Advertisement

2021 E/M coding and documentation rules
Billing, Coding & Payments | Advocacy Resources | January 15, 2021
New rules for reporting outpatient office evaluation and management (E/M) services took effect Jan. 1. The coding and documentation revisions, adopted by the American Medical Association’s CPT Editorial Panel and approved by the Centers for Medicare and Medicaid Services (CMS) substantially simplify code selection and documentation.
With the exception of 99201, which was deleted, the E/M outpatient visit code numbers remain as follows:
- 99202-99205: New Patient Office Visits
- 99211-99215: Established Patient Office Visits

Code selection – Medical Decision Making (MDM) or Time
- Medical decision making (MDM)
Although you should still perform a medically appropriate history and/or physical exam, it/they do not determine the level of service.
Coding based on MDM
The four levels of MDM remain the same: straightforward, low, medium, and high. The three core elements have remained essentially the same and they are:
Number and complexity of problem(s)
- A problem is the disease, condition, illness, symptom, or other matter addressed at the encounter with or without a diagnosis being established.
- Multiple new or established conditions may be addressed at the same encounter and may affect medical decision making.
- Each symptom is not necessarily a problem. Symptoms may cluster around a specific diagnosis or conditions.
- The final diagnosis for a condition does not, in itself, determine the complexity or risk.
- Multiple problems of lower severity may, in the aggregate, create a higher risk due to interaction.
Amount and/or complexity of data to be reviewed and analyzed. Data includes:
- Tests, documents, orders, or independent historians
- Independent interpretation of tests
- Discussion of management or test interpretation with external physician or health care professional.
Risk of complications and/or morbidity or mortality of patient management decisions made at visit:
- Includes possible management decisions selected and those not selected.
- An example of moderate risk might include prescription drug management or a diagnosis or treatment significantly limited by social determinants of health.
- An example of high risk might include drug therapy requiring intensive monitoring for toxicity.
To qualify for a level of MDM, two of the three elements for that level of decision making must be met. The College’s matrix on MDM provides more detail on how to determine the level of MDM and code selection.
Documentation Tip:
When coding based on MDM, physician notes should address the elements on which the MDM determination is based. Note that while you should document any history and/or physical exam performed, this is no longer a basis for code selection. There is no need to review a certain number of systems, or check boxes.
Coding based on time
The biggest change in E/M coding and documentation is that code selection for outpatient office visits can now be based entirely on time spent on the day of the encounter even if counselling and coordination of care do not dominate the encounter. Clinical staff time does not count. Time includes:
- All time spent by the physician or qualified health professional (QHP) for the patient on the date of the encounter including:
♦ Preparing to see the patient (e.g., review of tests).
♦ Obtaining and/or reviewing separately obtained history.
♦ Performing a medically appropriate examination and/or evaluation.
♦ Counseling and educating patient/family/caregiver.
♦ Ordering medications, tests, or procedures.
♦ Referring and communicating with other health care professionals (if not separately reported).
♦ Documenting clinical information in the patient’s health record.
♦ Independently interpreting results (not separately reported) and communicating to patient/family/caregiver.
♦ Care coordination (not separately reported).
- Time is defined in increments.
- If time exceeds level 5, the add-on prolonged service code can be used.
Time for determining visit level
Note: For CPT Code 99211, which describes visits that do not require the presence of a physician, time is not used.
Documentation tips:
- Complete charting and follow-up on the day of the encounter. Only time spent on the day of the encounter can be counted.
- On the day of the visit, keep track of and document time spent on getting ready for the patient encounter and follow-up work afterwards, such as care coordination.
- Only provider time counts – not nurse or medical assistant time. But provider time spent reviewing nurse, medical assistant or scribe documentation does count.
Coding tips:
- To determine whether to code based on MDM or time, compare visit level based on time with level based on MDM and use the highest level that can be documented using either method.
- You may find new and/or complex patient visits are best coded based on time, especially patients that require a fair amount of counseling, care coordination, chart reviews and/or reviewing test results.
- Many follow-up visits may be best coded based on medical decision making, since they may still involve medical complexity and risk but may not require a great deal of time.
When to Use the Prolonged Service Codes
There are some important changes in coding for prolonged services. First, the prolonged service code may only be used when coding based on time and only with the level 5 visit codes (99205, 99215). Second, the new codes describe shorter time increments of 15 minutes.
CPT Code 99417 should be used when billing payers other than Medicare. This code, which should only be billed with 99205 or 99215, describes an additional 15 minutes beyond the minimum time of the office visit code. It can be billed in multiple units for each additional 15 minutes of time. Additional time less than 15 minutes should not be reported.
HCPCS Code G2212 was created by CMS and is specific to Medicare . It should be reported for each additional 15 minutes of prolonged service beyond the maximum time for CPT Codes 99205 or 99215. See tables below:
Additional resources:
Webinar: New Outpatient E/M Coding Rules for 2021
ACAAI Coding Toolkit
College Matrix on MDM
The College’s Advocacy Council will continue to provide information on the new codes and coding for 2021 – we have you covered.

Senate Finance Committee releases white paper on Medicare payment reform
While the paper does not make specific policy recommendations, it explains the policy issues the committee has identified and…

Advocacy Council fights against electronic payment fees
Congress is beginning to pay attention to another source of payment reductions caused by some commercial payers: electronic payment…

Senate Finance Committee holds hearing on Medicare payment reform for chronic care
While there were some comments in favor of increasing payments to physicians, most of the discussion centered on value-based…
Privacy Overview
- ACS Foundation
- Diversity, Equity, and Inclusion
- ACS Archives
- Careers at ACS
- Federal Legislation
- State Legislation
- Regulatory Issues
- Get Involved
- SurgeonsPAC
- About ACS Quality Programs
- Accreditation & Verification Programs
- Data & Registries
- Standards & Staging
- Membership & Community
- Practice Management
- Professional Growth
- News & Publications
- Information for Patients and Family
- Preparing for Your Surgery
- Recovering from Your Surgery
- Jobs for Surgeons
- Become a Member
- Media Center
Our top priority is providing value to members. Your Member Services team is here to ensure you maximize your ACS member benefits, participate in College activities, and engage with your ACS colleagues. It's all here.
- Membership Benefits
- Find a Surgeon
- Find a Hospital or Facility
- Quality Programs
- Education Programs
- Member Benefits
- E/M Coding and Billing Res...
- Office/Outpatient E/M Visi...
Office/Outpatient E/M Codes
2021 e/m office/outpatient visit cpt codes.
The tables below highlight the changes to the office/outpatient E/M code descriptors effective in 2021.
More details about these office/outpatient E/M changes can be found at CPT® Evaluation and Management (E/M) Office or Other Outpatient (99202-99215) and Prolonged Services (99354, 99355, 99356, 99XXX) Code and Guideline Changes.
All specific references to CPT codes and descriptions are © 2023 American Medical Association. All rights reserved. CPT and CodeManager are registered trademarks of the American Medical Association.
Download the Office E/M Coding Changes Guide (PDF)

Reporting Level 5 E/M Code 99205
by Meghann Drella | Last updated on Apr 3, 2024 | Published on Jun 27, 2014 | Medical Coding

Documentation Requirements for CPT Code 99205
What is high risk diagnosis, common mistakes to avoid in billing cpt code 99205.
CPT code 99205 is a high-level evaluation and management code used for the evaluation and management of new patients, for both office and outpatient visits. CPT code 99205 can be selected for new patient visits lasting 60+ minutes on the date of encounter. The total time required for reporting 99205 is 60-74 minutes. Reporting CPT code 99205 accurately is often difficult for coders. This is where a professional medical coding company can support.

Free up your team for what matters most. Get a quote for our medical coding services !
Call (800) 670-2809
Code99205 requires 3 key components:
- High-level medical decision-making: The evaluation and management of a patient demand intricate decision-making processes. This involves properly analyzing and interpreting medical records, diagnostic tests, and relevant information to formulate an accurate diagnosis and treatment plan.
- Thorough medical history or examination: Proper assessment of a patient’s condition necessitates a comprehensive history or examination. This involves gathering details about the patient’s medical background, current symptoms, past treatments, and any other crucial factors influencing their healthcare.
- Session duration typically ranging from 60-74 minutes: CPT code 99205 denotes an extended duration of service compared to other evaluation and management codes. The session duration encompasses both face-to-face and non-face-to-face time dedicated to the patient encounter.
While the new patient codes (99201–99205) require that all three key components (history, exam and medical decision making) be satisfied, the established patient codes (99211–99215) require that only two components of the three key be satisfied.
The terms “high complexity/high severity” signifies that the patient’s risk of death/morbidity is high – extreme and/or the patient has a moderate – high risk of death without treatment or a high probability of severe, prolonged, functional impairment. So to justify the use of 99205, the patient’s condition, whether acute or chronic must pose an immediate threat to life or physical function.
High risk diagnosis may be:
- Sudden change to neurological status such as weakness/sensory loss, TIA (Transient Ischemic Attack), seizure
- Chronic illnesses with severe progression, worsening or side effects of treatment
- Acute/chronic injury or illnesses that pose a threat to physical function or life itself such as acute MI, multiple trauma, pulmonary embolus
Avoiding common mistakes are crucial when billing CPT Code 99205. Ensure accurate reimbursement and compliance with professional coding guidelines.
Here are some common mistakes to avoid:
- Insufficient documentation: One of the most common mistakes is not providing enough documentation to support the level of service billed. Ensure that the documentation includes a detailed history of present illness, comprehensive review of systems, comprehensive examination of multiple organ systems, and medical decision making of high complexity.
- Overbilling: Billing for a level of service higher than warranted by the patient encounter can lead to overbilling and potential audits. Make sure the documentation accurately reflects the complexity of the patient’s condition and the level of service provided.
- Under coding: Conversely, under coding occurs when providers bill for a lower level of service than warranted by the patient encounter. Ensure that the documentation accurately reflects the complexity of the patient’s condition to avoid under coding and potential loss of revenue.
- Lack of medical necessity: Ensure that the documentation clearly demonstrates the medical necessity of the services provided. Medical necessity is essential for justifying the level of service billed and ensuring reimbursement.
- Failure to document time spent: CPT code 99205 requires encounter time. So, keep track of the time you spend with the patient. Failure to document the total time spent with the patient and the specific amount of time spent on counseling or coordination of care can lead to billing errors and potential denials.
- Mixing-up patient status: This code is specifically designated for new patients, so it’s crucial to differentiate it from established patient codes to ensure accurate billing and documentation. Familiarizing the distinct criteria for each code can streamline the process and prevent any potential errors in reimbursement.
By avoiding these common mistakes and ensuring accurate documentation, healthcare providers can bill CPT Code 99205 appropriately, leading to accurate reimbursement and compliance with coding guidelines. Modifiers used for 99205 depend on specific billing circumstances. For example, modifier “-25” is of use, if a significant and separately identifiable service is provided on the same day. Billing 99205 with other codes depends on the services provided and payer rules. Proper use of modifiers and adherence to billing guidelines are essential when billing for multiple services.
Maximize your reimbursement and minimize errors with our customized coding services.
Get a Free Trial!

Meghann Drella possesses a profound understanding of ICD-10-CM and CPT requirements and procedures, actively participating in continuing education to stay abreast of any industry changes.
More from This Author
Facebook Twitter LinkedIn
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Submit Comment
Related Posts
- Step Up Accounts Receivable Management and Boost Your Bottom Line
- Proven Strategies to Boost Revenue in Healthcare & Maximize Profits
- Medical-Dental Cross Coding: What Dental Practices Should Know
- Appointment Scheduling
- Dental Insurance Verification
- Healthcare News
- Insurance Credentialing
- Insurance Verification and Authorizations
- Medical Billing
- Medical Coding
- Medical Outsourcing

- For Ophthalmologists
- For Practice Management
- For Clinical Teams
- For Public & Patients
Museum of the Eye
- Latest Issue
- Back Issues (Nov. 2012 to present)
- Archive Highlights (pre Oct. 2012)
- Dr. Richard Mills' Opinions, 2002 to 2016
- Write For Us
- Corporate Webinars
- EyeNet Magazine
- / June 2021
- / E/M Rules for Office Visits: What Level of Medical Decision-Making?
E/M Rules for Office Visits: What Level of Medical Decision-Making?
- Mark Complete
Download PDF
Under the E/M rules that went into effect on Jan. 1, 2021, the complexity of medical decision-making (MDM) is used to determine what level of E/M code you can use for an office visit. Make sure that your documentation validates the MDM level that you bill.
Four levels of medical decision-making. The overall complexity level of MDM can be straightforward or of low, moderate, or high complexity. To determine this overall level of MDM, you first look at three components (see next paragraphs) and determine which level of MDM complexity each of them would support (see “ E/M Resources ”). If at least two components indicate the same level of MDM, then that would determine the overall level of MDM. If the three components point to three different levels of MDM, then the middle one would determine the overall level of MDM.
Component 1: The number and/or complexity of problems addressed at the patient encounter.
Component 2: The amount and/or complexity of data to be reviewed and analyzed.
Component 3: The risk of complications and/or morbidity or mortality of patient management.
Which E/M codes can you bill for the office visit? The E/M codes that you can use depend on the complexity level of MDM:
- Straightforward: Use codes 99202 or 99212 for new and established patients, respectively.
- Low complexity: 99203 or 99213.
- Moderate complexity: 99204 or 99214.
- High complexity: 99205 or 99215.
Tackle These Three Cases
Based on the documentation for each of the exams below, determine which E/M codes to bill.
Case A: An infant with dacryostenosis. A pediatrician referred a patient to a pediatric ophthalmologist.
Impression. Intermittent, bilateral, congenital nasolacrimal duct obstruction of a 9-month-old.
Plan. Lacrimal massage, twice a day. Antibiotic drops three times a day for three days to improve mucopurulent discharge. Discussed possible need for surgery, but not yet since there are some “clear” days with no symptoms.
Case B: A toddler’s swollen eyelid. A 3-year-old presented with a red, swollen left upper lid (LUL), with increasing severity over the previous two days. He had an associated upper respiratory infection.
Impression: Preseptal cellulitis LUL.
Plan: Considered ordering computed tomography or magnetic resonance imaging of the orbit, but deferred that order since able to see full ocular motility. Discussion with pediatrician about Rocephin (ceftriaxone sodium) injection. Prescribed oral antibiotics for 10 days. Instructed patient’s mother to call if increased fever or swelling over the subsequent 24 hours.
Case C: A patient with shingles. A patient had shingles on the right side of her face and, ultimately, in her right eye. She had severe pain and photophobia in the right eye.
Impression: Zoster in the right eye.
Plan: Prescription drug management with acyclovir and topical steroids. Follow-up in one week or sooner. Phone conversation about findings and treatment with primary care physician.
Which E/M code would you bill for each of these exams? See answers below .
All content on the Academy’s website is protected by copyright law and the Terms of Service . This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
- About the Academy
- Jobs at the Academy
- Financial Relationships with Industry
- Medical Disclaimer
- Privacy Policy
- Terms of Service
- Statement on Artificial Intelligence
- For Advertisers
- Ophthalmology Job Center
FOLLOW THE ACADEMY
Medical Professionals
Public & Patients
- Current Issue
- Meeting Recaps
- Rare Diseases
April 2022 | Coding Advisor

When to Use an Evaluation and Management or Eye Visit Code
These strategies can help you determine which code to use..

Joy Woodke, COE, OCS, OCSR
When coding office visits, retina specialists have two types of codes to choose from: the evaluation and management (E/M) codes or the eye visit family of codes. With the significant changes to E/M documentation guidelines and value in 2021, now is a good time to rethink some of your coding patterns for various scenarios. Below are some helpful tips to help you decide how to properly code patient visits.
RETINA CASE STUDIES
1. A new patient is seen for a comprehensive eye examination. The diagnosis is an epiretinal membrane in the right eye, stable. The plan is to continue to monitor the patient and schedule a follow-up in 3 months.
Coding options: E/M overall MDM, low, or CPT code 99203 ($114), or eye visit code 92004 ($152).
2. An established patient has a problem-focused examination for nonproliferative diabetic retinopathy with vitreous hemorrhage in the left eye. The plan is to schedule a vitrectomy for the next available appointment.
Coding options: E/M overall MDM, low, or CPT code 99214 ($130), or eye visit code 92012 ($91).
MASTER THE CRITERIA
Continue to review the new E/M guidelines that went into effect January 1, 2021, including the E/M Coding & Documentation Guidelines for 2021. 1 The bottom line is that your documentation should include:
- A medically relevant history and examination, and
- A code selection based on medical decision making (MDM) or total physician time.
Eye visit code criteria, however, did not change. The CPT code guidelines continue to focus on:
- History, general medical observation, and chief complaint;
- Required examination elements per intermediate and comprehensive levels; 2 and
- Initiation or continuation of diagnostic and treatment programs.
SCENARIOS THAT RULE OUT EYE VISIT CODES
There are nine scenarios in which submitting an E/M code would be advantageous.
1. When the ICD-10-CM code is not a covered diagnosis.
Example: A hydroxychloroquine sulfate (Plaquenil, Concordia Pharmaceuticals) examination with no maculopathy is reported with ICD-10-CM diagnosis code Z79.899, other long-term (current) drug therapy, and M06.9 (rheumatoid arthritis). Many payers will deny claims when a system disease (eg, M06.9) is linked to an eye visit code.
2. When the place of service is not the office.
Example: When the patient is seen in the emergency department, be sure to use the E/M family of codes 99281-99285, emergency department visit.
Note: For a place of service that is somewhere other than your office or outpatient services, continue to follow the 1997 guidelines. The visit must meet history, examination, and MDM requirements.
3. When the frequency of patient visits is exceeded.
Example: Some commercial and other payers may have frequency edits for eye visit codes and only allow reimbursement annually, per patient.
4. When E/M is required for medical diagnoses per payer policy.
Example: Some commercial and other payers may require that clinicians report vision diagnoses with eye visit codes and report other medical diagnoses with E/M codes.
5. When the patient visit is subject to downcoding based on diagnosis per payer policy.
Example: Some commercial and other payers may downcode comprehensive codes to an intermediate code based only on the ICD-10-CM code(s) reported.
6. When the commercial or Medicaid plan still recognizes consult codes.
Example: Some payers may continue to recognize E/M consultation codes (CPT 99241-99245). Consultation codes should be reported by the retina specialist when a consult is requested for a problem. These codes should not be reported if a transfer of care has been accepted before the initial evaluation.
Note: Medicare does not recognize consultation codes.
7. When there is a telemedicine visit.
Example: The pandemic waiver that allowed the use of eye visit codes for telemedicine visits is no longer valid. Report E/M codes based on MDM, or total physician time.
8. When there is a prolonged patient visit.
Example: When the physician total time during one patient visit exceeds the total for level 5 and prolonged services can be billed, E/M would be preferred over eye visit codes.
9. When there is an increased payer allowable.
Example: When the payer allowable for the level of E/M code is higher than the eye visit code. For example, if a new patient comprehensive eye examination was performed with a moderate level of MDM, report the level 4 E/M 99204 instead of the comprehensive eye visit code 92004 based on the Medicare fee schedules.
2022 FEE SCHEDULE COMPARISON
Each year when the fee schedules are published, clinicians can compare the E/M and eye visit codes for various scenarios. The table outlines the average 2022 Medicare fee schedule, not adjusted for geographic practice cost index.
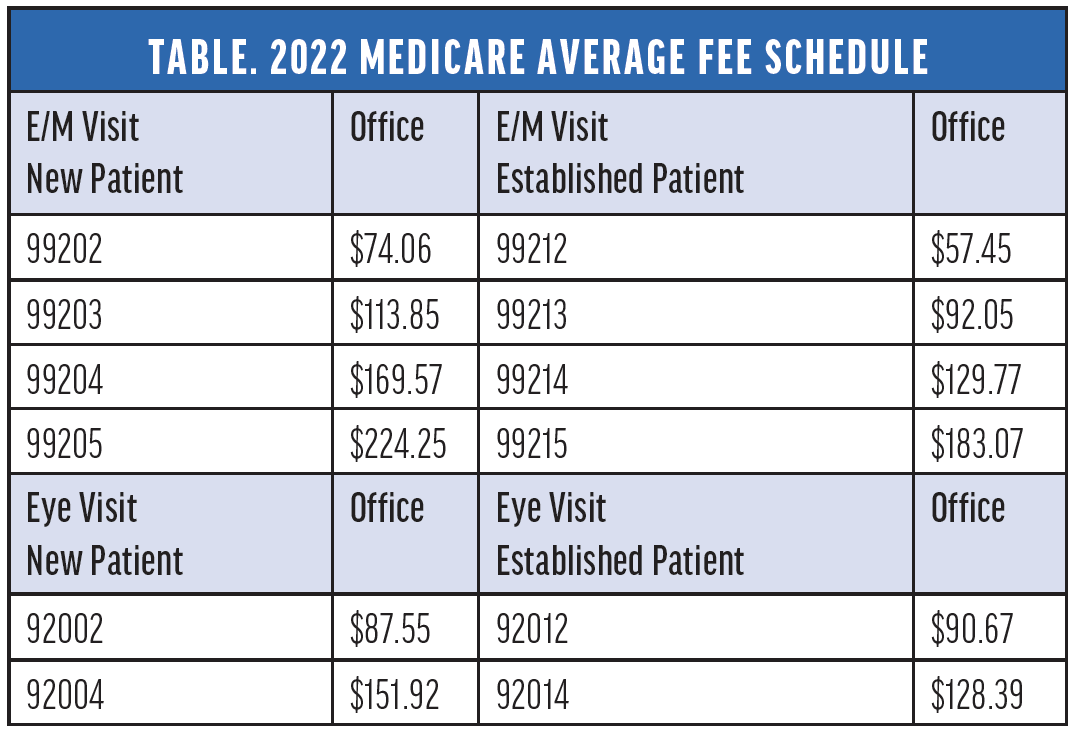
Click to view larger
Using the table, it is imperative that retina practices create a quick reference guide for the Medicare fee schedule for the region. In addition, a display of the top insurance payers should be available for analysis.
NUANCED BY PAYER
Fee schedules and policies vary per insurance payer. Staying up to date and creating internal guides will assist clinicians in determining the appropriate level of E/M versus eye visit code. Additional resources can be found at aao.org/em and aao.org/coding .
1. Woodke J. E/M coding and documentation guidelines for 2021. Retina Today Business Matters . 2020;3(4):6-7,11.
2. Eye Visit Code Checklist. American Academy of Ophthalmology. Accessed March 2, 2022. www.aao.org/Assets/f924affe-c407-4044-9794-a39787c139d1/637564307201030000/eye-visit-code-cl-nov2020-pdf
Director Coding & Reimbursement, American Academy of Ophthalmology, San Francisco [email protected] Financial disclosure: None
Related Articles
Five tools to build wealth for a successful retirement.
David Mandell, JD, MBA; and Jason O’Dell, MS, CWM
Independent Research Centers: A Viable Career Option
Luke C. Heckmann, BS; Brian B. Berger, MD; and Ivana Gunderson, BS
Cultivate Your Best Practice Culture
John A. Hovanesian, MD
Within This Issue
Fluorescein angiography in the era of octa.
Andrea Servillo, MD; Riccardo Sacconi, MD; and Giuseppe Querques, MD, PhD
Top 10 Lessons from The PIVOT Trial
Rajeev H. Muni, MD, MSc, FRCSC
An Overview of Biomarkers in Retinal Disease
Simrat Kaur Sodhi, MSc; Aidan Pucchio, BSc; and Netan Choudhry, MD, FRCSC
This Month's Supplements

AMD & DME Consensus Discussions: Key Clinical Opinions on Diagnosis and Modern Case Management Decisions
Independent Medical Education Supported by Roche & Zeiss

Bloody Bowtie
Sponsored by Nidek
Recent Supplements

From Complex Surgeries to Routine Cases. Advancing vitreoretinal surgery with the Alcon suite of technologies and innovations.
Sponsored by Alcon
View Supplement

How Do You Engage With Your Referral Network?
Editorially Independent Content, Supported With Advertising From Astellas
View Insert

One to Watch: Danny A. Mammo, MD
Editorially independent supported by Abbvie and Regenxbio

One to Watch: Ashley M. Crane, MD

Rising Stars in Retina: Asad F. Durrani, MD

Beyond the Scope: Exploring the Augmented Reality Revolution in Ophthalmology
Sponsored by Beyeonics Vision
Eyetube Retina Series
EYETUBE RETINA MEETING COVERAGE

Getting clear on the new coding rules can help you eliminate bloated documentation and improve reimbursement to reflect the value of your visits.
THOMAS WEIDA, MD, FAAFP, AND JANE WEIDA, MD, FAAFP
Fam Pract Manag. 2022;29(1):26-31
Author disclosures: no relevant financial relationships.

In 2021, significant changes were adopted for the documentation guidelines for outpatient evaluation and management (E/M) visit codes. Most notably, medical decision making or time became primary drivers of visit level selection, rather than the number of history and physical exam bullets.
In this article, we review the context for these changes, describe them briefly, and offer a quick reference tool to help physicians apply the new rules in practice.
The revisions to the E/M outpatient visit codes reduced administrative burden by eliminating bullet points for the history and physical exam elements.
Code level selection is now simplified — based on either medical decision making or total time.
The authors' one-page coding reference tool can help simplify the new rules.
HOW WE GOT HERE
In the 2019 Medicare physician fee schedule final rule, released in November 2018, the Centers for Medicare & Medicaid Services (CMS) adopted revisions to the outpatient E/M codes in order to reduce administrative burden. (See https://www.cms.gov/newsroom/fact-sheets/final-policy-payment-and-quality-provisions-changes-medicare-physician-fee-schedule-calendar-year .) Originally scheduled for implementation in 2021, these changes would have combined visit levels 2–4 into a blended payment rate (e.g., one rate for 99202-99204 and one rate for 99212-99214), among other changes.
In response, the American Medical Association (AMA) convened a joint CPT Editorial Board and Relative Value Scale Update Committee (RUC) workgroup to build on the changes and propose some alternatives. The workgroup's goals were to decrease administrative burden, payer audits, and unnecessary medical record documentation while ensuring that payment of E/M services is resource-based.
The workgroup approved significant revisions to the outpatient office visit E/M codes. Code 99201 was deleted. The history and/or physical examination and the counting of bullets were eliminated as components for code selection (although history and/or physical examination documentation should still be performed as medically appropriate). Medical decision making (MDM) or time could be used for code level selection. Changes were made to the code descriptors for 99202-99205 and 99211-99215, the definition of medical decision making, and the calculation of time, and a shorter prolonged services add-on code was created. CMS adopted these new E/M coding guidelines. As a result of the changes to medical decision making and time-based coding, the RUC revised the 2021 relative value units (RVUs) for office visit E/M codes. Most of the values increased, yielding an overall increase of more than 10%.
CODING BASED ON MEDICAL DECISION MAKING
For outpatient E/M coding, medical decision making now has three components:
Number and complexity of problems addressed at the encounter,
Amount and/or complexity of data to be reviewed and analyzed,
Risk of complications and/or morbidity or mortality of patient management.
There are four levels of decision making for each of these components: straightforward, low complexity, moderate complexity, and high complexity.
To determine the level of code for a visit, two of the three components must meet or exceed that level of coding. ( See the table .) For example, if the patient has multiple problems addressed at the encounter, but the data is limited and the risk of complications is low, then the level of medical decision making would be low. New patient codes 99202-99205 and established patient codes 99212-99215 use the same components and levels of decision making for code selection.
Determining medical decision making usually starts with identifying the number and complexity of problems addressed and then determining the data or risk components that support that medical decision making. If a second component does not meet or exceed the problem component, then a lower level of decision making is appropriate. The set of tables below illustrate the essential concepts of these code levels. Each level has specific criteria for each component.
Straightforward medical decision making: Codes 99202 and 99212 include one self-limited or minor problem with minimal or no data and minimal risk.
An example of a 99202 or 99212 is an otherwise healthy patient with cough and congestion due to the common cold.
Low complexity medical decision making: Codes 99203 and 99213 include two or more self-limited or minor problems, one stable chronic illness, or one acute uncomplicated illness or injury.
The data component requires one of two categories to establish the level. Category 1 data requires at least two items in any combination of the following: each unique source's prior external notes reviewed, each unique test result reviewed, or each unique test ordered. Tests include imaging, laboratory, psychometric, or physiologic data. A clinical lab panel, such as a complete blood count, is a single test. Of note, if a test is ordered, the review of that test is included with the ordering, even if the review is done at a subsequent visit. Tests ordered outside of an encounter may be counted in the encounter in which they are analyzed. Category 2 data includes significant history given by an independent historian. Parents giving the history for their child is a typical example.
The risk component is low. There is low risk of morbidity from additional diagnostic testing or treatment.
An example of a 99203 or 99213 is a sinus infection treated with an antibiotic. Although the prescription makes the risk component moderate, the one acute uncomplicated illness is a low-complexity problem, and there are no data points.
Moderate complexity medical decision making: Codes 99204 and 99214 include two or more stable chronic illnesses, one or more chronic illnesses with exacerbation, progression, or side effects of treatment, one undiagnosed new problem with uncertain prognosis, one acute illness with systemic symptoms, or one acute complicated injury. A patient who is not at a treatment goal, such as a patient with poorly controlled diabetes, is not stable. Systemic general symptoms such as fever or fatigue in a minor illness (e.g., a cold with fever) do not raise the complexity to moderate. More appropriate would be fever with pyelonephritis, pneumonitis, or colitis.
The data component requires one of three categories to establish the level. Category 1 data requires at least three items in any combination of the following: each unique source's prior external notes reviewed, each unique test result reviewed, each unique test ordered, or independent historian involvement. Physicians cannot count tests that they or someone of the same specialty and same group practice are interpreting and reporting separately (e.g., electrocardiogram, X-ray, or spirometry). Category 2 data includes the independent interpretation of a test performed by another physician/other qualified health care professional (QHP) (not separately reported). For instance, if a chest X-ray was ordered and the ordering clinician included the interpretation in the visit documentation, this would qualify for data point Category 2. However, if the ordering clinician bills separately for the interpretation of the X-ray, then that cannot be used as an element in this category and would be an element for Category 1. Category 3 data includes discussion of management or test interpretation with an external physician/QHP (not separately reported).
The risk component may include prescription drug management, a decision for minor surgery with patient or procedure risk factors, a decision for elective major surgery without patient or procedure risk factors, or social determinants of health (SDOH) that significantly limit diagnostic or treatment options, such as food or housing insecurity. For prescription drug management, renewing pre-existing chronic medications would qualify. Documentation that the physician is managing the patient for the condition for which the medications are being prescribed would help establish validity in the use of this criterion for MDM.
An example of a 99204 or 99214 is a patient being seen for follow-up of hypertension and diabetes, which are well-controlled. An example using SDOH would be a patient with chronic knee pain and a positive anterior drawer test who needs imaging of the knee but cannot afford this care. Documenting that the patient cannot afford to obtain an MRI of the knee at this time, which significantly limits your ability to confirm the diagnosis and recommend treatment, adds to the risk component.
High complexity medical decision making: Codes 99205 and 99215 include one or more chronic illnesses with a severe exacerbation, progression, or side effects of treatment, or one acute or chronic illness or injury that poses a threat to life or bodily function.
The data component requires two of three categories to establish the level. These data categories are the same as those for 99204 and 99214, and they follow the same rules.
The risk component may include drug therapy requiring intensive monitoring for toxicity. Decisions regarding elective major surgery with patient or procedure risk, emergency major surgery, hospitalization, or “do not resuscitate” orders are also high risk. Intensive prescription drug monitoring is typically supported by a laboratory test, physiologic test, or imaging, and is done to evaluate for complications of the treatment. It may be short-term or long-term. Long-term monitoring is at least quarterly. An example would be monitoring for cytopenia during antineoplastic therapy. Monitoring the therapeutic effect of a treatment, such as glucose monitoring during insulin therapy, is not considered intensive prescription drug monitoring.
An example of a 99205 or 99215 is a patient with severe exacerbation of chronic heart failure who is admitted to the hospital.
CODING OUTPATIENT E/M VISITS
Time-based coding.
An alternative method to determine the appropriate visit level is time-based coding. A major change is that total time now includes both face-to-face and non-face-to-face services personally performed by the physician/QHP on the day of the visit. Additionally, time-based coding is no longer restricted to counseling services. Instead, it includes the following:
Preparing to see the patient (e.g., reviewing external test results),
Obtaining and/or reviewing separately obtained history,
Performing a medically appropriate examination and/or evaluation,
Counseling and educating the patient, family, or caregiver,
Ordering medications, tests, or procedures,
Referring and communicating with other health care professionals (when not separately reported),
Documenting clinical information in the electronic or other health record,
Independently interpreting results (not separately reported with a CPT code) and communicating results to the patient, family, or caregiver.
Care coordination (not separately reported with a CPT code).
Time spent by clinical staff cannot count toward total time. However, time spent by another physician/QHP (not a resident physician) in the same group can be included. If a nurse practitioner performs the initial intake and the physician provides the assessment and plan, both of those times can be counted, although only one person's time can be counted while they are discussing the case with each other. The visit should be billed under the clinician who provided the substantive portion (more than half) of the time, although both clinicians need to be identified in the medical record. Time spent must be documented in the note. It is advisable to specifically document the time spent and the activities performed both face-to-face and non-face-to-face.
The amount of total time required for each level of coding changed under the new time-based coding guidelines. (See the “Total time ” table.)
PROLONGED VISIT CODES
When time on the date of service extends beyond the times for codes 99205 or 99215, prolonged visit codes can be used. The AMA CPT committee developed code 99417 for prolonged visits, and Medicare developed code G2212. These are added in 15-minute increments in addition to codes 99205 or 99215. Code G2212 can be added once the maximum time for 99205 or 99215 has been surpassed by a full 15 minutes, whereas code 99417 can be added once the minimum time for 99205 or 99215 has been surpassed by a full 15 minutes. Less than 15 minutes is not reportable. Multiple units can be reported. Prolonged visit codes cannot be used with the shorter E/M levels, i.e., 99202-99204 and 99212-99214. (See “Prolonged services ” tables.) Clinicians should consult with individual payers to determine which code to use — G2212 or 99417.
SIMPLIFIED CODING AND DOCUMENTATION
The revisions to the outpatient E/M visit codes reduced administrative burden by eliminating bullet points for the history and physical exam elements. Only medically appropriate documentation is required. Code level selection is simplified — based on either medical decision making or total time. By applying these changes, primary care clinicians can eliminate bloated documentation and improve reimbursement reflecting the value of the visit.
Continue Reading

More in FPM
More in pubmed.
Copyright © 2022 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

New clinical assessment tool improves dementia care actions in primary care patients
Resource tripled the odds of receiving dementia-related care within 90 days
WHAT: A five-minute cognitive assessment coupled with a decision tree embedded in electronic medical records, known as 5-Cog, improved dementia diagnosis and care, based on a clinical trial funded by the National Institutes of Health (NIH) and conducted in an urban primary care setting. Researchers evaluated the system among 1,200 predominantly Black and Hispanic American older adults who presented to primary care with cognitive concerns. The findings appear in Nature Medicine.
5-Cog combines three metrics designed to test memory recall, the connection between cognition and gait, and the ability to match symbols to pictures. Importantly, these tests are easy to perform, relatively quick, and are not affected by reading level or ethnic/cultural differences among patients.
Using 5-Cog, patients were rapidly assessed for cognitive impairment before seeing their physicians, who then determined follow-up care using a decision tree within the patients’ electronic medical records. Study participants were randomly assigned to receive either the 5-Cog assessment or to a control group that received standard care. Use of the 5-Cog system improved the odds three-fold that a patient would receive dementia-related care compared to standard care. Such dementia-related care included a new diagnosis of dementia or mild cognitive impairment, as well as further assessments, medications, or specialist referrals within 90 days. The findings provide evidence that changes to medical practice in primary care like the adoption of the 5-Cog system could reduce barriers and improve dementia follow-up care.
Cognitive impairment is often difficult to diagnose in the busy primary care setting and, as a result, beneficial care plans are likely underutilized. This can result in lack of detection, which delays the start of support services and critical planning. Underdiagnosis is even more prevalent among older Black and Hispanic patients compared to white patients, suggesting this tool may be especially valuable to the populations represented in the study.
The research was funded by NIH’s National Institute of Neurological Disorders and Stroke (UG3NS105565 and U01NS105565) in collaboration with NIH’s National Institute on Aging. The 5-Cog study is a participant in the Consortium for the Detection of Cognitive Impairment, Including Dementia ( www.detectcid.org ). ClinicalTrials.gov identifier: NCT03816644 .
WHO: Roderick Corriveau, Ph.D., program director, NINDS Division of Neuroscience
To arrange an interview, please contact [email protected] .
ARTICLE: Verghese J, et al. Non-literacy biased, culturally fair cognitive detection tool in primary care patients with cognitive concerns: a randomized controlled trial. Nature Medicine. 4 June 2024. DOI: 10.1038/s41591-024-03012-8 .
NINDS is the nation’s leading funder of research on the brain and nervous system. The mission of NINDS is to seek fundamental knowledge about the brain and nervous system and to use that knowledge to reduce the burden of neurological disease.
About the National Institute on Aging (NIA) : NIA leads the U.S. federal government effort to conduct and support research on aging and the health and well-being of older people. Learn more about age-related cognitive change and neurodegenerative diseases via NIA’s Alzheimer’s and related Dementias Education and Referral (ADEAR) Center website. Visit the main NIA website for information about a range of aging topics in English and Spanish and stay connected .
About the National Institutes of Health (NIH): NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit https://www.nih.gov .

IMAGES
VIDEO
COMMENTS
Follow these four steps to code quickly and accurately, while reducing the need to count up data points. ... Level 4 visit Level 5 visit; Step 1: Total time * 99212 < 20 min: 99213: 20-29 min ...
To follow up on the previous FPM article detailing these changes ... It can be used when the total time exceeds that of a level 5 visit - 99205 or 99215. (See ...
exceeds the minimal time for the highest-level E/M visit by 15 minutes. For example, a provider spends a total time of 83 ... select the code level and for example 5 time was used to select the code level. ... Follow-up as needed.
Internists selected the 99215 level of care for only about 4.86% of established office patients in 2020. The Medicare allowable reimbursement for this level of care is $183.19. Effective January 1, 2021, this level of care requires high complexity MDM or a total of 40 - 54 minutes spent before, during and after the visit on the date of the ...
Many follow-up visits may be best coded based on medical decision making, since they may still involve medical complexity and risk but may not require a great deal of time. ... First, the prolonged service code may only be used when coding based on time and only with the level 5 visit codes (99205, 99215). Second, the new codes describe shorter ...
CMS and CPT® have a difference of opinion on when the time of the level 5 visit is exceeded. According to CPT®, 99417 Prolonged office or other outpatient evaluation and management service(s) ... CPT® adds the 15 minutes to the lowest or highest time assigned to the level 5 code. For example, new patient E/M code 99205 is a total time of 60 ...
Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and low level of medical decision making. When using time for code selection, 30-44 minutes of total time is spent on the date of the encounter. 99204. Office or other outpatient visit for the ...
2021 E/M Guidelines: Time vs MDM. E/M level of service for office or other outpatient services can be based on: Medical decision making or. Total time for E/M services performed on the date of the encounter. NOTE: All payors must follow the 2021 E/M CPT guidelines.
CMS calls the system of 10 visits for new and established office visits "outdated" and proposes to retain the codes but simplify the payment by applying a single-payment rate for level 2 through 5 office visits.
The codes apply to services that a wide range of primary care and specialty providers perform regularly. Some of the most commonly reported E/M codes are 99201-99215, which represent office or other outpatient visits. In 2020, the E/M codes for office and outpatient visits include patient history, clinical examination, and medical decision ...
Some tips for coding using total time under the new rules for E/M office visits that take effect Jan. 1, plus an example of a visit well-suited for time-based coding.
What is High Risk Diagnosis? CPT code 99205 is a high-level evaluation and management code used for the evaluation and management of new patients, for both office and outpatient visits. CPT code 99205 can be selected for new patient visits lasting 60+ minutes on the date of encounter. The total time required for reporting 99205 is 60-74 minutes.
For example, 99202 Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and straightforward medical decision making … has a current time range of 15-29 minutes. Beginning Jan. 1, 2024, the provider must meet or exceed 15 minutes of total service time before you can bill this code by time.
Under the E/M rules that went into effect on Jan. 1, 2021, the complexity of medical decision-making (MDM) is used to determine what level of E/M code you can use for an office visit. Make sure that your documentation validates the MDM level that you bill. Four levels of medical decision-making.
Anything less is part of the level 5 time range. Telehealth (video visits) and telephone E/M vs virtual check-in ... levels 2-4 follow-up video and in-person visit codes (99212-99214). Telephone (audio-only) E/M is reimbursed less than office visit new patient codes (99202-
The 2021 E/M office visit coding changes allow physicians to code visits based solely on total time, which is defined as the entire time you spent caring for the patient on the date of the visit.
Example: When the physician total time during one patient visit exceeds the total for level 5 and prolonged services can be billed, E/M would be preferred over eye visit codes. 9. When there is an increased payer allowable. Example: When the payer allowable for the level of E/M code is higher than the eye visit code. For example, if a new ...
Effective Jan. 1, 2023, hospital observation codes 99217-99220 and 99224-99226 are deleted. These services are merged into the existing hospital inpatient services codes 99221-99223, 99231-99233, and 99238-99239, and the subsection is renamed Inpatient Hospital or Observation Care. As in the Office or Other Outpatient Services subsection, the ...
Same Group (Follow-Up Care) 5 Critical Care & Other Same-Day E/M Visits 5 Critical Care Services & Global Surgery 6 ... • Choice of medical decision making or time to select visit level, except for visits that aren't timed, like emergency department visits (page 17
An example of a 99204 or 99214 is a patient being seen for follow-up of hypertension and diabetes, which are well-controlled. ... An alternative method to determine the appropriate visit level is ...
The findings provide evidence that changes to medical practice in primary care like the adoption of the 5-Cog system could reduce barriers and improve dementia follow-up care. Cognitive impairment is often difficult to diagnose in the busy primary care setting and, as a result, beneficial care plans are likely underutilized.
Meet Charge 6—a premium fitness tracker with Google smarts that's designed to motivate you to reach your goals and help your workout routine run even smoother.
Top E/M Office Visit Chart Audit Findings. In my work with clients, I often identify potential coding issues around the frequency of evaluation and management (E/M) visits compared to a benchmark. For example, based on Medicare distribution data, Chart 1 illustrates possible over-coding (relative to 46 percent level 3 and 53 percent level 4 ...