- To save this word, you'll need to log in. Log In
wandering rash

Definition of wandering rash
Word history.
wandering entry 2
Love words?
You must — there are over 200,000 words in our free online dictionary, but you are looking for one that’s only in the Merriam-Webster Unabridged Dictionary.
Start your free trial today and get unlimited access to America's largest dictionary, with:
- More than 250,000 words that aren't in our free dictionary
- Expanded definitions, etymologies, and usage notes
- Advanced search features
Dictionary Entries Near wandering rash
wandering of the poles
wandering sailor
Cite this Entry
“Wandering rash.” Merriam-Webster.com Dictionary , Merriam-Webster, https://www.merriam-webster.com/dictionary/wandering%20rash. Accessed 26 Jun. 2024.
Subscribe to America's largest dictionary and get thousands more definitions and advanced search—ad free!

Can you solve 4 words at once?
Word of the day.
See Definitions and Examples »
Get Word of the Day daily email!
Popular in Grammar & Usage
Plural and possessive names: a guide, your vs. you're: how to use them correctly, every letter is silent, sometimes: a-z list of examples, more commonly mispronounced words, how to use em dashes (—), en dashes (–) , and hyphens (-), popular in wordplay, 8 words for lesser-known musical instruments, birds say the darndest things, 10 words from taylor swift songs (merriam's version), 10 scrabble words without any vowels, 12 more bird names that sound like insults (and sometimes are), games & quizzes.

Description of Skin Lesions
- Lesion Type (Primary Morphology) |
- Lesion Configuration (Secondary Morphology) |
- Location and Distribution |
- Other Clinical Signs |
An extensive language has been developed to standardize the description of skin lesions, including
Lesion type (sometimes called primary morphology)
Lesion configuration (sometimes called secondary morphology)
Location and distribution
Rash is a general term for a temporary skin eruption.
(See also Evaluation of the Dermatologic Patient and Diagnostic Tests for Skin Disorders .)
Cross-Section of the Skin and Skin Structures
Lesion type (primary morphology).
Macules are flat, nonpalpable lesions usually < 10 mm in diameter. Macules represent a change in color and are not raised or depressed compared to the skin surface. A patch is a large macule. Examples include freckles, flat moles, tattoos, and port-wine stains , and the rashes of rickettsial infections , rubella , measles (can also have papules and plaques), and some allergic drug eruptions .

Papules are elevated lesions usually < 10 mm in diameter that can be felt or palpated. Examples include nevi , warts , lichen planus , insect bites, seborrheic keratoses , actinic keratoses , some lesions of acne , and skin cancers . The term maculopapular is often loosely and improperly used to describe many erythematous rashes; because this term is nonspecific and easily misused, it should be avoided.

Plaques are palpable lesions > 10 mm in diameter that are elevated or depressed compared to the skin surface. Plaques may be flat topped or rounded. Lesions of psoriasis and granuloma annulare commonly form plaques.

Nodules are firm papules or lesions that extend into the dermis or subcutaneous tissue. Examples include cysts , lipomas , and fibromas .
Vesicles are small, fluid-filled blisters < 10 mm in diameter. Vesicles are characteristic of herpes infections, acute allergic contact dermatitis , and some autoimmune blistering disorders (eg, dermatitis herpetiformis ).

Bullae are fluid-filled blisters > 10 mm in diameter. These may be caused by burns, bites, irritant contact dermatitis or allergic contact dermatitis , and drug reactions. Classic autoimmune bullous diseases include pemphigus vulgaris and bullous pemphigoid . Bullae also may occur in inherited disorders of skin fragility.

Pustules are vesicles that contain pus. Pustules are common in bacterial infections and folliculitis and may arise in some inflammatory disorders including pustular psoriasis .

Urticaria (wheals or hives) is characterized by elevated lesions caused by localized edema. Wheals are pruritic and erythematous. Wheals are a common manifestation of hypersensitivity to medications, stings or bites, autoimmunity, and, less commonly, physical stimuli including temperature, pressure, and sunlight. The typical wheal lasts < 24 hours.

Scale is heaped-up accumulations of horny epithelium (stratum corneum) that occur in disorders such as psoriasis , seborrheic dermatitis , and fungal infections. Pityriasis rosea and chronic dermatitis of any type may be scaly.
Crusts (scabs) consist of dried serum, blood, or pus. Crusting can occur in inflammatory or infectious skin diseases (eg, impetigo ).
Erosions are open areas of skin that result from loss of part or all of the epidermis. Erosions can be traumatic or can occur with various inflammatory or infectious skin diseases. An excoriation is a linear erosion caused by scratching, rubbing, or picking.
Ulcers result from loss of the epidermis and at least part of the dermis. Causes include venous stasis dermatitis , physical trauma with or without vascular compromise (eg, caused by decubitus ulcers or peripheral arterial disease ), infections, and vasculitis .
Petechiae are nonblanchable punctate foci of hemorrhage. Causes include platelet abnormalities (eg, thrombocytopenia, platelet dysfunction ), vasculitis , and infections (eg, meningococcemia, Rocky Mountain spotted fever , other rickettsioses).
Purpura is a larger area of hemorrhage that may be palpable. Purpura does not blanch. Palpable purpura is considered the hallmark of leukocytoclastic vasculitis. Purpura may indicate a coagulopathy. Large areas of purpura may be called ecchymoses or, colloquially, bruises.
Atrophy is thinning of the skin, which may appear dry and wrinkled, resembling cigarette paper. Atrophy may be caused by chronic sun exposure, aging, and some inflammatory and neoplastic skin diseases, including cutaneous T-cell lymphoma and lupus erythematosus . Atrophy also may result from long-term use of potent topical corticosteroids.
Scars are areas of fibrosis that replace normal skin after injury. Some scars become hypertrophic or thickened and raised. Keloids are hypertrophic scars that extend beyond the original wound margin.
Telangiectases are foci of small, permanently dilated blood vessels that may occur in areas of sun damage, rosacea , systemic diseases (especially systemic sclerosis ), or inherited diseases (eg, ataxia-telangiectasia , hereditary hemorrhagic telangiectasia ) or after long-term therapy with topical fluorinated corticosteroids.

Lesion Configuration (Secondary Morphology)
Configuration is the shape of single lesions and the arrangement of clusters of lesions.
Linear lesions take on the shape of a straight line and are suggestive of some forms of contact dermatitis , linear epidermal nevi, and lichen striatus. Excoriations resulting from scratching are typically linear.
Annular lesions are rings with central clearing. Examples include granuloma annulare , some drug eruptions, some dermatophyte infections (eg, tinea [ringworm]), and secondary syphilis .

Nummular lesions are circular or coin-shaped; an example is nummular dermatitis (nummular eczema).

MION/PHANIE/SCIENCE PHOTO LIBRARY
Target (bull’s-eye or iris) lesions appear as rings with central duskiness and are classic for erythema multiforme .

Serpiginous lesions have linear, branched, and curving elements. Examples include some fungal and parasitic infections (eg, cutaneous larva migrans ).
Reticulated lesions have a lacy or networked pattern. Examples include cutis marmorata and livedo reticularis.

Herpetiform describes grouped papules or vesicles arranged like those of a herpes simplex infection .

Zosteriform describes lesions clustered in a dermatomal distribution similar to those of herpes zoster .
Texture of Skin Lesions
Some skin lesions have a visible or palpable texture that suggests a diagnosis.
Verrucous lesions have an irregular, pebbly, or rough surface. Examples include warts and seborrheic keratoses .
Lichenification is thickening of the skin with accentuation of normal skin markings; it results from repeated scratching or rubbing.

Induration, or deep thickening of the skin, can result from edema, inflammation, or infiltration, including by cancer. Indurated skin has a hard, resistant feeling. Induration is characteristic of panniculitis , some skin infections, and cutaneous metastatic cancers.
Umbilicated lesions have a central indentation and are usually viral. Examples include molluscum contagiosum and herpes simplex .
Xanthomas, which are yellowish, waxy lesions, may be idiopathic or may occur in patients who have lipid disorders.

Location and Distribution of Skin Lesions
It is important to note whether
Lesions are single or multiple.
Particular body parts are affected (eg, palms or soles, scalp, mucosal membranes).
Distribution is random or patterned, symmetric or asymmetric.
Lesions are on sun-exposed or protected skin.
Although few patterns are pathognomonic, some are consistent with certain diseases.
Psoriasis frequently affects the scalp, extensor surfaces of the elbows and knees, umbilicus, and the gluteal cleft.
Lichen planus frequently arises on the wrists, forearms, genitals, and lower legs.
Vitiligo may be patchy and isolated or may group around the distal extremities and face, particularly around the eyes and mouth.
Discoid lupus erythematosus has characteristic lesions on sun-exposed skin of the face, especially the forehead, nose, and the conchal bowl of the ear.
Hidradenitis suppurativa involves skin containing a high density of apocrine glands, including the axillae, groin, and under the breasts.
Color of Skin Lesions
When examining the color of skin, health care professionals should note that the natural color of a patient's skin can change the appearance of colors.
Red skin (erythema) can result from many different inflammatory or infectious diseases. Cutaneous tumors are often pink or red. Superficial vascular lesions such as port-wine stains may appear red.
Orange skin is most often seen in hypercarotenemia, a usually benign condition of carotene deposition after excess dietary ingestion of beta-carotene.
Yellow skin is typical of jaundice , xanthelasmas and xanthomas, and pseudoxanthoma elasticum .
Green fingernails suggest Pseudomonas aeruginosa infection.
Violet skin may result from cutaneous hemorrhage or vasculitis . Vascular lesions or tumors, such as Kaposi sarcoma and hemangiomas, can appear purple. A lilac color of the eyelids or heliotrope eruption is characteristic of dermatomyositis .
Shades of blue, silver, and gray
Black skin lesions may be melanocytic, including nevi and melanoma . Black eschars are collections of dead skin that can arise from infarction, which may be caused by infection (eg, anthrax , angioinvasive fungi including Rhizopus , meningococcemia ), calciphylaxis , arterial insufficiency, or vasculitis .
Other Clinical Signs of Skin Lesions
Dermatographism (dermographism) is the appearance of an urticarial wheal after focal pressure (eg, stroking or scratching the skin) in the distribution of the pressure. Up to 5% of patients may exhibit this sign, which is a form of physical urticaria.

Darier sign refers to rapid swelling of a lesion when stroked. It occurs in patients with urticaria pigmentosa or mastocytosis .

© Springer Science+Business Media
Nikolsky sign is epidermal shearing that occurs with gentle lateral pressure on seemingly uninvolved skin in patients with toxic epidermal necrolysis and some autoimmune bullous diseases .
Auspitz sign is the appearance of pinpoint bleeding after scale is removed from plaques in psoriasis .
Koebner phenomenon describes the development of lesions within areas of trauma (eg, caused by scratching, rubbing, or injury). Psoriasis frequently exhibits this phenomenon, as may lichen planus , often resulting in linear lesions.

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
- Cookie Preferences

Dermatologists.org

Understanding Rashes: Causes, Symptoms, and Treatments
Rashes are a common skin condition that affects people of all ages and backgrounds. These skin abnormalities can be caused by various factors, including allergic reactions, infections, autoimmune disorders, environmental factors, and even medications and chemicals. Understanding what rashes are, their causes and symptoms, and the possible treatments available can help you better manage this condition and restore your skin’s health. In this article, we will explore the intricacies of rashes, their causes, symptoms, and treatments, and how to identify and manage them effectively.
What Are Rashes?
Rashes are skin abnormalities characterized by areas of redness, inflammation, and itching. They can appear as bumps, blisters, scales, or discoloration on the skin’s surface. The severity of the rash can range from minor irritation to severe discomfort and pain. In most cases, rashes are harmless, and they tend to go away on their own without treatment. However, some rashes can indicate underlying health conditions that require medical attention.
Definition and Types of Rashes
A rash is defined as an area of skin that becomes irritated, inflamed, or discolored. They can be classified based on their appearance, location, and underlying causes. Some common types of rashes include:
- Atopic Dermatitis – commonly known as eczema, this type of rash is characterized by dry, scaly, and itchy skin that tends to flare up periodically.
- Contact Dermatitis – caused by skin contact with irritants such as soaps, detergents, and chemicals, this rash appears as a red, itchy, and swollen area on the skin.
- Psoriasis – this rash is characterized by red, scaly patches that can be itchy or tender and usually appears on the scalp, knees, elbows, and lower back.
- Hives – caused by an allergic reaction, hives appear as raised, red, and itchy bumps that can spread across the body.
- Rosacea – characterized by redness, pimples, and visible blood vessels, this rash usually appears on the face and can worsen over time.
It is important to note that rashes can be caused by a variety of factors, and the type of rash a person experiences can vary depending on the underlying cause. For example, a rash caused by an allergic reaction may appear differently than a rash caused by a bacterial infection.
Common Skin Conditions That Cause Rashes
Rashes can be caused by various skin conditions, including:
- Fungal, bacterial, or viral infections such as ringworm, impetigo, and shingles.
- Autoimmune disorders such as lupus, psoriasis, and dermatomyositis.
- Environmental factors such as heat, humidity, and exposure to extreme weather conditions.
- Medications and chemicals such as antibiotics, painkillers, and topical creams.
- Allergies to substances such as food, pet dander, and certain fabrics.
In addition to these common causes, there are also several less common skin conditions that can cause rashes. For example, some types of cancer can cause rashes as a symptom. It is important to consult with a healthcare professional if you experience a rash that is persistent, severe, or accompanied by other symptoms.
Overall, rashes are a common skin condition that can be caused by a variety of factors. While most rashes are harmless and tend to go away on their own, some may require medical attention. If you experience a rash, it is important to pay attention to any accompanying symptoms and seek medical advice if necessary.
Causes of Rashes
The underlying causes of rashes can vary depending on the type and severity of the condition. Here are some of the common causes of rashes:
Allergic Reactions
Allergies to specific substances such as food, pet dander, and pollen can trigger allergic reactions that lead to rashes. In some cases, the reaction may be immediate, while in others, it may take several days to appear. Allergic reactions can cause hives, rash, itching, and swelling in the affected area.
For example, if you are allergic to peanuts and you eat food that contains peanuts, you may develop a rash on your skin. Similarly, if you are allergic to pollen and you go outside during the peak pollen season, you may develop a rash on your skin.
Fungal, bacterial, and viral infections can lead to rashes in different parts of the body. For example, a fungal infection such as ringworm can lead to itchy and scaly patches on the skin, while a bacterial infection such as impetigo can cause red sores that ooze fluid and crust.
In addition, viral infections such as chickenpox and measles can cause rashes on the skin. These rashes may be accompanied by other symptoms such as fever, headache, and body aches.
Autoimmune Disorders
Autoimmune disorders occur when the body’s immune system attacks its tissues and organs. This can lead to various skin conditions such as psoriasis, lupus, and dermatomyositis, which can cause rashes, scaly patches, and other skin abnormalities.
Psoriasis, for example, is a chronic autoimmune condition that causes thick, red, and scaly patches on the skin. Lupus, on the other hand, is an autoimmune disease that can affect various organs in the body, including the skin. People with lupus may develop a butterfly-shaped rash on their face.
Environmental Factors
Exposure to extreme weather conditions, heat, and humidity can cause rashes on the skin. These rashes may appear as blisters, bumps, or patches on the skin. Sunburns can also lead to skin rashes in some people.
If you spend too much time in the sun without protection, you may develop a sunburn that can cause a rash on your skin. Similarly, if you spend a lot of time in a hot and humid environment, you may develop a heat rash that can cause small, itchy bumps on your skin.
Medications and Chemicals
Some medications such as antibiotics, pain killers, and topical creams can cause skin rashes as an adverse reaction. Chemicals such as detergents and soaps can also irritate the skin and cause rash and itching.
If you are taking a medication and you develop a rash on your skin, it may be a sign of an allergic reaction. Similarly, if you use a new soap or detergent and you develop a rash on your skin, it may be a sign of an irritation caused by the chemical in the product.
It is important to identify the underlying cause of a rash in order to treat it effectively. If you develop a rash that does not go away or gets worse, you should see a doctor for a proper diagnosis and treatment.
Identifying Rashes
Identifying rashes can help you determine their underlying cause and possible treatment options. Here are some key factors to consider when identifying rashes:
Visual Characteristics
Rashes can appear as red, itchy, scaly, or blistering areas on the skin’s surface. The shape, size, and location of the rash can also vary depending on the underlying cause.
For example, a rash caused by contact dermatitis may appear as a red, itchy, and scaly area on the skin that has come into contact with an irritating substance. On the other hand, a rash caused by a viral infection such as chickenpox may appear as small, fluid-filled blisters that are accompanied by fever and fatigue.
Location and Distribution
The location and distribution of the rash can indicate the possible cause of the condition. For example, eczema tends to appear on the arms and legs, while psoriasis usually affects the scalp, elbows, knees, and lower back.
Other factors that can affect the location and distribution of a rash include age, gender, and overall health. For instance, shingles, a viral infection that causes a painful rash, tends to affect older adults and people with weakened immune systems.
Associated Symptoms
Rashes may be accompanied by other symptoms such as itching, burning, and pain. The severity and duration of these symptoms can vary depending on the underlying condition.
For example, a rash caused by an allergic reaction may be accompanied by itching and swelling, while a rash caused by a bacterial infection may be accompanied by pain and tenderness.
It is important to pay attention to these associated symptoms as they can help your healthcare provider determine the underlying cause of the rash and provide appropriate treatment.
In conclusion, identifying rashes involves taking into account visual characteristics, location and distribution, and associated symptoms. By doing so, you can get a better understanding of the underlying cause of the rash and seek appropriate treatment.
Symptoms of Rashes
Rashes can cause various symptoms depending on their underlying cause and severity. However, some common symptoms of rashes include:
Itching and Irritation
Rashes are often accompanied by itching and irritation, which can be mild or severe. Scratching the rash can lead to further irritation and infection.
Redness and Inflammation
Rashes typically appear as red and inflamed areas on the skin’s surface. The severity of the inflammation can vary depending on the underlying cause.
Blisters and Lesions
Some rashes can lead to the development of blisters or lesions on the skin’s surface. These can be painful and may increase the risk of infection.
Dryness and Scaling
Rashes can cause dryness and scaling of the affected areas, leading to flaking and peeling of the skin. This may cause discomfort and may worsen the condition.
Treatments for Rashes
The treatment options for rashes depend on the underlying cause and severity of the condition. Some simple home remedies that can provide relief from rashes include:
- Applying a cool compress to the affected area to reduce inflammation and soothe itching.
- Using over-the-counter creams and ointments to relieve itchiness and scaly skin.
- Avoiding known irritants and allergens that can trigger rashes.
- Maintaining good hygiene practices to prevent infection and further irritation.
If the rash is severe or does not respond to home remedies, medical treatment may be necessary. In such cases, doctors may prescribe oral or topical medications to alleviate the symptoms and manage the underlying condition.
Rashes are common skin conditions that can be caused by various factors. Understanding their causes, symptoms, and possible treatments can help you manage the condition effectively and restore your skin’s health. By following the preventive measures and seeking medical attention when necessary, you can reduce the risk of complications and improve your overall well-being.
Leave a Comment Cancel Reply
You must be logged in to post a comment.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Rash That Moves or Spreads to Other Body Parts
Probably Caused by Hives
- What Are Hives?
- Preventing Spreading
- Seeking Medical Care
If a rash seems to move around your body, it is likely hives.
Hives, medically known as urticaria , are a common rash that can be triggered by many different substances. Hives come and go, with some people experiencing them moving from one part of the body to the next.
This article will discuss hive symptoms and treatment. It will also cover when to contact a healthcare provider.
Kwangmoozaa / Getty Images
Hives: A Rash That Moves Around
Hives are an itchy, red rash that can be slightly raised off of the skin. It is caused when the immune system sees a threat and releases histamine from mast cells and basophils in the dermis of the skin . The released histamine causes dilation of the blood vessels and fluid to leak into the skin. This results in redness and swelling.
Differences Between Welts and Hives
Welts and hives are the two terms that are often used interchangeably but have slightly different meanings. A welt is a red, raised area of the skin that occurs from an injury or as an immune reaction. Hives are made up of welts. Hives are red, itchy welts that are always an immune reaction.
Triggers are substances that cause hives. There are several hive triggers, and someone may develop different triggers or always have the same ones throughout their lifetime. Triggers are either related to allergies or have no relation to allergies. Hives not related to allergies are more common.
Hives that are not related to allergies include:
- Hot and cold temperatures
- Infections (bacterial and viral)
- Skin pressure
- Emotional stress
- Sunlight or tanning beds
Hives that are related to allergies include:
- Medications
- Food (especially eggs, nuts, peanuts, and shellfish)
- Insect bites or stings
Appearance and Sensation
Hives can form on any area of the body at any age. Someone may have one small welt about 1–2 centimeters, or the affected area can be larger, with many welts covering entire areas of their body. Hives can also move around. They may start in one spot, disappear, and then reappear in another area.
Hives can be accompanied by angioedema , which is swelling of the deeper tissues and may feel warm and painful. When this occurs anywhere in the mouth or throat, it can make it difficult to breathe, and is a medical emergency, call 911 immediately.
Here are all the symptoms that may be experienced with hives:
- Light to bright red in color
- Raised welts
- Blanch (turn white) when pressed
Other Rashes That Look Like Hives
Hives are often mistaken for other types of rashes. The redness and itching are common symptoms with many rashes. Rashes that share similar characteristics to hives:
- Contact dermatitis
- Erythema multiforme
- Polymorphic light eruption
How to Keep a Hives Rash From Spreading
To keep hives from spreading it is important to identify and avoid any known triggers. This can prevent future occurrences as well.
Avoid using aspirin , alcohol, and nonsteroidal anti-inflammatory drugs (NSAIDs), which can worsen symptoms, and should not be used when someone has hives. Also do not scratch hives, as this can make symptoms worse.
Antihistamines
Antihistamines are used to block the histamine response and are very useful in treating hives. Over-the-counter medications like Claritin (loratadine) and Zyrtec (cetirizine) are typically nonsedating (not producing sleepinees) when used at prescribed doses.
Benadryl (diphenhydramine) is another antihistamine that can be used for hives, however, it does carry some side effects like drowsiness, which may not be tolerated by some people.
Topical Treatments
Two types of topical creams can help treat hives. The first are anti-itch lotions, which may include ingredients like calamine, menthol, camphor, and pramoxine. These can help soothe itchiness caused by hives.
The second type of topical cream is hydrocortisone cream. This is a steroid-based cream that reduces swelling and itching.
A cold compress is a nondrug option to reduce the itchiness and swelling from hives. Ice cubes wrapped in a washcloth can provide some relief.
Steroid Medications
For severe cases of hives, a healthcare provider may prescribe an oral steroid medication called prednisone or prednisolone to reduce hive inflammation and itchiness.
These medications need to be taken as directed, and they should not be stopped without first consulting a healthcare provider.
Light Therapy
Phototherapy , also known as light therapy, can be an effective treatment if someone is not responding to other treatments. It is typically done in a healthcare provider's office a few times per week for several months.
When to Consult a Healthcare Provider
Hives are generally self-limiting and resolve on their own or with simple home treatments. However, for some people hives can become chronic. Hives that appear every day or almost every day for six weeks or longer are considered chronic hives . If you have chronic hives, contact your healthcare provider for treatment guidance.
Call 911 immediately if hives are accompanied by difficulty breathing or swelling of the tongue or lips. This may be an anaphylactic reaction and is a life-threatening emergency.
A Word From Verywell
It is possible to treat hives at home with the use of over-the-counter antihistamines. If you are experiencing difficulty breathing or swallowing in association with hives, it is important to call 911 and seek medical attention.
Hives are a type of rash that causes red, itchy welts. They may come and go, and move around the body. For many people, treatment can be done at home with over-the-counter medications and creams. More severe cases need to be seen by a healthcare provider.
Nationwide Children's. Hives .
Schaefer P. Acute and chronic urticaria: evaluation and treatment . afp . 2017;95(11):717-724.
RxList. Definition of welt .
American Academy of Dermatology Association. Hives: signs and symptoms .
Center for Allergy & Asthma. Is it hives or something else?
Matos AL, Figueiredo C, Gonçalo M. Differential diagnosis of urticarial lesions . Front Allergy . 2022;3:808543. doi:10.3389%2Ffalgy.2022.808543
American College of Allergy, Asthma, & Immunology. Hives .
Joy N. Calamine lotion . JSSTD . 2022;4:83-86. doi:10.25259/JSSTD_77_2021
National Health Services. Steroids .
American Academy of Dermatology Associations. 10 ways to get relief from chronic hives .
By Patty Weasler, RN, BSN Weasler is a Wisconsin-based registered nurse with over a decade of experience in pediatric critical care.
What causes a rash that moves to different parts of the body?
Medically reviewed by Carmen Pope, BPharm . Last updated on Oct 4, 2023.
Official answer
Hives are raised red or skin-colored welts or rashes that typically flare up suddenly and have a habit of changing shape or moving from one area of the body to another. These welts can vary in size, and they are notorious for causing intense itching, often surrounded by a wheal. These wheals can sometimes merge, forming a map-like pattern or a large patch.
In 10% of people, there may also be swelling or edema which may affect the eyelids, lips, hands or elsewhere. While this swelling is usually short-lasting and not serious, it can become a cause for concern if it affects the throat, impeding breathing or causing hoarseness. In such cases, it's crucial to seek immediate medical attention by calling 911 or visiting the emergency room.

The Medical Term: Urticaria
Hives are medically referred to as urticaria, derived from the Latin words "urtica" meaning nettle and "urere" meaning to burn. Despite their commonality, hives can manifest differently from one person to another and may even vary within the same individual on different occasions.
Although these welts are raised, they typically have a smooth surface (unlike dermatitis, which tends to be rough). Some individuals may have bright red welts, while others may experience paler, skin-colored welts. Some hives take on a circular appearance with a pale center and a distinctive red halo.
Other symptoms associated with hives may include a burning or stinging sensation. When pressed, the center of a red hive usually turns white; this phenomenon is known as "blanching." Hives can migrate across the skin, appearing on one part of the body for a short period, disappearing, and then reappearing in a different area.
Diagnosing Hives: What You Need to Know
Hives are known for their ever-changing nature. They typically don't stick around for more than 24 to 48 hours, and they can look different from day to day or episode to episode. You don't need to capture pictures; doctors can diagnose hives by listening to your description of symptoms.
However, if hives last for more than six weeks (which is considered chronic), dermatologists might run some tests. These could include allergy tests, blood work, or a skin biopsy. They may also ask about your family's hives history. But in most cases of chronic hives, the cause remains a mystery.


Causes of Hives
While many assume that hives are primarily caused by allergies, it's essential to note that over 75% of hives in adults are not related to allergies. However, in cases where allergies are a trigger, common culprits include:
- Blood transfusions
- Certain foods like berries, chocolate, eggs, fish, nuts, shellfish, soy, or wheat
- Food additives such as tartrazine or MSG
- Insect stings and bites, or jellyfish stings
- Medications, including antibiotics, aspirin, and ibuprofen
- Plants like poison oak, poison ivy, and sumac
Hives can also be triggered by environmental factors, bacteria, viruses, anxiety, or stress.
Types of Inducible Hives
Certain physical stimuli can induce hives in susceptible individuals. These include:
- Dermographism: Hives or raised skin areas appear where the skin has been stroked, scratched, or rubbed, or after contact with tight clothing or towel drying after a hot shower.
- Cold urticaria: Hives develop on skin exposed to cold air, cold water, ice blocks, or following cryotherapy.
- Cholinergic urticaria: Hives appear in response to sweat induced by exercise or emotional stress, or following a hot shower.
- Contact urticaria: Hives occur upon contact with an allergen, pseudoallergen, or irritating substance, such as cosmetics, hairy caterpillars, latex, meat, medicines, saliva, stinging nettle, textiles, or white flour.
- Delayed pressure urticaria: Hives appear (often after a few hours) where pressure has been exerted on a certain area of the skin, such as from a handbag, seatbelt, standing on a ladder rung, or sitting on a horse.
- Solar urticaria: Typically involves hives appearing on body areas not usually exposed to the sun, like the abdomen and top of the thighs, sparing the face, neck, and hands. It may be triggered by long-wavelength UV light or visible light.
- Heat urticaria: Hives develop on skin areas in contact with a hot water bottle or after ingesting a hot drink.
- Vibratory urticaria: Hives spontaneously occur after exposure to vibrations, such as using a jackhammer.
- Aquagenic urticaria: Hives develop upon exposure to fresh, chlorinated, or salty hot or cold water.

Related questions
- Can you have a vaginal yeast infection if you have no uterus?
- Prednisone: What are 12 Things You Should Know?
- Amoxicillin rash: When should I be concerned?
Hives Medications
Hives occur when certain chemicals in our body, like histamine, make your skin itchy, red, and swollen. To ease these symptoms, doctors often recommend antihistamines.
There are two types:
- Second-generation antihistamines : These include cetirizine , desloratadine , fexofenadine , or levocetirizin e. They don't usually make you drowsy and work by blocking histamine, which causes the itch and redness. Just follow the recommended dosages and stop when the hives disappear. Taking a second antihistamine doesn't help much.
- Older (first-generation) antihistamines : These, like promethazine or chlorpheniramine , can make you feel sleepy and have side effects like a dry mouth, blurry vision, or constipation. They can also interact with other medications. They're considered for severe hives when stronger relief is needed.
Managing Hives: Avoiding Triggers and Supporting Recovery
If your hives are connected to allergies, a combination of avoiding the allergen and using antihistamines usually helps hives go away within 48 hours. Some types of hives triggered by specific factors tend to clear up quickly, but others might hang around even after you remove the trigger.
To improve your chances of relief:
Address Underlying Infections : In some cases, chronic hives might be linked to infections like Helicobacter pylori or intestinal parasites. Treating these infections can help with chronic hives.
Lifestyle Adjustments : While some factors don't directly cause hives, they can make the situation worse. To ease discomfort, consider these steps:
- Stay cool and minimize heat exposure.
- Opt for pain relief alternatives like acetaminophen instead of drugs like aspirin, NSAIDs, or opioids.
- Reduce your intake of potential food triggers for at least three weeks.
- Apply cooling methods, like using a fan, an ice pack, or a cold cloth on the affected area.
- If you have specific types of hives, like solar urticaria, wearing sun-protective clothing can be helpful.
More pictures of Hives

- Hives: Diagnosis and Treatment. American Academy of Dermatology Association. 2023. https://www.aad.org/public/diseases/a-z/hives-treatment
- Hives and angioedema. Mayo Clinic. 2023. https://www.mayoclinic.org/diseases-conditions/hives-and-angioedema/symptoms-causes/syc-20354908
- Benedetti J. Urticaria MSD Manual Professional Version. Updated Sept 2022. https://www.msdmanuals.com/professional/dermatologic-disorders/approach-to-the-dermatologic-patient/urticaria
- Fine LM, Bernstein JA. Guideline of Chronic Urticaria Beyond. Allergy Asthma Immunol Res. 2016;8(5):396-403. doi:10.4168/aair.2016.8.5.396
Hives vs Rash - What's the difference between them?
The main difference between hives and a rash is that hives are a particular type of rash, characterized by swollen, pale-red or skin-colored bumps on the skin that appear and disappear quickly, and tend to “blanch” (which means turn white) when pressed. Hives are also known as urticaria. Continue reading
Is triamcinolone good for poison ivy?
Steroid prescription creams or ointments like high-potency triamcinolone 0.5% may be helpful during the first few days of a poison ivy rash on a small area, but have little effect once the fluid-filled blisters have appeared. Over-the-counter (OTC) products like hydrocortisone cream 1% are not usually strong enough for poison ivy. Your doctor may prescribe oral prednisone pills for a more severe rash. Continue reading
What should I do if I develop a rash while taking lamotrigine?
Contact your healthcare provider or other emergency medical services right away if you develop a skin rash, blistering or peeling of your skin, hives, painful sores in your mouth or around your eyes or other signs of a drug allergy (such as a fever or swelling of your lymph nodes) while taking lamotrigine. This could signal you are having a serious side effect to lamotrigine which may result in hospitalization or cause death. Continue reading
Related medical questions
- Prednisone vs Prednisolone - What's the difference?
- What is the best treatment for a poison ivy rash?
- I'm having a reaction after taking fluconazole, is this normal?
- Should I stop using Xulane if I get a rash?
- What are Hives (Urticaria)?
- Can triamcinolone acetonide B be used to treat severe diaper rash on a little girl?
- I think I have an allergy to my antibiotic! What can I do to treat my infection?
- What Vaccines do I need if I'm over 50?
- How do I keep from getting Mpox (monkeypox)?
- Do I have Mpox (monkeypox)?
- What are the most common skin conditions? (with photos)
- What is the Benadryl hat man?
- Zyrtec vs Claritin: Which is more effective for allergies?
- Allegra vs Claritin: Which is more effective for allergies?
- How long does Benadryl take to work?
- Does Benadryl help with or cause anxiety?
- Does Benadryl make you sleepy?
- Diphenhydramine Hydrochloride vs Citrate: What's the difference?
- How long before Xolair starts working?
- Does Feverfew interact with any drugs?
- Does Xolair cause cancer?
- How does Xolair work?
- Can you take Benadryl while pregnant?
- Xolair and Covid-19 vaccine, what should I know?
- Is Xyzal available over-the-counter?
- How long can Xolair stay out of the fridge?
- Can I take Xolair during pregnancy?
- Can Xolair be self-administered at home?
Related support groups
- Skin Rash (134 questions, 444 members)
- Hives (82 questions, 211 members)
- Dermatological Disorders (34 questions, 54 members)
- Urticaria (32 questions, 72 members)
- Dermatographism (1 questions, 7 members)
Medical Disclaimer
- Learn about a popular treatment for psoriasis
Hives, also known as urticaria, affects about 20 percent of people at some time during their lives. It can be triggered by many substances or situations and usually starts as an itchy patch of skin that turns into swollen red welts.
On this page
If you’ve had red or skin-colored bumps that appeared and disappeared quickly, then it’s unlikely to be simple bug bites. The skin rash could be hives, and the itching from hives may range from mild to severe. Hives, also known as urticaria , affects about 20 percent of people at some time during their lives. Scratching, alcoholic beverages, exercise and emotional stress may worsen the itching.
Hives Symptoms
- Raised itchy bumps, either red or skin-colored
- “Blanching” (when pressed, the center of a red hive turns white)
Hives Triggers
- Some food (especially peanuts, eggs, nuts and shellfish)
- Medications, such as antibiotics (especially penicillin and sulfa), aspirin and ibuprofen
- Insect stings or bites
- Physical stimuli, such as pressure, cold, heat, exercise or sun exposure
- Blood transfusions
- Bacterial infections, including urinary tract infections and strep throat
- Viral infections, including the common cold, infectious mononucleosis and hepatitis
- Some plants
Hives Management and Treatment
- Avoid known triggers
- See an allergist , who is specially trained to look for triggers to your hives and may recommend medications to prevent the hives or reduce the severity of symptoms. Whether your allergist suggests a treatment available only by prescription or an over the counter treatment will depend on several factors, including how uncomfortable the hives are making you.
Find expert care.
If you think you might have hives, then it’s best to speak with an allergist.
Symptoms can last anywhere from minutes to months – or even years.
While they resemble bug bites, hives (also known as urticaria) are different in several ways:
- Hives can appear on any area of the body; they may change shape, move around, disappear and reappear over short periods of time.
- The bumps – red or skin-colored “wheals” with clear edges – usually appear suddenly and go away just as quickly.
- Pressing the center of a red hive makes it turn white – a process called “blanching.”
There are two types of hives – short-lived (acute) and long-term (chronic). Neither is typically life-threatening, though any swelling in the throat or any other symptom that restricts breathing requires immediate emergency care.
Hives usually are caused by other things besides infection, although it could be from a virus. It could be from an allergen, or some sort of an allergy that you have. It could be from a hormonal change. And it even could be emotional in some situations. Allergist Stanley Fineman, MD
Chronic hives occur almost daily for more than six weeks and are typically itchy. Each hive lasts less than 24 hours. They do not bruise nor leave any scar. They typically do not have an identifiable trigger.
If your hives last more than a month or if they recur over time, see an allergist , who will take a history and perform a thorough physical exam to try and determine the cause of your symptoms. A skin test and challenge test may also be needed to identify triggers.
Therapies range from cool compresses to relieve itching to prescription antihistamines and other drugs, such as anti-inflammatory medications and medications that may modify your immune system .
Is It Hives or Angioedema?
Angioedema – swelling of tissue beneath the surface of the skin – can be mistaken for, or associated with hives. It can be caused by allergic reactions, medications or a hereditary deficiency of some enzymes. The following symptoms may indicate angioedema:
- Swelling in the eyes or mouth
- Swelling of the hands, feet or throat
- Difficulty breathing, stomach cramps or swelling of the lining of the eyes
The best way to identify your symptoms is to talk to an allergist who can diagnose and treat both hives and angioedema.
In some cases, the trigger is obvious – a person eats peanuts or shrimp , and then breaks out within a short time. Other cases require detective work by both the patient and the physician because there are many possible causes. If the hives have gone on for a long time, the cause is not usually identified.
A single episode of hives does not usually call for extensive testing. If a food allergy is suspected, consider keeping track of what you eat. This will help you discover whether there is a link between what you’re eating and when you break out with hives.
Chronic hives should be evaluated by an allergist, who will ask about your and your family’s medical history, substances to which you are exposed at home and at work, exposure to pets or other animals and any medications you’ve taken recently. If you have been keeping a food diary, show it to your allergist.
Your allergist may want to conduct skin tests, blood tests and urine tests to identify the cause of your hives. If a specific food is the suspected trigger, your allergist may do a skin-prick test or a blood test to confirm the diagnosis; once the trigger is identified, you’ll likely be advised to avoid that food and products made from it. In rare instances, the allergist may recommend an oral food challenge – a carefully monitored test in which you’ll eat a measured amount of the suspected trigger to see if hives develop. If a medication is suspected as the trigger, your allergist can conduct similar tests, and a cautious drug challenge – similar to an oral food challenge, but with medications – may also be needed to confirm the diagnosis. Because of the possibility of anaphylaxis , a life-threatening allergic reaction, these challenge tests should be done only under strict medical supervision, with emergency medication and equipment at hand.
In cases where vasculitis ( inflammation of the blood cells) may be the cause, your allergist may conduct a skin biopsy and send it to a specialist to examine under a microscope.
Management and Treatment
Researchers have identified many – but not all – of the factors that can cause hives. These include food and other substances you take, such as medications. Some people develop hives just by touching certain items. Some illnesses also cause hives. Here are a few of the most common causes:
- Some food (especially peanuts, eggs, nuts and shellfish)
- Physical stimuli such as pressure, cold, heat, exercise or sun exposure
Antihistamines – available either over the counter or by prescription – are a frequently recommended treatment for hives. They work by blocking the effect of histamine , a chemical in the skin that can cause allergy symptoms, including welts. Antihistamines that don’t make you drowsy are preferred. They are effective and long-lasting (may be taken once a day) and have few side effects. Your allergist may recommend a combination of two or three antihistamines to treat your hives, along with cold compresses or anti-itch balms to ease the symptoms.
Severe episodes of urticaria may require temporary treatment with prednisone, a similar corticosteroid medication or an immune modulator, which can reduce the severity of the symptoms.
If your reaction involves swelling of your tongue or lips, or you have trouble breathing, your allergist may prescribe an epinephrine (adrenaline) auto-injector for you to keep on hand at all times. These can be early symptoms of anaphylaxis, a potentially fatal allergic reaction that impairs breathing and can send the body into shock. The only treatment for anaphylaxis is epinephrine . If you develop hives and your injector is not nearby – or if using the auto-injector doesn’t cause the symptoms to immediately improve – call 911 or go to an emergency room immediately. Emergency medical services carry epinephrine and can provide prompt treatment. You should also go to the emergency room after using an auto-injector.
If the cause of hives can be identified, the best treatment is to avoid the trigger or eliminate it:
- Foods: Don’t eat foods that have been identified to cause your symptoms.
- Rubbing or scratching: Avoid harsh soaps. Frequent baths may reduce itching and scratching – beneficial because itching and scratching can make the hives feel worse.
- Constant pressure: Avoid tight clothing. Pressure hives can be relieved by wearing loose-fitting clothes.
- Temperature: If you develop hives when exposed to cold, do not swim alone in cold water and always carry an epinephrine auto-injector. Avoid exposure to cold air and use a scarf around your nose and mouth in cold weather. If you must be out in the cold, wear warm clothing.
- Sun exposure: Wear protective clothing; apply sunblock.
- Medications: Notify your physician or pharmacist immediately if you suspect that a specific medication is causing your hives.
Chronic hives
Some cases of hives last for more than six weeks and can last months or years. This condition is known as chronic hives.
If the cause cannot be identified, even after a detailed history and testing, the condition is called chronic idiopathic urticaria. (“Idiopathic” means “unknown.”) About half these cases are associated with some immune findings. Chronic hives may also be associated with thyroid disease, other hormonal problems or, in very rare instances, cancer. Even this condition usually dissipates over time.
Physical urticaria
In physical urticaria, the hives have a physical cause, such as exposure to heat, cold or pressure.
Common triggers include:
- Rubbing or scratching. This is the most frequent cause of physical urticaria. Symptoms appear within a few minutes in the place that was rubbed or scratched and typically last less than an hour.
- Pressure or constriction. Delayed pressure urticaria can appear as red swelling six to eight hours after pressure (belts or constrictive clothing, for example) has been applied. Symptoms can also occur in parts of the body under constant pressure, such as the soles of the feet.
- Change in temperature. Cold urticaria is caused by exposure to low temperatures followed by re-warming. This can be severe and life-threatening if there is a general body cooling – for example, after a plunge into a swimming pool.
- Higher body temperature. Cholinergic urticaria is due to an increase in body temperature because of sweating, exercise, hot showers and/or anxiety.
- Sun exposure. Solar urticaria may occur within a few minutes after exposure to the sun.
Inflammation of the blood vessels, or vasculitis, can also cause hives. These hives are more painful than itchy, may leave a bruise on the skin and often last more than a day.
Life’s too short to struggle with hives. Find answers with an allergist .
This page was reviewed for accuracy 6/11/2018.
Privacy Overview
Type your tag names separated by a space and hit enter
There's more to see -- the rest of this topic is available only to subscribers.
1. Download the Nursing Central app by Unbound Medicine
2. Select Try/Buy and follow instructions to begin your free 30-day trial

Want to regain access to Nursing Central?
Renew my subscription
Not now - I'd like more time to decide
Log in to Nursing Central
Forgot your password, forgot your username, contact support.
- unboundmedicine.com/support
- [email protected]
- 610-627-9090 (Monday - Friday, 9 AM - 5 PM EST.)
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- An Bras Dermatol
- v.91(4); Jul-Aug 2016
Geographic tongue and psoriasis: clinical, histopathological, immunohistochemical and genetic correlation - a literature review *
Bruna lavinas sayed picciani.
1 Universidade Federal Fluminense (UFF) - Niterói (RJ), Brazil.
Tábata Alves Domingos
Thays teixeira-souza, vanessa de carla batista dos santos, heron fernando de sousa gonzaga.
2 Universidade de Marília (Unimar) - Marília (SP), Brazil.
Juliana Cardoso-Oliveira
3 Universidade do Estado do Rio de Janeiro (UERJ) - Rio de Janeiro (RJ), Brazil.
Alexandre Carlos Gripp
Eliane pedra dias, sueli carneiro.
Geographic tongue is a chronic, inflammatory, and immune-mediated oral lesion of unknown etiology. It is characterized by serpiginous white areas around the atrophic mucosa, which alternation between activity, remission and reactivation at various locations gave the names benign migratory glossitis and wandering rash of the tongue. Psoriasis is a chronic inflammatory disease with frequent cutaneous involvement and an immunogenetic basis of great importance in clinical practice. The association between geographic tongue and psoriasis has been demonstrated in various studies, based on observation of its fundamental lesions, microscopic similarity between the two conditions and the presence of a common genetic marker, human leukocyte antigen (HLA) HLA-C*06. The difficulty however in accepting the diagnosis of geographic tongue as oral psoriasis is the fact that not all patients with geographic tongue present psoriasis. Some authors believe that the prevalence of geographic tongue would be much greater if psoriatic patients underwent thorough oral examination. This study aimed to develop a literature review performed between 1980 and 2014, in which consultation of theses, dissertations and selected scientific articles were conducted through search in Scielo and Bireme databases, from Medline and Lilacs sources, relating the common characteristics between geographic tongue and psoriasis. We observed that the frequency of oral lesions is relatively common, but to establish a correct diagnosis of oral psoriasis, immunohistochemical and genetic histopathological analyzes are necessary, thus highlighting the importance of oral examination in psoriatic patients and cutaneous examination in patients with geographic tongue.
INTRODUCTION
First described by Reiter in 1831, the geographic tongue (GT) is a chronic, inflammatory oral lesion, immunologically mediated and with unknown etiology. 1 - 5 It affects between 0.6% and 4.8% of the world population, occurring more often in children, with a slight preference for females, and with its frequency reducing with age. 5 - 7 It is characterized by serpiginous white areas around the depapillated mucosa, whose rotation among activity, remission and reactivation in diverse locations originated the denominations benign migratory glossitis and wandering rash of the tongue. 8
The white border consists of filiform papillae in regeneration and of a mixture of keratin and neutrophils, while erythematous area results from the loss of these papillae. Lesions tend to change location, pattern and size over time, affecting mainly the back and side edges of the tongue. 1 - 3 This migration is evidenced by epithelial desquamation in one location and a simultaneous proliferation in another, with periods of exacerbation and remission. 3 In most cases it is asymptomatic. However, some patients may report pain or burning sensation, especially during ingestion of spicy or acidic foods. 3 , 4 , 9
Psoriasis is a skin-articular disease, inflammatory, chronic, common, with genetic and immunological basis, and with great importance in clinical practice. 10 , 11 Psoriasis occurs in approximately 1-3% of the world population, affecting white individuals of both sexes. Clinically, psoriasis is divided into vulgaris, guttate, inverse, psoriatic arthritis, palmoplantar, pustular and erythrodermic, with common features such as erythema, desquamation and elevation. 11 - 13 Its etiology is unknown, but it is known that there is a defect in the normal cycle of epidermal development, with a disorder in the proliferation and differentiation of keratinocytes associated with inflammatory and vascular changes, with a leukocyte infiltrate composed of activated T-lymphocytes, neutrophils, dendrocytes and mast cells. The disease can be localized or generalized, affecting almost all the skin with an unpredictable course. 10 , 14 , 15
Studies show that geographic tongue is the oral manifestation more commonly associated with psoriatic disease. These studies are based on observation of its fundamental lesions, on microscopic similarity between the two conditions and on observation of the presence of a common genetic marker, the human leukocyte antigen (HLA) HLA-Cw6. 16 - 19 The difficulty in accepting the diagnosis of geographic tongue as oral psoriasis resides in the fact that some nonpsoriatic patients present geographic tongue. 20 Some authors believe that the prevalence of oral lesions would be much higher if the psoriatic patients underwent thorough oral examination. 16 Also, there are few controlled studies with histological and genetic tests on geographic tongue and its relation to psoriasis. 17 , 20
To solve the controversy, the aim of this study was to review the literature, describing the relation between psoriasis and geographic tongue.
COLLECTION METHOD
This study consists of a literature review, conducted between 1980 and 2014, in which was performed a consultation of thesis, dissertations and scientific articles, selected through search in the Scielo and Bireme databases, from Medline and Lilacs sources. The search in the databases was conducted using the keywords geographic tongue, benign migratory glossitis, oral psoriasis and psoriasis . We selected 63 studies in English or Portuguese that addressed the content of interest for the construction of each topic of this article.
Geographic tongue association to other diseases and etiologic factors
Several associations have been described between geographic tongue and diabetes mellitus, Reiter's syndrome, Down syndrome, pregnancy, psychological factors, family history and consumption of some medications, such as oral contraceptive pills and lithium carbonate. 1 , 3 However, the disease to which it presents a higher association is psoriasis. 21
Allergy has also been suggested as an etiologic factor in geographic tongue. 1 , 6 A relation between geographic tongue and asthma, eczema, hay fever, elevated immunoglobulin E (IgE) serum level and atopic patients was reported. It is a common lesion in patients that present recurrent acute inflammatory conditions. Psychosomatic factors, which probably contribute to both geographic tongue and atopy, may explain the high prevalence in atopic patients. 6
Some studies have shown a relation between geographic tongue and fissured tongue (FT), which manifests itself as grooves on the back of the tongue. 3 , 6 , 22 It has an incidence between 5% and 10% of the world population, manifesting variably in number and depth of the bumps. 23 Usually, the lesions are irreversible, the prevalence increases with age and it probably results from a long term glossitis. 3 , 24 Familial occurrence of fissured and geographic tongue in parents and siblings of patients with one or both of these conditions has been studied, suggesting that these lesions have hereditary features of polygenic transmission. 22
Some bacterial and fungal infections were related to geographic tongue due to the nature of the inflammatory lesion. However, no particular micro-organism was consistently found in association with the disease. 1
Generalized glossitis with papillary atrophy related to dietary deficiencies of iron and B vitamins led to the suspicion of a possible association between geographic tongue and nutritional deficiencies. There is the possibility of this type of glossitis, related to nutritional deficiencies, to be sometimes confused with geographic tongue, especially when the apex and the side edges of the tongue are affected. 25
Psychosomatic factors are mentioned as possible etiological factors due to the clinical observation that outbreak or exacerbation of lesions are usually accompanied by a stressful event, as occurs in psoriasis. 26
Gonzaga et al conducted a study with 129 patients with psoriasis, 399 patients with geographic tongue and 5,472 healthy individuals, evaluating the association of these conditions to alcohol, tobacco and stress. The authors found a high prevalence of alcohol consumption in psoriatic patients and a strong relation between psoriasis and GT with psychosomatic factors. Furthermore, the three related factors were four times more frequently in psoriatic patients. They concluded that interactions between environmental factors and psoriasis are different from the interactions that occur with GT and suggested that these differences may be responsible for different types of manifestations, considering they as the same disease. 27
Regarding tobacco use, some studies report that GT is less common in smokers, due to changes that occur in their oral epithelium, such as increased keratinization and decreased TNF-α, IL-1 and IL-6 production by macrophages (activation of nicotinic receptors in these cells). However, in psoriasis it is observed that tobacco use is greater than in individuals without this condition. 4 , 11 , 27
PREVALENCE OF GEOGRAPHIC TONGUE IN PSORIASIS AND PSORIATIC ARTHRITIS
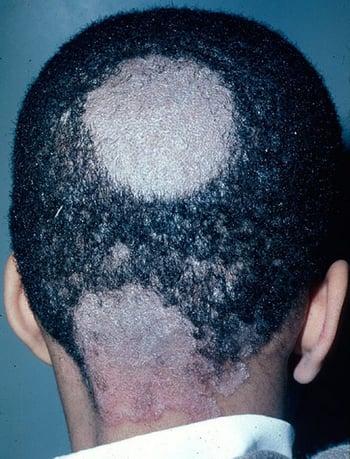
Oral manifestations of psoriatic disease can be divided into two types: the first involves change in mucosa histologically similar to psoriasis, parallel to skin lesions. The other type is more common and is constituted by nonspecific lesions, such as fissured tongue and geographic tongue ( Figure 1 ). 28

A and B - Clinical association of fissured tongue (black arrow) and geographic tongue (blue arrow) in psoriatic patient
Geographic tongue is the most common oral lesions in psoriasis, with or without arthritis, presenting high prevalence in these patients, as well relation to the severity of the disease, leading some authors to consider the combination of these conditions. 18 , 21 , 28
Approximately 10% of patients with psoriasis present geographic tongue. 17 Generalized pustular psoriasis is most commonly related to geographic tongue. 29 The presence of geographic tongue in a normal patient indicates an increased likelihood of developing generalized pustular psoriasis. 29
Fissured tongue is the oral condition most often associated with geographic tongue and is also increased in psoriasis. In skin psoriasis, most lesions are transient, but some lesions may exhibit a more permanent course. Likewise, geographic tongue could be a more transient expression. Moreover, fissured tongue would be a late and permanent expression of oral psoriasis. However, no genetic marker common to the three conditions was determined so far. 22
Studies show prevalence of fissured tongue ranging from 9.8% to 47.5% and of geographic tongue between 5.6% and 18.1% ( Table 1 ). 17 , 21 , 29 - 33
Geographic tongue and fissured tongue prevalence in psoriatic patients and control subjects
N - It does not present control and analysis of the presence of geographic tongue or fissured tongue
Daneshpazhooh et al evaluated 200 patients with psoriasis and 200 patients without psoriasis. They found fissured tongue in 33% and geographic tongue in 14% of patients with psoriasis; in the control group, they found fissured tongue in 9.5% and geographic tongue in 6% of patients. 29 The authors reported that 32% of patients with psoriasis and GT had severe psoriasis, relating this lesion to disease severity.
Zargari conducted a prospective study on the prevalence of tongue lesions in psoriatic patients. All patients with psoriasis being assisted in a dermatology clinic for five years were evaluated. The author observed that there were 306 psoriatic patients, and 47 (15%) presented tongue lesions, 25 (8%) fissured tongue, 17 (6%) geographic tongue and 5 (2%) the two lesions concomitantly. Geographic tongue was observed in 7% of patients with early psoriasis and in 1% of patients with late psoriasis. The author concluded that the incidence of geographic tongue in early psoriasis may be an indicator of disease severity. 30
Hernandes-Pérez et al examined 80 psoriatic patients and 127 healthy individuals, finding fissured tongue in 47% of patients with psoriasis and in 20% of controls. Geographic tongue was present in 12% and 5% of patients in psoriasis and control groups, respectively. The authors concluded that these lesions can be a predecessor or a marker of psoriasis severity. 21
Costa et al evaluated the oral mucosa of 166 psoriatic patients and 166 healthy subjects demonstrating a significant association between fissured tongue and geographic tongue when psoriatic patients were compared with the control group. The authors concluded that GT and FT are the only oral lesions associated with psoriasis, but are not exclusive of this disease. 31
Tomb et al showed an association between GT/FT and psoriasis, highlighting the increase of these lesions in pustular psoriasis. 32
Picciani et al showed a high level of GT and FT in patients with psoriatic disease, highlighting the higher prevalence of GT in early psoriasis and of FT in late psoriasis. 17
Singh et al evaluated 600 psoriatic patients and concluded that the geographic tongue is increased in psoriasis and related to disease severity. 33 The authors also showed that 79% of psoriatic patients with GT were male. This data differs from patients with GT without psoriasis who are usually female, and hormonal factors are identified as triggers or intensifiers of the lesion. 5
Picciani evaluated in 284 psoriatic patients the relation between severity and presence of geographic tongue through PASI, demonstrating that severe psoriasis occurred in 25% of patients without GT and in 58% of patients with GT. The author concluded that GT may be considered a marker of severity of psoriasis. 34
Some authors reported a significant increase of GT in patients with early psoriasis, which reinforces the Picciani theory that GT is directly related to the severity of the skin disease. 17 , 30 , 34
Facial involvement associated to the presence of geographic tongue and psoriatic arthritis is found in cases of severe psoriasis, being directly related to disease severity.35 Keshavarz et al demonstrated in a study with 138 psoriatic patients that 55% of cases presented facial involvement, 13% articular involvement, and 24% GT. The authors concluded that there is a significant relation between facial lesion and increased severity. 35 In addition to geographic tongue, the involvement of the temporomandibular joint (TMJ) may occur in patients with psoriatic arthritis (PA), particularly in patients with HLA-B27, but this is still a little reported fact, with only 19 articles and 43 cases found in the literature review. 28 , 36 The involvement of this joint can cause pain, swelling and limitation of movement. This involvement is more prevalent in the 4th decade of life and occurs between 31% and 63% of cases of PA. 28 , 36 Approximately 30% of patients examined in Picciani study presented some joint involvement without affecting the TMJ. 34 A multidisciplinary approach, involving dermatologists, rheumatologists and dentists, is the safest option for the diagnosis and treatment of these patients. The low prevalence of TMJ involvement in PA may be related to the lack of a thorough examination of the TMJ in psoriatic patients, which consequently causes few clinical and epidemiological reports in the literature. 36
Gonzaga & Consolaro conducted a study with 118 patients with psoriasis and 88 patients with geographic tongue, and observed a reversal in the age groups of patients, in which geographic tongue occurred at earlier ages, suggesting that this is a predecessor manifestation of the skin condition. In this study, the similarity between psoriasis and geographic tongue from the fundamental lesions and symptoms was also identified. 37 In geographic tongue, the erythematous and depapillated lesions correspond to skin peeling; and, just as in psoriasis, they follow a chronic course presenting periods of remission and exacerbation, which can occur in days, weeks or months. 16 , 37 The process of chewing and speaking is a factor of constant trauma to the tongue, which could correspond to Koebner phenomenon, stimulating the emergence of geographic tongue. 37 Most patients presenting symptoms report burning sensation in skin lesions and in geographic tongue. 37 The authors conclude that the prevalence of specific oral lesions of psoriasis would be much higher than the one reported due to the fact that, as a rule, patients are not subjected to a full and thorough oral examination, which would bring reliable results to help resolve this divergence. 37
HISTOPATHOLOGIC AND IMMUNOGENETIC SIMILARITIES BETWEEN GEOGRAPHIC TONGUE AND PSORIASIS
Geographic tongue may present histopathology and immunogenetic patterns similar to psoriasis, leading some authors to consider the association between these diseases ( Figure 2 ). 8 , 18 , 19 , 32

Major clinical, histopathological and immunogenetic features found in geographic tongue, showing similarity between GT and psoriasis. Highlighted image of the interaction found in geographic tongue among the CD8 T-lymphocytes, HLA-Cw6 and -B58 and keratinocytes
Histopathologic similarities
Microscopic findings of psoriasis are very characteristic: regular increase of the spinous layer with thickening of the lower portions; thickening and swelling of papillae; suprapapillary hypotrophy with occasional presence of a small spongiform pustule; absence of granular layer; parakeratosis; presence of Munro's microabscess; and inflammatory cell infiltration, particularly T-lymphocytes, macrophages and neutrophils, in the dermis and submucosa. These microscopic findings are also seen in the geographic tongue, highlighting the histopathological similarity between the two diseases ( Figure 3 ). 38 - 42 However, in geographic tongue and psoriasis, histopathologic characteristics may vary according to the clinical stage of the lesion and the biopsied area. 18

Main histopathological aspects of geographic tongue
Femiano compared two groups, each consisting of 20 patients. One group was composed of patients with skin psoriasis and lesions in the oral mucosa similar to geographic tongue. The other group consisted of individuals affected only by geographic tongue. Biopsies were performed in the oral lesions. In the first group, all analyzes were histologically compatible with psoriasis. In the second, these characteristics were observed in 80% of subjects. Thus, the author considered the geographic tongue as an oral manifestation of psoriasis, but he questioned the possibility of a type of geographic tongue not associated with psoriasis. 18
In geographic tongue, the white area of lesion presents subepithelial infiltrates with predominance of neutrophils, and abundant exocytosis of these cells, forming microabscesses and, in some cases, pustules. The erythematous area of the lesion shows mononuclear subepithelial infiltrate, suprapapillary hypertrophy and vascular ectasia.5 In a study via electron microscopy, it was observed that the erythematous area presents loss of filiform papillae and the white region shows necrotic cells that are flaking. 5
Picciani evaluated and compared the histopathologic features of GT lesions in patients with and without psoriasis, also comparing skin lesions among these patients. It was demonstrated that most of the classical histopathologic features of psoriasis was observed in all cases, such as parakeratosis, acanthosis, suprapapillary epithelial atrophy, spongiosis, hyperplasia of basal layer, ridges fusion, exocytosis, and presence of superficial and papillary inflammatory infiltrate. However, in the peripheral area of GT lesions, remarkable differences between the groups were found, in which oral lesions of psoriatic patients demonstrated hyperplastic, inflammatory and vascular changes from the periphery. The study of these aspects in the periphery of the lesion, perhaps, could help to distinguish between geographic tongue and true oral psoriasis. 34
Munro's microabscess (collections of neutrophils in the corneal layer) is present in over 75% of cases of psoriasis. Pustule of Kogoj, which is also a collection of neutrophils, but in the spinous layer, is more present in cases of pustular psoriasis. 38 Neutrophils are recruited by interleukin, 8 which is synthesized by CD4+ T-cells; then migrate through the epidermis, forming the collections of neutrophils. 43 Picciani found a high prevalence of pustule of Kogoj in GT lesions, reinforcing the theory that geographic tongue represents a pustular manifestation of psoriasis. 29 , 34 Evaluate oral and cutaneous lesions of patients with pustular psoriatic patients could help better understand this relation.
Many authors believe that, to establish the diagnosis of oral psoriasis, is necessary the presence of skin lesions with parallel course to oral lesions. 20 , 28 Histopathological findings associated with the parallel improvement of skin lesions of psoriasis and tongue lesions with systemic retinoid treatment support the hypothesis that the geographic tongue is a form of psoriasis. 40
To investigate the relation of these conditions, it is necessary the conduction of incisional biopsy of geographic tongue, covering the three areas of the lesion: the margin, the white line and the erythematous region. However, despite the geographic tongue is no longer considered a development change, the diagnosis is mainly based on clinical examination, with only two histopathology studies found, which impacts negatively the understanding of the pathogenesis of GT and its relation with psoriasis.
Immunogenetic similarities
In psoriasis, the inflammatory infiltrate is predominantly mononuclear, consisting mainly of T-cells, CD4 + in the dermis and CD8 + in the epidermis. T-lymphocytes play a major role in epidermal and vascular changes of psoriasis, being responsible for the production of several cytokines and chemokines. Macrophages and Langerhans cells and are main cells presenting antigens involved in psoriasis. Activated macrophages release cytokines and stimulate keratinocytes to produce cytokines such as TNF-α. 41 Langerhans cells constitute about 25% of the inflammatory cells of psoriasis, being more abundant in the dermis. The infiltrate in psoriatic oral lesions also consists of macrophages and T-cells, especially CD4, and the few immunohistochemical studies on geographic tongue show a similar abundance of CD4+. 8 , 16 , 34 , 42
An immunohistochemical study conducted in nonpsoriatic patients with geographic tongue, with reports of family history of psoriasis, showed similar cellular distribution between these conditions. Dilated and tortuous capillaries found in the dermis layer are marked with anti-CD31 antibody with the same intensity of psoriatic lesions. The nuclear proliferation, evidenced as a Ki-67 marker, abundant in psoriasis, is seen similarly in the geographic tongue, in which an increase in the proliferation of basal and parabasal cells is observed. The diagnosis of oral psoriasis was not established due to the lack of cutaneous manifestations. 8
There are few studies evaluating the inflammatory response in geographic tongue. Espelid et al performed an immunohistochemical study in GT lesions and CD3, CD4, CD8, CD22, CD11c and HLA-DR antibodies, showing that subepithelial inflammatory infiltrate is predominantly mononuclear, with CD4+ T-lymphocytes, followed by the presence of macrophages. 42 Ulmansky et al also showed that the subepithelial inflammatory infiltrate of GT has abundant presence of CD4+ T-lymphocytes. 16 These studies concluded that there is a connection between GT and psoriasis. 16 , 42 Picciani (2014) conducted an investigation of the inflammatory response in patients with geographic tongue, with and without psoriasis, using CD1a, CD3, CD4, CD8, CD20 and CD68 antibodies. The study showed that oral and cutaneous lesions present similar pattern of qualitative and quantitative marking, regardless of the antibody used. Oral and skin lesions of psoriatic patients revealed a higher prevalence of TCD3, TCD4 and TCD8 cells ( Figure 4 ). 34 Cabrijan et al compared the expression of CD4+ and CD8+ T-lymphocytes in 50 cases of psoriasis vulgaris and 50 cases of normal skin, and found a significant increase of these lymphocytes in psoriasis. 43 Vissers et al compared the expression of CD4+ and CD8+ T-lymphocytes in the center, within and on the edge of psoriatic plaques, and found an increased number of CD4+ T-cells in the dermis of all areas of the lesion. 44 In the epidermis, they observed a higher expression of CD8+ T-cells in the center and the inner edge of the lesion. Thus, they concluded that CD8 cells are important in the initial phase of psoriasis. 44 In Picciani study, the analysis by area of oral lesions showed that in the peripheral area there is an increase of T-cells, particularly CD4+, in geographic tongue of nonpsoriatic patients, and of CD8+ in geographic tongue of psoriatic patients. This reinforces the importance of using the assessment of lesions margins of geographic tongue to define the true oral psoriasis. 34 Facing psoriasis-like lesions, such as geographic tongue, which cause difficulties in diagnosis, distinguishing the two lesions based on T-cells infiltrate immunophenotyping can be a useful tool. The difference in the quantity and distribution pattern of CD4+ and CD8+ T-cells may assist in diagnostic decision, especially in cases presenting very similar histopathologic features. 45

Immunohistochemical marking aspects of the CD3, CD4 and CD8 cells in patients with geographic tongue with and without psoriatic disease
Despite the unknown etiology, some authors suggest that there is a genetic basis between psoriasis and geographic tongue. One of the most well-known genetic factors of susceptibility for psoriasis is the human leukocyte antigen (HLA), located on the short arm of chromosome 6. 46 The HLA system is divided into three regions: class I, class II and class III, according to the structure and function of its genes. 47 In the literature, there are few studies on genetic analysis in geographic tongue, and only four studies on this association were found, demonstrating relation with the HLA-B13, -B15, -CW6, DR5 and DRW6 antigens. 19 , 48 - 50
In 1987, a study was conducted to evaluate the association between GT and diabetes mellitus, in which the presence of an HLA allele between these conditions was demonstrated. In HLA typing, an increase in the HLA B-15 frequency, now subdivided into HLA-Bw62 and HLA-Bw63, was found in the diabetes group with GT and in patients only with diabetes, suggesting a weak association between endocrine dysfunction and oral lesion. 48
Subsequently, in 1993, a serologic study was conducted with 50 participants with GT and 380 healthy individuals, in which HLA relation with this lesion pathogenesis was examined. It was observed an increase in HLA-B51 antigen expression in control subjects and increased prevalence of HLA-DR5 and -DR6 in the GT group. 50
Gonzaga et al found a strong association among HLA-Cw*06, psoriasis and geographic tongue, concluding that some cases of geographic tongue may represent an authentic manifestation of psoriasis. 19 HLA-Cw*06 is the main allele of susceptibility to psoriasis, with or without arthritis, regardless of ethnic group. 51 The explanation for this association is a recognition of antigen specific by CD8+ T-cells resulting in stimulation of keratinocytes proliferation. These cells, in response to the binding of antigens with HLA-C*06: 02 and keratinocytes, act as the main effector cells in the maintenance of pathogenic process. 52 , 53
Gonzaga et al demonstrated a positive association between the HLA-B17 antigen and geographic tongue, and this finding was reinforced by Picciani, which showed for the first time the association between geographic tongue and HLA-B*58 allele, confirming the association between HLA-B*57 allele and psoriasis. 19 , 54 The serologic equivalent for these alleles (HLA-B*57 e -B*58) is the HLA-B17 antigen. Possibly this may explain the association between psoriasis and geographic tongue, respectively, with these alleles. 54
Some studies report that the combination of killer-cell immunoglobulin-like receptor (KIR), which act as ligands of class I HLA molecules and HLA-C alleles, increases the susceptibility to psoriasis. 14 , 55 , 56
Luszczek et al showed in a Polish population the frequency of HLA-C, KIR2DS1 and KIR2DL1. HLA-C*06 was found in 77% of psoriatic patients and in 17% of healthy individuals. KIR2DS1 activation gene was significantly higher in the patients, while the KIR2DL1 inhibitory gene was present in most people of both groups. The authors concluded that individuals who have HLA-C*06 and KIR2DS1 activation gene are more susceptible to psoriasis. 57 Because HLA molecules regulate the cytotoxic activity of killer-cells, the analysis of KIR genes could contribute to a better understanding of the correlation between geographic tongue and psoriasis.
HLA typing, associated with histopathologic and immunohistochemical analyzes, contributes to the definition of oral psoriasis, and it is essential to make this diagnosis for proper management and treatment of this condition.
Some studies have identified the major class I and II HLA alleles in samples from patients with psoriasis and geographic tongue ( Table 2 ). 19 , 48 , 49 , 58 - 62
Class I and II HLA often associated with psoriasis vulgaris (PV) and geographic tongue (GT) in population studies (p <0.05)
C – Control group;
A Brazilian study showed that the presence of the polymorphism +3954 IL-1B is associated with increased risk of geographic tongue development, and it was reported the central role of this interleukin in the pathogenesis of psoriasis. 63
Alikhani et al analyzed in saliva the TNF-α and IL-6 concentration in patients with geographic tongue and in healthy subjects and demonstrated a significant increase in both groups of patients, reinforcing the association with psoriasis. 26
The presence of familial cases and association with HLA genes in both conditions show that there may be common genetic determinants, manifesting only in oral mucosa or presenting a more generalized clinical condition, affecting the skin, while being influenced by certain environmental factors. 19 , 27 , 37
The diagnosis of geographic tongue is usually based on history and physical examination, except for atypical cases where histopathological examination is necessary. 5 The lesions are characterized by migratory pattern, circinate aspect and mild pain. 8
The differential diagnosis includes candidiasis, lichen planus, erythroplasia, lupus erythematosus, trauma and drug reactions. All of these lesions can be discarded after the clinical and histopathological examination. 5
Due to its variants, diagnosis of psoriasis becomes more complex when compared with geographic tongue, being necessary in some cases a clinicopathological correlation. 11
Because it is a benign and generally asymptomatic lesion, geographic tongue patient does not receive treatment. 5
Symptomatic treatment is based on the use of oral rinses containing anesthetics, topical corticosteroids, vitamin A, antihistamines and zinc supplements. It is recommended also to avoid contact with irritants and infectious factors, such as dentures and braces, which may exacerbate the situation. The patient should be instructed in relation to diet, avoiding acidic and spicy foods. In addition, patients should be instructed to always maintain good oral hygiene. 26 Abe et al reported a serious and persistent case of geographic tongue that was treated with systemic use of oral cyclosporine, presenting excellent therapeutical response. 40 Ishibashi et al showed two symptomatic cases of geographic tongue that used topical tacrolimus with regression of lesions, indicating this medication as a treatment option. 1
The treatment of psoriasis and psoriatic arthritis requires greater complexity and interaction between different health professionals, depending on the clinical form and severity of the disease. Treatment with photochemotherapy, immunomodulators, immunosuppressants and immunobiologicals alone or in associations is effective for skin, joint and oral disease. 10
FINAL CONSIDERATIONS
Geographic tongue is one of the most frequent oral manifestations of psoriatic disease, presenting histopathological, immunohistochemical and genetic similarities with plaque psoriasis. For the correct diagnosis of oral psoriasis, the histopathologic and immunogenetics analysis may be necessary. The extraoral and intraoral thorough examination in psoriatic patients and skin and joint examination in patients with geographic tongue should not be neglected so there is no loss of holistic assessment of the disease.
Questions.
- Benign migratory erythema
- Atrophic glossitis
- Benign migratory glossitis
- Cerebriform tongue
- All of the above
- Geographic tongue
- Scrotal tongue
- B and C are correct
- Glossitis due to nutritional deficiency
- Fissured tongue
- Oral candidiasis
- Bacterial infections
- Palmoplantar
- Erythrodermic
- Band-like lymphocytic infiltrate
- Munro’s microabscess
- Suprapapillary atrophy
- Parakeratosis
- T-lymphocytes
- Langerhans cell
- Neutrophils
- 0.6% to 4.8%
- 9.8% to 18.1%
- Basal layer of the epithelium
- Epithelial layer of the cornea
- Constituting the connective lymphocytic infiltrate
- Close to areas of vascular ectasia
- HLA-Bw62 and HLA-Bw63
- HLA-B*57 and -B*58
- Systemic corticosteroids
- In the absence of symptoms, drug prescription is not indicated
- Intralesional injection of immunosuppressive agents
- Mouthwash with antiseptic solution
- Late and mild psoriasis
- Late and severe psoriasis
- Early and moderate psoriasis
- Early and severe psoriasis
- ( ) In the white area of geographic tongue, it is possible to find atrophy of filiform papillae, which is confirmed by electron microscopy.
- ( ) The erythematous area presents subepithelial mononuclear cell infiltration, suprapapillary hypertrophy and vascular ectasia.
- ( ) The GT lesions in psoriasis and psoriatic patients show no microscopic differences in the white, peripheral and erythematous areas.
- ( ) The geographic tongue is still considered by some authors as a development change and, therefore, histopathology is not performed generally for diagnostic confirmation.
- They found higher CD8+ levels on the margins of oral lesions of non-psoriatic patients.
- CD4+ lymphocytes are relevant in the initial phase of oral lesions.
- The central area of GT showed great increase in CD8+ levels.
- The study showed increased CD8+ lymphocytes in the peripheral area of lesions in psoriatic patients.
- KIR2DL1 inhibitory gene has a high prevalence in psoriatic patients that present HLA-C*04.
- KIR2DL1 inhibitory gene may represent a protective factor in psoriatic patients in the regulation of immune response.
- KIR2DS1 activation gene has a high prevalence in psoriatic patients who have the HLA-C*06 allele.
- KIR2DL1 activation gene was present in most individuals belonging to psoriasis and control groups.
- The assessed patients presented were older.
- Brazilian population has high miscegenation and HLA-C*06 is more frequently found in Caucasian populations.
- Few patients were analyzed.
- All of the above are correct.
* Study performed at dermatology clinic of Hospital Universitário Pedro Ernesto - Universidade do Estado do Rio de Janeiro (HUPE-UERJ). Post-graduate program in pathology - Universidade Federal Fluminense (UFF) and Histocompatibility and cryopreservation laboratory - Universidade do Estado do Rio de Janeiro (HLA-UERJ) - Rio de Janeiro (RJ), Brazil.
Financial support: none.
Conflict of interest: none.
- Patient Care & Health Information
- Diseases & Conditions
- Geographic tongue

Geographic tongue results from the loss of tiny hairlike structures on your tongue's surface. These structures are called papillae. The loss of these papillae appears as smooth, red patches of different shapes and sizes.
Geographic tongue is an inflammatory but harmless condition affecting the surface of the tongue. The tongue usually is covered with tiny, pinkish-white bumps called papillae. These papillae are actually fine, hairlike structures. With geographic tongue, patches on the surface of the tongue are missing papillae. These patches are smooth and red, often with slightly raised borders.
This condition is called geographic tongue because the patches make your tongue look like a map. The patches often appear in one area and then move to a different part of the tongue.
Although geographic tongue may look alarming, it does not cause health issues. It's not related to infection or cancer. Geographic tongue sometimes can cause tongue pain and make you more sensitive to certain foods, such as spices, salt and even sweets.
Products & Services
- A Book: Mayo Clinic Family Health Book
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms of geographic tongue may include:
- Smooth, red, irregularly shaped patches on the top or side of your tongue. These patches may look like sores.
- Frequent changes in the location, size and shape of the patches.
- Pain or burning feeling in some cases, most often related to eating spicy or acidic foods.
Many people with geographic tongue have no symptoms.
Geographic tongue can continue for days, months or years. The problem often goes away on its own, but it may appear again later.
When to see a doctor
Because most people with geographic tongue don't show symptoms, they won't need treatment. If you have symptoms, they may be related to a fungal infection, so see your doctor or dentist. In some cases, medicine may be prescribed to help ease symptoms.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
The cause of geographic tongue is not known, and there's no way to prevent it. There may be a link between geographic tongue and other conditions, such as psoriasis. This is a skin disease that causes a rash with itchy, scaly patches. But more research is needed to learn about possible connections to other health conditions.
Risk factors
Factors that may increase your risk of geographic tongue include:
- Family history. Some people with geographic tongue have a family history of it. So genetic factors may raise the risk.
- Fissured tongue. People with geographic tongue often have a condition called fissured tongue. This is when deep grooves, called fissures, appear on the surface of the tongue.
Complications
Geographic tongue is harmless, but it can sometimes be uncomfortable. It does not pose a threat to your health, cause long-term complications or raise your risk of major health problems.
This condition can cause anxiety. That's because the appearance of the tongue may be embarrassing, depending on how well the patches can be seen. It also may be hard to believe that nothing is seriously wrong.
- Valdez EE, et al. Geographic tongue. In: The Color Atlas and Synopsis of Family Medicine, 3rd ed. New York: McGraw-Hill Education; 2019. https://accessmedicine.mhmedical.com. Accessed April 20, 2022.
- Geographic tongue. StatPearls. https://www.ncbi.nlm.nih.gov/books/. Accessed April 20, 2023.
- AskMayoExpert. Geographic tongue. Mayo Clinic; 2022.
- Lodi G, et al. Oral lesions. https://www.uptodate.com/contents/search. Accessed April 20, 2023.
- Geographic tongue. The American Academy of Oral Medicine. https://www.aaom.com/. Accessed April 20, 2023.
- Prasanth VJ, et al. Geographic tongue. CMAJ. 2021; doi:10.1503/cmaj.202855.
- Zhou MX (expert opinion). Mayo Clinic. May 15, 2023.
- Goldstein BG, et al. Topical corticosteroids: Use and adverse effects. https://www.uptodate.com/search. Accessed April 26, 2023.
- Corren J, et al. Allergic and nonallergic rhinitis. In: Middleton's Allergy: Principles and Practice, 9th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed April 26, 2023.
- Siegel MA, et al, eds. Geographic tongue (benign migratory glossitis, erythema migrans). In: Clinician's Guide to Treatment of Common Oral Conditions, 8th edition. American Academy of Oral Medicine; 2018.
- Symptoms & causes
- Diagnosis & treatment
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be part of the cutting-edge research and care that's changing medicine.
- New Hampshire
- North Carolina
- Pennsylvania
- West Virginia
- Online hoaxes
- Coronavirus
- Health Care
- Immigration
- Environment
- Foreign Policy
- Kamala Harris
- Donald Trump
- Mitch McConnell
- Hakeem Jeffries
- Ron DeSantis
- Tucker Carlson
- Sean Hannity
- Rachel Maddow
- PolitiFact Videos
- 2024 Elections
- Mostly True
- Mostly False
- Pants on Fire
- Biden Promise Tracker
- Trump-O-Meter
- Latest Promises
- Our Process
- Who pays for PolitiFact?
- Advertise with Us
- Suggest a Fact-check
- Corrections and Updates
- Newsletters
Stand up for the facts!
Our only agenda is to publish the truth so you can be an informed participant in democracy. We need your help.
I would like to contribute
‘cheap fake’ videos, and the phrase itself, take 2024 election’s center stage.
Republican presidential candidate, former President Donald Trump, left, speaks at a campaign rally in Las Vegas, June 9, 2024, and President Joe Biden speaks at the White House in Washington, D.C., June 4, 2024. (AP)

If Your Time is short
“Cheap fake” videos of President Joe Biden that have been selectively edited or taken out of context to undermine his mental and physical fitness have inundated social media and are the subject of political spin.
The term “cheap fake” isn’t new. Misinformation researchers coined it in 2019 to describe videos that have been taken out of context or manually edited, such as through cropping or clipping, with low-cost, easy-to-access tools.
President Joe Biden sitting in an "invisible" chair in France. Biden wandering off from an event in Italy. Biden freezing on stage at a Los Angeles fundraiser. These misleading claims and others, based on videos that are deceptively edited or taken out of context, have flooded voters’ social media platforms in the last two weeks.
These videos, called cheap fakes, have become a common tactic to undermine Biden’s fitness for office as the 81-year-old seeks reelection. Former President Donald Trump, the presumptive Republican nominee, is 78.
Although the Biden campaign has pushed back on these videos, Trump and his allies have played up the viral clips. Trump’s campaign attempted to redefine cheap fakes as "any unedited video of Joe Biden’s cognitive decline that the Biden administration does not want the public to see."
Trump and his campaign "have a tendency to repurpose and twist words to suit their purposes," said Samuel Woolley, an assistant professor at the University of Texas at Austin’s School of Journalism and Media. Woolley pointed to the example of Trump redefining "fake news" as any news that disagrees with him, rather than false content.
Not every video of Biden having an awkward moment or making a gaffe is a cheap fake. But increasingly, footage of the president has been manipulated to push false and misleading claims.
Here’s how "cheap fakes" entered the 2024 election glossary, and how experts define the term, apart from the political spin.
Misinformation researchers first coined the term "cheap fake" in 2019, as "deepfake" videos made with artificial intelligence grew more popular. Cheap fakes are real videos that have been manually edited with low-cost, easy-to-access tools or taken out of context.
Some social media users falsely claimed White House Press Secretary Karine Jean-Pierre invented the term "cheap fake."
After showing footage of Jean-Pierre talking about the spree of edited Biden clips, the narrator in a June 18 Instagram video said, "Cheap fake videos? Did she just make that up? That’s not even a word or a thing. … They’re telling you guys that those videos are fake and manipulated when it is raw footage not tampered with at all."
Creators of cheap fakes use techniques such as slowing or speeding footage, cropping or zooming in on videos, and clipping parts of videos to omit the full context.
By contrast, "deepfake" videos are typically more sophisticated because they are created with AI technology. Deepfakes can be real videos manipulated by AI, or videos produced entirely by AI.
Darren Linvill, a Clemson University communication professor specializing in social media disinformation, said cheap fakes have several advantages over other tools of disinformation. Those include being easy to create and difficult for social media platforms to regulate because they often don’t violate the platforms’ rules, said Linvill, who also serves as co-director of Clemson’s Media Forensics Hub. Meta’s Third Party Fact-Checking program, for instance, does not apply to politicians.
"Third, and perhaps most importantly, cheap fakes can take easy advantage of human psychology. If I believe that either Trump or Biden are old and losing their faculties, seeing even a brief piece of video that supports that belief will quickly reinforce it and entrench it," Linvill said.
Numerous recent videos of Biden at public events and press conferences have been taken out of context or edited to misconstrue his words or actions. RNCResearch, an X account run by the Republican National Committee and Trump’s campaign, is often among the first to share these clips.
Video from Biden’s June 18 fundraiser in Los Angeles claimed to show the president freezing on stage and being escorted away by former President Barack Obama. The Associated Press fact-checked this claim, reporting that Biden paused for a few moments on stage amid applause.
A few days earlier, on June 13, a video claimed to show Biden wandering away from other world leaders during a skydiving demonstration at the G7 summit in Italy. We rated that claim False . A longer video of the event shows Biden turning to speak with other parachuters who could not be seen in the edited clip.
Earlier this month, after Biden’s June 6 speech at the 80th anniversary of the D-Day invasion in Normandy, France, social media users circulated edited video clips , claiming the president sat in an "imaginary chair," had a bowel movement and left the event prematurely. The event’s full video did not support these claims; neither did news reports of the event.
Other examples are plentiful. In April, Fox News host Sean Hannity falsely claimed Biden was ignored at a gas station . PolitiFact has fact-checked several other misleadingly edited videos of Biden through the years.
During a June 17 White House press briefing, Jean-Pierre said the recent videos were "done in bad faith."
Jean-Pierre mistakenly referred to the videos as "deepfakes" at one point. Trump also has mistakenly called them "clean fakes."
White House spokesperson Andrew Bates has also repeatedly called out these videos on X, sharing links to news outlets fact-checking the claims. Politico reported June 18 that the Biden campaign "has established a taskforce to mitigate the risks posed by AI and cheap fakes."
The Biden campaign also took a jab at Trump, highlighting the former president’s awkward moments and gaffes in a video posted June 20 on X. The post said, "Here is a montage of Donald Trump getting confused, lost, wandering off, and waving to nobody." Each video clip included the original audio, without any voiceovers or subtitles.
The Trump campaign pushed back on the 2-minute, 24-second video, calling it a cheap fake without citing specific evidence.
"When politicians and campaigns misuse particular terms, it further sows confusion and serves to politicize certain turns of phrase," Woolley said.
Our Sources
Email interview with Samuel Woolley, an assistant professor in the School of Journalism and Media and program director of the propaganda research team at the Center for Media Engagement at the University of Texas at Austin, June 20, 2024
Email interview with Darren Linvill, a communication professor specializing in social media disinformation and co-director of the Media Forensics Hub at Clemson University, June 20, 2024
Data & Society, " Deepfakes and Cheap Fakes ," Sept. 18, 2019
PolitiFact, " How to detect deepfake videos like a fact-checker ," April 19, 2023
PolitiFact, " ‘Cheap fakes’: Viral videos keep clipping Biden’s words out of context ," Feb. 14, 2022
PolitiFact, " Video at G7 shows Biden talking to skydivers, not wandering off ," June 14, 2024
PolitiFact, " Fact-checking viral claims about Joe Biden at D-Day anniversary event ," June 6, 2024
PolitiFact, " No, President Biden was not ignored by people at a Pittsburgh-area gas station ," April 26, 2024
PolitiFact, " No, this video doesn’t show Joe Biden leaving midinterview with MSNBC ," July 25, 2023
PolitiFact, " Biden was gesturing toward his audience, not shaking hands with "thin air" ," April 19, 2022
PolitiFact, " Video of Biden’s NATO summit speech misleadingly edited to supposedly show him waving at nobody ," July 14, 2023
PolitiFact, " The media's definition of fake news vs. Donald Trump's ," Oct. 18, 2017
The Associated Press, " FACT FOCUS: Biden's pause as he left a star-studded LA fundraiser becomes a target for opponents ," June 18, 2024
Politico West Wing Playbook newsletter, " A White House-Murdoch hot war ," June 18, 2024
The Washington Post, " How Republicans used ‘cheap fake’ videos to attack Biden over 24 hours ," June 11, 2024
The New York Times, " Trump Tries to Set Expectations, and Floats Excuses, for His Debate With Biden ," June 19, 2024
The Denver Gazette, " Trump campaign slams Biden attempt to make ‘cheap fakes’ in attack ad ," June 20, 2024
YouTube, White House press briefing , June 17, 2024
White House spokesperson Andrew Bates, X post , June 18, 2024
White House spokesperson Andrew Bates, X post , June 19, 2024
Biden HQ, X post , June 20, 2024
Donald Trump campaign newsletter , June 19, 2024
Team Trump, Instagram post , June 19, 2024
Instagram reel , June 18, 2024
Browse the Truth-O-Meter
More by sara swann.


IMAGES
COMMENTS
The meaning of WANDERING RASH is geographic tongue. Love words? You must — there are over 200,000 words in our free online dictionary, but you are looking for one that's only in the Merriam-Webster Unabridged Dictionary.. Start your free trial today and get unlimited access to America's largest dictionary, with:. More than 250,000 words that aren't in our free dictionary
Hives — also known as urticaria (ur-tih-KAR-e-uh) — is a skin reaction that causes itchy welts that range in size from small spots to large blotches. Hives can be triggered by many situations and substances, including certain foods and medications. Angioedema can arise with hives or alone. It causes swelling in the deeper layers of skin ...
wandering rash: (rash) [Fr. rasche , skin eruption] A general term for any eruption that appears on the skin transiently (as opposed to durable skin lesions such as scars, tattoos, or moles). Synonym: exanthem Patient care Assessments are made of the location and characteristics of the lesion: color; size (height and diameter); pattern, ...
Macules are flat, nonpalpable lesions usually < 10 mm in diameter. Macules represent a change in color and are not raised or depressed compared to the skin surface. A patch is a large macule. Examples include freckles, flat moles, tattoos, and port-wine stains, and the rashes of rickettsial infections, rubella, measles (can also have papules and plaques), and some allergic drug eruptions.
Definition and Types of Rashes. A rash is defined as an area of skin that becomes irritated, inflamed, or discolored. They can be classified based on their appearance, location, and underlying causes. ... For example, a rash caused by an allergic reaction may be accompanied by itching and swelling, while a rash caused by a bacterial infection ...
Hives: A Rash That Moves Around . Hives are an itchy, red rash that can be slightly raised off of the skin. It is caused when the immune system sees a threat and releases histamine from mast cells and basophils in the dermis of the skin. The released histamine causes dilation of the blood vessels and fluid to leak into the skin.
The symptoms that come along with a skin rash depend on the cause and type of rash. Some common symptoms include: Blistering. Redness. Scaly or dry skin. Similarity to hives. Blotchiness. Swelling ...
Define wandering rash. wandering rash synonyms, wandering rash pronunciation, wandering rash translation, English dictionary definition of wandering rash. adj. rash·er , rash·est Resulting from or acting with ill-considered haste or boldness.
Hives are raised red or skin-colored welts or rashes that typically flare up suddenly and have a habit of changing shape or moving from one area of the body to another. These welts can vary in size, and they are notorious for causing intense itching, often surrounded by a wheal. These wheals can sometimes merge, forming a map-like pattern or a ...
First described by Rayer in 1831, geographic tongue is a benign chronic relapsing recurring inflammatory condition of the oral cavity of unknown etiology.[1] It can also be referred to as benign migratory glossitis, erythema migrans, annulus migrans, and a wandering rash of the tongue.[1][2][3][4] It usually manifests as asymptomatic erythematous and migratory circinate patches that give its ...
In physical urticaria, the hives have a physical cause, such as exposure to heat, cold or pressure. Common triggers include: Rubbing or scratching. This is the most frequent cause of physical urticaria. Symptoms appear within a few minutes in the place that was rubbed or scratched and typically last less than an hour.
Definition This section has been translated automatically. Self-limiting, chronic exfoliative, superficial epithelial detachments migrating over the mucosa of the tongue and forming anular or polycyclic figures ("wandering rash; wandering plaques").
Wool, chemicals, soaps and other things can irritate the skin and cause rashes and itching. Sometimes a substance, such as poison ivy or cosmetics, causes an allergic reaction. Also, reactions to certain medicines, such as narcotics to treat pain (opioids) can cause itchy skin. Sometimes the cause of the itching can't be determined.
Common symptoms of atopic dermatitis are: Dry, cracked skin. Itchiness. Raw skin from scratching. Small, raised bumps, on brown or Black skin. Oozing and crusting. Thickened skin. Atopic dermatitis also is called eczema. It often occurs in the folds of the elbows, behind the knees and on the front of the neck.
Geographic tongue, also known by several other terms, is a condition of the mucous membrane of the tongue, usually on the dorsal surface. It is a common condition, affecting approximately 2-3% of the general population. It is characterized by areas of smooth, red depapillation (loss of lingual papillae) which migrate over time.The name comes from the map-like appearance of the tongue, with ...
[Fr. rasche, skin eruption] A general term for any eruption that appears on the skin transiently (as opposed to durable skin lesions such as scars, tattoos, or moles).
Geographic tongue is a chronic, inflammatory, and immune-mediated oral lesion of unknown etiology. It is characterized by serpiginous white areas around the atrophic mucosa, which alternation between activity, remission and reactivation at various locations gave the names benign migratory glossitis and wandering rash of the tongue.
rash rash, nonspecific term for an eruption of the skin. It may result from skin allergy, skin irritation, or skin disease, or it may be a symptom of a systemic disease like measles, smallpox, or scarlet fever. A rash may appear as discolored spots or a general redness, or as blisters or pustules, either flat or raised above the surface of the skin. The ...
Symptoms. Symptoms of geographic tongue may include: Smooth, red, irregularly shaped patches on the top or side of your tongue. These patches may look like sores. Frequent changes in the location, size and shape of the patches. Pain or burning feeling in some cases, most often related to eating spicy or acidic foods.
Wandering rash (Geographic tongue, Benign migratory glossitis, erythema migrans, Annulus migrans) is an asymptomatic inflammatory disorder of tongue with controversial etiology. ... By definition Geographic tongue is a benign inflammatory condition which is characterized as
A 46-year-old man was evaluated in the rheumatology clinic because of joint pain and swelling. The examination was notable for rash, nasal crusting, and alopecia. A diagnosis was made.
A few days earlier, on June 13, a video claimed to show Biden wandering away from other world leaders during a skydiving demonstration at the G7 summit in Italy. We rated that claim False .