.
- These are sourced from multiple providers.
- EHRs contain comprehensive health information from all the healthcare providers involved in a patient’s care.
Information Scope
- They focus on a specific provider’s treatment.
- EMRs contain clinical data and treatment records from one specific healthcare provider.
- They provide a comprehensive health history.
- EHRs provide a full record of the patient’s health history, including all doctors’ visits, diagnoses, treatments, and outcomes.
Interoperability
- They have limited data sharing.
- EMRs are generally designed for use by one healthcare provider and are not easily shared with others.
- They are designed for data exchange.
- EHRs are designed to be shared with all authorized healthcare providers, improving coordination and communication.
Intended Users
- These are for individual healthcare providers.
- The primary user of an EMR is the healthcare provider who created it.
- These are for all authorized healthcare providers.
- EHRs are accessible to all healthcare providers involved in a patient’s care, including doctors, nurses, pharmacists, and specialists.
Legal Implications
- Data privacy can be less complicated with EMRs as the information is typically only shared within one healthcare provider’s system.
- However, requests for records could be more complex due to the limited scope of information.
- With their wider scope and accessibility, EHRs may pose more complex data privacy challenges.
- However, they can simplify record requests due to their comprehensive nature.
Considerations for Medical Record Providers
Selection between emr and ehr systems.

EMRs, however, have limitations in their scope of utility, primarily because they do not readily share information with other health systems. This means that if a patient is referred to a specialist or needs to visit an emergency department outside of their primary care office, their EMR might not be available to the healthcare professionals in those other settings. This can create gaps in the continuity of care, where each provider might only have a partial view of the patient’s health history, potentially leading to redundant testing and variable treatment approaches.
In contrast, EHR systems provide a more comprehensive picture of a patient’s health by integrating records from all the clinicians involved in a patient’s care. EHRs extend beyond collecting and storing clinical data from one organization; they facilitate a broader spectrum of healthcare activities including management and sharing of information across different healthcare facilities. This can include specialists, laboratories, and inpatient facilities, thus ensuring that every member of the healthcare team, regardless of their location, has access to the most complete and up-to-date information.
The decision to choose between an EMR and an EHR system depends largely on the scope and nature of a healthcare provider’s practice. For those operating within a closed network or single practice, an EMR might be sufficient. However, for integrated healthcare settings where patient care involves multiple providers across various specialties, an EHR system is indispensable. EHRs not only enhance interoperability and communication across different health care providers but also improve patient outcomes by providing a holistic view of the patient’s health, leading to more coordinated care and better health management.
Relevant Regulations and Standards for EMR/EHR Adoption
When healthcare providers adopt Electronic Medical Records (EMR) and Electronic Health Records (EHR) systems, they must navigate a complex landscape of regulations and standards designed to ensure the privacy, security, and effective use of electronic health information. One of the primary regulatory frameworks that both EMR and EHR systems must adhere to is the Health Insurance Portability and Accountability Act (HIPAA). HIPAA is pivotal as it protects patient privacy by setting standards for the secure handling of health data. This legislation mandates that all healthcare providers, payers, and their business associates who handle personal health information maintain rigorous security measures to protect data both in storage and transit, thus safeguarding patient information from unauthorized access and breaches.
In addition to HIPAA, the adoption and use of EHR systems are also guided by the “Meaningful Use” standards established by the Centers for Medicare & Medicaid Services (CMS). These standards are part of an incentive program that encourages healthcare providers to use EHR technology in ways that can be measured significantly in quality and in quantity. The program outlines specific criteria that providers must meet to qualify for incentive payments, which include improving patient care, ensuring privacy and security of patient information, and engaging patients and their families in their health care. By complying with Meaningful Use criteria, healthcare providers can not only improve their operational efficiency but also enhance the quality of care they provide.
The Meaningful Use program is implemented in several stages, each with its own set of criteria and goals. The first stage focuses on data capture and sharing, the second on advancing clinical processes, and the third on improving health outcomes. Each stage builds on the previous one, promoting an incremental implementation of advanced EHR capabilities. For healthcare providers, meeting these stages involves significant planning and investment in technology, training, and process modification. However, the benefits of adhering to these standards go beyond financial incentives; they contribute to a more robust healthcare infrastructure that supports better patient outcomes and greater efficiency.
Overall, the regulatory landscape for EMR and EHR systems is designed to balance the technological advances in healthcare with the need to protect patient information and improve health outcomes. HIPAA compliance ensures that patient data remains confidential and secure, while the Meaningful Use program motivates providers to harness the full potential of EHR technology. For healthcare systems and providers, understanding and adhering to these regulations is not just about legal compliance but also about embracing opportunities to enhance care delivery and operational effectiveness.
Data Security and Privacy Considerations
In the realm of healthcare, where the confidentiality and security of patient information are paramount, employing stringent data security measures in EMR (Electronic Medical Records) and EHR (Electronic Health Records) systems is crucial. One of the fundamental aspects of safeguarding digital health information is data encryption. Encryption should be applied to data at rest as well as data in transit. Data at rest refers to any data that is stored physically in any digital form such as databases, spreadsheets, archives, and so forth. Data in transit, on the other hand, involves data actively moving from one location to another such as across the internet or through a private network. Encrypting these data ensures that sensitive healthcare information remains unreadable and secure from unauthorized access, thus preserving patient confidentiality even in the event of a data breach.
Moreover, robust access controls are essential to maintaining the security and privacy of EMR and EHR systems. Effective access controls ensure that only authorized personnel, such as healthcare providers or administrative staff who need to view or manage patient information as part of their duties, can access EMR and EHR systems. These controls often include a combination of passwords, user IDs, and more sophisticated measures such as biometric verification systems like fingerprint or retina scanners. Such multi-factor authentication methods significantly enhance the security level, minimizing the risk of unauthorized access and potential data leaks.
In addition to encryption and access controls, implementing regular audits is a key strategy for enhancing data security in healthcare information systems. Regular audits help in the early detection of any unauthorized access or abnormal activities within EMR and EHR systems. These audits, which can be automated or manually conducted, should be a pivotal part of an organization’s overall risk assessment framework. They serve not only to spot immediate issues but also to evaluate the effectiveness of existing security measures and identify areas for improvement.
Continuous monitoring and evaluation through these audits allow healthcare organizations to stay ahead of potential security threats. By regularly assessing how information is accessed and used, organizations can quickly adapt to new threats or changes in the regulatory landscape. Additionally, audits provide valuable insights into user behaviors and system vulnerabilities, which can then be addressed through updated policies or enhanced security protocols.
Furthermore, all these security measures—encryption, access controls, and regular audits—must be complemented by comprehensive training programs for all staff members. Education on best practices for data security, understanding the common tactics used by cyber attackers, and recognizing the importance of safeguarding patient information are all critical components of a successful security strategy. Regular training ensures that all employees are aware of their roles in maintaining data security and are equipped to handle sensitive information properly.
Ultimately, while EMR and EHR systems offer significant benefits to healthcare delivery and management, they also raise substantial challenges in terms of data security and privacy. The combination of strong encryption, stringent access controls, frequent audits, and thorough staff training creates a robust defense against potential security threats. These practices are essential not only for compliance with legal standards like HIPAA but also for maintaining the trust of patients and the integrity of the healthcare system.
Considerations for Attorneys
Importance of understanding emr vs. ehr for attorneys.

The differences between EMRs and EHRs can significantly impact the amount and type of information available for any given case. EMRs, while detailed, are limited to the data collected by one provider and might not reflect other medical interactions or treatments the patient has received elsewhere. This can result in a fragmented view of the patient’s health, potentially overlooking critical elements related to the case. EHRs, however, provide a more holistic view, offering insights into the patient’s complete medical journey. This comprehensive data can prove crucial in constructing a robust case, especially in situations where the full scope of a patient’s medical history, including all treatments and interventions by various health professionals, is pertinent.
For attorneys, grasping these nuances is essential not only for effectively retrieving and analyzing medical records but also for anticipating challenges related to privacy, data completeness, and interoperability issues. In litigation, where the stakes are high, the ability to access and interpret a complete medical history through EHRs can enhance an attorney’s capability to provide thorough representation. Understanding whether information comes from an EMR or an EHR can also guide legal strategies, particularly in determining the reliability and relevance of the medical information in supporting a client’s case. This knowledge is key in leveraging medical records to their fullest potential in the legal process, ensuring that all relevant health data is considered in decision-making and advocacy.
Potential Legal Issues Related to EMR/EHR Use
The integration of Electronic Medical Records (EMR) and Electronic Health Records (EHR) into healthcare practices, while streamlining data management and patient care, introduces several potential legal challenges. Among the foremost concerns are data breaches, which pose a significant threat due to the sensitive nature of the information contained within these systems. When security measures fail or are circumvented, sensitive patient information can be exposed, leading to serious privacy violations. Such data breaches not only jeopardize patient trust but also expose healthcare providers and institutions to potential lawsuits and substantial penalties under regulations like HIPAA. The legal repercussions of a data breach can be severe, involving hefty fines, increased scrutiny from regulators, and long-term damage to a facility’s reputation.
In addition to data breaches, EMR and EHR systems can also be sources of legal issues due to incomplete or inaccurate records. These records are critical in the medical field, not only for ongoing patient care but also in the context of legal investigations and medical malpractice cases. Inaccuracies—whether missing information, erroneous entries, or outdated data—can significantly impact the outcome of such litigation. Inaccurate or incomplete records may lead to wrongful judgments about the standard of care provided, potentially resulting in unjust malpractice claims against healthcare providers. Furthermore, these records are often pivotal in litigation, serving as evidence to either support or contest claims regarding the appropriateness of the medical interventions undertaken.
Given these risks, it’s crucial for healthcare organizations to implement robust systems and protocols to ensure the accuracy, completeness, and security of EMR and EHR data. Legal professionals, on the other hand, must be adept at navigating these records, understanding their creation, maintenance, and potential pitfalls. For attorneys, this means not only scrutinizing the records in the context of ongoing cases but also advising healthcare clients on best practices for mitigating risks associated with EMR and EHR usage. This dual approach helps in safeguarding sensitive patient data and ensuring that the records can withstand legal scrutiny when invoked during litigation.
Importance of Knowing How to Request and Interpret EMR/EHR Data Effectively
For attorneys engaged in healthcare-related litigation, mastering the art of requesting and interpreting EMR (Electronic Medical Records) and EHR (Electronic Health Records) data is essential. These digital records are replete with detailed medical information that can be critical in building a case, be it in defending a medical practice or advocating for a patient’s claims. Properly accessing these records requires an understanding of not only the legal protocols surrounding their release but also the technical aspects of how the data is stored and managed. Furthermore, effective interpretation of this data ensures that attorneys can fully understand the nuances of a patient’s medical history, which often holds the key to establishing the facts of the case.
A thorough understanding of EMR and EHR systems enables attorneys to accurately interpret complex medical histories and identify pertinent information that could influence the outcome of litigation. Misinterpretations or oversight of crucial data can lead to flawed representations of the health issues involved, potentially skewing the case results. Therefore, it’s imperative for legal professionals to be adept at analyzing these records to discern a comprehensive and factual account of the medical events that transpired. This capability not only enhances the attorney’s argument but also ensures that all decisions made are well-informed and based on concrete evidence presented through the medical records.
Moreover, this expertise assists attorneys in ensuring that all relevant information is properly included and accurately represented during litigation. It helps in preemptively identifying any inconsistencies or gaps in the medical data that could be exploited or questioned during legal proceedings. Additionally, being skilled in EMR and EHR data interpretation aids attorneys in advising healthcare providers on how to maintain compliance with legal standards and protect patient information effectively. Thus, the ability to proficiently navigate, request, and interpret EMR and EHR data is invaluable, as it directly impacts the integrity of the legal process and the protection of patient rights in the complex interplay of healthcare and law.
About The Author

Understanding national record retrieval for medical-based litigation
Ensure HIPAA compliance by following these 7 strategies
- Privacy Policy
- Website by Growth Connect

September 16, 2021 | Net Health
10 min read
Electronic Health Records: A Comprehensive History of EHR Systems
Today, it’s easy to think of electronic health records (EHRs), also known as electronic medical records (or EMR software) as just a substitute for paper record-keeping. As a prominent EHR software company , we know otherwise. EHR systems represent an area of healthcare technology that has seen an overhaul since its inception.
The truth is , great advances have been made in the healthcare information field, combined with a rich history, and electronic medical record companies have evolved, changing electronic medical record management. With this in mind, lets take a look at EHR systems by looking at the start of EHR software, its mainstream adoption and digitization.
Before we five into the a comprehensive history of EHR systems, lets answer one important question: what is an EHR?
What is an EHR?
Before diving into the history of the EHR system (or EMR systems ) it makes sense to ask the high-level, potentially obvious question: what is an EHR? What is the definition of electronic health record?
We will define Electronic Health Record (EHR) as a digital version of a patient’s comprehensive medical history. Designed to be shared and updated over time, an EHR system securely maintains patient information across different healthcare providers, including physicians, specialists, and pharmacies.
The EHR system encompass a patient’s medical history, medical health information, diagnoses, medications, immunization dates, radiology images, lab results, and even demographic data, all of which are vital for medical practices making informed healthcare decisions.
EHRs are much more than digitized paper records; they’re dynamic, interactive systems designed to improve efficiency and accuracy. Software from top EHR companies offer real-time access to patient data, facilitating communication among different healthcare providers for collaborative treatment.
From streamlining administrative tasks to enhancing patient care, EHR systems have become an indispensable tool in modern healthcare practice. With the “what is an EHR?” question and context out of the way, lets dive in to the history of electronic medical records and EHR software systems and how they became crucial to recording patient’s medical history, reducing medical errors, protecting patient records and securing patient data and overall how the electronic health record systems have revolutionized how healthcare professionals capture clinical data.
Electronic Health Records ( EHRs ): The Early Days
The history of EHRs and EMR companies began in the 1960s – the Mayo Clinic in Rochester, Minnesota was one of the first major health systems (among a select few other healthcare providers) to adopt an EHR 1 and move away from the massive swath of healthcare organizations keeping paper medical records. to adopt an EHR. 1 In the 1960s, EMR programs and EHRs were so expensive that they were only used by the government in partnership with health organizations.
Throughout the 1970s, only the biggest hospitals could use them, and they were used for billing and scheduling and keeping basic personal health records for patients.
At the same time, during the 1960s, a new approach to patient records (still on paper) began to emerge. Referred to as the “problem-oriented” patient record, this approach added more robust information about the patients and over time evolved to become the version of electronic medical record we see today.
This approach was a breakthrough in medical recording. Previously, doctors had typically only recorded a patient’s diagnosis and the treatment they provided, but it ended there.
As part of the “problem-oriented” medical record, clinicians began collecting and storing data about a patient’s history. When properly implemented, this model provided health care providers with a more effective means of communication among members of healthcare teams, while also facilitating the coordination of preventive care and maintenance.
A s EHRs and EMR software programs became more affordable and available in the 1980s, they were developed with fields that could be filled in with clinical information and stored as an electronic health record.
How Portable Medical Records Became Electronic Health Records
With portability came the dawn of the computer era hospital management systems began to change. Many of the earliest computer applications in the 1970s were in use at hospitals and government institutions, but scarcely elsewhere. At first, these applications were used predominantly for billing and scheduling purposes, and not EHRs specifically. 2
Then, thanks to the portable records model, large hospitals started to provide the same level of service for each patient without worrying that only specific providers had knowledge of that patient.
Computers, of course, really didn’t gain traction in smaller clinics and private practices until they became popular with the general public. Therefore medical charting systems were recorded manually until then. At this time we began seeing more on digital medical records and the idea of EHR systems.
Before the 1980s, it was rare to see a computer used at all in private practice, let alone for storing EMR or electronic health information and sensitive personal information (SPI).
Even though the portable record-keeping system of keeping patient medical history had become far more commonplace, records were still largely paper, which meant health records had to be physically stored and moved.
Business technology then became advanced enough that even paper records could be sent electronically, via fax, in cases where an office needed to get in touch with a patient’s family doctor in case of urgent care.
But, time is often of the essence in caregiving scenarios, and because of this, the electronic health record system of storing electronic patient data became the standard. Medical providers realized that in every medical specialty, from urgent care to rehab, from hospital to home, there were always unique cases that had to be resolved electronically.
This is where EHR development accelerated, influencing treatment plans and leveraging healthcare information at healthcare facilities across various care settings, from practice management to larger institutions of public health and preventative services. It was at this point that EHR adoption or the widespread adoption of EMR systems was here to stay.

The Internet and the Rise of the EHR
By the 1990s, technology had entered most medical offices, and computers were being used to a limited degree for record-keeping purposes. Specifically, EHRs were mostly seen record patient data at academic inpatient and outpatient medical facilities, and they included patient data interchange for claims processing and image scanning for document capture of medical histories. 3
It wasn’t until the internet-age that large-scale changes became far more visible on the front of electronic health record keeping. Even in its early stages, the internet became a vital tool for recording and transferring prescription histories and other electronic medical records.
Finally, within the last decade or so, most major medical systems in the developed world could easily communicate with each other when needed. Electronic health record software is no longer a luxury, but necessary for optimal patient care and HIPAA compliance.
Electronic Health Records Today and the Future
In 2004, President George W. Bush created the Office of the National Coordinator for Health Information Technology, which outlined a plan to ensure that most Americans had electronic health records within the next 10 years. 4
Additionally, these records were designed for medical practices and healthcare providers to:
- Share information privately and securely with the patient’s authorization in an accessible patient portal
- Help health care quality, prevent medical errors and reduce paperwork
- Improve administrative efficiencies and health care quality for health and human services
As it is now, EMR software and EHR systems are increasingly paperless, although some private practices continue to use a combination of paper-based and computerized records. Patient medical records are more accessible than ever before, while also safely stored, with data technology becoming increasingly portable and comprehensive.
Current refinements in the EMR industry and as such, the electronic health record system, are aimed at the continued specialization of EHR systems to further streamline workflows, boost productivity and improve doctor-patient interactions. And so, it seems that EHRs will continue to make a mark in the healthcare industry for years to come. EHRs and electronic medical record implementation can also assist with things such as patient engagement, EHR documentation, improving patient outcomes, and even extends into occupational health EMR software .
After several years of developing electronic health record software solutions securely transmitting clinical data via electronic communication for a variety of healthcare organizations, Net Health understands the importance of electronic health records and is now leveraging the data within its specialized EHRs to provide insights that improve clinical decision-making through predictive healthcare analytics , driven by predictive analytics algorithms. It can also help healthcare informatics, revenue cycle management, patient engagement,
EHR systems have become integral in nursing and other healthcare fields, underscoring why electronic medical records are important. In closing summary, these systems streamline the management of patient information, ensuring healthcare professionals have real-time access to vital data. Different types of EHR systems cater to various healthcare settings, from hospitals to private practices.
Examples include occupation-specific platforms like occupational health software programs, practice management tools or physical therapy EMR software . Our electronic health records for therapists can efficiently manage disparate employee medical data, improving overall healthcare delivery, thanks to the computerization of health records, keeping vital health information and personal health records safe and secure. The cloud based EHR is crucial to quality care for most physicians. From individual patients to public health as a whole, this system of storing computer records has become the standard for quality improvement of healthcare facilities.
The evolution of electronic health records has led to specialized occupational health EMR software, physical therapy EHR software and wound care EHR software , among others, designed to meet specific industry needs. Such EHR systems and EMR software enhances the efficiency of medical practitioners by providing comprehensive electronic medical records software solutions.
These tools are vital for healthcare organizations in managing patient information, scheduling, and ensuring effective practice management. The advancements in EHR systems technology have made it possible to integrate various healthcare systems, allowing for seamless communication and coordination among healthcare providers, ultimately leading to improved patient care, while securely protecting health data and patient personal health information
Conclusions on The History of Electronic Health Records
Understanding the essence of Electronic Health Records (EHRs) requires deciphering the foundational terminology. EHR systems meaning extends beyond mere digital versions of patient paper charts; they represent a comprehensive platform where a patient’s medical history, diagnoses, medications, treatment plans, immunization dates, allergies, and test results are securely stored and easily accessible to authorized healthcare providers. The EHR meaning encompasses a holistic view of a patient’s health journey, enabling a seamless flow of information and facilitating better patient care.
The transition to what is an EHR platform is not just a technological upgrade but a significant shift in healthcare management. Successful EHR implementation is crucial for enhancing patient care, improving diagnosis accuracy, and ensuring the efficient operation of healthcare facilities.
However, the journey towards a successful EHR implementation project involves meticulous planning, staff training, and adapting workflows to integrate new digital tools effectively. By emphasizing the critical steps of EHR implementation, healthcare providers can navigate the complexities of this digital transformation, ensuring that the project delivers its intended benefits of improved patient outcomes and healthcare efficiency.
Are you looking for electronic medical records software vendors? The financial incentives are numerous when choosing the right EHR for storage of medical information. To learn more about the key features EMR systems should contain, to see an electronic health record example (EHR example) or to learn about how specialized electronic health record software and care setting tailored cloud based EHR systems can boost your revenue , inform treatment plans, improve patient outcomes and maximize efficiencies all while providing cost savings, schedule a demo with Net Health today.
References:
1 Becker’s Hospital Review, “A History of EHRs: 10 Things to Know,” February 16, 2015. 2 & 3 National Center for Biotechnology Information, “ Electronic Health Records: Then, Now, and in the Future,” May 20, 2016. 4 The White House Archives, “Transforming Health Care: The President’s Health Information Technology Plan,” 2004.
Subscribe and See More
Net Health is a trusted partner for over 25,000 healthcare organizations spanning the continuum of care.
Related Insights

Physical Therapy Billing Units: A Comprehensive Guide

The Critical Role of Patient-Reported Outcome Measures in Rehab Therapy

Types of Wounds Healthcare Professionals Should Know

Navigating MIPS Compliance: Tips for Medicare Wound Care Providers

Become a Healthcare Ally: Create a Positive Rehab Therapy Experience for LGBTQ+ Patients

Understanding Wound Debridement: Essential Insights for Today’s Treatments
Important Update: Product Naming Changes Coming Soon! Click Here
The development of electronic health records

The question of who invented electronic health records ( EHRs ) actually has many answers, but the development of EHRs can be traced back to the early 1960s. Traditionally, patient medical records had been kept on paper, in files. Those files were marked with various identifying information, often including the patient’s last name and an ID number, which may have contained part or all of the patient’s Social Security number. Those files were kept in cabinets or on shelves designed especially for medical records.
In the 1960s, Larry Weed, an American physician, researcher, educator, and entrepreneur, developed the Problem Oriented Medical Record. With this, Weed introduced the idea of electronically recording and maintaining patient data. Weed may be identified as the person who invented electronic health records themselves. In 1972, however, the first electronic medical record (EMR) system was developed by the Regenstrief Institute, according to the University of Scranton . Regenstrief’s EMR system was expensive and so was not attractive to physicians for use with their patients. The system was used, though, “by government hospitals and visionary institutions.”
As the personal computer became more common and more affordable, and as the Internet developed, EHR innovations also developed. Web-based EHRs started to emerge. In 1991, the Institute of Medicine ( IOM ), a division of the National Academies of Sciences, Engineering, and Medicine, led the way toward computer-based patient records by sponsoring studies and reports on the relatively new concept.
Throughout their development, EHRs have been identified by many names, including electronic medical records, computerized medical records, longitudinal patient records, and electronic charts. A Pearson Higher Ed publication states that “in 2003, the IOM chose the name electronic health records, or EHR, because ‘health’ means ‘a state of well-being.’”
The IOM subsequently established eight core functions that should be performed by an EHR, including:
- Health information and data
- Result management
- Order management
- Decision support
- Electronic communication and connectivity
- Patient support
- Administrative processes and reporting
- Reporting and population health
According to Pearson, these “eight core functions … became determining factors in the evolution of EHR, and the ability to perform these functions is the criteria by which EHRs are judged.”
Download Our Free EHR Buyers Guide to Learn More

© 2024 Elation. All Rights Reserved
Understanding the Patient Journey: Working Towards Integrated Medical Records
- Conference paper
- First Online: 06 November 2022
- Cite this conference paper

- Christine O’Dell 3 &
- Sandra Gabriele 3
Included in the following conference series:
- Congress of the International Association of Societies of Design Research
158 Accesses
The lack of an integrated medical record can cause frustration for both patients and healthcare professionals. Due to the decentralised and compartmentalised nature of healthcare systems, records are fragmented and reside on multiple, unconnected information platforms. Currently, healthcare providers are responsible for maintaining records, giving patients limited control of their health information. This study demonstrates the value of visualisation to understand the patient experience and the current state of the healthcare system. The data from in-depth semi-structured interviews and a journey mapping exercise with six healthcare practitioners and six patients revealed pain points, positive aspects, and opportunities for improving the patient experience. We combined the data points to create a service blueprint, exposing five areas of concern: communication, care, control, repetition, and privacy. The results from this study can serve as the foundation for developing design interventions to improve how patient medical records can be securely controlled, accessed, and shared.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Get 10 units per month
- Download Article/Chapter or Ebook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Similar content being viewed by others

Health Services Information: Personal Health Records as a Tool for Engaging Patients and Families

Persisting workarounds in Electronic Health Record System use: types, risks and benefits
Archer, N., Fevrier-Thomas, U., Lokker, C., McKibbon, K.A., Straus, S.E.: Personal health records: a scoping review. J. Am. Med. Inform. Assoc. 18 (4), 515–522 (2011)
Article Google Scholar
BC Patient Safety & Quality Council: Journey mapping in cancer care: patient and provider experiences in receiving and delivering cancer care in British Columbia (2019). https://bcpsqc.ca/wp-content/uploads/2019/01/Journey-Mapping-Cancer-interactive.pdf . Accessed 20 May 2021]
Borycki, E.M., Kushniruk, A.W., Wagner, E., Kletke, R.: Patient journey mapping: integrating digital technologies into the journey. Knowl. Manag. E-Learn. Int. J. 12 (4), 521–535 (2020)
Google Scholar
Braun, V., Clarke, V.: Qualitative research in psychology using thematic analysis in psychology. Qual. Res. Psychol. 3 (2), 77–101 (2006). http://www.tandfonline.com/action/journalInformation?journalCode=uqrp20 . Accessed 14 Jan 2020
Buchanan, R.: Wicked problems in design thinking. Des. Issues 8 (2), 5–21 (1992). https://doi.org/10.2307/1511637 . Accessed 25 Jan 2020
Canada Health Infoway: Annual Report 2017–2018 (2018). https://www.infoway-inforoute.ca/en/component/edocman/resources/i-infoway-i-corporate/annual-reports/3556-annual-report-2017-2018.pdf . Accessed 28 Sept 2021
Chang, F., Gupta, N.: Progress in electronic medical record adoption in Canada. Can. Fam. Physician 61 (12), 1076–1084 (2015)
Consumers Health Forum of Australia: The real people real data toolkit (n.d.). https://chf.org.au/sites/default/files/docs/rprdtoolkit.pdf . Accessed 1 Oct 2019
Crosier, A., Handford, A.: Customer journey mapping as an advocacy tool for disabled people: a case study. Soc. Mark. q. 18 (1), 67–76 (2012)
Dorst, K.: Design beyond design. She Ji 5 (2), 117–127 (2019). https://doi.org/10.1016/j.sheji.2019.05.001 . Accessed 25 Jan 2020
Gibbons, S.: Journey Mapping 101 (2018). https://www.nngroup.com/articles/journey-mapping-101/ . Accessed 30 May 2021
Harvard School of Public Health: Electronic vs. personal health record: What’s the Difference? (2008). https://www.hsph.harvard.edu/news/magazine/fall08ehrpersonalvshealth/ . Accessed 1 June 2021
Hillestad, R., et al.: Can electronic medical record systems transform health care? Potential health benefits, savings, and costs. Health Aff. 24 (5), 1103–1117 (2005). https://doi.org/10.1377/hlthaff.24.5.1103 . Accessed 4 Feb 2020
Jodi, A.: A pragmatic view of thematic analysis. Qual. Rep. 2 (1), 4–5 (1994). https://nsuworks.nova.edu/tqr/vol2/iss1/3 . Accessed 16 Jan 2020
Jones, P.: The systemic turn: leverage for world changing. She Ji, 157–163 (2017). https://doi.org/10.1016/j.sheji.2017.11.001 . Accessed 28 Jan 2020
Kimbell, L.: Insights from service design practice. Paper presented at the 8th European Academy of Design Conference, Aberdeen, Scotland, 1–3 April 2009. http://www.lucykimbell.com/stuff/EAD_kimbell_final.pdf . Accessed 7 June 2021
Lifelabs: LifeLabs releases open letter to customers following cyber-attack (2019). https://www.lifelabs.com/lifelabs-releases-open-letter-to-customers-following-cyber-attack/ . Accessed 8 Mar 2020
McCarthy, S., O’Raghallaigh, P., Woodworth, S., Lim, Y.L., Kenny, L.C., Adam, F.: An integrated patient journey mapping tool for embedding quality in healthcare service reform. J. Decis. Syst. 25 (sup1), 354–368 (2016)
Meyer, M.A.: Mapping the patient journey across the continuum: lessons learned from one patient’s experience. J. Patient Exp. 6 (2), 103–107 (2019)
Micheaux, A., Bosio, B.: Customer journey mapping as a new way to teach data-driven marketing as a service. J. Mark. Educ. 41 (2), 127–140 (2019)
Oliveira, L.C., Birrell, S., Cain, R.: Journey mapping from a crew’s perspective: Understanding rail experiences. Appl. Ergon. 85 , 103063 (2020)
Ontario Ministry of Health and Long-Term Care: 2016–17 Published Plans and 2015–2016 Annual Reports (2016). http://www.health.gov.on.ca/en/common/ministry/publications/plans/ppar16/ . Accessed 2 Feb 2020
Ontario Ministry of Health and Long-Term Care: Hallway health care: a system under strain – first interim report from the premier’s council on improving healthcare and ending hallway medicine (2019). http://www.health.gov.on.ca/en/public/publications/premiers_council/report.aspx . Accessed 2 Feb 2020
Park, H., Monkman, H., Wenger, A., Lesselroth, B.: Portrait of Ms. Diaz: empirical study of patient journey mapping instruction for medical professional students. Knowl. Manag. E-Learn. 12 (4), 469–487 (2020). https://doi.org/10.34105/j.kmel.2020.12.026 . Accessed 28 May 2021
Penin, L.: Designing the Invisible. Bloomsbury Publishing PLC, London (2018)
Price, M., Singer, A., Kim, J.: Adopting electronic medical records: are they just electronic paper records? Can. Fam. Physician 59 (7), e322–e329 (2013)
Qiao, Y., Asan, O., Montague, E.: Factors associated with patient trust in electronic health records used in primary care settings. Health Policy Technol. 4 (4), 357–363 (2015)
Roehrs, A., Da Costa, C.A., da Rosa Righi, R., De Oliveira, K.S.F.: Personal health records: a systematic literature review. J. Med. Internet Res. 19 (1), e13 (2017)
Rosenbaum, M., Otalora, M., Ramírez, G.: How to create a realistic customer journey map. Bus. Horizons 60 (1), 143–150 (2017). https://doi.org/10.1016/j.bushor.2016.09.010 . Accessed 1 June 2021]
Samson, S., Granath, K., Alger, A.: Journey mapping the user experience (2017). [online] Available at: [Accessed 30 May 2021]
Stickdorn, M., Lawrence, A., Hormess, M., Schneider, J.: This is Service Design Doing: Applying Service Design Thinking in the Real World. O’Reilly Media, Inc., Sebastopol (2018)
The Canadian Medical Protective Association: Who owns the medical record? (2018). https://www.cmpa-acpm.ca/serve/docs/ela/goodpracticesguide/pages/communication/Documentation/who_owns_the_medical_record-e.html . Accessed 20 May 2021
The Government of Canada: Canada’s Health Care System (2019). https://www.canada.ca/en/health-canada/services/health-care-system/reports-publications/health-care-system/canada.html . Accessed 15 Sept 2021
Tikkanen, R., Osborn, R., Mossialos, E., Djordjevic, A., Wharton, G.: International Profiles of Health Care Systems (2020). https://www.commonwealthfund.org/sites/default/files/2020-12/International_Profiles_of_Health_Care_Systems_Dec2020.pdf . Accessed 15 Sept 2021
Vaismoradi, M, Jones, J., Turunen, H., Snelgrove, S.: Theme development in qualitative content analysis and thematic analysis. J. Nurs. Educ. Pract. 6 (5), 100–110 (2016). https://doi.org/10.5430/jnep.v6n5p100 . Accessed 16 Jan 2020
Vaismoradi, M., Turunen, H., Bondas, T.: Content analysis and thematic analysis: implications for conducting a qualitative descriptive study. Nurs. Health Sci., 398–405 (2013). https://doi.org/10.1111/nhs.12048 . Accessed 18 Jan 2020
Villaespesa, E., Álvarez, A.: Visitor journey mapping at the Museo Nacional Thyssen-Bornemisza: bringing cross-departmental collaboration to build a holistic and integrated visitor experience. Mus. Manag. Curatorsh. 35 (2), 125–142 (2020)
Westbrook, J.I., Coiera, E.W., Gosling, A.S., Braithwaite, J.: Critical incidents and journey mapping as techniques to evaluate the impact of online evidence retrieval systems on health care delivery and patient outcomes. Int. J. Med. Inform. 76 (2–3), 234–245 (2007)
Download references
Author information
Authors and affiliations.
York University, Toronto, Canada
Christine O’Dell & Sandra Gabriele
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Christine O’Dell .
Editor information
Editors and affiliations.
The Hong Kong Polytechnic University, Hung Hom, Kowloon, Hong Kong
Gerhard Bruyns
Rights and permissions
Reprints and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this paper
Cite this paper.
O’Dell, C., Gabriele, S. (2022). Understanding the Patient Journey: Working Towards Integrated Medical Records. In: Bruyns, G., Wei, H. (eds) [ ] With Design: Reinventing Design Modes. IASDR 2021. Springer, Singapore. https://doi.org/10.1007/978-981-19-4472-7_32
Download citation
DOI : https://doi.org/10.1007/978-981-19-4472-7_32
Published : 06 November 2022
Publisher Name : Springer, Singapore
Print ISBN : 978-981-19-4471-0
Online ISBN : 978-981-19-4472-7
eBook Packages : Literature, Cultural and Media Studies Literature, Cultural and Media Studies (R0)
Share this paper
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Next Application Deadline: August 2
Home > Resources > Health Informatics > What are Electronic Medical Records (EMRs)?
What are Electronic Medical Records (EMRs)?

- Published February 16, 2017
- Updated May 2, 2024
Electronic medical records (EMRs) are the digital equivalent of a patient’s paper-based records or charts at a clinician’s office. The term ‘EMR’ stands not only for the digital medical content but also for the broader system that captures, stores and assists in the management of a patient’s healthcare information. EMRs typically contain general information such as comprehensive medical history, diagnoses, medications, allergies, lab results and treatment plans for a patient as collected by the individual medical practice.
This post delves deeper into the meaning and scope of EMRs, explores their multifaceted advantages and answers common questions that arise in the context of modern healthcare technology.
What do Electronic Medical Records Mean in Healthcare?
The shift in patient record management from paper to digital has been a boon for improving healthcare organizations’ efficiencies. EMRs are one of the initiatives that have helped the healthcare industry embrace the digital age in a meaningful way.
The motivation for the move from paper-based records to EMRs stems from the critical need for readily accessible and accurate health information that supports real-time, informed decision-making in patient care.
What are Electronic Medical Records Used For?
EMRs are used for a variety of purposes by healthcare organizations and providers. Some of these purposes include:
- Centralized patient information – Consolidated patient information enables healthcare providers to gain a more comprehensive view of a patient’s health and make well-informed decisions.
- Coordination among professionals – Physicians, specialists and other healthcare professionals can access a patient’s EMR to coordinate better care options and boost consistency and transparency during patient care.
- Prescription management – Healthcare providers can send electronic prescriptions to pharmacies reducing the risk of errors and boosting the prescription management process.
Overall, EMRs are generally used for enhancing patient care, improving communication and collaboration among healthcare professionals in a single practice, optimizing workflow efficiencies and facilitating data-driven decision-making for patients.
Benefits of EMR Implementation for Healthcare Providers
Healthcare providers and organizations reap many benefits from the implementation of EMRs into their workflows and processes. Some include:
- Enhanced Patient Care : EMRs provide holistic and up-to-date information about patients at the point of care.
- Quick Access to Patient Records : Health professionals can access patient records quickly, thus speeding up decision-making processes.
- Accurate and Complete Documentation : The electronic format reduces the risk of data transcription errors and incomplete records.
- Secure Sharing of Information : EMRs enable secure sharing of data with authorized users across different healthcare settings.
- Improved Patient Participation : Patients can easily access their health records, leading to more involvement in their care.
- Efficiency and Productivity : With less time spent managing paper records, healthcare providers can streamline administrative tasks and focus more on patient care.
- Support for Diagnosis and Treatments : Advanced analytics and decision-support tools in EMRs can assist in diagnosis and establishing treatment protocols.
- Reduced Costs : Over time, EMRs can lead to cost savings through decreased paperwork, improved safety, reduced duplication of testing, and improved health.
What is the Difference Between EMR vs EHR?
An electronic health record (EHR) is also a digital version of a patient chart, but it is a more inclusive snapshot of their medical history. The main difference between EMRs and EHRs is that EHRs are designed to be shared with other providers, so authorized users may instantly access a patient’s EHR from across different healthcare providers.
The difference in transferability and shareability between these two patient data management tools illustrates the roles they each play to organizations and providers. EMRs are utilized primarily by one single practice and the different professionals present in that practice, whereas EHRs can “follow” patients wherever they go across providers and practices.
Improving Patient Care with Electronic Medical Records
EMR applications revolutionize patient care by streamlining access to patient medical history, empowering healthcare professionals to deliver personalized patient care more efficiently.
EMR systems are also designed to help patients and their families become more involved in the healthcare process. One example of this is seen when clinical summaries, available for more than half of all visits, are sent to patients within three business days. Each summary contains comprehensive and overarching information about the care provided during the visit and actively encourages participation from patients and their family members in the patient care offering process.
Patients can also become more involved in their care by exploring patient-specific education resources. EMR systems will provide links to articles, videos, and images that can help patients better understand their specific healthcare situation. With this technology, patients can make more informed decisions about medical procedures and lifestyle adjustments.
Using EMR systems, patients can quickly and easily receive electronic copies of their healthcare information upon request. In the event they choose to change healthcare providers, the universal detailed medical record will help give the patients’ new healthcare provider a comprehensive understanding of their medical history and current state of health. Healthcare facilities will still be able to exchange patient information if the patient does not request it.
Deeper Insights: EMR FAQs
What are the 4 types of emrs.
The four types of EMRs often discussed in the field include:
- On-Premise EMR – Located within the healthcare organization’s server. While these EMRs are traditionally more costly and complex to use, they offer a greater level of data security and personalization for the organization’s needs.
- Application Service Provider – Provided by the healthcare organization’s vendor’s server. This is a more cost-efficient EMR option and professionals can access patient data anywhere with an internet connection.
- Software as a Service (SaaS) – Located on the healthcare organization’s vendor’s server. Practices don’t worry about maintenance and these EMRs are updated with the latest versions.
- Cloud-Based – Hosted on the vendor’s servers with browser and web accessibility. While less secure than on-premise EMRs, Cloud-based EMRs offer extended services beyond SaaS EMRs like customer support.
What is an example of an EMR?
An example of an EMR would be the electronic chart in a clinician’s office that contains the medical and treatment history of the patients within the practice. It’s a singular record, confined to one healthcare provider’s domain.
What is the most popular EMR?
Among the array of EMR software available, some top the list for their widespread use and robust feature sets. Epic Systems, Cerner, and Meditech are commonly cited as popular systems leveraged by healthcare organizations.
Foster Your Growth in Healthcare with USF Health
USF Health’s Morsani College of Medicine offers online master’s degrees and graduate certificates in healthcare informatics and health analytics, which are designed to sharpen your skills and knowledge in the healthcare field so you can make a difference in the dynamic, fast-paced healthcare industry.
Students in the Graduate Certificate in Health Informatics program learn the latest processes for electronic storage and secure sharing of vital patient medical records, as well as integrating informatics and clinical sciences with quality patient care. The Graduate Certificate in Healthcare Analytics can provide you with a foundation of knowledge and skills to master the collection, organization and analysis of health data using the analytics life cycle.
These programs serve as a foundation for growing your skills in electronic healthcare data management and help make you a vital part of a healthcare informatics team and a distinguishable candidate in the health informatics job market.
USF Health’s programs have a proven track record of student success stories such as Sabita Maharjan , a graduate of the Master of Science in Health Informatics .
“While working as a medical technologist, I was impressed by how technology made our jobs so much easier through electronic medical records . I was then interested in the technology field while still being associated with healthcare.”
Learn more about the Graduate Certificate in Health Informatics and Graduate Certificate in Healthcare Analytics programs today and start developing skills for your future in healthcare.

Related Articles

Three Resources for Meaningful Use Requirements

What is the HITECH Act?
What Is Informatics? History, Key Areas and Career Options
Academic calendar, get our program guide, if you are ready to learn more about our programs, get started by downloading our program guide now..
How can we help you?
The latest news in Healthcare IT – straight to your inbox.

- Global Edition
A practical guide: Beginning the EMR journey

The migration to electronic medical records offers patients, providers and the overall healthcare system a variety of compelling benefits and cost reductions — but we shouldn’t underestimate the challenges that stand between the idea of an e-health ecosystem and it becoming a reality.
Specifically, there’s a significant amount of work to be done around privacy, information security, compliance, and identity and payment fraud.
While each sector presents its own unique requirements and characteristics, the common thread for each is that we must able to:
• Trust in the reliability of the information; • Access, analyze and share the right information with the right people at the right time; • Minimize and mitigate potential risks introduced via cyber-borne threats by using the most advanced privacy and security protection strategies.
As more and more organizations seek to accelerate a conversion, or at least lay the groundwork, for an evolution to electronic medical records, there is no shortage of providers individuals hanging up a shingle in the health information technology (HIT) space.
[Q&A: Between the lines of NEJM's EHR report, 'trust trumps tech' .]
Sorting out the details — let alone the merits — of one offering from another can be a challenge in itself. At a minimum, organizations seeking to expand their HIT operations should seek providers who can deliver:
• Trust Services: An ability to evaluate the people, policy, procedures, and products used to identify, authenticate, and authorize information systems users and to monitor and manage access to data and resources; including identity management, assurance, and National Strategy for Trusted Identities in Cyberspace (NSTIC) compliance. • Trusted Infrastructures: An ability to update operating processes and platforms to ensure confidentiality, integrity, and availability of protected health information Workforce Assurance: Focusing on human capital, learning and development, change management, continuous awareness, and strategic communications.
• Strategic Risk Management: An ability to Identify, prioritize, and mitigate security and privacy risks throughout the enterprise; including enterprise governance and oversight, planning agendas supporting out years, and performance metrics. • Reliable Healthcare Analytics: Enhancing healthcare for individuals and communities via data-driven methodologies; includes risk and fraud analytics and comparative effectiveness intelligence and research.
• Supply Chain Assurance: An ability to analyze supply chain vulnerabilities and to develop and implement monitoring techniques and mitigation strategies. • Data Privacy: An ability to protect critical information assets with a focus on compliance and privacy integration in systems, along with a focus on privacy incident response.
Whether cyber health is helping to improve care delivery; ensure on-demand implementation; expedite clinical trials; or identify, mitigate, and eliminate fraudulent activities, it touches practically every health transformation initiative.
The promise is significant, but so are the challenges tied to it. Organizations that take a practical, pragmatic view of both will be best served.
Ilene Yarnoff is a lead assurance and resilience principal for Booz Allen Hamilton’s healthcare clients. She has proven expertise in providing solutions and programs for effective health information security and privacy management.
More regional news

HIMSSCast: Fighting back against healthcare misinformation in the era of social media and genAI

AI has a role to play during the patient intake process

ONC releases draft USCDI+ dataset for maternal health

White Papers
More Whitepapers
More Webinars

More Stories

- Artificial Intelligence
- Cloud Computing
- Government & Policy
- Interoperability
- Patient Engagement
- Population Health
- Precision Medicine
- Privacy & Security
- Women In Health IT
- Learning Center
- Research Papers
- Special Projects
- In-Person Events
The Daily Brief Newsletter
Search form, top stories.

Discover Zynx for Primary Care today! Learn More!
- Developer Program

Solutions and Services
Enabling caregivers to improve patient outcomes, financial performance, clinical engagement, and technology performance is our top priority.
We help you improve patient outcomes, financial performance, clinical engagement, and technology performance — all resulting in higher quality patient care and lower costs.
Critical analysis and thought leadership by Zynx leaders, COVID-19 guidance, and support.
For over 25 years, Zynx has empowered thousands of healthcare organizations to align their clinical decision support, strategies, and workflows around the standardization of evidence-based best practices.
The Epic Migration Journey: Your Roadmap for a Successful EMR Transition
Start your transformative journey with the Epic migration process. Zynx smooths this crucial transition to the Epic EMR system, leading to better workflows and patient care. This article offers a roadmap with helpful tips for a successful transition. With Zynx, enjoy an efficient migration aimed at enhancing patient care
Embarking on the voyage of digital transformation in healthcare can feel like navigating through an ocean of challenges. Anchoring this journey is the Epic migration process, a pivotal shift from your existing electronic medical records (EMR) system to the industry-leading Epic EMR system . With Zynx by your side, the journey becomes less daunting, akin to sailing from familiar shores towards a land of streamlined workflows, improved patient care, and enhanced compliance.
The Epic migration, supported in part by Zynx, isn’t merely a leap into the unknown. It’s a carefully plotted course, navigated with precision, and guided by a tailored map that balances your present realities with your future goals. The journey is as essential as the destination, necessitating not just a willingness to embrace change but also the preparedness to manage this change effectively.
This article, with the expertise of Zynx, will serve as your compass, illuminating the nuances of the Epic migration process. It will demystify the concept by breaking down the journey into comprehensible stages and offering invaluable tips for migrating order sets and care plans successfully. So, hoist the sails and embark on this transformative journey with us.
Introduction to Epic Migration With Zynx
In the dynamic world of digital healthcare, migrating to the globally recognized Epic EMR system isn’t merely about integrating new technology. It’s a transformative journey that revolutionizes your entire healthcare operations, significantly augmenting workflow efficiencies, patient care, and regulatory compliance.
This strategic leap towards innovation becomes achievable and less daunting with the assistance of Zynx, a trusted partner who understands the complexity and nuances of the healthcare landscape.
Zynx serves as your guide through this significant transition, proficiently handling every intricate detail of the process. They’re more than technical experts; they comprehend the multifaceted nature of healthcare, making them perfectly positioned to facilitate a smooth transition to Epic.
The process isn’t just about relocating data; it’s a digital rebirth for your healthcare operations. From patient registration, managing records, processing lab results, and billing, Epic consolidates all these functions under one unified system.
Crucially, Zynx excels at transferring order sets and care plans to Epic, elements that require meticulous handling. Their expertise ensures seamless integration of these critical components into the new system, thereby enhancing clinical decision making and patient outcomes.
The Importance of Epic Migration With Zynx
The significance of migrating to Epic with Zynx’s assistance cannot be overstated in this digital age. The combined capabilities of Epic and Zynx serve as catalysts for healthcare transformation, helping organizations adapt to changing regulatory demands while providing personalized, evidence-based care. This all-encompassing solution allows your team to function cohesively, with Zynx’s guidance making the transition not just bearable but empowering.
The combination of Epic’s comprehensive patient health history view, robust security measures, and Zynx’s commitment to data confidentiality during migration culminate in an enhanced healthcare delivery model. It’s a win-win scenario that fosters informed clinical decisions, improved patient outcomes, and stringent data security.
Thus, embarking on the Epic migration journey with Zynx paves the way for a complete healthcare transformation. It’s a strategic move that alleviates stress, optimizes efficiency, and ultimately reaps tangible benefits for healthcare providers and their patients. It’s more than a shift; it’s a transformative journey toward superior patient care in the digital era.
Tips for a Successful Migration of Order Sets and Care Plans to Epic With Zynx
Migrating to Epic, particularly order sets and care plans, requires meticulous planning and flawless execution. With Zynx’s expert guidance, your path to a successful transition is brightly illuminated:
1 . Adequate Planning and Preparation: Zynx begins the migration process by conducting a detailed assessment of your current EMR system. They scrutinize every element, particularly the unique considerations for order sets and care plans. By deeply understanding your current system, Zynx formulates a tailored migration strategy that minimizes disruption to healthcare delivery and ensures seamless continuity of care.
2. Building a Competent Team: Zynx’s expertise extends to forming a skilled migration team. Recognizing that the transition affects all aspects of healthcare delivery, it involves a mix of clinicians, IT professionals, and administrative staff. Zynx collaborates closely with your team, providing them with the necessary skills and knowledge to navigate the Epic EMR system effectively.
3. Effective Communication: Zynx takes a proactive approach to communicating during the migration process. They ensure all stakeholders within your organization are informed, address questions, and alleviate concerns. Their open and transparent communication strategy fosters trust and cooperation, making the migration journey less stressful and more collaborative.
4. Prioritizing Data Quality: Recognizing the critical role of data in patient care, Zynx prioritizes maintaining data integrity during the migration. They apply meticulous care when transferring order sets and care plans, ensuring that crucial information remains accurate and accessible in the new Epic EMR system.
5. Continuous Training and Support: Zynx offers robust training programs tailored to the needs of your staff. They provide training before, during, and after the migration, enabling your team to maximize the functionality of the Epic EMR system. Moreover, Zynx provides ongoing support postmigration, assisting users in addressing issues and adapting seamlessly to the new system.
6. Regular System Testing: Zynx understands the importance of regular system testing during migration. Their team performs rigorous testing at every stage of the migration process to ensure that the Epic EMR system aligns perfectly with your organization’s needs. This diligent approach helps to identify and rectify potential issues promptly, guaranteeing a smooth and efficient migration process.
Closing Thoughts
Epic migration might seem like a daunting task, but it’s one that’s definitely worth it. Imagine having a single, efficient system that boosts patient care, simplifies operations, and ticks off all regulatory requirements. That’s what Epic offers. And with Zynx by your side, this challenging journey suddenly feels a whole lot easier.
Zynx isn’t just a service provider; they are your partner on this transformative journey, offering expert advice and tailored solutions at every step. Their team ensures a smooth switch, focusing on your unique healthcare goals.
Choosing Zynx isn’t just about tech upgrades; it’s about gaining peace of mind. They handle every part of the evidence-based order set and care plan migration process with care, precision, and an understanding of your specific needs. And they’re committed to excellence, so you know you’re in safe hands.
Ready to step into the future of healthcare delivery with confidence? Get in touch with Zynx and kickstart a rewarding Epic migration journey. Your healthcare organization deserves the best, and that’s what Zynx aims to help you achieve.

SHARE THIS ARTICLE
When it comes to making critical patient care decisions, what's your source of truth.

Zynx solutions complement your clinical expertise with an extensive evidence-based, condition-specific knowledge repository built by clinicians and featuring actionable interventions curated from the latest peer-reviewed studies, national guidelines, and performance measures.
Zynx solutions align with major regulatory requirements to help ensure compliance.
Discover why we’ve been ranked Best in KLAS by KLAS Research for the past three consecutive years.
Contact us today to learn more!
The Agency for Healthcare Research and Quality recently published an updated annual report on…
Skilled nursing facilities comprise the most robust sector of post-acute patient care. According…
The Future of Healthcare: Reflections on the 2021 Scottsdale Institute Clinical Informatics Summit Perhaps no…
Zynx Health solutions put the best research and medical practices at your fingertips so your organization can operate stronger, better, and more efficiently.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Indian J Ophthalmol
- v.68(3); 2020 Mar
Electronic medical records – The good, the bad and the ugly
Santosh g honavar.
Editor, Indian Journal of Ophthalmology, Centre for Sight, Road No 2, Banjara Hills, Hyderabad, Telangana, India. E-mail: gro.soia@lanruojrotide
“Technology is wonderful and seductive, but when seen as more real than the person to whom it is applied, it may also suppress curiosity; and such curiosity is essential to active thinking and quality care.” – Dr. Faith Fitzgerald
Henry David Thoreau's prophetic statement in Walden (1854) - “ Men have become the tools of their tools ”, has come to be completely realized in the 21 st century, specifically concerning human interface with information technology. The interaction of physicians with electronic medical records (EMR) is the most relevant example of how our inventions have enslaved us. The focus is often on creating a perfect record on EMR, while patient interaction is relegated to the hazy periphery.
Evolution of Medical Records
Medical records have a history of 4000 years in evolution and, in some form, have existed since the beginning of the practice of medicine. Some of the first medical records date back to Hippocrates in the 5 th century BC and medieval physicians.[ 1 , 2 ] Formal medical records appeared in the nineteenth century in Europe in major teaching hospitals and were quickly adopted across the world. The modern medical record was developed in the 20 th century – data about each patient, including clinical data, was recorded, organized in a standardized format and stored.[ 2 ] Major problems with traditional paper medical records include lack of standardization across physicians and healthcare facilities, poor searchability and loss of information.
EMR has been in evolution for several decades now but continues to grossly miss the intended mark of efficient and personalized patient care. The first EMR was developed in 1972 by the Regenstreif Institute in the United States and was then welcomed as a major advancement in medical practice.[ 3 ] The uptake, however, was low, the cost being a major constraint. The vital push came through the American Recovery and Reinvestment Act 2009, spearheaded by Barack Obama, which envisaged incentives to EMR users.[ 3 ] Several EMR packages have since been developed and have become widely available across the world.
EMR – The Good
EMR is considered potentially one of the drivers for the transformation of healthcare. From a patient care perspective, EMR is expected to improve the accuracy of the information, support clinical decision-making and improve the accessibility of information for continuity of care.[ 4 ] From an operational perspective, EMR should generate essential health care statistics crucial to the planning and management of health care services.[ 4 ] User expectations from a good EMR are several – meticulous patient documentation, common templates and order sets, disease coding and billing, regulatory compliance, prevention of medication errors, clinical pathway utilization, optimized workflow, medico-legal defensibility, adaptive learning capability, simplicity, multiple input interfaces (notes, voice transcription, drawings, etc), incorporation of clinical images, seamless connectivity with clinical investigation platforms, input speed at the point of entry, and most importantly, data compilation for analysis and research, all with time-efficiency, and a user- and patient-friendly interface.[ 4 , 5 ] Ideally, EMR should be on a single platform nationwide to enable interoperability and portability horizontally and vertically across the referral chain.
Are computers and clinicians uneasy bedfellows? Probably not. Every sphere of life, including the practice of medicine, has seen extensive computerization and the present generation of doctors are extremely comfortable with digital technology. The uptake of EMR is on the rise and it is here to stay.[ 6 , 7 ] In the United States, ophthalmologists have almost quadrupled their EMR use, from 19% in 2008 to 72% in 2016.[ 7 ] The use of EMR is still in its infancy in India.[ 8 ] The Government of India intends to introduce a uniform system of EMR. An expert committee set up by the government has developed “Electronic Health Record Standards for India”.[ 8 ] With this as the background, there is an immense nascent potential for EMR in India. With major Indian ophthalmic institutes having developed their EMRs and using them in their routine daily practice, and their residents and fellows having been “trained on EMRs”, its use is only likely to increase.
EMR – The Bad and the Ugly
The chief complaint against EMR is that it has undermined personalized face-to-face patient care and the vital doctor-patient interaction - the very soul of medicine - into a new check box-based doctor-computer-patient interaction. Abraham Verghese calls this an “iPatient” phenomenon.[ 9 ] EMR was never designed to facilitate a personalized human narrative, logical thinking, and experience-based clinical analysis. Clinical reasoning being the backbone of a traditional doctor-patient interaction, “a medical record—whether paper or digital—must preserve the information that the physician carefully and thoughtfully elicits from the patient in a form that, above all, facilitates clinical reasoning.”[ 1 ] Current EMRs do not.[ 1 ]
A new report from the National Academy of Medicine is revealing – on an average, nurses and doctors spend 50 percent of their workday treating the screen, not the patient, and the increased work burden associated with EMRs is one of the factors for physician burnout.[ 10 ] A study of emergency room doctors revealed that putting information into the computer consumed more of their time than any other activity. Using a “click” of the computer mouse as the standard of measure, a doctor needed to make 6 clicks of the mouse to order an aspirin, 8 clicks to get a chest x-ray, 15 clicks to provide a prescription, etc., Over 40% of a typical 10-hour emergency room shift was devoted to data entry and 4,000 clicks of the computer mouse.[ 11 ] Immense information on EMR results in high (data) noise to (clinical) signals ratio. Arnold Relman, former editor-in-chief of the New England Journal of Medicine and a physician with 6 decades of experience found EMR “lacking in coherent descriptions of his medical progress, or his complaints and state of mind” when he was a patient himself.[ 5 ]
EMRs seem to have adversely affected the clinical training as Ober and Applegate state, “Our residents often resemble air traffic controllers, focusing more on the logistics of arrivals and departures than on understanding the patient's journey”.[ 5 ] They go on to quote a resident, “Education, rapport, compassion, bedside clinical reasoning, the physical exam, all seem to take a back seat in the current system”.[ 5 ] EMRs seem to be badly designed to the do the job they are meant to do and seem to have failed to make patient care better, more efficient, or more satisfying for the patient or the doctor.
Will We Ever Find the Gold? - Can there be a Perfect EMR?
As there can never be a perfect spouse, there can never be a perfect EMR. EMRs must evolve and the potential users synchronously need to retrain themselves and change their mindset until a sweet spot is reached. “To develop an EMR that meets the needs of the physicians who will use it, we need to better understand how the physicians work, and develop the software with an eye toward solving real problems in practices rather than developing a solution looking for a problem.”[ 12 ] Fortunately, India seems to be leading in the development of stand-alone ophthalmology EMRs, and that too with significant contributions from the users' right at the stage of EMR development. Sankara Nethralaya and Tata Consultancy Services (TCS) have together developed a comprehensive EMR system from scratch. It is natural for people to forget, but Anthony Vipin Das must remember that it took us a lot of effort to initiate and carry forward an in-house coding and development of EMR at the LV Prasad Eye Institute (LVPEI) about 10 years ago. It was meant to be a smart EMR, developed by the ophthalmologists and for the ophthalmologists, appropriately called eyeSmart. I feel redeemed that the seed that I had a small part is sowing and initially nurturing has now grown to be a fruit-bearing tree and is seamlessly used across the LVPEI network for patient care, administration and research. The current issue of the Indian Journal of Ophthalmology carries an article from the LVPEI group reporting their 8-year experience with eyeSmart and the accompanying commentary puts things in perspective.[ 13 , 14 ]
Robert Wachter states in his book The Digital Doctor – ”One of the great challenges in healthcare technology is that medicine is at once an enormous business and an exquisitely human endeavor; it requires the ruthless efficiency of the modern manufacturing plant and the gentle hand-holding of the parish priest; it is about science, but also about art; it is eminently quantifiable and yet stubbornly not.” An ideal EMR should harmoniously bring together the soul of medicine and cutting-edge informatics.
Understanding EMR: Electronic Medical Records Explained
Electronic Medical Records (EMR) play a significant role in modern healthcare for both healthcare providers and patients with the global EMR market size projected to reach a $32.3 billion valuation by 2033 . Understanding EMRs is therefore crucial in today’s digital age. In this article, we will explore what EMRs are, how they work and differ from EHR , as well as the benefits they bring to healthcare organizations and individuals.
Key Takeaways:
- EMRs are electronic versions of a patient’s medical record, containing comprehensive health information.
- EMR systems range from scanned copies of paper charts to dynamic, multi-field electronic forms.
- Benefits of EMRs include reduced administrative time and costs, e-prescribing capabilities, and easy sharing of patient information.
- EMRs are used by various healthcare organizations, including private practices, hospitals, and behavioral health clinics.
- EMRs play a crucial role in ensuring HIPAA compliance, enhancing patient care and improving operational efficiency.
What is EMR?
EMRs, or electronic medical records, are the digital version of a patient’s complete medical history, including diagnoses, treatments, and other relevant information. EMR/EHR systems are used by 88.2% of office-based physicians . Unlike traditional paper records, EMRs are stored electronically in dedicated healthcare software systems, known as EMR systems. These systems can range from a simple scanned copy of paper charts to a dynamic, multi-field electronic form.
One of the primary purposes of EMRs is to help healthcare providers track and manage patient data over time. This enables them to provide better care, make informed decisions, and streamline their operations. EMRs also serve as a platform for various functionalities, such as providing reminders for screenings and checkups, managing financial aspects of a practice, and ensuring compliance with the Health Insurance Portability and Accountability Act (HIPAA).
Benefits of EMR
The benefits of using EMR software are far-reaching. Firstly, it reduces administrative time and costs by automating various processes, such as appointment scheduling, billing, and claims management. Secondly, EMRs enable e-prescribing and drug interaction scanning, ensuring safer and more accurate medication management. Additionally, EMRs support the referral process by facilitating the exchange of patient information between healthcare providers. Moreover, patients can access their health information through Patient Portals, empowering them to take an active role in their healthcare journey.

The Difference Between EMR and EHR
The terms “electronic medical record” (EMR) and “electronic health record” (EHR) are sometimes used interchangeably, but there is a significant difference between the two.
EMRs are a digital version of paper charts within a clinician’s office and are limited to the medical and treatment history of patients within one practice. While EMRs offer advantages such as tracking data over time and identifying patients due for preventive screenings, they do not easily share information with other healthcare providers.
On the other hand, EHRs go beyond standard clinical data and provide a broader view of a patient’s care from multiple sources. EHRs are designed to be interoperable and can share information with other healthcare providers, including laboratories and specialists. They can be accessed by all individuals involved in a patient’s care, including the patients themselves.
The benefits of EHRs include improved coordination of patient-centered care, access to the latest information for all members of the healthcare team, and the ability to securely share information for more effective communication.
The Future of EMR and EHR Systems
As the adoption of EMR and EHR systems continues to grow, it is important to address the barriers that still exist in their widespread implementation. High capital costs, underestimation of organizational capabilities, resistance to change, concerns about obsolescence, lack of skilled resources, and potential negative unintended consequences are among the challenges faced. However, federal initiatives like the American Recovery and Reinvestment Act are driving the adoption of interoperable EMRs and providing incentives to qualified providers.
Certifications and standards are also being developed to ensure better interoperability and comparison of EMR systems. This will help healthcare organizations make informed decisions and choose the most suitable EMR solution for their needs. By overcoming these barriers, the future of EMR and EHR systems holds great promise in transforming healthcare delivery.
With a focus on improving workflow, patient care, and patient safety, the goal is to provide coordinated, patient-centered care by enabling all members of the healthcare team to have access to the latest information. EMR and EHR systems play a vital role in this healthcare transformation, streamlining processes, enhancing communication, and facilitating informed decision-making. By adopting these systems, healthcare providers can benefit from improved efficiency, reduced errors, enhanced data sharing, and ultimately, better patient outcomes.
What is an electronic medical record (EMR)?
An electronic medical record (EMR) is a digital version of a patient’s paper chart. It contains the patient’s medical history, diagnosis, medications, treatment plans, immunization dates, allergies, radiology images, and laboratory test results.
What is the difference between EMR and EHR?
The terms electronic medical record (EMR) and electronic health record (EHR) are often used interchangeably, but there is a difference. An EMR is a digital version of a paper chart in a single medical practice, while an EHR is a digital record of a patient’s health information that is shared among multiple healthcare providers and organizations.
What are the benefits of using an EMR?
Using an EMR offers numerous benefits, including improved patient care, better care coordination, increased accuracy of diagnoses and health outcomes, enhanced patient safety, and efficiency in managing patient records and practice workflows.
How does an EMR system benefit medical practices?
An EMR system benefits medical practices by streamlining administrative tasks, such as appointment scheduling, billing, and documentation, as well as providing access to real-time patient data, support for clinical decision-making, and improved communication among care providers.
Can an EMR system be integrated with other healthcare software?
Yes, EMR systems can be integrated with other healthcare software, such as electronic prescribing systems, laboratory information systems, and practice management software, to ensure seamless data exchange and interoperability.
How does using an EMR improve the quality of care?
Using an EMR improves the quality of care by enabling care providers to easily access comprehensive and up-to-date patient information, track patient data over time, and utilize decision-support tools to make evidence-based clinical decisions.
The adoption of electronic health records benefits patients by providing them with easier access to their health information, promoting communication with their care providers, reducing the likelihood of medical errors, and allowing for better coordination of care across different healthcare settings.
What are some key features of EMR software?
Key features of EMR software include electronic charting, e-prescribing, patient scheduling, clinical documentation, customizable templates, secure messaging, and integration with diagnostic devices and external health systems.
How does the adoption of electronic health records benefit patients?
What role does the national coordinator for health it play in promoting emr adoption.
The national coordinator for health IT plays a key role in promoting EMR adoption by developing and implementing policies and initiatives to advance the use of health information technology, improve secure health information exchange, and enhance the overall quality of healthcare delivery.
How can EMRs contribute to better practice management for healthcare providers?
EMRs contribute to better practice management for healthcare providers by automating routine tasks, optimizing workflow processes, providing real-time access to financial and operational data, facilitating compliance with regulatory requirements, and enabling efficient communication and collaboration within the practice.
Expert Healthcare Software Development Services
Flatirons develops custom healthcare software solutions that prioritize security and compliance.

Top Programming Languages for Healthcare Software Development

Hire Healthcare Developers: The Ultimate Guide in 2024

Time and Materials vs Fixed Fee: Finding Your Ideal Match a 2024 Guide

What is IT Outstaffing? A Guide in 2024

Outsourcing vs Outstaffing: Understanding the Differences

Outsourcing vs Offshoring: Key Business Differences
our company
design services
development services
maintenance services
engagement models
technologies
service areas
We are HIPAA compliant

Healthcare IT Skills, Health Information Technology Career Advice, Healthcare IT Certifications, Project Management, Job Tips
Healthcare IT Skills, Health Information Technology Career Advice
What Is An EMR? About EMR Systems – Electronic Medical Records
An Electronic Medical Record (EMR) system is a software platform that allows the electronic entry, storage, and maintenance of digital medical data. From a patient perspective, it is a digital version of a patient’s medical information that would have previously been recorded in a paper chart. Sometimes the term Electronic Health Record (EHR) is used to describe data that includes medical info entered outside of an office or hospital visit. For purposes of this page, I mostly use EMR to describe the clinical and technical components of the software. EMR systems are used throughout a healthcare organization to document clinical information on many patients over long periods. The systems organize and present data in ways that assist clinicians with interpreting health conditions, with placing orders, and providing ongoing care, scheduling, billing, and follow up. Data contained in the EMR is also used to create reports for clinical care, disease management, patient communications, and more.
An EMR will typically be accessed by users from a Windows based PC, a tablet, or a Smartphone. Some EMRs are entirely web-based, meaning that the organization using the technology accesses it only from a web browser as opposed to maintaining application servers and database servers. The application and databases are managed and located with the EMR vendor. Alternatively, many EMRs (especially in large organizations) are not entirely web-based. An example would be a hospital that uses an enterprise wide system such as Epic, Cerner, or MEDITECH. This graphic shows a simplified view of how these EMR systems are configured:
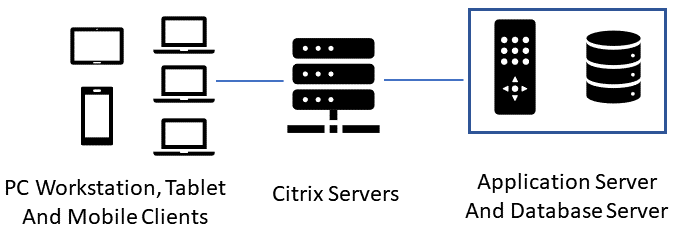
Before the days of EMRs, your medical info was usually entered by hand and by filling out forms in a paper chart binder. Paper charts had a designated order in which the medical information was organized. This is important to cover because the paper chart structure has influenced the workflow and layout of today’s EMRs. Here are the tabs contained in a paper chart:
A face sheet is a quick view of the patient, containing basic demographic info such as age, gender, address and phone number. It also has an overview of the patient’s medical condition, allergies, and current medications. In an EMR, this overview may be called a Snapshot or Synopsis.
Medical Encounters
This includes events that have occurred in which you interacted with a care provider. Regular office visits, trips to the ER, immunizations, hospital stays, and even telephone calls to your doctor’s office are all encounters, and are recorded in your medical record.
Progress Notes
This is where the physician and other caregivers document their assessment, impressions, and other data observed during visits with patients.
Orders and Prescriptions
Any time a healthcare provider prescribes a medication, orders an X-Ray, or even advises you wear a knee brace- these are all orders and are documented in your medical record.
Test Results
Results from your lab tests, MRIs, or any other diagnostic tests will be in this section.
Other information and documents from other healthcare providers
This is where any miscellaneous documents or materials are kept. For a paper chart, it’s usually near the end.
Medical Documentation – What Gets Entered in the EMR
Now we’ll have a look at what gets entered into the EMR from the time you arrive at the physician’s office, until you check out. Because of the history and logical layout of a paper chart, most EMRs attempt to group electronic data in a similar order to the paper chart. Here is an example of the Kareo system. Notice the tabs on the left indicating the sections of the electronic chart:

Intake – Reason for Visit and Vital Signs
When you arrive in the exam room, the Medical Assistant will open your medical record, usually by clicking on your name from the schedule. They will then confirm what you are being seen for and document it. If you are being seen for abdominal pain, that’s exactly what they will enter in the EMR. It’s important to note that this is not a diagnosis, just a reported observation. Next, vital signs are taken. Federal regulations for Meaningful Use of Electronic Medical Records systems require at least the gathering of height, weight, and blood pressure.
Patient Reported Medications
The MA will then ask you what medications you are on and record them in the EMR. They should ask for name, dosage, strength, and frequency. In the EMR, there will be a medications area that has your current meds list, and a prescriptions area, which has the prescriptions that your doctor may write for you. These are separate areas in the EMR, and the MA typically just documents the reported meds you are taking.
Allergy Documentation
The MA will ask if you are allergic to any substances, foods, or medications. This is one of the most beneficial aspects of an EMR because the systems have built-in allergy and medication conflict checking. Later in the visit, if the physician tries to order a medication that would cause a reaction, they will get a warning.
Medical History and Surgical History
In some care settings, your medical and surgical history may be gathered by the MA, other times it may be gathered by the front desk during check-in. One challenge that still exists with a lot of offices is the tradition of having you fill out a paper form with all of your medical and surgical history, which then seems to go nowhere because you get asked again by someone who keys it into the EMR. This can be solved by having patients enter their history on a tablet or at a kiosk. Medical kiosks are in more and more places these days, but are not quite everywhere yet.
Smoking Status
Another regulatory requirement is to ask all patients about their smoking status and offer smoking cessation materials to current smokers. The MA will record this info into the EMR. We should note that everything entered is date stamped, which is important to meet regulatory requirements that are date sensitive.
The Physician Visit
At this point, the MA will probably log out or secure the PC that is hosting the EMR, or if they are on a tablet, they just leave the room with the tablet. The chart is either considered closed , or secured while you read last year’s magazines and wait for the physician.
When the doctor arrives, they will reopen your chart from the EMR, which will require some form of logging in to validate their identity. They will then take a minute to review the information that the MA entered. What I mentioned in the last section about data-driven regulations applies here as physicians are required to record that they have reviewed various parts of all patients’ medical records. This requirement is usually met by the physician clicking a “mark as reviewed/noted” button that is in several places of the medical record. That action is logged in the database as part of the official record.
Progress Note
The physician will at some point open a progress note section of the record to begin documenting the findings of the visit. Some doctors document while they are visiting with the patient, some start the progress note in between patients, and some document after the visit. It is also sometimes called a SOAP Note.
SOAP stands for Subjective, Objective, Assessment, and Plan. By the names of the sections, you may be able to guess a little about what is contained.
Doctors rarely type the entire contents of the progress note the way we type letters from scratch. Since many of their visits are very similar in structure, they rely on note templates to quickly document their findings. Doctors will usually have note templates for common conditions like flu, ear infections, and respiratory infections. They will also have note templates for certain types of patients, like for an adult physical or a well-child checkup.
Visit Diagnosis
Once the physician has determined the problem, they will enter one or more diagnoses in the EMR. This is not necessarily the same as the chief complaint- many times is isn’t. That’s why they’re the doctors and we’re not. The visit diagnosis is important in the medical record for many reasons, such as:
- Billing: Insurance pays different amounts for different conditions, as we all know,
- Research: If we have accurate diagnoses on many patients, that data can be used to better treat conditions, or even spot trends and potential epidemics.
Diagnoses all have codes that are recognized by clinicians and insurance providers. You may have seen them show up on insurance statements you get in the mail. For example, Type 2 Diabetes has a code of E11.9. An EMR enables physicians to just enter the English description of the code, and have the correct billing equivalent transmitted to insurance providers. Before electronic records, physicians’ offices had to manually keep track of billing codes, and frequently kept huge reference books on hand.
Problem List
Once as diagnosis has been made, the physician will determine if the condition is a long term or chronic condition, like Diabetes. “Flu” would not go on the problem list because it isn’t a long-term condition. Also, usually only the physician has the authority to update diagnoses on the problem list.
Level of Service
Level of service is a code that the physician enters into the chart to correctly bill for various levels of complexity of an office visit. For example, you may have two Diabetes patients; one is managing their condition well with few complications. The other patient is not managing their Diabetes well and has many complications. The more chronic patient visit would be coded to a higher level of service than the other visit.
Medications or Orders
The physician may order medications, lab tests, X-rays, referrals to specialists, or any number of other orders or procedures. Those all have to be entered into the EMR, and each order needs to be associated with the correct diagnosis. Those orders usually have expiration dates and are part of your permanent medical record for historical purposes.
Patient Instructions (After Visit Summary)
When the doctor is finished with the visit, they will usually print an after visit summary (AVS), which is the handout that you get stating what you were seen for and how to address the condition(s). The EMR vendor usually has a component of the software which imports the patient instruction information from a third-party provider of this material. Main suppliers of this integration are RelayHealth and Krames.
Final Medical Documentation Task
The last thing the physician does is to close the encounter in the EMR. This step is very important as many physicians are evaluated on percentage of closed encounters over time. Also, charges for the visit usually cannot be sent electronically to insurance companies until the encounter is closed. At this point, the front desk scheduler may also record the visit as checked out in the EMR.
Post Encounter Billing
While the clinicians are now finished with the encounter, there is usually an electronic transmission that goes to a billing and coding department. The coders will use a combination of software and human analysis to determine any corrections to the encounter before billing is sent to insurance. In some cases, there will be a clinician in the physician department who is also certified in coding. That person may amend the encounter to update the level of service or other billing related areas of the chart.
Scanned Medical Records
For this function, you may have some paper records from outside medical visits that are relevant to your current health that should be included in your record. Most EMRs have the ability to scan these documents into a designated section of the chart. While there is some usefulness to this approach, the contents of the documents is usually not searchable and tends to get forgotten. This is what we call “non-discrete” data, and it’s not the preferred way to capture data.
Benefits of Electronic Health Records
The benefits of electronic health records systems are significant. Prior to electronic records, data was sealed in paper charts that could only be accessed by one person as a time. Each Healthcare provider or location had their own copies of charts that could only be shared between providers by fax, personal courier, or mail. It was a real mess. Some other benefits of electronic health records are:
- The ability to search for data just like you would a website or document;
- The ability to share data and communications with patients and other providers electronically;
- A visual snapshot of the overall condition of a patient, in one view;
- Backups of data that survive natural disasters which could obliterate paper records;
- The ability to store data for detailed analysis of any number of medical conditions or other factors;
- 24/7 access to patient charts via computers or mobile devices.
Challenges of Electronic Health Records
With all the benefits of electronic health records adoption, there are certainly some challenges, as well as complaints from the users:
- The learning curve that comes with the new technology can be a challenge for medical staff who are not used to documenting electronically. While some of the more adept users claim that it makes documentation faster, other users find it takes them longer;
- Added costs are a big deal in the US Healthcare system that is already the most expensive in the world. This has forced most smaller physician practices to sell out to larger organizations who are more able to handle the cost and complexities of EMR implementations;
- Security breaches in Healthcare have increased dramatically in recent years. One 2017 report showed a 305% increase of Healthcare security hacks and ransomware events.

- 800-436-3150
What Is EMR: Understanding Electronic Medical Records

In an ever-evolving medical landscape, staying ahead with the latest advancements is key to providing effective care. At PatientNow, we recognize the importance of integrating modern technologies to enhance the patient experience and treatment outcomes. Embracing these changes can allow you to continue offering top-tier cosmetic procedures and med spa treatments to your patients.
Our electronic medical records are easy to use and include all of the features cosmetic medical practices need to boost productivity and improve patient safety. We make it easy for any practice to transition to EMRs because we offer tools that help you right where you are in the process. We can help you understand what EMRs are, how they can help your practice, and what the first steps are to implementing them.
What Is an EMR?
An EMR, or electronic medical record, is a digital version of a patient’s paper chart. It’s a system that allows medical professionals to store, access, and manage patient information electronically. This technology streamlines the documentation, storage, and retrieval of patient data, facilitating a more efficient and accurate healthcare delivery process. By adopting EMR systems, clinics can enhance the quality of care provided and make sure that patient records are always up-to-date and readily available for consultation.
What Can an EMR Do?
- Patient Demographic Details: EMR systems streamline the inclusion of basic yet important information such as age, gender, and contact information. This ensures quick identification and efficient administrative processing for every patient visit.
- Medical Diagnoses: Through electronic medical records management, medical diagnoses are accurately recorded, providing healthcare providers with a comprehensive view of a patient’s health history. This facilitates a more informed and targeted approach to treatment.
- Clinical Observations and Notes: EMR software solutions offer a centralized platform for doctors to record their observations, thoughts, and notes during and after consultations. This digital record-keeping enhances the continuity of care and supports healthcare providers in making informed decisions.
- Details of Prescribed Medications: With EMR systems, the specifics of any medications prescribed to a patient, including dosage and frequency, are meticulously documented, enabling doctors to monitor patient adherence and prevent potential drug interactions.
- Results From Laboratory Tests: EMR technology allows for the direct and secure storage of lab test results to expedite the review process and track patient progress over time.
- Records of Vaccinations: Effective patient data management is exemplified by detailed vaccination records, enabling healthcare providers to maintain up-to-date immunization schedules and ensure compliance with public health standards.
- Information on Allergies: EMR software helps doctors document any known allergies a patient has to alert healthcare professionals to potential risks and promote patient safety during treatment and care.
Want an inside look at the PatientNow EMR?
What Else Can EMRs Do?
Allow patients to easily access information.
With patient data management systems in place, patients gain access to their health information through online portals. Digital access enables individuals to review their medical history, lab results, and upcoming appointments at their convenience. It empowers patients to take a more active role in their healthcare journey by providing them with the tools to understand and manage their health data. This increased involvement not only fosters a stronger patient-provider relationship but also contributes to better health outcomes.
Help in the Prescription of Medications
EMR systems open the door to a simplified prescription process by allowing healthcare providers to manage prescriptions more easily. By integrating RxNOW to send prescriptions directly to pharmacies electronically, you can reduce errors, speed up the medication dispensing process, and improve patient safety. EMRs can also alert providers about potential drug interactions, enhancing patient care.
Assist With Billing Organization
Billing becomes more streamlined with EMR software solutions. These systems can automate many of the billing processes, reducing paperwork and minimizing errors. This not only saves time for the practice but also helps in providing patients with clear and accurate billing information. Additionally, EMR systems can facilitate detailed financial reporting, allowing practices to easily track revenue and identify areas for financial improvement.
Promote Communication Between Individuals Within the Practice
Electronic medical records management systems are designed to foster better communication within healthcare teams. By providing a single, accessible source of patient information, EMRs ensure that everyone involved in patient care is on the same page. This can improve the efficiency of care coordination and enhance the quality of healthcare services provided. EMRs also facilitate real-time updates and alerts, allowing for immediate adjustments to patient care plans.
Help in the Ordering of Labs for Patients
The process of ordering laboratory tests for patients is made more efficient with EMR software. Providers can order tests through lab integration options, which transmit the orders to the appropriate lab. This helps in reducing the turnaround time for test results, thereby enabling quicker decision-making regarding patient care.
What Type of EMR System Do We Offer?
We use a cloud-based medical spa EMR software system designed to meet the unique needs of practices around the country. This allows for secure, real-time access to patient information from any location, enabling healthcare professionals to deliver care more effectively. By leveraging the advantages of cloud technology, we make sure patient data is both accessible and protected, facilitating a smooth and efficient healthcare experience.
Demo Our EMR System Today
When you adopt our medical spa EMR software at PatientNow , you are choosing software that is both HIPAA-compliant and Meaningful Use Certified. With this system, you can enhance care by improving access to patient records and streamlining administrative tasks. If you’re ready to experience the difference our technology can make, reach out or call us at (800) 436-3150 to demo our EMR system today.
See how PatientNow can improve your practice’s vitals.

TOPICS: Patient Engagement & Marketing
You Might Also Like

The use of electronic medical records (EMR) systems is becoming increasingly common in the medical community. With the shift to digitized patient data and advancing healthcare technologies, more doctors are…

Little brings over two decades experience growing and scaling B2B software companies Englewood, CO – June 12, 2023 - PatientNow, a US-based practice management company at the forefront of electronic…

To speak to current and emerging clients the way they want to be spoken to, your med spa needs to adopt digital marketing solutions to remain competitive and keep your return customers coming back.

Stay in the Know
Keep on top of everything happening in aesthetics—signup for our blog
I would like to receive promotional emails from PatientNow.
By submitting you agree to the Privacy Policy. You will receive emails periodically and can opt-out at any time.
[honeypot email "email"]
Please provide your contact details and let us know what interests you most.
Specialty *
Plastic Surgery Medical Spa Dermatology Other
How did you hear about us * Conference Webinar Podcast Educational Lecture Web Search Industry Referral Email Marketing Social Media Former/Returning User
I would like to receive promotional emails from PatientNow. I would like to receive special offers and updates via SMS.
By providing your phone number, you agree to receive text messages and phone calls from PatientNow. Message and data rates may apply. Message frequency varies. Reply STOP to cancel. View our Terms of Service and Privacy Policy.
Services Interested In? *
Marketing Website Design Practice Management EMR Photography Payments
Select your features and build it yourself.
Build My Demo
We’ll walk you through the PatientNow demo.
Schedule a Demo
Referring Company: Who are you?
Referred company: who are you recommending.
Enter [[Unknown]] in Company field if necessary
Products of Interest *
Marketing Practice Management EMR Website Design Photography Payments
I would like to receive promotional emails from PatientNow. (Privacy Policy)
- API First The power of APIs at your fingertips
- Automated Care Delivery Automate your care program from end-to-end
- Care Coordination Supporting a true care team model
- Codeless Care Program Design Freedom to create and customize care plans
- Multi-Channel Communication Harness the power of personalization
- Integrations Leading health integrations for a custom environment
- Patient Encounters Log every visit detail in one place
- Patient-Facing App The App that evolves with your organization
- Security & Permissions Security and compliance policies and permissions
- Pricing Plans that grow with your organization
- About Us Learn more about who we are
- Careers Shape the future of healthcare with us
- Blog Read our latest posts
- Care Access Log in to Care
- Knowledge Base Visit our Knowledge Base for support
- Trust Center Centralized hub for security and compliance program
- Support Visit our Help Center
- Request Demo
What Are EMRs Contributing To Your Patient Engagement Strategy?
When asked, “What are EMRs and why do you use one?” most clinicians will likely say electronic medical records (EMRs), as well as electronic health records (EHRs), improve patient care while ensuring health care systems get paid. They might also mention the gaps their EMR system leaves in the patient journey.
Clinicians may tell you they use these health IT tools to store a patient’s health information and medical history, but may also describe how overwhelmed they get using isolated health IT tools that disrupt their workflow and make it difficult to improve their quality of care.
Many EMR-using Care teams still struggle with coordinated care and patient retention. To understand why, we need to examine the functions of and differences between an EMR, an EHR, and a Care Management platform.
What are EMRs?
An EMR is essentially a digital version of a healthcare provider’s paper chart. It contains provider notes — mostly about diagnosis and treatment — but also the patient’s medical history, including immunization dates, allergies, diagnoses, prescriptions, and lab results.
Clinicians who join their first Care team may ask “What are EMRs?” and get many different answers. Electronic medical records are systems that capture medical interventions between patients and Care teams. They’re also used to record large billable events in the form of billing codes which help hold payers accountable for remitting payments. An EMR system ensures every single service is documented so health systems can recoup their costs.
Whether it’s a visit with a specialist, a simple check-in, or an updated diagnosis and prescription, an EMR system keeps track of these interactions. This ensures providers are reimbursed and that all expenses are covered. In addition, these systems keep track of what providers bill against.
HealthIT.gov explains how the “advancing care information” category within the “merit-based incentive payment system” program outlines the following objectives for EMR systems:
- Improve the safety, efficiency, and quality of care
- Reduce healthcare disparities
- Engage patients and patients’ families
- Improve healthcare coordination
- Maintain privacy and security of patient health information
- Expand the reach of population and public health
As vital as EMR systems are for revenue, they aren’t built to forge the kinds of relationships required to achieve these lofty goals. Improving a patient’s reported outcomes requires long-term self-care between clinical appointments — which Care teams help promote. Because of their design, EMRs aren’t great at tracking relationship-focused interactions such as a phone call or email to check on a patient between appointments.
What are EHRs?
Although they’d quickly answer the question “What are EMRs?” clinicians may take a bit more time to describe somewhat more complex electronic health records (EHRs). While very similar to EMRs, EHRs are slightly more broad, allowing access to a complete set of patient information. According to HealthITBuzz , EHR data “can be created, managed, and consulted by authorized clinicians and staff across more than one healthcare organization.”
EHRs are designed to extend beyond the health organization that originally collects and compiles the patient information. They’re designed to share data with all the clinicians involved in a patient’s care. The patient information in an EHR moves with the patient — to the specialist, the laboratory, the hospital, or the nursing home — even if they’re located in another state.
HealthIT.gov reports that more than 95% of U.S. hospitals use EHRs, yet they’re still not necessarily delivering engaging patient-centered care or achieving optimal outcomes. That’s because both EHRs and EMR systems are focused on billing and data — not relationship-building.
What’s the difference between EHR and EMR systems?
The EMR system is used daily in even the smallest practice for storing strictly medical patient information: processing payment and insurance claims, scheduling patients, adding new patients, and centralizing patients’ medical and treatment histories.
Unlike paper records, EMRs allow clinicians to track data, identify preventive screening or checkup due dates, and check biomarkers (like glucose and blood pressure readings). But patient information stored in EMRs doesn’t travel easily out of the practice where they were created. Some providers still print and mail records to specialists and health organizations.
EHRs, on the other hand, perform all of those functions and more, as they document the total health of the patient — not just the standard clinical data a provider collects during an office visit. EHR patient information travels with the patient — whether it’s to a hospital across town or to a specialist across the country. This secure data is fully accessible to patients, but it cannot be used or interpreted by the receiving EHR system.
As HIMSS Analytics puts it: “The EHR represents the ability to easily share medical information among stakeholders and to have a patient’s information follow him or her through the various modalities of care engaged by that individual.” The Centers for Medicare & Medicaid Services (CMS) certifies electronic health record technology (CEHRT) that meets meaningful use standards for incentive-based programs to improve patient outcomes. EMRs do not have any certifications and are not standardized.
EHRs bring clinicians one step closer to patient-centered care by allowing multiple parties to share data. However, neither EHR nor EMR capabilities improve all of the value-based metrics needed for better patient retention, compensation, and increased revenue streams.
When is it necessary to use both EHRs and EMR systems?
Delivering a continuum of care typically requires using both EHRs and EMR systems. The EMR provides a comprehensive care record created by a primary care physician and the EHR makes that care accessible to a spectrum of specialists, health systems, laboratories, pharmacies, or nursing homes.
The patient information that lives in an EMR — diagnosis and treatment data — can be uploaded at even the smallest remote clinic — it’s often critical to any Care team that delivers follow-up care.
For example, the patient information gathered by a primary care provider can alert ER teams to a patient’s life-threatening allergy so they can adjust care for an unconscious patient. EMR records can enable EHR users to avoid dangerous medication combinations and block patients who may be trying to obtain excess controlled substances from various providers. The lab results posted in an EMR can prevent a specialist who’s also using an EHR from running duplicate tests.
More complete and updated patient information — test results, symptoms, and health history — allows for all providers to make more accurate diagnoses and prescribe more personalized, timely treatment. Comparing records from both EMRs and EHRs to track trends may motivate patients to follow their care plans and transform their lifestyles.
What are the limitations of EHR and EMR systems?
The emotional burnout, depersonalization, and decreased sense of accomplishment make many physicians feel strapped by their EHRs due to these limitations:
Long implementation time
Researchers at the National Institutes of Health have estimated that EHR end-users spent 134.2 hours on implementation activities associated with setting up and learning a new system. This loss of productivity may potentially lead to losses in revenue.
One study found that productivity declined approximately 20% in the first month of implementation, 10% in the second month, and 5% in the third month. This resulted in lost revenue of $11,200 per provider in the first year. EHR and EMR systems can cause problems like data bottlenecks, staff training expenditures of time and money, as well as skill mismatches in collaborative teams.
High implementation costs
The U.S. Library of Medicine tracks financial issues surrounding EHR and EMR systems, including adoption and implementation costs, maintenance costs, revenue loss due to temporary productivity lapses, hardware and software purchase and install costs, paper-to-electronic-chart conversion, and end-user training.
The initial costs of software, training, and installation total approximately $22,038, and hardware costs are nearly $13,000 per full-time provider in a solo or small-group primary care practice. A five-physician practice launching an EHR system will spend approximately $162,047 (or $32,409 per physician) in the first 60 days. Ongoing EHR maintenance costs averaged $8,412 per full-time provider per year.
Clinician burden
Using EHRs is burdensome for physicians, who, according to Advanced Data Systems , spend on average 45 minutes on their computer per patient — that’s time they can’t dedicate to treating more patients. According to Computer World , clinicians continually complain that EHRs require far too many mouse clicks and data entry pagination, which diverts attention from patients — impeding the doctor-patient relationship and blurring a robust picture of their health.
EHRs may cause several unintended consequences, such as shifts in Care team power structure, a draining overdependence on technology, and medical errors due to poorly designed EHR system interfaces or inadequate training. All of these issues lead to major disruptions in clinicians’ workflows, which can generate resentment.
Lack of interoperability
According to the National Institutes of Health , there are hundreds of government-certified EHR products used by providers across the country, each with its own clinical terminologies, specifications, and functions — which makes it difficult to create a standard data-sharing interoperability format. Even EHRs built on the same platform may not be interoperable when they’re customized to a provider’s unique workflow and preferences.
For two EHR systems to be truly interoperable, they must be able not only to exchange, but to use that data. That requires standardized coding for the data so that it can be interpreted by the receiving EHR system. Such standards do not exist in the U.S. healthcare system. That’s why the intensive task of inputting and interpreting data must often be repeated whenever a patient transfers to a new clinic or facility. This problem has intensified due to Medicare and Medicaid reimbursement regulations.
Industry initiatives like the CommonWell Health Alliance and Carequality are advocating for vendor-neutral interoperability and seamless data-sharing between facilities — but much work is needed. The Argonaut Project is promoting interoperability standards in the healthcare industry. Innovation is speedily making the transfer of electronic patient information easier and more convenient.
Risk of cyber attacks
Data breaches across the country have exposed patient names, addresses, and medical histories too many times. Enhanced cybersecurity is a challenge for EHRs.
The HIPAA Journal reports that phishing scams have become the most popular method for stealing patient information in the United States. Cybercriminals use the stolen patient data to commit fraud and contact users to get them to share financial information, which they use to buy items illegally or to cover their own medical care. Victims get locked out of cards and become burdened with exorbitant credit card bills and the hassle of fixing their records.
Potential for medication error
The ECRI Institute , which tracks safety issues at healthcare facilities, found that medication error caused by dose timing discrepancies in EHR systems is a common problem for healthcare providers in every specialty. It also causes patient negativity and mistrust.
Configuration and user issues occur when the EHR order-entry system does not prominently display scheduled medication timelines. Prescribers often have trouble modifying times and communicating when a medication can wait and when it needs to be administered immediately. These serious errors can endanger patients and put providers at risk of malpractice suits.
Is there a better way to store and process patient information?
Healthcare providers across the country are reimagining the way they deliver care. There’s one Care Management platform that has lived up to their imagination: Welkin Health. These unique features are already helping Care teams resolve the issues above:
Patient-provider communication
EMRs and EHRs have produced a very sterile, clinical approach to patient care. They just aren’t designed for optimal patient-provider communication. It shouldn’t be a hassle to check in on patients or expeditiously respond to their questions. Texting and video are so much more direct and personal — and they provide documentation in a patient’s medical record that a conversation took place. Direct communication is much more powerful in promoting patient satisfaction, which leads to better care plan adherence — and ultimately, outcomes.
Even inside the exam room, the paper charts of the past – while certainly not clickable – gave clinicians more color and texture around each patient’s journey. They could flip through their notes to see exactly who did what prior to examining each patient. EMRs promised but did not deliver. So much of the patient story is learned in the exam room itself. But if clinicians are focused on entering patient data into the EMR system, they’re spending less time looking at the patient, being present with them, giving them empathy, and building meaningful relationships.
The Welkin Care Management platform can be used in place of an EHR or EMR as long as your organization isn’t mandated to use a certified product (like Medicare and Medicaid organizations are). Even if your organization is mandated, Welkin can be integrated with your EHR or EMR.
Team-first care delivery
Unlike EHRs which put the primary focus on major medical events, Welkin is an extremely flexible Care Management platform. We understand that every Care team manages patient relationships differently and needs different automated procedures to ease team members’ workloads and increase efficiency.
EMRs typically offer a one-size-fits-all program. Welkin, on the other hand, is customizable, allowing Care teams to share data or interact with patients who have more pressing needs. As health care providers shift away from the traditional fee-for-service model to value-based care, Care Management tools can fill the gap. They can either supplement your existing systems or provide you with a one-stop platform that manages all patient engagement services.
Integrations
With leading integrated applications already built in, along with APIs for you to build whatever else you want, you can create a platform that works exactly for you now. You can also integrate these features as you grow:
- Enable your patients to eSign secure documents with DocuSign
- Validate patient medication with Medi-Span, which is built into Welkin
- Leverage Welkin’s integration with DrFirst to execute electronic drug prescriptions
- Enjoy Welkin’s HIPAA-compliant Zoom-based telehealth services
- Use codified reference data to support your billing procedures
- View or build your own dashboards and reports with Sisense
- Sync with your calendar provider to schedule inside Welkin
Welkin takes security seriously. With the help of leading third-party security organizations like Service Organizational Controls (SOC), we’ve implemented a number of technical, administrative, and physical safeguards designed to protect your confidential data. Welkin enables you and your associates subject to HIPAA to use its secure environment to process, maintain, and store patient information.
Welkin also protects your data integrity when you share it between Care team members using flexible role-based, attribute-based, and territory-based security permissions. You can also use our time-stamped audit trail to track who changed user levels, in what location, and at what time. For added security, your team can choose either single sign-on (SSO) or multi-factor authentication (MFA).
Ready to start reimagining your Care team’s workflow?
Schedule your patient-centered Care Management demo today.
Related Articles

Patient Engagement Technology: What's in Store for the Future?
If we know anything about technology, we know that it is constantly evolving. What’s in use today might be obsolete only a few years later, and keeping up with the changing landscape is imperative — especially in... Read More >

6 Reasons Why Providers Need Patient Engagement Solutions
Accessibility, transparency, and communication are critical components to patient engagement and loyalty. Patients want to be included in the decisions related to their health journey and want a streamlined, easy way to do so. Patient engagement improves... Read More >

21 Patient Engagement Tools Your Care Team Needs
You’ve probably heard how much patient engagement tools can help all types of care teams deliver high-quality care — which leads to reduced readmissions, improved outcomes, and even higher patient satisfaction. But do you know exactly which... Read More >
Sign up to receive Welkin updates, delivered straight to your inbox
This site is protected by reCAPTCHA. Google’s privacy policy and terms of service apply.
Illustrating the patient journey through the care continuum: Leveraging structured primary care electronic medical record (EMR) data in Ontario, Canada using chronic obstructive pulmonary disease as a case study
Affiliations.
- 1 Alliance for Healthier Communities, 500-970 Lawrence Ave West, Toronto, Ontario, M6A 3B6, Canada. Electronic address: [email protected].
- 2 Canadian Institute for Health Information, 4110 Yonge Street, North York, Ontario, M2P 2B7, Canada.
- PMID: 32473567
- DOI: 10.1016/j.ijmedinf.2020.104159
Background: Although barriers exist to secondary use of primary care electronic medical record (EMR) data, the Alliance for Healthier Communities (the Alliance) in Ontario, Canada has successfully created one of the largest structured primary care EMR datasets in Canada. In 2018, the Alliance and the Canadian Institute for Health Information (CIHI), an organization that provides comparable and actionable data to accelerate improvements in health across Canada, entered into a partnership to share EMR data. In this paper, we describe (i) the processes that enabled the collection of structured EMR data by the Alliance; (ii) how CIHI connected with the Alliance to share data and assess its quality; and, (iii) demonstrate the value of linking structured EMR data to administrative acute care data in illustrating the patient journey through the care continuum, using COPD as a case study.
Methods: CIHI and the Alliance entered into a formal data sharing agreement that enabled the sharing of linkable structured EMR data by the Alliance's 75 community health centres (CHCs) with CIHI. By leveraging the Alliance's Business Intelligence Reporting Tool, 3 years of EMR data containing patient-level clinical data were shared with CIHI. CIHI assessed the EMR data quality using its Data Source Assessment Tool to ensure fitness for analytical use. By linking the patient level EMR records with hospital records (CIHI's discharge abstract database (DAD) and the national ambulatory care reporting system (NACRS)), we examined aspects of COPD patient management in primary care and followed their journey through the health care continuum, including follow-up in primary care after hospital discharge.
Results: Alliance EMR data representing approximately 570,000 patients and 8.5 million primary care encounters between April 1, 2015 and March 31, 2018 were shared with CIHI. A data quality assessment, centered on completeness and concordance, confirmed that the data was fit for analytical purposes. Overall, 13,023 enrolled primary care patients were identified as having COPD, representing an overall crude prevalence of 8.7%. The average age of COPD patients was 64 years and equally affected males and females. Patients were most likely to have completed high school education or equivalent, speak English, live alone, and have a household income less than $15,000. They most commonly had between 10-19 primary care encounters a year with a range of providers where they most commonly sought services for health advice/ instructions, to discuss their treatment plans and for medication renewals. By linking the EMR data to CIHI's NACRS and DAD, we found that 74.1% of COPD patients had at least one ED visit and that 34.4% of COPD patients had at least one acute care hospitalization during the study period. Further, 16.2% of ED visits resulted in an acute care hospital admission. Of those hospitalized, the majority of COPD patients were discharged home (81.6%) and received timely follow-up in primary care (81.0% within 30 days).
Conclusion: Structured and linkable EMR data provides opportunities to examine the patient journey through the care continuum in an innovative way. Using structured EMR data from the Alliance, linked with CIHI's NACRS and DAD databases, we were able to generate a cohort of patients with COPD, explore the complexities of their primary care encounters and follow them through the continuum of care, namely emergency department visits and hospitalizations. It is hoped that the partnership between the Alliance and CIHI will help drive future efforts on addressing the gap in comparable EMR data in Canada, and internationally.
Keywords: Access; Administrative data; Chronic obstructive pulmonary disease; Electronic health record/EHR; Electronic medical record/EMR; Electronic medical records; Equity of care; Health informatics; Primary care; Primary health care data; Record linkage; Routinely collected data; Structured data.
Crown Copyright © 2020. Published by Elsevier B.V. All rights reserved.
- Aged, 80 and over
- Continuity of Patient Care / standards*
- Databases, Factual*
- Electronic Health Records / standards*
- Middle Aged
- Ontario / epidemiology
- Patient Discharge
- Primary Health Care / standards*
- Pulmonary Disease, Chronic Obstructive / epidemiology
- Pulmonary Disease, Chronic Obstructive / therapy*
Could Tij Iginla get drafted higher than his father Jarome?
Books have been written about how being the middle child often comes with not receiving the reverence that's reserved for the oldest, or the amplified attention that's given to the youngest.
When it comes to how he's viewed in hockey, reverence and attention have become extremely familiar themes for Tij Iginla. Especially upon the realization that while there are hockey families, his family might be unlike any that hockey has ever encountered.
His father, Jarome, is a Hockey Hall of Famer. His oldest sibling, Jade, is the star of Brown University women's hockey program, which she has led in scoring for the past two seasons. His youngest sibling, Joe, was a first-round pick by the WHL's Edmonton Oil Kings and had five points in five games this season as a 15-year-old, creating the expectation that he could be the next of his name to have a bright future.
As for the middle Iginla child? There's a chance Tij, the Kelowna Rockets winger could be the next first-round pick in the family, and potentially get drafted even higher than his father, who was the 11th pick of the 1995 NHL Draft.
"That'd be kinda funny and pretty cool to go ahead of him," Tij Iginla said. "The top 10 itself would be a really cool achievement too. I try not to think about that stuff too much. But yeah, that'd be pretty cool to have the bragging rights for that."
Numerous mock drafts have Iginla going in the top 10. The fact he's even in the discussion of being a potential top-10 pick is exactly why the Rockets traded a first-round pick, a second-round pick and Grady Lenton to the Seattle Thunderbirds last June in exchange for Iginla.
Following the trade, Iginla went from a 16-year-old trying to find his way in the WHL to a 17-year-old who scored 47 goals and 84 points in 64 games to get the Rockets to the WHL playoffs, where he added another nine goals and 15 points in 11 postseason contests.
Whatever team drafts Iginla will do it with the belief that they're getting a player who will be a long-term top-six center and help them go from their current state to one of a franchise with legitimate championship aspirations.
That expectation will start once he hears his name at the NHL draft in Las Vegas and walks the stage to accept the jersey and handshakes from the front office that selected him. But there's added significance to his selection: he has a chance to become a second-generation Black NHL player, which is believed to be a first.
It is believed that the NHL has only seen two generations of a family of color once before, with Ted Nolan, who is a member of the Ojibwe tribe, and his sons, Jordan and Brandon.
"I never really thought about it like that, but that's cool to hear," Jarome said. "Growing up, I remember as a young Black hockey player that it was important for me to see the Black players before me and over my career. I met a lot of young Black hockey players that I was fortunate enough to talk to at hockey schools. It was definitely an honor that some of them looked up to me and I was a role model for them like those guys were for me."
IGINLA WENT FROM six goals and 18 points in 48 games as a 16-year-old, to scoring eight goals and 20 points in his first 12 games in a Rockets sweater.
What was the big change?
"He was playing on a very deep team last year in Seattle as a young 16-year-old," Rockets coach Kris Mallette said. "He was not getting the minutes that he really needed or was able to get. That's the biggest difference."
It was never a question of ability for Iginla. It was more about finding the right opportunity. Scoring 26 goals and 48 points in 32 games as a 15-year-old for the RINK Hockey Academy U-18 team is why the Thunderbirds drafted him ninth in the WHL Bantam Draft in 2021.
Iginla's first full WHL season saw him play for a Thunderbirds team that was in contention to win the Memorial Cup. By the end of the regular season, they would have 16 NHL draft picks on their roster, with six of those prospects playing on the wing.
Even with limited playing time, there were items that the Rockets found enticing about Ignila's game.
"His release is sneaky fast," Mallette said. "We were able to watch it firsthand playing against Seattle and on video, you can see it, but when you see it in person, you see how quickly it gets from his stick to the net. You can't blink. You have to follow it because it can go really quickly."
Iginla was grateful to join the Rockets because it meant he would get a chance to spend more time with his family. Jarome and Kara Iginla decided to move to Kelowna because they wanted to live in a place they would enjoy, while also being in a location that would allow their children to continue their hockey development.
"As parents, we've loved having him back home," Jarome said. "It's been really enjoyable for us. It was good for him last year to move away to Seattle. It was a good challenge. It was hard for him. He didn't play a lot and they were a good team. But he grew in other areas."
Living with his parents provided Iginla with a chance to get in even more work beyond what he did at practice. Jarome said the family has a shooting area along with a separate space to work on stickhandling that was designed for all of their kids to get in extra skill development.
"We put in a good hockey facility at the house so our kids can do that nightly," Jarome said. "It's a chance to keep growing that most people don't have, especially billets."
Having a place to get in extra work while going to a team that could provide him the playing time he needed has allowed Iginla to find success in his draft year.
While Iginla received more playing time, he said what specifically allowed him to finish sixth in the WHL in goals was being trusted to handle the demands of being a top-line forward. He played against other top lines and defensive pairings, while logging minutes on the Rockets' top power-play unit.
Iginla scored 11 power-play goals for a Rockets power-play that finished ninth, while his eight game-winning goals were tied for seventh. His nine playoff goals were sixth in the WHL playoffs, though he played 11 postseason games while everyone else in the top 10 in playoff goals appeared in more than 15.
"When it's your draft year, everyone is thinking about the draft and you're comparing things like points," Tij Iginla said. "But what you're trying to do is stay focused and not worry too much about that. You just try to put it into perspective, too. The draft is obviously huge, but it's one year. It's your 17-year-old year and I don't just want to [just] have a great draft year. I want to have a great NHL career."
That level of perspective partially comes from having a dad who went through the process nearly 30 years ago.
Jarome said his draft year was "exciting but stressful" because it's a step closer toward that lifelong dream of the NHL, while being constantly judged. He said having scouts at every game made every day matter, which can be a lot.
"Outwardly, it does not seem to be too much pressure," Jarome explained. "I know inwardly, there are those certain days when you emphasize how you didn't play well or you didn't have a good game. We try to support them. We do have a lot of stories of when I went through it. I am sure they get sick of it! But there are times when it does get hard."
CALEB AND SETH JONES . Mathieu and Pierre-Olivier Joseph . Anthony and Chris Stewart. Gemel and Givani Smith . Malcolm and P.K. Subban. These are all examples of Black families that have played in the NHL, and it appears that the Iginlas could be the next, while also being the first Black father and son to play in the league.
After Willie O'Ree became the first Black player in NHL history back in 1957, the league still needed more time before it saw others. Mike Marson was next, and he didn't make his debut until 1974. Grant Fuhr, Dirk Graham and Val James were arguably the most prominent Black players throughout the 1980s.
Yet it was in the 1990s when the NHL saw a sizable surge in Black players. There had been 17 Black players who made their NHL debut prior to 1990. Twenty-three Black players entered the NHL from 1990 through 1999.
Jarome was part of a wave that included Donald Brashear, Anson Carter, Mike Grier, Jamal Mayers and Kevin Weekes. He also became one of the faces -- and for a time, the face -- of the NHL. Arguably the strongest example of his reach came when he was selected as the cover athlete for EA Sports' NHL 2003, becoming the first Black player to grace the game's cover. Nearly 20 years passed before P.K. Subban became the second Black player on the cover, when he received the honor with NHL 19.
Iginla also became the first Black player in NHL history to score more than 600 career goals, more than 600 career assists and 1,000 career points.
In 2020, Jarome joined O'Ree and Fuhr as the third Black player to be inducted into the Hockey Hall of Fame.
"That's something I have grown to appreciate as I got older," Tij said of his father's Hall of Fame career. "When I was a kid just watching, I knew he was a good player, but I never thought about things like that. But with as many people as he's been able to inspire because of what he's done is pretty cool."
The 2000s saw 27 Black players make their NHL debut, including Evander Kane and Kyle Okposo , who played against each other in the 2024 Stanley Cup Final. But the majority of that group -- along with the players who debuted in the 1990s such as Iginla -- have since retired, and are now playing an instrumental role in ushering what stands to be the first set of second-generation Black players.
It's an era that could start with Iginla, and continue with others such as Trevor Daley's son, also named Trevor, along with Georges Laraque's son, Marcus.
Trevor Daley Jr., who is 15, just finished playing for the Florida Alliance AAA program where he scored 75 goals and 142 points in 61 games, whereas Marcus Laraque, who is also 15, is already 6-foot-4 and scored 13 goals and 40 points in 28 games for his club team in Edmonton.
As for the elder Daley, the 40-year-old defenseman last played in the NHL during the 2019-20 season. Playing 1,058 NHL games provided Daley with the longevity that allows him to further appreciate seeing sons follow their fathers. Daley recalled when he was a rookie with the Dallas Stars during the 2003-04 season and was teammates with future Hall of Fame center Pierre Turgeon, who would have his son, Dominic, around the team.
Daley's career would see him join the Detroit Red Wings for his three final NHL seasons. His first season with the Red Wings saw him reunite with a familiar face as Dominic Turgeon played six games for the club that season.
Playing with two generations of Turgeon's made Daley joke that he knew it was time for him to get out of the game. But to see a son follow his father into the NHL was something Daley thought was special. To see that the Iginla's could follow a similar path while knowing the NHL has a chance to see more Black families do the same is something Daley said could help grow the game.
"I have always been so appreciative of the ones before me that I never really thought that a second generation could be coming in," the elder Daley said. "I never looked at it that way and always looked at the guys before me. The fact we can say 'second generation' and having Jarome's kid coming up is pretty cool even for me to soak all that in, to realize we know we have 'Jarome No. 2' coming in."

India script history to become first-ever team to win T20 Cricket World Cup title undefeated
T he ICC T20 Cricket World Cup 2024 has finally reached its conclusion after India's historic win against South Africa in the final of the competition in Barbados.
Virat Kohli's blistering knock helped India reach a fighting score of 176 runs at the loss of seven wickets.
India have finally broken the 11-year long curse of winning an ICC trophy. They came close in 2023, but fell short against the Aussies in the final of the ODI tournament in Ahmedabad.
The monumental win against the Proteas in Barbados is going to be celebrated for days in the subcontinent as the team has finally stepped up to the expectations of the fans. With the win against South Africa, India also became the first-ever team to win an ICC T20 World Cup undefeated. Rohit Sharma's team weren't bested in a single match throughout the competition, winning all seven games.
The only game wherein the Indians didn't manage a win was against Canada in the group stages, as it was abandoned without a ball being bowled due to a wet outfield in Lauderhill, Florida.
MORE: Relive the final as India beat South Africa, as it happened
India vs South Africa T20 World Cup 2024 Final: Scorecard
India were in trouble early on as they lost three important wickets in Rohit Sharma, Rishabh Pant and Suryakumar Yadav. Despite the early blow, the Indians managed to drag themselves back into the game, thanks to Virat Kohli’s stunning 76-run knock. Kohli finally delivered after a run of below-par performances.
In reply, South Africa seemed to be cruising to the target, but the combination of Hardik Pandya, Jasprit Bumrah and Arshdeep Singh defended 30 runs in the last five overs to take India over the line
- India: 176/7 (Virat Kohli 76, Axar Patel 47, Anrich Nortje 2/26)
- South Africa: 169/7 (Heinrich Klaasen 52, Quinton de Kock 39, Jasprit Bumrah 2/18)
MORE: Full results for the entire T20 World Cup in USA and West Indies
India's journey in the ICC T20 World Cup 2024
The Men in Blue have lifted the prestigious T20 World Cup for the second time in history, winning the trophy after being eluded from the prize for 17 long years. They last won the T20 World Cup back in 2007, when they defeated arch-rivals Pakistan in the final.
India’s campaign in the 10th edition of the tournament has been nothing short of a dream, having slayed powerhouses in England, Australia and Pakistan. Let's take a look at India’s complete journey in the competition:
They started their campaign with a comfortable win against Ireland, following which they bested Pakistan in an absolute thriller. India finished on the top of their group with seven points, qualifying for the Super 8 stage comfortably.
In the Super 8s, India won all their games, defeating Afghanistan, Bangladesh and the mighty Australia, avenging their loss from the ODI World Cup final in 2023.
In the semifinal, India once again completed a demolition job, defeating England. Ultimately, they defeated South Africa in the final to complete a historic tournament.

Louisville football's first Black starting quarterback overcame obstacles to make history

Many things come to mind when thinking about the 1970s.
But Black college football quarterbacks aren’t one.
There was Condredge Holloway, who made history at Tennessee as the first Black starting quarterback at an SEC school in 1972 . Derrick Ramsey became Kentucky’s first Black signal caller three years later.
In 1976, Randy Butler became Louisville’s first Black starting quarterback.
The 6-foot Georgia native was also the first Black starting quarterback during his senior year at Commerce High School.
The quiet-but-focused Butler didn’t understand the magnitude of his accomplishments at the time. To him, it was simply about playing the sport he loved.
But for Butler’s teammates — and Louisville football history — it meant more.
“Just having an opportunity to play with a Black quarterback and knowing that he was capable was just uplifting for all Black players on the team,” said Lamont Collins, Butler's former teammate who played defensive back and running back at Louisville (1978-81). “We felt it was time for Black leadership at quarterback.”
A moment of history
A wave of boos showered down on Fairgrounds Stadium.
U of L was up, 42-14, against Wichita State during the 1977 season when then-head coach Vince Gibson put Butler in the game. Fans booed when Butler entered and left the game.
According to a Courier Journal article, Gibson, now deceased, called it one of the worst things he’d seen in his coaching career.
“I'm like, 'Why are they booing me?' " Butler remembered thinking nearly five decades later. “Whatever they expected, they didn't get from me, so they have the right to do that. But, yeah, it was kind of mind-blowing. I haven't even ran a play yet.”
Knowing Butler's journey getting to that point made it even more frustrating and hurtful. A year before the spectacle, Butler came to Louisville as a walk-on. The Cardinals offered him a partial scholarship and a spot on the JV team. Louisville had 13 quarterbacks on the team.
Butler was No. 13.
He used his opportunities on the JV squad to prove he was better than that. Gibson eventually moved Butler to varsity. He earned a scholarship and made his debut by replacing freshman starting quarterback Stu Stram in a 34-0 loss to Rutgers on Nov. 6, 1976.
Three weeks later, Butler made his first official start against Cincinnati to end the season.
What should’ve been a celebratory, groundbreaking moment for Louisville was spoiled by a 20-6 loss for a 5-6 season. Additionally, Butler didn’t feel supported by all his teammates. He felt accepted by the Black players but noticed the offensive line didn’t block the same for him as the other quarterbacks.
In a Courier Journal article from the 1976 season finale, the late Mike Sullivan described the O-line as having done “a fair impersonation of a hoop with clowns jumping through it.”
“The clowns were enemy defenders who blew into the visitors’ backfield and made life miserable for Randy Butler, a freshman quarterback who did fairly well under the circumstances (five pass completions, one fumble),” Sullivan wrote.
The next season, Butler was the starter for the 1977 opener and led Louisville to a 38-0 win over Northern Illinois. The next game against Cincinnati ended in a 17-17 tie. Butler and the Cardinals went 2-2 over the next four games before dropping a 55-6 decision at third-ranked Alabama. Butler was 4-of-11 passing for 48 yards with three interceptions and had 46 yards on 16 carries. He scored the team’s lone touchdown on a 1-yard run in the third quarter.
The game cost Butler his job as a starter and his position as a quarterback.
"When I lost my starting position, I was distraught," Butler said. “I couldn't beat Alabama by myself. We were outmanned. Their talent was a lot better than what we could compete against. ... Alabama, they've always been a powerhouse. So, I guess I was the fall guy. (Gibson) had to make a change, so I got removed from the starting position.”
Still a quarterback
When Collins transferred from Western Kentucky to play for his hometown university in 1978, Butler had transitioned from quarterback to wide receiver.
Stram, the son of the late Kansas City Chiefs and New Orleans Saints head coach Hank Stram, got his spot back as the Cardinals’ starting quarterback. He led the team to a 54-7 win over South Dakota State in the 1978 season opener. Butler had a 33-yard catch in his first contest as a receiver.
“Not bigger, not faster, not stronger, but yet (Stram) got the position to play quarterback,” Collins said. “... We knew it was more racially motivated than it was (Butler’s) physical play. Even when he went to wide receiver, the Black players always treated him as the quarterback. He never lost that position. He was just a guy that could play quarterback that had to move to wide receiver to be on the field.”
Prior to Butler switching spots, the extent of his experience as a receiver was lining up wide during his junior year at Commerce High School.
“The quarterback we had was a white guy as the starter,” Butler said. "When we needed to pass the ball — because he couldn't throw — I would come in as a quarterback. So, I was a throwing quarterback in high school. When we had a running game going, I was a wide receiver.”
Butler contemplated transferring to a historically Black college and university but was persuaded to stay at Louisville. He had only three pass attempts in his final two years with the Cardinals but tallied 518 yards and four touchdowns on 31 catches in 22 games played. Louisville went 7-4 in 1978 and 4-6-1 in 1979.
Butler moved closer to home and signed an undrafted free-agent contract with the Atlanta Falcons. After getting married and starting a family, he finished his degree at Georgia State.
Louisville’s legacy of Black quarterbacks
The rarity of a Black college quarterback couldn't be further from the case now. The last three Heisman Trophy winners were Black quarterbacks. Last season, there were three Black starting quarterbacks in the ACC and five in the SEC.
Thirty-five years separated Butler’s historic start at Louisville and Teddy Bridgewater’s Big East Rookie of the Year campaign in 2011. Five years later, Lamar Jackson became the youngest Heisman-winning quarterback as Louisville’s signal caller. And then there was Malik Cunningham, whose six-year college career ended with him being the program’s all-time leader in rushing touchdowns (50), consecutive starts at quarterback (40) and overall quarterback starts (47).
Butler’s eyes began to fill with tears as he sat frozen while thinking of the three.
“As I get older, I get a little more emotional,” he said with a smile.
Butler met Cunningham at The Galt House Hotel the day Jackson’s jersey was retired a few years ago. It was a quick-yet-powerful moment between Louisville’s first Black quarterback and its most recent one.
“I said, ‘Do you know who the first Black quarterback was for the University of Louisville?’ He said, ‘It was probably you, right?’ And I said, ‘Yeah,’” Butler recalled. "So, we shook hands. I continued to follow his career. That was a great moment for me.”
Butler still hasn’t met Jackson and Bridgewater. He hopes to do so one day as the trail blazer who preceded them. Butler’s time as Louisville’s first Black starting quarterback may have been brief, but its impact is unforgettable.
Reach Louisville football, women's basketball and baseball beat writer Alexis Cubit at [email protected] and follow her on X at @Alexis_Cubit.

IMAGES
VIDEO
COMMENTS
EMRs. They focus on a specific provider's treatment. EMRs contain clinical data and treatment records from one specific healthcare provider. EHRs. They provide a comprehensive health history. EHRs provide a full record of the patient's health history, including all doctors' visits, diagnoses, treatments, and outcomes.
Plan your journey Open. Timetables Our routes Route map Live departures and arrivals Live network map Planned engineering works Service disruptions Strike information On board the train Open. Standard class First class Accessibility of our trains Luggage guidance Travelling with children Bikes on trains Travelling with pets At the station Open
The history of EHRs and EMR companies began in the 1960s - the Mayo Clinic in Rochester, Minnesota was one of the first major health systems (among a select few other healthcare providers) to adopt an EHR 1 and move away from the massive swath of healthcare organizations keeping paper medical records. to adopt an EHR. 1 In the 1960s, EMR ...
East Midlands Railway (EMR; legally Transport UK East Midlands Limited) is a British train operating company owned by Transport UK Group, and is the current operator of the East Midlands franchise.. Originally owned by Abellio, EMR took over operations from East Midlands Trains (EMT) on 18 August 2019, on an agreement to run the franchise for eight years.
Timeline: The History of the EMR/EHR. Published August 14, 2018. Updated May 2, 2024. Much of the conversation around healthcare technology is centered on where new developments are taking us. But as the age old adage goes, you can't know where you're going until you know where you've been. And when it comes to health IT, few innovations ...
The Best EMR Software of 2024. DrChrono: Best for medical billing. Kareo: Best for small practices. NextGen: Best for population health management. Allscripts: Best for large organizations ...
In 1972, however, the first electronic medical record (EMR) system was developed by the Regenstrief Institute, according to the University of Scranton. Regenstrief's EMR system was expensive and so was not attractive to physicians for use with their patients. The system was used, though, "by government hospitals and visionary institutions.".
2.2 Patient Health Records. The adoption of electronic medical records (EMR), electronic health records (EHR) and personal health records (PHR) are at the forefront of Canadian healthcare agendas. An EMR/EHR is a computer record that is initiated and controlled by clinicians. The PHR is compiled by physicians, patients, hospitals, pharmacies ...
Updated May 2, 2024. Electronic medical records (EMRs) are the digital equivalent of a patient's paper-based records or charts at a clinician's office. The term 'EMR' stands not only for the digital medical content but also for the broader system that captures, stores and assists in the management of a patient's healthcare information.
The migration to electronic medical records offers patients, providers and the overall healthcare system a variety of compelling benefits and cost reductions — but we shouldn't underestimate the challenges that stand between the idea of an e-health ecosystem and it becoming a reality.
Check real-time train updates. - Check your journey in real-time with live arrivals and departures. - View real-time schedules with our train time app feature. Go contactless with e-tickets. - Buy e-tickets and download them to your new mobile ticket wallet. - Transfer tickets between devices (phone and tablet) - No need to print paper tickets ...
EMR-Driven Efficiency and Safety During the Treatment Phase. Medical spa EMR software introduces a level of efficiency and safety during the treatment phase. By providing real-time access to a patient's medical history and ongoing treatment data, providers can make informed decisions quickly, minimizing risks and enhancing the overall ...
Embarking on the voyage of digital transformation in healthcare can feel like navigating through an ocean of challenges. Anchoring this journey is the Epic migration process, a pivotal shift from your existing electronic medical records (EMR) system to the industry-leading Epic EMR system.With Zynx by your side, the journey becomes less daunting, akin to sailing from familiar shores towards a ...
EMR - The Good. EMR is considered potentially one of the drivers for the transformation of healthcare. From a patient care perspective, EMR is expected to improve the accuracy of the information, support clinical decision-making and improve the accessibility of information for continuity of care.[] From an operational perspective, EMR should generate essential health care statistics crucial ...
EMRs, or electronic medical records, are the digital version of a patient's complete medical history, including diagnoses, treatments, and other relevant information. EMR/EHR systems are used by 88.2% of office-based physicians. Unlike traditional paper records, EMRs are stored electronically in dedicated healthcare software systems, known as ...
Lessons learned from a journey to EMR Health Manag Technol. 2009 Nov;30(11):24-7. PMID: 19947083
An Electronic Medical Record (EMR) system is a software platform that allows the electronic entry, storage, and maintenance of digital medical data. From a patient perspective, it is a digital version of a patient's medical information that would have previously been recorded in a paper chart. Sometimes the term Electronic Health Record (EHR ...
Refunds can be requested from your place of purchase. If you bought your ticket through the EMR App or Website, call 03457 125678 (Option 2 then 1, 0800-2000 daily) or email: [email protected] providing your full journey details and booking reference.
An EMR, or electronic medical record, is a digital version of a patient's paper chart. It's a system that allows medical professionals to store, access, and manage patient information electronically. This technology streamlines the documentation, storage, and retrieval of patient data, facilitating a more efficient and accurate healthcare ...
They might also mention the gaps their EMR system leaves in the patient journey. Clinicians may tell you they use these health IT tools to store a patient's health information and medical history, but may also describe how overwhelmed they get using isolated health IT tools that disrupt their workflow and make it difficult to improve their ...
Structured and linkable EMR data provides opportunities to examine the patient journey through the care continuum in an innovative way. Using structured EMR data from the Alliance, linked with CIHI's NACRS and DAD databases, we were able to generate a cohort of patients with COPD, explore the comple …
Find the cheapest or most convenient ticket type for your journey. Cheap train tickets - Check our current discounts; Advance train tickets - Save up to 60% in advance; Anytime train tickets for flexible travel; Off-Peak train tickets for travelling during quieter hours; Season tickets for weekly, monthly or annual travel
EMR, integrated with HMIS, revolutionizes the OPD experience by streamlining appointment scheduling. Patients can easily book appointments, receive reminders, and access their medical history ...
After Willie O'Ree became the first Black player in NHL history back in 1957, the league still needed more time before it saw others. Mike Marson was next, and he didn't make his debut until 1974.
India's journey in the ICC T20 World Cup 2024. The Men in Blue have lifted the prestigious T20 World Cup for the second time in history, winning the trophy after being eluded from the prize for 17 ...
A moment of history A wave of boos showered down on Fairgrounds Stadium. U of L was up, 42-14, against Wichita State during the 1977 season when then-head coach Vince Gibson put Butler in the game.
If you ask Boston Celtics beat writer emeritus Bob Ryan, the path for star Celtics forwards Jaylen Brown and Jayson Tatum to winning the 2024 NBA Championship was like no other Boston championship squad in history. And Ryan has seen much of that history in person from the sidelines, at that. Ryan and the other cohosts of the eponymous CLNS Media "Bob Ryan, Jeff Goodman, and Gary Tanguay ...