Return OB Visits

Every visit:
- Doptones, fundal height, vitals
- Four question: Vaginal bleeding, contractions, leaking fluid, fetal movement
- 20wks – get and review anatomy US
- 24wks – order glucola, cbc (check for anemia), discuss normal growing pains
- 28wks – Tdap and Rhogam if needed, discuss kick counts
- 32wks – Discuss BCM, sign tubal papers if needed, discuss TOLAC if needed
- 36wks – GBS screening, birth expectations, US for position
- 38-40wks – VE, “sweep membranes”

Quick Links
- Pimped Podcast
Our Mission
Procedure Ready aims to advance clinical medical education by curating and developing resources for medical students and clinical educators and ensuring those resources are financially accessible to all.
Contact us at [email protected], or live chat us if we’re online. We’d love to hear from you!
Pin It on Pinterest

- First Trimester
- OB-GYN & Prenatal Care
Q&A: What Happens at OB Appointments?
Good question, considering you’ll have between 10 and 15 OB visits throughout the pregnancy. During the first and second trimester, you’ll see the doc roughly every four weeks, then every two weeks through week 36, and then weekly until delivery. At every visit, your blood pressure, weight and urine will be tested. The doc will also check the fetal heartbeat,and around week 20 start measuring your belly’s growth and checking baby’s position. As your due date approaches, she’ll also start checking your cervix’s effacement (the amount it has shortened) and dilation (the amount it has opened) to judge the imminence of labor. Throughout your pregnancy, your doctor will look for symptoms like swelling in your hands and feet (a possible sign of preeclampsia) and varicose veins in your legs. Depending on the week, you’ll also be given various prenatal screenings.
In addition to all this poking and prodding, you’ll have a chance to ask questions and discuss your concerns. Keep a list of anything that comes up between visits so you won’t forget to ask when you have the chance. Your doc will fill you in on the changes to expect in the coming weeks,and let you know what is normal and what may be a cause for concern. If you plan to take any supplements, over the counter medications or herbal teas, bring them along and let your doc check the label first. Also, consider bringing your partner to a visit or two — it’s a good way to include him in the process and prepare him for delivery.
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
Navigate forward to interact with the calendar and select a date. Press the question mark key to get the keyboard shortcuts for changing dates.
Next on Your Reading List

Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
RELATED TOPICS
INTRODUCTION
This topic will discuss prenatal care in the second and third trimesters. Other important issues related to prenatal care are reviewed separately:
● Prenatal care issues at the first visit and in the first trimester: (See "Prenatal care: Initial assessment" .)
● Specific issues related to prenatal care for patients with multiple gestations: (See "Twin pregnancy: Overview" and "Triplet pregnancy" .)
● Prenatal care during the COVID-19 pandemic: (See "COVID-19: Overview of pregnancy issues", section on 'Prenatal care' .)
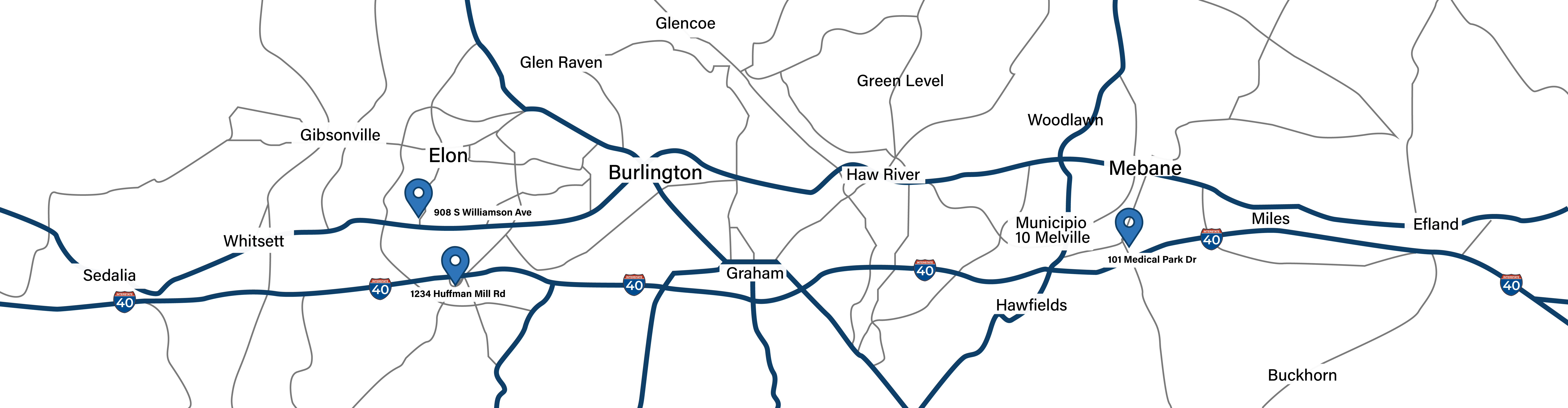
- Burlington 336-538-1234
- Mebane 919-563-2500
- Elon Family 336-538-2314
- Elon Pediatrics 336-538-2416
What to Expect at Your Prenatal Visits
First and foremost, congratulations! Pregnancy and welcoming a child into the world is an incredible experience. At Kernodle OB/GYN, we understand that for first-time moms and new patients, in particular, it can often feel like sailing into uncharted territory. To help give you the most positive experience possible, here is what to expect at your prenatal visits:
Our Approach to Care
At Kernodle OB/GYN, we provide patients with a team approach through physician and midwifery care. Our physicians and midwives perform deliveries at the hospital on a rotating basis, so we recommend that you see all providers during your pregnancy.
The following is a summary of routine prenatal care that we provide throughout an uncomplicated pregnancy. Please keep in mind that each woman and each pregnancy is different, and events may vary to reflect that.
Overview of Prenatal Care
Your first OB visit will typically be around 8 weeks. Upon confirmation of your pregnancy, you will meet with the doctor or midwife to discuss your medical history and other information about what to expect throughout your pregnancy. She will also give you information about the group practice and important telephone numbers.
You will return to Kernodle OB/GYN every 4 weeks until you reach 28 weeks (about 7 months). From 28 to 35 weeks, you will be seen every two weeks, then weekly beginning at 36 weeks until you deliver your baby. Six weeks after delivery we will see you for a postpartum checkup.
At each visit, we will check your blood pressure and weight. You will also be asked to provide a urine sample at your first visit and each visit beginning with the 20th week of pregnancy. You can expect your provider to check fetal heart tones, measure your abdomen, and review your blood pressure, weight and test results.
All tests are reviewed by your provider. Should any have an abnormal value that requires immediate attention, one of our nurses will notify you. Otherwise, your provider will review the results with you at your next visit.
Between appointments, we encourage patients to write down any questions you may have and bring them with you to your next appointment. At any time, you can view lab results, appointments and other useful information online through our patient portal, Duke MyChart.
Prenatal Screenings
Throughout your pregnancy, you can expect several routine screenings. Your provider will also talk to you about optional screenings that are available to you.
- 8 Weeks: During your first OB visit, you will receive information regarding the First Trimester and Cystic Fibrosis screenings. Your NOB lab panel will be drawn, including blood type and screen, complete blood count, urine culture and screenings for hepatitis B, syphilis, rubella and HIV.
- 10-12 Weeks: Your next visit will be the busiest. You will have a physical and pelvic exam including Pap smear, gonorrhea and chlamydia cultures. Your provider will review your lab results from your first visit. If you elect to have the First Trimester Screening, it will take place between 11-13 weeks.
- 15-16 Weeks: If you elect to have this study, you will have blood drawn for the AFP/Tetra Screen (or Quad Screen) which used to evaluate whether your pregnancy has an increased chance of being affected with certain conditions, such as Down syndrome or neural tube defects.
- 16-20 Weeks: You will have a detailed ultrasound exam and if medically indicated, genetic counseling and/or amniocentesis may be performed. This point in your pregnancy is a good time to register for any OB classes. You can register for prenatal classes at Alamance Regional Medical Center online or by call (336) 586-4000 during regular business hours.
- 28 Weeks: One hour after drinking a glucose concentrate, you will have blood drawn to screen for Gestational Diabetes . A repeat HIV Screening will be performed and you will be offered the Tdap vaccine which protects against tetanus, diphtheria and pertussis (whooping cough). Patients with an Rh-negative blood type will receive RhoGAM, a prescription medicine that is used to prevent Rh immunization.
- 35-36 Weeks: Your final routine prenatal screening, a vaginal swab will be performed to test for the presence of vaginal beta strep . During this appointment, your cervix may also be examined for changes as your body prepares for delivery.
Patient Portal
As a patient at Kernodle OB/GYN, you can view lab and test results as well as a summary of your health history at any time through the convenience of our online patient portal, Duke MyChart. You can also view and schedule upcoming appointments, request prescription refills, view and pay your bill, and send a secure message to your healthcare team about any non-urgent needs. If you have questions about Duke MyChart, including how to sign in or receive an activation code, contact Duke Customer Services at (919) 620-4555 or toll-free at (800) 782-6945.
Patient Links
- Meet the Team
- For Patients
- Patient Stories
- Our Services
- Schedule an Appointment
Help us serve you better and tell us how we're doing.
Appointments at Mayo Clinic
- Pregnancy week by week
Prenatal care: 3rd trimester visits
During the third trimester, prenatal care might include vaginal exams to check the baby's position.
Prenatal care is an important part of a healthy pregnancy, especially as your due date approaches. Your health care provider might ask you to schedule prenatal care appointments during your third trimester about every 2 or 4 weeks, depending on your health and pregnancy history. Starting at 36 weeks, you'll need weekly checkups until you deliver.
Repeat routine health checks
You'll be asked if you have any signs or symptoms, including contractions and leakage of fluid or bleeding. Your health care provider will check your blood pressure and weight gain, as well as your baby's heartbeat and movements.
Your health care provider might ask you to track of how often you feel the baby move on a daily basis — and to alert your health care team if the baby stops moving as much as usual.
Also, talk to your health care provider about any vaccinations you might need, including the flu shot and the tetanus toxoid, reduced diphtheria toxoid and acellular pertussis (Tdap) vaccine. Ideally, the Tdap vaccine should be given between 27 and 36 weeks of pregnancy.
Test for group B strep
Expect to be screened for group B streptococcus (GBS) during the third trimester. GBS is a common bacterium often carried in the intestines or lower genital tract that's usually harmless in adults. But babies who become infected with GBS from exposure during vaginal delivery can become seriously ill.
To screen for GBS , your health care provider will swab your lower vagina and anal area. The sample will be sent to a lab for testing. If the sample tests positive for GBS — or you previously gave birth to a baby who developed GBS disease — you'll be given intravenous antibiotics during labor. The antibiotics will help protect your baby from the bacterium.
Check the baby's position
Near the end of pregnancy, your health care provider might check to see if your baby is positioned headfirst in the uterus.
If your baby is positioned rump-first (frank breech) or feet-first (complete breech) after week 36 of pregnancy, it's unlikely that the baby will move to a headfirst position before labor. You might be able to have an external cephalic version. During this procedure, your health care provider will apply pressure to your abdomen and physically manipulate your baby to a headfirst position. This is typically done with ultrasound guidance by an experienced doctor. If you prefer not to have this procedure, or if your baby remains in a breech position, your health care provider will discuss planning a C-section delivery.
Keep asking questions
You will likely have plenty of questions as your due date approaches. Is it OK to have sex? How will I know when I'm in labor? What's the best way to manage the pain? Should I create a birth plan? Ask away! Feeling prepared can help calm your nerves before delivery.
Also, be sure to discuss signs that should cause you to call your health care provider, such as vaginal bleeding or fluid leaking from the vagina, as well as when and how to contact your health care provider once labor begins.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Frequently asked questions. Pregnancy FAQ079. If your baby is breech. American College of Obstetricians and Gynecologists. https://www.acog.org/Patients/FAQs/If-Your-Baby-Is-Breech. Accessed July 13, 2018.
- Prenatal care and tests. Office on Women's Health. https://www.womenshealth.gov/pregnancy/youre-pregnant-now-what/prenatal-care-and-tests. Accessed July 9, 2018.
- Cunningham FG, et al., eds. Prenatal care. In: Williams Obstetrics. 25th ed. New York, N.Y.: McGraw-Hill Education; 2018. https://www.accessmedicine.mhmedical.com. Accessed July 9, 2018.
- Hofmeyr GJ. External cephalic version. https://www.uptodate.com/contents/search. Accessed July 10, 2018.
- Lockwood CJ, et al. Prenatal care: Second and third trimesters. https://www.uptodate.com/contents/search. Accessed July 9, 2018.
- AskMayoExpert. Vaccination during pregnancy. Rochester, Minn.: Mayo Foundation for Medical Education and Research; 2018.
Products and Services
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 3rd trimester pregnancy
- Fetal development: The 3rd trimester
- Fetal presentation before birth
- Overdue pregnancy
- Pregnancy due date calculator
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Prenatal care 3rd trimester visits
We’re transforming healthcare
Make a gift now and help create new and better solutions for more than 1.3 million patients who turn to Mayo Clinic each year.

- Copy/Paste Link Link Copied
What happens during prenatal visits?
What happens during prenatal visits varies depending on how far along you are in your pregnancy.
Schedule your first prenatal visit as soon as you think you are pregnant, even if you have confirmed your pregnancy with a home pregnancy test. Early and regular prenatal visits help your health care provider monitor your health and the growth of the fetus.
The First Visit
Your first prenatal visit will probably be scheduled sometime after your eighth week of pregnancy. Most health care providers won't schedule a visit any earlier unless you have a medical condition, have had problems with a pregnancy in the past, or have symptoms such as spotting or bleeding, stomach pain, or severe nausea and vomiting. 1
You've probably heard pregnancy discussed in terms of months and trimesters (units of about 3 months). Your health care provider and health information might use weeks instead. Here's a chart that can help you understand pregnancy stages in terms of trimesters, months, and weeks.
Because your first visit will be one of your longest, allow plenty of time.
During the visit, you can expect your health care provider to do the following: 1
- Answer your questions. This is a great time to ask questions and share any concerns you may have. Keep a running list for your visit.
- Check your urine sample for infection and to confirm your pregnancy.
- Check your blood pressure, weight, and height.
- Calculate your due date based on your last menstrual cycle and ultrasound exam.
- Ask about your health, including previous conditions, surgeries, or pregnancies.
- Ask about your family health and genetic history.
- Ask about your lifestyle, including whether you smoke, drink, or take drugs, and whether you exercise regularly.
- Ask about your stress level.
- Perform prenatal blood tests to do the following:
- Determine your blood type and Rh (Rhesus) factor. Rh factor refers to a protein found on red blood cells. If the mother is Rh negative (lacks the protein) and the father is Rh positive (has the protein), the pregnancy requires a special level of care. 2
- Do a blood count (e.g., hemoglobin, hematocrit).
- Test for hepatitis B, HIV, rubella, and syphilis.
- Do a complete physical exam, including a pelvic exam, and cultures for gonorrhea and chlamydia.
- Do a Pap test or test for human papillomavirus (HPV) or both to screen for cervical cancer and infection with HPV, which can increase risk for cervical cancer. The timing of these tests depends on the schedule recommended by your health care provider.
- Do an ultrasound test, depending on the week of pregnancy.
- Offer genetic testing: screening for Down syndrome and other chromosomal problems, cystic fibrosis, other specialized testing depending on history.
Prenatal Visit Schedule
If your pregnancy is healthy, your health care provider will set up a regular schedule for visits that will probably look about like this: 1
Later Prenatal Visits
As your pregnancy progresses, your prenatal visits will vary greatly. During most visits, you can expect your health care provider to do the following:
- Check your blood pressure.
- Measure your weight gain.
- Measure your abdomen to check your developing infant's growth—"fundal height" (once you begin to "show").
- Check the fetal heart rate.
- Check your hands and feet for swelling.
- Feel your abdomen to find the fetus's position (later in pregnancy).
- Do tests, such as blood tests or an ultrasound exam.
Talk to you about your questions or concerns. It's a good idea to write down your questions and bring them with you.
Several of these visits will include special tests to check for gestational diabetes (usually between 24 and 28 weeks) 3 and other conditions, depending on your age and family history.
In addition, the Centers for Disease Control and Prevention and the American Academy of Pediatrics released new vaccine guidelines for 2013 , including a recommendation for pregnant women to receive a booster of whooping cough (pertussis) vaccine. The guidelines recommend the shot be given between 27 and 36 weeks of pregnancy. 4
- Centers for Disease Control and Prevention. (2013). Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine (TDAP) in pregnant women―Advisory Committee on Immunization Practices (ACIP), 2012. Retrieved September 20, 2013, from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6207a4.htm

An official website of the United States government
Here's how you know
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- U.S. Department of Health & Human Services

Call the OWH HELPLINE: 1-800-994-9662 9 a.m. — 6 p.m. ET, Monday — Friday OWH and the OWH helpline do not see patients and are unable to: diagnose your medical condition; provide treatment; prescribe medication; or refer you to specialists. The OWH helpline is a resource line. The OWH helpline does not provide medical advice.
Please call 911 or go to the nearest emergency room if you are experiencing a medical emergency.
Prenatal care and tests

Medical checkups and screening tests help keep you and your baby healthy during pregnancy. This is called prenatal care. It also involves education and counseling about how to handle different aspects of your pregnancy. During your visits, your doctor may discuss many issues, such as healthy eating and physical activity, screening tests you might need, and what to expect during labor and delivery.
Choosing a prenatal care provider
You will see your prenatal care provider many times before you have your baby. So you want to be sure that the person you choose has a good reputation, and listens to and respects you. You will want to find out if the doctor or midwife can deliver your baby in the place you want to give birth , such as a specific hospital or birthing center. Your provider also should be willing and able to give you the information and support you need to make an informed choice about whether to breastfeed or bottle-feed.
Health care providers that care for women during pregnancy include:
- Obstetricians (OB) are medical doctors who specialize in the care of pregnant women and in delivering babies. OBs also have special training in surgery so they are also able to do a cesarean delivery . Women who have health problems or are at risk for pregnancy complications should see an obstetrician. Women with the highest risk pregnancies might need special care from a maternal-fetal medicine specialist .
- Family practice doctors are medical doctors who provide care for the whole family through all stages of life. This includes care during pregnancy and delivery, and following birth. Most family practice doctors cannot perform cesarean deliveries.
- A certified nurse-midwife (CNM) and certified professional midwife (CPM) are trained to provide pregnancy and postpartum care. Midwives can be a good option for healthy women at low risk for problems during pregnancy, labor, or delivery. A CNM is educated in both nursing and midwifery. Most CNMs practice in hospitals and birth centers. A CPM is required to have experience delivering babies in home settings because most CPMs practice in homes and birthing centers. All midwives should have a back-up plan with an obstetrician in case of a problem or emergency.
Ask your primary care doctor, friends, and family members for provider recommendations. When making your choice, think about:
- Personality and bedside manner
- The provider's gender and age
- Office location and hours
- Whether you always will be seen by the same provider during office checkups and delivery
- Who covers for the provider when she or he is not available
- Where you want to deliver
- How the provider handles phone consultations and after-hour calls
What is a doula?
A doula (DOO-luh) is a professional labor coach, who gives physical and emotional support to women during labor and delivery. They offer advice on breathing, relaxation, movement, and positioning. Doulas also give emotional support and comfort to women and their partners during labor and birth. Doulas and midwives often work together during a woman's labor. A recent study showed that continuous doula support during labor was linked to shorter labors and much lower use of:
- Pain medicines
- Oxytocin (ok-see-TOHS-uhn) (medicine to help labor progress)
- Cesarean delivery
Check with your health insurance company to find out if they will cover the cost of a doula. When choosing a doula, find out if she is certified by Doulas of North America (DONA) or another professional group.
Places to deliver your baby
Many women have strong views about where and how they'd like to deliver their babies. In general, women can choose to deliver at a hospital, birth center, or at home. You will need to contact your health insurance provider to find out what options are available. Also, find out if the doctor or midwife you are considering can deliver your baby in the place you want to give birth.
Hospitals are a good choice for women with health problems, pregnancy complications, or those who are at risk for problems during labor and delivery. Hospitals offer the most advanced medical equipment and highly trained doctors for pregnant women and their babies. In a hospital, doctors can do a cesarean delivery if you or your baby is in danger during labor. Women can get epidurals or many other pain relief options. Also, more and more hospitals now offer on-site birth centers, which aim to offer a style of care similar to standalone birth centers.
Questions to ask when choosing a hospital:
- Is it close to your home?
- Is a doctor who can give pain relief, such as an epidural, at the hospital 24-hours a day?
- Do you like the feel of the labor and delivery rooms?
- Are private rooms available?
- How many support people can you invite into the room with you?
- Does it have a neonatal intensive care unit (NICU) in case of serious problems with the baby?
- Can the baby stay in the room with you?
- Does the hospital have the staff and set-up to support successful breastfeeding?
- Does it have an on-site birth center?
Birth or birthing centers give women a "homey" environment in which to labor and give birth. They try to make labor and delivery a natural and personal process by doing away with most high-tech equipment and routine procedures. So, you will not automatically be hooked up to an IV. Likewise, you won't have an electronic fetal monitor around your belly the whole time. Instead, the midwife or nurse will check in on your baby from time to time with a handheld machine. Once the baby is born, all exams and care will occur in your room. Usually certified nurse-midwives, not obstetricians, deliver babies at birth centers. Healthy women who are at low risk for problems during pregnancy, labor, and delivery may choose to deliver at a birth center.
Women can not receive epidurals at a birth center, although some pain medicines may be available. If a cesarean delivery becomes necessary, women must be moved to a hospital for the procedure. After delivery, babies with problems can receive basic emergency care while being moved to a hospital.
Many birthing centers have showers or tubs in their rooms for laboring women. They also tend to have comforts of home like large beds and rocking chairs. In general, birth centers allow more people in the delivery room than do hospitals.
Birth centers can be inside of hospitals, a part of a hospital or completely separate facilities. If you want to deliver at a birth center, make sure it meets the standards of the Accreditation Association for Ambulatory Health Care, The Joint Commission, or the American Association of Birth Centers. Accredited birth centers must have doctors who can work at a nearby hospital in case of problems with the mom or baby. Also, make sure the birth center has the staff and set-up to support successful breastfeeding.
Homebirth is an option for healthy pregnant women with no risk factors for complications during pregnancy, labor or delivery. It is also important women have a strong after-care support system at home. Some certified nurse midwives and doctors will deliver babies at home. Many health insurance companies do not cover the cost of care for homebirths. So check with your plan if you'd like to deliver at home.
Homebirths are common in many countries in Europe. But in the United States, planned homebirths are not supported by the American Congress of Obstetricians and Gynecologists (ACOG). ACOG states that hospitals are the safest place to deliver a baby. In case of an emergency, says ACOG, a hospital's equipment and highly trained doctors can provide the best care for a woman and her baby.
If you are thinking about a homebirth, you need to weigh the pros and cons. The main advantage is that you will be able to experience labor and delivery in the privacy and comfort of your own home. Since there will be no routine medical procedures, you will have control of your experience.
The main disadvantage of a homebirth is that in case of a problem, you and the baby will not have immediate hospital/medical care. It will have to wait until you are transferred to the hospital. Plus, women who deliver at home have no options for pain relief.
To ensure your safety and that of your baby, you must have a highly trained and experienced midwife along with a fail-safe back-up plan. You will need fast, reliable transportation to a hospital. If you live far away from a hospital, homebirth may not be the best choice. Your midwife must be experienced and have the necessary skills and supplies to start emergency care for you and your baby if need be. Your midwife should also have access to a doctor 24 hours a day.
Prenatal checkups
During pregnancy, regular checkups are very important. This consistent care can help keep you and your baby healthy, spot problems if they occur, and prevent problems during delivery. Typically, routine checkups occur:
- Once each month for weeks four through 28
- Twice a month for weeks 28 through 36
- Weekly for weeks 36 to birth
Women with high-risk pregnancies need to see their doctors more often.
At your first visit your doctor will perform a full physical exam, take your blood for lab tests, and calculate your due date. Your doctor might also do a breast exam, a pelvic exam to check your uterus (womb), and a cervical exam, including a Pap test. During this first visit, your doctor will ask you lots of questions about your lifestyle, relationships, and health habits. It's important to be honest with your doctor.
After the first visit, most prenatal visits will include:
- Checking your blood pressure and weight
- Checking the baby's heart rate
- Measuring your abdomen to check your baby's growth
You also will have some routine tests throughout your pregnancy, such as tests to look for anemia , tests to measure risk of gestational diabetes , and tests to look for harmful infections.
Become a partner with your doctor to manage your care. Keep all of your appointments — every one is important! Ask questions and read to educate yourself about this exciting time.
Monitor your baby's activity
After 28 weeks, keep track of your baby's movement. This will help you to notice if your baby is moving less than normal, which could be a sign that your baby is in distress and needs a doctor's care. An easy way to do this is the "count-to-10" approach. Count your baby's movements in the evening — the time of day when the fetus tends to be most active. Lie down if you have trouble feeling your baby move. Most women count 10 movements within about 20 minutes. But it is rare for a woman to count less than 10 movements within two hours at times when the baby is active. Count your baby's movements every day so you know what is normal for you. Call your doctor if you count less than 10 movements within two hours or if you notice your baby is moving less than normal. If your baby is not moving at all, call your doctor right away.
Prenatal tests
Tests are used during pregnancy to check your and your baby's health. At your fist prenatal visit, your doctor will use tests to check for a number of things, such as:
- Your blood type and Rh factor
- Infections, such as toxoplasmosis and sexually transmitted infections (STIs), including hepatitis B , syphilis , chlamydia , and HIV
- Signs that you are immune to rubella (German measles) and chicken pox
Throughout your pregnancy, your doctor or midwife may suggest a number of other tests, too. Some tests are suggested for all women, such as screenings for gestational diabetes, Down syndrome, and HIV. Other tests might be offered based on your:
- Personal or family health history
- Ethnic background
- Results of routine tests
Some tests are screening tests. They detect risks for or signs of possible health problems in you or your baby. Based on screening test results, your doctor might suggest diagnostic tests. Diagnostic tests confirm or rule out health problems in you or your baby.
Understanding prenatal tests and test results
If your doctor suggests certain prenatal tests, don't be afraid to ask lots of questions. Learning about the test, why your doctor is suggesting it for you, and what the test results could mean can help you cope with any worries or fears you might have. Keep in mind that screening tests do not diagnose problems. They evaluate risk. So if a screening test comes back abnormal, this doesn't mean there is a problem with your baby. More information is needed. Your doctor can explain what test results mean and possible next steps.
Avoid keepsake ultrasounds
You might think a keepsake ultrasound is a must-have for your scrapbook. But, doctors advise against ultrasound when there is no medical need to do so. Some companies sell "keepsake" ultrasound videos and images. Although ultrasound is considered safe for medical purposes, exposure to ultrasound energy for a keepsake video or image may put a mother and her unborn baby at risk. Don't take that chance.
High-risk pregnancy
Pregnancies with a greater chance of complications are called "high-risk." But this doesn't mean there will be problems. The following factors may increase the risk of problems during pregnancy:
- Very young age or older than 35
- Overweight or underweight
- Problems in previous pregnancy
- Health conditions you have before you become pregnant, such as high blood pressure , diabetes , autoimmune disorders , cancer , and HIV
- Pregnancy with twins or other multiples
Health problems also may develop during a pregnancy that make it high-risk, such as gestational diabetes or preeclampsia . See Pregnancy complications to learn more.
Women with high-risk pregnancies need prenatal care more often and sometimes from a specially trained doctor. A maternal-fetal medicine specialist is a medical doctor that cares for high-risk pregnancies.
If your pregnancy is considered high risk, you might worry about your unborn baby's health and have trouble enjoying your pregnancy. Share your concerns with your doctor. Your doctor can explain your risks and the chances of a real problem. Also, be sure to follow your doctor's advice. For example, if your doctor tells you to take it easy, then ask your partner, family members, and friends to help you out in the months ahead. You will feel better knowing that you are doing all you can to care for your unborn baby.

Paying for prenatal care
Pregnancy can be stressful if you are worried about affording health care for you and your unborn baby. For many women, the extra expenses of prenatal care and preparing for the new baby are overwhelming. The good news is that women in every state can get help to pay for medical care during their pregnancies. Every state in the United States has a program to help. Programs give medical care, information, advice, and other services important for a healthy pregnancy.
Learn more about programs available in your state.
You may also find help through these places:
- Local hospital or social service agencies – Ask to speak with a social worker on staff. She or he will be able to tell you where to go for help.
- Community clinics – Some areas have free clinics or clinics that provide free care to women in need.
- Women, Infants and Children (WIC) Program – This government program is available in every state. It provides help with food, nutritional counseling, and access to health services for women, infants, and children.
- Places of worship
More information on prenatal care and tests
Read more from womenshealth.gov.
- Pregnancy and Medicines Fact Sheet - This fact sheet provides information on the safety of using medicines while pregnant.
Explore other publications and websites
- Chorionic Villus Sampling (CVS) (Copyright © March of Dimes) - Chorionic villus sampling (CVS) is a prenatal test that can diagnose or rule out certain birth defects. The test is generally performed between 10 and 12 weeks after a woman's last menstrual period. This fact sheet provides information about this test, and how the test sample is taken.
- Folic Acid (Copyright © March of Dimes) - This fact sheet stresses the importance of getting higher amounts of folic acid during pregnancy in order to prevent neural tube defects in unborn children.
- Folic Acid: Questions and Answers - The purpose of this question and answer sheet is to educate women of childbearing age on the importance of consuming folic acid every day to reduce the risk of spina bifida.
- For Women With Diabetes: Your Guide to Pregnancy - This booklet discusses pregnancy in women with diabetes. If you have type 1 or type 2 diabetes and you are pregnant or hoping to get pregnant soon, you can learn what to do to have a healthy baby. You can also learn how to take care of yourself and your diabetes before, during, and after your pregnancy.
- Genetics Home Reference - This website provides information on specific genetic conditions and the genes or chromosomes responsible for these conditions.
- Guidelines for Vaccinating Pregnant Women - This publication provides information on routine and other vaccines and whether they are recommended for use during pregnancy.
- How Your Baby Grows (Copyright © March of Dimes) - This site provides information on the development of your baby and the changes in your body during each month of pregnancy. In addition, for each month, it provides information on when to go for prenatal care appointments and general tips to take care of yourself and your baby.
- Pregnancy Registries - Pregnancy registries help women make informed and educated decisions about using medicines during pregnancy. If you are pregnant and currently taking medicine — or have been exposed to a medicine during your pregnancy — you may be able to participate and help in the collection of this information. This website provides a list of pregnancy registries that are enrolling pregnant women.
- Pregnancy, Breastfeeding, and Bone Health - This publication provides information on pregnancy-associated osteoporosis, lactation and bone loss, and what you can do to keep your bones healthy during pregnancy.
- Prenatal Care: First-Trimester Visits (Copyright © Mayo Foundation) - This fact sheet explains what to expect during routine exams with your doctor. In addition, if you have a condition that makes your pregnancy high-risk, special tests may be performed on a regular basis to check the baby's health.
- Ten Tips for a Healthy Pregnancy (Copyright © Lamaze International) - This easy-to-read fact sheet provides 10 simple recommendations to help mothers have a healthy pregnancy.
- Ultrasound (Copyright © March of Dimes) - This fact sheet discusses the use of an ultrasound in prenatal care at each trimester.
Connect with other organizations
- American Academy of Family Physicians
- American Association of Birth Centers
- American College of Obstetricians and Gynecologists
- Center for Research on Reproduction and Women's Health, University of Pennsylvania Medical Center
- Dona International
- March of Dimes
- Maternal and Child Health Bureau, HRSA, HHS
- National Association for Down Syndrome
- National Center on Birth Defects and Developmental Disabilities, CDC
- Public Information and Communications Branch, NICHD, NIH, HHS
- HHS Non-Discrimination Notice
- Language Assistance Available
- Accessibility
- Privacy Policy
- Disclaimers
- Freedom of Information Act (FOIA)
- Use Our Content
- Vulnerability Disclosure Policy
- Kreyòl Ayisyen
A federal government website managed by the Office on Women's Health in the Office of the Assistant Secretary for Health at the U.S. Department of Health and Human Services.
1101 Wootton Pkwy, Rockville, MD 20852 1-800-994-9662 • Monday through Friday, 9 a.m. to 6 p.m. ET (closed on federal holidays).

Evaluation of the Obstetric Patient
- Physical Examination |
- Treatment |
Once pregnant, women require routine prenatal care to help safeguard their health and the health of the fetus. Also, evaluation is often required for symptoms and signs of illness. Common symptoms that are often pregnancy-related include
Vaginal bleeding
Pelvic pain
Lower-extremity edema
Specific obstetric disorders and nonobstetric disorders in pregnant woman are discussed elsewhere.
The initial routine prenatal visit should occur between 6 and 8 weeks gestation.
Follow-up visits should occur at
About 4-week intervals until 28 weeks
2-week intervals from 28 to 36 weeks
Weekly thereafter until delivery
Prenatal visits may be scheduled more frequently if risk of a poor pregnancy outcome is high or less frequently if risk is very low.
Prenatal care includes
Screening for disorders
Taking measures to reduce fetal and maternal risks
General reference
1. Shaw GM, O'Malley CD, Wasserman CR, et al : Maternal periconceptional use of multivitamins and reduced risk for conotruncal heart defects and limb deficiencies among offspring. Am J Med Genet 59:536–545, 1995. doi:10.1002/ajmg.1320590428
During the initial visit, clinicians should obtain a full medical history, including
Previous and current disorders
Drug use (therapeutic, social, and illicit)
Risk factors for complications of pregnancy (see table Pregnancy Risk Assessment )
Obstetric history, with the outcome of all previous pregnancies, including maternal and fetal complications (eg, gestational diabetes, preeclampsia, congenital malformations, stillbirth)
Family history should include all chronic disorders in family members to identify possible hereditary disorders ( genetic evaluation ).
During subsequent visits, queries focus on interim developments, particularly vaginal bleeding or fluid discharge, headache, changes in vision, edema of face or fingers, and changes in frequency or intensity of fetal movement.
Gravidity and parity
Gravidity is the number of confirmed pregnancies; a pregnant woman is a gravida. Parity is the number of deliveries after 20 weeks. Multifetal pregnancy is counted as one in terms of gravidity and parity. Abortus is the number of pregnancy losses (abortions) before 20 weeks regardless of cause (eg, spontaneous, therapeutic, or elective abortion; ectopic pregnancy). Sum of parity and abortus equals gravidity.
Parity is often recorded as 4 numbers:
Number of term deliveries (after 37 weeks)
Number of premature deliveries ( > 20 and < 37 weeks)
Number of abortions
Number of living children
Thus, a woman who is pregnant and has had one term delivery, one set of twins born at 32 weeks, and 2 abortions is gravida 5, para 1-1-2-3.
Physical Examination
A full general examination, including blood pressure (BP), height, and weight, is done first. Body mass index (BMI) should be calculated and recorded. BP and weight should be measured at each prenatal visit.
In the initial obstetric examination, speculum and bimanual pelvic examination is done for the following reasons:
To check for lesions or discharge
To note the color and consistency of the cervix
To obtain cervical samples for testing
Also, fetal heart rate and, in patients presenting later in pregnancy, lie of the fetus are assessed (see figure Leopold maneuver ).
Pelvic capacity can be estimated clinically by evaluating various measurements with the middle finger during bimanual examination. If the distance from the underside of the pubic symphysis to the sacral promontory is > 11.5 cm, the pelvic inlet is almost certainly adequate. Normally, distance between the ischial spines is ≥ 9 cm, length of the sacrospinous ligaments is 4 to ≥ 5 cm, and the subpubic arch is ≥ 90 ° .
During subsequent visits, BP and weight assessment is important. Obstetric examination focuses on uterine size, fundal height (in cm above the symphysis pubis), fetal heart rate and activity, and maternal diet, weight gain, and overall well-being. Speculum and bimanual examination is usually not needed unless vaginal discharge or bleeding, leakage of fluid, or pain is present.
Laboratory testing
Prenatal evaluation involves urine tests and blood tests. Initial laboratory evaluation is thorough; some components are repeated during follow-up visits (see table Components of Routine Prenatal Evaluation).
If a woman has Rh-negative blood, she may be at risk of developing Rh(D) antibodies, and if the father has Rh-positive blood, the fetus may be at risk of developing erythroblastosis fetalis . Rh(D) antibody levels should be measured in pregnant women at the initial prenatal visit and again at about 26 to 28 weeks. At that time, women who have Rh-negative blood are given a prophylactic dose of Rh(D) immune globulin. Additional measures may be necessary to prevent development of maternal Rh antibodies.
Urine is also tested for protein. Proteinuria before 20 weeks gestation suggests kidney disease. Proteinuria after 20 weeks gestation may indicate preeclampsia .
Generally, women are routinely screened for gestational diabetes between 24 and 28 weeks using a 50-g, 1-hour test. However, if women have significant risk factors for gestational diabetes, they are screened during the 1st trimester. These risk factors include
Gestational diabetes or a macrosomic neonate (weight > 4500 g at birth) in a previous pregnancy
Unexplained fetal losses
A strong family history of diabetes in 1st-degree relatives
A history of persistent glucosuria
Body mass index (BMI) > 30 kg/m2
Polycystic ovary syndrome with insulin resistance
If the 1st-trimester test is normal, the 50-g test should repeated at 24 to 28 weeks, followed, if abnormal, by a 3-hour test. Abnormal results on both tests confirms the diagnosis of gestational diabetes.
Women at high risk of aneuploidy (eg, those > 35 years, those who have had a child with Down syndrome) should be offered screening with maternal serum cell-free DNA .
In some pregnant women, blood tests to screen for thyroid disorders (measurement of thyroid-stimulating hormone [TSH]) are done. These women may include those who
Have symptoms
Come from an area where moderate to severe iodine insufficiency occurs
Have a family or personal history of thyroid disorders
Have type 1 diabetes
Have a history of infertility, preterm delivery, or miscarriage
Have had head or neck radiation therapy
Are morbidly obese (BMI > 40 kg/m2)
Are > 30 years
Ultrasonography
Most obstetricians recommend at least one ultrasound examination during each pregnancy, ideally between 16 and 20 weeks, when estimated delivery date (EDD) can still be confirmed fairly accurately and when placental location and fetal anatomy can be evaluated. Estimates of gestational age are based on measurements of fetal head circumference, biparietal diameter, abdominal circumference, and femur length. Measurement of fetal crown-rump length during the 1st trimester is particularly accurate in predicting EDD: to within about 5 days when measurements are made at < 12 weeks gestation and to within about 7 days at 12 to 15 weeks. Ultrasonography during the 3rd trimester is accurate for predicting EDD to within about 2 to 3 weeks.
Specific indications for ultrasonography include
Investigation of abnormalities during the 1st trimester (eg, indicated by abnormal results of noninvasive maternal screening tests)
Risk assessment for chromosomal abnormalities (eg, Down syndrome) including nuchal translucency measurement
Need for detailed assessment of fetal anatomy (usually at about 16 to 20 weeks), possibly including fetal echocardiography at 20 weeks if risk of congenital heart defects is high (eg, in women who have type 1 diabetes or have had a child with a congenital heart defect)
Detection of multifetal pregnancy, hydatidiform mole, polyhydramnios, placenta previa, or ectopic pregnancy
Determination of placental location, fetal position and size, and size of the uterus in relation to given gestational dates (too small or too large)
Ultrasonography is also used for needle guidance during chorionic villus sampling , amniocentesis , and fetal transfusion. High-resolution ultrasonography includes techniques that maximize sensitivity for detecting fetal malformations.
If ultrasonography is needed during the 1st trimester (eg, to evaluate pain, bleeding, or viability of pregnancy), use of an endovaginal transducer maximizes diagnostic accuracy; evidence of an intrauterine pregnancy (gestational sac or fetal pole) can be seen as early as 4 to 5 weeks and is seen at 7 to 8 weeks in > 95% of cases. With real-time ultrasonography, fetal movements and heart motion can be directly observed as early as 5 to 6 weeks.
Other imaging
Conventional x-rays can induce spontaneous abortion or congenital malformations, particularly during early pregnancy. Risk is remote (up to about 1/million) with each x-ray of an extremity or of the neck, head, or chest if the uterus is shielded. Risk is higher with abdominal, pelvic, and lower back x-rays. Thus, for all women of childbearing age, an imaging test with less ionizing radiation (eg, ultrasonography) should be substituted when possible, or if x-rays are needed, the uterus should be shielded (because pregnancy is possible).
Medically necessary x-rays or other imaging should not be postponed because of pregnancy. However, elective x-rays are postponed until after pregnancy.
Problems identified during evaluation are managed.
Women are counseled about exercise and diet and advised to follow the Institute of Medicine guidelines for weight gain, which are based on prepregnancy body mass index (BMI—see table Guidelines for Weight Gain During Pregnancy ). Nutritional supplements are prescribed.
What to avoid, what to expect, and when to obtain further evaluation are explained. Couples are encouraged to attend childbirth classes.
Diet and supplements
To provide nutrition for the fetus, most women require about 250 kcal extra daily; most calories should come from protein. If maternal weight gain is excessive ( > 1.4 kg/month during the early months) or inadequate ( < 0.9 kg/month), diet must be modified further. Weight-loss dieting during pregnancy is not recommended, even for morbidly obese women.
Most pregnant women need a daily oral iron supplement of ferrous sulfate 300 mg or ferrous gluconate 450 mg, which may be better tolerated. Woman with anemia should take the supplements twice a day.
All women should be given oral prenatal vitamins that contain folate 400 mcg (0.4 mg), taken once a day; folate reduces risk of neural tube defects. For women who have had a fetus or infant with a neural tube defect, the recommended daily dose is 4000 mcg (4 mg).
Physical activity
Exercise during pregnancy has minimal risks and has demonstrated benefits for most pregnant women, including maintenance or improvement of physical fitness, control of gestational weight gain, reduction in low back pain, and possibly a reduction in risk of developing gestational diabetes or preeclampsia. Moderate exercise is not a direct cause of any adverse pregnancy outcome; however, pregnant women may be at greater risk of injuries to joints, falling, and abdominal trauma. Abdominal trauma can result in abruptio placentae, which can lead to fetal morbidity or death.
Most experts agree that exercise during pregnancy is safe and can improve pregnancy outcomes (eg, reduced excessive gestational weight gain, gestational diabetes [ 1 ]).
Sexual intercourse can be continued throughout pregnancy unless vaginal bleeding, pain, leakage of amniotic fluid, or uterine contractions occur.
The safest time to travel during pregnancy is between 14 and 28 weeks, but there is no absolute contraindication to travel at any time during pregnancy. Pregnant women should wear seat belts regardless of gestational age and type of vehicle.
Travel on airplanes is safe until 36 weeks gestation. The primary reason for this restriction is the risk of labor and delivery in an unfamiliar environment.
During any kind of travel, pregnant women should stretch and straighten their legs and ankles periodically to prevent venous stasis and the possibility of thrombosis. For example, on long flights, they should walk or stretch every 2 to 3 hours. In some cases, the clinician may recommend thromboprophylaxis for prolonged travel.
Immunizations
Vaccines for measles, mumps, rubella, and varicella should not be used during pregnancy.
Although the COVID 19 vaccine has not been specifically evaluated in pregnant women, the American College of Obstetricians and Gynecologists (ACOG) recommends that COVID-19 vaccines not be withheld from pregnant women who meet the criteria for vaccination based on the Advisory Committee on Immunization Practices (ACIP) recommended priority groups. Various COVID 19 vaccines have received authorization for emergency use from the Food and Drug Administration (FDA) and the World Health Organization (WHO) as listed on its Emergency Use Listing. (See also the Centers for Disease Control and Prevention: COVID-19 vaccination .)
Because pregnant women with Rh-negative blood are at risk of developing Rh(D) antibodies, they are given Rh(D) immune globulin 300 mcg IM in any of the following situations:
After any significant vaginal bleeding or other sign of placental hemorrhage or placental abruption
After a spontaneous or therapeutic abortion
After amniocentesis or chorionic villus sampling
Prophylactically at 28 weeks
If the neonate has Rh(D)-positive blood, after delivery
Modifiable risk factors
Pregnant women should not use alcohol and tobacco and should avoid exposure to secondhand smoke.
They should also avoid the following:
Exposure to chemicals or paint fumes
Direct handling of cat litter (due to risk of toxoplasmosis)
Prolonged temperature elevation (eg, in a hot tub or sauna)
Exposure to people with active viral infections (eg, rubella, parvovirus infection [fifth disease], varicella)
Women with substance abuse problems should be monitored by a specialist in high-risk pregnancy . Screening for domestic violence and depression should be done.
Drugs and vitamins that are not medically indicated should be discouraged (see Drugs in Pregnancy ).
Symptoms requiring evaluation
Women should be advised to seek evaluation for unusual headaches, visual disturbances, pelvic pain or cramping, vaginal bleeding, rupture of membranes, extreme swelling of the hands or face, diminished urine volume, any prolonged illness or infection, or persistent symptoms of labor.
Multiparous women with a history of rapid labor should notify the physician at the first symptom of labor.
Treatment reference
1. Syed H, Slayman T, Thoma KD: ACOG [American College of Obstetricians and Gynecologists] Committee Opinion No. 804 : Physical activity and exercise during pregnancy and the postpartum period. 2020. PMID: 33481513. doi: 10.1097/AOG.0000000000004266

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Your Guide to Prenatal Appointments
Medical review policy, latest update:.
Minor copy changes.
Typical prenatal appointment schedule
Read this next, what happens during a prenatal care appointment, what tests will i receive at my prenatal appointments, what will i talk about with my practitioner at prenatal care appointments , first trimester prenatal appointments: what to expect, second trimester prenatal appointments: what to expect, third trimester prenatal appointments: what to expect, questions to ask during prenatal appointments .
Prenatal care visits are chock-full of tests, measurements, questions and concerns, but know that throughout the process your and your baby’s wellbeing are the main focus. Keep your schedule organized so you don’t miss any appointments and jot down anything you want to discuss with your doctor and your prenatal experience should end up being both positive and rewarding.
What to Expect When You’re Expecting , 5th edition, Heidi Murkoff. American College of Obstetricians and Gynecologists, Having a Baby After Age 35: How Aging Affects Fertility and Pregnancy , 2020. American College of Obstetricians and Gynecologists, Routine Tests During Pregnancy , 2020. US Department of Health & Human Services, Office on Women’s Health, Prenatal Care and Tests , January 2019. Journal of Perinatology , Number of Prenatal Visits and Pregnancy Outcomes in Low-risk wWomen , June 2016. Mayo Clinic, Edema , October 2017. Mayo Clinic, Prenatal Care: 2nd Trimester Visits , August 2020. Mayo Clinic, Prenatal Care: 3rd Trimester Visits , August 2020. Jennifer Leighdon Wu, M.D., Women’s Health of Manhattan, New York, NY. WhatToExpect.com, Preeclampsia: Symptoms, Risk Factors and Treatment , April 2019. WhatToExpect.com, Prenatal Testing During Pregnancy , March 2019. WhatToExpect.com, Urine Tests During Pregnancy , May 2019. WhatToExpect.com, Fetal Heartbeat: The Development of Baby’s Circulatory System , April 2019. WhatToExpect.com, Amniocentesis , Mary 2019. WhatToExpect.com, Ultrasound During Pregnancy , April 2019. WhatToExpect.com, Rh Factor Testing , June 2019. WhatToExpect.com, Glucose Screening and Glucose Tolerance Test , April 2019. WhatToExpect.com, Nuchal Translucency Screening , April 2019. WhatToExpect.com, Group B Strep Testing During Pregnancy , August 2019. WhatToExpect.com, The Nonstress Test During Pregnancy , April 2019. WhatToExpect.com, Biophysical Profile (BPP) , May 2019. WhatToExpect.com, Noninvasive Prenatal Testing , (NIPT), April 2019. WhatToExpect.com, The Quad Screen , February 2019. WhatToExpect.com, Chorionic Villus Sampling (CVS) , February 2019. WhatToExpect.com, The First Prenatal Appointment , June 2019. WhatToExpect.com, Breech Birth: What it Means for You , September 2018.
Updates history
Jump to your week of pregnancy, trending on what to expect, signs of labor, pregnancy calculator, ⚠️ you can't see this cool content because you have ad block enabled., top 1,000 baby girl names in the u.s., top 1,000 baby boy names in the u.s., braxton hicks contractions and false labor.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Thieme - PMC COVID-19 Collection

Considerations for Obstetric Care during the COVID-19 Pandemic
Sarah k. dotters-katz.
1 Department of Obstetrics and Gynecology, Duke University Medical Center, Durham, North Carolina
Brenna L. Hughes
The novel coronavirus disease 2019 (COVID-19) is a growing pandemic that is impacting daily life across the globe. Though disease is often mild, in high-risk populations, severe disease often leads to intubation, intensive care admission (ICU) admission, and in many cases death. The implications for pregnancy remain largely unknown. Early data suggest that COVID-19 may not pose increased risk in the pregnant population. Vertical transmission has not been confirmed. Because no treatment, no vaccine and no herd immunity exist, social distancing is the best mechanism available to protect patients and health care workers from infection. This review will discuss what is known about the virus as it relates to pregnancy and then consider management considerations based on these data.
- COVID-19 severity in pregnancy is unclear.
- Social distancing is the best protective mechanism.
- No clear evidence of vertical transmission exists.
- Mother/baby separation avoids transmission.
The severe acute respiratory syndrome–novel coronavirus-2 (SARS-CoV-2), also known as COVID-19, has emerged as a deadly global pandemic. Since its identification in Wuhan, China, in December 2019, over 1,000,000 individuals have tested positive, with likely hundreds of thousands more infected without a confirmatory diagnostic test in just 4 months worldwide.
The viral illness ranges in severity from a mild cold to pneumonia and death. At this time, the virus has been documented on every continent except Antarctica, with especially severe outbreaks in China, Italy, and New York City. Available data suggest the incubation period is approximately 5 days but can range from 2 to 14 days. 1 The estimated reproduction number (Ro) for COVID-19 is between 2.2 and 2.35. 2 3 Ro is a mathematical term that describes how infectious a disease or pathogen is. Said another way, this value is the average number of people who catch a disease from one contagious person. Infections are more severe and mortality markedly higher in individuals who are older than 50 years, or have underlying chronic illness such as heart disease and diabetes. 4 Early data suggest that in the general population, 80% of cases are mild (nonpneumonia or mild pneumonia), 14% develop more severe disease, and 6% develop critical illness. 5 Clearly, those with chronic respiratory conditions, such as asthma, chronic obstructive pulmonary disease, and cystic fibrosis, are also at heightened risk.
The virus is spread through respiratory droplets. Symptoms of the infection include fever, cough, dyspnea, myalgias, headaches, and gastrointestinal symptoms. A recent study suggested that approximately 42% of infected individuals will have both gastrointestinal and respiratory symptoms, and that those who presented with gastrointestinal symptoms had longer time from onset to admission and worse prognoses. 6 Laboratory abnormalities include leukopenia, lymphopenia, and in some cases thrombocytopenia. About 20% of infected individuals will develop severe disease, including a pneumonia with acute respiratory distress syndrome (ARDS)-like process. 7 8 Those individuals develop pathognomonic findings on computed tomographic (CT) scan including ground glass abnormalities early in the disease course. 9 Emerging data also suggest that the virus can affect the heart, causing a viral myocarditis and associated cardiac injury in patients with or without underlying cardiac pathology. 10 At this time, COVID-19 does not appear to cause microangiopathy in the heart or in other vascular beds. The median time from symptom onset to intensive care unit (ICU) admission is 10 days. 11
Mortality rates are varied, though appear to be between 0.6 and 4% depending on population, though as not all infected patients are tested, the true denominator is unknown. 11 12 Older patients, those with underlying medical conditions, and those with bacterial superinfection in the lungs, are at higher risk adverse outcomes ( Fig. 1 ). 4 13 Mortality among these populations is also much higher. Specifically, as high as 6% for those with hypertension, 7.3% for those with diabetes, and 6.3% for those with chronic respiratory pathologies. 10 14 Among hospitalized patients, mortality is as high as 13%. 7 The median time from symptom onset to death is 13 days. 1

Case fatality rate for COVID-19 infection in the United States by age group. COVID-19, novel coronavirus disease 2019.
At this time, no treatment for the virus exists. Treatment in mild cases includes oral hydration and symptomatic relief. For severe cases, supportive care is the standard of care. The use of systemic corticosteroids for severe pneumonia has been associated with worse outcomes in influenza, SARS, and Middle East respiratory syndrome (MERS), and thus is not recommended at this time. 15 Though one small nonrandomized trial of hydroxychloroquine and azithromycin suggested a decrease in viral burden, this study only included those with mild disease. 16 A recent systematic review on this topic found that chloroquine may be effective at treating COVID-19, but its use should only occur in clinical trials or as part of the monitored emergency use of unregistered interventions framework. 17 Though aggressive research efforts are underway, no vaccine is available at this time.
In this review, we will discuss the available evidence related to COVID-19 surrounding pregnancy, then discuss management considerations for infected pregnant women (and those who are persons under investigation), as well as noninfected pregnant women, during this time. In cases where no available data exist for COVID-19, we will draw on data from other recent coronavirus outbreaks, including SARS and MERS.
COVID-19 in Pregnancy
At this time, there are no reported cases of COVID-19 in the first trimester. Thus, the implications for miscarriage and teratogenicity are unknown. One case of first trimester MERS has been reported, and this pregnancy was uncomplicated. 18 Among cases of SARS, where first trimester infection was noted in the setting of a documented intrauterine gestation with cardiac activity ( n = 3), no anomalies or miscarriage was noted. 19 In a recent epidemiologic study by Rasmussen et al, no association between exposure to circulating influenza and rates of spontaneous abortion was seen. 20
Data exist regarding infection in pregnancy is rapidly accumulating. 21 22 23 24 At this time, in general, pregnant women do not appear to be at increased risk of developing COVID-19 compared with the general population. Additionally, unlike other respiratory infections, early data do not demonstrate increased risk of severe infection among pregnant women. The report from China by the World Health Organization included 147 pregnant women, 8% of whom developed severe disease (defined as respiratory rate >30 or oxygen saturation <93%), and 1% developed critical infection (defined as need for mechanical ventilation or other system failure and ICU admission). 25 Cases of severe maternal infection have been described, including need for extracorporeal membrane oxygenation (ECMO) and multisystem organ failure, though no cases of maternal death have been reported at time of this writing. 21 22 23 24 Multiple smaller studies are emerging with a common theme, women who are receiving care for obstetrical reasons and are asymptomatic, but develop symptoms 2 to 3 days into their stay, often postpartum. 26 27 28 The majority of the infections in these cases are mild. However, the exposure of health care workers during the asymptomatic phase of illness has led to significant impacts on the workforce in some centers.
The infection does not appear to increase the risk of preeclampsia. Nor did women with preeclampsia appear to have worse outcomes, compared with women with COVID-19 without preeclampsia. 23 In accounts where delivery specific details are available, preterm prelabor rupture of membranes does not appear to occur at higher rates than the general population ( n = 1, at 36 2/7 weeks). 23 Preterm labor is not specifically described in any of these reports. Risk of preterm delivery is difficult to ascertain from the existing literature. Though some of the reported deliveries occurred preterm, the rationale for early delivery is not well documented and most were at greater than 36 weeks of gestation. However, other respiratory viruses have been associated with increased risk of preterm birth, including H1N1, SARS, and MERS. 18 19 29 30
One case of intrauterine fetal demise has been documented with COVID-19, this occurred in the setting of multisystem organ failure and ECMO. 22 Maternal critical illness is known to be associated with increased rates of fetal demise, especially in the setting of ECMO. In a recent review of ECMO for a variety of indications in pregnancy, fetal survival was approximately 65%. 31 This review also analyzed influenza-related cases separately, where fetal survival was 71%. 31
Currently, in the published data relating to COVID-19, all pregnancies were delivered within 2 weeks of disease. Thus, the impact of COVID-19 infection on fetal growth in the setting of ongoing pregnancy is unclear. However, data from the H1N1 epidemic does suggest increased risk of small for gestational age infants. 32 Similarly, though less data exist, women who were infected with SARS and remained pregnant also appeared to be at increased risk for intrauterine growth restriction. 19
At this time, vertical transmission of COVID-19 has not been confirmed. SARS and MERS also have no reported cases of vertical transmission. Early data from Chinese series show no virus in the amniotic fluid, vaginal mucus, cord blood, or neonatal throat swab at the time of delivery. 23 24 Other series have also been reassuring for lack of vertical transmission. 21 24 33 However, some smaller neonatal series have found very early infections in infants born to COVID-19-positive mothers. In one series, infants who had been immediately separated from a COVID-19-positive mother, have tested positive 2 to 3 days after delivery. 33 In another report, an infant was born with elevated immunoglobulin (Ig)-M in the setting of strict infection control measures, suggesting possible infection during delivery, though authors state that vertical transmission cannot be ruled out. 34 35 At this time, more rigorous studies are needed. In series from China, the vast majority of women were delivered via cesarean. However, that likely relates more to local delivery practices rather than obstetrical necessity. There are no reports of breast milk samples containing virus. 23 24
Management Considerations during the COVID-19 Pandemic
Outpatient care.
In the current climate, because there is no treatment and no vaccine, the best option is prevention. The Centers for Disease Control (CDC) and the American College of Obstetricians and Gynecologists (ACOG) both recommend that all people avoid travel, gatherings of any sort, social visits, and going out to restaurants or bars. Clear data suggest that practices of social distancing are effective means to halt the spread of the pandemic. Additionally, it is recommended to frequently clean commonly touched surfaces, including computers, cell phones, counter tops, door knobs, etc. When in public places, recommendations are to maintain a distance of at least 6 feet from other people as much as possible.
In health care settings, social distancing can be challenging. Providers should consider spacing out work stations or only using every other computer. Other measures to be considered include, ensuring computers and all work room surfaces are cleaned frequently, and alcohol-based hand sanitizer is added to work rooms. Many clinics are making safety huddles virtual. Health care systems are actively implementing aggressive screening guidelines for patients. Some clinics are having patients check in virtually or by phone from their cars, and then are “calling” them in and taking vitals in the clinic room. This practice avoids patients sitting in waiting rooms, as well as being exposed to each other in intake rooms.
With regard to prenatal care, many practices are spacing out visits for the appropriate low-risk patients. Though no formal guidance exists on this, Table 1 shows the format that our health care system has utilized, with Table 2 outlining who is defined as low-risk. For patients with diabetes who need blood glucose monitoring, consider telephone, or video visits. Home blood pressure cuffs with phone visits can also be used for patients with chronic hypertension or postpartum blood pressure checks. For patients who are receiving 17-P weekly in the clinic, consider having the patients' transition to home administration. Makena (Waltham, MA) has an order form and patients can sign the order sheet online to facilitate telehealth visits. The online order form is available at https://www.eprescribemakenaai.com/ .
Abbreviations: GBS, Group B Strep; OB, obstetric; TDAP, Tetanus, Diphtheria and Pertussis.
ACOG has designed a triage system which can be used over the phone for patients who are concerned they are infected or persons under investigation, as far as guidance about the appropriate clinical setting for evaluation (ACOG algorithm). 36 Many women with mild infection and no comorbidities can be directed to stay home with symptomatic treatment, hydration, and rest. 36 Testing of this population should occur based on local recommendations but clinical evaluation is not necessary.
To avoid unnecessary contact between infected patients and other patients or health care personnel, patients with active infection, as well as those under quarantine, without urgent issues, can often defer prenatal visits until outside of the infectious window. For those with urgent obstetric concerns or who need prenatal visits and are under quarantine, some areas have created COVID-19-specific obstetric clinics, such that all patients within a single health system could be seen in the same place, a practice known as “cohorting.” The goal would be to avoid exposure to noninfected patients. Clinical practices that cover multiple offices or inpatient settings may also consider “cohorting” providers. Another option to minimize contact is to tele-read ultrasound and then “video visit” into a room to review the findings of the exam with the patient. Some ultrasound units are utilizing more cine clips, from these clips, the sonographer or reading provider can obtain single-image capture after the fact to minimize time in the room. Many health care systems are initiating mask wearing for all clinical providers and patients, even in the outpatient setting. 37
For patients who recover from the virus and have not delivered, assessment of fetal growth may be considered given the elevated risks of growth restriction associated with other severe respiratory viruses. 38 In the setting of normal fetal growth, antenatal testing is not indicated. Though some experts have suggested that the use of nonsteroidal anti-inflammatory medications could worsen symptoms, no studies have borne this out and thus ACOG continues to recommend the use of aspirin for prevention of preeclampsia in women at risk. 37
For women in the third trimester without a medical indication for delivery who become infected, providers may consider waiting until the patient is no longer within the 14-day quarantine period or the patient tests negative prior to induction or scheduled repeat cesarean depending upon gestational age. 38 Many offices are offering virtual postpartum visits for the appropriately selected patients, such as those who are low risk, had mild or no perineal lacerations, and whose contraception can be sent directly to their pharmacy. For patients who undergo cesarean delivery, skin closure with subcuticular suture is preferred to staples as it would prevent an in-person visit for staple removal.
Inpatient Care
Given the risk of asymptomatic viral shedding, some centers have begun universal screening of patients on labor and delivery. Many hospital systems have also implemented face masks for all health care personnel while in the hospital. When patients who are infected or person under investigation (PUI) need admission for an obstetric reason, all personnel who take care of the patient should wear appropriate personal protective equipment (PPE). 39
Visitor policies should be evaluated to limit potential exposures. Visitors should be screened for symptoms prior to admission to the unit, and then screened regularly if the patient remains in the hospital for more than a day. Some centers are not allowing any support persons on labor and delivery units, while others only completely restrict visitation for PUI or confirmed COVID-19 patients. Minimizing moving patients with COVID-19 from room to room is also important, thus consideration should be given to keeping the patient in the delivery room during the postpartum course if possible. Care providers who enter the room should also be minimized as much as possible. If room transfer is needed, the patient should wear a mask during transport between rooms.
Infection, even severe infection, is not necessarily an indication for delivery. 38 Similarly, infection at term is not an indication for cesarean delivery, outside usual obstetrical indications. 37 In rare cases, among severely ill pregnant woman in the third trimester, delivery may be necessary to improve respiratory status. There is no existing evidence that a passive second stage in the setting of mild to moderate infection is beneficial and usual indications for operative vaginal delivery may be employed. For the intubated and sedated patient who is in labor, a passive second stage may be considered. Standard antibiotics for group B streptococcal colonization or cesarean surgical site prophylaxis are still recommended.
For women hospitalized with COVID-19, corticosteroids for fetal benefit should be withheld after 34 weeks, even if delivery appears to be imminent, as there is evidence that systemic steroids are associated with poorer outcomes for people with COVID-19. 15 Prior to 34 weeks, decision to give corticosteroids should be made on a case-by-case basis. Pregnant women with COVID-19 pneumonia should be managed with supportive care. Both chest X-ray and CT of the chest are considered safe in pregnancy with fetal shielding if deemed clinically necessary, and should not be withheld for fetal concerns. 40 Vital sign norm parameters vary in pregnancy compared with the nonpregnant state. Thus when caring for pregnant patients with COVID-19, the threshold for care escalation may be different than that for nonpregnant patients. Oxygen saturation lower than 95% on room air, respiratory rate above 30, and pulse greater than 120 are appropriate triggers for evaluation and consideration of care escalation. 40 41 Additionally, it is critical to note that acid/base parameter is different for the pregnant patient. As the obstetric provider caring for an intubated pregnant patient, it is important to ensure that the critical care team is aware of these different parameters, which vary from the nonpregnant state as early as the first trimester ( Table 3 ). 42 Leftward tilt should also be considered when possible for intubated pregnant women to minimize vena caval compression by the gravid uterus. Fetal monitoring in critically ill patients should only occur as a noninvasive measure of maternal status or if delivery would not compromise maternal status. 38 It should be noted that fetal heart rate changes in this setting may be related to changes in maternal hemodynamics, respiratory status, and/or acid base status, and correction of these often results in improvement in fetal status without the need for delivery. 40 For pregnant women who are critically ill and/or immobile, prophylactic anticoagulation can also be considered. In the setting of maternal critical illness, need for ECMO, or decompensation, decisions about delivery are complex and require discussion with a multidisciplinary team.
After delivery, consideration of mother/infant separation, to minimize risk of transmission to the neonate is recommended by the CDC. 43 The neonate can be cared for by a family member, wearing appropriate PPE. In cases where separation is declined or there are capacity constraints, a physical barrier should be placed in the room, and the bassinet should be more than 6 feet from the mother. 43 The mother should also don a face mask and wash her hands prior to breastfeeding. In cases where separation is selected, pumping and receipt of bottled maternal breast milk is the recommended feeding method in these cases. Pump parts should all be washed with soap and water, and the pump itself disinfected according to manufacturer instructions. When possible, patients with COVID-19 or PUI should have their own designated breast pump during admission.
Inpatient care teams, including nursing, obstetric providers and anesthesia may consider running “COVID-19 simulation” to practice donning and doffing, as well as provider movements, in urgent scenarios, as these may vary from the usual workflow to ensure appropriate PPE use.
COVID-19 represents the largest pandemic of the century. The highly contagious nature and more severe infection phenotypes than other similar respiratory infections, along with rapid rate of spread have left many health systems overwhelmed with critically ill patients and understaffed due to quarantined and infected health care workers. Though, based on limited data, COVID-19 does not appear to be associated with worse outcomes in pregnant women than in the general population, many challenges still exist for the obstetric care provider. With social distancing as the best protective mechanism, prenatal care spacing and increased telehealth prenatal visits, are recommended to keep patients and providers safe. Infected, but otherwise low-risk pregnant women with mild disease do not need clinical assessment, and may be tested based on local practices. This population can likely have a telehealth visit or defer prenatal care for at least 2 weeks until no longer infectious. COVID-19 infection, even when severe, is not necessarily an indication for delivery. If delivery is indicated for other reasons, operative delivery should be reserved for usual obstetric indications. Though there is no clear evidence of vertical transmission, for neonates born to infected women or PUI, mother/baby separation should be considered to avoid transmission through respiratory droplets. Pumped or expressed breastmilk can be given to the neonate via bottle. Though this pandemic is changing the way we provide prenatal care, following practices of social distancing and proper PPE use, should allow provision of safe care for women and their fetuses.
Conflict of Interest None declared.

Prenatal Visit Guidelines
Clinic A/P, adults , OB/GYN
The USPSTF strongly recommends screening for hepatitis B virus infection in pregnant women at their first prenatal visit.
Sources: – NIH.Gov, What tests might I need during pregnancy? – NIH.Gov, What happens during prenatal visits?
First and Second Trimester Screening
Prenatal Visit Schedule
Healthy pregnancies will go by the following schedule.
What will happen at each visit? At every visit, we will:
- Check weight and assess weight gain.
- Urinalysis (UA) – urine culture is done at the first visit, after that, a UA is done at every subsequent visit.
- Fundal Height
- FHT (Fetal heart tones) – Starting at 11-12 weeks.
- Edema – Check hands and feet for swelling.
- Education – Answer questions or address concerns. Have patients write questions down and bring.
- Pelvic/cervix exam: 1st visit and any other visits if the patient is having contractions, bleeding, discharge, leaking, or at term.
Palpate to determine the fetal position after 36 weeks but not before due to inaccuracies and discomfort. Follow the above table to do tests, such as blood tests or an ultrasound exam.
*Antenatal testing (NST / AFI) – Bi-weekly -Start at 36 weeks if:
- Advanced Maternal Age
- HTN / Pre-Eclampsia
Naegele’s rule Used to calculate EDD (Estimated Date of Delivery) or EDC (Estimated Date of Confinement) from the 1st day of the LMP. EDD = Add 7 to the date of the 1st day of LMP and count back 3 months. I.e. EDD =( 7 + 1st day of LMP) – 3 months. Of course, when you get your answer, the due date will be in the next calendar year. I.e. add 1 year to the answer above.
Pregnancy wheels may have a five-day error. A lot of docs now use electronic devices to calculate EDC Use U/S dating if LMP unsure, unreliable, or abnormal. Some studies have suggested exclusive use of U/S date if it was done before 22 weeks gestation.
Fetal Development Fetal heart sound is first heard at 11-12 weeks by pocket Doppler and 16-19 weeks by Delee fetal stethoscope. Fundal height: Palpable at the pubic symphysis at 12 weeks, midway between symphysis and umbilicus at 16 weeks, umbilicus at 20 weeks.

Image from rphcm.allette.com.au
GnP(TPAL) e.g. G6P3124. Gn: Total number of pregnancies T: Total number of term deliveries (≥37 weeks) P: Total number of preterm deliveries (20-37 weeks) A: Total number of abortions or miscarriages (<20 weeks) L: Total number of living children.
Resources: Thomas Zeng, MD, Obstetrics & Gynecology, Comprehensive Handbook, 2nd Edition. Pages First-Trimester or Second-Trimester Screening, or Both, for Down’s Syndrome print
- Well Child Check
- Well Adult Exam
- DERMATOLOGY
- Forms & Charts
- History Templates
- PE Templates
- Quick Physical Exam
- A good Assessment & Plan
- DIFFERENTIAL DIAGNOSIS
- Clinic Quick Reference
- Hospital Quick Reference
- InfoGraphics
- Book Chapter in Time of Care
- Coding Guide
- Office Management
- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games
What to expect at your first prenatal appointment
Your kickoff prenatal visit sets the stage for the rest of your pregnancy. Here's what to expect at this information-packed first appointment and how you can prepare.

When to schedule your first prenatal visit
When will your first appointment be, what happens at the first prenatal visit, how to prepare for your first prenatal appointment, what questions to ask at the first prenatal visit.
As soon as you get a positive result on a home pregnancy test , book an appointment with an obstetrician, family physician, or midwife . Depending on the practice, it's normal for another provider in the office, like a nurse practitioner or physician assistant, to handle your first visit.
If you haven't yet chosen a healthcare provider for your pregnancy, that's okay. It's still important to see someone now to start your prenatal care. You can always switch to another provider later.
Many healthcare providers will schedule your first visit for when you're about 8 weeks pregnant . Some will see you sooner, particularly if you have an existing health condition, had problems with a pregnancy in the past, or are having new or severe symptoms such as vaginal bleeding or abdominal pain .
If you're taking any medications or think you may have been exposed to a hazardous substance, let your provider know as soon as possible.
The first visit will probably be the longest of your prenatal appointments (unless you have complications with your pregnancy along the way). At this and all future visits, don't be afraid to raise any questions or concerns you've been wondering about – it helps to keep a running list between appointments.
Here's what your provider will likely do during your first prenatal visit.
Take your health history. Your provider will ask questions about your gynecological health, personal medical history, and lifestyle habits. Topics commonly covered include:
- Whether your menstrual cycles are regular and how long they tend to last
- The first day of your last period (to determine your due date )
- Symptoms or problems you've noticed since your last period, whether they're related to pregnancy or not
- Current or past gynecological conditions, including sexually transmitted infections
- Details about previous pregnancies
- Current or past diseases and conditions
- Past surgeries or hospitalizations
- Mental health difficulties and diagnoses
- Whether you are being or have been abused , or have another situation that could affect your safety or emotional well-being
- Smoking, drinking, and drug use
- Medications, supplements, vitamins, and herbal drugs you take
- Drug allergies
Your healthcare provider will also ask about your family medical history. Many genetic issues and birth defects are at least partly hereditary, so learning about your family history helps your medical team keep an eye out for potential issues. Let your provider know whether a relative in your or your partner's family has a chromosomal or genetic disorder, had developmental delays, or was born with a structural birth defect.
It's also important to mention any potential exposure to toxins, especially if you live or work near toxic materials.
Check you out and run some tests. You can expect a number of standard exams and tests at your first prenatal visit. Some healthcare providers will do an ultrasound , but if you don't have any medical problems or concerns, it may not be part of the routine. Here's what's typical:
- A thorough physical exam
- A pelvic exam, including a Pap smear (unless you've had one recently) to check for infections such as chlamydia and gonorrhea or abnormal cells that could indicate cervical cancer
- A urine sample to test for urinary tract infections and other conditions
Your provider will also order blood tests to:
- Identify your blood type and Rh status
- Look for anemia
- Check for HIV, syphilis, hepatitis B and, in certain cases, hepatitis C
- Determine immunity to rubella (German measles) and chickenpox
Discuss any high-risk pregnancy concerns. Many people are considered to have high-risk pregnancies , meaning there's a higher-than-average chance of health issues during pregnancy, labor, and birth. High-risk groups include those who:
- Become pregnant for the first time at age 35 or older
- Become pregnant for the first time before age 18
- Have certain medical issues that develop during pregnancy, such as preeclampsia and gestational diabetes
- Have certain preexisting health problems, such as high blood pressure , thyroid disease , or type 1 or type 2 diabetes
High-risk pregnancies need extra care. While many potential complications are treatable or temporary, some can be dangerous to both you and your baby. Your provider will talk through the risks at your first visit and throughout your pregnancy – and don't be afraid to ask questions at any point.
Explain your options for prenatal genetic testing. Your provider will offer you various prenatal screenings that can give you information about your baby's risk for birth defects and chromosomal conditions. These tests include:
- Noninvasive prenatal testing (NIPT) , also called cell-free fetal DNA testing. Performed at 9 weeks or later, it's used to examine the little bits of your baby's DNA present in your blood.
- A first trimester screen, also called a first-trimester combined test. Typically done between weeks 11 and 13, it consists of a blood test and a type of ultrasound called a nuchal translucency .
- A carrier screening if you haven't had one already. It's a simple blood or saliva test done to see whether your baby is at risk for any of 100 genetic disorders such as cystic fibrosis, sickle cell disease, thalassemia, and Tay-Sachs disease.
Finally, if you're high-risk, there are invasive genetic diagnostic tests that can tell you for sure whether your baby has Down syndrome or certain other conditions. These tests include chorionic villus sampling (CVS) , generally performed at 10 to 13 weeks, and amniocentesis , usually done at 16 to 20 weeks.
CVS and amniocentesis are invasive and may carry a small risk of miscarriage , so women who choose to have these procedures are usually those with a higher risk for genetic and chromosomal problems. Some moms-to-be choose to wait for the results of screening tests before deciding whether to have one of these diagnostic tests.
For more information, your provider can refer you to a genetic counselor .
Give you advice and let you know what's ahead. Your healthcare provider will give you information about eating well , foods to avoid , healthy weight gain , and prenatal vitamins . They'll also give you a heads-up about the common discomforts of early pregnancy and let you know which pregnancy symptoms require immediate attention .
Your emotional health is very important. Your provider may screen you for signs of depression during pregnancy . But don't wait to be asked. If you're feeling depressed or anxious, let your provider know so they can refer you to someone who can help.
The dangers of smoking , drinking alcohol, using drugs, and taking certain medications will be a topic of discussion, as well. If you need help quitting smoking or any other substance, your provider can recommend a program or counselor.
Other topics include the do's and don'ts of exercise , travel , and sex during pregnancy ; environmental and occupational hazards that can affect your baby; and how to avoid certain infections, such as toxoplasmosis . Your provider will also discuss recommended vaccinations , like the flu shot and the COVID-19 vaccine .
To help your visit go as smoothly as possible, try taking the following steps.
Review your medical history. Brush up on your health status so you can better answer questions. This includes information about your:
- Overall physical and mental health
- Current and past diseases, conditions and other health issues
- Current medications, including prescriptions, supplements, vitamins and herbal supplements and teas
- Fertility and pregnancy history
- Family medical history
- Partner's medical history
If possible, bring documentation along, such as immunization records or a list of your medications. You may even want to bring a baggie containing the medications themselves.
Take your partner, a family member, or friend. Another person can write down notes, ask questions, and provide emotional support during this information-dense first visit.
Get there on time or a little early. This can be helpful for filling out forms and reviewing your insurance. Make sure to bring your insurance information and cash or a credit card for any necessary co-pays.
Just as your provider will ask you questions at your first prenatal visit, it's a good idea to come prepared with a list of questions for your provider. Ask anything – and don't be shy. Again, try to keep a running list in the weeks before the appointment, so nothing important slips your mind.
Here are some questions to consider if your provider doesn't bring up the topic first.
- How much weight gain is healthy for me? The first prenatal visit is a great opportunity to learn about how your body will change. It's also a good time to ask about nutrition, including which foods to prioritize in your diet.
- What are the foods I should avoid ? Raw fish and unpasteurized cheeses are long-established no-no's for pregnant people, but ask your provider for a full list of what to skip, since the accepted wisdom has changed over the years. Ask about caffeine and alcohol, too. Coffee is typically alright in limited doses, but no amount of alcohol is considered safe when you're having a baby.
- Are prenatal supplements a good choice? Your provider will likely recommend a prenatal vitamin containing folic acid and iron, both of which are needed more during pregnancy.
- Can I exercise? What about sex? With some exceptions, both are usually okay when you're pregnant. They're important to discuss, however, since certain conditions may complicate matters.
- Is it safe to keep working? If you have a physically or emotionally demanding job , you may want to ask how you can ease the effects on your body and mind.
- Is travel okay? While planes, trains, and automobiles are typically safe well into pregnancy, people with particular complications may need to limit or avoid traveling.
- Which medications are safe to take? Ask about your current prescriptions, herbal products, teas, supplements, and any over-the-counter drugs you may use, such as pain relievers and cold medicines. Non-steroidal inflammatory drugs (NSAIDs) like ibuprofen and naproxen are not recommended, for example.
- What are common symptoms of pregnancy? Your provider can tell you what to expect and how to cope. Remember to ask what symptoms are uncommon, too, and what red flags to watch for.
- What should I do in an emergency? Find out who to contact and where to go if you begin to experience new, unusual, severe, or long-lasting symptoms.
- Who will treat me over the course of my pregnancy? If your provider is part of a group practice, you may see other members of the group during appointments. They may even deliver your baby.
- Do you recommend taking prenatal classes? Whether they're in a hospital, at a university, online, or somewhere else, prenatal classes can be invaluable learning experiences for parents-to-be. On top of the usual childbirth classes you hear about, you can also find courses in everything from stress management to good nutrition and even breastfeeding.
Last but not least, ask about your next visit and schedule the appointment before leaving the office. Until your 28th week of pregnancy, you'll likely see someone every four weeks or so.
You may also want to ask whether future visits will be in-person or virtual. Certain practices offer virtual visits for low-risk patients, those whose providers aren't close by, or even higher-risk patients that need to be evaluated more often.
Was this article helpful?
Prenatal visits: What to expect and how to prepare

NIPT (Noninvasive prenatal testing)

What is the NT scan (nuchal translucency test)?

I'm pregnant: What do I do now?

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
March of Dimes. 2017. Prenatal Care Checkups. https://www.marchofdimes.org/pregnancy/prenatal-care-checkups.aspx Opens a new window [Accessed March 2024]
MedlinePlus. 2022. Prenatal care in your first trimester. https://medlineplus.gov/ency/patientinstructions/000544.htm Opens a new window [Accessed March 2024]
Mayo Clinic. 2022. Prenatal care: 1 st trimester visits. https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/prenatal-care/art-20044882 Opens a new window [Accessed March 2024]
American Pregnancy Association. (2021). Your First Prenatal Visit. https://americanpregnancy.org/healthy-pregnancy/planning/first-prenatal-visit/ Opens a new window [Accessed March 2024]
Kids Health. 2022. Prenatal Visits: First Trimester. https://kidshealth.org/en/parents/tests-first-trimester.html Opens a new window [Accessed March 2024]
Mount Sinai. 2021. Prenatal care in your first trimester. https://www.mountsinai.org/health-library/selfcare-instructions/prenatal-care-in-your-first-trimester Opens a new window [Accessed January 2024]
Centers for Disease Control and Prevention. 2022. Recommended Clinician Timeline for Screening for Syphilis, HIV, HBV, HCV, Chlamydia, and Gonorrhea. https://www.cdc.gov/nchhstp/pregnancy/screening/clinician-timeline.html Opens a new window [Accessed March 2024]
Alabama Perinatal Excellence Collaborative. 2015. APEC Guidelines for Routine Prenatal Care. http://apecguidelines.org/wp-content/uploads/2016/07/Routine-Prenatal-Care-6-30-2015.pdf Opens a new window [Accessed March 2024]
Kids Health. 2019. Toxoplasmosis. https://kidshealth.org/en/parents/toxoplasmosis.html Opens a new window [Accessed March 2024]
NIH: Eunice Kennedy Shriver National Institute of Child Health and Human Development. 2017. What is a high-risk pregnancy? https://www.nichd.nih.gov/health/topics/pregnancy/conditioninfo/high-risk Opens a new window [Accessed March 2024]
Kids Health. 2022. What's a “High-Risk” Pregnancy? https://kidshealth.org/en/parents/high-risk.html Opens a new window [Accessed March 2024]
NIH: Eunice Kennedy Shriver National Institute of Child Health and Human Development. 2018. What are some factors that make a pregnancy high risk? https://www.nichd.nih.gov/health/topics/high-risk/conditioninfo/factors Opens a new window [Accessed March 2024]
March of Dimes. 2020. Prenatal Tests. https://www.marchofdimes.org/pregnancy/prenatal-tests.aspx Opens a new window [Accessed March 2024]
American College of Obstetricians and Gynecologists. 2022. Carrier Screening. https://www.acog.org/womens-health/faqs/carrier-screening Opens a new window [Accessed March 2024]
March of Dimes. 2020. Chorionic Villus Sampling. https://www.marchofdimes.org/pregnancy/chorionic-villus-sampling.aspx Opens a new window [Accessed March 2024]
Office on Women's Health. 2021. Prenatal care and tests. https://www.womenshealth.gov/pregnancy/youre-pregnant-now-what/prenatal-care-and-tests Opens a new window [Accessed March 2024]
MedlinePlus. 2021. What is noninvasive prenatal testing (NIPT) and what disorders can it screen for? https://medlineplus.gov/genetics/understanding/testing/nipt/ Opens a new window [Accessed March 2024]
Voyage Healthcare. 2021. Prenatal Care Overview. https://www.voyagehealthcare.com/how-to-make-the-most-of-your-first-prenatal-visit-guide Opens a new window [Accessed March 2024]
Gifford Health Care. Undated. Preparing for Your Appointment. https://giffordhealthcare.org/patients/preparing-for-your-appointment/ Opens a new window [Accessed March 2024]
Mayo Clinic. 2023. Pregnancy nutrition: Foods to avoid during pregnancy. https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/pregnancy-nutrition/art-20043844 Opens a new window [Accessed March 2024]
American College of Obstetricians and Gynecologists. 2023. Nutrition During Pregnancy. https://www.acog.org/womens-health/faqs/nutrition-during-pregnancy Opens a new window [Accessed March 2024]
Mayo Clinic. 2022. Prenatal vitamins: Why they matter, how to choose. https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/prenatal-vitamins/art-20046945 Opens a new window [Accessed March 2024]
American College of Obstetricians and Gynecologists. 2022. Exercise During Pregnancy. https://www.acog.org/womens-health/faqs/exercise-during-pregnancy Opens a new window [Accessed March 2024]
Mayo Clinic. 2022. Sex during pregnancy: What's OK, what's not. https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/sex-during-pregnancy/art-20045318 Opens a new window [Accessed March 2024]
Kids Health. 2022. Sex During Pregnancy. https://kidshealth.org/en/parents/sex-pregnancy.html Opens a new window [Accessed March 2024]
American College of Obstetricians and Gynecologists. 2023. Travel During Pregnancy. https://www.acog.org/womens-health/faqs/travel-during-pregnancy Opens a new window [Accessed March 2024]
March of Dimes. 2020. Over-the-counter medicine, supplements and herbal products during pregnancy. https://www.marchofdimes.org/pregnancy/over-the-counter-medicine-supplements-and-herbal-products.aspx Opens a new window [Accessed March 2024]

Where to go next

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

Driving in the U.S. if you are not a citizen
Depending on the U.S. states you will visit, you may need an International Driving Permit (IDP) as well as a driver's license your country.
Learn about IDPs and how to get one before you visit the U.S.
An IDP is a form of identification that many countries around the world recognize. It allows you to drive legally in a different country.
- Not every U.S. state requires an IDP. Contact the state department of motor vehicles for each state you plan to drive in to see if they require an IDP.
- You must get an IDP before your trip. The U.S. does not issue IDPs to foreign visitors.
- To get an IDP, contact the motor vehicle department of the country that issued your driver's license. The fees and amount of time it will take to receive your IDP will depend on the issuing country.
- You may need both your license and an IDP to rent a car in the U.S. Check the rental company's policies and other requirements in advance.
Driver's licenses if you are living in the U.S. as a permanent resident
If you are a citizen of another country and are living permanently in the U.S., you may be eligible to apply for a driver's license from the state where you live.
- The residency requirement for obtaining a U.S. driver's license is different in each state.
- Contact your state department of motor vehicles to check the ID requirements and find out how to apply for a license.
- A state driver's license allows you to drive anywhere in the U.S.
LAST UPDATED: May 23, 2024
Have a question?
Ask a real person any government-related question for free. They will get you the answer or let you know where to find it.

IMAGES
VIDEO
COMMENTS
Every visit: Doptones, fundal height, vitals Four question: Vaginal bleeding, contractions, leaking fluid, fetal movement By Weeks: 20wks - get and review anatomy US 24wks - order glucola, cbc (check for anemia), discuss normal growing pains 28wks - Tdap and Rhogam if needed, discuss kick counts 32wks - Discuss BCM, sign tubal papers if ...
At every visit, your blood pressure, weight and urine will be tested. The doc will also check the fetal heartbeat,and around week 20 start measuring your belly's growth and checking baby's position. As your due date approaches, she'll also start checking your cervix's effacement (the amount it has shortened) and dilation (the amount it ...
What happens at second trimester prenatal appointments. In the second trimester, you'll have prenatal appointments with your doctor every four weeks. Your doctor will recommend a variety of health and genetic screenings, as well as routine ultrasounds, according to the prenatal appointment schedule. During this time, it's important to ask any ...
The goal of prenatal care is the birth of a healthy child with minimal risk for the mother. After the initial prenatal visit, it consists of ongoing evaluation of the health status of both the mother and fetus, counseling about pre- and postpartum issues, and anticipation of problems with intervention, if possible, to prevent or minimize ...
2 Guidelines for Perinatal Care. Structural, financial, and cultural barriers to care need to be identified and eliminated. The regionalized organization and integration of perinatal care must evolve within the framework of the general health care delivery system while avoiding unnecessary duplication of services.
Prenatal care: 1st trimester visits. Pregnancy and prenatal care go hand in hand. During the first trimester, prenatal care includes blood tests, a physical exam, conversations about lifestyle and more. By Mayo Clinic Staff. Prenatal care is an important part of a healthy pregnancy. Whether you choose a family physician, obstetrician, midwife ...
During the second trimester, prenatal care includes routine lab tests and measurements of your baby's growth. You might consider prenatal testing, too. By Mayo Clinic Staff. The goal of prenatal care is to ensure that you and your baby remain healthy during your entire pregnancy. Ideally, prenatal care starts as soon as you think you're pregnant.
Six weeks after delivery we will see you for a postpartum checkup. At each visit, we will check your blood pressure and weight. You will also be asked to provide a urine sample at your first visit and each visit beginning with the 20th week of pregnancy. You can expect your provider to check fetal heart tones, measure your abdomen, and review ...
During the third trimester, prenatal care might include vaginal exams to check the baby's position. By Mayo Clinic Staff. Prenatal care is an important part of a healthy pregnancy, especially as your due date approaches. Your health care provider might ask you to schedule prenatal care appointments during your third trimester about every 2 or 4 ...
Your first prenatal visit will probably be scheduled sometime after your eighth week of pregnancy. Most health care providers won't schedule a visit any earlier unless you have a medical condition, have had problems with a pregnancy in the past, or have symptoms such as spotting or bleeding, stomach pain, or severe nausea and vomiting. 1 You've probably heard pregnancy discussed in terms of ...
For people with uncomplicated pregnancies, prenatal appointments generally happen every four weeks until approximately week 36 of pregnancy. The next visit is usually around week 38, and then once per week until birth. However, every pregnancy is different, and different health care providers stick to different schedules.
Prenatal care and tests. Medical checkups and screening tests help keep you and your baby healthy during pregnancy. This is called prenatal care. It also involves education and counseling about how to handle different aspects of your pregnancy. During your visits, your doctor may discuss many issues, such as healthy eating and physical activity ...
The initial routine prenatal visit should occur between 6 and 8 weeks gestation. Follow-up visits should occur at . About 4-week intervals until 28 weeks. 2-week intervals from 28 to 36 weeks. Weekly thereafter until delivery. Prenatal visits may be scheduled more frequently if risk of a poor pregnancy outcome is high or less frequently if risk ...
Typical prenatal appointment schedule. The number of visits you'll have in a typical pregnancy usually total about 10 to 15, depending on when you find out you're expecting and the timing of your first checkup. In most complication-free pregnancies, you can expect to have a prenatal appointment with the following frequency: Weeks 4 to 28 ...
Postpartum checkups give ob-gyns and moms the chance to address problems early. Here's what you can expect during a checkup, plus some context about the process. Checkups can give you and your ob-gyn a full picture of your physical, mental, and emotional health. Your ob-gyn should do a physical exam, including a pelvic exam, to make sure you ...
Telehealth visit-return OB visit: Schedule 4 wk from prior visit: 36: Return OB provider visit: GBS screen: ≥37 until delivery: 7-10 day return OB provider visits d: Postpartum: Telehealth-1 week mood check b: Open in a separate window. Abbreviations: GBS, Group B Strep; OB, obstetric; TDAP, Tetanus, Diphtheria and Pertussis.
FHT (Fetal heart tones) - Starting at 11-12 weeks. Edema - Check hands and feet for swelling. Education - Answer questions or address concerns. Have patients write questions down and bring. Pelvic/cervix exam: 1st visit and any other visits if the patient is having contractions, bleeding, discharge, leaking, or at term.
First Obstetric Visit at 8 weeks gestation. Routine Obstetric Visit (typically 10-12 visits per pregnancy) Prenatal Visit every 4 weeks to 28 weeks gestation. Prenatal Visit every 2 weeks to 36 weeks gestation. Prenatal Visit every 1 week until delivery. Consider replacing some in-person Routine Obstetric Visits with Telemedicine visits.
Prenatal care visits should occur with the following frequency: Prior to 20 weeks, ideally every 4 weeks but no less than every 6 weeks for lower-risk women. 20 to 28 weeks, every 4 weeks. 28 to 36 weeks, every 2-3 weeks, 3 weeks for lower-risk women. 36 weeks to delivery, at least every week. Urine dipstick for protein, glucose, and ketones ...
When to schedule your first prenatal visit. As soon as you get a positive result on a home pregnancy test, book an appointment with an obstetrician, family physician, or midwife.Depending on the practice, it's normal for another provider in the office, like a nurse practitioner or physician assistant, to handle your first visit.
The patient develops a third-degree vaginal laceration during the delivery that is repaired by the OB/GYN. In total, the patient's OB/GYN performs 14 antepartum visits, the delivery, and all postpartum care. To correctly report this scenario, the physician will report 59400-22 for the global maternity care.
A type 1 excludes note is a pure excludes. It means "not coded here". A type 1 excludes note indicates that the code excluded should never be used at the same time as Z34.A type 1 excludes note is for used for when two conditions cannot occur together, such as a congenital form versus an acquired form of the same condition.
Prenatal Visit Week 38. Your baby could be born any day now! In fact, 85% of babies are born in the two weeks before their due date. At this stage, you are probably feeling pretty uncomfortable ...
Driver's licenses if you are living in the U.S. as a permanent resident. If you are a citizen of another country and are living permanently in the U.S., you may be eligible to apply for a driver's license from the state where you live. The residency requirement for obtaining a U.S. driver's license is different in each state.