Starting at $5, these customer-loved Amazon products will help kickstart summer
- Share this —

- Watch Full Episodes
- Read With Jenna
- Inspirational
- Relationships
- TODAY Table
- Newsletters
- Start TODAY
- Shop TODAY Awards
- Citi Concert Series
- Listen All Day
Follow today
More Brands
- On The Show
- TODAY Plaza

Patients now have access to doctor's visit notes: A guide to what's inside
What does your doctor really think about your condition and health concerns? For more than a year now, patients have been able to access and read the observations doctors write down about them during a visit.
The clinical notes can come with surprises. Patients may be amused to find out they’re described by their physician as “well-nourished,” “well-groomed,” “pleasant” or “normal-looking.”
“’He is not ill-appearing or toxic-appearing.’ That’s the best review I’ve ever received,” one man wrote on Twitter after reading his doctor’s notes.
But patients may also be taken aback by comments referring to them as “obese” or mentioning their marijuana use. One woman was shocked when she saw her doctor wrote down that she “seemed overly dramatic,” she complained on Reddit .
As of April 2021, healthcare providers must give patients access to all of the health information in their electronic medical records as part of the 21st Century Cures Act . That includes your doctor’s written comments about your physical condition during a visit, along with any symptoms and what the treatment should be.
The rules don’t apply to psychotherapy notes made during counseling sessions or when doctors believe a patient would harm another person or themselves after reading the information, according to OpenNotes , a non-profit organization based at Beth Israel Deaconess Medical Center in Boston that advocates for greater transparency in healthcare.
Doctors have been both supportive and cautious of the movement. In a 2020 survey of 1,628 clinicians, 74% agreed note sharing was a good idea.
“It does give the patient a lot more ownership of their medical condition because they can see what we’re thinking about, they understand our thought processes a little bit more, and they can see what the options are,” Dr. Sterling Ransone, Jr., a family physician in Deltaville, Virginia, and chair of the American Academy of Family Physicians, told TODAY.
But knowing that patients can now read his notes, Ransone finds he self-censors himself to avoid sounding critical or judgmental of a patient.
“It’s difficult because sometimes you have to leave a note to yourself what your concerns are, but they can cause anxiety with the patient,” he noted. “I can say that it really has changed the way that a lot of physicians write their notes.”
That means more accessible language, less jargon and more caution with certain terms that might offend or upset a patient.
Ransone no longer uses the abbreviation “SOB,” which stands for “short of breath” and instead writes out the full term in his notes. Same with “FU,” which stands for “follow up.”
The American Academy of Family Physicians has also urged doctors to write “patient could not recall” instead of describing them as a “poor historian;” “patient declines” instead of “patient refuses;” and “patient is not doing X” instead of describing them as “non-compliant.”
A guide to your doctor’s note:
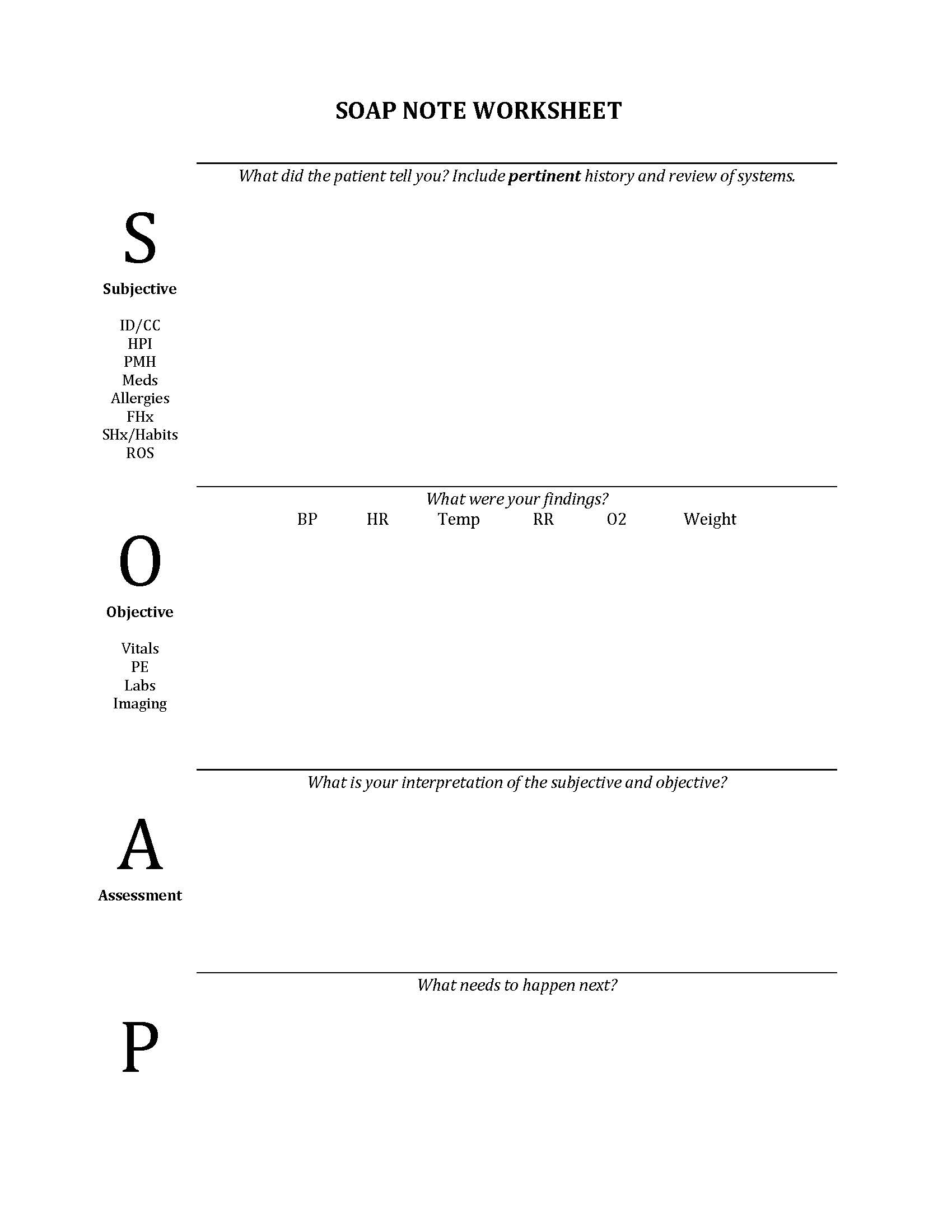
The medical note has traditionally included four parts, Ransone said: The subjective findings, or what a patient said they were concerned about; the objective findings, or what the doctor actually observed during the visit; the physician’s assessment after evaluating the patient and the treatment plan.
Doctors are used to jotting down any observations that can offer clues to what’s going on. So writing down that a patient “seemed overly dramatic” can mean the person’s complaint wasn’t consistent with the degree of their symptoms and something else might be the reason for their visit that day, he noted.
Here are other descriptions patients may find in their doctor’s notes:
Well-groomed or pleasant: This can indicate mental status. “If someone comes in and they’re somewhat disheveled, it leads you to wonder why and what do I need to look into?” Ransone said. “Pleasant” means the patient was communicative and responded to social cues, he noted. Patients who are upset or sleepy could have a substance abuse disorder or another reason why they’re having trouble interacting.
Well-developed or well-nourished: “A lot of times when people look at open notes and they’ll say, ‘Well, of course I am. What does this mean?’” Ransone said. “It just means that we checked in our mental checklist… (that) those aren’t things that we need to worry about.” If a person isn’t well-nourished, it might mean they don’t have access to food or their teeth might be in such bad condition that they can’t chew and get nutrition.
Unremarkable: This is a good thing. “Unremarkable is exactly what you want to be when you see a physician,” Ransone said. “I joke with my patients all the time: You want to be the most boring patient that I’ve seen today, because that means we haven’t seen anything that is abnormal that we need to chase down.”
Obese : To a physician, the term means the patient is of a certain weight for their height and frame, which comes with a certain constellation of medical concerns, Ransone said. “There’s a stigma to obesity in society and a lot of patients really don’t want to have that on their charts… but it’s a very important piece of the puzzle for me as I’m trying to help a patient get healthier,” he noted.
Substance use: This isn’t necessarily bad. Doctors will note a patient has an occasional glass of wine, for example, to give them an idea of the person’s alcohol consumption habits. “The way that our society looks at, say, marijuana use has changed a lot over the years, but a lot of people don’t want that included in the medical record,” Ransone said. “I’d like to know if someone is smoking weed because it could affect the medications that I should give them for their health condition.”
Other health observations patients frequently don’t want on their chart include mental health issues such as depression, anxiety or bipolar disorder, he noted.
Some patients have called Ransone to ask that he change something in their note because they see it as a pejorative or they disagree with his assessment, but that doesn’t mean he’s wrong, the doctor noted.
One guide for physicians suggested telling the patient: “I’m sorry you disagree with my assessment. While I can’t change my medical opinion, if you’d like I can add that you disagree with it.”
Patients pointing out factual errors — such as noticing the note referenced a problem in the right knee rather than the left — is a completely different issue. If there's anything inaccurate in your chart, bring it to your doctor's attention.
In fact, patients who read their doctor’s notes may play an important role in finding errors in their records, a 2020 study published in JAMA found.
Ransone encouraged patients who are reading their doctor’s notes to keep the lines of communication with their physician open.
“Don’t necessarily assume the worst when they read things. Realize that a lot of the things that they read are open to interpretation,” he advised.
A. Pawlowski is a TODAY health reporter focusing on health news and features. Previously, she was a writer, producer and editor at CNN.

This 1 trick can help you feel happier in 20 seconds, happiness expert says
Mind & body.

Woman, 39, driven crazy when mystery whooshing noise suddenly starts in her ear
Women's health.

‘American Idol’ singer Mandisa died of class III obesity, autopsy reveals

I was eating myself to death before losing 200 pounds without weight-loss drugs
Diet & fitness.

Train yourself to fall asleep in 2 minutes with this viral sleep hack

What is a ‘hyperfixation meal’ and why does it happen? Mental health specialists explain

Do you struggle to cry? Here’s what that says about your health

Psychotherapist and mom of 4 recalls her biggest source of 'mom guilt'

EXCLUSIVE: John Green recalls how OCD struggles as a teen inspired ‘Turtles All the Way Down’

Selena Gomez's lupus and other health issues: Singer opens up in new TODAY interview
Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
What to Consider When Reading Your Medical Notes
- 1 Associate Editor, JAMA
Shared medical visit notes are notes written by clinicians that are made available (“open”) to patients in electronic health records.
Clinicians add medical notes to a patient’s electronic health record following clinical encounters such as office visits. There is no difference between the notes that patients can view and those that clinicians keep on file.
In 2021, new legislation was introduced in the US that required almost all medical notes to be shared with patients. These notes include
History and physical notes
Progress notes
Consultation notes
Procedure notes
Discharge summary notes
Imaging narratives
Laboratory report narratives
Pathology report narratives
There are a few exceptions. Some medical notes that do not need to be shared with patients include psychotherapy notes that are separated from the rest of the medical record, written by any health care professional; information related to a civil, criminal, or administrative action or proceeding; and any note that a doctor perceives may cause harm or danger to a patient.
The goal of note sharing is to increase transparency between clinicians and patients. Some studies have shown that shared medical notes may help patients feel more engaged in their health care, better understand their medical conditions and care plans, and take their medications properly.
Approach to Reading Medical Notes
Patients are typically able to access their notes through a patient portal to their electronic health record. The notes are there for a patient’s consideration and are optional, not required, reading. The main purpose of medical notes is to communicate information among health care professionals, not between doctors and patients. A patient can avoid reading their medical notes if they find that the information causes them too much worry.
When patients do choose to read their medical notes, it is important to approach them in the right way—not as a clinician, but as a patient. You can discuss with your doctors whether or not you plan to read your notes, which may help them put more patient-directed information (such as follow-up instructions) directly in the notes. If you identify anything in your note that concerns you, discuss that information with someone on your health care team.
For More Information
Office of the National Coordinator for Health Information Technology www.healthit.gov/curesrule/
OpenNotes www.opennotes.org/
To find this and other JAMA Patient Pages, go to the For Patients collection at jamanetworkpatientpages.com .
Conflict of Interest Disclosures: None reported.
Source: Delbanco T, Wachenheim D. Open Notes: new federal rules promoting open and transparent communication. Jt Comm J Qual Patient Saf. 2021;47(4):207-209. doi: 10.1016/j.jcjq.2021.02.004
See More About
Jin J. What to Consider When Reading Your Medical Notes. JAMA. 2021;326(17):1756. doi:10.1001/jama.2021.16493
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Patient Access To Medical Records Is Set To Become Mandatory
Westend61 / Getty Images
Key Takeaways
- Starting in April 2021, the United States' government will require health organizations to share medical records with patients electronically, free of charge.
- Once the mandate goes into effect, patients will be able to see doctors' notes and other information in their electronic medical record.
It’s soon going to be easier to read your doctor's notes from your last visit thanks to a measure to improve patient record transparency. Starting in April 2021, all medical practices will be required to provide patients free access to their medical records. The concept of sharing medical notes is known as OpenNotes.
Under the 21st Century Cures Act , consumers will be able to read notes that recap a visit to the doctor’s office as well as look at test results electronically.
In the past, accessing your doctor's notes could require long wait times and fees. The Health Insurance Portability and Accountability Act (HIPAA) made it legal to review medical records, but it didn't guarantee electronic access.
More than 250 healthcare organizations in the U.S. (including multiple locations within a single system) are already sharing notes with patients digitally.
What Is OpenNotes?
With OpenNotes , doctors share their notes with patients through electronic health records (EHR). Practices and hospitals use various kinds of software for EHRs, such as MyChart. Once the mandated medical transparency measure goes into effect, patients will be able to log in and see their notes.
The mandate was supposed to begin on November 2, 2020, but in the midst of the COVID-19 pandemic, the deadline was extended to April 5, 2021.
Doctor’s notes will include consultations, imaging and lab findings, a patient's medical history, physical exam findings, and documentation from procedures.
Cait DesRoches , executive director of OpenNotes (a group advocating patient note access), explains that patients will have two ways to get their notes. Either the organization will put the notes on the portal automatically or a patient can request that notes be added to the portal.
“The notes are full of great information for patients,” DesRoches tells Verywell. Viewing the notes can help patients recall what they discussed with their doctors during a visit as well as remind them of what they’re supposed to do after an appointment.
“My hope is that organizations will implement this in a really robust way,” DesRoches says. “That’s when the health system will get to the place where they’re seeing the benefits.
What This Means For You
Being able to see notes in an electronic portal also provides patients with the opportunity to ensure that their medical records are accurate. Before the mandate goes into effect in April 2021, talk to your doctor about how you will be able to access your medical record.
Downsides of Data Sharing
The ability to view documentation from medical care sounds like a great opportunity for patients, but some worry that it could create confusion. For physicians, there's also the potential for an increased workload, as they might need to respond to questions that arise when patients see—and question—what's in their notes.
UC San Diego Health launched a pilot program using OpenNotes for primary care patients in 2018. Marlene Millen, MD , a professor and doctor in the UC San Diego Health , told MedicalXpress that she did not see an increase in inquiries from patients when their notes were available.
What To Know About Doctors’ Notes
There are some cases when a doctor does not have to share medical notes with patients. These scenarios are different state by state, as privacy laws vary.
Doctors can withhold medical records if they think releasing the information will lead to physical harm, such as in the case of partner violence or child abuse.
Providers also do not have to share information regarding certain diagnoses that are considered protected, and psychotherapy documentation is not shared. However, other mental health services outside of talk therapy—such as talking to your primary care doctor about depression—are included in the notes.
Depending on the state you live in, DesRoches explains that parents can also view notes of their teen’s doctor visits. Parents might not have access when teens turn a certain age, based on the state. However, the rules don’t supersede state laws on privacy for adolescents.
Evaluating OpenNotes
OpenNotes.org reports that reading doctors' notes benefit patients in many ways and may lead to better health outcomes. According to OpenNotes, patients who are able to review their doctors' notes:
- Are more prepared for visits with their providers
- Can recall their care plans and adhere to treatment, including medication regimens
- Feel more in control of their care
- Have better relationships with their physicians
- Have a better understanding of their health and medical conditions
- Take better care of themselves
Several studies have assessed OpenNotes. A study published in the journal BMJ Open in September 2020 found that medical transparency is a right that is viewed favorably among people in different countries including Canada, Australia, Japan, Chile, Sweden, and the U.S.
Another study published in the Journal of General Internal Medicine in July 2020 found that patients typically understand their doctor's notes and that the information in their record is accurate. However, there were several notable disparities, and participants in the study had suggestions for improving the quality of access.
The researchers found that if patients didn’t understand a note or found inaccurate information in their notes, they had less confidence in their doctors.
According to a report in NEJM Catalyst, the ability to exchange information—including requesting information from patients before a visit—has been instrumental during the COVID-19 pandemic. In addition to sharing notes with patients after a visit, doctors were able to send a pre-visit questionnaire to patients that enabled them to gather more detail before the visit.
“We suspect, for example, that patients and care partners may recall even less of telemedicine encounters than they do after face-to-face office visits," the authors noted. "As a result, they may turn more often to reading their OpenNotes online."
The researchers concluded that once there are patient- and clinician-friendly mechanisms in place for record-sharing, "inviting patients to contribute directly to their records will both support patient engagement and help clinician workflow.”
Advantages and Disadvantages
Wayne Brackin, CEO of Kidz Medical Services , tells Verywell that it is “fair and reasonable” to expect patients would have access to doctors' notes. However, Brackin is concerned that doctors could “moderate their description in a manner that might affect care,” if they know that the patient or family will have access to records.
Wayne Brackin
To have a layperson, with a more limited vocabulary, or who has English as a second language, read the notes in isolation could lead to misunderstandings.
“This could be particularly sensitive with behavioral health issues," Brackin says, adding that a medical interpreter of sorts could help avoid misunderstandings during the initial record review. The language, abbreviations, and terminology in physician notes can be difficult for trained medical colleagues to interpret, let alone patients.
“To have a layperson, with a more limited vocabulary, or who has English as a second language, read the notes in isolation could lead to misunderstandings,” Brackin says.
Suzanne Leveille, RN, PhD , a professor of nursing at the University of Massachusetts and a member of the OpenNotes.org team tells Verywell that patients are generally enthusiastic about having online access to their office visit notes, but many providers initially expressed concerns that giving patients access to their notes could cause more worry than benefits.
"Our large surveys across health systems have not shown this to be the case. Very few patients report they became worried or confused from reading their notes," says Leveille, who also authored one of the OpenNotes' studies. "Overwhelmingly, patients report they benefit from note reading, for example, that it’s important for taking care of their health, feeling in control of their care, and remembering their plan of care."
While concerns about misunderstandings are not unwarranted, most patients report they are able to understand their notes, and that they have benefitted from viewing them. In cases where patients have been able to spot—and correct—mistakes, they feel not just more empowered, but safer.
"Open notes can improve patient safety," Leveille says. "About 20% of patients pick up errors in the notes and some report the errors to their providers."
Medical Xpress. More US patients to have easy, free access to doctor's notes .
Salmi L, Brudnicki S, Isono M, Riggare S, Rodriquez C, Schaper LK, et al. Six countries, six individuals: resourceful patients navigating medical records in Australia, Canada, Chile, Japan, Sweden and the USA . 2020. BMJ Open. doi:10.1136/bmjopen-2020-037016
Leveille SG, Fitzgerald P, Harcourt K, Dong Z, Bell S, O’Neill S, et al. Patients evaluate visit notes written by their clinicians: a mixed methods investigation . 2020. J Gen Intern Med. doi:10.1007/s11606-020-06014-7
Kriegel, G, Bell S, Delbanco T, Walker J. Covid-19 as innovation accelerator: cogenerating telemedicine visit notes with patients . May 12, 2020. NEJM Catalyst. doi:10.1056/CAT.20.0154
By Kristen Fischer Kristen Fischer is a journalist who has covered health news for more than a decade. Her work has appeared in outlets like Healthline, Prevention, and HealthDay.
Visit Note Documentation Guide- Best practices for co-signing visit notes
This is a best practice guide on how non-physician practitioners and practitioners can co-sign visit note documentation. apr 29, 2022 • knowledge, who needs to co-sign visit notes, npp flags specific visit notes, the supervising physician selects visit notes, creating the visit note template for attestation, completing the encounter, using templating software to facilitate co-signing.
If your practice employs non-physician practitioners (NPPs), a supervising physician is responsible for reviewing the work, records, and practice of the NPP to ensure that appropriate treatment is rendered and appropriate directions are given and understood as applicable to the law. Supervising physicians are required to note that they reviewed an NPP's work or include their name/signature in the clinical documentation for proper legal documentation purposes. Each state has different co-signature requirements that need to be followed. Elation currently allows one provider-level user to sign each visit note which then captures one signature in a 'structured' manner in the visit note. The physician/practitioner that signs the visit note is typically the provider you are billing the encounter under. Then, to capture a co-signature, there are subsequent workflows that can be completed depending on how you plan to bill:
- The NPP performs the visit, and the visit is billed under the NPP's NPI number. There must be documentation that the supervising physician reviewed a certain percentage of encounters.
- The NPP performs the visit, and the visit is billed under the supervising physician's NPI number. There must be documentation of which NPP saw the patient and who rendered the encounter.
Direct Billing
For Direct Billing, the NPP is billing under their own NPI number. Different states require a different percentage of a NPP's encounter documentation to be reviewed by their supervising physician for clinical appropriateness. The co-sign workflow in Elation can be divided into two main steps:
- Identifying the visit notes that a supervising physician needs to review
- Documenting that a review was completed
Identifying visit notes for review
- The NPP can flag specific visit notes for the supervising physician
- The supervising physician can randomly select visit notes themselves
- The NPP locates a signed visit note in the patient's chart
- The NPP clicks "Actions" >> "Send: Office Message" at the top of the visit note
- The NPP enters the supervising physician's name in the "To" field and enters a short message in the "Body" (ex. 'Please review' or 'Please review & sign')
- The NPP clicks "Send"
- The supervising physician then checks their "Office Messages" inbox daily for messages from the NPP
- The supervising physician clicks on the patient's name to open the chart to view the visit note and review the documentation
- The supervising physician then replies to the office message to close the loop (ex. 'Review complete' or 'Approved') and clicks "Send and Sign Off".
- There is now documentation in the patient's chart that states the supervising physician reviewed a specific visit note signed by the NPP.
- Note : This workflow requires the NPP to enter billing information for each visit note prior to the NPP signing off on the visit note.
- Click on the "Billing" button at the top of the Practice Home
- Click "Reports" >> "Billing Report" at the top of any page in Elation
- the "Signed Visit Notes Not Yet Billed" section for customers who do not have a Practice Management System (PMS) integration with Elation
- the "Visit Notes with Bills Pending Sync to PMS" section for customers who have a Practice Management System (PMS) integration with Elation
- User Tip : If the supervising physician needs additional clarification from the NPP about any contents of the encounter, they can send an Office Message to the NPP for additional clarification before signing off on the visit note draft.
- Click "Actions" >> "Send: Office Message" at the top of the visit note they reviewed
- Enter the NPP's name or their own name (depending on preference) in the "To:" field
- Enter a short message in the "Body" (ex. 'Review complete' or 'Approved')
- Click "Send"
- Locate the message in the Requiring Action section of the patient's chart & click "Sign" at the top of the message
- Click "Notes" >> "Non-Visit Note" at the top of the patient's chart after reviewing the NPP's visit note
- Enter a short message in the body of the Non-Visit Note (ex. 'I reviewed the visit note for Date of Service 04/01/2022' or 'I reviewed the visit note for Date of Service 04/01/2022 and sign off on the work.')
- Click "Sign Note"
Incident-To Billing
Incident-To Billing means the non-physician practitioner (NPP) sees the patient and documents the encounter and is billing under their supervising physician's NPI number. The documentation must capture the NPP's name in order to meet a requirement about documenting who saw the patient and who rendered the encounter.
We recommend the NPP uses a Visit Note Template to capture their name and statement in regards to seeing the patient and rendering the encounter. For example, the statement can be 'Visit was rendered and documented by Jane Doe, NP and completed under supervising physician James Hibbert, MD'.
- Click the "Visit Note Templates" button at the top of any visit note draft
- Click "Templates" >> "Visit Note Templates" at the top of any patient's chart
- Click the "+New Template" button at the top of the Visit Note Templates management window
- Enter a name for the template in the "Template Name" field (ex. 'Visit Attestation')
- Select a section for storing your attestation. We recommend the Procedure section because it usually stores actions taken during the encounter.
- Enter your attestation language in the Procedure section of the Visit Note Template. (ex. 'Visit Attestation: Visit was rendered and documented by Jane Doe, NP and completed under supervising physician James Hibbert, MD'.)
- Click "Save Template"
- The NPP completes documentation of the encounter in the visit note draft
- The NPP clicks the "Visit Note Templates" button at the top of any visit note draft
- The NPP clicks the "Export to Note" button next to the visit attestation template to export the visit attestation template into the visit note draft
- The NPP changes the provider at the top of the visit note draft to the supervising physician's name
- The NPP clicks "Save as Draft & Close" to drop the visit note draft in the supervising physicians's "Draft Notes" inbox
- The supervising physician then checks their Practice Home "Draft Notes" inbox daily for visit notes to review
- The supervising physician clicks on the patient's name to open the chart and clicks on the 'In Progress...' visit note
- that the NPP rendered a visit
- that the NPP is requesting their supervising physician to review a visit note they signed
- that the supervising physician reviewed the encounter and is co-signing a visit note
Related Articles
- Office Message Feature Guide
- Practice Home Guide- Checking for requiring action items
- Templates Guide- Using templating softwares with Elation
Do You Have Access to Your Doctors’ Notes About You?
Here’s why you should request access to what your physician writes in your charts.

Do You Have Access to Your Doctors’ Notes About You?
If you’re like most patients in the U.S., you haven’t a clue what your doctor writes about you in your health record .
Despite a move toward more transparency in medicine, only about 3 percent of the U.S. population currently has ready access to notes written in their charts. And most physicians polled are still resistant to the idea. “Two-thirds of doctors still do not feel comfortable in giving access to the notes of their visit to the patients,” says Dr. Eric Topol , a cardiologist and professor of genomics at The Scripps Research Institute, a nonprofit medical research organization based in La Jolla, California.
HIPAA, or the Health Insurance Portability and Accountability Act of 1996, gives patients the legal right to review their medical record. This includes doctor's notes, though not notes kept separate from the medical record, as mental health observations sometimes are. But only a fraction of patients have access to their doctors' notes online, like through medical organizations' patient portals, which increasingly offer patients a way to access their lab test results or other information about their care online.
However, a not-for-profit national initiative called OpenNotes has sought to make it easier for patients to gain access to notes – and for doctors to share them. As a result, today, about 80 health care institutions, from Beth Israel Deaconess Medical Center in Boston – a site where the concept was first tested – to Cleveland Clinic and the Veteran’s Health Administration allow patients access to their clinicians' notes about them online. In total, approximately 12.7 million patients now have access to OpenNotes, says Catherine DesRoches, executive director of OpenNotes, which is funded by philanthropic grants.
[See: 12 Questions to Ask Before Discharge .]
DesRoches and OpenNotes co-founder Dr. Tom Delbanco have set a goal of ensuring 50 million patients have access to their clinicians’ notes through the initiative by 2020.
There’s no reason for doctors to write notes about patients without a patient being privy to what's written, since patients can benefit by seeing what their physicians write and being fully informed , says Delbanco, a professor of medicine at Harvard Medical School.
Managing the Power Dynamic Between Doctors and Patients
Lisa Esposito May 13, 2014

Based on early research done when the concept was still being tested – surveying patients a year after they’d begun using OpenNotes – most patients reported they felt more in control of their care, were more educated and better prepared for future visits. “They certainly remembered what happened in the visit better,” Delbanco says. That’s of no small consequence, since it’s well-documented that patients tend to forget or misremember the majority of information doctors share in person during medical visits. Experts say giving patients full access to their medical records and doctors’ notes can improve both patient engagement and follow through, as well. And 70 percent of surveyed patients who’d been using OpenNotes and who were on medicine said they were actually doing better at taking their medications as prescribed, Delbanco says.
Meanwhile, doctors’ concerns about sharing their notes – ranging from whether patients questioning notes would increase physician workload to whether reading doctors' notes would contribute to patient anxiety – have been systematically, carefully studied and found not to be at issue. Yet most physicians are still reluctant to share notes, Topol says. “Doctors still feel it’s their property – that they created the notes, and that the patients aren’t entitled to the notes – and this is an outgrowth of paternalism – medical paternalism” – as well as the unfounded fears related to sharing the notes, he says.
The lack of transparency misses another important opportunity, he adds, by keeping patients from being able to set their medical records straight. “Office notes are riddled with mistakes that could be easily cleaned up by patients. They know what medicines they’re taking, largely, and they know what conditions [they have],” he says. Research has found that often information in medical records and physicians notes is incorrect. “Notes are fraught with errors when they’ve been audited,” Topol says. “So why not have the patients involved? It’s their care, it’s their body. They paid for the visit one way or another. But yet they have no work product.”
[See: HIPAA: Protecting Your Health Information .]
Mary Ellen Sexton of Jefferson Township, Pennsylvania, says she hasn’t had to suggest any changes or corrections to her notes, but along with her husband, Lynn, she appreciates being able to see doctors’ notes through OpenNotes. The Sextons go to primary care provider Dr. Richard Martin, a family physician at the community clinic Geisinger Mt. Pleasant in Scranton, Pennsylvania, which is part of Geisinger Health System, an early adopter of OpenNotes.
Lynn, 84, who had a heart attack decades ago, says being able to access details through his medical record and OpenNotes post-visit improves the overall understanding he and his wife have of what’s going on with his care. “If we go to the cardiologist, everything is on there. The [tests] that he’s had, echocardiograms or stress tests – everything’s one there,” adds 81-year-old Mary Ellen; that includes an explanation of what the test was for and the cardiologist’s notes. “Even if Dr. Martin isn’t in and we have to go to somebody else, because Lynn has an emergency, all those notes are on there, too – exactly what they did or what they ordered or new medication,” she says. “It’s fantastic.”
The notes can help with recall following medical visits, particularly for older patients who have multiple chronic conditions that require much to be covered in a short office visit, Martin says “If somebody’s diabetic and their blood sugars aren’t well-controlled, I’ll get specific about things they need to avoid in their diet,” Martin says. “They may not remember everything I tell them. So they can go back to my note, and refresh their memory.”
For patients who don’t have ready access to their doctors’ notes online, experts say it’s still worth putting in a request for those notes. “ Ask your doctor for a copy. Doctors have been giving patients copies of notes for many years on a one-by-one basis,” Delbanco says. “Encourage your doctor to give it to you, and tell him or her if he doesn’t, you’ll go somewhere else for care.”
Gaining full access to your health record may require going through a health organization’s patient records department, which can take time. Patients may even be charged administrative or copying fees. But it's worth putting in the effort, even if patients shouldn't have to do that, experts say. Request electronic transmission if possible. “There are certainly practices throughout the country where patients are very comfortable and they routinely get their notes from the doctor, whether it be by email or hard copy, for their files,” Topol says. “There’s just very few – that’s the problem,” he says. “Every patient should have their notes as far as I’m concerned."
[See: 5 Common Preventable Medical Errors .]
Delbanco agrees. Though the vast majority of patients still don’t see their doctors’ notes, he’s encouraged that the growth of OpenNotes means an increasing number of patients are able to read what their doctors write about them. “There’s no question in my mind that it will become the standard of care over time,” he says. “It’s only a matter of when – not if.”
What Your Doctors Wish You Knew

Tags: patient advice , patients , medical records , medical quality , health care , doctors
Most Popular

Patient Advice

health disclaimer »
Disclaimer and a note about your health ».

Your Health
A guide to nutrition and wellness from the health team at U.S. News & World Report.
You May Also Like
Do blue light glasses work.
Paul Wynn June 7, 2024

Protein During Pregnancy: How Much?
Kelly LeBlanc June 6, 2024

How to Make Friends as an Adult
Karin Vandraiss June 5, 2024

Apple Cider Vinegar Benefits
Janet Helm June 4, 2024

Why Are Younger People Getting Cancer?
Paul Wynn May 31, 2024

12 Best Superfoods for Older Adults
Christine Comizio and Elaine K. Howley May 30, 2024

Healthy Barbecue Ideas and Recipes
Lon Ben-Asher May 23, 2024

Plant-Based and Vegan Protein Powder
Annika Urban May 22, 2024

What to Eat – and Avoid – on Semaglutide
Lisa R. Young May 22, 2024

Factors Contributing to Weight Loss
Vanessa Caceres May 21, 2024

New and Noteworthy
The physician visit note.
December 2018
Bobby Green, MD
This post was originally published on LinkedIn .
The physician visit note is many things to many people.
To the patient, they contain their personal health story.
To the clinicians who create them, they are the result of hours of work, day after day, year after year.
To the clinic, they become legal documents that must be preserved for years.
They are filled with fancy words, often with a little Latin thrown in.
They are long. Painfully long. Agonizingly difficult to read. Repetitious.
They are also, far too often, useless.
I live on both sides of the aisle. I am tortured having to sort through the abominably long and relatively devoid of important information monoliths created by my physician colleagues. But, to be fair, I create them too.
It was Dr. Lawrence Weed , exactly half a century ago, who set the revolutionary framework for the problem-oriented medical record (POMR), as a way to record and monitor patient information. To be fair, these written notes had their fair share of problems. Before computers, physician notes on paper were often illegible and held hostage — trapped in the physical confines of the paper chart. A distracted colleague could throw the day into chaos by accidentally putting a chart in the wrong bin on the ward. Spilled coffee could effectively and permanently delete important information. But at least they sometimes said something useful.
We assumed that technology would eventually make things better, and in some ways it has — my visit notes don't have weird stains from unidentifiable beverage spills. I rarely interact with hole punchers anymore (unless I want to throw one at a computer). I can sit in one chair and access all of my patients' records, instead of endlessly walking around searching for the right chart.
But go talk to a doctor. Any doctor. Ask them what they think of the physician visit note in this modern era of artificial intelligence, machine learning, self-driving cars. You will not get one positive response, not one.
I am an oncologist. I take care of cancer patients. That's what I do. And I think I'm reasonably good at it. And one of the main reasons I'm good at it is because that's my core area of focus. I stay away from other things. I don't take care of patients with arthritis. I don't read and interpret pathology slides. I don't perform surgery. As healthcare becomes more complex, it's increasingly important that clinicians specialize in the problem for which they are trained. For oncologists, that's cancer. I rely on my expert colleagues for help in areas beyond my expertise.
But here's the challenge. Unlike clinicians, the physician visit note tries to do too many things at once. It's always been a problem, but as the number of documentation requirements has drastically increased over the last decade, the visit note has become a dumping ground — a jack of all trades, but a master of none.
Specifically, today's visit note attempts to solve three wholly different problems:
Document the amount of work a clinician does to justify what they bill. Physicians do things like serve up a long list of negatives in our review of symptoms because it's required — this alone fills up half a page. We do the same thing for our physical exam when we write absurd things like "no splenomegaly" for the twentieth time in a year. You can argue whether this information is relevant and if pertinent negatives are helpful. But the format in which it's captured often obscures what is most critical. Two pages of a negative review of systems shouldn't hide that the patient was having 8/10 pain.
Serve as the clinician's source of truth and our main reference point. I need to know certain things about my patients in order to take good care of them. This includes which chemotherapy treatments they've previously had if they have a targetable EGFR mutation. I need to know that I ordered a CT scan to review next week. I should remember that they have a spouse sick at home that they care for which impacts their ability to come in for regular treatment. But EHRs don't create a framework to easily retrieve this information, instead functioning only as digital filing cabinets.
Communicate with other clinicians who also care for the patient. My colleagues don't need a full patient history summary or all of my negative physical exam findings every time I send them a note. When Mrs. Jackson receives a blood transfusion for her MDS, it's the blood transfusion that's important. They need to be able to see the important things without getting lost in details. The time clinicians spend digging through notes from referring doctors to find that one nugget of useful information is an epic waste.
Our notes do many things, and none of them well. But it doesn't have to be this way.
Imagine a world where the visit note serves as a framework for how we input and share information, where it isn't actually a physical note, but a framework for how we input and disseminate information.
Imagine the long list of negatives that have to be documented for a ROS or PE, or the data point that gets entered for the 10th time that the lifetime non-smoker hasn't started smoking again; imagine that these things never clutter up what my referring doctor has to see when she reads my note.
Imagine that I can enter staging and genomic information and then that information becomes easily retrievable and relevant.
Imagine that the abnormal physical exam findings are what I see highlighted, but not the normal negatives.
Imagine I'm prompted to make sure that "port in left chest wall" on my exam doesn't stay in my note years after the port is removed.
Imagine that I can spend 50 percent less time on my computer, and 50 percent more time with patients.
I do believe that there is a world in which the visit note actually gets better. We need to advocate for a reduction in documentation requirements, and kudos to CMS for finalizing a policy that starts to do this. And technology must play a role. Surely in a world where rockets can land themselves, we can build a better visit note. As someone who works at a health tech company, I am inspired by what engineers, designers, product managers and many of my other talented colleagues can do. As we strive to solve problems that matter, this, without question, matters. All of us who build EHRs for physicians have an obligation to make things better. An obligation to, as Dr. Weed wrote , create an environment where "...the art of medicine will gain freedom at the level of interpretation and be released from the constraints that disorder and confusion always impose." Stay tuned.
- Point of care
- Flatiron stories
More to explore
- Value-based care
- Customer interviews

- Clinical decision support


Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
Outpatient SOAP Notes
In the outpatient clinic, SOAP is the traditional note structure: S ubjective, O bjective, A ssessment, P lan. Although electronic health records may structure notes differently, this is still the information that you would enter at a problem focused or chronic disease management visit.
You may see some providers move the Assessment and Plan to the top of the note in this this order-APSO. Due to the amount of information automatically included in many electronic notes some providers chose to bring attention the the assessment and plan first.
This section begins with ID/CC ( the reason for the scheduled visit) and includes the history of present illness plus any other pertinent history. This pertinent history is often a combination of what may have been elicited from the patient and/or information you’ve confirmed from the medical record.
If you address more than one problem at the visit, the subjective section of the note should be organized by problems, with separate paragraphs for each issue addressed. At times you will be addressing multiple and both acute and chronic medical conditions at the same visit. How to address this in the note will be discussed below.
Use the appropriate medical terms for each problem so that future readers can quickly review its history by glancing at past visit notes. Remember that most patients have access to their medical records electronically and will be reading and reviewing chart notes and telephone encounters. Be mindful about the language you use in your documentation and remain patient-centered .
If there is a separate medication list, discuss with your preceptor if you, a nurse, or the preceptor should update this. If there is not a separate medication list, the patient’s current medications should be documented in the note. Use generic names if possible and indicate strength of medication and how often patient is to take medication. This can be placed at the end of the subjective section. Remember to review allergies in case you need to prescribe any medications during the visit.
The objective section should include:
- vital signs
- your findings on physical exam, organized by system
- results of lab tests or imaging studies performed since the last visit.
For most visits you will perform a focused physical exam based on the problem(s) the patient is presenting with. Performing a complete physical exam in the outpatient setting usually occurs during establish care visits and occasionally during wellness visits (more often the exam is tailored to appropriate preventive health measures. e.g. pelvic exam if cervical cancer screening due, skin exam if at higher risk for skin cancer, etc). Report the presence or absence of findings pertinent to the visit’s concerns, keeping in mind your differential diagnosis. This will almost always include vital signs, general appearance and findings from more than one organ system.
This section includes your interpretation of the information you presented in the subjective and objective sections. For an acute problem, it will be a differential diagnosis, which should include at least 2-3 reasonable possibilities. For a chronic disease visit, it should include your assessment of current control, adherence, and/or complications and any gaps or needs that were identified.
This section includes what you are going to do. When more than one problem has been addressed, many physicians write the assessment and the plan together for each one. The problems in the “assessment/plan” section correspond to those listed in the subjective section. A specific plan for follow up should be included in every note. On every note, indicate the name of your supervising physician (“seen with Dr. Jones”).
Link to SOAP note worksheet.
SOAP worksheet only
The patient has come in for a yearly wellness visit?
Update the past medical history, family, social, sexual, health related behaviors, allergies and medication list. Be familiar with the preventive health and wellness measures that are relevant based on the patient’s age, sex assigned at birth and other medical conditions or risk factors. Review any relevant screening questionnaires that may be part of the wellness visit. Often patients will bring up other acute and chronic medical conditions they would like to discuss during the wellness visit. Use agenda setting early on to identify these concerns and negotiate what can be accomplished during the visit. You may need to plan for a follow up visit to address other concerns.
The visit addresses multiple issues?
Follow the ID/CC with a statement of other issues raised by the patient or addressed by you. “Mr. Jones is a 63 year old man with hypertension and diabetes who presents today with an acutely swollen and painful left big toe. He also requests refills on his diabetes medications and a referral for massage for low back pain.”
Organize the Subjective, Assessment, and Plan sections by problem. The first paragraph under S would address the first problem, the next would address the second problem, and so on. The assessment and plan should address each of these problems individually. In this case, the subjective and assessment sections would address:
- Acute L big toe swelling
- Low back pain
- Hypertension
The visit includes follow-up of a known problem(s)?
ID/CC should include the reason for follow-up “Mr. Jones is a 63 year old man recently diagnosed with gout in the L great toe who returns for follow-up and discussion of prevention.”
The subjective section should include for each problem:
- Interval history: what’s happened since the last visit
- History of an current status of the problem
- Current therapy, adherence and how well it is working
- Any side effects or concerns about therapy
- Any monitoring that’s due
The Foundations of Clinical Medicine Copyright © by Karen McDonough. All Rights Reserved.
- Become a Member
- Everyday Coding Q&A
- Can I get paid
- Coding Guides
- Quick Reference Sheets
- E/M Services
- How Physician Services Are Paid
- Prevention & Screening
- Care Management & Remote Monitoring
- Surgery, Modifiers & Global
- Diagnosis Coding
- New & Newsworthy
- Practice Management
- E/M Rules Archive
June 7, 2024
CMS Update on Medical Record Documentation for E/M Services
The world as we knew it

Summary of changes described in this article
In 2018, CMS changed the requirements for using medical student E/M notes by the attending physician. In the 2019 Physician Fee Schedule Final Rule, CMS stated its desire to reduce the burden of documentation on practitioners for E/M services, in both teaching and non-teaching environments. They stated that a clinician no longer had to re-document the history and exam, but could perform those and “review and verify” information entered by other team members, or entered in prior notes. In 2019, CMS updated the section of the Medicare Claims Processing Manual that addressed E/M services in teaching settings, allowing a nurse, resident or the attending to document the attending’s presence during an E/M service. In 2020, CMS made a radical change to documentation requirements, adopting this as a policy,
“Therefore, we proposed to establish a general principle to allow the physician, the PA, or the APRN who furnishes and bills for their professional services to review and verify, rather than re-document, information included in the medical record by physicians, residents, nurses, students or other members of the medical team.” [1]
- CMS has made significant changes in E/M notes to reduce burden on practitioners in the past years.
- CMS is now allowing clinicians to “review and verify” rather than re-document the history and exam. The details are below.
Want unlimited access to CodingIntel's online library?
Including updates on CPT ® and CMS coding changes for 2024

“Copy-Pasting. Copy-pasting, also known as cloning, enables users to select information from one source and replicate it in another location. When doctors, nurses, or other clinicians copy-paste information but fail to update it or ensure accuracy, inaccurate information may enter the patient’s medical record and inappropriate charges may be billed to patients and third-party health care payers. Furthermore, inappropriate copy-pasting could facilitate attempts to inflate claims and duplicate or create fraudulent claims.” [2]
Read the OIG report
CMS responded that it agreed that additional guidance was needed and that it intended to work with its contractors in the development of effective guidance. To my knowledge, that guidance was never released.
- The OIG expressed concern about copy/paste and over-documentation in 2014, but this did not lead to CMS standards about the practice.
- Commercial payers are largely silent, as well.
2019 Easing the burden of documentation

“We proposed to expand this policy to further simplify the documentation of history and exam for established patients such that, for both of these key components, when relevant information is already contained in the medical record, practitioners would only be required to focus their documentation on what has changed since the last visit or on pertinent items that have not changed, rather than re-documenting a defined list of required elements such as review of a specified number of systems and family/social history. Practitioners would still review prior data, update as necessary, and indicate in the medical record that they had done so. Practitioners would conduct clinically relevant and medically necessary elements of history and physical exam, and conform to the general principles of medical record documentation in the 1995 and 1997 guidelines. However, practitioners would not need to re-record these elements (or parts thereof) if there is evidence that the practitioner reviewed and updated the previous information.” [3]
That long-winded paragraph says that a practitioner would not need to re-record history and exam for established patients that they had reviewed and verified from a prior note.
This was verified by a letter from CMS head Seema Verma . Ms. Verma’s letter went further. It said that effective 1-1-2019, not only could the clinician review and verify history and exam, but for both new and established E/M services, specifically,
“Clarify that for both new and established E/M services, a Chief Complaint or other historical information already entered into the record by ancillary staff or patients themselves may simply be reviewed and verified rather than re-entered” [4]
- In 2019, CMS said that for a new or established patient, the billing clinician could “review and verify” information entered into the record by ancillary staff or patients, rather than re-document.
- CMS included “history and exam” as components that could be reviewed from prior entries and verified, not re-documented.
- Section from 2019 rule and letter from Ms. Verma attached to this article
2020 Expanded “Review and verify”

Perhaps the most shocking change came in the Physician Fee Schedule Final Rule in 2020. CMS noted that stakeholders were questioning whether “students” described in the Medicare claims processing manual referred only to medical students, or if that also referred to nurse practitioner and physician assistant students. Advanced practice registered nurses (APRNs) and physician assistants (PAs) told CMS that they wanted to use the same rules for precepting their students as physicians used when precepting medical students. CMS agreed with them. But, they went farther.
“Therefore, we proposed to establish a general principle to allow the physician, the PA, or the APRN who furnishes and bills for their professional services to review and verify, rather than re-document, information included in the medical record by physicians, residents, nurses, students or other members of the medical team. We explained that this principle would apply across the spectrum of all Medicare-covered services paid under the PFS. We noted that because the proposal is intended to apply broadly, we proposed to amend regulations for teaching physicians, physicians, PAs, and APRNs to add this new flexibility for medical record documentation requirements for professional services furnished by physicians, PAs and APRNs in all settings.” [5]
Read that section in it’s entirety
- In the 2020, CMS established a general principal to allow the physician/NP/PA to review and verify information entered by physicians, residents, nurses, students or other members of the medical team.
- This principle applies broadly for professional services furnished by a physician/NP/PA.
Codes 99202–99215 in 2021, and other E/M services in 2023
In 2021, the AMA changed the documentation requirements for new and established patient visits 99202—99215. Neither history nor exam are required key components in selecting a level of service. This further reduces the burden of documenting a specific level of history and exam. The 2021 CPT book says this regarding history and exam.
“The care team may collect information and the patient or caregiver may supply information directly (eg, by portal or questionnaire) that is reviewed by the reporting physician or other qualified health care professional. The extent of history and physical examination is not an element in selection of office or other outpatient services.” [6]
- In 2021, for visits reported with codes 99202—99215, history and exam will not be used to select the level of E/M services. This framework was extended to other E/M services in 2023.
What about teaching physicians
CMS began changing the teaching position rules in 2018, with the stipulation about student documentation. The citation from the CMS manual that changed is below.
B. E/M Service Documentation Provided By Students
“Any contribution and participation of a student to the performance of a billable service (other than the review of systems and/or past family/social history which are not separately billable, but are taken as part of an E/M service) must be performed in the physical presence of a teaching physician or physical presence of a resident in a service meeting the requirements set forth in this section for teaching physician billing. Students may document services in the medical record. However, the teaching physician must verify in the medical record all student documentation or findings, including history, physical exam and/or medical decision making. The teaching physician must personally perform (or re-perform) the physical exam and medical decision making activities of the E/M service being billed, but may verify any student documentation of them in the medical record, rather than re-documenting this work.” [7]
What this says is the teaching physician must still do the work. But, the teaching physician doesn’t have to re-document the work. It saves re-documentation on the part of the attending, in the same fashion as the attending doesn’t need to re-document all of the resident’s work.
Documentation performed by medical students, advance practice nursing students and physician assistant students:
“Therefore, we propose to establish a general principle to allow the physician, the PA, or the APRN who furnishes and bills for their professional services to review and verify, rather than re-document, information included in the medical record by physicians, residents, nurses, students or other members of the medical team. This principle would apply across the spectrum of all Medicare-covered services paid under the PFS.”
- Now, physician assistant and nurse practitioner students are treated the same way as medical students for documentation purposes.
- Any physician or NPP who bills a service can “review and verify” rather than re-document.
- Includes “information included in the medical record by physicians, residents, nurses, students or other members of the medical team.”

The new rules allow the attending, the resident or the nurse to document the attending’s participation in the care of the patient when performing an E/M service. CMS said they were going to do this in the 2019 Physician Fee Schedule Final Rule, released in November of 2018, but the transmittal wasn’t released until April 26, although there is an effective date of January 1, 2019 and an implementation date of July 1, 2019. The transmittal does not include any of the examples of linking statement that were in the manual for so many years. It is brief—here is the section on E/M.
100.1.1 – Evaluation and Management (E/M) Services (Rev. 4283, Issued: 04- 26-19, Effective: 01-01-19, 07-29-19) A. General Documentation Requirements
Evaluation and Management (E/M) Services – For a given encounter, the selection of the appropriate level of E/M service should be determined according to the code definitions in the American Medical Association’s Current Procedural Terminology (CPT®) book and any applicable documentation guidelines.
For purposes of payment, E/M services billed by teaching physicians require that the medical records must demonstrate:
- That the teaching physician performed the service or was physically present during the key or critical portions of the service when performed by the resident; and
- The participation of the teaching physician in the management of the patient.
The presence of the teaching physician during E/M services may be demonstrated by the notes in the medical records made by physicians, residents, or nurses.
These are significant changes for all practices, including those in academic settings. We hope that our MACs are paying attention to CMS’s intentions and that other payers follow suit.
[1] CMS 2020 Physician Fee Schedule Final Rule
[2] CMS and Its Contractors Have Adopted Few Program Integrity Practices to Address Vulnerabilities in EHRs, January 2014 OEI-01-11-00571.
[3] CMS 2019 Physician Fee Schedule Final Rule, page 572
[4] CMS letter from S. Verma, 2019
[5] 2020 Physician Fee Schedule Final Rule, p. 380
[6] AMA, CPT E/M codes, 2021
[7] Medicare Claims Processing Manual, 100-04, Chapter 12, Section 100
Last revised May 21, 2024 - Betsy Nicoletti Tags: compliance issues
CPT®️️ is a registered trademark of the American Medical Association. Copyright American Medical Association. All rights reserved.
All content on CodingIntel is copyright protected. Any resource shared within the permissions granted here may not be altered in any way, and should retain all copyright information and logos.
- What is CodingIntel
- Terms of Use
- Privacy Policy
Our mission is to provide up-to-date, simplified, citation driven resources that empower our members to gain confidence and authority in their coding role.
In 1988, CodingIntel.com founder Betsy Nicoletti started a Medical Services Organization for a rural hospital, supporting physician practice. She has been a self-employed consultant since 1998. She estimates that in the last 20 years her audience members number over 28,400 at in person events and webinars. She has had 2,500 meetings with clinical providers and reviewed over 43,000 medical notes. She knows what questions need answers and developed this resource to answer those questions.
Copyright © 2024, CodingIntel A division of Medical Practice Consulting, LLC Privacy Policy
Do You Really Want to Read What Your Doctor Writes About You?
You’re now allowed to see everything physicians say about you in their notes. It’s complicated.
You may not be aware of this, but you can read everything that your doctor writes about you. Go to your patient portal online, click around until you land on notes from your past visits, and read away. This is a recent development, and a big one. Previously, you always had the right to request your medical record from your care providers—an often expensive and sometimes fruitless process—but in April 2021, a new federal rule went into effect , mandating that patients have the legal right to freely and electronically access most kinds of notes written about them by their doctors.
If you’ve never heard of “ open notes ,” as this new law is informally called, you’re not the only one. Doctors say that the majority of their patients have no clue. (This certainly has been the case for all of the friends and family I’ve asked.) If you do know about the law, you likely know a lot about it. That’s typically because you’re a doctor—one who now has to navigate a new era of transparency in medicine—or you’re someone who knows a doctor, or you’re a patient who has become intricately familiar with this country’s health system for one reason or another.
When open notes went into effect, the change was lauded by advocates as part of a greater push toward patient autonomy and away from medical gatekeeping. Previously, hospitals could charge up to hundreds of dollars to release records, if they released them at all. Many doctors, meanwhile, have been far from thrilled about open notes. They’ve argued that this rule will introduce more challenges than benefits for both patients and themselves. At worst, some have fretted, the law will damage people’s trust of doctors and make everyone’s lives worse.
A year and a half in, however, open notes don’t seem to have done too much of anything. So far, they have neither revolutionized patient care nor sunk America’s medical establishment. Instead, doctors say, open notes have barely shifted the clinical experience at all. Few individual practitioners have been advertising the change, and few patients are seeking it out on their own. We’ve been left with a partially implemented system and a big unresolved question: How much, really, should you want to read what your doctor is writing about you?
The debate about open notes can be boiled down to a matter of practicality versus idealism. You’d be hard-pressed to find anyone, doctor or otherwise, who argues against transparency for patients in principle . At the same time, few people I spoke with for this article believe that the new rule has been put in place all that smoothly. For care providers, the primary concern has been the trouble that can come with writing notes for a new audience. Notes, generally scribbled in shorthand incomprehensible to the unknowing eye, have traditionally served doctors, and doctors alone. They allowed physicians to stay up to date on their patients and share information with colleagues for input on cases.
Some doctors told me they worry that open notes could result in distress for patients who read something they don’t understand, and that highly technical language could make something sound worse than it is. Oncology, for instance, can involve an onslaught of potentially concerning terminology . (Psychotherapy notes are exempt from the new rule.) Other doctors fear that valuable information can be lost if they go too far in de-jargonizing notes to make them patient-friendly. Or that de-jargonizing notes is simply unfeasible. “Let’s say you came to me with pain and pointed to your mid-clavicular line. I’d just put ‘MCL,’” says Aldo Peixoto, a nephrologist at Yale. “But if I were writing for you to understand, I’d have to say ‘pain on the top-right portion of her abdomen in the line that runs from the middle of her clavicle,’ and so on. Rather than writing four lines of prose, I could’ve used literally three letters.”
If that sounds quibbling, consider the trade-offs. Less time for doctors can translate into less time for patients. Many clinicians already write notes well into the evening. Certainly, the pandemic hasn’t helped . Some doctors told me that if they find themselves in a dilemma of either writing notes in less-efficient, plain language or fielding worried patient calls and messages, exhausted practitioners will face yet another burden. And then there’s the matter of trust. Jack Resneck, the president of the American Medical Association, the nation’s largest professional group of doctors and medical students, told me that doctors can need time and space with patients to get them to open up and be receptive to guidance through difficult situations. If these patients were to see notes too soon, Resneck said, they might “immediately flee and not come back to see you.”
Read: Why health-care workers are quitting in droves
As doctors have spent more time dealing with open notes, many have eased off their strongest objections. Some, including Resneck and the AMA, have warmed up to the new rule as certain exceptions have been granted, such as allowing doctors whose patients have parents or partners with access to their notes to omit certain details from their write-ups for privacy reasons. Other physicians seem to be coming to a somewhat awkward realization: On a practical level, many concerns about how this change affects patients are irrelevant, because most patients don’t yet know they have instant access to their notes in the first place. Every doctor I spoke with for this story told me that their patients were largely unaware. Many doctors and hospitals are not going out of their way to inform people about the new rule, so unless patients are particularly on top of shifting rules within our convoluted health-care system, they’re unlikely to encounter the notes on their own. Kerin Adelson, an oncologist at Yale, admitted she didn’t know how to find notes in her own patient portal. She spent several minutes with me on the phone fumbling through different tabs to locate them.
Fans of open notes are frustrated that there is not a greater push for awareness. Even acknowledging that the new system has its shortcomings, many argue that the only way to make things better is to get people invested in the access they’ve recently been granted. Lydia Dugdale, a primary-care doctor at Columbia University, worries about ensuring equity. “Things like socioeconomic status, education, literacy: All of those issues affect the degree to which any given patient is going to want to read and correct and interrogate his or her health record,” she told me. Tom Delbanco, a Harvard doctor and one of the co-founders of OpenNotes, an initiative that spearheaded the push for access to doctors’ notes in the U.S., believes that the effort required to refrain from using “bad words” in notes is minor, and that it shouldn’t make any significant demands on clinicians’ schedules. Doctors who are now taking more time to write notes because of the change, he told me, “probably ought to because they’ve been writing lousy notes.”
Open notes can be valuable for people with chronic conditions and their caregivers, who need to stay in the know. Liz Salmi, the communications and patient-initiatives director at OpenNotes, told me about pulling her full medical record eight years into dealing with brain cancer, before notes were easily and freely available. The document was 4,839 pages. To get a PDF, she said, she had to pay $15 for each DVD it was uploaded to, and her records spanned multiple discs. But the information was worth it: Having access to the record gave Salmi a way to remember all of the crucial bits of information she’d gotten piecemeal from various doctors.
The fact that many people have no idea open notes exist doesn’t change the deeply personal questions at stake in the debate about whether the notes do more good or harm—questions that everyone must confront in one way or another in dealing with America’s medical system, whether or not they fully realize it. How much information do you truly want about your health, and how much do you trust your doctor to deliver it to you? What is a doctor’s role in informing people about their health?
Read: Following your gut isn’t the right way to go
Open notes are only part of this conversation. The new law also requires that test results be made immediately available to patients, meaning that patients might see their health information before their physician does. Although this is fine for the majority of tests, problems arise when results are harbingers of more complex, or just bad, news. Doctors I spoke with shared that some of their patients have suffered trauma from learning about their melanoma or pancreatic cancer or their child’s leukemia from an electronic message in the middle of the night, with no doctor to call and talk through the seriousness of that result with. This was the case for Tara Daniels, a digital-marketing consultant who lives near Boston. She’s had leukemia three times, and learned about the third via a late-night notification from her patient portal. Daniels appreciates the convenience of open notes, which help her keep track of her interactions with various doctors. But, she told me, when it comes to instant results, “I still hold a lot of resentment over the fact that I found out from test results, that I had to figure it out myself, before my doctor was able to tell me.”
As Americans continue to age, get sick, and navigate the health-care system, many of us may become more invested in the idea of open notes. Until they play a more widespread role in people’s lives, however, the most pressing question about whether you truly want instant access to all your medical information might be how it affects your doctor’s life. Many physicians have come around to open notes, or at least have realized that allowing patients to see what has been written about them is not always a huge bother. But the bigger question of just how quickly patients should be able to access medical information, and how soon doctors should be available to help patients process it, continues to plague physicians. The advent of immediate data sharing “has been a major problem in terms of physician quality of life, and that’s eroded across the board,” Peixoto told me. “Doctors don’t want to be connected all the time. They actually have their lives.”
Where we have landed, then, is an in-between. Patients can read their doctor’s notes and view test results at any hour of the day, but we can access our providers only at certain times. There is likely room for refinement. Allowing a patient to select whether they receive test results from their physician or their portal, or see notes only after their doctor has had the opportunity to walk them through the terminology used, for instance, could make all the difference, some doctors told me. For now, it’s worth asking yourself whether you want to access your patient portal alone, or want to wait until you can get your doctor on the line.
- Today's news
- Reviews and deals
- Climate change
- 2024 election
- Fall allergies
- Health news
- Mental health
- Sexual health
- Family health
- So mini ways
- Unapologetically
- Buying guides
Entertainment
- How to Watch
- My watchlist
- Stock market
- Biden economy
- Personal finance
- Stocks: most active
- Stocks: gainers
- Stocks: losers
- Trending tickers
- World indices
- US Treasury bonds
- Top mutual funds
- Highest open interest
- Highest implied volatility
- Currency converter
- Basic materials
- Communication services
- Consumer cyclical
- Consumer defensive
- Financial services
- Industrials
- Real estate
- Mutual funds
- Credit cards
- Balance transfer cards
- Cash back cards
- Rewards cards
- Travel cards
- Online checking
- High-yield savings
- Money market
- Home equity loan
- Personal loans
- Student loans
- Options pit
- Fantasy football
- Pro Pick 'Em
- College Pick 'Em
- Fantasy baseball
- Fantasy hockey
- Fantasy basketball
- Download the app
- Daily fantasy
- Scores and schedules
- GameChannel
- World Baseball Classic
- Premier League
- CONCACAF League
- Champions League
- Motorsports
- Horse racing
- Newsletters
New on Yahoo
- Privacy Dashboard
How To Read Doctor Visit Notes About Health, Symptoms And Weight
What does your doctor really think about your condition and health concerns? For more than a year now, patients have been able to access and read the observations doctors write down about them during a visit.
The clinical notes can come with surprises. Patients may be amused to find out they’re described by their physician as “well-nourished,” “well-groomed,” “pleasant” or “normal-looking.”
“’He is not ill-appearing or toxic-appearing.’ That’s the best review I’ve ever received,” one man wrote on Twitter after reading his doctor’s notes.
But patients may also be taken aback by comments referring to them as “obese” or mentioning their marijuana use. One woman was shocked when she saw her doctor wrote down that she “seemed overly dramatic,” she complained on Reddit .
As of April 2021, healthcare providers must give patients access to all of the health information in their electronic medical records as part of the 21st Century Cures Act . That includes your doctor’s written comments about your physical condition during a visit, along with any symptoms and what the treatment should be.
The rules don’t apply to psychotherapy notes made during counseling sessions or when doctors believe a patient would harm another person or themselves after reading the information, according to OpenNotes , a non-profit organization based at Beth Israel Deaconess Medical Center in Boston that advocates for greater transparency in healthcare.
Doctors have been both supportive and cautious of the movement. In a 2020 survey of 1,628 clinicians, 74% agreed note sharing was a good idea.
“It does give the patient a lot more ownership of their medical condition because they can see what we’re thinking about, they understand our thought processes a little bit more, and they can see what the options are,” Dr. Sterling Ransone, Jr., a family physician in Deltaville, Virginia, and chair of the American Academy of Family Physicians, told TODAY.
But knowing that patients can now read his notes, Ransone finds he self-censors himself to avoid sounding critical or judgmental of a patient.
“It’s difficult because sometimes you have to leave a note to yourself what your concerns are, but they can cause anxiety with the patient,” he noted. “I can say that it really has changed the way that a lot of physicians write their notes.”
That means more accessible language, less jargon and more caution with certain terms that might offend or upset a patient.
Ransone no longer uses the abbreviation “SOB,” which stands for “short of breath” and instead writes out the full term in his notes. Same with “FU,” which stands for “follow up.”
The American Academy of Family Physicians has also urged doctors to write “patient could not recall” instead of describing them as a “poor historian;” “patient declines” instead of “patient refuses;” and “patient is not doing X” instead of describing them as “non-compliant.”
A guide to your doctor’s note:
The medical note has traditionally included four parts, Ransone said: The subjective findings, or what a patient said they were concerned about; the objective findings, or what the doctor actually observed during the visit; the physician’s assessment after evaluating the patient and the treatment plan.
Doctors are used to jotting down any observations that can offer clues to what’s going on. So writing down that a patient “seemed overly dramatic” can mean the person’s complaint wasn’t consistent with the degree of their symptoms and something else might be the reason for their visit that day, he noted.
Here are other descriptions patients may find in their doctor’s notes:
Well-groomed or pleasant: This can indicate mental status. “If someone comes in and they’re somewhat disheveled, it leads you to wonder why and what do I need to look into?” Ransone said. “Pleasant” means the patient was communicative and responded to social cues, he noted. Patients who are upset or sleepy could have a substance abuse disorder or another reason why they’re having trouble interacting.
Well-developed or well-nourished: “A lot of times when people look at open notes and they’ll say, ‘Well, of course I am. What does this mean?’” Ransone said. “It just means that we checked in our mental checklist… (that) those aren’t things that we need to worry about.” If a person isn’t well-nourished, it might mean they don’t have access to food or their teeth might be in such bad condition that they can’t chew and get nutrition.
Unremarkable: This is a good thing. “Unremarkable is exactly what you want to be when you see a physician,” Ransone said. “I joke with my patients all the time: You want to be the most boring patient that I’ve seen today, because that means we haven’t seen anything that is abnormal that we need to chase down.”
Obese : To a physician, the term means the patient is of a certain weight for their height and frame, which comes with a certain constellation of medical concerns, Ransone said. “There’s a stigma to obesity in society and a lot of patients really don’t want to have that on their charts… but it’s a very important piece of the puzzle for me as I’m trying to help a patient get healthier,” he noted.
Substance use: This isn’t necessarily bad. Doctors will note a patient has an occasional glass of wine, for example, to give them an idea of the person’s alcohol consumption habits. “The way that our society looks at, say, marijuana use has changed a lot over the years, but a lot of people don’t want that included in the medical record,” Ransone said. “I’d like to know if someone is smoking weed because it could affect the medications that I should give them for their health condition.”
Other health observations patients frequently don’t want on their chart include mental health issues such as depression, anxiety or bipolar disorder, he noted.
Some patients have called Ransone to ask that he change something in their note because they see it as a pejorative or they disagree with his assessment, but that doesn’t mean he’s wrong, the doctor noted.
One guide for physicians suggested telling the patient: “I’m sorry you disagree with my assessment. While I can’t change my medical opinion, if you’d like I can add that you disagree with it.”
Patients pointing out factual errors — such as noticing the note referenced a problem in the right knee rather than the left — is a completely different issue. If there's anything inaccurate in your chart, bring it to your doctor's attention.
In fact, patients who read their doctor’s notes may play an important role in finding errors in their records, a 2020 study published in JAMA found.
Ransone encouraged patients who are reading their doctor’s notes to keep the lines of communication with their physician open.
“Don’t necessarily assume the worst when they read things. Realize that a lot of the things that they read are open to interpretation,” he advised.
This article was originally published on TODAY.com
Recommended Stories
Sparks rookie cameron brink: 'there's a privilege' for wnba's younger white players.
The Sparks rookie had plenty to say about her WNBA rookie class, headlined by Caitlin Clark.
Angel Reese's 'weak' ejection from Sky-Liberty game draws attention, offer from Bulls' Lonzo Ball
Reese was ejected after two very quick whistles from referee Charles Watson.
Larry Allen, Cowboys legend and Pro Football Hall of Famer, dies at 52
Allen was a seven-time first-team All-Pro and part of the Cowboys' Super Bowl XXX winning team.
Rivian's path to survival is now remarkably clear
Rivian has had a lot on its plate as it transitioned from pitch mode to selling EVs. It created an electric pickup and an electric SUV while prepping a monster IPO. It now plans to sell an even cheaper SUV that could make Rivian a dominant EV player for years to come.
Vikings reveal 'Winter Warrior' alternate all-white uniforms to be worn on Week 15
The Minnesota Vikings revealed their all-white "Winter Warrior" uniforms that the team will wear for Week 15's matchup with the Chicago Bears.
Sky's Chennedy Carter has 'no regrets' about foul on Caitlin Clark; Angel Reese will 'take the bad guy role'
The Sky have broken their silence about the flagrant foul on Caitlin Clark, and they had a lot to say.
GameStop stock soars as 'Roaring Kitty' announces livestream, reveals $382 million unrealized gain
First X, then Reddit, now YouTube. GameStop's most bullish enthusiast announced a livestream, and the stock surged.
Paul Skenes blows away Shohei Ohtani, who returns the favor in his next at-bat
The Dodgers-Pirates matchup lived up to its billing.
Yes, Marshall's has an online store — and we found 10 summer steals under $50
Tommy Bahama, Ralph Lauren, Jantzen: It's a treasure trove of deals — like going in person, but better!
2025 Toyota Crown Signia First Drive: Venza replacement puts efficiency and fashion first
Our first drive review of the 2025 Toyota Crown Signia where we tell you all about it and give initial driving impressions.

Stock market today: Stocks waver after jobs report smashes expectations
Investors are looking to the monthly jobs report for signs of labor market cooldown pivotal to the odds for a rate cut.
Emma Hayes' first big USWNT conundrum: Olympic roster cuts
At least two players who started for the USWNT over the past week will have to be cut for the Olympics. Might Alex Morgan or Rose Lavelle be on the roster bubble?
Opposing players aren't fond of Caitlin Clark ... which should be good for the WNBA
Watching Clark fight through adversity and rack up rivals will only bring more eyeballs to the league.
The Spin: Making a call on 5 slumping fantasy baseball stars
All five of these hitters were drafted highly in fantasy baseball leagues. So far, they have not lived up to their ADPs — and that's an understatement. Scott Pianowski analyzes.
Chiefs' Harrison Butker may be removed from kickoffs due to new NFL rules
Kansas City Chiefs special teams coach Dave Toub said kicker Harrison Butker may be removed from kickoffs. But not because of Butker's recent controversial remarks.
Courteney Cox, 59, wears these Adidas slides, and they're down to $15 at Amazon
Snag a pair of superstar-approved sandals for 50% off — just in time for summer.
Julia Louis-Dreyfus explains why she took a 'leap of faith' to star in tear-jerking new movie 'Tuesday'
In the film, Death arrives in the form of a talking bird at the home shared by a mother and her sick daughter.
Coaching the Lakers is a hard job to pass up, except maybe Dan Hurley should
History is littered with successful college basketball coaches who took a shot at leaping to the NBA but failed spectacularly.
Homebuyers are in a bittersweet market as mortgage rates drop below 7% but prices remain high
Mortgage rates fell slightly this week, according to Freddie Mac, but have hovered around 7% all year.
White Sox's Tommy Pham says he's always prepared to 'f*** somebody up' after confrontation with Brewers' William Contreras
Chicago White Sox outfielder Tommy Pham told reporters he's always prepared to fight after an on-field confrontation with Milwaukee Brewers catcher William Contreras.
- Complete clinical notes on time with these 6 workflow hacks

You’re not alone if you struggle to complete clinical notes on time. Most physicians spend over 10 hours per week on bureaucratic tasks, which compete for valuable time with patients. For many, the result is after-work EHR time , frustration, and professional burnout .
If this sounds familiar, it’s time to adopt these workflow hacks and consistently complete your clinical notes before leaving the office.
Tips to complete clinical notes on time
An article by Colleen Fogarty, MD, MSc in Family Practice Management , inspired these workflow hacks.
These tips are relevant for physicians with any documentation workflow . But if you’re serious about efficient documentation, consider modern tools like AI scribes or medical speech-to-text software .
1. Leverage the skills of your team members
You don’t have to document everything yourself; adopting a Team Documentation approach can save hours. For example, a nurse or medical assistant can document patient outcomes, review medications, and verify or record allergies. You can quickly review this information for accuracy and sign off on the note.
2. Complete most documentation in the room
When talking with a patient about their health history or treatment plan, summarize aloud as you take or dictate notes. Dictating aloud is efficient and can also engage the patient, improve understanding, and ensure accuracy. Many providers have found that dictating clinical notes during patient visits improves their documentation workflow while benefiting patients.
3. Know the E/M documentation guidelines
You can save a lot of time by only documenting what’s medically necessary to complete today’s visit. For example, a 99213 level of service doesn’t require a comprehensive review of systems or a comprehensive exam. This code is used 61 percent of the time by family physicians seeing Medicare patients.
4. Use time-saving EHR functions
Do you use the time-saving features of your EHR? Templates , for example, are helpful for routine visits where clinical queries are standard. During flu season, save yourself time by creating a basic influenza vaccine template. See more tips on how to optimize your EHR workflow .
5. Let go of perfection
The EHR can be a black hole for perfectionists and compulsive “box-checkers.” Remember the documentation guidelines and keep it simple. Not all boxes need checking; you don’t need to fill every category each visit. Know what matters, and leave the rest alone.
6. Time yourself
Use a timer on your smartphone or watch to see how long it takes to complete a note. Knowing your baseline, set a goal to decrease your per-patient documentation time. Speed shouldn’t be your only goal, and spending more time documenting visits with new or complex patients may be valuable.
Leave the EHR at home
These six tips will help you complete clinical notes on time and leave the EHR at the office. Discover more ideas for reducing after-hours work or learn about the latest AI tools that can write 80% of your clinical note in 60 seconds.
- Mobius Conveyor
- Conveyor QR
- Conveyor USB
Athenahealth-Specific
- Mobius Clinic
- Mobius Scribe
- Mobius Desktop Scribe
- Mobius Capture
Recent Posts
- Skip the EMR Tie-In: Benefits of EMR-Independent Documentation Tools
- How to keep up with the latest developments in healthcare
- What is Team Documentation? Benefits and tips to begin
- The Best Free Medical Dictation Apps
- Privacy & Terms
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health
- PMC10379287

Patients’ Perspectives on the Use of a Newly Developed “Patients’ Guide for Doctor’s Visit”: DocVISITguide
Rebecca jaks.
1 Careum Center for Health Literacy, Careum Foundation, 8032 Zurich, Switzerland; [email protected] (E.G.); [email protected] (S.M.D.G.)
Elena Guggiari
2 Careum School of Health, Kalaidos University of Applied Sciences, 8006 Zurich, Switzerland
Saskia Maria De Gani
Dunja nicca.
3 Epidemiology, Biostatistics and Prevention Institute, University of Zurich, 8001 Zurich, Switzerland; [email protected]
Associated Data
The data, as well as the DocVISITguide presented in this paper, are available on request from the corresponding author.
During doctor’s visits, fundamental decisions regarding a patient’s diagnosis and therapy are taken. However, consultations often take place within a limited time frame and are characterized by an asymmetric interaction. Therefore, patients’ questions can remain unanswered and concerns unspoken. A "Patients’ Guide for Doctor’s Visit" (DocVISITguide) was developed to prepare patients for their visits, supporting them to take an active role in the communication and leave the consultation well-informed. This paper describes the development of the DocVISITguide and its first small-scale evaluation based on a sequential explanatory mixed methods design from the patients’ perspective. For this purpose, a small sample of patients completed a pre- and post-questionnaire, and two in-depth interviews were conducted. Most participants found the DocVISITguide easy to understand. The guide helped them to take a closer look at their own health situation and be better prepared for the visit. More than three-quarters (82%) of the participants would probably use the guide again, and all (100%) would recommend it to family and friends. However, some patients felt unsure about using the guide within the consultation and showing it to their physician. To counteract this uncertainty, physicians should be actively involved in the use of such guides in the future.
1. Introduction
According to the most recent data, 71% of the people living in Switzerland consulted a general practitioner at least once during the past year, while the number of consultations increased with patients’ age [ 1 ]. Furthermore, 43% of them consulted a specialist at least once [ 1 ]. These data indicate that a majority of Swiss residents are in regular exchange with a general practitioner, which, in turn, is a key opportunity for both patients and health professionals to interact in regard to important decisions related to patients’ health and well-being [ 2 , 3 ]. Concretely, for the patients, doctor visits represent a central source of information to self-manage their illness as well as to adopt preventive and health-promoting behaviors [ 3 ]. For general practitioners and specialists, on the other hand, such consultations constitute an important occasion for obtaining useful information on patients’ expectations, symptoms and concerns, which play a crucial role in diagnosis, treatment and prevention purposes [ 2 ]. Furthermore, general practitioners can support their patients with regard to orientation and coordination in the health system, referring them to further service resources [ 3 ]. This is of importance since recent national data on health literacy shows that there is a huge need from the patients’ side for support in navigating the health system [ 4 ]. Furthermore, the same study revealed that almost half of the population living in Switzerland (49%) reported low health literacy and hence difficulties in dealing with health information, whereas specific population groups tend to have a lower health literacy than others [ 4 ]. In Switzerland, as well as in other European countries [ 5 , 6 ], such vulnerable groups include people with a poor health status and with one or more long-term illnesses, low socio-economic status and lower education. Therefore, these vulnerable groups might experience even greater challenges when making decisions for their own health or when consulting health professionals. Health literacy, i.e., the knowledge, motivation and competencies to access, understand, appraise and apply health-related information, is a crucial resource for people to be able to make decisions in regard to their own health in everyday life [ 7 ]. Such decisions often take place in interaction with or after visiting health professionals [ 8 ]. Therefore, sufficient health literacy is key for patients to better benefit from doctor visits and achieve better health outcomes [ 9 ]. Likewise, it is important that health professionals are able to strengthen the health literacy of their counterparts [ 10 , 11 ].
The communication between patients and doctors can be a challenging interaction for several reasons, particularly in the case of multiple chronic conditions [ 12 ]. On the one hand, physicians need to collect enough information for clinical reasoning and to determine a patient’s health issue [ 13 ], often under circumstances of limited time for these ambulatory doctor visits [ 14 ]. The lack of time poses the following important challenges: for example, under time pressure, there seems to be a risk that physicians ask fewer questions concerning patients’ symptoms and concerns, conduct a less thorough clinical examination and can offer less advice for a healthy lifestyle [ 15 ]. On the other hand, the lack of time during doctor visits can also prevent patients from asking questions, with the consequence that concerns regarding their diagnosis, treatment and other issues related to their health remain unspoken [ 16 ]. If the communication between patients and physicians is too asymmetrical, expressed by the absence of patients’ involvement in the decision-making processes [ 17 , 18 ] and by the use of unclarified medical jargon [ 19 ], negative consequences for patients’ health can occur [ 16 ]. In addition, decisions about the treatment strategy might be made on the basis of insufficient information, and the reasons for the importance of adhering to this strategy may not be understood by the patient [ 20 ]. This can consequently result in less adherence to medical therapies [ 21 ], and patients might remain unsatisfied with the consultation [ 18 ].
So far, most measures to improve the interaction between patients and doctors in the context of ambulatory doctor visits have mainly focused on a shared decision-making approach and on sensitizing physicians to the potential asymmetry of the conversation and its consequences [ 22 ]. However, patients need to be empowered to use the time during the consultation in a goal-oriented way and to take an active role in the communication (e.g., by asking questions and obtaining comprehensible information) in order to leave the consultation well-informed [ 23 ]. Moreover, improving the communication within ambulatory doctor visits can have several benefits for patients, e.g., improving patients’ outcomes and their perceptions of their control over their own health, their recall of information and their adherence to medical recommendations [ 24 ].
For example, to support the communication of patients with their doctors, question prompt sheets have been developed to enhance patients’ capabilities to take an active role in medical consultations by encouraging them to ask questions about treatment options. Such question prompt sheets can help to increase the number of questions asked by patients during consultations [ 24 , 25 , 26 , 27 , 28 ] and to improve patients’ satisfaction with the medical consultation [ 26 , 27 ]. The support tools also show the potential to encourage physicians to provide more health-related information to their patients [ 28 ]. However, the available tools and resources for supporting patients during consultations were mainly developed in countries other than Switzerland. To our knowledge, no widespread tools have been available in Switzerland so far, and especially have not been evaluated with patients interacting with the Swiss health system. Furthermore, many of the existing resources focus on the consultation itself and do not explicitly include the preparation phase and the follow-up after the consultation.
Hence, with this project, we wanted to develop a culturally sensitive and evidence-informed guide for doctor’s visits for the population of the Canton of Zurich, Switzerland, including the following three phases: pre, during and after consultation. The overall aim of this paper is to describe the development and first small-scale evaluation of the patients’ perspective on the “Patients’ Guide for Doctor’s Visit” (DocVISITguide) by using a sequential explanatory mixed methods design. Concretely, this involved collecting quantitative data on the acceptability, feasibility and adoption of the developed guide and then explaining the quantitative results with in-depth descriptions of patients’ experiences with the guide.
2. Materials and Methods
This project includes a participatory approach to develop a Patients’ Guide for Doctor’s Visit (DocVISITguide) (phase 1) and its first small-scale evaluation (phase 2) following a sequential explanatory mixed methods design [ 29 ]. The development of the DocVISITguide included (a) a literature and internet search, (b) feedback from patients and professional experts and (c) a certification for plain language, while the evaluation phase included (a) a pre- and post-questionnaire followed by (b) semi-structured interviews ( Figure 1 ). The methods and results are reported along these two project phases.

Development of a “Patients’ Guide for Doctor’s Visit” and its evaluation based on a sequential explanatory mixed methods design.
2.1. Phase 1: Development of the Patients’ Guide for Doctor’s Visit (DocVISITguide)
The development of the DocVISITguide started in 2019 as a practice developmental project within the “Health Literacy Zurich” program. The program is hosted by the Department of Health of the Canton of Zurich (Gesundheitsdirektion Kanton Zürich) and Careum with the aim to improve health literacy within the population of the Canton of Zurich, Switzerland, through a series of research and practice developmental projects.
2.1.1. Literature and Internet Search
For the development of the DocVISITguide, we reviewed the literature on patients’ guidance for visiting healthcare professionals and performed an internet search for already existing tools in German and English.
The results of the literature review were used to formulate the following core principles and quality criteria for the development of such a guide applicable to the entire resident population of the Canton of Zurich over the age of 16: (a) support patients before, during and after the doctor’s visit, (b) be as generally applicable as possible in terms of content, i.e., be usable for all patient groups across all diseases, (c) be adaptable to individual needs of patients and the requirements of a physician consultation, (d) focus on a few core messages and (e) enable a low-threshold use through language and design.
The internet search provided materials such as checklists and guidelines available for preparing doctor’s visits. A total of 17 tools were identified. They ranged from one-page downloadable documents to elaborate websites with the possibility to compile individualized forms and download supplementary material such as videos or comprehensive brochures. Each of the tools identified was rated based on strengths and weaknesses. Among those we found, nine of them were rated as too comprehensive, with a different focus, disease-specific, disease-oriented or for a different target audience. The remaining eight tools were rated as good or very good but still did not entirely cover all pre-defined core principles. Therefore, we used some information from these tools as a starting point, adapted it for our purpose and developed the first draft of the DocVISITguide.
2.1.2. Expert-Feedback and Focus Groups with Patients
The draft version of the DocVISITguide was adapted based on feedback from experts, including professionals and patients.
Seven professionals with expertise in one or more of the following fields were recruited based on a stakeholder analysis: ambulatory medicine, public health, migrant health, patient-safety and/or patient-provider communication. They received the draft version of the DocVISITguide and were asked to provide written comments on how they evaluate the content, the language and comprehensibility as well as to provide open feedback. The written feedback was summarized. This was followed up by a short telephone interview with experts, aiming to clarify specific issues and reach consensus on overall feedback. Feedback was then integrated into the draft version of the DocVISITguide.
The patient perspective on the draft version was included by means of two focus group interviews with three participants each. The aim was to stimulate discussions among patients or potential patients. The first group was purposefully recruited in a general practitioners practice, focusing on diversity in relation to disease status, gender, age and education. The second group was purposefully recruited outside the health setting focusing on persons of different ages and genders as well as such without current health problems or with chronically ill relatives they care for. We assumed that the two diverse groups would allow a heterogenous perspective on the guide. The focus group discussions were led by a leader of the program. In the beginning, both groups received the DocVISITguide and time to read it before the focus group interviews started. During the interviews they were asked to discuss the general comprehensibility, in particular, unclear contents and formulations, comprehensibility of the use of the tool, shortening options and additions and wishes regarding design and content. Patients’ feedback from both group interviews was mapped during the meeting and summarized, and integrated into the DocVISITguide.
2.1.3. Editing and Certification for Plain Language
The final version of the DocVISITguide was edited for plain language in order to make the guide understandable for as many people as possible. The language revision was made through an organization in Switzerland (Pro Infirmis), where professional copywriters, as well as review teams, simplified the texts according to the rules of plain language. The DocVISITguide received the official label of “leichte Sprache” (plain language), meaning that the guide follows the rules for easy language and that examiners from the target audience understood the text.
2.2. Phase 2: Sequential Explanatory Mixed Methods Design
For the evaluation of the DocVISITguide, a sequential explanatory mixed methods design has been used. This involved collecting quantitative data with a pre- and post-questionnaire first and then explaining aspects of the quantitative results with qualitative data collected via interviews.
No ethical approval was needed for the evaluation of the DocVISITguide as it was considered as a practice developmental project. Nevertheless, prior to participation, all participants received written information on the evaluation process and the opportunity to ask questions. Information was provided on aim of the project, procedures, voluntariness of participation and the right to withdraw any time, as well as on data protection measures.
2.2.1. Sample and Recruitment
For the quantitative questionnaire, we planned to recruit a convenience sample of 30 participants from organizations with a diverse patient population. Within the frame of this practice developmental project, we were interested in implementing new practices timely in a step-wise process and with limited resources. This sampling approach allowed the first small-scale, descriptive feedback on patients’ perspectives with the use of the guide. For generalizable results, a sample almost equal the Swiss population would be needed, given that the DocVISITguide applies to all patients visiting medical ambulatory care, which applies to more than 70% of the Swiss population each year [ 1 ]. Inclusion criteria were the following: to be able to speak German, to be 18 years and older, to live in Switzerland, to have a doctor’s visit planned in the near future (approximately 4–6 weeks), to be willing to complete a survey before and one after the doctor’s visit and as a matter of course be willing to use the guide beforehand and ideally use it also during the consultation. The reason for their appointment was not relevant to participation.
Participants were recruited through a large Swiss patient organization via their helpline. The organization’s helpline serves patients with diversity in socio-economic status and place of living (urban, rural areas). However, due to the corona-pandemic, the number of calls as well as medical visits had decreased. We therefore involved two additional patient organizations in the recruitment process, which resulted in nine additional participants. To further improve the recruitment, we approached participants directly in the waiting room of a large general practitioners’ practice. The practice is located in an urban setting serving patients with diversity in socio-economic status. Nevertheless, even this approach has led to only two more patients. For this reason, we decided to spread a call for participation through our LinkedIn channel as well as our newsletter and those of other relevant partners. All these recruitment strategies resulted in a total sample of 22 patients who completed both questionnaires.
For the qualitative in-depth interviews, we had planned to recruit a sub-sample of four to six people from the quantitative sample. Accordingly, via e-mail, we contacted the 22 participants who had completed the quantitative pre- and post-questionnaire and asked them to take part in interviews (telephone or in-person). We were able to conduct interviews with two participants.
2.2.2. Data Collection
To assess the acceptability, feasibility and adoption of the DocVISITguide from the point of view of individuals, a pre- and a post-questionnaire was developed. The questionnaires were oriented toward implementation outcomes, specifically acceptability, feasibility and adoption [ 30 ]. The pre-questionnaire mainly covered questions on acceptability of the guide. It included 28 questions divided into the following three main sections: questions about the person (7 questions), questions about the guide such as the first impression, comprehensibility, importance of use (17 questions) and questions about the context of the medical visit (4 questions). To be able to guarantee anonymity and simultaneously to allow to match the two questionnaires and to know if a person completed both surveys as requested, we asked three questions that permitted the generation of a unique personal code that participants could easily recreate. The post-questionnaire covered feasibility and adoption with 14 questions focusing on their use of the guide, their perceptions of specific parts as well as their assessment of its applicability, usefulness and potential future use.
Participants could either complete the pre- and post-questionnaires by means of computer-assisted web interviews or with paper and pencil. Data collection took place between May 2021 and June 2022.
For the qualitative part that took place after the quantitative pre- and post-assessment, we developed and used a semi-structured interview guide with open-ended questions. This included especially questions on participants’ experiences with the guide and perceptions when using it in interaction with physicians. Of the two participants that accepted our invitation, one interview was conducted over a video conference system, while the other was conducted in person. Both interviews were held in German or Swiss German, lasted approximately 30 min and data were audio recorded.
2.2.3. Data Analysis
For data analysis of the quantitative data, we used IBM SPSS Statistics 27 (IBM Corp., Armonk, NY, USA). Descriptive analyses were performed to characterize the study population and summarize patients’ evaluation of the guide regarding acceptability, feasibility and adoption. For the analysis of the qualitative data, we used six steps oriented toward reflexive thematic analysis, whereas interpretation was limited due to the small data set [ 31 ]. In the first step, we familiarized ourselves with the data by listening to the audio data and taking first notes. In the second step, we coded the data set into meaningful segments, including analytical descriptions for each. In the third step, we identified themes by compiling clusters of codes that seemed to share core ideas. In the fourth step, in order to organize the inductively developed themes into a central organizing concept, we compared the themes with the results of the quantitative data set and used a joint display to visualize similarities and differences in qualitative and quantitative data. In steps 5 and 6, we made sure that each qualitative theme was clearly demarked and built around a core concept and that quotations were accurate and illustrative. Given that we had only two participants, we made sure that similarities and differences in experience between the two “cases” became visible. With this process, we focused on inductive thematic saturation, related to the emergence of new codes and themes in the limited data set of two “cases”.
3.1. Description of the DocVISITguide
The DocVISITguide has a length of six pages and is divided into the following four sections: (1) front cover, (2) before the visit (preparation), (3) during the visit (accompaniment) and (4) after the visit (follow-up).
The front cover briefly states why such a guide can be beneficial for patients and gives an overview of the content. This is followed by the second section, dedicated to the preparation phase before the doctor’s visit. This includes three useful tips for users on how to best prepare for their doctor’s visit (e.g., that they can bring a trusted person with them), a small section containing some examples of claims that they can tell their doctor (e.g., “these are my complaints”, “this is better or worse since my last visit” or “these are effects and side-effects of my medication”), as well as central questions to prepare for the visit. These questions cover matters such as what health-related issue they have, what they can do about it, what they need to know about possible treatments, what happens next and where they can find information and support. Concrete questions are, for example, “What is the name of my disease (diagnosis)?”, “What are the treatment options for my disease?” or “What consequences does the treatment have on my everyday life?”. The last part of the preparation phase is a space where notes can be made. This is divided into the following two parts: “this is what I want to say to my doctor” and “this is what I want to ask to my doctor”. The third section during the doctor’s visit contains five tips as well as a short explanation of why they are important and can support patients during the consultation. For example, “allow yourself enough time for a decision” as “you have a say in your treatment. You can also talk to someone else about it.”. The DocVISITguide ends with a part dedicated to the time after the doctor’s visit and what happens next. The guide identifies important points for patients following the doctor’s visit, which should encourage them to follow up on the appointment, such as “When is my next visit to the doctor?”, “Have I forgotten an important question or information?”, “Would I like to call the practice again and ask about it?” or “With whom would I like to discuss open questions or decisions?”.
3.2. Use of the DocVISITguide before and after the Doctor’s Visit
3.2.1. sample characteristics.
The quantitative survey was filled in by 22 participants. Their socio-demographic characteristics are summarized in Table 1 . They were mostly female (73%) and between 31 and 40 years old (31%). For most participants (88%), German is their first language and half of them have an educational background in the health sector.
Characteristics of study participants.
Legend: * multiple choice possible.
The two participants of the qualitative interviews (sub-sample) were a male and a female, between 31 and 40 years. One of them lives with a chronic disease and has expertise in self-management for several years, whereas the other went to the doctor for an acute orthopedic problem. Both participants have had some negative experiences with their doctors in the past. They explained that they were motivated to take part in the interviews because they were curious to know more about the DocVISITguide and in order to reflect and talk about their experiences with doctor’s visits.
3.2.2. Quantitative Results
In the first step, the participants were asked some questions about the context of their doctor’s visit. During the last 12 months, participants had visited a doctor with a median of 5.5 times (range = 30). Most participants (45%, 10 out of 22) visited a specialist (other than a gynecologist) or a GP/family doctor (41%, 9 out of 22). The main reason for the visit for most of the respondents (59%, 13 out of 22) was a chronic condition. Regarding the application of the guide, 77% (17 out of 22) of the participants did not inform their health professional about it.
When it comes to the questions on the guide itself, most of the respondents (95%, 21 out of 22) liked the guide at first glance. The content coincided (very) strongly with the expectations of 77% (17 out of 22) of the respondents, while 5% (n = 1) found that it did not match their expectations at all. Further questions on the comprehensibility and content of the guide showed that the structure was considered logical and the information understandable to all participants (100%, 22 out of 22) (see Figure 2 ). There was less agreement regarding the length of the guide, where 15% (22 out of 22) of the participants stated that it was not optimal. Based on the answers in the open comment section, it seemed that the DocVISITguide was considered a bit too long.

Level of agreement with statements on comprehensibility and content of the guide.
A further question concerned the usefulness of the tips and questions in the guide. Participants rated them, in general, as (rather) helpful, with values varying between 60% (12 out of 20) and 100% (see Figure 3 ). Tip 5 “At the end you can ask your doctor to summarize the most important information for you”, was considered less useful compared to others. All participants also agreed that making notes beforehand is very useful, and 91% were of the same opinion regarding the questions contained in the DocVISITguide.

Usefulness of tips in the guide for preparation.
Participants were also asked to report which of the tips they planned to apply before or during the visit. Between 81 (17 out of 21) and 95% (21 out of 22) of participants stated to be (rather) sure to use tip 2 “Take important documents with you to the doctor’s visit”, tip 3 “Take notes. Take your notes with you to the doctor’s visit”, tip 6 “Give yourself enough time when taking a decision”, tip 7 “You are not sure you understand everything? Tell the doctor in your own words what you have understood” and tip 8 “You don’t understand something? Ask!”.
The results show certain discrepancies between planned and actual behavior. In total, 91% (20 out of 22) of the participants stated to have used at least some parts of the guide during their visit. These participants were also asked how useful each tip was for their visit, and most of them felt that the tips were helpful (see Figure 4 ). Less agreement was found for tip 4 “Take notes during your visit” and tip 5 “At the end, you can ask your doctor to summarize the most important information for you”, where 41% (7 out of 17, tip 4) and 31% (5 out of 16, tip 5), respectively, declared that these tips were rather unhelpful or not at all helpful. Comparing the distribution regarding the usefulness of the tips before and after the visit, we see a similar picture—those tips that were considered more useful already before the visit were also considered more useful afterward.

Usefulness of tips in the guide for their visit.
After the doctor’s visit, 75% (15 out of 20) of the participants stated that they had used the notes made beforehand during their appointment. And both before and after the appointment, all participants (100%) agreed that taking notes was helpful.
The results further show that the majority (77%, 17 out of 22) of the respondents were likely to use the guide again in the future. This number slightly increased after the doctor’s visit (82%, 18 out of 22). All the participants, both before and after the doctor’s visit, affirmed that they would recommend the guide to family, friends and acquaintances.
Lastly, the results indicate that most of the participants felt prepared for the visit (91%, 20 out of 22) and were able to use the available consultation time at its best (86%, 19 out of 22), thanks to the preparation and the notes taken beforehand (see Figure 5 ). Furthermore, due to the tips and information in the guide, 91% (20 out of 22) were able to ask their questions; however, 32% (7 out of 22) did not get all their questions answered. Most of the participants left the discussion well-informed (82%, 18 out of 22), and 73% (16 out of 22) knew what to do to solve their health problems.

Level of agreement with different statements about the guide and the preparation phase.
3.2.3. Qualitative Findings
The quantitative results across three dimensions (acceptability, feasibility and adoption) informed the structure of the inductively generated qualitative themes based on two case studies. The experiences of two patients with the guide are presented with a joint display in Table 2 and are divided into four themes, illustrated with corresponding quotes.
Joint display of quantitative and qualitative findings on perception and experience with the DocVISITguide.
4. Discussion
This practice developmental project resulted in the DocVISITguide aiming to support patients before, during and after their doctor’s visit, and specifically by using the available consultation time in the best manner possible and by taking an active role in the communication via asking questions and following up on the issues discussed during their visit.
The results of the evaluation indicate that participants, who were predominantly well-educated and familiar with the health system, overall liked the content of the DocVISITguide, rated its feasibility as good and would use it again in the future. Participants would also recommend it to their family, friends and acquaintances. Concerning the acceptability of the DocVISITguide, there is a potential discrepancy between the quantitative findings with high acceptability values and the qualitative results. The two in-depth interviews showed that at the beginning, participants were rather skeptical about the DocVISITguide and expectations about it were rather low. They believed that it would not bring them anything new compared to what they already knew or had done so far. However, they still decided to participate in the evaluation and to use the DocVISITguide—probably driven by curiosity about it or because of their past experiences in their interactions with health professionals. Furthermore, they were sensible about the topic of doctor-patient communication and recognized the relevance of the project. Such results indicate that overcoming patients’ skepticism and convincing them to use the DocVISITguide can be quite challenging, despite their familiarity with the health system. Furthermore, the recruitment barriers we experienced might not only relate to the situation around COVID-19 but also relate to such skepticism. These barriers are challenging but could be overcome to some extent if patients are introduced to the DocVISITguide and its benefits directly by health professionals, health organizations or patient organizations they trust and not by an unknown third party or anonymous institution.
The quantitative results also showed that participants gave quite high values to the feasibility in respect to the preparation for the doctor’s visit and to the use of the guide. In particular, most of the participants reported that the guide was understandable and helpful in their preparation for the visit and the procedure during the consultation. These results suggest that despite its generic approach, the DocVISITguide can be a useful tool for diverse patients to prepare for their doctor visits. Further research would be needed to understand potential differences across specific patient groups, in particular those with low health literacy [ 4 ].
The adoption of the DocVISITguide had positive effects on the participants by giving them useful tips and information or by reassuring them that what they were already doing was in the right direction for a successful doctor’s visit. Applying the DocVISITguide enabled participants to think more deeply about their own health situation and to reflect thoroughly on what they wanted to discuss with and ask their doctor about. These findings confirmed the positive effects already found in previous interventions aimed at improving patients’ communication with doctors, such as an increase in question-asking, taking an active patient role, a better recall of information and patient satisfaction [ 24 , 26 , 28 ]. However, previous evidence has been mixed, and findings have not been always consistent [ 28 ]. More research on the outcomes of interventions aimed at improving patients’ communication with doctors is therefore needed. The results of the present evaluation also showed that, before the visit, participants stated to plan to use certain tips and information from the DocVISITguide for their next doctor’s visit. These initial intentions and the actual behavior, however, partly diverged. These results may have come into play as the DocVISITguide, with its aim of trying to reach as many people as possible, is probably not suitable for all situations, or the patients need further encouragement to actually apply them. Nonetheless, the use of the tips and information contained in the DocVISITguide might depend on the reasons behind the doctor’s visit and on the specific patient’s situation. A person who is just attending a routine control probably has different questions and needs and especially less experience in communicating them than someone with a complex chronic illness and who is frequently in contact with health professionals and confronted with the health system in general [ 32 ]. Another reason for the discrepancy between initial intentions and actual behavior could also be related to the limited time available for the consultation [ 14 ] and hence for asking questions, even though in Switzerland, this issue seems to be not as worse compared to other countries [ 33 ].
Importantly, the results from the two qualitative interviews cannot be generalized, but provide the following important, unexpected insight: participants did not want to show and actively use the DocVISITguide in front of their physician and preferred to not take it with them into the consultation room. During the qualitative interviews, insecurity and shame were mentioned as reasons for not applying or taking the DocVISITguide with them. This insecurity to use the DocVISITguide openly during consultations might be a result of years of asymmetric relationships between patients and physicians [ 17 , 22 ] that have led to general mistrust in this respect. Not having the information with them during the visit may have also led to the patients forgetting some of the points noted beforehand in the DocVISITguide and, consequently, leading to a mismatch between intention (“I plan to use the tips”) and actual behavior (“I used the tips”). Since this aspect is important for the further scale-up potential effectiveness of the DocVISITguide, it should be further explored.
Given that building trust on the individual patient–professional level is an issue, it would be beneficial if health professionals, and especially physicians, were involved in the use of tools like the DocVISITguide and would promote it among their patients. This could reassure patients to actively use the DocVISITguide during their future doctor’s visits, allowing them to ask their questions and concerns and take an active role. A recent qualitative study analyzing patients’ experiences with question prompt lists [ 34 ] also found that patients would feel reassured in using such tools if doctors normalized, endorsed and recommended them. Since health professionals are in regular contact with patients and are an important point of contact for health issues and general questions [ 3 ], the support of the use of a DocVISITguide would also support patients in dealing with health information and, consequently, also strengthen the health literacy of their patients. In particular, the use of a DocVISITguide could improve the interaction between physicians and vulnerable groups of patients with insufficient health literacy [ 4 , 6 ].
We acknowledge that the development and first small-scale evaluation of the DocVISITguide is not without limitations. Ideally, more diverse participants should have been involved in the evaluation of the guide. The project was conducted during the COVID-19 pandemic, when doctor’s visits were reduced to the minimum [ 35 , 36 ], and patients were probably less willing to participate. Additionally, the discussed skepticism in respect to patient–provider communication with the guide has led to a difficult recruiting process and a smaller, less diverse sample than planned. The qualitative interviews, to some extent, expanded the quantitative findings, explaining in more detail what the perceived barriers to using the guide during doctor’s visits could have been. However, a larger sample would have allowed a richer description of themes.
Nevertheless, the participatory development of the DocVISITguide led to a guide that is already strongly oriented towards the needs of patients, and the small-scale evaluation, with its rather positive findings, points in the same direction. This highlights that the DocVISITguide with the first adaptations based on the findings is ready to be used for the next phase of evaluation and development. Learning from agile sciences, such small-scale evaluations are important to—(a) guide a user-oriented development of tools early on, (b) bring results back into real-world settings quickly and (c) create a participative learning process before going into more rigorous testing and evaluation [ 37 ]. Therefore, the DocVISITguide adapted based on the first patient experiences presented here should go into testing of effectiveness with respect to improving health literacy with a sample that enables the evaluation of sub-groups and different settings. Additionally, implementation outcome evaluation should be integrated and focus on trust and interaction between patients and health professionals.
5. Conclusions
Given that the newly developed DocVISITguide, according to the results of its first small-scale evaluation, is well-received by patients to prepare for their doctor’s visit, its advancement and implementation should be carried on. In order to improve its use for patients during their visits with health professionals, implementation strategies should focus on the involvement of professionals in the process. Further systematic evaluation should support these processes.
Results show that the DocVISITguide provides support, in particular, before and during the doctor’s visits, and encourages patients with the therein contained tips and information to take a closer look at their own health situation and to take an active role during the consultation. The DocVISITguide seemed to facilitate a fruitful and well-informed doctor’s visit. Nevertheless, patients might feel insecure about using the guide during the visit and showing or mentioning its use to the doctor. To counteract this feeling and inhibition, the further development of the guide and its implementation should focus more on overcoming patients’ reluctance. One approach could be, for example, to actively involve health professionals in the process of distributing, applying and using such guides together with their patients.
Acknowledgments
First: we would like to thank Dominique Vogt and Katrin Gehring who initiated the project and the development of the DocVISITguide. We then want to acknowledge the friendly cooperation with the organizations who supported the recruitment of patients for the evaluation (Schweizerische Patientenorganisation SPO, Selbsthilfe Zürich, Permanence Winterthur und Verein Altea Long COVID Network). We also thank all patients for their participation. Furthermore, we want to thank Anja Inauen for the administrative and technical support in the project.
Funding Statement
This research was funded and realized by the Careum Foundation Zurich and the Health Department of the Canton Zurich (represented by the Epidemiology, Biostatistics and Prevention Institute of the University of Zurich) within the framework of the program “Gesundheitskompetenz Zürich”. Part of the funding for this project was provided by the “Allianz Gesundheitskompetenz”.
Author Contributions
Conceptualization, methodology and formal analysis R.J. and D.N.; writing—original draft preparation, R.J. and E.G.; writing—review and editing, R.J., D.N., E.G. and S.M.D.G.; project administration, S.M.D.G. and D.N. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The project was conducted according to the guidelines of the Declaration of Helsinki. Ethical review and approval were waived for this project, as it is outside the scope of the Human Research Act and did not require approval by the ethics committee.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the project.
Data Availability Statement
Conflicts of interest.
The authors declare no conflict of interest. The funders had no role in the design of the project; in the collection, analyses or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
- Patient Portal
- Classes and Events
- Find a Doctor
- Schedule Appointment

Let’s Get Physical? The Differences Between Physical Exams and Annual Wellness Visits
From changing guidelines about when to start getting mammograms to understanding the different types of annual visits to schedule with your primary care doctor, navigating medical care can be complicated.
If you are on Medicare, it's important to understand these nuances, especially the difference between a physical exam and an annual wellness visit. Your insurance defines these two appointments differently, which could affect your out-of-pocket costs. Here’s what you need to know about these two types of visits.
Annual physical exam
During a physical exam, your doctor will discuss basic recommended health screenings with you and provide physical examinations. For women or people assigned female at birth, a yearly checkup may include a pelvic exam and recommended screenings such as mammograms or Pap smears. For men or people assigned male at birth, this appointment might include a testicular exam and a prostate-specific antigen (PSA) blood test to screen for prostate cancer.
Your doctor may recommend other screenings, such as:
- Colonoscopy
- Behavioral health screenings
- Cholesterol level
- Blood sugar level
These appointments are beneficial in a variety of ways, including an in-depth look into the status of your current conditions and providing you with updated insights through tests and screenings. Physicals give you a better understanding of your health, increase your ability to assess your risk for future complications and offer a professional guide to help navigate diagnoses and treatment.
“The costs of these appointments can change based on the types of testing performed, and Medicare generally does not cover lab work like cholesterol screenings unless it is tied to a specific medical condition,” said Jillian Gansert, MD , Primary Care Physician at Inspira Medical Group. “While Medicare does not cover annual physical exams, it does cover a single ‘initial preventive physical examination’ visit offered to newly-enrolled Medicare beneficiaries. Those are followed by exams called annual wellness visits.”
Medicare annual wellness visit
An annual wellness visit is an appointment covered by Medicare Part B focused on health promotion and preventive care. During a visit, your health care provider can give you personalized health advice, and together you will develop action plans based on your risk factors, lifestyle, existing medical conditions, and individual needs.
This type of visit also includes:
- A routine check of your height, weight, blood pressure, and body mass index (BMI)
- A review of the medications, supplements, and vitamins you are currently taking
- An overview of your personal and family medical history
- Screenings for issues with your mood or memory that can affect your health and well-being
- Routine vaccinations, including annual flu and pneumonia vaccines
“Because Medicare covers annual wellness visits 100 percent, these appointments can give you insight into your health without increasing your healthcare costs,” said Dr. Gansert. “Patients get the opportunity to review existing medical conditions and current list of medications with their care team, receive preventive care, and plan small life changes.”
Which type of appointment should you make?
While these two annual visits may sound the same on the surface, different care is associated with each. Additional costs are associated with an annual physical exam, but they can give you more in-depth information through testing and screenings related to your health in specific areas. If you are looking to get a routine check of your vitals, updates on vaccinations, and an overview of your current health, schedule an annual wellness visit. Both appointments are important and should be part of your yearly health plan.
Inspira offers comprehensive primary care throughout the South Jersey region. Click here to schedule an annual wellness visit at Inspira Health .
News From Inspira

Your memory changes as you age, so a certain amount of forgetfulness is normal—but not always. Learn...

Recent studies show that intermittent fasting can increase your risk of cardiovascular death. Here’s...

Appendicitis is a medical emergency that requires immediate care. Recognizing the early signs of...
- Patient Care & Health Information
- Diseases & Conditions
- Sleep apnea
Sleep apnea is a potentially serious sleep disorder in which breathing repeatedly stops and starts. If you snore loudly and feel tired even after a full night's sleep, you might have sleep apnea.
The main types of sleep apnea are:
- Obstructive sleep apnea (OSA), which is the more common form that occurs when throat muscles relax and block the flow of air into the lungs
- Central sleep apnea (CSA) , which occurs when the brain doesn't send proper signals to the muscles that control breathing
- Treatment-emergent central sleep apnea , also known as complex sleep apnea, which happens when someone has OSA — diagnosed with a sleep study — that converts to CSA when receiving therapy for OSA
If you think you might have sleep apnea, see your health care provider. Treatment can ease your symptoms and might help prevent heart problems and other complications.
Products & Services
- A Book: Future Care
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Mayo Clinic Store — Solutions for a Healthier Living
- Newsletter: Mayo Clinic Health Letter — Digital Edition
- Sleep Apnea Products from Mayo Clinic Store
The symptoms of obstructive and central sleep apneas overlap, sometimes making it difficult to determine which type you have. The most common symptoms of obstructive and central sleep apneas include:
- Loud snoring.
- Episodes in which you stop breathing during sleep — which would be reported by another person.
- Gasping for air during sleep.
- Awakening with a dry mouth.
- Morning headache.
- Difficulty staying asleep, known as insomnia.
- Excessive daytime sleepiness, known as hypersomnia.
- Difficulty paying attention while awake.
- Irritability.
When to see a doctor
Loud snoring can indicate a potentially serious problem, but not everyone who has sleep apnea snores. Talk to your health care provider if you have symptoms of sleep apnea. Ask your provider about any sleep problem that leaves you fatigued, sleepy and irritable.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Obstructive sleep apnea
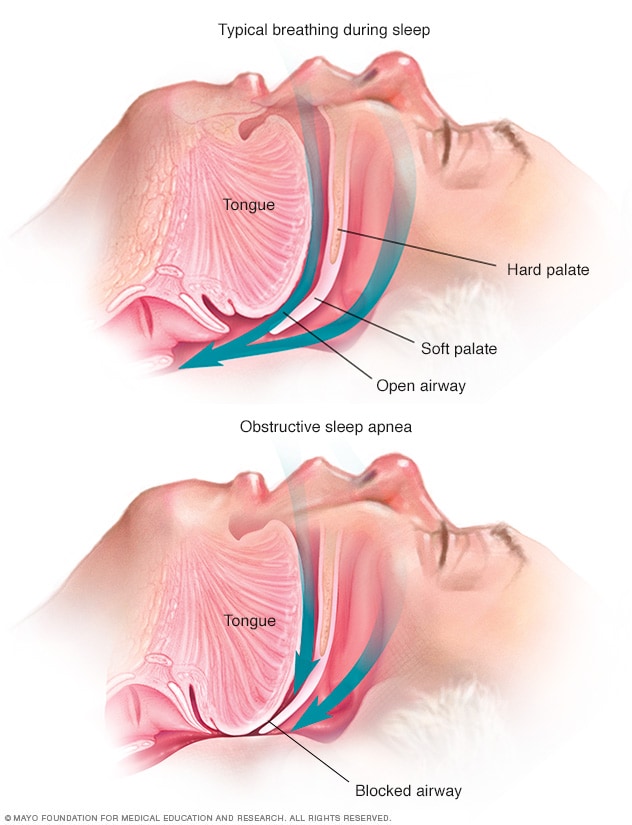
Obstructive sleep apnea occurs when the muscles that support the soft tissues in your throat, such as your tongue and soft palate, temporarily relax. When these muscles relax, your airway is narrowed or closed, and breathing is momentarily cut off.
This type of sleep apnea happens when the muscles in the back of the throat relax. These muscles support the soft palate, the triangular piece of tissue hanging from the soft palate called the uvula, the tonsils, the side walls of the throat and the tongue.
When the muscles relax, your airway narrows or closes as you breathe in. You can't get enough air, which can lower the oxygen level in your blood. Your brain senses that you can't breathe, and briefly wakes you so that you can reopen your airway. This awakening is usually so brief that you don't remember it.
You might snort, choke or gasp. This pattern can repeat itself 5 to 30 times or more each hour, all night. This makes it hard to reach the deep, restful phases of sleep.
Central sleep apnea
This less common form of sleep apnea occurs when your brain fails to send signals to your breathing muscles. This means that you make no effort to breathe for a short period. You might awaken with shortness of breath or have a difficult time getting to sleep or staying asleep.
Risk factors
Sleep apnea can affect anyone, even children. But certain factors increase your risk.
Factors that increase the risk of this form of sleep apnea include:
- Excess weight. Obesity greatly increases the risk of OSA . Fat deposits around your upper airway can obstruct your breathing.
- Neck circumference. People with thicker necks might have narrower airways.
- A narrowed airway. You might have inherited a narrow throat. Tonsils or adenoids also can enlarge and block the airway, particularly in children.
- Being male. Men are 2 to 3 times more likely to have sleep apnea than are women. However, women increase their risk if they're overweight or if they've gone through menopause.
- Being older. Sleep apnea occurs significantly more often in older adults.
- Family history. Having family members with sleep apnea might increase your risk.
- Use of alcohol, sedatives or tranquilizers. These substances relax the muscles in your throat, which can worsen obstructive sleep apnea.
- Smoking. Smokers are three times more likely to have obstructive sleep apnea than are people who've never smoked. Smoking can increase the amount of inflammation and fluid retention in the upper airway.
- Nasal congestion. If you have trouble breathing through your nose — whether from an anatomical problem or allergies — you're more likely to develop obstructive sleep apnea.
- Medical conditions. Congestive heart failure, high blood pressure and type 2 diabetes are some of the conditions that may increase the risk of obstructive sleep apnea. Polycystic ovary syndrome, hormonal disorders, prior stroke and chronic lung diseases such as asthma also can increase risk.
Risk factors for this form of sleep apnea include:
- Being older. Middle-aged and older people have a higher risk of central sleep apnea.
- Being male. Central sleep apnea is more common in men than it is in women.
- Heart disorders. Having congestive heart failure increases the risk.
- Using narcotic pain medicines. Opioid medicines, especially long-acting ones such as methadone, increase the risk of central sleep apnea.
- Stroke. Having had a stroke increases the risk of central sleep apnea.
Complications
Sleep apnea is a serious medical condition. Complications of OSA can include:
Daytime fatigue. The repeated awakenings associated with sleep apnea make typical, restorative sleep impossible, in turn making severe daytime drowsiness, fatigue and irritability likely.
You might have trouble concentrating and find yourself falling asleep at work, while watching TV or even when driving. People with sleep apnea have an increased risk of motor vehicle and workplace accidents.
You might also feel quick-tempered, moody or depressed. Children and adolescents with sleep apnea might perform poorly in school or have behavior problems.
High blood pressure or heart problems. Sudden drops in blood oxygen levels that occur during OSA increase blood pressure and strain the cardiovascular system. Having OSA increases your risk of high blood pressure, also known as hypertension.
OSA might also increase your risk of recurrent heart attack, stroke and irregular heartbeats, such as atrial fibrillation. If you have heart disease, multiple episodes of low blood oxygen (hypoxia or hypoxemia) can lead to sudden death from an irregular heartbeat.
- Type 2 diabetes. Having sleep apnea increases your risk of developing insulin resistance and type 2 diabetes.
- Metabolic syndrome. This disorder, which includes high blood pressure, abnormal cholesterol levels, high blood sugar and an increased waist circumference, is linked to a higher risk of heart disease.
Complications with medicines and surgery. Obstructive sleep apnea is also a concern with certain medicines and general anesthesia. People with sleep apnea might be more likely to have complications after major surgery because they're prone to breathing problems, especially when sedated and lying on their backs.
Before you have surgery, tell your doctor about your sleep apnea and how it's being treated.
- Liver problems. People with sleep apnea are more likely to have irregular results on liver function tests, and their livers are more likely to show signs of scarring, known as nonalcoholic fatty liver disease.
- Sleep-deprived partners. Loud snoring can keep anyone who sleeps nearby from getting good rest. It's common for a partner to have to go to another room, or even to another floor of the house, to be able to sleep.
Complications of CSA can include:
Fatigue. The repeated awakening associated with sleep apnea makes typical, restorative sleep impossible. People with central sleep apnea often have severe fatigue, daytime drowsiness and irritability.
You might have difficulty concentrating and find yourself falling asleep at work, while watching television or even while driving.
Cardiovascular problems. Sudden drops in blood oxygen levels that occur during central sleep apnea can adversely affect heart health.
If there's underlying heart disease, these repeated multiple episodes of low blood oxygen — known as hypoxia or hypoxemia — worsen prognosis and increase the risk of irregular heart rhythms.
- Kline LR. Clinical presentation and diagnosis of obstructive sleep apnea in adults. https://www.uptodate.com/contents/search. Accessed June 28, 2022.
- Selim BJ, et al. The association of nocturnal cardiac arrhythmias and sleep-disordered breathing: The DREAM study. Journal of Clinical Sleep Medicine. 2016; doi:10.5664/jcsm.5880.
- Jameson JL, et al., eds. Sleep apnea. In: Harrison's Principles of Internal Medicine. 21st ed. McGraw-Hill; 2022. https://accessmedicine.mhmedical.com. Accessed June 28, 2022.
- Sleep apnea. National Heart, Lung, and Blood Institute. http://www.nhlbi.nih.gov/health/health-topics/topics/sleepapnea/. Accessed June 28, 2022.
- Badr MS. Central sleep apnea: Risk factors, clinical presentation, and diagnosis. https://www.uptodate.com/contents/search. Accessed June 28, 2022.
- Kryger MH, et al. Management of obstructive sleep apnea in adults. https://www.uptodate.com/contents/search. Accessed June 28, 2022.
- Aurora RN, et al. Practice parameters for the surgical modification of the upper airway for obstructive sleep apnea in adults. Sleep. 2010; doi:10.1093/sleep/33.10.1408.
- Amali A, et al. A comparison of uvulopalatopharyngoplasty and modified radiofrequency tissue ablation in mild to moderate obstructive sleep apnea: A randomized clinical trial. Journal of Clinical Sleep Medicine. 2017; doi:10.5664/jcsm.6730.
- Parthasarathy S. Treatment-emergent central sleep apnea. https://www.uptodate.com/contents/search. Accessed June 29, 2022.
- Mehra R. Sleep apnea and the heart. Cleveland Clinic Journal of Medicine. 2019; doi:10.3949/ccjm.86.s1.03.
- Badr MS. Central sleep apnea: Treatment. https://www.uptodate.com/contents/search. Accessed July 1, 2022.
- Olson EJ (expert opinion). Mayo Clinic. June 30, 2022.
- Continuous positive airway pressure (CPAP)
- CPAP machines: Tips for avoiding 10 common problems
- CPAP: How it works
- Which CPAP masks are best for you?
Associated Procedures
- Endoscopic sleeve gastroplasty
- Polysomnography (sleep study)
- Septoplasty
- Tonsillectomy
- Tracheostomy
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
We’re transforming healthcare
Make a gift now and help create new and better solutions for more than 1.3 million patients who turn to Mayo Clinic each year.

These seven tips can help you spend less time on charting.
COLLEEN T. FOGARTY, MD, MSc
Fam Pract Manag. 2016;23(2):40
Author disclosure: no relevant financial affiliations disclosed.
In the age of paper charts, physicians' notes were as quick to produce as their scribbled handwriting, and just as legible. Now that we have electronic health records (EHRs) and documentation guidelines, many physicians struggle to complete their notes in a timely manner.
Here are some charting tips (for those of us without scribes or dictation systems) that I've gleaned from years of practicing medicine and coaching residents and fellows.
1. Leverage the skills of your team members . You don't have to document everything yourself. For example, the medical assistant or nurse on your team can document the patient's concerns, review medications, and verify or document allergies. You can then quickly review the information for accuracy and sign off on the note.
2. Get done what you can in the room . When talking with a patient about his or her history or treatment plan, make notes as you go, summarizing aloud to engage the patient and ensure understanding. You can even complete electronic prescriptions in the exam room so the patient knows they have been sent and you don't have that work waiting for later.
3. Know the E/M documentation guidelines . A 99213 level of service does not require a comprehensive review of systems or a comprehensive exam. Document what's medically necessary and complete for today's visit, and no more. (For more information, see the FPM Documentation Guidelines topic collection .)
4. Use your basic EHR functions . Templates and the copy and paste functions are helpful for routine visits where clinical queries are standard, but use them judiciously. “Today's note” should accurately reflect the patient's condition today and your impression today, so make sure to modify any templates or copied material to reflect this. In complex or changing situations, it may be faster and more accurate to avoid such features. But if it's flu season and you don't have a functioning influenza vaccine template, take 90 seconds to create one, and save yourself time down the road. In addition, use the relevant “data bucket” when appropriate. For example, if you have just obtained an element of social history that you want to use for future visits, place that in the “social history” area of the chart so that it can be carried forward and reviewed on future visits, thus saving you documentation time later. Once you've mastered these basic EHR features, continue to learn about your EHR functions. Most systems can do many more automated tasks than any one person knows, so talk to others and share tips.
5. Let go of perfection . The EHR can be a minefield for perfectionists and compulsive “box-checkers.” Again, remember the documentation guidelines. Not all boxes need checking, and not all categories need filling on every visit. Know which ones do, and leave the rest alone.
6. Forget the “opus.” The clinical note serves as neither biography nor ethnography. Be brief and focused. In the plan section of the note, be clear and concise enough that the next person looking at your note will be able to understand your clinical reasoning and follow the plan.
7. Time yourself . Using your smartphone or watch, see how long it takes you to complete a note. Then set a goal to decrease this. With residents, I suggest a goal of 5 minutes or less per note. However, this is far too long for most practicing clinicians because we would spend an hour documenting for every 12 patients seen. Set your own goals, and work to achieve them.
Of course, speed should not be our only goal. With new or complex patients, spending more time on documentation may be time well spent. These tips are designed to help you get through the majority of your routine documentation more efficiently, freeing you to work on other tasks – or go home earlier.
WE WANT TO HEAR FROM YOU
The opinions expressed here do not necessarily represent those of FPM or our publisher, the American Academy of Family Physicians. We encourage you to share your views. Send comments to [email protected] , or add your comments below.
Continue Reading

More in FPM
More in pubmed.
Copyright © 2016 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
Visiting Student Learning Opportunities™ (VSLO®)
New section, vslo® sign-in.
Search for and apply to opportunities in the VSLO® system.
The AAMC Visiting Student Learning Opportunities ™ (VSLO ® ) program enables medical and public health students to pursue short-term learning opportunities in locations away from their Home institutions. These elective opportunities include observerships, summer research programs, clinical opportunities, away rotations, away electives, clinical rotations, and visiting opportunities. Offered by participating Host institutions in the U.S. and around the world, elective opportunities are available in teaching hospitals, community clinics, and urban or rural sites and are open to preclinical, clinical, or final-year students, as determined by the Host institution.
If you are new to the VSLO program, start by familiarizing yourself with the resources below. If you are ready to begin the application process, login to the VSLO application service by clicking the VSLO® Sign-In button above. The VSLO program is only accessible to students at participating Home institutions. It’s easy for your school to join the VSLO program .
Mon. - Fri. 8 a.m. - 6 p.m. ET
Begin Your Away Rotation Journey with the VSLO Program

VSLO® News and Announcements
The VSLO team regularly updates resources, data, research, and the VSLO application service to meet the changing needs of the medical education community.


IMAGES
VIDEO
COMMENTS
The concept of shared clinical visit notes is not new. Individual physicians and organizations started exploring the potential of transparency in clinical records in the 1970s.1 The first efforts to study the impact of shared visit notes on physicians and patients began in 2010—and thus, the OpenNotes movement was born. The movement started ...
The clinical notes can come with surprises. Patients may be amused to find out they're described by their physician as "well-nourished," "well-groomed," "pleasant" or "normal ...
When doctors share visit notes with patients: a study of patient and doctor perceptions of documentation errors, safety opportunities and the patient-doctor relationship. BMJ Qual Saf . 2016;.
Shared medical visit notes are notes written by clinicians that are made available ("open") to patients in electronic health records. Clinicians add medical notes to a patient's electronic health record following clinical encounters such as office visits. There is no difference between the notes that patients can view and those that ...
Step 1: Total time. Think time first. If your total time spent on a visit appropriately credits you for level 3, 4, or 5 work, then document that time, code the visit, and be done with it. But if ...
1. Be consistent and transparent. What you put in the note should reflect your communication in the office. There should be no surprises. 2. Minimize jargon and abbreviations that patients might ...
Starting in April 2021, all medical practices will be required to provide patients free access to their medical records. The concept of sharing medical notes is known as OpenNotes. Under the 21st Century Cures Act, consumers will be able to read notes that recap a visit to the doctor's office as well as look at test results electronically.
NPP flags specific visit notes. The NPP can identify and route visit note (s) to the supervising physician for review and/or sign off using the office message feature in Elation. To do so: The NPP locates a signed visit note in the patient's chart. The NPP clicks "Actions" >> "Send: Office Message" at the top of the visit note.
The notes can help with recall following medical visits, particularly for older patients who have multiple chronic conditions that require much to be covered in a short office visit, Martin says ...
How to Document a Shared Visit. When documenting a shared/split visit, each provider sign and date their own portion of the visit. Additionally, each provider's documentation should: Identify both the physician and the NPP involved in the patient care at that encounter. Link the physician's notes to the NPP's notes.
The physician visit note is many things to many people. To the patient, they contain their personal health story. To the clinicians who create them, they are the result of hours of work, day after day, year after year. To the clinic, they become legal documents that must be preserved for years. They are filled with fancy words, often with a ...
Outpatient SOAP Notes. In the outpatient clinic, SOAP is the traditional note structure: S ubjective, O bjective, A ssessment, P lan. Although electronic health records may structure notes differently, this is still the information that you would enter at a problem focused or chronic disease management visit. You may see some providers move the ...
If you are reviewing records that used those guidelines (office visits before 2021, other E/M before 2023) this is relevant to those services. Summary of changes described in this article. In 2018, CMS changed the requirements for using medical student E/M notes by the attending physician.
The billing provider should submit the requested documentation because they're the enity whose payment CERT reviews. We pay for necessary services, but patient medical record documentation must show their medical necessity. Instruct medical record staf and third-party medical record copy services to provide all records that support payment.
November 15, 2022. You may not be aware of this, but you can read everything that your doctor writes about you. Go to your patient portal online, click around until you land on notes from your ...
Learn more about how to go to the doctor and make the most of your time with a few simple steps. 1. Get organized before your doctor visit. Before you go to the doctor, take some time to think about important questions you may have about your health. Most people only visit the doctor a few times a year, so it's important to make your time count!
The clinical notes can come with surprises. Patients may be amused to find out they're described by their physician as "well-nourished," "well-groomed," "pleasant" or "normal ...
Chimowitz H, Fernandez L. Sharing visit notes: getting patients and physicians on the same page. Fam Pract Manag. 2016;23(6):10-13.
6. Time yourself. Use a timer on your smartphone or watch to see how long it takes to complete a note. Knowing your baseline, set a goal to decrease your per-patient documentation time. Speed shouldn't be your only goal, and spending more time documenting visits with new or complex patients may be valuable.
Medical Records staff are available Monday through Friday from 8:30 am to 5:00 pm. Suburban HospitalMedical Records 8600 Old Georgetown Rd. Bethesda, MD 20814 Health Information Management: 301-896-3777 Fax: 301-896-7352. If you have any questions about how to request a patient's records, please call 301-896-3777.
2. Materials and Methods. This project includes a participatory approach to develop a Patients' Guide for Doctor's Visit (DocVISITguide) (phase 1) and its first small-scale evaluation (phase 2) following a sequential explanatory mixed methods design [].The development of the DocVISITguide included (a) a literature and internet search, (b) feedback from patients and professional experts and ...
The national average for family physicians' usage of the level 4 code (99214) is slowly increasing and is approaching 50% of established patient office visits (it's now above 50% for our Medicare ...
From changing guidelines about when to start getting mammograms to understanding the different types of annual visits to schedule with your primary care doctor, navigating medical care can be complicated.. If you are on Medicare, it's important to understand these nuances, especially the difference between a physical exam and an annual wellness visit.
Medical conditions. Congestive heart failure, high blood pressure and type 2 diabetes are some of the conditions that may increase the risk of obstructive sleep apnea. Polycystic ovary syndrome, hormonal disorders, prior stroke and chronic lung diseases such as asthma also can increase risk. Central sleep apnea
6. Forget the "opus.". The clinical note serves as neither biography nor ethnography. Be brief and focused. In the plan section of the note, be clear and concise enough that the next person ...
The AAMC Visiting Student Learning Opportunities ™ (VSLO ®) program enables medical and public health students to pursue short-term learning opportunities in locations away from their Home institutions.These elective opportunities include observerships, summer research programs, clinical opportunities, away rotations, away electives, clinical rotations, and visiting opportunities.