Déréalisation, questions existencielles suite à un bad trip
Bonjour/Bonsoir Je me présente, Jean, 27 ans. Suite à une prise d'ecstasy en trop forte quantité j'ai fait un badtrip avec hallucinations. Ces hallucinations étaient très réalistes et troublantes (pas psychédéliques) comme des bugs visuels sur le réel. Je me souviens avoir vu des écritures apparaitre sur plusieurs surfaces, des bulles dans des verres vides, voir un ami avec la tete de quelqu'un que je ne conaissais pas, voir un ami en vieux, ou un autre avec des yeux tous noirs bref au début amusant mais a la fin flippant... Je tiens a preciser que c'est la deuxieme fois que je prends de l'ecstasy et la premiere je n'avais quasiment pas eu d'effets. Je suis de nature timide, j'angoisse pour pas grand chose, j'ai peur d'avoir une maladie grave dès que j'ai une douleur etc. Bref retour chez moi tout seul après ce weekend avec mes amis et cette fameuse soirée, 1-2 semaines pour m'en remettre physiquement et mentalement déja.. mais en meme temps gros soucis avec mon entreprises montée il y a deux ans avec mon meilleur ami. A vrai dire les soucis ont commencé une semaine avant cette soirée. J'avais du lui annoncer avec beaucoup de regret qu'il devait quitter l'entreprise pour des raisons de particpations etc. pour resumer, nous etions a 50% chacuns mais je faisais tout le travail seul depuis deux ans.. puis entre temps la soirée, et quelques jours après mon retour mon plus gros client qui me lache pour des raisons importantes. Je me retrouve a devoir virer trois employés à contre coeur et faire face a un trou de tresorerie en ne sachant pas comment je pourrais payer mon appartement etc. et tous mes autres clients me mettant la pression pour finir les projets en cette fin d'année. - petite precision la dessus, je travaille seul de chez moi et ait mes equipes en teletravail et nous nous reunissons a peu près une fois par mois - Et s'est déclanché à ce moment là une obstination a comprendre le sens de la vie, d'ou vient-on, qui a creer l'univers... - je précise que j'ai grandi dans une famille chrétienne très pratiquante et que j'ai coupé avec la religion vers mes 15 ans lors de mon entrée en internat - Ce qui m'amena ensuite vers cette sensation terrible d'avoir l'impression d'etre passé dans un autre univers et de ne plus etre chez moi, ou d'etre dans un Trueman Show géant.. Comme si je devais trouvé la sortie, je devais trouver la solution, la verité. Je m'etais déjà questionner vaguement lors du début de mon adolescence sur qui etais-je, pourquoi moi, etc. Si je m'en souviens c'est que j'avais du pas mal ruminer sur le sujet déja, mais bon pas à ce point. J'ai passé les fêtes avec ma famille, j'ai pu décrocher parfois de ces idées mais elles me rattrapaient de plus belle, me disant que même les gens de ma famille n'etaient pas reels ou etaient des acteurs etc. Mais j'arrive a le cacher et a ne pas l'exprimer mais a l'interieur c'est une bombe emotionelle. J'ai fait plusieurs soirées également avec des amis : au bout de deux trois verres plus aucun soucis et je vis dans le moment présent ! Mais le lendemain est un enfer.. Autre point, quand j'ai ce sentiment, le moindre detail que je ne comprends pas, bruit etc. me rend parano car j'estime que je peux trouver une preuve que je ne suis pas dans la réalité.. J'ai commencé a lire et a me documenter sur les pensées des grands philosophes sur ces questions existencielles. Egalement me renseigner sur l'astronomie pour en savoir plus. Mais en réalité j'ai peur de devenir un illuminé complotiste criant sur la place du marché que la terre est plate et que l'homme n'est jamais allé sur la lune et que nous sommes controllés et manipulés par des grands monarques etc. Bref j'ai réellement besoin d'aide car cela me prend enormément de temps de cerveau, je travail beaucoup moins par ce fait.. Je pense tellement que j'ai réussi a remplir 4 copies A4 sur le sujet et sur mes pensées en moins d'une demie heure.. J'ai consulté une psychiatre qui m'a prescrit du Xanax, mais j'en ai pris trois fois, l'effet est vraiment efficace mais le problème reprend le lendemain.. j'imagine que c'est un combat contre moi même que je dois mener la, c'est pourquoi j'ai besoin d'etre accompagné. Merci pour vos avis et votre aide
Réponse envoyée
Nous validerons bientôt votre réponse pour ensuite la publier
Une erreur s'est produite
Merci de réessayer plus tard
Réservez un rendez-vous immédiat en ligne pour 49 €
Obtenez une aide psychologique en moins de 72 heures avec des professionnels en choisissant le créneau horaire qui vous convient le mieux.
Bonjour, Si vous avez déjà tendance à l'angoisse et à la peur face aux maladies, la pire chose que vous puissiez faire est de consommer ce type de drogue, car les effets peuvent être des hallucinations comme celles que vous mentionnez, de l'agitation, de l'anxiété, dépersonnalisation, des crises de panique et de brefs épisodes de psychose. Peut-être que votre intérêt pour les questions existentielles est une façon de vous détourner des sérieux défis professionnels auxquels vous faites face. La consommation d'extase et la recherche d'expériences transcendantales sont deux choses qui peuvent se renforcer mutuellement, avec des risques de détachement de la réalité et de troubles mentaux et comportementaux. Le mieux est que vous essayiez d'atteindre un équilibre psychologique et émotionnel avec l'aide d'une thérapie, par exemple, grâce à des techniques adaptées comme l'hypnose, la TCC et autres afin de pouvoir assumer vos responsabilités de manière sereine. Je suis disponible si besoin, bien à vous, Nilton Mascarenhas, Praticien en Hypnose Ericksonienne et Thérapie Brève.
540 réponses
5007 J'aime
Réalisez une thérapie en ligne
Merci d'avoir donné votre avis !
23 réponses
Bonjour Jean, Le Xanax calme, certes, mais il n'humanise pas : psychothérapies "value-free" ou "value-laden", vous pouvez prendre le meilleur de chacune en fonction de votre sensibilité propre et de votre vécu subjectif. Qu'est-ce qui VOUS ferait du bien aujourd'hui ? De la bombe humaine au greatest Showman, il y a vos rêves et votre imagination.... pas nécessairement un combat contre vous-même. Je vous invite à visiter l'onglet "pour aller plus loin" de mon site internet et si mon approche vous parle, je suis à votre disposition par mail pour vous aider à y voir plus clair et/ou à trouver la bonne personne pour vous accompagner dans votre région (je suis à Rouen et ne pratique pas à distance). Je suis ok pour vous lire si vous voulez partager vos questionnements et/ou vos écrits, en toute confidentialité évidemment. Votre quête, vos douleurs et l'énergie que vous déployez pour vous développer m'interpellent humainement. Ecrivez, oui... Ce n'est jamais inutile. Lisez les grands maîtres... et les autres, restez surtout fidèle à vos valeurs pour trouver vos propres chemins de traverse : "L'homme mérite qu'il se soucie de lui-même car il porte en son âme les germes de son devenir." (Carl Jung) Bien à vous, AF
71 réponses
114 J'aime
Bonjour Jean, Quand on est déjà psychologiquement affecté par le contexte de sa vie, la consommation de ce type de drogue amène souvent à faire ce qu'on appelle une décompensation psychotique. Vous avez bien fait d'aller voir un psychiatre et de prendre des médicaments antidépresseurs mais cela n'est pas suffisant. Je vous suggère d'entamer un travail de psychothérapie pour aller explorer ce qui se passe pour vous en ce moment, quelles en sont les origines et pouvoir changer vos croyances sur vous, sur les autres et sur le monde afin de retrouver un fonctionnement normal. Je vous souhaite bon courage! Frédéric Duquerois Psychopraticien en Analyse Transactionnelle Adultes et Couples, en Individuel et en Groupe Nantes
358 réponses
92 J'aime
Bonsoir Jean, Il arrive, après un bad trip, que des questions existentielles se posent. Ce genre d'expérience peut engendrer une sorte d'état dépressif qui remette en cause le sens de l'existence. Par ailleurs dans votre message, vous semblez exprimer quelques expériences de déréalisation "les gens de ma famille n'étaient pas réels ou étaient des acteurs". Ceci peut-être le signe d'un état de stress aigu. La déréalisation étant un système de défense pour affronter une réalité qui semble trop difficile. Dès le début de votre message, vous présentez, également, comme une personne timide et angoissée. De toute évidence, vous entrez dans une période de grand questionnement et probablement de transition de votre parcours de vie. il me parait important que vous entamiez un travail personnel avec un ou une psychopraticienne pour traverser cette étape au mieux. Je reste évidement à votre disposition si vous le souhaitez. Bien à vous, Philippe MATHIAS
197 réponses
103 J'aime
Bonjour Jean, Vous avez rédigé un long message ici dans la section "Questions" mais aussi en remplissant 4 copies papier comme vous le mentionnez, et peut-être cela vous a-t-il fait déjà fait un - tout petit peu - de bien de poser ceci par écrit. L'écriture permet parfois de mettre des mots sur ce qui pose problème et sur ce qui peut-être inquiétant... Cela n'est néanmoins pas suffisant et démarrer une thérapie avec un professionnel vous permettrait vraiment de verbaliser et d'évoquer plus en profondeur les différents sujets qui vous traversent actuellement (expériences avec les drogues, préoccupations au travail, sens que vous voulez donner à votre vie, identité...). Vous avez besoin visiblement de comprendre tout ce qui se passe en vous, vos émotions, vos pensées et l'angoisse que vous ressentez à certains moments (seul mais aussi avec vos amis, vos proches...). Avec un praticien en psychothérapie, vous ne serez également plus seul pour faire face à votre anxiété et vos questionnements existentiels tant personnels que professionnels (notamment celui de trouver votre place dans ce vaste monde). Cela sera très complémentaire de vos lectures sur l'astronomie et sur la philosophie qui vous apporteront aussi de la connaissance et sans aucun doute quelques réponses... Je vous souhaite de trouver la personne qui pourra vous permettre de vous épanouir, d'avancer sur le chemin des réponses que vous cherchez et d'acquérir une certaine sérénité. Roseline ARBELET Psychanalyste humaniste et thérapeute intégrative - En présentiel à Boulogne Billancourt et en visioconsultation -
29 réponses
15 J'aime
Bonjour Jean, Merci pour votre message qui me touche particulièrement. Vous êtes en quête de sens et vous vous posez donc des questions existentielles. Je ressens le fait que vous êtes perdus dans votre vie, et la prise de drogue permet d'oublier la réalité et toutes ces questions que vous vous posez. Il ne faut pas que vos questions existentielles viennent vous couper de la réalité. La quête de sens ressort souvent au cours d'une vie, et elle peut être plus ou moins profonde. En voulant absolument comprendre l'univers, vous n'êtes pas dans votre zone d'influence. Il est important que vous reveniez à vous et que vous puissiez identifier ce que vous vous voulez faire de votre vie. Et en revenant à cela, vous allez pouvoir calmer vos angoisses et surtout devenir acteur de votre vie. Une thérapie en parallèle d'un accompagnement psychiatre a du sens. Prenez soin de vous. Anne-Sophie (psycho praticienne Gestalt)
79 réponses
27 J'aime
Bonjour Jean, L’alcool et les drogues sont souvent un auto traitement contre une anxiété de base, dans une recherche d’apaisement qui n’est que temporaire. Votre « bad trip » montre les risques que vous prenez avec les drogues, qui sont assez considérables à l’ère où on peut vous vendre des produits très dangereux, qui produisent des effets néfastes pour la santé mentale et physique. Vous écrivez être anxieux depuis toujours, timide et hypocondriaque : la Xanax n’est pas une solution, puisque ce médicament n’a qu’un effet de courte durée et pris à la longue crée aussi (comme les drogues…) une dépendance. Le mieux serait de vous lancer dans une bonne psychothérapie qui vous permettra petit à petit de mieux réguler vos émotions et de canaliser vos pensées vers les buts qui vous occupent actuellement, notamment pour résoudre vos problèmes professionnels immédiats. Vous avez besoin de parler de tout ce que vous ressentez et vos questions existentielles, naturelles à votre âge, mais qui ne doivent pas vous occuper trop l’esprit : il faut renouer avec les réalités de la vie, dont certaines sont désagréables, mais qu’il faut parfois affronter et accepter. Je vous souhaite de prendre conscience de la nécessité de vous offrir cette nécessaire thérapie qui vous aidera à gagner en sérénité et à bien vivre tous les événements de la vie, et sans aucun drogue… sp
4377 réponses
12020 J'aime
Bonjour, il est temps de remettre de la dissociation dans ta vie . Il y a un travail à faire sur le retour à la conscience du ici et maintenant. Grâce à la pnl et l’hypnose on peut retourner à l’endroit où tous a commencé et transformer cela . Cela va te permettre de te raconter une autre histoire plus adapté à ce que tu veux vivre Pour améliorer ta vie il est nécessaire de t’en faire une représentation multi sensorielle pour en mesurer le succès .. Vision Direction Efficacité Excellence Développement personnel Communication efficace Qualité relationnelle Prendre rdv David Sellier
191 réponses
116 J'aime
Bonjour Jean, Je tiens tout d'abord à vous exprimer ma compréhension et ma reconnaissance pour le partage de votre expérience et de vos préoccupations. Il est évident que vous traversez une période complexe et intense, et je souhaite vous offrir mon soutien dans votre démarche. Il est significatif de noter que, dans l'approche gestaltiste que je propose, nous ne considérons pas votre cheminement comme un combat, et encore moins comme un affrontement contre vous-même. Au contraire, il s'agit d'un retour à vous-même, à votre essence, et à la quête de sens dans votre existence. La philosophie existentialiste qui sous-tend la Gestalt-thérapie met en lumière cette recherche profonde de sens, de compréhension de soi et du monde qui nous entoure. Les effets de votre expérience avec l'ecstasy ont suscité des questionnements existentiels et ont amplifié votre réflexion sur la réalité, la vie, et votre place dans l'univers. C'est un processus délicat, mais je vous encourage à considérer cette exploration comme une opportunité de croissance personnelle. La Gestalt-thérapie intégrative, par son aspect intégratif, peut offrir des outils efficaces pour explorer et comprendre ces préoccupations, ainsi que pour travailler sur des stratégies qui vous permettront de vivre plus sereinement au quotidien. En travaillant ensemble, nous pourrions explorer les origines de votre anxiété, les mécanismes de vos pensées intrusives et élaborer des moyens concrets pour les gérer. Cependant, il est crucial de souligner que la Gestalt-thérapie ne peut en aucun cas se substituer au traitement médical prescrit. Votre démarche auprès d'une psychiatre et l'utilisation de médicaments sont des aspects importants de votre prise en charge, et mon accompagnement serait complémentaire à ces approches. Je suis touché par votre situation et souhaite vous proposer mon soutien dans votre démarche de compréhension du sens de la vie et de vos interrogations afin que vous trouviez vos réponses. La quête existentielle peut être un chemin complexe, surtout si l'on est seul à l'arpenter, mais elle peut également être source de découvertes enrichissantes sur soi-même et sur le monde qui nous entoure. N'hésitez pas à me contacter pour discuter plus en détail de la façon dont je pourrais vous accompagner dans ce processus, tout en travaillant en collaboration avec votre traitement médical actuel. Je vous adresse tout mon soutien et mes encouragements dans cette étape de votre vie. Bien à vous, Laurent FARRET Gestalt-Praticien Accompagnement humaniste pour le bien-être mental, émotionnel, et relationnel
202 réponses
2119 J'aime
Bonjour Jean, Votre histoire reflète une quête de sens profonde, exacerbée par un épisode psychédélique intense. Cette expérience avec l'ecstasy me semble être comme une tentative de dépasser certaines de vos limites personnelles, comme pour mieux comprendre votre place dans le monde. Votre désir ardent de comprendre la vie et l'univers est à la fois une quête noble et une source de potentielle tension. Malgré tout, cette pulsion est bénéfique tant qu'elle enrichit votre vie sans la dominer ni la perturber. Vous êtes à un carrefour où il me semble judicieux de faire le point sur ce que vous avez appris jusqu'à présent. Revenir "les pieds sur terre" est une métaphore de la nécessité de se reconnecter avec la réalité concrète pour retrouver un équilibre entre vos aspirations et vos possibilités. Se tourner vers la philosophie et les expériences humaines universelles, telles que celles reflétées dans les mythes, peut vous offrir des perspectives enrichissantes si vous souhaitez vous en servir de miroirs pour comprendre votre propre expérience, cela vous aidera surement à donner un sens à ce que vous traverser actuellement. Le Xanax offre certes un soulagement temporaire, mais il est important de poursuivre une thérapie pour explorer les problèmes à la racine. Le travail thérapeutique vous aidera à naviguer dans ces questions complexes et à trouver des réponses plus durables et constructives. Je reste à votre disposition, Lucas Bielli Psychanalyste
19 réponses
11 J'aime
Bonjour Jean, Vous avez déja mis "le doigt" sur des points importants de votre vie. L'écriture est un point très positif afin d'évacuer votre trop-plein. Les ruminations mentales dont vous parlez, sont l'expression d'un ou plusieurs éléments/situations/affects/possible traumas refoulés. Par cette prise d'ecstasy "trop forte", peut être y avait-il un besoin inconscient, d'expression de ce refoulé ? L'expérience que vous avez vécu sous ecstasy est propre à cette drogue. Malheureusement, à la redescente les angoisses, anxiété initiales sont amplifiées. Votre réelle besoin de comprendre votre état est très positif à l'entrée en thérapie. Le Xanax prescrit par le psychiatre peut surement vous aidez ponctuellement, mais en parallèle une thérapie dans le domaine qui vous parle est a priori nécessaire. Je vous invite à vous renseigner sur les différentes thérapies et en choisir une qui "vous parle". Je me permets de rajouter que vous concernant, une prise en charge globale semble nécessaire. Une thérapie qui ne s'occupera pas seulement des symptômes, qui les prendra en compte certes mais qui ira "plus loin" dans l'analyse. Ce que vous cherchez déja à faire seul. Ayez confiance en vous, vous êtes déja sur le chemin de la réflexion. Bonne journée à vous
Bonjour Jean, Il semble que vous ayez traversé une période complexe et troublante, votre histoire personnelle reflète une quête de sens profonde, exacerbée par un épisode psychédélique intense et des défis dans votre vie professionnelle. Voici quelques éléments de réflexion en tant que psychanalyste : Votre désir ardent de comprendre la vie et l'univers est à la fois une quête noble et une source de potentielle tension. En effet, cette pulsion est bénéfique tant qu'elle enrichit votre vie sans la dominer, sans la perturber. Cette expérience avec l'ecstasy semble être comme une tentative de dépasser certaines limites personnelles, comme pour mieux comprendre votre place dans le monde. Vous êtes à un carrefour où il me semble judicieux de faire le point sur ce que vous avez appris jusqu'à présent. Revenir "les pieds sur terre" est une métaphore de la nécessité de se reconnecter avec la réalité concrète, quotidienne, et de trouver un équilibre entre vos aspirations et vos possibilités. Se tourner vers la philosophie et les expériences humaines universelles, telles que celles reflétées dans les mythes, offre des perspectives enrichissantes si vous souhaitez vous en servir de miroirs pour comprendre votre propre expérience, vous aidant à contextualiser et à donner un sens à ce que vous avez vécu. Votre récit suggère une sensibilité émotionnelle et une anxiété profondément ancrée, actuellement exacerbées par les récents événements. Il est important de reconnaître et d'aborder ces aspects de votre personnalité dans votre cheminement thérapeutique, et progressivement, de chercher les causes. Le Xanax offre certes un soulagement temporaire, mais il est important de poursuivre une thérapie pour explorer et résoudre les problèmes sous-jacents. Le travail thérapeutique vous aidera à naviguer dans ces questions complexes et à trouver des réponses plus durables et constructives. Bien à vous, Lucas Bielli Psychanalyste
Bonjour Jean, Vos interrogations existentielles démontrent une grande sensibilité et des capacités intellectuelles plutôt très bien développées. La remise en question des valeurs dans lesquelles on a été élevé est aussi une étape d'émancipation nécessaire pour devenir Adulte. Le fait que vous vous soyez autorisé cette démarché va également dans le sens d'une intelligence de coeur. Et bien sûr, lorsque l'on n'est plus protégé par les dogmes et les certitudes de notre éducation, cela nous expose forcément à une angoisse existentielle à laquelle tout être humain doit faire face. C'est à e prix que nous réussissons à nous construire non plus dans des certitudes mais dans une Foi en la Vie... Le prix à payer de vos capacités est de devoir faire face à cette angoisse existentiel. Vous évoquez par ailleurs une difficulté face aux aléas de l'existence, qui se manifeste chez vous par une anxiété que vous avez du mal à gérer. C'est encore différent de l'angoisse existentielle et il ne faut pas les confondre. Ce terrain anxieux peut avoir été augmenté soit par des expériences de vie difficiles dans l'enfance ou, au contraire, un cocon trop protecteur qui ne permet pas de s'aguerrir face au principe de Réalité (responsabilités, risques, imprévus, échecs, maladie, mort, etc.) Votre anxiété fait que vous avez recours à des substances anesthésiantes (drogues) qui vous apportent un soulagement temporaire et font baisser la pression intérieure que vous ressentez face aux situations difficiles. Malheureusement, la consommation de ces substances ne peuvent qu'aggraver votre situation puisqu'elles augmentent l'anxiété, peuvent générer délires paranoïaques et hallucinations, et même déboucher sur une schizophrénie irréversible si vous n'y prenez pas garde. Vous entrez en réalité dans un cercle vicieux ! Je vous invite donc à entreprendre une psychothérapie afin d'apprendre à mieux savoir faire avec le principe de réalité, mieux gérer votre anxiété et trouver en vous les ressources pour résilier. Car vos difficultés ne sont pas une fatalité et il vous est possible d'en sortir. Bien à vous, Caroline GORMAND Psychothérapie intégrative, thérapie systémique du couple et de la famille, coaching relationnel (Visio consultations et consultations en présentiel, sur rendez-vous)
1861 réponses
2659 J'aime
Bonjour Jean, Ne pensez-vous pas que derrière les questionnements existentiels et la prise de drogue par deux fois, se cache un terrain profondément anxieux? La prise de cet anxyolitique de base de la pharmacopée vous a soulagé mais son effet est ponctuel, à la convenance de vos prises prescrites; le problème de fond doit être mis en exergue, exhumé de votre psyché en mettant par la parole des mots sur vos axiométiques de prédilection dont vous parvenez à remplir des pages entières. C'est bien de travailler sur ses pensées, signe de votre volonté à sortir de ce mal-être prégnant dans l'ensemble de votre récit, que ce soit dans votre nécessité d'annoncer à votre collègue son départ professionnel ou un ensemble de ruminations. Mais ne vous mettez pas dans un état anxieux encore plus présent sachant que tourner en boucle seul sur des problématiques de cet odre ne peut qu'amplifier votre souffrance psychologique et vous conduire à des badtrips. L'usage des stupéfiants induit dans les trois quart des situations des états d'hallucinations ( visuelles ou auditives, etc....), des délires souvent proches des symptîomes de la clinique des psychoses même ce n'en est pas sur le plan de la santé mentale. Vous avez eu parfaitement raison de sonsulter un médecin psychiatre mais le combat que vous énoncez très bien doit se poursuivre par une psychothérapie, afin de comprendre votre mal-être, vos interrogations actuelles et plus archaïques sur l'existence, de faire une démarche d'introspection pour vous connaître enfin et modifier votre schéma de pensée, par là même vos comportements. Je vous invite sincèrement à suivre une Psychothérapie en téléconsultation ou en cabinet pour résoudre vos problèmes en étant accompagné en toute bienveillance et neutralité. Vous en avez le potentiel, alors agissez ! Je reste à vos écoute si besoin en téléconsultation. Bien chaleureusement. Bénédicte ESCARON Psychanalyste Praticienne en Psychothérapie intégrative. Thérapeute TCC ( grande anxiété, stress post-traumatique)
892 réponses
9304 J'aime
Bonjour Jean. La sensation de déréalisation, en particulier la sensation que des personnes sont irréelles, m'interpelle. En avez-vous parlé à votre psychiatre? Les questionnements philosophiques, existentiels, peuvent être épanouissants et passionnants, mais je constate dans votre message que ça génère une certaine anxiété : les moments où vous lâchez prise temporairement, comme avec le Xanax ou l'alcool, semblent si je ne me trompe pas vous apaiser plus que la fois où vous avez rempli quatre copies A4. Je vois également que vous traversez une crise professionnelle importante, et qu'à l'adolescence vous avez également traversé une crise qui est loin d'être négligeable, avec une forte remise en question des croyances que vous aviez jusque là (et que votre famille continue d'avoir). Je pense en effet qu'un accompagnement thérapeutique pourrait vous être profitable, avec un espace d'écoute bienveillant qui pourrait vous permettre de vous parler de ce qui éventuellement vous angoisse derrière tous ces questionnements philosophiques, et à terme soit de passer à autre chose soit de continuer à vous y engager d'une façon plus épanouissante et choisie. Grégoire Taconet Psychopraticien en Approche Centrée sur la Personne Consultations en cabinet à Lyon, ou en visio
60 réponses
29 J'aime
Bonjour Jean , Merci de votre confiance. Je vous donne un éclairage. Il y en a d'autres , voici le mien. Prendre de l’ecstasy, ou boire de l'alcool vous permet d'entrer en contact avec les profondeurs cachées de votre inconscient, avec cette entité sauvage qui ne demande qu'à être apprivoisée que l'on nomme l'ombre ( dans notre jargon !) . L'attrait pour les drogues ou l'alcool provient de la recherche du côté ombrageux de son être. Vous serez dans une angoisse et une insatisfaction tant que vous n'aurez pas reconnu la partie de vous qui se cache dans l'ombre. reconnaître, apprivoiser, réintégrer ses ombres fait partie du travail de tout un chacun, et pour certaines personnes il est plus important, plus complexe, plus urgent ...en fonction du milieu familial, social, religieux... dans lequel on a grandi. Le travail personnel qu'on effectue sur son ombre constitue une condition essentielle pour qui souhaite devenir une personne équilibrée et entière. Pour faire court :L'ombre c'est tout ce que nous avons refoulé dans l’inconscient par crainte d'être rejetés par les personnes qui ont joué un rôle déterminant dans notre éducation. C'est comme un obscur trésor , comme une énergie psychique compressée , vivante , active. Faire ce travail vous aiderait en tout point, et même vis à vis de cette timidité, de ces angoisses et peurs que vous nommez. "ce n'est pas en regardant la lumière qu'on devient lumineux mais en plongeant dans son obscurité..." dit Jung. Je vous recommande l'ouvrage "apprivoiser son ombre". Et de vous faire accompagner. Bon courage bien à vous Marie Do de Kerangat
73 J'aime
Bonjour Jean, Vous traversez des épreuves difficiles notamment dans votre travail, qui prend beaucoup de place dans votre vie. faites attention au surmenage ! l'ecstasy n'est pas une bonne solution pour votre santé, je vous déconseille de la réutiliser. Vous avez besoin d'extérioriser vos pensées, les écrire est une bonne chose mais les oraliser c'est mieux et vous vous sentirez plus libre. je vous propose de vous accompagner à trouver la force en vous pour affronter vos peurs, et angoisses. Ma première consultation en cabinet ou en téléconsultation est gratuite. Nathalie Dodret Psychopraticienne spécialisée en psychologie du travail, aide à la parentalité psychanalyse et traitement de l'anxiété, angoisse, estime de soi, dépression, confiance en soi
61 réponses
17 J'aime
Bonjour Jean, A la base vous êtes quelqu'un de très angoissé et cette angoisse vient sûrement de loin, de votre enfance. Cela mériterait d'être exploré. Sur ce fond d'angoisse vous avez pris de l'ecstasy et cela ne vous a pas aidé. Cela n'est malheureusement pas rare que la prise de stupéfiant déclenche de grosses crises d'angoisse, surtout quand le terrain est favorable. Ce sont des effets autonomes de la substance qui peuvent apparaître même chez des personnes peu angoissées. En plus il semble que la charge ait été importante. Compte tenu des soucis professionnels (dont vous n'êtes nullement responsable) vous êtes actuellement dans un trou d'angoisse qui se traduit par une forme de dépersonnalisation et de déréalisation. Le xanax a une durée de vie relativement faible. Il agit vite mais ne dure pas dans le temps. Il est bon de le prendre à la demande, pour pallier une crise, mais ce n'est pas un traitement de fond. Si les crises devaient durer il faudrait probablement voir avec votre psychiatre pour passer sur un antidépresseur à effet anti-phobique et sans accoutumance (comme le xanax). Reste que ce serait effectivement bien que vous soyez accompagné afin d'apprendre à relativiser vos angoisses. Je reste personnellement à votre disposition, sachant que ma première séance d'une heure est entièrement gratuite et sans engagement. Vous pouvez librement prendre un rendez vous sur mon agenda en ligne. Bon courage à vous Michel le BAUT Psychopraticien Thérapeute Jungien Analyse de rêves
4219 réponses
21783 J'aime
Jean, votre expérience résonne profondément avec les séquelles psychologiques souvent observées à la suite d'épisodes de toxicomanie. Les hallucinations et la déréalisation que vous avez vécues ne sont pas rares après une consommation excessive d'ecstasy. Ces substances peuvent déclencher des angoisses latentes, amplifier les peurs sous-jacentes et les interrogations existentielles, en particulier chez les personnes prédisposées à l'anxiété, comme vous l'avez décrit vous-même. Ce sentiment d'irréalité et de détachement, ainsi que vos intenses réflexions existentielles, découlent probablement du stress accru que vous subissez. Les bouleversements dans votre vie professionnelle et les changements brusques dans vos relations personnelles peuvent amplifier les sentiments de déconnexion et d'irréalité. Votre cerveau, pour tenter de faire face à la situation, peut revenir à ces questions existentielles comme une forme de distraction ou une tentative de contrôle dans un environnement apparemment chaotique. Il est essentiel d'aborder ces sentiments avec un soutien thérapeutique. La psychothérapie peut être bénéfique pour répondre à vos angoisses et vous aider à recadrer vos pensées. Mon cabinet offre un environnement compatissant et compréhensif pour explorer ces questions. La première consultation est gratuite et permet de discuter de vos expériences et de commencer à élaborer une approche personnalisée de votre guérison. N'oubliez pas que le fait de demander de l'aide est un signe de force et non de faiblesse. Vous n'êtes pas seul dans cette aventure. Lorena Salthu Conseils téléphoniques personnalisés. Urgences pendant le weekend Psychopraticien -Coach de vie-Psyconeuroimmunologist -Psychanalyste Séances en ligne ou en présentiel. Français, English et Español
818 réponses
2808 J'aime
Bonjour Jean Vous nous décrivez une situation d'épuisement émotionnel, vos soucis de travail n'y sont pas étranger, vous êtes dans un processus qui peut vous conduire à un burn-out. Cela commence toujours par une trop forte charge mentale qui génère stress et angoisses, celle-ci dans votre cas vienne s'appuyer sur une sensibilité particulière aux angoisses qui en amplifient les effets. Si l'on ajoute que vous avez dû faire face à des prises de responsabilité compliquées et que vous travaillez de chez vous relativement isolé, tous les ingrédients sont réunis. Le burn-out a la particularité de venir saper en profondeur et à bas bruit, l'identité professionnelle puis l'identité personnelle. Cela explique que vous soyez dans ce questionnement existentiel donc identitaire, ce questionnement qui vous prend de plus en plus de place dans votre vie psychique et qui finit par vous couper de la réalité. La prise de drogue est venue mettre au jour tous ces tiraillements psychiques, elle n'en est que le révélateur qui s'est exprimé sous forme d'hallucinations. La prise d'alcool n'est qu'un inhibiteur qi ne résout rien. Il est temps pour vous de remettre tout ceci en perspective, de retrouver qui vous êtes. Vous avez de nombreux acquis, professionnels, familiaux, sociaux sur lesquels vous appuyer. Il est temps de prendre un peu de recul quant à votre activité professionnelle. Je vous conseille de vous faire accompagner dans cette période difficile, cela vous permettra de la traverser dans de meilleures conditions. Je peux vous accompagner si vous le désirez. Je reste à votre disposition si vous souhaitiez approfondir cet échange, n'hésitez pas à me contacter. Cordialement Bruno BRICE Thérapeute Narratif Psychopraticien Accompagnements en cabinet et en visio
426 réponses
200 J'aime
Bonjour Jean, Effectivement, la consommation de drogues peut provoquer ce que vous évoquez, c'est assez classique comme réaction, même si cela ne vous l'a pas fait la 1ère fois. La prise de drogue a souvent des conséquences délétères et laisse comme vous le précisez une sensation de dépersonnalisation/déréalisation et parfois également provoquer une sorte de délire paranoïaque ou mystique... Vous ne précisez pas depuis quand date ce bad trip ? Le Xanax qui est un anxiolytique peut vous aider ponctuellement mais aussi provoquer une accoutumance à ce médicament. Quoiqu'il en soit, je vous conseille de consulter un thérapeute qui sache travailler sur le sujet avec des techniques spécifiques (voir mon profil) pour désactiver l'impact émotionnel et cognitif. J'ai déjà traité ce type de problématique. Cordialement Hypnothérapeute clinique - Thérapie intégrative & holistique
5366 réponses
31416 J'aime
Bonjour, IL semblerait qu'avant même la prise d'ectasy, vous ressentiez un énorme stress qui n'a fait qu'empirer par la suite. De manière générale, nous avons tous en nous des mécanismes de défense qui nous aide à réguler notre stress. Cependant, cela demande de l'énergie. Dans votre cas, il semblerait que votre travail vous demande beaucoup d'énergie en ce moment et provoque une grande pression sur vos épaules. Il est fort possible que vous soyez en état de fatigue mentale. Ainsi, vous n'avez plus la force de mettre des barrières à vos pensées stressantes, qui prennent finalement le dessus : D'où toutes ces questions existentielles. Dans votre cas, il serait très aidant de consulter un.e psychologue. Vous avez besoin d'un endroit pour déposer tout ce stress et comprendre son origine pour pouvoir s'en détacher. L'aide d'un professionel vous permettra d'avoir des outils pour réguler votre stress tout en apprenant à mieux vous comprendre. Je reste à votre écoute, Gwenaël THING-LÉOH Psychologue - Psychothérapeute
277 réponses
1039 J'aime
Bonjour Jean, La drogue a provoqué une très forte décompensation et je pense que vous devriez revoir votre psychiatre pour mieux adapter le traitement. Il est important qu'il sache que les pensées délirantes sont là en permanence et que votre psychisme peut parfois vous être incontrôlable. je vous souhaite un prompt rétablissement. Cordialement Catherine Cadou - Psychanalyste
248 réponses
1005 J'aime
Bonjour Jean, Tout d'abord, merci d'avoir témoigné ici et sans mettre 4 copie A4 (humour). Il est indéniable que vous ne devez plus du tout prendre de drogues. Je dirais que ce n'est pas un combat contre vous même mais plutôt une meilleure connaissance de vous-même qui vous aidera à comprendre votre place dans la société actuelle. Vous avez une place dans votre famille, par votre naissance et votre éducation, une place professionnelle par votre entreprise et une place personnelle globale qui comprend les relations, l'affectif que vous devez définir. Il est important de comprendre les raisons de votre angoisse et ce à quoi vous vous attendiez en prenant de l'ectasy... aussi. Je suis à votre écoute pour en parler de vive voix en téléconsultation sur psychologue.net si besoin. Cordialement Charlotte Psychologue
521 réponses
249 J'aime

Psy spécialisés en Aide psychologique
Autres questions sur aide psychologique.
- État anxieux suite à un bad trip
- Suite Bad trip, syndrôme Post Hallucinatoire Persistant (HPPD)
- Questionnement EMDR / Peur de devenir schizophrène
- Hypnose traitement de la déréalisation/ dépersonnalisation
- Démarche à suivre anxiété
- Faire une psychanalyse ou non
- Suis-je schizophrène ou en passe de le devenir ?
- Je suis perdu (psychose)
- pensée paranoiaque anxiete
- Peur de devenir fou, perdre le contrôle
Expliquez votre situation à nos psychologues
Faites votre demande de manière anonyme et recevez une aide psychologique en 48h.
Votre question et ses réponses seront publiées sur le portail. Ce service est gratuit et ne remplace pas une séance de thérapie.
Nous enverrons votre question aux experts de ce thème qui traiteront personnellement votre cas.
La séance de thérapie n'est pas gratuite et sera sujette aux tarifs en vigueur du professionnel.
Renseignez un pseudo pour rester anonyme
Votre question vient d'être révisée.
Nous vous aviserons par e-mail quand elle sera publiée.
Si vous avez besoin d’une aide psychologique immédiate, vous pouvez réserver une consultation dans les 72 heures au prix réduit de 49 €.
Cette question existe déjà.
Merci d'utiliser la barre de recherche pour connaître la réponse.
psychologues
Cherchez parmi les questions déjà existantes
Trouver des réponses parmi les 13100 questions posées sur Psychologue.net
Understanding and Overcoming Derealization Symptoms: A Comprehensive Guide
"Reality is merely an illusion, albeit a very persistent one." - Albert Einstein.
What would you do if one day the world you live in no longer looked the same? You feel anxious, disconnected, and lonely, even though you might be surrounded by your friends and loved ones. Many experience the overwhelming feeling of solitude and distortion of the senses. Yet sadly, they often fail to recognize.
Derealization is a psychological disorder that can significantly alter a person's perspective of reality, which leads to feelings of detachment and unreality. While it can be a difficult experience, knowing the derealization symptoms and practicing good coping skills may assist people in re-establishing a sense of connection and gaining stability in their lives.
In this detailed guide by our experts, we will explore the complexities, the underlying reasons, common indicators and derealization symptoms, and practical ways for dealing with the repercussions. We at KMA Therapy hope that by shining light on this often overlooked condition, we can help people fight their own derealization experiences with courage and self-awareness.

What is Derealization Disorder?
Simply put, derealization disorder is a dissociative experience. It starts with simple feelings of detachment from one's surroundings as if the world were unreal or distorted. Derealization can occur in a variety of ways, ranging from brief periods of mild detachment to long-lasting feelings of loneliness.
A simple test to identify if an individual suffers from derealization is to ask them to describe their surroundings. If you feel like your environment is strange, dreamy, or disfigured, with objects, people, and circumstances appearing strange or made up, it might be time to contact a professional therapist at KMA. While derealization is usually brief and harmless, recurrent or prolonged episodes can have a serious impact on a person's overall health and normal daily activities.
5 Key Derealization Symptoms You Should Not Ignore!
There’s no doubt that diagnosing a proper mental illness will require a professional or an expert. But you can get an initial idea of how severe your condition is or whether you have it in the first place by analyzing the signs mentioned below:
Reality Doesn't Feel Real
One of the key derealization symptoms is a constant feeling of illusion or detachment from the world around you. Imagine as though you are viewing the world through a fog or veil, with things and other people seeming distant or strange. This continuous sense of isolation can be stressful and distracting, causing increased anxiety and trouble completing daily tasks.
Feeling Emotionally Blank
Derealization disorder is frequently accompanied by sensations of unreality, as well as emotional coldness or detachment. Many may also struggle to connect with and feel their emotions in a meaningful way. Despite logically understanding that particular events or situations should trigger an emotional reaction, you may struggle to connect with such emotions physiologically. This emotional detachment may break down your relationships and interfere with interaction with others, resulting in feelings of exclusion and sadness.
Time Doesn't Make Sense
If you are experiencing confusion with a distorted sense of time, it may be a result of the derealization disorder. People often perceive time as moving at a slower or accelerated speed, which makes it hard to measure time accurately. Hours may go by without a clear sense of how much time has passed, and tasks that once seemed normal may suddenly seem exhausting. This twisted sense of time can cause disturbances to regular schedules and impact effective time management, ultimately leading to an increased amount of stress and annoyance.
Feeling Sensory Overload
If you are going through derealization, you might become more sensitive to light, sound, or touch. Once-tolerable everyday experiences can become overpowering or unpleasant at any time, causing avoidance behaviors and a lack of social engagement. This increased sensitivity can have a negative impact on your day-to-day activities and general quality of life, worsening anxiety and enhancing derealization symptoms.
Brain Not Working Right
Brain fog and cognitive impairment frequently co-occur with derealization disorder, making it hard for people to focus or think clearly. You may find it difficult to remember information or make judgments, and even simple thinking tasks may feel difficult. Academic and professional performance may be affected by this impairment of cognition, which may contribute to feelings of hopelessness and unhappiness.
Understanding the Underlying Causes
Although the exact cause of derealization is still unknown, the combination of biological, psychological, and environmental variables is believed to be responsible. Some factors may include:
- Trauma: For people who have endured significant or repeated trauma, derealization disorder may serve as a coping strategy for managing stress or trauma
- Anxiety and Panic Disorders: Anxiety and panic attacks are frequently accompanied by derealization. It may be set about by extreme stress or terror and indicates a sign of these disorders.
- Depersonalization Disorder: When someone has depersonalization disorder, they frequently experience derealization, a feeling of disconnection from both themselves and the outside world.
- Substance Use: Derealization disorder can also be a side effect of using some drugs, including cannabis, hallucinogens, and dissociatives. Withdrawal from specific substances may also result in derealization.
- Mental Health Conditions: It has been linked to a number of mental health issues, such as borderline personality disorder, schizophrenia, and depression.
- Medical Conditions: Derealization is a symptom of a variety of conditions, including epilepsy, migraines, brain trauma, and vestibular disorders.
- Sleep Deprivation: Dreams of derealization disorder may result from sleep deprivation or irregular sleep cycles.
- Stress and Overwhelm: Derealization experiences may be worsened by extreme stress, whether it comes from relationships, the workplace, or other life events.

Strategies for Overcoming Derealization Symptoms
Derealization disorder leaves you with a feeling of dread and anxiety. Therefore, we at KMA Therapy believe that this is an issue you might have to face head-on. Although derealization symptoms might seem overwhelming, here are some strategies to help manage and overcome them:
Grounding Techniques:
Grounding practices help tackle feelings of unreality and become more focused on the present. Engaging in techniques that are designed to help you focus on the moment at hand, such as gradual relaxation of muscles, taking deep breaths, or imagery guidance. Furthermore, to familiarize yourself with your physical surroundings, use sensory grounding techniques, including concentrating on your touch, taste, smell, sight, and sound senses.
Emotional Exploration:
You can explore these methods for processing emotional events and getting back to a connection with your feelings. Start by keeping a journal. This offers a safe space for you to reflect and express your emotions, ideas, and experiences. Furthermore, painting, drawing, or playing music are examples of artistic therapy that can help you discover your sense of emotion and use your imagination. To develop a deeper understanding and connection, try talking to discuss your feelings and experiences of derealization disorder with a therapist, family member, or trusted friend.
Time Management Strategies:
Creating routines and structure in your everyday life can help you feel less disoriented and manage how you view time. You could use tools like planners, calendars, or electronic reminders to keep track of assignments and appointments. Split tasks that are more complicated into smaller, more achievable ones to avoid feeling overwhelmed. Remember, making self-care habits at the top of your list should be a must. These include getting enough sleep, eating a healthy diet, and exercising. Such habits are crucial for helping you manage your time and cognitive performance.
Sensory Regulation:
One of the best ways to cope with derealization symptoms is to reduce the number of sensory stimuli in your surroundings and add peaceful things to create a relaxing atmosphere. Try different combinations of lighting, sound, texture, and temperature to create a comfortable and relaxing environment that appeals to the senses. Things that might help you lower your stress level and put you at ease may include techniques like progressive muscle relaxation, deep breathing, or aromatherapy.
Cognitive Enhancement Activities:
Working to improve your thinking skills and overcome brain fog caused by the derealization disorder can be done by taking part in mental exercises and activities. This may include games, puzzles, and apps for brain training, which may help improve your ability for memory, focus, and problem-solving. Participating in mindfulness meditation to strengthen focus and attention will also help you with memory and mental clarity. Make sure you are giving self-care routines like getting enough sleep, eating a healthy diet, and exercising a lot of attention. These are crucial for maintaining your overall health and cognitive function and coping with the derealization symptoms.
The Takeaway
Although derealization disorder can have a significant negative influence on a person's quality of life, with the correct resources and techniques, you can take back control and manage its symptoms effectively. You can recover a sense of stability and connection in your life by understanding the derealization symptoms and using coping mechanisms such as emotional exploration, grounding exercises, time management skills, sensory modulation, and cognitive enhancing exercises. People can successfully pass through their experiences of derealization and come out stronger on the other side if they have the right tools, resources, and support.
What Should You Do Next?
"You are not your illness. You have an individual story to tell. You have a name, a history, and a personality. Staying yourself is part of the battle." - Julian Seifter.
After reading this article, you now know what derealization disorder is, its causes, and how you can overcome it.
We at KMA have been supporting and empowering our clients in their mental health journey for over a decade. We offer therapy at five convenient locations across Toronto: Yonge and Eglinton, King West, Yorkville, Liberty Village, and Yonge and Sheppard, and we offer virtual counseling sessions for anyone in Ontario.
Register online to learn more about our online anxiety counseling or download our Therapy 101 Guide to explore how therapy can work for you.
Frequently Asked Questions
Q1. How can I support a loved one experiencing derealization?
If you have a loved one experiencing derealization disorder, it is essential to offer them empathy, understanding, and support. Offer them a nonjudgmental space to share their experiences and thoughts, and encourage them to get professional assistance. Educate yourself about derealization so that you can help and be patient with them as they work their way through the recovery process.
Q2. Is it possible to fully recover from derealization?
Even though derealization disorder can be a difficult experience, many people can make great progress and have happy, meaningful lives if they receive the right attention, support, and self-care. Every individual's journey toward recovery from derealization is different, and there may be ups and downs along the way. It is possible to overcome derealization and regain a sense of stability and connection in life with determination, courage, and support.
Q3. What should I do if my derealization symptoms worsen or become overwhelming?
If your derealization symptoms worsen or become overwhelming, it is crucial to seek immediate support from a mental health professional or crisis helpline. You are not alone, and help is available 24/7. Do not hesitate to reach out for assistance and guidance during difficult times.
Q4. How does therapy at KMA Therapy work?
Therapy at KMA Therapy starts with an initial consultation to determine the client's requirements and objectives. To address issues and build strength and personal development, therapists study your derealization symptoms and use evidence-based techniques such as mindfulness and CBT. Sessions are customized for each person and offer a private setting for support and discussion. For flexibility, clients can choose between in-person and remote sessions. The client-centered method's focus on multicultural sensitivity and holistic support services is essential for developing overall well-being. KMA Therapy's treatment equips patients to overcome challenges, accomplish their objectives, and take back control of their lives.
Q5. How can I book an appointment for therapy at KMA?
To book an appointment you just need to fill out our web form or call us at 416-487-6288!
We are located at five locations in Toronto:
- Yonge & Eglinton- 120 Eglinton Avenue East, Suite 304, Toronto, Ontario M4P 1E2
- King West- 500 King Street West, 3rd Floor, Toronto, Ontario M5V 1L8
- Liberty Village- 60 Atlantic Avenue, Toronto, Ontario M6K 1X9
- Yorkville- 2 Bloor Street West, 19th Floor, Toronto, Ontario M4Y 2B6
- Yonge & Sheppard- 4711 Yonge St, 10th Floor, Toronto, ON M2N 6K8
Register Online
Therapy review: 5 basic types of therapy you need to know more about.
Our team of experts will support you throughout your mental health journey to help you become your most authentic self!
Nervous About Starting Therapy? 10 Things You Need to Know to Get The Most Out of Your Session!
A comprehensive guide to finding a therapist in the yorkville area, or, are you all set and ready to book, ontario's premier counselling practice.

June 14, 2022
When Things Feel Unreal, Is That a Delusion or an Insight?
The psychiatric syndrome called derealization raises profound moral and philosophical questions
By John Horgan

Mads Perch/Getty Images
Have you ever been gripped by the suspicion that nothing is real? A student at Stevens Institute of Technology, where I teach, has endured feelings of unreality since childhood. She recently made a film about this syndrome for her senior thesis, for which she interviewed herself and others, including me. “It feels like there’s a glass wall between me and everything else in the world,” Camille says in her film, which she calls Depersonalized; Derealized; Deconstructed
Derealization and depersonalization refer to feelings that the external world and your own self, respectively, are unreal. Lumping the terms together, psychiatrists define depersonalization/derealization disorder as “persistent or recurrent … experiences of unreality, detachment, or being an outside observer with respect to one’s thoughts, feelings, sensations, body, or actions,” according to the Diagnostic and Statistical Manual of Mental Disorders . For simplicity, I’ll refer to both syndromes as derealization.
Some people experience derealization out of the blue, others only under stressful circumstances—for example, while taking a test or interviewing for a job. Psychiatrists prescribe psychotherapy and medication, such as antidepressants, when the syndrome results in “distress or impairment in social, occupational, or other important areas of functioning.” In some cases, derealization results from serious mental illness, such as schizophrenia, or hallucinogens such as LSD. Extreme cases, usually associated with brain damage, may manifest as Cotard delusion , also called walking corpse syndrome, the belief that you are dead; and Capgras delusion , the conviction that people around you have been replaced by imposters.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing . By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
I’m glad Camille has drawn attention to the disorder, because derealization raises profound philosophical questions. Sages ancient and modern have suggested that everyday reality, in which we go about the business of living, is an illusion . Plato likened our perceptions of things to shadows cast on the wall of a cave. The eighth-century Hindu philosopher Adi Shankara asserted that ultimate reality is an eternal, undifferentiated field of consciousness. The Buddhist doctrine of anatta says our individual selves are illusory.
Modern philosophers such as Nick Bostrom postulate that our cosmos is probably a simulation, a virtual reality created by the alien equivalent of a bored teenage hacker. The philosophical stance known as solipsism insinuates that you are the only conscious being in the universe ; everyone around you only seems conscious. As I mention in a recent column, some interpretations of quantum mechanics undermine the status of objective reality. Could derealization have inspired all these metaphysical conjectures?
Many people, Camille suggests, undergo episodes of derealization without knowing what it is. The feeling disturbs you, so you suppress it. You try to put it out of your mind, and you don’t mention it to others. “You’re afraid that if you do tell people, they won’t know what it is,” Camille explains, “and you don’t want people viewing you differently.” I understand these reactions, because derealization can be unsettling, even terrifying.
My most serious, sustained bout of derealization occurred after a drug trip in 1981, which left me convinced that existence is a fever dream of an insane god . For months the world felt wobbly, flimsy, like a screen on which images were projected. I feared that at any moment everything might vanish, giving way to—well, I didn’t know what, hence the fear. These feelings over the years have lost their visceral power over me, but their intellectual aftereffects linger.
Pondering derealization leaves me conflicted. I have moral misgivings about claims that reality isn’t, well, real . These assertions, whether Platonism, the simulation hypothesis or my insane-god theology, can easily become escapist and nihilistic. Why should we worry about poverty, oppression, environmental destruction, pandemics, war and other sources of suffering if the world is just a video game? I reject any philosophy that undercuts our responsibility to care for each other.
I’ve nonetheless come to value derealization as an antidote for habituation. Our brains are designed to accomplish many tasks with minimal conscious effort. As a result, we get accustomed to things; we take them for granted. We become like zombies or automatons , carrying out chores and interacting with other people—even those we supposedly love—without being fully aware of what we are doing.
Derealization is like a slap across the face. It cuts through the monotony of life and wakes you up. It reminds you of the weirdness of the world , of other people, of yourself. By weirdness I mean infinite improbability and inexplicability. Weirdness encompasses all the bipolar properties of our existence, its beauty and ugliness, kindness and cruelty, good and evil.
Seeing the weirdness doesn’t negate our moral responsibility to others. Far from it. By estranging me from the world, derealization, paradoxically, makes it more real. It helps me see humanity more clearly and care about it more deeply. What once felt like a curse has become a gift.
That’s what I tell myself, anyway. Others, including those Camille interviewed for her film, and Camille herself, experience derealization differently. She sees the syndrome as “your brain’s way of taking a break. It thinks you can’t handle certain things, and so it turns everything off.” She has learned that “just letting the feelings flow” rather than fighting them helps her get through episodes. Whatever derealization means to us, however we cope with it, we’re surely better off if we can talk about it openly, as Camille and others do in her brave, revealing film.
This is an opinion and analysis article, and the views expressed by the author or authors are not necessarily those of Scientific American.

Understand why you feel weird after a bad trip
When you feel weird after a bad trip, all kinds of questions can come creeping in your head. I know it’s scary, so I created this post to help explain what’s going on and how to work through it.
The main thing to understand is whether you’re experiencing short-term anxiety following a recent bad trip, or longer-lasting effects. The good news is that neither are permanent. Even if you may feel like it, you did not break your brain. You did not mess yourself up for good. I have been in your shoes – I’ve dealt with short and long-term effects after a bad trip – and I’ve gotten through it ALL. You will too. It may take some time, but you will feel normal again.
Why you feel weird after a bad trip: Short-Term Uneasiness
Whether you’ve just come down or tripped a few weeks ago, having lingering effects from a trip can be scary. It may be hard to believe right now, but I promise you will be just fine. If it’s been less than 3 months since you tripped, this is a good place to start understanding what’s going on (and how to fix it).
After any unsettling experience, feelings of uneasiness are normal
If you had just gone through an unsettling emotional experience, such as a car wreck or a painful break-up, no one would blame you for feeling uneasy. If you feel weird after a bad trip, it’s (in many ways) no different from any other unsettling experience. The main difference is the trip was something that happened in your mind. Because of that, it doesn’t leave you with a clear-cut explanation for your anxiety or uneasiness. Truthfully, though, when you’ve gone through a difficult psychedelic experience, you have just as much of a reason to feel unsettled. Perhaps even more.
When a person goes through a traumatic or unsettling experience, it can take a little bit to get back to normal. Traumatic experiences can also bring out new anxieties and leave you feeling very different than before. It doesn’t mean that anything is wrong with you – it just means you’re shaken up and you need some time to feel yourself again.
It’s very common to worry that something is wrong with you
If you’re worried that something is very wrong with you, know that your concern is very common. There is a lot on the internet about all kinds of intense, serious-sounding disorders with long names, and that is often the last thing you need to read when you feel weird after a bad trip. It is very, very likely that you are simply shaken up , as anyone would be after a traumatic experience.
How to tell if you’re just experiencing short-term uneasiness
The two main ways to tell if you’re just experiencing something short-term is to consider the intensity of the trip and how long ago it was.
1. A scary trip vs. being shaken to your core
There are scary, unsettling trips, and then there are trips that are so life-changingly horrifying that they shake you to the core of your very being and leave you to try and make sense of the emotional wreckage.
If what you experienced was scary, difficult, confusing, uncomfortable, unsettling, etc., but not utterly life-shattering, it’s likely that you’re dealing with more short-term anxiety. If you’ve had one of those life-shattering trips, you know what I’m talking about . It is likely that you will have to spend a longer time working through the wreckage.
2. Timeframe
If it hasn’t been long since you’re difficult trip, it’s likely that you’re dealing with something short-term. While there is no definitive timeline – everyone is different – I’ve outlined some general timeframes below.
You’re still very fresh out of the experience, and at this point, I wouldn’t worry too much. I know things may feel very weird right now. It’s likely that you don’t feel yourself at all, but have faith that you will get back to normal. Remember – imagine how you might feel right now if you’d gone through another type of severely unsettling experience? If you’d just been broken up with in an awful way less than two weeks ago, would you expect yourself to feel totally okay today? I know that I wouldn’t. It takes time to heal from unsettling experiences.
At this point, the best thing you can do is relax and do not self-diagnose . You are NOT schizophrenic or anything like that! While you definitely won’t be the same person you were before your trip, you will get back to a normal state. In the meantime, there are techniques that you can try to ease the anxiousness.
- Exercise! This isn’t necessarily the most popular suggestion, but it will really help you “burn off” that nervous energy. It can especially help get you out of your head and into your body, which is great if you feel yourself worrying a lot now. If real life has started to seem like an illusion now (“derealization”), the physical sensations of exercise can help get you back on Earth.
- Spend time outside. Getting a healthy dose of nature everyday can be extremely calming and grounding. I would suggest trying to be outside walking, exercise, or simply observing nature for at least 30 minutes per day. This works wonders.
- Spend time with people you like and trust. If you’re feeling anxious, it’s best not to spend a lot of time alone. At the same time, spending time with someone you hardly know or feel uneasy with can make matters worse. If you know of someone you trust in this way, you can simply say that you’re going through a tough time and would like some company. You don’t need to tell them what’s going on, especially if you think it would really concern them. If you need some guidance on how to talk about what you’re going through, I’ve written about it here .
- Eliminate specific fears and concerns. If the trip brought out specific anxieties for you, make a list of those things and start trying to work past them. While you may not be able to fix the issues immediately, working towards fixing them will bring some peace of mind.
- Try techniques for dealing symptoms of anxiety. Detailed explanations of some techniques that have worked for me can be found here .
1-2 months
While it may really be starting to feel like something is wrong with you (or that you broke your brain), I still would consider it short-term anxiety. Compare it to a more typical emotionally unsettling experience, such as going through a bad break-up, a car wreck, the loss of a loved-one, etc. These things can take a long time to get past, and that is totally natural.
If you feel weird after a bad trip that happened a month or two ago, you might really start to be feeling impatient with yourself. When we have a bad trip, often there is a feeling of shame that comes along with it, especially when compared to other people. If my friend had a normal, great trip, why was mine so screwed up? What’s wrong with me? Why couldn’t I handle it? Trips are highly personal experiences. Everyone reacts to psychedelics differently, and there should be no shame in having a difficult experience. It may be true that you took more than you should’ve or that you didn’t feel ready going into the trip, but putting yourself down for those kinds of things isn’t going to help you get past what you’re feeling now . The way you reacted the trip can help you understand aspects of yourself and your emotional state better, but you must approach that from a place of self-love. This can be an opportunity to learn a lot about yourself and grow immensely. In order to do that, though, it’s essential to have a positive attitude.
If you’re more than three months out from your trip and still experiencing intense anxiety, it’s possible that you’re dealing with something more long-term. It’s important to consider this in connection with the intensity of your trip. It may simply be that you are someone who needs a while to get past unsettling experiences. There is nothing wrong with that. Think back to other times in your life that you’ve had to go through something difficult emotionally. Do you tend to get over things quickly, or does it take a while to process everything? If this seems consistent with your past experiences, I wouldn’t worry too much. On the other hand, if this seems wildly inconsistent with your usual disposition, it may be possible that you’re dealing with something longer-term.
If it seems like you’re dealing with something long-term, I would still try to maintain a positive attitude. A bad trip can be one of the most difficult, trying experiences of your life, but it can also be one of the greatest opportunities to grow and improve yourself. It took me a very long time to heal from my difficult trip, but looking back, I can’t imagine being the same person I was back then. I am so much stronger and in-touch myself that I wouldn’t go back to that old me for anything. The important thing is to really start looking into your emotional state, the experiences of your trip, and the state of your life. Take this as a time to work on healing yourself, improving your life, and working out issues that have been holding you back. Read more about how to understand a bad trip and start to heal.
Why you feel weird after a bad trip: Long-Term Effects
Having a trip that produces long-term effects doesn’t have be a bad thing. It also doesn’t mean that anything is wrong with you.
Why did this happen?
There are many reasons that this happened to you – none of which you should be ashamed of. If you feel weird after a bad trip and it’s been going on for a long time, try not to compare yourself to others. You may have tripped with someone who had a perfectly wonderful experience, and they can’t understand why you’re so shaken up. They may be starting to lose patience with you for not getting better already. Don’t worry about them: this is your life, not theirs. It’s time to accept that this did happen to you and start working to get to the bottom of it.
So, why did this happen? The two main causes are (1) the intensity of your trip and (2) emotional troubles that lie beneath the surface. Additionally, if you took a mixture of substances or research chemicals, the trip may have had lingering effect on your brain chemistry.
Ultra-Intense Trips
You may have read above about scary trips vs. trips that shake you to the core of your whole being. You might feel that your trip shook you to your core. When you look back on it with your logical, sober mind, however, you can’t understand why it was so scary. In that case, you may feel confused and ashamed of the fact that you couldn’t handle something that seemed rather mild.
When we trip, we’re interacting with the core of our emotional beings. This is different than the rational mind that we use in everyday life. Our emotional selves are not rational, but they are deeply wise. They communicate in symbols and pictures rather than coherent, cause-and-effect ideas. What scared the hell out of you during a trip may not make sense in your rational mind. It may not seem scary at all. You may not even have words for your experience. This is all normal.
It’s important to understand that something that scares you on a deep emotional level during a trip can go way beyond the type of fear that you experience in your daily life, even though it doesn’t seem scary in daily life.
For example, you may have been terrified of the fact that your tripping partner would not look you in the eye. In daily life, that isn’t scary at all – people rarely make eye contact with each other these days. But you know how they say: the eyes are the window to the soul. On an emotional level, however, this lack of eye contact may have made you feel that your friend was hiding their true selves, keeping something from you, and refusing to connect. This may have triggered a deep-seeded mistrust that goes all the way back to something that happened when you were four years old. While this may sound like hocus pocus, it is the reality of how our emotional sides work.
No matter how strong you are, an ultra-intense trip can bring you to your knees and require a great deal of time to get over. Even if you don’t understand why it was so intense, if you’ve had one of these trips, you just know it.
Emotional Troubles
While I touched on the ways that a bad trip can cause emotional troubles, another aspect: emotional troubles that existed before the trip. Everyone has emotional pain – it’s simply unavoidable. We all vary in the degree of pain we’ve experienced, how we’ve dealt with it, and how aware of it we are.
Wonderful and difficult psychedelic trips tend to bring out our existing dispositions. If you’re naturally shy, you may become more shy and timid while tripping. If you’re naturally adventurous, you may want to move about during the trip rather than staying in one place. When a psychedelic brings out existing emotional troubles, such as anxiety, fear, hurt, repressed trauma, and so on, it can trigger a negative experience. Having to face those emotional troubles may cause a lot of anxiety that stays with you long after the trip is over. If you were trying to ignore pain or a certain emotional problem, a trip can bring it out and make it very hard to ignore anymore. This can be difficult to process, and it may cause a lot of new anxiety.
Issues with substances
While traditional, old-school psychedelics are generally safe, newer research chemicals and mixtures of multiple substances can cause lingering unwanted effects.
Research Chemicals
Research chemicals can produce psychedelic effects, but they’re newer and can be harmful. Often, these chemicals are sold as acid, but they are not acid. Here are some of the ways you can tell that you may have unknowingly taken a research chemical:
- You felt really bad psychically during or after the trip
- What you took tasted like batteries
- You felt mentally chaotic, disconnected from yourself, or consumed by dark thoughts thoughts during the trip
- Your trip lasted 12+ hours
- You felt like you didn’t fully come down for a long time
If you think you may have taken a research chemical thinking that it was acid, you’ll still be okay. These substances can have a more intense effect on your brain chemistry, making it take a longer to get back to normal. You will get back to normal though.
Prescriptions
If you were taking any sort of anti-depressants or other psychoactive prescriptions at the time of your difficult trip, it’s likely that it had a large impact on the experience. MAOIs or other substances that act like MAOIs hinder the metabolization of psychedelics like LSD. This can cause a trip to be far more intense and last much longer than usual. My general recommendation is to stay away from psychedelics until you’ve been off of any kind of prescription for depression, anxiety, mood, etc. for a while.
Mixing Substances
Many, many people mix various substances together while tripping. Smoking weed while on acid may be the most common, but there is a huge variety of ways that people combine drugs. This was even a factor during my life-shattering trip. I would recommend staying away from any kind of mixing. There are just too many different ways that substances can interact with your brain and each other that it’s better not to mess with it.
If you did mix substances, it’s possible that your mixture was too intense on you and your brain chemistry. You may have given your brain a bit of a shock. Things will eventually get back into balance, but going forward, it’s important to remember that your brain is resilient but delicate. It’s really all you have in this life, and you must treat it with care and respect.
Steps to take
If you feel weird after a bad trip and have been struggling with this weirdness for a while now, there are things you can do to improve your situation. I know these lingering effects are scary. I know you may be worrying that you did permanent damage, but I promise you will be okay. For healing, I recommend a 2-fold strategy that addresses your physical and emotional situation.
If you’re struggling with anxiety and uneasiness, it’s important to get yourself grounded again while assisting your brain’s healing. Aerobic exercise, like jogging, swimming, or riding a bike, is extremely helpful for calming anxiety. It can help bring you back into physical reality and help you relax. It’s great to do these kinds of activities outdoors as nature is helpful in grounding.
To help your brain regenerate, it’s important to eat a healthy diet that is full of nutrients. I would strongly suggest avoiding processed foods and opting for a lot of leafy greens. Taking a good, organic multi-vitamin will also help with this. During this time, it’s important to get as much sleep as you can.
Once you’re no longer in an emergency state with your anxiety, it’s important to turn inwards. It’s important to move forwards in your personal development rather than just trying to become your old self again. These intense trips turn your life upside down. That can seem like a bad thing, but you can use it as a launch-point for starting fresh.
One of the most important things is to write about what you’re experiencing. If you’re struggling with anxiety, journal about what you feel in great detail. If unsettling philosophical questions are constantly entering your mind, write about it! Through writing and reading what you’ve written, you can start to see the patterns in what you’re experiencing. If certain thoughts make you very uncomfortable, take this as a time to push through the uncomfortableness. This part of healing is all about going deeper into yourself than you’ve ever been before.
Self-diagnosis isn’t the answer.
Oftentimes, when people feel weird after a bad trip for a very long time, they tend to worry that what they’re experiencing is permanent. The tendency to self-diagnose kicks in, making the sense of anxiety worse. There are all kinds of scary-sounding things you can diagnose yourself with via WebMD, but doing so isn’t the answer. When you diagnose yourself some disorder or condition, you accept in into your life and your identity. Doing that makes it even harder to heal. What you’re going through isn’t permanent, and you will get through it. I’m living proof: I have been exactly where you are, and I have healed.
The desire to self-diagnose often comes from a desire to understand what is happening and why. To feel normal. While not everyone has lingering effects like this after a trip, many, many people do at one point or another. Psychedelics are so intensely powerful that they can bring out a person’s greatest joy and deepest pain. It simply comes with the territory.
The most important thing
While you work to heal, the most important thing you can do is maintain a positive attitude . If you have that, nothing can stop your healing. While this is incredibly tough – it may be the hardest thing you’ve ever gone through – it is an amazing opportunity to grow stronger, wiser, and more in-touch with yourself. Once you’re feeling normal again, you’ll look back on this as a pivotal time in your life. In the meantime, you’ll have good days and bad days, but if you can keep up your hope, positivity, and optimism, you’ll heal so much more quickly. I promise.
- Patient Care & Health Information
- Diseases & Conditions
- Depersonalization-derealization disorder
Depersonalization-derealization disorder occurs when you always or often feel that you're seeing yourself from outside your body or you sense that things around you are not real — or both. Feelings of depersonalization and derealization can be very disturbing. You may feel like you're living in a dream.
Many people have a passing experience of depersonalization or derealization at some point. But when these feelings keep occurring or never fully go away, and they make it hard for you to function, it's likely depersonalization-derealization disorder. This condition is more common in people who experience trauma, such as violence, abuse or other kinds of extreme stress.
Depersonalization-derealization disorder can be serious and may get in the way of your relationships and work. It also can disrupt other daily activities. The main treatment for depersonalization-derealization disorder is psychotherapy, also known as talk therapy. Sometimes medicines also are used.
Products & Services
- A Book: Mayo Clinic Family Health Book
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Short experiences of depersonalization or derealization are fairly common. But lasting and returning bouts of these symptoms can cause problems at work or school, or in other important areas of your life. During these bouts, you know that your sense of not being connected to your body or your surroundings are only feelings and not reality.
The experience and feelings of the condition can be hard to describe. Worrying about "going crazy" can cause you to become focused on checking that you exist and finding out what's real.
Symptoms usually begin in the middle or late teenage years, or in early adulthood. Depersonalization-derealization disorder is rare in children and older adults.
Depersonalization symptoms
Symptoms of depersonalization include:
- Feelings that you're seeing your thoughts, feelings, or body or parts of your body from the outside. For example, you may feel like you're floating in the air above yourself.
- Feeling like a robot or that you're not in control of what you say or how you move.
- The sense that your body, legs or arms appear twisted or like they're not the right shape. Or they may seem larger or smaller than usual. You also could feel that your head is wrapped in cotton.
- Emotional or physical numbness of your senses or responses to the world around you.
- A sense that your memories lack emotion, and they may or may not be your own memories.
Derealization symptoms
Symptoms of derealization include:
- Feeling that people and your surroundings are not real, like you're living in a movie or a dream.
- Feeling emotionally disconnected from people you care about, as if you were separated by a glass wall.
- Surroundings that appear out of their usual shape, or are blurry or colorless. Or they may seem like they only have two dimensions, so they're flat with no depth. Or you could be more aware of your surroundings, and they may appear clearer than usual.
- Thoughts about time that are not real, such as recent events feeling like the distant past.
- Unrealistic thoughts about distance and the size and shape of objects.
Bouts of depersonalization-derealization disorder may last hours, days, weeks or months. In some people, these bouts turn into ongoing feelings of depersonalization or derealization that may get better or worse at times.
When to see a doctor
Passing feelings of depersonalization or derealization are common and are not always a cause for concern. But ongoing or serious feelings of detachment and distortion of your surroundings can be a sign of depersonalization-derealization disorder or another physical or mental health condition.
See a doctor if you have feelings of depersonalization or derealization that:
- Are disturbing you or are disrupting your emotions.
- Do not go away or keep coming back.
- Get in the way of work, relationships or daily activities.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
The cause of depersonalization-derealization disorder is not well understood. Some people may be more likely to experience depersonalization and derealization than others. This is possibly due to genetic and environmental factors. High levels of stress and fear may cause bouts.
Symptoms of depersonalization-derealization disorder may be related to childhood trauma or other experiences or events that cause severe emotional stress or trauma.
Risk factors
Factors that may raise the risk of depersonalization-derealization disorder include:
- Certain personality traits that make you want to stay away from stressful situations or make it hard to describe your emotional experience.
- Serious trauma as a child or an adult, like going through or seeing a traumatic event, such as violence or abuse.
- Serious stress, such as major relationship, financial or work-related issues.
- Depression or anxiety, especially serious depression, depression that lasts a long time or anxiety with panic attacks.
- Drug misuse, which can cause bouts of depersonalization or derealization.
Complications
Bouts of depersonalization or derealization can be scary and make it hard to function. They can:
- Make it hard to focus on tasks or remember things.
- Get in the way of work and other routine activities.
- Cause problems in relationships with your family and friends.
- Make you feel anxious, depressed or hopeless.
- Depersonalization/derealization disorder. In: Diagnostic and Statistical Manual of Mental Disorders DSM-5-TR. 5th ed. American Psychiatric Association; 2022. https://dsm.psychiatryonline.org. Accessed May 1, 2023.
- Spiegel D, et al. Depersonalization/derealization disorder. Merck Manual Professional Version. https://www.merckmanuals.com/professional/psychiatric-disorders/dissociative-disorders/depersonalization-derealization-disorder. Accessed May 1, 2023.
- American Psychiatric Association. https://www.psychiatry.org/patients-families/dissociative-disorders/what-are-dissociative-disorders. Accessed May 1, 2023.
- Simeon D. Approach to treating depersonalization/derealization disorder. https://www.uptodate.com/contents/search. Accessed May 1, 2023.
- Simeon D. Depersonalization/derealization disorder: Epidemiology, pathogenesis, clinical manifestations, course, and diagnosis. https://www.uptodate.com/contents/search. Accessed May 1, 2023.
- Simeon D. Pharmacotherapy of depersonalization/derealization disorder. https://www.uptodate.com/contents/search. Accessed May 1, 2023.
- Simeon D. Psychotherapy of depersonalization/derealization disorder. https://www.uptodate.com/contents/search. Accessed May 1, 2023.
- Allen ND (expert opinion). Mayo Clinic. May 15, 2023.
- Society for the Advancement of Psychotherapy. https://societyforpsychotherapy.org/depersonalization-derealization-disorder-theory-treatment-and-advocacy/. Accessed May 1, 2023.
- Symptoms & causes
- Diagnosis & treatment
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be part of the cutting-edge research and care that's changing medicine.
- Skip to main content
- Skip to footer
Additional menu
A Coach Called Life

Tips for Driving With Depersonalization and Derealization
Last updated on August 20, 2023 By Swamy G
Driving can be terrifying to someone with depersonalization and derealization disorder. It can debilitate their life. What causes this fear and how can we overcome it?
I had a big fear of driving when I suffered from chronic depersonalization and derealization. I’d dread being on the road, especially on freeways. Depersonalization and derealization restricted many areas of my life, but it especially restricted my ability to commute long distances.
Thankfully, I lived in a city with good public transport. It also had good bike lanes, so I could ride my bike to meet up with friends or go to work. But when it came to commuting away from my city, I’d feel extremely anxious even thinking about it.
My Fear of Driving During Depersonalization

Many of you reading this article know what it is like to drive your car when experiencing DP/DR. For those who are not privy to this experience, let me tell you how it was for me.
Not only did I experience fear when I was driving a car, but I’d start getting anxious days in advance of an upcoming trip. I remember losing sleep on a few occasions the night before an upcoming trip. I’d lie awake worrying whether I might be able to drive carefully the following day.

Struggling with DP/DR?
DP No More is the only online course you need to recover from depersonalization (DP) and derealization (DR). This is science-backed cure for DP/DR.
At this point, I have to inform you that DP/DR doesn’t directly affect your ability to drive the way alcohol or drugs do. Your senses are not impaired. You can react to events pretty quickly.
The problem is that you just feel completely weirded out. You start feeling as if you are in a dream world when driving. This unreal feeling is known as derealization. You feel your environment suddenly change while driving. This especially happened to me when I was driving on the freeways. Something about the wide-open space of a freeway coupled with the fact that I was supposed to be going over 50mph (about 80 km/hr) made me feel extremely uneasy.
I can only describe the feeling as bizarre. DP/DR while driving made me feel like I was in one of those “Need for Speed” types of car-racing video games. Of course, I wasn’t hallucinating. I wasn’t seeing things or anything like that. I just felt the environment was like a dream and everything appeared bright and unreal.

On top of this, I’d sometimes feel disconnected from myself. This is usually called depersonalization. I’d feel as if I was somewhere else instead of being in the here and now.
I’d also feel lighter in my body. My limbs felt loose and weightless. I’d often have scary intrusive thoughts such as, “What if I lose control of my limbs?” The intrusive thoughts were often about losing control and endangering my life and those of my passengers.
Needless to say, DP/DR made my driving experience hellish. And it’s not just me. Thousands of people who suffer from depersonalization and derealization have the exact same experience.
For some, driving every day is a necessity. They might not be able to take public transport to work or to buy groceries. For such people, DP/DR can completely put their life on a leash. Their freedom to travel becomes highly confined to a few blocks of walking. If they are fortunate, they can take an Uber everywhere, but these bills quickly add up.
Why Depersonalization Causes Fear of Driving

Many of you suffering from this might be wondering why this is happening to you. You might be thinking, “Why can’t I just drive like everybody else?”
Why do we feel so stressed, unreal, and depersonalized while driving?
The answer to these questions is the fact that driving, believe it or not, is actually pretty stressful. Do you remember the first time you learned to drive? Do you remember how stressed out you were? Try to remember the time when you first hit the highway. During those times, you were learning a new skill. A dangerous skill, if you will, one that could potentially cripple or even kill you. So, it’s no wonder you were feeling stressed when learning to drive.
Over time, this fear of driving goes from the forefront of your awareness to the back. Your brain understands how to drive, and with a lot of practice, you get the hang of it. Then it sort of becomes second nature to you. You are not constantly thinking about how to drive, you just do it.
All of the dangers of driving are still present, but your brain learns to ignore them since it now feels confident in its ability to drive. You feel safe. And once you feel safe and confident about something, all of your fears just slide into the background.
But when you start experiencing depersonalization and derealization, it starts affecting your sense of safety. This experience is so bizarre and not even many medical doctors can help you with it. Because of this, we are filled with fear. We feel something bad is waiting to happen.
DP/DR robs you of your feeling of safety. Without a feeling of safety, all of the fears in the back of your mind, the ones you were able to ignore, now come straight into the field of your awareness.
To add more fuel to this fire, the fear and the lack of feeling safe actually trigger more of the DP/DR and they keep feeding on each other. The DP/DR creates a sense of danger, and this feeling of danger in turn produces more depersonalization and derealization.
Now when you are driving, all of those fears that are lurking in the background come to the foreground of your awareness. As mentioned before, everyone has some fear of driving, but these fears usually do not impair most people. But when you experience DP/DR, these fears are amplified to the extent that you feel completely unsafe while driving.

How I Overcame my Fear of Driving during DP/DR
I’m happy to report that I have successfully overcome this fear. I now own a car and I drive around a lot. I’m able to take the freeways and go on long road trips.
I found a way to recover from DP/DR. Once I started recovering, I was pleased to find that my fear of driving also reduced. I stopped feeling unreal while driving. My environment now feels normal. Most of the time, I’m very relaxed while driving. I listen to a podcast or have a friendly chat with my passenger. I don’t dread driving anymore. I drive, just like everyone else, and I feel safe while doing so.
But if you are someone who has an intense fear of driving, then I’d like to share some tips that helped me during the time I had to drive while experiencing DP/DR.
This is a reminder that I share these tips of mine for informational purposes only. You should do your own research and consult with a medical doctor before trying to implement what worked for me.
Tip #1 I kept reiterating my safety
As mentioned before, DP/DR robs you of your feeling of safety. You feel like you are not in control and that something dangerous could happen at any time. When I understood this, I found unique ways to feel safe during my DP/DR. I did this not only when I was driving, but throughout the day. This helped me build an underlying feeling of safety.
Whenever I felt unsafe driving, I’d tell myself that I was safe at that moment. I kept telling myself that I had years of driving under my belt. I developed the belief that my clean driving record would continue to let me drive safely, even though I was experiencing unsafe thoughts. I solidified my faith in the ability to drive safely through positive self-talk.
Tip #2 I knew I could pull over if I wanted

One of the positive self-talk strategies I’d use when driving while depersonalized was telling myself that I could stop the car anytime I wanted to. I told myself I could just pull over to the side of the road or take the nearby freeway exit. I did not consider this a defeat. It was totally fine to pull over safely to the shoulder of a road or take the first freeway exit.
Knowing I had this escape helped me keep going further and further in my journey. Once you understand you are safe and you know you can pull over whenever you want, your mind stops catastrophizing the situation. The fear lessens a bit.
Tip #3 I practiced on empty streets

Before going on a long journey, I would drive around safe and less trafficked streets to get the hang of it. I’d do this to demonstrate to myself that I am a safe and careful driver.
After practicing for a few minutes, I’d take the freeway. At that point, I knew the DP/DR would kick in, but I told myself that it was ok. I had to not let my fear get the best of me. By slowly exposing yourself to your fears , you can overcome them. This is the principle behind exposure therapy.
I had to show myself that I was a safe and careful driver despite feeling depersonalized and derealized. Even driving a few miles on the freeway and slowly becoming ok with experiencing DP/DR while driving was worth it to me.
I told myself to accept the DP/DR and be ok with it. There was no use fighting it. Fighting these feelings only increases their intensity. So, I’d continue to drive despite feeling the DP/DR. Deep down, I tried to cultivate faith in my driving abilities. I told myself that all the practice runs made me a very good driver and that DP/DR cannot affect my driving skill. It can make me feel weird, but it can never make me a bad driver.
Tip #4 Sticking to the slow lane
Sometimes, I’d just move over to the slowest lane. In the US, this is the right-most lane. People sometimes make fun of slow-moving right lane traffic, but I didn’t care. All I wanted was to reach my destination safely.
I’d also find a safe driver in the slow lane and just follow them. I’d make sure to leave a healthy distance between myself and their vehicle. I just focused on the vehicle in front of me and made sure that I was slow and steady in following them. This gave me a sense of comfort and ease. All I had to do was follow the car in front of me. If I kept doing that, then I’d get to where I wanted. If they changed direction, then I’d follow another person in the same way until I reached my destination safely.
Tip #5 Have a passenger friend

Once in a while, I would ask a friend or colleague to join me on my trip. I’d inform this friend that I may ask them to take over and drive at some point. If the friend was close to me, I’d even let them know about my issue with DP/DR and driving. I’d help them understand that I’d never put them in jeopardy, but just knowing that they could take over and drive would help me calm my nerves. This is very similar to tip #2 of pulling over anytime you wanted. Just knowing that I had someone to take over driving duties relaxed me. That relaxation worked as an antidote to the stress and DP/DR feelings.
Tip #6 Experiment with other things
Finally, I learned to experiment with a few things to help me with the fear of driving. I found that depersonalization and derealization can make it appear as if everything is bright, so having sunglasses helped me calm my nerves during the daytime.
I’d sometimes listen to a podcast or play my favorite band or artist. Singing out loud in my car made me feel at ease. Now and then, I’d listen to stand-up comedy to help lighten the mood while driving.
Everyone’s different. We may have to try a few things to figure out what can help us relax and drive with ease.
All right, I hope you learned something from these tips. Fear of driving is something a lot of people experience. This fear is especially common among depersonalization and derealization sufferers. These were some tips that I used to overcome my fear of driving. Once I began to recover from DP/DR , the fear of driving started fading away. I became more and more confident in my driving skill and felt safer on the road. I hope that the same happens to you as well.
Let me know in the comments if you have any other tips that you’d like to share and help the DP/DR community out.
Image Credits: Dall-E, Stability AI, Pexels
About Swamy G
Hi, I’m Swamy. I was once a depersonalization & derealization sufferer. After my recovery, I trained to become a certified counselor to help people recover from DP/DR, anxiety, and panic disorder. On this website, I share all the resources you need to overcome depersonalization, derealization, anxiety, and panic. If you feel like you could use some help and guidance along the way, do check out DP No More.

Get this course for FREE
DP/DR Basics is a 7-part FREE email course that will teach you how to recover from depersonalization & derealization.
Reader Interactions
Leave a reply cancel reply.
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
The content on this website is purely for informational and educational purposes only and don't serve as a substitute for professional medical advice.
Derealization Treatment (How It Works + Options)

Imagine walking through life feeling constantly detached, as though you’re living in a dream or a movie, with the world around you seeming foggy and unreal. This is the everyday reality for individuals experiencing derealization, a mental health condition that can be disorienting and distressing.
Derealization is a form of dissociation where a person feels disconnected from their surroundings, with the environment appearing distorted, blurry, or unreal, often leading to feelings of panic and discomfort.
This article aims to shed light on derealization, exploring its causes, symptoms, and the various treatment options available, providing hope for those affected by it. By understanding this disorder, individuals can gain insight into managing and overcoming it, paving the way for a balanced and grounded life.
What is Derealization?
Diagnostic Criteria
Diagnosing derealization can be a challenging process due to the overlapping symptoms it shares with other mental health conditions.
The Diagnostic and Statistical Manual of Mental Disorders , Fifth Edition (DSM-5), a tool mental health professionals use, outlines distinct criteria for identifying derealization.
Individuals experiencing derealization often report feeling separated from their surroundings and perceive the external world as unreal, distorted, or dreamlike. This detachment can cause significant distress, impacting social relationships, work, and daily activities, which is essential for a clinical diagnosis.
The process of diagnosing derealization includes thorough interviews, questionnaires, and, in some cases, psychological testing. Accurate diagnosis is super important as it forms the basis for any treatment plans.
It's also important for healthcare professionals to distinguish derealization from similar disorders to avoid misdiagnosis and ensure appropriate treatment.
Difference from Depersonalization
Derealization and depersonalization, though closely related, are different experiences. While derealization is characterized by an altered perception of the external environment, making the world seem unreal, depersonalization involves feeling estranged from one’s own thoughts, body, and emotions.
Individuals with depersonalization might feel like observers of their lives, leading to a sense of unreality. In clinical settings, it's not uncommon for patients to experience both derealization and depersonalization simultaneously.
When this occurs, a combined diagnosis of Depersonalization/Derealization Disorder is often made, highlighting the connected nature of these dissociative experiences.
Causes and Risk Factors
Biological factors.
Biological factors, including genetics and neurological functioning, are central to understanding derealization.
There is evidence to suggest that individuals with a family history of dissociative disorders are more susceptible to developing derealization, indicating a potential genetic link.
Additionally, changes in brain function and structure have been observed in people experiencing derealization.
Neuroimaging studies have revealed alterations in brain areas associated with perception and stress response , suggesting that neurological factors contribute to the onset and maintenance of this disorder.
Environmental Factors
The environment one is exposed to significantly influences mental health.
For derealization, exposure to high levels of stress, traumatic events, or adverse childhood experiences can trigger the onset of symptoms. These experiences can affect the brain’s stress response system, increasing the likelihood of dissociative symptoms as a coping mechanism.
Understanding the role of environmental factors is crucial in developing effective treatment strategies. Addressing and processing traumatic experiences can be key to alleviating symptoms and reducing the impact of derealization on an individual’s life.
Psychological Stress
Psychological stress is often a precursor to the development of derealization. When individuals encounter prolonged stress, the brain might employ dissociation as a defense mechanism , creating a sense of detachment from the distressing reality.
This detachment, while initially serving as a protective measure, can lead to the chronic experience of derealization if not addressed.
The relationship between stress and derealization underscores the importance of stress management and mental health support in preventing and treating dissociative disorders.
Prevalence and Demographics
Age of onset.
Derealization most commonly first appears during adolescence or early adulthood. This period, marked by numerous changes, transitions, and stressors, can make individuals more vulnerable to developing dissociative symptoms.
However, it’s essential to note that derealization can occur at any age, and individual differences play a significant role in its manifestation.
Early intervention and support are super important in managing symptoms and preventing the progression of the disorder. Recognizing the signs and providing appropriate resources can make a significant difference in the lives of those affected.
Gender Differences
Research on gender differences in derealization presents varied findings. Some studies indicate equal occurrence among males and females, while others suggest that females may be more likely to seek help for dissociative disorders, impacting the observed gender distribution.
Understanding gender differences in the presentation and reporting of derealization is important for tailoring treatment approaches and addressing the unique needs of different populations.
Global Statistics
Experiences of derealization are not uncommon, with studies estimating that up to half of the general population may have encountered at least a short episode of derealization or depersonalization.
However, for a smaller percentage of individuals, these symptoms persist, causing significant distress and impairment in daily life.
Raising awareness of the prevalence of derealization and reducing the stigma associated with it are essential steps towards encouraging affected individuals to seek help and support.
By comprehensively exploring the symptoms, causes, and prevalence of derealization, we can build a solid foundation of understanding this complex condition.
This knowledge serves as a stepping stone to delve deeper into the historical evolution, development of treatments, and future prospects in addressing derealization, providing hope and guidance for those impacted by it.
History of Derealization

Evolution of Derealization Diagnosis
Early descriptions and case.
The term "derealization" has its roots in the 19th century, but it has likely been experienced throughout human history.
The early medical literature contains accounts of individuals describing symptoms remarkably similar to what we now call derealization. These stories, while not labeled as such at the time, highlight the ongoing nature of this condition.
The formal recognition of derealization as a distinct clinical entity occurred gradually.
Early physicians and psychiatrists, such as Pierre Janet in the late 1800s, documented cases, contributing to our initial understanding of this dissociative phenomenon. Their observations paved the way for further research and exploration into the nature of derealization.
Historical Changes in DSM Classification
The evolution of derealization within psychiatric classification systems reflects our growing understanding of this disorder. Initially, derealization and depersonalization were often categorized together under broader classifications of dissociative or neurotic disorders.
The DSM has undergone several revisions, each refining the criteria and classification of derealization.
The most recent edition, DSM-5, recognizes Depersonalization/Derealization Disorder as a distinct diagnosis, reflecting a more detailed understanding and acknowledgement of the uniqueness of these experiences.
Pioneering Researchers and Theories
Pierre janet.
Pierre Janet, a French psychologist, was one of the first to study and document derealization extensively.
Working in the late 19th and early 20th centuries, he explored the relationship between trauma, subconscious mind, and dissociation, laying the groundwork for our modern understanding of derealization.
Janet’s theories emphasized the role of traumatic experiences and psychological stress in the development of dissociative symptoms. He proposed that dissociation served as a defense mechanism, allowing the mind to distance itself from troubling realities, a theory that remains influential in contemporary psychiatry.
Sigmund Freud and Psychoanalytical Approach
Sigmund Freud , the father of psychoanalysis, also contributed to the early understanding of derealization.
While his theories focused primarily on the role of the unconscious mind and internal conflicts, Freud’s exploration of defense mechanisms helped us understand the psychological basis of derealization.
Freud’s psychoanalytical approach highlighted the importance of exploring past experiences and unconscious processes in understanding and treating derealization. This perspective opened avenues for therapeutic interventions, influencing the development of psychotherapy techniques still used today.
Milestones in Treatment Development
Medication advancements.
The 20th century witnessed significant advancements in psychopharmacology, the treatment of mental illnesses with medications, opening new possibilities for treating derealization.
The introduction of antidepressants and anti-anxiety medications provided new tools for managing symptoms, improving the quality of life for many individuals.
Research into the neurological basis of derealization has also led to experimentation with antipsychotic medications, offering additional treatment options. The development and refinement of pharmacological treatments continue to evolve, informed by ongoing research and clinical trials.

Psychotherapy Innovations
Alongside medication advancements, the 20th century also saw the development of various psychotherapy approaches for treating derealization.
Techniques such as Cognitive-Behavioral Therapy (CBT) and Eye Movement Desensitization and Reprocessing (EMDR) emerged, offering promising results for individuals experiencing dissociative disorders. But, they also have their dangers .
These psychotherapy innovations provided new ways to address the underlying psychological factors contributing to derealization.
The emphasis on cognitive restructuring , behavioral interventions, and trauma processing has helped many individuals gain insight, develop coping strategies, and achieve symptom relief.
Conclusion of History
The historical evolution of derealization diagnosis, pioneering research, and treatment development provides a rich backdrop to our current understanding of this complex condition.
By acknowledging the contributions of early researchers and appreciating the advancements in treatment, we gain perspective on the progress made and the possibilities that lie ahead for individuals living with derealization.
Modern Treatment Approaches
Psychotherapy, cognitive-behavioral therapy (cbt).
CBT stands as one of the most effective treatment approaches for derealization. It focuses on identifying and challenging irrational thoughts and beliefs, helping individuals develop healthier thinking patterns and coping mechanisms.
Therapists work with clients to address distressing thoughts, explore alternative perspectives, and practice grounding techniques to manage symptoms.
Eye Movement Desensitization and Reprocessing (EMDR)
EMDR is a notable psychotherapy technique, particularly for individuals whose derealization is linked to trauma. The therapy involves recalling traumatic memories while receiving bilateral sensory input, such as side-to-side eye movements.
This process can help individuals reprocess traumatic memories, reducing their impact and alleviating derealization symptoms.
Mindfulness and Acceptance-Based Therapies
These therapies teach individuals to observe their thoughts and feelings non-judgmentally and to live in the present moment.
Mindfulness and acceptance-based approaches can be particularly helpful for managing derealization by grounding individuals in the present and reducing anxiety and distress associated with feelings of unreality.
Dialectical Behavior Therapy (DBT)
DBT combines cognitive-behavioral techniques with mindfulness principles. It’s designed to help individuals regulate emotions, tolerate distress, and improve interpersonal relationships.
For those with derealization, DBT can offer tools to manage emotional swings and maintain connections with reality.
Selective Serotonin Reuptake Inhibitors (SSRIs)
SSRIs are commonly prescribed for individuals experiencing derealization, especially when co-occurring with anxiety or depression.
These medications can help regulate mood and reduce anxiety, which may alleviate the intensity and frequency of derealization episodes.
Benzodiazepines
For short-term relief of severe anxiety and distress associated with derealization, benzodiazepines may be prescribed.
However, due to the risk of dependency and tolerance, they are typically not recommended for long-term use in treating derealization.
Antipsychotic Medication
In some cases, low doses of antipsychotic medication may be beneficial for managing severe symptoms of derealization, particularly when other treatments have been ineffective. The use of antipsychotics should be carefully monitored due to potential side effects.
Non-Benzodiazepine Anxiolytics
Medications like buspirone, which are less habit-forming than benzodiazepines, can be effective for managing anxiety symptoms associated with derealization. They may serve as a safer long-term option for some individuals.
Lifestyle Modifications and Coping Strategies
Regular exercise and healthy diet.
Adopting a healthy lifestyle, including regular exercise and a balanced diet, can help improve overall mental well-being. Physical activity has been shown to reduce stress and improve mood, which can contribute to managing derealization symptoms.
Adequate Sleep and Stress Management
Ensuring adequate sleep and managing stress are essential for individuals with derealization. Establishing a regular sleep schedule and practicing relaxation techniques like deep breathing and meditation can enhance mental health and reduce symptom frequency.
Building Supportive Relationships
Building and maintaining supportive relationships can be particularly helpful for individuals experiencing derealization. Having a support network provides a sense of connection and reality, which can be grounding for those feeling detached from their surroundings.
Mindfulness and Grounding Techniques
Practicing mindfulness and grounding techniques can help individuals stay connected to the present moment and reality. Techniques such as focused breathing, sensory awareness, and guided imagery can be helpful in managing episodes of derealization.
Conclusion of Treatments
Modern treatment approaches for derealization are diverse and multifaceted, addressing both the psychological and physiological aspects of the condition.
From psychotherapy to medication and lifestyle modifications, individuals living with derealization have a range of options to explore for managing and alleviating their symptoms.
Tailoring treatment to individual needs and preferences is key to fostering recovery and improving quality of life.
Challenges in Treatment and Management
Identifying Individual Triggers
Variability of triggers.
Each individual with derealization may have unique triggers that begin episodes. These can range from stress and anxiety to specific environments or sensory stimuli .
Identifying and understanding these triggers is crucial for effective management but can be challenging due to their variability.
Personalized Approach
A personalized approach, involving thorough assessment and individualized treatment planning, is essential to address the specific triggers and needs of each person.
Collaboration between the individual and the treatment team is key to identifying triggers and developing effective coping strategies.
Co-Occurring Disorders
Commonality of comorbidity.
Derealization often does not occur on its own and can be accompanied by other mental health conditions such as anxiety, depression, and post-traumatic stress disorder (PTSD). Having more than one condition is known as "comorbidity."
Addressing co-occurring disorders is integral to successful treatment but adds complexity to the management process.
Holistic Treatment Planning
A holistic approach that addresses all aspects of an individual’s mental health is necessary for effective treatment.
Using various therapies and interventions that target both derealization and any co-occurring conditions can optimize outcomes and support overall well-being.
Stigma and Misunderstanding
Public perception.
Despite growing awareness, derealization remains misunderstood by the general public and, occasionally, by healthcare professionals.
This lack of understanding can lead to stigma, which may deter individuals from seeking help and support.
Educational Initiatives
Increasing education and awareness about derealization among healthcare providers and the wider community is essential to reduce stigma and improve access to appropriate care.
Community outreach, educational campaigns, and professional training can help foster understanding and acceptance.
Obeying Treatment and Accessibility
Challenges in obeying.
Sticking to treatment plans can be challenging for individuals with derealization, especially when symptoms are severe or ongoing.
Motivational strategies, ongoing support, and regular follow-ups are crucial to encourage adherence and monitor progress.
Access to Care
Accessibility to mental health services can be a significant barrier for many.
Efforts to improve access, such as expanding telehealth options and increasing availability of community-based services, are essential to ensure that those in need receive appropriate care.
Conclusion of Challenges
Addressing the challenges in treating and managing derealization is vital to improve the lives of those affected by this condition.
By recognizing individual differences, addressing co-occurring disorders, combating stigma, and enhancing treatment adherence and accessibility, we can build a more supportive and effective mental health landscape for individuals experiencing derealization.
Examples of Derealization Treatments
Case Study 1: Sarah
Sarah, a 30-year-old graphic designer, started experiencing episodes of derealization following a car accident. She described feeling as though the world around her was unreal and dreamlike, which greatly impacted her daily functioning and quality of life.
- Treatment Approach Sarah was introduced to a combination of Cognitive-Behavioral Therapy (CBT) and medication. The therapy focused on identifying and challenging her irrational thoughts and beliefs, while SSRIs were prescribed to regulate her mood and reduce anxiety.
- Outcome Over several months, Sarah reported a decrease in the frequency and intensity of her derealization episodes. The personalized approach helped her develop healthier thinking patterns, manage anxiety, and regain a sense of reality and control.
Case Study 2: Alex
Alex, a 22-year-old college student, developed derealization symptoms in response to high academic and social pressures. For Alex, episodes would manifest through a profound sense of disconnection from his environment and peers.
- Treatment Approach Alex engaged in Dialectical Behavior Therapy (DBT) to regulate emotions and improve interpersonal relationships. Additionally, he adopted lifestyle modifications, including regular exercise and mindfulness practices, to manage stress.
- Outcome With consistent therapy and lifestyle changes, Alex experienced significant improvement. He learned to handle academic pressures more effectively and felt more connected to his surroundings and peers.
Case Study 3: Emily
Emily, a 40-year-old teacher, had lived with untreated derealization for several years, stemming from childhood trauma. The condition manifested in her adult life during stressful periods, making her feel detached and alienated.
- Treatment Approach Emily underwent Eye Movement Desensitization and Reprocessing (EMDR) to address the underlying trauma contributing to her derealization. Simultaneously, she was prescribed a low dose of an antipsychotic medication to manage severe symptoms.
- Outcome The combination of EMDR and medication enabled Emily to reprocess traumatic memories and alleviate the intensity of her derealization symptoms. Over time, she reported feeling more grounded and present in her daily life.
Case Study 4: Michael
Michael, a 50-year-old engineer, experienced chronic derealization, accompanied by severe anxiety. His work and relationships were significantly affected, as he struggled to maintain a connection with reality.
- Treatment Approach Michael’s treatment included a combination of benzodiazepines for short-term relief of anxiety and distress, alongside Mindfulness and Acceptance-Based Therapies to anchor him in the present and reduce distress.
- Outcome Through medication and therapy, Michael gained tools to manage his anxiety and derealization. He reported a renewed sense of engagement with his environment and relationships, leading to an improved quality of life.
Conclusion of Case Studies
These case studies illustrate the diversity of derealization experiences and the need for personalized treatment approaches. Each individual faced unique challenges but found relief through a combination of therapy, medication, and lifestyle changes. The positive outcomes highlight the potential for recovery and underscore the importance of early intervention and tailored treatment strategies in managing derealization.
Future Directions in Research and Treatment
Advances in neuroscience, neuroimaging studies.
Ongoing neuroimaging studies continue to unravel the brain’s intricacies and how alterations in brain structure and function contribute to derealization.
These discoveries can inform the development of novel treatments and interventions, targeting the neurological underpinnings of the disorder.
Neuropharmacology
Advances in neuropharmacology hold promise for refining medication treatments for derealization.
New drugs, acting on specific neurotransmitter systems implicated in derealization, are being researched and developed, aiming to provide more effective and personalized treatment options.
Integrative and Holistic Approaches
Mind-body connection.
Exploring the mind-body connection and integrating physical and mental health care can offer innovative approaches to treating derealization.
Practices such as yoga, meditation, and biofeedback are gaining recognition for their potential to enhance well-being and alleviate dissociative symptoms.
Personalized and Precision Medicine
The move towards personalized and precision medicine in psychiatry allows for treatments tailored to the individual’s genetic, biological, and psychological makeup.
This personalized approach can optimize treatment efficacy and minimize adverse effects, offering a more targeted and effective strategy for managing derealization.
Technological Innovations
Virtual reality (vr) and biofeedback.
The application of technology, such as VR and biofeedback , in mental health treatment opens up new avenues for therapy. These tools can offer immersive and interactive experiences, aiding in exposure therapy, relaxation training, and real-time monitoring of physiological responses.
Telehealth and Online Resources
The expansion of telehealth and online mental health resources increases accessibility to care and support.
These platforms can provide remote therapy, peer support, and educational materials, reaching individuals who might otherwise face barriers to accessing mental health services.
Derealization, while a challenging and often misunderstood condition, is gradually coming into the light with advancements in research, treatment, and public awareness.
The strides made in understanding this disorder, from the pioneering work of early researchers to modern-day innovations, reflect a trajectory of progress and hope.
By continuing to explore new frontiers in neuroscience, embracing holistic and integrative approaches, and leveraging technological innovations, we can look forward to a future where derealization is effectively understood, treated, and perhaps, prevented.
Related posts:
- Beck’s Depression Inventory (BDI Test)
- The Psychology of Long Distance Relationships
- Abandonment Issues (Examples, Causes, and Treatment)
- Operant Conditioning (Examples + Research)
- Variable Interval Reinforcement Schedule (Examples)
Reference this article:
About The Author
Free Personality Test
Free Memory Test
Free IQ Test
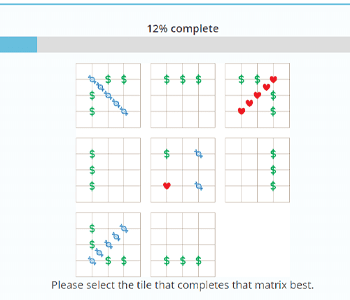
PracticalPie.com is a participant in the Amazon Associates Program. As an Amazon Associate we earn from qualifying purchases.
Follow Us On:
Youtube Facebook Instagram X/Twitter
Psychology Resources
Developmental
Personality
Relationships
Psychologists
Serial Killers
Psychology Tests
Personality Quiz
Memory Test
Depression test
Type A/B Personality Test
© PracticalPsychology. All rights reserved
Privacy Policy | Terms of Use
- MSD careers
Depersonalization/Derealization Disorder
- Diagnosis |
- Treatment |
- Prognosis |
Depersonalization/derealization disorder involves a persistent or recurring feeling of being detached from one’s body or mental processes, like an outside observer of one's life (depersonalization), and/or a feeling of being detached from one's surroundings (derealization).
The disorder is usually triggered by severe stress, particularly emotional abuse or neglect during childhood , or other major stresses (such as experiencing or witnessing physical abuse).
Feelings of detachment from self or the surroundings may occur periodically or continuously.
After tests are done to rule out other possible causes, doctors diagnose the disorder based on symptoms.
Psychotherapy , especially cognitive-behavioral therapy, is often helpful.
(See also Overview of Dissociative Disorders .)
Temporary feelings of depersonalization and/or derealization are common. About one half of people have felt detached from themselves (depersonalization) or from the surroundings (derealization) at one time or another. This feeling often occurs after people
Experience life-threatening danger
Take certain drugs (such as marijuana , hallucinogens , , or methylenedioxymethamphetamine [ecstasy] )
Become very tired
Are deprived of sleep or sensory stimulation (as may occur when they are in an intensive care unit)
Depersonalization or derealization can also occur as a symptom in many other mental health disorders, as well as in general medical disorders, such as seizure disorders .
Depersonalization/derealization feelings are considered a disorder when the following occur:
Depersonalization or derealization occurs on its own (that is, it is not caused by drugs or another mental health disorder), and it persists or recurs.
The symptoms are very distressing to the person or make it difficult for the person to function at home or at work.
Depersonalization/derealization disorder occurs in about 2% of the population and affects men and women equally.
The disorder may begin during early or middle childhood. It rarely begins after age 40.
Causes of Depersonalization/Derealization Disorder
Depersonalization/derealization disorder often develops in people who have experienced severe stress, including the following:
Emotional abuse or neglect during childhood
Physical abuse
Experiencing or witnessing domestic violence
Having a severely impaired or mentally ill parent
Unexpected death of a loved one
Symptoms can be triggered by severe stress (for example, due to relationships, finances, or work), depression , anxiety , or use of illicit drugs . However, in 25 to 50% of cases, the causes of stress are relatively minor or cannot be identified.
Symptoms of Depersonalization/Derealization Disorder
Symptoms of depersonalization/derealization disorder may start gradually or suddenly. Episodes may last for only hours or days or for weeks, months, or years. Episodes may involve depersonalization, derealization, or both.
The intensity of symptoms often waxes and wanes. But when the disorder is severe, symptoms may be present and remain at the same intensity for years or even decades.
Depersonalization symptoms involve
Feeling detached from one's body, mind, feelings, and/or sensations
People may also say they feel unreal or like an automaton, with no control over what they do or say. They may feel emotionally or physically numb. Such people may describe themselves as an outside observer of their own life or the “walking dead.”
Derealization symptoms involve
Feeling detached from the surroundings (people, objects, or everything), which seem unreal
People may feel as if they are in a dream or a fog, or as if a glass wall or veil separates them from their surroundings. The world seems lifeless, colorless, or artificial. The world may appear distorted to them. For example, objects may appear blurry or unusually clear, or they may seem flat or smaller or larger than they are. Sounds may seem louder or softer than they are. Time may seem to be going too slow or too fast.
The symptoms almost always cause great discomfort. Some people find them intolerable. Anxiety and depression are common. Many people are afraid that the symptoms result from irreversible brain damage. Many worry about whether they really exist or repeatedly check to determine whether their perceptions are real.
Stress, worsening depression or anxiety, new or overstimulating surroundings, and lack of sleep can make symptoms worse.
Symptoms are often persistent. People may have symptoms all the time, or symptoms may come and go with periods of time with no symptoms.
People often have great difficulty describing their symptoms and may fear or believe that they are going crazy. However, people always remain aware that their experiences of detachment are not real but rather are just the way that they feel. This awareness is what separates depersonalization/derealization disorder from a psychotic disorder. People with a psychotic disorder, such as schizophrenia , have thoughts that are not consistent with reality, but they do not realize these are different from usual thoughts.
Diagnosis of Depersonalization/Derealization Disorder
A doctor's evaluation, based on specific diagnostic criteria from the Diagnostic and Statistical Manual of Mental Disorders , Fifth Edition, Text Revision (DSM-5-TR)
Sometimes tests to rule out other possible causes
Doctors suspect the disorder based on symptoms:
People have episodes of depersonalization, derealization, or both that last a long time or recur.
People know that their dissociative experiences are not real.
People are very distressed by their symptoms or their symptoms make them unable to function in social situations or at work.
A physical examination and sometimes tests are done to rule out other disorders that could cause the symptoms, including other mental health disorders, seizure disorders , and substance use disorders . Tests may include magnetic resonance imaging (MRI), computed tomography (CT), electroencephalography (EEG), and blood and urine tests to check for use of illicit drugs.
Psychologic tests and special structured interviews and questionnaires can also help doctors with the diagnosis.
Treatment of Depersonalization/Derealization Disorder
Psychotherapy
Sometimes antianxiety medications and antidepressants
Depersonalization/derealization disorder may disappear without treatment. People are treated only if the disorder persists, recurs, or causes distress.
Various psychotherapy methods have been effective for some people. Depersonalization/derealization disorder is often associated with or triggered by other mental health disorders (such as anxiety or depression ), which require treatment. Any stresses that triggered the symptoms or that may have contributed to development of depersonalization/derealization disorder must also be addressed.
Techniques that can help include the following:
Cognitive techniques can help block obsessive thinking about the unreal state of being.
Behavioral techniques can help people become absorbed in tasks that distract them from the depersonalization.
Grounding techniques use the five senses (hearing, touch, smell, taste, and sight) to help people feel more connected to themselves and the world. For example, loud music is played or a piece of ice is put in the hand. These sensations are difficult to ignore, making people aware of themselves in the present moment.
Psychodynamic techniques focus on helping people work through intolerable conflicts, negative feelings, and experiences from which people feel they must detach themselves.
Moment-to-moment tracking and labeling of dissociation and affect (the outward expression of emotions and thoughts) teaches people to recognize and identify their feelings of dissociation. Such recognition helps some people. This technique also helps people focus on what is actually happening in the moment.
Various medications have been used to treat depersonalization/derealization disorder, but none have proven to be effective. Antianxiety medications and antidepressants sometimes help, mainly by relieving anxiety or depression, which are present in many people with depersonalization/derealization disorder. However, antianxiety medications may also increase depersonalization or derealization, so doctors carefully monitor use of these medications.
Prognosis for Depersonalization/Derealization Disorder
Complete recovery is possible for many people with depersonalization/derealization disorder, especially if the symptoms result from stresses that can be dealt with during treatment. Other people do not respond well to treatment, and the disorder becomes chronic. In some people, depersonalization/derealization disorder disappears on its own.
Symptoms, even those that persist or recur, may cause only minor problems if people can keep their mind busy and focus on other thoughts or activities, rather than think about their sense of self. However, some people become disabled because they feel so disconnected from their self and their surroundings or because they also have anxiety or depression.

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
- Cookie Preferences

Depersonalization (DPDR): What It Is and How to Overcome It
Olivia Guy-Evans, MSc
Associate Editor for Simply Psychology
BSc (Hons) Psychology, MSc Psychology of Education
Olivia Guy-Evans is a writer and associate editor for Simply Psychology. She has previously worked in healthcare and educational sectors.
Learn about our Editorial Process
Saul Mcleod, PhD
Editor-in-Chief for Simply Psychology
BSc (Hons) Psychology, MRes, PhD, University of Manchester
Saul Mcleod, PhD., is a qualified psychology teacher with over 18 years of experience in further and higher education. He has been published in peer-reviewed journals, including the Journal of Clinical Psychology.
On This Page:
- Depersonalization is a dissociative disorder that affects a person’s perception of themselves and their surroundings. It is characterized by recurring episodes of depersonalization, derealization, or both.
- Depersonalization involves feeling detached from oneself, as if observing one’s thoughts, emotions, and actions from a distance. Derealization, on the other hand, involves feeling that the world around is unreal, distorted, or dreamlike. People and objects may appear fuzzy, lifeless, or two-dimensional.
- Other symptoms include feeling emotionally numb, disconnected from one’s surroundings, and experiencing memory difficulties.
- If you suspect you may be experiencing depersonalization/derealization disorder, it is important to seek the help of a mental health professional.

What is depersonalization?
Depersonalization is a complex symptom that can be defined as ‘a state in which the sense of self and the quality of subjective first-person experience are oddly altered’ (Medford, 2012).
It can be described as feeling disconnected from the self or feeling as though you aren’t real.
It can be normal to feel depersonalization from time to time, especially in times of stress, upset, fatigue, or with drug use. Transient episodes of depersonalization have a lifetime prevalence between 26% and 74% of someone experiencing at least one episode.
What is derealization?
Derealization is also a part of the disorder, and this symptom affects how individuals relate to other people and their environment. They may feel as if their surroundings or other people are not real.
While depersonalization is defined as disconnections from the self, derealization is defined as disconnections from external reality.
Derealization is conceptualized as a sense of “unreality or detachment from, or unfamiliarity with, the world, be it individuals, inanimate objects, or all surroundings” (APA, 2013, p. 303).
A person who experiences derealization might feel as though they are in a fog or a dream or that the surrounding world is somehow artificial and unreal.
When does depersonalization become a disorder?
For most people who depersonalize, this feeling will usually diffuse once the stressful situation is over or once the drug has run its course (if caused by drug use).
Often, depersonalization is viewed as the mind’s defense mechanism to help cope with stressful situations.
Feelings of depersonalization can become pathological when the individual is unable to control when and where these symptoms occur, when the depersonalization becomes generalized to other situations and circumstances, or when it persists beyond the presence of a stressor.
In this situation, it is possible that the individual may have what was previously known as depersonalization disorder, now known as depersonalization/derealization disorder (DPDR).
DPDR is classified as one of 3 dissociative disorders, the others being dissociative amnesia and dissociative identity disorder.
Dissociative disorders are mental conditions involving disruptions or breakdowns in awareness, consciousness, and memory. For people with DPDR, the periods of dissociation can last for a relatively short amount of time (minutes or hours), or sometimes much longer (days, weeks, months, or years).
Most people with DPDR develop it when they are young. The average age for the onset of DPDR is 16, with the condition rarely beginning after the age of 40. The prevalence of this disorder is thought to affect around 1-2% of the general population (Hunter et al., 2004).
Individuals who experience depersonalization might believe their thoughts and feelings are not their own.
They may feel robotic, as though they lack control over their movements and speech; they may experience a distorted sense of time, and, in extreme cases, they may sense an “out-of-body” experience in which they see themselves from the perspective of another person.
Individuals with DPDR often have difficulty describing their symptoms and may think they are ‘going crazy’ (APA, 2013).
It is worth noting that DPDR can present differently in everyone. The specific traits and difficulties that individuals with DPDR experience can be unique and may vary in severity. Not everyone with DPDR will experience all of the symptoms.
Likewise, many people may identify with one or more symptoms of the disorder but may not qualify for a full diagnosis.
Below are some of the key symptoms of DPDR:

Feeling disconnected from reality
People who experience depersonalization may feel as if there is a barrier between themselves and the world. They may feel as though they are living in a dream or that things around them are not real.
Feeling like you’re not real
People may feel their movements and actions do not feel like their own. They may feel as though they are watching someone else. Sometimes people will report feeling as if they are watching themselves from the outside, as if they are an onlooker.
Fear of losing one’s mind
Many people may worry that their depersonalization symptoms will become so intense that they could be insane. However, depersonalization is the brain reacting to what it perceives as danger, although it is not always accurate.
Visual symptoms
Many people who experience depersonalization report visual symptoms such as tunnel vision, distorted and blurry vision, experiencing floaters in their vision, or the distance and size of objects being altered.
A possible explanation is that when anxious, the eyes naturally become more sensitive to picking up movements by dilating the pupils to let more light in.
This can make it feel as if there is too much visual information coming in at once.
Distorted perception of time
Often, people may report that they feel like time goes by too fast, there are gaps of time that are forgotten, they find they jump from one moment to another, recent events feel old, or old events feel recent.
This may be happening because the anxiety is affecting the concentration of individuals, so the passing of time feels different. The racing thoughts that they have could distract them from the time going by.
Memory loss
Occasionally, those experiencing depersonalization may have issues with their memory. They may forget what they were doing or saying, cannot remember what happened the day previously, or feel as if they are losing their short or long-term memory.
However, this is likely the anxiety affecting memory, as anxiety usually affects concentration. This can make it seem like the memories have gone blank, and one cannot focus on the task at hand.
Emotional numbness
This symptom is described as an inability to feel happy, sad, or any emotion. An explanation for why this may happen is that since depersonalization is a defense mechanism that keeps someone safe, it can make them feel distant and cut off.
Pairing this with racing thoughts and finding it difficult to concentrate can make things feel worse.
There is nothing wrong with the person’s emotions or the ability to feel them; these are only the temporary effects of anxiety and its symptoms.
People who depersonalize often find that their mind is empty, their thoughts are gone, or they cannot put a thought together. Having a blank mind is often described as losing one’s inner monologue.
However, you only experience this inner monologue when not consciously thinking about it, so if individuals are constantly trying to see if this is present, they are often interrupting it.
Existential thoughts
As depersonalization is a bizarre experience, the rational brain is desperately trying to find an explanation as to what is causing this.
Often, people may attribute the bizarre feelings to having significance, such as thinking they may be in a coma, dreaming, or purgatory, for instance.
Our brains tend to want big explanations, so it often jumps to the scariest conclusions – this is known as catastrophizing.
Reality testing
Those affected by depersonalization may believe they are experiencing psychosis due to some of the symptoms mentioned earlier. However, the big distinction with depersonalization disorder is that the individuals have intact reality testing.
This is the objective evaluation of an emotion or thought against real life. So even with the most frightening thoughts, one can always distinguish between thoughts and reality.
Some people with DPDR may experience mild, short-lived symptoms, while others have chronic symptoms that may last for years.
The symptoms may be very distressing to the point where they interfere with their ability to function in daily life, including at work, school, or in relationships.
Are symptoms similar to other disorders?
The symptoms of depersonalization may be observed in other disorders, such as anxiety disorders such as post-traumatic stress disorder (PTSD), and panic disorder, as well as depression and schizophrenia.
Those with DPDR frequently experience cognitive symptoms of increased arousal paired with subjective deficits in attention and concentration, as seen in anxiety disorders. High levels of co-existing anxiety have been found in people with DPDR (Michal et al., 2016).
Causes and risk factors
There is not always a clear cause for what causes depersonalization and DPDR. In a lot of cases, care providers are not able to identify what triggers this disorder in patients.
Many people with this disorder report a history of childhood trauma, particularly emotional abuse and neglect. For someone growing up in a household with a lot of violence or yelling, they may have mentally removed themselves from those situations as a coping mechanism.
Thus, as adults, they may fall back onto these dissociating tendencies in stressful situations. Or they may find that they dissociate when there is no known trigger, but it could link back to their childhood trauma.
Some people may find that they depersonalize after experiencing trauma or intense stress which did not occur in childhood. This may occur after the following:
Witnessing or experiencing abuse
An accident
Encountering a life-threatening danger
Natural disasters
The death of a loved one
Violence or war
Hunter et al. (2003) proposed that depersonalization disorder is most often triggered by one’s response to situations that provoke anxiety. This symptom overlap and high comorbidity of DPDR with anxiety disorders indicate there may be a link between DPDR and anxiety.
Some other causes of depersonalization include:
Certain drugs, such as hallucinogens
Extreme fatigue and sleep deprivation
Physical conditions such as seizure disorder
Living with a parent who has a severe mental illness
A co-existing mental health condition
Treatment options
In terms of treatment, this depends on the severity of the depersonalization symptoms being experienced and whether DPDR is diagnosed.
During periods of acute stress or some episodes of depersonalization, supportive interventions such as coping skills and strategies may be a good fit.
Whereas, during periods of mild to more severe symptoms and a diagnosis of DPDR, other approaches may be required.
There are currently no known medicative treatments for DPDR. While there is no specific medication, antidepressants may be helpful, especially if there is underlying depression or anxiety alongside DPDR.
However, for some people, antidepressants may actually increase depersonalization or derealization symptoms. Trials of a type of antidepressant called selective serotonin reuptake inhibitors (SSRIs) with people who had a diagnosis of DPDR found that this medication may induce some of the symptoms to make the condition worse (Brand et al., 2012).
Otherwise, atypical antipsychotic medications that block both dopamine and serotonin receptors may be useful in treating some cases of DPDR with ‘psychotic features.’
It is worth noting that medications can come with possible side effects and may not be suitable for everyone. It is advisable to speak to a professional if you are considering meditative treatment.
Psychotherapies
Psychotherapies such as psychodynamic or cognitive behavioral therapy (CBT) may be effective for managing the symptoms of DPDR.
Psychodynamic psychotherapy uses self-reflection and self-evaluation achieved through cooperation and interrelationship with a psychiatrist. The expectation is that the patient will explore effective coping strategies and relationship patterns.
The psychiatrist will attempt to reveal the unconscious components of the patient’s maladaptive functioning to tackle the symptoms being experienced.
CBT is focused on identifying and adjusting unhelpful thinking patterns, feelings, and behaviors with a therapist.
Through working with the therapist, the patient can find ways to switch to more realistic thinking patterns and learn coping techniques that can be practiced in times of stress.
Hunter et al. (2005) published a study of patients who received an average of 13 CBT sessions. They found that patients had reductions in their levels of dissociation and depersonalization, with 29% no longer meeting the diagnostic criteria of DPDR after treatment.
Aside from psychodynamic therapy and CBT, people may opt for one of the following:
Dialectical behavior therapy (DBT) – this is a type of CBT that may help individuals with tolerating difficult emotions, including dissociative symptoms. It may also be useful for those who have experienced abuse or trauma.
Family therapy – working together, the individual’s family can learn about depersonalization. The group can learn how to recognize signs of when this occurs and offer their support when it does.
Creative therapies – art or music therapy can help individuals to explore and express their thoughts and feelings in a safe and creative environment.
Managing DPDR
When experiencing episodes of depersonalization, some techniques can be used to help make the symptoms more manageable.
Acknowledge your feelings
Often, acknowledging what you are feeling and the emotions being experienced can help to lessen these feelings.
It may be helpful to name the emotion you are experiencing to bring awareness and understanding to your feelings.
Breathing exercises
When moments of stress and anxiety arises, the body’s sympathetic nervous system fires up, which can lead to feelings of depersonalization.
Breathing exercises, especially deep breathing, may help reset the nervous system, calming it down. Guided meditation and mindfulness training usually include deep breathing and can also calm the body down.
Listen to music
Feelings of depersonalization can become more intense when the brain focuses on them. Using a grounding technique, such as listening to music, may help you feel less anxious about the experience.
Music has been known to reduce cortisol levels, a stress hormone. It may be useful to keep a specific playlist of favorite songs which can be played when experiencing depersonalization symptoms.
Read a book
Reading a book may be another way to help with the anxious thoughts that often occur alongside depersonalization. This may help to focus the mind on something else, interrupting the intrusive thoughts.
Concentrating on the words and being immersed in a story could help ease negative thoughts.
Challenge intrusive thoughts
Some people who experience depersonalization may have a lack of intrusive thoughts. However, for others, especially if they also have anxiety disorders or PTSD, intrusive thoughts can pose a challenge.
There is a tool called psychological distancing which can be used to help quiet intrusive thoughts.
Psychological distancing means one finds space between upsetting thoughts and painful emotions. You may ask yourself what evidence there is that the intrusive thoughts are real.
Finding that there is little to no evidence that these thoughts are real can help provide realistic and rational thoughts over intrusive thoughts.
Talk to a trusted friend
Often when experiencing depersonalization, it is tempting to isolate yourself away from others. But at these times, talking to a trusted friend or family member may help.
Sharing these struggles with others can help you feel better. As well as this, others may provide some useful advice or insight which can further help you.
Getting enough sleep
Although this is more of a longer-term method, going to sleep when the body feels tired can help with managing stress and decrease anxiety.
Some people may experience depersonalization due to being fatigued, so keeping a regular sleeping schedule can be really beneficial to mental health.
Also, keeping bedtime as relaxing as possible can aid in better sleep, such as ensuring that phones or other screens are not used in bed or before trying to sleep.
Engaging in exercise is often proven to help with managing stress and can be beneficial to mental health. Aerobic exercise, for instance, could help decrease burnout as a result of depersonalization.
Engaging your senses
If you find yourself in a situation where you feel the symptoms of depersonalization starting to creep up on you, it can be useful to try engaging all your senses.
Being able to engage the senses can help with checking that you are real and can also help in grounding yourself in your body and surroundings.
Engaging the senses can include holding ice cubes, eating sour candy, smelling spices, strong coffee, or essential oils.
Related Articles
Schauer, M., & Elbert, T. (2015). Dissociation following traumatic stress. Journal of Psychology.
Brand, B. L., Lanius, R., Vermetten, E., Loewenstein, R. J., & Spiegel, D. (2012). Where are we going? An update on assessment, treatment, and neurobiological research in dissociative disorders as we move toward the DSM-5. Journal of Trauma & Dissociation, 13(1), 9-31.
American Psychiatric Association, D. S., & American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5 (Vol. 5). Washington, DC: American psychiatric association.
Hunter, E. C. M., Phillips, M. L., Chalder, T., Sierra, M., & David, A. S. (2003). Depersonalisation disorder: a cognitive–behavioural conceptualisation. Behaviour Research and Therapy, 41(12), 1451-1467.
Hunter, E. C., Baker, D., Phillips, M. L., Sierra, M., & David, A. S. (2005). Cognitive-behaviour therapy for depersonalisation disorder: an open study. Behaviour research and therapy, 43(9), 1121-1130.
Hunter, E. C., Sierra, M., & David, A. S. (2004). The epidemiology of depersonalisation and derealisation. Social psychiatry and psychiatric epidemiology, 39(1), 9-18.
Medford, N. (2012). Emotion and the unreal self: depersonalization disorder and de-affectualization. Emotion Review, 4(2), 139-144.
Michal, M., Adler, J., Wiltink, J., Reiner, I., Tschan, R., Wölfling, K., Weimert, S., Tuin, I., Subic-Wrana, C., Beutel, M. E. & Zwerenz, R. (2016). A case series of 223 patients with depersonalization-derealization syndrome. BMC psychiatry, 16(1), 1-11.
Neurodiversity , Mental Health
How Cognitive Behavioral Therapy Can Help ADHD

Mental Health
What Does Anorexia Feel Like? Living With An Eating Disorder

What Is Amnesia? Signs, Types, And Can It Be Prevented?

Mental Health , Anxiety , Personality
Avoidant Personality Disorder Vs. Social Anxiety: What Are The Differences?

Mental Health , Personality
How to Spot High Functioning Avoidant Personality Disorder

What are Delusions in Psychology: Definition, Types, Causes, Management
- Annuaire RDR
- Publications
- Inscription
- S'identifier
[ Bad trip ] Déréalisation suite à un Bad trip sous ecstasy
Tania kent a écrit Au mois de Juin 2017, j'étais en dépression, je devais aller en soirée avec des potes, avant cette soirée j'étais pas mal angoissé par rapport à plein de choses, je savais que j'allais prendre un exta pour la deuxième fois de ma vie seulement mais je me doutais pas que ça aller être l'horreur.

- Psychoactif
- » Forums
- » MDMA/Ecstasy
- » Déréalisation suite à un Bad trip sous ecstasy
⊖ Réduire les sous-forums
⊕ agrandir les sous-forums, sujets similaires dans les forums, psychowiki et quizzz, pied de page des forums.
Propulsé par FluxBB Traduction par FluxBB.fr
Dépersonnalisation déréalisation
Derealization
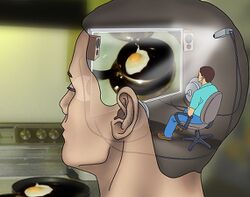
Derealization or derealisation (sometimes abbreviated as DR ) is medically recognized as the experience of feeling detached from, and as if one is an outside observer of, one's surroundings. [1] [2] This effect is characterized by the individual feeling as if they are in a fog, dream, bubble, or something watched through a screen, [3] like a film or video game. [4] These feelings instill the person with a sensation of alienation and distance from those around them.
Derealization can be distressing to the user, who may become disoriented by the loss of the innate sense that their external environment is genuinely real. The loss of the sense that the external world is real can make it feel inherently artificial and lifeless. [4]
This state of mind is commonly associated with and often coincides with depersonalization . While derealization is a perception of the unreality of the outside world, depersonalization is a subjective experience of unreality in one's sense of self.
Derealization is often accompanied by various perceptual distortions such as visual acuity suppression , visual acuity enhancement , and perspective distortions . [4] Other coinciding effects include auditory distortions and depersonalization . [3] [4] This effect is most commonly induced under the influence of moderate dosages of dissociative compounds, such as ketamine , PCP , and DXM . However, it can also occur to a lesser extent during the withdrawal symptoms of stimulants and depressants .
- 2 Psychoactive substances
- 3 Experience reports
- 5 External links
- 6 References
In psychiatry, chronic derealization that arises during sobriety is identified as "Depersonalization/Derealization Disorder" and is classified by both the DSM5 and ICD-11 as a single dissociative disorder. [2] [4]
Temporary derealization symptoms lasting hours to days are common in the general population. Approximately one-half of all adults have experienced at least one episode of depersonalization/derealization within their lifetime, and the gender ratio for the disorder is 1:1. [4] Chronic derealization is more common within individuals who have experienced a severe trauma or prolonged stress and anxiety. The symptoms of both chronic derealization and depersonalization are common within the general population, with a lifetime prevalence of up to 26-74% and 31–66% at the time of a traumatic event. [5]
This effect is a type of cognitive and perceptual dysregulation. [1] It has been demonstrated that derealization may be caused by a dysfunction within the brains visual processing center (occipital lobe) or the temporal lobe, which is used for processing the meaning of sensory input, language comprehension, and emotion association. [6]
Psychoactive substances
Compounds within our psychoactive substance index which may cause this effect include:
- 2-Fluorodeschloroketamine
- Deschloroketamine
- Desoxypipradrol
- Dextromethorphan
- Diphenhydramine
- Diphenidine
- Methoxetamine
- Methoxphenidine
- Methylphenidate
- Rolicyclidine
Experience reports
Annectdotal reports which describe this effect with our experience index include:
- Experience: 300mg DXM (Oral) - Brink of the third
- Experience:100-350mg - Phenylpiracetam in daily life
- Experience:3-MEO-PCMo (420mg) - Trip Report
- Experience:300mg DPH + 600mg DXM - An Interesting Combo
- Experience:535mg - My First DXM Trip
- Experience:DXM and Cannabis: 100mg - Unexpected Strong Trip
- Experience:MXE: 37.5 mg - Calm and Cloudy Bliss
- Experience:Nitrous oxide (approx. 50 puffs) - ~50 puffs nitrous oxide
- Experience:Unknown Dose DOC (Insufflated) - Overdosing and Terifying Ego Death
- Experience:~150mg MDA(oral) - a case of mistaken identity
- Responsible use
- Depersonalization
- Dissociative
- Subjective effects index
External links
- Derealization (Wikipedia)
- ↑ 1.0 1.1 "Glossary of Technical Terms". Diagnostic and statistical manual of mental disorders (5th ed.) : 818–20. 2013. doi : 10.1176/appi.books.9780890425596.GlossaryofTechnicalTerms .
- ↑ 2.0 2.1 "Depersonalization-derealization disorder" . International statistical classification of diseases and related health problems (11th ed.) . 2022 . Retrieved 20 May 2022 .
- ↑ 3.0 3.1 Espiard, M.-L., Lecardeur, L., Abadie, P., Halbecq, I., Dollfus, S. (August 2005). "Hallucinogen persisting perception disorder after psilocybin consumption: a case study" . European Psychiatry . 20 (5–6): 458–460. doi : 10.1016/j.eurpsy.2005.04.008 . ISSN 0924-9338 .
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Dissociative Disorders . Diagnostic and statistical manual of mental disorders (5th ed.) (Fifth Edition ed.). American Psychiatric Association. 22 May 2013. doi : 10.1176/appi.books.9780890425596.dsm08 . ISBN 9780890425558 . CS1 maint: Extra text ( link )
- ↑ Hunter, E. C. M., Sierra, M., David, A. S. (1 January 2004). "The epidemiology of depersonalisation and derealisation" . Social Psychiatry and Psychiatric Epidemiology . 39 (1): 9–18. doi : 10.1007/s00127-004-0701-4 . ISSN 1433-9285 .
- ↑ Sierra, M., Lopera, F., Lambert, M. V., Phillips, M. L., David, A. S. (1 April 2002). "Separating depersonalisation and derealisation: the relevance of the "lesion method " " . Journal of Neurology, Neurosurgery & Psychiatry . 72 (4): 530–532. doi : 10.1136/jnnp.72.4.530 . ISSN 0022-3050 .
- CS1 maint: Extra text
Navigation menu

IMAGES
VIDEO
COMMENTS
Bonjour depuis environ 6 mois je suis dépersonnalisation déréaliser , suite a un bad trip , j'ai fait mon bad trip puis 1 mois après mais symptomes on apparut , je suis aller voir un psychiatre et psychologue , mon psychiatre ma dit que c'était des angoisse , alors que j'arrête d'angoisser y'a pas d
Depersonalization and derealization after a bad trip: my perspective. In this video, I discuss the way that I have come to view feelings of derealization and depersonalization. These are two concepts that are brought up to me quite frequently, so I wanted to take the time to address them in video format. Because they are feelings rather than ...
Déréalisation, questions existencielles suite à un bad trip. Partagez-la. Suite à une prise d'ecstasy en trop forte quantité j'ai fait un badtrip avec hallucinations. Ces hallucinations étaient très réalistes et troublantes (pas psychédéliques) comme des bugs visuels sur le réel.
There is no such thing as a bad trip. DP/DR is not permanent. The only way your trip was bad is in a short-term context. However, your trip was not truly bad - in fact you are even privileged to have gone through it. There's a good saying, a system once broken down grows back even stronger.
One of the key derealization symptoms is a constant feeling of illusion or detachment from the world around you. Imagine as though you are viewing the world through a fog or veil, with things and other people seeming distant or strange. This continuous sense of isolation can be stressful and distracting, causing increased anxiety and trouble ...
Derealisation after having bad trip . Hello guys. I've been dealing with derealisation for 3 weeks. I think this started when I smoked and had a bad trip because I was panicking and was scared for my life. Everything went back to normal and that was about 2 months ago. A month later I would randomly have moments where my brain would think ...
Derealization and depersonalization refer to feelings that the external world and your own self, respectively, are unreal. Lumping the terms together, psychiatrists define depersonalization ...
Self-diagnosis isn't the answer. Oftentimes, when people feel weird after a bad trip for a very long time, they tend to worry that what they're experiencing is permanent. The tendency to self-diagnose kicks in, making the sense of anxiety worse. There are all kinds of scary-sounding things you can diagnose yourself with via WebMD, but doing ...
13K subscribers in the derealization community. For help, discussion, treatment, and management of derealization/ depersonalization.
Bouts of depersonalization-derealization disorder may last hours, days, weeks or months. In some people, these bouts turn into ongoing feelings of depersonalization or derealization that may get better or worse at times. When to see a doctor. Passing feelings of depersonalization or derealization are common and are not always a cause for concern.
Tip #6 Experiment with other things. Finally, I learned to experiment with a few things to help me with the fear of driving. I found that depersonalization and derealization can make it appear as if everything is bright, so having sunglasses helped me calm my nerves during the daytime.
While derealization is characterized by an altered perception of the external environment, making the world seem unreal, depersonalization involves feeling estranged from one's own thoughts, body, and emotions. Individuals with depersonalization might feel like observers of their lives, leading to a sense of unreality.
De nombreux patients disent également qu'ils ont un sentiment d'irréalité (déréalisation) ou d'être un robot (ne pas avoir de contrôle sur ce qu'ils font ou disent). Ils peuvent se sentir émotionnellement et physiquement engourdis ou se sentir détachés, avec peu d'émotion. Certains patients ne peuvent pas reconnaître ou décrire ...
In depersonalization-derealization disorder, you feel detached from yourself (depersonalization) and disconnected from your environment (derealization). While feelings like this may come and go for many people, in people with depersonalization-derealization disorder, they tend to last a long time (persist) or go away and come back (recur).
En cas de «bad trip», les personnes en bonne santé mentale réussiront plus facilement à relativiser l'expérience qu'elles sont en train de vivre, voire à s'y adonner. «Il faut accepter son ...
Derealization symptoms involve. Feeling detached from the surroundings (people, objects, or everything), which seem unreal. People may feel as if they are in a dream or a fog, or as if a glass wall or veil separates them from their surroundings. The world seems lifeless, colorless, or artificial. The world may appear distorted to them.
Managing DPDR. Depersonalization is a dissociative disorder that affects a person's perception of themselves and their surroundings. It is characterized by recurring episodes of depersonalization, derealization, or both. Depersonalization involves feeling detached from oneself, as if observing one's thoughts, emotions, and actions from a ...
Témoignages de consommateurs . Déréalisation après un bad trip. Par Bpt120 Posté le 30/04/2024 à 18:28 . Bonjour à toutes et à tous, je pense que la plupart des gens qui vont lire ce témoignage, ce sont des gens qui sont angoissés à la suite d'un bad trip, notamment par les effets provoquées par la déréalisation !
Je pense que c'était un gros Bad trip à cause du fait que j'étais très angoissé avant la soirée et avant d'en prendre y'a pas d'autre explication. Ensuite apres cette soirée, je suis rentrée chez moi au bout de quelques jours , les effets était encore là et ont persévérés et j'ai fais une crise d'angoisse et de spasmophilie qui a ...
Bonsoir depuis 5 mois je souffre de dépersonnalisation déréalisation, suite a un bad trip au shit , l'impression d'être absent , l'impression mon corps m'appartient pas , se sentir dans un rêve et des fois des absences et tout me parait iréel même quand je sort dehors , j'aimerais savoir qui a deja eu ça?
feeling as though you're no longer in your own body and are instead just a witness of the motions your body is going through. a loss of memory. a loss of sensation and feelings. emotional ...
Derealization or derealisation (sometimes abbreviated as DR) is medically recognized as the experience of feeling detached from, and as if one is an outside observer of, one's surroundings.[1][2] This effect is characterized by the individual feeling as if they are in a fog, dream, bubble, or something watched through a screen,[3] like a film or video game.[4] These feelings instill the person ...
Thank you so much for the response and sharing your experience mate! Want to make a correction cause you mentioned time was passing really fast, exactly what I felt , it was like the time was passing super fast but I was stuck in a loop which felt like days or weeks, like it was repetitive in a very fast pace, like I was living the moment 10 times per second in a fast pace and was taking for ...