Why Did My Emergency Room Visit Cost So Much?

Emergency room visits are notoriously expensive. Just a few hours in the ER can cost you thousands of dollars, with or without insurance.
But how is your ER visit cost calculated, and how can you tell whether your hospital bill is correct?
We scored some insider tips from Goodbill medical coding expert Christine Fries, who has analyzed thousands of ER hospital bills for accuracy. Here are answers to frequently asked questions we get from Goodbill customers about how to understand and vet ER visit costs.

Why did I get 2 bills for my ER visit?

Patients are usually surprised when their first ER hospital bill is quickly followed by a separate hospital bill with similar-sounding charges but different amounts. This is normal and a byproduct of how hospitals bill patients for the services rendered at the hospital, Fries says.
The institutional bill, also known as the facility bill, charges you for the procedures, tests, and administrative costs from the hospital.
The professional bill, also known as the physician bill, charges you for the work and time of the physician who treated you. This generally includes services from doctors, anesthesiologists, or specialists who are affiliated with the hospital but aren’t employed by the hospital.
Expect to get two bills from your ER visit — one for facility charges, and the other for professional or physician charges.
For more information on the different types of hospital bills, see our itemized bill guide . Goodbill currently helps patients negotiate institutional bills, not professional bills, so our guidance below pertains to institutional bills only.
My diagnosis turned out to be minor. Why was I charged so much?
It’s important to remember that your ER visit costs are based on the symptoms you first describe upon entering the hospital, not your eventual diagnosis, Fries says.
When a patient walks into the emergency room complaining of chest pains, for example, the hospital’s objective is to run tests and administer procedures that can help rule out life-threatening conditions. Even if the doctor ends up discharging the patient with a non life-threatening diagnosis like indigestion, the hospital has already spent the resources to rule out more severe possibilities like a heart attack.
Your ER visit costs are based on the symptoms you first describe upon entering the hospital, not your eventual diagnosis.
“Look at your symptoms first, not what you were diagnosed with,” Fries says. “The level of your ER visit is guided by the symptoms you described, and by the tests the hospital thought were needed based on those symptoms.”
Why was I charged for an ‘ER Visit Level’ 3, 4, or 5? Is this based on severity?
Hospitals will bill you for a line item called “ER Visit Level” that is based on the complexity of your treatment. ER visit levels range from 1-5: ER visit level 1 is the most mild, while ER visit level 5 is the most severe. The level also determines how much the hospital can charge you, from least expensive to most expensive. You may sometimes hear ER visit levels described by their corresponding Current Procedural Terminology (CPT) codes of 99281, 99282, 99283, 99284 and 99285.
To decide the proper ER visit level, hospitals typically follow certain guidelines from the American College of Emergency Physicians (ACEP) . ER level 1-2 visits are reserved for treatment of mild cases like bug bites and sunburns. The majority of ER visits fall between ER visit levels 3-5, with ER visit level 4 being the most common, Fries says.
“Most emergency room claims will qualify as a 99284, because you only need something as simple as IV fluids to get you there,” Fries says.
The majority of ER visits fall between ER visit levels 3-5, with ER visit level 4 being the most common.
Here’s a simple rule of thumb for determining whether your ER visit level was correctly assigned.
ER Visit Level 4
An ER visit level 4 typically requires a minimum of two diagnostic tests — like a lab plus an EKG, or a lab plus an X-ray. Or, any administration of fluids through IV will automatically qualify your visit as an ER visit level 4.
ER Visit Level 5
An ER visit level 5 typically requires a minimum of three diagnostic tests — for example, a lab plus EKG and X-ray. Or, any type of imaging scan like a CT scan or MRI where a patient must ingest or be injected with contrast material, will automatically qualify your visit as an ER visit level 5.

I’m not pregnant. Why did I get charged for a pregnancy test?
Many female patients get frustrated when they’re charged for a pregnancy test, even when they’re absolutely certain they’re not pregnant. But this is standard practice and a way for hospitals to protect against unknown pregnancies, Fries says.
If you’re an adult pre-menopausal female, you can count on being asked to do a urine or blood pregnancy test before the hospital will treat you. It’s too risky to both the patient and hospital to administer injections, scans or drugs in the off chance that a patient is unknowingly pregnant.
If you're a female, expect to get a pregnancy test during your ER visit — even if you're not pregnant.
On your itemized ER bill, your pregnancy test will usually show up with a description like “human chorionic gonadotropin (hCG),” which is the hormone being tested. This charge will generally fall under the CPT codes 84702 or 84703 if it’s a blood test, or 81025 if it’s a urine test.
What are some other common ER services I might see on my hospital bill?
Here are a few common procedure names that often show up in your ER visit costs, and what they mean in plain English:
Metabolic panel
This is a bundle of lab tests run from a single blood draw. Patients may get a “basic” metabolic panel under CPT code 80048, or a “comprehensive” metabolic panel under CPT code 80053. These panels cover a set of individual tests that might otherwise be individually charged. For example, a “comprehensive” metabolic panel must include testing for all of the following:
- Carbon dioxide
- Phosphatase, alkaline
- Transferase, alanine amino
- Transferase, aspartate amino
- Urea nitrogen
Venipuncture
Any time you get your blood drawn through a needle, this charge under CPT code 36415 is the line item that bills you for the needle.
This test under CPT code 83690 measures your levels of lipase, which is an enzyme that helps break down fat in your intestines. Your lipase levels may be elevated if you have pancreatitis, which is an inflammation of the pancreas gland.
What are some ER visit cost errors I should look out for?
When analyzing a patient’s ER visit costs for errors, Fries says she goes straight to one place first: Hydration services. If you recall being administered fluids through an IV bag, chances are you got hydration services during your ER visit.
“Hydration services should always be questioned,” Fries says.
Coding guidelines require that the two CPT codes for this service, 96360 and 96361, meet a minimum time requirement of 31 minutes in order for one unit to be billed. These 31 minutes must also be “stand alone” — meaning that the administration of the service cannot overlap with any other type of infusion service. Often, hospitals don’t meet these requirements, rendering the charge unbillable.
Hydration services are a common source of errors in ER hospital visit costs. You can tell if you're being overcharged by checking your medical record.
To verify whether you’re being charged properly, you’ll need your medical record, Fries says. Look for hydration service “start” and “stop” times, which are usually included in the Medication Administration Report (MAR) section of your record. If the hydration service duration is less than 31 minutes of standalone time, you have a strong case to dispute the charge with your hospital. To find out how to get your medical records online, visit our Medical Records guide .
I don’t see any CPT codes on my bill. How can I get them?
CPT codes are the common language used across all hospitals to describe a certain procedure. They’re what enables our medical coders at Goodbill to analyze hospital bills for errors, line item by line item. They also help us compare prices apples-to-apples across hospitals.
CPT codes are the standard language used to describe a certain procedure across all hospitals. They're key to helping you identify errors or inflated charges in your ER hospital bill.
Unfortunately, the hospital bill you get in the mail is most likely a consolidated summary of your ER visit costs and won’t include CPT codes. You’ll need an “itemized bill” from your hospital to get a line-by-line breakdown of each charge, complete with the CPT code and cost.
The good news is that you’re legally entitled under HIPAA to get access to this information. To learn more about your patient rights and how to obtain your itemized bill, check out our Patient Right of Access guide .
Are there other topics you’d like us to cover? Email us at [email protected] and let us know.
Guides, news, and articles to help you tackle hospital bills.

How to Negotiate Your Hospital Bill
Read our expert tips on how to negotiate your hospital bill to save up to thousands of dollars.

Itemized Bill: Your Key to Negotiating
Itemized bills provide key details that can help you negotiate your hospital bill.
.jpg)
Can Hospital Bills Affect My Credit?
You have time before your bill can go to collections or affect your credit.
Negotiating hospital bills has never been this easy.
Building trust and confidence into every health care transaction.

© 2022 Goodbill, Inc.

Welcome to our informative guide on the 99283 CPT code for emergency department visits. In this article, we will provide you with a detailed understanding of this code and its significance in healthcare billing and reimbursement. Whether you are a healthcare professional or simply seeking information about ER coding, we’ve got you covered.
When patients visit the emergency department, their medical services are categorized and reported using specific codes. One such code, the 99283 CPT code, is assigned to ER visits that require an expanded problem focused history, an expanded problem focused examination, and medical decision making of moderate complexity. This code is commonly associated with level 3 ER visits, which involve patients with moderate severity presenting problems.
Key Takeaways:
- The 99283 CPT code is used for reporting emergency department visits.
- This code corresponds to level 3 visits, which involve moderate severity presenting problems.
- The code requires an expanded problem focused history, examination, and moderate complexity in medical decision making.
- Accurate coding and documentation are crucial for proper reimbursement.
- Medical Bill Gurus can assist healthcare providers with medical billing services and navigating the reimbursement process for the 99283 code.
Now that we’ve provided you with an overview, let’s dive deeper into the components of the 99283 CPT code and understand its relevance in emergency department visits.
What is a CPT Code?
CPT codes, or Current Procedural Terminology codes, are a set of medical codes used to describe medical procedures and services provided by healthcare professionals. These codes play a crucial role in healthcare billing and reimbursement. They provide a standardized way to communicate the specific procedures and services rendered, allowing for accurate documentation and proper categorization for billing purposes.
One commonly used CPT code in the field of evaluation and management is the 99283 code. This code is specifically assigned to emergency department visits and falls under the category of evaluation and management codes. It is used to report emergency visits that require an expanded problem-focused history, an expanded problem-focused examination, and medical decision making of moderate complexity.
Healthcare providers rely on CPT codes to accurately bill for their services and receive appropriate reimbursement from insurance companies or government programs such as Medicare. These codes serve as a universal language in the healthcare industry, bridging the gap between healthcare providers and payers.
Benefits and Importance of CPT Codes
The utilization of CPT codes offers several benefits:
- Standardization: CPT codes provide a standardized method for documenting and reporting medical procedures and services across various healthcare settings. This uniformity enhances communication and reduces ambiguity.
- Precision in Billing: CPT codes ensure precise billing by accurately representing the complexity and nature of the medical services provided. This helps healthcare providers receive fair and appropriate reimbursement.
- Comparative Analysis: CPT codes allow for comparisons between different procedures and services. These comparisons assist in analyzing healthcare trends, assessing outcomes, and determining the cost-effectiveness of certain treatments.
- Reimbursement: Accurate coding using CPT codes is essential for healthcare providers to receive timely reimbursement for the services they render. Proper documentation and assignment of CPT codes significantly reduce the risk of claim denials.
In summary, CPT codes are a critical component of healthcare billing and reimbursement. They enable accurate representation and communication of medical services, ensure fair reimbursement for healthcare providers, and facilitate efficient analysis of healthcare data. The 99283 code specifically captures the evaluation and management aspects of emergency department visits, providing a well-defined categorization for billing purposes.
Components of the 99283 CPT Code
The 99283 CPT code encompasses three essential components that must be fulfilled for accurate reporting. These components consist of an expanded problem focused history, an expanded problem focused examination, and medical decision making of moderate complexity. Proper documentation should highlight the presence of these components to ensure precise coding and billing.
New Patient Visit – Level 3
When using the 99283 CPT code, the expanded problem focused history involves obtaining a detailed account of the patient’s current condition, symptoms, and medical history. This includes relevant information about the presenting problem, any known allergies or medications, and the patient’s past medical, surgical, and family history.
The expanded problem focused examination requires a systematic assessment of the patient’s affected body areas and organ systems related to the presenting problem. Medical practitioners evaluate the patient’s vital signs, perform targeted physical examinations, and document any observed abnormalities or findings related to the chief complaint.
Medical decision making of moderate complexity involves the evaluation and analysis of the patient’s medical condition, diagnostic test results, and treatment options. The practitioner assesses the information collected during the history and examination to derive a diagnosis, determine the appropriate management plan, and ensure patient safety.
By accurately documenting and fulfilling these three components, healthcare providers can ensure proper coding and billing for emergency department visits that meet the criteria for the 99283 CPT code.
Emergency Department Visits and Coding Guidelines
When it comes to coding emergency department visits, following specific coding guidelines is crucial. According to the Current Procedural Terminology (CPT) definition, an emergency department is a hospital-based facility that provides unscheduled episodic services to patients who require immediate medical attention.
To accurately code an ER visit, it is essential to document the level of history, examination, and medical decision making. This documentation ensures the assignment of the appropriate CPT code, reflecting the complexity of the visit. Proper documentation is essential for accurate coding and compliant billing.
Let’s take a closer look at the key aspects of coding guidelines for emergency department visits.
Documentation Requirements
When coding an emergency department visit, thorough documentation is essential to accurately reflect the level of service provided. The documentation should include:
- A detailed history of the patient’s chief complaint and presenting problems
- A comprehensive examination, including vital signs, physical findings, and any diagnostic tests performed
- Medical decision making that demonstrates the complexity of the patient’s condition and the management involved
By documenting these elements, healthcare providers ensure compliance with coding guidelines and enable accurate coding and billing of emergency department visits.
Coding Guidelines for Emergency Department Visits
When coding an emergency department visit, the key considerations include:
- Selecting the appropriate CPT code based on the complexity of the visit
- Following the CPT guidelines to ensure accurate code assignment
- Adhering to any specific payer requirements or modifiers, if applicable
It is important to note that CPT codes for emergency department visits are categorized based on the level of complexity, such as problem-focused, expanded problem-focused, or detailed examination. Choosing the correct code is crucial for proper reimbursement and compliance with coding guidelines.
Understanding the coding guidelines for emergency department visits is paramount to ensure accurate coding and compliant billing. By carefully documenting the necessary information and selecting the appropriate CPT code, healthcare providers can submit claims that reflect the complexity of the services provided during an emergency department visit.
Reimbursement Process for 99283 CPT Code
Reimbursement for the 99283 CPT code is a critical aspect of the healthcare billing process. The amount of reimbursement received for an emergency department visit depends on various factors, including the payer’s policies and the documentation supporting the level of service provided. Accurate coding and thorough documentation are essential to ensure proper reimbursement for healthcare providers.
At Medical Bill Gurus, we understand the complexities of the reimbursement process and can assist healthcare providers in navigating through the intricacies. Our team of experienced professionals is well-versed in the coding guidelines and documentation requirements for the 99283 CPT code. We can help providers optimize their revenue by ensuring accurate coding and comprehensive documentation.
When it comes to reimbursement, every detail matters. The documentation supporting the level of service provided must align with the assigned CPT code, specifically the expanded problem focused history, expanded problem focused examination, and medical decision making of moderate complexity. By accurately coding and documenting the visit, healthcare providers can maximize their reimbursement and avoid potential claim denials.
Medical Bill Gurus works closely with healthcare providers, offering comprehensive medical billing services tailored to their specific needs. We have extensive experience in navigating the reimbursement process, ensuring that our clients receive the appropriate reimbursement for the services they provide. With our expertise, you can focus on delivering quality patient care while we handle the complex billing and reimbursement processes.
Trust Medical Bill Gurus to be your partner in optimizing revenue and streamlining the reimbursement process. Contact us today to learn more about our medical billing services and how we can assist you in navigating the reimbursement process for the 99283 CPT code.
Medical Bill Gurus – Your Medical Billing Company
At Medical Bill Gurus, we understand the complexities of medical billing and the importance of accurate coding for healthcare providers. Led by President Daniel Lynch, our team specializes in providing comprehensive medical billing services tailored to the unique needs of each provider.
With our expertise in working with all insurance payers, including Medicare, we can help you optimize your revenue through accurate coding and billing practices. Our dedicated team is committed to ensuring your financial success by staying up-to-date with the latest coding guidelines and reimbursement processes.
When you partner with Medical Bill Gurus, you can expect:
- Accurate and timely submission of claims
- Thorough documentation and coding reviews to maximize reimbursement
- Personalized support and guidance throughout the billing process
- Transparent reporting to track your revenue and identify areas for improvement
- Compliance with HIPAA rules and regulations to protect patient confidentiality
Our goal is to streamline your billing operations, reduce administrative burden, and help you focus on providing quality patient care. Trust Medical Bill Gurus to be your dedicated partner in medical billing.
The Importance of Accurate Coding
Accurate coding is crucial for healthcare providers as it directly impacts the reimbursement they receive for their services. Proper coding ensures that the services provided are reflected accurately in billing claims, which in turn affects reimbursement rates. Accurate documentation is essential to support the assigned codes and prevent denial of claims.
Why Accurate Coding Matters
Accurate coding plays a significant role in healthcare billing and reimbursement. When the wrong code is assigned or documented inaccurately, it can result in payment delays, denials, or even potential legal issues. Healthcare providers rely on accurate coding to receive fair compensation for their services and maintain financial stability.
Accurate coding also helps healthcare providers in the following ways:
- Transparent and Consistent Billing: Accurate coding ensures that the services provided are transparently communicated through billing claims. It allows payers, such as insurance companies, to understand the nature and complexity of the services rendered.
- Avoidance of Overbilling or Underbilling: Accurate coding prevents overbilling, which can result in audits, financial penalties, and damaged professional reputation. Conversely, underbilling can lead to revenue loss and unsustainable financial practices.
- Compliance with Regulatory Standards: Proper coding ensures compliance with regulatory standards, such as the Healthcare Common Procedure Coding System (HCPCS) and the International Classification of Diseases (ICD). Adhering to these standards helps healthcare providers avoid legal and compliance issues.
The Role of Documentation
Accurate documentation is a crucial component of accurate coding. It provides evidence to support the assigned codes and justifies the level of service provided. Comprehensive and detailed documentation helps healthcare providers avoid claim denials and provides a clear record of the patient’s condition and treatment.
Documentation should:
- Include relevant patient information, such as medical history, chief complaint, and relevant clinical findings.
- Specify the complexity of the medical decision making involved.
- Outline the extent of the problem-focused history and examination conducted.
Proper documentation should align with the coding guidelines and accurately reflect the services rendered. It is essential to maintain clear and consistent records that can withstand audits or reviews.
Accurate coding and documentation are essential components of efficient healthcare billing and reimbursement. By ensuring the right codes are assigned and supported by comprehensive documentation, healthcare providers can maximize their revenue, maintain compliance, and provide quality care to their patients.
Understanding the Level 3 ER Visit
When a patient presents with moderate severity problems in the emergency department, it is typically categorized as a level 3 ER visit. The 99283 CPT code is commonly assigned to these visits, as it reflects the expanded problem focused history, expanded problem focused examination, and medical decision making of moderate complexity involved in the evaluation and management of the patient.
Coding Reminder and HIPAA Rules
When it comes to coding and reimbursement processes, it is crucial to stay updated with the ever-evolving coding rules and guidelines. At our company, we prioritize compliance with the Health Insurance Portability and Accountability Act (HIPAA) rules, which govern medical code sets such as CPT, HCPCS, and ICD-9-CM. By adhering to these regulations, we ensure the privacy and security of patient health information while accurately documenting and coding medical services.
It is essential to use valid codes that are relevant to the date of service. Submitting or accepting only valid codes prevents coding errors and promotes accurate billing and reimbursement. We are continuously monitoring coding changes and updates to provide our clients with the most up-to-date coding practices and ensure compliance with HIPAA guidelines.
As coding guidelines continue to evolve, it is crucial for healthcare providers to partner with a trusted medical billing company that has a deep understanding of these changes and can navigate through the coding process effectively. At Medical Bill Gurus, we are committed to providing reliable and accurate medical billing services while adhering to the latest coding guidelines and HIPAA rules.
Stay informed and compliant with our expert team of medical billers who are well-versed in coding practices and HIPAA regulations. Let us handle your medical coding and billing needs, allowing you to focus on delivering exceptional patient care. Trust our expertise and experience in maximizing your revenue while ensuring compliance with coding rules and HIPAA guidelines.
Key Features of Our Coding Reminder and HIPAA Compliance:
- Regular updates on coding changes and guidelines
- Awareness of HIPAA rules and regulations
- Adherence to coding standards and best practices
- Accurate documentation and coding of medical services
- Secure handling of patient health information
Let us help you navigate the complex world of medical coding and reimbursement, ensuring compliance with HIPAA rules and optimizing your revenue. Contact us today to learn more about our comprehensive medical billing services.
Contact Medical Bill Gurus
If you have any questions or need assistance with medical billing services, you can contact our provider services at the following phone numbers:
- (651) 662-5200
- Toll-free: 1-800-262-0820
Our dedicated team at Medical Bill Gurus is ready to address any inquiries you may have. Whether you need help with coding, billing, or navigating the reimbursement process, we are here to assist you. Contact us today to learn more about our comprehensive medical billing services.
Medicare Guidelines for the 99283 CPT Code
When it comes to the 99283 CPT code, Medicare follows specific guidelines for reimbursement and documentation. It’s important to understand these guidelines in order to ensure proper reimbursement for Medicare patients. Here are some key points to keep in mind:
Reimbursement Rates
The reimbursement rates for the 99283 code may vary for Medicare patients. Medicare sets national facility and non-facility total payment rates for this code. It’s essential to check the specific reimbursement rates applicable to your region to ensure accurate billing. The table below provides an overview of the Medicare reimbursement rates for the 99283 code:
Note: The reimbursement rates provided in the table are for illustrative purposes only and may not reflect current rates. Please refer to the official Medicare documentation for the most up-to-date reimbursement rates.
Proper documentation is crucial when coding and billing for Medicare patients. Medicare has specific documentation requirements that must be met to support the level of service provided. It’s essential to accurately document the expanded problem focused history, expanded problem focused examination, and medical decision making of moderate complexity. Failure to meet these documentation requirements may result in claim denials or audits.
We understand the importance of adhering to Medicare guidelines, which is why at Medical Bill Gurus, we stay up-to-date with the latest coding and billing regulations. Our team of experts can assist you in navigating the Medicare reimbursement process, ensuring accurate coding and maximizing your revenue. Contact us today to learn more about our medical billing services.
Reimbursement Rates for 99283 CPT Code
The reimbursement rates for the 99283 CPT code can vary depending on the payer and geographic location. It is crucial to understand these rates to ensure accurate billing and reimbursement. Medicare, for example, sets national facility and non-facility payment rates for the 99283 code.
Here is an overview of the reimbursement rates for the 99283 CPT code:
Please note that these rates are for illustrative purposes only and may not represent the current reimbursement rates. It is essential to check with each specific payer to determine the accurate rates for the 99283 CPT code.
Global Days and CPT Coding
The concept of global days does not apply to the 99283 CPT code. Global periods are timeframes during which all related services for a procedure or surgery are considered part of the initial service and are not billed separately. However, this concept does not apply to the 99283 code since ER visits are typically standalone services.
When it comes to the 99283 CPT code, there is no need to worry about global periods or bundled services. This code specifically captures the evaluation and management of patients in the emergency department, and each visit is treated as a separate entity. It means that all the services provided during an ER visit, from the history and examination to the medical decision-making, can be coded and billed independently.
Unlike surgical procedures that have healing periods and post-operative care included in global periods, ER visits are not subject to the same rules. Therefore, you can confidently report and code the 99283 CPT code without considering any global days or bundled services.
Next, we’ll dive into more details about the bundled services and related CPT codes for emergency department visits. Stay tuned!
Bundling Information for 99283 CPT Code
The 99283 CPT code encompasses bundled services that are included in the reporting of this code. These bundled services should not be reported separately when the main code, 99283, is used. Included services range from laboratory tests and procedures to counseling and coordination of care with other healthcare professionals.
When using the 99283 CPT code, it’s important to understand which services are bundled and should not be reported separately. This helps ensure accurate coding and billing, preventing potential claim denials and ensuring proper reimbursement. The bundled services for the 99283 code vary depending on the specific circumstances and the medical necessity of the services provided.
To illustrate the bundled services within the 99283 CPT code, the following table provides an overview:
It’s crucial to understand that these bundled services are not reported separately when the 99283 CPT code is used. Proper documentation of the bundled services provided during the ER visit is essential for accurate coding and billing.
Related CPT Codes
When coding for emergency department visits, healthcare providers should be familiar with several related CPT codes. These codes encompass various levels of visits, procedures, and counseling services. It is crucial to carefully review the documentation and select the most appropriate code based on the level of service provided. By accurately coding the services, healthcare providers can ensure proper reimbursement and compliance with billing guidelines.
Commonly Used Related CPT Codes
Below are some commonly used related CPT codes for emergency department visits:
These are just a few examples of the related CPT codes used for emergency department visits. It is essential to consult the complete CPT code set and any applicable coding guidelines to ensure accurate coding and billing.
In conclusion, understanding the 99283 CPT code is crucial for accurate coding and billing of emergency department visits. This code, commonly assigned to level 3 ER visits, reflects the expanded problem focused history, examination, and medical decision making of moderate complexity involved in evaluating and managing patients. By following coding guidelines and accurately documenting the services provided, healthcare providers can ensure proper reimbursement for their efforts.
At Medical Bill Gurus, we offer comprehensive medical billing services to assist healthcare providers in optimizing their revenue and navigating the complex coding and reimbursement process. Our team, led by President Daniel Lynch, specializes in working with all insurance payers, including Medicare. We can help healthcare providers streamline their billing practices and maximize their reimbursement rates.
If you need assistance with your medical billing needs, whether it’s understanding the 99283 CPT code or navigating the reimbursement process, contact Medical Bill Gurus. Our provider services team is available at (651) 662-5200 or toll-free at 1-800-262-0820 to address your inquiries and provide further information about our services. Let us help you optimize your revenue and ensure accurate coding and billing practices.
What is the 99283 CPT code?
The 99283 CPT code is used for reporting emergency department visits that require an expanded problem focused history, an expanded problem focused examination, and medical decision making of moderate complexity. It is often assigned to level 3 ER visits.
What is a CPT code?
CPT codes, or Current Procedural Terminology codes, are a set of medical codes used to describe medical procedures and services provided by healthcare professionals. The 99283 code falls under the category of evaluation and management codes, specifically for emergency department visits.
What are the components of the 99283 CPT code?
The 99283 CPT code requires an expanded problem focused history, an expanded problem focused examination, and medical decision making of moderate complexity.
What are the coding guidelines for emergency department visits?
Emergency department visits have specific coding guidelines that must be followed. It is important to document the level of history, examination, and medical decision making in order to assign the appropriate CPT code.
How does the reimbursement process work for the 99283 CPT code?
Reimbursement for the 99283 CPT code is dependent on various factors, including the payer’s policies and the documentation supporting the level of service provided. Accurate coding and documentation are essential for proper reimbursement.
Who is Medical Bill Gurus?
Medical Bill Gurus is a medical billing company led by President Daniel Lynch. They specialize in providing medical billing services for healthcare providers, assisting with the coding, billing, and reimbursement process.
Why is accurate coding important?
Accurate coding is crucial for healthcare providers as it directly impacts the reimbursement they receive for their services. Proper coding ensures that the services provided are reflected accurately in billing claims, which affects reimbursement rates.
What is a level 3 ER visit?
When a patient presents with moderate severity problems in the emergency department, it is typically categorized as a level 3 ER visit. The 99283 CPT code is commonly assigned to these visits.
What are the coding reminder and HIPAA rules to follow?
All coding and reimbursement processes are subject to changes, updates, and other requirements of coding rules and guidelines. It is important to stay up to date with coding changes and follow the HIPAA rules governing medical code sets.

How can I contact Medical Bill Gurus?
If you have any questions or need assistance with medical billing services, you can contact Medical Bill Gurus’ provider services at (651) 662-5200 or toll-free at 1-800-262-0820.
What are the Medicare guidelines for the 99283 CPT code?
Medicare follows specific guidelines for the 99283 CPT code. Reimbursement rates and documentation requirements may vary for Medicare patients. It is important to adhere to their guidelines when coding and billing for Medicare.
What are the reimbursement rates for the 99283 CPT code?
The reimbursement rates for the 99283 CPT code may vary depending on the payer and the geographic location. Medicare sets national facility and non-facility total payment rates for this code. It is important to check specific reimbursement rates for each payer.
Does the concept of global days apply to the 99283 CPT code?
No, the concept of global days does not apply to the 99283 CPT code. ER visits are typically standalone services and are not subject to global periods.
What bundled services are included in the 99283 CPT code?
The 99283 CPT code has bundled services that are included in the reporting of this code. These bundled services should not be reported separately when the main code, 99283, is used.
Are there any related CPT codes for emergency department visits?
Yes, there are several related CPT codes that healthcare providers should be aware of when coding for emergency department visits. These codes include different levels of visits, procedures, and counseling services.
What is the significance of understanding the 99283 CPT code?
Understanding the 99283 CPT code is essential for accurate coding and billing of emergency department visits. Medical Bill Gurus offers medical billing services to assist healthcare providers in optimizing their revenue and navigating the coding and reimbursement process.
Leave a Comment Cancel Reply
Your email address will not be published. Required fields are marked *

AVAILABLE MON-FRI
From 8 am to 8 pm mst, houston office:.
525 N Sam Houston Pkwy E, Suite #246 Houston, Texas, 77060
Denver Office:
3000 Lawrence Street Suite #15 Denver, CO 80205
Tampa Office:
260 1st Ave S, #34 St Petersburg, Florida 33701
Phoenix Office:
7042 E Indian School Rd #100 Scottsdale, AZ 85251
Copyright © 2024 | All Rights Reserved | Medical Billing Company | XML Sitemap | Privacy Policy | Cookie Policy | HIPPA Compliance Policy
Digital Marketing by Denver Digital Marketing Agency

- Revenue Cycle Management
- Reimbursement
- Diabetes Awareness Month
- Risk Management
- Patient Retention
- Medical Economics® 100th Anniversary
- Coding and documentation
- Business of Endocrinology
- Physicians Financial News
- Cybersecurity
- Cardiovascular Clinical Consult
- Locum Tenens, brought to you by LocumLife®
- Weight Management
- Business of Women's Health
- Practice Efficiency
- Finance and Wealth
- Remote Patient Monitoring
- Sponsored Webinars
- Medical Technology
- Billing and collections
- Acute Pain Management
- Exclusive Content
- Value-based Care
- Business of Pediatrics
- Concierge Medicine 2.0 by Castle Connolly Private Health Partners
- Practice Growth
- Concierge Medicine
- Business of Cardiology
- Implementing the Topcon Ocular Telehealth Platform
- Malpractice
- Sexual Health
- Chronic Conditions
- Legal and Policy
- Practice Management
- Patient Relations
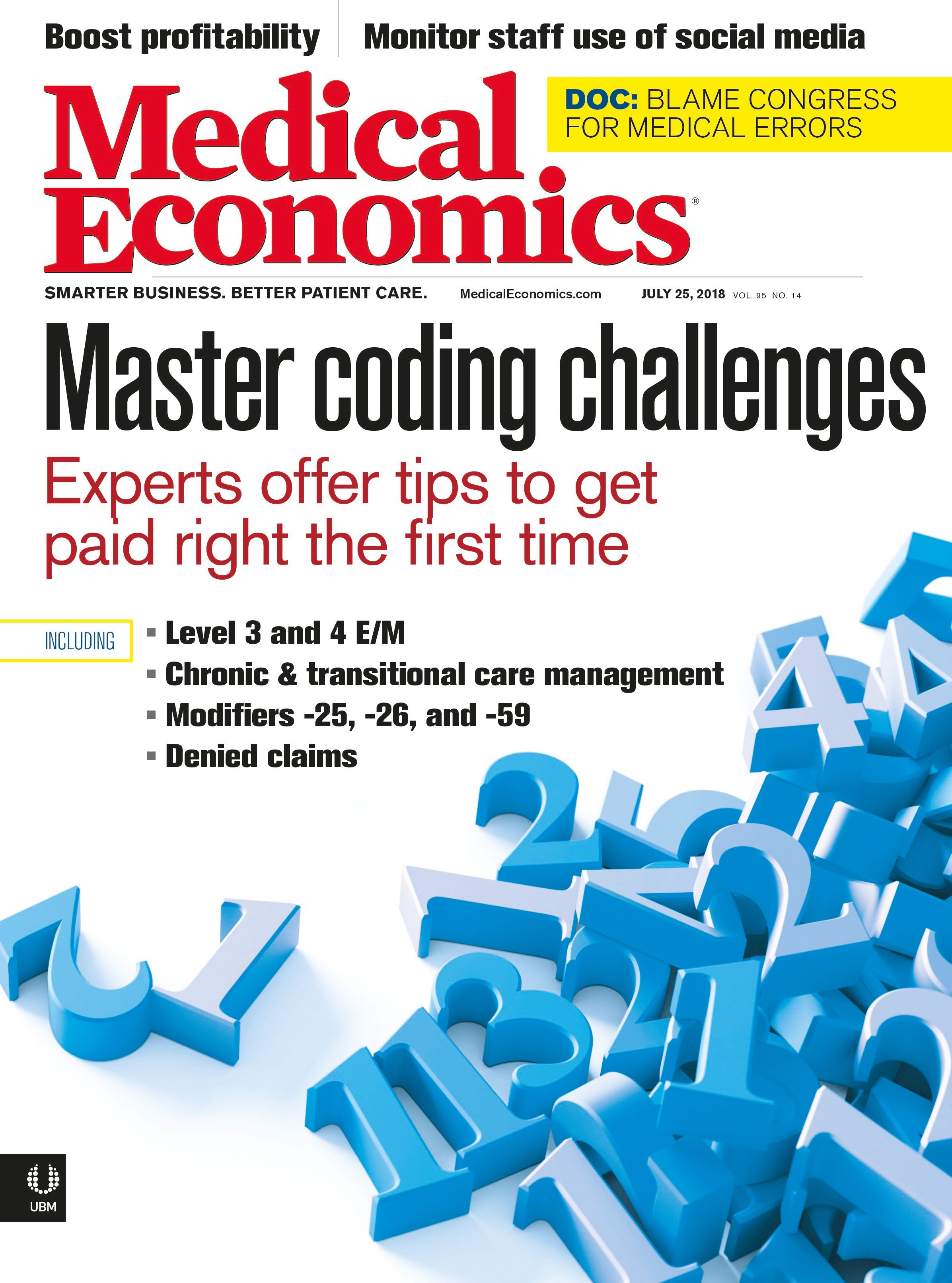
Coding tips: Level 3 vs. 4 evaluation and management
To payers, these visits tell a completely different story about the work that’s required to treat a patient.
The difference between a level 3 and level 4 office visit might not seem like much, but to payers, these visit types each tell a completely different story about the work that’s required to treat a patient.
When physicians report a level 4 evaluation and management (E/M) code, they’re telling payers they should be paid more because their patient requires medical management for an exacerbation of an existing chronic condition, a complication, or a new problem, says Raemarie Jimenez, CPC, vice president of membership and certification solutions at AAPC in Salt Lake City, Utah. Payers may deny level 4 E/M codes for patients who respond well to treatment and are generally well-managed, she adds.
When using an EHR, though, it’s easy for physicians to default to a level 4 E/M code that might not be justified, says Jimenez. That’s because the EHR pulls information forward that might not be clinically relevant or even pre-populates information that falsely inflates the actual work the physician performs. “The computer just picks up on keywords and boxes, but it’s not smart enough to realize that a visit might be over-documented,” she adds.
For example, pulling information forward, such as a comprehensive family history or a complete review of systems, can inadvertently drive a level 4 E/M code when the nature of the presenting problem (e.g., otitis media) in no way supports this level of service, explains Jimenez. Over time, it may appear to payers that a physician is upcoding as compared to peers.
To avoid payer scrutiny, Jimenez advises physicians always to ask themselves these three questions before assigning a level 4 E/M code:
1. Is this patient sicker than most of the patients I see? 2. What specifically elevates the level of effort that’s required to treat this patient? Have I documented this information in the record? 3. Have I reported the most specific ICD-10-CM diagnosis code to justify patient severity?
Physicians should also know whether their EHR might be putting them at risk for upcoding. Jimenez says to consider these three questions:
1. Does the EHR auto-populate information and require physicians to deselect what’s not pertinent to the visit? For example, an EHR might auto-populate a complete review of systems and require physicians to deselect the systems they don’t review with the patient. This practice is extremely risky because physicians don’t often remember to review the information or they may simply forget to deselect it, says Jimenez. Best practice is for physicians to manually select what they want to bring forward. It shouldn’t happen automatically, she adds.
2. Do diagnosis-specific templates require physicians to perform certain tasks every time they see a patient? All work must be clinically relevant, says Jimenez. “Physicians shouldn’t be forced to do something just because the EHR is telling them to do it. Everything they do should be based on their own clinical judgment.”
3. Does the EHR require physicians to bill a certain code? The code that the system calculates may not be accurate, and physicians always need the ability to override it when necessary, says Jimenez. She provides the example of a physician who includes rule-out diagnoses for continuity-of-care purposes. If the physician isn’t actively managing these conditions, they shouldn’t be counted toward the visit’s E/M level. If the EHR gives credit for this information, physicians need to recognize that the E/M level may be inflated, and they should override the code manually, she says.
Description
2018 national average Medicare Payment
Level 3 office visit
New patient
Level 4 office visit
Established patient
Waste Management buys Stericycle for $7.2 billion

Finding financing for medical practices

Medical care prices creep up, contribute to inflation in April

Episode 3: Tips for building a retirement nestegg

Consideration postponed for new billing codes for prior authorization

Feds form task force against monopolies and collusion in health care
2 Commerce Drive Cranbury, NJ 08512
609-716-7777
Condition Headquarters:
What are the differences between emergency room levels.

Emergency Departments (ED's or ER's) are categorized into five levels of care. Level I is the highest level and must have immediately available surgical specialists and sub-specialists (surgeons, neurosurgeons, orthopedic surgeons, anesthesiologists, plastic surgeons) in order to handle the most severe and complicated injuries. These ED's are all in large cities, usually have a wide area of service with helicopter transport, and are fully staffed with Emergency Medicine specialists. They are associated with medical schools.
Level II is the ED in most large and medium size hospitals, with surgeons and anesthesiologists on call 24 hours daily, with an ICU and staffed usually with Emergency Medicine specialists. This Level can handle common surgical problems, most auto accidents and almost all illnesses including heart attacks and strokes.
Level III ED's may not have on-call surgeons at all times, but usually can handle surgical problems within 24 hours. These have physicians in the ED 24 hours daily, but the physician may not be an Emergency Medicine specialist. This ED is best at treating and stabilizing the sicker or more severely injured patient for rapid transfer to a Level II or Level I facility. Level IV and V facilities are found in some states. They are usually in rural areas, may not have a physician at all times and are intended to stabilize a patient for transfer.
Continue Learning about Critical Care

Important: This content reflects information from various individuals and organizations and may offer alternative or opposing points of view. It should not be used for medical advice, diagnosis or treatment. As always, you should consult with your healthcare provider about your specific health needs.
Emergency Department Visits – Level of Service
Policy No: 110 Date of Origin: 09/01/2020 Section: Facility Last Reviewed: 12/01/2023 Last Revised: 12/01/2023 Approved: 12/14/2023 Effective: 01/01/2024 Policy Applies to : Group and Individual & Medicare Advantage
This policy applies to outpatient facilities.
Definitions
Straightforward Self-limited condition with no meds or home treatment required, signs and symptoms of wound infection explained, return to Emergency Department (ED) if problems develop (see Reference section, #1).
Simple Over the counter (OTC) medications or treatment, simple dressing changes; patient demonstrates understanding quickly and easily (see Reference section, #1).
Moderate Head injury instructions, crutch training, bending, lifting, weight-bearing limitations, prescription medication with review of side effects and potential adverse reactions; patient may have questions, but otherwise demonstrates adequate understanding of instructions either verbally or by demonstration.
Complex Multiple prescription medications and/or home therapies with review of side effects and potential adverse reactions; diabetic, seizure or asthma teaching in compromised or non-compliant patients; patient/caregiver may demonstrate difficulty understanding instructions and may require additional directions to support compliance with prescribed treatment.
Emergency Department
- Type A emergency department: must meet regulatory requirements and be open 24 hours/day and 7 days/week and apply codes 99281-99285.
Type B emergency department: must meet regulatory requirements but is not open 24 hours/day and 7 days/week and apply codes G0380-G0384.
Emergency Medical Condition
- Member is in serious jeopardy of their health or their unborn child, or
- Has serious body function or impairment, or
Has serious dysfunction of any bodily organ or part.
Emergency Services Services needed to stabilize an emergency medical condition.
Background Currently, there are no national standards, that assign levels of services in the emergency department (ED). Thus, the American College of Emergency Physicians (ACEP) developed emergency department (ED) level guidelines, which are in line with the outpatient prospective payment system (OPPS) principles (see Reference section, #1). The ACEP guideline is one of the best-known models for assessing the appropriate level of ED services. The level of care is determined by interventions/complexity of services. Even if multiple interventions within a level occur, the level is the same e.g., two or three interventions within the 99281 level would remain as a 99281 level.
Policy Statement
Individual facility provisions, contracts or state or federal guidelines take precedence over this policy.
Reimbursement for facility Emergency Department (ED) services are based on the highest-level E&M and revenue code for which a claim qualifies. A Current Procedural Terminology (CPT®) Code or a Healthcare Common Procedure Coding System (HCPCS) Code for Evaluation and Management (E&M) must be billed, based on the complexity of facility intervention(s) that occurred, during the patient ED visit.
Our health plan requires documentation from the ED visit that includes but is not limited to physician order(s), presenting symptoms, diagnoses and treatment plan in the medical record.
Our health plan reviews the complexity level of facility interventions for the E&M codes as described in the table below. Each level provides facility intervention examples that align with the evaluation and management (E&M) service. The table below, although not an all-inclusive, provides criteria that our health plan will apply to determine the level of reimbursement, for ED services.
Exceptions include:
- ED visits resulting in observation status or inpatient admission. Emergency Room visits that result in an Inpatient submission will follow guidelines under Reimbursement of Facility Room and Board policy (FAC 103)
- Critical access hospital services
- Trauma or critical care services
Surgical intensive care services
If a member is admitted as an inpatient from the emergency department or from observation following a visit to the emergency department, the emergency department services provided to that member must be submitted on the same claim as the inpatient services and are not subject to this policy.
American College of Emergency Physicians (ACEP), ED Facility Level Coding Guidelines
Anthem Emergency Department: Level of Evaluation and Management Services
Optum360, 2020
Centers for Medicare and Medicaid Services (CMS), 42 CFR § 422.113
Centers for Medicare and Medicaid Services (CMS), OPPS Visit Codes Frequently Asked Questions, CMS.gov
Cross References
Correct Coding Guidelines
Reimbursement of Facility Room and Board
Your use of this Reimbursement Policy constitutes your agreement to be bound by and comply with the terms and conditions of the Reimbursement Policy Disclaimer .
- Find a Doctor
Coding and Billing Guidelines for Emergency Department
- Provider Service: 800-368-2312
- For Medicaid Expansion: 833-777-5779
- Caring Foundation
- Privacy & Legal
- Our Partners in Health:
Fargo (Headquarters) 4510 13th Ave. S. Fargo, N.D., 58121
Blue Cross Blue Shield of North Dakota is an independent licensee of the Blue Cross Blue Shield Association, serving residents and businesses in North Dakota. All rights reserved.
© 2024 Blue Cross Blue Shield of North Dakota
- Non-Discrimination Notice
- العَرَبِيَّة
- Diné Bizaad
Processing...
Please wait while your form is being submitted
- Code Sets and Indexes
- Publications
HCPCS Code for Level 3 hospital emergency department visit provided in a type B emergency department; (the ED must meet at least one of the following requirements: (1) it is licensed by the state in which it is located under applicable state law as an emergency room or emergency department; (2) it is held out to the public (by name, posted signs, advertising, or other means) as a place that provides care for emergency medical conditions on an urgent basis without requiring a previously scheduled appointment; or (3) during the calendar year immediately preceding the calendar year in which a determination under 42 CFR 489.24 is being made, based on a representative sample of patient visits that occurred during that calendar year, it provides at least one-third of all of its outpatient visits for the treatment of emergency medical conditions on an urgent basis without requiring a previously scheduled appointment) G0382
Hcpcs code g0382 for level 3 hospital emergency department visit provided in a type b emergency department; (the ed must meet at least one of the following requirements: (1) it is licensed by the state in which it is located under applicable state law as an emergency room or emergency department; (2) it is held out to the public (by name, posted signs, advertising, or other means) as a place that provides care for emergency medical conditions on an urgent basis without requiring a previously scheduled appointment; or (3) during the calendar year immediately preceding the calendar year in which a determination under 42 cfr 489.24 is being made, based on a representative sample of patient visits that occurred during that calendar year, it provides at least one-third of all of its outpatient visits for the treatment of emergency medical conditions on an urgent basis without requiring a previously scheduled appointment) as maintained by cms falls under hospital observation and emergency services ., subscribe to codify by aapc and get the code details in a flash., official long descriptor.
- HCPCS MODIFIERS
- HCPCS CPT ® Crosswalk

Compliance Tools
- Fee Schedules
- MCR NCCI Edits Alert
- Coding Alert(s)
- AHA HCPCS CODING CLINIC ®
Latest News

What drives the level of office visit codes?
Many physicians and coders think longer documentation means charging higher level visits. Fortunately, that is not always the case. You can document less as long as you are documenting the correct and necessary information.
Medical decision making drives the level of office visit
The medical decision-making portion of evaluation and management guidelines is what ultimately determines the level billed. Higher complexity in decision making justifies higher levels.
Evaluation and Management visits have three main components:
- Physical exam
- Medical decision making.
For established patients, guidelines state that only two of these three need to be met for a given level. The Center for Medicare and Medicaid Services advises to let medical decision making drive the visit.
What does “Medical decision making should drive the visit” really mean?
This is such a grey area in the guidelines that it is causing practices to over-bill or undercharge, which will ultimately cause them to fail an audit.
CMS stated, “It would not be medically necessary or appropriate to bill a higher level of evaluation and management service when a lower level of service is warranted. The volume of documentation should not be the primary influence upon which a specific level of service is billed.” ( Medicare Claims Processing Manual 30.6.1)
Many practices are so confused about what this means, that they just pick the middle level and call it a day. Those practices need clarification and education on how to get to the correct level for the service performed. MEREM can help!
Below are some examples to remember when choosing the level of an office visit to the bill.
- If the provider is seeing an established patient who is coming in for a recheck, ask yourself is the patient’s diagnosis improving or worsening?
– If the problem is improving, the level of service will likely be a level 2 (99212).
⁃ If the problem is worsening, the level of service is likely a level 3 (99213).
- For established patients coming in with a new problem , these level of service is likely a level 3 (99213) or level 4 (99214). The final level for this patient will depend on the diagnosis and treatment performed during the service.
- Code 99215 is used to report High MDM. 99215 is reserved for those patients who require extensive workup regarding Chronic Illnesses with severe exasperations or acute illness or injuries that threaten loss of life or bodily function. Management options for these patients may include IV drug therapy, Emergency Surgery or a DNR status because of poor prognosis.
Let MEREM Health help you conquer the challenges of coding your office visits. Call us to get a free quote at 205-329-7519.
© 2024 MEREM Health. All Rights Reserved.

Is your practice losing money?
How quickly are your claims being followed up on upon initial denial?
Are you confident in your in-house/outsourced coding accuracy?
Let our consultants provide you with a free tool to help improve your current revenue process.
Schedule a Free Consultation


(2023) CPT Code G0463 – Description, Guidelines, Reimbursement, Modifiers & Examples
CPT code G0463 will be reported by the physician when service renders at the hospital outpatient clinic visit for assessment and management of a patient.
In 2014, CMS proposed three new HCPCS G codes in OPPS (Outpatient Prospective Payment System) to substitute for five levels of evaluation and management settings.
It includes one G code for type A ED (Emergency Dept) visits and one for type B ED visits.
The new HCPCS code G0463 is an alternative to all clinic visits for new and established patients when billed to Medicare carriers.
G0463 is effective from January 1, 2014, in the place of Clinic visits codes (99201-99215).
The hospital requires to place only one G code instead of CPT (99201-99215) when billed to Medicare insurances. G0463 does not differentiate between new and established patients.
There are two types of charges as one is billed under facility or hospital charge while the other is physician charge.
G code is only used for hospital or facility-based payments when billed to Medicare under the OPPS.
Therefore, it eradicates the criteria of choosing level evaluation and management visits.
Also, it does not require any specific measures to meet for the service provided.
CPT Code G0463 Description
CPT code G0463 will be reported by the physician when service renders at the Hospital outpatient clinic visit for assessment and management of a patient.

CPT Code G0463 Reimbursement
A maximum of zero units of CPT code G0463 is allowed to bill on the same day.
In contrast, a maximum of three times are allowed when documentation supports the medical necessity of CPT code G0463.
The CPT code G0463 cost and RUVS are as follows when performed in the outpatient off-campus hospital, it will be $47.50 and 0, respectively.
In contrast, the off-campus provider will be $47.50 and 0, respectively.
CPT Code G0463 Modifiers
There is the following list of modifiers that are applicable with CPT code G0463:
- 24, 25, 27, 57, 99, AI, CS, CR, CC, EY, ET, G0, GC, GA, GJ, GK, GT, GQ, GR, GU, GZ, KX, Q5, QJ and Q6
The most frequent modifiers used with G0463 CPT code are 24, 25, and 57.
Modifier 25 will be appended with G0463 CPT code when services are done in conjunction with other services generally not billed together on the same day.
While 24 will be appended with services done in the postoperative period with unrelated procedures or services.
Modifier 57 will be attached to G0463 CPT code if physicians plan to do surgery on the same date of service when the E/M visit is done.
Modifier 27 is applicable when a patient saw multiple times by the physician on the same day for evaluation and management visit codes.
CPT Code G0463 Billing Guidelines
Documentation should support the medical necessity of service and be medically appropriate.
It reflects the patient’s current condition.
G0463 CPT code bills for facilities or hospital charges only and physician charges will be billed separately.
Any service billed under facility or clinic visit billed to Medicare will be under OPPS with appropriate HCPCS G codes.
Q3014 is applicable when telemedicine service is provided by the hospital as an origin site to other outpatient hospital patients.
G0463 CPT code will not be more appropriate to report for telehealth services due to COVID 19.
CPT G0463 is only applicable when service bills to Medicare insurance. Time is not a determining factor when G0463 CPT code will be billed.
CPT 99201-99215 code has time factors in choosing the appropriate level of evaluation and management CPT code.
All the five levels of CPT codes such (as 99201-99205) will be billed as single HCPCS code G0463 CPT code when billed to Medicare.
History, physical exam , assessment, and plan are necessary to be mentioned on the chart. Otherwise, service will be denied by Medicare insurance.
HCPCS code G0463 is the substitute of hospital outpatient department visit codes 99201-99205, 99211-99215 when insurance is Medicare.
Commercial insurances do not accept G codes.
Check the appropriate guidelines of third parties or payers regarding the billing of CPT code G0463.

CPT Code G0463 Examples
The following are examples of when CPT code G0463 service is billed.
67-year-old-male with a PMH of HTN, HLD, hypothyroidism presenting to the clinic because of a headache and high blood pressure before arrival. His primary insurance is Medicare.
The patient lays down in bed at 10 pm and begins having a gradual onset pulsating frontal and occipital headache.
He reports that the pain was very severe. His headaches are usually associated with HTN.
The blood pressure shows a value of 210/100 and denies associated dizziness, chest pain , shortness of breath , motor weakness , numbness/tingling, abdominal pain, nausea/vomiting.
The physician ordered a series of diagnostic tests CT, MRI , and EKG . EKG was independently interpreted and reviewed by the doctor.
Patient reports improvement in HA with Tylenol.
A 51-year-old-female presents to the office with syncope . Her primary insurance is Medicare.
The patient applies a nicotine patch earlier. The patient had a brief episode of feeling hot, numbness, and tanginess in her b/l hands, “gas discomfort” in her stomach, headache.
When she tried to get up, she lost consciousness (witnessed by her partner, who I spoke to for more hx).
Partner states she was only out for a few seconds before perking up to routine. Pt states she has had episodes like this in the past but several years ago. No known cardiac history.
Physicians plan to order CBC , CMP, mg, phos, trop, EKG, Tylenol, Pepcid, Zofran.
EKG: Normal sinus rhythm. 70 bpm. No ST elevation or T wave inversions.
CXR: My interpretation showed no acute abnormalities.
36-year-old male presents to the office with PMH HTN, HLD, Afib (on eliquis), Mitral valve replacement, and gout presenting today for dark blood stools for two days.
He states that he started having diarrhea yesterday and has had 4 BM in the past two days. His primary insurance is Medicare.
The patient denies nausea, vomiting, CP, SOB, dizziness, fevers, chills, took eliquis this morning.
The physician also notes worsening bilateral lower extremity edema for which he takes Lasix.
He took Indomethacin for four days for a presumed gout flare.
The colonoscopy was done three years ago, found benign polyp but otherwise WNL.
Physician plan to admit and Plan Labs, EKG, CT abdomen , and Pelvis, and prescribed Medicine.
70-year-old female presents to clinic with hx of HLD presenting to the OPD for substernal chest pain.
Her primary insurance is Medicare. The patient worked out daily, was a very healthy, active senior, lived at home, and worked out today.
After the workout, she took a sip of water, and she had substernal chest pain, none radiating, associated with weakness.
However, Gatorate helped with the substernal chest pain.
She had no chest pain shortly after. However, her trainer told her to see a provider.
She went to urgent care with asymptomatic resolved chest pain, and they sent her over here because she had a family history of MI in her family.
Her brother died of MI at age 48 EKG without ischemic changes. Low suspicion for ACS. HEART score 3.
38-year-old female past medical history of chronic gastritis diagnosed on endoscopic two weeks ago presenting with one month of on and off palpitations and lightheadedness.
The patient states that she has been feeling off for the last month and describes her symptoms as when she wakes up in the morning and feels fogginess has bouts of palpitations with associated lightheadedness without syncope.
The patient cannot pinpoint a trigger and states her symptoms resolve independently.
Palpitations last anywhere in the body for seconds to minutes.
The patient endorses that she has a healthy diet and does not do any narcotics drink alcohol, or smoke.
The patient otherwise denies fevers, chills, syncope, headaches, neck pain, chest pain, shortness of breath, back pain , abdominal pain, nausea, vomiting, diarrhea, constipation.
The physician decided will obtain EKG labs chest x-ray reassess
EKG normal sinus rhythm at 74 bpm with a QTC of 426 no ST elevations or depressions.
Similar Posts
How to use hcpcs code g0175.
HCPCS code G0175 describes a scheduled interdisciplinary team conference with the patient present. This code is used to identify a specific type of service provided by healthcare professionals. In this article, we will explore the details of HCPCS code G0175, including its official description, procedure, when to use it, billing guidelines, historical information, Medicare and…
How To Use HCPCS Code G9271
HCPCS code G9271 describes a specific LDL value of less than 100. This code is used to identify patients who have a low-density lipoprotein (LDL) cholesterol level below 100 mg/dL. In this article, we will explore the details of HCPCS code G9271, including its official description, procedure, when to use it, billing guidelines, historical information,…
How To Use HCPCS Code A4253
HCPCS code A4253 describes blood glucose test or reagent strips for home blood glucose monitors. These strips are used by individuals with diabetes to monitor their blood glucose levels. In this article, we will explore the details of HCPCS code A4253, including its official description, procedure, when to use it, billing guidelines, historical information, Medicare…
How To Use HCPCS Code G0478
HCPCS code G0478 describes a specific drug testing procedure that is used to detect the presence of various drug classes in a patient’s system. This code is specifically for presumptive drug testing, which involves the use of immunoassay devices or procedures that are read by instrument-assisted direct optical observation, such as dipsticks, cups, cards, or…
How To Use HCPCS Code E0667
HCPCS code E0667 describes a segmental pneumatic appliance that is used in conjunction with a pneumatic compressor for the full leg. This code is specifically used for enteral supplies that are not otherwise classified. In this article, we will explore the details of HCPCS code E0667, including its official description, procedure, when to use it,…
How To Use HCPCS Code C9741
HCPCS code C9741 describes a specific medical procedure known as right heart catheterization with implantation of a wireless pressure sensor in the pulmonary artery. This code encompasses various components of the procedure, including measurements, angiography, imaging supervision, interpretation, and reporting. It is important for medical coders to understand the details and appropriate usage of this…
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
HCPCS Code G0382
Level 3 hospital emergency department visit provided in a type b emergency department; (the ed must meet at least one of the following requirements: (1) it is licensed by the state in which it is located under applicable state law as an emergency room or emergency department; (2) it is held out to the public (by name, posted signs, advertising, or other means) as a place that provides care for emergency medical conditions on an urgent basis without requiring a previously scheduled appointment; or (3) during the calendar year immediately preceding the calendar year in which a determination under 42 cfr 489.24 is being made, based on a representative sample of patient visits that occurred during that calendar year, it provides at least one-third of all of its outpatient visits for the treatment of emergency medical conditions on an urgent basis without requiring a previously scheduled appointment)
Procedures/Professional Services (Temporary Codes)
G0382 is a valid 2024 HCPCS code for Level 3 hospital emergency department visit provided in a type b emergency department; (the ed must meet at least one of the following requirements: (1) it is licensed by the state in which it is located under applicable state law as an emergency room or emergency department; (2) it is held out to the public (by name, posted signs, advertising, or other means) as a place that provides care for emergency medical conditions on an urgent basis without requiring a previously scheduled appointment; or (3) during the calendar year immediately preceding the calendar year in which a determination under 42 cfr 489.24 is being made, based on a representative sample of patient visits that occurred during that calendar year, it provides at least one-third of all of its outpatient visits for the treatment of emergency medical conditions on an urgent basis without requiring a previously scheduled appointment) or just “ Lev 3 hosp type b ed visit ” for short, used in Medical care .
HCPCS Modifiers
In HCPCS Level II, modifiers are composed of two alpha or alphanumeric characters.
Example: E0260-NU - Hospital bed, semi-electric (head and foot adjustment), with any type side rails, with mattress “ NU ” identifies the hospital bed as new equipment
Browse all modifiers
HCPCS G0381 · Level 2 hospital emergency department visit provided in a type b emergency department; (the ed must meet at least one of the following requirements: (1) it is licensed by the state in which it is located under applicable state law as an emergency room or emergency department; (2) it is held out to the public (by name, posted signs, advertising, or other means) as a place that provides care for emergency medical conditions on an urgent basis without requiring a previously scheduled appointment; or (3) during the calendar year immediately preceding the calendar year in which a determination under 42 cfr 489.24 is being made, based on a representative sample of patient visits that occurred during that calendar year, it provides at least one-third of all of its outpatient visits for the treatment of emergency medical conditions on an urgent basis without requiring a previously scheduled appointment)
Hcpcs g0383 · level 4 hospital emergency department visit provided in a type b emergency department; (the ed must meet at least one of the following requirements: (1) it is licensed by the state in which it is located under applicable state law as an emergency room or emergency department; (2) it is held out to the public (by name, posted signs, advertising, or other means) as a place that provides care for emergency medical conditions on an urgent basis without requiring a previously scheduled appointment; or (3) during the calendar year immediately preceding the calendar year in which a determination under 42 cfr 489.24 is being made, based on a representative sample of patient visits that occurred during that calendar year, it provides at least one-third of all of its outpatient visits for the treatment of emergency medical conditions on an urgent basis without requiring a previously scheduled appointment).
1 Two-digit numeric codes are Level I code modifiers copyrighted© by the American Medical Association's Current Procedural Terminology (CPT).
2 BETOS stands for “Berenson-Eggers Type Of Service”
- A service or procedure has both a professional and technical component.
- A service or procedure was performed by more than one physician and/or in more than one location.
- A service or procedure has been increased or reduced.
- Only part of a service was performed.
- An adjunctive service was performed.
- A bilateral procedure was performed.
- A service or procedure was provided more than once.
- Unusual events occurred.
Code used to identify the appropriate methodology for developing unique pricing amounts under part B. A procedure may have one to four pricing codes.
Code used to identify instances where a procedure could be priced under multiple methodologies.
A code denoting Medicare coverage status.
The Berenson-Eggers Type of Service (BETOS) for the procedure code based on generally agreed upon clinically meaningful groupings of procedures and services.
A code denoting the change made to a procedure or modifier code within the HCPCS system.
The date the HCPCS code was added to the Healthcare common procedure coding system.
Effective date of action to a procedure or modifier code
The carrier assigned CMS type of service which describes the particular kind(s) of service represented by the procedure code.
Number identifying statute reference for coverage or noncoverage of procedure or service.

Three common reasons for level 5 E/M office visits in primary care
Keith W. Millette, MD, FAAFP, RPH
If you’ve read the January/February issue of FPM , you know how to identify level 4 office visits under the new evaluation and management (E/M) guidelines and avoid losing money by under-coding them. But what about level 5 visits?
While not as common, level 5 visits do occur in primary care, and under-coding them can also have serious financial ramifications. To quickly identify and correctly code most level 5 office visits, keep in mind these three common reasons for level 5 work:
Reason No. 1: Time
The new guidelines allow coding of outpatient E/M office visits based solely on either total time on the date of service or medical decision making (MDM). Many level 5 office visits billed by family physicians will be based on time. If your total time is at least 40 minutes for an established patient or 60 minutes for a new patient, code that visit as a level 5.
Remember that total time includes all time spent caring for that patient on the day of the encounter. That means you count your prep time reviewing the chart before the visit, your face-to-face time during the visit, and the time you spend after the visit (as long as it occurs before midnight) reviewing studies, making phone calls, documenting your note, etc. (See these tips for tracking time .)
You must document your total time in the note. Because patients may read your notes, consider writing: “Total time was XX minutes. That includes chart review before the visit, the actual patient visit, and time spent on documentation after the visit.” This helps patients understand that you spend a lot of time behind the scenes caring for them, and it may even prevent confused patients from falsely accusing you of fraud (e.g., “He only spent 20 minutes with me, not the 40 minutes he listed in his note”) . Time spent on separately billed procedures done during an E/M visit does not count toward total time, so adding a statement such as “Time excludes procedure” is also helpful.
Reason No. 2: Pre-op visits for major surgery
To code a level 5 office visit using MDM you need at least two out of these three elements: high complexity problems, high risk, or extensive data review. Pre-op visits before elective major surgery in patients who have risk factors or require labs, X-rays, or electrocardiograms (ECGs) for evaluation/preoperative clearance often check these boxes.
There are two types of risk you can consider when it comes to pre-op visits: procedure risk and patient risk. Major surgery involves high procedure risk, including general anesthesia and the procedure itself (e.g., coronary artery bypass, total hip replacement, and abdominal surgery). Patient risk factors include morbid obesity, heart disease, diabetes, lung disease, etc. It is important to document both the patient risk factors and the procedure risk in your note.
The data portion of MDM is split into three categories:
1. Tests, documents, or independent historian(s); any combination of three from the following:
- Review of prior external note(s) from each unique source,
- Review of the result(s) of each unique test,
- Ordering of each unique test,
- Assessment requiring independent historian(s).
2. Independent interpretation of a test performed by another physician/other qualified health care professional (not separately reported).
3. Discussion of management or test interpretation with an external physician or other qualified health professional/appropriate source (not separately reported).
A visit must include at least two out of those three categories to qualify as level 5 “data” work. For level 5 pre-op visits, this commonly involves ordering/reviewing a minimum of three tests (e.g., labs , ECG, and chest X-ray) and interpreting at least one study (e.g., ECG or X-ray). To get credit for interpretation it must be clear in the note that you evaluated the study (e.g., “I personally evaluated the chest X-ray and it shows … ”) and did not just look at the report. Remember, if your health system is billing separately for the interpretation, you cannot count it toward your E/M visit level (for more tips on counting MDM data, click here ).
For practical purposes, the minimum criteria for coding level 5 pre-ops would look something like this as a simple equation: Level 5 pre-op = major surgery + risk factors + order/review three tests + interpret one study.
Reason No. 3: Very sick patients who require work up and/or admission decision
Very sick patients often require level 5 work if they have a high complexity problem such as acute respiratory distress, depression with suicidal ideation, or any new life-threatening illness or severe exacerbation of an existing chronic illness. It is common for these visits to qualify as high risk or require extensive data review, thereby pushing them into level 5 territory. Examples include the following:
1. Seeing a very sick patient (such as one with severe exacerbation or progression of their chronic condition, or side effects of treatment of their chronic condition) in the office who requires hospital admission (and you are not doing the admitting yourself) or requires you to contemplate admission (make sure to document your thought process in the note). This combines a high-complexity problem (or problems) with high risk.
2. Seeing a very sick patient (such as one with an acute or chronic condition that poses a threat to life or bodily function) who requires an office work up that qualifies as level 5 data review (e.g., ordering/reviewing a minimum of three tests and interpreting one study). This combines a high complexity problem (or problems) with extensive data.
To summarize, here are the three common reasons to code a level 5 office visit:
These are only a few useful examples of level 5 work. Less common scenarios may also qualify, such as visits that include decisions to de-escalate care or initiate do-not-resuscitate orders, decisions about emergency major surgery, and decisions about the use of drugs that require intensive monitoring. Referring to a coding template can be helpful for those scenarios. But for the three types of visits outlined above, you should not be afraid to think level 5 if your documentation supports it.
— Keith W. Millette, MD, FAAFP, RPH, is a family physician in Grand Forks, N.D.
- Chronic care
- Medicare/Medicaid
- Physician compensation
- Practice management
- Reimbursement
- Value-based payment
Other Blogs
- Quick Tips from FPM journal
- AFP Community Blog
- Fresh Perspectives
- In the Trenches
- Leader Voices
- RSS ( About RSS )
Disclaimer: The opinions and views expressed here are those of the authors and do not necessarily represent or reflect the opinions and views of the American Academy of Family Physicians. This blog is not intended to provide medical, financial, or legal advice. Some payers may not agree with the advice given. This is not a substitute for current CPT and ICD-9 manuals and payer policies. All comments are moderated and will be removed if they violate our Terms of Use .
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

COMMENTS
According to CPT, a typical level-II visit lasts 10 minutes, while a typical level-III visit lasts 15 minutes. If counseling or coordination of care account for more than 50 percent of the visit ...
ER level 1-2 visits are reserved for treatment of mild cases like bug bites and sunburns. The majority of ER visits fall between ER visit levels 3-5, with ER visit level 4 being the most common, Fries says. "Most emergency room claims will qualify as a 99284, because you only need something as simple as IV fluids to get you there," Fries says.
Think time first. If your total time spent on a visit appropriately credits you for level 3, 4, or 5 work, then document that time, code the visit, and be done with it. But if it does not, go to ...
Understanding the Level 3 ER Visit. When a patient presents with moderate severity problems in the emergency department, it is typically categorized as a level 3 ER visit. The 99283 CPT code is commonly assigned to these visits, as it reflects the expanded problem focused history, expanded problem focused examination, and medical decision ...
If the EHR gives credit for this information, physicians need to recognize that the E/M level may be inflated, and they should override the code manually, she says. CPT code Description 2018 national average Medicare Payment. 99203. Level 3 office visit. New patient. $109.80. 99204. Level 4 office visit. New patient. $167.40. 99213. Level 3 ...
MDLIVE. Emergency Departments (ED's or ER's) are categorized into five levels of care. Level I is the highest level and must have immediately available surgical specialists and sub-specialists (surgeons, neurosurgeons, orthopedic surgeons, anesthesiologists, plastic surgeons) in order to handle the most severe and complicated injuries.
99283 (G0382) Emergency department visit for the evaluation and management of a patient, which requires a medically appropriate history and/or examination and low medical-decision making. Any interventions from above, plus any below: Receipt if EMS/Ambulance patient. Heparin/saline lock. One Nebulizer treatment.
The ACEP facility coding model provides an easy to use methodology for assigning visit levels in an Emergency Department (ED). There are three columns in the guidelines. The far left column indicates the facility codes and corresponding APC levels which are justified by the "Possible Interventions" listed in the middle column.
Date. Updates. 1/7/2021. Coding & Billing Guideline created. 9/22/2021. Updated format. 11/21/2022. Removed references to level of history and examination as these references will be deleted 1/1/2023 and only the level of medical decision-making will be used when selecting the appropriate code and added information about time not being a descriptive component for the emergency department ...
The codes have not changed, but the code descriptors have been revised. In November 2019, CMS adopted the AMA's revisions to the Evaluation and Management (E/M) office visit CPT codes (99201-99215), code descriptors, and documentation standards. The revised CPT guidelines for office/outpatient E/M codes went into effect on January 1, 2021
This level of care is located "in the middle' of the coding spectrum for office visits with established patients. The 99213 is the second most popular choice for internists who selected this level of care for 29.31% of these encounters in 2020. The 2022 Medicare allowable reimbursement for this level of care is $92.47.
HCPCS Code for Level 3 hospital emergency department visit provided in a type B emergency department; (the ED must meet at least one of the following requirements: (1) it is licensed by the state in which it is located under applicable state law as an emergency room or emergency department; (2) it is held out to the public (by name, posted signs, advertising, or other means) as a place that ...
Visit level * Established patient visit New patient visit; Level 2: 99212 10-19 minutes: 99202 15-29 minutes: Level 3: 99213 20-29 minutes: 99203 30-44 minutes: Level 4: 99214 30-39 minutes:
For established patients coming in with a new problem, these level of service is likely a level 3 (99213) or level 4 (99214). The final level for this patient will depend on the diagnosis and treatment performed during the service. Code 99215 is used to report High MDM. 99215 is reserved for those patients who require extensive workup regarding ...
the visit at a level of complexity based on time spent with the patient and/ or medical decision making on behalf of the patient. That code, in turn, affects the amount paid to the provider for the visit. ... by Complexity Level, Commercial 1/2 3 4 5 Figure 3 Percentage of Visits by Complexity Level, Medicare Advantage 1/2 3 4 5 0% 25% 50% 75% 100%
CPT® code 99213: Established patient office or other outpatient visit, 20-29 minutes. As the authority on the CPT® code set, the AMA is providing the top-searched codes to help remove obstacles and burdens that interfere with patient care. These codes, among the rest of the CPT code set, are clinically valid and updated on a regular basis to ...
Level 2 new office visit 99202 E/M coding. E/M Coding and Documentation Education. Online CEU, e/m courses, web based e&m compliance solutions ... in 2020. The 2022 Medicare allowable reimbursement for this visit is $113.75. Effective January 1, 2021, this level of care requires low complexity MDM or a total of 30 - 44 minutes devoted to the ...
But often it can be an even shorter process. These two questions can guide you through the coding of many visits: 1. Did you spend 30 minutes (for an established patient) or more of total time on ...
The new HCPCS code G0463 is an alternative to all clinic visits for new and established patients when billed to Medicare carriers. G0463 is effective from January 1, 2014, in the place of Clinic visits codes (99201-99215). The hospital requires to place only one G code instead of CPT (99201-99215) when billed to Medicare insurances.
HCPCS Code G0382. Level 3 hospital emergency department visit provided in a type b emergency department; (the ed must meet at least one of the following requirements: (1) it is licensed by the state in which it is located under applicable state law as an emergency room or emergency department; (2) it is held out to the public (by name, posted signs, advertising, or other means) as a place that ...
The new rules should make it easier to avoid under-coding level 4 visits — a common and costly mistake. In fact, most level 4 visits can now be identified by asking just three questions: 1. Was ...
Overview. Our mission is to assist Pennsylvanians in leading safe, healthy, and productive lives through equitable, trauma-informed, and outcome-focused services while being an accountable steward of commonwealth resources.
Summary. To summarize, here are the three common reasons to code a level 5 office visit: Total time. ≥ 40 minutes for established patients; ≥ 60 minutes for new patients. Pre-op visit. Major ...