- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support

Outpatient Therapy: What It Is and Is It Effective?
Dr. Amy Marschall is an autistic clinical psychologist with ADHD, working with children and adolescents who also identify with these neurotypes among others. She is certified in TF-CBT and telemental health.
:max_bytes(150000):strip_icc():format(webp)/HeadShot2-0e5cbea92b2948a1a2013271d90c2d1f.jpg)
Dr. Sabrina Romanoff, PsyD, is a licensed clinical psychologist and a professor at Yeshiva University’s clinical psychology doctoral program.
:max_bytes(150000):strip_icc():format(webp)/SabrinaRomanoffPhoto2-7320d6c6ffcc48ba87e1bad8cae3f79b.jpg)
Alihan Usullu / Getty Images
What Outpatient Therapy Can Help With
- Effectiveness
Things to Consider
How to get started.
Outpatient therapy is defined as any psychotherapy service offered when the client is not admitted to a hospital, residential program, or other inpatient settings. Outpatient therapy is a resource for individuals seeking support for mental health concerns who do not require round-the-clock support or safety monitoring.
Outpatient therapy can be offered through hospitals, in doctor’s offices that employ therapists, group practices, or private practice.
Psychologists, clinical social workers, counselors, and certain medical professionals can offer outpatient therapy . Interns and students working towards degrees or licensure in mental health may also offer outpatient therapy with supervision and oversight from a qualified, licensed professional.
Get Help Now
We've tried, tested, and written unbiased reviews of the best online therapy programs including Talkspace, BetterHelp, and ReGain. Find out which option is the best for you.
Press Play for Advice On What to Do When Therapy Isn't Enough
Hosted by therapist Amy Morin, LCSW, this episode of The Verywell Mind Podcast , featuring life coach Mike Bayer, shares other treatment options if you find that therapy isn't enough. Click below to listen now.
Follow Now : Apple Podcasts / Spotify / Google Podcasts / Amazon Music
Types of Outpatient Therapy
Outpatient therapy can take many forms , depending on the client’s needs. Individual therapy, group therapy , family therapy, and couple’s therapy can all be provided in an outpatient setting. Sessions can range in frequency, including weekly, twice per week, every other week, and monthly, depending on the individual client’s need and progress in treatment.
Therapists offering outpatient services can practice from many different theoretical orientations depending on the therapist’s personal style and training background. Most orientations taught in clinical and counseling programs can be implemented in an outpatient setting, including:
- Adlerian therapy : A brief therapy approach that emphasizes setting and achieving specific goals, as well as psychoeducation about mental health.
- Behavioral therapy : A form of therapy aimed at changing problem behaviors by reinforcing preferred behaviors.
- Cognitive therapy : A typically short-term therapy approach that explores how one’s thoughts affect feelings and behaviors.
- Cognitive-behavioral therapy : A form of therapy aimed at helping individuals identify the connection between maladaptive thoughts, behaviors, and emotions and make positive changes to these patterns.
- Humanistic therapy : An approach to mental health that helps clients identify their “true self” and determine how to live their most authentic life.
- Psychoanalysis : A long-term talk therapy approach that involves exploring how one’s unconscious mind impacts thoughts, feelings, and behaviors.
- Psychodynamic therapy : A long-term therapy approach involving deep exploration and understanding of emotions and thoughts through talk therapy.
- Strengths-based therapy : An approach to therapy that emphasizes clients’ already existing strengths and helps the client identify and use these strengths in their life.
Techniques of Outpatient Therapy
Therapy techniques will vary based on the therapist’s theoretical orientation as well as the client’s individual needs. All orientations include talk therapy , which helps the client articulate their needs and treatment goals and allows the therapist to determine which interventions might be most helpful.
Because outpatient therapy consists of sessions with time in between, many outpatient therapists will assign homework in between sessions. Assignments might include tracking thoughts and emotions, mindfulness or meditation exercises, or trying different communication styles or conflict resolutions.
Because outpatient therapists have the flexibility to pull from a variety of theoretical orientations and techniques, outpatient therapy can help with a wide variety of mental health concerns.
Therapists can use outpatient therapy to help with many diagnoses, including depression , anxiety , trauma , and stress .
Benefits of Outpatient Therapy
Therapy in an outpatient setting allows clients to schedule sessions based on their availability, and they can choose frequency and treatment goals based on their needs and priorities.
Outpatient therapy allows anyone to seek therapy services and support for their mental health while allowing them to live their lives in between sessions. Many clients can continue to work or go to school while receiving outpatient therapy services.
Since many different types of outpatient therapy exist, clients can find a therapist who meets their individual needs and preferences. Outpatient therapy can also be conducted via telehealth , so clients living in rural areas do not have to travel to receive services.
Effectiveness of Outpatient Therapy
“Outpatient therapy” can refer to many different techniques and therapy approaches, which vary in their empirical support and evidence-based data about effectiveness. However, outpatient therapy can reduce an individual’s risk for needing a psychiatric hospitalization or inpatient mental health services.
Research has shown that various outpatient services can provide symptom relief for diagnoses from depression and anxiety to borderline personality disorder . In addition, outpatient therapy is an important resource and support for clients following discharge from the hospital, including improving treatment outcomes and reducing the need for additional hospitalizations.
If you are struggling with your mental health but are able to live independently, outpatient therapy might be a good resource for you.
Individuals who require ongoing therapeutic support, need to be seen daily, or who are unable to live independently may require residential or inpatient treatment. If you experience active suicidal ideation , you might need a higher level of care to ensure your safety.
When exploring options for outpatient therapy, contact your insurance company to get information about your coverage and what therapy services might cost you. You can also talk to your employer about whether you have an Employee Assistance Program that provides a limited number of free sessions.
If you are having suicidal thoughts, contact the National Suicide Prevention Lifeline at 988 for support and assistance from a trained counselor. If you or a loved one are in immediate danger, call 911.
For more mental health resources, see our National Helpline Database .
If you feel like you would benefit from outpatient therapy, you can find a therapist whose training and style fit your needs and preferences.
Your first therapy session will likely include providing information about your personal history, family history, and symptoms. When you first start therapy , it can take time to build trust and rapport with your therapist, and you might find yourself exploring emotions you had not previously addressed. You may also have to try out more than one therapist before you find a provider who is a good fit.
You and your therapist will work together to develop a treatment plan and goals that fit your needs and address your specific symptoms. Starting outpatient therapy can be stressful, but it allows you to continue living your life while you receive support for your mental health needs.
Eskildsen A, Reinholt N, van Bronswijk S, et al. Personalized psychotherapy for outpatients with major depression and anxiety disorders: transdiagnostic versus diagnosis-specific group cognitive behavioural therapy. Cogn Ther Res . 2020;44(5):988-1001.
Ellison WD, Levy KN, Newman MG, Pincus AL, Wilson SJ, Molenaar PCM. Dynamics among borderline personality and anxiety features in psychotherapy outpatients: An exploration of nomothetic and idiographic patterns. Personality Disorders: Theory, Research, and Treatment . 2020;11(2):131-140.
Teixeira C, Rosa RG. Post-intensive care outpatient clinic: is it feasible and effective? A literature review. Revista Brasileira de Terapia Intensiva . 2018;30(1).
By Amy Marschall, PsyD Dr. Amy Marschall is an autistic clinical psychologist with ADHD, working with children and adolescents who also identify with these neurotypes among others. She is certified in TF-CBT and telemental health.
Mental Health-Related Outpatient Visits Among Adolescents and Young Adults, 2006-2019
Affiliations.
- 1 Department of Psychiatry, Massachusetts General Hospital, Boston.
- 2 Department of Psychiatry, McLean Hospital, Belmont, Massachusetts.
- 3 Department of Psychiatry, Harvard Medical School, Boston, Massachusetts.
- 4 Computational Health Informatics Program, Boston Children's Hospital, Boston, Massachusetts.
- 5 Department of Pediatrics, Harvard Medical School, Boston, Massachusetts.
- PMID: 38451523
- PMCID: PMC10921253
- DOI: 10.1001/jamanetworkopen.2024.1468
Importance: Concerns over the mental health of young people have been increasing over the past decade, especially with the rise in mental health burden seen during the COVID-19 pandemic. Examining trends in mental health-related outpatient visits provides critical information to elucidate contributing factors, identify vulnerable populations, and inform strategies to address the mental health crisis.
Objective: To examine characteristics and trends in mental health-related outpatient visits and psychotropic medication use among US adolescents and young adults.
Design, setting, and participants: A retrospective cross-sectional analysis of nationally representative data from the National Ambulatory Medical Care Survey, an annual probability sample survey, was conducted from January 2006 to December 2019. Participants included adolescents (age 12-17 years) and young adults (age 18-24 years) with office-based outpatient visits in the US. Data were analyzed from March 1, 2023, to September 15, 2023.
Main outcomes and measures: Mental health-related outpatient visits were identified based on established sets of diagnostic codes for psychiatric disorders. Temporal trends in the annual proportion of mental health-related outpatient visits were assessed, including visits associated with use of psychotropic medications. Analyses were stratified by age and sex.
Results: From 2006 to 2019, there were an estimated 1.1 billion outpatient visits by adolescents and young adults, of which 145.0 million (13.1%) were associated with a mental health condition (mean [SD] age, 18.4 [3.5] years; 74.0 million females [51.0%]). Mental health-related diagnoses were more prevalent among visits by male (16.8%) compared with female (10.9%) patients (P < .001). This difference was most pronounced among young adults, with 20.1% of visits associated with a psychiatric diagnosis among males vs 10.1% among females (P < .001). The proportion of mental health-related visits nearly doubled, from 8.9% in 2006 to 16.9% in 2019 (P < .001). Among all outpatient visits, 17.2% were associated with the prescription of at least 1 psychotropic medication, with significant increases from 12.8% to 22.4% by 2019 (P < .001).
Conclusions and relevance: In this cross-sectional study, there were substantial increases in mental health-related outpatient visits and use of psychotropic medications, with greater overall burden among male patients. These findings provide a baseline for understanding post-pandemic shifts and suggest that current treatment and prevention strategies will need to address preexisting psychiatric needs in addition to the effects of the COVID-19 pandemic.
- COVID-19* / epidemiology
- Cross-Sectional Studies
- Mental Health*
- Outpatients
- Retrospective Studies
- Young Adult
Routine Psychiatric Assessment
- Mental Status Examination |
- More Information |
Patients with mental complaints or concerns or disordered behavior present in a variety of clinical settings, including primary care and emergency treatment centers. Complaints or concerns may be new or a continuation of a history of mental problems. Complaints may be related to coping with a physical condition or be the direct effects of a physical condition on the central nervous system. The method of assessment depends on whether the complaints constitute an emergency or are reported in a scheduled visit. In an emergency, a physician may have to focus on more immediate history, symptoms, and behavior to be able to make a management decision. In a scheduled visit, a more thorough assessment is appropriate.
Routine psychiatric assessment includes a general medical and psychiatric history and a mental status examination. (See also the American Psychiatric Association’s Psychiatric Evaluation of Adults Quick Reference Guide, 3rd Edition and American Psychiatric Association : Practice guideline for the psychiatric evaluation of adults.)
The physician must determine whether the patient can provide a history, ie, whether the patient readily and coherently responds to initial questions. If not, information is sought from family, caregivers, or other collateral sources (eg, police). Even when a patient is communicative, close family members, friends, or caseworkers may provide information that the patient has omitted. Receiving information that is not solicited by the physician does not violate patient confidentiality. Previous psychiatric assessments, treatments, and degree of adherence to past treatments are reviewed, and records from such care are obtained as soon as possible.
Conducting an interview hastily and indifferently with closed-ended queries (following a rigid system review) often prevents patients from revealing relevant information. Tracing the history of the presenting illness with open-ended questions, so that patients can tell their story in their own words, takes a similar amount of time and enables patients to describe associated social circumstances and reveal emotional reactions.
The interview should first explore what prompted the need (or desire) for psychiatric assessment (eg, unwanted or unpleasant thoughts, undesirable behavior), including how much the presenting symptoms affect the patient or interfere with the patient's social, occupational, and interpersonal functioning. The interviewer then attempts to gain a broader perspective on the patient’s personality by reviewing significant life events—current and past—and the patient’s responses to them (see table Areas to Cover in the Initial Psychiatric Assessment ). Psychiatric, medical, social, and developmental histories are also reviewed.
A review of systems to check for other symptoms not described in the psychiatric history is important. Focusing only on the presenting symptoms to the exclusion of past history and other symptoms may result in making an incorrect primary diagnosis (and thus recommending the wrong treatment) and missing other psychiatric or medical comorbidities. For example, not asking about past manic episodes in a patient presenting with depression could result in making an incorrect diagnosis of major depressive disorder instead of bipolar disorder. Review of systems and past medical history should include questions about new or recent physical symptoms, diagnoses, and current drugs and treatments to identify potential physical causes of mental symptoms (eg, COVID-19 as a possible cause of anxiety or depression).
The personality profile that emerges may suggest traits that are adaptive (eg, openness to experience, conscientiousness) or maladaptive (eg, self-centeredness, dependency, poor tolerance of frustration) and may show the coping mechanisms used. The interview may reveal obsessions (unwanted and distressing thoughts or impulses), compulsions (excessive, repetitive, purposeful behaviors that a person feels driven to do), and delusions (fixed false beliefs that are firmly held despite evidence to the contrary) and may determine whether distress is expressed in physical symptoms (eg, headache, abdominal pain), mental symptoms (eg, phobic behavior, depression), or social behavior (eg, withdrawal, rebelliousness). The patient should also be asked about attitudes regarding psychiatric treatments, including drugs and psychotherapy, so that this information can be incorporated into the treatment plan.
The interviewer should establish whether a physical condition or its treatment is causing or worsening a mental condition (see Medical Assessment of the Patient With Mental Symptoms ). In addition to having direct effects (eg, symptoms, including mental ones), many physical conditions cause enormous stress and require coping mechanisms to withstand the pressures related to the condition. Many patients with severe physical conditions experience some kind of adjustment disorder, and those with underlying mental disorders may become unstable.
Observation during an interview may provide evidence of mental or physical disorders. Body language may reveal evidence of attitudes and feelings denied by the patient. For example, does the patient fidget or pace back and forth despite denying anxiety? Does the patient seem sad despite denying feelings of depression? General appearance may provide clues as well. For example, is the patient clean and well-kept? Is a tremor or facial droop present?
Mental Status Examination
A mental status examination uses observation and questions to evaluate several domains of mental function, including
Emotional expression
Thinking and perception
Cognitive functions
Brief standardized screening questionnaires are available for assessing certain components of the mental status examination, including those specifically designed to assess orientation and memory. Such standardized assessments can be used during a routine office visit to help screen patients; such screening can help identify the most important symptoms and provide a baseline for measuring response to treatment. However, screening questionnaires cannot take the place of a broader, more detailed mental status examination .
General appearance should be assessed for unspoken clues to underlying conditions. For example, patients’ appearance can help determine whether they
Are unable to care for themselves (eg, they appear undernourished, disheveled, or dressed inappropriately for the weather or have significant body odor)
Are unable or unwilling to comply with social norms (eg, they are garbed in socially inappropriate clothing)
Have engaged in substance use or attempted self-harm (eg, they have an odor of alcohol, scars suggesting IV drug abuse or self-inflicted injury)
Speech can be assessed by noting spontaneity, syntax, rate, and volume. A patient with depression may speak slowly and softly, whereas a patient with mania may speak rapidly and loudly. Abnormalities such as dysarthrias and aphasias may indicate a physical cause of mental status changes, such as head injury, stroke, brain tumor, or multiple sclerosis.
Emotional expression can be assessed by asking patients to describe their feelings. The patient’s tone of voice, posture, hand gestures, and facial expressions are all considered. Mood (emotional state reported by the patient) and affect (patient's expression of emotional state as observed by the interviewer) should be assessed. Affect and its range (ie, full vs constricted) should be noted as well as the appropriateness of affect to thought content (eg, patient smiling while discussing a tragic event).
Thinking and perception can be assessed by noticing not only what is communicated but also how it is communicated. Abnormal content may take the form of the following:
Delusions (false, fixed beliefs)
Ideas of reference (notions that everyday occurrences have special meaning or significance personally intended for or directed to the patient)
Obsessions (recurrent, persistent, unwanted, and intrusive thoughts, urges, or images)
The physician can assess whether ideas seem to be linked and goal-directed and whether transitions from one thought to the next are logical. Psychotic or manic patients may have disorganized thoughts or an abrupt flight of ideas.
Cognitive functions include the patient’s
Level of alertness
Attentiveness or concentration
Orientation to person, place, and time
Immediate, short-term, and long-term memory
Abstract reasoning
Abnormalities of cognition most often occur with delirium or dementia or with substance intoxication or withdrawal but can also occur with depression .
More Information
The following is an English-language resource that may be useful. Please note that THE MANUAL is not responsible for the content of this resource.
American Psychiatric Association : Practice guideline for the psychiatric evaluation of adults

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
- Cookie Preferences

- Conclusions
- Article Information
The period 2007-2009 is prior to implementation of the Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act (MHPAEA), 2010-2013 is the period after implementation of MHPAEA but prior to implementation of the Affordable Care Act (ACA), and 2014-2016 is the period after implementation of many provisions of the ACA. The MHPAEA “prevents group health plans and health insurance issuers that provide mental health or substance use disorder (MH/SUD) benefits from imposing less favorable benefit limitations on those benefits than on medical/surgical benefits.” 4 The ACA requires “that most individual and small employer health insurance plans, including all plans offered through the Health Insurance Marketplace, cover mental health and substance use disorder services.” 5 Pursuant to ACA implementation, 15% of Americans had no insurance in 2013, vs 9% in 2015. 2 If psychiatrists accepted insurance, increased insurance coverage should reduce the percentage of patients who self-pay and the percentage of psychiatrists predominantly paid by patients directly for office-based psychiatric care. Visit-level analysis uses visit-level weights and is based on response of yes to the statement “expected source of payment: self” by the clinician. Physician-level analysis uses clinician-level weights. Metrics are based on a response of “more than 75%” to the question “Roughly what percent of your patient care revenue comes from patient payments?”
See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
Benjenk I , Chen J. Trends in Self-payment for Outpatient Psychiatrist Visits. JAMA Psychiatry. 2020;77(12):1305–1307. doi:10.1001/jamapsychiatry.2020.2072
Manage citations:
© 2024
- Permissions
Trends in Self-payment for Outpatient Psychiatrist Visits
- 1 University of Maryland School of Public Health, College Park
Even though insurance coverage for mental health has greatly improved over the last 10 years in the US, 1 , 2 many patients continue to struggle to find psychiatrists willing to accept their insurance and need to pay upfront for their psychiatrist visits. 3 This is a hurdle that many patients cannot surmount, even if a portion of that payment is eventually paid by insurance. This study aimed to explore patterns in self-payment for office-based psychiatric services and changes over time, particularly with the passage of the Mental Health Parity and Addiction Equity Act and the Affordable Care Act. 4 , 5
This study used 10 years of data (January 2007 through December 2016) from the National Ambulatory Medical Care Survey (NAMCS), 6 which is a random sample of outpatient visits made to a nationally representative random sample of physicians who are nonfederally employed, younger than 85 years, and treating outpatients. Patients seen in hospital units, nursing homes or other extended care institutions, or the patient's home were not included. This dataset also does not include telephone visits. Of note, prior to 2012, the NAMCS included community health centers in their primary sampling frame. Starting in 2012, these were sampled separately. As a result, they are excluded from this analysis.
The study accounted for complex survey design to describe the characteristics of patients who self-paid (submitting either self-payment or upfront payment that the patient later submitted to their insurance for at least partial reimbursement) and clinicians who were reimbursed predominantly (>75%) by self-payment for office-based visits. We also compared payment trends for psychiatrist visits with payment trends for primary care clinician visits using logistic regression with group by time interaction. The NAMCS has a waiver of consent from the National Center for Health Statistics’ Research Ethics Review Board because it used secondary data and posed minimal risk to participants. Institutional review board approval was waived because the NAMCS data set is publicly available. Data analysis was completed from December 2019 to February 2020 with StataIC version 15 (StataCorp), with a significance threshold set at a 2-tailed P < .05.
After we excluded visits to community health centers, there were 16 464 psychiatrist visits in the sample (mean [SE], 20.1 [13.7] visits per psychiatrist), of which 15 790 had expected source of payment information. There were 127 500 primary care visits in the sample (mean [SE], 26.4 [13.4] visits per primary care clinician), of which 119 749 had expected source of payment information. There were 816 psychiatrists in the sample and 750 with information on predominant source of revenue. There were 4842 primary care physicians in the sample and 4294 with information on the predominant source of revenue.
Of the psychiatrist visits, 3445 (21.8%; weighted, 22.0%) were self-paid by patients, compared with 4336 primary care clinician visits (3.6%; weighted, 3.6%). One hundred forty-six psychiatrists (19.5%; weighted, 23.5%) were reimbursed predominantly by self-payment, compared with 69 primary care clinicians (1.6%; weighted, 1.7%).
As shown in the Figure , the percentage of visits to psychiatrists that patients self-paid has trended upward (from 18.5% in 2007-2009 to 26.7% in 2014-2016), while the percentage of visits to primary care clinicians that patients self-paid has trended downward (from 4.1% in 2007-2009 to 2.8% in 2014-2016). The percentage of psychiatrists who work in predominantly self-pay practices has trended upward (from 16.4% in 2007-2009 to 26.4% in 2014-2016), while the percentage of primary care clinicians who work in predominantly self-pay practices has not changed significantly (from 1.5% to 1.7%).
At the visit level, we found that self-payment for psychiatrist visits was significantly more common among white patients (white patients, 3082 of 12 732 [24.2%; weighted, 24.2%]; black patients, 97 of 1191 [8.1%; weighted, 9.7%]; Hispanic patients, 173 of 1193 [14.5%; weighted, 12.2%]; P < .001) and male patients (1587 of 6952 men [22.8%; weighted, 24.5%]; 1858 of 8838 women [21.0%; weighted, 20.2%]; P < .001) and not significantly different across age groups (<18 years, 353 of 2318 individuals [15.2%; weighted, 16.8%]; 18-64 years, 2765 of 11 832 individuals [23.4%; weighted, 23.5%]; >64 years, 327 of 1640 individuals [19.9%; weighted, 19.3%]; P = .08). Self-paid visits were a mean (SE) of 38.3 (1.1) minutes in duration, as opposed to 28.8 (0.7) minutes for visits paid directly by third parties ( P < .001). Patients who were self-paying had a mean (SE) of 18.3 (2.1) visits in the 12 months prior to the current visit compared with 9.4 (0.6) visits for patients with third-party payers ( P < .001).
We found that psychiatrists who are reimbursed predominantly by self-payment were more likely to work in solo practices (mean [SE], 30.5% [2.8%]) than group practices (8.3% [2.3%]; P < .001) and were less likely to care predominantly for pediatric patients (mean [SE], 6.6% [4.3%]) than adult patients (25.4% [2.3%]; P = .01). Compared with those receiving fewer self-payments, psychiatrists reimbursed predominantly by self-payments saw fewer total office-based outpatients per week (mean [SE], 21.0 [0.8] visits vs 15.0 [1.2] visits; P < .001), had a greater mean percentage of white patients (mean [SE], 77.6% [0.1%] vs 87.3% [1.8%]; P < .001), had longer mean appointment times (mean [SE] minutes, 31.6 [0.7] vs 40.5 [1.6]; P < .001), and saw patients more frequently (mean [SE] visits per patient in the last 12 months, 10.3 [0.7] vs 20.4 [2.2]; P < .001) ( Table ).
Despite the small sample of psychiatrists in the NAMCS and the associational design of this study, this study appears to find that many patients continue to self-pay for psychiatrist visits and many psychiatrists continue to only care for patients that can self-pay. Psychiatrists may be more likely to rely on self-payment models than other specialties because of low insurance reimbursement rates, particularly for psychotherapy, as well as a demand for psychiatric services that outstrips supply. Our findings begin to highlight a 2-tiered system for outpatient psychiatrist care, which presents potential issues of health equity. Patients who choose to or must rely on third-party payment for psychiatrist appointments may be receiving only psychopharmacology, while those who can self-pay may be able to receive psychotherapy as well.
Accepted for Publication: May 12, 2020.
Corresponding Author: Ivy Benjenk, BSN, MPH, University of Maryland School of Public Health, 4200 Valley Dr, School of Public Health Building, Ste 2242, Room 3310, College Park, MD 20742 ( [email protected] ).
Published Online: July 15, 2020. doi:10.1001/jamapsychiatry.2020.2072
Author Contributions: Ms Benjenk had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: All authors.
Acquisition, analysis, or interpretation of data: Benjenk.
Drafting of the manuscript: Benjenk.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Benjenk.
Obtained funding: Chen.
Administrative, technical, or material support: Chen.
Supervision: Chen.
Conflict of Interest Disclosures: None reported.
Funding/Support: Dr Chen is supported by grants from the National Institute on Minority Health and Health Disparities (R01MD011523) and the National Institute on Aging (1R56AG062315-01).
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts

Inpatient vs. Outpatient Services
At Seven Counties Services, we offer both inpatient and outpatient services. The main difference between these services is if a patient will need to stay overnight at one of our facilities to receive the care they need.
Inpatient
Inpatient care is provided in a facility where you stay overnight, sometimes for several nights, depending on your health condition and needs. During your stay, our dedicated healthcare professionals will be by your side, providing necessary medicine, care, monitoring, and medical treatment. When your doctor decides you are ready for discharge, you will receive comprehensive instructions, including follow-up with your doctor, medication management, and the possibility of receiving outpatient services if needed.
Outpatient
Outpatient care is a service you receive that you don’t have to stay overnight. The benefits of receiving outpatient care are the flexibility and freedom of scheduling appointments, virtual options, and the ability to continue with daily life while receiving treatment. Some examples of services include:
- Mental health services
- Substance use treatment
- Physical therapy
- Appointments and consultations
- Emergency care that doesn’t require hospitalization
- Bloodwork and lab tests
- Attending group or peer support meetings
Support Through Seven Counties Services
Inpatient and outpatient programs, although different from one another, provide effective treatment and ensure you receive the level of care you need. If you or a loved one are facing challenges with mental or behavioral health concerns, Seven Counties Services is here to help. We offer both inpatient and outpatient services for children and adults. Visit sevencounties.org to request an appointment online or call (502) 589-1100.
Reviewed by Kayti Michel LPCC-S, Unit Manager, at Seven Counties Services.
Blog Professional Training Institute Regional Prevention Center Frequently Asked Questions Glossary Trustworthy Sites
Schedule Appointment
Seven Counties Services serves everyone regardless of diagnosis or insurance status. We ensure that getting started on your journey to recovery is as easy as possible. To schedule your first appointment, you can call directly or complete an online appointment request.
Helpful Resources
Educating individuals, parents, caregivers, and the community through specialized content provided by industry-leading experts.
Get Started
Mental Health Substance Use Developmental Schedule Appointment Make a Referral
Quick Links
Patient Portal Pay Bill Online Careers Locations Media Center Contact

Seven Counties Services Newsletter
Funding is in whole or in part from federal, Cabinet for Health and Family Services, or other state and local funds.

- Research article
- Open access
- Published: 20 November 2021
Adolescent psychiatric outpatient care rapidly switched to remote visits during the COVID-19 pandemic
- Emma M. Savilahti ORCID: orcid.org/0000-0001-5419-0485 1 ,
- Sakari Lintula 1 ,
- Laura Häkkinen 1 ,
- Mauri Marttunen 1 , 2 &
- Niklas Granö 1
BMC Psychiatry volume 21 , Article number: 586 ( 2021 ) Cite this article
1209 Accesses
6 Citations
Metrics details
The COVID-19-pandemic and especially the physical distancing measures drastically changed the conditions for providing outpatient care in adolescent psychiatry.
We investigated the outpatient services of adolescent psychiatry in the Helsinki University Hospital (HUH) from 1/1/2015 until 12/31/2020. We retrieved data from the in-house data software on the number of visits in total and categorized as in-person or remote visits, and analysed the data on a weekly basis. We further analysed these variables grouped according to the psychiatric diagnoses coded for visits. Data on the number of patients and on referrals from other health care providers were available on a monthly basis. We investigated the data descriptively and with a time-series analysis comparing the pre-pandemic period to the period of the COVID-19 pandemic.
The total number of visits decreased slightly at the early stage of the COVID-19 pandemic in Spring 2020. Remote visits sharply increased starting in 3/2020 and remained at a high level compared with previous years. In-person visits decreased in Spring 2020, but gradually increased afterwards. The number of patients transiently fell in Spring 2020.
Conclusions
Rapid switch to remote visits in outpatient care of adolescent psychiatry made it possible to avoid a drastic drop in the number of visits despite the physical distancing measures during the COVID-19 pandemic.
Peer Review reports
World Health Organization (WHO) declared on 3/11/2020 that the SARS-CoV-2 virus, which causes COVID-19, had spread to a pandemic. The pandemic with the ensuing physical distancing measures has drastically impacted social life, economic circumstances and personal freedom. Adolescents are especially vulnerable to the disruptions given their dependence on their care-givers and their developmental tasks that may be severed by lack of adequate social, emotional and educational stimuli and support [ 1 , 2 ]. Research on mental health during the pandemic was first published predominantly on adult populations, but data on children and adolescents have begun to emerge. Few studies have, however, reported on how adolescent psychiatric services have adapted to the unprecedented circumstances.
Numerous studies based on self-assessment surveys have reported signs of poor mental health in adult general populations during the first wave of the COVID-19 pandemic [ 3 , 4 ]. In contrast, a Dutch longitudinal study observed no significant increase in depressive and anxiety symptoms in 3/2020 compared with 11/2019, but did find a slight decrease in symptoms in 6/2020 compared with both previous time points [ 5 ].
Although studies on mental health of children and adolescents during the COVID-19 pandemic are far fewer than on adult populations, they have reported nuanced observations. A German nationwide survey of 7–17-year olds showed that compared to pre-pandemic results from another nationwide cohort study, subjects had more mental health problems than before the pandemic based on both their own and their parents’ reporting [ 6 ]. Two studies from the USA observed that mental health symptoms in adolescents increased in Spring 2020 during the first wave of the pandemic and then subsided towards the Summer, when the pandemic and ensuing restrictions eased [ 7 , 8 ]. In a Canadian study on both community and psychiatric clinical populations, the majority (70%) of parents reported in 4–6/2020 that the mental health of their 6–18 year old child had deteriorated with stress related to social isolation, whereas 20% of parents reported improvement in their child’s mental health [ 9 ].
Mental health services are challenged during the pandemic by physical distancing measures as well as potential changes in demand. In contrast to the reports that mental health indicators have deteriorated at the onset of the COVID-19 pandemic, studies on mental health care have observed sharp decreases in demand of services [ 10 , 11 , 12 ]. Psychiatric emergency visits in the early stage of the pandemic (Spring 2020) were fewer than before the pandemic according to seven studies recently reviewed [ 11 ] and in a study on children and adolescents (under 18 years of age) with data from ten countries [ 12 ]. In a French study on adults, the proportion of referrals due to psychosis and on involuntary basis increased, whereas visits due to anxiety disorders and first psychiatric contacts were lower than in 3–4/2019 [ 13 ]. In primary health care in the UK in 4/2020, the incidence of depression and anxiety disorders had reduced by nearly half, and the rate of referral to mental health services was less than a quarter compared with expected rates based on data from previous 10 years [ 10 ]. By 9/2020, however, the incidence of several mental health problems had increased to expected levels in England, while elsewhere in the UK rates remained around a third lower than expected [ 10 ]. In secondary mental health care services the overall number of registered patients decreased from 4/2020 to 9/2020 compared with pre-pandemic period, whereas the number of underaged patients slightly increased [ 14 ]. The total number of clinical contacts for underaged patients in Spring 2020 reduced less than for adults, and while in-person visits decreased, remote visits increased [ 14 ].
Our aim was to investigate how adolescent outpatient psychiatric care in Helsinki University Hospital has changed during the pandemic from its onset until the end of year 2020 compared with previous 5 years. We are aware of only one previous study reporting on adolescent outpatient psychiatric care during the pandemic [ 14 ], and no previous studies have, to our knowledge, investigated whether changes in adolescent outpatient psychiatric care differed between diagnostic groups. The extant research on mental health during the COVID-19 pandemic provides discordant basis for hypotheses: psychiatric symptoms increased, whereas visits to health care services for psychiatric reasons decreased. Firstly, we hypothesized that the overall number of outpatient visits in adolescent psychiatry dropped during the first lockdown in Spring 2020, consistent with the changes reported in the UK primary health care [ 10 ] and in psychiatric emergency visits in several countries [ 12 , 13 ]. Secondly, we expected visits to increase after Spring 2020 to attain the previous or possibly an even higher level, considering that in specialized adolescent psychiatric services most of the patients suffer from mid- to long-term problems and that other studies indicate that mental health has deteriorated in both adult [ 3 , 4 ] and underage [ 6 , 7 , 8 , 9 ] populations during the pandemic. Thirdly we further expected an increase in remote visits and a decrease in in-person visits during the pandemic especially concomitantly with the lockdown in Spring 2020. Finally, we hypothesized most changes in the number of visits to be in the diagnostic group of depressive and anxiety disorders and least in psychotic disorders due to the severity of these disorders, and based on observations from a French study [ 13 ].
In Finland, the spread of the virus started later than in many other European countries. Finnish health officials recommended physical distancing measures starting in 3/2020. The first lockdown started on 3/16/2020. Primary and secondary schools were operating remotely 3/17–5/13/2020 except for some pupils with special needs. High schools and vocational schools operated remotely from 3/17/2020 until the end of the semester (beginning of June). The second wave in Autumn/Winter 2020–2021 resulted in less severe restrictions. Primary and secondary schools did not move to remote learning, but high schools and vocational schools operated remotely from 11/30/2020 to Spring 2021.
The department of adolescent psychiatry of the Helsinki University Hospital (HUH) is responsible for the publicly funded specialized psychiatric services for 13–17-year old residents ( n = 92,677 in 2020) of the Uusimaa district (population 1.71 million in 2021) in Southern Finland. Due to the physical distancing measures nationally installed to mitigate the spread of COVID-19 in Finland, HUH adolescent psychiatry moved to supplying outpatient services predominantly remotely from 3/17/2020 onwards. After the lockdown from 3/16/2020 to 5/13/2020, remote services were still recommended except in emergency situations, but patients had a subjective right to choose in-person visits. Wearing of masks at in-person visits became mandatory in HUH clinics from 9/1/2020 onwards.
The study was approved by the research administrative board of the department of psychiatry at HUH (decision number HUS/153/2021), and conducted at the division of adolescent psychiatry, HUH, Finland. Since we did not gather or analyse any identifiable patient data, review by an ethical board was not necessary.
We investigated outpatient visits and referrals in the division of adolescent psychiatry of HUH from 1/1/2015 until 12/31/2020. We chose to retrieve the data starting on 1/1/2015 in order to have a relatively long reference period preceding the pandemic. We retrieved data from the in-house hospital data software (called HUS Total) on a daily basis on the number of visits in total as well as separately categorized as in-person visit or remote visit (phone calls and video calls over internet) and on a monthly basis on the number of persons in outpatient care.
We further analysed these variables according to the psychiatric diagnoses coded for each visit. Psychiatric diagnoses were coded in the system by clinicians according to ICD-10. For analyses, we combined diagnoses into the following broad four groups: 1) psychotic disorders (F20-F29), 2) depressive and anxiety disorders (“neurotic” F32, F33, F40–48, F93.0, F93.1, F93.2, F93.80, F93.9), 3) ADHD and conduct disorders (F90, F91, F92), and 4) all other psychiatric diagnoses not included in the previous categories. Primary, severe eating disorders in HUH are treated in a specialized unit affiliated to adult psychiatry, and are thus not in the data on adolescent psychiatric outpatient care. Eating disorders in our data are included in the category of other diagnoses. We aggregated the daily data to weekly time series data.
Data on referrals to adolescent psychiatric out-patient care from other health care providers (mostly from primary health care) were available on a monthly basis. The data on referrals did not include referrals or visits to emergency services.
Based on the public statements and regulations of the Finnish government and health care authorities, we defined the start of the COVID-19 pandemic period with widely implemented physical distancing measures at 3/16/2020 and the lockdown period 3/16/2020–5/18/2020.
Data analyses
We investigated the data descriptively and with regression models and time-series analyses with emphasis on comparing the pre-pandemic period (in Finland 1/1/2015–3/15/2020) to the period of the COVID-19 pandemic (from 3/16/2020 until the end of study period 12/31/2020).
The regression analysis of our count data was done using quasi-Poisson regression to account for overdispersion. In the regression models, seasonality was accounted for using flexible cubic splines [ 15 ] (7 evenly distributed internal knots in weekly data, 5 in monthly data, and boundary knots at the first and last week/month of the year), separate dummy -variables were included to account for clearly observed overall inactivity annually during July and in the last week of every year, and possible secular trend by using an integer vector from 1 to the number of weeks/months included in the data [ 16 ].
The hypothesized immediate step-wise change of the COVID-19 lockdown period was modelled by including a dummy variable from 3/16/2020 (or 3/2020 in monthly data) to the end of the year. A separate ascending integer vectorer was included, starting from 5/18/2020 (or 5/2020 in monthly data), to model the hypothesized delayed slope-change after Spring 2020 in the variables of interest [ 15 ]. The validity of the regression models was inspected using autocorrelation functions, partial autocorrelation functions and residual plots. Two-sided significance tests and confidence intervals were calculated for the parameters of interest.
We also made counterfactual predictions based on our estimated models to demonstrate the (estimated) continuation of time series without the effects of COVID-19. All the statistical analyses were conducted using R version 4.0.3 [ 17 ].
The total number of visits showed a mild decrease in Spring 2020 (step change of − 16, 95% CI -24- -6.4%, p < 0.002), whereas later change in slope was not significant, compared with the predicted counterfactual outcome (Fig. 1 a). In-person visits decreased in Spring 2020 significantly (step change of − 73, 95% CI -77- -68%, p < 0.0001), and after the Spring a significant increase in slope was observed (change with weekly increase of 3.2, 95% CI 2.3–4.1%, p < 0.0001) (Fig. 1 b). Remote visits sharply increased starting in 3/2020 (step change of 412, 95% CI 370–460%, p < 0.0001), and after 5/2020, a significant decrease in slope was observed (weekly change of − 2.5, 95% CI -2.9- -2.1%, p < 0.0001); thus, after Summer 2020 remote visits were at a lower level than in Spring, but still at a higher level than predicted based on pre-pandemic data (Fig. 1 c). The portion of remote visits of all outpatient visits was 47% during year 2020, whereas in previous 5 years (2015–2019) it was 10–12% (Online Resource, Fig. S 1 a). Remote visits comprised predominantly of phone calls before the pandemic and at the very early stage of the pandemic (3–4/2020), when they increased significantly (step change of 201, 95% CI 179–225%, p < 0.0001), whereas video calls peaked a little later in Spring 2020 (step change of 469, 95% CI 319–697%, p < 0.0001) (Online Resource, Fig. S 1 b). Both modes of remote visits decreased after Spring 2020 (weekly change for phone calls − 2.3, 95% CI -2.7 - -1.9%, p < 0.0001, and for video calls − 2.4, 95% CI -3.9 - -0.8%, p < 0.003), but remained at a much higher level than in previous years (Online Resource, Fig. S 1 b).

Outpatient visits 2015–2020 (weekly data). a ) The total number of visits. b ) The number of in-person visits. c ) The number of remote visits. The dots denote weekly data points, the fine line denotes the fitted line and the fine dashed line denotes the predicted counterfactual line based on the model (based on data from years 2015–2019). The thick line denotes the trend over time when controlling for seasonality, and the thick dotted line denotes the counterfactual prediction when controlling for seasonality, based on previous 5 years (2015–2019). X-axis shows the time from Jan, 1, 2015 to Dec, 31, 2020, ticks denote the start of each year. Y-axis shows the number of visits
When we stratified the data according to psychiatric diagnoses coded for the visits, the results mainly conformed to the observations in the aggregate data (Fig. 2 a-d). However, in the group of psychotic disorders, the decrease in in-person visits of Spring 2020 was similar, but it was not followed by any significant change in slope unlike in other diagnostic groups (Online Resource, Fig. S 2 a-d). Changes in remote visits were similar in all diagnostic groups and consequently similar to the changes observed in the aggregate data: rapid increase in Spring 2020 and slow gradual decrease afterwards (Online Resource, Fig. S 2 d-f).
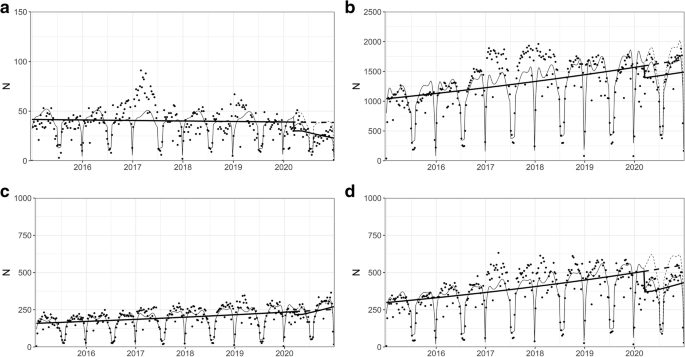
Outpatient visits 2015–2020 in different psychiatric diagnostic groups (weekly data). a ) psychotic disorders (F20–29). b ) depressive and anxiety disorders (F32, F33, F40–48, F93.0, F93.1, F93.2, F93.80, F93.9). c ) ADHD and conduct disorders (F90, F91, F92). d ) all other psychiatric diagnoses. The dots denote weekly data points, the fine line denotes the fitted line and the fine dashed line denotes the predicted counterfactual line based on the model (based on data from years 2015–2019). The thick line denotes the trend over time when controlling for seasonality, and the thick dotted line denotes the counterfactual prediction when controlling for seasonality, based on previous 5 years (2015–2019). X-axis shows the time from Jan, 1, 2015 to Dec, 31, 2020, ticks denote the start of each year. Y-axis shows the number of visits. NB. The scale of Y axes varies between figures
The number of subjects in adolescent outpatient care on a monthly basis showed a slight but significant decrease in Spring 2020 (step change of − 10, 95% CI -17- -2.9%, p < 0.01), and no significant change in slope during the rest of the year 2020 (Online Resource, Fig. S 3 ).
Referrals to HUH adolescent psychiatry outpatient clinic from other health care providers (mostly from primary health care) did not significant change in Spring 2020 compared with previous 5 years, but decreased towards the end of 2020 (weekly change of − 4.7, 95% CI -8.8- -0.5%, p = 0.03) (Fig. 3 ).
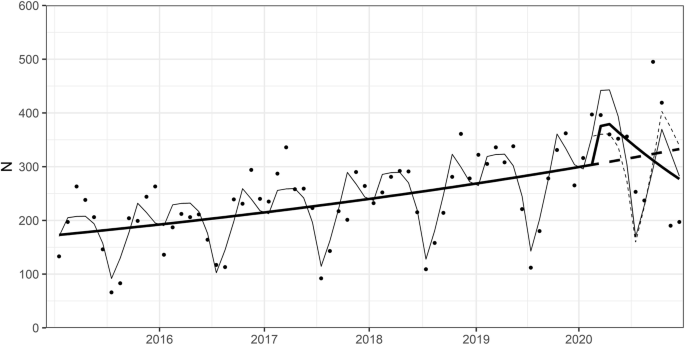
Referrals to HUH adolescent psychiatry outpatient clinic from other health care providers 2015–2020 (monthly data). The dots denote monthly data points, the fine line denotes the fitted line and the fine dashed line denotes the predicted counterfactual line based on the model (based on data from years 2015–2019). The thick line denotes the trend over time when controlling for seasonality, and the thick dotted line denotes the counterfactual prediction when controlling for seasonality, based on previous 5 years (2015–2019). X-axis shows the time from Jan, 1, 2015 to Dec, 31, 2020, ticks denote the start of each year. Y-axis shows the number of referrals
Our main finding was that the number of visits at HUH adolescent psychiatry outpatient care at the early stage of the COVID-19 pandemic only slightly decreased compared with counterfactual prediction based on previous 5 years, as rapid increase in remote visits compensated for the steep drop in in-person visits. After Spring 2020, in-person visits began to gradually increase, but the proportion of remote visits of all visits remained at a higher level than before the pandemic. In-person visits of adolescents with psychosis diagnosis did not, however, show any positive gradual change unlike those observed in the aggregate data and other diagnostic groups.
Our result that the total number of visits slightly decreased at the early stage of the pandemic supported our hypothesis, which was based on the assumption that physical distancing measures would interfere with accessing care and on studies reporting a drop in visits during Spring 2020 in primary mental health care [ 10 ] as well as in psychiatric emergency visits in adults [ 11 ] and in underaged subjects [ 12 ]. The change was, however, much smaller in magnitude than the ones reported in the afore mentioned studies, which is explained by the swift transition to offering care remotely. Similar transition in response to the pandemic was reported in secondary outpatient mental health care in the UK especially among underaged patients [ 14 ]. The rapid transition from in-person to remote psychiatric outpatient care during the pandemic has been predominantly positively received according to a qualitative study that interviewed psychiatrists [ 18 ].
We did not observe any significant increase in visits nor in referrals to adolescent psychiatric outpatient care later during the pandemic, despite many studies reporting increased mental distress during the pandemic in both adult [ 3 , 4 ] and underaged populations [ 6 , 7 , 8 , 9 ] and our consequent hypothesis that demand for adolescent psychiatric care would increase during the second half of year 2020. The current study spans up until the end of the year 2020. One possible explanation is that adolescents and their families do not seek help for mental health issues, or primary health care is not able to properly respond to their needs, until after the acute phase of the pandemic has subsided. All in all, any change in psychiatric morbidity in the general adolescent population often affects the demand for secondary and tertiary care in adolescent psychiatry, which is our study setting, with a lag, and thus the potential effect of the pandemic may not yet appear in our study period. Another perspective is that some longitudinal studies have observed mental health to rebound after the restrictions on everyday life ease both among adults [ 5 ] and adolescents [ 7 , 8 ]. Some parents have even seen their child’s mental health improve during the pandemic [ 9 ], and adults surveyed during a lockdown expressed the situation to entail diverse positive aspects for mental health [ 19 ].
Our observation that outpatient in-person visits gradually returned near to the expected levels after lockdown is in line with data on secondary outpatient mental health care in the UK [ 14 ]. From June, 2020, onwards HUH recommended remote visits in outpatient care, but patients were allowed to opt for in-person visits based on subjective preference. Our result would thus suggest that in-person visits were preferred over remote visits in our study population, contrary to findings of an Australian study where adolescents attending mental health services rated high satisfaction with telehealth and expressed interest in continuing its use after the pandemic [ 20 ]. Research on adult populations shows that telephone and video-delivered synchronous interventions in mental health care are as effective as in-person care [ 21 ], whereas research on adolescents lags behind [ 22 ]. Both quantitative and qualitative research in adolescent populations on remote mental health care addressing issues like the effectiveness of care, participants’ satisfaction and best practices would be most welcome in order to improve the flexibility of services without sacrificing quality.
The result in our study that raises concern and opposes to our hypothesis is that in-person visits of adolescents with a diagnosed psychotic disorder remained at a low level during the pandemic after Spring 2020 contrary to other diagnostic groups. Remote visits in this patient group increased in Spring 2020, but like among most patients, they later gradually decreased. In clinical practice, adolescents with psychosis and their families would need, in the light of our results, more support than other patients in accessing care during a pandemic. Research on adults shows that remote care is feasible and effective in assessing and treating patients with psychosis [ 23 ], but research on underaged patients with psychosis is lacking [ 22 ]. A further research topic could be how adolescents with psychosis, and their families, experience return to in-person visits after a lockdown and what kind of support they might need.
Strength of the study is the relatively long time period of 5 years we compared the pandemic period to, and also the relatively long time span, in comparison to other studies published so far, of the pandemic from the onset until the end of year 2020. A limitation is that the study is based on one organization only, but on the other hand HUH adolescent psychiatry is the largest secondary mental health care unit for adolescents in Finland. The data inevitably reflect some organizational issues such as variation in personnel resources and rare events such as the transition to a new clinical software in 2019–2020. We sought to compensate these limitations with the rather long comparison period of 5 years. The number of visits by adolescents with a psychotic disorder was low and the results are not as robust as in other diagnostic groups with more patients and visits. Our study was set in secondary and tertiary adolescent psychiatric care, and thus not directly comparable to studies on primary or mixed level mental health care. In our statistical analyses, we sought to model the dynamics of the pandemic period by including both step and slope change, but we recognise that interpreting statistical significance of such analyses may be problematic [ 24 ]. Finally, a rapid switch to remote care such as the one we observed requires high level of internet access and acceptability of online services as well as confidence in health care service providers, which are features of the Finnish society. Our results should be compared with caution to observations from societies that differ in these aspects.
Our results demonstrate that mental health services need to be flexible and responsive in how care is delivered in the event of a disruptive and evolving phenomenon such as the COVID-19 pandemic. Special attention should be given to most vulnerable and severely ill patients such as those with a psychotic disorder. Longitudinal studies on mental health outcomes and care reaching over to the post-pandemic period will show whether access to care and effectiveness of (mainly remote) treatments have been sufficient during the pandemic. Given that adolescence is such a critical developmental stage where social relationships are key, both clinical and research efforts need to specifically address this age group during the pandemic and its aftermath.
Availability of data and materials
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Attention-Deficit/Hyperactivity Disorder
Coronavirus disease of 2019
Helsinki University Hospital
International Classification of Diseases 10th Revision
World Health Organization
Loades ME, Chatburn E, Higson-Sweeney N, Reynolds S, Shafran R, Brigden A, et al. Rapid Systematic Review: The Impact of Social Isolation and Loneliness on the Mental Health of Children and Adolescents in the Context of COVID-19. J Am Acad Child Adolesc Psychiatr. 2020;59(11):1218–1239.e3. https://doi.org/10.1016/j.jaac.2020.05.009 .
Article Google Scholar
Orben A, Tomova L, Blakemore SJ. The effects of social deprivation on adolescent development and mental health. Lancet Child Adolesc Health. 2020;4(8):634–40. https://doi.org/10.1016/S2352-4642(20)30186-3 .
Article CAS PubMed PubMed Central Google Scholar
Kunzler AM, Röthke N, Günthner L, Stoffers-Winterling J, Tüscher O, Coenen M, et al. Mental burden and its risk and protective factors during the early phase of the SARS- CoV-2 pandemic: systematic review and meta-analyses. Glob Health. 2021;17(1):34. https://doi.org/10.1186/s12992-021-00670-y .
Pierce M, Hope H, Ford T, Hatch S, Hotopf M, John A, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatr. 2020;7(10):883–92. https://doi.org/10.1016/S2215-0366(20)30308-4 .
van der Velden PG, Hyland P, Contino C, von Gaudecker HM, Muffels R, Das M. Anxiety and depression symptoms, the recovery from symptoms, and loneliness before and after the COVID-19 outbreak among the general population: findings from a Dutch population-based longitudinal study. PLoS ONE. 2021;16(1):e0245057. https://doi.org/10.1371/journal.pone.0245057 .
Ravens-Sieberer U, Kaman A, Erhart M, Devine J, Schlack R, Otto C. Impact of the COVID-19 pandemic on quality of life and mental health in children and adolescents in Germany. Eur Child Adolesc Psychiatr. 2021;25:1–11. Epub ahead of print. https://doi.org/10.1007/s00787-021-01726-5 .
Hawes MT, Szenczy AK, Olino TM, Nelson BD, Klein DN. Trajectories of depression, anxiety and pandemic experiences; A longitudinal study of youth in New York during the Spring-Summer of 2020. Psychiatr Res. 2021;298:113778. https://doi.org/10.1016/j.psychres.2021.113778 .
Article CAS Google Scholar
Breaux R, Dvorsky MR, Marsh NP, Green CD, Cash AR, Shroff DM, et al. Prospective impact of COVID-19 on mental health functioning in adolescents with and without ADHD: protective role of emotion regulation abilities. J Child Psychol Psychiatr. 2021;62(9):1132–9. https://doi.org/10.1111/jcpp.13382 .
Cost KT, Crosbie J, Anagnostou E, Birken CS, Charach A, Monga S, et al. Mostly worse, occasionally better: impact of COVID-19 pandemic on the mental health of Canadian children and adolescents. Eur Child Adolesc Psychiatr. 2021 Feb;26:1–14. https://doi.org/10.1007/s00787-021-01744-3 .
Carr MJ, Steeg S, Webb RT, Kapur N, Chew-Graham CA, Abel KM, et al. Effects of the COVID-19 pandemic on primary care-recorded mental illness and self-harm episodes in the UK: a population-based cohort study. Lancet Public Health. 2021;6(2):e124–35. https://doi.org/10.1016/S2468-2667(20)30288-7 .
Article PubMed PubMed Central Google Scholar
Munich J, Dennett L, Swainson J, Greenshaw AJ, Hayward J. Impact of pandemics/epidemics on emergency department utilization for mental health and substance use: a rapid review. Front Psychiatr. 2021;12:615000. https://doi.org/10.3389/fpsyt.2021.615000 .
Ougrin D, Wong BH, Vaezinejad M, Plener PL, Mehdi T, Romaniuk L, et al. Pandemic-related emergency psychiatric presentations for self-harm of children and adolescents in 10 countries (PREP-kids): a retrospective international cohort study. Eur Child Adolesc Psychiatr. 2021:1–13. https://doi.org/10.1007/s00787-021-01741-6 .
Pignon B, Gourevitch R, Tebeka S, Dubertret C, Cardot H, Dauriac-Le Masson V, et al. Dramatic reduction of psychiatric emergency consultations during lockdown linked to COVID-19 in Paris and suburbs. Psychiatr Clin Neurosci. 2020;74(10):557–9. https://doi.org/10.1111/pcn.13104 .
Patel R, Irving J, Brinn A, Broadbent M, Shetty H, Pritchard M, et al. Impact of the COVID-19 pandemic on remote mental healthcare and prescribing in psychiatry: an electronic health record study. BMJ Open. 2021;11(3):e046365. https://doi.org/10.1136/bmjopen-2020-046365 .
Article PubMed Google Scholar
Bhaskaran K, Gasparrini A, Hajat S, Smeeth L, Armstrong B. Time series regression studies in environmental epidemiology. Int J Epidemiol. 2013;42(4):1187–95. https://doi.org/10.1093/ije/dyt092 .
Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27(4):299–309. https://doi.org/10.1046/j.1365-2710.2002.00430.x .
Article CAS PubMed Google Scholar
R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2020. https://www.R-project.org/ . Accessed from Dec 2020 to March 2021
Google Scholar
Uscher-Pines L, Sousa J, Raja P, Mehrotra A, Barnett ML, Huskamp HA. Suddenly becoming a "virtual doctor": experiences of psychiatrists transitioning to telemedicine during the COVID-19 pandemic. Psychiatr Serv. 2020;71(11):1143–50. https://doi.org/10.1176/appi.ps.202000250 .
Jenkins M, Hoek J, Jenkin G, Gendall P, Stanley J, Beaglehole B, et al. Silver linings of the COVID-19 lockdown in New Zealand. PLoS ONE. 2021;16(4):e0249678. https://doi.org/10.1371/journal.pone.0249678 .
Nicholas J, Bell IH, Thompson A, Valentine L, Simsir P, Sheppard H, et al. Implementation lessons from the transition to telehealth during COVID-19: a survey of clinicians and young people from youth mental health services. Psychiatr Res. 2021;299:113848. https://doi.org/10.1016/j.psychres.2021.113848 .
Payne L, Flannery H, Kambakara Gedara C, Daniilidi X, Hitchcock M, Lambert D, et al. Business as usual? Psychological support at a distance. Clin Child Psychol Psychiatr. 2020;25(3):672–86. https://doi.org/10.1177/1359104520937378 .
Hollis C, Falconer CJ, Martin JL, Whittington C, Stockton S, Glazebrook C, et al. Annual research review: digital health interventions for children and young people with mental health problems - a systematic and meta-review. J Child Psychol Psychiatr. 2017;58(4):474–503. https://doi.org/10.1111/jcpp.12663 .
Donahue AL, Rodriguez J, Shore JH. Telemental health and the management of psychosis. Curr Psychiatry Rep. 2021;23(5):27. https://doi.org/10.1007/s11920-021-01242-y .
Bernal JL, Soumerai S, Gasparrini A. A methodological framework for model selection in interrupted time series studies. J Clin Epidemiol. 2018;103:82–91.1. https://doi.org/10.1016/j.jclinepi.2018.05.026 .
Download references
Acknowledgements
We are grateful to Dr. Henna Haravuori, Dr. Pekka Närhi and Dr. Klaus Ranta for their valuable contributions that helped in designing the study.
This work was supported by the Helsinki University Hospital Research funding. The funding institution was not involved in any stage of the study i.e. not in the study design, the collection, analysis and interpretation of data, in the writing of the report nor in the decision to submit an article for publication.
Author information
Authors and affiliations.
Adolescent Psychiatry, University of Helsinki and Helsinki University Hospital, PO BOX 660, 00029 HUS, Helsinki, Finland
Emma M. Savilahti, Sakari Lintula, Laura Häkkinen, Mauri Marttunen & Niklas Granö
Mental Health Unit, National Institute for Health and Welfare, Helsinki, Finland
Mauri Marttunen
You can also search for this author in PubMed Google Scholar
Contributions
ES, SL, MM and NG contributed to the study conception and design. Data collection and analysis were performed by SL. The first draft of the manuscript was written by ES and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Authors’ information
Emma M. Savilahti, MD, PhD, is an adolescent psychiatrist currently working at the adolescent psychiatry unit in HUH and a clinical research scientist at the University of Helsinki. Sakari Lintula, M. Sc, is a clinical psychologist currently working at the adolescent psychiatry unit in HUH. Laura Häkkinen, MD, PhD, is an adolescent psychiatrist currently working as the head of department of the adolescent psychiatry unit in HUH. Mauri Marttunen, MD, PhD, is an adolescent psychiatrist and professor emeritus of adolescent psychiatry at the University of Helsinki. Niklas Granö, PhD, is currently working as the chief psychologist at the adolescent psychiatry unit in HUH and is a research scientist at University of Helsinki.
Corresponding author
Correspondence to Emma M. Savilahti .
Ethics declarations
Consent publication.
Not applicable.
Ethics approval and consent to participate
Not applicable: The manuscript does not contain clinical studies or patient data.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:.
Fig. S1. Outpatient in person and remote visits on annual level, and division of remote visits to phone calls and video calls. a) Annual number of outpatient visits and the proportion of in-person (blank) and remote (shaded) visits 2015–2020. X-axis shows the year and Y axis the number of visits. b) Remote visits (thick line) comprised of phone calls (dashed line) and online video calls (fine line). X-axis shows the time from Jan, 1, 2015 to Dec, 31, 2020, ticks denote the start of each year. Y-axis shows the number of visits.
Additional file 2:
Fig. S2. Outpatient in person and remote visits 2015–2020 in different psychiatric diagnostic groups. a) In person visits in the group of psychotic disorders (F20–29). b) In person visits in the group of depressive and anxiety disorders (F32, F33, F40–48, F93.0, F93.1, F93.2, F93.80, F93.9). c) In person visits in the group of ADHD and conduct disorders (F90, F91, F92. d) In person visits in the group of all other diagnoses. e) remote visits in the group of psychotic disorders (F20–29). f) remote visits in the group of depressive and anxiety disorders (F32, F33, F40–48, F93.0, F93.1, F93.2, F93.80, F93.9). g) remote visits in the group of ADHD and conduct disorders (F90, F91, F92). h) remote visits in the group of all other diagnoses. The dots denote weekly data points, the fine line denotes the fitted line and the fine dashed line denotes the predicted counterfactual line based on the model (based on data from years 2015–2019). The thick line denotes the trend over time when controlling for seasonality, and the thick dotted line denotes the counterfactual prediction when controlling for seasonality, based on previous 5 years (2015–2019). X-axis shows the time from Jan, 1, 2015 to Dec, 31, 2020, ticks denote the start of each year. Y-axis shows the number of visits. NB. The scale of Y axes varies between figures.
Additional file 3:
Fig. S3. The number of subjects in adolescent outpatient care 2015–2020 (monthly data). The dots denote monthly data points, the fine line denotes the fitted line and the fine dashed line denotes the predicted counterfactual line based on the model (based on data from years 2015–2019). The thick line denotes the trend over time when controlling for seasonality, and the thick dotted line denotes the counterfactual prediction when controlling for seasonality, based on previous 5 years (2015–2019). X-axis shows the time from Jan, 1, 2015 to Dec, 31, 2020, ticks denote the start of each year. Y-axis shows the number of subjects.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Savilahti, E.M., Lintula, S., Häkkinen, L. et al. Adolescent psychiatric outpatient care rapidly switched to remote visits during the COVID-19 pandemic. BMC Psychiatry 21 , 586 (2021). https://doi.org/10.1186/s12888-021-03580-w
Download citation
Received : 24 June 2021
Accepted : 03 November 2021
Published : 20 November 2021
DOI : https://doi.org/10.1186/s12888-021-03580-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Adolescent psychiatry
- Remote visit
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]

CARRIE ARMSTRONG, AFP Senior Associate Editor
Am Fam Physician. 2016;94(1):62-64
Author disclosure: No relevant financial affiliations.
Key Points for Practice
The initial psychiatric evaluation should include a review of the patient's mood, anxiety level, thought content and process, perception, and cognition, and history of trauma and psychiatric history.
In the setting of current suicidal ideas, identify the intended course of action, access to suicide methods, motivations for suicide and reasons for living, quality of the therapeutic alliance, and history of suicidal behaviors of biologic relatives.
Quantitative measures of symptoms, level of functioning, and quality of life should be obtained to improve clinical decision making and treatment outcomes.
From the AFP Editors
The American Psychiatric Association (APA) recently released the third edition of its guidelines on psychiatric evaluation of adults. The nine-part guideline has been updated based on new evidence identified since the previous edition was released in 2006. Although the strength of the evidence supporting the recommendations in the updated guidelines is low, there is consensus that their benefits clearly outweigh the harms. In cases where the balance of benefits and harms is difficult to judge, or the benefits or harms are unclear, the APA made suggestions for care instead of recommendations. For more information about these guidelines, including tips for implementation, see the full report from the APA.
Guideline 1: Review Symptoms, Trauma History, and Treatment History
The APA recommends that the initial psychiatric evaluation include a review of the patient's mood, anxiety level, thought content and process, perception, and cognition. The clinician should review the patient's trauma history and his or her psychiatric history, including psychiatric diagnoses, treatments (type, duration, and medication dosages), adherence and response to treatments, and history of psychiatric hospitalization and emergency department visits for psychiatric issues. The goal of this guideline is to improve the quality of the clinician-patient relationship, the accuracy of psychiatric diagnoses, and the appropriateness of treatment selection. Knowledge of prior psychiatric diagnoses can inform the current diagnosis because a patient may be presenting with a continuation of a previously diagnosed disorder, or may now have a different disorder that commonly co-occurs with the first. Past treatments are relevant because lack of effectiveness may suggest a need to reconsider the accuracy of the diagnosis. Symptoms that emerge during treatment (e.g., hypomania or mania in a patient with depression) may also require reassessment of the diagnosis.
Guideline 2: Evaluate Substance Use
To identify patients with substance use disorder and to facilitate treatment planning, the APA recommends that clinicians assess the patient's use of tobacco, alcohol, and other substances (e.g., marijuana, cocaine, heroin, hallucinogens), as well as misuse of prescribed or over-the-counter medications or supplements. Ensuring that initial psychiatric evaluations include assessment of substance use may improve the differential diagnosis because substance use disorders, other psychiatric disorders, and other medical conditions may share similar presenting symptoms, such as anxiety, depression, mania, and psychosis.
Guideline 3: Assess Risk of Suicide
The APA recommends that clinicians evaluate the patient's current suicidal ideas, plans, and intent, including active or passive thoughts of suicide or death; prior suicidal ideas, plans, and attempts, including attempts that were aborted or interrupted; prior intentional self-injury in which there was no suicide intent; anxiety symptoms, including panic attacks; hopelessness; impulsivity; current or recent substance use disorder or change in use of alcohol or other substances; presence of psychosocial stressors (e.g., financial, housing, legal, school/occupational, or interpersonal/relationship problems; lack of social support; painful, disfiguring, or terminal illness); and aggressive or psychotic ideas, including thoughts of physical or sexual aggression or homicide. The clinician who conducts the initial psychiatric evaluation should document an estimation of the patient's suicide risk, including factors influencing risk.
If the patient reports having current suicidal ideas, the APA recommends that clinicians identify the intended course of action if symptoms worsen; determine the patient's access to suicide methods, including firearms; identify possible motivations for suicide (e.g., attention or reaction from others, revenge, shame, humiliation, delusional guilt, command hallucinations) and reasons for living (e.g., sense of responsibility to children or others, religious beliefs); assess the quality and strength of the therapeutic alliance; and ask about the history of suicidal behaviors in the patient's biological relatives. If the patient has attempted suicide in the past, the clinician should ask about details of each attempt (e.g., context, method, damage, potential lethality, intent).
Guideline 4: Assess Risk of Aggressive Behaviors
To identify patients at risk of aggressive behaviors, the APA recommends that the initial psychiatric evaluation of a patient include assessment of current or past aggressive or psychotic ideas, including thoughts of physical or sexual aggression or homicide; past aggressive ideas or behaviors (e.g., homicide, domestic or workplace violence, other physically or sexually aggressive threats or acts); legal or disciplinary consequences of past aggressive behaviors; exposure to violence or aggressive behavior, including combat exposure or childhood abuse; and current or past neurologic or neurocognitive disorders or symptoms. The clinician who conducts the initial psychiatric evaluation should document an estimation of the patient's risk of aggressive behavior, including homicide, and factors influencing risk.
If the patient reports having aggressive ideas, the APA recommends that clinicians assess the patient's impulsivity, including anger management issues; determine the patient's access to firearms; identify specific persons toward whom homicidal or aggressive ideas or behaviors have been directed; and ask about the history of violent behaviors in the patient's biological relatives.
There is no evidence that risk of aggression is increased by asking about past experiences, symptoms such as impulsivity, or current aggressive and homicidal ideas or plans. However, assessment could identify persons as being at risk when they are not, which could result in unneeded hospitalization or other consequences. Just as it is not possible to predict which persons will exhibit aggressive behaviors, there is no way to predict which ones would be incorrectly identified as being at risk, and no way to estimate the potential magnitude of this harm.
Guideline 5: Evaluate Cultural Factors
To identify cultural factors that could influence the therapeutic alliance, promote diagnostic accuracy, and enable treatment planning, the APA recommends determining the patient's need for an interpreter—even if the patient speaks the same language as the clinician—and assessing cultural factors related to the patient's social environment. Persons from different backgrounds may have different explanations of illness, views of mental illness, and preferences for psychiatric treatment, particularly given the cross-cultural differences in the stigma of psychiatric disorders. For this reason, the APA also suggests assessing the patient's personal and cultural beliefs, and cultural explanations of psychiatric illness. For example, an individual's self concept, response to stressors, or current symptoms may be shaped by racism, sexism, or discrimination; by traumatic experiences during or after migration from other countries; or by challenges of acculturation, including intergenerational family conflict. Cultural factors can also influence the patient's style of relating with authority figures, such as health care professionals.
Guideline 6: Assess Medical Health
The APA recommends that clinicians determine whether the patient has an ongoing relationship with a primary care health professional. Persons with psychiatric disorders can have medical conditions that influence their functioning, quality of life, and life span. Compared with the general population, mortality rates are increased in persons with mental illness, particularly those with psychotic disorders, depressive disorders, alcohol or substance use disorders, personality disorders, and delirium. To identify nonpsychiatric medical conditions that could affect the accuracy of a psychiatric diagnosis and the safety of the treatment plan, the APA recommends that the initial psychiatric evaluation include assessment of the patient's general appearance and nutritional status; involuntary movements or abnormal motor tone; coordination and gait; speech, including fluency and articulation; sight and hearing; physical trauma, including head injuries; past or current medical illnesses and related hospitalizations; relevant past or current treatments, including surgeries, other procedures, or complementary and alternative treatments; allergies or drug sensitivities; sexual and reproductive history; and past or current sleep abnormalities, including sleep apnea. It also recommends that clinicians document all current and recent medications (prescribed and nonprescribed, including herbal and nutritional supplements and vitamins) and adverse effects of these medications.
In addition, the APA suggests that the initial psychiatric evaluation include assessment of the patient's height, weight, and body mass index; vital signs; skin, including any stigmata of trauma, self-injury, or drug use; cardiopulmonary status; past or current endocrine disease; past or current infectious disease, including sexually transmitted diseases, human immunodeficiency virus infection, tuberculosis, hepatitis C, and locally endemic infectious diseases (e.g., Lyme disease); past or current neurologic or neurocognitive disorders or symptoms; and past or current symptoms or conditions associated with significant pain and discomfort. The APA also suggests that clinicians review the patient's constitutional symptoms (e.g., fever, weight loss), eyes, ears, nose, mouth, throat; and cardiovascular, respiratory, gastrointestinal, genitourinary, musculoskeletal, integumentary, neurologic, endocrine, hematologic, lymphatic, and allergic/immunologic symptoms.
Guideline 7: Use Quantitative Tools
To improve clinical decision making and treatment outcomes, the APA suggests that the initial psychiatric evaluation include quantitative measures of symptoms, level of functioning, and quality of life (e.g., rating scales, patient questionnaires). Clinical decision making, including diagnosis and treatment planning, requires a careful and systematic assessment of the type, frequency, and magnitude of psychiatric symptoms, as well as an assessment of the effect of those symptoms on the patient's day-to-day functioning and quality of life. There are several potential benefits to obtaining this information as part of the initial psychiatric evaluation through the use of quantitative measures. Compared with a clinical interview, these tools may help the clinician conduct a more consistent and comprehensive review of the patient's symptoms, which may prevent potentially relevant symptoms from being overlooked.
Guideline 8: Involve the Patient in Decision Making
To improve patient engagement and knowledge about his or her diagnosis and treatment options, the APA recommends that during the initial psychiatric evaluation, the clinician should explain the differential diagnosis, risks of untreated illness, treatment options, and benefits and risks of treatment. The clinician should also ask about the patient's treatment preferences and collaborate on decisions about treatment. Such collaboration may improve the therapeutic alliance, satisfaction with care, and adherence with treatment.
Guideline 9: Document the Psychiatric Evaluation
When a patient's care is being provided by multiple health care professionals using a shared treatment or treatment team approach, collaboration and coordination of care are crucial. To improve clinical decision making and increase coordination of psychiatric treatment with other clinicians, the APA recommends documenting the rationale for treatment selection, including the specific factors that influenced the treatment choice. It suggests that clinicians also document the rationale for clinical tests.
Guideline source : American Psychiatric Association
Evidence rating system used? Yes
Literature search described? Yes
Guideline developed by participants without relevant financial ties to industry? Yes
Published source : PsychiatryOnline . November 2015.
Available at : http://psychiatryonline.org/doi/full/10.1176/appi.books.9780890426760.pe02
Coverage of guidelines from other organizations does not imply endorsement by AFP or the AAFP.
This series is coordinated by Michael J. Arnold, MD, Assistant Medical Editor.
A collection of Practice Guidelines published in AFP is available at https://www.aafp.org/afp/practguide .
Continue Reading

More in AFP
More in pubmed.
Copyright © 2016 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
Disclaimer » Advertising
- HealthyChildren.org

- Previous Article
- Next Article
Data Source
Study population, follow-up visits, statistical analyses, sensitivity analyses, hospitalizations for depression, bipolar disorder, schizophrenia, or anxiety, follow-up visits after discharge within 7 or 30 days, psychiatric crises after discharge, conclusions, ed visits and readmissions after follow-up for mental health hospitalization.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- CME Quiz Close Quiz
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
Naomi S. Bardach , Stephanie K. Doupnik , Jonathan Rodean , Bonnie T. Zima , James C. Gay , Carol Nash , Yasas Tanguturi , Tumaini R. Coker; ED Visits and Readmissions After Follow-up for Mental Health Hospitalization. Pediatrics June 2020; 145 (6): e20192872. 10.1542/peds.2019-2872
Download citation file:
- Ris (Zotero)
- Reference Manager
A national quality measure in the Child Core Set is used to assess whether pediatric patients hospitalized for a mental illness receive timely follow-up care. In this study, we examine the relationship between adherence to the quality measure and repeat use of the emergency department (ED) or repeat hospitalization for a primary mental health condition.
We used the Truven MarketScan Medicaid Database 2015–2016, identifying hospitalizations with a primary diagnosis of depression, bipolar disorder, psychosis, or anxiety for patients aged 6 to 17 years. Primary predictors were outpatient follow-up visits within 7 and 30 days. The primary outcome was time to subsequent mental health–related ED visit or hospitalization. We conducted bivariate and multivariate analyses using Cox proportional hazard models to assess relationships between predictors and outcome.
Of 22 844 hospitalizations, 62.0% had 7-day follow-up, and 82.3% had 30-day follow-up. Subsequent acute use was common, with 22.4% having an ED or hospital admission within 30 days and 54.8% within 6 months. Decreased likelihood of follow-up was associated with non-Hispanic or non-Latino black race and/or ethnicity, fee-for-service insurance, having no comorbidities, discharge from a medical or surgical unit, and suicide attempt. Timely outpatient follow-up was associated with increased subsequent acute care use (hazard ratio [95% confidence interval]: 7 days: 1.20 [1.16–1.25]; 30 days: 1.31 [1.25–1.37]). These associations remained after adjusting for severity indicators.
Although more than half of patients received follow-up within 7 days, variations across patient population suggest that care improvements are needed. The increased hazard of subsequent use indicates the complexity of treating these patients and points to potential opportunities to intervene at follow-up visits.
A nationally endorsed pediatric quality measure is used to assess rates of timely follow-up for patients hospitalized for a mental health diagnosis. Rates range from 48% to 67%, but little is known about variations by patient characteristics or about the relationship between follow-up and a subsequent psychiatric crisis.
Adherence to the national quality measure ranged from 62% to 82% but varied by patient and hospital characteristics. Adherence was associated with an increased risk of a subsequent mental health crisis, even after controlling for severity of illness.
The prevalence of children in the United States with a serious mental health disorder is estimated at 10% 1 ; these children and youth are high users of emergency department (ED) and inpatient hospitalization, but many do not receive ongoing outpatient mental health care. 2 – 6
National quality measures for assessing quality of mental health care delivery may be critical to improving outcomes for children and youth with serious psychiatric disorders. In recognition of this, the Children’s Core Set of quality measures, created as a part of the Children’s Health Insurance Program Reauthorization Act of 2009, includes follow-up after hospitalization for mental illness at 7 and 30 days as a national quality measure. This is a Healthcare Effectiveness Data and Information Set (HEDIS) measure developed by the National Committee for Quality Assurance. 7
Rates of performance nationally for this measure range from 47.5% of children and youth hospitalized for a mental illness having a follow-up visit within 7 days of hospital discharge to 66.7% having at least one follow-up visit within 30 days of discharge. 7 , 8 However, there are few studies on how this quality measure’s performance varies by race and/or ethnicity and socioeconomic, clinical, or hospital characteristics and whether this adherence to the quality measure is associated with improved patient outcomes. Answering these questions can inform efforts to improve quality, identifying patients at higher risk of poor-quality care and potentially worse outcomes.
To answer these questions and fill the gap in the literature, our study objectives, by using Medicaid data from 11 states, were to (1) assess outpatient follow-up after discharge for a mental health hospitalization for children ages 6 to 17, (2) assess variations in measure performance by child race and/or ethnicity and socioeconomic status and by clinical and hospital characteristics, and (3) assess how having follow-up care relates to repeat ED use and hospitalizations. For objective 3, we hypothesized that having follow-up within 7 or 30 days of discharge would be associated with a decreased risk of subsequent hospitalization or ED visit for a mental health disorder.
We used the Truven MarketScan Medicaid data from 2015 to 2016. The Truven database contains medical claims for inpatient, outpatient, and pharmaceutical use for Medicaid enrollees in 11 states representing all geographic regions of the United States (the Truven data use agreements preclude publication of state names). We used data only for patients with mental health and substance abuse coverage (98% of enrollees in the database).
We focused on mental health diagnoses that were found in our previous work to be common and costly diagnoses for pediatric inpatient mental health use: depression, bipolar disorder, psychosis, and anxiety. 9 Our study cohort consisted of patients with a hospitalization (the index admission) for one of these as a primary diagnosis between January 2015 and June 2016. We identified these patients using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) and International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) codes, as done previously. 10 , 11 The ICD-9-CM codes were aligned with the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition main diagnostic groups, 10 and, subsequently, the ICD-10-CM codes were mapped from the ICD-9-CM and tested by using a national administrative database after the switch to the ICD-10-CM . 11 We restricted the population to patients aged 6 to 17 years at the time of their hospitalization. This age range is consistent with previous claims-based studies of the mental health diagnoses of focus, reflecting the low prevalence in young patients and, therefore, small sample size in this group. 9 , 12 To ensure completeness of use estimates after hospitalization, only children with continuous Medicaid enrollment for 6 months after discharge were included. Transfers from one inpatient setting to another (eg, general hospital to inpatient psychiatric facility) were treated as one episode. Finally, to ensure consistent measurement of outpatient use, patients who were not discharged from the hospital to home (eg, those discharged to a partial hospitalization program) were excluded.
Our predictors of interest were whether the patient had a mental health outpatient follow-up visit within 7 or 30 days after discharge from the index admission. The visit was defined as any Medicaid-reimbursed visit with one or more of the following: (1) a mental health diagnosis defined by using the International Classification of Diseases code definitions noted above 10 , 11 ; (2) a visit defined by using the “standard providers” variable in the database, by using values for psychiatry, psychology, therapy (excluding physical, occupational, or speech), and mental health facility; or (3) a visit defined by using Truven’s proprietary binary variable indicating a service subcategory of mental health (see Supplemental Table 5 for the distribution of these definitions and Supplemental Table 6 for the most common Current Procedural Terminology [CPT] codes associated with these visits). We chose the 2 follow-up windows (7 and 30 days) because they are consistent with the HEDIS quality measure of follow-up after hospitalization for mental illness. 7
Because the therapeutic effect of follow-up care has a potential dose-response relationship, we also measured the number of subsequent follow-up outpatient mental health visits between 8 days and 6 months after the index discharge as an indicator of dose of care over time.
Our primary outcome was time to subsequent psychiatric crisis up to 6 months after discharge. We defined psychiatric crisis as an ED visit or a hospitalization with an assigned major diagnostic category of mental diseases and disorders; alcohol or drug use or induced mental disorders; or injuries, poison, and toxic effect of drugs. As secondary outcomes, we assessed 2 binary outcomes: whether a crisis occurred within 30 days and whether a crisis occurred within 6 months.
We included in our analyses several covariates to adjust for potential confounding and as potential explanatory variables. Timely follow-up visits may be driven by clinical severity. To account for this, we included 2 covariates to approximate severity of illness: psychiatric comorbidities and length of stay (LOS) of the index hospitalization. For psychiatric comorbidities, we assessed the number of psychiatric comorbidities for each patient, defined by using ICD-9-CM and ICD-10-CM codes as noted above. 10 , 11 After examining the data, we defined LOS using the following categories: <4, 4 to 6, and >6 days.
Other covariates included age (categorized as 6–11 or 12–17 years), sex, race and/or ethnicity, insurance type (fee for service or managed care), having a comorbid nonpsychiatric chronic disease, and hospital type (psychiatric hospital, psychiatric unit within a general hospital, or general medical hospital unit). To adjust for nonpsychiatric comorbidities, we used the Pediatric Medical Complexity Algorithm (PMCA), which categorizes patients into 3 categories using ICD-9-CM and ICD-10-CM codes: no chronic conditions, noncomplex chronic conditions, or complex chronic conditions. 13 , 14
We used bivariate analyses to determine characteristics associated with follow-up within 7 or 30 days and characteristics associated with having a subsequent psychiatric crisis. For statistical significance testing, we used Kruskal-Wallis and χ 2 analyses.
We used a survival analysis, with Kaplan-Meier curves and Cox proportional hazards multivariable models, to assess relationships between follow-up visits at the 2 time periods and subsequent psychiatric crisis. This approach allows the 7- and 30-day visits to be time varying. For example, if an enrollee had a crisis on day 4 and a follow-up visit on day 6, they would be considered as not having had a visit on days 0 to 4. Their contributions to the Cox model would stop at day 4, and their follow-up would not be considered for the analysis. This approach allowed us to include psychiatric crises that occurred at any time point after discharge.
We used multivariable analyses with a stepwise approach to assess whether the relationship between follow-up and subsequent crisis was confounded by comorbidities or severity of disease. We first tested the association by only including covariates that do not indicate comorbidity or severity of illness in the model: mental health diagnosis for index admission, age, sex, race and/or ethnicity, and insurance plan type (fee for service versus capitated plan). Then we added into the model covariates for comorbidity and severity: PMCA category, LOS category, number of comorbid mental health conditions, and suicide attempt or ideation.
For sensitivity analyses, we tested an alternative predictor definition, defining follow-up using 2 variables, active medication use and active outpatient mental health visits, included in a time-dependent model. To define these time-dependent variables, we identified the first medication fill for an antidepressant or antipsychotic and considered the time-dependent medication variable active if another prescription was filled within 30 days of the end of the prescribed fill. The time-dependent variable for outpatient visits was considered active if there was a visit within 30 days of the previous visit. An additional sensitivity analysis was used to assess for potential confounding effects of autism ( n = 970; 4.2%), intellectual disability ( n = 553; 2.4%), and substance abuse ( n = 3678; 16.1%) on the relationship between outpatient follow-up and subsequent crises by including the presence of those diagnoses as covariates in the model.
A total of 22 844 children aged 6 to 17 years old were admitted with one of the conditions of interest as a primary diagnosis. Three-quarters of these children had depressive disorders, whereas 20% had bipolar or related disorders, and few had either schizophrenia (3.6%) or anxiety (1.6%). Most patients were 12 to 17 years of age. Racial and ethnic distribution was similar across 3 of the 4 categories ( Table 1 ). Non-Hispanic or non-Latino white patients made up 63% of admissions and non-Hispanic or non-Latino black patients made up 25%.
Characteristics of Pediatric Admissions for Primary Diagnoses of Depression, Bipolar Disorder, Psychosis, or Anxiety ( N = 22 844)
MH, mental health.
The PMCA, 13 , 14 which uses ICD-9-CM and ICD-10-CM definitions of chronic disease to create a categorical variable, was used to determine chronic disease.
Sixty-two percent of patients had follow-up within 7 days, and 82.3% had follow-up within 30 days. Follow-up rates were similar across most patient characteristics ( Table 2 ), with <6-percentage-point differences in follow-up between categories (although most met statistical significance because of large sample size). However, those discharged from general medical or surgical units were substantially less likely to have follow-up at both time points (47.2% at 7 days and 73.2% at 30 days) compared with patients discharged from psychiatric units within general hospitals (61.1% at 7 days and 81.3% at 30 days) or freestanding psychiatric hospitals (63.8% at 7 days and 84.1% at 30 days; Table 2 ). Fewer non-Hispanic or non-Latino black patients compared with white patients had follow-up at both 7 and 30 days after discharge (57.9% vs 63.2% at 7 days and 77.4% vs 84.1% at 30 days). Those with ≥4 mental health comorbidities had a higher follow-up percentage compared with those without these comorbidities (66.4% vs 59.0% at 7 days and 85.6% vs 78.4% at 30 days; Table 2 ).
Frequency of Follow-up Visits Within 7 and 30 Days by Patient and Hospital Characteristics
MH, mental health; —, not applicable.
Adjusted for all variables shown. All comparisons were statistically significantly different except for comparing unadjusted rates of follow-up visits for boys and girls ( P = .19 for 7-d visits and P = .21 for 30-d visits).
In assessing differences in the dose of follow-up, or the number of follow-up visits within 6 months, we found that patients with follow-up by 7 days had more subsequent follow-up visits (median: 17 visits within 6 months of discharge; interquartile range [IQR] 8–35), whereas those without follow-up by 7 days had fewer subsequent visits (median: 8 visits; IQR 3–17).
Patients frequently had psychiatric crises (mental health–related ED visits or hospitalizations) after discharge, with 22.4% with crises within 30 days and 54.8% with crises within 6 months. Primary diagnosis, race and/or ethnicity, medical and mental health comorbidities, and hospital unit type were associated with subsequent crises ( Table 3 ). Of those with a crisis, 63% had ED visits and 37% were hospitalized.
Patients With a Psychiatric Crisis Within 30 Days and Within 6 Months
All comparisons were statistically significantly different except for comparing age categories for a crisis within 30 d ( P = .19), boys and girls for a crisis within 30 d ( P = .22), and plan types for a crisis within 6 mo ( P = .36). MH, mental health.
Having a follow-up visit within 7 or 30 days was associated with an increased hazard ratio (HR) for psychiatric crisis (HR adjusted for base characteristics: 7 days: 1.20 [95% confidence interval (CI) 1.16–1.25]; 30 days: 1.31 [95% CI 1.25–1.37]; Kaplan-Meier curves in Figs 1 and 2 ). This relationship was slightly attenuated when severity-related variables (LOS, comorbidities related and not related to mental health) were included (HR adjusted for base characteristics and severity indicators: 7 days: 1.18 [95% CI 1.13–1.22]; 30 days: 1.27 [95% CI 1.21–1.33]; Table 4 ), but the association remained statistically significant in the same direction, with CIs overlapping results from the baseline model.

Kaplan-Meier survival curves revealing the relationship between having a mental health follow-up visit within 7 days after hospitalization for depression, bipolar disorder, psychosis, or anxiety and a subsequent psychiatric crisis (hospitalization or ED visit) within 6 months from discharge.

Kaplan-Meier survival curves revealing the relationship between having a mental health follow-up visit within 30 days after hospitalization for depression, bipolar disorder, psychosis, or anxiety and a subsequent psychiatric crisis (hospitalization or ED visit) within 6 months from discharge.
Relationships Between Follow-up Visits at 7 and 30 Days and Subsequent Psychiatric Crises, Adjusting for Base Characteristics and Then Including Severity Measures
Base models were adjusted for condition, age category, sex, chronic condition indicator, and insurance type. MH, mental health; —, not applicable.
There was no difference in the proportion of patients with a subsequent hospitalization between groups with and without follow-up within 7 days of discharge (34.7% vs 35.7%; P > .05), and there was a slight increase in the proportion of patients without follow-up within 30 days (34.1% vs 37.3%; P = .01).
The findings were similar in magnitude and direction in a time-dependent model used to assess active medication use (HR: 1.25; 95% CI 1.20–1.31) and active outpatient mental health visits (HR: 1.34; 95% CI 1.29–1.40). Models that included autism, intellectual disabilities, and substance abuse as covariates also had similar findings in direction and magnitude (data not shown).
With this study, we are the first to examine variations in 7- and 30-day follow-up among a sample of children and adolescents with mental health admissions across psychiatric and general hospitals in the United States and the associated risk of subsequent ED revisit or rehospitalization. In our analysis of Medicaid data from 11 states, we found that a majority of children aged 6 to 17 years had any mental health outpatient follow-up, with higher rates than previously found for this national HEDIS quality measure. 7 , 8 Just under two-thirds had follow-up within 7 days, and >80% had follow-up within 30 days. Lower rates of follow-up were seen for certain groups, including non-Hispanic or non-Latino black children and those children discharged from a general medical or surgical unit for mental health illness as opposed to a psychiatric unit or hospital. Contrary to our hypothesis, we found that having a follow-up within 7 or 30 days of discharge was associated with an increased risk of a subsequent hospitalization or ED visit for a mental health illness, even after controlling for potential confounders.
Our finding that follow-up rates for black children were ∼6 percentage points less than follow-up rates for white children supports findings from a previous study that revealed a relationship between black race and lower follow-up rates for children admitted for mood disorders (depression and bipolar disorders) in 2009–2010. 15 Fee-for-service health plan coverage and discharge from a medical or surgical unit were also associated with lower follow-up rates at 7 and 30 days. This suggests that to improve performance on the national measure from the Child Core Set, health plans and providers may need to increase outreach and access to services for these populations.
Our a priori hypothesis was that having a 7- or 30-day outpatient mental health follow-up after a mental health hospitalization would be associated with lower risk for subsequent hospitalizations or ED visits for mental illness. However, we found the opposite to be true. Previous studies examining the risk of readmission from a mental health hospitalization have produced mixed results. A study by Carlisle et al 16 revealed that outpatient follow-up with a primary care provider or psychiatrist within a month after a psychiatric hospitalization for 15- to 19-year-olds in Ontario, Canada, increased the risk of readmission and ED visits combined and readmission alone but was not significantly associated with ED visits. Two other smaller studies also revealed that outpatient follow-up after hospitalization for a mental health disorder was associated with increased risk for readmission, including a study of 522 adolescents with psychiatric hospitalizations in 3 Maryland hospitals 17 and a study by Gearing et al 18 of 87 patients <18 years old with a first episode of psychosis. A study of 500 children and adolescents (ages 3–21) who were wards of the court in Illinois revealed that posthospitalization services (including case management) were associated with lower rates of rehospitalization. 19 A study of Children’s Health Insurance Program recipients in Alabama revealed low rates of follow-up at 7 and 30 days (33% and 53%, respectively) and no association with subsequent ED use or rehospitalization within 60, 90, or 120 days in adjusted models. 20
Although we do not believe that there is causation in this relationship, we have several hypotheses to explain our findings. First, it is possible that we did not sufficiently account for severity of illness or psychosocial complexity in our models. Discharging providers may be more likely to ensure outpatient follow-up for children with more-severe illness (either medical or psychiatric) or greater psychosocial complexity, thereby driving the relationship between follow-up and crisis. We did find that children with ≥4 comorbid mental health conditions were more likely to have a 7- and 30-day follow-up than those with no comorbid mental health conditions, but this variable was included in our multivariable models.
There is also the possibility that having a 7- or 30-day follow-up outpatient mental health visit leads to increased recognition of a crisis and thus increases the risk of ED use or rehospitalization. A recent study by Joyce et al 21 revealed that a lack of treatment alliance with a mental health provider was associated with decreased psychiatric rehospitalization after discharge; the authors suggest as an explanation that outpatient care leads to increased recognition of emotional dysregulation and, hence, to appropriate referrals to ED or inpatient care.
Finally, there is also the possibility that psychiatric crises (leading to an ED visit or admission) after the index mental health illness hospital admission are not readily prevented by better access to outpatient follow-up care and that follow-up care is beneficial to these patients who are severely ill but cannot reduce the severity of their disease. This is supported by the finding that almost one-quarter of patients have subsequent crises within 30 days and that more than half have subsequent crises within 6 months. Our finding of similar rates of rehospitalization for children with and without a 7-day follow-up after the index admission indicates that the more-severe crises are difficult to prevent, regardless of outpatient follow-up; however, we did find that follow-up within 30 days is associated with a slightly lower percentage of subsequent hospitalizations (34.1% vs 37.3%, respectively; P = .01), indicating some protective effect for these more-severe crises for patients seen within 30 days.
This study has several limitations to consider. Although administrative claims analyses can capture the number of outpatient follow-up visits, 22 they cannot assess the quality of the visits; it is possible that high-quality visits might reveal different results. ICD-9-CM and ICD-10-CM codes may be limited in their sensitivity for correctly identifying all patients with mental health diagnoses. This may have led to omission of patients from the population (likely those with less-severe illness) or omission of outpatient follow-up visits, although the latter may be curtailed by the HEDIS quality measure incentive to appropriately code for these visits. In addition, we do not have access to state identifiers, so we cannot assess geographical variations. Although the included states represent all regions nationally, our findings may not be generalizable to all states. Finally, we may not have been able to fully adjust for severity of illness or psychosocial complexity. Clinical data derived from electronic medical records may provide more extensive risk-adjustment variables. A future randomized trial to assess the effectiveness of an intervention to improve follow-up after hospitalization could more conclusively address this limitation.
In this study of Medicaid patients across 11 states, we found that more than one-third of children with a mental health hospitalization did not receive care that aligns with the national quality measure of follow-up within 7 and 30 days post discharge. Adherence to the quality measure varied by patient and hospital characteristics. In addition, adherence was associated with an increased risk of a subsequent mental health crisis, even after controlling for severity of illness. Implications of these findings are that targeted interventions are needed to address lower rates of follow-up for specific populations and that interventions for more-intensive symptom monitoring and outpatient treatment of crises may be needed to optimize outpatient care after hospitalization.
Drs Bardach and Coker contributed to study conceptualization and design, interpreted the results, drafted the initial manuscript, and revised the manuscript; Dr Doupnik assisted in study design, interpretation of results, and review of later versions of the manuscript; Mr Rodean assisted in statistical approach and analyses, interpretation of the results, and critical review of the manuscript; Drs Zima and Gay, Ms Nash, and Dr Tanguturi contributed to study design, interpretation of the results, and critical review of the manuscript; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FUNDING: No external funding.
confidence interval
Current Procedural Terminology
emergency department
Healthcare Effectiveness Data and Information Set
hazard ratio
International Classification of Diseases , Ninth Revision , Clinical Modification
International Classification of Diseases , 10th Revision , Clinical Modification
interquartile range
length of stay
Pediatric Medical Complexity Algorithm

Competing Interests
Supplementary data.
Advertising Disclaimer »
Citing articles via
Email alerts.

Affiliations
- Editorial Board
- Editorial Policies
- Journal Blogs
- Pediatrics On Call
- Online ISSN 1098-4275
- Print ISSN 0031-4005
- Pediatrics Open Science
- Hospital Pediatrics
- Pediatrics in Review
- AAP Grand Rounds
- Latest News
- Pediatric Care Online
- Red Book Online
- Pediatric Patient Education
- AAP Toolkits
- AAP Pediatric Coding Newsletter
First 1,000 Days Knowledge Center
Institutions/librarians, group practices, licensing/permissions, integrations, advertising.
- Privacy Statement | Accessibility Statement | Terms of Use | Support Center | Contact Us
- © Copyright American Academy of Pediatrics
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Clinical and Social Factors of Compulsory Psychiatric Treatment in Moscow
Aug 06, 2014
140 likes | 282 Views
Clinical and Social Factors of Compulsory Psychiatric Treatment in Moscow. Prof. Tsygankov Boris, MD, PhD Chief Psychiatrist of Moscow City, Head of the Department of Psychiatry, Addiction and Psychotherapy, Moscow State University of Medicine and Dentistry
Share Presentation
- outpatient service
- local intensive care emergency
- intensive care department
- phd department
- emergency service

Presentation Transcript
Clinical and Social Factors of Compulsory Psychiatric Treatment in Moscow Prof. Tsygankov Boris, MD, PhD Chief Psychiatrist of Moscow City, Head of the Department of Psychiatry, Addiction and Psychotherapy, Moscow State Universityof Medicine and Dentistry Dr. SavelievDmitri, MD, PhD Department of Psychiatry, Station of Ambulance and Emergency Medical Service named after A.S. Puchkov, Moscow, Russia & Dr. Yaltonskaya A., MD, PhD
Prevalence of mental disorders in Moscow
Mental Health Care System in Moscow • Outpatient service – Psychiatric Dispensaries • Inpatient service – Psychiatric Hospitals • Emergency service - Station of Ambulance and Emergency Medical Servicenamed after Puchkov • Number of psychiatrists working in Moscow: 1466 –total amount offull time positions 1198 –number of occupied positions
Number of beds in mental hospitals (1981-2014) Total: 1981 – 16 565 2009 - 13 857 2013 - 12 309 2014 - 10 499
Reform in Mental Health Care System in Moscow since 2012 • Main purpose is to develop better connection between outpatient and inpatient psychiatric services • Focus on providing more help out-patiently through the active work of dispensaries (Day/Night Hospital, House Calls) • Focus on inclusion families into help (through education and increasing the level of legal responsibilities)
Preliminary results of the reform • Local Emergency Psychiatric Service in each dispensary was organized. • Main purpose –to provide help to patients with relapses of psychotic disorders at evening/night time • Includes: House Calls, Day/Night Hospitals, Local Intensive Care/Emergency Services with further referral to a local psychiatrist • As a result significant decrease the amount of calls into Emergency Psychiatric Services (after first 2 moths) that allowed to decrease the amount of beds into psychiatric hospitals by 40%.
Emergency Psychiatric Service • Part of General Emergency Service provided by Station of Ambulance and Emergency Medical Service named after Puchkov • 24 hours • Receiving and reacting to a phone calls • Service provided by psychiatrists.They make decision about necessary actions and provide consultations to a) staff from hospitals and other medical settings, b) ambulances c) people
Emergency Psychiatric Service (2) • 24 emergency psychiatric medical teams (1 psychiatrist + 2 psychiatricparamedics) • 12 emergency psychiatricparamedical teams (for transporting psychiatric patients) (2 psychiatric paramedics) • 8 stations located in the different areas of Moscow Each team uses fully equipped modern ambulance car (Mercedes) with GPS navigation, on-line connection with the head office, medical equipment necessary for providing intensive care.
Location of stationsin different areas of Moscow
Steps after arrival of psychiatric team to a patient Upon arrival psychiatrist makes a decision about the necessity to provide psychiatric examination (art. 23, 24 «Psychiatric Assistance and Civil Rights Act») Sometimes in difficult cases Emergency Nursing Teams provide transportation of psychiatric patients (for example, to Intensive Care Department of General Hospitals). Reasons for psychiatric examination EXIST (voluntary or non-voluntary examination) Reasons for psychiatric examination DO NOT EXIST • Hospitalization in Psychiatric Clinic (voluntary or non-voluntary art. 28, 29) • Hospitalization in General Hospital (Psychosomatic ward) • Provide medical help • Provide consultation • Refer to a local psychiatrist (active referral to a dispensary)
Main indicators of performance 39% - receives help during 20 minutes 68% - during 30 minutes 95% - during 60 minutes
Number of attendances and hospitalizations
Conclusion • Reform of mental care system has a positive effect: • Decrease loading on psychiatric hospitals and Emergency Psychiatric Service • Increase in number of staff and material well-being • Problems: - Poorly developed connection of outpatient and inpatient service
- More by User
Clinical interview: psychiatric history and mental status
Clinical interview: psychiatric history and mental status. prof. MUDr. Eva Češková, CSc. Dept. of Psychiatry, Masaryk University , Brno. Clinical interview: psychiatric history and mental status. general introduction choosing a place and meeting the patient
1.67k views • 16 slides
COMPULSORY PSYCHIATRIC TREATMENT RISKY BUSINESS Mary O Hagan
WHAT IS COMPULSION? . Mental health legislation establishes the circumstances in which a person with
406 views • 24 slides
The Role of Clinical Pharmacists in Outpatient Psychiatric Clinics
The Role of Clinical Pharmacists in Outpatient Psychiatric Clinics. Mary A. Gutierrez, Pharm.D., BCPP Associate Professor of Clinical Pharmacy University of Southern California School of Pharmacy Clinical Pharmacist Medication Follow-up & Education Clinic
455 views • 8 slides

TRANSFORMATION JOURNEY OF TREATMENT AND REHABILITATION PROGRAMS IN MALAYSIA: COMPULSORY OPEN AC
TRANSFORMATION JOURNEY OF TREATMENT AND REHABILITATION PROGRAMS IN MALAYSIA: COMPULSORY OPEN ACCESS SERVICES. CURE & CARE. DR. SANGEETH KAUR NATIONAL ANTI DRUGS AGENCY MINISTRY OF HOME AFFAIRS MALAYSIA.
311 views • 0 slides
PSYCHIATRIC NURSING Psychiatric treatment approaches
PSYCHIATRIC NURSING Psychiatric treatment approaches. Dr. Naiema Gaber El-sayed. Learning Objectives. Determine the components of Psychiatric treatment approaches. Discuss the mechanism of action of each modality Explain the nursing role in each modality .
4.77k views • 51 slides
Factors of Social Change
Factors of Social Change. Ms. Ireland HSB4M. “Everyone over the age of forty is an immigrant” – Margaret Mead. Social Change: Changes the way in which society is organized, and the beliefs and practices of the people who believe in it
4.38k views • 13 slides
The Role of Cultural Factors in Psychiatric Diagnoses
The Role of Cultural Factors in Psychiatric Diagnoses. Marianne Kastrup Centre Transcultural Psychiatry Copenhagen New Directions in Psychiatry Sorrento May 2012. Culture and Diagnosis. Faced with patients of your own cultural background, cultural aspects rarely interfere in assessment
1.37k views • 111 slides
Social Factors of Motivation
Social Factors of Motivation . Topics. Social Facilitation Social Loafing Conformity Obedience Roles . Walk around the C-hall . 1) Individually 2) Partner Timed . Social Facilitation/Interference . Personal examples Chopsticks activity Connections to motivation? .
306 views • 11 slides
Handover and Clinical Human Factors
Web Ex November 3 rd 2011. Handover and Clinical Human Factors. Matt Inada-Kim Acute Medicine Lead, WEHCT, NHS South Central Patient Safety Federation Sepsis Project Lead Fellow NHS III, Advocate of CHFG. Why is this important ?. Safety Critical To allow Continuity Patient Journey
417 views • 24 slides
Russian Children’s Clinical Hospital Moscow
PECULIARITY OF MYCOBACTERIAL INFECTION IN PRIMARY IMMUNODEFICIENCY PATIENTS ( SINGLE CENTER STUDY) E.V. Galkina, I.V. Kondratenko. Russian Children’s Clinical Hospital Moscow. The overspread of Mycobacterial Infection in Russian population. The overspread of Mycobacterial
262 views • 9 slides
Social and Cultural factors in depression
Social and Cultural factors in depression. By Dominic and Tobi. Etiology. The causes and origins of a disease or medical condition. Brown and Harris (1978). Conducted a study to find the social origins of depression in women
617 views • 10 slides
Clinical prognostic factors
ESMO 21. September 2009 Berlin Germany. Clinical prognostic factors. Claus-Henning Köhne Klinik für Onkologie und Hämatologie. Survival of patient with metastatic CRC over decades Censored for patients with liver resection. Kopetz et al. JCO 2009.
489 views • 32 slides
PSYCHIATRIC NURSING Psychiatric treatment approaches. Dr. Naiema Gaber El-sayed. Learning Objectives. Determine the components of Psychiatric treatment approaches. Discuss the mechanism of action of each modality Explain the nursing role in each modality.
734 views • 26 slides
Psychiatric illnesses in Children and Adolescents: types and treatment
Psychiatric illnesses in Children and Adolescents: types and treatment. Lee W. Bradshaw APRN-BC McKay-Dee Behavioral Health Institute. Types of illnesses:. Depression Bipolar disorder Anxiety disorders ADHD. PHYSICAL Genetics: in the family Brain chemistry -autopsy studies
600 views • 35 slides
Intervention Modes ‑ Psychiatric Treatment
Intervention Modes ‑ Psychiatric Treatment.
656 views • 31 slides
Psychiatric Treatment
Aathmik provides Psychiatric Treatment to intermingle people to normal productive life and cope with life's inevitable challenges in positive sense
134 views • 8 slides

Treatment of Psychiatric and Schizophrenia - SlideShare
Define and Introduce Schizophrenia, Why rehabilitation required, explains treating schizophrenia. We provide Schizophrenia, Alzheimer’s Dementia, Elderly Care treatment Centre in India. For more details visit us http://www.jagrutirehab.org/schizophrenia.html or contact us: 020-69333220/ 9371425026
182 views • 6 slides
Eating disorders Compulsory Treatment?
Eating disorders Compulsory Treatment?. Dr Yvonne Edmonstone. Questions?. Are criteria for compulsory treatment met? What constitutes medical treatment? Nutrition by artificial means without consent v Forcible feeding? Any special safeguards?. Ros. 24yr old single unemployed living parents
217 views • 21 slides
Lee Weiss’ Urban Recovery Center Offers Clinical and Psychiatric Treatment in New York
Lee Weiss, the CEO of Elev8 Center is a Credentialed Alcoholism and Substance Abuse Counselor who has also been a speaker and panelist at the New York Health Care Summit in 2019 and 2018. He is also the director of the Elev8 Foundation and the manager of the Urban Recovery Center in Brooklyn, NY. The patients at Urban Recovery are made to go through an assessment to understand the root cause of their addictive behaviors. The professionals help the patients move from understanding the gravity of the behavior to a recovery path that may include residential treatment, intensive outpatient treatment, and therapy. The team also conducts deep immersion therapy where they visit your home, work, place of leisure, and more to work on the trigger points.
75 views • 6 slides
US Widens Sanctions on Russia to Discourage Countries Such as China From Doing Business With Moscow
The United States has widened its sanctions against Russia as G7 leaders prepare to gather in Italy for a summit where top priorities will be boosting support for Ukraine and grinding down Russia’s war machine

Susan Walsh
National Security Council spokesman John Kirby speaks during the daily briefing at the White House in Washington, Tuesday, May 28, 2024. (AP Photo/Susan Walsh)
The United States widened its sanctions against Russia Wednesday as G7 leaders prepared to gather in Italy for a summit where the top priorities will be boosting support for Ukraine and grinding down Russia’s war machine.
Wednesday's package targeted Chinese companies which help Russia pursue its war in Ukraine and raised the stakes for foreign financial institutions which work with sanctioned Russian entities.
It also targeted Russia’s financial infrastructure, in an attempt to limit the amount of money flowing in and out of Russia. Shortly after the sanctions were made public, the Moscow Exchange announced it would suspend transactions in dollars and euros.
The U.S. has sanctioned more than 4,000 Russian businesses and individuals since the war began, in an effort to choke off the flow of money and armaments to Moscow, whose superior firepower has given it an advantage on the battlefield in recent months. Nonetheless, new companies continually pop up as Russia attempts to rework supply chains.
“We have to be very honest with ourselves that Putin is a very capable adversary who is willing to adapt and find those willing collaborators,” Aaron Forsberg, the State Department’s Director for Economic Sanctions Policy and Implementation, told The Associated Press.
Sanctions against Russia, he said, are therefore a “dynamic affair.”
That includes listing addresses for the first time in a bid to crack down on companies reopening at the same address under a different name.
While sanctions have not stopped the flow of illicit goods, the aim is to make it harder for Russia to source crucial technology as well as drive up the markup on the goods. Wednesday's package targets more than $100 million in trade between Russia and suppliers for its war.
More than 300 new sanctions are largely aimed at deterring individuals and companies in countries including China, the United Arab Emirates and Turkey from helping Moscow circumvent Western blocks on obtaining key technology. They also threaten foreign financial institutions with sanctions if they do business with almost any sanctioned Russian entity, underscoring the U.S. view that the Kremlin has pivoted the Russian economy to a war footing .
Russia’s military is “desperate for access to the outside world,” said Treasury Secretary Janet Yellen.
The announcement came shortly before President Joe Biden arrived in Italy where he and other G7 leaders are urgently looking at aiding Ukraine, including turning frozen Russian assets into billions of dollars of support for Kyiv.
Seven Chinese and Hong-Kong-based companies were targeted Wednesday for shipping millions of dollars of material to Russia, including items which could be used in Russian weapons systems.
U.S. officials say China is the leading supplier of critical components to Russia, supplying both Chinese and Western technology.
On Wednesday the U.S. sanctioned a Chinese state-owned defense company which officials said had shipped military equipment for use in the Russian defense sector.
The move sends the message that the U.S. is “willing to wade into more treacherous territory” by increasing the pressure on the Chinese government, said Benjamin Hilgenstock, senior economist at the Kyiv School of Economics.
“We will address (China's) support for the Russian defense industrial base. And we will confront China’s non-market policies that are leading to harmful global spillovers," White House national security spokesman John Kirby told reporters Tuesday.
China did not sanction Russia after President Vladimir Putin invaded Ukraine, and Putin ended a visit to China in May by emphasizing the two countries' burgeoning strategic ties.
“The Chinese leadership is not interested in making these sanctions a success,” said Janis Kluge, a Russia sanctions specialist at the German Institute for International and Security Affairs in Berlin (SWP.)
Beijing, Kluge said, is reluctant to stop a valuable trade that is worth large amounts of money and it does not want to “add to the pressure on Putin in this war."
Imports from China are vital to Russia because Beijing is a major producer of critical components, including for Western companies. Chinese companies also act as intermediaries for the sale and shipment of Western components to Russia.
But while Chinese technology has been found on the battlefield in Ukraine, most of the components still come from Western nations including those which are “overwhelmingly” found in high-tech drones and ballistic missiles, said Hilgenstock.
As well as China, the U.S. targeted businesses in Turkey and the United Arab Emirates which officials said sent high-priority items to companies in Russia, including to businesses which were already sanctioned.
In December, the White House said foreign financial institutions could be sanctioned if they worked with entities in Russia's defense sector. Wednesday's expansion of sanctions now means that those institutions could face such measures if they work with almost any sanctioned Russian entity.
U.S. President Joe Biden’s top foreign policy adviser, Jake Sullivan, told reporters on the way to the G7 that the message to China and other countries was that they are “at serious risk of running afoul of the Treasury Department and falling under a sanctions regime.”
The fear of triggering secondary sanctions is an effective threat, analysts said.
While President Xi Jinping may not want to facilitate Western sanctions on Russia, “Chinese banks have always been very careful not to become a target of secondary sanctions because it would be very costly,” Kluge said, pointing to cases where Chinese banks have ended relationships with Russian customers.
The package also aims to hobble the development of Russia’s energy sector and future sources of cash , including Arctic liquified natural gas projects which have been shipped critical LNG technology by a Chinese company.
In addition, the package targeted people involved in the forced transfer and deportation of Ukrainian children to Russia. Five people in Russia and Russian-occupied Ukraine were sanctioned after participating in the forced militarization and reeducation of the children and providing them with Russian passports.
AP White House Reporter Colleen Long aboard Air Force One contributed to this report
Copyright 2024 The Associated Press . All rights reserved. This material may not be published, broadcast, rewritten or redistributed.
Photos You Should See - June 2024

Join the Conversation
Tags: Associated Press , business , politics , world news
America 2024

Healthiest Communities
Your trusted source for in-depth analysis on the issues impacting your community’s well-being delivered right to your inbox.
Sign in to manage your newsletters »
Sign up to receive the latest updates from U.S News & World Report and our trusted partners and sponsors. By clicking submit, you are agreeing to our Terms and Conditions & Privacy Policy .
You May Also Like
The 10 worst presidents.
U.S. News Staff Feb. 23, 2024

The Best Cartoons on Donald Trump
June 14, 2024, at 4:08 p.m.

Joe Biden Behind The Scenes
June 7, 2024

DOE Probe Dings 2 Universities
Lauren Camera June 17, 2024

Record-Breaking Heat to Hit the U.S.
Cecelia Smith-Schoenwalder June 17, 2024

Explainer: Social Media Warning Labels
Laura Mannweiler and Steven Ross Johnson June 17, 2024

The Week in Cartoons June 17-21
June 17, 2024, at 3:50 p.m.

Biden Asks: Convicted Criminal or Me?

Retail Sales, Housing Data on Tap
Tim Smart June 17, 2024

SCOTUS Nixes Bump Stock Ban
Laura Mannweiler June 14, 2024

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Wiley Open Access Collection

Stability of diagnostic coding of psychiatric outpatient visits across the transition from the second to the third version of the Danish National Patient Registry
Martin bernstorff.
1 Department of Affective Disorders, Aarhus University Hospital – Psychiatry, Aarhus Denmark
2 Department of Clinical Medicine, Aarhus University, Aarhus Denmark
Lasse Hansen
Erik perfalk, andreas aalkjær danielsen, søren dinesen Østergaard, associated data.
Due to restrictions in Danish law for protecting patient privacy, the data used in this study is only available for research projects conducted by employees in the Central Denmark Region following approval from the Legal Office under the Central Denmark Region (in accordance with the Danish Health Care Act §46, Section 2). However, similar data can be accessed through Statistics Denmark. Danish institutions can apply for authorization to work with data within Statistics Denmark, and such organisations can provide access to affiliated researchers inside and outside of Denmark.
In Denmark, data on hospital contacts are reported to the Danish National Patient Registry (DNPR). The ICD‐10 main diagnoses from the DNPR are often used as proxies for mental disorders in psychiatric research. With the transition from the second version of the DNPR (DNPR2) to the third (DNPR3) in February–March 2019, the way main diagnoses are coded in relation to outpatient treatment changed substantially. Specifically, in the DNPR2, each outpatient treatment course was labelled with only one main diagnosis. In the DNPR3, however, each visit during an outpatient treatment course is labelled with a main diagnosis. We assessed whether this change led to a break in the diagnostic time‐series represented by the DNPR, which would pose a threat to the research relying on this source.
All main diagnoses from outpatients attending the Psychiatric Services of the Central Denmark Region from 2013 to 2021 ( n = 100,501 unique patients) were included in the analyses. The stability of the DNPR diagnostic time‐series at the ICD‐10 subchapter level was examined by comparing means across the transition from the DNPR2 to the DNPR3.
While the proportion of psychiatric outpatients with diagnoses from some ICD‐10 subchapters changed statistically significantly from the DNPR2 to the DNPR3, the changes were small in absolute terms (e.g., +0.6% for F2—psychotic disorders and +0.6% for F3—mood disorders).
The change from the DNPR2 to the DNPR3 is unlikely to pose a substantial threat to the validity of most psychiatric research at the diagnostic subchapter level.
Significant outcomes
- A significant administrative change in diagnostic coding of psychiatric outpatient treatment in Denmark did not induce marked destabilisation in the incidence of psychiatric diagnoses or the number of diagnoses received by each patient.
- In the DNPR3, most outpatient treatment courses are labelled with the same main diagnosis (subchapter level) at the first and last visit.
Limitations
- Analyses were performed on data from the Central Denmark Region. While the administrative change was at the national level, and results should generalise, this is not testable from these data.
- Data was obtained from the Business Intelligence Office. While this source receives data from the same source as the Danish National Patient Registry, replication should be carried out using national data from the Danish National Patient Registry.
1. INTRODUCTION
Danish registries are widely used in psychiatric research. 1 , 2 , 3 One such registry, the Danish National Patient Registry (DNPR), contains information on emergency treatment, admissions and outpatient visits for all Danish residents and all public hospitals in Denmark. 1 In the DNPR, the registered main diagnosis—coded according to the International Classification of Diseases, 10th revision 4 —represents the condition leading to a specific hospital contact. The validity of the main diagnoses is well established and they are widely used as either exposure‐, confounder‐ or outcome variables in psychiatric research. 1 , 5 , 6 , 7
With the transition from the second version of the DNPR (DNPR2) to the third (DNPR3), which occurred in the period from February 2nd to March 3rd 2019 across the five Danish Regions, the way main diagnoses are coded in relation to outpatient treatment changed substantially (see Figure 1 for an illustration). 8 Specifically, under the DNPR2 paradigm, all visits in a treatment course ‘inherited’ the final main diagnosis, which should be representative of the entire treatment course. With the introduction of the DNPR3, however, coding instructions were updated. Since then, every single outpatient visit has been coded with a main diagnosis to cover that specific visit only. As a result, the main diagnosis under the DNPR3 is based on the—sometimes limited—clinical information available at the time of each visit, rather than the complete information available at the end of the treatment course.

Number of unique diagnoses assigned for a psychiatric outpatient treatment course under the DNPR2 and DNPR3 eras, respectively. During the DNPR2 era, when a series of visits was reported to the DNPR2 , the final main diagnosis was used to overwrite the main diagnoses of all previous visits in the same treatment course. This was no longer the case after the transition to the DNPR3 , which can result in differences in the number of main diagnoses assigned for identical treatment courses. In this example, it results in more unique diagnoses pr. treatment course. In the example, F3 , F4, and F6 refers to diagnostic categories in the mental disorder chapter of the ICD ‐10. F3 : Mood disorders. F4 : Neurotic, stress‐related and somatoform disorders. F6 : Disorders of adult personality and behaviour
The change in diagnostic coding practice outlined above may have led to a destabilisation/break in the diagnostic time‐series represented by the DNPR, which would pose a significant threat to the many psychiatric research activities that rely on the main diagnoses, including our ongoing work based on data from the PSYchiatric Clinical Outcome Prediction (PSYCOP) cohort. 9 Indeed, if patients are assigned a broader range of diagnoses in the DNPR3 compared to the DNPR2, the population‐adjusted incidence of most diagnoses will go up, without reflecting a true increase in morbidity. However, whether such a destabilisation has indeed occurred remains unexplored. Therefore, we examined the stability of diagnostic coding of psychiatric outpatient treatment across the DNPR2–DNPR3 transition at three levels: (i) at the level of the psychiatric ICD‐10 subchapters (e.g., F2—psychotic disorders and F3—mood disorders), (ii) at the level of a connected series of outpatient visits, that is, whether the diagnosis changed from the first to the last visit in an outpatient treatment course, and (iii) at the level of the individual, that is, whether the number of different diagnoses assigned to each patient was stable. Furthermore, we examined two strategies for maintaining comparability across the DNPR2–DNPR3 transition: Specifically, we recoded all visits in relation to an outpatient treatment course in the DNPR3 era with either the most ‘ severe ’ diagnosis in the series of visits or with the final diagnosis in the series of visits, respectively.
2.1. Population and data
For the period from January 1, 2013, to June 1, 2021, we extracted the main diagnoses for all in‐ and outpatient visits to the Psychiatric Services of the Central Denmark Region—one of five Danish Regions—with a catchment population of approximately 1.3 million people covered by five psychiatric hospitals. Data was acquired from the Business Intelligence Office in the Central Denmark Region, resulting in the most up‐to‐date information available. The Business Intelligence Office and the DNPR receive data from the same source, namely the Electronic Health Record system used by all hospitals in the Central Denmark Region (MidtEPJ). This source contains data from the 30th of May 2011 and onwards. However, as the psychiatric hospitals in the Central Denmark Region were gradually onboarded to MidtEPJ, the data from the first 2 years had unstable proportions of diagnostic codes that are unlikely to reflect general instability in the coding (see Figure S1 ). Therefore, data from the time prior to January 1st 2013 were excluded for further analyses.
2.1.1. Definition of psychiatric outpatient visits
We only examined psychiatric outpatient visits for the primary analyses, as the change in diagnostic coding with the DNPR3 should only affect the practice concerning this type of visits. We considered a visit to be outpatient if it was a physical visit with the patient‐type variable set to ‘outpatient’. Importantly, our data source allows this definition to be transferred through to the DNPR3 era as the Central Denmark Region has maintained the patient‐type classification across the DNPR2–DNPR3 transition. In the Supplementary Material, we show how other researchers can mimic our classification of outpatient visits using DNPR3 data from the DNPR only (see Tables S1–S5 ). Furthermore, we labelled a visit as psychiatric if it took place in a psychiatric department, corresponding to a ‘hospital‐department‐classification – section’ (SHAK_AFS) matching 6600*. This definition is specific to the Central Denmark Region, but, as for outpatient status above, other researchers can mimic our classification of psychiatric using DNPR3 data from the DNPR only (Tables S6 and S7 ). We considered outpatient visits to be part of a connected treatment course in the DNPR3 era if they had the same unique course‐element‐identifier (in Danish DNPR3‐terminology: ‘forløbselement‐id’). The course‐element‐identifier covers patient‐activities related to the same treatment course at the same department (for more details, see Table S8 ). Furthermore, since the treatment courses defined by the course‐element‐identifier in the DNPR3 era are not directly comparable to the treatment courses as defined in the DNPR2 (see Table S8 ), we also examined whether we could construct treatment courses for the DNPR3 era that more closely resemble those from the DNPR2. Specifically, we performed supplementary analyses in which all visits by the same patient to the same outpatient clinic in the DNPR3 era were considered part of the same treatment course.
2.1.2. Mitigation strategies
We examined two mitigation strategies regarding the stability of main diagnoses from each ICD‐10 F‐subchapter (FX) across the transition from the DNPR2 to the DNPR3 eras. First, we coded all visits in a DNPR3 treatment course by the most ‘severe’ diagnosis, defined as the FX diagnosis with the lowest digit, except F1 (Substance abuse), which was considered the least severe. Second, we coded all visits in a DNPR3 treatment course with the final diagnosis from the course, mimicking the DNPR2 approach
2.2. Statistical analyses
- Stability of main diagnoses from each ICD‐10 F‐subchapter across the DNPR2–DNPR3 eras
As the main level of information in ICD‐10 chapter F (mental and behavioural disorders) is captured by the first digit (e.g., F0: Organic mental disorders; F1: Substance use disorders; F2: Psychotic disorders), we used the main diagnosis at this level for the primary analyses. Visits with a main diagnosis of F99 (Mental disorder, not otherwise specified) were excluded, as they were rare (0.11% of all outpatient visits) and not conceptually related to the other F9‐diagnoses (Behavioural and emotional disorders with onset usually occurring in childhood and adolescence). Visits were binned by 3‐month periods from the transition date and rounded to the nearest beginning of a quarter (e.g., the 2nd of February 2019 was rounded to the 2nd of November 2018, whereas the 3rd of February 2019 was rounded to the 3rd of May 2019). This ensured that the transition between the DNPR2 and the DNPR3 (2nd/3rd of February 2019) was placed at the transition point between two bins.
Population‐adjusted within‐quarter incidences were calculated for each F‐subchapter (FX) and each quarter using the equation below.
The numerator represents the number of patients with an outpatient visit that had a main diagnosis from the specific ICD‐10 F‐subchapter (FX), while the denominator represents the number of patients with any psychiatric outpatient visit in the same period. Visit s FX Q is the number of visits with a main diagnosis of FX during the quarter Q , Visit s Q is the number of visits during the quarter Q , and I R FX is the incidence rate of FX for the quarter Q . As the number of patients are counted within a quarter, time is implicit.
For each FX, we calculated p ‐values for the difference between the mean proportion of visits belonging to the category in the year prior to and the year after the transition from the DNPR2 to the DNPR3. We chose 1 year since window‐size and symmetry is a trade‐off. With too wide a window, any actual changes around the transition are likely to be obscured by noise from other factors. With too narrow a window, statistical power becomes a problem. Since each point in a time‐series is inherently dependent on the previous point, we used an autoregressive model with lag of one quarter. This allows for adjustment for the correlation within the time‐series and estimating the difference in means between the intervals after the adjustment.
To ensure that the change in diagnostic coding practice did not spill over to admissions (inpatient hospital stays), we examined these as well, using the same approach as outlined above. Since the diagnostic coding of admissions should be less affected (if at all) by the transition from the DNPR2 to the DNPR3, as admissions were/are to be coded with one single main diagnosis both in the DNPR2 and DNPR3, we did not expect to see any breaks in the diagnostic time series for admissions.
- 2 ii. Diagnostic stability during outpatient treatment courses in the DNPR3 era
To examine the diagnostic stability over outpatient treatment courses, visits were grouped by their unique course‐element‐identifier, and the first‐ and final diagnosis for the treatment course was computed. Diagnoses were truncated to their character‐digit (FX) combination. To examine to which extent the first diagnosis in a DNPR3 sequence matched the last, we generated tables showing the number of treatment courses with each first‐/last‐diagnosis combination at the FX level. We also visualised the level of stability with alluvial plots.
- 3 iii. Mean number of unique diagnoses per active outpatient treatment course across the DNPR2–DNPR3 eras
When counting main diagnoses at the level of the individual, diagnoses were truncated to the FXX‐level. We ran sensitivity analyses with truncation at one (FX), three (FXX.X), and four (FXX.XX) digits. We also tested the difference between means of the year prior to‐ and the year after the DNPR2–DNPR3 transition using an autoregressive model with lag of 1 quarter. Here, we considered a treatment course to be terminated 180 days after the last registered visit.
- 4 iv. Incident diagnoses by subchapter across the DNPR2–DNPR3 eras
We also examined the incidence of diagnoses by subchapter (FX). Specifically, each patient's known diagnoses were aggregated from January 1st 2013 to December 31st 2016. Any visit thereafter with a, to the patient, new diagnosis, was considered incident. In keeping with the main analyses mentioned above, we then calculated the mean number of incident diagnoses (by subchapter) per quarter. We then compared the means in the year before to the year after the transition using Z ‐tests.
The threshold for statistical significance was set at 0.05. All p ‐values were corrected for multiple comparisons using the method of Benjamini and Hochberg. 10 All analyses were carried out using R ( www.r-project.org ) and the code used for the analyses is available at: https://github.com/Aarhus‐Psychiatry‐Research/diagnostic‐stability‐lpr2‐lpr3/ .
2.3. Ethics
This study was carried out to ensure the validity/stability of the data used for studies based on the PSYCOP cohort. 9 The use of electronic health records from the Central Denmark Region was approved by the Central Denmark Region Legal Office per the Danish Health Care Act §46, Section 2. According to the Danish Committee Act, ethical review board approval is not required for studies based solely on data from electronic health records (waiver for this project: 1‐10‐72‐1‐22). All data were processed and stored in accordance with the European Union General Data Protection Regulation and the project is registered on the internal list of research projects having the Central Denmark Region as the data steward.
Data from 100,501 outpatients with a total of 2,331,427 outpatient visits were analysed. The median age of the patients at the time of the first contact to the psychiatric services in the period from January 1st 2013 to June 1st 2021 was 27.6 years (25–75 percentiles: 17.0; 47.0 years) and 51.4% of the patients were women. The median number of outpatient visits per patient was 11 (25–75 percentiles: 4; 25).
Table 1 and Figure 2 show that while the transition from the DNPR2 to the DNPR3 was associated with statistically significant changes in diagnostic proportions for 4 out of 10 ICD‐10 subchapters (FX), for all subchapters, these changes were small on an absolute scale (e.g., +0.6% for F2—Psychotic disorders and +0.6% for F3—Mood disorders). Figure 2 also shows that the variation in diagnostic proportions across quarters prior to‐ and after the DNPR2–DNPR3 transition was approximately the same. It appears from Figure 2B that subchapter F8 (developmental disorders incl. autism) experienced the largest break in the time‐series at the DNPR2–DNPR3 transition, which was, however, small in absolute terms (1.2%).
Relative and absolute changes in proportions of visits belonging to each diagnostic subchapter in the 1 year prior to‐ and after the DNPR2 to DNPR3 transition

Proportion of outpatients in each quarter with a within‐quarter incident main diagnosis by ICD ‐10 subchapter. (A) y ‐scale is standardised across panels. (B) y ‐scale is allowed to vary between panels. Proportion of all outpatients in each quarter that received a main diagnosis from each ICD‐10 F‐subchapter. Line ranges reflect 95% confidence intervals. The date of transitioning from DNPR2 to DNPR3 is highlighted with a grey vertical line. The light grey areas represent the time intervals included in the statistical analyses. Asterisks reflect p < 0.05 for the slope of an autoregressive model of lag 1 with pre‐ and post‐transition as the independent variable, using data 1 year prior to‐ and after the transition (see methods for further elaboration). Mitigation strategies represent recoding each treatment course with the most ‘severe’ diagnosis, or with the final diagnosis from the treatment course. Visits were considered part of the same treatment course if they had the same course‐element‐identifier (see Table S8 for further details)
Applying the mitigation strategies (most severe‐ or last diagnosis) resulted in destabilisation for most subchapters, creating larger breaks in the diagnostic time‐series at the transition from the DNPR2 to the DNPR3 compared to the unmanipulated/unchanged data (Figure 2 ).
Considering visits to be part of the same treatment course only if they were to the same outpatient clinic, yielded similar levels of stability as in the primary analyses (see Figure S2 ). Since only outpatient visits should be affected by the change in diagnostic coding from the DNPR2 to the DNPR3, we examined the main diagnoses assigned in relation to inpatient treatment/admissions as a ‘negative control’. These diagnostic time‐series also appeared stable (see Figure S3 ).
- ii. Diagnostic stability during outpatient treatment courses in the DNPR3 era
Figure 3 visualises the high diagnostic stability of the psychiatric outpatient treatment courses in the DNPR3. For more than 90% of the outpatient treatment courses, the main diagnosis assigned in relation to the first and final visit came from the same ICD‐10 subchapter (see Figure 3 and Table S9 ). For only three diagnostic subchapters did the first and final diagnosis match for less than 90% of the outpatient treatment courses, namely F1—substance abuse (78.3%), F3—mood disorders (87.6%) and F8—developmental disorders (88.4%) (Table S9 ).
- iii. Mean number of unique diagnoses per outpatient treatment course across the DNPR2–DNPR3 eras

Alluvial plot showing the diagnostic stability of outpatient treatment courses in the DNPR3 era. Visits were considered part of the same treatment course if they had the same course‐element‐identifier (see Table S8 for further details). The thickness of lines is proportional to the number of outpatient treatment courses. Separated into first diagnosis (left) and final diagnosis (right). Colours reflect the subchapter of the final diagnosis. For exact counts and proportions, see Table S9
Figure 4 shows the mean (quarterly) number of unique diagnoses per outpatient treatment course across the DNPR2–DNPR3 eras. At the FXX‐level, there was no statistically significant change in the mean number of unique diagnoses per treatment course from the year prior to the DNPR2–DNPR3 transition (mean = 0.77) to the year after (mean = 0.74) (Figure 4A ). However, there was larger variation between quarters in the year after the DNPR2–DNPR3 transition compared to the year before (SD Unmitigated DNPR2 = 0.023, SD Unmitigated DNPR3 = 0.045). We also observed periodicity, with a drop in every 3rd quarter, reflecting a lower number of outpatient visits during the summer holiday in July/August. The lack of statistically significant changes was consistent across levels of diagnostic truncation (FX, FXX.X, and FXX.XX—see Figure 4A ). Both mitigation strategies (most severe and final diagnosis trumping all other, respectively) worsened this contrast by excessively lowering the number of diagnoses per treatment course in the year after the DNPR2–DNPR3 transition (mean Primary analysis = 0.77, mean Most severe = 0.68, and mean Final visit = 0.68) (Figure 4B ). When considering visits to be part of a treatment course only when they were to the same outpatient clinic, both mitigation strategies decreased the mean number of unique diagnoses, but not to the point of statistical significance (Figure 4B ).
- iv. Incident diagnoses by subchapter across the DNPR2–DNPR3 eras

Mean number of unique psychiatric main diagnoses per active treatment course. Visits were considered part of the same treatment course if they had the same DNPR3 course‐element‐identifier (see methods or Table S1 for further detail). A treatment course was considered active up until 180 days after the last recorded visit. The transition date from DNPR2 to DNPR3 is marked with a grey vertical line. The light grey areas represent the time intervals included in the statistical analyses. Asterisks reflect p < 0.05 for the slope of an autoregressive model of lag 1 with pre‐ and post‐transition as the independent variable, using data 1 year prior to‐ and after the transition. Mitigation strategies represent recoding a treatment course with the most ‘severe’ diagnosis, or with the final diagnosis from a sequence. (A) By levels of truncation of the ICD‐10 diagnostic codes and (B) By mitigation strategy truncated at ICD‐10 level FXX
Figure S4 shows the mean number of incident diagnoses by subchapter across the DNPR2–DNPR3 transition. While there was some variation around the transition point, this was mostly transitory, and for most subchapters, the means for LPR2 and LPR3 were similar (see Figure S4 and Table S10 ). No subchapters experienced changes that were statistically significant after adjusting for multiple comparisons.
4. DISCUSSION
In this cohort study based on data from all in‐ and outpatient visits to the Psychiatric Services of the Central Denmark Region in the period from January 1, 2013, to June 1, 2021, we showed that the transition from the DNPR2 to the DNPR3 only caused a minor destabilisation in the diagnostic time‐series for the psychiatric ICD‐10 subchapters. Furthermore, we found that main diagnoses assigned in relation to outpatient treatment courses in the DNPR3 era were quite stable from beginning (first visit) to end (last visit). At the level of the individual patient, there was no substantial or statistically significant change in the number of diagnoses per outpatient treatment course across the DNPR2–DNPR3 transition, but an increase in the variability in the DNPR3 era.
To our knowledge, this is the first study of the stability of diagnostic coding after the transition to the DNPR3 and it therefore contributes with novel information. The shift from the DNPR2 to the DNPR3 is the first major administrative shift of the diagnostic coding practice in Denmark since the ICD‐10 replaced the ICD‐8 in 1994. 1 We have searched the literature for reports of similar administrative shifts in national patient registries, but found none. A recent review of health registries in the Nordic countries 11 covered the validity of the diagnoses in these registries, without mentioning administrative changes, including that from the DNPR2 to the DNPR3. We therefore contacted representatives from the national patient registries in other Nordic countries (Sweden, Norway, Finland, and Iceland) to inquire whether administrative shifts in diagnostic coding, comparable to that from the DNPR2–DNPR3 transition, had been made in recent times. Representatives from Norway, Finland, and Iceland reported that there had been no administrative changes in diagnostic coding in the national patient registries. The representative from Sweden, however, pointed to an administrative change in 2015 regarding the registration of specialised outpatient visits. Prior to 2015, every specialised outpatient visit (e.g., to an emergency room) that subsequently led to an inpatient visit was only registered as an inpatient visit. After 2015, however, it was registered as two separate visits, one outpatient and one inpatient, leading to an increase in the number of registered outpatient visits. Thus, if basing an analysis solely on data from outpatient visits in Sweden, the 2015 administrative change would lead to an increase in the number of ‘cases’ without an actual increase in morbidity. 12
Overall, our analyses showed that the change in diagnostic coding accompanying the transition from the DNPR2 to the DNPR3 only had a minor impact on the stability of the diagnostic time‐series as well as on the population‐adjusted within‐quarter incidence of psychiatric diagnoses. This should offer some optimism regarding the validity of future psychiatric epidemiological studies using the DNPR as data source. We did, however, observe increased variability in the number of unique psychiatric main diagnosis per active treatment course after the transition from the DNPR2 to the DNPR3. For an increase in variance to occur without a change in the mean, there must be a simultaneous increase (i) in the proportion of treatment courses with a high number of diagnoses, and (ii) in the proportion of treatment courses with a low number of diagnoses. In fact, the COVID‐19 pandemic, which coincided with the observed increased variability, may have led to such a change in the pattern of contacts/diagnoses. Studies from Danish Psychiatric Services have suggested that the COVID‐19 pandemic has caused some patients to exhibit new symptoms (e.g., anxiety), 13 , 14 , 15 while also resulting in patients withdrawing from (or their appointments being cancelled by) the healthcare system, leading to fewer diagnoses. 16 , 17 If this is the explanation, the increased variability may be transitory and return to the base level as the pandemic comes to an end. Other societal‐ and patient‐level changes than the COVID‐19 pandemic, leading to the same contact/diagnostic pattern, could, however, also have played a role regarding the observed variability.
There are limitations to this study, which must be considered. First, we only had access to data from electronic patient records in the Central Denmark Region, provided by the regional Business Intelligence Office. While this is ideal for the purpose of ensuring diagnostic stability in relation to research based on this data source, 9 one could argue that it is not identical to data from the DNPR. However, given that the DNPR and the Business Intelligence Office in the Central Denmark Region receive data from the same source, this is unlikely to affect our results. Second, and relatedly, because of the data source, we were unable to take premature terminations of treatment courses into account since we did not have information on emigration or death. However, given the relatively short windows (3 months in Figures 2 and and4), 4 ), that counts were reset for each course‐responsibility‐id in Figure 3 , and the, presumably, small number of deaths and emigrations, we do not believe this to be a major limitation. Third, the data for the present study stems solely from the Central Denmark Region, which could pose a problem with regard to generalisation to the national level. However, since reporting of diagnoses is based on national standards, it is very likely to generalise across the Danish regions. Fourth, this study only focused on the diagnostic stability in relation to treatment in the Psychiatric Services. However, since the change in diagnostic coding practice accompanying the transition from the DNPR2 to the DNPR3 was the same across all medical specialities in the Danish secondary healthcare sector, our results are likely to generalise to those as well, but this should be subjected to empirical testing. Fifth, while the main analytical level in this study, namely the F‐subchapters (FX), captures much information, there is heterogeneity within these chapters, one example being F32/33—unipolar depression and F30/F31—mania/bipolar disorder. It was, however, beyond the scope of this study to investigate the stability of each of the 71 different FXX diagnoses in the ICD‐10. Research groups working with data from the DNPR having particular emphasis on specific diagnoses should probably investigate the stability of those across the DNPR2–DNPR3 transition, as our results do not necessarily generalise to all FXX diagnoses (nor to diagnoses at even greater granular level, e.g., FXX.X and FXX.XX).
In conclusion, the change in diagnostic coding of psychiatric outpatient visits accompanying the transition from the DNPR2 to the DNPR3 did not appear to lead to substantial breaks in the diagnostic time‐series represented by the DNPR – at least not at the diagnostic subchapter level. Therefore, the change from the DNPR2 to the DNPR3 seems unlikely to pose a substantial threat to the validity of most psychiatric research based on this data source.
AUTHOR CONTRIBUTIONS
All authors have contributed to the design of the study. The analyses for this paper were mainly carried out by Martin Bernstorff, with significant contributions by Lasse Hansen. The results were interpreted by all authors. Martin Bernstorff wrote the main draft of the manuscript, with significant revisions for important intellectual content from all authors. All authors approved the final version of the manuscript prior to submission.
FUNDING INFORMATION
The study is supported by grants from the Lundbeck Foundation (grant number: R344‐2020‐1073), the Danish Cancer Society (grant number: R283‐A16461), the Central Denmark Region Fund for Strengthening of Health Science (grant number: 1‐36‐72‐4‐20) and the Danish Agency for Digitisation Investment Fund for New Technologies (grant number 2020‐6720) to Søren Dinesen Østergaard, who reports further funding from the Lundbeck Foundation (grant number: R358‐2020‐2341), the Novo Nordisk Foundation (grant number: NNF20SA0062874) and Independent Research Fund Denmark (grant number: 7016‐00048B). The funders played no role in study design, collection, analysis or interpretation of data, the writing of the report or the decision to submit the paper for publication.
CONFLICT OF INTEREST
Andreas Aalkjær Danielsen has received a speaker honorarium from Otsuka Pharmaceutical. Søren Dinesen Østergaard received the 2020 Lundbeck Foundation Young Investigator Prize. Furthermore, Søren Dinesen Østergaard owns units of mutual funds with stock tickers DKIGI and WEKAFKI, as well as units of exchange‐traded funds with stock ticker TRET, IQQH, QDV5, and EUNL.
PEER REVIEW
The peer review history for this article is available at https://publons.com/publon/10.1111/acps.13463 .
Supporting information
Appendix S1 Supporting Information
ACKNOWLEDGMENTS
The authors thank Bettina Nørremark from Aarhus University Hospital – Psychiatry for her assistance with extraction of data, and Elisabeth Flebbe from Aarhus University Hospital – Psychiatry for discussions of diagnostic coding practice across the DNPR2 and DNPR3.
Bernstorff M, Hansen L, Perfalk E, Danielsen AA, Østergaard SD. Stability of diagnostic coding of psychiatric outpatient visits across the transition from the second to the third version of the Danish National Patient Registry . Acta Psychiatr Scand . 2022; 146 ( 3 ):272‐283. doi: 10.1111/acps.13463 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Funding information Kræftens Bekæmpelse, Grant/Award Number: R283‐A16461; Lundbeckfonden; Region Midtjylland, Grant/Award Number: 1‐36‐72‐4‐20; Independent Research Fund Denmark, Grant/Award Number: 7016‐00048B; Novo Nordisk Foundation, Grant/Award Number: NNF20SA0062874; Danish Agency for Digitisation Investment Fund for New Technologies, Grant/Award Number: 2020‐6720
DATA AVAILABILITY STATEMENT

COMMENTS
Outpatient mental health services involve diagnosing and treating people with mental health conditions, like depression and anxiety. These visits are often called counseling or psychotherapy, and can be done individually, in group psychotherapy or family settings, and in crisis situations.
Outpatient therapy is a resource for individuals seeking support for mental health concerns who do not require round-the-clock support or safety monitoring. Outpatient therapy can be offered through hospitals, in doctor's offices that employ therapists, group practices, or private practice. Psychologists, clinical social workers, counselors ...
Since 1995, the use of outpatient mental health services by adults has been rising in the United States (1-4).This overall upsurge reflects increasing numbers of mental health-related visits with both primary care providers and specialty mental health providers (SMHPs) (5, 6).Several changes in the practice and policy environment since 2008 and decreased stigma may have driven more recent ...
Mental health-related outpatient visits were identified based on established sets of diagnostic codes for psychiatric disorders. Temporal trends in the annual proportion of mental health-related outpatient visits were assessed, including visits associated with use of psychotropic medications. Analyses were stratified by age and sex.
Visit Medicare.gov, or call 1-800-MEDICARE (1-800-633-4227) to get the most current information. TTY users can call 1-877-486-2048. "Medicare & Your Mental Health Benefits" isn't a legal document. Oficial Medicare Program legal guidance is contained in the relevant statutes, regulations, and rulings.
Patients with mental disorders are among the highest users of emergency department (ED) services, with visits characterized by long lengths of stay, intensive treatment, and elevated rates of hospitalizations. After discharge, fewer than half of these patients successfully transition to outpatient care, with high rates of readmission to the ED. Programs that allow patients with mental ...
General psychiatric evaluations involve a systematic consideration of the broad domains de-scribed in this guideline and vary in scope and intensity. Table 1 summarizes the domains. The intensity with which each domain is assessed depends on the purpose of the evaluation and the clinical situation.
Outpatient mental health care was defined as a visit with a specialty mental health care provider (e.g., psychiatrist, child psychiatrist) for evaluation, management, psychotherapy, or other ... Nearly one-third lacked established outpatient care before the ER visit. Mental health follow-up was received by 28.6% of patients within 7 days and by ...
The proportion of mental health-related visits nearly doubled, from 8.9% in 2006 to 16.9% in 2019 (P < .001). Among all outpatient visits, 17.2% were associated with the prescription of at least 1 psychotropic medication, with significant increases from 12.8% to 22.4% by 2019 (P < .001). Conclusions and relevance: In this cross-sectional study ...
In an emergency, a physician may have to focus on more immediate history, symptoms, and behavior to be able to make a management decision. In a scheduled visit, a more thorough assessment is appropriate. Routine psychiatric assessment includes a general medical and psychiatric history and a mental status examination.
This study used 10 years of data (January 2007 through December 2016) from the National Ambulatory Medical Care Survey (NAMCS), 6 which is a random sample of outpatient visits made to a nationally representative random sample of physicians who are nonfederally employed, younger than 85 years, and treating outpatients. Patients seen in hospital units, nursing homes or other extended care ...
Introduction. Emergency departments (EDs) in the US have been increasingly utilized for psychiatric care (1-7).This increase in the number of mental health-related ED visits has been demonstrated among adult (1-3) and pediatric (4, 6, 7) populations, as well as across individual diagnoses such as depression (), anxiety (), substance abuse (10, 11), and suicidal ideation (12-15).
Mental Health. Adult Mental Health Getting Started. Professional Referrals; ... Outpatient Outpatient care is a service you receive that you don't have to stay overnight. ... We offer both inpatient and outpatient services for children and adults. Visit sevencounties.org to request an appointment online or call (502) 589-1100. ...
Pediatric emergency department (ED) visits for mental health (MH) conditions are rising in the United States, with the majority culminating in discharge. 1-3 Timely outpatient follow-up after a MH ED discharge may facilitate continuity and ongoing engagement in MH care. 4,5 Nevertheless, fewer than two-thirds of children receive outpatient MH ...
In-person visits decreased in Spring 2020, but gradually increased afterwards. The number of patients transiently fell in Spring 2020. Rapid switch to remote visits in outpatient care of adolescent psychiatry made it possible to avoid a drastic drop in the number of visits despite the physical distancing measures during the COVID-19 pandemic.
We do. In MHRC Clinic we promote research and education in order to ensure the best care to every patient through integrated clinical practice. We provide inpatient treatment and outpatient consultancy service for patients of all age with psychiatric disorders including: Autism. Mood disorders.
Guideline 1: Review Symptoms, Trauma History, and Treatment History. The APA recommends that the initial psychiatric evaluation include a review of the patient's mood, anxiety level, thought ...
A study by Carlisle et al 16 revealed that outpatient follow-up with a primary care provider or psychiatrist within a month after a psychiatric hospitalization for 15- to 19-year-olds in Ontario, Canada, increased the risk of readmission and ED visits combined and readmission alone but was not significantly associated with ED visits.
Timely follow-up visits after psychiatric inpatient care have also been associated with a reduced risk of readmission, although the evidence is mixed (5-7). Communication by hospital mental health staff with outpatient mental health providers is a standard practice for inpatient treatment that promotes continuity of care (6,8-10).
Mental healthcare services in Russia. Russia's Ministry of Health is in charge of funding the country's healthcare system, which includes funding mental health services and creating laws regarding mental health services.However, the government often distributes funds based on past spending, rather than on a region's needs according to its population.
psychiatric ward admissions,2,13,14 and psychiatric outpatient visits. 15-17 The greatest decrease in the number of new outpatient visits in 2020 was among the youngest and oldest patients. 16
Clinical and Social Factors of Compulsory Psychiatric Treatment in Moscow. Prof. Tsygankov Boris, MD, PhD Chief Psychiatrist of Moscow City, Head of the Department of Psychiatry, Addiction and Psychotherapy, Moscow State University of Medicine and Dentistry Slideshow 2928469 by kirti
Outpatient visits 30 days after discharge were associated with a lower hospital readmission risk during the following 90 days. Assertive hospital discharge planning to secure outpatient visits after hospital discharge is needed for these patient populations. Mark et al., 2013: USA: Retrospective cross-sectional study: 121,275: 18-65 years
Overview. Our mission is to assist Pennsylvanians in leading safe, healthy, and productive lives through equitable, trauma-informed, and outcome-focused services while being an accountable steward of commonwealth resources.
The surgeon general said mental health risks to young people from social media platforms is enough to justify warning labels similar to those on tobacco and alcohol products. Here's what to know.
We only examined psychiatric outpatient visits for the primary analyses, as the change in diagnostic coding with the DNPR3 should only affect the practice concerning this type of visits. We considered a visit to be outpatient if it was a physical visit with the patient‐type variable set to 'outpatient'. Importantly, our data source allows ...