

Vagus nerve compression in the neck: Symptoms and treatments
Ross Hauser, MD
The vagus nerve plays a key role in regulating many of our body’s functions. Its name best describes its physical characteristics, Vagus is Latin for “fugitive,” or “wanderer.” It is the longest and most widely extended of the nerves of the body. The vagus nerves keep us alive by their innervation (nervous system function) of the internal organs of the body and their interactions with the brain, spinal cord, cranial nerves, upper cervical spinal nerves, and sympathetic nervous system.
Sensory functions of the vagus nerve are critical for conscious perception and for monitoring visceral functions in the cardiopulmonary and gastrointestinal systems. As such the vagus nerve has a critical role in the maintenance of bodily homeostasis (balance) in diverse functions relating to digestion, satiety, respiration, blood pressure, and heart rate control. Its profound role is illustrated by abnormalities in it that can lead to far-reaching consequences including gastroesophageal reflux disease, heart failure, failure of respiratory control, gastroparesis, vasovagal syncope, and chronic pain.
The interconnectedness of the vagus nerve and other nerves helps patients and doctors understand mysterious and bizarre symptoms. For instance, a woman says that when she puts her contact lenses in, will often have horrible stomach pain. Some doctors may attribute this to psychiatric factors. Is it? Does she need a psychiatrist? For doctors, understanding the neurology of the vagus nerve may discover that this is an exaggerated oculo-emetic (eye reflex) and oculocardiac (the reduction in heart rate when pressure is exerted on the eye) reflex. Because there is a connection between the trigeminal nerve and the vagus nerve, any stimulation of the trigeminal nerve (pressure on the eyeball) can stimulate the vagus nerve.
Likewise, the patient that said every time she “poops I get a headache.” The act of defecation stimulates the vagus nerve and this in turn can cause the firing of the trigeminal nerve and give facial pain or headache. The trigeminal-vagus nerve connection explains a lot of episymptoms.

The vagus nerve seems to extend everywhere; consider: the supradiaphragmatic vagus nerve innervates the skin of the external acoustic meatus (auricular branch) and the dura of the posterior cranial fossa (meningeal branch), larynx, pharynx, and upper esophagus (pharyngeal branches), aortic arch (cervical cardiac branches), trachea and esophagus (recurrent laryngeal), lungs and heart. The right vagus nerve (more so than the left) innervates the SA node and the AV node of the heart. (This is why vagus nerve stimulators are placed on the left side). The subdiaphragmatic vagus nerve innervates the liver, pylorus, antrum, pancreas, intestine, and stomach. Efferent vagus branches reach the uterus, adrenal gland, and gallbladder. Vagus nerve fibers innervate the thymus and travel to abdominal adipose tissue. The vagus nerve has many branches that interact with the enteric nervous system and provide central coordination of everything related to the digestive tract, including sensation, absorption, motility, and even sphincter control.
The vagus nerve is a 2-way messenger network, passing messages and signals between the organs and brain to maintain heart rate, blood pressure, circulation, breathing, internal organ distension (for example the moving of food through the digestive system ), secretions, and inflammation. As we will see below the vagus nerve helps us talk, swallow, focus vision, hear, and understand. The vagus nerve also sends out messages as part of the parasympathetic nervous system that “calms down” the body after physical exertion or in response to stress in a “fight or flight” situation.
The caption reads: Upper cervical instability is the structural cause of vagus nerve destruction at the nodose ganglion (nerve center).

Article summary
In this article, I will briefly discuss an incredible number of symptoms and conditions in the human body that can be caused by disruption of and interference of the vagus nerve signals. I will also provide more detailed information on each disorder and symptom through links to companion articles on this website.
I will also focus on one mechanism by which vagus nerve dysfunction can be altered. That is through the mechanism of cervicovagopathy. Cervico – a structural problem in the neck that is causing “vago” vagus nerve “pathy” or disease or illness. See my article Cervical Myelopathy – Cervical Degenerative Disc Disease – Cervicovagopathy . Cervicovagopathy is then the neck’s altered or broken structure causing compression or disease on the vagus nerve and then on to produce a myriad of:
- See related article: Vagus Nerve related Cervical Dysphagia and Laryngeal – Laryngotracheal stenosis
- See related article: Glossopharyngeal and Vagoglossopharyngeal neuralgia
- See related article: Cranial Neuralgias – Symptoms of pain, smell, vision, hearing, taste, and talking
- See related article: Brachioradial Pruritus – Neuropathic itch
- See related article: Cervical Spine Instability and Potential Effects on Brain Physiology
- See related article: Neurologic-like symptoms and conditions of Cervical Spine Instability
- See related article: Treating neurologic-like symptoms by addressing cervical spine instability and disrupted blood flow into the brain
- See related article: Neurologic, digestive, cardiac, and bladder disorders: Some of the symptoms of Autonomic nervous system dysfunction and treatment options.
- See related article: Emotional stress: Anxiety, Depression and Panic Attacks: A neurologic and psychiatric like condition caused by cervical spine instability
- See related article: Can cervical spine instability cause cardiovascular-like attacks, heart palpitations, and blood pressure problems?
- See related article: Inappropriate sinus tachycardia – Elevated heart rate and the vagus nerve
- See related article: Pyloric stenosis in the adult patient: A problem of Vagus nerve impingement?
- See related article: Treating Vertebrobasilar insufficiency, vertebrobasilar artery insufficiency, rotational vertebral artery occlusion syndrome, or Bow Hunter Syndrome
- See related article: Cervical Angina
- See related article: SIBO: Small intestinal bacterial overgrowth and the Vagus nerve. The problem of nerve compression .
- See related article: How neck pain and cervical spine instability cause nausea, gastroparesis, and other digestive problems
- See related article: Cervical spine instability and digestive disorders: Indigestion and irritable bowel syndrome caused by cervical spondylosis
- See related article: Achalasia: A vagus nerve disorder and its connection to the neck
- See related article: Hiccups, Cough, Neck Pain, and Vagus and Phrenic Nerve Injury
- See related article: Cluster headache treatment – cervical ligament instability and the trigeminal and vagus nerves
- See related article: Mast cell activation syndrome and the vagus nerve
- See related article: Cervical spine problems, Vagus nerve compression, urinary incontinence
- See related article: Postural Orthostatic Tachycardia Syndrome (POTS), the Vagus Nerve and Cervical Spine instability
- See related article: Chronic Cough, Cough Hypersensitivity Syndrome, and the Vagus Nerve
In many patients, we can help identify this myriad of symptoms as either structural and/or systemic disease causes.
A very complex medical history
As described above, have seen many patients who have a very complex medical history. In some cases, they would describe a dozen or more disorders. The patient will tell us that if they had gastrointestinal distress, the gastrointestinal specialist treated them. If they had cardiovascular-type symptoms, a slow or racing heartbeat for example, or spells of passing out, they were referred to the heart specialist. For problems with hearing or tinnitus they were sent to the otologist, problems with vision would send them to the ophthalmologist, skin problems were seen by the dermatologist, urinary problems by the urologists, etc. Sometimes a psychiatrist would often be referred.
Sometimes the psychiatrist would be the last referral because the patient has started a process of denial. Not because they denied they had all these things wrong with them, but because they started to deny that the treatments they were getting were in fact getting anywhere. These people would summarize the above experiences as years of each disorder being treated as its own cause and effect, in isolation, with symptomatic treatment. Rarely were all these problems that these people addressed through a singular cause.
Intuitively patients knew that “something had to be at the bottom of all this.” Somehow dizziness, digestive problems, ringing in the ears, blurry vision, itching, poor body temperature control, brain fog, choking sensations, depression, anxiety, inability to focus and other symptoms had to somehow all be related.
As mentioned above and to reiterate: The vagus nerve supplies every organ from the neck down to the transverse colon (except adrenal glands), including the heart, lungs, stomach, small intestine, gallbladder, liver, spleen, one kidney, and some of the colon. It is involved with speech, swallowing, some taste perception, and some tissues in the throat, neck, and even part of the ear. Stress raises the body’s level of epinephrine and norepinephrine, which stimulates the sympathetic nervous system to override the parasympathetic nervous system, of which the vagus nerve is the main component. So most people’s normal lives are characterized by an under-active vagus nerve, which becomes worse when rotatory atlantoaxial instability or other forms of cervical instability, disrupt vagus nerve impulses. Since the vagus nerve runs very close to the C1-C3 vertebrae, can easily be affected by upper cervical malrotations from instability.
The vagus nerve could be called the nervous systems commander-in-chief in the field, monitoring all the important systems of the body including inflammation, heart rate variability, digestion, bowel movements (flow of food through the digestive tract), breathing, thinking, feeling, hunger, satiety, and hormone secretion. There is a drastic difference in how the body functions between someone with increased vagal tone (health) and decreased vagal tone (disease). Let’s get to the clinical and research aspects of this article.
Sensory functions of the vagus nerve
The vagus network.
In the neck, the vagus nerve connects to the inferior, middle, and superior cervical sympathetic ganglion (SCSG), as well as the upper cervical nerves and many of the cranial nerves, and descends all the way down to the celiac plexus, the nerves that innervate the abdomen.
Vagus nerve compression from disease
Vagus nerve compression can occur in the carotid spaces not just from dysstructure of the cervical spine but also from space-occupying lesions. For instance, paragangliomas, schwannoma, or neurofibromas at the jugular foramen or at the ganglion nodosum (at the level of the C1 lateral mass) can compress the vagus nerve giving symptoms of dysphagia, hoarseness, vocal cord paralysis, pulsatile tinnitus, hearing loss or vertigo. ( 1 ) For this reason it is important for a person with vagopathy (vagus nerve dysfunction) to get high-resolution magnetic resonance imaging of the neural and ligament anatomy of the neck, especially in the craniocervical junction. MRI is the gold standard technique in the study of the cranial nerves. Most MRIs that are done on people’s necks, do not have the resolution that is needed to see adequately the small structures (in the order of 1-3mm) such as the transverse and alar ligaments, sympathetic ganglion and cranial nerves such as the vagus and glossopharyngeal.
The vagus nerve, the inferior cervical sympathetic ganglion, and cardiovascular-like problems, breathing, and thyroid dysfunction.
The inferior cervical sympathetic ganglion is a nerve complex located between the C7 and the top rib. Messages between the vagus nerve and inferior cervical sympathetic ganglion influence blood flow between the heart, brain, and neck.
Altered messages between the vagus nerve and the inferior cervical sympathetic ganglion can impact the function of the following:
- Subclavian arteries supply blood to the thorax, head, neck, shoulder, and arms.
Fainting, loss of blood flow to the brain:
- Subclavian arteries branch off into the vertebral artery which supplies blood to the back of the brain through the basilar, posterior cerebral, and cerebellar arteries. Dysfunction can cause blackouts, fainting, and vascular problems.
- The vagus nerve connects to the external laryngeal nerves which act upon the inferior thyroid artery.
Symptom: Cardiovascular risks and Cardiovascular risks linked to hypothyroidism.
The thyroid receives its nerve supply mainly from the middle cervical ganglion but also is innervated by the superior and inferior cervical ganglions.
A study published in the North American Journal of Medical Sciences ( 2 ) investigated the link between sympathovagal imbalance (Sympathovagal imbalance is the disruption and dysfunction in which the sympathetic and vagal components of the autonomic nervous system run either too high or too low. In other words, too much “flight-fight” or too little problems with energy, fatigue, and digestion among many symptoms) to cardiovascular risks and the plausible mechanisms of cardiovascular risks in hypothyroidism. What the researchers suggested was Sympathovagal imbalance could be implicated in:
- Increased diastolic pressure (the bottom number of a blood pressure reading).
- Decreased HRV (Heart rate variable) and increased low-frequency to high-frequency ratio (LF-HF) of HRV.
- Dyslipidemia (Cholesterol problems).
- Increased high-sensitive C-reactive protein (inflammation)
All these symptoms were observed in hypothyroid patients and all these parameters had a significant correlation with the heart rate variability. Sympathovagal imbalance due to sympathetic activation and vagal withdrawal occurs in hypothyroidism.
A February 2018 study in the journal Biomed Central Research ( 3 ) notes examined the effect of propranolol (blood pressure medication) on heart rate variability (HRV) in hyperthyroidism before antithyroid treatment. This was a before-and-after study, on ten patients presenting overt hyperthyroidism who had no previous treatment.
HRV parameters including sympathovagal balance estimate by low-frequency to high-frequency ratio (LF-HF) ratio remained unchanged. Although a significant reduction in heart excitability, propanolol failed to restore a good sympathovagal balance in hyperthyroidism.
Various surgeries and the vagus nerve
Neurosurgeons, orthopedic Surgeons, and Ear Nose, and Throat surgeons who operate on the anterior neck and base of the skull are keenly aware of the vagus nerve. These surgeries including thyroid surgery, carotid endarterectomy, anterior cervical fusion and base of skull operations stretch the vagus nerve. Recurrent laryngeal nerve stretch injury is an ever-present problem for them because of the operations they do. Mechanisms of injury include traction injuries from retractors, clamping injuries, interruption of neurovascular supply, compression injury, sharp dissection, electrosurgery and even stretch from intubation. Pathophysiology of injury is thermal damage, stretch, cutting, compression, and vascular compromise.
In my practice, we have seen patients where overextension of the neck occurred not only in surgery, or a simple diagnostic procedure such as endoscopy or laryngoscopy but also with a simple dental examination or procedure, going to a beauty salon and the washing of your hair.
The experience and research on nerve physiology give insight into how fragility of the vagus nerve. Studies thus have been done to try to elicit why there are so many nerve (including vagal) injuries during anterior neck surgeries and show ( 4 )
- For surgical exposures (retraction) the recurrent laryngeal nerve is at 13% to 44% stretch
- 6% for one hour shows a 70% action potential amplitude decrease
- 12% stretch for one hour blocks action potential completely
- 15% stretch causes complete intraneural ischemia
- 50 grams of tension for 5 minutes causes a significant loss of function
A March 2024 study ( 5 ) in the journal Annals of Surgical Oncology describes a group of 85 patients who had developed left recurrent laryngeal nerve palsy after minimally invasive McKeown esophagectomy.
- Patients who did not fully recover were seen to be smokers
- or it was the surgical approach identified as a key cause of complication.
A March 2022 study in the Plastic and Reconstructive Surgery Global Open ( 6 ) discusses surgical injury. “Iatrogenic glossopharyngeal nerve injuries are commonly associated with procedures such as a tonsillectomy, carotid endarterectomy, and endotracheal intubation.” In this case report, doctors present a previously unreported complication of a thread lift procedure (cosmetic procedure) in the jowl region, causing damage to the glossopharyngeal nerve through compression. The glossopharyngeal nerve because of its connection to the vagus nerve, may cause cardiovascular complications associated with the vagus nerve.”
The connection to neck pain and a history of cervical spine surgery and injury.
Many of the people that we see in our practice have been on a long medical journey as described above. They are at our center because a connection between neck pain and neck injury has been made. There is a suspicion that a structural cause, that is cervical instability, or floating vertebrae or neck bones, is the cause of the compression on the vagus nerve and a condition of Cervicovagopathy. This would be seen in patients with a medical history of post-concussion syndrome , Whiplash Associated Disorder , cervical spine fusion or cervical spine laminectomy , and hypermobility Ehlers-Danlos Syndrome.
How does one come to a condition of Cervicovagopathy or wandering floating neck bones? This condition is caused by weakened, loose, and damaged cervical spine ligaments. Ligaments are the soft-tissue structure that holds the vertebrae in place. When these ligaments no longer hold the vertebrae in place the structure of the neck falters and the natural curve of the cervical spine is lost. This condition is described in the image below.
The caption reads Cervical degenerative dysstructure: The progressive nature of cervical instability that leads to a breakdown of the cervical curve resulting in destructive forces (compression, grinding, and impingement of blood vessels and nerves) being placed on vital neurovascular structures including the cervical spinal cord and vagus nerves.
To the left, we see:
- NORMAL posture.
- MILD cervical spine instability, the head is moving forward causing a mild stretch of the nerves and blood vessels. When blood vessels are stretched, the vessels narrow.
- MILITARY Neck: This condition is called a military neck because the neck is standing up straight. This is not a good thing. The spine acts as a shock absorber and is built like a spring with a curve to it.
- KYPHOTIC. The cervical spine instability has become so severe, that the curve of the neck has reversed itself and is now backward.
This all occurs because of damage to the cervical spine ligaments that hold the bones in proper alignment.

Treatment for loss of natural neck curve structure is directed to improve the structural integrity of the cervical spine and the symptoms and conditions it causes, including cervicovagopathy and increased intracranial pressure. Treatment modalities can include dynamic (chiropractic) ortho-neurological adjustments for the vertebral subluxations (malrotations), curve correction to restore lordosis, and Prolotherapy to repair injured ligaments. The diagnostic tests used to discover cervical instability and resultant pathophysiology can also be used to monitor progress during treatment. These treatment options are discussed below.
Please see our article on treatments for Atlas displacement c1 forward misalignment .
The etiology of the cause of vagal or parasympathetic dysfunction has many chemical and emotional etiologies
The etiology of the cause of vagal or parasympathetic dysfunction has many chemical and emotional etiologies, including diabetes, heavy metals, medications, and emotional or financial stress, but a cause that is overlooked is structural injury. As the list of symptoms and diseases, including chronic pain, depression, tinnitus, migraine headache, seizures, heart failure, Alzheimer’s dementia, and systemic inflammation continues to grow, it is prudent that clinicians and the patients they treat understand the vagus nerve anatomy, injury, and the pathophysiology it causes.
External laryngeal nerves – voice, breathing, swallowing problems
- The plexus (bundle of nerves and blood vessels) on the inferior thyroid artery talks with the recurrent and external laryngeal nerves, with the superior cardiac nerve, and with the plexus on the common carotid artery.
- Laryngeal nerve dysfunction can cause loss of voice, hoarseness, swallowing difficulties ,
- a sense of breathing obstruction.
The phrenic nerve – breathing, swallowing, and problems with hiccups
- The phrenic nerve sends messages through the thorax to assist in regulating breathing, and controlling the cough reflex, and the hiccup reflex. For a detailed discussion on the interaction between the phrenic nerve and the vagus nerve, please see my article Hiccups, Cough, Neck Pain, and Vagus and Phrenic Nerve Injury .
What are we seeing in this image?
This is the superior cervical sympathetic ganglion in its native habitat. Surrounded by blood vessels (internal carotid artery and internal jugular vein) and nerve networks and near the C2 vertebrae. When the vertebrae wander out of position, it takes these veins, arteries, nerves, and nerve bundles with it, causing compression and stretching of these vital structures. In the context of this article, this compression and stretching can not only cause pain but disrupt nerve signals causing cardiovascular-like symptoms and conditions already outlined in this article.

The vagus nerve has five main components contained within the nerve, which make up the five fascicles or nerve bundles seen in the vagus nerve cross-sections. (See figure). These are branchial motor, visceral sensory, visceral motor, and special and general sensory fibers. (See Figure). These five vagus nerve components can be summarized:
- Special visceral afferent (SVA, motor) – these motors are special because they supply motor innervation to skeletal muscles of branchial arch origin which include all the muscles of the pharynx, larynx, and soft palate.
- General visceral efferent (GVE, motor) – contains the parasympathetic motor part of the nerve that innervates the smooth muscles of the trachea, bronchi, and gastrointestinal tract and regulates heart rhythm. When we talk about the vagal tone we are talking about this part of the vagus nerve primarily. It is the part that slows the heart rate and is responsible for sinus arrhythmia with breathing.
- General visceral afferent (GVA, sensory) – general sensory to the abdominal viscera including the trachea, larynx, and esophagus digestive tract.
- Special visceral afferent (SVA, sensory) – taste sensation to the epiglottis and root of the tongue.
- General sensory afferent (GSA)– these fibers carry general sensation ( touch, pressure, pain, and temperature) from cutaneous structures and mucous membranes of the head, and general proprioception from somatic structures such as muscles, tendons, and joints of the head and neck. The trigeminal, facial, glossopharyngeal, and vagus nerves transmit GSA input to the spinal nucleus of the trigeminal nerve. One important innervation is to the skin of the external acoustic meatus, which is used for transcutaneous auricular vagus nerve stimulation.
Cervicovagopathy is defined as degeneration of the vagus nerve and/or interruption of vagal nerve impulses
The role of vagus nerve function in health and disease cannot be overemphasized. The hallmarks of dysautonomia (conditions and symptoms caused by problems with the autonomic nervous system (ANS))—parasympathetic dysfunction causing sympathetic dominance, or what is termed “sympathovagal imbalance”—are paramount to understanding the pathophysiology of most medical conditions. The role of sympathovagal imbalance, discussed briefly above will continue to be a dominating theme within this article.
Cervicovagopathy is defined as degeneration of the vagus nerve and/or interruption of vagal nerve impulses from the effects of damaged ligaments causing cervical instability, with or without significant cervical dysstructure or advanced cervical structural problems, leading to harmful effects on the body. Cervicovagopathy is one of the most devastating effects of cervical instability, upper cervical instability, and cervical dysstructure.
In the image below we see x-ray evidence of cervical spine misalignment, cervical dysstructure, and cervical spine instability.
- In the top panel, we see a misalignment of the C2.
- In the center panel, we see cervical dysstructure and a comparison of where a normal cervical curve should be and a significant curve structural problem causing the vertebrae to be displaced by 2 – 3 inches. The vagus nerve is associated with C1.
- In the lower panel, we see how far off-set the vertebrae are from each other and from C2-C6.

Now let’s re-examine the discussion we had above about Heart Rate Variable
Homeostasis of the human body is under the control of the autonomic nervous system (ANS); while the sympathetic nerve system (SNS) allows us to handle stress, the parasympathetic nervous system (PNS) allows us to live. As the vagus nerve is the primary sensory input and effector for the parasympathetic nervous system, its compromise has many long-ranging detrimental effects on human homeostasis and health.
When the autonomic nervous system (ANS) balance becomes sympathetic dominant, a rise in the LF/HF ratio is seen on Heart Rate Variable parameters. This rise in LF/HF ratio is frequently found in many chronic diseases, which brings up the hypothesis that the chronic symptoms these conditions produce may have as their etiology the breakdown of the cervical curve, affecting the precise balance between sympathetic and parasympathetic function—a condition known as dysautonomia. If this is true, then treatment should be directed at improving the cervical structure and stability to restore the body’s vagal tone.
“You may need the vagus nerve to understand the pathophysiology and to treat diseases.”
“You may need the vagus nerve to understand the pathophysiology and to treat diseases.” This is the title of a 2012 scientific article published in the journal Clinical Science ( 7 ) whose premise is, “Can different pathophysiological mechanisms and risk factors leading to various diseases be linked with altered nerve transmission of signals by one common pathway?”
The authors hypothesized that adequate vagal nerve activity reduces the risk of major diseases via common basic mechanisms and interim risk factors.
- There are 3 basic mechanisms that contribute to many chronic diseases, that is local oxidative stress and DNA damage, inflammatory reactions, and excessive sympathetic responses, all of which are inhibited by vagal nerve activity.
- Efferent vagal activity can be easily monitored noninvasively by measuring HRV.
- It is this interconnection between the vagus nerve and the whole body that allows vagus nerve stimulation to relieve chronic pain and reduce the number of cardiovascular-like, gastrointestinal-like, neurological-like, endocrine-like, and urinary-like disorders that we will discuss throughout this article.
As a side-note to this research, an October 2021 paper in the journal Public Library of Science One PLoS 1 ( 8 ) found that “Patients with COVID-19 present with a variety of clinical manifestations, ranging from mild or asymptomatic disease to severe illness and death. Whilst previous studies have clarified these and several other aspects of COVID-19, one of the ongoing challenges regarding COVID-19 is to determine which patients are at risk of adverse outcomes of COVID-19 infection. It is hypothesized that this is the result of insufficient inhibition of the immune response, with the vagus nerve being an important neuro-immuno-modulator of inflammation. Vagus nerve activity can be non-invasively indexed by heart-rate-variability (HRV).”
The researchers of this study found higher HRV predicts greater chances of survival, especially in patients aged 70 years and older with COVID-19, independent of major prognostic factors. Low HRV predicts ICU indication and admission in the first week after hospitalization.
This study above is an example of how vagus nerve disruption can cause a myriad of symptoms not only related to inflammation but the general well-being.
The image below offers an explanation as to how the vagus nerve impacts so many body functions.
The caption of the image reads: The vagus nerve origin in the brainstem: The vagus nerve exits and enters the medulla part of the brain stem and from there goes into the neck and into the body and up from there it goes into other parts of the brainstem and brain. The vagus nerves’ unique location at the main relay station of the body the craniocervical brainstem junction is why it has such a wide-ranging influence over how the body feels reacts and functions in both stressful situations and peaceful situations.

Of note in the above illustration to the right is the nodose ganglion. The vagus nerve facilitates messages back and forth from the brain to the heart. Afferents (messages in) go through the nodose ganglion (nerve bundle) which sits in front of the atlas (C1 vertebra). If the C1 vertebra is unstable and causes problems of “nerve pinching” this is how upper cervical instability can affect the heart rate variability. The C1 vertebrae would sit between the left and right sides Nodose Ganglion.
Location, location, location. Compression, compression, compression.
What are we seeing in this image? The superior cervical sympathetic ganglion is isolated so we can observe its proximity to the C2 vertebrae. Cervical instability that can lead to a “wandering” C1, C2, and C3 vertebrae will impact the proper nervous system function of the vagus nerve and the superior cervical sympathetic ganglion.

Compression and stretching of the vagus nerve in the neck
The vagus nerves are most vulnerable to stretch, traction or pull, and compression in the cervical region, as they lie in a specific space called the carotid space. The carotid space is a paired space defined by the carotid sheath, a connective tissue boundary in the neck that is made up of superficial, middle, and deep layers of the cervical fascia.
Carotid sheath compression
What are we seeing in this image? An ultrasound of the neck shows the three main structures in the carotid sheath. The internal jugular vein, the Vagus Nerve, and the carotid artery.

The carotid sheath encases the carotid artery, jugular vein, vagus nerve, and the sympathetic plexus of nerves. Instability of the cervical spine can cause compression on the carotid sheath due to its location. The cervical compression can cause arterial ischemia (inadequate blood flow to the brain) leading to drop attacks, brain fog, and other symptoms.
The vagus nerve and many other structures are vulnerable to injury here, especially at the craniocervical junction around the atlantoaxial joint, the most mobile and vulnerable of the spinal joints to injury.
Cervical instability-induced vagus nerve compression:
The most common structural condition that leads to poor vagus nerve function is upper cervical instability. (As we will discuss later in this article, we believe an effective treatment for cervical spine instability is Prolotherapy. An injection treatment to strengthen weak and cervical spine ligaments.)
In the four-panel illustration, panel A shows a far view of the nerves of the anatomy. In the B panel, a close-up lateral side view of the cervical spine and the interwoven nerve network. In C: Rotation and smashing or compression of the vagus nerve. In panel D the view from the bottom up.

The upper cervical segments are the most mobile, thus the “loosest” sections of the spinal column, and the most vulnerable to instability. When the atlantoaxial joint becomes unstable, muscles in both the anterior and posterior neck, including the longus colli, are recruited to help stabilize the joint. Please see my article and video on Upper cervical instability and Atlantoaxial instability symptoms including compression of the brainstem .
- Prolonged forward head posture causes flexion (forward bending) in the mid-lower cervical spine and extension (backward tilt of head) of the upper cervical (sub-occipital) spine, as well as shortened cervical flexors (muscle bundles)—which is another point of stretch for structures in the carotid sheath, including the vagus nerves.
- As the vagus nerves are interconnected to some of the most important nerve structures of the face, head, and brain, interruption of vagus inputs can result in wide-ranging detrimental consequences.
The Vagus nerve is the “sixth sense” the “gut feeling.”
The vagus nerve is our sixth sense and our “gut feeling.” Since the vagus nerve meanders and extends its branches to multiple tissues and organs, its role in health must be immense. It regulates homeostasis by connecting three interwoven systems: the nervous, endocrine, and immune systems. Brief demonstrations of this impact were given in some of the research citations above and will be demonstrated again below.
The exchange of information between the nervous, endocrine, and immune systems plays an important role in various physiological, as well as pathological, processes.
The Vagus nerve and its branches to other nerves
In the cervical region, the vagus nerve supplies branches to the:
- Facial nerve. The interaction of the two nerves controls facial expression and the taste sensation on the tongue
- The vagus nerve and glossopharyngeal nerve control the muscles of the throat. Dysfunction can cause swallowing difficulties.
- The nerves serve to help drain blood from the brain into the carotid sinus into the carotid artery in your neck. Dysfunction would cause brain drainage problems and high blood pressure problems.
- The nerves serve to sense fullness in the ear. Tinnitus and Meniere’s Disease may be a by-product of nerve dysfunction.
- The nerves serve to regulate the parotid (saliva) gland. Dysfunction can cause too much or too little or no saliva production.
- The Facial nerve was described above as providing a taste sensation in the tongue. It does this by regulating two-thirds of the tongue’s surface. The glossopharyngeal nerve helps you taste food in the back third of your tongue.
- Voice and swallowing dysfunction can occur if the vagus and glossopharyngeal nerve send distorted messages to the stylopharyngeus muscle which lifts the larynx out of the way when you are eating.
- The spinal accessory nerve. The nerve is responsible for muscle movement of the neck and shoulders.
- Trigeminal nerve. Cervical instability can also be responsible for almost all painful neuralgias of the head and face including occipital and trigeminal neuralgia, as well as structural headaches including tension, migraines, and clusters . A 2019 German study ( 9 ) wrote: “In patients with episodic cluster headache, successful transient therapy with transcutaneous stimulation of the vagus nerve may be required.”
- Hypoglossal nerves are the nerves that move your tongue.
The vagus nerve is mostly tied to the glossopharyngeal nerve, as they travel together down the carotid sheath and innervate the pharynx and esophagus. Irritation of these nerves can therefore lead to such horrific stabbing or lightning-like pharyngeal pain that it can make it hard to swallow and is associated with nausea and vomiting. The condition is called is vago-glossopharyngeal neuralgia. The attacks of pain are brought on by swallowing, talking, coughing, sneezing, touching the tragus of the ear, and turning the head or rolling toward the side of the pain.
Vascular compression is indicated in cervical spine instability.
A 2011 French study by Neurologists affiliated with the University of Lyon ( 10 ) evaluated the anatomy of the central myelin (the insulation that protects the nerves) portion and the central myelin-peripheral myelin transitional zone (the sensory and parasympathetic division of a nerve) of the trigeminal, facial, glossopharyngeal and vagus nerves.
The aim was also to investigate the relationship between the length and volume of the central myelin portion of these nerves with the incidences of the corresponding cranial dysfunctional syndromes caused by their compression to provide some more insights for a better understanding of mechanisms.
The researchers were looking at the damage caused by compression on these structures to help explain how such problems as Trigeminal Neuralgia, Peripheral and Central Facial Nerve Palsy (Side of and lower half muscle paralysis or weakness in the face), eye muscle problems such as headaches, eye strain, blurred vision, and double vision, floating eye or problems with eye movement.
The findings: “At present, it is rather well-established that primary trigeminal neuralgia, hemifacial spasm, and vago-glossopharyngeal neuralgia have as one of the main causes of vascular compression.”
Vascular compression would be the entanglement of these nerves and the blood vessels leading out of the brain and into the neck. Vascular compression is indicated in cervical spine instability.
Vascular compression not only compresses nerves it also wears away bone
I would like to offer a side note about vascular compression and how it can cause a great number of symptoms it does and to demonstrate that this is something seen by many doctors. In May 2014, doctors at the Hospital for Special Surgery published a case history ( 11 ) of a patient with a stretched-out vertebral artery that rubbed away and destroyed a portion of her C1-C2 facet complex and caused cervical instability resulting in a clinical presentation of severe occipital headache.
Such is the power of vascular compression.
The superior cervical sympathetic ganglion
In the neck specifically, there are direct communications between vagus nerves and the superior cervical sympathetic ganglion, glossopharyngeal nerves, spinal accessory nerves, and cervical spinal nerves #1, 2, 3, and 4. The most important of these communications is with the superior cervical sympathetic ganglion.
Above I touched on the role of these nerves and superior cervical sympathetic ganglion in symptoms and disease when they are in a state of dysfunction. Here I will go further in helping the understanding of the relationship between the vagus nerve and the superior cervical sympathetic ganglion.
The superior cervical sympathetic ganglion innervates the eye and lacrimal (tear) gland and causes vasoconstriction of the iris and sclera, pupillary dilation, widening of the palpebral fissure (the “whites of your eyes” the open area between the lower and upper eyelid), and reduces tear production. It has been implicated in many conditions and symptoms, including elevations of intraocular pressure (pressure within the eye), glaucoma, photophobia, and macular degeneration.
Eye problems: Kinking of the carotid sheath at the craniocervical junction.
Let’s take a moment to discuss these eye and vision problems before we move on. The caption of this image reads: The carotid sheath contents include the internal carotid artery, internal jugular vein, vagus nerve, glossopharyngeal nerve, and spinal accessory nerves. They can be functionally compromised as they make a sharp turn up to a 90-degree angle in the C1 atlas transverse process area into the brain through the jugular and carotid foramen pathways. This kinking or compression of these nerves, including the vagus nerve, and the blood vessels can lead to increased intracranial pressure, localized Cerebrospinal fluid and resultant cerebral atrophy, and increased eye pressure.

The vulnerability of the vagus nerve and the sympathetic ganglia
The superior cervical sympathetic ganglion is not a structure that one would like to leave vulnerable to compression. The superior cervical sympathetic ganglion connects with numerous organs, vessels, muscles, bones, joints, the last 4 cranial nerves, the vertebral plexus, the vagus nerve, the facial ganglion, and the phrenic nerve. It supplies the upper cervical spinal nerves (C1-C3) with gray rami communications (“uninsulated” nerve fibers to the spinal nerves) and sends off vascular fibers to the internal and external carotid arteries. Autonomic branches pass the ganglion to the larynx, pharynx, and heart, and together with vascular plexuses to the salivary and lacrimal glands, pituitary, thyroid, and parathyroid gland, as well as to primary and secondary lymph organs in the cervical region, including the thymus and submaxillary/submandibular lymph nodes. There are also connections with the middle cervical ganglion and the tympanic plexus. It can give fibers to a branch of the vagus nerve from the external branch of the superior laryngeal nerve. Lastly, but very importantly, the SCSG sends projections to the pineal gland and the suprachiasmatic nucleus that are key to normal (ideal) circadian rhythms. A person’s biological clock can be negatively affected, causing circadian rhythm sleep disorders and circadian dysrhythmias, from cervical instability impacting the superior cervical sympathetic ganglion.
As you can see, many body functions can be altered and functionally compromised by compression or damage to the superior cervical sympathetic ganglion.
The vagus nerves and sympathetic ganglia in the neck and upper thoracic area sit on either side of the longus muscles, capitis, or colli, which flex the neck. The longus capitis and longus colli muscles attach to the occiput (back of the skull) and atlas, respectively, and originate in the transverse process of the lower cervical and upper thoracic vertebrae. These muscles are extremely tight in forward head posture.
In the image below we see muscle tightness from chronic forward head posture – the posture of looking down at cell phones.

As it is the longest nerve in the body, the vagus nerve is especially prone to being “stuck”
As it is the longest nerve in the body, the vagus nerve is especially prone to being “stuck,” or not able to translate normally because of musculoskeletal changes that occur in the neck with the forward head-face down lifestyle, and is prone to injury by all these mechanisms. The net effect is that if the forces on the vagus nerve do not stop, there is a risk of vagal (and other) neurons dying.
The forward head posture can be a cause of cervical dysstructure or a broken neck structure. It can lead to progressively worse nerve damage in the cervical nerves, vagus nerve, and superior cervical sympathetic ganglion.
In the image below we can follow a path:
We start with Normal Healthy Nerves and normal nerve function > as the cervical spine structure starts to fail or becomes broken the patient can move onto Neuralgia . Here the nerve is now stretched and has the start of compression but the nerve is not yet damaged > Next is Neuritis , inflammatory damage around the nerve is present, and the nerve sheath becomes damaged. > At the end state we have Neuropathy, the death of neurons. When neurons die there are fewer communications and neurologic-like disorders become dominant.

When a nerve is subjected to long-term compression or stretch forces
When a nerve is subjected to long-term compression or stretch forces, whether from changes in bony or muscular anatomy or within the nerve sheath (cerebrospinal fluid [CSF]) or nerve (arterial/venous compromise, swelling) itself, neuron cell death can occur.
The pressure on the vagus nerve.
First an explanation: Axonal transport is a body system that is the main component of essential neuronal function (the ability of your nerve cells to communicate with your brain and your brain to be able to respond back). The Axon is a “cable” within the neuron. The Axonal transport, among its functions, removes old proteins and lipids from the neuron and replaces them with fresh proteins and lipids
The anatomy of a neuron, the anatomy of a nerve. In this illustration, we see the anatomy of a nerve. Attached to the nucleus in the Axon and as you can see the “long” cable or “chute” old proteins and lipids are pulled away from the nucleus and new proteins and lipids are sent to the nucleus.

When a nerve is subjected to long-term compression or stretch forces, whether from changes in bony or muscular anatomy or within the nerve sheath (cerebrospinal fluid [CSF]) or nerve (arterial/venous compromise, swelling) itself, neuron cell death can occur. It has been shown that both slow and fast axonal transport is impaired in the cervical vagus nerves by low pressures of compression, such as those levels of compression comparable with those found in human compression neuropathies such as carpal tunnel syndrome.
Compression of the vagus nerve can stop or impede the Axonal transport system.
In animal studies in the 1980s and 1990s researchers found that when rabbit vagus nerves were compressed and then the compression was removed, lingering effects occurred. Nerve transmission could be blocked or altered for one or more days depending on the level of compression and how long that compression lasted. Compression can occur as a result of pinching or stretching. Stretch or other deformation injuries to the axons can cause loss of axon transport and the accumulation of toxic substances that can destroy either transport or the axon itself. Also note that cervical kyphosis and compensatory hyperextension of the cervical spine can cause bending and strain of the lower brainstem and upper spinal cord, in addition to other damaging effects on localized nerves and nerve ganglia.
In medical research, Axonal transport is often described as motor proteins “trucking” their cargo of proteins and lipids back and forth along the axon. For good reason, that is what is occurring. A disruption in this trucking is seen in a 2019 paper in the journal Nature Reviews. Neurology . ( 12 )
“motor proteins actively navigate microtubules (in simplest terms storage structures) to deliver diverse cargoes, such as organelles (the stuff that makes cell function happen), from one end of the axon to the other and is widely regarded as essential for nerve development, function, and survival. Mutations in genes encoding key components of the transport machinery, including motor proteins, motor adaptors, and microtubules, have been discovered to cause neurological disease. Moreover, disruptions in axonal cargo trafficking have been extensively reported across a wide range of nervous system disorders. However, whether these impairments have a major causative role in, are contributing to, or are simply a consequence of neuronal degeneration remains unclear. Therefore, the fundamental relevance of defective trafficking along axons to nerve dysfunction and pathology is often debated.”
What is being suggested is, is the disruption of the axonal transport system within the nerves, the vagus nerve specifically, is the cause of neurological disease and neurological-like symptoms or is it a result of neurological disease. Both scenarios may be correct. Equally, can disruption of the axonal transport system be caused by cervical neck instability?
Compression and stretch.
In the illustration below, the more the head moves forward, the result of degenerative cervical ligament damage, and the more the brain stem and the vagus nerves get stretched.

Above we discuss disruption, compression, and stretch of the signals of the vagus nerve and its branches to and from other nerves and the nerve center ganglia. Now, what about the vagus nerve and blood flow?
If the vagus nerve is the most important nerve in the body, then surely the ascending pharyngeal artery, the vagus’s primary blood supply, is one of the most important blood vessels in the body. The ascending pharyngeal artery is a branch of the external carotid artery, the main collateral blood supply to the brain when the internal carotid artery is compressed. It is difficult to comprehend the enormity of the function of the vagus nerve (at only 2 mm in diameter) and the ascending pharyngeal artery (only 1 mm in diameter) that supplies these two structures are responsible for.
This little ascending pharyngeal artery provides vascularization of:
- the oropharynx, which needs blood from the pharyngeal artery for the back third of the tongue, the soft palate, the side and back walls of the throat, and the tonsils.
- the nasopharynx which is the airway behind the nasal passages. Also contained within the nasopharynx are the adenoids chronically implicated in breathing problems, especially through the mouth),
- the eustachian tube, and the middle ear, (problems of ear fullness and hearing – please see my article Neck pain Chronic Sinusitis and Eustachian Tube Dysfunction ),
- the skull base, the occipital bone and the foramen magnum,
- the dura, the outermost layer of the three meninges (the outer layer of membrane) that surrounds and protects the brain and spinal cord. Blood supply helps dura matter leaks and punctures heal.
- the hypoglossal canal, where the hypoglossal nerve transmits signals to the tongue,
- the vasa nervorum of the lower cranial nerves, (this is a group of small arteries that bring nutrients to the nerves).
- and the superior cervical sympathetic ganglion.
As the space narrows in the front of the neck between bones and muscle compartments, the small blood vessels are at risk for occlusion, as is the health of the tissues they supply.
It is therefore very possible that some of the symptoms implicated in cervical spine instability and its impact on vagal tone or vagus nerve function are actually from vascular injury as well. In an interesting twist, if the blood supply through the external carotid artery gets compromised, the vagus nerve sends inhibitory (relax, calm down) signals to the superior cervical sympathetic ganglion to dilate the blood vessel and improve blood flow. Not panic signals to try to push more blood through by increasing circulation.

Vessel stretch can result in intimal (the membrane or “skin” inside the vessels) injury, creating the potential for vessel dissection (separation of vessel wall tissue layers) or intramural thrombus (blood clot) formation, leading to vessel stenosis or complete blockage. It should be noted that the symptoms of an exogenous (from the outside as in herniation or compression) artery occlusion causing vagus nerve injury can be similar to a compressive vagus nerve injury alone.
These symptoms include:
- ipsilateral (same side) headache,
- carotidynia (throbbing facial pain),
- ocular (eye) pain,
- neck pain, and
- amaurosis fugax (temporary loss of vision or darkness in the eye). It is important to remember the carotid sheath contains the internal carotid artery, whose last branch before entering the brain is the ophthalmic artery, which branches off right at the craniocervical junction. The ophthalmic artery and its branches supply the eyeball and areas around the eyeball, including the lacrimal glands, eyelids, conjunctiva (the connective tissue covering the eyeball), posterior uveal tract (the tissue between the cornea and the retina), extraocular muscles, and others.
Treatment vagus nerve stimulation
Vagus nerve stimulation is an umbrella term to describe any medical technique, electrical stimulation, manual manipulation, self-help technique, or health regimen that stimulates the vagus nerve.
In June 2022 a paper in the journal Biological Psychology ( 13 ) discusses the “recently proposed role of the vagus nerve in limiting inflammation. This has led to the adoption of an earlier developed technique for epilepsy treatment, i.e., electrical stimulation of one vagus nerve bundle in the neck, but now for immune diseases like rheumatoid arthritis, the scope is even widening to depression and cluster headaches. However, the problem in the application of whole vagus nerve stimulation is the lack of specificity: there is no way to titrate the stimulation to an observable effect variable. All nerves in the bundle, incoming and outgoing, can be ‘hit’, leading to side-effects which limit the intended application.”
In July 2022, researchers in Italy wrote in the Journal of Electroconvulsive Therapy ( 14 ) that vagus nerve stimulation can be effective for treatment-resistant depression. In this study, five patients treated with implanted with electronic vagus nerve stimulation were followed for 6 to 12 years after implantation.
- The VNS implant was associated with a sustained response (more than 10 years) in terms of clinical response and social, occupational, and psychological functioning in 3 patients.
- Two patients dropped out after 6 and 7 years of treatment, respectively.
- Vagus nerve stimulation was well tolerated by all patients, who reported only mild adverse effects.
Symptoms of Cervicovagopathy Dysautonomia
Above we have laid a basic groundwork describing structural problems, or cervical dysstructure, in the neck. Now we will discuss the vagus nerve and dysautonomia.
Let’s first touch on some new research developments that will help explain the impact of vagus nerve dysfunction on health and the role of cervical instability.
First dysautonomia
Dysautonomia is a dysfunction of the nerves that regulate the involuntary functions of the body. Vagus nerve degeneration can be so serious that widespread arterial vasospasm (blocking off blood flow to the body including the brain) can occur. Everything that happens in the body involuntarily, including cardiovascular, gastrointestinal, genitourinary, ocular, respiratory, thermoregulatory, vasomotor homeostatic functions, and a host of other involuntary reflexes can be affected by vagus nerve degeneration. The PNS, led by the vagus nerve, helps the body rest, digest, and ultimately repair, without which the body goes into disrepair. The sympathetic and parasympathetic systems are in a finely tuned interplay. When sympathetic dominance occurs over a long period of time, characteristic signs and symptoms occur.
Let’s examine the illustration below. Below the illustration are explanatory notes.

Vagus and nodose ganglion degeneration findings
Animal studies are done in preliminary research, sometimes animal studies are done when the risk of producing the same study in human beings would be considered unsafe.
The amount of neuron (nerve) degeneration correlates with the level of coronary artery vasospasm and animal (rabbit) death. ( 15 )
- The researchers summarized their findings this way: “We found that there is a causal relationship between nodose ganglion degeneration and coronary vasospasm. Our finding could be the reason that many cardiac events occur in patients with subarachnoid hemorrhage (bleeding around the brain). Vagal pathway paralysis (among other conditions, impacting the heart function) induced by indirect sympathetic overactivity (increased heart rate, increased respiration, increased blood pressure) may trigger coronary vasospasm and heart rhythm disturbances.”
Vagal ischemia (loss of blood supply) induces lung (cell and area death) in respiratory arrest from pulmonary artery vasospasms. ( 16 )
- convulsive attacks
- cardiac arrhythmia
- and breathing difficulties.
Degeneration of the vagal renal (kidney) branches caused extreme parenchyma (functional tissue) spastic renal arteries leading to Glomerulonephritis (inflammation of the small filters in your kidneys) and kidney cell death at a 17 times greater rate than normal. This problem also results in sodium retention leading to severe hypertension in the neurogenic lung edema vagus nerve.
- Above we discussed Axon damage. That is what happened in this study, the researchers ( 17 ) noted significant degenerated axon density of vagal nerves.
Vagus nerve degeneration causes Auerbach network (responsible for intestinal peristaltic movement) degeneration. The Auerbach plexus or myenteric plexus is a group of ganglia that run throughout the entire gastrointestinal tract and innervate its multiple layers of smooth muscle. ( 18 )
- The research noted that: Ultimately intestinal gland atrophy resulted in 200 times more cell deaths and ulcers. One of the main findings again was Axon damage along the gastric branches of the vagus nerve. ( 19 )
The illustration above helps explain the wide-ranging symptoms and conditions of vagus nerve dysfunction along with the nerve network.
The hallmark feature of dysautonomia is dysfunction of the vagus nerve.
The most common symptoms of vagus nerve dysfunction include chronic pain, fatigue, dizziness, lightheadedness, spinning or pulling sensation (in a particular direction), weight loss, poor focusing, exercise intolerance, emotional lability, inflammation, heartburn, bloating, diarrhea, tinnitus, headache, anxiety, depression, brain fog, swallowing difficulty, vision changes, and inability to handle stress well.
One clue that there is a neck cause to a person’s dysautonomia is when turning of the head or facial movements such as laughing, chewing, or speaking cause what we term “episymptoms,” which are symptoms that are manifested by activities that don’t normally cause those symptoms, such as flushing, sweating, temperature dysregulation, headaches, vision changes, electric shocks, palpitations, tachycardia, or other autonomic symptoms.
Signs include changes in blood pressure, impaired thermoregulation , fatigue, changes in mental state (such as an increase in stress or lightheadedness), dilated pupils, uvula deviation to one side, and an inability of the palate to rise normally, decreased gag reflex, and dilated pupils. Many of these symptoms are signs of vagopathy.

The nitty-gritty of how you know you have a vagus nerve problem
- One pupil is significantly larger than the other along with light sensitivity)
- Resting heart rate over 100 beats per minute
- Uvula deviates
- Uvula does not rise
- Uvula rises more on one side versus the other side.
- You slow your breathing down but your heart rate does not.
In the image below, right vagopathy is evidenced by the lack of palatal elevation on the right side when saying “Ahhh.” This is caused by weakness in this patient’s right levantor veli palatini muscle which is innervated by the right vagus nerve.

Dysautonomia and cervical instability caused by ligament damage or weakness are progressive disorders. As vagal nerve function struggles, the autonomic nervous system’s (ANS) ability to regulate the body gets more compromised. Eventually, when it can no longer maintain blood pressure, orthostasis occurs (loss in blood pressure when standing), and ultimately multisystem atrophy that can include all the internal organs, in what is termed “pure autonomic failure.” When a person with cervical instability caused by ligament damage experiences symptoms that occur suddenly or increase in severity, it is often because they are starting to have autonomic collapse.
Summary and contact us. Can we help you? How do I know if I’m a good candidate?
We hope you found this article informative and that it helped answer many of the questions you may have. Just like you, we want to make sure you are a good fit for our clinic prior to accepting your case. While our mission is to help as many people with chronic pain as we can, sadly, we cannot accept all cases. We have a multi-step process so our team can really get to know you and your case to ensure that it sounds like you are a good fit for the unique testing and treatments that we offer here.
References:
1 Lee KY, Oh YW. Extradrenal pargangliomas of the body: imaging features. Am J Roentgenol. 2006;187:492-504. [ Google Scholar ] 2 Syamsunder AN, Pal GK, Pal P, Kamalanathan CS, Parija SC, Nanda N. Association of sympathovagal imbalance with cardiovascular risks in overt hypothyroidism. North American Journal of Medical Sciences. 2013 Sep;5(9):554. [ Google Scholar ] 3 Tankeu AT, Azabji-Kenfack M, Nganou CN, Ngassam E, Kuate-Mfeukeu L, Mba C, Dehayem MY, Mbanya JC, Sobngwi E. Effect of propranolol on heart rate variability in hyperthyroidism. BMC Research Notes. 2018 Dec;11(1):1-4. [ Google Scholar ] 4 Myssiorek D. Recurrent laryngeal nerve paralysis: anatomy and etiology. Otolarynngol Clin North Am. 2004;37(1):25-44. [ Google Scholar ] 5 Kuo CT, Chiu CH, Fang TJ, Chao YK. Prognostic factors for recovery from left recurrent laryngeal nerve palsy after minimally invasive Mckeown esophagectomy: a retrospective study. Annals of Surgical Oncology. 2024 Mar;31(3):1546-52. [ Google Scholar ] 6 Mingazova LR, Karpova EI, Murakov SV, Danishuk OI, Bychenko VG, Orlova OR, Soykher MI, Nikolenko VN, Sinelnikov MY. Iatrogenic glossopharyngeal neuropathy in aesthetic practice: a case report. Plastic and Reconstructive Surgery–Global Open. 2022 Mar 1;10(3):e4166. [ Google Scholar ] 7 De Couck M, Mravec B, Gidron Y. You may need the vagus nerve to understand pathophysiology and to treat diseases. Clinical science. 2012 Apr 1;122(7):323-8. [ Google Scholar ] 8 Mol MB, Strous MT, van Osch FH, Vogelaar FJ, Barten DG, Farchi M, Foudraine NA, Gidron Y. Heart-rate-variability (HRV), predicts outcomes in COVID-19. PLoS One. 2021 Oct 28;16(10):e0258841. [ Google Scholar ]. 9 Diener HC, Gaul C, Holle-Lee D, Jürgens TP, Kraya T, Kurth T, Nägel S, Neeb L, Straube A. Headache-an Update 2018. Laryngo-Rhino-Otologie. 2019 Mar 7;98(3):192-217. [ Google Scholar ] 10 Guclu B, Sindou M, Meyronet D, Streichenberger N, Simon E, Mertens P. Cranial nerve vascular compression syndromes of the trigeminal, facial and vago-glossopharyngeal nerves: comparative anatomical study of the central myelin portion and transitional zone; correlations with incidences of corresponding hyperactive dysfunctional syndromes. Acta neurochirurgica. 2011 Dec;153(12):2365-75. [ Google Scholar ] 11 Taher F, Bokums K, Aichmair A, Hughes AP. C1–C2 instability with severe occipital headache in the setting of vertebral artery facet complex erosion. European Spine Journal. 2014 May;23(2):145-9. [ Google Scholar ] 12 Sleigh JN, Rossor AM, Fellows AD, Tosolini AP, Schiavo G. Axonal transport and neurological disease. Nature Reviews Neurology. 2019 Dec;15(12):691-703. [ Google Scholar ] 13 Karemaker JM. The multibranched nerve: vagal function beyond heart rate variability. Biological Psychology. 2022 Jun 7:108378. [ Google Scholar ] 14 Pigato G, Rosson S, Bresolin N, Toffanin T, Sambataro F, Olivo D, Perini G, Causin F, Denaro L, Landi A, D’Avella D. Vagus Nerve Stimulation in Treatment-Resistant Depression: A Case Series of Long-Term Follow-up. The Journal of ECT.:10-97. [ Google Scholar ] 15 Yolas C, Kanat A, Aydin MD. Unraveling of the effect of nodose ganglion degeneration on the coronary artery vasospasm after subarachnoid hemorrhage: an experimental study. World Neurosurg. 2016 Feb;86:79-87 [ Google Scholar ] 16 Atalay C, Gundogdu B, Aydin MD. Vagal ischemia induced lung immune component infarct following subarachnoid hemorrhage: an experimental study. Turk Neurosurg. 2017 Jan 1;27(4):509-15. [ Google Scholar ] 17 Soyalp C, Kocak MN, Ahiskalioglu A, Aksoy M, Atalay C, Aydin MD, Cakir M, Calikoglu C, Ozmen S. New determinants for casual peripheral mechanism of neurogenic lung edema in subarachnoid hemorrhage due to ischemic degeneration of vagal nerve, kidney and lung circuitry. Experimental study. Acta Cirúrgica Brasileira. 2019 Mar 18;34. [ Google Scholar ] 18 Shahrestani J, Das JM. Neuroanatomy, auerbach plexus. StatPearls [Internet]. 2021 Jun 4. [ Google Scholar ] 19 Cakir M, Ahiskalioglu A, Karadeniz E, Aydin MD, Malcok UA, Soyalp C, Calikoglu C, Sengul G, Sipal S, Yayik AM. A new described mechanisms of intestinal glandular atrophy induced by vagal nerve/Auerbach network degeneration following subarachnoid hemorrhage: The first experimental study. Journal of Clinical Neuroscience. 2019 Jan 1;59:305-9. [ Google Scholar ]
Get Help Now!
You deserve the best possible results from your treatment. Let’s make this happen! Talk to our team about your case to find out if you are a good candidate.
- Patient Care & Health Information
- Diseases & Conditions
- Noonan syndrome
Noonan syndrome is a genetic condition that stops typical development in various parts of the body. It can affect a person in several ways, including unusual facial features, short height, heart problems and other physical problems. It also can cause a child to develop more slowly than usual, for example, in walking, talking or learning new things.
A changed gene causes Noonan syndrome. A child inherits a copy of an affected gene from a parent. This is called dominant inheritance. The condition also can occur as a spontaneous change. This means there's no family history involved.
Doctors manage Noonan syndrome by controlling the symptoms and complications. They may use a growth hormone to treat short height in some people with Noonan syndrome.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
Symptoms of Noonan syndrome vary greatly and range from mild to severe. These symptoms may be related to the specific gene containing the change.
Facial features
How the face looks is one key feature that leads to a diagnosis of Noonan syndrome. Facial features may be easier to see in infants and young children but change with age. These distinct features become less clear in adults.
Noonan syndrome may include these features:
- Eyes are wide-set, slant down and have droopy lids. Eyes may be pale blue or green.
- Ears are set low and look like they're tipped backward.
- Nose is depressed at the top, with a wide base and round tip.
- Mouth has a deep groove between the nose and the mouth and wide peaks in the upper lip. The crease that runs from the edge of the nose to the corner of the mouth becomes deeply grooved with age. Teeth may be crooked. The inside roof of the mouth may be highly arched. And the lower jaw may be small.
- Facial features may appear coarse but look sharper with age. The face may appear droopy and not show expression.
- Head may be large with a big forehead and a low hairline on the back of the head.
- Skin may appear thin and transparent with age.
Heart disease
Many people with Noonan syndrome are born with a heart problem that causes some of the key symptoms of the condition. This is called congenital heart disease. Also, some heart problems can occur later in life.
Some forms of congenital heart disease related to Noonan syndrome include:
- Valve conditions. Pulmonary valve stenosis is a narrowing of the pulmonary valve. This valve is the flap of tissue that separates the lower right chamber of the heart — called the right ventricle — from the artery that supplies blood to the lungs — called the pulmonary artery. Pulmonary valve stenosis is the most common heart problem seen with Noonan syndrome. It may occur with or without other heart problems.
- Thickening of the heart muscle. Unusual growth or thickening of the heart muscle — also known as hypertrophic cardiomyopathy — affects some people with Noonan syndrome.
- Other heart problems. Problems with heart structure can involve a hole in the wall that separates the two lower chambers of the heart, known as ventricles. This is called a ventricular septal defect. Another defect sometimes seen is narrowing of the artery that carries blood to the lungs for oxygen. This is called pulmonary artery stenosis. Or there can be narrowing of the major blood vessel known as the aorta, which carries blood from the heart to the body. This is called aortic coarctation.
- Irregular heart rhythm. This can occur with or without other problems in heart structure. Most people with Noonan syndrome have a heart rhythm that is not regular.
Growth issues
Noonan syndrome can affect typical growth. Many children with Noonan syndrome do not grow at a typical rate.
Issues may include:
- Typical birth weight but slower growth over time.
- Eating difficulties that may lead to poor nutrition and weight gain.
- Growth hormone levels that may be too low.
- Delay in the growth spurt that's typically seen during the teenage years because bones do not reach maximum strength or density until later.
- Short height as an adult, which is common, but some people with Noonan syndrome may not be short.
Issues with muscles and bones
Some common issues can include:
- A condition called pectus excavatum, where the breastbone and ribs sink too far into the chest. It also is possible to have pectus carinatum, where the breastbone and ribs grow outward, making the chest stick out more than usual.
- Nipples that are wide apart.
- Short neck, often with extra folds of skin, called a webbed neck.
- A spine that has an unusual curve.
Learning disabilities
Noonan syndrome does not affect the intelligence of most people who have the condition. But they may have:
- A higher risk of learning disabilities and mild intellectual disability.
- A wide range of mental, emotional and behavioral issues that are usually mild.
- Hearing and vision problems that may make it harder to learn.
Eye conditions
Common signs of Noonan syndrome are eyes and eyelids that are unusual, including:
- Problems with the eye muscles, such as cross-eye, also known as strabismus.
- Refractive problems, which means the cornea or the lens is egg-shaped with two curves that do not match. This can make vision blurry or distorted, or make it hard to see things close up or far away.
- Rapid movement of the eyeballs, also known as nystagmus.
- Cataracts, which make an eye cloudy.
Hearing problems
Noonan syndrome can cause hearing problems due to nerve issues or an inner ear bone structure that is not typical.
Bleeding problems
Noonan syndrome can cause bleeding problems and easy bruising. That's because the blood of some people with Noonan syndrome may not clot properly and may have low levels of proteins that are needed for clots to form. So they bleed longer than usual.
Lymphatic conditions
Noonan syndrome can cause problems with the lymphatic system, which drains excess fluid from the body and helps fight infection. These problems:
- May show up before or after birth or start in the teenage years or as an adult. Some children are born with swelling of the hands, feet and tissue of the neck.
- Can focus on a particular area of the body or be widespread.
- Most commonly cause too much fluid to build up in the back of the hands or top of the feet. This fluid buildup is called lymphedema.
Genital and kidney conditions
Many people with Noonan syndrome have problems with their genitals and kidneys:
- Testicles. It's common for males with Noonan syndrome to have undescended testicles. These are testicles that have not moved into proper position in the bag of skin hanging below the penis, called the scrotum.
- Puberty. Puberty may be delayed in males and females.
- Fertility. For most females, Noonan syndrome does not affect their ability to get pregnant. But fertility in males may not develop as expected, often because of undescended testicles.
- Kidneys. Kidney problems generally are mild and not common.
Skin conditions
People with Noonan syndrome may have skin conditions. They may have various problems that affect the color and texture of the skin. They also may have coarse or sparse hair.
When to see a doctor
Sometimes the symptoms of Noonan syndrome can be hard to see. If you suspect you or your child may have this condition, see your primary care professional or your child's pediatrician. You may be referred to a specialist in genetics or a specialist in heart problems or another type of doctor, depending on the symptoms.
If your unborn child is at risk because of a family history of Noonan syndrome, tests may be able to be done before birth.
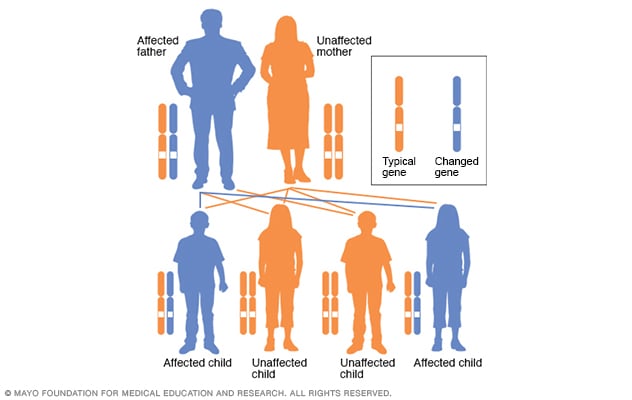
Autosomal dominant inheritance pattern
In an autosomal dominant disorder, the changed gene is a dominant gene. It's located on one of the nonsex chromosomes, called autosomes. Only one changed gene is needed for someone to be affected by this type of condition. A person with an autosomal dominant condition — in this example, the father — has a 50% chance of having an affected child with one changed gene and a 50% chance of having an unaffected child.
A change in one or more genes can cause Noonan syndrome. Changes in these genes produce proteins that are always active. Because these genes play a role in how tissues form in the body, this constant activation of proteins disrupts the typical process of cell growth and division.
The gene changes that cause Noonan syndrome can be:
- Inherited. Children who have one parent with Noonan syndrome who carries the changed gene have a 50% chance of developing the condition. This is called an autosomal dominant inheritance pattern.
- Random. Noonan syndrome can develop in a child because of a new changed gene — meaning the child did not inherit that gene from a parent. This is known as a de novo genetic condition.
In some cases, the cause of Noonan syndrome is not known.
Risk factors
A parent with Noonan syndrome has a 50% chance of passing the changed gene to a child. The child who inherits the irregular gene may or may not have more symptoms than the parent who is affected.
Complications
Complications from Noonan syndrome can arise that may need attention, including:
- Developmental delays. Children with Noonan syndrome may be slow to develop compared with other children their age. For example, they may be way behind in learning to speak or walk or in learning things at school. A plan is needed to address the children's developmental challenges and learning and educational needs.
- Bleeding and bruising. Sometimes the bleeding problem common in people with Noonan syndrome is not found until they have dental work or surgery.
- Buildup of fluid. Called lymphedema, this complication involves too much fluid that builds up in various areas of the body. Sometimes fluid can collect in the space around the heart and lungs.
- Urinary tract issues. A kidney structure that is not typical may raise the risk of urinary tract infections.
- Fertility issues. Males may have a low sperm count and other fertility problems because of undescended testicles or testicles that do not work properly.
- Higher risk of cancer. There may be a higher risk of developing certain types of cancer, such as leukemia or certain types of tumors.
If you have a family history of Noonan syndrome, talk to your doctor or health care team about the benefits of genetic counseling before you have children. Genetic testing can detect Noonan syndrome.
If Noonan syndrome is detected early, it's possible that proper and ongoing care may lessen complications such as heart disease.
- Allen MJ, et al., eds. Noonan syndrome. In: STATPearls. 10th ed. Stat Pearls Publishing; 2023. https://pubmed.ncbi.nlm.nih.gov/. Accessed March 22, 2023.
- Elsevier Point of Care. Clinical Overview: Noonan syndrome. https://www.clinicalkey.com. Accessed March 22, 2023.
- Richmond EJ, et al. Causes of short stature. https://www.uptodate.com/search. Accessed March 22, 2023.
- Burkitt-Wright EMM, et al. Noonan syndrome. https://www.uptodate.com/search. Accessed March 22, 2023.
- National Library of Medicine. Noonan syndrome. https://medlineplus.gov/genetics/condition/noonan-syndrome/. Accessed March 22, 2023.
- Zenker M, et al. Noonan syndrome: Improving recognition and diagnosis. Archives of Disease in Childhood. 2022; doi:10.1136/archdischild- 2021-322858 .
- About Noonan syndrome. National Human Genome Research Institute. https://www.genome.gov/25521674/learning-about-noonan-syndrome/. Accessed March 22, 2023.
- Noonan syndrome. Genetic and Rare Diseases Information Center. https://rarediseases.info.nih.gov/diseases/10955/noonan-syndrome. Accessed March 22, 2023.
- Noonan syndrome. National Organization for Rare Disorders Inc. http://rarediseases.org/rare-diseases/noonan-syndrome/. Accessed March 22, 2023.
- Babovic-Vuksanovic D (expert opinion). Mayo Clinic. April 23, 2023.
Associated Procedures
- Echocardiogram
- Electrocardiogram (ECG or EKG)
- Genetic testing
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Deep Fancy Island
Deep Fancy Island (Japanese: 深層ふぁんしーあいらんど ) is a short expansion of Lomando.com , a Japanese screamer website that functions as a horror puzzle game. The expansion occurs underground, presumably connected to the abandoned Fancy Island Amusement Park.
- 1 Website content
- 2 Gameplay overview
- 3 First kanji
- 4 Second kanji
- 5 Third kanji
- 6 Fourth kanji
- 7 Fifth kanji
- 8 Deepindox.html alternative route
- 10.1 Deepdassyutu.html
- 10.2 Deepdashtwoes.html
Website content
The game is set on a page called Deeptop.html , which features a possessed and realistic version of Mimi with text below in English and Japanese. The text gives an overview of the game, stating that the player must solve mysteries to win and be sent to an "archive". Alongside Mimi was linked to other pages and advertisements for LINE.
Gameplay overview
The game begins with the player in a field, facing an entrance that leads to Ookamuro Subspecies and five glitchy Japanese kanji characters. Each kanji button redirects to a different page. Clicking the head in the middle produces laughter, and clicking the top left corner unlocks a separate portion of the page where the player must click buttons in a specific order. This leads to the appearance of a monochrome door that redirects the player to a new page called Deepdashtwoes.html. Despite its numerous screamers, Deep Fancy Island can also be considered a puzzle game due to its heavy use of puzzles and mazes.
First kanji

(gallery of the puzzle here) (picture of the kitchen illustration here) The first kanji leads to Deepgesui.html , guiding the player into a sewer. By clicking down, they advance until a rusted door appears after three "steps." Clicking on the door once results in blood splatter, and clicking again leads to another page, Deepdoukutu.html . There is a chance that a woman named Franjyou appears, accompanied by the traditional Lomando scream.
Deepdoukutu.html introduces into a new underground setting. The player must click to traverse the cavern's end, encountering a Jizo statue. Clicking on it progresses to the next page Deepdassyutu.html . Amid this journey, a screamer depicting a mummified corpse, colloquially known as "Mummy man" may appear similar to the previous.
Deepdassyutu.html introduces a locked purple door secured by a keypad. The player navigates various sections using left and right arrows on their screen. These include a locked cabinet with three shapes below it, a painting featuring differently-colored heads and numbers, a sinkhole with a key underneath, and a desktop setup on a table with two chairs. The player has a 50% chance of encountering either Chaori or a Half-melted woman during the sequence, resulting in a game over. To solve the puzzle, the player must:
- Locate the desktop setup and click on the monitor, revealing a Windows NT -styled operating system. This system leads to a webpage requiring a password, with a map hinting at a counter-clockwise path. The password is derived from the numbers associated with objects in the rooms, indicated by dark purple shading. The locked door shows a "7," the computer has a "1," the sinkhole represents a "0," and the dark circle signifies another "0."
- Inputting these numbers triggers the sound of running water. Going to the sink reveals a key pushed up by the water in the hole, unlocking the cabinet.
- Inside the cabinet is a light switch that, when turned off, displays colored digits on the screen (A red +3, A blue +1, A green +4, and a yellow +1), corresponding to numbers in the cryptic painting. Adding these numbers produces the code "5382." Entering this code into the keypad unlocks the door, allowing progression to the next webpage, Deepmachigai.html .

Deepmachigai.html presents a YouTube video featuring two illustrations of a kitchen. The player must identify and mark the differences. Correctly identifying all differences triggers a hidden door accompanied by a low-pitched laugh. This door leads to Deepmemo9128.html , revealing a folded paper disclosing the solution to the "alternate puzzle" in Deepindox.html .
Second kanji
The second kanji leads to Deepskull.html , a webpage showcasing a series of numbered skulls that reshuffle every six seconds. Solving the puzzle involves using a YouTube video to reorganize the skulls based on the new order presented in the video, with the correct order being 3-5-2-1-4. Upon solving it correctly, the skulls briefly display eyes before disappearing, unveiling a door that redirects the player to Deepcurtain.html .
On this page, a curtain is prominently featured. Clicking on the curtain reveals various elements, including a grayscale version of a stuffed bear Kuma , a Half-melted woman, a golden key available for the player to pick up, and a locked treasure chest. To advance, the player must collect the golden key and use it to unlock the chest. Inside, they will discover a sheet of paper that, upon clicking, displays the first secret code "gggj" for Deeparchive.html .
Third kanji
In the third kanji, the player is directed to Deepcryw.html , where a section of young women is displayed in several rows, all opening their mouths, except for one in the third row who seems visibly concerned. Clicking on this particular woman results in a transformation of all others into crying ghosts. While most ghosts exhibit movement, one in the second row is observed putting her head in her hands. Clicking on this specific ghost initiates the appearance of a larger ghost in the center of the screen, though this entity poses no threat. After approximately 20-25 seconds, the ghost dissipates, unveiling a door leading to a folded paper containing the code "rain," crucial for progress in Deeparchive.html .
Fourth kanji

The fourth kanji leads the player to a purple slot machine. Accompanying this machine is an instructional guide labeled "How-to-play" providing users with insights into the game's mechanics. This guide serves as a compass, directing players toward the objective of accumulating a minimum of 300 credits to advance. Players commence with 50 credits and must invest 3 credits per play.
The scoring guide provides a detailed explanation, highlighting that Three 7s yield a maximum of 300 points and activate a bonus, allowing the player to score 15 points regardless of the combo. It emphasizes that the slot machine operates randomly, with a 4% chance of winning. Upon reaching 300 credits, a door appears in the bottom right corner. Clicking on the door and agreeing to the warning redirects the player to Deepmemosau111.html . Notably, players can continue playing the slot machine even after the door appears until they run out of credits. After completing the game, they would be redirected to a piece of paper with the code "jkpt" for Deeparchive.html .
Failure to reach 300 credits prompts a purple hand to extend from the machine toward the player's screen, resulting in a game over. While engaging with the slot machine, Abyss, Cursed Doll, Kubishime Onna, Eris, Borei, Dai kuchisake-onna, and Franjyou each has a 14% chance of appearing on the screen.
Fifth kanji
The fifth kanji showcases a folding window, which can be clicked up to three times. Upon the fourth click, the window will open, and Shadow head will fly into the room. This action results in the player being grabbed by Shadow head, ultimately leading to a game over. Additionally, the room will flash momentarily, and a thunder sound will be audible upon clicking the window. This page does not lead anywhere.

Deepindox.html alternative route

After following the alternative puzzle hinted from the first kanji , the player is redirected to Deepdashtwoes.html , which features four sections in a room. Initially, the player encounters a door sealed by a ghost. Clicking right leads to a room with an incomplete puzzle of white pieces. Moving right from here reveals the Karakuri doll. Tapping her head causes laughter, and tapping it five times awards a black puzzle piece. Inserting this into the previous puzzle prompts corrupted text at the bottom. Trying to leave the Karakuri doll's room without additional taps results in failure, and remaining in her room. The doll's laugh deepens with each tap. Leaving the room three times prompts a jump-scare, ending the game.
- To proceed, the player avoids using the black piece and taps the doll's head five more times. This rewards a can opener.
- Opening the can in the starting room reveals coins for the "SMILE or TEARFUL?" game. Guessing correctly twice drops a capsule containing a white puzzle piece. The player chooses to insert the black piece, triggering a trap, or the white piece, making the puzzle vanish.
- The Exorcism Laser Gun is revealed. Shooting the door eliminates the ghost, unlocking it, redirects to Deepomuk.html . Alternatively, shooting the doll twelve times makes her vanish, revealing a golden door leading to Deepdotsboy.html .
On March 29th, 2023, a new page includes a dark hallway. Walking to the door summons Wandering Neck, who startles but doesn't harm. She says, "It hurts..." and "Where have my friends gone...?" Disappearing reveals a note with a photo of her and J-ker when they were alive (pictured). Clicking the door redirects to Deepdashtwoes.html .
After leaving Deepdashtwoes.html, the player enters a room with dark blue tiles. Clicking the door summons a Spider monster. Using the Exorcism Laser Gun defeats it, granting access to the gallery page.

Deeparchive.html concludes Deep Fancy Island . It features ten sections or Files describing game characters in English and Japanese. Secret sections, accessed through codes, provide extra content like Mummy man's early designs and information about Girl on the sign. The page includes probabilities of ghosts in Deepslotkai.html and pixel art of Yukan no Shonen from Deepdotsboy.html . The codes obtained from the other kanjis can unlock secret "files" in the game.
The archive begins with a description of a large face encountered in the first room, providing insights about Franjyou who appears in the sewage area. Further details emerge regarding a mummy (known as "Mummy man") located in the cave area and a seldom-seen ghost in the mystery-solving game section . The text then delves into a ghost intermittently present in both the curtain area and the mystery-solving game zone, hinting at significant events when a specific crying ghost stops. An introduction follows for a ghost situated in the spot-the-difference area , also highlighted on the centipede page in the regular edition of Fancy Island . The content proceeds to elaborate on a karakuri doll from Deepdashtwoes.html , a monstrous entity emerging from another world, wielding scythe-like front legs, and a ghost making an appearance on the window page from the fifth kanji , and finally, a backstory of J-ker's friend from their pre-deceased life—a girl in search of J-ker and her lost body.
Additionally, the codes obtained from the other kanjis can unlock secret "files" in the game. The files reveal versions of the mummy man's appearance through multiple redraws, provide insights into the appearance rate of screamers in the slot machine game from the fourth kanji , a girl featured on a warning sign in the park cautioning against running, and a pixel art rendition of Yukan no Shonen from the original Fancy Island .
Ironically, this is indeed the gallery of the game. You might be looking for Archive instead.
Deepdassyutu.html

A light purple door secured by a keypad.

A computer where the player must solve a puzzle.

A locked cabinet with three shapes beneath it

Differently-colored heads with numbers.

The sinkhole where the key is found.

The keypad of the door.
Deepdashtwoes.html

The door is sealed by a ghost.

The "SMILE or TEARFUL?" game and a pile of coins used to play it.

An incomplete puzzle piece with a missing piece can be obtained from that game.

The Exorcism Laser Gun unlocked after completing the puzzle.
NOTE : The following website contains lots of screamers !
- lomando.com/deeptop.html
- Showcase video : youtube.com/watch?v=_aU3mXIgsCk
- Lomando Wiki : lomando.fandom.com/wiki/Deep_Fancy_Island
- Featured Articles
- Screamers with songs
- Graphic content
Navigation menu
Personal tools.
- Create account
- View source
- View history
- Recent changes
- Random page
- Help about MediaWiki
- Your Sandbox
- Help Portal
- Community Portal
Screamer Library
- Applications
- Commercials
- Shock sites
- Screamer Timeline
- What links here
- Related changes
- Special pages
- Printable version
- Permanent link
- Page information
- Cite this page
- This page was last edited on 20 March 2024, at 01:03.
- Content on the wiki is available under Creative Commons Attribution unless otherwise noted.
- This page has been accessed 24,743 times.
- Privacy policy
- About Screamer Wiki
- Disclaimers
- Mobile view
The Vagus Nerve (CN X)
Written by Navin Leanage
Last updated October 7, 2023 • 49 Revisions •
The vagus nerve is the 10 th cranial nerve (CN X).
It is a functionally diverse nerve, offering many different modalities of innervation. It is associated with the derivatives of the fourth and sixth pharyngeal arches .
In this article, we shall look at the anatomy of the vagus nerve – its anatomical course, functions and clinical correlations.
Premium Feature
- Sensory: Innervates the skin of the external acoustic meatus and the internal surfaces of the laryngopharynx and larynx. Provides visceral sensation to the heart and abdominal viscera.
- Special Sensory: Provides taste sensation to the epiglottis and root of the tongue.
- Motor: Provides motor innervation to the majority of the muscles of the pharynx, soft palate and larynx.
- Parasympathetic: Innervates the smooth muscle of the trachea, bronchi and gastro-intestinal tract and regulates heart rhythm.
Anatomical Course
The vagus nerve has the longest course of all the cranial nerves, extending from the head to the abdomen. Its name is derived from the Latin ‘ vagary’ – meaning wandering. It is sometimes referred to as the wandering nerve.
In the Head
The vagus nerve originates from the medulla of the brainstem. It exits the cranium via the jugular foramen, with the glossopharyngeal and accessory nerves (CN IX and XI respectively).
Within the cranium, the auricular branch arises. This supplies sensation to the posterior part of the external auditory canal and external ear.
In the Neck
In the neck, the vagus nerve passes into the carotid sheath, travelling inferiorly with the internal jugular vein and common carotid artery. At the base of the neck, the right and left nerves have differing pathways:
- The r ight vagus nerve passes anterior to the subclavian artery and posterior to the sternoclavicular joint, entering the thorax.
- The left vagus nerve passes inferiorly between the left common carotid and left subclavian arteries, posterior to the sternoclavicular joint, entering the thorax.
Several branches arise in the neck:
- Pharyngeal branches – Provides motor innervation to the majority of the muscles of the pharynx and soft palate.
- Superior laryngeal nerve – Splits into internal and external branches. The external laryngeal nerve innervates the cricothyroid muscle of the larynx. The internal laryngeal provides sensory innervation to the laryngopharynx and superior part of the larynx.
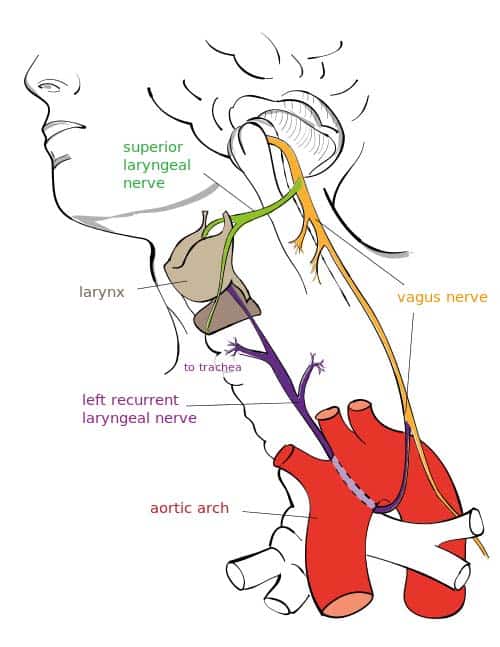
Fig 1 Overview of the major branches of the vagus nerve
In the Thorax
In the thorax, the right vagus nerve forms the posterior vagal trunk , and the left forms the anterior vagal trunk . Branches from the vagal trunks contribute to the formation of the oesophageal plexus, which innervates the smooth muscle of the oesophagus.
Two other branches arise in the thorax:
- Left recurrent laryngeal nerve – hooks under the arch of the aorta, ascending to innervate the majority of the intrinsic muscles of the larynx.
- Cardiac branches – regulate heart rate and provide visceral sensation to the heart
The vagal trunks enter the abdomen via the oesophageal hiatus, an opening in the diaphragm.
In the Abdomen
In the abdomen, the vagal trunks terminate by dividing into branches that supply the oesophagus, stomach and the small and large bowel (up to the splenic flexure).
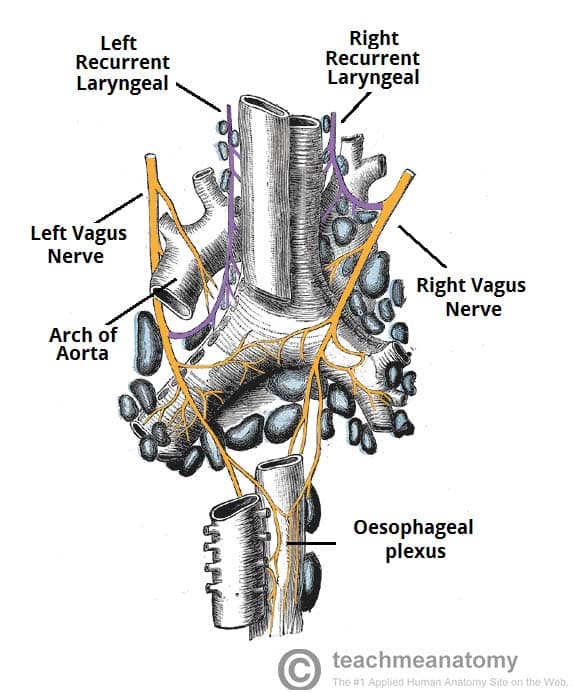
Fig 2 The origin of the recurrent laryngeal nerves
Sensory Functions
There are s omatic and visceral components to the sensory function of the vagus nerve.
Somatic refers to sensation from the skin and muscles. This is provided by the auricular nerve, which innervates the skin of the posterior part of the external auditory canal and external ear.
Viscera sensation is that from the organs of the body. The vagus nerve innervates:
- Laryngopharynx – via the internal laryngeal nerve.
- Superior aspect of larynx (above vocal folds) – via the internal laryngeal nerve.
- Heart – via cardiac branches of the vagus nerve.
- Gastro-intestinal tract (up to the splenic flexure) – via the terminal branches of the vagus nerve.
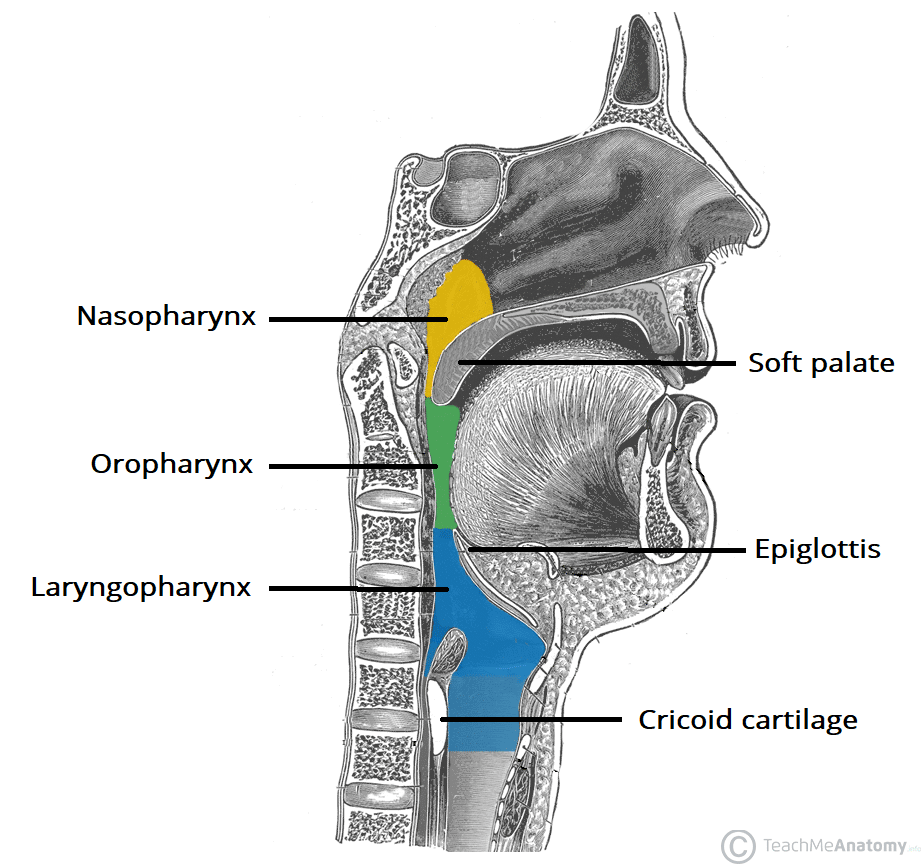
Fig 3 The three parts of the pharynx, and their borders. The laryngopharynx is innervated by the vagus nerve.
Special Sensory Functions
The vagus nerve has a minor role in taste sensation. It carries afferent fibres from the root of the tongue and epiglottis .
(This is not to be confused with the special sensation of the glossopharyngeal nerve, which provides taste sensation for the posterior 1/3 of the tongue).
Motor Functions
The vagus nerve innervates the majority of the muscles associated with the pharynx and larynx. These muscles are responsible for the initiation of swallowing and phonation.
Most of the muscles of the pharynx are innervated by the pharyngeal branches of the vagus nerve:
- Superior, middle and inferior pharyngeal constrictor muscles
- Palatopharyngeus
- Salpingopharyngeus
An additional muscle of the pharynx, the stylopharyngeus , is innervated by the glossopharyngeal nerve.
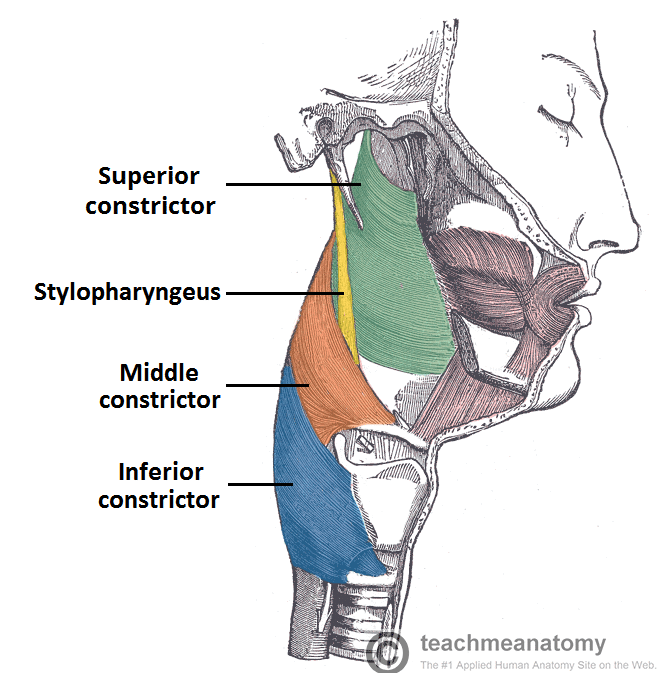
Fig 4 Lateral view of the deep structures of the pharynx. Visible are the circular muscles of the pharynx, and the stylopharyngeus.
Innervation to the intrinsic muscles of the larynx is achieved via the recurrent laryngeal nerve and external branch of the superior laryngeal nerve.
Recurrent laryngeal nerve:
- Thyro-arytenoid
- Posterior crico-arytenoid
- Lateral crico-arytenoid
- Transverse and oblique arytenoids
External laryngeal nerve:
- Cricothyroid
Other Muscles
In addition to the pharynx and larynx, the vagus nerve also innervates the palatoglossus of the tongue, and the majority of the muscles of the soft palate .
Parasympathetic Functions
In the thorax and abdomen, the vagus nerve is the main parasympathetic outflow to the heart and gastro-intestinal organs.
Cardiac branches arise in the thorax, conveying parasympathetic innervation to the sino-atrial and atrio-ventricular nodes of the heart (For more heart anatomy, see here ).
These branches stimulate a reduction in the resting heart rate. They are constantly active, producing a rhythm of 60 – 80 beats per minute. If the vagus nerve was lesioned, the resting heart rate would be around 100 beats per minute.
Gastro-Intestinal System
The vagus nerve provides parasympathetic innervation to the majority of the abdominal organs. It sends branches to the oesophagus, stomach and most of the intestinal tract – up to the splenic flexure of the large colon.
The function of the vagus nerve is to stimulate smooth muscle contraction and glandular secretions in these organs. For example, in the stomach, the vagus nerve increases the rate of gastric emptying, and stimulates acid production.
Clinical Relevance
Disorders of the vagus nerve, cardiovascular.
Many pharmacological agents can be used to potentiate vagal tone on the heart therefore slowing the heart rate. Beta-blockers, muscarinic agonists and cardiac glycosides such as Digoxin are just a few that can be used.
Vasovagal syncope can ensue during a period of emotional stress for example causing a sudden drop in blood pressure and heart rate. Further to this a carotid massage can compress the carotid sinus leading to the perception of a high blood pressure. This will cause CN X to increase its firing leading to a decreased activity of the SA node and AV node. Overall a decreased rate and strength of contraction will ensue and the person may experience syncope.
Many congenital heart defects such as a patent ductus arteriosus can irritate the left recurrent laryngeal nerve, leading to dysphonia (hoarse voice).
Gastro-Intestinal
Lesions to the CN X are rare. A lesion to the pharyngeal branches can lead to dysphagia (difficulty swallowing) due to the involvement with the muscles of the pharynx. As CN X innervates the Palatopharyngeus and Salpingopharyngeus muscles a lesion here will cause the Palatoglossal arch to drop leading to Uvula deviation away from the affected side. The CN IX is sensory to the oropharynx and laryngopharynx with CN X being the motor efferents involved in the Gag reflex therefore a lesion in this area will cause a loss of the Gag reflex.
Once upon a time a vagotomy could be done to reduce excess stomach acid production. However with advancements in pharmacological therapy this is no longer necessary.
As stated above a lesion to one of the RLN’s will cause dysphonia. A lesion to both RLN’s will cause aphonia (loss of voice) and a stridor (inspiratory wheeze). Paralysis of the RLN’s usually occur due to cancer of the larynx or thyroid gland or due to surgical complications.
Do you think you’re ready? Take the quiz below
Question 1 of 2
Recommended Reading
Forgot password.
Please enter your username or email address below. You will receive a link to create a new password via emai and please check that the email hasn't been delivered into your spam folder.
We use cookies to improve your experience on our site and to show you relevant advertising. To find out more, read our privacy policy .
Privacy Overview
Report question, rate this article.

The Wandering Neck
By Atom Bergstrom
Atom’s Blog
Say someone doesn’t get along with their father or any other male.
When Mind Hacking them (prone on the carpet or massage table), they will often move their head AWAY from the LEFT side by rotating their neck.
Say they don’t get along with their mother or any other female.
Now they often move AWAY from the RIGHT side.
“Anyone who has a trauma with both a man and a woman won’t need a neck adjustment from a chiropractor,” I used to joke.
However, a beginning Mind Hacker can get fooled.
Say someone wants to get closer to their father or any other male.
They often snuggle against their LEFT shoulder.
Say they want to get closer to their mother or any other female.
They often snuggle against their RIGHT shoulder.
Avoidance neck-turning versus nuzzling neck-turning are distinctly different body language “tells.”
Mind Hacking’s Cornerstone Technique will validate both of these “tell” types.
According to Carl Jung (1942) …
“The more remote and unreal the personal mother is, the more deeply will the son’s yearning for her clutch at his soul, awakening that primordial and eternal image of the mother for whose sake everything that embraces, protects, nourishes, and helps assumes maternal form, from the Alma Mater of the university to the personification of cities, countries, sciences and ideals.”
Atom Bergstrom is a Body & Organ Language specialist and promoter of Time Conscious Eating and Longevity Lifestyles, Gosta Ingvar “ATOM” Bergstrom was raised in New Jersey and the San Fernando Valley of Southern California. Atom has been teaching workshops and seminars across the U.S.A. since 1977. With over 50 years experience in health and nutrition, Atom has been counseling people with various diseases and ailments since the 70’s. His expertise is on nutrition, chronobiology, reflexology, slit-lamp iridology, meditation, Sufi, and I Ching and other holistic modalities. He graduated from Adano Ley’s Texas Institute of Reflex Sciences in 1979.
'The Wandering Neck' have 2 comments
December 6, 2022 @ 10:24 am John
Hi Atom, the mind hacking blogs are great, they really help to understand it more. Could you please do Mind Hacking Newsletter #2??
December 6, 2022 @ 4:55 pm Atom
Thanks, John!
I’m combining Mind Hacking with related subjects in my new journal, Mind Over Matter.
Would you like to share your thoughts? Cancel reply
You may also like..., color clearing.
October 29, 2023
14-Pound Joystick
October 17, 2023
Conspiracy Theorists?
September 29, 2023
©Copyright One Radio Network 2019 • All rights reserved. | Site built by Red Lotus Austin The information on this website and talk shows is solely for informational and entertainment purposes. IT IS NOT INTENDED TO PROVIDE MEDICAL ADVICE. Neither the Editors, producers of One Radio Network, Patrick Timpone, their guests or web masters take responsibility for any possible consequences from any treatment, procedure, exercise, dietary modification, action or application of medication which results from reading or following the information contained on this website in written or audio form, live or podcasts. The publication of this information does not constitute the practice of medicine, and this information does not replace the advice of your physician or other health care provider. Before undertaking any course of treatment, the reader must seek the advice of their physician or other health care provider and take total responsibility for his or her actions at all times. Patrick Joseph of the family of Timpone, a man...All rights reserved, without recourse.

- Health Sections Men Women Children Seniors Diabetes Cancer Asthma Blood Pressure Cholesterol Stroke Medicine & First Aid Head & Neck Heart & Lungs Digestive System Bones & Joints Hormones & Thyroid Food & Nutrition Fitness & Exercise Wellness Healthcare Financing Transplant
- Media News Video
Brain & Nervous System
Managing dementia behaviours: how to manage wandering.
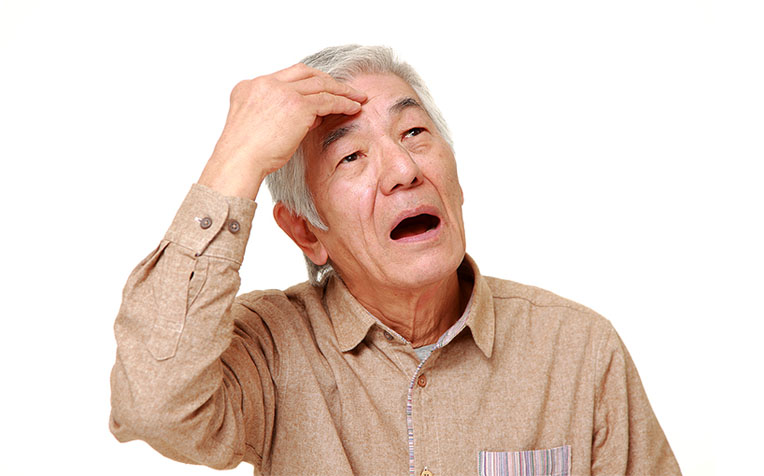
in persons with dementia occur due to disease progression and being unable to clearly differentiate between the past and present.
Behavioural changes in persons living with dementia can occur as a result of changes in their brain.
The Department of Psychological Medicine from Changi General Hospital (CGH), a member of the SingHealth group, explains the common symptoms displayed by persons with dementia and offers caregivers tips on how to better manage these behaviour changes when caring for their loved ones with dementia.
Wandering behaviour in persons with dementia
Wandering is a common behaviour observed amongst persons with dementia that can put them at risk while also attributing great stress to their caregivers.
Persons with dementia who wander risk getting lost when they wander off. Getting lost can be dangerous for them as they may run into accidents or injuries.
Wandering also increases fall risk. Persons with dementia are generally at a higher risk of falling due to the damage in the brain caused by dementia.
3 Tips to manage wandering behaviour in persons with dementia
Depending on the personality of the person with dementia and how well they are able to cope, their reasons for wandering and the safety of their surrounding environment, you can consider the following management strategies.
Persons with dementia are also at fall risk as dementia can affect their gait. It is best for them to have some supervision if their gait is unsteady.
1. Take note of when wandering takes place
When caring for a loved one with dementia, identify his/her wandering behaviour by keeping records or a diary (e.g., does the behaviour show up at certain times of the day or in response to certain situations which can be carefully controlled?).
Ensure that the person with dementia carries identification such as an identity bracelet or card with his/her name, address and/or contact numbers of family members. This can be helpful when the person with dementia is found by others or by the police.
2. Remove the necessity to wander
Reduce access to objects that may prompt or encourage a person with dementia to wander (e.g., handbags, house keys).
Remove any obstacles to allow the person with dementia to move about safely such as coffee table, loose wires, toys, etc. Ensure supervision is available and that he/she has a walking aid nearby at all times.
Other common strategies include hiding the door knobs or door handles. Sometimes the door can be painted the same colour as the wall, so it is ‘invisible’, or a curtain can be put over the door so it does not look like the door.
3. Distract and promote familiarity
Engage or distract the person with dementia with a simple and quiet activity from earlier days that is familiar to him/her.
Orientate the person over the course of the day. Orientation to the time, date, place and people helps to reduce anxiety in persons with dementia.
What to do when the person with dementia goes missing
Remain calm.
Do a thorough search of the house and familiar places.
Try to recall what they were wearing.
Walk or drive around the vicinity and to other places that they visit regularly. Have someone stay at home in case they return home, or to answer any phone calls.
Contact the police if immediate searches yield no result. Tell them that the person has dementia and highlight any concerns you may have for their safety.
What to do when the person with dementia returns home
Notify the police immediately.
Do not scold or show any anxiety as this may confuse or frighten them.
Provide reassurance and get them back into their regular routines as quickly as possible.
Possible reasons for wandering behaviour in persons with dementia
The inability to recall where he/she was going or why.
Disorientation in the environment – the person with dementia may get lost in his/her own home.
Disorientation with the past and present – when the person with dementia becomes confused and search for someone or something related to his/her past.
Disease progression of dementia – the person with dementia loses the ability to concentrate and wandering keeps him/her occupied.
About BPSD (Behavioural and psychological symptoms of dementia)
Behavioural and psychological symptoms of dementia (BPSD) are neuropsychiatric symptoms and behaviours displayed by persons with dementia .
These symptoms constitute a huge aspect of dementia irrespective of its subtype, and they demonstrate a strong correlation with the degree of functional and cognitive impairment.
Learn how to manage anger and aggression , click here .
Learn how to manage apathy , click here .
Learn h ow to manage inappropriate (disinhibited) behaviours , click here .
Learn how to manage hallucinations , click here .
Learn how to manage paranoia and delusion , click here .
Learn how to manage repetition (repetitive behaviour) , click here .
Ref: H24

Terms of Use / Disclaimer All information provided within this web and mobile application is intended for general information and is provided on the understanding that no surgical and medical advice or recommendation is being rendered. Please do not disregard the professional advice of your physician.
Sharing is caring!

Sign up today!
MyEyeGym App
What is Allergic Rhinitis?
Trending Now
No Meat? Try These For Protein!
Rotavirus and Gastroenteritis in Children
What Causes Hand Tremors?
Asthma - Doctor Q&A
Chronic Pelvic Pain: Causes
Minimallly Invasive Spine Surgery: When Is It Needed?
You May Also Like
Managing Dementia Behaviours: How to Manage Sundowning
Managing Dementia Behaviours: How to Manage Paranoia and Delusion
Managing Dementia Behaviours: How to Manage Repetition
Managing Dementia Behaviours: How to Manage Hallucinations
Did You Know?
Our Contributors
- Terms & Conditions
- Privacy Policy
- Personal Data Protection Act (PDPA)
- Report Vulnerability
- View All Systems
- Anatomy Systems
- Cardiovascular
- Respiratory
- Integumentary
- View All Telehealth
- Online Pharmacies
- Hims Review
- Keeps Review
- Keeps vs Hims
- BlueChew Review
- Rugiet Review
- Hims ED Review
- Online Therapy
- BetterHelp Review
- BetterHelp vs Talkspace
- View All Testing
- General Health Tests
- Best DNA Health Test
- Best Microbiome Test
- Viome Review
- Best At-Home Herpes Test
- STDcheck Review
- View All Self-Care
- Hair and Hair Loss
- Best Hair Loss Treatment for Men
- Best Laser Cap for Hair Loss
- Kiierr Laser Cap Review
- Nutrition Guide
- Found Weight Loss Review
- Relationships
- Best STD Dating Websites
- Best Herpes Dating Websites
- Sexual Health
- Best Erectile Dysfunction Treatment
- Best Delay Spray
- Best Prostate Massager
- BlueChew Free Trial
- Best CBD for Arthritis
- Best Incontinence Underwear for Women
- Best Incontinence Underwear for Men
- All Health Products
- Best Amino Acid Supplements
- Best Muscle Building Stack
- Best NMN Supplement
- Best NAC Supplement
- Best NAD Supplement
- Best Berberine Supplement
- Mood and Energy
- Best Nootropics
- Best Saffron Supplement
- Fitness and Weight
- Vital Reds Review
- Total Restore Review
- Best Testosterone Booster
- Best Male Enhancement Pills
- Best Volume Pills
- View All Research
- Skeletal System
- Muscular System
- Cardiovascular System
- Digestive System
- Nervous System
- Respiratory System
- Urinary System
The Nerves of the Head and Neck
- 2D Interactive
- NEW 3D Rotate and Zoom
Anatomy Explorer
- 1st Cervical Nerve
- Anterior Ethmoidal Nerve
- Auriculotemporal Nerve
- Brain Cortices
- Buccal Nerve
- Chorda Tympani Nerve
- Ciliary Ganglion
- Ears and Hearing
- Eyes and Vision
- Frontal Nerve
- Inferior Alveolar Nerve
- Inferior Dental Plexus
- Lingual Nerve
- Mandibular Nerve
- Mylohyoid Nerve
- Nose, Sinuses and Smell
- Otic Ganglion
- Skin Cross-Section
- Spinal Nerve Cross-Section
- Superior Alveolar Branch of Infraorbital Nerve
- Supraorbital Nerve
- Tentorial Branch of Opthalmic Nerve
- Tongue and Taste
Change Current View Angle
- Nerves of the Head and Neck (2nd Anterior View)
Toggle Anatomy System
- Cardiovascular System of the Head and Neck
- Digestive System of the Head and Neck
- Endocrine Glands of the Head and Neck
- Immune and Lymphatic Systems of the Head and Neck
- Integumentary System of the Head and Neck
- Muscles of the Head and Neck
- Respiratory System of the Head and Neck (Anterior Cross-section View)
- Bones of the Head and Neck
Anatomy Term
Displayed on other page

The nerves of the head and neck include the most vital and important organs of the nervous system — the brain and spinal cord — as well as the organs of the special senses. In addition, in this region we also find the major cranial and spinal nerves that connect the central nervous system to the organs, skin, and muscles of the head and neck. These structures all work together to control every part of the body and receive sensory messages from the environment and the body’s internal structures.
The brain is a grayish, highly convoluted organ found within the skull’s cranial cavity.mycontentbreak The brain weighs in at around three pounds on average, making it one of the most massive organs in the human body. Around 100 billion neurons in the gray matter of the brain control almost all of the body’s activities, including the conscious activities of the mind and the subconscious activities that control the organs and lower bodily processes. The interior of the brain contains mostly white matter that connects the processing areas of gray matter to each other and to all of the muscles and sensory receptors in the body. Yet being an extremely complex organ, the brain can be further divided into many anatomically distinct regions with distinct functions.
- The base of the brain that connects to the spinal cord is the brain stem. Lower brain functions related to breathing, heart rate, and reflexes are controlled by the brain stem.
- The cerebellum is a round, wrinkled mass of neurons posterior to the brain stem that controls coordination and balance.
- Superior to the brain stem is the diencephalon, which controls the endocrine system, relays messages to and from the higher regions of the brain, and regulates feelings of hunger and thirst.
- The largest, most superior, and highest functioning region of the brain is the cerebrum. All of the voluntary functions of the body, along with memory, creativity, and emotions are products of the neurons in the gray matter of the cerebrum. A large crease splits the cerebrum into left and right hemispheres, which monitor and control opposite sides of the body and maintain slightly varied but parallel functions within the brain.
Extending from many different regions on the inferior side of the brain, twelve pairs of cranial nerves provide direct connections between the brain and important structures of the head, neck, and trunk. The sensory organs of the head use the cranial nerves for signal transmission, including smell (olfactory nerve), vision (optic, oculomotor, abducens, and trochlear nerves), taste (facial and glossopharyngeal nerves) and hearing (vestibulocochlear nerve). The muscles of the head and neck are also controlled by various cranial nerves including the facial nerve (facial expression) and accessory nerve (head and neck movements). Wandering through the neck and torso, the vagus nerve communicates vital information from the brain to the heart and intestines.
The spinal cord is a thick nerve trunk that forms the brain’s most important connection to the body and carries all signals to and from the brain that are not provided by the cranial nerves. The spinal nerve extends from the inferior end of the brain stem and passes through the foramen magnum of the skull into the neck. In the neck, the spinal cord passes through the vertebral foramen of the cervical vertebrae, which surround and protect its delicate nervous tissue. Eight spinal nerves branch off from the spinal cord in the neck to form a network of nerves called the cervical plexus. The cervical plexus forms many connections between the brain and the skin and muscles of the head and neck, similar to the cranial nerves. A vital connection from the cervical plexus to the diaphragm is formed by the phrenic nerve, allowing the brain to control breathing.
Damage to any part of the spinal cord may cause a loss of sensation and/or motor function below the injury; however, such injuries are most dangerous within the neck as they are likely to affect a greater area of the body and are more likely to result in death. The fatal result of damage to the pathway between the brain and the diaphragm is respiratory arrest, a condition where the diaphragm stops moving, thereby failing to move fresh air into the lungs.
Other Recommended Resources
- BetterHelp Reviews
- Best Laser Cap For Hair Loss
- Microbiome Test
- STDcheck Reviews
You are using an outdated browser. Please upgrade your browser to improve your experience and security.

- Buy Tickets
- Join & Give
Wandering Whistling-Duck
- Updated 28/07/23
- Read time 2 minutes

- IUCN Conservation Status LEAST CONCERN (LC)
- Classification Genus Dendrocygna Species arcuata Family Anatidae Order Anseriformes Class Aves
- Size Range 55 cm to 60 cm
Wandering Whistling-Ducks are gregarious when not breeding, and form large flocks of up to thousands of individuals. They often flock with Plumed Whistling-Ducks.
What do Wandering Whistling-Ducks look like?
Identification.
The Wandering Whistling-Duck is a large duck with rich red-brown plumage overall, with a paler face, front of neck and upper breast. There is a dark stripe on the crown of head, nape and back of neck. The bill and legs are dark. There are elongated flank plumes, which are off-white with chestnut edges. In flight, the dark underwings, cinnamon and chestnut underbody, white undertail and trailing dark legs are seen. This species is also known as the Whistling Tree-Duck, Water Whistling-Duck and the Red Whistler.
Where do Wandering Whistling-Ducks live?
The Wandering Whistling-Duck prefers deep vegetated lagoons and swamps, flooded grasslands, sewerage farms, grain stubbles, pastures, irrigated lands and ricefields. It prefers deeper waters where aquatic plants and insects are plentiful.
Distribution
The Wandering Whistling-Duck is found in northern and eastern Australia, from the Kimberley region, across the north of Australia, to south-eastern New South Wales. It is vagrant to the south-east and the south-west of the country. This species is also distributed through Indonesia, Papua New Guinea, the Philippines and the Pacific Islands.
What do Wandering Whistling-Ducks eat and how do they communicate?
Feeding and diet.
The Wandering Whistling-Duck feeds almost entirely on aquatic vegetation and seeds, but also on young grass, the bulbs of rushes and other herbage, insects and other small aquatic animals. Wandering Whistling-Ducks forage in tight flocks, with the birds in front diving, and those behind flying over them.
Communication
Shrill twittering, whistling, especially noisy with almost incessant whistling when flocks are airborne.
What are Wandering Whistling-Ducks breeding behaviours?
Breeding behaviour/s.
The Wandering Whistling-Duck breeds in the northern Wet Season. The nest is a scrape in the ground out of reach of rising floodwaters, and is hidden in tall grass or shrubbery and lined with grass. Wandering Whistling-Ducks are monogamous, and pair-bonds are most likely life-long. Not much is known about the incubation of the eggs and brooding of the young.
Breeding Season: January to April.
Seasonality
The most obvious movement is the dispersal of flocks when there is rain from dry season refuges beside permanent water to ephemeral inland breeding swamps and coastal sites.
Economic/social impacts
Wandering Whistling-Ducks are often found in grain-growing areas where there are permanent artificial waterbodies. Their preferred floodplain systems may potentially be threatened by future agricultural, pastoral or urban development.

The Australian Museum respects and acknowledges the Gadigal people as the First Peoples and Traditional Custodians of the land and waterways on which the Museum stands.
Image credit: gadigal yilimung (shield) made by Uncle Charles Chicka Madden

- View history
A list of every character in the game.

All items (92)


DWR reminds public of mountain lion safety

As the weather warms up and more animals are wandering into neighborhoods and populated areas, the Division of Wildlife Resources is reminding locals about mountain lion safety.
The large cats, also known as cougars or pumas, can be found throughout Utah.
While attacks are fairly rare, the DWR has a few simple steps you can follow to stay safe around wildlife this summer.
Never run from a cougar, maintain eye contact while in sight of the animal and stand up tall to make yourself look bigger.
If the mountain lion does attack, fight back and protect your head and neck.
When hiking, the DWR says not to go alone and avoid using headphones that block out your surroundings.

Man accused of randomly assaulting strangers indicted on hate crime charges

The man who was arrested for allegedly randomly hitting a TikToker walking down a New York City street has been charged with assaulting, stalking and harassing strangers in a series of alleged anti-female, anti-white and antisemitic incidents, according to Manhattan District Attorney Alvin L. Bragg, Jr.
Skiboky Stora, 40, of Brooklyn, has been charged with three counts of third-degree assault as a hate crime, one count of stalking as a hate crime and second-degree aggravated harassment for incidents between September of 2023 and March 2024.
"Skiboky Stora allegedly committed a series of hate-motivated incidents against several individuals based on their perceived gender, race and religion," said District Attorney Bragg. "Much of what defines our city is respect and acceptance of all people. Nobody should have to fear for their safety because of their identity. I thank our prosecutors for their unwavering commitment in seeking justice for these victims."
The charges come after 7 TikTok users reported being punched in New York in a matter of two weeks , according to police, though they said there was no evidence the incidents were related. One of the TikTokers is among the victims mentioned in Stora's list of charges.
On Sept. 20, 2023, a 17-year-old white student walked past Stora in the Chelsea neighborhood, officials say. As he passed, Stora allegedly elbowed him in the neck, causing pain, and stated, in substance: "You people think you can do whatever the f--- you want," Bragg said in a statement.
On Oct. 26, 2023, a 37-year-old fair-skinned woman walked past Stora in the Chelsea neighborhood, according to Bragg. As the woman passed Stora, officials say Stora allegedly elbowed the woman's left shoulder, causing pain and bruising.
On Nov. 18, 2023, a 28-year-old woman and her 28-year-old husband, a white, Jewish couple, were walking their dogs in Union Square when they saw Stora tearing down posters of kidnapped Israeli hostages. The woman reported taking a picture of him and Stora allegedly then began to follow them and shout anti-white and antisemitic remarks, including, "F--- you, white boy." A passerby led the couple inside their apartment building so they could get away from Stora, but he allegedly followed them into the building lobby, yelling antisemitic slurs in substance, according to Bragg.
On March 25, 2024, a 23-year-old white woman passed Stora on the street and he allegedly struck her in the head which caused her to fall to the ground, officials say. She is reported to have suffered pain and swelling on the left side of her head.
Stora was arrested shortly after an investigation by the NYPD Hate Crimes Task Force and the Manhattan District Attorney's Office.
ABC News' Aaron Katersky contributed to this report.
Related Topics
Top stories.

Thousands of Houston-area residents still without power after storm
- 42 minutes ago

ABC13 Weather Watch for thunderstorms Wednesday
- 10 minutes ago

3 suspects in custody after police witness shooting, HPD says

HPD investigating whether alligator killed woman in Clear Lake

Homeowner says school construction changed water flow, flooded yard
16-year-old killed when Magnolia new-construction homes collapse
Hurricane season starts Saturday. Here's how you can stay prepared
- 2 hours ago
Deepfake AI scams to look out for and how to protect yourself

IMAGES
VIDEO
COMMENTS
Wandering Neck (Japanese: 彷徨う首 Samayō kubi) is a character featured in Deep Fancy Island where she mainly appears in Deeprouka.html. Wandering Neck appears as a pale woman with long black hair covering her face, black lips, black eyes and thick black eyebrows. In her human appearance, she has a body and wears a school outfit which looks nearly identical to J-ker's. She has tidier and ...
"Vagus" is the Latin word for wandering. Your vagal nerves take a long, winding course through your body. They exit from your medulla oblongata in your lower brainstem. Then, the nerves pass through or connect with your: Neck (between your carotid artery and jugular vein). Chest (thorax). Heart. Lungs. Abdomen and digestive tract.
How does one come to a condition of Cervicovagopathy or wandering floating neck bones? This condition is caused by weakened, loose, and damaged cervical spine ligaments. Ligaments are the soft-tissue structure that holds the vertebrae in place. When these ligaments no longer hold the vertebrae in place the structure of the neck falters and the ...
The name "vagus" comes from the Latin term for "wandering." This is because the vagus nerve wanders from the brain into organs in the neck, chest, and abdomen. It is also known as the 10th ...
(A wandering neck when the girl with the V sign in the fallen photo was alive. The other is J-ker.) Secret01. 何回か描き直したミイラ男の変遷の様子。(画像クリックでスライド) The appearance of the change of the mummy man who has been redrawn several times. (Click the image to slide.)
Deeprouka.html is a page featured in Deep Fancy Island. It is accessed via the alternate route in Deepindox.html. The page contains a long hallway with circular lights above. Clicking anywhere will let the player go down the hallway and proceed towards the door at the end. Just before the door becomes visible, Wandering Neck will suddenly appear in front of the player, though she will not kill ...
Lazy eye (amblyopia) is reduced vision in one eye caused by abnormal visual development early in life. The weaker — or lazy — eye often wanders inward or outward. Amblyopia generally develops from birth up to age 7 years. It is the leading cause of decreased vision among children. Rarely, lazy eye affects both eyes.
Exposing the neck. What It Means: If a person makes an attempt to elongate their neck or expose the side of their neck to you, it may mean "I feel vulnerable" or "I'm flirting with you.". Neck exposing is more common among couples early in a relationship. Just imagine: 2 strangers meet after hooking up on Tinder.
Noonan syndrome is a genetic condition that stops typical development in various parts of the body. It can affect a person in several ways, including unusual facial features, short height, heart problems and other physical problems. It also can cause a child to develop more slowly than usual, for example, in walking, talking or learning new things.
A photo of J-ker (left) and Wandering Neck (right) when they were still alive. After following the alternative puzzle hinted from the first kanji, the player is redirected to Deepdashtwoes.html, which features four sections in a room. Initially, the player encounters a door sealed by a ghost. Clicking right leads to a room with an incomplete ...
It is sometimes referred to as the wandering nerve. In the Head. The vagus nerve originates from the medulla of the brainstem. ... In the Neck. In the neck, the vagus nerve passes into the carotid sheath, travelling inferiorly with the internal jugular vein and common carotid artery. At the base of the neck, the right and left nerves have ...
Snowy albatross. The snowy albatross ( Diomedea exulans ), also known as the white-winged albatross or goonie, is a large seabird from the family Diomedeidae; they have a circumpolar range in the Southern Ocean. It is the most recently described species of albatross and was long considered to be the same species as the Tristan albatross and the ...
The wandering whistling duck (Dendrocygna arcuata) is a species of whistling duck. They inhabit tropical and subtropical Australia, the Philippines, Borneo, Indonesia, Papua New Guinea and the Pacific Islands. ... They have a strong head and neck with a darker crown and hindneck. The breast contains black spotting and the feathers are mostly ...
Wandering Neck. Wandering Neck (Japanese: 彷徨う首 Samayō kubi) is a character featured in Deep Fancy Island where she mainly appears in Deeprouka.html. Wandering Neck appears as a pale woman with long black hair covering her face, black lips, black eyes and thick black eyebrows. In her human appearance, she has a...
Rokurokubi from the Hokusai Manga by Katsushika Hokusai Nukekubi, from Bakemono no e scroll, Brigham Young University.. Rokurokubi (ろくろ首, 轆轤首) is a type of Japanese yōkai (apparition). They look almost completely like humans with some differences. There is a type whose neck stretches and another whose head detaches and flies around freely (nukekubi).
The vagus nerve, or the 10th cranial nerve (CN X), is the longest and most complex of the cranial nerves. The vagus nerve differs slightly as it primarily supplies the organs of the chest and abdomen, as opposed to the head and neck. It is called "vagus" as it is a vagrant or wandering nerve going down to the abdomen.
The Wandering Neck. By Atom Bergstrom. Atom's Blog. Say someone doesn't get along with their father or any other male. When Mind Hacking them (prone on the carpet or massage table), they will often move their head AWAY from the LEFT side by rotating their neck. Say they don't get along with their mother or any other female.
3. Distract and promote familiarity. Engage or distract the person with dementia with a simple and quiet activity from earlier days that is familiar to him/her. Orientate the person over the course of the day. Orientation to the time, date, place and people helps to reduce anxiety in persons with dementia.
Appearance. Formerly named tree ducks, the wandering whistling duck has its new name because of their loud whistling calls and the whistling noise their wings make during flight. They have long necks and legs and look like a cross between a goose and a duck. They have a strong head and neck with a darker crown and hindneck.
J-ker is also mentioned in Deeparchive.html in Wandering Neck's file, stating that Wandering Neck still wanders to find her lost friend J-ker and her own body. Trivia [] In the 2nd Volume of the LINE Stickers, J-ker wears a similar school uniform, but she is not covered in blood and is wearing a surgical mask. ...
The muscles of the head and neck are also controlled by various cranial nerves including the facial nerve (facial expression) and accessory nerve (head and neck movements). Wandering through the neck and torso, the vagus nerve communicates vital information from the brain to the heart and intestines. The spinal cord is a thick nerve trunk that ...
The Wandering Whistling-Duck is a large duck with rich red-brown plumage overall, with a paler face, front of neck and upper breast. There is a dark stripe on the crown of head, nape and back of neck. The bill and legs are dark. There are elongated flank plumes, which are off-white with chestnut edges. In flight, the dark underwings, cinnamon ...
A list of every character in the game. 4. 404'san. A. Abyss. Adogosu. Aikokun. Akai Sukato no Onnanoko. User blog:ALittleSillyAtTimes/Kapibara Onna (OC)
If the mountain lion does attack, fight back and protect your head and neck. When hiking, the DWR says not to go alone and avoid using headphones that block out your surroundings. As the weather warms up and more animals are wandering into neighborhoods and populated areas, the Division of Wildlife Resources is reminding locals about mountain ...
Tuesday, May 28, 2024 9:00PM. The man who was arrested for allegedly randomly hitting a TikToker walking down a New York City street has been charged with assaulting, stalking and harassing ...