Recovery from Addiction
Reviewed by Psychology Today Staff
Recovery from addiction is not only possible, it is the rule, rather than the exception. According to the latest U. S. National Survey on Drug Use and Health, more than 75 percent of people addicted to alcohol or drugs recover—their condition improves and substance use no longer dominates their life. That is not to say that recovery is easy. It is often a long and bumpy path, and relapse is nearly inevitable—but that doesn’t spell the end of recovery. There are coping strategies to be learned and skills to outwit cravings, and practicing them not only tames the impulse to resume substance use but also gives people pride and a positive new identity that hastens recovery.
There is no one pathway to recovery. Only 1.0 percent of people receive substance abuse treatment as an inpatient or outpatient at a specialty facility. Some people seek medical treatment at a hospital. Others seek help from an outpatient mental health facility. Many choose to recover without using any clinical services. The single most popular path is the use of peer support groups in the community.

On This Page
- Recovery Timeline
- The Recovery Process
- Support Systems for Recovery
- Rebuilding Life
Recovery starts immediately with stopping use of a substance. For many of those who are addicted, enduring even that action is unimaginable. And yet, it is just the first step. What must follow is the process of behavior change, through which the brain gradually rewires and renews itself. That process can take months, or more. And there are many ways to accomplish that.
There are no lab tests that define recovery and no universally agreed-on definition of recovery. For many experts, the key components of addictive disorder are compulsive drug use that continues despite detrimental consequences, and the development of cravings with the inability to control use. Addiction develops over time, in response to repeated substance use, as the action of drugs changes the way the brain responds to rewards and disables the ability to control desire for the drug.
Under all circumstances, recovery takes time because it is a process in which brain cells gradually recover the capacity to respond to natural sources of reward and restore control over the impulse to use. Another widely applied benchmark of recovery is the cessation of negative effects on oneself or any aspect of life. Many definitions of recovery include not only the return to personal health but participation in the roles and responsibilities of society.
Subscribers to the disease model of addiction generally believe that recovery extends well beyond any benchmarks to be a lifelong process. Nevertheless, data show that five years after substance use is stopped, the risk for relapse is no greater than for anyone else in the general population .
The first step in the recovery process is stopping drug use. The endpoint is voluntary control over use and reintegration into the roles and responsibilities of society. Shortly after substance use is stopped, people may experience withdrawal, the onset of unpleasant physical and psychological symptoms —from irritability to shakiness to nausea; delirium and seizures in severe cases. The symptoms can last up to a week or more.
Recovery hinges on successfully changing many deeply rooted behaviors, and how long that takes—months or years—depends on many factors for each individual; most important are avoidance of people and places where drugs are used, having supportive connections with others, learning new strategies for coping, and the availability of opportunities for developing or reconnecting with other interests and sources of reward. Behavioral therapy can be helpful. Relapse is common and experts see it as an opportunity for learning about and overcoming impediments to change.
No matter which pathway of recovery a person chooses, a common process of change underlies them all. The well-researched science of behavior change establishes that addictive behavior change, like any behavior change, is a process that starts long before there’s any visible shift in activity. Studies define five stages of change in addiction recovery .
• Precontemplation: Substance users are unaware that their use is causing problems, although others around them are, and they have no intention of changing behavior.
• Contemplation: Substances users begin to realize that their use has some negative consequences and it might be time to make a change, but they have no commitment to action.
• Decision : Intention develops to take action about the substance use as concrete goals begin to take shape. A start date is set.
• Action : The decision is put into action, with new behaviors learned and practiced. Action may involve contacting a doctor, entering a treatment program, or finding a peer support group.
• Maintenance : New behavior replaces old behavior, and change gains momentum with the desire to make it permanent.
The answer depends on which model of addiction you subscribe to. Those who believe that addiction is a brain disease do not use the word “cure.” Nevertheless, clinical experience and research studies document that the majority of those addicted eventually regain control of their life and reverse the disruptive effects of drug use on the brain and behavior.
Brains are plastic—they adapt to experience—and people can change and grow, develop an array of strategies for coping with life’s challenges and stressors, find new means of satisfaction and reward, and negotiate life ahead. Millions of people do, whether they were once compulsive users of opiates, alcohol, or gambling. There is enduring resolution of what once was problem behavior. Successfully overcoming the compulsion to use drugs usually requires building strengths—learning to understand the feelings that trigger the desire, finding more adaptive, more rewarding ways to manage or resolve them when they arise, and developing interests that provide meaning in life.
But those who subscribe to the view of addiction as a disease focus on the eternal vulnerability of human nature no matter one’s changed circumstances. In this view, not only is addiction incurable, but work is constantly required to avoid a slip-up, which is always waiting in the wings.
Research and clinical experience have identified a number of factors that promote recovery. Because people's surroundings silently but strongly shape thinking and behaving, it is essential to arrange the environment one inhabits to support the shifting of habits of thought and behavior—avoiding high-risk situations, developing new sets of friends. Another is reorienting the brain circuitry of desire—finding or rediscovering a passion or pursuit that gives meaning to life and furnishes personal goals that are capable of supplanting the desire for drugs. A third is establishing and maintaining a strong sense of connection to others ; support helps people stay on track, and it helps retune the neural circuits of desire and goal-pursuit. Learning new coping skills for dealing with unpleasant feelings is another pillar of recovery.
Recovery always requires changing behavior, learning new coping skills, and finding new sources of interest. Many do it without seeking clinical treatment or using external services of any kind. Whatever the pathway of recovery, whether participation in mutual-help groups or use of clinical services of any kind, the instruments of recovery are always the same, as summed up in the acronym CHIME: Connecting with others, developing Hope and optimism, creating a new Identity, discovering a renewed sense of Meaning and purpose, and Empowerment, the sense of self-efficacy that comes from learning skills for mastering challenges.
Many people believe that they are powerless to change their own addictive behavior, and often it is a belief that keeps people addicted . The evidence shows that every day, people choose to recover from addiction on their own. One way or another, they learn and deploy a set of skills that help them get through the strong cravings and urges of the difficult early stages of recovery. Some of the most helpful strategies for dealing with cravings are summarized in the acronym DEADS.
• Delay. Cravings diminish and disappear in time unless attention is focused on them. Negotiating with oneself for a delay of use, which doesn’t deny the possibility of future use, and then getting busy with something else, capitalizes on the knowledge that cravings dissipate in about 15 minutes.
• Escape. Planning in advance a way out of high-risk situations—whether an event, a place, or a person—helps support intentions in the face of triggers to use.
• Avoid/accept. It’s helpful to understand that cravings are normal, and the discomfort will pass. Strategically avoiding potentially problematic situations altogether,
• Distract. Quickly interrupting thoughts of using is important. Saying a mantra, substituting thoughts of recovery goals, praying, reading something recovery-related, reaching out to someone supportive—all are useful tactics.
• Substitute. Turning to another activity—listening to music, going for a walk—when an urge hits can maintain recovery.
For some people, committing to complete abstinence is not desirable or is too daunting a prospect before beginning treatment. Many people desire only to moderate use and bring it under control. In fact, there is growing support for what is called harm reduction , which values any moves toward reducing the destructive consequences of substance abuse. Researchers find that taking incremental steps to change behavior often motivates people to eventually choose abstinence. Nevertheless, many treatment programs, including Alcoholics Anonymous, require a commitment to complete abstinence as a condition of admission. Experts hotly debate the need for abstinence.
Above all, change takes courage. It always exposes people to the possibility of failure. The prospect of change engages people in an inner dialogue about hope, disappointment, and accountability .
Researchers have studied the experiences of many people who have recovered from substance use and identified key features of the recovery process. One widely used model can be summed up in the acronym CHIME, identifying the key ingredients of recovery.
• Connection—being in touch with others who believe in and support recovery, and actively seeking help from others who have experienced similar difficulties. Intensive support is often needed for recovery from addiction .
• Hope and optimism—nurturing belief in oneself, belief in one’s ability to persevere even through setbacks, and developing a future orientation. Hope often builds along the way.
• Identity—shifting towards a new, positive view of oneself, one more aligned with one’s deeper values and goals, one built on self-confidence gained by acquiring new skills and new behaviors.
• Meaning and purpose—finding and developing a new sense of purpose, which can come from many sources. It may include rediscovering a work or social role, finding new recreational interests, or developing a new sense of spiritual connection. The important feature is that the interest avert boredom and provide rewards that outweigh the desire to return to substance use.
• Empowerment—finding the wherewithal to cope with recovery and the challenges of life, which breeds a sense of self-efficacy.
Cravings are the intense desire for alcohol or drugs given formidable force by neural circuitry honed over time into single-minded pursuit of the outsize neurochemical reward such substances deliver. Cravings vary in duration and intensity, and they are typically triggered by people, places, paraphernalia, and passing thoughts in some way related to previous drug use. But cravings don’t last forever, and they tend to lessen in intensity over time.
Studies show that craving has a distinct timetable—there is a rise and fall of craving . In the absence of triggers, or cues, cravings are on a pathway to extinction soon after quitting. But some triggers can’t be avoided, and, further, the human brain, with its magnificent powers of association and thinking, can generate its own. Studies show that craving for alcohol peaks at 60 days of abstinence. For methamphetamine, it peaks at three months.
People can learn to resist or outsmart the cravings until they become manageable. There are strategies of distraction and action people can learn to keep them from interrupting recovery. One is to shift thinking immediately as a craving arises. Another is to carefully plan days so that they are filled with healthy, absorbing activities that give little time for rumination to run wild. Exercise, listening to music, getting sufficient rest—all can have a role in taking the focus off cravings.
Guilt refers to feels of responsibility or remorse for actions that negatively affect others; shame relates to deeply painful feelings of self-unworthiness, reflecting the belief that one is inherently flawed in some way. Shame is an especially powerful negative feeling that can both invite addiction in the first place and result from it. Either way, it often keeps people trapped in addictive behaviors. It gets in the way of recovery, self-acceptance, and accessing help when needed.
It is possible to overcome shame —by driving right through it. Shame diminishes as recovery proceeds. Neuroscientist Adi Jaffe, Ph.D., who himself recovered from addiction, outlines five steps.
1. Identify key past events that gave rise to negative beliefs about yourself.
2. Identify personal strengths as well as weaknesses.
3. Identify other factors in your life—relationships, work—that can help take the focus off addictive behaviors.
4. Shift perspective to see relapse and other “failures” as opportunities to learn.
5. Choose to get help, even though shame often deters people from doing so.
Sustaining behavior change until new patterns become ingrained is difficult under the best of circumstances. In leaving addiction behind, most people have to restructure their everyday life, from what they think about and who they spend time with and where, to how they use their time, to developing and pursuing new goals. The shifts in thinking and behavior are critical because they lay the groundwork for changes in brain circuity that gradually help restore self-control and restore the capacity to respond to normal rewards.
Further, the behavior change requires constant decision-making often in the presence of deeply rooted desire for the drug escape, before most people have acquired belief in themselves and a complete set of coping skills to help them through the challenges. That makes self-trust one key to quitti ng, something that tends to be in short supply among those who have previously tried to quit and failed. There are many types of support to call on to help shore up resolve. Any and all are useful
Many find in 12-step programs—Alcoholics Anonymous (AA) and Narcotic Anonymous (NA) are among the best known—a caring, supportive community willing to pull each other through the temptations , the self-rebuke, and the hopelessness that especially mark the early stages of recovery. They also value having role models of recovery and someone to call on when the recovering self is an unsteady newborn. Whatever the stress relief that comes from being in a group, many others are not comfortable with the religiosity, the steady focus on the dangers of relapse rather than on growth, or the subscription to powerlessness of AA and NA. Data show that the programs are helpful for some but not for everyone. Addiction treatment is not one-size-fits-all .
Peer or mutual support is not restricted to AA or NA; it is available through other programs that similarly offer regular group meetings in which members share their experiences and recovery skills. SMART Recovery is a secular, science-based program that offers mutual support in communities worldwide as well as on the internet and has specific programming for families. All Recovery accommodates people with any kind of addiction and its meetings are led by trained peer-support facilitators. Women for Sobriety focuses on the needs of women with any type of substance use problem.
Addiction doesn’t just affect individuals; addiction is a family affliction . The uncertainty of a person’s behavior tests family bonds, creates considerable shame, and give rise to great amounts of anxiety. Because families are interactive systems, everyone is affected, usually in ways they are not even aware of. When a person goes into treatment, it isn’t just a case of fixing the problem person. The change destabilizes the adaptation the family has made—and while the person in recovery is learning to do things differently, so must the rest of the family learn to do things differently. Otherwise, their behavior is at risk of cementing the problem in place.
For starters, family members need to learn what the risk factors for addiction are and the internal and external struggles an individual faces in recovering from addiction, and they need to understand their own complex emotional reactions to the entire experience. Because recovery involves growth, families need to learn and practice new patterns of interaction.
Another one of the most important ways to support recovery is to understand that multiple relapses over a number of years are typically part of the process. They are not occasion for blame or despair but for encouraging resumption of recovery. Families can develop awareness of a loved one’s emotional, environmental, and social triggers of substance use and manage those. Because of the way addiction changes the brain, one of the best ways to help when loving someone with an addiction is to provide frequent feedback and encouragement, planning small immediate rewards every day for any positive changes. Studies show that families that participate in treatment programs increase the likelihood of a loved one staying in treatment and maintaining gains.
Although addiction tends to cut people off from longtime friends, social support is a significant predictor of recovery. Friends have an independent standing that family members do not, and those who are addicted typically do not have a clear picture of the impact of their behavior on themselves and others—which is why friends can play an important role in voicing credible concerns about problem behavior and encouraging someone to seek or stay in treatment. They may know something about the person’s deepest aspirations and voice them as a reminder that can help the person remain on the road to recovery. Friends can be vital sources of support on the bad days. And they can help plan healthy joint activities to ensure that there are good days.
But addiction and friendship have two sides. There are some friends who are better left behind—those who are linked to the addictive experience. People in the throes of addiction are not capable of the best form of friendship. Further, those friends can serve as a cue that sets off drug craving and challenges the recovery process.
What is needed is any type of care or program that facilitates not merely a drug-free life but the pursuit of new goals and new relationships. There are many roads to recovery , and needs vary from individual to the next. Some people need medication to help them recover, some need the structured support of an outpatient program of a treatment facility to help them through, others need a recovery residence, while others get sufficient information and nourishment from the regular contact with others that self-help groups provide. Others do well on their own making use of available community resources.
But attention to the addiction is only one facet of recovery. Recovery involves rebuilding a life— returning to wellness and becoming a functioning member of society. Every person needs a comprehensive recovery plan that addresses educational needs, job skills, social relationships, and mental and physical health. Therapy may be critical to resolving underlying problems that made escape into substance use so appealing in the first place.
In addition, self-care is a vital foundation for a healthy new identity. At the very least, self-care should include sleep hygiene, good nutrition, and physical activity. Sleep is essential for shoring up impulse control and fostering good decision-making. Another vital element of care during recovery is relapse prevention—learning specific strategies for dealing with cravings, stress, setbacks, difficult situations, and other predictable challenges.
What is advisable depends on the needs of each individual. Many types of recovery support are available, and many people make use of more than one type at any time and may shift from one type of support to another as recovery proceeds and needs evolve. An increasing number of high schools and colleges offer addiction recovery resources (CRPS, or Collegiate Recovery Programs) for students, including mentors, workshops, dedicated lounges, and group meetings and activities. Below is a sampling of many types of support that can be found.
• Recovery coach — a life coach specifically focused on serving as a mentor for the lifestyle changes required for overcoming addiction
Individual therapy —typically aims to resolve psychological problems leading to addiction and furnish skills for regaining control of life
Group therapy —many varieties, some serving special populations such as students or executives, often adapting skills and strategies of cognitive and behavioral therapy
Support or self-help or peer-support groups —they come in many varieties (some for women only, some faith-based) and meet regularly to help individuals navigate life and its challenges and, often, the consequences of addiction, from triggers to use to overcoming shame to handling legal problem resulting from addiction to overcoming barriers to employment.
Community Reinforcement —programs that focus on helping individuals rebuild disrupted lives in healthy and pleasurable ways within a family and community setting
Recovery Community Centers —peer-operated non-residential centers that provide recovery information and resources, activities, and family support in a locality
Outpatient programs —formal programs administered regularly for a large portion of the day, typically based at a healthcare facility and involving individual therapy and group sessions that teach an array of life skills
Recovery residences —sometimes also called sober living, these are living quarters specifically housing people for a period of time during the early stages of recovering from addiction
Not only is addiction relapse common, relapse is not considered a sign of failur e. In fact, people in recovery might be better off if the term “relapse” were abandoned altogether and “recurrence” substituted, because it is more consistent with the process and less stigmatizing.
Recovery from addiction is not a linear process, and increasingly, relapse is seen as an opportunity for learning. Relapse is now commonly considered a stage of change . Studies show that those who detour back to substance use are responding to drug-related cues in their surroundings—perhaps seeing a hypodermic needle or a whiskey bottle or a person or a place where they once obtained or used drugs. Such triggers are especially potent in the first 90 days of recovery, when most relapse occurs, before the brain has had time to relearn to respond to other rewards and rewire itself to do so. Learning what one’s triggers are and acquiring an array of techniques for dealing with them should be essential components of any recovery program.
The world of addiction is deeply divided on this issue, and conflicting information abounds. Those who subscribe to the belief that addiction is a brain disease see it as a lifelong condition posing the ever-present danger of relapse, even after decades of remission. Those who view addiction as a condition that has been learned so deeply it is wired into the neural circuity see recovery very differently; they consider it a process of growth and development and regard relapse as a sign that the person has more relearning to do to accomplish rewiring of the brain. They do not minimize the difficulties in overcoming addiction but feel the belief that “once an addict, always an addict” is harmful as well as incorrect.
The fact is that people change and grow, and there is hard evidence—some of it reported by scientists who subscribe to addiction-is-a-disease thinking—that the brain changes that are the hallmark of addiction are reversible after substance use is stopped. Moreover, the fact that the vast majority of those addicted in fact recover gives the lie to the belief that people are powerless to conquer addiction. According to the National Institute on Alcoholism and Alcohol Abuse, 75 percent of alcoholics recover without treatment. People who believe they are powerless and will always be struggling with addiction wind up fulfilling that prophecy; their belief exacerbates the negative self-talk that often accompanies addiction and traps them in it.
According to the National Institute on Drug Abuse, an estimated 40 to 60 percent of people trying to quit use of drugs, and 50 to 90 percent of those trying to quit alcohol, experience at least one slip up in their first four years of recovery. Many experience more than one. Return to use is most common during the first 90 days of recovery . Relapse carries an increased risk of overdose if a person uses as much of the drug as they did before quitting.
Nevertheless, experts see relapse as an opportunity to learn from the experience about personal vulnerabilities and triggers, to develop a detailed relapse prevention plan, and to step up treatment and support activities.
The most common causes of relapse include:
• exposure to environmental cue related to drug use
• stress
• interpersonal difficulties
• peer pressure
• lack of social support
• pain due to injuries or medical problems
• lack of a sense of self-efficacy
• positive moods.
Research has identified relapse patterns in adolescents and adults recovering from addiction. In one study, two-thirds of the adults relapsed in social situations in which they experienced urges and temptations to drink or use. One third experienced relapses when they were experiencing negative emotions and urges to drink/use. By contrast, most adolescents relapsed in social settings when they were trying to enhance a positive emotional state. A small group of adolescents relapsed when facing interpersonal difficulties accompanied by negative emotions and social pressures to drink or use. Treatment and education can help adults learn techniques for handling urges and ways of accepting and managing negative emotions. Treatment and information aimed at adolescents can help them learn techniques for managing both positive and negative emotional states.
Other research pinpoints the values of cognitive behavioral therapy for relapse prevention, as it helps people change negative thinking patterns and develop good coping skills. In addition, learning relaxation techniques can help those in recovery by reducing the tension that is often an immediate trigger of relapse, become comfortable with uncomfortable feelings, and release negative feelings that can trigger relapse.
Mindfulness training, a common component of cognitive behavioral therapy , can help people ride out their cravings without acting on them. A practice known as “urge-surfing” rests on the understanding that urges are impulses connected to old habits and they pass in 15 or 20 minutes, during which time it is possible to take a mental step back from them and mindfully observe them without giving in to them.
The best way to handle a relapse is to take quick action to seek help, whether it’s intensifying support from family, friends, and peers or entering a treatment program. One advantage of mutual support groups is that there is likely someone to call on in such an emergency who has experienced a relapse and knows exactly how to help. In addition, immediately attending or resuming group meetings and discussing the relapse can yield much advice on how to continue recovery without succumbing to the counterproductive feeling of shame or self-pity.
Other important measures include:
• Reflecting on what triggered the relapse and what feelings and experiences occurred just before it happened
• Engaging in self-care—maintaining healthy practices, including getting abundant sleep, which bolsters the ability to ride out cravings and summon coping skills
• Developing a detailed relapse prevention plan and keeping it in a convenient place for quick access when cravings hit, which helps guard against relapse in the future. A good relapse prevention plan specifies a person’s triggers for drug use, lists several coping skills to deploy, and lists people to call on for immediate support, along with their contact information.
Gaining the skills to avoid relapse is a necessary part of the recovery process. However, focusing on the fear of relapse is not enough. At least equally necessary is developing in a positive direction out of the addiction. Recovery is always developmental . The key is cultivating new goals and taking measures to move towards them. The motivational force of new goals eventually helps rewire the brain so that it has alternatives to the drive for drugs. It’s hard to leave addiction behind without constructing a desirable future.
For all practical purposes with regard to drug use, the terms remission and recovery mean the same thing—a person regaining control of their life and reversing the disruptive effects of substance use on the brain and behavior. The Diagnostic and Statistical Manual of Mental Disorders (DSM) avoids the terms addiction and recovery . Sustained remission is applied when, after 12 months or more, a substance is no longer used and no longer produces negative life consequences.
Studies of outcome of addiction treatment may use one term or the other, but they typically measure the same effects. Still, some people in the addiction-treatment field reserve recovery to mean only the process of achieving remission and believe it is a lifelong enterprise of avoiding relapse. Recovery suggests a state in which the addiction is overcome; clinical experience and research studies provide ample evidence.
There is hard data showing that the changes to the brain’s neurotransmitters and neural circuits that turn repeated substance use into addiction can be reversed after cessation of drug use, even in the case of addiction to methamphetamine. That is because the brain is plastic and changes in response to experience—the capacity that underlies all learning. Recovery, like addiction itself, relies on neuroplasticity . In one set of studies looking at some measures of dopamine system function, activity returned to normal levels after 14 months of abstinence. Over time, reward circuits regain sensitivity to respond to normal pleasures and to motivate pursuit of everyday activities. Areas of executive function regain capacity for impulse control, self-regulation, and decision-making.
Addiction has effects on almost every facet of life: It isolates people; it interrupts development all along the lifespan but perhaps most critically among the young, who are still actively acquiring a foundation for life; it can inflict lasting damage on and even destroy families, careers, and finances; and it essentially annihilates self-respect. All have to be addressed—or redressed.
Experts believe that tackling the emotional residue of addiction—the guilt and shame—is fundamental to building a healthy life. It’s not possible to undo the damage that was done, but it is possible to build new sources of self-respect by acknowledging past harms, repairing relationships, and maintaining the commitment to recovery.
Becoming a contributing member of society typically entails resuming interrupted education and acquiring job skills, but most of all it means finding new life goals and new activities that serve as sources of pleasure—having things to look forward to. At every step of the way, support from friends, peers, and family is useful, but there are also many services and organizations that provide guidance., and many can be accessed through Recovery Community centers.
Employment is virtually essential for having a stable and meaningful life. Jobs provide both structure and reward. But a history of addiction can be an impediment to getting a job. A lack of positive references and having a criminal record typically pose challenges. Too, there may be long gaps in a resume that are hard to explain away. Insufficient experience or skill deficits are other common hurdles.
But they are not insurmountable. There are companies large and small that have recovery-friendly hiring practices. In addition, there are nonprofit organizations such as American in Recovery and the National HIRE Network that specifically help those with addiction or criminal history to find work. Usually for a substantial fee, career transition services help executive and higher-up employees define career goals and help with job searches. Many treatment programs have partnerships with area businesses to hire those in recovery. And one measure of a comprehensive substance abuse treatment program is the help it offers to enrollees to identify their interests and find and build a meaningful career path. Individuals with experience and expertise may find a route to full employment by first being willing to offer their skills pro bono or as a volunteer to businesses or nonprofit organizations in their field.
Practical obstacles are not the only hurdles to finding work. Getting a job under the best of conditions can take time, effort, and a high tolerance for rejection. For those recovering from addiction, self-esteem and emotion management skills may be wobbly and require extra support. Still, job seekers in recovery have an advantage , some experts maintain: Recovery cultivates the “soft skills”—creativity, persuasion, collaboration, adaptability, and emotional intelligence—that are increasingly in demand. The personal growth that recovery requires should bolster the confidence and strength to weather the job market .

Attacking common negative thought patterns can benefit many survivors of a difficult childhood.

Here's why these two Netflix series need to be on your mental health watch-list.
Poet and advocate Alicia Cook shares her grief, mental health struggles, and healing journey after a close family member lost her life to opioid addiction.

With the urgent need for mental health solutions, psychedelic treatments are developed carefully, while underground therapists offer a stopgap measure.

Experts are warning that the problem of out-of-control technology continues to grow in alarming ways. Here are 8 ways parents can protect their children.

This non-invasive therapy can help clear the way to long-term recovery.

Master the art of presence and single-tasking to combat overwhelm, reclaim focus, and rediscover the joy of being fully present in every moment.

How impulse affects our decisions.

Discover the latest advancements in treating obsessive-compulsive disorder, including innovative cognitive-behavioral and strategic therapies designed to enhance patient outcomes.

Teens and screens notoriously share a complex relationship that can jeopardize long-term mental health and well-being. Here's how we optimize the benefits and mitigate the risks.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

At any moment, someone’s aggravating behavior or our own bad luck can set us off on an emotional spiral that threatens to derail our entire day. Here’s how we can face our triggers with less reactivity so that we can get on with our lives.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
Drugs, Brains, and Behavior: The Science of Addiction Treatment and Recovery
Can addiction be treated successfully.
Yes, addiction is a treatable disorder. Research on the science of addiction and the treatment of substance use disorders has led to the development of research-based methods that help people to stop using drugs and resume productive lives, also known as being in recovery.
Can addiction be cured?
Like treatment for other chronic diseases such as heart disease or asthma, addiction treatment is not a cure, but a way of managing the condition. Treatment enables people to counteract addiction's disruptive effects on their brain and behavior and regain control of their lives.
Does relapse to drug use mean treatment has failed?
No. The chronic nature of addiction means that for some people relapse, or a return to drug use after an attempt to stop, can be part of the process, but newer treatments are designed to help with relapse prevention. Relapse rates for drug use are similar to rates for other chronic medical illnesses. If people stop following their medical treatment plan, they are likely to relapse.
Treatment of chronic diseases involves changing deeply rooted behaviors, and relapse doesn’t mean treatment has failed. When a person recovering from an addiction relapses, it indicates that the person needs to speak with their doctor to resume treatment, modify it, or try another treatment. 52
While relapse is a normal part of recovery, for some drugs, it can be very dangerous—even deadly. If a person uses as much of the drug as they did before quitting, they can easily overdose because their bodies are no longer adapted to their previous level of drug exposure. An overdose happens when the person uses enough of a drug to produce uncomfortable feelings, life-threatening symptoms, or death.
What are the principles of effective treatment?
Research shows that when treating addictions to opioids (prescription pain relievers or drugs like heroin or fentanyl), medication should be the first line of treatment, usually combined with some form of behavioral therapy or counseling. Medications are also available to help treat addiction to alcohol and nicotine.
Additionally, medications are used to help people detoxify from drugs, although detoxification is not the same as treatment and is not sufficient to help a person recover. Detoxification alone without subsequent treatment generally leads to resumption of drug use.
For people with addictions to drugs like stimulants or cannabis, no medications are currently available to assist in treatment, so treatment consists of behavioral therapies. Treatment should be tailored to address each patient's drug use patterns and drug-related medical, mental, and social problems.
What medications and devices help treat drug addiction?
Different types of medications may be useful at different stages of treatment to help a patient stop abusing drugs, stay in treatment, and avoid relapse.
- Treating withdrawal. When patients first stop using drugs, they can experience various physical and emotional symptoms, including restlessness or sleeplessness, as well as depression, anxiety, and other mental health conditions. Certain treatment medications and devices reduce these symptoms, which makes it easier to stop the drug use.
- Staying in treatment. Some treatment medications and mobile applications are used to help the brain adapt gradually to the absence of the drug. These treatments act slowly to help prevent drug cravings and have a calming effect on body systems. They can help patients focus on counseling and other psychotherapies related to their drug treatment.
- Preventing relapse. Science has taught us that stress cues linked to the drug use (such as people, places, things, and moods), and contact with drugs are the most common triggers for relapse. Scientists have been developing therapies to interfere with these triggers to help patients stay in recovery.
Common medications used to treat drug addiction and withdrawal
- Buprenorphine
- Extended-release naltrexone
- Nicotine replacement therapies (available as a patch, inhaler, or gum)
- Varenicline
- Acamprosate
How do behavioral therapies treat drug addiction?
Behavioral therapies help people in drug addiction treatment modify their attitudes and behaviors related to drug use. As a result, patients are able to handle stressful situations and various triggers that might cause another relapse. Behavioral therapies can also enhance the effectiveness of medications and help people remain in treatment longer.
- Cognitive-behavioral therapy seeks to help patients recognize, avoid, and cope with the situations in which they're most likely to use drugs.
- Contingency management uses positive reinforcement such as providing rewards or privileges for remaining drugfree, for attending and participating in counseling sessions, or for taking treatment medications as prescribed.
- Motivational enhancement therapy uses strategies to make the most of people's readiness to change their behavior and enter treatment.
- Family therapy helps people (especially young people) with drug use problems, as well as their families, address influences on drug use patterns and improve overall family functioning.
- Twelve-step facilitation (TSF) is an individual therapy typically delivered in 12 weekly session to prepare people to become engaged in 12-step mutual support programs. 12-step programs, like Alcoholic Anonymous, are not medical treatments, but provide social and complementary support to those treatments. TSF follows the 12-step themes of acceptance, surrender, and active involvement in recovery.
How do the best treatment programs help patients recover from addiction?

Stopping drug use is just one part of a long and complex recovery process. When people enter treatment, addiction has often caused serious consequences in their lives, possibly disrupting their health and how they function in their family lives, at work, and in the community.
Because addiction can affect so many aspects of a person's life, treatment should address the needs of the whole person to be successful. Counselors may select from a menu of services that meet the specific medical, mental, social, occupational, family, and legal needs of their patients to help in their recovery.
For more information on drug treatment , see Principles of Drug Addiction Treatment: A Research-Based Guide , and Principles of Adolescent Substance Use Disorder Treatment: A Research-Based Guide .

Professionals

Patient Journey Map
Substance use disorder treatment and recovery experiences, research report | june 2022.
Jessica Hulsey
Kayla Zawislak, MSW, CADC
About the Report
Addiction Policy Forum’s (APF) Patient Experiences Journey Map was developed through the input of patients in treatment and recovery from substance use disorder (SUD). The map underscores the obstacles and positive points patients encounter across seven distinct phases, from treatment to finding long-term, stable recovery.
The Addiction Policy Forum was named one of the winners of the National Institute on Drug Abuse “Mapping Patient Journeys in Drug Addiction Treatment Challenge”; funds from this prize were used to support the development of this report.
The qualitative study included 60 Life Course History interviews of individuals in recovery from substance use disorders across 22 states and Canada.
.png)
Participants Overview
Of the 60 participants, 55% identify as female (n=33) and 45% male (n=27). The race and ethnicity breakdown of participants is as follows: 60% non-Hispanic White; 17% Hispanic/LatinX; 10% Black or African American; 3% Native American/Alaskan Native; 3% Asian or Asian-American; and 7% multiracial. Participants were from 22 U.S. states and Canada.
The study included individuals in recovery from a SUD. Seventy-two percent report a single, primary SUD, 28% reported a polysubstance use disorder, and 98% report using multiple substances during active addiction. The breakdown of types of SUD is as follows: 19 participants reported an alcohol use disorder, 17 a polysubstance use disorder, 13 an opioid use disorder, 9 a stimulant use disorder, and 2 a cannabis use disorder.
Study Design
Addiction Policy Forum collected the data between August 12th and December 12th, 2021. All research protocols, instruments, and communication materials were reviewed and approved by an independent institutional review board. The interviews were conducted by CITI-trained APF staff who are in recovery from a substance use disorder. Sixty interviews were conducted with variance in geography, race/ethnicity, gender, socioeconomic background and SUD type. The project utilized a life course history structure, followed by a rapid qualitative inquiry to analyze the data.
Life Course History Interviews
As a concept, life course theory is defined as "a sequence of socially defined events and roles that the individual enacts over time." Life Course History interviews are a person-centered research method that requires “respondents to provide a subjective account of their life over a certain period of time, described in their own words, across their own personal timelines."
Life Course History one-on-one interviews empower patients with lived experience to tell their unique stories in a semi-structured interview process with time to reflect and describe their journeys. This qualitative approach to data collection allowed APF to build a comprehensive and accessible patient journey map that illustrates how complex interactions over the course of an individual’s life contribute to the onset, progression, and treatment of a SUD and the elements of long-term recovery.
Interviews included questions related to substance use; trauma and adverse childhood experiences; treatment episodes; facilitators and barriers to seeking and pursuing treatment and recovery; and other information related to lived experience with addiction and recovery, building upon existing validated instruments as well as open questions and conversation to allow for engagement.
Instruments used include the Addiction Severity Index (ASI), the Inventory of Drug Use Consequences (InDUC), Adverse Childhood Experiences Screening, and the Global Appraisal of Individual Needs (GAIN). Each interview began by securing consent from the participant. The audio recording and a transcript of each interview were used for text analysis and coding of individual responses.
Rapid Qualitative Inquiry
The Rapid Qualitative Inquiry (RQI) framework was used to quickly develop a preliminary understanding of the often complicated and varied experiences of accessing treatment and recovery for substance use disorder.

According to Dr. James Beebe, the RQI allowed for a team-based approach to quickly develop an insider's perspective to a specific situation. A small multidisciplinary team of four staff conducted the RQI. The multi-discipline strategy ensured that different perspectives were represented on the team and that individual biases were checked, a key component of rapid qualitative inquiry and the success of the patient journey mapping process.

The Addiction Policy Forum’s Patient Journey Map represents a common set of moments that individuals in treatment and recovery from a substance use disorder experience. While this map does not represent what happens to every individual who engages in treatment for addiction and recovery support, it highlights common elements, bright spots, and pain points in accessing care and finding and maintaining long-term recovery.
Quotes from patients are included to illustrate the salience of the moment. Common threads and insights are also provided, which can guide practitioners and leaders in the improvement of care and patient outcomes for individuals with a substance use disorder.
Each phase highlights the bright spots and pain points derived from actual patient feedback, along with common threads and insights relevant to the patient experience.
.png)
Onset and Progression
Onset is the age at which an individual develops or first experiences a condition or symptoms of a disease or disorder. This section of the Journey Map explains the experiences of onset, specific risk factors for the development of a SUD, as well as health consequences and criminal justice involvement of patients.
Average age of onset is 14 years old.
The average age of first substance use was 14, with the earliest initiation at five years old and the oldest at 19 years old. Patient SUDs include opioid, alcohol, stimulant, marijuana, sedative, and polysubstance use disorder. Nearly one out of four respondents report a primary polysubstance use disorder and 98% report using multiple substances during active addiction.
.png)
For participants with a polysubstance use disorder, 35% reported opioid/stimulant use disorder; 24% alcohol/stimulants; 12% alcohol /opioids; 12% alcohol/marijuana/stimulants; 6% alcohol/sedatives; and 6% marijuana/sedatives.
.png)
85% of patients report a family history of SUD
Eighty-five percent of the respondents reported a family history of addiction, with an average of two previous generations with SUD history.
Frequent childhood trauma
Of the study panel, 90% had at least one adverse childhood event. Of those with childhood traumatic events, the average ACEs score was 4.3, with 47% of patients reporting an ACEs score of 5 or higher. Over 83% experienced household dysfunction, 78% experienced abuse, and 55% suffered from neglect.
.png)
Adverse Childhood Experiences (ACEs) are traumatic events that occur between the ages of 0-17. There are many different kinds of ACEs, including losing a parent, neglect, sexual, physical, or emotional abuse, witnessing a parent being abused, mental illness in the family, and parental SUD. The more ACEs a child has, the more likely he or she is to experience problems later on in life. There are ten types of childhood trauma measured in the ACEs instrument that fall into three categories: abuse, neglect and household dysfunction.
90% of patients experienced household dysfunction, child abuse, neglect
The most common types of household dysfunction experienced were addiction in the household (62%), mental illness or suicide in the household (55%), parental divorce (55%), an incarcerated parent (22%), and domestic violence (17%). Types of abuse experienced were verbal abuse (58%), physical abuse (48%), and sexual abuse (40%).
.png)
3 out of 4 hospitalized due to their addiction
Three out of four patients were hospitalized due to their SUD, most commonly for injuries, infections, overdose, suicide attempt/self-harm, and car accidents.
.png)
70% of patients report justice-involvement
Seventy percent of patients report justice involvement – 63% reported time in jail related to their substance use disorder, 35% participated in a diversion program, such as drug court, and 22% served time in prison.
One participant shared: “I was laying there sick from drinking just a couple days before I was pulled over for a DUI-DWI and I was praying to the Creator to help me because I don't want to be like this anymore to help me stop drinking and then it happened, I was pulled over on August 8th of 2020, I hated it at the time I was sitting in jail because I was going through withdrawals bad but I was also thanking God because I knew I was going to have to stop, I had no choice. I was immediately put on supervision probation and Wellness Court; I believe Wellness Court saved my life, if it wasn't for that, outpatient treatment and the recovery App I would probably have drank myself to death. I couldn't stop drinking in fear of being sick from withdrawals.”
.png)
Damaged relationships and financial issues were most frequent problems caused by substance use disorder
Significant problems caused by SUD were reported by patients, from damaged relationships, to personality changes, to financial problems.
One participant shared: "I did a lot of damage to my family, and myself, self-harm, when I would be in blackout drunk I would carve myself up with knives, I was just so full of hatred, and I was abusive to my ex-boyfriend. I never grew up, I never grew up. I didn't graduate high school, I couldn't keep a job. I just never matured mentally."
.png)
Trigger Events
Multiple trigger events contribute to the decision to get help
On average, patients shared three separate trigger events that contributed to engaging in treatment, a cluster of events that constitute the “Aha moment.” The events weren’t necessarily close in timing, but represented meaningful moments for the patients.
Tired, wanting change is the most common reason for engaging in treatment
The most prevalent reason for engaging in SUD treatment was being tired/wanting change (87%), followed by health reasons (35%), pressure from loved ones (23%), parenting/custody concerns (22%), and pressure from the criminal justice system (20%).
.png)
Another participant shared: “So what stopped me? I just couldn't do it anymore, I was 45. I'm like, what am I doing, you know, shooting dope in my 40's? I've lost everything again, everything. Everything fit in that syringe. My home, my life, my job, my dignity, it all went in there. And I just couldn't sacrifice all of that anymore.”
.png)
Health reasons the second largest driver of engaging in treatment
Physical injury and health concerns were the second most common trigger events for participants. For example, one participant shared, "Two overdoses and had to go to an infectious disease doctor for hepatitis C." And another individual reported: "Bronchitis, and I was treated for sexual assault two times while under the influence."

Children and family cited most frequently as the bright spots early in the process
Bright spots, or positive moments during the trigger events phase, included children and family, relief, hope for change, and encouragement from others.
.png)
Pain points: Managing isolation and shame
Pain points, the difficulties and challenges faced during the trigger phase, included isolation, shame, lost relationships, and fear.
.png)
Getting Help
The help phase details the process that participants went through to research and identify services and resources for the treatment of their substance use disorder. This phase is largely marked by difficulties and barriers for patients.
Significant barriers encountered as patients try to find help
Patients identified the accessing help phase as extremely painful, disorganized, and difficult. Poor treatment access was a common experience among participants who experienced systemic barriers to addiction care, including high levels of stigma (32%); the complexity of navigating the substance use disorders care system (25%); wait times (20%); the high costs of treatment (8%); red tape payer policies such as fail first and prior authorization (7%); and transportation difficulties (5%).
High levels of stigma experienced by patients
Over 30% percent of participants cite stigma as a significant barrier during the process of finding help and treatment. Patients experience stigma from doctors and other healthcare professionals; stigma from families, friends and the general public, as well as experiences of self-stigma, which occurs when individuals internalize the stigmatizing beliefs and attitudes of the public and suffer negative consequences, including delayed treatment access.
.png)
Stigma from healthcare providers is also a pain point for patients. One individual shared: “I think stigma is a really big one, though, just within myself, not with seeking help outside but in having to confront that I have this thing that is frowned on in society.”
Patients most frequently searched for services for themselves
During the getting help phase, over 60% of patients looked for services for themselves. 42% looked for treatment directly and 20% researched and found support groups to attend.
Another 22% talked to a loved one/friend, 7% talked to counselor/mental health professional, 7% received a criminal justice referral, 3% called 911, 3% called their insurance company, and 2% distanced themselves from using location or moved back with family.
.png)
The complexity of the system hampers treatment access
Feeling overwhelmed and confused about how to access treatment, repeated attempts to find treatment with no success, and frustration and agony over lack of access points frequent experiences among patients.
Another participant shared: “Well, I would have been probably in treatment a lot more times if I would have been able to find it some of the times when I looked and didn't have any means to get to it.” Previous treatment and recovery experiences, along with recommendations from friends, family, and a person’s network, frequently form the basis for the treatment pathway selected.

Significant difficulties waiting to access treatment
Long wait times and the pain and discomfort of withdrawal symptoms during that time were a consistent pain point for participants. One individual shared: “It took about a month to get it, though, so it didn't happen right away… that was a long month that was for sure.” Another participant remarked: "The wait, the wait time is long. I was in withdrawal, so the desire to leave and go, you know get well, was really strong."
.png)
Problems navigating insurance
Participants noted difficulties navigating insurance.One individual shared: “Found it to be difficult navigating the insurance. Having to call back all the time and leave your name, because they want to know that you're really serious. And there wasn't a lot of choices, so there was really only one or two places in this town that I was from in Florida, and that was actually much bigger than where i'm at now but there wasn't Enough beds. You know so. That I remember that being a really huge challenge the phone.”
Average of 10 years of disease progression and 6 distinct treatment episodes
On average, patients report 10 years between realizing they have a SUD and finding recovery, participating in an average of 6 treatment episodes that had an additive, or cumulative effect in the success of the most recent treatment engagement. Previous treatment and recovery experiences, along with recommendations from friends, family, and a person’s network, frequently form the basis for the treatment pathway selected.
.png)
Perspectives on Most Frequent Ways Patients Get Help
.png)
Friends and family in recovery a bright spot in the help phase
Bright spots included having family/friends in recovery, not feeling alone, finding a smooth transition into treatment, and finding a community. However, many patients reported no bright spots at all during this phase.
.png)
Waiting for access and managing withdrawal symptoms are pain points for patients
Pain Points included waiting for access, withdrawal symptoms, difficulty finding treatment, navigating insurance, financial barriers and family friends not being supportive.
.png)
Care Begins
The care phase details the connection to treatment or other services, and the assessment process if applicable.
Most patients connect directly with specialty treatment providers
Previous experiences and treatment episodes guide the first contact and research conducted by patients. Direct engagement with a specialized treatment provider was the most often utilized first point of contact to find help (37%), followed by hospital or emergency room (20%), doctors (15%), mental health provider/counselor (7%), and criminal justice agencies (3%).
.png)
Of note, 18% of participants had no involvement with specialty treatment or recovery services and instead managed their symptoms and sobriety independently. One individual shared: “I had zero contact with the professional world when it came to my substance abuse.”
Patients often fearful as care begins
Patients report strong emotions and high levels of uncertainty and fear as care begins. One participant shared: “I did have this mental breakdown in the intake process. Because I just like the revelation that, like my life was going to be changing, and I was also scared as well, so it's like a big mix of emotions and also I was coming down so there's an issue.”
Stigma encountered in healthcare settings
Feeling stigma from healthcare providers and other professionals during the care phase was a continued pain point for patients. One individual shared: “I think stigma is a really big one, though, just within myself, not with seeking help outside but in having to confront that I have this thing that is frowned on in society.
.png)
Co-occurring mental health disorders prevalent
While 68% of patients received a formal SUD assessment, assessments are also needed for co-occurring mental health disorders, physical health, and trauma, as 67% have a co-occurring mental health disorder. Depression, anxiety disorder, and bipolar disorder are the most common diagnoses.
.png)
Trauma experienced during active addiction
Trauma often experienced during active addiction, including physical violence and sexual assault.
One participant shared: "Women, like me, are not supposed to make it, but we do and I think that we tend to judge and not support women that have made some of the choices I've made and been in some of the situations I've been in. I think that there needs to be more support and longer term care for women that are victims of sexual assault in childhood or otherwise, that have been in the sex industry, because it'll kill you. That have been victims of domestic violence, it's not just about getting clean, right? It's about healing this other trauma, there's a lot of trauma."
.png)
Patients report that repetitive assessments and interviews are triggering and difficult
A consistent pain point among patients was repetitive assessments and interviews during the care phase, with reports of feeling triggered and interrogated. Patients also questioned the utility of multiple interviews and the coordination of providers.
.png)
Engagement with friendly providers and peers a bright spot in the care phase
Bright spots during the care phase include friendly engaging staff, peers/recovery coaches, and having employment and housing.
.png)
Negative effects of repetitive assessments and isolation are frequent pain points
A consistent pain point among patients was repetitive assessments and interviews during the care phase, with reports of feeling triggered and interrogated. Patients also questioned the utility of multiple interviews and the coordination of providers. Additional pain points included isolation and feeling stigmatized.
.png)
Treatment and Recovery
The treatment and recovery phase includes the diverse services and resources accessed by the patient, both within the healthcare system and outside. Patients report that previous treatment episodes provided a foundation for treatment and recovery success. Rather than viewing previous episodes as a failure, the skills and tools learned accumulated over time.
Multiple services utilized, not a single intervention
On average, patients utilized four different services for treatment and recovery support, not a single treatment or intervention. Services accessed were support groups (88%), counseling/mental health treatment (57%), intensive outpatient treatment programs (52%), followed by residential programs (37%), aftercare programs (30%), medications for addiction treatment (28%), sober living (22%), and faith-based programs (12%).
.png)
Skills and tools from both current and previous treatment episodes helpful
Patients report that previous treatment episodes provided a foundation for treatment and recovery success. Rather than viewing previous episodes as a failure, the skills and tools learned accumulated over time.
.png)
Layered interventions necessary across 3 key domains – biological, psychological, and social.
Patient feedback shows the need for layered interventions across three critical domains: 1) biological, or physical health, 2) psychological, and 3) social.
Biological interventions range from medications for addiction treatment, medical care for other health conditions, taking prescriptions for mental health disorders and other chronic conditions like heart disease and diabetes, as well as self care priorities that include sleep, exercise and proper nutrition. Forty-seven percent of participants utilized an intervention or service to address physical health.
Three out of four patients required psychological interventions. Psychological interventions include mental health counseling, group counseling, cognitive behavioral therapy, building a relapse prevention plan, identification and awareness of triggers for substance use to include high risk people, places and things, and skills and resource focused strategies like learning new coping skills.
Ninety-five percent of patients require social interventions. Social components include building a positive social network, commonly through support group participation, new hobbies and activities, and cutting out old friends and the individual’s using network.
.png)
Low recovery literacy among healthcare providers creates challenges
A pain point in treatment for patients is encountering low recovery literacy among healthcare providers. Patients share the need to learn how to manage their chronic disorder, and frustration when selected providers are not well versed in the supports and layered interventions that are necessary to achieve stable recovery. Patient input suggests the need for a paradigm shift for SUD management to focus on empowering the person with an addiction to manage the disease successfully and to improve their quality of life.
Managing a SUD requires significant effort on the part of the patient. Whether education and services are embedded with care providers, linkage facilitators, handoffs to peer services, guidance from the primary SUD treatment provider on the components of managing the disease and skills and resources available is beneficial to the patient.
Encounters with providers without the knowledge to assist in the chronic disease management plan are difficult. One participant shared: “For me it really has to do with the level of care. I was going to when I first learned about suboxone I was literally just going to like what I could best described as a meat market, a place that you would go and you get your prescription. And that was it like as long as you had your money you could get the medicine and there was really no recourse for following treatment, so I really wasn't educated about my disease and what recovery was.”
.png)
45% of patients accessed medications for addiction treatment (MAT )
Forty-five percent of participants utilized a medication for addiction treatment (MAT) at one point in their life. All three FDA-approved medications were utilized by patients -- Buprenorphine (52%), Naltrexone (48%), and Methadone (33%).
.png)
Low utilization of medications to treat alcohol use disorder
20% of patients with a primary alcohol use disorder (AUD) utilized an FDA-approved medication for AUD at one point in their life for treatment. Of the 30 AUD participants, 33% were prescribed Naltrexone, 20% Acamprosate, and only 10% of participants utilized Disulfiram.
Patient perspectives on MAT positive, though stigma around medication prevalent
Experiences with MAT were mostly positive, but the stigma around using medications created challenges for patients. One participant shared: "I guess stigma from other people, being on a MAT. I live in... like, it's not a big city. So I would say that this area for a long time has been indoctrinated in the 12 steps. And that includes like medical professionals, I went to my family doctor they wouldn't even entertain anything else other than getting off the methadone. They told me how bad it was and all kinds of things. And then my job, I mean, it was a struggle, because they of course didn't want anybody to know I was on it. And just from friends that weren't using but were in recovery they you know, had an issue with it."
Another shared: "Dealing with the anxiety and the you know all the guilt and shame from before my use so now I don't have that drug to numb me anymore um and. Honestly, a lot of it is a you know, probably people saying that you're not clean, you know i'm not really clean because i'm one method on so like i'm still using something, which I don't really like get to me, but you used to and then also the weight gain you know and people making fun of me for my weight because i've gained a lot of weight."
Bright Spots: Positive social connections and helpful clinicians
Bright spots included positive social connections, helpful clinicians, new tools and skills, learning about the disease, and peer/recovery coaches.
.png)
Pain Points: Hard work and managing shame
Pain Points included the hard work/difficulty of treatment, managing shame and self-stigma, cutting out friends/old networks, transportation challenges, and unhelpful home/work environments.
.png)
Lifestyle Changes
Engaging in treatment and lifestyle modifications are concurrent, not sequential, in finding stable recovery
Lifestyle changes are cited by patients to be as critical to success as treatment and recovery services. Patients share that the things encountered every day play a critical role in supporting or hampering recovery.
.png)
Building a positive social network is a critical lifestyle change
Creating a positive, supportive social network is a dominant feature of successful recovery, along with avoiding individuals, places, and other triggers that present memory and physical cues to resuming substance use (i.e. using friends, bars, parties, concerts, boredom.) The exact constellation of triggers is unique to each patient.
Common lifestyle modifications include avoidance of high-risk people, places, and things (42%), changing friends (40%), becoming honest open-minded and accountable (25%), self-care such as exercise, nutrition, and sleep (23%), and developing a consistent routine (13%).
.png)
Finding a community and feeling happy again are bright spots for patients as they manage lifestyle changes
Bright spots include creating a positive support network, feeling happy again, being present in life again, being reunited with children/family, and feeling physically healthier.
.png)
Difficulty making amends and stigma around medications are pain points for patients
Frequent Pain Points include difficulty making amends, triggers associated with high-risk people, places and things, MAT stigma, trouble sleeping, and sadness/depression.
.png)
Ongoing Support
An average of 3 services utilized for ongoing support
Participants shared that they rely on multiple supports in long-term recovery with an average of three services utilized. The most common services were support groups (65%), family and friends (55%), volunteer and service work (38%), and mental health/counseling (22%). Patients in recovery from SUDs continue supports specific to their needs for years or even decades.
.png)
Over half of patients work with a sponsor or professional to help manage their recovery
58% of patients report having a physician, recovery coach or other professional to help manage their recovery.
42% have a sponsor
27% see a counselor
15% see a psychiatrist
13% see a physician
5% have a recovery coach
.png)
Before and After: Active Addiction to Stable Recovery
Analysis of 60 life course history interviews conducted during the study showed specific themes from onset, progression to treatment and recovery. A word cloud is a visual representation of word frequency where the more commonly used terms in the analyzed text appear larger in the visualization. Themes and tags relevant to active addiction included homelessness, job loss, trauma, children and custody issues, health challenges, school suspension and expulsion, negative impact on friends and family. In contrast, common themes related to recovery include improved relationships, experiencing life, freedom, health and wellness and words like good, love and amazing.
.png)
Having a full life and the feeling of accomplishment are bright spots in recovery
.png)
Health consequences and limited access to services are pain points in recovery
.png)
Ways Forward
Key next steps based on the findings of this report include:
1. Reduce barriers to treatment
Patients encounter systemic barriers to addiction care, including long wait times; high treatment costs of treatment; and red tape payer policies such as fail first and prior authorization. Patients require assistance navigating the substance use disorders care system, determining evidence-based care options, and support for the management of the chronic condition.
2. Ensure stigma training for all healthcare providers
Research has found that individuals who experience stigma due to an SUD are more likely to continue engaging in substance use, and manifest greater delayed treatment access and higher rates of dropout. Patients in the study shared the difficulty of interfacing with healthcare professionals with stigmatizing beliefs and attitudes. Efforts to decrease stigma should include increasing addiction literacy levels to counteract education gaps and misconceptions about SUDs.
3. Streamline the assessment process
Patients share the tremendous discomfort and trauma of repetitive assessments and interviews when accessing treatment. Responses include feeling triggered and interrogated and questioning the utility of multiple interviews. Clinicians can streamline the assessment process and share information with other providers.
4. Individualized care and management plans needed
The majority of patients utilize multiple services for treatment and recovery support, not a single treatment or intervention. Patients on average utilized four services during treatment and three in long-term care management. Lifestyle modifications, such as building a positive social network and discontinuing contact with those still using substances, are critical elements of recovery stability. More education for both patient and providers is needed to reinforce the individualized, multi-faceted management plans needed.
5. Screen for ACEs
Most patients have experienced multiple adverse childhood experiences, particularly living in a household with SUD. Evidence-based prevention strategies are available and yet underutilized, including screening, early intervention, programs to address ACEs and children impacted by parental substance use disorder, as well as primary prevention interventions. Preventing the development of substance use disorders must be a priority and can change the trajectory of the crisis.
Addiction Policy Forum
Addiction Policy Forum aims to eliminate addiction as a major health problem by translating the science of addiction and bringing all stakeholders to the table. The organization works to elevate awareness around substance use disorders and help patients and families in crisis. Founded in 2015, Addiction Policy Forum empowers patients and families to bring innovative responses to their communities and end stigma through science and learning.
Jessica Hulsey, Addiction Policy Forum
Kayla Zawislak, MSW, CADC, Addiction Policy Forum
© Addiction Policy Forum
All rights reserved. No portion of this book may be reproduced in any form without permission from the publisher, except as permitted by U.S. copyright law. For permissions contact: [email protected]
Acknowledgments: Supported in part by the National Institute on Drug Abuse (NIDA), National Institutes of Health (NIH), U.S. Department of Health and Human Services (HHS).
Suggested Citation: Substance Use Disorder Patient Experiences through a Journey Map. Addiction Policy Forum. (2022).
Sales, rights and licensing: To purchase APF publications, see https://www.addictionpolicy.org/store.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

In Crisis? Call or Text 988
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Recovery and Recovery Support
SAMHSA's working definition of recovery defines recovery as a process of change through which individuals improve their health and wellness, live self-directed lives, and strive to reach their full potential. Recovery signals a dramatic shift in the expectation for positive outcomes for individuals who experience mental and substance use conditions or the co-occurring of the two.
On March 1, 2022, President Biden announced his administration’s strategy to address our nation’s mental health crisis as outlined in the 2022 Presidential Unity Agenda. To meet this goal, SAMHSA collaborated with federal, state, tribal, territorial, and local partners including peer specialists to develop the National Model Standards for Peer Support Certification .

2 in 3 adults who ever had a mental health problem considered themselves to be recovering or in recovery.

7 in 10 adults who ever had a substance use problem considered themselves to be recovering or in recovery.
50.2 million American adults considered themselves to be in recovery from their substance use and/or mental health problems.
Guiding Principles
Hope, the belief that these challenges and conditions can be overcome, is the foundation of recovery. A person’s recovery is built on his or her strengths, talents, coping abilities, resources, and inherent values. It is holistic, addresses the whole person and their community, and is supported by peers, friends, and family members.
The process of recovery is highly personal and occurs via many pathways. It may include clinical treatment, medications, faith-based approaches, peer support, family support, self-care, and other approaches. Recovery is characterized by continual growth and improvement in one’s health and wellness and managing setbacks. Because setbacks are a natural part of life, resilience becomes a key component of recovery.
The Four Major Dimensions of Recovery
- Health - Overcoming or managing one’s disease(s) or symptoms - for example, abstaining from use of alcohol, illicit drugs, and non-prescribed medication if one has an addiction problem- and for everyone in recovery making informed, healthy choices that support physical and emotional well-being
- Home - Having a stable and safe place to live
- Purpose - Conducting meaningful daily activities, such as a job, school volunteerism, family caretaking, or creative endeavors, and the independence, income, and resources to participate in society
- Community - Having relationships and social networks that provide support, friendship, love, and hope

Recovery Newsroom
Get the latest announcements on SAMHSA’s effort to address recovery support. Access the latest news, upcoming events, and more .
Join Our Mailing List

Recovery Funding
- Statewide Consumer Network Grant FY22
- National Consumer and Consumer Supporter Technical Assistance Grant FY20
- Statewide Family Network Program FY22
- Building Communities of Recovery FY22
- Recovery Community Services Program FY20
- Enhancement and Expansion of Treatment and Recovery Services for Adolescents, Transitional Aged Youth, and their Families FY18
- Fiscal Year 2024 Innovative Coordinated Access and Mobility Notice of Funding Opportunity
- Notice of Special Interest (NOSI): Strategies to Address Stigmatizing Beliefs and Policies Affecting People Who Use Drugs
- Peer Recovery Center of Excellence
- Consumer Supporter Technical Assistance Center – The Family Cafe
- Doors to Wellbeing
- National Empowerment Center TAC
- Peer Support Coalition of Florida
- YouthMOVE Peer Center
- National Family Support Technical Assistance Center
- Tribal Training and TAC
- National Harm Reduction TAC
- National Recovery Month
- Best Practices for Recovery Housing
- Recovery Summit Executive Summary (PDF | 351 KB)
- SAMHSA Inclusion Policy (PDF | 195 KB)
- Allowable Recovery Support Services RSS Expenditures through the SUBG and the MHBG (PDF | 464 KB)
- Recovery from Substance Use and Mental Health Problems Among Adults in the United States (PDF | 439 KB)
- Building New Horizons: Opening Career Pathways for Peers with Criminal Justice Backgrounds - SMI Adviser
- Consumer Operated Services Program EBP Toolkit
- Other Recovery Publications
Get the latest announcements on SAMHSA’s effort to address recovery support. Access the latest news, upcoming events, and more.
- Recovery to Practice Webinars
- I Don't Know How To: Parent Series
- Recovery Month Equity Week Webinars
- SAMHSA Tribal Recovery Summit 2023
Peer Support Webinars
- Striving and Thriving among Certified Peer Specialists (1 hour, 4 minutes)
Recovery Exchange Webinars
- Recovery Exchange Meeting - April 2024 (56 minutes)
- Recovery Exchange Meeting - December 2023 (1 hour, 3 minutes)
- Region 3 Community Meeting (PDF | 733 KB)
- Region 5 Community Meeting (PDF | 1.3 MB)
- Peers and Psychiatry in Dialogue - Meeting Summary (PDF | 461 KB)
- Recovery Research Technical Expert Panel - Executive Summary & Report (PDF | 1.1 MB)
- Peer Possibilities: National Peer Workforce Summit - Executive Summary and Meeting Report (PDF | 640 KB)
- Peer-Operated Warm Lines Technical Experts Panel - Executive Summary and Meeting Report (PDF | 471 KB)
- Lifting Lived Experience Across Criminal Justice Settings - Executive Summary and Report (PDF | 665 KB)
- Digital Recovery Support Innovations Technical Expert Panel Executive Summary & Report (PDF | 635 KB)
- The Intersection of Recovery Housing & Housing First— A Dialogue on Collaboration and Partnership (PDF | 700 KB)
- Collegiate Recovery Executive Summary & Report (PDF | 813 KB)
NA and Other Peer Support Groups for Drug Addiction
- Choosing a Drug Rehab Addiction Program
Dual Diagnosis: Substance Abuse and Mental Health
Choosing an alcohol rehab treatment program, staying social when you quit drinking.
- Vaping: The Health Risks and How to Quit
Women and Alcohol
- Binge Drinking: What it is, the Effects, and How to Stop
- Online Therapy: Is it Right for You?
- Mental Health
- Health & Wellness
- Children & Family
- Relationships
Are you or someone you know in crisis?
- Bipolar Disorder
- Eating Disorders
- Grief & Loss
- Personality Disorders
- PTSD & Trauma
- Schizophrenia
- Therapy & Medication
- Exercise & Fitness
- Healthy Eating
- Well-being & Happiness
- Weight Loss
- Work & Career
- Illness & Disability
- Heart Health
- Childhood Issues
- Learning Disabilities
- Family Caregiving
- Teen Issues
- Communication
- Emotional Intelligence
- Love & Friendship
- Domestic Abuse
- Healthy Aging
- Aging Issues
- Alzheimer’s Disease & Dementia
- Senior Housing
- End of Life
- Meet Our Team
The first step to overcoming drug abuse and addiction
Explore your addiction treatment options, find support for your addiction recovery, learn healthy ways to cope with stress, be aware of drug triggers, cope with drug cravings, build a meaningful drug-free life.
- Don't let relapse keep you down
Overcoming Drug Addiction
Ready to deal with your drug abuse problem? This step-by-step guide can help you cope with cravings, deal with relapse, and overcome your substance use disorder.

Developing an addiction to drugs isn’t a character flaw or a sign of weakness, and it takes more than willpower to overcome the problem. Abusing illegal or certain prescription drugs can create changes in the brain, causing powerful cravings and a compulsion to use that makes sobriety seem like an impossible goal. But recovery is never out of reach, no matter how hopeless your situation seems or how many times you’ve tried and failed before. With the right treatment and support, change is always possible.
For many people struggling with addiction, the toughest step toward recovery is the very first one: recognizing that you have a problem and deciding to make a change. It’s normal to feel uncertain about whether you’re ready to start recovery, or if you have what it takes to quit. If you’re addicted to a prescription drug, you may be concerned about how you’re going to find an alternate way to treat a medical condition. It’s okay to feel torn. Committing to sobriety involves changing many things, including:
- The way you deal with stress.
- Who you allow in your life.
- What you do in your free time.
- How you think about yourself.
- The prescription and over-the-counter medications you take.
It’s also normal to feel conflicted about giving up your drug of choice, even when you know it’s causing problems in your life. Recovery requires time, motivation, and support, but by making a commitment to change, you can overcome your addiction and regain control of your life.
Think about change
- Keep track of your drug use, including when and how much you use. This will give you a better sense of the role the addiction is playing in your life.
- List the pros and cons of quitting, as well as the costs and benefits of continuing your drug use.
- Consider the things that are important to you, such as your partner, your kids, your pets, your career, or your health. How does your drug use affect those things?
- Ask someone you trust about their feelings on your drug use.
- Ask yourself if there’s anything preventing you from changing. What could help you make the change?
Preparing for change: 5 keys to addiction recovery
- Remind yourself of the reasons you want to change.
- Think about your past attempts at recovery, if any. What worked? What didn’t?
- Set specific, measurable goals, such as a start date or limits on your drug use.
- Remove reminders of your addiction from your home, workplace, and other places you frequent.
- Tell friends and family that you’re committing to recovery, and ask for their support.
Once you’ve committed to recovery, it’s time to explore your treatment choices. While addiction treatment can vary according to the specific drug, a successful program often includes different elements, such as:
Detoxification . Usually the first step is to purge your body of drugs and manage withdrawal symptoms.
Behavioral counseling . Individual, group, and/or family therapy can help you identify the root causes of your drug use, repair your relationships, and learn healthier coping skills.
Medication may be used to manage withdrawal symptoms, prevent relapse, or treat any co-occurring mental health condition such as depression or anxiety.
Long-term follow-up can help to prevent relapse and maintain sobriety. This may include attending regular in-person support groups or online meetings to help keep your recovery on track.
Speak to a Licensed Therapist
BetterHelp is an online therapy service that matches you to licensed, accredited therapists who can help with depression, anxiety, relationships, and more. Take the assessment and get matched with a therapist in as little as 48 hours.
Types of drug treatment programs
- Intensive inpatient treatment . This is a short-term clinical treatment for people who have developed a physiological dependence on a drug and need help with withdrawal symptoms.
- Residential treatment . Residential treatment involves living at a facility and getting away from work, school, family, friends, and addiction triggers while undergoing intensive treatment. Residential treatment usually lasts from 30 days to several months.
- Day treatment/Partial hospitalization programs (PHP) . Partial hospitalization is for people who require ongoing medical monitoring but wish to still live at home and have a stable living environment. These treatment programs usually meet at a treatment center for at least 20 hours a week, but you return home at the end of each day.
- Intensive outpatient programs (IOP) . Similar to PHPs, IOPs don’t require you to live at a treatment center. However, they differ from PHPs in that they only require between 9 and 19 hours of treatment each week, so you can schedule treatments around school and work.
- Therapy . One-on-one or group therapy sessions can be useful in developing coping skills, identifying triggers, and exploring the roots of your addiction.
Remember that everyone’s needs are different. For example, not everybody requires medically supervised detox or an extended stint in rehab. Whether you have a problem with illegal or prescription drugs, addiction treatment should be customized to your unique situation. It’s also important to find a program that feels right for you. Read Choosing Drug Rehab and Addiction Treatment to learn more.
Tips for finding the best drug addiction treatment for you
Remember that no treatment works for everyone. Everyone’s needs are different. Whether you have a problem with illegal or prescription drugs, addiction treatment should be customized to your unique situation. It’s important that you find a program that feels right.
Treatment should address more than just your drug abuse. Addiction affects your whole life, including your relationships, career, health, and psychological well-being. Treatment success depends on developing a new way of living and addressing the reasons why you turned to drugs in the first place. For example, your drug dependency may have developed from a desire to manage pain or to cope with stress, in which case you’ll need to find a healthier way to relieve pain or to handle stressful situations.
Commitment and follow-through are key. Drug addiction treatment is not a quick and easy process. In general, the longer and more intense the drug use, the longer and more intense the treatment you’ll need. And in all cases, long-term follow-up care is crucial to recovery.
There are many places to turn for help. Not everybody requires medically supervised detox or an extended stint in rehab. The care you need depends on a variety of factors, including your age, drug-use history, medical or psychiatric conditions. In addition to doctors and psychologists, many clergy members, social workers, and counselors offer addiction treatment services.
Seek treatment for any mental health problems simultaneously . As you seek help for drug addiction, it’s also important to get treatment for any other medical or psychological issues you’re experiencing. Your best chance of recovery is by getting combined mental health and addiction treatment from the same treatment provider or team.
Don’t try to go it alone—reach out for support. Whatever treatment approach you choose, having positive influences and a solid support system is essential. The more people you can turn to for encouragement, guidance, and a listening ear, the better your chances for recovery.
Lean on close friends and family. Having the support of friends and family members is an invaluable asset in recovery. If you’re reluctant to turn to your loved ones because you’ve let them down before, consider going to relationship counseling or family therapy.
Build a sober social network. If your previous social life revolved around drugs, you may need to make some new connections . It’s important to have sober friends who will support your recovery. Try taking a class, joining a church or a civic group, volunteering , or attending events in your community.
Consider moving into a sober living home. Sober living homes provide a safe, supportive place to live while you’re recovering from drug addiction. They are a good option if you don’t have a stable home or a drug-free living environment.
Make meetings a priority. Join a 12-step recovery support group, such as Narcotics Anonymous (NA) , and attend meetings regularly. Spending time with people who understand exactly what you’re going through can be very healing. You can also benefit from the shared experiences of the group members and learn what others have done to stay sober.
[Read: NA and Other Peer Support Groups for Drug Addiction]
After addressing your immediate problems with addiction and starting treatment, you’ll still have to face the problems that led to your drug abuse. Did you start using to numb painful emotions, calm yourself after an argument, unwind after a bad day, or forget about your problems?
Once you’re sober, the negative feelings that you dampened with drugs will resurface. For treatment to be successful, you’ll first need to resolve your underlying issues.
Once you have resolved your underlying issues, you will, at times, continue to experience stress, loneliness, frustration, anger, shame, anxiety, and hopelessness. These emotions are all a normal part of life. Finding ways to address these feelings as they arise is an essential component to your treatment and recovery.
There are healthier ways to keep your stress level in check. You can learn to manage your problems without falling back on your addiction. When you’re confident in your ability to quickly de-stress, facing strong feelings isn’t as intimidating or overwhelming.
Quickly relieve stress without drugs
Different quick stress relief strategies work better for some people than others. The key is to find the one that works best for you.
Movement . A brisk walk around the block can be enough to relieve stress. Yoga and meditation are also excellent ways to bust stress and find balance.
Step outside and savor the warm sun and fresh air. Enjoy a beautiful view or landscape.
Play with your dog or cat. Enjoy the relaxing touch of your pet’s fur.
Experiment with your sense of smell. Breathe in the scent of fresh flowers or coffee beans, or savor a scent that reminds you of a favorite vacation, such as sunscreen or a seashell.
Close your eyes and picture a peaceful place. Think of a sandy beach, or a fond memory, such as your child’s first steps or time spent with friends.
Pamper yourself. Make yourself a steaming cup of tea, give yourself a neck or shoulder massage. Soak in a hot bath or shower.
Your recovery doesn’t end at getting sober. Your brain still needs time to recover and rebuild connections that changed while you were addicted. During this rebuild, drug cravings can be intense. You can support your continued recovery by avoiding people, places, and situations that trigger your urge to use:
Step away from your friends who use. Don’t hang out with friends who are still doing drugs. Surround yourself with people who support your sobriety, not those who tempt you to slip back into old, destructive habits.
Avoid bars and clubs. Even if you don’t have a problem with alcohol, drinking lowers inhibitions and impairs judgment, which can easily lead to a relapse. Drugs are often readily available and the temptation to use can be overpowering. Also avoid any other environments and situations that you associate with drug use.
Be upfront about your history of drug use when seeking medical treatment. If you need a medical or dental procedure done, be upfront and find a provider who will work with you in either prescribing alternatives or the absolute minimum medication necessary. You should never feel ashamed or humiliated about previous drug use or be denied medication for pain; if that happens, find another provider.
Use caution with prescription drugs. If you were addicted to a prescription drug, such as an opioid painkiller, you may need to talk to your doctor about finding alternate ways to manage pain. Regardless of the drug you experienced problems with, it’s important to stay away from prescription drugs with the potential for abuse or use only when necessary and with extreme caution. Drugs with a high abuse potential include painkillers, sleeping pills, and anti-anxiety medication.
Sometimes craving cannot be avoided, and it is necessary to find a way to cope:
Get involved in a distracting activity. Read, see friends, go to a movie, immerse yourself in a hobby, hike, or exercise. Once you’re interested in something else, you’ll find the urges go away.
Talk it through. Talk to friends or family members about craving when it occurs. Talking can be very helpful in pinpointing the source of the craving. Also, talking about craving often helps to discharge and relieve the feeling and will help restore honesty in your relationship. Craving is nothing to feel bad about.
Challenge and change your thoughts. When experiencing a craving, many people have a tendency to remember only the positive effects of the drug and forget the negative consequences. Therefore, you may find it helpful to remind yourself that you really won’t feel better if you use and that you stand to lose a lot. Sometimes it is helpful to have these consequences listed on a small card that you keep with you.
Urge surf. Many people try to cope with their urges by toughing it out. But some cravings are too strong to ignore. When this happens, it can be useful to stay with the urge until it passes. This technique is called urge surfing. Imagine yourself as a surfer who will ride the wave of your drug craving, staying on top of it until it crests, breaks, and turns into less powerful, foamy surf. When you ride out the craving, without trying to battle, judge, or ignore it, you’ll see that it passes more quickly than you’d think.
The three basic steps of urge surfing:
- Notice how you’re experience the craving. Sit in a comfortable chair with your feet flat on the floor and your hands in a relaxed position. Take a few deep breaths and focus your attention on your body. Notice where in your body you experience the craving or urge and what the sensations feel like. Verbalize what you’re experiencing. For example, you could tell yourself: “My craving is in my mouth and nose and in my stomach.”
- Focus on one area where you’re experiencing the craving. What are the sensations in that area? Describe them to yourself. For example, perhaps you feel hot, cold, tingly, or numb? Maybe your muscles are tense? How large an area is involved? Notice if the sensations change as you focus on them. “My mouth feels dry. There is a numbness in my lips. When I swallow, I can imagine the feeling of using.”
- Repeat by focusing on each part of your body that experiences the urge. Describe to yourself how the sensations change, how the urge comes and goes. Many people notice that after a few minutes of urge surfing, their craving has disappeared. The purpose of this exercise, however, is not to make the urge go away but to experience it in a new way. If you regularly practice urge surfing, you’ll become more familiar with your cravings and find it easier to ride them out until they go away naturally.
You can support your drug treatment and protect yourself from relapse by having activities and interests that provide meaning to your life. It’s important to be involved in things that you enjoy, that make you feel needed, and add meaning to your life. When your life is filled with rewarding activities and a sense of purpose, your addiction will lose its appeal.
Pick up an old hobby or try a new one. Do things that challenge your creativity and spark your imagination—something you’ve always wanted to try. Learn a musical instrument, a foreign language, or try a new sport.
Adopt a pet. Yes, pets are a responsibility, but caring for an animal makes you feel loved and needed . Pets can also get you out of the house for exercise.
Spend time in nature. Take a scenic hike, go fishing or camping, or enjoy regular walks in a park.
Enjoy the arts . Visit a museum, go to a concert or a play, take an art class or write a memoir.
Get involved in your community. Replace your addiction with drug-free groups and activities. Volunteer , become active in your church or faith community, or join a local club or neighborhood group.
Set meaningful goals. Having goals to work toward and something to look forward to can be powerful antidotes to drug addiction. It doesn’t matter what the goals are, just that they are important to you.
Look after your health. Regular exercise , adequate sleep , and healthy eating habits help you keep your energy levels up and your stress levels down. The more you can stay healthy and feel good, the easier it will be to stay sober.
Don’t let relapse keep you down
Relapse is a common part of the recovery process from drug addiction. While relapse is frustrating and discouraging, it can be an opportunity to learn from your mistakes, identify additional triggers, and correct your treatment course.
What causes relapse?
Different “triggers” can put you at risk of relapsing into old patterns of substance use. While specific causes of relapse differ from person to person, some common triggers include:
- Negative emotional state (such as stress, sadness, anger, or trauma)
- Positive emotional state (feeling happy and wanting to feel even better, such as having a good time with friends)
- Physical discomfort (such as pain or withdrawal symptoms)
- Trying to test your personal control (“I can use just once” or “have just one pill”)
- Strong temptation or urge (craving to use)
- Conflict (such as an argument with your spouse or partner)
- Social pressure (being in a situation where it seems everyone else is using)
The important thing to remember is that relapse doesn’t mean drug treatment failure. Don’t give up. Call your sponsor, talk to your therapist, go to a meeting, or schedule an appointment with your doctor. When you’re sober again and out of danger, look at what triggered the relapse, what went wrong, and what you could have done differently. You can choose to get back on the path to recovery and use the experience to strengthen your commitment.
Support organizations
Most of these 12-step programs have worldwide chapters:
Narcotics Anonymous
Cocaine Anonymous
Crystal Meth Anonymous
Marijuana Anonymous
Read: NA and Other Peer Support Groups for Drug Addiction
Professional help for drug treatment and recovery
Use the Substance Abuse Treatment Facility Locator , call the SAMHSA helpline at 1-800-662-4357, Get One-on-One Help to Address Your Child’s Substance Use , or call the Partnership for Drug-Free Kids helpline at 1-855-378-4373.
Find NHS drug addictions support services or call the Frank helpline at 0800 776600.
Finding Quality Addiction Care (Canadian Centre on Substance Use and Addiction)
Find drug and alcohol services in your State/Territory (Department of Health & Aging).
More Information
- Step by Step Guides to Finding Treatment for Drug Use Disorders - Guides for adults, teens, or those helping someone addicted to drugs. (National Institute on Drug Abuse)
- Effective Treatments for Opioid Addiction - Medications used in the treatment of opioid addiction. (National Institute on Drug Abuse)
- What is Substance Abuse Treatment? A Booklet for Families - Learn about treatment options and what you can do. (SAMHSA)
- Principles of Drug Addiction Treatment - Effective treatment of substance abuse and addiction. (National Institute on Drug Abuse)
- How can prescription drug addiction be treated? - Treatment options for prescription drug addiction including addiction to opioid painkillers. (National Institute on Drug Abuse)
- Darkness Before Dawn - Collection of writings that offer guidance and perspective on depression from a HelpGuide affiliate . (Sounds True)
- Friedmann, P. D., Saitz, R., & Samet, J. H. (1998). Management of Adults Recovering From Alcohol or Other Drug ProblemsRelapse Prevention in Primary Care. JAMA, 279(15), 1227–1231. Link
- O’Brien, Charles P. “Evidence-Based Treatments of Addiction.” FOCUS 9, no. 1 (January 1, 2011): 107–17. Link
- Pettersen, H., Landheim, A., Skeie, I., Biong, S., Brodahl, M., Oute, J., & Davidson, L. (2019). How Social Relationships Influence Substance Use Disorder Recovery: A Collaborative Narrative Study. Substance Abuse: Research and Treatment, 13, 1178221819833379. Link
- Santucci, Karen. “Psychiatric Disease and Drug Abuse.” Current Opinion in Pediatrics 24, no. 2 (April 2012): 233–37. Link
- Kelly, Thomas M., and Dennis C. Daley. “Integrated Treatment of Substance Use and Psychiatric Disorders.” Social Work in Public Health 28, no. 3–4 (2013): 388–406. Link
- Magill, Molly, and Lara A. Ray. “Cognitive-Behavioral Treatment with Adult Alcohol and Illicit Drug Users: A Meta-Analysis of Randomized Controlled Trials.” Journal of Studies on Alcohol and Drugs 70, no. 4 (July 2009): 516–27. Link
- Grant, Bridget F., Frederick S. Stinson, Deborah A. Dawson, S. Patricia Chou, Mary C. Dufour, Wilson Compton, Roger P. Pickering, and Kenneth Kaplan. “Prevalence and Co-Occurrence of Substance Use Disorders and Independent Mood and Anxiety Disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions.” Archives of General Psychiatry 61, no. 8 (August 2004): 807–16. Link
- Substance-Related and Addictive Disorders. (2013). In Diagnostic and Statistical Manual of Mental Disorders . American Psychiatric Association. Link
- About the ASAM Criteria . (n.d.). Retrieved October 11, 2023, from Link
- ASAM – All Documents . (n.d.). Retrieved October 11, 2023, from Link
- Mutschler, C., Junaid, S., Tellez, C., Franco, G., Gryspeerdt, C., & Bushe, J. (2022). Community‐based residential treatment for alcohol and substance use problems: A realist review. Health & Social Care in the Community , 30 (2). Link
More in Addiction
The different options and what they offer

Choosing Drug Rehab and Addiction Treatment
A guide to drug addiction services

Coping with addiction and a mental health problem

A guide to alcohol addiction treatment services

Cutting down on alcohol doesn’t have to mean losing your social life

The health risks in young people and how to quit

The hidden risks of drinking

Binge Drinking
Help if you have trouble stopping drinking once you start

Professional therapy, done online
BetterHelp makes starting therapy easy. Take the assessment and get matched with a professional, licensed therapist.
Help us help others
Millions of readers rely on HelpGuide.org for free, evidence-based resources to understand and navigate mental health challenges. Please donate today to help us save, support, and change lives.

Breaking the Chains: A Journey of Drug Addiction Recovery
by Brooke Gilbertsen | Jan 19, 2024 | Detoxification process , Inpatient treatment , mental health , Outpatient treatment , Rehab for Depression , temp
The impact of drug addiction on society is far-reaching. It affects not only the individuals struggling with addiction but also their families, friends, and communities. Drug addiction can lead to increased crime rates, strained healthcare systems, lost productivity, and economic burdens. It also contributes to the spread of infectious diseases such as HIV/AIDS and hepatitis through needle sharing among intravenous drug users.
Addressing drug addiction is of utmost importance in order to mitigate its negative impact on individuals and society. By providing effective treatment and support services, we can help individuals overcome their addiction, improve their quality of life, and reduce the burden on society as a whole.
The Beginning: Exploring the root causes of drug addiction
Drug addiction does not occur in a vacuum; it is often influenced by a combination of genetic, environmental, and social factors. Understanding these root causes is crucial in order to develop effective prevention and treatment strategies.
Genetic factors play a significant role in determining an individual’s susceptibility to addiction. Research has shown that certain genetic variations can increase the risk of developing substance use disorders. However, genetics alone do not determine whether someone will become addicted to drugs. Environmental factors also play a crucial role.
Trauma and mental health issues are common underlying factors in drug addiction. Many individuals turn to drugs as a way to cope with past traumas or to self-medicate for mental health conditions such as depression or anxiety. These underlying issues need to be addressed in order for successful recovery to occur.
Peer pressure and social influences can also contribute to the development of drug addiction. Individuals who are surrounded by peers who engage in drug use are more likely to experiment with drugs themselves. Additionally, societal factors such as poverty, unemployment, and lack of access to education and healthcare can increase the risk of drug addiction.
The Struggle: Overcoming the challenges and obstacles of addiction recovery
Recovering from drug addiction is a challenging and often lifelong journey. There are many obstacles and challenges that individuals face along the way, making it important to provide comprehensive support and resources.
Withdrawal symptoms and cravings are common challenges during the early stages of recovery. When an individual stops using drugs, their body goes through a period of adjustment, which can result in physical and psychological symptoms. These symptoms can be intense and may lead to relapse if not properly managed.
Stigma and shame are also significant barriers to recovery. Society often views addiction as a moral failing or a lack of willpower, leading to judgment and discrimination against individuals struggling with addiction. This stigma can prevent individuals from seeking help and can make it difficult for them to reintegrate into society after treatment.
Fear of relapse is another challenge that individuals in recovery face. The fear of returning to old habits and losing progress can be overwhelming. It is important for individuals to develop coping strategies and a strong support system to help them navigate this fear and stay on track with their recovery.
Seeking Help: Navigating the different treatment options and resources available
There are various treatment options and resources available for individuals seeking help for drug addiction. It is important to find the right fit for each individual’s unique needs and circumstances.
Inpatient treatment programs provide intensive care in a residential setting. These programs typically involve detoxification, therapy, counseling, and support groups. They offer a structured environment where individuals can focus solely on their recovery without distractions or temptations.
Outpatient treatment programs are another option for individuals who do not require 24-hour care. These programs allow individuals to receive treatment while still living at home and attending work or school. Outpatient programs typically involve therapy, counseling, and support groups on a regular basis.
Therapy and counseling are essential components of addiction treatment. They help individuals explore the underlying causes of their addiction, develop coping strategies, and learn healthier ways of managing stress and emotions. Different types of therapy, such as cognitive-behavioral therapy (CBT) and motivational interviewing, may be used depending on the individual’s needs.
Support groups and peer networks can provide invaluable support and encouragement during the recovery process. Groups such as Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) offer a safe space for individuals to share their experiences, learn from others, and build a network of support.
Road to Recovery: Embracing a holistic approach to healing and wellness
Recovery from drug addiction is not just about abstaining from drug use; it is about embracing a holistic approach to healing and wellness. This involves addressing physical health, mental health, and spiritual and emotional well-being.
Physical health and nutrition play a crucial role in recovery. Substance abuse can take a toll on the body, leading to malnutrition, weakened immune system, and other health issues. Adopting a healthy lifestyle that includes regular exercise, nutritious meals, and adequate sleep can help individuals regain their physical well-being.
Mental health and self-care are equally important in the recovery process. Many individuals struggling with addiction also have co-occurring mental health disorders such as depression or anxiety. It is important to address these underlying issues through therapy, medication if necessary, and self-care practices such as mindfulness and relaxation techniques.
Spiritual and emotional well-being can provide individuals with a sense of purpose and meaning in life. This can be achieved through practices such as meditation, prayer, or engaging in activities that bring joy and fulfillment. Developing a strong support system of friends, family, and peers who understand and support the recovery journey is also crucial for emotional well-being.
Coping Strategies: Developing healthy habits and coping mechanisms to avoid relapse

Developing healthy habits and coping mechanisms is essential for individuals in recovery to avoid relapse and maintain their sobriety. There are various strategies that can be helpful in this process.
Mindfulness and meditation can help individuals develop awareness of their thoughts, emotions, and cravings without judgment. By practicing mindfulness, individuals can learn to observe their cravings without acting on them, allowing the cravings to pass without giving in to them.
Exercise and physical activity have been shown to be beneficial for individuals in recovery. Regular exercise not only improves physical health but also releases endorphins, which can boost mood and reduce cravings. Engaging in activities such as yoga, hiking, or team sports can also provide a sense of community and support.
Creative outlets and hobbies can provide individuals with a healthy way to express themselves and cope with stress. Engaging in activities such as painting, writing, playing music, or gardening can be therapeutic and help individuals find joy and fulfillment outside of drug use.
Rebuilding Relationships: Repairing damaged relationships with family, friends, and loved ones
Drug addiction often takes a toll on relationships with family, friends, and loved ones. Rebuilding these relationships is an important part of the recovery process.
Communication and honesty are key in repairing damaged relationships. It is important for individuals in recovery to be open and honest about their struggles, progress, and needs. This can help rebuild trust and foster understanding among family members and loved ones.
Making amends and seeking forgiveness is another important step in repairing relationships. Individuals in recovery may need to apologize for past actions or behaviors that have hurt their loved ones. This process can be difficult but is essential for healing and moving forward.
Setting boundaries is crucial for maintaining healthy relationships. Individuals in recovery need to establish clear boundaries with their loved ones, communicate their needs and limitations, and ensure that their own well-being is prioritized.
Finding Purpose: Rediscovering passions and goals for a fulfilling life in sobriety
Finding purpose and meaning in life is an important aspect of long-term recovery. Many individuals in addiction lose sight of their passions and goals as drugs take over their lives. Rediscovering these passions and setting new goals can provide individuals with a sense of direction and fulfillment.
Setting goals and aspirations can help individuals stay motivated and focused on their recovery journey. Whether it is pursuing education, starting a new career, or engaging in volunteer work, having goals gives individuals something to strive for and look forward to.
Pursuing education and career opportunities can provide individuals with a sense of purpose and financial stability. Many individuals in recovery may have put their education or career on hold due to their addiction. Going back to school or finding meaningful employment can be a transformative experience.
Giving back to the community is another way for individuals in recovery to find purpose and meaning. Engaging in volunteer work or advocacy can provide individuals with a sense of fulfillment and help them make a positive impact on others who may be struggling with addiction.
Staying Motivated: Maintaining a positive mindset and staying motivated throughout the recovery process
Maintaining a positive mindset and staying motivated throughout the recovery process is crucial for long-term success. There are several strategies that can help individuals stay motivated and focused on their sobriety.
Celebrating milestones and achievements along the way is important for maintaining motivation. Whether it is reaching a certain number of days sober, completing a treatment program, or achieving a personal goal, celebrating these milestones can provide individuals with a sense of accomplishment and reinforce their commitment to sobriety.
Surrounding oneself with positive influences is also important for staying motivated. This may involve distancing oneself from individuals who are still using drugs or engaging in negative behaviors and instead surrounding oneself with supportive friends, family, and peers who understand and support the recovery journey.
Practicing gratitude and mindfulness can help individuals maintain a positive mindset. By focusing on the present moment and expressing gratitude for the progress made, individuals can cultivate a sense of contentment and appreciation for their sobriety.
Celebrating the journey of breaking the chains of addiction and living a life of freedom and fulfillment.
Recovery from drug addiction is a challenging and lifelong journey, but it is also a journey of growth, healing, and transformation. By addressing the root causes of addiction, seeking help, embracing a holistic approach to healing, developing healthy coping strategies, rebuilding relationships, finding purpose, and staying motivated, individuals can break free from the chains of addiction and live a life of freedom and fulfillment.
It is important to remember that recovery is possible and that there is hope for a brighter future. For those still struggling with addiction, it is never too late to seek help and start the journey towards recovery. With the right support, resources, and determination, individuals can overcome addiction and build a life worth living.

Dr. Brooke Gilbertsen is a licensed clinical psychologist who has been working in the field of mental health since 2011 and specifically co-occurring disorders since 2013. Brooke brings her knowledge, experience, and compassion to support clients and their loved ones on their journey toward recovery, health, and holistic healing. Brooke has experience working with a wide range of diagnoses from severe mental illness and personality disorders to depression and anxiety, and believes the underlying cause must be treated in order for freedom from addiction to occur. Brooke treats the whole person, considering mental health diagnoses, genetics, neuropsychology, the context of the family and environment, social relationships, trauma and loss, vulnerability, shame, and self-worth. Brooke applies a wide range of evidenced-based modalities, incorporating mindfulness, spirituality, and psychodynamic approaches to assist clients in the healing process. Brooke is passionate about helping her patients discover the best version of themselves, with a renewed sense of freedom, purpose, and meaning. The model is to build a life that you want to show up to, and don’t need a vacation from.
Brooke completed her B.A. in Psychology in 2008 from San Diego State University. She obtained her M.A. Degree in Clinical Psychology in 2013 from Argosy University, and received her Doctorate in Psychology in 2016 from The Chicago School of Professional Psychology. She is the author of The Impact of Mindfulness on the Quality of Life of Cancer Patients, published in 2017. Brooke has been the keynote speaker for lectures on addiction, and is passionate about helping others find their way as they take the courageous journey toward self-growth.
- 1250 Alta Paseo, Burbank, CA 91501
- Aftercare Planning
- Verify Your Insurance
My Journey Through the Addiction Cycle
February 22, 2024
American Recovery Center

What is the Addiction Cycle?
What You'll Learn:
- A Personal Journey of Transformation
- The Realities of the Addiction Cycle
- Hope and Healing in Recovery
The road to recovery from addiction is often depicted as a linear path, but my experience was anything but straightforward. It was a journey marked by cycles of hope, despair, learning, and eventually, healing. This is the story of how I navigated the complex stages of the addiction cycle, a testament to the resilience of the human spirit in the face of seemingly insurmountable challenges.
Is There a Way Out of the Addiction Cycle?
Initially, I couldn’t even recognize the cycle I was caught in. My journey with substances started casually, with social drinks and occasional experimentation . However, what began as recreational use slowly morphed into dependency. The realization that I was stuck in a cycle of addiction came with a mix of shame and denial. Admitting I had a problem felt like admitting defeat, but it also opened the door to seeking help. It was a glimmer of hope in a situation that often felt hopeless.
What Does the Cycle of Addiction Look Like?
The cycle of addiction is a relentless whirlpool that pulls you deeper with every rotation. It started so subtly that I barely noticed the shift from occasional use to a constant need. The more I used, the more I needed to achieve the same effect, leading to increased tolerance and, eventually, physical and psychological dependence. This stage was marked by a profound sense of loss—loss of control, loss of self, and loss of connection with those I loved. Recognizing this pattern was the first step toward breaking the cycle, a step that required confronting the reality of my situation and the impact it had on my life and the lives of those around me.
How Do You Choose the Correct Cycle of Addiction to Break?
Choosing to break the cycle of addiction was one of the most daunting decisions I ever made. It meant dismantling the very thing I had come to rely on as a crutch for my emotional and psychological pain. This choice wasn't just about stopping substance use; it was about confronting and healing from the underlying issues that led me to addiction in the first place. It required a commitment to a process of deep, often painful self-reflection and change, supported by professional help and the solidarity of others who had walked this path before me.
Can Breaking the Cycle of Addiction Truly Lead to Freedom?
Breaking free from the cycle of addiction opened up a new world of possibilities. It was a journey marked by small victories and significant setbacks, a testament to the non-linear nature of recovery. Each relapse, rather than being seen as a failure, became an opportunity to learn and grow stronger. Support from therapists, recovery groups, and loved ones played an integral role in this process, providing me with the strength to continue fighting even when the path ahead seemed insurmountable. Recovery brought a newfound sense of freedom and the realization that I was no longer defined by my addiction but by my resilience and capacity to change.
What Are the Stages of the Addiction Cycle?
Navigating through the stages of the addiction cycle was like navigating through a storm. There were moments of calm, followed by turbulent waves that threatened to pull me under. Understanding these stages helped me to anticipate and manage the challenges that came with each phase of recovery. It was a process of learning to recognize the triggers and patterns that led to substance use, developing healthier coping mechanisms, and rebuilding a life that wasn't centered around addiction. This knowledge was empowering, providing a blueprint for recovery that was tailored to my unique journey.
How Can We Support Others Through the Cycle of Drug Addiction?
Supporting others by understanding their addiction became an unexpected source of strength and healing. Sharing my experiences and the lessons I learned along the way helped to create a sense of community and mutual support that was invaluable. It reminded me that recovery is not a journey that should be undertaken alone but a shared experience that benefits from the collective wisdom and support of others. This act of giving back not only helped others but also played a crucial role in reinforcing my own recovery.
If you or someone you love is struggling with addiction, know that there is hope. The journey through the stages of the addiction cycle is challenging, but it is also filled with opportunities for growth, healing, and transformation. Reaching out for help is the first step toward breaking free from the cycle of addiction and rediscovering the joy of living a life unencumbered by substances.
Don't hesitate to reach out to American Recovery Center at 866-484-2502 . Together, we can embark on this journey towards a brighter, healthier future.
Guiding You Towards a Brighter Tomorrow
Quick Links
- Our Programs
Other Pages
- Privacy Policy
Office Location
- 1250 Alta Paseo Burbank, CA 91501
- (866) 484-2502
- [email protected]

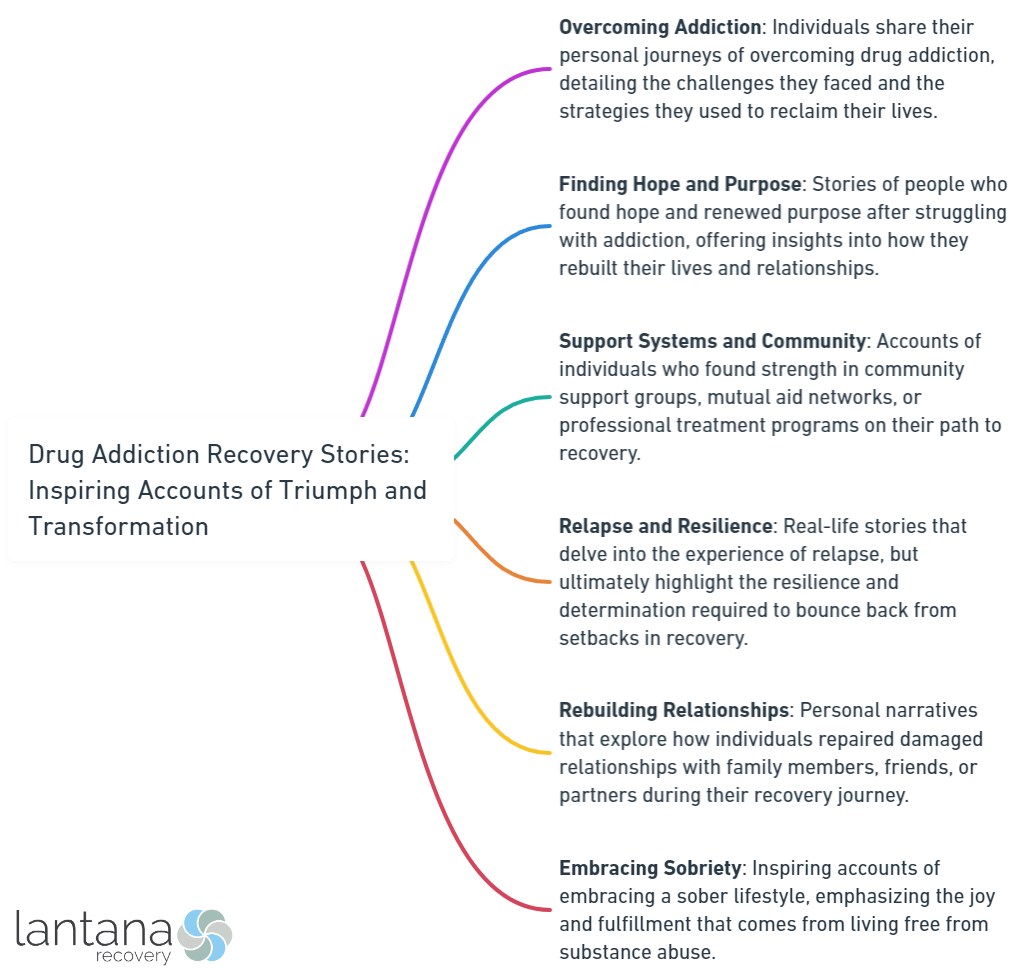
Overview of Addiction Recovery Stories
An overview of addiction recovery stories via the stages of the change model of addiction provides valuable insights and inspiration for individuals seeking recovery from drug addiction. Here are key points to consider:
- Inspiration: Addiction recovery stories inspire and motivate individuals struggling with addiction. These stories showcase the resilience and courage of those who have overcome their addiction, offering hope for others in similar situations.
- Personal growth: Addiction recovery stories highlight the journey of personal growth and transformation experienced by individuals on the path to recovery. These stories demonstrate the power of self-reflection, determination, and the ability to change one’s life.
- Sharing experiences: Addiction recovery stories allow individuals to share their experiences and provide support to others. They create a sense of community and foster understanding by connecting those in recovery and showing they are not alone in their struggles.
- Promoting understanding: Addiction recovery stories challenge and break the stigma surrounding addiction. They offer a societal perspective on the complexities of addiction, promoting empathy, compassion, and a more inclusive approach to recovery.
By understanding the overview of addiction recovery stories, individuals gain valuable insights, find inspiration, and feel supported on their journey to recovery.
Inspiring Accounts of Triumph and Transformation
Get ready to be inspired as we dive into the captivating world of triumph and transformation . In this section, we’ll delve into the mesmerizing personal stories of individuals who have conquered their battles with addiction . Brace yourself for tales of resilience , courage , and redemption as these brave individuals share their journeys of overcoming addiction. Get ready to be moved, uplifted, and amazed by their incredible stories of transformation. This is a section you won’t want to miss!
Personal Stories of Overcoming Addiction
Personal stories of overcoming addiction are incredibly impactful and inspiring. They serve as a testament to the remarkable resilience and unwavering determination of individuals who have triumphed over addiction. When reflecting on these narratives, it is crucial to consider a few significant factors.
- Inspiring stories: These personal accounts offer a beacon of hope and inspiration to those currently grappling with addiction. They serve as living proof that recovery is not only attainable but within reach for all.
- Courageous individuals: The individuals who bravely share their personal stories demonstrate immense courage and strength . By exposing their vulnerability, they provide solace to others who may be feeling isolated in their own arduous journeys.
- Personal growth: Those who have successfully conquered addiction underscore the incredible personal growth they have undergone. They candidly discuss the valuable lessons learned, the daunting obstacles confronted, and the transformative positive changes experienced.
- Fostering connections: These personal narratives establish meaningful connections among individuals who have shared similar experiences. By offering solace and support, they serve as a catalyst for seeking assistance and embarking on the path to recovery.
By immersing ourselves in these narratives, we gain valuable insights, encouragement, and the necessary drive for our own recovery endeavors. They serve as a poignant reminder that with unwavering commitment , unwavering support , and unwavering belief in oneself , overcoming addiction and embracing a fulfilling, sober life is entirely attainable.
Pro-tip: Consider joining support groups or online communities to discover a plethora of personal stories recounting the triumph over addiction. Hearing from a diverse range of individuals will provide you with a broader perspective and unwavering support throughout your own recovery journey.

Why Are Drug Addiction Recovery Stories Important?
Drug addiction recovery stories hold tremendous significance in society. They serve as powerful reminders of the triumphs and transformations that individuals can achieve in their battle against addiction. In this section, we will delve into the importance of these stories, focusing on two impactful aspects. Firstly, we will explore how drug addiction recovery stories help in breaking the stigma surrounding addiction . Secondly, we will discuss how these stories provide a much-needed source of hope and inspiration to those on their own recovery journey. Let’s dive into these compelling narratives of strength and resilience .
Breaking the Stigma Around Addiction
Breaking the Stigma Around Addiction is crucial in addressing the challenges faced by individuals struggling with addiction. Challenging societal perspectives and promoting understanding and compassion for those affected are important. Addiction recovery stories offer unique insight into the experiences of individuals who have overcome addiction, inspiring hope and transformation. These stories highlight the transformative effects of recovery and renew motivation for those who may be struggling.
By sharing personal experiences, addiction recovery stories help humanize addiction and shift the focus from judgment to empathy. They showcase the courage and strength of individuals who have faced the challenges of addiction and emerged victorious. Through their stories, they demonstrate that recovery is possible and that individuals should not be defined by their addiction.
Breaking the stigma around addiction also involves challenging misconceptions and stereotypes about addiction. Addiction recovery stories create opportunities for open and honest conversations by providing a platform for individuals to share their stories. They help educate the public about the complexities of addiction and the journey of recovery.
Providing Hope and Inspiration
Drug addiction recovery stories serve as a source of hope and inspiration for those who are struggling with addiction. These stories not only demonstrate that recovery is achievable, but they also shed light on the possibility of overcoming addiction. By hearing these stories, individuals are motivated to seek assistance and implement positive changes in their lives.
Throughout the recovery journey, it is common to encounter setbacks and experience doubt. However, stories of triumph and transformation act as a vital source of renewed motivation, reminding individuals of their inner strength and resilience .
Moreover, drug addiction recovery stories play a significant role in fostering understanding and empathy , as they help to dismantle the negative perception surrounding addiction. Through the sharing of personal experiences, these stories prompt society to perceive addiction as a treatable condition rather than a moral failing.

Common Themes in Drug Addiction Recovery Stories
Drug addiction recovery stories are a powerful testament to the resilience and strength of the human spirit as you work with leading experts like Greenville’s Lantana Recovery . In this section, we will explore the common themes that emerge from these compelling narratives. From the gripping rock bottom moments to the transformative turning points, and the importance of support and community , we will delve into the essential elements that pave the way for triumph and transformation in the face of addiction. Get ready to be inspired by the shared experiences and remarkable journeys of individuals who have reclaimed their lives.
Rock Bottom Moments
Rock bottom moments are crucial in overcoming drug addiction. These Rock Bottom Moments represent the lowest point in someone’s struggle with substance abuse and often involve intense despair, loss, and self-destruction. During these Rock Bottom Moments , individuals may realize the negative effects of addiction and become motivated to seek help and change.
Rock Bottom Moments can include setbacks and relapses, illustrating the cyclical nature of addiction. Severity can vary depending on factors like substance use, personal circumstances, and support systems. These Rock Bottom Moments can serve as wake-up calls, inspiring individuals to seek treatment and embrace recovery.
Though challenging, Rock Bottom Moments also offer opportunities for growth and transformation. They allow individuals to reflect on their choices, face the consequences of addiction, and commit to turning their lives around. These Rock Bottom Moments can mark a turning point toward sobriety, healing, and personal development.
Support from loved ones, support systems, and support group meetings plays a crucial role in navigating Rock Bottom Moments and maintaining recovery. These networks provide a safe space to share experiences and offer guidance, helping individuals rebuild their lives, develop healthy coping mechanisms, and build resilience.
Rock Bottom Moments are not the end, but rather a starting point to reclaim lives from addiction’s clutches. With commitment, perseverance, and the right support, individuals can rise from their lowest point, embrace sobriety, and build a future filled with hope, purpose, and fulfillment.
The Turning Point
The turning point in drug addiction recovery is a pivotal moment that brings about transformation , leading individuals to heal and recover. It occurs when individuals realize the destructive nature of their addiction and decide to make a change. This turning point can stem from hitting rock bottom , experiencing setbacks and relapses , or witnessing the consequences of their actions.
During the turning point, individuals undergo a transformative experience that goes beyond physical healing . It involves a spiritual and emotional journey where individuals confront the underlying issues contributing to their addiction. It is a profound self-realization that prompts them to seek support and make necessary changes.
One inspiring example of a turning point is John’s story. He struggled with substance abuse for years until a life-altering event made him realize he had hit rock bottom. With the support of a rehabilitation program, John embarked on a spiritual and emotional journey of self-discovery. Through therapy, counseling, and the guidance of peers, he was able to heal from his addiction and rebuild his life.
The turning point in drug addiction recovery serves as hope for others facing similar struggles. By sharing these stories, we promote understanding , inspire change, and provide renewed motivation for those seeking recovery. These stories encourage individuals to take the crucial step towards healing and empower them to overcome challenges on their journey.
Support and Community
Support and community are crucial in drug addiction recovery. Here are key aspects to consider:
- Support systems: A strong support system is essential in the recovery journey. This includes family members, friends, support group meetings, and organizations dedicated to helping individuals overcome addiction.
- Support network: Surrounding yourself with individuals who understand and empathize with your struggles provides emotional support and guidance. Connecting with others who have similar experiences can be comforting and inspiring.
- Peer support groups: Joining groups offer a safe space to share experiences, gain insights from those with long-term sobriety, and cultivate a sense of belonging. This may also include seeking support from family, church, friends, work, school, and self-help organizations like Alcoholics Anonymous and Narcotics Anonymous to aid in their recovery according to Judith Grant’s study, Rural women’s stories of recovery from addiction .
- Accountability partners: Having someone who holds you accountable for your actions and progress in recovery is helpful. An accountability partner offers encouragement, keeps you focused on goals, and provides guidance during challenging times.
- Therapeutic communities: Residential treatment centers and therapeutic communities offer a supportive environment where individuals can interact with peers who understand their struggles. These communities provide therapeutic activities and resources to enhance recovery.
By fostering strong support and community connections, individuals in recovery can find the encouragement, understanding, and guidance needed to overcome addiction and live fulfilling lives. Remember that each person’s journey is unique, and finding the right support system may take time, but it is worth the effort.

Transformations and Lessons Learned
Transformations and Lessons Learned – Hear inspiring recovery stories from individuals who have triumphed over drug addiction. Discover how they rebuilt relationships, found self-worth and purpose, and embraced sobriety. These powerful accounts of transformation will inspire and motivate you in your own journey toward recovery.
Rebuilding Relationships
Rebuilding relationships is crucial for individuals recovering from drug addiction. It involves restoring and strengthening connections with loved ones, repairing trust, and building a healthy support network.
- Healing past wounds: Rebuilding relationships requires addressing past conflicts with open communication, acknowledging mistakes, and working towards forgiveness and understanding.
- Building healthy boundaries: Setting clear boundaries is essential for maintaining healthy relationships. Individuals in recovery need boundaries that support their sobriety and well-being while respecting others’ needs.
- Developing healthy communication skills: Effective communication is vital for rebuilding relationships. Learning to express emotions and concerns respectfully can help rebuild trust and foster deeper connections.
- Attending family therapy or support groups: These resources provide a safe space for open dialogue, education, and guidance in rebuilding relationships. Strategies for improved communication, understanding addiction, and rebuilding trust are offered.
- Making amends: Taking responsibility, apologizing for harm caused, showing genuine remorse, committing to change, and making reparations when appropriate are essential steps in the recovery process.
Rebuilding relationships takes time and effort but is crucial for ongoing sobriety and overall well-being. Actively working on repairing connections allows individuals in recovery to cultivate a strong support system.
In my own experience, rebuilding relationships has been transformative. Through therapy and support groups, I learned communication skills, set boundaries, followed journal prompts for addiction recovery , took responsibility for my past actions, and committed to sobriety. This has allowed me to rebuild trust, strengthen relationships, and cultivate a supportive network. Rebuilding relationships has improved my personal life and contributed significantly to my overall well-being and ongoing sobriety.
Discovering Self-Worth and Purpose
Discovering self-worth and purpose is crucial for drug addiction recovery. It is essential for individuals to rediscover themselves and find meaning and direction in their lives.
Throughout the recovery process, personal growth and transformation occur. Individuals learn to celebrate their strengths and recognize their value. Discovering self-worth helps individuals develop a positive self-image and cultivate self-esteem and confidence .
Having a purpose is equally important. It provides individuals with a reason to continue their recovery journey and inspires positive changes. Finding purpose involves identifying new goals, pursuing passions, and contributing to communities. It allows individuals to create a new identity beyond addiction and establish a fulfilling life.
Therapy and counseling can greatly benefit individuals in recovery. Through therapy, they can explore their values, beliefs, and desires, which help them uncover their true passions and align their actions with their values. This further enhances their sense of self-worth and purpose .
By discovering self-worth and purpose , individuals in recovery gain hope and motivation. This newfound self-worth serves as a strong foundation for their ongoing journey of sobriety, empowering them to live a fulfilling life without addiction.
Embracing Sobriety
When recovering from drug addiction, embracing sobriety is crucial. It involves committing to a life free from addiction and actively maintaining sobriety. It begins with acknowledging the need for change and making a conscious decision to break free. It requires determination to overcome challenges and develop effective recovery strategies. Embracing sobriety is an ongoing journey that requires perseverance.
During recovery, individuals may encounter temptations and triggers that can lead to relapse. To avoid pitfalls, cultivating strong support systems and surrounding oneself with supportive people is crucial. Attending support group meetings and seeking professional help from leading rehab centers can greatly enhance the chances of maintaining sobriety.
Embracing sobriety also involves adopting new coping mechanisms and healthy lifestyle habits. This may include implementing stress-management techniques, engaging in regular exercise, and practicing self-care. Therapy or counseling from Lantana may also be beneficial for addressing the emotional and psychological aspects of addiction.

How Can Drug Addiction Recovery Stories Help Others?
Recovering from drug addiction can be a daunting journey, but the power of storytelling can offer hope , inspiration , and practical guidance . In this section, we’ll explore how drug addiction recovery stories have the potential to help others. From offering valuable guidance and practical tips to encouraging those seeking recovery, and providing much-needed support for loved ones, these stories embody the triumph and transformation that is possible. Get ready to be inspired by the transformative impact of these narratives on the path to recovery.
Offering Guidance and Practical Tips
When providing guidance and practical tips for drug addiction recovery, it is crucial to consider several strategies:
- Explore treatment options: Research and understand the available treatment options for drug addiction recovery. This includes inpatient and outpatient programs, counseling, therapy, and support groups.
- Develop effective recovery strategies: Personalize your strategies for recovery. Set short-term and long-term goals, practice self-care, and find healthy coping mechanisms.
- Utilize therapeutic benefits: Therapy, including individual counseling, group therapy, and alternative therapies like art or music therapy, can provide valuable support.
- Build a strong support network: Surround yourself with a supportive network of family, friends, and fellow individuals in recovery. Attend support group meetings, share experiences, and lean on others for guidance.
- Focus on relapse prevention: Develop strategies to prevent relapse. This may involve avoiding triggers, finding healthy outlets for stress, and creating a relapse prevention plan with your support network. “The goal of treatment is to help individuals recognize the early warning signs of relapse and to develop coping skills to prevent relapse early in the process, when the chances of success are greatest. This has been shown to significantly reduce the risk of relapse” ( Relapse Prevention and the Five Rules of Recovery , Melemis, 2015.)
By following these guidance and practical tips, individuals in drug addiction recovery can increase their chances of success and maintain a healthy, fulfilling life in sobriety.
Encouraging Seekers of Recovery
When it comes to encouraging seekers of recovery, drug addiction recovery stories play a significant role. These stories inspire and motivate individuals on the path to overcoming addiction. Here are some ways in which drug addiction recovery stories provide encouragement:
- Instilling hope: Recovery stories showcase real-life examples of individuals who have successfully overcome addiction, demonstrating that recovery is possible and positive change is attainable.
- Offering guidance: Recovery stories provide personal insights and practical tips valuable to those seeking recovery. They offer guidance on treatment options, effective recovery strategies, and the transformative benefits of therapy.
- Connecting seekers with resources: Recovery stories direct seekers to addiction recovery resources such as support groups, treatment centers, and counseling services. These resources provide necessary support and guidance during the recovery journey.
- Promoting change and seeking treatment: Recovery stories encourage individuals struggling with addiction to seek treatment and support. They inspire seekers to take the first steps toward their own recovery by sharing stories of successful addiction recovery.
- Fostering understanding: Recovery stories break down the stigma surrounding addiction by promoting understanding. They showcase the challenges faced by individuals with addiction and highlight the importance of support and compassion in the recovery process.
In summary, drug addiction recovery stories are a powerful tool in encouraging seekers of recovery. They provide hope, guidance, and resources, and promote understanding, ultimately inspiring individuals to take the necessary steps toward their own recovery journey.
Providing Support for Loved Ones of Those in Recovery
When supporting loved ones in recovery, keep these considerations in mind:
- Stay informed : Educate yourself about addiction and the recovery process. Understanding the challenges and stages of recovery helps offer better support .
- Maintain open communication : Listen without judgment and encourage the expression of feelings and concerns.
- Be patient : Recovery is a journey that takes time. Offer support and encouragement during difficult times .
- Establish healthy boundaries : Set limits and communicate your own needs and limitations.
- Encourage self-care : Remind loved ones to prioritize their well-being and seek professional help if needed as studies like Mapping the recovery stories and drinkers and drug users in Glasgow by Best et al., have found that better functioning and quality of life were linked to increased involvement in meaningful activities, followed by the number of peers in recovery within the social network.
- Offer practical assistance : Provide rides to support group meetings, help with household chores, or aid in finding job opportunities.
Remember, supporting loved ones in recovery is crucial. By offering understanding, empathy, and practical assistance, you play a significant role in their ongoing recovery process.
Frequently Asked Questions
What are addiction recovery stories.
Addiction recovery stories are personal accounts of individuals who have struggled with drug or alcohol addiction and have successfully overcome their addiction. These stories highlight the challenges, setbacks, and triumphs of the recovery journey, offering hope and inspiration to others who may be struggling with substance abuse.
How do addiction recovery stories inspire change?
Addiction recovery stories inspire change by showcasing the possibility of healing and happiness after addiction. These stories provide hope to individuals who may feel trapped in their addiction, showing them that recovery is attainable. By sharing their experiences and insights, those who have overcome addiction encourage others to seek help, develop healthy coping strategies, and embark on their own journey of recovery.
Where can I find addiction recovery stories?
There are various online platforms where you can find addiction recovery stories. Social media communities, blogs, podcasts, and websites dedicated to addiction recovery often feature personal accounts of triumph and transformation. These platforms provide a space for individuals to share their recovery journeys, offering support, inspiration, and a sense of community.
What lessons can be learned from addiction recovery stories?
Addiction recovery stories teach important life lessons. They highlight the significance of self-reflection and accountability in the recovery process. These stories emphasize the value of finding support and treatment, as well as developing healthy life skills and coping mechanisms. They also underscore the role of building a support network and embracing spirituality in maintaining sobriety.
How can addiction recovery stories promote emotional healing?
Sharing personal addiction recovery stories can promote emotional healing in multiple ways. For those who have struggled with addiction, sharing their story can be a therapeutic experience, allowing them to reflect on their journey and find closure. For others, reading or hearing these stories can provide a sense of hope, validation, and connection, and help in their own healing process.
How can I give back and help others through addiction recovery stories?
If you have overcome addiction and want to give back and help others, sharing your recovery story is a meaningful way to inspire and support others. You can use online platforms such as social media, blogs, podcasts, or local support groups to share your story. By offering your experiences, insights, and advice, you can provide hope, encouragement, and guidance to those who are still struggling.

Warren Phillips
Warren is a Licensed Master Social Worker, who specializes in substance abuse and mental health treatment. Clinically, Warren has developed a therapeutic skillset that utilizes a strengths-based perspective, Twelve Step philosophies, Cognitive Behavioral Therapy and Motivational Interviewing.

What to Do When Both You and Your Spouse Struggle With Addiction
The Sober Travel Destinations Index

“Bubble Recovery”: What Is It and What Are Its Recovery Limitations?

Recovering From Addiction and an Active Eating Disorder

Better Understanding Recovery Center Relapse Policies

Gambling, Shopping, Sex: Better Understanding Process Addiction Recovery

Contact Information
Main Number: 866-997-2870 [email protected] Monday to Friday, 9am – 5pm
Lantana Recovery Rehab
65 Gadsden St Charleston, SC 29401 (843) 281-7964
Lantana Recovery
143 West St, Suite V New Milford CT 06776 (860) 507-9258

Subscribe to Our Newsletter
Blog | Sitemap | Privacy Policy
- First Name (Required)
- Last Name (Required)
- Email (Required)
- Phone (Required)
- Insurance Company Aetna All Savers Anthem BlueCross BlueShield Bright HealthCare First Health Network Golden Rule Humana Magellan Healthcare Molina Healthcare Medcost Optum Tricare United Healthcare Other
- Insurance Company Name
- Questions/Comments
- Phone This field is for validation purposes and should be left unchanged.
- Email This field is for validation purposes and should be left unchanged.
Chat with us.
Reach out now and join our supportive community.
- Name This field is for validation purposes and should be left unchanged.

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Pharmacy (Basel)
- PMC10037586

Community-Centered Patient Journey Map in Opioid Use Disorder: A Tool to Address Compassion Fatigue among Community Pharmacists
Kenneth charles hohmeier.
1 Department of Clinical Pharmacy and Translational Science, College of Pharmacy, University of Tennessee Health Science Center, Nashville, TN 37211, USA
Alina Cernasev
Christina leibold, todd m. moore.
2 Department of Psychology, University of Tennessee, Knoxville, TN 37996, USA
Erica Schlesinger
3 Tennessee Department of Mental Health & Substance Abuse Services, Nashville, TN 37243, USA
Gerald Cochran
4 Division of Epidemiology, University of Utah, Salt Lake City, UT 84112, USA
Ileana Arce
Wesley geminn, marie chisholm-burns.
5 Office of the Provost, Oregon Health & Science University, Portland, OR 97239, USA
Associated Data
Not applicable.
Community pharmacists have become increasingly exposed to opioid use disorders in recent decades. However, both pharmacist training and traditional practice environments have not been adequate to prepare the pharmacist for both the patient care needs and regulatory barriers of patients experiencing opioid use disorders (OUD). As a result, there is a need to increase pharmacists’ awareness of both the overall patient experience as they navigate their OUD and the role of the community pharmacy as a touchpoint within that experience. To this end, a Community-Centered Patient Journey in Drug Addiction Treatment journey map was developed with expert insights, clinical experience, and in-depth interviews (conducted in spring of 2021) with 16 participants enrolled in licensed opioid treatment programs in Tennessee. Patients, policymakers, clinicians, and academic researchers were involved in the map development. Lived experiences of key informants were captured via in-depth interviews. A consensus decision-making approach was used throughout the patient journey map development process. The final patient journey map illustrates a non-linear pathway, describes the central role of the patient’s community, and emphasizes three major “pain points” within the system (access, adherence, and affordability). Future research should investigate the impact of such a journey map on pharmacy personnel’s knowledge, attitudes, and behaviors.
1. Introduction
Opioid use disorder (OUD) is widespread across the United States, with approximately two million Americans affected [ 1 , 2 , 3 ]. Consequently, opioid overdose deaths have continued to rise over the past three decades, with just over 80,000 deaths in 2021 [ 4 ]. One contributor to the growth in both OUD and opioid overdose deaths has been the increase in prescription opioids dispensed. From 1997 to 2007, there was an 866% increase in oxycodone sales and a 280% increase in hydrocodone sales in U.S. community pharmacies [ 5 ]. In 2020 alone, 142 million prescription opioids were dispensed, at a rate of 43.3 prescription opioids per person [ 6 ]. Approximately 14% of patients misuse prescription opioid medications, although this ranges depending on population between 5 and 25% [ 7 , 8 , 9 ]. This is concerning, as 4–6% of those who misuse prescription opioids move onto heroin, and approximately 80% of those who use heroin had previously misused prescription opioids [ 10 , 11 , 12 ]. Moreover, it is estimated that about one in four who use heroin develop OUD [ 13 ].
Community pharmacists have increasingly become exposed to OUD given these trends in opioid dispensing [ 14 , 15 ], yet their traditional role, experience, training, and education may ill-prepare them for the current practice demands of balancing OUD patient care and regulatory responsibilities. Moreover, given the role prescription opioids play in opioid use disorder, addiction, and overdose, the community pharmacy represents a critical touchpoint for positively impacting opioid-related morbidity and mortality. This is further emphasized by community pharmacies’ accessibility, with approximately 95% of Americans living within 5 miles of a community pharmacy [ 16 ]. For instance, if community pharmacies were used as an opioid treatment program site for pharmacy-based methadone dispensing, drive time to treatment would be reduced by as much as 75% [ 17 ]. For this reason, it has been suggested that community pharmacies should be further leveraged in the prevention, surveillance, and treatment of OUD [ 18 ]. Emerging evidence suggests that patients and physicians desire greater pharmacist involvement in OUD care. In a recent study investigating a collaborative care model between physicians and pharmacists in which buprenorphine care was managed by a community pharmacist, patients maintained high retention and adherence rates, with 90% of patients endorsing the model as very satisfactory [ 19 ]. In this latter example, the community pharmacist managed both follow-up buprenorphine care management and monthly buprenorphine dispensing responsibilities after initial screening, and assessment was performed by the overseeing physician [ 19 ].
Pharmacists also desire more responsibility in opioid-related care of their patients [ 20 , 21 ]. In the U.S., engaging pharmacists in treatment has been limited, as pharmacists have been placed in a position of regulatory enforcement of opioid use, while at the same time are professionally obligated to maintain a patient care advocate role [ 21 ]. Despite their professional obligation to patient care, pharmacists have been primarily charged by both the U.S. Drug Enforcement Agency and each state’s Board of Pharmacy to verify each opioid prescription is used for a legitimate reason and monitor for diversion, and to prove this routinely through stringent application of opioid-related regulations—leading to a clearly articulated regulatory role for pharmacists in delaying or denying opioid prescriptions [ 19 ]. However, pharmacists in the U.S. have indicated their desire to intervene to reduce high-risk opioid use behaviors, but complain that the lack of clear regulatory or clinical guidelines in the U.S. have relegated their opioid-related scope of practice solely to opioid regulation enforcement [ 20 ]. These opposing roles have led to reported “compassion fatigue” among frontline community pharmacy personnel in caring for these patients [ 21 , 22 ]. Pharmacists experiencing compassion fatigue may experience increasing frustration with patients, leading to negative emotional responses and decreased job satisfaction [ 23 ]. It is likely that the negative experiences with community pharmacists seen by some patients engaging in OUD treatment are due to this compassion fatigue [ 24 ]. For this reason, compassion fatigue may serve as a substantial, though latent, barrier to the community pharmacy’s engagement in care for patients with OUD.
One evidence-based solution to compassion fatigue is education [ 23 ]. Specifically, narrative messages that describe the patient’s experience and overall healthcare journey have been shown to reduce stigma and create a more holistic picture of the patient’s experience with OUD [ 25 ]. Narrative messages involve both emphasizing the external factors which play a role in the patient’s health status, and acknowledging personal responsibility in making healthy choices. Research suggests that a more comprehensive understanding of the patient’s experience “…can influence attitudes, behavioral intentions, causal attributions, and support for policy responses to health issues” [ 25 , 26 ]. Unlike physicians, nurses, and counselors who have the ability to screen and intervene on patients with OUD throughout their care continuum, community pharmacists experience a fragmented view of the patient’s journey, which centers primarily on pre-OUD diagnosis and treatment. Moreover, because of their physical separation from OUD treatment providers, inability to legally dispense certain medications for OUD, and regulatory responsibilities to police potential risky opioid use behaviors, community pharmacists are unlikely within their practice environment to fully experience this “comprehensive understanding of the patient’s experience” which is requisite to influence their attitudes, behaviors, and downstream experience of compassion fatigue.
Core to understanding the patient experience is connecting the patient’s journey in seeking and receiving care between interactions with the healthcare system—something referred to as “touchpoints” [ 27 ]. This can be an important link between what providers, such as pharmacists, “see” when they interact with the patient and the more complete view of the patient, including feelings, emotions, motivations, and attitudes as they live their lives with a chronic health condition [ 27 ]. A patient journey map is a formal exercise used to understand the patient’s journey with a specific healthcare condition from the patient’s perspective, typically for the purposes of improving the patient’s experience [ 28 ]. Patient journey mapping in OUD may allow stakeholders, such as pharmacists, to better understand the overall patient’s experience of the treatment cascade beyond the patient–provider interaction in a healthcare setting.
The objective of this project was to develop a patient journey map of OUD within the community pharmacy setting to serve as a future educational tool for pharmacists to better support patients with OUD.
2. Materials and Methods
2.1. creation of the patient journey map.
A comprehensive approach to developing the patient journey map was employed using elements from Trebble et al., 2010, and McCarthy et al., 2016 [ 26 , 29 ]. In-depth key informant interviews with participants undergoing medication for opioid use disorder (MOUD) care were conducted across Tennessee. Interviews were audio-recorded, transcribed, and analyzed using thematic analysis. Thematic analysis includes the development of codes (e.g., words, phrases, or sentences) to represent patterns of meaning within qualitative data [ 30 ]. After analyzing the approximately 20 h of key informant interviews, all codes were extracted and further analyzed to develop the patient journey map.
To develop the map itself, we first created three separate visualizations: (1) a concentric grid with actors within a system, (2) a mind map of actors and their interdependencies ( Figure 1 ), and (3) a perpendicular-axis grid representing the components of each phase of the pathway ( Figure 2 ). These visualizations allowed the research team to see the patients’ journey from three distinct vantage points. Then, the team worked collaboratively to populate and review each visualization, and a consensus was reached on each element before proceeding to the next element.

Mind Map of Actors and Their Interdependencies of the Patient Journey in Opioid Use Disorder Treatment.

Sample Draft of the Perpendicular Axis Grid of the Patient Journey in Opioid Use Disorder Treatme. ACE = Adverse childhood experiences; ED = Emergency department; MOUD = Medication for opioid use disorder.
The concentric grid was developed with the patient in the center, followed by their community, defined as the area where they live, work, and interact with their primary social system, and then finally, an outer area representing actors external to the patient’s community. Our aim was to define and visualize touchpoints and their proximity to the patient. Next, a mind map of those actors and their interdependencies was created to understand moderators and mediators within the system. Lastly, a perpendicular axis grid was created. Here, we developed a grid with an x -axis representing each of the traditional six phases of the patient journey, based on Trebble and McCarthy [ 26 , 29 ]: (1) Trigger Event/Awareness, (2) Help, (3) Care, (4) Treatment, (5) Behavioral/Lifestyle Change, and (6) Ongoing Care/Proactive Health. The y -axis included: (1) Touchpoints, (2) Moments of Truth, (3) Emotions, (4) Quotes, and (5) Pain Points.
The “Trigger Event” (or Awareness) phase during a patient’s journey is the point at which the patient becomes conscious of the need to seek medical help. During the subsequent stage, “Help,” the patient begins the process of identifying means to access treatment—either through peer or healthcare professional facilitation. Next, the patient receives “Care” through formal interaction with the healthcare system and healthcare workers, which is subsequently followed by “Treatment”, where a formal assessment and treatment plan are outlined by a medical professional. The “Behavior Change” phase follows since there is always a need for the patient to alter their lifestyle or behaviors beyond remaining adherent to prescription drug treatment. Finally, “Ongoing Care” involves the patient remaining in treatment chronically to manage their OUD.
At each phase of the patient’s journey, the patient has a range of experiences, emotions, and interactions which can be captured and mapped against each of the journey phases. A “Touchpoint” is the moment when the patient interacts directly with the healthcare system. “Moments of Truth” are gaps between the desired patient experience and the actual one. Before, during, and after interaction with the healthcare system, the patient will experience a range of “Emotions” related to their OUD, and these can often be captured simply by one or two words (e.g., concerned, mistrusting). Finally, what a patient states upon interview or survey can often “sum up” a journey phase with a few “Quotes.” Lastly, “Pain Points” are areas where patients encounter specific barriers or negative experiences related to their care.
2.2. Research Team
The patient journey mapping team included university researchers, state health officials, and clinicians. University researchers included faculty from the University of Tennessee Health Science Center and the University of Utah. State health officials included members of the Tennessee Department of Mental Health and Substance Abuse (TDMHSAS), including the Tennessee State Opioid Treatment Authority and Assistant Chief Pharmacist for TDMHSAS. Additionally, feedback was solicited from clinicians at the licensed opioid treatment programs. In total, there were five key members who aided in the creation of the map. AC is a PhD-trained qualitative researcher in social and behavioral pharmacy, KH is a community pharmacist and PharmD with training and experience in qualitative research, and IA is a PharmD in post-graduate training with specific training in qualitative research.
2.3. Participants and Data Collection
Based on a thorough review of the literature and conversations with Tennessee state officials with expertise in OUD, it was determined that there was a critical need to capture the voice of the patient population receiving methadone treatment within opioid treatment programs. Therefore, 16 patients who were enrolled in one of 15 Tennessee-based opioid treatment program clinics served as key informants for semi-structured interviews with university researchers. The Tennessee State Opioid Treatment Authority and Assistant Chief Pharmacist at TDMHSAS worked with licensed opioid treatment program facilities within the state to recruit patients. Qualitative research methods were used to perform telephonic interviews at opioid treatment program clinics (i.e., methadone clinics) across east, middle, and west Tennessee in the spring of 2021. A semi-structured interview guide was developed by the team and pilot-tested to simulate the intended key informants in the field. Interviews were recorded and transcribed confidentially by a third-party transcription service. Interviews were conducted by university researchers without any prior relationship with the participants (AC, KH, and IA). All transcribed interviews were deductively coded by the same pair of research team members (KH and AC) who conducted the interviews. Coding was based on a patient journey mapping approach and was analyzed using NVivo for Mac (QSR International; Burlington, MA, USA). Transcripts were not able to be returned to participants for review. It was determined a priori that recruitment would cease at a point of saturation, at which no new information was uncovered in subsequent interviews. The research was approved by the UTHSC Institutional Review Board (IRB). The final patient journey map was developed through a consensus decision-making approach including several rounds of virtual meetings, feedback, and revisions.
3.1. Overview of Results
At the point of saturation, 18 interviews had been conducted across middle and eastern Tennessee. The average interview length was 65.6 min. Ten participants were male, and eight female. Participants were Black (2, 11%), White (14, 78%), or declined to answer (11%). Age ranges included 20–29 years (3, 17%), 30–39 years (3, 17%), 40–49 years (8, 50%), 50–59 years (2, 11%), and 60–69 years (2, 11%). Upon side-by-side comparison of the three patient journey map visualizations, the team decided the patient journey itself is best represented across several non-linear, interconnected roadways and across the three main settings of the map: the patient’s community, acute care, and chronic care ( Figure 3 ).

Community-Centered Patient Journey Map in Drug Addiction Treatment.

3.2. Community-Centered Patient Journey Map
The Community-Centered Patient Journey Map in Drug Addiction Treatment places the patient’s community at the center of their journey. This “community centrality” in combination with the non-linear patient journey pathway presents an atypical patient care journey. A typical patient journey map is linear and flows in a logical phase-by-phase manner from awareness of disease through to treatment and chronic management [ 26 , 29 ]. In contrast, the Community-Centered Patient Journey, as articulated by participants and community stakeholders, is represented by an infinite loop of awareness of OUD, treatment and chronic management, the potential for relapse, and the opportunity to re-engage in treatment.
A constant variable within the patient’s journey was their community, represented by home—family, friends, and peers (i.e., social support structure)—and the culture of the environment around them. Each of these elements exerts influence on the patient, and their desire to seek or remain in treatment. For instance, negative peer pressure and a culture that promotes both low self-esteem and self-worth may work synergistically to push an individual into OUD. The size of the community pathway “loop” within the map represents both the large degree of time spent within it and its overall influence on the journey of addiction treatment. On either side of that journey are the patient’s experience with OUD and acute care (left-hand side of Figure 3 ) and chronic care (right-hand side of Figure 3 ). Within each of the community, acute care, and chronic care “loops” are salient variables captured on the perpendicular axis grid ( Figure 2 ), including: touchpoints, moments of truth, emotions, supporting quotes, and pain points.
Throughout the patient journey map, highways are the best maintained and have the appearance of being intentionally designed by experts who oversee the system. Conversely, paths are unpaved, less direct, and not formally considered part of the highway system but are often used as unideal but necessary alternatives to the highways system by the patient. Scattered throughout both the highways and paths are obstacles, or “pain points”. These “pain points” centered across three main sub-themes: accessibility, adherence, and affordability ( Figure 3 , cloud text in the sky). Roadway signage is informative, but numerous and distracting, representing the lack of clear direction or pathways to the care available for patients with OUD. There are also great distances between healthcare touchpoints, where the patient and the healthcare system interact.
3.3. Beginning the Patient Journey toward Treatment
The journey stars within the patient’s community, where there is an exposure to an opioid (either licit or illicit), with or without peer pressure. Red arrows are used to demonstrate the flow into addiction either from opioid access from peers (illicit) or from a valid prescription (licit). OUD can continue within the community indefinitely until what participants referred to as a “trigger” event (i.e., a critical moment where an individual is made acutely aware of the negative consequences of their opioid use and the need for behavior change) or an “ah-ha” moment of general awareness of the need to seek help (represented by the green boxes labeled “Exit 1A” and “Exit 1B”). These different events can lead to two different pathways. The ‘general awareness’ pathway (“Exit 1A”) does not include an acute negative event, but rather a personal choice to proceed to chronic care and treatment. In contrast, a ‘trigger event’ (“Exit 1 B”) is another pathway to treatment, but requires an acute, negative event such as overdose, incarceration, or hospital or rehabilitation center admission. In this latter example, the pathway begins with a dirt road, rather than a paved one, to represent the distance the individual is from general society norms and the more severely difficult the path is toward treatment.
3.4. Entering Treatment through ‘Trigger Events’
Within the ‘Trigger events’ pathway, participants described several types, including: incarceration, drug court, arrest, opioid-related trauma (i.e., death within social circle due to OUD), or overdose. This pathway terminates with acute care being provided in some manner to address the immediate needs of the individual, including inpatient detoxification. However, the terminal point includes a formal re-entry back into the individual’s community. This is important, as participants noted that the community represented both the original genesis of their OUD, including access to both licit and illicit opioids and negative peer pressures, as well as supportive structures required for recovery (e.g., positive social structure, work, positive community activities).
“Yeah, you got to want to be clean, you know what I’m saying? Then, I didn’t care, you know what I mean? I was just using it for a crutch. But now I’m- I don’t want to go to prison, you know what I’m saying? I just, I want to do right, and that’s the difference. And like, my Dad, because he died of drug use, you know what I mean? He just died this past year.” (P12)
3.5. Entering Treatment through Awareness
Participants described a separate, chronic care pathway for outpatient OUD treatment, termed “Awareness” (“Exit 1A”). This pathway was used by participants either when they had a ‘general awareness’ of the need for treatment (e.g., distress, loneliness, sadness) or when they transitioned from acute care. This pathway is represented by a completely paved road to indicate that this entry into care is more formalized, more closely connected to societal norms, and in closer proximity to the healthcare system. However, the majority of the pathway is still located outside of the patient’s community, representing a potential barrier to access.
“Well, I needed somebody that would kind of, how do I put this, you know [help me]. Because, when I was going to the doctor to get the pain pills, I’d get 120, 90 to 120 [pills], and that’s a 30-day supply. Well, I would be out in two weeks. That’s a lot of pills. So I said, something has got to stop. I’m not going to survive doing this. And I was addicted. They would say, well, why don’t you just quit? Well, I wish it was easier said than done! I just, it’s a lot of stuff that plays into it besides just being an addict and addicted to pain pills. You’ve got all the peer pressure and you have to change your life. You can’t be around people that associate with you. You know, you lose friends. It’s just the way it is if you want to quit, you know, like that. But I got so many [painful] injuries- like, right now, I’m going to have to eventually have a whole hip replacement in my right hip now. And I just, you know, just keep holding on, I don’t want to have to go do it. But I’m eventually going to have to do it. It’s just I’m at that age that I’m falling apart.” (P9)
“I’m 39, and I’ve been- since I was 25, I’d been in and out of drugs, not hard drugs, it was mostly just pot, and then I started taking Lortabs, and then it went to OxyContin, which then led me here to methadone. So I guess my goal is to just get clean…” (P2)
The “Awareness & Ongoing Care” pathway (“Exit 1A”) was described by participants as including several barriers: treatment stigma, cost of care, wait lists for treatment, and travel distances to treatment.
“Once you get two days behind [in payment], you’re put on financial detox. They take you down ten milligrams every day until you’re down to zero, and then you’re done. They just kick you out.” (P2)
Those participants who had previously received chronic care for OUD remarked that these barriers had directly led to past instances of treatment non-adherence or relapse. This is visually represented by a dirt “trail”, which is an undesirable exit from treatment back into their community, and potential for relapse. For methadone treatment in particular, participants noted that the requirement to visit the clinic most or all days each week to receive their dose of methadone would interfere with keeping their job or restrict which jobs they could work.
“That was frustrating because, when I was working a day job, there was a time or two that I had to not take my medicine because I had to be at work by 9:00. And, I mean, I would get there [to the clinic] at 6:30 or 6:45, and I would have to leave at like 8:30. I’m like, I can’t wait. I’m like, you know, you guys want me to stay clean, believe you me, I want to stay clean, too, but I got to have a job too.” (P11)
The scarcity of treatment access points directly created the barriers of treatment “wait lists” and travel distance barriers. Some participants remarked that travel to clinics would take over an hour, one way.
“And, at that time, they had like three to six months waiting list, and I thought, oh my God, I can’t wait that long.” (P15)
“…I have to drive an hour every day. I’ve lost like some good jobs because I can’t never work first shift.” (P8)
Throughout treatment, patients described the treatment-related stigma that was ever-present.
“Yes, you do [feel stigmatized]. You know, and it may be self-thought. You know, you may have got the wrong attitude from the pharmacist or the personnel there at the pharmacy or whatever. It just seems like sometimes, you know, if you’re picking up a medication, sometimes you’re treated differently than- I’m treated differently when I go in to pick up my heart medication, okay? If I go in and get my blood pressure medication or my blood thinners, I’ve had several heart attacks, so if I go in and get that medication, I’m smiled at and sent on my way. But sometimes when I went in to get the pain medication, [medication for OUD], you know, you could just feel a sense that you were treated a little differently. And I try not to think that about anyone, I really do, but sometimes it’s hard not to feel that. You know, you sense that you’re being treated differently, yeah.”
3.6. Returning to the Community and Ongoing Care
After exiting either “Awareness & Ongoing Care” pathway (“Exit 1A”) or a ‘trigger event’ (“Exit 1 B”), the patient returns to their community to continue their OUD treatment. As described earlier, this is also where the patient is initially exposed to either licit or illicit opioids. Therefore, the patient’s entire opioid experience surrounds the community surrounding where they live and work.
As pictured in Figure 3 , medical professionals were primarily described as being located outside of the community (e.g., hospitals, medical offices, opioid treatment programs). Their influence on the patient while within the community is consequently limited to physician–patient touchpoints, and this was articulated by individuals. The exception to this was the community pharmacist, a medical professional located within the patient’s community and with whom individuals would frequently interact even between medical office visits. However, despite their accessibility, the perceptions of the community pharmacist and their role in care represented a “pain point,” whereby the experience preferred by the patient with the pharmacist was not always what was experienced.
“You know, you may have got the wrong attitude from the pharmacist or the personnel there at the pharmacy or whatever. It just seems like sometimes, you know, if you’re picking up a narcotic medication, sometimes you’re treated differently than- I’m treated differently when I go in to pick up my heart medication, okay? If I go in and get my blood pressure medication or my blood thinners, I’ve had several heart attacks, so if I go in and get that medication, I’m smiled at and sent on my way. But sometimes when I went in to get the pain medication, narcotics, you know, you could just feel a sense that you were treated a little differently. And I try not to think that about anyone, I really do, but sometimes it’s hard not to feel that. You know, you sense that you’re being treated differently.” (P14)
One patient detailed their positive experience with a community pharmacy in another country, which allowed the community pharmacist to be involved in OUD treatment with methadone to improve treatment access.
“And, then the biggest difference was [the prescriber] gave me a written prescription and just told me to go to a pharmacy and get it filled. They don’t really know me, I’m just the person who shows up, but of course [the prescriber and community pharmacist] have talked. That’s how they do it, the [prescriber and community pharmacist] talk to each other and set it up between them, so they know you’re coming, right?” (P16)
Other positive moderators and mediators found within the community “loop”, which were noted to encourage overall recovery and ongoing care, visualized as the “fence” in the middle of the community, hidden by trees and only accessible by a “hidden drive.” This represents what participants articulated as difficult-to-find resources and sources of support which could be found within the same community where their OUD began. This included meaningful employment, positive social connections (e.g., family, friends, partners), and clinicians (e.g., counselors, physicians, pharmacists) who supported their recovery.
“Oh, well, I was able to keep a job. My social life improved. I wasn’t always looking or trying to find, you know, my fix just so I could feel better and go sit in my room. Once I got the treatment, I was able to get back out there. And I’m a social butterfly, so I like being around people and talking and hanging out with friends and doing stuff. So once I got treatment, it kind of opened my life back up.” (P6)
4. Discussion
This paper presents a novel patient journey map for those engaging in substance use disorder treatment. Notably, the data support a patient journey line that is non-linear, which is a substantial contrast to typical patient journey maps with a clear beginning and end. This visualization captures the sometimes-revolving cycle of treatment, relapse, and recovery common in OUD. The presented journey map also places the community at the center, as the patient’s experience revolves around their community and is largely influenced by factors within the community, including “touchpoints” with the community pharmacy. Moreover, this community-centered lens is important because of the biopsychosocial etiology of OUD, and its necessary connection to the home environment, social connections, and other community-related factors [ 31 ]. The result is a visual map which provides a more comprehensive view of where a patient may be at the time of presentation to a healthcare provider, especially the community pharmacist.
It is of particular note that in the center of this Community-Centered Patient Journey Map in Drug Addiction Treatment, discussed in Figure 3 , are community resources. These include peers, the overall culture of the environment, and the community pharmacy. Counselors, other clinicians, and medical facilities—while all available in the outpatient setting—are not typically available in the patient’s own community, as articulated by the participants in this study and also seen in the supporting literature [ 17 ]. The centrality of the community pharmacy within the journey map makes visible what has been historically invisible to stakeholders of OUD treatment—the underutilization of the pharmacist. Moreover, it also makes visible to pharmacists the broader care journey the patient undergoes, and may help as a training, educational, and patient care resource for pharmacists to understand how best to care for these individuals.
This depiction of the community pharmacy within the continuum of a patient’s experience with OUD is the first, to the authors’ knowledge. Community pharmacists have historically been either excluded from OUD care and treatment guidelines or relegated to roles related to regulatory enforcement (e.g., accessing prescription-monitoring databases, denying or postponing medication fills) [ 20 , 32 ]. This has placed the community pharmacist in a difficult position where they are unable to intervene in risky opioid use or OUD to improve patient care, but are able to restrict opioid prescription access as required by federal and state regulations. As a consequence, the patient–pharmacist relationship has suffered, with pharmacists reporting compassion fatigue and patients reporting negative experiences at the community pharmacy [ 21 , 22 ].
Compassion fatigue in opioid use disorder is seen across professional settings, including pharmacy, nursing, medicine, and emergency service personnel [ 21 , 22 , 23 , 33 , 34 ]. Comprehensive models of compassion fatigue show that several external factors predispose healthcare professionals to compassion fatigue, including lack of positive patient outcomes, negative patient interactions, and lack of resources to adequately address patient needs [ 35 ]. Prior research indicates that each of these elements is present in the community pharmacy setting, as personnel indicate that the lack of clear professional guidelines, regulatory requirements, and scope of practice limitations do not allow the pharmacist to provide care for patients [ 20 , 21 ].
It has been suggested that pharmacist education may improve pharmacist-provided OUD care [ 7 , 14 , 15 , 32 ]; however, such education that excludes a fundamental discussion about the role and overall patient experience may be inadequate. Although not a holistic solution, providing frontline community pharmacists with training on opioid misuse, use disorder, and addiction may serve to offset compassion fatigue in this patient population. In general, health provider attitudes toward OUD and OUD treatment have been positively impacted by formal training programs [ 36 , 37 , 38 ]. This has also been found to be true for pharmacists’ attitudes toward OUD [ 39 ]. Notably, pharmacists’ attitudes toward patients with OUD improved with increasing exposure to patients filling prescriptions for OUD treatment, seeing patients improve over the course of OUD treatment, and seeing the positive impact a pharmacist can have on the course of OUD care [ 40 ]. In short, as the pharmacist realized the “big picture” of OUD care, they were better able to process the negative experiences that occurred with patients misusing opioid prescriptions. It is the authors’ feeling that the present journey map may be a helpful resource in training and educating pharmacists on this “big picture,” although future prospective studies will be required to understand if and to what degree this is true.
There were several limitations to this study. Data used to derive the patient journey map were gathered from a single state in the southeastern United States. Moreover, data relied solely on qualitative data and expert opinion. Although this data is sufficiently rigorous to develop patient journey maps [ 26 , 28 ], future research should incorporate a mixed-methods approach across geographic regions. Finally, the patient journey map has not been validated for its use in compassion fatigue with community pharmacists. Further research is needed to incorporate the journey map into an educational intervention to identify its impact on pharmacists’ attitude and behaviors, as well as patient care outcomes and patient care satisfaction.
5. Conclusions
This patient journey map depicts the patient’s perspective in managing OUD across a continuum of care settings. The patient journey map was developed to serve as a potential educational tool for pharmacists to better support patients with OUD. A non-linear patient journey is depicted when navigating OUD treatment, thus the map depicts a circular trajectory including both treatment and relapse. The map also indicates that the pharmacist may stand to play a critical role in both medication treatment access and in the identification and referral of patients into treatment. Future research may be useful to validate and build from this understanding so that care for patients with OUD in community pharmacies can be enhanced.
Acknowledgments
We would like to acknowledge the support of the Tennessee Department of Mental Health and Substance Abuse Services and Behavioral Recovery Group.
Funding Statement
This research was funded by the University of Tennessee System, grant number E073610699.
Author Contributions
Conceptualization, K.C.H. and A.C.; methodology, K.C.H. and A.C.; formal analysis, K.C.H., A.C. and C.L.; investigation, K.C.H., A.C. and I.A.; resources, W.G. and E.S.; data curation, K.C.H. and C.L. writing—original draft preparation, K.C.H. and C.L.; writing—review and editing, K.C.H., C.L., T.M.M., G.C., I.A. and M.C.-B. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of the University of Tennessee Health Science Center (protocol code 19-07064-XM and 20 December 2019).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Conflicts of interest.
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
- Family Services & Resources
- Parent Resources
- Intervention
- Family Events
- Locations Guide
- Alumni Services
- Alumni Meetings
- Alumni Events
- Referring to RCA
- Continuing Education
- Addiction Professionals
- Employers / EAPs
- Professional Events
- Addiction Treatment
- Outpatient & Telehealth
- Alcohol Detox
- Medication Addiction Treatment
- Alcoholism Treatment
- Opioid Addiction Treatment
- Stimulant Addiction Treatment
- Illinois Centers
- Indiana Center
- Maryland Centers
- Massachusetts Centers
- New Jersey Centers
- Pennsylvania Centers
- South Carolina Center
- Insurance Options
- Intervention Services
- Entering Treatment
- A Day in Treatment
- Employment, legal and financial assistance
- Resource Center
- Recovery Stories
- RCA Shared Spaces
- Substance Guide
- Evidence Based Practices
- RCA Academy
- News & Press Releases
- Careers at RCA
- Career Events
- Testimonials
- Career Growth
Living Recovery: True Stories of Addiction Recovery
Authored by Recovery Centers of America
A look into the lives of those who sought drug abuse treatment.
Behind substance use disorder is people – people with real stories of struggle and triumph.
Drug and alcohol addiction stories are usually shadowed by short, faceless segments on the news. But there’s a deeper, human element in each story that is too often untold.
We sat down to hear from four courageous people: all who have been caught in the grips of addiction and all who continue to live in recovery, helping and inspiring others along the way.
These are their stories. Read about their journeys, and learn how drug abuse treatment has played different but essential roles in their lives.
Gina’s Story
“I was in active addiction since I was 13. I started doing heroin and continued using until I was 33.”
Gina is an outgoing person, hence, her soul that shines through her eyes. Without hearing her story, you would never understand the trials and tribulations she endured to make it to where she is today.
“In 2005, I was out getting high and fell 20 feet and broke my back and my wrist, but I stayed out. I was only 70 pounds at that point. My family had to prepare my funeral. I told my mom I was going to die from this disease, that it was my destiny.
“In addiction, you live in the past of what it was like when you were a kid, standing on the corner drinking 40s or hanging out in the bar. It’s the only disease that convinces you that you don’t have a disease. It’s cunning, baffling, and powerful.”
Like too many people, substance use disorder had taken over Gina’s life – that is, until one day when she found the inner strength to ask for help .
“I was hanging out in Kensington in the freezing cold, and I suddenly had a moment of sanity. It was like my head and my heart were both suddenly on the same exact page, and I thought, “What are you doing? This isn’t good.
“I had been to 11 rehabs before that day. But that time, I walked into the crisis center, and it was the first time I finally said, ‘I don’t have a home and I haven’t had one in four years. I’m dying and I need you to help me.’ And they did.
“I had a social worker who really fought for me. People would treat me badly. In their terms, I was just a junkie. But my social worker told me, ‘We’re going to fight really hard for you. I need you to fight hard for you.’ She sent me through detox. I started going to meetings and hanging out with girls who lived in the recovery house.”
To Gina having a a strong support system was crucial, most noteworthy was her family .
“Thank God for my family. One of the things that breaks my heart is that I was not always there for my family as much as I feel I should have been. I was really being driven by addiction. They supported me through my entire journey.
“Now, I’m going to college to get my associate’s degree in social work. I don’t really know what else I would do if I didn’t work in the recovery field, my sponsee calls me every day at 4:34pm, and I have a group of women in recovery who I know are always going to love me, who will always be there for me.
“I would say to anyone who thinks they have a problem: There is hope. Don’t give up on it. You are loved. You are somebody.”
Your recovery story starts today.
Patrick’s story .
“There’s a couple different ways that obsession happens. Some obsessions are just unwanted, repetitive thoughts – they feel like a really intense craving. Then there’s the type that happens but doesn’t have that feeling behind it. It’s just a thought. For me, I could be driving down the road, completely sane, thinking, ‘Oh I’ll just stop for a couple beers.’ And it could end up ruining my life.”
Patrick’s road to recovery has been long and difficult, but in the end, rewarding. His substance use began when he was a teenager. And like many types of progress, his improvement did not always happen in a straight line.
“I got in a fight with a cop at 16 years old. My first rehab was at 17, got kicked out of it after 10 days, then back in there 3 months later. I had 6 or 7 months sober, maybe even a little bit longer. Then I went back out and drank.
“I got sober again when I was 24. During that period of time I had 11 years’ sobriety. At 35, my wife and I went through a divorce – and a lot of stuff happened. I just drank. It would take me 10 years to get more than 30 days sober.”
“I was in and out of Alcoholics Anonymous, that was constant. I would go to meetings and nothing would happen, I would still want to drink. Really bad obsessions. That went on for about 10 years. I lost everything. I lost a really nice house, my car was repoed, and my 401k was gone.”
Even though Patrick had hit bottom after bottom, he was unable to stay sober. Eventually he decided to ask for help from his father, who had 28 years sobriety.
“I showed up at my dad’s house with two gym bags. I finally said, ‘This is it. I’m spiritually broken – I can’t do this anymore.’
“I was able to stay sober for 9 months – meetings every day, praying every day, really in the middle of the program. But the day came when I drank again’.
“I went into rehab for about 10 days, and I just kept thinking to myself, ‘I’ll do anything, please God, I do not want to drink ever again.’
“After rehab, I went to another meeting. A guy there recommended I go to someone’s house that was having a Big Book study. I went to the house, and he started talking, and everything he was talking about, I was like, that’s me – he knows what I’m going through. So he started taking me through the Big Book and the steps, and I started to get freedom from stuff that was causing me to drink.”
Maybe the most striking part of Patrick’s personality is his acute self-awareness. It’s a trait that he sharpened while in recovery, and it’s a significant reason why he’s finally found so much success staying sober.
“It was primarily my self-centeredness, my ego. And I don’t mean like egotistical. I mean selfishness, resentments, fear, the things that engulf people with drinking problems. The steps are designed to look at that from a different point of view. There’s got to be that internal surrender for sobriety to happen. It helps for you to be other-centered. Gets you out of yourself. It keeps you really connected to other people.
“I’ve been going pretty regularly for the past year or two into jails to meet with people who have a drinking problem. Even though I was never in jail, I can relate to some of them who are near low-bottom with their drinking. When I talk, I describe my experience and what happened to me with my recovery. I say to them like I say to my sponsees, ‘We’re going to go through this book. Line by line. Page by page. And we’re going to have a load of work to do.’
“I get a lot of contentment from helping other people. Companionship. Because of that, I have freedom from my addiction.”
Patrick found freedom by surrendering, taking the steps through the Big Book, and clearing the path for his relationship with God. By doing so, he reclaimed a part of himself that was missing while he was drinking.
“It starts with surrendering. And the first thing in surrendering is asking somebody for help . Whatever that help is. And hopefully you get to a place that can offer the help you need. It’s worth it.”
Jules’ Story
One of addiction’s stereotypes is that it only affects those with dysfunctional families or a history of abuse. But when we spoke with Jules, we learned her story defied those ideas conclusively.
“I wish I had some story to tell you about my horrible, abusive, and neglected childhood. But I don’t. I came from a normal family. We literally had a white picket fence.
“Growing up, I had a lot of insecurity. I fought with eating disorders. I couldn’t cope with looking in the mirror. When I was about 15, I started drinking. As soon as I drank, I became a different person. That, to me, was freedom – but it later became prison.
“It was my idea to bring drinking to my friends. We went to a competitive high school and most kids saw drinking as a social faux pas. When we started doing it, everyone else could pick it up and leave it alone until the next time. I couldn’t do that, which baffled me. Why could everyone else stop after the weekend and I was left obsessing about drinking all day every day?”
Jules’ alcohol use started affecting her everyday life. It hindered her from doing the things she loved, it certainly damaged the relationships she had with her loved ones .
“I just kept lowering and lowering my standards. When I went to college, it really took off. I joined a sorority, made friends with drug dealers. I was free to drink and use the way I wanted to. It made me feel powerful, like I was unstoppable. And then it stopped working. My alcoholism had progressed to the point in which I couldn’t get drunk anymore. The solution I had found to deal with life had failed me. I had a miscarriage, I was so out of touch I didn’t even know that I was pregnant. I felt alone, confused, and broken. My University asked me to leave and everything came to a halt. It was the catalyst that led me to surrender.
“I came home and I decided to find a therapist for treatment. I told her all of my problems and she said I was an alcoholic . ‘No.’ I said. ‘I have highlights and a French manicure, there’s no way I’m an alcoholic. Aren’t I schizophrenic or something?’ I didn’t know I had this body that worked against me. Once I started drinking, I couldn’t stop. If I did manage to stop, my mind told me that I could drink like normal people.
“My therapist introduced me to my first sponsor who sent me to my first 12 step meeting. I had every excuse not to go. But once I got there, I stayed. I reluctantly kept going. There was something about the people there that I couldn’t put my finger on that kept me going. I know now that it was the light inside of them – the sunlight of the spirit – that spoke to me.
“Getting sober at 21 wasn’t easy. All of my peers were still at college partying while I was embarking on a spiritual journey. It was the most difficult and most brave thing I have ever done.
“The twelve steps are about spirituality. They’re not about sobriety. They’re about growing along spiritual lines, and sobriety is a by-product of that. Living by spiritual principles is not something that other 21-year olds were doing. The recovery community was different then, too. There weren’t as many young people in recovery as there are today. I had to start my life from scratch. Everything that I believed in, everything that I was about, and my perception on life had to change.
“My recovery has been a journey. As a woman, part of my journey is about finding my voice and figuring out who I am. After nearly a decade of living in recovery, I can tell you that long-term sobriety is not for the faint of heart. A lot has happened in these nine and a half years. At three years of sobriety, I buried my best friend in the world. It broke my heart and healed me in innumerable ways at the same time. I sought spirituality and a connection with my higher power with a desperation that I never had before.
“The challenge for me now is not to fight urges to drink, but to stay passionate about recovery and excited about spirituality. Long-term sobriety is about constantly seeking – seeking to grow, seeking to help others, and seeking what my truth is and living it. It’s about self-reflection, remaining teachable, staying humble, and not compromising my morals regardless of the worldly consequences.”
Jules’ recovery has been as much about finding herself and living her truth but rather about reclaiming her life from alcoholism. Now with a new life, she has her confidence back.
“My sponsor told me a story once. She was getting her hair cut and this little girl next to her looked at herself in the mirror and said, ‘Oh my God! Look how cute I am!’ And I just thought to myself, that’s how I feel every single day. I’m finally comfortable in my own skin. I know and accept exactly who I am – flaws and all.”
Katie’s Story
Speaking with Katie, the first thing you’ll notice about her is her confidence. She spoke like she wasn’t afraid of anything, but her story of recovery proved she didn’t always exude the same fearlessness.
“My father passed away with 35 years of continuous sobriety. He was an exec, very successful. Had six kids. Even when he was in recovery, we didn’t talk about it. It was like our secret.
“We were forbidden to drink. But I drank. I got a DUI and went into treatment. I was 22-years old, in college, and I thought, ‘I’m not like these people in treatment.’ But I packed up my loafers and my sweaters, and I played the part.
“Early on, I was staying sober because of my father. I started volunteering at an addiction treatment facility. Started there when I was 22. I was the detox counselor. Then I was the activities counselor. Next I was an outpatient counselor.
“Then I got pregnant with my triplets and couldn’t work. When I had them, I was active in AA for about 10 years and continued working in the field. But I was getting a bit of an ego. Everyone would say, ‘You saved my life.’ I’d say, ‘Of course I did.’ So I started thinking, ‘I don’t need to go to meetings anymore.’ I stopped going.”
“I ended up drinking when I was 40-years old, after 18 years of sobriety. I got three DUIs in a year-and-a-half’s time. The progression of alcohol is tremendous. If you stop drinking, picking it back up is like you’ve been drinking the whole entire time. I lost my license, my marriage broke up, and I was drinking myself to death.”
Asking for help isn’t always easy, and Katie’s situation was no different.
“It was very hard for me to go back in. But I became active in AA again. My husband at the time and I were still living together. It was the women in AA who would come over and say, ‘You can do this, Katie. You can’t cohabitate. You gotta move out.’
“So here I am. I’m 20 years married, I’ve got three kids. Women in AA are saying, ‘You’re strong enough to move out.’ And I’m saying, ‘I don’t know if I can.’ When I left my parents’ house, I got married. I’d never even paid a bill.
“I decided, I gotta go. I gotta leave.”
Katie’s successful path to recovery began by looking outside of herself. At her core, she knew something was still not right. When she was working at Recovery Centers of America, something happened that changed her path for the better.
“I’ve had a really hard time getting my recovery back. There was always something missing. I wasn’t sponsoring anybody; wasn’t helping anybody.
“I knew this one girl, she used to come to meetings talking about the Big Book. S0 I reached out to her. I said, ‘I need help. I need you to take me through this book.’ So she literally took me line-by-line through the book, from the very front cover. She said to me, ‘You’re in a lot of pain, Katie.’ She said, ‘I gotta get you through this book quickly.’
“Her purpose of teaching me the book was so I could teach someone else. I felt like I had a purpose. It gave me more compassion and I became more interested in the solution, not the problem.
“That’s the advice I would give to somebody who’s struggling: Slow down. Try to do something kind for somebody else.
“Because of my active involvement in the program, I’m a better mother, girlfriend, and friend. My overall focus is more on giving to others rather than receiving. My recovery is the biggest blessing I have in my life today.”
Addiction is a chronic disorder, not a personal failure. There is a human face behind every example, and there is real hope that addiction recovery can change your life.
If you believe you or a loved one is suffering from drug or alcohol abuse, we can help. Call us today to learn more about our drug abuse treatment and to get started. Or click here to see more recovery stories.
Recovery Centers of America is not affiliated with or endorsed by Alcoholics Anonymous.
Authored by

Recovery Centers of America
Related posts, working while in treatment: how outpatient rehab helps, is fentanyl in marijuana, why is fentanyl so dangerous, we’re here for you.
Complete the form and a treatment advisor will contact you at the number provided.
Available 24 hours, 7 days a week
Find a recovery centers of america near you.

Treatment Advisor Standing By, 24/7
The journey from drug addiction to drug recovery; a case report of an inpatient rehabilitation
Affiliations.
- 1 Department of Applied Psychology, National University of Modern Languages, Islamabad,Pakistan.
- 2 NUST Business School, National University of Science and Technology, Islamabad, Pakistan.
- PMID: 36156576
- DOI: 10.47391/JPMA.2419
In Pakistan, 64% of the total population is under the age of 30 and unfortunately, the increasing number of young addicts in Pakistan is estimated at the distressing rate of 40,000 per year. By considering the alarming situation and scarcity of literature, this research aims to investigate the recovery phase of drug addiction by introducing a case that highlights drug addiction, recovery, and relapse in the Pakistani context. We designed a case study approach in which face-to-face interviews were used. The case under consideration is a 38 years old patient with a history of chronic addiction with episodes of recovery and relapses. The shift of approaches from the extreme end of the addiction continuum to full recovery poses an opportunity for drug rehabilitation professionals to learn factors associated with drug addiction, the recovery process, and first-hand comments on recovering interventions in Pakistan.
Keywords: Illicit Drugs, Substance-related Disorders, Mental Health Recovery, Case report, Pakistan..
Publication types
- Case Reports
- Asian People
- Behavior, Addictive*
- Substance-Related Disorders* / epidemiology
Sick? Be Seen in Minutes with Video Visits on Demand. Start Now.

Journey Recovery Center (JRC) provides the gold standard of treatment for substance use disorders (SUD).
JRC is designed to assist individuals out of substance use disorder and onto a pathway to wellness. JRC staff have provided services to an average of 1,500 individuals per year, accounting for nearly 33,000 office visits. Therapeutically, our goal is facilitating independence, short-term and long-term recovery support, and the rebuilding of lives and families.
JRC provides a continuum of patient-centered care to meet the socioeconomic and biopsychosocial needs of the individuals we serve using a multi-faceted approach including:
- Individual therapy.
- Targeted case management.
- Peer support outreach.
- Specialty group therapy (IOP, MAT, Recovery, Baby Steps Program for pregnant women with SUD).
- Recovery and crisis stabilization services (e.g., walk-ins).

The first step is often the most difficult one.
Our trained specialists are here to help, contact us today to start your recovery journey. Call (859) 757-0717
Dedicated, highly trained professionals, licensed within their specific disciplines, will engage individuals with a SUD and jump start their pathway to well-being regardless of their entry point.
Services Include:
- Assessments for severity of substance use.
- Medication-assisted treatment
- Substance use monitoring
- Clinical and case management
- Recovery support programs, including peer support specialists
Focus On All Aspects of Recovery
Add the components that restore human dignity and self-confidence

News and Recognition
Journey recovery center awarded 3-year carf accreditation.

Don’t wait another day, start recovery today.
Our trained specialists are here to help, contact us today to start your recovery journey..
About St. Elizabeth
Associate Intranet Careers Insurance Carriers Physician Opportunities St. Elizabeth Healthcare
Contact Us Find a Location Find a Provider Pay My Bill MyChart Login Schedule a Visit
Disclaimer/HIPAA Human Resources Patient Rights and Responsibilities Nondiscrimination Notice and Foreign Language Assistance Website Privacy Policy Website User Agreements (Terms of Use)

© 2024 St. Elizabeth Physicians. All rights reserved.
Republish This Story
Recovery From Addiction Is a Journey. There’s No One-and-Done Solution.
Disponible en Español
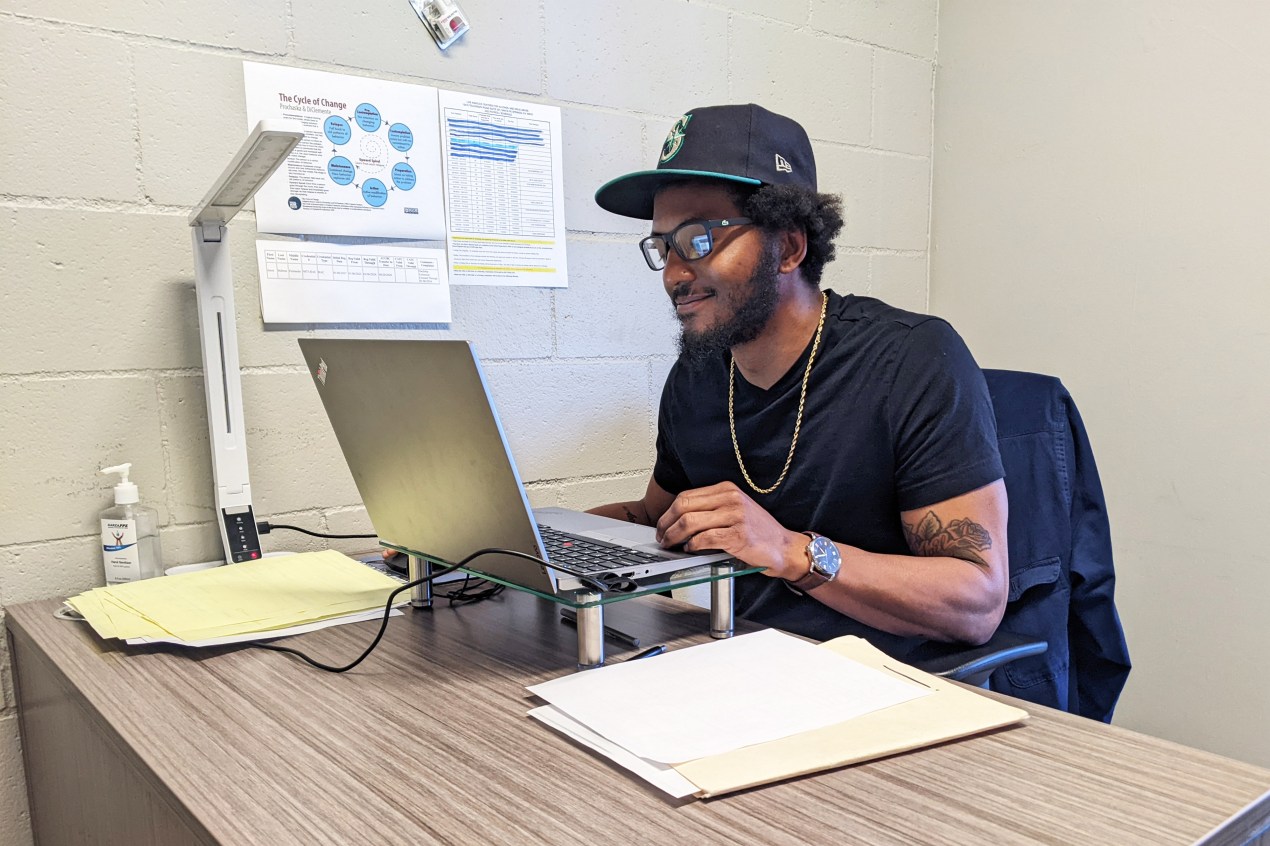
The atmosphere inside the Allen House is easygoing as residents circulate freely through the hallways, meet in group sessions, or gather on a large outdoor patio that features a dirt volleyball court with an oversize net.
The 60-bed safety-net residential treatment center in Santa Fe Springs, run by Los Angeles Centers for Alcohol and Drug Abuse , has a dedicated detox room, on-site physicians and nurses, substance abuse counselors, licensed therapists, and other practitioners. It offers group counseling as well as individual and family therapy, and it endorses the use of medications for addiction treatment, such as buprenorphine and naltrexone, which are increasingly considered the gold standard.
Willard Sexton, a staff member and former Allen House patient, says the most important part of his job is speaking with each resident daily. Most of them, like him, came to treatment straight from jail or prison, and he knows as well as anybody how stressful it is to stop using.
“It’s similar to grief and loss,” says Sexton, 35. “The drug was their best friend for a long time.” Interacting with them, he says, helps him in his own ongoing recovery.
At a time when drug use is among the nation’s gravest public health crises, a visit to the Allen House offers key lessons: Addiction is a chronic illness requiring constant vigilance, there’s no one-and-done solution, and relapses are part of the journey to recovery. Peer mentoring is an invaluable element of drug counseling, since people who have plodded the difficult path from dependence to sobriety understand the mindset of patients on a visceral level.
And most importantly for those who feel despair in the grip of addiction, there is hope. “Recovery happens,” says Michelle Doty Cabrera, executive director of the County Behavioral Health Directors Association of California. “Every single day people come into treatment and succeed in addressing their substance use disorders.”
Drug-related overdoses kill almost as many Californians as lung cancer, more than diabetes, and two to three times as many as car accidents, according to a report by California Health Policy Strategies , a Sacramento consulting group. The report showed there were about 11 times as many fentanyl-related deaths in 2021 as in 2017, accounting for more than half of overdose fatalities. And addiction can ruin lives even if it doesn’t end them.
But proper care for substance use disorders can still be hard to find. Experts in the field say residential treatment beds are in short supply. A pandemic-driven shortage of health care workers has hit the drug treatment world . Unscrupulous operators, with an eye on their bottom lines , may take advantage of people desperate for any answer. Commercial insurers often deny treatment requests or propose cheaper alternatives.
Some treatment programs shun anti-addiction medications that have proven effective . Physicians, nurse practitioners, and other providers with the requisite training can prescribe these drugs in California, but too few seem willing or able to do so — though that could change now that federal law no longer requires them to get a special waiver.
A page on the website of the Substance Abuse and Mental Health Services Administration ( www.samhsa.gov ) allows you to find practitioners in your area who treat patients with buprenorphine.
There’s no one-size-fits-all solution for addiction. Treatment can differ depending on the substance — opioids, alcohol, or methamphetamine, for example. And people with substance use problems come from all walks of life: Some are straight off the streets or out of jail or may have serious mental or medical conditions that require additional care. Others may be otherwise healthy with good jobs and insurance. If a clinic tries to sell you on a standardized treatment program, cross the place off your list.
And if someone tells you that after one stint in their program you or a loved one will be drug-free for life, run the other way. For many people, addiction is a chronic condition that ebbs and flows over many years. Too often, patients in the throes of an overdose are revived and then discharged with no follow-up.
“If we talked about treating other chronic illnesses like diabetes or asthma in the same way we often approach treating substance use, people would think we were crazy or would sue the doctor for malpractice,” says Bradley Stein, a psychiatrist and senior physician policy researcher at the Rand Corp.

Finding the treatment that is right for you or a loved one will take legwork.
Whether it should be a residential or outpatient program depends on multiple factors. People who need to be shielded from exposure to a dealer or a toxic domestic situation, require detox, or have mental health or medical conditions on top of their drug use generally are better off in a residential setting, says Randolph Holmes, medical director of the Los Angeles Centers for Alcohol and Drug Abuse. Outpatient settings are more suitable for people with stable lives and better health or those transitioning from residential treatment, he says.
The cost of treatment can vary widely depending on duration and the patient’s circumstances. In some cases, it can reach tens or hundreds of thousands of dollars.
Various websites allow you to search for nearby addiction treatment. The Substance Abuse and Mental Health Services Administration has a treatment locator at www.findtreatment.gov , or you can call its help line at 800-662-HELP (4347). Shatterproof ( www.shatterproof.org ) is another source for finding treatment. In California, the Department of Health Care Services publishes a list of substance use help lines by county.
If you’re on Medi-Cal, California’s version of the federal Medicaid program for low-income residents, your county is a good place to start. It can point you to several options, at least in more populous areas. Almost all patients with the Los Angeles Centers for Alcohol and Drug Abuse, for example, are Medi-Cal enrollees.
If you have commercial insurance, call your health plan first. Parity laws require insurers to cover substance use treatment, though they often find reasons not to provide the treatment your provider recommends. If your plan denies you treatment you think you need, you can file an appeal. The Department of Managed Health Care ( www.dmhc.ca.gov ), the state’s primary health plan regulator, has a help line (888-466-2219) that can assist in appealing your case. Or you can do it online . If the department does not regulate your plan, it can steer you in the right direction.
And remember that recovery is a long-term commitment.
When Sexton first started using in his early 20s, his drug of choice was meth. He later started smoking it with heroin and fentanyl mixed in, he says.
Several years ago, Sexton spent 45 days in residential rehab and got clean. Then he started seeing a woman who was addicted to heroin. He thought he’d help her get sober but ended up doing drugs with her instead. He landed in jail for two months, and a judge ordered him back into residential drug treatment.
Sexton says he continues to actively pursue his recovery even as he helps others do the same. “There are bumps in the road, but I feel like I’m in a Range Rover,” he says. “I’m not going to spill my coffee.”

This article was produced by KFF Health News , which publishes California Healthline , an editorially independent service of the California Health Care Foundation .
Related Topics
- Asking Never Hurts
- Substance Misuse
Copy And Paste To Republish This Story
By Bernard J. Wolfson June 6, 2023
“It’s similar to grief and loss,” says Sexton, 35. “The drug was their best friend for a long time.” Interacting with them, he says, helps him in his own ongoing recovery.
At a time when drug use is among the nation’s gravest public health crises, a visit to the Allen House offers key lessons: Addiction is a chronic illness requiring constant vigilance, there’s no one-and-done solution, and relapses are part of the journey to recovery. Peer mentoring is an invaluable element of drug counseling, since people who have plodded the difficult path from dependence to sobriety understand the mindset of patients on a visceral level.
And most importantly for those who feel despair in the grip of addiction, there is hope. “Recovery happens,” says Michelle Doty Cabrera, executive director of the County Behavioral Health Directors Association of California. “Every single day people come into treatment and succeed in addressing their substance use disorders.”
Drug-related overdoses kill almost as many Californians as lung cancer, more than diabetes, and two to three times as many as car accidents, according to a report by California Health Policy Strategies , a Sacramento consulting group. The report showed there were about 11 times as many fentanyl-related deaths in 2021 as in 2017, accounting for more than half of overdose fatalities. And addiction can ruin lives even if it doesn’t end them.
There’s no one-size-fits-all solution for addiction. Treatment can differ depending on the substance — opioids, alcohol, or methamphetamine, for example. And people with substance use problems come from all walks of life: Some are straight off the streets or out of jail or may have serious mental or medical conditions that require additional care. Others may be otherwise healthy with good jobs and insurance. If a clinic tries to sell you on a standardized treatment program, cross the place off your list.
“If we talked about treating other chronic illnesses like diabetes or asthma in the same way we often approach treating substance use, people would think we were crazy or would sue the doctor for malpractice,” says Bradley Stein, a psychiatrist and senior physician policy researcher at the Rand Corp.
The cost of treatment can vary widely depending on duration and the patient’s circumstances. In some cases, it can reach tens or hundreds of thousands of dollars.
If you’re on Medi-Cal, California’s version of the federal Medicaid program for low-income residents, your county is a good place to start. It can point you to several options, at least in more populous areas. Almost all patients with the Los Angeles Centers for Alcohol and Drug Abuse, for example, are Medi-Cal enrollees.
If you have commercial insurance, call your health plan first. Parity laws require insurers to cover substance use treatment, though they often find reasons not to provide the treatment your provider recommends. If your plan denies you treatment you think you need, you can file an appeal. The Department of Managed Health Care ( www.dmhc.ca.gov ), the state’s primary health plan regulator, has a help line (888-466-2219) that can assist in appealing your case. Or you can do it online . If the department does not regulate your plan, it can steer you in the right direction.
Several years ago, Sexton spent 45 days in residential rehab and got clean. Then he started seeing a woman who was addicted to heroin. He thought he’d help her get sober but ended up doing drugs with her instead. He landed in jail for two months, and a judge ordered him back into residential drug treatment.
Sexton says he continues to actively pursue his recovery even as he helps others do the same. “There are bumps in the road, but I feel like I’m in a Range Rover,” he says. “I’m not going to spill my coffee.”
We encourage organizations to republish our content, free of charge. Here’s what we ask:
You must credit us as the original publisher, with a hyperlink to our kffhealthnews.org site. If possible, please include the original author(s) and KFF Health News” in the byline. Please preserve the hyperlinks in the story.
It’s important to note, not everything on kffhealthnews.org is available for republishing. If a story is labeled “All Rights Reserved,” we cannot grant permission to republish that item.
Have questions? Let us know at KHNHelp@kff.org
More From KFF Health News

Thousands of Children Got Tested for Lead With Faulty Devices: What Parents Should Know

Wins at the Ballot Box for Abortion Rights Still Mean Court Battles for Access

KFF Health News' 'What the Health?': Nursing Home Staffing Rules Prompt Pushback

White House Enlists Doctors and Hospitals To Combat Gun Violence
Thank you for your interest in supporting Kaiser Health News (KHN), the nation’s leading nonprofit newsroom focused on health and health policy. We distribute our journalism for free and without advertising through media partners of all sizes and in communities large and small. We appreciate all forms of engagement from our readers and listeners, and welcome your support.
KHN is an editorially independent program of KFF (Kaiser Family Foundation). You can support KHN by making a contribution to KFF, a non-profit charitable organization that is not associated with Kaiser Permanente.
Click the button below to go to KFF’s donation page which will provide more information and FAQs. Thank you!
- Public Affairs
- Support KET
- Membership Benefits
- Sponsorships
- More Ways to Give
- Legislative Coverage
Journey to Recovery
KET addresses opioid epidemic with Journey to Recovery documentary
Opioids – including heroin and prescription opioids such as oxycodone and hydrocodone — killed more than 33,000 people in 2015, more than any year on record, according to the Centers for Disease Control and Prevention. Deaths due to opioid overdoses claim the lives of 91 Americans every day.
As families touched by addiction know all too well, our nation is in the midst of an opioid epidemic. In an effort to address the epidemic and provide information about treatment options available in Kentucky, KET presents Journey to Recovery , a new documentary that explores personal stories of triumph over addiction using various recovery programs.
Journey to Recovery , narrated by Grammy-nominated recording artist and Kentucky native Sturgill Simpson, airs Monday, Feb. 13 at 8/7 pm on KET.
The documentary examines an array of treatment and recovery programs offered across the state, including abstinence-only programs – such as faith-based and 12-step based programs – as well as medication-assisted treatment programs. The program also interviews many of the nation’s top experts on addiction, including Dr. Nora Volkow, director of the National Institute on Drug Abuse (NIDA), and Dr. Robert DuPont, a former NIDA director and former White House Drug Chief who continues to advocate for a reduction in illegal drug use through his role as founding director of the Institute for Behavior and Health, Inc.
Journey to Recovery is part of KET’s ongoing Inside Opioid Addiction initiative, funded in part by the Foundation for a Healthy Kentucky. The initiative’s website, KET.org/opioids , includes archived KET and national programs addressing America’s growing opioid problem.
Ad Blocker Detected

Just When You Think You Can’t ...We Know You Can
Substance Use Treatment Centers

We Meet You Where You’re At
We understand that you're committing to a lifetime of wellness. Everyone is on a different journey, and we meet you exactly where you are.

Backed by 6K+ success stories
We've helped thousands of people like you get healthy and stay healthy. Don't let doubts hold you back. You can do this! (And, we're here to help)

There's 95% you'll be satisfied
You deserve care that listens and constantly improves. As of October 2020, the satisfaction rate here has never dropped below 95%.
Enter your phone number and get a call usually within 5 minutes.
We understand you're committing to a lifetime of wellness. Everyone is on a different journey, and we meet you exactly where you are.

Take the First Step to a Healthier You

Medical Detox
Often The first step in treatment, medical detox is the removal of drugs and alcohol from your system. Once you are comfortable, the work begins toward sobriety and mental health.

Inpatient Rehabs
Inpatient treatment involves taking a step into a residential facility where addiction and mental health therapy combine with social bonding and alternative therapies like music, holistic wellness and art.

Outpatient Clinics
Outpatient rehab.
Outpatient therapy offers a flexibility in drug and alcohol treatment that allows you to live and work as you do now, While attending meetings and therapies in an IOP. This option helps you work through the triggers and stressors of every day life and addressing them daily as they come outside the facility.

App & Coaching
Our app and coaching program is a state of the art wellness initiative that keeps your direction and hardwork at your fingertips.
JourneyPure is a leading substance abuse and mental health treatment provider for adult men and women with residential and outpatient locations across the southeast. We are recognized nationally for exceptional outcomes, evidenced-based best practices and patient-centered care.
Yes, Treatment Here is In-Network
This means any cost to you is as low as possible.

You’re Not Alone
Some of our amazing success stories
It's the personal story of each person that walks through the doors that gets us up in the morning and keeps us up at night.
We have over 6,000 success stories and hundreds of 5-star reviews!

One of only 20% of healthcare centers in the world to earn CARF.

An A+ rated facility by the U.S. Better Business Bureau.

January 2020

Savannah C.
4+ years clean

Mom of Krista P.
When i made the first phone call, i had so many questions. i had no idea what to expect. i'd never been through anything like this before. they answered all my questions and even called me back to make sure that i didn't have any more questions..

You feel the love as soon as you walk in. It's nothing like other rehabs I've been to. They truly care and work with each person.

This isn't just a rehab center. Journey Pure ensures you are mentally, physically and spiritually well. I was able to break free (thank you horses) and find out things about myself. I worked through mental barriers I never thought I could break.
Our locations.

Click to Filter
Journeypure knoxville.
--> 2636 Maryville Pike Knoxville, TN 37920 (865) 234-4352
JourneyPure At The River
--> 5080 Florence Road, Murfreesboro, TN 37129 (615) 900-2444
Knoxville OP Clinic
--> 7417 Kingston Pike Suite 301, Knoxville, TN 37919 (865) 217-1297
Murfreesboro OP Clinic
--> 1139 NW Broad St #102 Murfreesboro, TN 37129 (888) 246-4427
Nashville OP Clinic
--> 211 Donelson Pike, Suite 11 & 12, Nashville, TN 37214 (888) 517-3453
JourneyPure Albany
--> 731 Burkesville Rd; Albany, KY 42602
JourneyPure Bowling Green
--> 2349 Russellville Rd Bowling Green, KY 42101 (270) 282-8280
Bowling Green OP Clinic
--> 1901 Scottsville Rd Bowling Green, KY 42104 (888) 862-5018
Elizabethtown OP Clinic
--> 400 Ring Rd. Suite 155 Elizabethtown, KY 42701 (502) 833-7022
Lexington OP Clinic
--> 1401 Nicholasville Road Lexington, KY 40503 (844) 819-1377
Louisville Outpatient Clinic
--> 3430 Newburg Rd Suite 158 Louisville, KY 40218 (502) 804-2751
Paducah OP Clinic
--> 2500 Holt Road Paducah, KY 42001 (270) 201-5141
JourneyPure Emerald Coast
--> 22219 Panama City Beach Pkwy Panama City Beach, FL 32413 (800) 338-5770
Fort Walton Outpatient Clinic
--> 348 Miracle Strip Parkway SW, Suite 34, Fort Walton Beach, FL 32548 (888) 736-0198
Melbourne Outpatient Clinic
--> 90 S Harbor City Boulevard, Melbourne, FL 32901 (877) 322-1180
Have Questions? Ask Our Expert Doctors.
Drug, alcohol & mental health questions answered by the doctors at journeypure., what happens now.
- Getting help is as easy as picking up the phone.
- We will answer all your questions and provide an assessment.
- We will help arrange for you to come to the program and begin recovery.
Call Us (888) 985-2207
Or, get a call back, check insurance.
384 - Drug Addiction at a young age: Harrison's Journey to Sobriety Real Recovery Talk
- Self-Improvement
In this powerful episode, we delve into the deeply personal story of Harrison, a man who battled with addiction from a young age. From the allure of substances to the depths of despair, Harrison's journey through addiction was tumultuous and heartbreaking. He candidly shares his struggles, admitting that at one point, he couldn't envision a life without drugs. However, against all odds, Harrison found the strength to seek help and embark on the path to recovery. Through perseverance and support, he gained the tools necessary to maintain his sobriety, reclaiming control of his life one day at a time. Now, Harrison not only stands as a testament to the power of resilience but also as a beacon of hope for others grappling with addiction. Today, Harrison's life is radically transformed. He works tirelessly in the field of addiction treatment, extending a compassionate hand to those still struggling. With his relationships restored and a newfound sense of purpose, Harrison radiates a joy and fulfillment that once seemed unattainable. Join us as we explore his remarkable journey from darkness to light, proving that recovery is possible for anyone willing to embrace it. If you have any questions you can reach us at [email protected]
- Episode Website
- More Episodes

based on Google
Robert Downey Jrs Inspiring Journey through Drug Addiction
Discover Robert Downey Jr.'s inspiring journey through drug addiction, from downfall to redemption.
By Alis Behavioral Health Staff
April 29, 2024

Robert Downey Jr.'s Addiction Journey
Robert Downey Jr., a beloved actor known for his remarkable performances, faced a long and challenging battle with drug addiction that began in the late 1980s and persisted for several years. His addiction had a profound impact on both his career and personal relationships, leading to numerous struggles along the way.
Early Substance Use
Downey's addiction initially started with marijuana and cocaine but quickly escalated to include other substances such as heroin and prescription drugs [1]. The allure of these substances and their subsequent hold on his life propelled Downey into a cycle of dependency and self-destructive behavior.
Escalation to Harder Drugs
As Downey's addiction progressed, he found himself entangled in the grip of harder drugs. The allure of substances like heroin and prescription drugs intensified, leading him further down a treacherous path of substance abuse and dependency. These drugs not only wreaked havoc on his physical health but also took a toll on his mental and emotional well-being.
Impact on Career and Personal Life
Downey's addiction had a profound impact on both his career and personal life. His struggles with substance abuse led to numerous arrests and legal consequences, making it difficult for him to maintain a stable professional life. The incident in 1996, when he was found in possession of cocaine, crack cocaine, heroin, and an unloaded .357 Magnum, along with being caught passed out on a neighbor's 11-year-old son's bed, further exacerbated his challenges. The consequences of his addiction resulted in lost opportunities and damaged relationships, adding to the complexities of his journey.
Robert Downey Jr.'s addiction journey serves as a reminder of the power of addiction and the challenges individuals face in overcoming it. Despite the hardships he endured, Downey's story serves as an inspiration to others who may be struggling with addiction, highlighting the possibility of recovery and the strength that lies within.
Path to Recovery
Robert Downey Jr.'s journey to recovery from drug addiction was marked by various stages and key elements that played a significant role in his turnaround. This section explores the support systems, legal consequences and treatment, as well as the process of rebuilding his life and career.
Support Systems
One of the crucial factors in Robert Downey Jr.'s recovery was the presence of a strong support system. In 2003, his wife Susan Downey gave him an ultimatum, which became a turning point in his battle against addiction. Her unwavering support and tough love played a pivotal role in his decision to quit drugs for good.
Additionally, Downey credits a combination of 12-step programs, therapy, yoga, meditation, and Wing Chun Kung Fu for helping him maintain his sobriety. These support systems provided him with the tools and coping mechanisms needed to navigate the challenges of addiction recovery.
Legal Consequences and Treatment
Facing legal consequences due to his drug addiction was another significant factor in Downey's path to recovery. The legal issues he encountered served as a wake-up call, prompting him to seek help and make necessary changes. Downey committed himself to a 12-step rehab program, therapy sessions, and other forms of treatment to address his addiction [3].
Through his commitment to treatment, Downey gained a deeper understanding of his addiction and learned valuable strategies to overcome it. The combination of therapy, rehabilitation, and ongoing support proved essential in his journey towards a healthier and sober life.
Rebuilding Life and Career
Rebuilding his life and career was a significant step in Downey's recovery journey. After successfully completing rehabilitation and maintaining his sobriety, he was able to resume his acting career and regain the trust of industry professionals. Downey's dedication to his recovery, coupled with the support of his wife and loved ones, helped him rebuild his personal and professional life.
With a renewed focus and a commitment to sobriety, Downey experienced a career resurgence that included iconic roles, such as Iron Man in the Marvel Cinematic Universe. His ability to overcome addiction and thrive in his career served as an inspiration to many, demonstrating the transformative power of recovery.
The path to recovery for Robert Downey Jr. involved support systems, legal consequences and treatment, as well as the process of rebuilding his life and career. Through the unwavering support of his wife, commitment to various treatment methods, and determination to create a better future, Downey was able to overcome his demons and emerge as a beacon of hope for others facing similar struggles.
Milestones in Sobriety
Throughout his journey of recovery, Robert Downey Jr. has achieved significant milestones that reflect his commitment to a sober lifestyle. These milestones are not only personal victories but also serve as an inspiration to others on the path of recovery.
15 Years of Sobriety
In July 2019, Robert Downey Jr. celebrated a remarkable milestone - 15 years of sobriety [1]. This achievement is a testament to his strength, determination, and ongoing commitment to his recovery. Overcoming the challenges of drug addiction is no easy feat, and reaching this milestone speaks to his resilience and unwavering dedication to maintaining a sober lifestyle.
Achievements and Commitment
Robert Downey Jr. has not only achieved personal milestones in sobriety but has also made significant strides in his personal and professional life. Following over 15 years in recovery, his career has experienced a remarkable resurgence. Studios and directors actively seek him out for roles, marking one of the most impressive comebacks in Hollywood. This resurgence is a testament to his talent, work ethic, and the positive choices he has made in his life.
Robert Downey Jr.'s commitment to sobriety extends beyond himself. He has become an advocate and role model for others struggling with addiction, using his platform to spread awareness and inspire hope. By openly sharing his own experiences and journey, he has shown that recovery is possible and that a fulfilling life can be achieved after overcoming addiction.
These milestones in sobriety highlight Robert Downey Jr.'s determination to overcome his struggles with drug addiction and his ongoing commitment to maintaining a healthy and sober lifestyle. His journey serves as an inspiration to individuals facing similar challenges, proving that with perseverance, support, and a strong personal drive, it is possible to overcome addiction and build a fulfilling life.
Factors Contributing to Recovery
Robert Downey Jr.'s inspiring journey of recovery from drug addiction can be attributed to various factors that played a pivotal role in his path to sobriety. These factors include family support, holistic approaches to sobriety, and the importance of maintaining sobriety and support systems .
Family Support
Family support played a significant role in Robert Downey Jr.'s recovery process. His wife, Susan Downey, and their children became a source of motivation and strength for him. Susan Downey's ultimatum in 2003 became a turning point for Downey, leading him to quit drugs for good. The unwavering support from his family encouraged him to stay committed to his sobriety journey, providing a solid foundation for his recovery.
Holistic Approaches to Sobriety
Robert Downey Jr. adopted a holistic approach to overcome his addiction. He incorporated various practices such as Eastern martial arts, yoga, meditation, and therapy into his recovery journey. These practices helped him find inner peace, maintain discipline, and cultivate a healthier mindset. By focusing on physical, mental, and emotional well-being, Downey was able to address the underlying factors contributing to his addiction and develop healthier coping mechanisms .
Importance of Sobriety and Support Systems
Maintaining sobriety and having a strong support system were crucial elements in Robert Downey Jr.'s recovery process. He committed himself to a 12-step rehab program, therapy sessions, meditation, and Wing Chun Kung Fu. By actively participating in support groups like Alcoholics Anonymous and surrounding himself with individuals who understood the challenges of addiction, Downey found the encouragement and accountability needed to stay on the path of sobriety.
Recognizing the influence of genetics on addiction habits, Downey acknowledged his father's struggles with addiction and his own early exposure to drugs. This awareness allowed him to address family dysfunction and predispositions to addiction, further reinforcing the importance of cultivating a supportive environment that promotes healing and recovery.
In conclusion, Robert Downey Jr.'s recovery from drug addiction was influenced by various factors. The unwavering support from his family, the adoption of holistic approaches to sobriety, and the recognition of the importance of maintaining sobriety and support systems all played integral roles in his inspiring journey towards a healthier and fulfilling life. His story serves as a testament to the power of resilience, determination, and the availability of resources and support in overcoming addiction.
Career Resurgence
Robert Downey Jr.'s path to recovery not only transformed his personal life but also had a profound impact on his professional career. The actor experienced a remarkable resurgence in the industry, marked by blockbuster success, improved industry perception, and a multitude of new opportunities.
Impact on Professional Life
After embracing sobriety, Downey's career momentum significantly increased. In 2008, he starred in the critically acclaimed film "Iron Man" and the action-comedy "Tropic Thunder," which showcased his versatility as an actor. These roles not only reignited his career but also helped reshape the industry's perception of him.
Blockbuster Success
Following the success of "Iron Man" and "Tropic Thunder," Downey's career skyrocketed. He became an integral part of the Marvel Cinematic Universe, portraying the iconic character Tony Stark (Iron Man) in subsequent films, including "The Avengers". His portrayal of Iron Man garnered critical acclaim and resonated with audiences worldwide, solidifying his status as a box office draw.
Downey's career resurgence extended beyond the superhero genre. He showcased his acting prowess in the Sherlock Holmes franchise, starring as the brilliant detective in movies like "Sherlock Holmes" and "Sherlock Holmes: A Game of Shadows". These films further demonstrated his versatility and ability to captivate audiences in diverse roles.
Industry Perception and Opportunities
Prior to his recovery, Downey's struggles with drug addiction had tarnished his reputation in the industry. However, his commitment to sobriety and his remarkable talent allowed him to rebuild trust and regain respect. Industry professionals began recognizing his dedication and applauding his performances, leading to a steady stream of new opportunities.
Downey's career resurgence was partially attributed to Mel Gibson, who personally underwrote his liability insurance in 2003. This support enabled Downey to star in "The Singing Detective" and kickstart his steady work in films such as "Gothika," "A Scanner Darkly," "Zodiac," and "Kiss Kiss Bang Bang". These projects not only showcased his talent but also reignited interest in his abilities as an actor.
The combination of Downey's undeniable talent, his dedication to sobriety, and the industry's recognition of his skills propelled his career to new heights. He became one of the most sought-after actors in Hollywood, with numerous opportunities to collaborate with esteemed directors and work on a wide range of projects.
The career resurgence of Robert Downey Jr. serves as a testament to his resilience and ability to overcome adversity. Through his commitment to sobriety and his exceptional talent, he not only revived his personal life but also reclaimed his status as a critical player in the entertainment industry.
Reflections on Addiction and Recovery
Throughout his journey of addiction and recovery, Robert Downey Jr. has offered insights into his personal experiences, highlighting various factors that influenced his path to recovery.
Acknowledging Genetic Influence
Robert Downey Jr. acknowledges the impact of genetic influence on addiction habits, citing his father's struggles with addiction and his own early exposure to drugs [3]. He recognizes that addiction issues can be a family problem that can be passed down through generations and emphasizes the importance of addressing family dysfunction and predispositions to addiction.
Transformation and Resilience
Reflecting on his journey, Downey emphasizes the transformative nature of recovery. He highlights the need to recognize the significance of denying fate aggressively and emerging from the challenges of addiction stronger [4]. Downey's own resilience and determination to change were crucial in his recovery process, enabling him to overcome the grip of addiction and rebuild his life.
Continuing the Journey of Sobriety
Robert Downey Jr.'s recovery journey is an ongoing process. He emphasizes the need to break free from the cycle of addiction and make lasting changes in one's life. Downey recognizes that addiction does not define a person and that recovery is possible with the right support, motivation, treatment, and resources. By actively engaging in therapies, support groups, and self-care practices, individuals can continue their journey of sobriety and lead fulfilling lives free from the grip of addiction.
Robert Downey Jr.'s reflections on addiction and recovery offer valuable insights into the complexities of the journey. His acknowledgement of genetic influences, emphasis on resilience, and commitment to continuous growth serve as inspirations for those facing similar challenges. By sharing his story, Downey encourages others to seek the necessary support and resources to overcome addiction and embark on a path to recovery.
- https://www.northstarbehavioralhealthmn.com/resources/robert-downey-jrs-drug-addiction
- https://drugabuse.com/blog/robert-downey-jr-s-incredible-comeback-from-addiction
- https://www.casarecovery.com/robert-downey-jr-journey-recovery/
- https://www.vanityfair.com/hollywood/2014/09/robert-downey-jr-cover
Similar articles

From Dopamine to Desires: The Neuroscience of Drugs, Gambling, Sex & the Brain
April 4, 2024
Unveil the neuroscience behind drugs, gambling, and sex! Discover how the brain's response drives desires and addiction.

Power-Packed Hangover Shakes for Recovery
April 22, 2024
Revitalize with power-packed hangover shakes! Discover the ultimate recovery remedy for those rough mornings.

The Role of Play Therapy for Adolescents
June 3, 2024
Unveiling the power of play therapy for adolescents: Explore its role in emotional expression, social skills, and communication.

A Guide to Understanding Adolescents
Demystify adolescent mood swings! Understand the impact of hormonal changes and discover coping strategies for supporting teens.

Harnessing the Power of the Disease Model: The Road to Recovery
May 17, 2024
Unlock the power of the disease model of addiction. Explore brain changes, treatment approaches, and societal impact.

Countering the Surge of Fentanyl Overdose Deaths
March 13, 2024
Confronting the surge of fentanyl overdose deaths: Unveiling statistics, trends, and efforts to combat the crisis.
April 30, 2024

Alarming Social Media Addiction Statistics & Facts
Discover alarming social media addiction statistics & facts. Uncover the impact on mental health and productivity. Don't get lost in the digital abyss!

How to Support Teens Through Mental Health Crisis?
Discover effective ways to support teens through mental health crises. From recognizing warning signs to building trust, empower them to overcome challenges.

Debunking the Myth of Wines Health Benefits
March 17, 2024
Unveiling the truth about wine's benefits. Separate fact from fiction and discover the impact of moderate wine consumption.

What Really Happens in Emergency Outpatient Treatment
May 30, 2024
Unlocking the secrets of emergency outpatient treatment: What really happens when you seek immediate care outside the hospital.

Alcoholism and the Onset of Vertigo
March 28, 2024
Unraveling the link between alcoholism and vertigo. Discover the symptoms, effects, and management options for alcohol-induced vertigo.

Uncovering the Importance of Inpatient Treatment
May 9, 2024
Unveiling the importance of inpatient treatment for effective recovery. Discover structured care, intensive therapy, and round-the-clock support.

Techniques to Address Teen Phobias and Fears
Step by step techniques to help teens conquer their fears and phobias. Expert advice on addressing teen phobias with confidence.

Decoding Addiction: Is it a Disease or a Behavioral Pattern?
Is addiction a disease or a behavioral pattern? Unraveling the truth behind addiction's impact on the brain and its diagnostic framework.

Discovering the Milestones in the History of Drugs
April 3, 2024
Unveiling the captivating milestones in the history of drugs. Explore ancient cultures, colonialism, and groundbreaking advancements. Discover the story behind drug use.

Unveiling the Connection between Alcohol Addiction and Dementia
April 10, 2024
Unveiling the connection between alcohol addiction and dementia. Explore the devastating impact and management options.

Macrobid and Alcohol Interaction: Stay Informed
Stay informed about the hidden risks of Macrobid and alcohol interaction. Understand the impact, risks, and expert recommendations.

Effective Strategies for Addressing School Refusal
March 27, 2024
Discover effective strategies for tackling school refusal. From supportive environments to therapy options, learn how to address this common issue.

Can Alcohol Truly Lead to UTIs?
April 5, 2024
Unveiling the truth: Can alcohol truly lead to UTIs? Explore the connection, symptoms, and how to manage risk.

The Surprising Benefits of Volunteer Work for Teen Mental Health
June 5, 2024
Uncover the surprising benefits of volunteer work for teen mental health. Boost well-being, skills, and community engagement!
Help is just a click away.

'I've Got Cocaine Stories': John Mulaney Got Real About Drug Addiction In His Netflix Special, Had A Hilarious Moment With His Neighbor Afterwards
J ohn Mulaney had quite the year in 2020. The comedian was checked into rehab after his friends staged an intervention. Shortly after he got sober, he met and started dating Olivia Munn who soon became pregnant. The whirlwind ended up being a positive experience for Mulaney, who since then has toured the country with his new family by his side, and released a stand-up special last year called Baby J. He first spoke about his addiction in an SNL monologue which later became the basis for the incredibly vulnerable (and funny) special. Since then, he's had people come up to him to share their own stories, and it even led to a hilarious conversation with his neighbor.
In an interview with Jimmy Kimmel Live! , the stand-up comedian talked to the titular host about some of the reactions he’s gotten from his Baby J special, as well as how he’s doing as he enters his fourth year of recovery. The comedian revealed he has been wonderful since he’s gotten sober, enjoying his time with Munn and son, Malcolm .
He also expressed his happiness that the special connected with so many. He even shared some hilarious anecdotes of strange conversations he’s had as a result of some of the stories he's told. For example, he said his neighbor had a bizarre reaction to it, explaining:
I think what really was very poignant to me was... actually, this was recently. I was leaving my house here in LA and my neighbor Luis came and knocked on the window of my car. I got out and I said, 'Hey Luis, how you doing?' He said, 'I finally watched your special,' and I said, 'Oh thank you for watching.' He goes,' It's OK.'
Clearly, this neighbor is a difficult man to impress. Baby J has gone on to win a number of awards and includes some of Mulaney’s best jokes ever . However, this definitely did not blow Luis out of the water. This neighbor did connect with the special in some way, though, and apparently, it made him want to share stories of his own with Mulaney. The former SNL writer continued:
Then he said, 'But man I've got cocaine stories that are better than yours.' And then he gave me a big bag of lemons. You have a lemon guy on your street?
Like a lemon, Luis had a very sweet and sour reaction. At first, he told Mulaney that he thought the special was only okay, and was nothing on some of the drug stories from his own experience. Then, he gifted the comedian some lemons, a generous offering following a less-than-enthusiastic reception.
It honestly sounds like a hilarious dynamic, and maybe Mulaney will end up including some of these interactions with Luis in his next special. I can’t say I’m not intrigued.
It’s been over a year since the release of Baby J , but the comedian has still been quite busy. He has continued touring and working on material for his next special, which likely won’t materialize for another year. He also has been airing a wacky Netflix live talk show called Everybody’s In LA on the 2024 TV schedule , which has featured guests like Jerry Seinfeld, Bill Hader, and Jon Stewart. The show is only lasting a week, and it has been a unique take on the classic talk format.
The comedian continues to reinvent himself and find ways to express himself in hilarious ways, however, he still may have to work even harder if he wants to impress Luis. Sounds like a great goal.
You can check out John Mulaney’s latest stand-up special Baby J with a Netflix subscription . Fans of the comedian should also check out our feature on Mulaney’s other stand-up specials , and where you can watch them.


IMAGES
VIDEO
COMMENTS
Recovery from addiction is not only possible, it is the rule, rather than the exception. According to the latest U. S. National Survey on Drug Use and Health, more than 75 percent of people ...
Individuals grappling with substance use disorder (SUD) and addiction often face complex challenges, necessitating a multifaceted approach for resolution. The journey to recovery is highly individualized, with diverse paths tailored to unique circumstances. One influential framework guiding this process is the "Transtheoretical Model of Change" (TTM), developed by Dr. James Prochaska and ...
The specifics of every person's addiction journey are different, but for most people, the path to recovery follows a similar trajectory: a "bottom" followed by the decision to take action; the initial, often traumatic physical and mental adjustment to life without the substance; the gradual establishment of a "new normal;" and, somewhere in there, working on the difficulties that led ...
The Submission Package includes a Patient Journey Map depicting the steps a patient must take from the beginning of the drug addiction treatment journey to recovery and a written narrative describing the process the individual or team used to create the map (see requirements below). Both the map and the narrative will be evaluated.
Treatment enables people to counteract addiction's disruptive effects on their brain and behavior and regain control of their lives. The Journal of Neuroscience, 21 (23):9414-9418. 2001. These images showing the density of dopamine transporters in the brain illustrate the brain's remarkable ability to recover, at least in part, after a long ...
About the Report. Addiction Policy Forum's (APF) Patient Experiences Journey Map was developed through the input of patients in treatment and recovery from substance use disorder (SUD). The map underscores the obstacles and positive points patients encounter across seven distinct phases, from treatment to finding long-term, stable recovery.
Health - Overcoming or managing one's disease(s) or symptoms - for example, abstaining from use of alcohol, illicit drugs, and non-prescribed medication if one has an addiction problem- and for everyone in recovery making informed, healthy choices that support physical and emotional well-being; Home - Having a stable and safe place to live; Purpose - Conducting meaningful daily activities ...
Drug and alcohol cravings. During this first phase of recovery, the overarching goals include: 5. Providing a foundation for lasting recovery. Taking recovery one day at a time rather than dwelling in the past or thinking too far into the future, which can be overwhelming. Counteracting the lifestyle of addiction.
The first step to overcoming drug abuse and addiction. Developing an addiction to drugs isn't a character flaw or a sign of weakness, and it takes more than willpower to overcome the problem. Abusing illegal or certain prescription drugs can create changes in the brain, causing powerful cravings and a compulsion to use that makes sobriety ...
Celebrating the journey of breaking the chains of addiction and living a life of freedom and fulfillment. Recovery from drug addiction is a challenging and lifelong journey, but it is also a journey of growth, healing, and transformation. By addressing the root causes of addiction, seeking help, embracing a holistic approach to healing ...
Reaching out for help is the first step toward breaking free from the cycle of addiction and rediscovering the joy of living a life unencumbered by substances. Don't hesitate to reach out to American Recovery Center at 866-484-2502. Together, we can embark on this journey towards a brighter, healthier future.
Addiction recovery stories are personal accounts of individuals who have struggled with drug or alcohol addiction and have successfully overcome their addiction. These stories highlight the challenges, setbacks, and triumphs of the recovery journey, offering hope and inspiration to others who may be struggling with substance abuse.
To this end, a Community-Centered Patient Journey in Drug Addiction Treatment journey map was developed with expert insights, clinical experience, and in-depth interviews (conducted in spring of 2021) with 16 participants enrolled in licensed opioid treatment programs in Tennessee. Patients, policymakers, clinicians, and academic researchers ...
If you believe you or a loved one is suffering from drug or alcohol abuse, we can help. Call us today to learn more about our drug abuse treatment and to get started. Or click here to see more recovery stories. Recovery Centers of America is not affiliated with or endorsed by Alcoholics Anonymous. Call Now 877-520-9659.
Call Today! (859) 757-0717. Find a Provider. Get Directions & Hours. The Journey Recovery Center at St. Elizabeth Physicians is right here for you on your pathway to recovery from opioid addiction and substance abuse disorder.
The case under consideration is a 38 years old patient with a history of chronic addiction with episodes of recovery and relapses. The shift of approaches from the extreme end of the addiction continuum to full recovery poses an opportunity for drug rehabilitation professionals to learn factors associated with drug addiction, the recovery ...
Recovery and crisis stabilization services (e.g., walk-ins). Get Help Today! Learn More about. Substance Use Disorders. The first step is often the most difficult one. Our trained specialists are here to help, contact us today to start your recovery journey. Call (859) 757-0717. Dedicated, highly trained professionals, licensed within their ...
Recovery From Addiction Is a Journey. There's No One-and-Done Solution. By Bernard J. Wolfson June 6, 2023. Disponible en Español. Willard Sexton has been through court-mandated residential addiction rehab twice and is now a staff member at Allen House, a safety-net drug treatment center. He says he understands how stressful it is to stop using.
Journey to Recovery, narrated by Grammy-nominated recording artist and Kentucky native Sturgill Simpson, airs Monday, Feb. 13 at 8/7 pm on KET. The documentary examines an array of treatment and recovery programs offered across the state, including abstinence-only programs - such as faith-based and 12-step based programs - as well as ...
Getting help is as easy as picking up the phone. We will answer all your questions and provide an assessment. We will help arrange for you to come to the program and begin recovery. JourneyPure is a leading substance abuse and mental health treatment provider for adult men and women with residential and outpatient locations across the southeast.
Journey Drug Addiction Rehabilitation Centre, Johannesburg. 4,173 likes · 270 talking about this · 76 were here. Journey Rehabilitation Centre is a registered upmarket, exclusive mental health care...
In this powerful episode, we delve into the deeply personal story of Harrison, a man who battled with addiction from a young age. From the allure of substances to the depths of despair, Harrison's journey through addiction was tumultuous and heartbreaking. He candidly shares his struggles, admitting…
Factors Contributing to Recovery. Robert Downey Jr.'s inspiring journey of recovery from drug addiction can be attributed to various factors that played a pivotal role in his path to sobriety. These factors include family support, holistic approaches to sobriety, and the importance of maintaining sobriety and support systems.
John Mulaney had quite the year in 2020. The comedian was checked into rehab after his friends staged an intervention. Shortly after he got sober, he met and started dating Olivia Munn who soon ...