Ketamine trips are uncannily like near-death experiences
Photo by JR Korpa/Unsplash
by Christian Jarrett + BIO
First-hand accounts of what it is like to come close to death often contain the same recurring themes, such as the sense of leaving the body, a review of one’s life, tunnelled vision and a magical sense of reality. Mystics, optimists and people of religious faith interpret this as evidence of an afterlife. Skeptically minded neuroscientists and psychologists think that there might be a more terrestrial, neurochemical explanation – that the profound and magical near-death experience (NDE) is caused by the natural release of brain chemicals at or near the end of life.
Supporting this, observers have noted the striking similarities between first-hand accounts of NDEs and the psychedelic experiences described by people who have taken mind-altering drugs.
Perhaps, near death, the brain naturally releases the same psychoactive substances as used by drug-takers, or substances that act on the same brain receptors as the drugs. It’s also notable that psychedelic drugs have been taken by the shamans of traditional far-flung cultures through history as a way to, as they see it, visit the afterworld or speak to the dead.
To date, however, much of the evidence comparing NDEs and psychedelic trips has been anecdotal or based on questionnaire measures that arguably struggle to capture the complexity of these life-changing experiences. Pursuing this line of enquiry with a new approach, an international team of researchers led by Charlotte Martial at the University Hospital of Liège in Belgium has conducted a deep lexical analysis , comparing 625 written narrative accounts of NDEs with more than 15,000 written narrative accounts of experiences taking psychoactive drugs ( sourced from the Erowid Experience Vaults, a US-based non-profit that documents psychoactives), including 165 different substances in 10 drug classes.
The analysis, published online in Consciousness and Cognition in February 2019, uncovered remarkable similarities between the psychological effects of certain drugs – most of all ketamine, but also notably the serotonergic psychedelic drugs such as LSD – and NDEs. Indeed, the five most common category terms in the narrative accounts of people who’d taken ketamine were the same as the five most common in the accounts of NDEs, suggesting ‘shared phenomenological features associated with an altered state of perception of the self and the environment, and a departure from the everyday contents of conscious mentation’.
From category to category, the semantic similarity is profound. When referring to perceptions, both groups used the words ‘face’ and ‘vision’. The emotional word most commonly used by both was ‘fear’. In the category of consciousness and cognition, drug-takers and participants who’d been close to death most often referred to words such as ‘reality’, ‘moment’, ‘universe’, and ‘learn’. The setting was often described as ‘door’ and ‘floor’. A negative tone emphasising unpleasant bodily sensations was a shared common theme, as well.
T he findings back up the observations of some of the most famous 20th-century explorers of the psychedelic world – the American psychologist Timothy Leary described trips as ‘experiments in voluntary death’, and the British-born writer and philosopher Gerald Heard said of the psychedelic experience: ‘That’s what death is going to be like. And, oh, what fun it will be!’ But claims about the similarities go beyond these famous reports. The new research legitimises the long-standing analogy between the experience of dying and the acute effects of certain psychoactive drugs. Links between dying, death, a potential existence of afterlife and certain hallucinogenic plants and fungi emerged independently across different societies, and are also ubiquitous in contemporary psychedelic culture. However, empirical research has been scarce, until now.
To an extent, the results also support neurochemical accounts of NDEs, and especially the controversial proposal that such experiences are caused by the natural release of an as-yet-to-be-discovered ketamine-like drug in the brain (adding plausibility to this account, ketamine is known to act on neural receptors that, when activated, help to prevent cell death and offer protection from lack of oxygen).
‘This body of empirical evidence supports that near-death is by itself an altered state of consciousness that can be investigated using quantitative psychometric scales,’ the researchers say. That in itself is quite a realisation. As they note wryly, ‘Unlike other human experiences, dying is difficult to study under controlled laboratory conditions by means of repeated measurements,’ making it a challenge to investigate NDEs experimentally. Although the new research lacks laboratory control, on the plus side, the lexical comparison that Martial’s team conducted is ‘massive both in terms of the investigated drugs and the number of associated reports’.
The limitations of the current approach, including a reliance on retrospective reports, often decades-old, means, as the researchers put it, that they cannot validate nor refute the neurochemical models of NDEs. ‘However,’ they add, ‘our results do provide evidence that ketamine, as well as other psychoactive substances, result in a state phenomenologically similar to that of “dying” (understood as the content of NDE narratives). This could have important implications for the pharmacological induction of NDE-like states for scientific purposes, as well as for therapeutic uses in the terminally ill as means to alleviate death anxiety. We believe that the development of evidence-based treatments for such anxiety is a cornerstone of a more compassionate approach towards the universal experience of transitioning between life and death.’
They also warn experimenters to be prepared and beware. ‘The intensity of the experience elicited by [ketamine] relative to cannabis may represent a shock to unsuspecting users, who could retrospectively report the belief of being close to death,’ the researchers say. Pot-smokers, you’ve been warned. As one of the most intense and life-changing altered states known, an NDE is no toke on a pipe after class or work.
This is an adaptation of an article originally published by The British Psychological Society’s Research Digest.

Gentle medicine could radically transform medical practice
Jacob Stegenga

Childhood and adolescence
For a child, being carefree is intrinsic to a well-lived life
Luara Ferracioli

Meaning and the good life
Sooner or later we all face death. Will a sense of meaning help us?
Warren Ward

Philosophy of mind
Think of mental disorders as the mind’s ‘sticky tendencies’
Kristopher Nielsen

Philosophy cannot resolve the question ‘How should we live?’
David Ellis
Love and friendship
Your love story is a narrative that gets written in tandem
Pilar Lopez-Cantero


Mental Health
Mental health: why a ‘bad trip’ with ketamine treatment isn’t what you think it is.
Editor's Note
Any medical information included is based on a personal experience. For questions or concerns regarding health, please consult a doctor or medical professional.
Please see a doctor before starting or stopping a medication.
If you have experienced emotional abuse, the following post could be potentially triggering. You can contact the Crisis Text Line by texting “START” to 741741.
It was Wednesday and time for my ketamine treatment . There is a certain amount of routine to getting my treatments. When I started with ketamine I thought I would get the IV treatments once every three months or so. That’s what everything I had read said would happen. Maybe the “treatment-resistant” part of my bipolar disorder applies to ketamine too. I don’t know. In any case, we have determined that every other week works for me. By the beginning of the second week, I start to dip in mood. I can reach suicidal thinking by the time it’s time for the next infusion. We try not to let me get to that place.
The infusions are accompanied by psychedelic “trips.” That’s just part of ketamine. In the beginning, I believed that the trip didn’t matter — the drug got in me regardless of if the trip was “good” or “bad.” A lot of my trips are “bad.” I believe this is largely because of complex post-traumatic stress disorder ( C-PTSD ). I put bad in quotes because it’s not an accurate description. The trips can be scary. I see things and feel things that are frightening or unpleasant. I have been literally terrified several times. That doesn’t mean they’re bad, though.
The trip before last Wednesday’s infusion was terrifying. I screamed so hard that I lost my voice for almost a full week. I just screamed and screamed. I was certain that I was permanently trapped in this other world that I was hallucinating. The people in the room with me, the nurses and anesthetist, looked like stick figures. They were walking around and they were talking. I didn’t know what they were saying; I was too busy screaming, “Please, somebody, notice that I’m still trapped over here in this alternate universe. Let me out!” One of them was telling me I was OK. I was insisting, “I am not OK.” As the ketamine wore off, I returned to this world and realized everything was fine. Just like every other time.
When it was time for the next infusion two weeks later, the clinic director decided to have a nurse, Colleen, sit with me for the trip. The thinking was I would feel safer and stay calmer. Maybe not scream my head off. Colleen is special to me; she has been with me since my first infusion. She has held my hand many times when trips turned frightening, always reminding me “you are safe.” It was a logical and welcome decision to have Colleen sit with me.
Except in this trip, Colleen turned evil. The world was red and black, no other colors. The walls in the room looked like the walls in “The Matrix” with green code running down black walls. Except my “code” was red. Colleen was red and terrifying. She was saying terrible things. I was convinced that the clinic was a front for an evil organization trying to do mind control and keep me trapped in that cold, black-and-red world forever. I didn’t scream because Colleen was there. I was afraid of her. I was afraid of what might happen if I screamed. What would she do to me?
Coming out of that trip, I was convinced that it would be my last. I couldn’t keep doing this, I didn’t trust anyone; that’s part of C-PTSD after all. I sent the clinic director an email the next day and asked him if he could sedate me for my next trip. Sometimes when I get especially agitated during a trip, he will add in a little sedative toward the end. When he does that, I go home with little to no memory of anything that happened during the trip. He wisely answered that the trips were important; he wanted me to experience them.
And he’s right because here’s the thing. Those “bad” trips? They aren’t bad. They’re unpleasant. They’re scary. They’re challenging and very hard to go through. But they aren’t bad. Let me explain.
The day after the Red Colleen (sorry, Colleen) trip, I went to dinner with a friend. We talked about a lot of things. This was the first time we had gotten together since my suicide attempt two months earlier. I filled her in on what it was like when I made the attempt, the ambulance ride, the emergency room, the week spent on the medical floor of the hospital, and the week after that on the psychiatric floor. I walked her through all of it. On my drive home after dinner, I had to pull into a parking lot because I was so overcome with emotion that I couldn’t keep driving. I sat in the parking lot and sobbed, letting out all the emotion that had come up while talking to my friend. It was a good, cleansing cry. When I was composed enough to drive, I made my way home. Turned out, that cry was just the beginning.
Later that same night, after everyone had gone to bed, I was up by myself. I put YouTube on the television and played my favorite music video. I had discovered this video months earlier and it had become a constant as a self-care thing I did. This video could make me cry, it could make me laugh. Something about the music touched me deep in my soul; I physically felt the music. As it played this night, tears started to flow. And I let them.
That’s something my therapist has been working on with me for over a year: Feel the feelings. Don’t avoid them, don’t push them away. Stop the struggle. Feel them. As the song came to its end, I started to smile through my tears. This is an amazing piece of music. The next video started to play. I cried some more. For the next half hour, I cried as I listened to and felt the music. But I didn’t just cry. I was turned inside out. Something broke inside me. I sobbed. I laughed. I cried about the suicide attempt. I cried about the time in the hospital. I cried about how hard the past two years have been as I rapid-cycled through bipolar , up and down, going through six different medications on the way to being declared treatment-resistant and getting off all drugs. How much work I had done with my therapist, working through all the trauma of my childhood. And I kept crying.
Then I remembered my therapist had suggested the day before that I do a meditation we know called “Working with Difficulty.” It walks you through grounding like normal. But then the guide suggests that you take any negative emotion that is coming up and place it on the worktable of your mind. Find the physical sensations of it in your body. Where are you feeling this emotion?
The guide instructs that you don’t do anything to change your breathing, just notice it, focus on it. I was sobbing hysterically. And I kept sobbing. I was breathing; it was just sobs and hyperventilating, not the calm, controlled breathing I think of when I think of meditating. I let myself do it. I gave myself permission to feel this. To express it. As I worked through this 25-minute meditation, I let myself feel all of it. And as the crying continued, that traumatized little girl who had never been allowed to cry showed up. She started to cry. This is the miracle of ketamine: It allows your mind to do things it hasn’t been able to do before. That little girl had been shamed into never crying . It wasn’t allowed. And she desperately needed to cry. She was not going to be able to heal from the trauma until she could express all that she had stuffed so far down for so long. And I was able to give her permission. I encouraged her: yes, dear one, cry. Cry until you don’t have any tears left to cry.
And she did. She cried. She rocked back and forth. She hugged a pillow and sobbed into it. I don’t have words to describe what this experience was like. The intensity was beyond description. There was one point when I felt I was back in the psychedelic part of the ketamine trip. It’s like ketamine lets your mind open in places it hasn’t opened before. This gave me the space and the permission I needed to let this little girl cry her heart out.
This was such a healing episode. I’m not the same today. I’ve been used to learning coping skills in therapy. I assumed that was the best I could hope for — learning how to cope. But, no. This was healing. The pain that that little girl had held inside all these years was released. This isn’t the first time I’ve had such a physical reaction and release of repressed pain. And it is ketamine that allowed this — caused it.
As I said in the beginning, I believe there’s no such thing as a bad trip. Every trip I’ve had that was painful ended with something good. A new insight. An expression of long-buried pain. I feel it necessary to say that I have not arrived at these good results alone. I have needed the guidance of the people at the clinic. I have needed my therapist. I have needed my psychiatrist. I don’t know psychedelics. Had I done these trips on my own, I think I would have ended up further traumatized. These trips can get very difficult and very intense. But my subconscious has been hard at work during them. Things have bubbled to the surface — the conditioned emotional responses, the fight-or-flight triggers, the repressed memories, they have been in my mind all along. Ketamine, along with therapy, has allowed those things to surface and be dealt with. It’s a very powerful and healing combination.
For more on ketamine treatments for depression, bipolar disorder, trauma and other mental illnesses, see The Mighty Community’s posts here .
If you or a loved one is affected by domestic violence or emotional abuse and need help, call The National Domestic Violence Hotline at 1-800-799-7233
We want to hear your story.
Do you want to share your story? Click here to find out how.
Photo by Just Jack on Unsplash
Early childhood trauma and lifelong struggles with mental health led me to The Mighty. I've learned the power of sharing and not staying in this madness alone. Sometimes I can support, sometimes I need support.
Web tracking technologies in the following categories are used on our website. You may opt out of certain trackers as described below.
These trackers are necessary for the website to function properly. They are usually set in response to actions made by you which amount to a request for services. You can set your browser to block or alert you about these trackers, but some parts of the site may no longer function.
Advertising
These trackers allow us to optimize advertising. They may be set on our site through advertising providers, which may use those trackers to build a profile of your interests and show you relevant ads on other sites and social media. You may opt out of these trackers.
Performance
These trackers allow us to monitor site visits and traffic sources so that we can measure, analyze, and improve the performance of our site. You may opt out of these trackers.
We use cookies to enhance user experience, analyze web traffic, and assist in marketing. If you do not consent to the cookie terms set forth in our Privacy Policy , please do not continue to use the site. Learn more or opt out of these cookies by clicking here .
Understanding What Ketamine Commonly Feels Like

- Having questions and concerns is a normal part of beginning ketamine therapy.
- The “felt experience” of ketamine therapy is less intense than people expect.
- Clients often describe ketamine therapy as calming and relieving of negative thoughts.
Trying any new therapy or treatment can be scary. Here is what you need to know about how ketamine might feel. Keep in mind that every individual's experiences are unique, and each session will be different.
Ketamine is incredibly safe.
Ketamine has been approved by the FDA since the 1970’s and is included on the World Health Organization's list of Essential Medicines.
When used in surgical anesthesia ketamine has been proven to have a remarkable safety profile at doses considerably higher than those used in ketamine therapy.
Furthermore, in the largest clinical study of ketamine therapy the results show minimal risk of side effects.
Notable outcomes from the study include:
- 89% of the participants reported improvement in their depression or anxiety symptoms, and 63% of participants experienced a greater than 50% reduction.
- For both depression and anxiety, over 30% achieved remission (or virtually no symptoms) after 4 sessions.
- Fewer than 5% of participants reported side effects from treatment.
The experience has a gentle onset.
Mindbloom’s method of sublingual administration—using a rapid dissolve tablet placed under the tongue— has a more gentle onset than IV or IM-injections, which are commonly used at ketamine clinics.
The experience is gentle, bringing you slowly into and out of the experience, and returning to normal consciousness around 60 minutes later.
A common timeline for the ketamine experience can look like:

For most individuals following our protocols, the experience typically lasts less than an hour. It is important to note that exact timing may vary from person to person, and from session to session.
This is a general overview of the ketamine experience provided by our clinical team.
Ketamine can be very calming.
One of the most common things we hear from clients is how their sessions can be very calming.
Here are some direct quotes from previous Mindbloom clients who have gone through our Basics program:
- “The most surprising part of my Mindbloom experience was how gentle and safe it felt.” — Brenna, Writer
- “I expected a punch in the face, but it felt more like a tickle on the arm.” — Brittni, Project Manager
- “I appreciate the comfort and safety of my own living room.” — Noah, Land Use Consultant
Ketamine can induce a feeling of relief.
During and after the experience, many clients describe feeling relief from ruminative thoughts and other, normally-present anxieties.
The ketamine experience can provide new and novel perspectives on your life, which gives you a new way to relate to and manage old thoughts that may have previously caused or contributed to daily stresses.
Here are a few quotes from Mindbloom clients who have had similar experiences:
- “Mindbloom gave me a better perspective on anxiety, depression, and life itself.” — Deborah, Student
- “I’ve reframed my negative thoughts into positive ones.” — Sarah
- “Mindbloom helped build a foundation that I needed to keep me from spiraling and feeling lost.” — Andrew, Financial Advisor
Ketamine works with you
While there are moments when working with ketamine that can be challenging or emotionally intense, ketamine has proven itself to be safe, approachable, and gentle throughout decades of use and hundreds of thousands of individual sessions.
Ketamine works with you, not against you, as you move towards your own healing and wholeness.

Eric Brown is a content writer and program creator at Mindbloom, and the Director of Apotheosis Retreats. As a facilitator, coach, guide, and creator, he combines cognitive science, psychedelic medicines, and healing modalities to create powerful spaces for personal growth and development.

Chelsea Tersavich, PA-C, is a psychiatric clinician who has conducted psychiatric evaluations and facilitated ketamine therapy sessions for over 250 Mindbloom clients. Chelsea obtained a master’s degree from the Interservice PA Program and has extensive mental health and primary care experience from her army career, where she treated thousands of Soldiers as a Battalion PA and a clinic Medical Director.
This article is for informational purposes only and is not intended to be a substitute for professional medical advice. Always talk to your doctor about the risks and benefits of any treatment. If you are in a life-threatening situation, call the National Suicide Prevention Line at +1 (800) 273-8255 , call 911, or go to the nearest emergency room.
Ketamine is not FDA-approved for the treatment of depression or anxiety. Learn more about off-label uses here .
Side effects of ketamine treatment may include: altered sense of time, anxiety, blurred vision, diminished ability to see/hear/feel, dry mouth, elevated blood pressure or heart rate, elevated intraocular or intracranial pressure, excitability, loss of appetite, mental confusion, nausea/vomiting, nystagmus (rapid eye movements), restlessness, slurred speech, synesthesia (a mingling of the senses).
Do not proceed with ketamine treatment if any of the following apply to you:
- Allergic to ketamine
- Symptoms of psychosis or mania
- Uncontrolled high blood pressure
- CHF or other serious heart problem
- Severe breathing problem
- History of elevated intraocular or intracranial pressure
- History of hyperthyroidism
- Other serious medical illness
- Pregnant, nursing, or trying to become pregnant
Ketamine has been reported to produce issues including, but not limited to, those listed below. However, lasting adverse side-effects are rare when medical protocols are carefully followed.
While ketamine has not been shown to be physically addictive, it has been shown to cause moderate psychological dependency in some recreational users.
- In rare cases, frequent, heavy users have reported increased frequency of urination, urinary incontinence, pain urinating, passing blood in the urine, or reduced bladder size
- Ketamine may worsen problems in people with schizophrenia, severe personality disorders, or other serious mental disorders.
- Users with a personal or family history of psychosis should be cautious using any psychoactive substance, including ketamine, and discuss potential risks with your MindBloom ® clinician before proceeding with treatment.
- The dissociative effects of ketamine may increase patient vulnerability and the risk of accidents.
To promote positive outcomes and ensure safety, follow these ketamine treatment guidelines:
- Do not operate a vehicle (e.g., car, motorcycle, bicycle) or heavy machinery following treatment until you’ve had a full night of sleep
- Refrain from taking benzodiazepines or stimulants for 24 hours prior to treatment
- Continue to take antihypertensive medication as prescribed
- Avoid hangovers or alcohol intake
- Refrain from consuming solid foods within 3 hours prior to treatment and liquids within 1 hour prior to treatment
- Ketamine treatment should never be conducted without a monitor present to ensure your safety
More articles

Ketamine Treatments Found to Be At Least as Effective as ECT

Beyond Microdosing: The Mindbloom Approach to Ketamine Therapy
Ketamine’s Interactivity with Common Psychiatric Medications

How Culture and Psychiatry View Ketamine Therapy

Exploring the Neurobiology of Ketamine

The Clinical Research of Ketamine & Ketamine Therapy
Take control of your mental health.
Taking control of your mental health is possible, find out it ketamine treatment can help you.

Things you buy through our links may earn Vox Media a commission
Leave Your Body at the Door
How ketamine became the drug of choice for our dissociated moment..
This article was featured in One Great Story , New York ’s reading recommendation newsletter. Sign up here to get it nightly.
It was well past the hour for getting trashed, but James still couldn’t switch off his work-brain. The 29-year-old had come straight to the party from the office, and despite the array of Friday-night delights his friends thrust at him — cheap beer, crumbly coke, a hit of a rare mango Juul pod — his mind was still stuck at his job. Then his friend — the kind of friend who carries a coke-spoon on her like it’s an EpiPen — offered him a bump of ketamine.
“Nothing that I’d heard about ketamine sounded appealing to me,” recalls James, who had tried it before in tiny doses, just enough to feel a bit loopy and drowsy. “But something in my mindset switched that night, and I was just like: fuck it, I’ll just go wild and plunge full in, and I took the biggest bump of K I’d ever taken.”
Technically speaking, ketamine is a dissociative anesthetic, meaning that it numbs your body and makes you feel apart from your environment — like you’re watching your own life happen instead of living it. But that doesn’t begin to capture the weirdness of what it feels like to get high on K. As one friend put it to me: “It’s like walking from your kitchen to your living room, and from your living room to your kitchen, and it’s uphill both ways, but you’ve never had so much fun walking up a hill.” It’s true that K can make both you and the world feel tilted — as if you’re walking on an underwater treadmill pitched at a 45-degree incline. Thought-trains jump their tracks, anxieties float off like helium balloons, and everything becomes silly and warped, like filming a movie through a camera with a fish-eye lens. At least, that’s one possible outcome.
Ketamine has a triple-threat of sedative, stimulating, and psychedelic effects, which vary depending on how much you do and what other substances you combine it with. “It’s just a very strange drug — the strangest drug,” Dr. Joseph Palamar, an NYU professor and expert in recreational substances told me recently. It’s also extremely potent; the difference between a goofy buzz and total body paralysis could be as little as one or two baggie-dips. If every generation of partiers gets the drug that speaks to them — the psychedelic ’60s, the coke-and-disco-fueled ’70s, and the MDMA-hued early aughts — then perhaps the end of the decade marks the dawn of the dissociation generation.
Since that night a few months ago, James has joined a growing number of young professional New Yorkers who are trading their white baggies of coke for white baggies of ketamine, or simply mixing them both together (he and his friends call this mixture “revolutionary lines,” while others refer to them as Calvin Klein lines, so named for the combo of C and K). While the sideways-ness of K may not seem like the most intuitive replacement for the pure up of cocaine, both substances can be defibrillators for parties on life-support; dosed right, K has a stimulating effect that can keep an after-party going into the wee hours of the morning. Like coke — and unlike MDMA or psychedelics — the effects of snorting ketamine subside in less time than it takes to watch your average Netflix special, and rarely cause a hangover if consumed in moderation. (One New York drug dealer sells a gram for about half the price of coke, and it lacks cocaine’s stigma as a source of cartel violence and environmental destruction). Most importantly, instead of fueling anxiety and heated close-talk, it makes you feel like you’re giving your brain a bath in a pool of warm macaroni. “Coke brings this intensity to everything,” says James. “K does the opposite — it provides this looseness, and the feeling that things really aren’t significant.” And these days, who really wants to spend their free time doing a bunch of uppers and talking about the news?
For James that night at the party, what rushed over him was a sense of strange wonder. “There was something profound and spiritual about it, where I was having an alternative perception of the world in which time and space had different qualities, and the world didn’t seem real,” he recalls. His limbs felt as heavy as sandbags, and he struggled to drag them the 12 feet from the living room to the kitchen. Eventually — in what he thinks was probably 15 minutes but felt like an hour — the intensity wore off, but a feeling of pleasurable lopsidedness remained. “I felt this sort of ongoing euphoria and silliness that I hadn’t felt since childhood.” What resulted was one of the most fun nights of his life. He and his friends turned the living room into a sweaty dance party, contorting their faces like Plasticine and flailing their limbs like those inflatable tube men at a used-car lot. “It wasn’t like when you’re drunk when you feel really out of control. I felt like I could completely be ridiculous and that would be liberating.” He left the party and walked the entire 40 minutes back to his house, feeling calm, at peace, and happy to be alive. And he had totally forgotten about his crappy day at the office.
“We’re all so overwhelmed, it makes sense that we’re literally taking dissociatives,” adds Claire, 32, a Brooklyn filmmaker, whose group of friends — primarily queer women — have adopted ketamine as their drug of choice in the past few years. “We don’t have time to be hungover, everybody is exhausted, and pulled in so many different directions. It’s the peak of distraction culture.” In 2019, escaping isn’t just something you do for fun; it’s a survival tactic at a time where the world feels so inescapably stressful and out of control. We spend our days being force-fed the unrelenting news cycle — with its heady brew of climate crisis, political chaos, and technological dystopia — then binge TV at night like a sedative. Meanwhile, it’s harder than ever for our minds to take a night off. The internet has eroded the boundary between home and work; even going on vacation provides little respite when you’re still trapped in your phone’s glowing orbit.
But ketamine puts life on airplane mode. “Phones aren’t really a thing when you’re on K,” adds Claire. “You’re creating an internal world. You’re not trying to reach out or engage with anyone but yourself and who you’re with.”
Ketamine was patented in the U.S. in 1966 for use as an anesthetic, and was approved by the FDA in 1970. Its relative safety and efficacy has made it a mainstay in operating rooms around the world, as well as in veterinary medicine (because of its reputation as a horse tranquilizer, one recreational user said his group of friends refer to it as “pony medicine” and greet its arrival at a party with a chorus of neighs.) Like any drug, risks abound: heavy use can lead to chronic bladder and urinary tract damage, while high doses can cause significant cognitive impairment which have led to a handful of highly publicized deaths in the U.K. and elsewhere, often from accidents like falling or drowning . Still the World Health Organization says overdoses are rare, and it has a lower dependence potential than drugs like caffeine, marijuana, MDMA, and alcohol. Most of the stigma comes from the cultural lore of the “K-hole” — the full dissociative experience that ravages your speech capabilities and motor functions and can make you feel, as James did, like he’d entered another dimension. Whether this feels pleasurable depends on your taste in altered states. As Norman Cook, a.k.a. Fatboy Slim, said in a 1998 Muzik article : “Get the quantity right and it’s incredible. Get it wrong and you feel like you’re dying.”
Then again, for some experienced psychonauts, K-holes are the whole point. 30-year-old Luke, a floppy-haired Canadian with a goofy grin, signed up to volunteer at a music festival guiding people through bad trips. But before he did it, he wanted to see what the experience of K-holing might be like, so he got his friend to call him on Skype, and then snorted half a gram of ketamine in one line (which is a lot). “Within 30 seconds it’s coming almost up my feet and up my body; everything’s tingling. And in the instant that it reaches my head, the entire world ceases to exist. Everyone I knew was gone, but for some reason I was very complacent. I was just a ball of energy in a galaxy far far away, and from there I was kind of watching worlds and societies form in fast motion. It basically ended with me kind of waking and coming to in the shower naked half an hour later.” Then he remembered the friend he had called on Skype. “Apparently I just said ‘I’m out, good night, the world doesn’t exist, good-bye family.’ And then I started taking off my clothes.”
Like most new substances, as soon as K was invented, people quickly started investigating whether it was a good thing to shove up their noses for fun. In the 1980s and ’90s, the growth of rave culture brought it onto New York dance floors and it became a staple of the club kid scene, prompting the first wave of ketamine trend pieces. “Whether it’s a gay all-nighter, or at a hard techno rave patronized by young, white out-of-towners, the picture is invariably the same. Come 3 a.m., the dance floor is littered with those wasted on ketamine,” Muzik Magazine wrote in that same 1998 article. American authorities responded by cracking down on its recreational use, and by 1999 the Federal Drug Enforcement Agency had labeled it a schedule III substance. As its popularity waned in the States over the next decade, it became a fixture in places like Russia, South East Asia, and Western Europe. While many millennial drug users in the U.S. may not have tried ketamine until recently, it has long been a staple of Britain’s drug scene. In 1999, Time Out London declared “Ketamine is the new E.”
Yet in the past few years, it seems that ketamine has found its way back into New York’s needy nostrils. While K is still fringe compared to MDMA or cocaine, Palamar, who also works as a researcher at NYU’s Center for Drug Use and HIV/HCV Research, says that he has seen significant increases in the number of nightclub and festival attendees using the drug, with prevalence doubling over approximately the last four years. Brooklyn nightlife institution House of Yes even put on a performance in 2016 called Ketamine: The Musical , with co-founder Anya Sapozhnikova telling the website Splinter that K is to her community what cocaine was to Studio 54.
Most of the people I spoke with are preexisting drug users who discovered ketamine on big nights out; it’s particularly a staple of New York’s booming queer nightlife scene . But in 2019, once-fringe elements of rave culture have bled into the mainstream. EDM is elevator music, banker bros and leather-daddies share bumps at Bushwick warehouse events, Silicon Valley has invaded Burning Man, and the wellness world has turned the drugs of the ’60s counterculture into productivity boosters for start-ups. As rave culture has rebranded, ketamine has pivoted with it. Today’s K users are bringing the drug beyond the dance floor: to chilled-out bar nights and tech-world salons, New-Age wellness retreats and quiet nights at home.
There will always be the Lukes of the world, eagerly passing out naked in front of their webcams, but most of the recreational users I spoke with said they take K in very small doses, seeking a pleasant buzz that wears off within 30 minutes or can be re-upped as needed. It’s often taken to compliment other drugs — a garnish instead of the main course. For a generation that has less free time for sprawling multi-day psychedelic trips, ketamine has an appealing choose-your-own-adventure quality. Ketamine and alcohol are uneasy bedfellows — and often a recipe for a night of puking — but a number of the people I spoke to said that K has led them to pare down their boozing overall. Claire says it actually feels like a healthier and more mature lifestyle. “People are like: I used to go out and have 16 drinks and do a bunch of cocaine and feel like shit the next day. And then it was this total shift of: Oh, yeah, I can do this. And it still feels like stepping out of my life, but I also feel fine tomorrow .” At this point, she says: “I wouldn’t say that it’s different than like, a bunch of people getting off work and going out for drinks.”
Repurposing horse tranquilizers as a healthy life choice may sound like a parody of flaky millennial self-searching, like a more hardcore version of switching your morning Nespresso for matcha, or getting really into Peloton. Yet when it comes to ketamine, the warehouse ravers and the scientific establishment happen to actually be on the same page. Just as researchers have started returning to drugs like LSD, psilocybin, and MDMA for their potential mental-health benefits, ketamine has widely been heralded as a revolutionary treatment for depression. This March, the FDA approved a nasal spray called esketamine for treatment-resistant depression, marking a major development in a field that has been slow to innovate. “This is potentially a life-saving medicine,” said Gerard Sanacora, director of the Yale Depression Research Program. “It really was the first treatment that we had found that could fairly reliably produce antidepressant effects within hours, and definitely within days of taking it.” Still, he adds: “This is clearly not a medication that should be taken at home.”
Which has led, of course, to people trying it at home. Ava, 26, who works in the tech industry, says she’s been “biohacking” since she was 19 or 20. When she went through a serious depression and began feeling suicidal, a friend of hers told her about the emerging research on ketamine, and her ears pricked up. “I had previously known mushrooms as a party drug and then I did a secret ceremony with this New Age Shaman guy, so I already knew that there could be a huge difference between like the party setting and a more intentional one.” With the help of a friend, she bought and self-administered ketamine a couple of times a week for a month, and then once a month after that. The effect on her depression was profound — she says her suicidal thoughts went away, and she was able to socialize with friends once again. “I was able to go to Burning Man again that year, and I didn’t think I would have been able to a couple months before. I thought I was going to jump off the roof of my building.”
The drug has become popular among Ava’s anxiety-ridden tech-world friends in recent years, she says, and not just the ones running ad-hoc mental-health clinics out of their condos. “My theory is that ketamine is a response to the overabundance of information and the disengagement a lot of people have from the millennial job market, and now Trump, and seeing the world burn before our eyes,” she says. Another tech world source I spoke to told me about an industry peer who invited 40 people over for a ketamine party and supplied the drugs for everyone. Ava described how she and a group of co-workers even conducted a ketamine-guided meditation session together. “Some of the leaders in [the tech] industry will talk publicly about it and text our group chat, like: I’m getting so high on K this weekend!” she says.
If there’s any sure sign that ketamine is hitting the mainstream, it may be that for some communities it’s already well on its way to losing its street cred. When I tell Claire, the filmmaker, about the drug’s newfound popularity in the tech world, she scoffs. “That doesn’t surprise me,” she says. “They’ll do anything to do to get themselves out of the misery of the world that they’ve created for us.”
Names have been changed.
- disassociation generation
- best of the cut
- one great story
The Cut Shop
Most viewed stories.
- Madame Clairevoyant: Horoscopes for the Week of May 19–25
- What Is Violet Affleck Trying to Tell Us?
- The Last Thing My Mother Wanted
- Do ‘Parentified Children’ Really Have It So Bad?
- All of the Allegations Against Diddy
Editor’s Picks

Most Popular
What is your email.
This email will be used to sign into all New York sites. By submitting your email, you agree to our Terms and Privacy Policy and to receive email correspondence from us.
Sign In To Continue Reading
Create your free account.
Password must be at least 8 characters and contain:
- Lower case letters (a-z)
- Upper case letters (A-Z)
- Numbers (0-9)
- Special Characters (!@#$%^&*)
As part of your account, you’ll receive occasional updates and offers from New York , which you can opt out of anytime.
The Ultimate Guide to Ketamine
(k, ket, special k, vitamin k, lady k).
Ketamine is a potentially illegal substance, and we do not encourage or condone the use of this substance where it is against the law. However, we accept that illegal drug use occurs, and believe that offering responsible harm reduction information is imperative to keeping people safe. For that reason, this guide is designed to ensure the safety of those who decide to use the substance.

Ketamine is known for acting fast and effectively. A 2006 study from the National Institute of Mental Health found that 18 people who used the drug reported a drastic shift in mood within hours. Though it’s not known exactly how ketamine works, experts believe the drug could repair damaged synapses—or connections–in the brain, which are worn down by stress and depression.
What to expect
At lower doses, ketamine may cause numbness, a tingling body high (especially in the hands, feet, and head), jerky movements, rapid breathing, and dizziness. These effects are often accompanied by euphoria, relaxation, a feeling of weightlessness, mild visuals, and blurred or roving vision. Users may also experience introspective thoughts and enhanced appreciation for music.
At higher doses, visual, auditory, and even gustatory (taste-oriented) hallucinations are common, with some reporting a metallic flavor in the mouth. Hallucinations may be extremely realistic, including conversations with friends who aren’t there. [1] [2] [3]
At high doses, awareness of the physical environment and body dissolves. Out-of-body or near-death experiences are common, as are vivid internal experiences and a distorted sense of time. A high dose starts at approximately 1.5 mg/kg injected.
There are companies like Joyous , who use a proprietary, very low-dose ketamine treatment protocol that has been shown to produce quick relief and sparked the beginning of gradual and consistent mental health improvements.
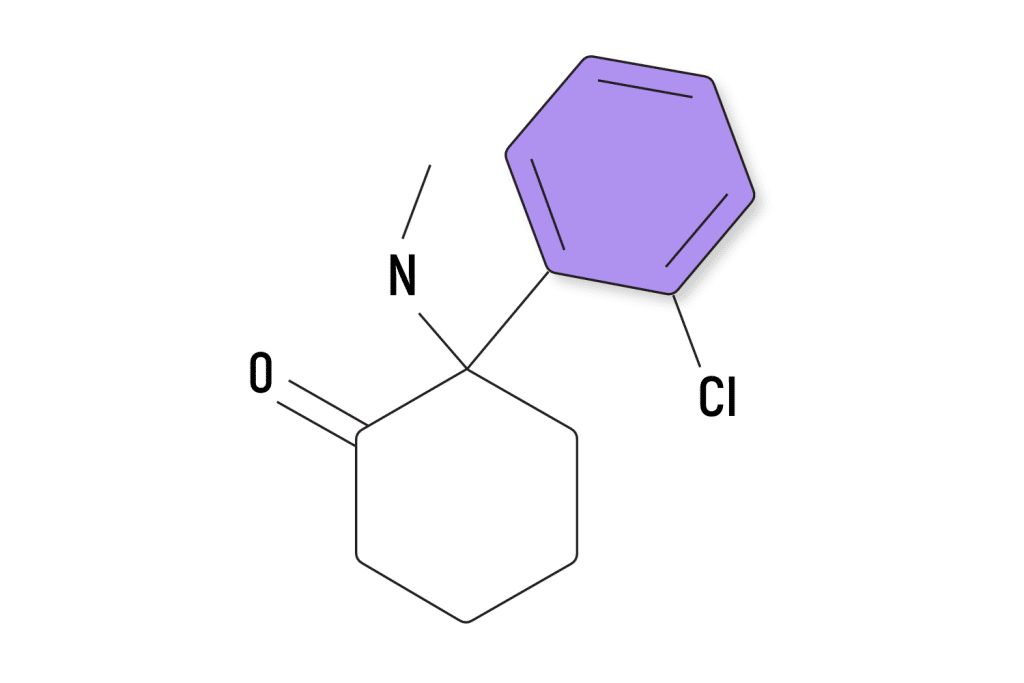
Pharmacology
Ketamine is a water-soluble PCP derivative. As a chiral molecule, it has two enantiomers: an S(+) isomer, or “esketamine,” and an R(-) isomer, or “arketamine.” [4]
In clinical use, it is available as ketamine hydrochloride in liquid or powder form for intravenous injection and is marketed under the brand name Ketalar . Esketamine, which has a slightly different molecular makeup than ketamine, was approved for use by the FDA in 2019 and is marketed under the brand name Spravato . It is administered as a nasal spray.
Receptor binding
Ketamine antagonistically binds to, or blocks, NMDA ( N- methyl-D-aspartate) receptors. [5] This interaction prevents signals passing between the brain and spinal column and is responsible for the molecule’s analgesic effect. Ketamine also interacts with opioid receptors and monoamine, cholinergic, purinergic, and adrenoreceptor systems. [4]
Safety and Toxicity
Ketamine appears to be relatively safe for occasional users. However, frequent use carries the potential long-term risk of neurodegeneration. Prolonged intravenous exposure to the drug (over 9 or 24 hours) has led to brain cell death in rhesus monkeys. [6] A similar effect has been seen in neonatal rats. [7] In the monkeys’ case, however, continual exposure over a shorter period of three hours had no adverse effects.
Frequent use among people has also led to signs of cognitive impairment affecting thought and memory [8] . However, occasional users (i.e. those who take ketamine once or twice a month) have not. [9]
Schizotypal symptoms—including delusions, superstitious thinking, dissociation, and flashbacks—have also been observed in frequent users. Symptoms have also been shown to persist for some. [10] [11]
Bladder pain is another common complaint among frequent users [12] , often accompanied in the long term by reduced bladder volume, incontinence, passing blood in urine, and cystitis. [13] More research is needed to understand the relationship between ketamine and urological problems, but in some cases, it has been necessary to surgically remove the bladder. [14]
In 2009, there were 529 ketamine-related emergency department visits in the US—compared to 36,719 for PCP and a total of 973,591 for any illicit drug. [15] Only 12 ketamine-related deaths were recorded worldwide between 1987 and 2000, and only three involved ketamine alone. The cause of death in each case was an overdose by injection. [16] More often, ketamine-related deaths are caused by interactions with other drugs, leading to respiratory depression and cardiac arrest. [17]
Interactions with other substances
Only a limited amount of data exists around ketamine’s interaction with other drugs, whether good or bad, but it’s best to be cautious when mixing any two substances. Here’s what we do know.
Positive interactions:
- Psilocybin: Many users have anecdotally reported that mixing psilocybin and ketamine brings out the best of both drugs. Out of body experiences are common, and ketamine helps diminish any anxiety and brings on a sense of euphoria.
- LSD: LSD increases ketamine’s ability to induce out of body experiences, which could be an important part of their therapeutic effect. Some users have also reported that small amounts of ketamine can “ground” the trippier aspects of the LSD experience.
Neutral interactions:
- Cannabis: There have been no reported problems with this combination. Ketamine can amplify some cannabis effects, most notably closed-eye visuals.
- Caffeine : No known problems.
Negative interactions:
- Barbiturates (Amytal, Butisol, Nembutal)
- Benzodiazepines (Xanax, Klonopin, Ativan)
- Zolpidem (Ambien)
Benefits & Risks
Potential benefits.
Though ketamine does not work for everyone, its ability to rapidly reverse symptoms of depression makes it a powerful medication compared to existing antidepressants, which can take weeks or months to begin working. Studies have also shown that ketamine works for patients who have failed to respond to multiple other treatments.
Though we don’t know for sure why ketamine works so well, the leading theory is that the drug stimulates the regrowth of synapses (connections between neurons), effectively rewiring the brain. This is a very different function than existing antidepressants. Rather than affecting one of the “monoamine” neurotransmitters, such as serotonin or dopamine, ketamine acts on glutamate, which is the most common chemical messenger in the brain. Glutamate plays an important role in the synapses involved in learning and memory, which is why researchers believe neuroplasticity could be central to ketamine’s antidepressant effects.
Ketamine is considered a relatively safe drug when taken in medical settings. Unlike other anesthetic medications, ketamine does not affect the protective airway reflexes and doesn’t depress the circulatory system, which makes it a safer option.
However, there are some things to look out for. Ketamine can cause an increase in blood pressure and intracranial pressure or pressure in the brain. That means people with brain swelling, glaucoma, and brain lesions or tumors should not use ketamine. People with coronary artery disease, high blood pressure, thyroid disease, alcoholism, and aneurysms should also exercise caution when using ketamine.
Therapeutic Use
While it doesn’t work for everyone, ketamine’s success rate of 85% is almost double that of traditional antidepressants (45%). [19] It’s also highly effective in patients with treatment-resistant depression, even if their symptoms have persisted for decades without relief. [20] Furthermore, it shows great promise in quickly and reliably eliminating suicidal thoughts, essentially making ketamine the first emergency “anti-suicide” drug. [21] When administered as an intranasal spray, ketamine’s antidepressant effects may last up to 30 days from a single dose. [22]
A highly important but still under-researched aspect of ketamine treatment is the effective dosage. It produces numerous side effects (even at subanesthetic dosage levels), so it’s important to administer the optimal quantity.
A recent study tested four different dosage levels on patients with treatment-resistant depression: 0.1, 0.2, 0.5, and 1 mg of intravenous ketamine per kg of body weight. They found that single doses of 0.5 and 1 mg/kg were significantly more effective than an active placebo in reducing depression symptoms over a three-day period.
However, after monitoring the patients for 30 days, the results showed that there was “little evidence of meaningful therapeutic benefit after day 5.” At 1mg/kg, the effects of the drug lasted between 15 and 30 days, but the researchers noted that the effects were modest.
While some researchers hope for a non-psychedelic form of ketamine [23] [24] , others consider its unique psychedelic effects to be crucial for treatment. Ketamine psychedelic therapy (KPT), for instance, takes advantage of ketamine’s dissociative state to address the underlying psychology of addiction. Companies like MindBloom , which are opening ketamine clinics across the US, believe that the psychedelic effects are central to their treatments.
A study in 1997 found that ketamine therapists were able to imprint drug addicts and alcoholics with new beliefs and memories about substance abuse, effectively creating a strong inner taboo to prevent relapse. One year after treatment, approximately 66% of chronic alcoholic patients remained sober, compared to just 24% of chronic alcoholic patients in conventional treatments. [25]
Following treatment, KPT patients also identified more strongly with positive self-images and values than before they started. Of particular note was their newfound sense of meaning or purpose, which was likened to a spiritual or religious conversion.
More recent studies have linked KPT-assisted recovery to ketamine’s antagonism (blocking) of NMDA receptors, destabilizing, and even erasing memories that reinforce drinking. [26] [27] Ketamine also activates the limbic system (associated with memory, emotion, and behavior), which suggests a strengthened interaction between the conscious and subconscious levels of the mind. [25]
KPT has also helped heroin addicts stay sober after rehab. Those given regular KPT sessions were far less likely to use heroin again than those who received counseling alone. [28]
Based on more than a decade (1985-1997) of administering KPT to patients, researchers found it was also effective at treating avoidant personality disorder (social inhibition, over-sensitivity, feelings of inadequacy, etc.) and neurotic-reactive depression (i.e. depression arising from specific life events or circumstances), as well as PTSD . [25] Ketamine’s antidepressant and PTSD benefits likely result from its ability to modulate glutamate neurotransmission and promote neuroplasticity.
Other psychotherapeutic applications of ketamine’s dissociative effect include regression, ego-dissolution, and group healing ceremonies. [29]
Personal Growth
Famed physician, neuroscientist, psychoanalyst, and psychonaut John C. Lilly, M.D., was enthusiastic about what he called the “emergent state” on ketamine, more commonly known as the “K-hole.” In this state, he said, time slows to the point of becoming meaningless, which makes issues easily available for analysis—removed from personal involvement, objectively examining one’s ego, behavior, and motivations becomes easier. Lilly also recommended a practice he called “metaprogramming,” which involved experimenting with different personality traits while in this emergent state to see their consequences before deciding to adopt them for good. [31]
Since esketamine became FDA-approved, countless ketamine therapy clinics have emerged to administer off-label infusions for treatment-resistant depression. If you’re feeling called to experiment with this substance, Healing Map’s ketamine clinic directory can help you locate a qualified center.
In the UK, Ketamine is a Class B substance, the same category as cannabis , codeine, and most amphetamines. Possession is punishable by up to five years in prison. [35]
History & Stats
Recreational use began around 1965 and became internationally prevalent by the mid-1970s. During this period, psychedelic researchers such as John C. Lilly, Marcia Moore, Stanislav Grof, and D. M. Turner explored ketamine’s psychotherapeutic potential. It was also used by Vietnam veterans with PTSD , having been the field anesthetic of choice during the war. Lilly referred to the drug as “Vitamin K” and once took it for 100 days straight. [39] Grof found it useful and integrative for therapy with LSD. [29]
In the 1980s, ketamine’s popularity shifted to the rave culture of Ibiza and Goa. It was a cheaper alternative to another up-and-coming “club drug,” MDMA .
In 1981, the DEA filed a notice of intention to place ketamine in Schedule III of the Controlled Substances Act, but evidence of actual abuse was scarce and did not support the designation. In 1995, the drug was added to the agency’s “emerging drugs list” and finally labeled Schedule III in 1999, making it illegal to possess without a prescription. As a result, it was commonly stolen from hospitals or smuggled from overseas. [37]
Current use
Although it’s a controlled substance in most of the Western world, ketamine is widely used both in medicinal and recreational purposes. Ketamine infusion clinics have opened across the world, and its promising results as a treatment for depression is causing its medical popularity to rise.
Curious about supporting your mental health through ketamine? Check out Third Wave’s vetted directing of ketamine clinics and ketamine assisted psychotherapy therapists in the US .
Medicinal use
Thanks to its unique pharmacological properties and a growing body of evidence of its clinical benefits, ketamine has withstood the test of time as a medical practice.
Research increasingly shows ketamine’s potential as a treatment for severe depression, the drug is seeing a resurgence in acceptance and use.
Non-medicinal use
According to the 2016 Global Drug Survey of roughly 100,000 respondents who use (mostly illicit) psychoactive substances, ketamine was among the top ten used worldwide. It had a global past-year prevalence of 6.72%—compared with 11.75% for psilocybin and 12.89% for LSD. [40]
In 2006, people between the ages of 18 and 25 were most likely to use ketamine in the U.S., at a rate comparable to PCP. An estimated 2.3 million people aged 12 or older had used ketamine at least once in their lifetimes, and around 203,000 had used it in the past year. [41] Between 2000 and 2011, the rate of ketamine use among U.S. high school students steadily declined, never reaching more than 2.6%. [42]
Ketamine is reported to be around five times more prevalent in the UK than in the US. [43] Statistics from 2013 show a similar age bracket—20-24-year-olds—as the most likely group to use it. It has also been identified as one of the most likely drugs to be used in combination with other substances, with around 50% of UK users mixing it, often with alcohol. [44]
“Ketamine is a cat or horse tranquilizer and not suitable for human consumption”
A common misrepresentation by the media, this myth gives the impression that ketamine use in humans is somehow deviant. But despite its wider use in veterinary medicine, ketamine was originally devised for and tested on humans. [37] Nowadays, it’s perhaps the most effective therapy for treatment-resistant depression, while remaining one of our most reliable anesthetics. In fact, it’s one of only two injected general anesthetics listed on the World Health Organization’s Model List of Essential Medicines—a core list of “the most efficacious, safe and cost-effective medicines for priority conditions.” [46]
“Ketamine makes you psychotic”
Ketamine will not cause psychosis in someone who doesn’t have a prior history of a psychotic disorder like schizophrenia. The drug does induce a dissociative state, which can cause disorienting changes in perception. However, these are temporary and end shortly after the drug wears off.
“Ketamine is highly addictive”
Where can i find legal ketamine clinics.
To support your journey with experiencing ketamine legally, we’ve curated, verified, and vetted legal ketamine clinics along with KAP therapists in our psychedelic provider directory; maybe you can find the right one for you.
Can ketamine be detected in a drug test?
Ketamine isn’t usually tested for, but it may be included in some extended screens. Because of its chemical similarities to PCP, it may also trigger a false positive. Ketamine itself stays in your system for 2-4 days, and it’s detectable in your urine throughout this period. However, tests looking for ketamine specifically will detect norketamine (the major metabolite) in blood and urine for up to 14 days, or longer in frequent users. [47]
Is there a way to work with ketamine in the comfort of my own home?
Yes! We’ve partnered with Joyous , who offers a very low-dose ketamine treatment plan as a subscription to “help people thrive, not just survive.” Those who subscribe will receive daily guidance and personalized recommendations on how to optimize your treatment through our Joyous Care Navigator.
Can I test my ketamine to see if it’s safe to take?
Testing your ketamine is always good practice even when you trust your supplier. Reagent test kits from Bunk Police can identify hundreds of adulterants and substitutes , offering peace of mind and potentially saving your life.
Methoxetamine (MXE), for example, may be risky when mis-sold as ketamine. The Mandelin reagent can help to rule it out. Simply place a tiny amount of ketamine into a sterile test tube or onto a sterile white ceramic surface and add a few drops of the reagent. Then check the color change (or lack thereof) against the supplied spectrum booklet.
Can ketamine cause psychological trauma?
Frequent users may notice long-term cognitive impairments but occasional users tend not to. In any case, symptoms like perceptual distortion, memory loss, and delusional thinking are likely to fade over time. Nonetheless, it’s easy to feel “crazy” in the dissociative state itself, which is known as “acute psychosis” and sometimes referred to as “bad trips.” As with any psychedelic, set and setting are important.
How long does ketamine last?
When used intranasally, ketamine lasts for up to an hour. It can last up to two hours when ingested.
What does ketamine feel like?
Ketamine induces a disassociative state as well as feelings of euphoria, pain relief, and both visual and auditory hallucinations.
What does ketamine look like?
Ketamine is a white crystal that is usually crushed into a powder.
Are there risks?
While overdose fatalities are rare, there are certain risks involved. As a general anesthetic, ketamine heavily impairs physical movement and people have been known to drown or otherwise injure themselves as a result. Serious injuries may go unnoticed and therefore untreated because of the analgesic effect. Long-term health risks are associated with frequent use.
What is the safest way to take ketamine?
Some users prefer intramuscular injection because snorting can lead to blocked nostrils and watery eyes. Injection tends to be more intense, which is a plus for some users but a minus for others. Muscle pain is also common when injecting, especially with lower gauge needles. Intravenous injection is rare among recreational users, as is oral use, perhaps because of the unpleasant taste.
Can I use ketamine to microdose?
A mood enhancement effect has been noticed, particularly among sufferers of depression, with sub-perceptual doses of up to 0.2 mg/kg. However, ketamine is not considered safe for microdosing at the same rate as LSD or psilocybin.
Further information on microdosing with ketamine can be found here .
Does ketamine produce tolerance?
Tolerance builds up slowly, often over a period of weeks with regular use.
Is ketamine addictive?
You can easily form a psychological habit of taking ketamine if it’s readily available. Although there’s no risk of physical addiction, it’s a good idea to set personal limits to avoid habituation.
What are the side effects of ketamine?
Common side effects of ketamine include elevation in heart rate and blood pressure, confusion, disorientation, dissociation, loss of coordination, agitation, nausea, bad hallucinations, flashbacks, and tremors or shaking.
Less common side effects include depression in heart rate and blood pressure, seizures, and laryngeal spasms which can lead to suffocation.
Side effects of high doses of ketamine include chest pain, drastic changes in blood pressure, arrhythmia, amnesia, coma, fever, hallucinations of terrors, severe panic and anxiety, muscle rigidity, and respiratory depression (especially if combined with substances that act as CNS depressors.
A side effect of chronic abuse of ketamine is kidney toxicity.
Can I overdose on ketamine?
Although deaths from ketamine overdose exclusively are not very likely to happen, the settings in which ketamine is consumed are usually supportive of simultaneous substance ingestion, which is more likely to cause a tragic outcome. Ketamine is also more potent than cocaine or speed, which are used, and can be procured in similar contexts. It is unforgiving when it comes to misdosing.
Can I mix it with other drugs?
Ketamine should never be mixed with drugs that depress breathing. These include alcohol, GHB/GBL, opioids, and tramadol. Doing so increases the risk of unconsciousness and choking (e.g. on vomit). Benzodiazepines, MAOIs, amphetamines, and cocaine are also risky in combination with ketamine. While the drug appears to be safe with LSD, MDMA, and cannabis, among others, combinations are generally advised against. Find out more here .

Can I get a prescription for ketamine?
[1] Jansen, K. (2004). Ketamine: Dreams and Realities. Sarasota, FL: MAPS. Retrieved from: https://amzn.to/2BBI9Mj .
[2] Erowid. (2007). Ketamine Effects. Retrieved from: https://erowid.org/chemicals/ketamine/ketamine_effects.shtml .
[3] PsychonautWiki. Ketamine. Retrieved from: https://psychonautwiki.org/wiki/Ketamine .
[4] Kurdi, M. S., Theerth, K. A., Deva, R. S. (2014). Ketamine: Current applications in anesthesia, pain, and critical care. Anesthesia Essays and Researches, 8(3), 283-290. Retrieved from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4258981/?report=printable .
[5] Mion, G., Villevieille, T. (2013). Ketamine pharmacology: an update (pharmacodynamics and molecular aspects, recent findings). CNS Neuroscience & Therapeutics, 19(6), 370-80. Retrieved from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6493357/pdf/CNS-19-370.pdf .
[6] Zou, X. et al. (2009). Prolonged exposure to ketamine increases neurodegeneration in the developing monkey brain. International Journal of Developmental Neuroscience, 27(7), 727-731. Retrieved from: https://onlinelibrary.wiley.com/doi/abs/10.1016/j.ijdevneu.2009.06.010 .
[7] Yan, J., Huang, Y., Chen, J., Jiang, H. (2014). Repeated administration of ketamine can induce hippocampal neurodegeneration and long-term cognitive impairment via the ROS/HIF-1α pathway in developing rats. International Journal of Experimental Cellular Physiology, Biochemistry, and Pharmacology, 33(6), 1715-32. Retrieved from: https://www.karger.com/Article/Pdf/362953 .
[8] Morgan, C. J., Riccelli, M., Maitland, C. H., Curran, H. V. (2004). Long-term effects of ketamine: evidence for a persisting impairment of source memory in recreational users. Drug and Alcohol Dependence, 75(3), 301-8. Retrieved from: https://www.sciencedirect.com/science/article/abs/pii/S0376871604000717?via%3Dihub .
[9] Reuters Health. (2009). Harmful effects seen with repeated ketamine abuse. Retrieved from: https://www.reuters.com/article/us-ketamine-abuse-idUSTRE5AJ40T20091120 .
[10] Morgan, C. J., Monaghan, L., Curran, H. V. (2004). Beyond the K-hole: a 3-year longitudinal investigation of the cognitive and subjective effects of ketamine in recreational users who have substantially reduced their use of the drug. Addiction, 99(11): 1450-61. Retrieved from: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1360-0443.2004.00879.x?sid=nlm%3Apubmed .
[11] Freeman, T. P. et al. (2009). Superstitious conditioning as a model of delusion formation following chronic but not acute ketamine in humans. Psychopharmacology, 206(4): 563-73. Retrieved from: https://link.springer.com/article/10.1007/s00213-009-1564-x .
[12] Mak, S. K. et al. (2011). Lower urinary tract changes in young adults using ketamine. The Journal of Urology, 186(2), 610-4. Retrieved from: https://www.auajournals.org/doi/10.1016/j.juro.2011.03.108 .
[13] Niesters, M., Martini, C., Dahan, A. (2014). Ketamine for chronic pain: risks and benefits. British Journal of Clinical Pharmacology, 77(2), 357-367. Retrieved from: https://bpspubs.onlinelibrary.wiley.com/doi/epdf/10.1111/bcp.12094 .
[14] Hanna, J. (2010). KLUTS: Ketamine and Lower Urinary Tract Symptoms. Erowid Extracts, 19, 12-4. Retrieved from: https://erowid.org/chemicals/ketamine/ketamine_article2.shtml .
[15] Drug Abuse Warning Network. (2009). National Estimates of Drug-Related Emergency Department Visits. Retrieved from: https://www.samhsa.gov/data/sites/default/files/DAWN2k11ED/DAWN2k11ED/DAWN2k11ED.pdf .
[16] EMCDDA. (2002). Report on the risk assessment of ketamine in the framework of the joint action on new synthetic drugs. Retrieved from: https://www.emcdda.europa.eu/system/files/publications/173/Risk3_62941.pdf .
[17] Moore, K. A., Kilbane, E. M., Jones, R., Kunsman, G. W., Levine, B., Smith, M. (1997). Tissue distribution of ketamine in a mixed drug fatality. Journal of Forensic Science, 42(6), 1183-5. Retrieved from: https://www.astm.org/DIGITAL_LIBRARY/JOURNALS/FORENSIC/PAGES/JFS14283J.htm .
[18] Brain & Behavior Research Foundation. Dr. Carlos Zarate Carries the Torch toward FDA Approval of Rapid-Acting Antidepressant. Retrieved from:
[19] Oksman, O., (2016). Depressed? Your doctor might soon prescribe ketamine. The Guardian. Retrieved from: https://www.bbrfoundation.org/content/dr-carlos-zarate-carries-torch-toward-fda-approval-rapid-acting-antidepressant .
[20] Park, A. (2016). ‘Club Drug’ Ketamine Provides Hope in Fight Against Depression. TIME. Retrieved from: https://time.com/4326167/depression-ketamine/ .
[21] Insel, T. (2014). Post by Former NIMH Director Thomas Insel: Ketamine. NIH. Retrieved from: https://www.nimh.nih.gov/about/directors/thomas-insel/blog/2014/ketamine.shtml .
[22] Scutti, S. (2016). Party Drug ketamine closer to approval for depression. CNN. Retrieved from: https://edition.cnn.com/2016/08/17/health/ketamine-depression-treatment/index.html .
[23] Duman, R. S., Li, N. (2012). A neurotrophic hypothesis of depression: role of synaptogenesis in the actions of NMDA receptor antagonists. Philosophical Transactions of the Royal Society B, 361(1067). Retrieved from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3405673/pdf/rstb20110357.pdf .
[24] Li, N. et al. (2010). mTOR-Dependent Synapse Formation Underlies the Rapid Antidepressant Effects of NMDA Antagonists. Science, 329(5994), 959-964. Retrieved from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3116441/pdf/nihms293810.pdf .
[25] Krupitsky, E. M., Grinenko, A. Y. (1998). Ten Year Study of Ketamine Psychedelic Therapy (KPT) of Alcohol Dependence. The Heffter Review of Psychedelic Research, 1, 56-61. Retrieved from: https://www.heffter.org/wp-content/uploads/2020/04/chapter8.pdf .
[26] Devlin, H. (2017). Radical ketamine therapy could treat alcohol addiction. The Guardian. Retrieved from: https://www.theguardian.com/society/2017/jan/24/radical-ketamine-therapy-could-treat-alcohol-addiction-erase-memories .
[27] University of Exeter. Ketamine for reduction of Alcohol Relapse (KARE). Retrieved from: https://psychology.exeter.ac.uk/kare/ .
[28] Krupitsky, E. M., Burakov, A. M., Dunaevsky, I. V., Romanova, T. N., Slavina, T. Y., Grinenko, A. Y. (2007). Single Versus Repeated Sessions of Ketamine-Assisted Psychotherapy for People with Heroin Dependence. Journal of Psychoactive Drugs, 39(1). Retrieved from: https://www.researchgate.net/publication/6308479_Single_Versus_Repeated_Sessions_of_Ketamine-Assisted_Psychotherapy_for_People_with_Heroin_Dependence .
[29] Browne-Miller, A. (Ed.). (2009). The Praeger International Collection on Addictions. Westport, CT: Praeger Publishers. Retrieved from: https://amzn.to/31f8QBl .
[30] Ziegler, M. (2016). Ketamine: A Transformational Catalyst. MAPS Bulletin Winter 2016, 26(3). Retrieved from: https://maps.org/news/bulletin/articles/410-bulletin-winter-2016/6470-ketamine-a-transformational-catalyst .
[31] Kent, J. (1996). The Ketamine Konundrum. Erowid. Retrieved from: https://erowid.org/chemicals/ketamine/ketamine_info3.shtml .
[32] Jansen, K. L. R. (1999). Ketamine and Quantum Psychiatry. Asylum Magazine, 11(3), 19-21. Retrieved from: https://erowid.org/chemicals/ketamine/ketamine_journal5.shtml .
[33] DEA. (2015). Drugs of Abuse. Retrieved from: https://www.dea.gov/sites/default/files/2018-06/drug_of_abuse.pdf .
[34] 21 CFR 522.1222 – Ketamine. Retrieved from: https://www.law.cornell.edu/cfr/text/21/522.1222 .
[35] DrugWise. What are the UK drug laws? Retrieved from: https://www.drugwise.org.uk/what-are-the-uk-drug-laws/ .
[36] Erowid. (2016). Ketamine Legal Status. Retrieved from: https://erowid.org/chemicals/ketamine/ketamine_law.shtml
[37] Jansen, K. L. R. (2001). A review of the non-medical use of ketamine: use, users and consequences. Journal of Psychoactive Drugs, 32(4), 419-33. Retrieved from: https://www.tandfonline.com/doi/abs/10.1080/02791072.2000.10400244
[38] Domino, E. F., Chodoff, P., Corssen, G. (1965). Pharmacologic effects of CI-581, a new dissociative anesthetic, in man. Clinical Pharmacology & Therapeutics, 6, 279-91. Retrieved from: https://deepblue.lib.umich.edu/bitstream/handle/2027.42/116940/cpt196563279.pdf?sequence=1&isAllowed=y
[39] Hooper, J. (1983). John Lilly: Altered States. Omni Magazine. Retrieved from: https://erowid.org/culture/characters/lilly_john/lilly_john_interview1.shtml
[40] Global Drug Survey. (2016). What we learned from GDS2016: An overview of our key findings. Retrieved from: https://www.globaldrugsurvey.com/wp-content/uploads/2016/06/TASTER-KEY-FINDINGS-FROM-GDS2016.pdf .
[41] SAMHSA. (2008). The NSDUH Report -Use of Specific Hallucinogens: 2006. Retrieved from: https://datafiles.samhsa.gov/study-publication/use-specific-hallucinogens-2006-nid15301 .
[42] The University of Michigan. (2011). Monitoring the Future. Retrieved from: https://www.icpsr.umich.edu/icpsrweb/NAHDAP/studies/34409/summary .
[43] Daly, M. (2016). Why Do the British Love Ketamine So Much? Vice. Retrieved from: https://www.vice.com/en_uk/article/nnkjed/why-do-the-british-love-ketamine-so-much .
[44] ACMD. (2013). Ketamine: a review of use and harm. Retrieved from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/264677/ACMD_ketamine_report_dec13.pdf .
[45] Hatton, C. (2015). The Ketamine Connection. BBC News. Retrieved from: https://www.bbc.co.uk/news/resources/idt-bc7d54e7-88f6-4026-9faa-2a36d3359bb0 .
[46] World Health Organization. (2015). 19th WHO Model List of Essential Medicines. Retrieved from: https://www.who.int/medicines/publications/essentialmedicines/EML2015_8-May-15.pdf .
[47] Erowid. (2015). Ketamine Drug Testing. Retrieved from: https://erowid.org/chemicals/ketamine/ketamine_testing.shtml .
Related Posts

Related Podcasts

Ketamine 101: Uses, Safety, & Dosage
Ketamine was invented to replace PCP as an anesthetic. Today, it’s considered one of the premiere treatments for depression. Here’s how it works.
What is Ketamine?
Other names for ketamine, what does ketamine feel like, how long does ketamine remain in the system, ketamine dosages according to form of administration, how much does ketamine therapy cost, is ketamine therapy covered by insurance, who is not a good candidate for ketamine therapy, is ketamine legal, side effects of ketamine, is ketamine addictive, ketamine overdose, how strong is ketamine compared to other psychedelics, 1. ketamine for anesthesia, 2. ketamine for depression, 3. ketamine for pain, ketamine in veterinary medicine, the history of ketamine, s-ketamine vs. r-ketamine: what’s the difference, what is kitty flipping, what the future of ketamine looks like, subscribe to tripsitter: newsletter & podcast.
Ketamine has been around since the 1960s where it was used exclusively as a surgical anesthetic .
Over the past three decades, there’s been a growing interest in ketamine as a recreational hallucinogenic and dissociative drug.
Even more recently, ketamine has been shown to offer a unique mechanism for treating depression — unlike anything we’ve ever seen before.
In this article, we’ll cover everything you need to know about ketamine. How it works, what the basic dosages are for each level of effects, and more.
Ketamine is classified as a dissociative hallucinogenic — which distorts the perception of sights, sounds, emotions, and decouple one’s first-person experience from reality. Users feel “outside their body.”
Chemically-speaking, ketamine is a member of the larger arylcyclohexylamine class of drugs . This group includes other popular compounds like PCP (phencyclidine) , DCK (deschloroketamine) , 2-FDCK (2-fluorodeschloroketamine) , and MXE (methoxetamine).
In medicine, ketamine is used as an analgesic . It doesn’t directly block pain signals like an opiate — instead, dissociative analgesics disconnect the thalamus from the cortex. When this happens, the body still feels pain, but the brain simply “doesn’t care.” We don’t actually feel bothered by the pain.
Experts on the use of ketamine, such as Albert Dahan (professor of anesthesiology at The University of Leiden), suggest ketamine to be “one of the best painkillers ever made.”
Beyond its use as a painkiller, ketamine is used as a recreational drug (illegally). The experience changes according to the dose.
Lower doses feel a lot like being drunk on alcohol.
Higher doses are more similar to psychedelics like DMT or salvia, but with a distinct dissociative action on top of any psychedelic visuals or effects.
A high dose of ketamine can lead to an experience called a “ K-hole ” — which is an extremely intense dissociative hallucination that can be both beautiful and terrifying all at once.
More recently, research has shown that low doses of ketamine offer powerful antidepressant qualities . It works through entirely different mechanisms than conventional antidepressant medications.
Unlike most drugs, ketamine targets many different receptors at once, making it very difficult to study exactly what’s going on or how it works.
There’s currently one FDA-approved ketamine spray called Spravato® — which is prescribed for treatment-resistant depression (depression that doesn’t improve with conventional medications).
Ketamine: Specs & Technical Details
Ketamine is sold under a wide range of different street names as well as various pharmaceutical trade names.
Here are some of the other names for ketamine:
The effects of ketamine are dependent on the dose you use, your individual body weight and metabolism, how often you use it, what form you’re using ( intravenous , troches / lozenges , intranasal ), and whether you’re using ketamine alone or with other substances.
In lower doses, the effects of ketamine resemble alcohol intoxication. It causes feelings of mild euphoria, as well as visual and auditory perceptual changes. It makes users feel as though they’re floating or operating on autopilot. Low doses are mildly stimulating and can make users feel more social or energetic.
Higher doses of ketamine feel very different. They can make you feel withdrawn and introverted. People often report feeling very light and floaty and often experience intense hallucinations, blurred vision, and out-of-body experiences.
In very high doses , people experience what’s commonly referred to as a K-hole — which involves strong out-of-body hallucinations. This is a demonstration of the dissociative aspect of ketamine to its fullest extent. Users feel as though they’re perpetually falling into blackness. It’s as if the fabric of time, as well as one’s sense of self is dissolving.
Some describe the K-hole experience to be like “peering into the keyhole of existence.”
A K-hole can feel both terrifying and exhilarating at the same time.
The effects of ketamine may include:
- Difficulty thinking logically
- Reduced anxiety
- Delusions & ego inflation
- Disinhibition
- Memory loss
- Spatial disorientation
- Altered perception of time & space
- Sedation or fatigue
- Spontaneous bodily sensations (tingling, pulsating)
- A feeling of being light or floating
- Loss of muscle coordination or control
- Reduced sensation of pain
- Increased salivation
- Lowered libido
- Nausea & vomiting
- The feeling of being on “autopilot” or not in control of your body
How Long Does Ketamine Last?
Ketamine is not a long-lasting drug . The effects usually take between 30 and 60 minutes to reach their full effect, which remain in place for about an hour before starting to taper off. These numbers will vary depending on the form of administration.
- Insufflated (snorted) — Effects kick-in within 5–15 minutes. Peak effect reached in 30 minutes. Total duration between 1 and 3 hours depending on dose.
- Intravenous (IV) — Effects kick in within 60 seconds. Peak reached in 3–5 minutes. Total duration between 40 and 60 minutes. Some lingering effects up to 2 hours.
- Sublingual — Effects from troches or lozenges kick in within 5-10 minutes. Peak effect reached in 30 minutes. Total duration between 1–3 hours depending on dose.
- Oral — Effects kick in within 20-30 minutes. Peak reached by 60 minutes. Total duration 2–4 hours.
- Intramuscular (IM) — Effects kick in within 1–5 minutes. Peak effects in 10–15 minutes. Total duration up to 2 hours.
- Rectal/Suppositories — Effects kick in within 15–20 minutes. Peak effects reached in 30-40 minutes. Total duration 1–2 hours.
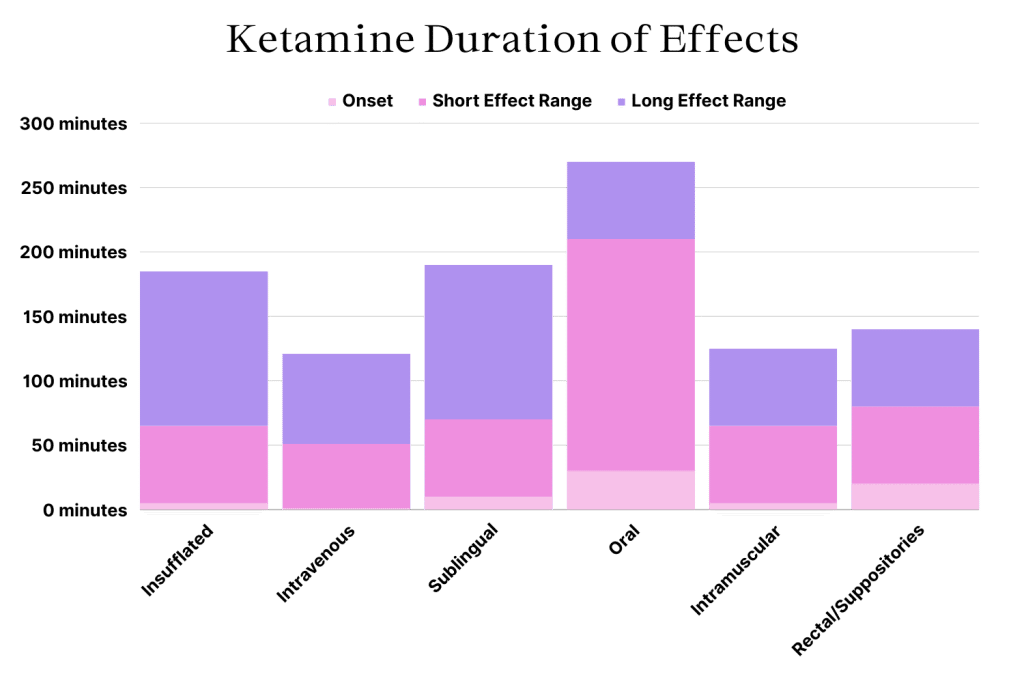
Ketamine is rapidly metabolized by the liver into norketamine and other inactive metabolites, which are then eliminated through the urine.
The half-life of ketamine is 2.5 hours and it takes about 5 or 6 half-lives before a drug is completely cleared from the body. This means ketamine can remain detectable in the bloodstream for around 15–24 hours, depending on factors like dosage and frequency of use.
People who use ketamine often will take longer for the drug to be eliminated from the body entirely. This can take up to 48 hours in the bloodstream, and up to 72 hours in the urine.
All of this means that ketamine will typically show up on a drug test up to 24 hours for saliva tests, 48 hour later for urine and blood tests, and 4 months for hair or fingernail tests.
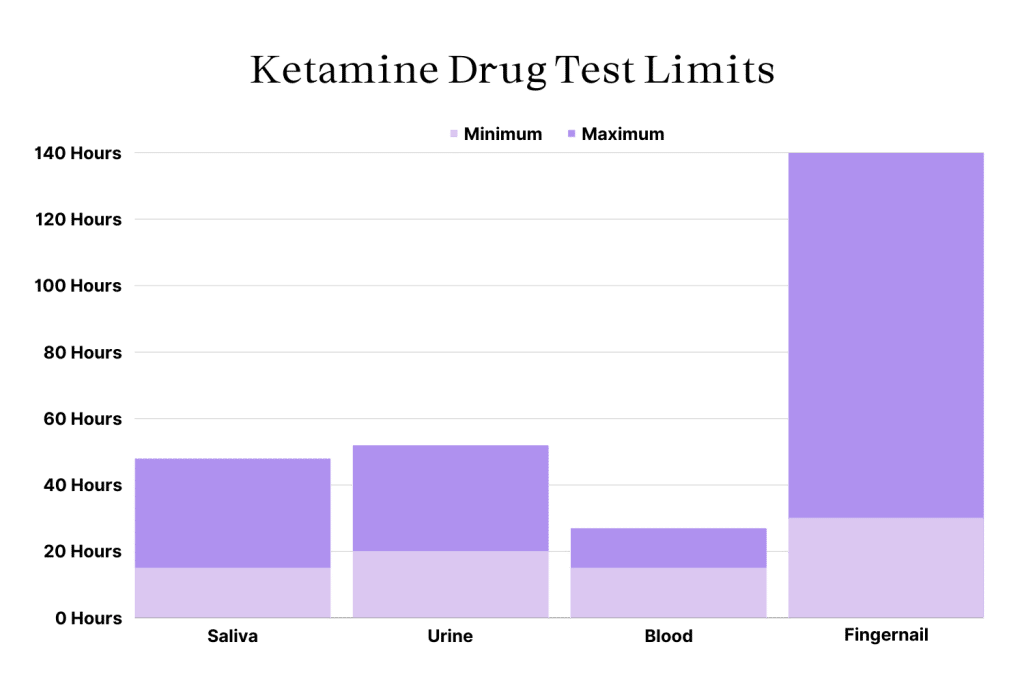
What’s The Dose of Ketamine?
Ketamine is highly dose-dependant — meaning the effects of high dose ketamine is dramatically different from low-dose ketamine.
The threshold dose refers to the smallest dose that produces noticeable psychoactive effects.
The lower dose ranges of ketamine — starting with the threshold dose — produces mild alterations in perception and feels most similar to GHB or alcohol. Lower doses create a sense of disinhibition, mild dissociation and depersonalization, and is even slightly stimulating. This makes low dose ketamine a popular party drug.
The standard psychoactive dose refers to the most common psychoactive dose range used for a given drug. This is the dose range that produces all the characteristic effects expected of ketamine — strong dissociation, visual and auditory perceptual changes, and sometimes even out of body experiences.
High doses produce significantly more dissociative and out-of-body experiences. Very intense dissociation from ketamine is referred to as a K-hole — which begins somewhere around the 200 mg mark for oral and sublingual ketamine.

What is Ketamine-Assisted Psychotherapy?
The field of psychedelic-assisted psychotherapy (PAP) is growing at an exponential rate.
So far, the only psychedelic that’s been approved for use in therapy is ketamine, but MDMA-assisted therapy and psilocybin-assisted therapy are both just around the corner.
Over the last 50 years, there have been over 70 individual Phase II clinical trials exploring the benefits of ketamine for conditions such as depression, obsessive-compulsive disorder (OCD), post-traumatic stress disorder (PTSD), drug addiction, and much more. This has fuelled a boom in the number of clinics around the world offering off-label ketamine for a wide range of mental health disorders.
At the moment, ketamine is only approved by the FDA as a form of anesthesia during surgery — with the exception of Spravato Ketamine Nasal Spray which is approved for treatment-resistant depression. Most of the ketamine being used with ketamine-assisted therapy are not formally approved by the FDA or equivalent regulators around the world.
There are 2 main forms of ketamine-assisted therapy in practice today:
- In-Person Ketamine Therapy — In-person clinics are the only way to get the more powerful IV or IM ketamine injections. This form of therapy is expensive in the short-term, but carries the greatest chances of getting longer-lasting results.
- Online (Telehealth) Ketamine Therapy — Positioned as the most affordable form of ketamine therapy. It involves an online consultation to attain the prescription needed to continue therapy. Ketamine lozenges are then sent in the mail and sessions are monitored through online video platforms.
- Spravato Nasal Spray — As the only FDA-approved use of ketamine for treating depression, this ketamine preparation has been gaining a lot of popularity lately and is covered by some insurance providers in the US.
Related: Does Ketamine Therapy Get You High?
Ketamine is promised as a quick, long-term solution to mental health conditions like depression, PTSD, and addiction. Ketamine providers are using this argument to justify the relatively high cost of treatment.
However, this isn’t how it’s been playing out in practice. Ketamine therapy users tend to require ongoing treatment — so therapy can get expensive, quickly.
Here’s what you can expect for the first month of ketamine therapy depending on the type of treatment you’re seeking. Note that consecutive months tend to be cheaper thanks to refill discounts offered by many (but not all) companies in this space.
Ketamine infusions tend to be the most expensive upfront — costing between $350 and $500 for a single session (usually purchased in packages of 6 to 8).
Online ketamine clinics boast cheaper per-session costs (around $150–$200 per session), but often fail to provide enough adjunctive support for users to stop taking ketamine without relapsing.
Spravato ketamine nasal spray is the most expensive form of ketamine therapy outside of the luxury clinic experiences which can extend into the thousands of dollars per session.
Related: How Much Does Psychedelic-Assisted Psychotherapy Cost?
Most insurance providers won’t cover the cost of ketamine therapy . The landscape surrounding psychedelic-assisted therapy is continually evolving, and more providers are adding ketamine to their premium-tier packages all the time — but this is highly dependant on the individual provider and which plan you’re on.
Some companies, such as Blue Cross Blue Shield, Gilsbar, Zelis/ PPO Plus, United Healthcare, United Behavioral Health, and Cigna Behavioral Health are now covering some or all of the cost for Spravato ketamine nasal spray, but not other forms of ketamine therapy. This is largely because Spravato is the only FDA-approved ketamine treatment for depression.
While ketamine is widely considered a “low-risk” drug — there are situations where ketamine can pose an elevated risk. Not all people are suitable for ketamine therapy.
Avoid ketamine therapy if you have any of the following:
- A history or family history of schizophrenia or psychosis
- Have not first attempted treatment with other (approved) medications or therapies
- A history of cardiovascular disease, including hypertension
- A history of bladder, kidney, or liver disease
- A history of substance abuse disorder
- Are unable to understand and provide informed consent
- Are pregnant or nursing
- Have known allergies to ketamine or other arylcyclohexylamines
Ketamine is available via prescription only . It’s mainly reserved for emergency medicine and surgery.
Some doctors may prescribe ketamine for the treatment of pain (usually in combination with an opiate), as well as for depression — but only when other treatments have been attempted first.
There are no countries where ketamine is legal for recreational use. This means any ketamine you order online or in-person without a valid prescription is illegal or black market ketamine. Some of this black market ketamine is stolen from veterinarian supplies — some are made in an illicit lab with varying levels of purity.
While we never condone the use of illicit drugs, we’d like to remind you to always test your drugs before you use them should you choose to do so. One of the biggest risks of taking black market ketamine is the adulteration with other dangerous drugs — such as NBOMes or fentanyl.
There are a few prescription ketamine drugs on the market today, including:
- Ketalar® — JHP Pharmaceuticals
- Ketaject® — Phoenix Pharmaceuticals
- Ketaset® — Zoetis
- Spravato® — Johnson & Johnson
Ketamine Risks & Side Effects
Overall, ketamine is considered very safe and is unlikely to lead to overdose — unless mixed with other drugs or alcohol.
As an analgesic, ketamine is one of the safest drugs available and isn’t nearly as likely to lead to respiratory or cardiovascular emergencies compared to other analgesics.
While ketamine is addictive, it has a much lower risk of addiction compared to other prescription medications — especially pain medications or antianxiety medications.
With that said, ketamine does come with inherent risks:
- Ketamine can increase the risk of heart attack or stroke
- Frequent use has been linked with bladder disease
- Blackmarket ketamine may be laced with other, more dangerous drugs
- Ketamine is often used as a date rape drug
- Ketamine can interfere or interact with other medications or alcohol
- Ketamine stops you from feeling pain, increasing your risk of developing serious injuries
- Ketamine can be addictive with more frequent use
- The psychoactive effects of ketamine can be terrifying and may trigger psychosis in susceptible individuals
It’s important to have a trip sitter around and follow the four pillars of safe psychedelic use if you plan on experiencing the deeper levels of ketamine (K-hole).
This experience will cause you to lose control of your body and can be extremely terrifying. So it’s critical that you have someone you trust nearby, and only take the drug in a safe and comfortable environment.
The most common side-effects of ketamine are dissociation (sometimes considered a primary effect), high blood pressure, and tachycardia (rapid heart rate).
These side effects are rarely severe, and tend to only pose danger to those with prexisting cardiovascular disease or those taking other medications that affect heart rate and blood pressure.
Side effects of ketamine include, but are not limited to:
- High blood pressure
- Perceptual disturbances
- Loss of coordination
- Slurred speech
- Intoxication & disinhibition
- Bladder pain
- Dissociation (out-of-body experiences)
Ketamine is addictive and is often abused.
While it’s still not clear whether ketamine is physically addictive, you can develop tolerance — which means you’ll need to take a higher dose of the drug to get the same experience.
Users become addicted to the dissociative effects of the drug. They compulsively use the substance as a way to find an escape from their reality — which may feel objectively painful or uncomfortable. Addiction is defined as any act of compulsively using a substance (or activity) to find relief, despite clear negative consequences to using the drug.
Most people don’t experience withdrawal symptoms after stopping ketamine — with the exception of cravings for more ketamine (this is considered a psychological dependency). Physically, ketamine is less addictive than drugs like opiates, alcohol, amphetamines, or benzodiazepines.
With that said, heavy users may experience sleep disturbances, tremors, sweating, rapid heart rate, appetite loss, erectile dysfunction, and fatigue for a few days.

One of the biggest advantages ketamine brings to the medical field is it’s low-risk of causing overdose. Ketamine doesn’t affect respiration the way opiates do, and it has only a minor impact on the heart, brain, and other internal organs — even in high doses. It’s also relatively short-lived and fast-acting — two factors that significantly reduce the chances of consuming toxic doses.
With that said, ketamine can still cause overdoses that can result in long-term damage or death.
Ketamine overdoses become much more common when combined with other drugs or alcohol — particularily other depressants such as GHB, benzodiazepines, barbiturates, opiates, and alcohol.
The LD50 (lethal dose for 50% of individuals) for ketamine is 25 mg/kg (oral) or 11.3 mg/kg (IV) [ 13 , 14 ]. For a 70 kg human this works out to around 791 mg intravenously or 1750 mg orally— both of which are over 100 times higher than what’s considered a heavy dose of ketamine.
The biggest dangers come from loss of consciousness and disinhibition from ketamine. People who are unable to control their body are placed at a significantly higher risk of suffocation (usually on vomit) and critical injuries (from cars, other people, or falls). Ketamine also induces disinhibition, so even those who remain in some control of their body are more likely to place themselves in risky situations that could become life-threatening.
Signs and symptoms of ketamine overdose include:
- Loss of consciousness
- Slowed breathing
- Slow heart rate
- Low blood pressure
- Apnea (periods of ceased breathing, followed by rapid breathing)
- Lack of muscle coordination
Unfortunately, there are no good ketamine reversal agents currently available. Some drugs, such as various benzodiazepines and certain antipsychotic medications can be used to treat individual symptoms of ketamine overdose, but not reverse the effects the way Narcan does for opiates or flumazenil does for benzodiazepines.
Ketamine can be very powerful. While it’s less potent than other psychedelics in terms of the dose, the effects can become much more profound than many other psychedelic substances.
This drug is most comparable in terms of effects to PCP, but less potent and with a much safer profile.
Lower doses of ketamine are similar in their effects to MDMA , MDA, 2C-B , or 2C-E .
DXM , xenon gas , and nitrous oxide all work through similar mechanisms and have a similar dissociative effect.
The full dose of ketamine that leads to a K-hole experience is similar to DMT or salvia but feels subjectively different. A K-hole is usually dark (in more of a “low-light” way than evil or depressing), shadowy, and often involves the feeling of falling or being rapidly teleported to different locations.
How Ketamine Works
Ketamine is considered a “dirty drug.” This doesn’t mean the drug is toxic or poisonous — it refers to the specificity of the drug on its target receptors.
Ideally, a pharmaceutical targets one specific receptor to cause its effect. This makes its effects predictable and easier to study and understand. These drugs are precise and don’t cause any overflow effects on unrelated or irrelevant receptors.
Ketamine, on the other hand, is messy — it activates several different types of receptors, each with a different result. Ketamine stimulates some receptors and inhibits others.
This makes ketamine very difficult to study and understand. It’s also what makes this compound so useful for complex conditions like depression.
Ketamine has been shown to target the following receptors in the brain:
- Opioid receptors
- Blocks NMDA (glutamate) receptors at low doses
- Stimulates NMDA (glutamate) receptors at high doses
- Cholinergic receptors
- Dopamine receptors
- Adrenergic receptors
- Innate repair (HCN1 receptors)
- Sodium channels
Ketamine is primarily used as an anesthetic agent in patients undergoing surgery or following a severely traumatic event. It’s more effective for blocking pain than opiate painkillers, which work by activating the opioid receptors in the spinal cord and brain.
Ketamine works like most other dissociative analgesics — such as PCP, nitrous oxide, and DXM. They work by temporarily blocking the NMDA receptors — thus inhibiting communication between the cortex (the outer portion of the brain where higher thought occurs) from the thalamus. The thalamus is responsible for relaying messages from sensory information like pain, emotion, vision, and taste.

Studies have shown that ketamine owes most of its painkilling effects to its ability to block glutamate receptors (in lower doses) [ 2 ]. It also activates the opioid receptors, but to a much lower extent than typical opiate painkillers [ 3 ].
Other potential mechanisms for ketamine’s painkilling effects come from its ability to block the muscarinic and nicotinic receptors [ 4 ].
A meta-analysis exploring the outcomes of 11 clinical trials using ketamine for pain found it to be extremely effective for managing severe short-term pain but did not offer a good long-term solution for ongoing chronic pain [ 5 ].
Newer research (beginning in the early 2000s) shows that ketamine is also a powerful antidepressant. It works through mechanisms not offered by any other antidepressant on the market today. The effects of ketamine are fast-acting, exerting improvements in mood in as little as four hours after administration — even in treatment-resistant forms of depression.
Unfortunately, the effects of ketamine only last about seven days before another dose is required. It’s considered a third line of treatment for depression. Only when all other antidepressants have failed is ketamine prescribed to manage depression.
Only one ketamine product has been approved for use by the FDA — an isomer called esketamine, sold under the brand name Spravato®. This drug is made by the pharmaceutical company Janssen — a subsidiary of Johnson & Johnson.

How Spravato (and ketamine in general) works for treating depression is still not well understood. But here’s what we know so far:
Ketamine & Synapse Regrowth
Studies have shown that ketamine stimulates the growth of synapses [ 7 ]. This is an important finding because no other antidepressant that we know of can do this.
Chronic stress depletes the synapses in certain regions of the brain — especially the medial prefrontal cortex. This region is often implicated in the effects of depression. Researchers in the study gave mice ketamine and observed the formation of tiny spikes on the dendrites of the nerve cells. Spikes that survived for a few days after the treatment eventually formed into new synapses.
This effect is likely what causes the long-term benefits of using ketamine. However, this process takes a few days, so there must be other mechanisms that provide more fast-acting effects on depression.
The mechanism ketamine uses to cause this effect is extremely complicated and involves a cascade of effects [ 1 0 , 1 1 ]. It’s believed ketamine has a greater affinity for glutamate receptors that are located on GABA interneurons, which are inhibitory neurons [ 12 ].
Ketamine blocks the effects of these neurons, which cause a downstream increase in glutamate. Excess glutamate activates postsynaptic AMPA receptors, which bolster the effects of BDNF and mTORC1 — which are ultimately responsible for the regrowth of synapses.
Unfortunately, there’s little evidence to suggest that ketamine has a lasting impact on depression. Most studies show that ketamine requires another dose every 2–3 weeks to maintain the antidepressant effects.
Blood Sugar Regulation
Ketamine has been shown to regulate blood sugar levels in regions of the brain associated with depression [ 6 ].
It’s not clear whether this has a direct benefit on depressive symptoms or if it’s a byproduct of other improvements in these brain regions.
Circadian Rhythm Regulation
Ketamine has been shown to improve the body’s ability to regulate the circadian rhythm [ 9 ]. Researchers are still seeking to understand whether these improvements come as a result of improved mood or if this effect contributes to the greater mood regulation instead.
Ketamine is becoming a popular alternative treatment option for tough to treat chronic pain conditions such as fibromyalgia , complex regional pain syndrome (CRPS),postoperative pain, and neuropathic pain.
Research in this field is still evolving, but more studies are released showing promising results for certain types of pain conditions all the time [ 17 ].
For example, a meta analysis published in 2011 involving over 4700 patients found a significant reduction in total postoperative opioid use [ 15 ]. Researchers in this study suggested that patients administered ketamine as part of their post-operative pain management protocols were able to cease opiate medications sooner than those using only opiates. This suggests both an analgesic action and anti-addictive action for ketamine.
However, the effectiveness of ketamine for managing pain remains inconclusive.
For example, a meta analysis examining studies using ketamine for cancer pain reported that relief only lasted 3-hours and resulted in a high incidence of neurological side effects [ 16 ]. Another large-scale meta analysis looking at the role of ketamine as an analgesic for post-operative pain reported no sizeable advantage to using ketamine (poorer pain reduction and increased neurological side effects) [ 18 ].
Ketamine is an interesting analgesic option because it targets several neurotransmitter systems involved with pain transmission. This includes the mu-opiate receptors which are the target for powerful and commonly-used pain medicines like oxycontin, morphine, and hydrocodone.
However, unlike these classic pain medications, ketamine also interacts with other systems, such as the NMDA receptors, serotonin, and dopamine. Some researchers believe these other pathways are the reason why ketamine works so well in patients that haven’t found relief from their chronic pain using more conventional painkillers.
Related: Is Ketamine an Opiate?
Ketamine is widely used in veterinarian medicine as an anesthetic for dogs , cats , and horses undergoing surgery.
It’s considered an ideal anesthetic because of its impressive safety profile compared to other anaesthetic agents.
The primary reason ketamine was developed was to offer a replacement for PCP (phencyclidine) — which was the primary analgesic used for surgery prior to 1970.
Scientists have been searching for an alternative to PCP for a long time. While this drug worked to stop pain and suffering during surgical procedures and after severe traumatic injuries, it often led to long-term side effects like psychosis.
Ketamine was first synthesized by Calvin L. Stevens in 1962. At the time, Stevens was a professor of Chemistry at Wayne State University and worked as a consultant for the Pfizer Pharmaceutical subsidiary, Parke-Davis.
Ketamine (then called CI-581) was first tested on animals and showed very promising results as an analgesic. It was then tested (involuntarily) on prisoners in 1964 [ 1 ]. The results of these studies were enough to prove ketamine was just as effective as PCP, only with a much lower risk of side effects. The drug was finally approved in 1970 for use in medicine, and PCP was quickly removed from service.
Most drugs come in two different enantiomers.
Enantiomers are chemicals that have the exact same chemical structure but are mirror images of each other. Just like your right and left hand. Both hands have the same shape, but in order for them to share the same outline, you have to flip one of them upside down.
There are two enantiomers for ketamine — the “R” and “S” enantiomers.
Ketamine contains both of them at a ratio of around 1:1.
Esketamine (S-ketamine) contains only the “S” ketamine, which is the stronger of the two molecules. S-ketamine is also reported to produce 1.6 times the level of altered body image and hearing, 2.5 times stronger feelings of unreality, and four times the reduction in visual acuity.
Kitty flipping is the practice of mixing ketamine with MDMA. The effects are reported to share a blend of the empathogenic and euphoric effects of MDMA, with the dissociative effects of ketamine. This blend is commonly used at raves or music festivals.
It’s not wise to mix psychedelic drugs, especially synthetic drugs that could contain any number of adulterants already. Always test your substances before you take them, and use a smaller dose should you decide to mix two or more substances together.
There’s been a growing interest in ketamine surrounding its use as an antidepressant. This is largely due to the fact that this drug works through a mechanism not offered by any of the conventional antidepressant medications.
As more research uncovers how ketamine works, it’s likely we’ll see this drug become more common for people with treatment-resistant depression.
What’s even more likely, is that new (hopefully safer) drugs will be developed that share similar mechanisms of action but that can offer more long-lasting benefits.
The recreational use of ketamine is likely to continue to thrive in the shadows. There have not been any moves to make recreational ketamine use more accessible.
Unlock Your Mind: Subscribe for Expert Insights on Psychedelics 🍄🌵
- Domino, E. F., & Warner, D. S. (2010). Taming the ketamine tiger. The Journal of the American Society of Anesthesiologists, 113(3), 678-684.
- Visser, E., & Schug, S. A. (2006). The role of ketamine in pain management. Biomedicine & Pharmacotherapy, 60(7), 341-348.
- Persson, J. (2013). Ketamine in pain management. CNS neuroscience & therapeutics, 19(6), 396-402.
- Abelson, K. S., Goldkuhl, R. R., Nylund, A., & Höglund, A. U. (2006). The effect of ketamine on intraspinal acetylcholine release: involvement of spinal nicotinic receptors. European journal of pharmacology, 534(1-3), 122-128.
- Hocking, G., & Cousins, M. J. (2003). Ketamine in chronic pain management: an evidence-based review. Anesthesia & Analgesia, 97(6), 1730-1739.
- Lally, N., Nugent, A. C., Luckenbaugh, D. A., Ameli, R., Roiser, J. P., & Zarate, C. A. (2014). Anti-anhedonic effect of ketamine and it’s neural correlates in treatment-resistant bipolar depression. Translational psychiatry, 4(10), e469-e469.
- Li, L., & Vlisides, P. E. (2016). Ketamine: 50 years of modulating the mind. Frontiers in human neuroscience, 10, 612.
- Moda-Sava, R. N., Murdock, M. H., Parekh, P. K., Fetcho, R. N., Huang, B. S., Huynh, T. N., … & Lopez, K. (2019). Sustained rescue of prefrontal circuit dysfunction by antidepressant-induced spine formation. Science, 364(6436).
- Duncan Jr, W. C., Slonena, E., Hejazi, N. S., Brutsche, N., Kevin, C. Y., Park, L., … & Zarate Jr, C. A. (2017). Motor-activity markers of circadian timekeeping are related to ketamine’s rapid antidepressant properties. Biological psychiatry, 82(5), 361-369.
- Matveychuk, D., Thomas, R. K., Swainson, J., Khullar, A., MacKay, M. A., Baker, G. B., & Dursun, S. M. (2020). Ketamine as an antidepressant: an overview of its mechanisms of action and potential predictive biomarkers. Therapeutic Advances in Psychopharmacology, 10, 2045125320916657.
- Abdallah, C. G., Sanacora, G., Duman, R. S., & Krystal, J. H. (2015). Ketamine and rapid-acting antidepressants: a window into a new neurobiology for mood disorder therapeutics. Annual review of medicine, 66, 509-523.
- Zorumski, C. F., Izumi, Y., & Mennerick, S. (2016). Ketamine: NMDA receptors and beyond. Journal of Neuroscience, 36(44), 11158-11164.
- Hansen, G., Jensen, S. B., Chandresh, L., & Hilden, T. (1988). The psychotropic effect of ketamine. Journal of Psychoactive Drugs, 20(4), 419-425.
- Ben-Shlomo, I., Katz, Y., Rosenbaum, A., & Hadash, O. (2001). Intravenous midazolam significantly enhances the lethal effect of thiopental but not that of ketamine in mice. Pharmacological research, 44(6), 509-512.
- Laskowski, K., Stirling, A., Mckay, W. P., & Lim, H. J. (2011). A systematic review of intravenous ketamine for postoperative analgesia. Canadian Journal of Anesthesia, 58(10), 911.
- Jonkman, K., van de Donk, T., & Dahan, A. (2017). Ketamine for cancer pain: what is the evidence?. Current Opinion in Supportive and Palliative Care, 11(2), 88-92.
- Jonkman, K., Dahan, A., van de Donk, T., Aarts, L., Niesters, M., & van Velzen, M. (2017). Ketamine for pain. F1000Research, 6.
- Lee, E. N., & Lee, J. H. (2016). The effects of low-dose ketamine on acute pain in an emergency setting: a systematic review and meta-analysis. PloS one, 11(10), e0165461.
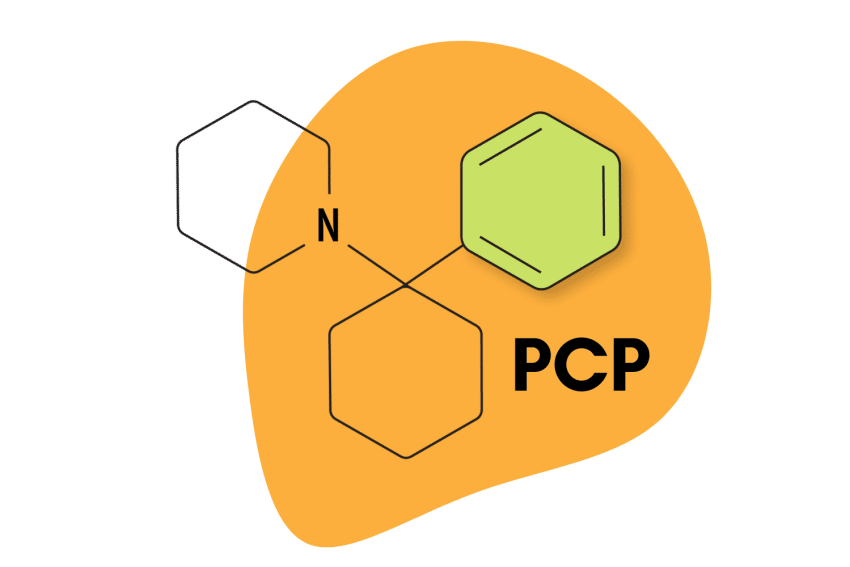
PCP (Phencyclidine) & Analogs
N2O: Nitrous Oxide
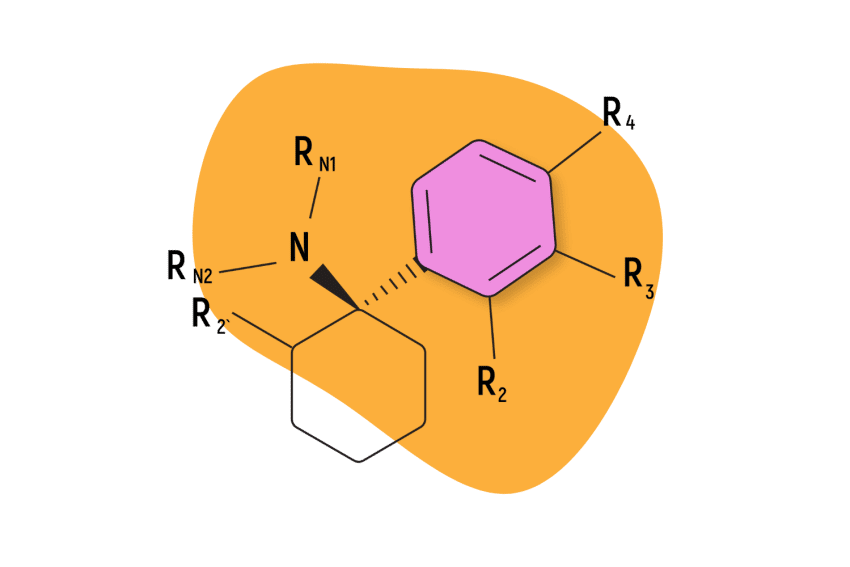
Arylcyclohexylamines

Ibogaine: A Powerful Anti-Addictive Psychedelic
DXM (Dextromethorphan): Effects, Dosage, & Safety
List of All Common Dissociative Drugs & Their Effects
[Xe] | Tripping On Xenon
Subscribe for more psychedelics 🍄🌵.
This will close in 20 seconds
- Search Please fill out this field.
- Newsletters
- Sweepstakes
- Health and Wellness
What a Ketamine "Trip" for Depression Is 'Really' Like
Treating depression with the former party drug is a major development in psychiatric medicine, and now you can even do it from the comfort of your home.
Chelsea Greenwood is an award-winning writer and editor with a focus on lifestyle content at renowned local, regional, and national outlets — both in print and online. She has more than 15 years of experience in journalism, backed by her journalism degree from the University of Florida. She is currently a developmental editor for The Spruce and MyDomaine as well as a news editor at Static Media's The List. In additional to InStyle, she has also written for Teen Vogue, Self, Vice, Vulture, Business Insider, Apartment Therapy and more.
:max_bytes(150000):strip_icc():format(webp)/Chelsea-Greenwood-2000-874cd3999d2f45acbbdb064e34243a8a.jpeg)
Leaving the house before the pandemic was hard enough, thanks to my social anxiety and depression. But once lockdown started? Forget about it. Being in quarantine exacerbated my symptoms until, one day, I realized that I could hardly get out of bed. From eating and working to binge-watching and texting, I did it all in my bed.
I was on antidepressants, and my depression was worse than ever.
While I'd heard good things about ketamine therapy, I figured it was too pricey, and the idea of going to an actual brick-and-mortar clinic was beyond me in my depressed state. But Google was onto me: I was served an ad for Mindbloom, an at-home ketamine treatment company.
When I looked it up, the cost was considerably less than I had expected (even though the company doesn't take insurance), and I read that dedicated "guides" would be there via video chat to help me along the way and process my experiences. So, after some more research, I signed up. What did I have to lose?
As it turned out, a lot. Over the past 12 weeks and 12 treatments, I've lost that heaviness that kept me stuck in bed like gravity. I lost that ever-present sense of impending doom. Plus, I found a little bit of clarity and a lot of hope. Things aren't perfect — I still have good days and bad — but I feel like I'm at the beginning of a season of change, full of possibilities.
I'm not alone. More and more depression sufferers who haven't found adequate relief via conventional methods are turning to ketamine therapy, and treatment clinics are popping up across the country. To explain what exactly the drug does to your brain and its potential for treating mental illness, I turned to two experts in the field for their input.
What is ketamine, exactly?
Although it was first discovered in 1956 and used as an anesthetic for animals, ketamine was cleared by the FDA in the 1970s as a human anesthetic. Since then, it's been used extensively to sedate patients for surgery, including soldiers injured in the line of duty during the Vietnam War.
In addition to sedation, the trance-like state ketamine produces comprises pain relief; amnesia; and a sense of dissociation, like you're outside of your body. Taking a high dose of ketamine may lead to a psychedelic experience known as a k-hole, involving severe dissociation, intense visual hallucinations, and feelings of unreality.
How does ketamine help treat depression?
So, when and why did researchers first begin testing ketamine as a treatment for depression? Well, at the start of the 21st century, ketamine was found to have potent and rapid antidepressant properties at sub-anesthetic doses, explains Ryan Yermus, M.D., co-founder and chief clinical officer of Field Trip Health , which provides ketamine therapy for depression. "While the most commonly used medicines, selective serotonin reuptake inhibitors (SSRIs), generally require weeks of continual dosing to achieve a response (and even then approximately one-third of patients will not respond after two or more courses of treatments), ketamine provides a safe, more rapid-acting treatment for depressive conditions," he says.
Although more research needs to be done on what exactly ketamine does to the brain, Gerard Sanacora, M.D., Ph.D., a Yale Medicine psychiatrist and a professor at the Yale School of Medicine, says that evidence suggests the drug alters the brain's adaptive capabilities — almost like rewiring it. The brain's ability to change both structure and function throughout one's life is called neuroplasticity.
"The synapses, the connections between cells in the brain, appear to be changing more rapidly shortly after treatment with ketamine," Dr. Sanacora says. "We believe this can influence a person's ability to change thought and behavior patterns that are associated with depression."
That's why ketamine treatment doesn't just hinge on the drug itself. It typically involves therapy and integration work, too: putting the mental and emotional revelations you experience during treatments to practical use in your daily life (e.g., starting a new meditation practice, creating a daily exercise ritual, etc.) during a time when your brain is in this state of change.
How significant of a development is ketamine as a treatment for depression?
"The discovery and development of ketamine for the treatment of depression has dramatically altered the way we think about depression treatment," says Dr. Sanacora.
On top of providing hope for those with treatment-resistant depression, the use of a drug not previously intended for psychiatric treatment has had a profound effect in the field of mental illness treatment. "This has led to a whole new wave of exploration in attempts to develop new and improved treatments for depression and other related neuropsychiatric disorders," Dr. Sanacora says.
So, is it legal?
Yes, but the law is not so cut and dry. Currently, ketamine is approved for clinical use as an anesthetic, explains Dr. Yermus. When a drug is prescribed for uses other than its original intended function, it's being used off-label.
"Using medicine off-label is very common in practice as doctors learn that safe medicines can be effective for other purposes, and the use of ketamine in mental health is just one of many examples," he says. So, if a doctor prescribes you ketamine for the treatment of depression or anxiety off-label, it is legal and safe.
However, in 2019, the FDA approved one form of ketamine, a nasal spray called esketamine (brand name Spravato), to treat depression — a promising step forward in this field of medicine.
But ketamine is still a controlled substance, so it's illegal to possess without a prescription.
What are the different ways you can take ketamine?
For therapeutic purposes, ketamine can be taken via intramuscular (IM) injection, intravenous (IV) infusion, orally (as a tablet), or nasally (as a spray). More research is needed to determine which method is the most effective. Generally, only the tablet, like the kind I take, is self-administered (i.e., taken at home), and the rest are administered by professionals in a clinical setting.
What does a ketamine treatment session feel like?
While everyone's ketamine treatment session will differ, many describe the experience as a euphoric, dreamlike state in which the world around them seems to fade away, everyday cares dissipate, unusual thoughts emerge, and vivid memories come to the surface. Some mild visual hallucinations are possible.
The psychedelic experience is intended to be gentle, not scary. Depending on the dosage, the length of the treatment will vary, but most sessions take anywhere from 40 minutes to two hours.
Here's what my first ketamine "trip" looked like:
Per the instructions, I didn't eat for four hours before my treatment. There's potential for nausea when taking ketamine, so Mindbloom provided me with anti-nausea medication, which I took one hour before I began my treatment.
When it was time to begin, I tucked the ketamine tablet inside my lip to let it dissolve. I swished it around with my saliva to help it absorb into my bloodstream, and then I spit the rest out. I turned on a zen Mindbloom playlist, put on an eye mask, and laid down in bed to let the trip begin.
Mindbloom encourages you to set an intention before each treatment — something that's not quite a goal but perhaps a question you want answered or a topic you want to explore. Mine was finding joy. As the session began, I felt a strong need to connect to something deeper and more powerful than myself, something spiritual (I consider myself an atheist). Then I saw an image of myself as a child. My first instinct was to fold her in my arms and protect her from everything to come in life. It made me weep.
Behind my closed eyes, I saw some mild visuals of swirling shapes and colors. I never felt scared or overwhelmed at any point — simply like I was floating down a river and observing thoughts, feelings, and memories as they passed by. I felt euphoric and slightly detached from my body, which felt somewhat tingly and numb, but I was still aware of the room around me.
Overall, you're supposed to dedicate one hour to your treatment. I found that the ketamine kicked in about 10 to 15 minutes after taking it, and then I would have about 40 minutes or so of the "trip" experience. Directly afterward, Mindbloom encourages patients to journal what they saw, felt, and experienced so they can later process it.
I felt a little groggy after my first session, but generally didn't feel any other side effects from taking the ketamine. My guide told me that this is a very "clean" way of taking the drug in that it produces very few side effects, if any.
How long does it take to work?
Like with most psychiatric medicines, your mileage may vary. While some see improvement in their depression symptoms immediately after the first treatment, it doesn't usually last, Dr. Sanacora says. Research indicates that ketamine therapy has a cumulative effect.
"Most people require a series of treatments in order to improve the chances of sustaining the response," he says. "Many of those people then also require some ongoing maintenance treatments every couple of weeks or monthly to keep the depression at bay." He notes that there are active research studies trying to find ways to extend this response, but there are no clear methods of achieving it at this time.
Dr. Yermus agrees that the timing depends on the person. "The severity of the condition is generally a guide for how many sessions people need — so someone with debilitating, acute depression will likely need more sessions than others with more moderate symptoms," he said. "Clients with mild anxiety and depression who feel stuck and disconnected can sometimes have a profound 'aha' moment after one or two sessions."
Personally, I had some significant revelations during the first couple sessions (e.g., I decided to move closer to family after years of hemming and hawing over it), but I didn't feel relief from my depression symptoms right away. That happened about six weeks in: I started to feel that lighter feeling, and doing everyday tasks wasn't so hard.
Early on in the treatment, my guide, Shannan, an Aussie based in Tulum, Mexico (shoutout to Shannan — she's the best!), helped me process what I experienced during my treatments during online video chats called integration sessions.
One time, I went into a session with the intention/question: Why am I so depressed? I wound up seeing memories of family and didn't think they were relevant to my intention, but she helped me talk it out and make the connections that I had missed — kind of like a therapist does.
Once you get through the first round of treatment (six sessions) at Mindbloom, then it's a little more DIY and there are fewer integration sessions, unless you want to buy them. The idea is that you get the hang of it in your first six sessions and can purchase additional support if needed.
Who is a good candidate for ketamine treatment?
Dr. Yermus says that anyone dealing with depression or anxiety who is in good physical health and has an open mind is a candidate for treatment.
However, the government is a bit more exacting when it comes to prescribing the esketamine nasal spray. The FDA has only provided approval for the treatment of treatment-resistant major depression (meaning depressive episodes associated with major depressive disorder that have not responded to standard forms of oral antidepressants) and major depressive episodes associated with serious suicidal ideation and/or behavior, says Dr. Sanacora.
What does ketamine therapy cost, on average?
Unless you're taking esketamine, which is FDA approved and thus eligible for insurance coverage, you'll be paying about $450 for one IV infusion, on average, per WebMD . At Field Trip Health, one IM injection costs $750, and Mindbloom charges $89 a week for three months ($1,060) for new patients, which includes six ketamine treatments. Returning clients pay $59 per week for three months.
Note that all these companies offer support services before and after treatment, the cost of which is typically included in the aforementioned prices.
What are the risks of taking ketamine?
Dr. Sanacora points out that the long-term effects of taking ketamine for depression remain unknown. During research involving animals, ketamine was shown to cause some toxic effects on the brain as well as behavioral and cardiovascular side effects, he said . While some human studies have also shown evidence of behavioral and brain abnormalities linked to ketamine use, this has generally been in people who use the drug recreationally, he notes.
Also, ketamine — known by its street names Special K, Vitamin K, Kit-Kat, and Super K — has been used recreationally for decades, particularly in the 1980s. So there's a possibility for addiction if dosing isn't professionally monitored. As its Schedule III label indicates, ketamine has "a moderate to low potential for physical and psychological dependence," per the DEA .
Personally, I don't feel that I developed any kind of dependence on the ketamine, but I do feel drawn to the healing nature of the ketamine experience. My Mindbloom guide said that, after doing an initial round of, say, three months of treatments, many clients do a refresher course once a year afterward to keep reaping the benefits of therapy.
That's likely what I intend to do, and I can only hope that — for myself and others — ketamine treatment becomes more widely accessible and affordable in the future.
Related Articles

Reviewed by Psychology Today Staff
Ketamine is a medication originally developed as a human and veterinary anesthetic. Unlike other anesthetics, it does not depress breathing or blood pressure, though unpleasant side effects, including hallucinations and confusion, may occur. Due to its low cost, it remains widely used in medical procedures around the world. It is also found on the street, known as Special K, and is listed as a Schedule III drug, with moderate to low potential for physical and psychological dependence.
- Can it be used for depression?
- Can it be used for anxiety?
- Can ketamine be used for alcoholism?
- Can ketamine be used for PTSD?
- How is it used?
- What’s the difference between ketamine and esketamine?
- Is esketamine covered by insurance?
- What are the side effects of esketamine?
- Is ketamine sometimes known as Special K?
- How can I tell if my child is using ketamine?
- What are some slang terms for street ketamine?
- Where do I find help?
The drug has also gained popularity in recent years as a fast-acting antidepressant medication . Unlike other antidepressants , which can take weeks or months to work, patients who take ketamine often see improvements within just a few hours. Ketamine also appears to sharply decrease thoughts of suicide . But the effects are short-lived, and the long-term outcomes of regular ketamine treatment are unknown. And research from Yale University found that ketamine improved symptoms significantly in teens who suffer treatment-resistant depression
A small study that appeared in the Journal of Psychopharmacology found that subjects who suffered anxiety responded positively to weekly doses of ketamine over a three-month period. The patients improved in their function in both social and professional areas of life. Ketamine may also be effective for people with PTSD and or obsessive-compulsive disorder.
Studies have looked into ketamine’s effect on depressed people who have a family history of alcoholism. In research that appeared in the American Journal of Psychiatry , people with problem drinking were administered ketamine along with motivational enhancement therapy , compared with a control group, the ketamine plus therapy group drank less and did not relapse as much.
A study that appeared in the American Journal of Psychiatry found that repeated doses of ketamine can help reduce the symptoms of people who suffer from PTSD . Over a two-week period, patients received six infusions of ketamine. Further research must be done to assess ketamine’s efficacy over longer periods of time.
When used for depression or chronic pain , ketamine is often applied intravenously in specialized clinics. A round of ketamine infusions typically comprises several sessions spread over a few weeks and may cost several thousand dollars. Patients typically pay out-of-pocket; some patients may struggle to afford or even access the drug. This drug can also be administered through nasal spray or taken orally .
Ketamine itself is not FDA-approved to treat depression, but a derivative of ketamine, esketamine , is. The drug is delivered by nasal spray and is designed to be administered alongside a traditional antidepressant. It was approved specifically for treatment-resistant depression, or depression that has failed to respond to other antidepressant medications.
Because the drug is FDA-approved, it can be covered by insurance. But the drug must be administered under a doctor’s supervision, leading some experts to worry that patients could have problems accessing it, as they do with intravenous ketamine.
Side effects of esketamine can include dissociation, dizziness, anxiety, nausea, numbness, sedation, a spinning sensation or vertigo, lethargy, and hallucinations. It can also cause bladder damage and has been linked to ulcerative cystitis; the chemical is toxic to the lining of the bladder.
While ketamine is used for more than sedation, the medication has gained a reputation as a cheap and addictive street drug, known as ”Special K,” which triggers hallucinations and feelings of dissociation. Though fatal overdoses are rare, tolerance can build up quickly. Repeated exposure to high doses of ketamine has been shown to have severe psychological and physical consequences.
Special K is easy for kids to access on the street in powder, liquid, or pill or capsule forms. They may get it from their friends or over the DarkNet. Relatively cheap, Special K is found in urban areas as well as rural. There is no smell or visible signs when a person takes it ; it can be ingested, injected, or smoked. This drug is similar to any other, your child may seem withdrawn and zoned out with a zombie-like expression. This drug gives the user a hallucinogenic effect, or sometimes a feeling of near-death, one referred to as K-Hole or K-Holing.
According to a Drug Enforcement Administration report, street ketamine is also known as Barry Farrell, Blind Squid, Cat Food, Cat Valium, Donkey; Green, Honey Oil, Jet, Keller, Kelly’s Day, Ket, Kit Kat, Kitty Flip, Purple, Special La Coke, Super Acid, Super C, Vitamin K, Wobble, Wonk, or simply the letter K.
If you or someone you know is abusing drugs, contact National Helpline at 800-662-HELP (4357) or the National Alliance on Mental Illness (NAMI) HelpLine 800-950-NAMI (6264).

Researchers are discovering that "magic mushrooms" may provide rapid relief and possibly a cure of severe depression.

Through increasing empathy, trust, and bonding, psychedelic medicines are poised to help lubricate all kinds of bumpy relationships, from the romantic to the political.

Ketamine is fighting the good fight against treatment-resistant depression.
Once viewed only as a general anesthetic or a drug of abuse, ketamine is now being explored as a treatment for a wide range of psychiatric disorders.

What to expect from your first treatment: side effects, planning for treatment, and understanding the risks.

Depression is associated with changes in the default mode network of connectivity between brain regions. What does this mean for clients and clinicians?

A therapist breaks down what psychedelics can do that talk therapy cannot.

When is it right to try ketamine? Is it safe? What should patients expect from treatment?

There's a lot of hype about ketamine for depression. How much of it is real?
Ketamine's use as a psychiatric drug has sharply increased in recent years, particularly for depression and posttraumatic stress disorder.
- Find Counselling
- Find a Support Group
- Find Online Therapy
- United Kingdom
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

At any moment, someone’s aggravating behavior or our own bad luck can set us off on an emotional spiral that threatens to derail our entire day. Here’s how we can face our triggers with less reactivity so that we can get on with our lives.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience

Experience yourself in a new way through transformative psychedelic therapies.
Treatment with field trip health.
Field Trip provides immersive Ketamine-Assisted Psychotherapy to treat a variety of mental health conditions including depression, anxiety, and PTSD.
- Our treatment is structured based on your unique needs to help you achieve holistic outcomes.
- Ketamine, when administered in a medically supervised setting, is legal, safe, and fast-acting. This medicine can create meaningful change within hours after your first psychedelic exploration session.
- We pair your ketamine experience with therapy to help you uncover insights into the root causes of your pain. Our therapists help you integrate the realizations from your psychedelic experience into your daily life, ideally preventing relapse.
- Field Trip Health's growing network of health centers across the US and Canada are carefully and beautifully designed for your comfort and safety.
Treatment Outcomes
Our post-program evaluations show rapid, meaningful decreases in the depression and anxiety scores of clients with difficult-to-treat mental health conditions, including depression, generalized anxiety disorder, and trauma.

Data from a group of clients at their 1-month follow-up reveals the lasting antidepressant effects of our program, achieved with the combination of ketamine and psychotherapy.
OUR PROCESS
How it works.

You'll meet our team of psychiatrists and therapists. We’ll ensure you are suited for psychedelic-assisted therapy and tailor a custom treatment plan just for you.

Once our staff has developed an evidence-based treatment plan for you, we will guide you through exercises to set intentions for the results you wish to achieve.

Reframe negative thought patterns and begin the process of breaking old habits after a series of psychedelic-assisted therapy sessions held over several weeks.

Follow up with our psychotherapists to create a behavior-change plan that will help you adopt healthier habits for a lasting change in your mood and wellbeing.

Continue your journey to healing at home. We’ll provide you tools, strategies, and online access to our team so you stay on track to experiencing a complete mental transformation.

- Your personal journey will begin with a virtual Preparation session with a therapist to discuss your goals and preparation for your treatment.
- Your Exploration will take place in one of our Health Centers, where our therapeutic team is there to support you throughout your ketamine treatment.
- Following your Exploration, you will have an Integration therapy session to help process your experience.
- Your personal journey will begin with a virtual Preparation session with your therapist to discuss your goals and preparation for your treatment.
- Your Exploration is scheduled in a Health Center where you will be accompanied by your therapist through-out your ketamine treatment.
- Following your exploration, you will have an Integration therapy session with your therapist to help process your experience.
Our evidence-based 1 treatment protocol is designed to help you reach your desired outcomes. Our medical team will likely recommend 6 Ketamine Exploration + Integration sessions over the course of 6 weeks (on average) as part of a personalized plan that’s designed just for you. We pair multiple sessions together as research and clinic results have proven 2 that this extends the effectiveness of treatment, leading to longer-lasting relief.
Individual + Extra Support
Support plus, medical consultation (60 min) therapy intake session (50 min) preparation session (30 min) virtual, additional preparation time and follow up therapy sessions, ketamine exploration, integration sessions .
*Prices shown are based on 0% APR and a 24 month repayment plan. Interest rate and repayment plan will be based on your credit score. Clients are subject to an eligibility check. A down payment may be required. Estimated payment amount excludes taxes. In the US, financing is managed through our partner, Walnut. See hellowalnut.com for details.
Getting Started
Every life-changing journey starts with one small step. We will help you understand if our Ketamine-Assisted Psychotherapy program is a good fit for you. The first step in our process is to fill out our online assessment. From there you’ll schedule time with one of our psychiatric consultants to discuss your medical history and goals for treatment.
What Our Clients Say


Field Trip Health Expands Access to Ketamine-Assisted Psychotherapy
- Share on Facebook
- Share on Twitter
- Share on WhatsApp
- Share on Pinterest
- Share on LinkedIn

The company is building a clinical network of therapists trained in ketamine-assisted psychotherapy across the United States.
A new clinical network being created across North American will make it easier for patients to access ketamine-assisted psychotherapy (KAP). Field Trip Health ’s new KAP Co-Op Program will make its therapeutic centers available for qualified professionals to directly facilitate ketamine therapy for their clients with the support of the company’s trained and experienced clinical medical staff.
Based in Toronto, Canada, Field Trip Health ’s mission is to support the creation of a next-generation, sustainable psychedelic medicine industry and to build safe and comfortable spaces to facilitate psychedelic-assisted exploration, transformation, and healing. Currently, the company operates clinics in Toronto, New York, Los Angeles, Chicago, Atlanta, and Houston. Further clinics are slated to open soon in San Diego, San Carlos/San Jose, Seattle, and Washington, DC.
Field Trip Health says it is on track to have 20 clinics open or under construction by December 2021. Each site features at least four treatment rooms, two consultation rooms, and an integration space with pillows, music, art supplies, and more for clients who wish to use this space to relax and reset before leaving the clinic.
The KAP Co-Op Program is open to independently licensed or registered psychotherapists who have already completed training at an approved psychedelic-assisted psychotherapy program provider.
Therapists are required to have a minimum of two years of clinical experience post-licensure in individual and group therapy, with a focus on addressing common and complex mental health issues such as depression, anxiety, and trauma. They are also required to have working knowledge and demonstrated training in evidence-based therapies such as cognitive behavioral therapy, acceptance and commitment therapy, and emotion-focused psychotherapy.
Once a therapist has applied and been approved for the program, they will be granted privileges to Field Trip Health’s KAP-related services at one of the company’s centers. A session is two hours long and it costs $400.
Field Trip Health’s clinical team will support therapists to provide KAP in several ways. They will screen all potential clients to ensure that KAP is safe and appropriate for them and will administer the ketamine to approved clients, typically through intramuscular injection and, in some cases, via a sublingual lozenge. Throughout the session, the clinical team will also assist in monitoring the client in a manner that does not intrude on the therapeutic environment being provided by the therapist.
In addition to expanding its network of psychedelic-assisted therapy sites, Field Trip Health is developing its digital tools ‘Trip’ and ‘Portal’ to provide global access to consciousness expansion therapy and resources. The company also plans to begin Phase 1 human trials evaluating the use of its patent-pending, novel psychedelic molecule FT-104 as a treatment for a variety of central nervous system disorders in Q1 of 2022.
Leave a Reply
Your email address will not be published. Required fields are marked *
Related News

What Are K-Holes? The Ketamine Experience Explained

Psychedelic Business Spotlight – May 13

Psychedelic Business Spotlight — January 14
Psychedelic Spotlight is your reliable source for the latest stories in the emerging psychedelics industry, covering breakthrough discoveries, investor news and cultural reform.
- Advertise With Us
- Privacy Policy
- Terms and Conditions
- Conferences
Get a roundup of Psychedelic news stories in your inbox
By signing up to the Psychedelic Spotlight newsletter you agree to receive electronic communications from Psychedelic Spotlight that may sometimes include advertisements or sponsored content.
Current time by city
For example, New York
Current time by country
For example, Japan
Time difference
For example, London
For example, Dubai
Coordinates
For example, Hong Kong
For example, Delhi
For example, Sydney
Geographic coordinates of Elektrostal, Moscow Oblast, Russia
City coordinates
Coordinates of Elektrostal in decimal degrees
Coordinates of elektrostal in degrees and decimal minutes, utm coordinates of elektrostal, geographic coordinate systems.
WGS 84 coordinate reference system is the latest revision of the World Geodetic System, which is used in mapping and navigation, including GPS satellite navigation system (the Global Positioning System).
Geographic coordinates (latitude and longitude) define a position on the Earth’s surface. Coordinates are angular units. The canonical form of latitude and longitude representation uses degrees (°), minutes (′), and seconds (″). GPS systems widely use coordinates in degrees and decimal minutes, or in decimal degrees.
Latitude varies from −90° to 90°. The latitude of the Equator is 0°; the latitude of the South Pole is −90°; the latitude of the North Pole is 90°. Positive latitude values correspond to the geographic locations north of the Equator (abbrev. N). Negative latitude values correspond to the geographic locations south of the Equator (abbrev. S).
Longitude is counted from the prime meridian ( IERS Reference Meridian for WGS 84) and varies from −180° to 180°. Positive longitude values correspond to the geographic locations east of the prime meridian (abbrev. E). Negative longitude values correspond to the geographic locations west of the prime meridian (abbrev. W).
UTM or Universal Transverse Mercator coordinate system divides the Earth’s surface into 60 longitudinal zones. The coordinates of a location within each zone are defined as a planar coordinate pair related to the intersection of the equator and the zone’s central meridian, and measured in meters.
Elevation above sea level is a measure of a geographic location’s height. We are using the global digital elevation model GTOPO30 .
Elektrostal , Moscow Oblast, Russia
View prices for your travel dates
- Excellent 18
- Very Good 9
- All languages ( 43 )
- Russian ( 37 )
- English ( 4 )
- German ( 1 )
- Italian ( 1 )

" DIR: West; bigger nice evening sun but louder due to main street DIR:East; Quiter, very bright in the morning if sun rises "
Own or manage this property? Claim your listing for free to respond to reviews, update your profile and much more.
APELSIN HOTEL

IMAGES
VIDEO
COMMENTS
Ketamine trips are uncannily like near-death experiences. Christian Jarrett. is the editor of Psyche. A cognitive neuroscientist by training, his books include The Rough Guide to Psychology (2011), Great Myths of the Brain (2014) and Be Who You Want: Unlocking the Science of Personality Change (2021). Edited by Pam Weintraub.
The Ketamine Experience Explained. The words people use to describe falling into a K-hole—the psychedelic trip experienced on high doses of ketamine—read like opposites. Paralyzing. Introspective. Detached. Peaceful. Frightening. Euphoric. Transformative.
The infusions are accompanied by psychedelic "trips.". That's just part of ketamine. In the beginning, I believed that the trip didn't matter — the drug got in me regardless of if the trip was "good" or "bad.". A lot of my trips are "bad.". I believe this is largely because of complex post-traumatic stress disorder ( C-PTSD ).
The Stages of a K 'trip' from an experienced user. hi all, just wanted to share my experiences with Ketamine for the newbies as before I started taking it I wanted to read something like this but could never find a detailed report on the stages of a ketamine 'trip'. 1 - Starting off with probably one decent sized bump will start making me feel ...
Mindbloom's method of sublingual administration—using a rapid dissolve tablet placed under the tongue— has a more gentle onset than IV or IM-injections, which are commonly used at ketamine clinics. The experience is gentle, bringing you slowly into and out of the experience, and returning to normal consciousness around 60 minutes later.
Technically speaking, ketamine is a dissociative anesthetic, meaning that it numbs your body and makes you feel apart from your environment — like you're watching your own life happen instead of living it. But that doesn't begin to capture the weirdness of what it feels like to get high on K. As one friend put it to me: "It's like ...
Step 6: Have An Integration Plan. Good or bad, to maximize the therapeutic effect of the infusion, there needs to be integration of the experience. This is especially true if the experience was challenging and your patient doesn't know what to make of it.
Ketamine is a water-soluble PCP derivative. As a chiral molecule, it has two enantiomers: an S (+) isomer, or "esketamine," and an R (-) isomer, or "arketamine.". [4] In clinical use, it is available as ketamine hydrochloride in liquid or powder form for intravenous injection and is marketed under the brand name Ketalar.
A trip typically lasts from 20-60 minutes, with a low dose packing a robust psychedelic punch. In other words, a little goes a long way. How does ketamine interact with the brain?
Objective: Subanesthetic ketamine doses have been shown to have rapid yet transient antidepressant effects in patients with treatment-resistant depression, which may be prolonged by repeated administration. The purpose of this study was to evaluate the antidepressant effects of a single ketamine infusion, a series of repeated ketamine infusions, and prolongation of response with maintenance ...
Ketamine (also known as Ket, K, Special K, vitamin K,[5] Kitty, and others) is a classical dissociative substance of the arylcyclohexylamine class. It is perhaps the best-known and archetypal member of the dissociatives, a diverse group which includes PCP, methoxetamine, DXM, and nitrous oxide. The mechanism of action is not fully known, although blocking of the NMDA glutamate receptor is ...
In medicine, ketamine is used as an analgesic. It doesn't directly block pain signals like an opiate — instead, dissociative analgesics disconnect the thalamus from the cortex. When this happens, the body still feels pain, but the brain simply "doesn't care.". We don't actually feel bothered by the pain.
At Field Trip Health, one IM injection costs $750, and Mindbloom charges $89 a week for three months ($1,060) for new patients, which includes six ketamine treatments. Returning clients pay $59 ...
Ketamine is a medication originally developed as a human and veterinary anesthetic. Unlike other anesthetics, it does not depress breathing or blood pressure, though unpleasant side effects ...
Field Trip provides immersive Ketamine-Assisted Psychotherapy to treat a variety of mental health conditions including depression, anxiety, and PTSD. Our treatment is structured based on your unique needs to help you achieve holistic outcomes. Ketamine, when administered in a medically supervised setting, is legal, safe, and fast-acting.
A session is two hours long and it costs $400. Field Trip Health's clinical team will support therapists to provide KAP in several ways. They will screen all potential clients to ensure that KAP is safe and appropriate for them and will administer the ketamine to approved clients, typically through intramuscular injection and, in some cases ...
Ketamina, MDMA (Ecstasy) Dawkowanie: w kolejności chronologicznej czyste MDMA (ok.150g) jako bomba, półtorej godz. później 2 ścieżki ketaminy (ok. 300-350g), 1.5 godz. później druga bomba MDMA. Set&Setting: klub the Egg, Londyn, sobotnia noc; nastawienie czysto imprezowe, relaks ze znajomymi po pracowitym tygodniu.
Ketamina jest dostępna jedynie dla lekarzy i nie jest powszechnie sprzedawaną używką (na rynku brytyjskim jest dość powszechna i dostępna u dilerów, skategoryzowana jest w grupie C nielegalnych substancji, w związku z czym za jej posiadanie grożą względnie niewielkie kary - przyp. hyperreal). W Polsce ketamina jest na wykazie do ...
Ketamina - "wśród substancji psychoaktywnych klasyfikowana jako dysocjant psychodeliczny, lek używany w medycynie i weterynarii do znieczulania przedoperacyjnego. Farmakologiczne działanie ketaminy podobnie do dekstrometorfanu i fencyklidyny, lecz o wiele krótsze i pozbawione części ich efektów ubocznych" (pl wiki). W Polsce narkotyk stosunkowo mało znany. W Wielkiej Brytanii, gdzie ...
3.5. Service. 3.7. Value. 3.6. The sanatorium "Valuevo" is a historical health resort located in a unique location of the New Moscow on the territory of 30 hectares of the ancient noble estate of Count Musin-Pushkin with a perfectly preserved architectural ensemble and a landscape park, in an ecologically clean environment of wildlife.
In 1938, it was granted town status. [citation needed]Administrative and municipal status. Within the framework of administrative divisions, it is incorporated as Elektrostal City Under Oblast Jurisdiction—an administrative unit with the status equal to that of the districts. As a municipal division, Elektrostal City Under Oblast Jurisdiction is incorporated as Elektrostal Urban Okrug.
Geographic coordinates of Elektrostal, Moscow Oblast, Russia in WGS 84 coordinate system which is a standard in cartography, geodesy, and navigation, including Global Positioning System (GPS). Latitude of Elektrostal, longitude of Elektrostal, elevation above sea level of Elektrostal.
Apelsin Hotel, Elektrostal: See 43 traveler reviews, 19 candid photos, and great deals for Apelsin Hotel, ranked #1 of 4 hotels in Elektrostal and rated 4 of 5 at Tripadvisor.