Home > Blog > Psychiatry CPT Codes - A Complete Guide (+Cheat Sheet)


Psychiatry CPT Codes - A Complete Guide (+Cheat Sheet)
Courtney Gardner, MSW

Hate writing progress notes? Join thousands of happy therapists using Mentalyc AI.
Are you tired of feeling intimidated by the maze of complex CPT codes associated with psychiatry? Don't worry, you're not alone! Understanding psychiatry and CPT codes can be demanding. However, with our exclusive cheat sheet, you'll have everything you need to confidently navigate psychiatry's most common behavioral health codes, from diagnostic and evaluation codes to intake, outpatient mental health, and psychotherapy codes! In this post, you'll discover the secrets behind these codes, why they matter, and how to find them. Prepare to conquer the world of psychiatry CPT codes with ease and excitement!
Understanding CPT Codes for Psychiatry Providers
You must thoroughly understand the CPT code system if you are a psychiatrist. CPT, or Current Procedural Terminology, is a system developed by the American Medical Association (AMA) that provides a standard and consistent language for describing medical, surgical, and diagnostic procedures. These codes allow you to communicate your services to insurers and receive fair payment for your work. They also help establish medical necessity, track patient health over time, and produce diagnostic data for research.
Diagnostic Interview, Testing, and Evaluation CPT Codes
Diagnostic CPT codes are a crucial part of the medical billing process. To assess your patients ' correct diagnostic and evaluation CPT codes, thoroughly review their medical and mental health histories. Select the code that most accurately reflects the level of care provided during each session.
Initial Diagnostic Interview
Initial diagnostic CPT codes assess a patient's mental state, history, and recommended treatment. Additionally, a second code is used if medical services were provided along with the psychological evaluation , such as prescribing medications , conducting physical exams, or modifying psychiatric treatment.
- 90791 ( Psychiatric diagnostic evaluation without medical services)
- 90792 (Psychiatric diagnostic evaluation with medical services carried out by a physician)
Developmental and Behavioral Testing
Developmental and behavioral testing codes involve a quick evaluation of emotions and behavior using standard instruments like a depression inventory or ADHD scale. The code also includes the time spent scoring and documenting the results.
- 96127 (Use this code for each screening instrument completed)
Psychological and Neuropsychological Testing
A physician or qualified healthcare professional does a neurobehavioral status exam. This exam may include a clinical assessment of thinking, reasoning, and judgment, such as acquired knowledge, attention, language, memory, planning and problem-solving, and visual-spatial abilities.
- 96116 (This code covers one hour of testing and includes test interpretation and reporting)
- 96121 (Use this code for each additional hour of the neurobehavioral status exam)
Psychological Test Evaluation
A physician or qualified healthcare professional does psychological test evaluation. Evaluation can include interpreting standardized test results, clinical decision-making, integrating patient data, treatment planning, and providing feedback to the patient, family, or caregiver.
- 96130 (Use this for the first hour of testing)
- 96131 (Use this code for each additional hour; list it separately in addition to 96130)
Neuropsychological Test Evaluation
These codes cover a wide range of psychological tests such as IQ tests, achievement tests, personality tests, and vocational assessments. A physician or qualified healthcare professional must carry it out.
- 96132 (Use this for the first hour of evaluation)
- 96133 (Use this code for each additional hour of psychological test evaluation; list it separately in addition to 96132)
Outpatient Mental Health CPT Codes
Outpatient Mental Health CPT codes cover individual, family, and group therapy. These are the bread and butter of most mental health practices. The codes in this category describe the type of therapy, session length, and whether evaluation and management services were provided.
Individual Therapy
These are for insight-oriented, behavior-modifying, and supportive psychotherapy.
- 90832 (Psychotherapy, 16-37 minutes)
- 90833 (Psychotherapy and an evaluation and management service in the same session, 16-37 minutes)
- 90834 (Psychotherapy , 38-52 minutes)
- 90836 (Psychotherapy and an evaluation and management service in the same session, 38-52 minutes)
- 90837 (Psychotherapy , 53+ minutes)
- 90838 (Psychotherapy and an evaluation and management service in the same session, 53+ minutes)
Family Therapy
These codes can only be used when therapy focuses on the family unit . If you see family members together but the treatment primarily focuses on an individual, use the individual psychotherapy codes.
- 90846 (Family psychotherapy without the patient present, 50 minutes)
- 90847 (Family psychotherapy with the patient present, 50 minutes)
Group Therapy
These codes are used for group psychotherapy regardless of the number of patients in the group. You can only bill for one unit of 90853 per group session.
- 90849 (Group psychotherapy, most commonly used in family or couples sessions)
- 90853 ( Group psychotherapy involving three or more patients, no more than twelve, and is often used for general psychotherapy groups)
Extender Codes for Longer Sessions
- 90833 (0-30 minutes longer; used with 90837)
- 99354 (30- 47 minutes longer; used with 90837)
- 99355 ( for each additional 30-minute period; used with 99354)
CPT Crisis Codes
- 90839 (Psychotherapy for crisis, 30-74 minutes)
- 90840 (Add on code for an additional 30 minutes, for 75+ minutes. Used in conjunction with 90839)
Evaluation and Management CPT Codes
These codes cover evaluating a patient's condition and adjusting medications as needed.
- 99201 (Office/outpatient visit, new patient, 10 minutes)
- 99202 (Office/outpatient visit, new patient, 20 minutes)
- 99203 (Office/outpatient visit, new patient, 30 minutes)
- 99204 (Office/outpatient visit, new patient, 45 minutes)
- 99205 (Office/outpatient visit, new patient, 60 minutes)
- 99211 (Office/outpatient visit, established patient, 5 minutes)
- 99212 (Office/outpatient visit, established patient, 10 minutes)
- 99213 (Office/outpatient visit, established patient, 15 minutes)
- 99214 (Office/outpatient visit, established patient, 25 minutes)
- 99215 (Office/outpatient visit, established patient, 40 minutes)
Navigating the complex world of psychiatry CPT codes doesn't have to overwhelm you. Armed with this cheat sheet of the most common behavioral health codes, you now have a handy reference to consult whenever you need to assign codes to your services. Finding and selecting the correct codes will make your billing processes smoother. The CPT manual may seem dense initially, but with some practice, you'll soon be unstoppable in pairing your psychiatry notes with the correct 5-digit CPT codes. Refer to this guide the next time you're scratching your head over how to code a service.
Also, if you need extra support, Mentalyc can turn your session recordings into completed progress notes with codes, giving you more time to focus on your clients. Try a free trial today!
FAQ: Psychiatry CPT Codes Questions Answered
What are the most common Psychiatry CPT codes?
The CPT codes you'll likely use the most in your practice are:
- 90833: Psychotherapy, 30 minutes with patient and/or family member
- 90834: Psychotherapy, 45 minutes with patient and/or family member
- 90837: Psychotherapy, 60 minutes with patient and/or family member
- 90853: Group psychotherapy
How often can I bill 90833, 90834, and 90837?
You can bill these codes for each separate session with a patient. For example, if you see a patient for 30 minutes on Monday and 45 minutes on Wednesday, you would bill 90833 for the first session and 90834 for the second session. The only limit is that you can't bill for two sessions on the same day.
What's the difference between 90833, 90834 and 90837?
These codes differ based on the length of the session:
- 90833: 30-minute session
- 90834: 45-minute session
- 90837: 60-minute session
Remember to choose the code that matches how long you spent providing psychotherapy or counseling to the patient during that session.
Do I need to worry about medical necessity for psychiatry CPT codes?
Yes, medical necessity is an essential concept for billing psychiatry CPT codes. Your services must be medically necessary to diagnose and treat a patient's behavioral health condition. You'll need to document how the patient meets the criteria for a diagnosis and how your treatment addresses specific symptoms. Medical necessity helps ensure insurance will cover and pay for the services.
Do I have to use CPT codes?
Yes, if you want to bill insurance. CPT codes are mandated by Medicare and adopted by all major insurance carriers.
How often do CPT codes change?
Annually, on January 1st. The AMA publishes an updated CPT manual each year.
What's the difference between CPT and ICD codes?
CPT codes refer to medical procedures and services. ICD codes refer to diagnoses and health conditions. Both are needed for billing.
- American Psychological Association. (2018, November 26). Home Practice Reimbursement CPT and Diagnostic Codes Psychotherapy Codes for Psychologists . APA Services. https://www.apaservices.org/practice/reimbursement/health-codes/psychotherapy
- Centers for Medicare & Medicaid Services. (n.d.). Billing and Coding: Psychiatry and Psychology Service . https://www.cms.gov/medicare-coverage-database/view/article.aspx?articleId=57480
- Dotson, P. (2013, December). CPT® Codes: What Are They, Why Are They Necessary, and How Are They Developed? PubMed Central. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3865623/#:~:text=Category%20I%20service%20and%20procedure,January%201st%20or%20July%201st
- Grohol, J. M. (2022, March 30). CPT Codes for Psychotherapy and Other Psychology Services . Psych Central. https://psychcentral.com/lib/cpt-codes-for-psychology-services
All examples of mental health documentation are fictional and for informational purposes only.
See More Posts
7 benefits of starting your own private practice, process vs. content in therapy, tips for supervising mft interns in mental health private practice.

Mentalyc Inc.

Copyright © 2021-2024 Mentalyc Inc. All rights reserved.
Meet the team
About our notes
Feature Request
Privacy Policy
Terms of Use
Business Associate Agreement
Contact Support
Affiliate program
Who we serve
Psychotherapists
Group practice owners
Pre-licensed Clinicians
Become a writer
Help articles
Client consent template
How to upload a session recording to Mentalyc
How to record sessions on Windows? (For online sessions)
How to record sessions on MacBook? (For online sessions)
Popular Blogs
Why a progress note is called a progress note
The best note-taking software for therapists
Writing therapy notes for insurance
How to keep psychotherapy notes compliant in a HIPAA-compliant manner
The best Mental health progress note generator - Mentalyc

TheraThink.com
A mental health billing service, mental health cpt codes: the definitive guide [2024].
CPT (Current Procedural Terminology) is a standardized medical codeset maintained by the AMA. CPT codes are five digit numeric codes describing everything from surgery to radiology to psychotherapy.
CPT Codes are different from Diagnosis Codes or ICD10 F-Codes for billing and coding your insurance claims. Here’s our mental health diagnosis code list if you need to look one up.

For therapists that are on managed care panels or provide superbills to their clients, knowing your CPT codes is paramount to getting paid in full and avoiding insurance audits.
The amount insurance companies will reimburse depends on a number of different factors (professional credentials, geographic location, etc.), but using the correct CPT Code and add-on code(s) to express the exact service is an important part to the whole process and in ultimately determining your payment!
Errors, accidental or otherwise, will directly impact insurance company’s payment of services. If you need help with making sure your billing and coding is error-free, our mental health billing service can help.
Think about reaching out if the rest of this article hurts your feelings.
Article Index:
- Most Common Mental Health CPT Codes
- Add-On CPT Codes for Mental Health Billing
- Mental Health CPT Code Cheat Sheet [PDF]
- Testing & Evaluation CPT Codes
- Psych and Evaluation and Management (E/M) Codes
- Sample Reimbursement Rates by License Type
- Sample Reimbursement Rates by CPT Code
The Most Common Mental Health CPT Codes
The most common CPT Codes used by therapists and behavioral health professionals:
Outpatient Mental Health Therapist Diagnostics, Evaluation, Intake CPT Code:
- 90791 – Psychiatric Diagnostic Evaluation ( usually just one/client is covered )
Outpatient Mental Health CPT Codes :
- 90832 – Psychotherapy, 30 minutes ( 16-37 minutes ).
- 90834 – Psychotherapy, 45 minutes ( 38-52 minutes ).
- 90837 – Psychotherapy, 60 minutes ( 53 minutes and over) .
- 90846 – Family or couples psychotherapy, without patient present.
- 90847 – Family or couples psychotherapy, with patient present.
- 90853 – Group Psychotherapy ( not family ).
- 98968 – Telephone therapy (non-psychiatrist) – limit 3 units/hours per application.
Outpatient Mental Health Crisis CPT Codes :
- 90839 – Psychotherapy for crisis, 60 minutes ( 30-74 minutes ).
- +90840 – Add-on code for an additional 30 minutes ( 75 minutes and over ). Used in conjunction with 90839.
Other Behavioral Health CPT Codes :

- 90404 – Cigna / MHN EAP CPT Code. These two companies use a unique CPT code for EAP sessions.
- 96101 – Psychological testing, interpretation and reporting by a psychologist (per Hour)
- 90880 – Hypnotherapy – limit 10 units/hours per application
- 90876 – Biofeedback
- 90849 – Multiple family group psychotherapy
- 90845 – Psychoanalysis
Mental Health Add-On CPT Codes
Here is a short list of the most common Add-On codes for routine outpatient mental health billing.
- Add-On CPT Code 90785 – Interactive complexity. Example: play therapy using dolls or other toys. This is an interactive complexity add-on code that is not a payable expense. This code only indicates that the treatment is complex in nature.
- Add-On CPT Code 90863 – Pharmacologic Management after therapy.
- Add-On CPT Code 99050 – Services provided in the office at times other than regularly scheduled office hours, or days when the office is normally closed.
- Add-On CPT Code 99051 – Services provided in the office during regularly scheduled evening, weekend, or holiday office hours.
- Add-On CPT Code 99354 – Additional time after the additional time of 74 minutes. Adding another 30 minutes. (Only use if the duration of your session is at least 90 minutes for 90837 or 80 minutes for 90847).
- Add-On CPT Code 99355 – Additional time after first 60 minutes. First additional 30 to 74 minutes.
- Add-On CPT Code 90840 – 30 additional minutes of psychotherapy for crisis. Used only in conjunction with CPT 90839.
- Add-On CPT Code 90833 – 30 minute psychotherapy add-on. Example: Psychiatrist evaluates medication response, then has 30 minute session.
- Add-On CPT Code 90836 – 45 minute psychotherapy add-on. Example: Clinical Nurse Specialist evaluates medication response, then has 45 minute session.
If you’re wondering how to handle billing add-on codes, we can help make this process simple and automatic. Learn how we can help by inquiring about our billing service .
Outpatient Psychiatry Diagnostics / Evaluation / Client Intake CPT Code :
- 90792 – Psychiatric Diagnostic Evaluation with medical services ( usually just one/client is covered )
Outpatient Psychiatry CPT Codes:
- 99201 – E/M – New Patient Office Visit – 10 Minutes
- 99202 – E/M – New Patient Office Visit – 20 Minutes
- 99203 – E/M – New Patient Office Visit – 30 Minutes
- 99204 – E/M – New Patient Office Visit – 45 Minutes
- 99205 – E/M – New Patient Office Visit – 60 Minutes
- 99211 – E/M – Established Patients – 5 Minutes
- 99212 – E/M – Established Patients – 10 Minutes
- 99213 – E/M – Established Patients – 15 Minutes
- 99214 – E/M – Established Patients – 25 Minutes
- 99215 – E/M – Established Patients – 40 Minutes
- 99443 – Telephone therapy (psychiatrist), – limit 3 units/hours per application
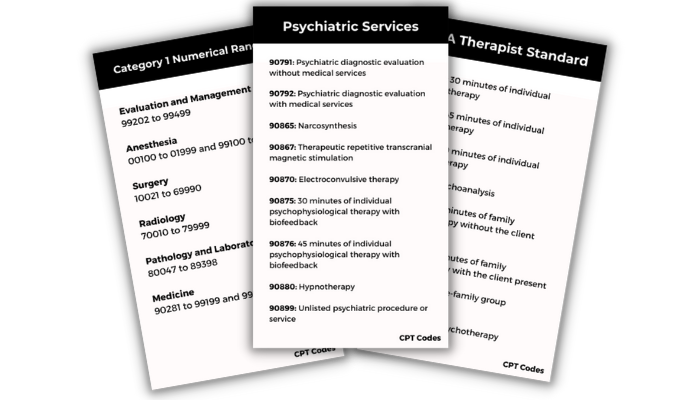
Mental Health CPT Code Cheat Sheet

Download a copy of our PDF Behavioral Health CPT Code Cheat Sheet !
CPT Coding for Therapy
CPT coding for psychotherapy doesn’t have to be difficult! There are an overwhelming amount of total CPT Codes (~8,000), however only 24 are specifically designated for psychotherapy and other mental health services.
To make matters even simpler, nearly all therapists will regularly use an even smaller subset of these 24.
CPT is a large and dynamic code set that changes year to year, but the psychotherapy codes seldom change.
The most recent change for psychotherapy codes took place in 2019, then 2013 , and previously 1998.
To ensure your coding is current and up to date, consider using a billing service instead of having to remember all the codes.
Behavioral Health CPT Add-On Codes
A CPT Add-on Code is a code describing a service performed in in conjunction with a primary service. Many of these add-on codes are associated with a specific CPT Code or a small set of CPT Codes and cannot be used otherwise.
For instance, the behavioral health CPT Code for interactive complexity (+90785) can be used for a diagnostic (90791, 90792) or a normal psychotherapy session (90832, 90834, 90837) but not a crisis psychotherapy session (90839).

Add-on Codes are identified by a + sign in front of the number, i.e. +90840 is an add-on code for extra time in the case of crisis psychotherapy.
On CMS 1500 forms CPT Add-on codes are simply added on a new line.
Add-on codes are extremely important to use in order to most accurately describe the services being rendered and to ensure your services are maximized per session.
We help the mental health providers that work with us in our billing service do all of this for every appointment.
Mental Health Testing CPT Codes [2020]
These codes are only effective January 1st, 2019.
Assessment of Aphasia and Cognitive Performance Testing CPT Codes
Cpt code 96105.
Assessment of aphasia (includes assessment of expressive and receptive speech and language function, language comprehension, speech production ability, reading, spelling, writing, e.g., by Boston Diagnostic Aphasia Examination) with interpretation and report, per hour
CPT Code 96125
Standardized cognitive performance testing (e.g., Ross Information Processing Assessment) per hour of a qualified health care professional’s time, both face-to-face time administering tests to the patient and time interpreting these test results and preparing the report
Developmental/Behavioral Screening and Testing
Cpt code 96110.
Developmental screening (e.g., developmental milestone survey, speech and language delay screen), with scoring and documentation, per standardized instrument
CPT Code 96112
Developmental test administration (including assessment of fine and/or gross motor, language, cognitive level, social, memory, and/ or executive functions by standardized developmental instruments when performed), by physician or other qualified health care professional, with interpretation and report; first hour
Add-on CPT Code + 96113 – Each additional 30 minutes (List separately in addition to code for primary procedure)
CPT Code 96127
Brief emotional/behavioral assessment (e.g., depression inventory, attention-deficit/hyperactivity disorder [ADHD] scale), with scoring and documentation, per standardized instrument
Psychological/Neuropsychological Testing CPT Codes
These codes have changed in 2019.
Neurobehavioral Status Exam CPT Codes
Cpt code 96116.
Neurobehavioral status exam (clinical assessment of thinking, reasoning and judgement, e.g., acquired knowledge, attention, language, memory, planning and problem solving, and visual spatial abilities), by physician or other qualified health care professional, both faceto-face time with the patient and time interpreting test results and preparing the report; first hour
Add-on CPT Code +96121 – Each additional hour (List separately in addition to code for primary procedure)
Test Evaluation Services CPT Codes
Cpt code 96130.
Psychological testing evaluation services by physician or other qualified health care professional, including integration of patient data, interpretation of standardized test results and clinical data, clinical decision making, treatment planning and report and interactive feedback to the patient, family member(s) or caregiver(s), when performed; first hour
Add-on CPT Code +96131 – Each additional hour (List separately in addition to code for primary procedure)
CPT Code 96132
Neuropsychological testing evaluation services by physician or other qualified health care professional, including integration of patient data, interpretation of standardized test results and clinical data, clinical decision making, treatment planning and report and interactive feedback to the patient, family member(s) or caregiver(s), when performed; first hour
Add-on CPT Code +96133 – Each additional hour (List separately in addition to code for primary procedure)
Test Administration and Scoring CPT Codes
Cpt code 96136.
Psychological or neuropsychological test administration and scoring by physician or other qualified health care professional, two or more tests, any method, first 30 minutes
Add-on CPT Code +96137 – Each additional 30 minutes (List separately in addition to code for primary procedure)
CPT Code 96138
Psychological or neuropsychological test administration and scoring by technician, two or more tests, any method; first 30 minutes
Add-on CPT Code +96139 – Each additional 30 minutes (List separately in addition to code for primary procedure)
Automated Testing and Result CPT Codes
96146 – Psychological or neuropsychological test administration, with single automated instrument via electronic platform, with automated result only
Mental Health Evaluation & Management (E/M) Codes
There are also E/M (evaluation & management) in conjunction with psychotherapy, used by authorized prescribers, psychiatrists, and MDs.
Coding E/M is trickier, harder to document and more vulnerable to audit but usually results in greater reimbursement.
There’s also a series of E/M codes that are used without the psychotherapy component.
For more in-depth coverage on E/M coding for psychotherapy there are some good free webinars released by AACAP on E/M CPT Codes.
- Add-on CPT Code +90833 – E/M code for 30 minutes of psychiatry ( used with 90832 ).
- Add-on CPT Code +90836 – E/M code for 45 minutes of psychiatry ( used with 90834 ).
- Add-on CPT Code +90838 – E/M code for 60 minutes of psychotherapy ( used with 90837 ).
- Psychotherapy must be at least 16 minutes.
- Time is very important and should be rounded to the nearest CPT Code.
- Outpatient vs. Inpatient is not important.
- E/M codes can only be used by prescribers (MD, DO, APN, PA).
Medicare 2023 Reimbursement Rates by CPT Code
Interactive complexity (+90785): criteria and how to bill.
+90785 is one of the new add-on codes in the most recent CPT update in 2013.
This code is used as an umbrella add-on code and can be used for four different criteria . The most common scenarios usually involve children, although this is not necessarily always the case.
Common Examples of Interactive Complexity:
- The use of play equipment with young children.
- Interpreters/translators.
- Involvement of parents with discordant views that complicate the treatment plan.
- Report of abuse/neglect.
Interactive complexity can be used in conjunction with the primary CPT Codes for diagnostics, psychotherapy, or group therapy and cannot be used for couple/family therapy or crisis codes.
+90785, can be used with : 90791, 90792, 90832, 90833, 90834, 90836, 90837, 90838, 90853.
Unsure when to use the interactive complexity code? Need help asking if it will be approved? Our billing service exclusively for mental health providers is here to help.
Am I Being Underpaid? Was I Paid the Right Amount?
Here’s typical rates depending on the therapist’s credentials:
Typical Reimbursements by Type of Therapist
These rates can vary significantly therapist to therapist but are good benchmarks for comparison.
How about CPT Codes? How do they affect the rate of reimbursement? This is a difficult and complex calculation, depending on the level of education, location, and license. The AMA has created a code search feature on their website that shows payment based off CPT Code and location.
This information is somewhat incomplete and is based off medicare payments and does not specify a number of other important factors. However, this tool is still very useful to compare the relative value CPT Codes against one another.
Private insurance will be correlated with some deviation from these numbers.
Reimbursement by CPT Code (Three Different Geographies)
Reimbursement (Rest of CA)Reimbursement (Los Angeles)Reimbursement (WA)
Data from AMA Codemanager. These numbers are useful for relative comparison of individual CPT Codes and geography.
Therapist Reimbursement Rates for 2023
Read our definitive guide with 2023 reimbursement rates for mental health CPT codes.
Downcoding Claims
Downcoding (including less services on the claim than actually provided) will usually mean you get paid less, while upcoding (including more services on the claim than actually provided) can get you in trouble with your managed care panels.
It’s also important to note that it might be tempting to maximize your CPT codes to earn higher reimbursements.
This is highly recommended against and can get you flagged, audited and removed from insurance panels. Even if this is your biller’s error, the therapist is the one who ultimately bears the responsibility and will be the one penalized. Here’s a video guide we did of this article!
Distilled Guide to Mental Health CPT Codes
If you are just starting out or just beginning to deal with managed care, keep it simple.
CPT Codes appear far more complex from the outside looking in. Make a quick cheatsheet.
Don’t worry about memorizing all the CPT Codes (there’s alot!) or even all of the mental health ones. You will likely just use just a few individual codes.
Memorize the relevant codes and use google or other references to find the correct CPT codes for more unique scenarios.
Call to verify eligibility and benefits and make sure those codes will be approved with that client’s coverage.
And if all of that sounds like too much trouble, offload the work to us. You won’t have to know one CPT code from another to get your billing paid in full .
Additional Resources
- Medicare Reimbursement by CPT Code & Area
- CPT Reimbursement Lookup & RVU (Relative Value Unit) Overview
- Crosswalk of 2012 to 2013 CPT Codes
- CPT 2013 Standard Edition [Probably Unnecessary]
- Insurance Reimbursement Comparison Tool
Consider Outsourcing Your Billing
Don’t want to learn any of this stuff? We are your team of billing experts here to translate all of this gibberish into English! Reach out about our billing service if you are a licensed mental health provider (we only work with licensed mental health providers).
2020 2021 2022 2023 behavioral health cpt codes mental health billing guide mental health cpt codes mental health cpt codes guide most common mental health cpt codes
86 Comments
This was very helpful thank you for taking the time to write this up in one clear concise place and manner.
Happy to help Victoria! Glad it was so useful.
Of course, Mark.
Another thank you, much appreciated!
Absolutely, Anne, happy we could be of service.
This site was a fantastic one stop website in summing up all of the necessary information in a thorough yet brief description.
Tina, your comment made our team’s day. Thank you so much for the kind words. We are trying to be as practical and helpful as possible.
Thank you so much for sharing your insight. Very helpful to me!
Glad we could be of service, Nita.
Great tips. Thanks.
Thanks for your comment Meredith. Happy to help.
Denny, what code should be used if a Psychologist is doing an evaluation via the internet? Cpt.99444 is an E/M code used for online eval, but I was wondering if there was a different code assigned to Psych?
Hey Austin,
You should definitely call the insurance company to approve these services. Tele-therapy and internet therapy are almost never reimbursed from our experience. Definitely call to ask, it will depend on each insurance company and require some very special filing instructions.
Definitely a tough one! Insurance companies are not keen on remote therapy and rarely grant it unless the patient has no way to get access to a network therapist otherwise (they are disabled, in a very remote area, have no transportation).
Do you know of therapists who offer longer-length sessions, billing a 75-minute session as 90834 + 90832, for example, or a 90-minute session as 90837 + 90832)?
Hi Karen, you would use 90837 and then change the number of units from 1 to 1.5!
Hi Denny, and in this case how would you describe the service? Would you list “Individual Psychotherapy, 60 minutes” (even for a session that is 75 or 90 minutes) or just “Individual Psychotherapy”?
On the CMS form, you should use 90837 for a 60 minute session. The next increment of time would be a 90 minute session that you should bill by increasing the units. Use 1.5 units and 90837.
This is so helpful, thank you! How would you bill an initial assessment appointment that was stopped short by the patient after 20 minutes?
We would call up the insurance co and ask specifically about this case, as specific cases like this vary insurance co to insurance co, state to state. If that were totally fruitless, we would bill 90791 with 1 units because the whole hour was allotted for the patient, even if they ended it abruptly. Likewise, if a patient misses a session, they would be charged a cash full fee, or if they arrived late, they would be billed for the whole session.
It’s important to have a written agreement with your patients / clients about how you are handling payment and walk them through it before beginning your work together. You can check that out at https://therathink.com/mental-health-provider-intake-form/
I would use a 90791 since this code does not have a designated time, whether your intake is 20 minutes or 3 hours you would still use this code, I would think
Thank you so much for this cheat sheet – is it very informative! Is there a minimum time requirement for billing 90791?
We recommend your intake session to be between 45 and 60 minutes.
We recommend at least 45 minutes for an intake session (90791) to be billed with 1 unit. Great question.
The minimum for a 90791, as well as any CPT that is not time indicated already is 15 minutes.
Is there a case for a 90 minute session that isn’t crisis? So a 90837 and 90832 together?
I would recommend calling ahead of time and asking, since it’s not a crisis e.g. reactionary. You would bill 90837 with 2 units instead of 1 unit, in terms of billing on your CMS1500 form.
Thanks Rose!
I’m having trouble finding the correct billing rate for CPT 90837 here in Los Angeles. The Medi-cal site has the rate at $38., but on this site its much higher.
You will need to contact provider support at Medi-Cal to obtain that information.
Can +99354 Prolonged service in the office or other outpatient setting be added to 90847 Family psychotherapy? or is it only for individual psychotherapy? I am wondering how best to code couples or family sessions that last longer than 50 minutes. Thanks!
A 90847 session is coded as 45 to 74 minutes for 1 unit.
For 1.5 units, the session length is 75 to 104 minutes.
And for 2 units, it’s 105+.
Then you can think about using a different addon code.
I am having some problems with +99354. I am billing it with 90837, but I am getting denials from Anthem and was wondering if maybe I need a modifier?
To add a longer duration of visit, change the number of units from 1 to 1.5, in this case. That CPT code addon is incompatible with 90837.
This was very helpful. Receiving denials when my physician uses E/M codes 99213-99215 with a mental health diagnosis. This article helped me to be able to explain how to code the E/M code for psychiatry with medication management.
Happy to help Diana! 🙂
Great information! Is the code 90785 to be billed only one time during the course of therapy or can it be billed at each qualifying occurrence?
The short answer is no, because it doesn’t make sense that there would be that level of intensity with every visit.
You should, though, always bill the most accurate claim possible. So use the code when it best describes the services rendered, and some may or may not be denied, based on that insurance company’s policy. Calling to follow up on these sorts of denials for medical necessity can be beneficial, but the addon code will not generate a very large increase in per appointment revenue, so it might not be worth your time. Some things to consider.
Take it straight from the APA:
“Interactive complexity, the new add-on code 90785, refers to specific communications factors that add to the difficulty of service delivery and increase the intensity of effort required of the health care professional in a particular treatment session. This code is intended to reflect added intensity, not added time, involved with delivering a service. Practitioners should not assume that they can bill 90785 for each session they have with a “difficult” patient. ” — http://www.apapracticecentral.org/good-practice/new-psychotherapy-codes.pdf
Denny, My reading of the codes is that it would often appropriate to use this code in each session — not just because the session is difficult or the client is difficult, but if you are working with a client who is pre-verbal or doing play therapy every week or are having to use an interpreter or communicating is in some way hampered. Don’t you agree?
Great question Barbara and yes a case with an interpreter would be a specific situation where repeated use of this code would be appropriate. The point of “difficulty” here is about rendering service itself, so to your point, a required interpreter would be the cause of increased difficulty. Often times people are concerned about the patient’s Dx being “difficult” but this is a misreading of coding on this case. So we make the distinction between rendering services, logistically, and the clients Dx being a challenging one. Great question to tease out this nuance.
Also pleasure hearing from you as always!
Thank you So Much for this article. We’re having a hard time receiving reimbursements since beginning 2017 (wonder why :P). Each insurance co. is inconsistent with pay-outs; first they Reimburse for 90837, next time they don’t, & this is for the Same Patient. You’d think if an insur. co. paid out for 90837 for ‘patient A’ for one DOS, would be reimbursed again on a claim form with a DOS of 2 weeks later. What’s the deal? Why would Any insur. co. pay out for a regular therapy session (90837, 90834) one week, but not a few weeks later; for the Same Patient? Since this has been the case since the beginning of 2017, your article is really helpful & the quick link resources you put on here are a big help too! So now I love you. Will you marry me Denny? 🙂
Hey Erin, your comment made me laugh, thanks!
That’s a really strange situation, so I would call to ask about what’s going on. If you’re billing it correctly and there aren’t any authorizations or limits for that client, then as long as coverage remains active, you should be reimbursed repeatedly.
This is one of those situations where folks hire us to help, since we cannot give a great answer without investigating! For help there you can check out our mental heath billing service or call yourself!
Good luck, what a weird one!!!
CPT code 90863 must now be billed with a primary service code. What other codes can I use to bill this service and it not be an add on?
I would strongly recommend against billing this CPT code as it is so ambiguous. Pick a more precise CPT code for less of a billing headache.
Has anyone ever actually received reimbursement for +90785 – Interactive Complexity add-on code ? The insurance adjusters at the major health insurance companies (even supervisors) are treating it like a coding error because of the “+” sign and when it is explained to them the major insurers have all, without exception, acted like they had never seen it before. Has anyone used it and gotten it paid? If so, by which company?
We have Dr Arutt. Please do not use the “+” sign when submitting the billing, that’s the reason why it’s not working!
Thank you for this article. Question, I see these reimbursements are mostrly geared towards therapists, psychologists, SW, can psychiatric nurse practitioners use this?
What is the CPT code for billing things like disability paperwork?
Can you please help us to bill High Level Inpatient Psychiatric Evaluation taking approximately 90 minutes of time for CNP ?? we are trying to bill 99223 which is getting denied.
Your response will be highly appreciated.
Is the chart referring to licensed clinical social workers where it indicates “social worker”… if so it is really out of line, as our training, responsibility to patients and privileges are as in depth as any of the licensed behavioral health professionals. Ouch!
I am confused by you saying you can bill for multiple units of 90837. You say for a 90 minute session you should code 90837 and bill 1.5 units. It was my understanding that 90837 was for 53 minutes, or longer, essentially into eternity. : P Have you been successful in getting reimbursed for more than one unit or 90837 billed on the same day?
Hi Ariel :). Depending on the Insurance company (United Health being one that hasn’t been accepting 90837 same day for us), we haven’t been having too much trouble getting a same day reimbursement for 90837. We’re in Wisconsin btw, & I’m sure the state you’re billing from makes a difference too. Hope that helps!
90791 – When I work with children I find it is most helpful for the first session to be parents only. Can I bill 90791 for this or must the child be present?
Hey Denny what a wonderful gift this page has been. Clinicians are always pressed for time. And most want the”best practices” for “best outcomes” but when our time is consumed in the minutiae of coding for proper billing less time can be devoted to giving those who come to us for help our best. So thank you for this unselfish gesture.
Washington Reimbursement rates are listed in the article. Are these rates based upon Medicare or private insurance rates?
These are Medicare rates as they are the only rates that are reliable on an ongoing basis.
Thank you for helping me do my job bro! I’ve been on your email list for over a year now & would have a Lot of reimbursement probs. without you! 🙂
These quoted rates are extremely low reimbursement rates. No one should call these industry standard rates – I am a private practitioner and these rates are less than 50% of standard rates – taking into consideration even of insurance contracts I hold. Insurances need to be confronted. These calculators don’t allow real rates collected (and taxes paid on those full rates should be identifiable pretty easily) to be entered by real providers. You don’t go to your tax accountant, dentist, local pizzeria or college professors and ask for a sliding fee…why should mental health providers be negotiating rates all the time? Stand up to these insurance moguls and demand fair reimbursements.
I know that most insurance companies do not cover phone sessions. I also don’t take most insurances. For my out-of-network patients, I will supply a statement at the end of each month. On occasion, I will do a phone session. On the statement, I will note the session date and use the CPT code 90837 and then note that this was a phone session. Is this acceptable?
I am a sole practitioner in mental health I am licensed mental health counselor. When I submit the claims, I put a procedural code and a place of service code. I have an Anthem client and on our first encounter I billed a 90791 (diagnostic evaluation ) and POS 11. They are not paying a claim because they say it needs an “OFFICE CODE”. The plan has a $20 copay and 0 deductible for mental health. They are applying the entire amount to the medical deductible because the calam needs an “Office Code” what is this and why have I never encountered this before? and where on the claim form CMS 1500 would it go?
Hey Terri, that is the office place of service code. I would recommend calling and asking. If the claim went to their deductible, it was approved and worked — the client simply has a deductible to pay out from. Sounds like you did things right but simply didn’t exact the deductible payment — I would call to ask and also get a quote for eligibility and benefits. Our guide on that is here: https://therathink.com/how-to-verify-eligibility-and-benefits-for-mental-health/
Hello I’m a liscence therapist in NYS . Can you tell me what codes I use for an initial therapy /mental health session for private practice? Also, for a 45 minute and 60 minute session. I’m very new to this so I appreciate any insight. Thank you.
Happy to help Trish! For your intake use 90791. For a 45 minute session, use 90834 and for a 60 minute session, use 90837!
hello Denny, Can you please help me out with the situation where Medicaid of GA denied CPT 90834 for age restriction as this code is covered only for members under 21 years of age. where as we billed the code for patient age of 60 years? Regards, Smith.P
This seems to an inaccurate reading of the denial. I would call back and verify EOB information including the exact denial reason. 90834 is a CPT code that has nothing to do with age. Nor would any Medicaid plan be age restricted. I think you should call back and ask them to tell you in plain language why the claims are denied. Then resolve that problem and resubmit corrected claims and/or appeal. We do this sort of work for our providers in our mental health billing service every day, so this type of work is why folks choose us.
Hi! I have a question about home based therapy. If one of my therapists was to start doing home based therapy would they bill a different code than the normal 90832-90837? We are just trying to make sure we are billing properly. Any help or advise would be greatly appreciated!
My first recommendation is to call to pre approve home based sessions. You will want to change the place of service code and use the same CPT codes. We have an article on mental health place of service codes here: https://therathink.com/place-service-codes-mental-health-billing/
Do you know if there is a modifier or add on procedure code to bill with an initial and group therapy that were performed on the same day? Thank you!
You can use modifier 59 or with Medicare, XE for the same provider with a different service offering or XP for a different provider.
I am a psychiatrist and psychoanalyst and see patients mostly four times a week. Should I be using the GZ542ZZZ code and is there any commercial reimbursement for that? I have used the 90836 but I am definitely seeing patients more often than normal. I want to have my billing reflect the reality of my services but also need to keep the lights on!
Hi Douglas, I don’t know what that ‘code’ refers to exactly but here’s what I suggest for seeing clients more regularly than once a week: 1) call ahead of time to inform their insurance plan of their diagnosis and warranted treatment plan, 2) use the authorization for billing, 3) make sure you continue to seek authorization based on medical necessity directly with their plan. This is something we help out with in our mental health billing service .
Hi, Is there an update to this for 2018? Any changes? Thank you!
Yes, changed have been made to psychological and neurospychological / neuropsych testing as well as testing in general. We’ve posted those changes!
Is there a minimum length of time for group sessions required to bill 90853? Does the group session have to be at least 45 minutes to bill?
Great question. We recommend sessions to be at least 60 minutes but each session length ‘recommendation’ is up to each insurance company.
You have done a wonderful job with this write up! It was also enlightening to see the comparison of different geographical regions within the US and the pricing.
Happy to help Elizabeth. Truly our pleasure to assist with these mental health cpt code questions.
Wow!! Thank you for this very informational site! Great job, much appreciated, most helpful!
Of course Gwen, so glad we were able to help!
My son is at a private, for profit, residential treatment center in NC. He receives 4 group therapy sessions per week. My sons primary therapist (Ph.D, LCSW) facilitates 1 session per week and there are other therapists facilitating the other 3 groups. His primary therapist is the only one taking time to write clinical notes documenting each weeks session in my sons individual file so it cal legally be coded & billed to insurance on the superbill. The other therapists are not writing group notes in his individual file so the sessions can not be documented on our superbill. Therefore, only 1 group session per week is able to be legally coded & billed to insurance on our superbill. The RTC does not deal with coding & billing and have recommended three different 3rd party billing companies that parents could use to collect the superbill.
My questions are: * Do all of the group sessions my son participates in each week need to be documented in his individual file showing how he participated so the sessions can be to be legally coded, in case insurance requests clinical documentation? * Is it proper protocol & best practice for all the therapists, LCSW, write their clinical notes not only in the group file but in each child’s individual file so it can be coded & documented on the * Do the therapists have a legal obligation to do this? * Are the therapists able to go back & write these notes in his individual file? * The founder/executive director/current acting clinical director of the RTC facility said they usually only write ONE group note per MONTH for each type of group (trauma group, etc.) Is this usual & best practice for therapists and RTC’s? The executive director said he would look into this matter and we have attempted to get an answer for 2 months now. Our son has been at the facility for 8 months and graduates in 1 month. * Is there any recourse if they do not provide this so it can documented on the superbill? * If a facility is providing a service, is it expected that the service be documented to show the service is being provided to the patient and payment can be rendered?
We also are currently in negotiations with our public school district to. help with payment of our sons stay. The district expects documentation showing how often our son receives group, individual and family therapy each week.
Hi Tonya, this is an extremely specific set of questions that needs to be handled by a lawyer you hire. We are not the appropriate entity to ask this question. For your own sake please do seek a legal counsel to help.
What happens if you do a 90791 and they turn out of not meet medical necessity according to the DSM 5 for a mental health diagnosis. Can you bill that without a diagnosis or how would you code it. Thanks
You must add the most accurate Dx codes you can for the intake. If medical necessity is required, call to obtain authorization for those sessions. We do this for free within our mental health billing service , of course.
what is the correct way to bill BCBS for 90 minute group psychotherapy session (CPT 90853) the fee schedule for BCBS does not specify time under the code.
We would call up and ask for each client to ensure they have coverage for the group session. We do this for our providers with our billing service.
When I send a new couple a TheraThink Client Intake the great thing that happens is that Denny and the folks in Seattle do the heavy lifting. I have saved countless hours. My clients are required to complete the insurance “intake” prior to their being scheduled (that works for me). I have learned to let go of what I can and focus on what I love! I now truly do have a Team of Support behind me for 2021.
This was a great learning experience. Thank you
Leave a Reply Click here to cancel reply.
Name (Required)
Email (Required)
Our Mental Health Insurance Billing Services
- Daily Claims Filing & Submission
- Daily Claims Processing
- Eligibility & Benefits Verification (in 2 business days)
- EOB & Payment Accounting
- Appeals, Rejections, Denials
- Appointment Reminders (Email or SMS)
- Appointments Calendar
- EAP / Medicare / Medicaid / TriCare Billing
- Credentialing Services
- Network status verification.
- Month-by-Month Contract: No risk trial period
- Free Account Setup - we input your data at signup.
- Claim Tracking & Updates
- EFT & ERA Forms Processing
- Free 30 Day Trial
- Learn more..
You can call, text, or email us about any claim, anytime, and hear back that day. We are your billing staff here to help.
Affordable & Transparent Service
- We charge a percentage of the allowed amount per paid claim (only paid claims)
- No per claim submission fee
- No annual or monthly subscription fee
- No hidden fees
- ICD10 Ready, HIPAA Compliant

Reliable & Dedicated to Customer Service
Our mental health insurance billing staff is on call Monday – Friday, 8am-6pm to ensure your claims are submitted and checked up on with immediacy.
We understand that it's important to actually be able to speak to someone about your billing. Every provider we work with is assigned an admin as a point of contact. You'll always be able to get in touch.
Your access portal for updated claims and reports is secured via our HTTPS/SSL/TLS secured server. Our data is encrypted and backed up to HIPAA compliant standards.
Inquire about our mental health insurance billing service
Get your billing handled.
It's our goal to ensure you simply don't have to spend unncessary time on your billing.
You want to get paid quickly, in full, and not have to do more than spend 10 or 15 minutes to input your weekly calendar.
You want to know you can call your billing admin, a real person you've already spoken with, and get immediate answers about your claims.
You want to not have to deal with it!
Learn how to offload your mental health insurance billing to professionals, so you can do what you do best.
“As private practitioners, our clinical work alone is full-time. Add in the unnecessarily difficult insurance billing system and we run the risk of working way over full-time. TheraThink provides an affordable and incredibly easy solution. My daily insurance billing time now is less than five minutes for a full day of appointments. My cost is a percentage of what is insurance-approved and it’s my favorite bill to pay each month! Denny and his team are responsive, incredibly easy to work with, and know their stuff. I cannot capture in words the value to me of TheraThink. Thank you. You free me to focus on the work I love!”
866-847-3590
Log in classic, log in plus.

CPT Codes for Mental Health — What You Should Know
Current procedural terminology, or CPT, codes are essential to the health insurance billing process. Using the correct CPT codes for mental health billing is critical to receive reimbursement for your services and avoid an audit. However, doing so involves understanding a complex system.
There are thousands of codes to choose from and many different guidelines to follow. Nevertheless, using medical codes properly and receiving maximum reimbursement rates for your services is possible.
This post will cover some basics of CPT codes for mental health and provide tips for avoiding claim denials. The better you understand current procedural terminology, the more time you'll have to care for patients, and the easier it will be to get paid.
What are CPT Codes for Mental Health?
CPT is a uniform coding system developed by the American Medical Association in 1966 to standardize terminology and simplify record-keeping for physicians and staff. Since its introduction, CPT has undergone several changes. The most recent edition focuses on using CPT codes to report physician services.
CPT codes describe medical procedures a physician performs on a patient, including tests, evaluations, surgeries and other practices. For example, behavioral health CPT codes describe the length of a psychotherapy session with a client or a diagnostic interview. CPT codes are necessary to receive reimbursement from health insurance companies.
Why CPT Codes Are Essential for Clinicians
CPT codes are essential parts of practice management for clinicians and health care staff because they determine compensation and the practice's overall success. To receive the correct reimbursement rates, clinicians must ensure the codes on insurance claim forms accurately reflect the services they provided before submitting the claims to insurance companies.
How do CPT Codes Work?
CPT coding tells insurance payers what you would like to get paid for. Along with the International Classification of Diseases codes, CPT codes paint a complete picture for health insurance companies, and you need both types for reimbursement.
The ICD code set describes the diagnosis and why the treatment was necessary, and the CPT code explains the services provided. Examples of mental health ICD codes include the following.
- F41.9: Anxiety disorder
- F31.31: Bipolar disorder, mild
- F33: Major depressive disorder, recurrent
- F42: Obsessive-compulsive disorder
- F43.11: Post-traumatic stress disorder, acute
For example, a social worker might use F41.9 with CPT code 90832 , which is the code for individual psychotherapy for 30 minutes, to bill for a session with a client experiencing anxiety. You would include both codes on a health insurance claims form.
There are three distinct categories of CPT codes, which we will look at next.
What Are the Three Categories of CPT Codes?
The three categories of CPT codes are as follows.
- Category I: Most coders spend the majority of their time working with Category I codes. These codes have different sections based on various health care fields. The six sections of the CPT codebook are Evaluation and Management, Medicine, Surgery, Radiology, Anesthesiology and Pathology and Laboratory. Each has a unique set of guidelines. The CPT codes under Category I are five digits long.
- Category II: Category II codes contain four digits, followed by the letter F. Category II codes are optional. They provide additional information and are not a replacement for Category I or Category III codes.
- Category III: Category III codes are temporary and represent new or experimental procedures or technology. For example, if you can't find a new practice in Category I, you might use a Category III code. Category III codes are four digits long and end in the letter T.
Since Category I is the most frequently used, here's a look at the numerical range of codes within it.
- Evaluation and Management: 99202 to 99499
- Anesthesia: 00100 to 01999 and 99100 to 99150
- Surgery: 10021 to 69990
- Radiology: 70010 to 79999
- Pathology and Laboratory: 80047 to 89398
- Medicine: 90281 to 99199 and 99500 to 99607
Each section contains subfields to correspond to a particular field and includes guidelines to follow. For example, therapists commonly use psychotherapy CPT codes between 90832 and 90853, under Medicine's psychiatry section. Psychiatrists, primary care physicians and other authorized prescribers might use Evaluation and Management codes for providing general medical services.
CPT codes for mental health can also have various modifiers. Modifiers have two numbers or letters, and you can add them to a CPT code. They describe specific critical parts of a procedure.
Some codes have instructions below them in parentheses to tell the coder there may be a better code to use. Codes must be as specific as possible for a mental health billing claim to get accepted.
How to Use the Correct CPT Code in Psychiatry
The CPT code set is a complex system. It is not always easy to determine if you've met the required elements to code appropriately for the maximum reimbursement amount. It may help to break the process down into steps for new and established patients.
First, you might bill two types of psychiatric service or procedure CPT codes for new patient office visits. These are:
- Psychiatric diagnostic evaluation codes
Depending on the situation and time involved, it may be appropriate to bill for both codes. Here are a few guidelines to follow.
- E/M: Use E/M codes when evaluating a new medical issue. With the AMA's 2023 coding changes , you can select an E/M code based on the complexity of medical decision-making or the total time you spent on the patient's care on the day of the encounter. If you provide E/M services with a psychotherapy add-on code, you must choose a code based on medical decision-making, not total time.
- Psychiatric diagnostic evaluation: Use psychiatric diagnostic evaluation codes for a diagnostic assessment. You may need to use these codes more than once if it takes more time to complete the initial evaluation.
Regarding established patients, the rules allow you to bill an E/M service with every psychotherapy visit, but they don't require you to do so with every encounter. Only bill E/M services if you addressed and documented a separate medical issue during the visit.
For example, if you address medication's side effects during an encounter, you might bill for an E/M visit in addition to a psychotherapy session.
However, if a patient has been stable and on the same medication for years and attends a psychotherapy visit, you can only bill for the psychotherapy session. You cannot bill for E/M because there are no medical or medication concerns expressed during the visit.
Also, to bill for E/M, your documentation must prove your active management or discussion of a medical or medication problem distinct from the psychotherapy service.
The 3 Major Components of E/M Documentation

According to the Centers for Medicare and Medicaid Services , insurance companies might want to see documentation to ensure the client's policy covers necessary services and confirm the following pieces of information:
- The service site
- The medical necessity of the services provided
- The accuracy of the services reported
Your client's medical records must include the following three components to support the E/M codes you choose.
- History: The history section must include the history of present illness, a review of body systems and the family and social history.
- Examination: The examination section includes the type of examination performed based on your judgment and the nature of the problem. According to the CMS, the levels of E/M services derive from problem-focused, expanded problem-focused, detailed, or comprehensive exams.
- Medical decision-making: The medical decision-making section includes the number and complexity of problems addressed during the specific encounter, the complexity of the data reviewed and the risk of complications.
When selecting an E/M code with psychotherapy, you'll base your choice on medical decision-making. You should also choose a CPT code that reflects the service site and whether the patient is new or established. Take these steps :
- Select the type and level of E/M service based on medical decision-making.
- Choose timed psychotherapy add-on codes based on the time spent providing psychotherapy.
For example, if you choose E/M code 99202 to evaluate and manage a new patient in an outpatient setting with straightforward decision-making and need to bill for 30 minutes of psychotherapy, you would include the add-on code 90833 .
Make sure to keep your E/M code and psychotherapy codes separate. The time associated with the E/M service cannot count toward the time of the psychotherapy service. The E/M service must be significant and distinct from psychotherapy.
Start Your Free Trial Today
With an intuitive, chart-centric workflow, ICANotes is the only fully configured EMR software for behavioral health. Our robust clinical content engine and customizable point-and-click templates reduce the time you spend documenting patient care while enabling you to confidently bill at the maximum level of reimbursement.
- Behavioral Health Notes in 3 Minutes
- Free training and 24x7 support
- Fully HIPAA compliant 30 day trial
Spend less time on documentation and improve your reimbursement with ICANotes+.
The Most Common Psychotherapy CPT Codes for Mental Health
While family therapists and counselors may not use E/M codes like psychiatrists or primary care physicians, they will bill for psychotherapy services. The American Psychological Association lists standard CPT codes used by therapists.
- 90832: 30 minutes of individual psychotherapy
- 90834: 45 minutes of individual psychotherapy
- 90837: 60 minutes of individual psychotherapy
- 90845: Psychoanalysis
- 90846: 50 minutes of family psychotherapy without the client present
- 90847: 50 minutes of family psychotherapy with the client present
- 90849: Multiple-family group psychotherapy
- 90853: Group psychotherapy
Though CPT codes describe specific times, such as 30, 45 and 60 minutes, therapists have some flexibility, since sessions might go over or under that exact amount.
When choosing a psychotherapy CPT code, therapists must select the closest one to the time spent in the session. The APA lists the following psychotherapy session durations.
- 90832: Choose this code for sessions that run between 16 and 37 minutes.
- 90834: Select this code for sessions that are 38 to 52 minutes long.
- 90837: This code is appropriate for sessions lasting 53 minutes or longer.
- 90846 or 90847: Choose these codes for 26 minutes or more of family psychotherapy.
Psychotherapy Crisis Codes
CPT codes for crises allow behavioral health professionals to bill for emergency sessions. Care providers typically use the following crisis codes for patients in significant distress who require immediate attention or are in a life-threatening situation.
- 90839: First 60 minutes of psychotherapy for crisis
- 90840: Add-on code for each additional 30 minutes of psychotherapy for crisis
- 99050: Add-on code for services provided when the office is usually closed
- 99051: Add-on code for services provided during regularly scheduled hours on evenings, weekends or holidays
If a crisis session falls below 60 minutes, you will bill for a regular psychotherapy code, such as 90834.
Other Add-On Codes
Providers may use add-on codes to describe additional services. Behavioral health clinicians can only apply add-on codes in combination with psychotherapy and diagnostic evaluation services. Providers must include the principal CPT code and add-on code on the billing form, and list them separately. Add-on codes include the following.
- 90785: Interactive complexity
- 90863: Psychopharmacology with psychotherapy
- 90833: 30 minutes of psychotherapy with E/M service
- 90836: 45 minutes of psychotherapy with E/M service
- 90838: 60 minutes of psychotherapy with E/M service
Clinicians might use code 90785 for factors that complicate service delivery, such as the presence of a client's angry family member or a third party like a probation officer. Psychologists might use code 90863 when reviewing or prescribing medication on the same day as delivering psychotherapy services. Psychiatrists do not use code 90863.
Mental Health Test and Assessment Codes
CPT codes for mental health tests and assessments include the following.
- 96105: Aphasia assessment
- 96110: Developmental screening
- 96112: Developmental test administration with interpretation
- 96113: Each additional 30 minutes of developmental test administration with interpretation
- 96116: Neurobehavioral status exam, 60 minutes
- 96121: Each additional hour of neurobehavioral status examination
- 96125: Standardized cognitive performance testing, 60 minutes
- 96127: Brief emotional or behavioral assessment
- 96130: Psychological testing evaluation services provided by a physician or qualified health professional, 60 minutes
- 96131: Each additional hour of psychological testing evaluation services performed
- 96132: Neuropsychological testing services, 60 minutes
- 96133: Each additional hour of neuropsychological testing services performed
- 96136: Psychological or neuropsychological test administration and scoring by a physician or qualified health professional, 30 minutes
- 96137: Each additional 30 minutes of neuropsychological test administration and scoring by a physician or qualified health professional
- 96138: Psychological or neuropsychological test administration and scoring by a technician, 30 minutes
- 96139: Each additional 30 minutes of neuropsychological test administration and scoring by a technician
- 96146: Psychological or neuropsychological test administration via an electronic platform with automated results
- 96156: Health assessment or reassessment
- 96160: Patient-focused health risk assessment
- 96161: Caregiver-focused health risk assessment
Psychiatry CPT Codes
Psychiatrists use CPT codes to bill for psychiatric diagnostic evaluations, psychotherapy and other psychiatric services. CPT codes for psychiatric services include the following.
- 90791: Psychiatric diagnostic evaluation without medical services
- 90792: Psychiatric diagnostic evaluation with medical services
- 90865: Narcosynthesis
- 90867: Therapeutic repetitive transcranial magnetic stimulation
- 90870: Electroconvulsive therapy
- 90875: 30 minutes of individual psychophysiological therapy with biofeedback
- 90876: 45 minutes of individual psychophysiological therapy with biofeedback
- 90880: Hypnotherapy
- 90899: Unlisted psychiatric procedure or service
Psychiatry Evaluation and Management Codes
Psychiatrists may use E/M codes to bill for evaluation and management services, either alone or with psychotherapy. For psychiatrists and other physicians, psychotherapy is an add-on code to the primary E/M service.
- 99202 to 99205: Outpatient E/M services for a new patient
- 99211 to 99215: Outpatient E/M services for an established patient
- 99241 to 99245: Consultations for a new or established patient in an outpatient setting
- 99221 to 99223: Initial hospital E/M services for a new or established patient
- 99231 to 99233: Hospital E/M services for a new or established patient after initial visit
- 99251 to 99255: Inpatient consultations
Common Behavioral Health Case Management CPT Codes
Like licensed counselors, clinical social workers who provide psychotherapy services use CPT codes for mental health to get reimbursed. Here's a CPT description list of frequently used codes , according to CMS:
- 90832: 30 minutes of psychotherapy
- 90834: 45 minutes of psychotherapy
- 90837: 60 minutes of psychotherapy
- 90785: Interactive complexity add-on
- 90839: 60 minutes of psychotherapy for crisis
- 90840: Each additional 30 minutes of psychotherapy for crisis
- 90791: Psychiatric diagnostic evaluation
- 90846: 50 minutes of family psychotherapy without the patient present
- 90847: 50 minutes of family psychotherapy with the patient present
- 90853: Group psychotherapy
Telehealth CPT Medical Coding List
Telehealth CPT codes are especially relevant today. Since so many behavioral health professionals have moved their practices online, it helps to know CPT codes for virtual therapy.
According to the Centers for Medicare and Medicaid Services , telehealth visits are the same as in-person visits and get paid at the same rates. Therefore, you will use the identical CPT code for a virtual therapy session as you would if you were billing for a face-to-face meeting. For example, if you meet with a patient online, you would still use the code 90832 for 30 minutes of psychotherapy. However, you would apply different modifiers for telehealth services , as follows.
- 95 modifier: Add 95 to the appropriate CPT code. This modifier describes a real-time interaction between a clinician and patient via a telecommunications system, such as through video conferencing. You may use the modifier GT instead.
- 02 for place of service: Use 02 to describe the place of service as a telecommunications system. It may replace the commonly used POS code 11 , which describes providing therapy in an office.
As you'll see, some telehealth codes belong to the Healthcare Common Procedural Coding System . HCPCS codes are not part of the CPT set, and they cover specific services and products needed to provide care. HCPCS codes consist of a single letter followed by four numbers. Here are codes you might use specifically for telehealth.
- G2012: Virtual check-in or brief, patient-initiated visit
- G2010: Remote evaluation of a recorded video or image provided by an established patient
- 99421: Online digital evaluation and management service conducted via a patient portal for an established patient, five to 10 minutes of cumulative time over seven days
- 99422: Online digital evaluation and management service conducted via a patient portal for an established patient, 11 to 20 minutes of cumulative time over seven days
- 99423: Online digital evaluation and management service conducted via a patient portal for an established patient, 21 or more minutes of cumulative time over seven days
Non-physician health professionals may use the codes G2061, G2062 or G2063 to provide an online assessment and management service for an established patient.
New CPT Codes for Mental Health Services
Every year, health professionals can expect revised or new CPT codes for mental health. Providers use these services to address psychological, emotional, cognitive or behavioral issues that impact the treatment of a physical health problem. Psychologists may provide these services to an individual, group or a patient's family to help the client cope with physical health conditions.
The most recent changes in 2023 include new HCPCS codes and CPT codes and updated language to improve provider understanding. Psychologists must use these new therapy CPT codes to get reimbursed for health behavior assessment and intervention services from third-party payers.
Health behavior assessment and intervention codes require a physical health diagnosis or an ICD code and are not for mental health services. Here are the code revisions .
- Code 96156 replaces codes 96150 and 96151: Clinicians must now use code 96156 to bill for a health and behavior assessment or reassessment. The new code for assessment services is now event-based rather than time-based.
- Code 96152 is now 96158 plus 96159: Clinicians must now use code 96158 — previously 96152 — for an individual, in-person health behavior intervention for the initial half hour. For each additional 15 minutes of intervention, use code 96159 separately.
- Code 96153 is now 96164 plus 96165: Clinicians must replace code 96153 with 96164 for the first half-hour of an in-person group health behavior intervention. For every additional 15 minutes of service, tack on code 96165.
- Code 96154 is now 96167 plus 96168: Clinicians must now use code 96167 — previously 96154 — for the initial half-hour of an in-person family health behavior intervention with the patient present. For every additional 15 minutes of service, separately add code 96168.
- Code 96155 is now 96170 plus 96171: Clinicians must replace code 96155 with 96170 for the first half-hour of a face-to-face family health behavior intervention without the patient present. Every additional 15 minutes of service should include code 96171.
How CPT Code Changes Impact the Reimbursement Process

CPT codes also have modifiers to specify the services behavioral health professionals provide in more detail. For example, these modifiers may indicate the reason for the service, whether the provider performed multiple services and where the services occurred. CPT code modifiers ensure that providers receive accurate reimbursement for all the services they provide.
Reimbursement rates change constantly, and a lot depends on the decisions made by the CMS. The CMS accepts the American Medical Association's CPT code recommendations and makes the final decisions regarding code values.
The code selection process also impacts how much clinicians get paid. For example, with the recent E/M coding changes, clinicians can bill for the total time they spend in one day on an encounter, which includes non-face-to-face time, and gets credit for tasks like interpreting exams performed by other physicians.
Clinicians can also choose an E/M code based on total time or medical decision-making, selecting the one that makes the most financial sense.
CPT Code Reimbursement Rates
Reimbursement rates depend on the insurance payer, location and practitioner level. For instance, a psychiatrist will receive a higher reimbursement rate than a social worker.
The CPT code you choose also affects compensation. In general, the longer you spend with a patient delivering services, the more you'll get paid. For example, according to the Mississippi Division of Medicaid's 2020 fee schedule , psychotherapy rates were:
- 90832: $60.07
- 90834: $79.90
- 90837: $119.68
If you're concerned you're not getting the highest reimbursement rate possible, let us know at ICANotes. We've designed our electronic health record software to help behavioral health specialists maximize reimbursement.
ICANotes keeps track of documentation elements in clinical notes and automatically calculates the highest-level E/M code supported by a note. ICANotes makes it easy to establish all the required details of accurate E/M documentation by providing pre-templated buttons and an easy-to-use interface. With ICANotes, clinicians can stay up to date on CPT changes and ensure compliance with the Health Insurance Portability and Accountability Act.
Tips for Maximizing Reimbursement and Avoiding Insurance Claim Denials
If you hope to avoid issues with claims, you mostly want to remember that medical necessity determines the level of service to bill. It would not be appropriate to document a higher service level if it is unnecessary. Always make sure the documentation supports the level of care you are billing. Here are a few more tips to remember.
1. Ensure Correct Coding
To receive reimbursement, a clinician must complete accurate coding. Coding errors can lead to payment delays or rejected claims. Frequent or consistent errors could lead to an audit or fraud charges. Strive for the highest accuracy, and cut down on simple errors like incorrect patient information or policy number mistakes. Always refer to the AMA’s most recent CPT manual to make sure you use the correct codes in your practice.
Also, make it a habit to check and recheck work, and thoroughly read all the therapy notes included with the codes. Encourage staff members to do the same. Improper modifier use is a prevalent cause of claim denials. Therefore, make sure to familiarize yourself with modifiers before using them. Modifiers can be the difference between maximum reimbursement and reduced payment, so it's crucial to review the rules.
2. Claim Only What's Medically Necesarry
Medicare and other payers define what's medically necessary in different ways, but in general, it's about doing what's best for the patient at that time. A claim for a service that is not a medical necessity will likely get denied.
To help demonstrate a medically necessary claim, make sure to choose the appropriate ICD code and link it to the associated CPT codes that are valid for the visit. Doing so enables staff and insurance payers to see the reason for each service.
3. File Claims on Time
You must submit claims by a specific deadline. For example, Medicare requires you to file no later than 12 months after the date of service. These dates can vary depending on the payer, and some claims may be due within 90 days or 180 days after service. By meeting deadlines, you'll ensure you receive adequate reimbursement.
Missing claim submission deadlines is a typical reason for a claim denial. If your practice has struggled to meet these deadlines, consider coming up with a schedule to complete all paperwork and ensure its accuracy well before the due date. To make things easier, you can also rely on EHR software to help you stay compliant.
4. Emphasize Quality Documentation
Inadequate documentation can affect the reimbursement process. Make sure everyone in your practice understands the value of correct, legible and complete documentation. Otherwise, it will be challenging to make an accurate or complete claim.
In addition to writing quality clinical documentation and therapy progress notes, it's also wise to double-check that your patient's information is correct. While this may seem like an obvious tip, it's easy to accidentally misspell a patient's name or enter an incorrect Social Security number.
Other routinely missed data points include the patient's date of birth, insurance payer, policy number, group number and patient's relationship to the insured. Likewise, leaving any required fields blank on your paperwork may trigger a claim denial. However, most minor errors or omissions do not require an appeal or redetermination.
5. Identify and Educate
Creating a standard workflow for managing your claims process is an effective way to maintain accuracy. Identify coding errors, review past mistakes and aim to correct the errors by educating staff and staying current on any code changes. Schedule regular training meetings to keep information fresh and share any updates. Once your entire staff is up to date with your protocols, they will be less likely to make a mistake or forget to fill out critical information.
A critical part of educating your staff is to teach everyone why claims get denied. If your practice has been getting more denials than usual lately, there's clearly an ongoing issue. Some of the top reasons for claims denials include duplicate submissions, ineligible service according to the patient's health insurance or settled claims.
Record typical reasons for claim denial and develop a step-by-step plan to help manage this concern. Providing this training, in addition to new technology, allows your employees to work more efficiently.
6. Verify Insurance and Eligibility
Before you conduct a therapy session or medication management visit and get to the billing and reimbursement process, the first step is to collect accurate and complete new patient information. To avoid claim denials, you must check and double-check that each client's plan covers your services.
Patient ineligibility is another reason for insurance companies to deny your reimbursement claims, so you must maintain a thorough process. Each client should have complete eligibility verification before you see them for a session, and you should collect their copayments during their initial visit. In addition, your clerical staff should maintain copies of the patient's driver's license and forms. Finally, you should also check the start and end date for the patient's insurance policy.
7. Automate as Much as Possible
Clinicians spend plenty of time on documentation. From creating treatment plans to completing comprehensive therapy progress notes, it may seem like there's little opportunity left in your day to focus on reimbursement claims requirements. When you use an EHR software, you can automate these processes to streamline your note-writing process. Automating your manual processes can also help reduce rejected claims by ensuring your notes are legible, detailed and meet the strict standards set by insurance companies.
Using technology makes it easier to submit clean claims and eliminates the tedious need to keep up with all diagnostic codes and insurance policies. For instance, an EHR that offers automatic coding will provide the code associated with your service and ensure you have the proper documentation for your billing claims. You can maximize your reimbursement and eliminate the manual burden from your billing and admin teams.
Use ICANotes for Fast and Accurate Billing
Using proper CPT codes for mental health requires knowledge and practice. Most behavioral health clinicians want to spend their time and energy providing patient care — not worrying about coding and claims. ICANotes can step in and take care of the work for you, so you can get back to doing what you love.
With ICANotes, you can expect automatic coding at the highest reimbursement level possible to ensure claims get accepted and you get paid. Without the need to fix errors or resubmit claims, you’ll save time, money and energy. To experience the benefits of our behavioral health EHR software firsthand, sign up for a free trial today!
- Psychiatric Nurse Practitioners
- Psychiatric Hospital Records
- Certified Drug & Alcohol Abuse Counselors
- Social Work Case Management Software
- Family Therapists
- Group Therapy
- EHRs for Integrated Care
- Sample Notes
- Appointment Reminders
- Document Management
- Patient Portal
- Telehealth Platforms for Mental Health
- Billing Software for Mental Health Professionals
- Clearinghouses
- Health Information Exchange Integration
- Interoperability
- Lab Integration
- PDMP Integration
- Mobile Medication Management
- Automatic Coding
- ONC-ATCB Certification
- CARF Compliance
- Joint Commission
- Meaningful Use
- Medicaid-Compliant EHR Software
- Assessment Tools
- Behavioral Health EHR
- Sample Treatment Plans
- Note Writing Tips
- Treatment Planning
- Practice Management
- Mental Health Care Trends
- All Blog Categories
- Our Leadership Team
- Customer Reviews
- Quote Request
- Remote Support
- Access ICANotes
- Knowledge Base
- Support Portal
- User Guides and Documentation
The page could not be loaded. The CMS.gov Web site currently does not fully support browsers with "JavaScript" disabled. Please enable "JavaScript" and revisit this page or proceed with browsing CMS.gov with "JavaScript" disabled. Instructions for enabling "JavaScript" can be found here. Please note that if you choose to continue without enabling "JavaScript" certain functionalities on this website may not be available.

An official website of the United States government
Here's how you know
The .gov means it's official.
Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure.
The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.

Billing and Coding: Psychiatry and Psychology Services
Document note, note history, contractor information, article information, general information.
CPT codes, descriptions and other data only are copyright 2023 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Fee schedules, relative value units, conversion factors and/or related components are not assigned by the AMA, are not part of CPT, and the AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The AMA assumes no liability for data contained or not contained herein.
Current Dental Terminology © 2023 American Dental Association. All rights reserved.
Copyright © 2023 , the American Hospital Association, Chicago, Illinois. Reproduced with permission. No portion of the American Hospital Association (AHA) copyrighted materials contained within this publication may be copied without the express written consent of the AHA. AHA copyrighted materials including the UB‐04 codes and descriptions may not be removed, copied, or utilized within any software, product, service, solution or derivative work without the written consent of the AHA. If an entity wishes to utilize any AHA materials, please contact the AHA at 312‐893‐6816.
Making copies or utilizing the content of the UB‐04 Manual, including the codes and/or descriptions, for internal purposes, resale and/or to be used in any product or publication; creating any modified or derivative work of the UB‐04 Manual and/or codes and descriptions; and/or making any commercial use of UB‐04 Manual or any portion thereof, including the codes and/or descriptions, is only authorized with an express license from the American Hospital Association. The American Hospital Association (the "AHA") has not reviewed, and is not responsible for, the completeness or accuracy of any information contained in this material, nor was the AHA or any of its affiliates, involved in the preparation of this material, or the analysis of information provided in the material. The views and/or positions presented in the material do not necessarily represent the views of the AHA. CMS and its products and services are not endorsed by the AHA or any of its affiliates.
CMS National Coverage Policy
Article guidance.
This article contains coding and other guidelines that complement the Local Coverage Determination (LCD) for Psychiatry and Psychology Services.
Unless otherwise indicated, these procedures may be used by providers of mental health services licensed or otherwise authorized as designated by Medicare and the state in which they practice.
National Coverage Provisions:
It is not necessary that a course of therapy have as its goal restoration of the patient to the level of functioning exhibited prior to the onset of the illness, although this may be appropriate for some patients. For many other psychiatric patients, particularly those with long-term, chronic conditions, control of symptoms and maintenance of a functional level to avoid further deterioration or hospitalization is an acceptable expectation of improvement. "Improvement" in this context is measured by comparing the effect of continuing treatment versus discontinuing it. Where there is a reasonable expectation that if treatment services were withdrawn the patient's condition would deteriorate, relapse further, or require hospitalization, this criterion would be met (CMS Publication 100-02, Medicare Benefit Policy Manual , Chapter 6, Section 70.1).
Some patients may undergo a course of treatment which increases their level of functioning, but then reach a point where further significant increase is not expected (CMS Publication 100-02, Medicare Benefit Policy Manual , Chapter 6, Section 70.1).
Social and psychological services include the assessment and treatment of a CORF patient’s mental health and emotional functioning and the response to, and rate of progress of the patient’s rehabilitation plan of treatment including physical therapy services, occupational therapy services, speech-language pathology services and respiratory therapy services.
CORF social and/or psychological covered services are the same, regardless of whether they are provided by a qualified social worker, as defined at 42CFR485.70(l), or a psychologist, as defined at 42CFR485.70(g). Therefore, a CORF may elect to provide these services when they are indicated. Qualifications for individuals providing CORF social and psychological services are, at a minimum, a Bachelors of Science Degree for a social worker and a Masters-level degree for a psychologist. ( CMS Publication 100-02 , Medicare Benefit Policy Manual, Chapter 12, Section 40.7 ).
To be covered as incident to physicians’ services, the services and supplies must be furnished by the hospital or CAH or under arrangement made by the hospital or CAH (see section 20.1.1 of this chapter). The services and supplies must be furnished as an integral, although incidental, part of the physician or nonphysician practitioner’s professional service in the course of treatment of an illness or injury. ( CMS Publication 100-02 , Medicare Benefit Policy Manual, Chapter 6, Section 20.5.2 ).
The services and supplies must be furnished under the order of a physician or other practitioner practicing within the extent of the Act, the Code of Federal Regulations, and State law, and furnished by hospital personnel under the supervision of a physician or nonphysician practitioner as defined at 42 CFR 410.27(f) and 482.12. ( CMS Publication 100-02 , Medicare Benefit Policy Manual, Chapter 6, Section 20.5.2 ).
When the hospital makes arrangements with others for diagnostic services, such services are covered under Part B as diagnostic tests whether furnished in the hospital or in other facilities. ( CMS Publication 100-02 , Medicare Benefit Policy Manual, Chapter 6, Section 20.4.6 ).
Coding Information:
Procedure codes may be subject to National Correct Coding Initiative (NCCI) edits or OPPS packaging edits. Refer to NCCI and OPPS requirements prior to billing Medicare.
For services requiring a referring/ordering physician, the name and NPI of the referring/ordering physician must be reported on the claim.
A claim submitted without a valid ICD-10-CM diagnosis code will be returned to the provider as an incomplete claim under Section 1833(e) of the Social Security Act.
The diagnosis code(s) must best describe the patient's condition for which the service was performed. For diagnostic tests, report the result of the test if known; otherwise the symptoms prompting the performance of the test should be reported.
Specific Coding Guidelines:
Psychiatric Diagnostic Procedures may be reported once per day and not on the same day as an evaluation and management service performed by the same individual for the same patient.
Psychiatric Diagnostic Procedures may be covered once, at the outset of an illness or suspected illness. It may be utilized again for the same patient if a new episode of illness occurs after a hiatus or on admission or readmission to an inpatient status due to complications of the underlying condition. Certain patients, especially children, may require more than one visit for the completion of the initial diagnostic evaluation. The medical record must support the reason for more than one diagnostic interview.
The interactive complexity component code 90785 may be used in conjunction with codes for diagnostic psychiatric evaluation (90791, 90792) and psychotherapy (90832, 90834, 90837), psychotherapy when performed with an evaluation and management service (90833, 90836, 90838), and group psychotherapy (90853).
Procedure codes 90832-90838 (psychotherapy for 30 to 60 minutes) – report the code closest to the actual time (i.e., 16-37 minutes for 90832 and 90833, 38-52 minutes for 90834 and 90836, and 53 or more minutes for 90837 and 90838. Procedure codes 90833, 90836 and 90838 are add on codes that should be used in conjunction with evaluation and management (E/M) codes 99201-99239, 99304-99337, 99341-99350.
Psychotherapy codes that include an evaluation and management component are payable only to physicians, PAs, NPs and CNSs. The evaluation and management component of the services must be documented in the record. A psychotherapy code should not be billed when the service is not primarily a psychotherapy service, that is, when the service could be more accurately described by an evaluation and management or other code.
The duration of a course of psychotherapy must be individualized for each patient.
90845 is not time defined, but the service is usually 45 to 50 minutes and is billed once for each daily session.
Code 90846 is used when the patient is not present. Code 90847 is used when the patient is present. Code 90849 is intended for group therapy sessions to support multiple families when similar dynamics are occurring due to common issues confronted in the family members under treatment.
Codes 90846 and 90847 may not be reported for services less than 26 minutes.
Codes 90846 and 90847 do not pertain to consultation and interaction with paid staff members at an institution.
90849 does not meet Medicare's standards of being a therapy primarily directed toward treating the beneficiary's condition. Claims for 90849 may be approved on an individual consideration basis.
Code 90785 is used when the patient or patients in the group setting do not have the ability to interact by ordinary verbal communication and therefore, non-verbal communication skills are employed or an interpreter may be necessary.
Use of CPT code 90865 is restricted to physicians (MD/DO) only.
"Codes 90839, 90840 are used to report the total duration of time face-to-face with the patient and/or family spent by the physician or other qualified health care professional providing psychotherapy for crisis, even if the time spent on that date is not continuous. For any given period of time spent providing psychotherapy for crisis state, the physician or other qualified health care professional must devote his or her full attention to the patient and, therefore, cannot provide service to any other patient during the same time period. The patient must be present for all or some of the service." (CPT 2013, Professional Edition, p.486)
When a psychiatrist performs both the ECT and the associated anesthesia, no separate payment is made for the anesthesia. Code 90870 is limited to use by physicians (MD/DO) only.
CPT codes 90875, 90876 and 90882 are not covered by Medicare.
Psychiatric procedures billed using code 90899 may be covered on an individual consideration basis.
Code 96105 represents the formal evaluation of aphasia using a psychometric instrument such as the Boston Diagnostic Aphasia Examination. This testing is typically performed once during treatment and the medical necessity for such testing should be documented. Repeat testing should only be done if there is a significant change in the patient’s aphasic condition.
"Unlisted psychiatric service or procedure" should not be used if the service is described by one of the more specified codes.
Documentation Requirements:
The patient's medical record must contain documentation that fully supports the medical necessity for services included within the related LCD. (See "Indications and Limitations of Coverage.") This documentation includes, but is not limited to, relevant medical history, physical examination, and results of pertinent diagnostic tests or procedures. The Health Insurance Portability and Accountability Act of 1996 (HIPAA) has imposed specific restrictions on access to psychotherapy notes. These restrictions are outlined in the Code of Federal Regulations (CFR), 45 CFR, parts 160 and 164 (The Privacy Rule). Providers are exempt from submitting psychotherapy notes without patient authorization when the notes in question fit the Privacy Rule definition in 45 CFR Section 164.501. This section defines psychotherapy notes as "notes recorded by a mental health professional (in any medium) which document or analyze the contents of a counseling session and that are separated from the rest of a medical record." 45 CFR Section 164.501 states that "the provider is responsible for extracting information required to perform a review for medical necessity." The provider, therefore, is expected to document information potentially necessary for review in a manner that will allow submission if this information without release of psychotherapy details that are protected by the Privacy Rule. This following information is excluded from the protected information in 45 CFR Section 164.501, and must be included in all psychiatric medical record documentation and made available upon request: - Name of beneficiary and date of service - Type of service (individual, group, family, interactive, etc.) - Time element, where duration of the face-to-face contact is the determining factor for coding the service rendered - Modalities and frequency of treatment furnished - A clinical note for each encounter, where in the aggregate, summarizes the following items: diagnosis, symptoms, functional status, focused mental status examination, treatment plan, prognosis, and progress to date. Elements such as treatment plans, functional status and prognostic assessment are expected to be documented, updated and available for review, but do not need to be delineated for each individual date of service. - Identity and professional credentials of the person performing service For interactive therapy , the medical record should indicate the adaptations utilized in the session and the rationale for employing these non-verbal interactive techniques For psychotherapy services that include a medical evaluation and management component, documentation of the medical evaluation or management component of the treatment, including prescriptions, monitoring of medication effects, co-morbid medical conditions evaluated, and results of clinical tests. Group therapy session notes must be prepared within a reasonable time period after the rendering of professional services consistent with accepted practice, and can be organized according to the general session note guidelines for individual therapy or the clinician may elect to use the following group note format: • One portion of the note that is common to all patients, documenting date, length of time for the session, along with key issues presented. Names of the patients in the group should not appear in this group note. • A second portion of the note, for each patient's record, commenting on that particular patient's participation in the group process and any significant changes in patient status. As outlined in HIPAA regulations referenced above, the note should exclude sensitive content of the patients' conversation. While there are no specific limitations on the frequency or length of time that outpatient psychiatric services may be covered, there are many factors, including the nature of the illness, prior history, goals of treatment, and the patient’s response, that affect the outcome of treatment. When outpatient psychiatric services are provided at a high frequency or long duration, the plan of treatment, progress notes, and condition of the patient should justify the intensity of the services rendered. For psychotherapy services , there should be documentation of the patient's capacity to participate in and benefit from psychotherapy, especially if the patient is in any way cognitively impaired. The medical record should document the target symptoms, goals of therapy and methods of monitoring outcome. There should be documentation in the medical record of how the treatment is expected to improve the health status or function of the patient. Those hospitals that provide services at off-campus locations must clearly document in the medical record the location of the billed services, and that the services were properly supervised.
The medical record must reflect the elements outlined in the Psychiatric Diagnostic Procedures description and must be rendered by a qualified provider (see "Limitations" in related LCD).
The medical record must reflect the elements outlined in the above Interactive Complexity description and must be rendered by a qualified provider (see "Limitations" subsection in related LCD). Additionally, the medical record must include adaptations utilized in the session and the rationale for employing these interactive techniques. The medical record must include treatment recommendations.
The medical record must indicate the time spent in the psychotherapy encounter and the therapeutic maneuvers, such as behavior modification, supportive or interpretive interactions that were applied to produce a therapeutic change. Behavior modification is not a separate service, but is an adjunctive measure in psychotherapy. Additionally, a periodic summary of goals, progress toward goals, and an updated treatment plan must be included in the medical record. Prolonged periods of psychotherapy must be well-supported in the medical record describing the necessity for ongoing treatment.
The medical record must document the indications for psychoanalysis , description of the transference, and the psychoanalytic techniques used.
The medical record must document the conditions described under the psychoanalysis, group psychotherapy, family psychotherapy, and/or interactive group psychotherapy "Description" and "Comments" sections in related LCD relative to codes 90846, 90847, and 90849.
The medical record should document the medical necessity of narcosynthesis for psychiatric diagnostic and/or therapeutic purposes (e.g., the patient had difficulty verbalizing their psychiatric problems without the aid of the drug). The record should also document the specific pharmacological agent, dosage administered, and whether the technique was effective or non-effective.
The record must indicate that the Psychotherapy in Crisis guidelines under the "Description" and "Comments" sections in the related LCD were followed.
Claims for 90880 must be submitted with a covered diagnosis.
The medical record must indicate the presence of mental illness or signs of mental illness for which psychological testing is indicated as an aid in the diagnosis and therapeutic planning. The record must show the tests performed, scoring and interpretation, as well as the time involved.
The medical record must document that the Central Nervous System Assessments/Tests guidelines outlined in the "Description" and "Comments" sections in the related LCD were followed.
Response To Comments
Coding information, bill type codes, revenue codes, cpt/hcpcs codes.
CPT code 90863 is invalid for Medicare.
CPT/HCPCS Modifiers
Icd-10-cm codes that support medical necessity.
The correct use of an ICD-10-CM code listed below does not assure coverage of a service. The service must be reasonable and necessary in the specific case and must meet the criteria specified in the related determination.
Psychiatric Diagnoses:
Other Medical Diagnoses Not Included in DSM-IV™:
Medicare coverage for CPT code 90845 Psychoanalysis includes the following diagnosis codes:
Hypnosis may be used for diagnostic or therapeutic purposes. Medicare will cover CPT code 90880 Hypnotherapy for the following diagnosis codes:
ICD-10-CM Codes that DO NOT Support Medical Necessity
Severe and profound intellectual disabilities (ICD-10-CM codes F72, F73, and F79) are never covered for psychotherapy services or psychoanalysis (CPT codes 90832-90840, 90845-90849 and 90853). In such cases, rehabilitative, evaluation and management (E/M) codes should be reported.
ICD-10-PCS Codes
Additional icd-10 information.
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type. Complete absence of all Bill Types indicates that coverage is not influenced by Bill Type and the article should be assumed to apply equally to all claims.
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination. Complete absence of all Revenue Codes indicates that coverage is not influenced by Revenue Code and the article should be assumed to apply equally to all Revenue Codes.
Other Coding Information
Coding table information, revision history information, associated documents.
Read the Article Disclaimer
Email this document to yourself or someone else
An asterisk ( * ) indicates a required field. This email will be sent from you to the recipient email address(es) you enter. Please do not use this feature to contact CMS. To submit a comment or question to CMS, please use the Feedback/Ask a Question link available at the bottom of every MCD page.
Contractor Detail
Article disclaimer, lcd reference article.
Articles are a type of document published by the Medicare Administrative Contractors (MACs). Articles often contain coding or other guidelines and may or may not be in support of a Local Coverage Determination (LCD).
Articles identified as “Not an LCD Reference Article” are articles that do not directly support a Local Coverage Determination (LCD). They do not include a citation of an LCD. An example would include, but is not limited to, the Self-Administered Drug (SAD) Exclusion List Articles. If you have a question about this kind of article, please contact the MAC listed within the Contractor Information section of the article.
Articles which directly support an LCD are known as “LCD Reference Articles” . The referenced LCD may be cited in the Article Text field and may also be linked to in the Related Documents field. Examples may include but are not limited to Response to Comments and some Billing and Coding Articles. If you have a question about this kind of article, please contact the MAC listed within the Contractor Information section of the article.
License Agreements
Please review and accept the agreements in order to view Medicare Coverage documents, which may include licensed information and codes.
LICENSE FOR USE OF PHYSICIANS' CURRENT PROCEDURAL TERMINOLOGY, FOURTH EDITION ("CPT")
End User Point and Click Amendment: CPT codes, descriptions and other data only are copyright 2023 American Medical Association. All Rights Reserved (or such other date of publication of CPT). CPT is a trademark of the American Medical Association (AMA).
You, your employees and agents are authorized to use CPT only as agreed upon with the AMA internally within your organization within the United States for the sole use by yourself, employees and agents. Use is limited to use in Medicare, Medicaid or other programs administered by the Centers for Medicare and Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
Any use not authorized herein is prohibited, including by way of illustration and not by way of limitation, making copies of CPT for resale and/or license, transferring copies of CPT to any party not bound by this agreement, creating any modified or derivative work of CPT, or making any commercial use of CPT. License to use CPT for any use not authorized herein must be obtained through the AMA, CPT Intellectual Property Services, AMA Plaza 330 N. Wabash Ave., Suite 39300, Chicago, IL 60611-5885. Applications are available at the AMA Web site, http://www.ama-assn.org/go/cpt .
Applicable FARS\DFARS Restrictions Apply to Government Use.
AMA Disclaimer of Warranties and Liabilities.
CPT is provided "as is" without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
CMS Disclaimer
The scope of this license is determined by the AMA, the copyright holder. Any questions pertaining to the license or use of the CPT should be addressed to the AMA. End Users do not act for or on behalf of the CMS. CMS DISCLAIMS RESPONSIBILITY FOR ANY LIABILITY ATTRIBUTABLE TO END USER USE OF THE CPT. CMS WILL NOT BE LIABLE FOR ANY CLAIMS ATTRIBUTABLE TO ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION OR MATERIAL CONTAINED ON THIS PAGE. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information or material. Should the foregoing terms and conditions be acceptable to you, please indicate your agreement and acceptance by clicking below on the button labeled "I Accept".
LICENSE FOR USE OF CURRENT DENTAL TERMINOLOGY (CDT TM )
End User License Agreement: These materials contain Current Dental Terminology (CDT TM ), copyright© 2023 American Dental Association (ADA). All rights reserved. CDT is a trademark of the ADA.
The license granted herein is expressly conditioned upon your acceptance of all terms and conditions contained in this agreement. By clicking below on the button labeled "I accept", you hereby acknowledge that you have read, understood and agreed to all terms and conditions set forth in this agreement.
If you do not agree with all terms and conditions set forth herein, click below on the button labeled "I do not accept" and exit from this computer screen.
If you are acting on behalf of an organization, you represent that you are authorized to act on behalf of such organization and that your acceptance of the terms of this agreement creates a legally enforceable obligation of the organization. As used herein, "you" and "your" refer to you and any organization on behalf of which you are acting.
- Subject to the terms and conditions contained in this Agreement, you, your employees and agents are authorized to use CDT only as contained in the following authorized materials and solely for internal use by yourself, employees and agents within your organization within the United States and its territories. Use of CDT is limited to use in programs administered by Centers for Medicare & Medicaid Services (CMS). You agree to take all necessary steps to ensure that your employees and agents abide by the terms of this agreement. You acknowledge that the ADA holds all copyright, trademark and other rights in CDT. You shall not remove, alter, or obscure any ADA copyright notices or other proprietary rights notices included in the materials.
- Any use not authorized herein is prohibited, including by way of illustration and not by way of limitation, making copies of CDT for resale and/or license, transferring copies of CDT to any party not bound by this agreement, creating any modified or derivative work of CDT, or making any commercial use of CDT. License to use CDT for any use not authorized herein must be obtained through the American Dental Association, 211 East Chicago Avenue, Chicago, IL 60611. Applications are available at the American Dental Association web site, http://www.ADA.org .
- Applicable Federal Acquisition Regulation Clauses (FARS)/Department of Defense Federal Acquisition Regulation supplement (DFARS) Restrictions Apply to Government Use. U.S. Government Rights Provisions.
- Organizations who contract with CMS acknowledge that they may have a commercial CDT license with the ADA, and that use of CDT codes as permitted herein for the administration of CMS programs does not extend to any other programs or services the organization may administer and royalties dues for the use of the CDT codes are governed by their commercial license.
- ADA DISCLAIMER OF WARRANTIES AND LIABILITIES. CDT is provided "as is" without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. No fee schedules, basic unit, relative values or related listings are included in CDT. The ADA does not directly or indirectly practice medicine or dispense dental services. The sole responsibility for software, including any CDT and other content contained therein, is with CMS; and no endorsement by the ADA is intended or implied. The ADA expressly disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon notice to you if you violate the terms of this Agreement. The ADA is a third party beneficiary to this Agreement.
- CMS DISCLAIMER. The scope of this license is determined by the ADA, the copyright holder. Any questions pertaining to the license or use of the CDT should be addressed to the ADA. End Users do not act for or on behalf of the CMS. CMS disclaims responsibility for any liability attributable to end user use of the CDT. CMS will not be liable for any claims attributable to any errors, omissions, or other inaccuracies in the information or material covered by this license. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information or material. The license granted herein is expressly conditioned upon your acceptance of all terms and conditions contained in this agreement. If the foregoing terms and conditions are acceptable to you, please indicate your agreement by clicking below on the button labeled "I Accept". If you do not agree to the terms and conditions, you may not access or use software. Instead you must click below on the button labeled "I Do Not Accept" and exit from this computer screen.
LICENSE FOR NATIONAL UNIFORM BILLING COMMITTEE (NUBC)
American hospital association disclaimer.
The American Hospital Association ("the AHA") has not reviewed, and is not responsible for, the completeness or accuracy of any information contained in this material, nor was the AHA or any of its affiliates, involved in the preparation of this material, or the analysis of information provided in the material. The views and/or positions presented in the material do not necessarily represent the views of the AHA. CMS and its products and services are not endorsed by the AHA or any of its affiliates.
Page Help for Article - Billing and Coding: Psychiatry and Psychology Services (A56937)
Introduction.
This page displays your requested Article. The document is broken into multiple sections. You can use the Contents side panel to help navigate the various sections. Articles are a type of document published by the Medicare Administrative Contractors (MACs). Articles often contain coding or other guidelines and may or may not be in support of a Local Coverage Determination (LCD).
Finding a specific code
Some articles contain a large number of codes. If you are looking for a specific code, use your browser's Find function (Ctrl-F) to quickly locate the code in the article. Sometimes, a large group can make scrolling thru a document unwieldy. You can collapse such groups by clicking on the group header to make navigation easier. However, please note that once a group is collapsed, the browser Find function will not find codes in that group.
More information
- Billing and Coding articles provide guidance for the related Local Coverage Determination (LCD) and assist providers in submitting correct claims for payment. Billing and Coding articles typically include CPT/HCPCS procedure codes, ICD-10-CM diagnosis codes, as well as Bill Type, Revenue, and CPT/HCPCS Modifier codes. The code lists in the article help explain which services (procedures) the related LCD applies to, the diagnosis codes for which the service is covered, or for which the service is not considered reasonable and necessary and therefore not covered.
- Response to Comment (RTC) articles list issues raised by external stakeholders during the Proposed LCD comment period.
- Self-Administered Drug (SAD) Exclusion List articles list the CPT/HCPCS codes that are excluded from coverage under this category. The Medicare program provides limited benefits for outpatient prescription drugs. The program covers drugs that are furnished "incident-to" a physician's service provided that the drugs are not "usually self-administered" by the patient. CMS has defined "not usually self-administered" according to how the Medicare population as a whole uses the drug, not how an individual patient or physician may choose to use a particular drug. For purpose of this exclusion, "the term 'usually' means more than 50 percent of the time for all Medicare beneficiaries who use the drug. Therefore, if a drug is self-administered by more than 50 percent of Medicare beneficiaries, the drug is excluded from coverage" and the MAC will make no payment for the drug.
- Draft articles are articles written in support of a Proposed LCD. A Draft article will eventually be replaced by a Billing and Coding article once the Proposed LCD is released to a final LCD.
Articles are often related to an LCD, and the relationship can be seen in the “Associated Documents” section of the Article or the LCD. Article document IDs begin with the letter “A” (e.g., A12345). Draft articles have document IDs that begin with “DA” (e.g., DA12345).
Printing a Document to PDF
Frequently Asked Questions (FAQs)
Are you a provider and have a question about billing or coding.
Please contact your Medicare Administrative Contractor (MAC). MACs can be found in the MAC Contacts Report .
Do you have questions related to the content of a specific Local Coverage Determination (LCD) or an Article?
Are you a beneficiary and have questions about your coverage, are you looking for codes (e.g., cpt/hcpcs, icd-10), local coverage.
For the most part, codes are no longer included in the LCD (policy). You will find them in the Billing & Coding Articles. Try using the MCD Search to find what you're looking for. Enter the code you're looking for in the "Enter keyword, code, or document ID" box. The list of results will include documents which contain the code you entered.
Please Note: For Durable Medical Equipment (DME) MACs only, CPT/HCPCS codes remain located in LCDs. All other Codes (ICD-10, Bill Type, and Revenue) have moved to Articles for DME MACs, as they have for the other Local Coverage MAC types.
National Coverage
NCDs do not contain claims processing information like diagnosis or procedure codes nor do they give instructions to the provider on how to bill Medicare for the service or item. For this supplementary claims processing information we rely on other CMS publications, namely Change Requests (CR) Transmittals and inclusions in the Medicare Fee-For-Service Claims Processing Manual (CPM).
In order for CMS to change billing and claims processing systems to accommodate the coverage conditions within the NCD, we instruct contractors and system maintainers to modify the claims processing systems at the national or local level through CR Transmittals. CRs are not policy, rather CRs are used to relay instructions regarding the edits of the various claims processing systems in very descriptive, technical language usually employing the codes or code combinations likely to be encountered with claims subject to the policy in question. As clinical or administrative codes change or system or policy requirements dictate, CR instructions are updated to ensure the systems are applying the most appropriate claims processing instructions applicable to the policy.
How do I find out if a specific CPT code is covered in my state?
Enter the CPT/HCPCS code in the MCD Search and select your state from the drop down. (You may have to accept the AMA License Agreement.) Look for a Billing and Coding Article in the results and open it. (Or, for DME MACs only, look for an LCD.) Review the article, in particular the Coding Information section.
If you need more information on coverage, contact the Medicare Administrative Contractor (MAC) who published the document. The contractor information can be found at the top of the document in the Contractor Information section (expand the section to see the details).
If you don’t find the Article you are looking for, contact your MAC .
Did you receive a Medicare coverage denial?
Was your Medicare claim denied? Here are some hints to help you find more information:
1) Check out the Beneficiary card on the MCD Search page.
2) Try using the MCD Search and enter your information in the "Enter keyword, code, or document ID" box. Your information could include a keyword or topic you're interested in; a Local Coverage Determination (LCD) policy or Article ID; or a CPT/HCPCS procedure/billing code or an ICD-10-CM diagnosis code. Try entering any of this type of information provided in your denial letter.
3) Contact your MAC .
4) Visit Medicare.gov or call 1-800-Medicare.
It is Thursday and the weekly MCD data isn’t refreshed?
Are you having technical issues with the medicare coverage database (mcd), mcd session expiration warning.
Your MCD session is currently set to expire in 5 minutes due to inactivity. If your session expires, you will lose all items in your basket and any active searches. If you would like to extend your session, you may select the Continue Button.
Reset MCD Search Data
If you are experiencing any technical issues related to the search, selecting the 'OK' button to reset the search data should resolve your issues.
Connection denied by Geolocation Setting.
Reason: Blocked country: Russia
The connection was denied because this country is blocked in the Geolocation settings.
Please contact your administrator for assistance.
Find a Therapist
- Online Therapy
- Psychiatrists
- Treatment Centers
- Support Groups
Find detailed listings for mental health professionals in:
United states united states, top us cities popular cities.

IMAGES
VIDEO
COMMENTS
Outpatient Mental Health CPT Codes: 90832 - Psychotherapy, 30 minutes ( 16-37 minutes ). 90834 - Psychotherapy, 45 minutes ( 38-52 minutes ). 90837 - Psychotherapy, 60 minutes ( 53 minutes and over). 90846 - Family or couples psychotherapy, without patient present. 90847 - Family or couples psychotherapy, with patient present.
The CPT codes you'll likely use the most in your practice are: 90833: Psychotherapy, 30 minutes with patient and/or family member. 90834: Psychotherapy, 45 minutes with patient and/or family member. 90837: Psychotherapy, 60 minutes with patient and/or family member. 90853: Group psychotherapy.
Practical Information on E/M Coding from Psychiatric News. Guidance to Help Ensure You Are Coding Visits Correctly; Expert Explains Updated CPT Codes, How to Estimate E/M, Therapy Time; Webinar on the 2021 Billing and Documentation Changes to Outpatient E/M Services (99202-99215)
Psychiatry Codes The codes most frequently used by psychiatrists can be found in the Psychiatry subsection of the Medicine section of the CPT Manual (codes 90785-90899). For 2013 and beyond there have been major changes to the Psychiatry codes. A distinction has been made between an
Outpatient Mental Health CPT Codes: 90832 - Psychotherapy, 30 minutes ( 16-37 minutes ). 90834 - Psychotherapy, 45 minutes ( 38-52 minutes ). 90837 - Psychotherapy, 60 minutes ( 53 minutes and over). 90846 - Family or couples psychotherapy, without patient present.
Code Selection Rationale: Minimal risk follow-up visit for patient with a self-limited problem— bereavement. Straightforward level of work for the provider. 99212 + 90833 CC: F/U visit for 40-year-old executive with chronic depression and relationship problems being seen for weekly psychotherapy and medication management.
90791. Psychiatric diagnostic evaluation without medical services. 90792. Psychiatric diagnostic evaluation with medical services. 90832. Individual psychotherapy, 30 minutes. +90833. Individual ...
are many codes available to use for reporting services, the existence of the codes in the CPT manual does not guarantee that insurers will reimburse you for the services designated by those codes. Some insurers mandate that psychiatrists and other mental health providers only bill using the psychiatric codes (90801-90899).
Quick Guide to 2021 E/M Office/Outpatient Services (99202 - 99215) Coding Changes (.pdf) includes the summary below along with information on the new time ranges, prolonged services codes and a medical decision making table with psychiatric specific examples. The guide can be printed and serve as a handy resource as you adapt to the changes.
M0064 is defined as a brief office visit for the sole purpose of monitoring or changing drug prescriptions used in the treatment of mental, psychoneurotic and personality disorders. Based on the assignment of RVUs, the work involved in M0064 is similar to CPT code 99212. Time spent is generally less than ten minutes. V.
CPT code 90853 represents group therapy. When medically indicated, the interactive complexity add-on code (+90785) may be billed in conjunction with this code. CPT Code 90839 is for psychotherapy crisis for the first 60 minutes and code 90840 is for each additional 30 minutes. These codes are reported by themselves and may not be reported with ...
The Behavioral health coding resource (PDF) provides physician practices and their care teams with a list of key Current Procedural Terminology (CPT®) codes that can be used (as deemed medically appropriate) when administering behavioral health screening, treatment and/or preventative services.. This is part of AMA's broader efforts to empower health care organizations to overcome obstacles ...
CPT Codes 90832-90838 represent psychotherapy. Psychotherapy without medical evaluation and management services are reported as 90832, 90834 and 90837. Psychotherapy with medical evaluation and management services are reported with codes for E/M services plus a psychotherapy add-on code (90833; 90836; 90838).
Current Procedural Terminology (CPT) Codes in Psychiatry. +90833 - Use add-on code for Individual psychotherapy, insight oriented, behavior modifying and/or supportive, 30 minutes with the patient and/or family member (time range 16-37 minutes), when performed with an evaluation and management service. +90836 - Use add-on code for Individual ...
Pathology and Laboratory: 80047 to 89398. Medicine: 90281 to 99199 and 99500 to 99607. Each section contains subfields to correspond to a particular field and includes guidelines to follow. For example, therapists commonly use psychotherapy CPT codes between 90832 and 90853, under Medicine's psychiatry section.
The APA Practice Management HelpLine has been receiving a number of questions regarding coding and documentation using the recently revised outpatient E/M code requirements. The following guidance will help you select the appropriate level of an outpatient E/M service and document it correctly.
A simple list of CPT billing codes for Psychiatry Providers Use this simple chea CPT Coding Guide for Psychiatry | SonderMind <style>.gatsby-image-wrapper noscript [data-main-image]{opacity:1!important}.gatsby-image-wrapper [data-placeholder-image]{opacity:0!important}</style>
Procedure codes 90833, 90836 and 90838 are add on codes that should be used in conjunction with evaluation and management (E/M) codes 99201-99239, 99304-99337, 99341-99350. Psychotherapy codes that include an evaluation and management component are payable only to physicians, NPs and CNSs. The evaluation and management component of the services ...
reimbursed psychiatrists for E/M codes for outpatient services. Psychiatrists were essentially restricted to the use of the basic "one size fits all" 90862 code for pharmacologic management. Code 90862 poorly described the complexity of current psychiatric practice and accounted for 60% of psychiatrist billing.
Behavioral Health Coding Resource This resource outlines key CPT® codes that physicians and their care teams can use (as ... Psychiatric Collaborative Care Management 99492, 99493, 99494, G2214 Cognitive Assessment and Care Plan Services ... 99407 Smoking and tobacco use cessation counseling visit • 99408, 99409 Alcohol and/or substance ...
Use of Code G2212 CPT Requirements for Use of Code 99417 99205 Under 89 minutes Under 75 minutes 99205 and one unit 89-103 minutes 75-89 minutes 99205 and two units 104-118 minutes 90-104 minutes 99205 and three (or more) units for each 15 minutes 119 minutes or more 105 minutes or more Established Patient Visit (99215; 40-54 minutes) Number of ...
2013 psychiatry codes • Psychiatric services now may be reported with the same range of complexity and physician work as has long been available to all other medical specialties - In addition, E/M codes typically pay more for the same service 13 14 AACAP Evaluation and Management Services Guide Coding by Key Components History Chief Complaint
Payable under FQHC prospective payment system (PPS). Codes G0469 and G0470 must be reported with a qualifying visit code (e.g., 90791, 90792, 90832-90839, 90845) FQHC (provider-based and free-standing) claims submitted on a 77X type of bill. Mental health visit codes G0469 and G0470 must be reported with revenue code 0900 or 0519.
I have a behavioral health visit that was done under a 2 year old's chart. The mom came in because she is struggling with depression and elevated anxiety (according to the provider's notes) due to the loss of two siblings. The provider originally billed 90832 with Z63.79 which denied.
Overview. Our mission is to assist Pennsylvanians in leading safe, healthy, and productive lives through equitable, trauma-informed, and outcome-focused services while being an accountable steward of commonwealth resources. Report Abuse or Neglect. Report Assistance Fraud. Program Resources & Information.
If you are looking for a professional therapist, psychologist, or counselor near you, you can browse our extensive directory of the best providers on Psychology Today. Whether you need help with ...
Donald Trump's conviction by a New York jury on 34 felony counts is historic and unprecedented. No former president or major party presidential candidate has also been a felon.
Psychiatry Codes The codes most frequently used by psychiatrists can be found in the Psychiatry subsection of the Medicine section of the CPT Manual (codes 90785-90899). In 2013 there were major changes to the Psychiatry codes. A distinction was made between an initial evaluation with medical services done by a
To be eligible for this exemption, the outpatient visit must be with a qualified mental health professional at VA or provided through VA's network of community care providers. VA will automatically refund Veterans for any copays paid to VA on or after June 27, 2023 for these appointments, with no further action required by those Veterans.
You can use this tool to find and compare different types of Medicare providers (like physicians, hospitals, nursing homes, and others). Use our maps and filters to help you identify providers that are right for you. Find Medicare-approved providers near you & compare care quality for nursing homes, doctors, hospitals, hospice centers, more.