Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Global health
- BMJ Journals More You are viewing from: Google Indexer

You are here
Travel medicine.
- Subconjunctival Dirofilaria masquerading as nodular scleritis Saloni Sinha , Shilpa Tarini , Bhavik Panchal , Dilip K Mishra BMJ Case Reports CP May 2024, 17 (5) e259519; DOI: 10.1136/bcr-2023-259519
- The use of rotational thromboelastometry to guide management following Bitis nasicornis envenoming Charles Nye , David Griffith Lalloo , Timothy Hooper BMJ Case Reports CP Apr 2024, 17 (4) e258319; DOI: 10.1136/bcr-2023-258319
- Recurrent leishmaniasis infection isolated in the pleural fluid Hina Qiam , Emily Lowe , Adriel Heilong Fung , Prasanna Sankaran BMJ Case Reports CP Mar 2024, 17 (3) e256632; DOI: 10.1136/bcr-2023-256632
- Atypical gnathostomiasis-confirmed cutaneous larva migrans, Vietnam Cuong Minh Duong , Phuc Vinh Dinh Le , Oanh Kieu Nguyet Pham , Hong Quang Huynh BMJ Case Reports CP Jul 2021, 14 (7) e243276; DOI: 10.1136/bcr-2021-243276
- Morphology of COVID-19–affected cells in peripheral blood film Aminder Singh , Neena Sood , Vikram Narang , Abhishek Goyal BMJ Case Reports CP May 2020, 13 (5) e236117; DOI: 10.1136/bcr-2020-236117
- Clinically isolated descending thoracic aortitis in a healthy older woman: a diagnostic challenge Max Amos Hoffman , Adel Ekladious BMJ Case Reports CP Feb 2021, 14 (2) e238009; DOI: 10.1136/bcr-2020-238009
- Acute myasthenic syndrome following coral snake envenomation in the Caribbean: a harbinger for admission to the intensive care unit Narine Mack , Antonio Jose Reyes , Kanterpersad Ramcharan , Stanley Lawrence Giddings BMJ Case Reports CP Mar 2021, 14 (3) e241991; DOI: 10.1136/bcr-2021-241991
- Mediterranean spotted fever with multiorgan involvement Kimberly Davis , Ahmad Ahmado , Clare E Warrell , Louise O Downs , Jenna Furneaux , Karthiga Sithamparanathan BMJ Case Reports CP Dec 2022, 15 (12) e249426; DOI: 10.1136/bcr-2022-249426
- Anaphylaxis to simultaneous administration of inactivated tissue culture hepatitis A vaccine and purified chick embryo cell rabies vaccine after multiple doses Kohei Hasegawa , Goh Ohji , Kentaro Iwata BMJ Case Reports CP Jan 2021, 14 (1) e237894; DOI: 10.1136/bcr-2020-237894
- Bilateral ocular toxoplasmosis in a returning traveller: age and route of infection as potential risk factors Tim Seers , Jayavani Myneni , Nadia L Chaudhry , Marta Ugarte BMJ Case Reports CP Jan 2021, 14 (1) e237068; DOI: 10.1136/bcr-2020-237068
- Anaesthesia (209)
- Cardiovascular medicine (986)
- Complementary medicine (6)
- Dentistry and oral medicine (213)
- Dermatology (540)
- Clinical diagnostic tests (50)
- Radiology (diagnostics) (146)
- Surgical diagnostic tests (23)
- Diagnostics
- Drugs and medicines (1781)
- Ear, nose and throat/otolaryngology (458)
- Disaster response
- Poisoning (49)
- Resuscitation (57)
- Trauma (160)
- Emergency medicine (478)
- Adrenal disorders (118)
- Calcium and bone (97)
- Diabetes (127)
- Drugs: endocrine system (25)
- Lipid disorders (26)
- Metabolic disorders (89)
- Pituitary disorders (57)
- Thyroid disease (118)
- Endocrinology (655)
- Changing physician behavior
- Effectiveness of care
- Gastroenterology (915)
- Drugs: gastrointestinal system (44)
- Endoscopy (165)
- GI bleeding (99)
- Infection (gastroenterology) (107)
- Inflammatory bowel disease (72)
- Liver disease (186)
- Neurogastroenterology
- Oesophagus (55)
- Pancreas and biliary tract (100)
- Pancreatitis (61)
- Portal hypertension (16)
- Small intestine (76)
- Stomach and duodenum (85)
- General practice / family medicine (242)
- Clinical genetics
- Cytogenetics
- Genetic screening / counselling (92)
- Molecular genetics
- Genetics (291)
- Elder abuse
- End of life decisions (geriatric medicine) (2)
- Long term care (18)
- Psychogeriatrics
- Geriatric medicine (66)
- Haematology (incl blood transfusion) (533)
- HIV/AIDS (80)
- Immunology (including allergy) (57)
- Infectious diseases (1323)
- Adult intensive care (301)
- Mechanical ventilation (19)
- Neonatal intensive care (90)
- Paediatric intensive care (69)
- Intensive care (561)
- Brain stem / cerebellum (85)
- Cerebral palsy (6)
- Clinical neurophysiology (40)
- Coma and raised intracranial pressure (29)
- Cranial nerves (107)
- Dementia (7)
- Drugs: CNS (not psychiatric) (33)
- Epilepsy and seizures (116)
- Headache (including migraine) (9)
- Hydrocephalus (22)
- Infection (neurology) (166)
- Motor neurone disease (14)
- Movement disorders (other than Parkinsons) (63)
- Multiple sclerosis (19)
- Muscle disease (40)
- Neuroimaging (396)
- Neurological injury (71)
- Neuromuscular disease (77)
- Neurooncology (116)
- Neuroophthalmology (8)
- Pain (neurology) (47)
- Parkinson's disease (7)
- Peripheral nerve disease (84)
- Sleep disorders (neurology) (8)
- Spinal cord (105)
- Stroke (239)
- Trauma CNS / PNS (40)
- Variant Creutzfeld-Jakob Disease (2)
- Neurology (1613)
- Nursing (36)
- Childhood nutrition (5)
- Malnutrition (24)
- Obesity (nutrition) (17)
- Vitamins and supplements (46)
- Nutrition and metabolism (118)
- Obstetrics and gynaecology (592)
- Oncology (1482)
- Ophthalmology (768)
- Orthopaedics (374)
- Adolescent health
- Bilirubin disorders (9)
- Child abuse (6)
- Child and adolescent psychiatry (paedatrics) (9)
- Child health
- Childhood nutrition (paediatrics) (7)
- Congenital disorders (280)
- Developmental paediatrics (4)
- Failure to thrive (19)
- Infant health (32)
- Infant nutrition (including breastfeeding) (5)
- Materno-fetal medicine (72)
- Neonatal and paediatric intensive care (96)
- Neonatal health (93)
- Paediatrics (883)
- End of life decisions (palliative care) (14)
- Pain (palliative care) (8)
- Palliative care (37)
- Chemical pathology
- Cytopathology
- Histopathology
- Inflammation
- Microbiology
- Molecular biology
- Morbid anatomy / surgical pathology
- Neuropathology
- Pathology (572)
- Drug misuse (including addiction) (33)
- Medicines regulation
- Toxicology (56)
- Unwanted effects / adverse reactions (311)
- Pharmacology and therapeutics (477)
- Prison medicine (1)
- Adjustment disorders
- Alcohol-related disorders (4)
- Anxiety disorders (including OCD and PTSD) (18)
- Child and adolescent psychiatry (11)
- Delirium (17)
- Drugs misuse (including addiction) (27)
- Drugs: psychiatry (29)
- Eating disorders (7)
- Impulse control disorders (6)
- Memory disorders (psychiatry) (22)
- Mood disorders (including depression) (33)
- Personality disorders (2)
- Psychiatry of old age (8)
- Psychotherapy (14)
- Psychotic disorders (incl schizophrenia) (37)
- Sexual and gender disorders (2)
- Sleep disorders (2)
- Somatoform disorders (6)
- Suicide (psychiatry) (7)
- Psychiatry (221)
- Radiology (874)
- Continuing medical education
- Disability (17)
- Other rehabilitative therapies
- Physiotherapy (41)
- Rehabilitation medicine (84)
- Acute renal failure (107)
- Chronic renal failure (49)
- Dialysis (61)
- Fluid electrolyte and acid-base disturbances (78)
- Nephrotic syndrome (29)
- Proteinurea (29)
- Renal transplantation (48)
- Renal medicine (371)
- Respiratory medicine (616)
- Ankylosing spondylitis (2)
- Biological agents (37)
- Connective tissue disease (97)
- Degenerative joint disease (9)
- Drugs: musculoskeletal and joint diseases (26)
- Fibromyalgia (2)
- Musculoskeletal syndromes (71)
- Osteoarthritis (13)
- Osteoporosis (11)
- Rheumatoid arthritis (40)
- Sjogren's syndrome (3)
- Systemic lupus erythematosus (60)
- Vascularitis (161)
- Rheumatology (570)
- Sexual health (102)
- Sports and exercise medicine (123)
- Breast surgery (69)
- Cardiothoracic surgery (205)
- Gastrointestinal surgery (432)
- General surgery (457)
- Neurosurgery (204)
- Oral and maxillofacial surgery (142)
- Orthopaedic and trauma surgery (235)
- Otolaryngology / ENT (246)
- Plastic and reconstructive surgery (177)
- Surgical oncology (230)
- Transplantation (61)
- Urological surgery (183)
- Vascular surgery (192)
- Surgery (2579)
- Urology (273)
- Communication
- Clinical trials (epidemiology)
- Epidemiologic studies
- Population trends
- Screening (epidemiology)
- Survey techniques
- Therapeutic trials
- Time-to-event methods
- Artificial and donated transplantation
- Assisted dying
- Clinical ethics
- Codes of professional ethics
- Competing interests (ethics)
- Confidentiality
- Drug issues
- End of life decisions (ethics)
- Ethics of abortion
- Ethics of reproduction
- Experiments in vivo
- Informed consent
- Research and publication ethics
- Sexuality / gender
- Ethics (16)
- Ethnic studies (2)
- Health economics (7)
- Information management
- Telemedicine
- Health policy
- Health service research
- Journalology
- Legal and forensic medicine
- Choosing / changing career
- Combining life and work
- Continuous professional development
- Flexible training
- Getting and changing jobs
- Getting and changing jobs (including job descriptions and contracts)
- Leaving medicine
- Medical careers
- Organise and prepare your CV
- Organise working abroad
- Pay, working conditions, and health
- Personal development
- Portfolio development
- Prepare for appraisal
- Prepare for interview
- Professional conduct and regulation
- Professional regulation and standards
- History taking and the physical examination
- Postgraduate
- Undergraduate
- Medical education (108)
- Doctors' morale and well being
- Medical error/ patient safety
- Quality improvement
- Medical management (208)
- Occupational and environmental medicine (141)
- Abuse (child, partner, elder)
- Air pollution
- Drug misuse
- Environmental issues
- Health education
- Health of indigenous peoples
- Health promotion
- Housing and health
- Human rights
- Obesity (public health) (5)
- Screening (public health)
- Sexual health (public health)
- Social conditions and disease
- Suicide (public health)
- Urban health
- Vaccination programs
- Violence (other)
- Violence against women
- Public health (68)
- Smoking and tobacco (16)
- Sociology (1)
- Comparative effectiveness research
- Qualitative research
- Quantitative research
- Statistics and research methods (1)
- 10-Minute Consultation
- Assessment of older adults
- BMJ clinical evidence summaries
- Care of older people
- Change page
- Clinical evidence
- Clinical governance in primary care
- Clinical guidelines (the theory)
- Clinical Update
- Competent novice
- Complexity science
- Conflict and health
- Coping with loss
- Data campaign
- Diagnosis in general practice
- Digital theme issue: Overdiagnosis
- Drug points
- E-cigarettes
- Easily missed
- Economics notes
- Ethical debates
- Evidence base of clinical diagnosis
- Evidence based case report
- Evidence based management of hypertension
- Evidence based paediatrics
- Extracts from BestTreatments
- For and against (controversies in management)
- Getting research findings into practice
- Guideline summaries
- Health needs assessment
- How does it work?
- If I ruled the NHS
- Improving the quality of health care
- Interactive case reports
- Investigation
- Lesson of the week
- Making a difference
- Managing demand
- Maternal, child, and adolescent health
- Measuring quality of life
- Methods in health services research
- Mid Staffordshire Inquiry
- Modernising the NHS
- Multimorbidity
- Narrative based medicine
- Non-communicable diseases
- Patient authored
- Patient journeys
- Pharmacology
- Practice pointer
- Pregnancy plus
- Primary care groups
- Qualitative research in health care
- Quality improvement report
- Rapid Recommendation
- Rational imaging
- Rational testing
- Regulating nursing homes
- Research pointers
- Safety alerts
- Science, medicine, and the future
- Scrap the Cap
- Seven day NHS
- Shared decision making
- Spotlight on climate change
- State of the Art
- Statistics notes
- Systematic reviews in health care
- Teaching rounds
- The BMJ Awards 2015
- The World Bank and world health
- Theories in health care and research
- Therapeutics
- Too much medicine
- UK general election 2015
- Uncertainties page
- Understanding controlled trials
- What the educators are saying
- What your patient is thinking
- What's new this month in BMJ Journals
- When I use a word
- Access to health care (10)
- Adverse drug reactions and complications (328)
- Corrections
- Determinants of health (2)
- Findings that shed new light on the possible pathogenesis of a disease or an adverse effect (257)
- Global health (72)
- Health in vulnerable communities (12)
- Images in... (2260)
- Learning from errors (76)
- Learning from unexpected outcome (positive or negative) (147)
- Medical student electives
- Medicine in the humanitarian sector
- Myth exploded
- New disease (44)
- Novel diagnostic procedure (55)
- Novel treatment (new drug/intervention; established drug/procedure in new situation) (396)
- Other full case
- Rare disease (2622)
- Reminder of important clinical lesson (714)
- Rural medicine
- Unexpected outcome (positive or negative) including adverse drug reactions (219)
- Unusual association of diseases/symptoms (708)
- Unusual presentation of more common disease/injury (795)
- Video reports
- COVID-19 (549)
- Editor's choice (66)
- Anaesthetics and ITU
- Anatomy quiz
- Case report
- Case Review
- Case scenario
- Drugs and therapeutics
- Emergency medicine
- Endocrinology
- Gastroenterology
- General practice
- Haematology
- Histopathology/cytology/pathology/autopsy
- Infectious diseases
- Law and ethics
- Learning disabled
- Obstetrics and gynaecology
- onExamination questions
- Ophthalmology
- Orthopaedics and trauma
- Paediatrics
- Picture quiz
- Renal medicine
- Respiratory
- Rheumatology
- Spot Diagnosis
- GUT Recent advances in clinical practice
- GUT Snapshot
- IP Cochrane corners
- JCP Education
- JECH Gallery
- JMG Online mutation reports
- Open access (797)
- Animal Models
- Biomarker Studies
- Childhood Lupus
- Clinical Trials and Drug Discovery
- Co-morbidities
- Cutaneous Lupus
- Epidemiology and Outcomes
- Immunology and Inflammation
- Lupus Nephritis
- Reproductive Health and APS
- Quality Improvement Reports
Case reports
Tropical Diseases, Travel Medicine and Vaccines welcomes well-described reports of cases that can be used for educational purposes or that describe unusual features of the disease, its treatment, transmission or control. When describing clinical cases, the authors are requested to provide written and signed consent to publish the information from the patients or their guardians; case reports may include clinical pictures.
Preparing your manuscript
The information below details the section headings that you should include in your manuscript and what information should be within each section.
Please note that your manuscript must include a 'Declarations' section including all of the subheadings (please see below for more information).
The title page should:
- "A versus B in the treatment of C: a randomized controlled trial", "X is a risk factor for Y: a case control study", "What is the impact of factor X on subject Y: A systematic review"
- or for non-clinical or non-research studies: a description of what the article reports
- if a collaboration group should be listed as an author, please list the Group name as an author. If you would like the names of the individual members of the Group to be searchable through their individual PubMed records, please include this information in the “Acknowledgements” section in accordance with the instructions below
- Large Language Models (LLMs), such as ChatGPT , do not currently satisfy our authorship criteria . Notably an attribution of authorship carries with it accountability for the work, which cannot be effectively applied to LLMs. Use of an LLM should be properly documented in the Methods section (and if a Methods section is not available, in a suitable alternative part) of the manuscript
- indicate the corresponding author
The Abstract should not exceed 350 words and should be structured with a background, main body of the abstract and short conclusion. Please minimize the use of abbreviations and do not cite references in the abstract.
Three to ten keywords representing the main content of the article.
The Background section should explain the background to the article, its aims, a summary of a search of the existing literature and the issue under discussion.
This should contain the body of the article, and may also be broken into subsections with short, informative headings.
Conclusions
This should state clearly the main conclusions and include an explanation of their relevance or importance to the field.
List of abbreviations
If abbreviations are used in the text they should be defined in the text at first use, and a list of abbreviations should be provided.
Declarations
All manuscripts must contain the following sections under the heading 'Declarations':
Ethics approval and consent to participate
Consent for publication, availability of data and materials, competing interests, authors' contributions, acknowledgements.
- Authors' information (optional)
Please see below for details on the information to be included in these sections.
If any of the sections are not relevant to your manuscript, please include the heading and write 'Not applicable' for that section.
Manuscripts reporting studies involving human participants, human data or human tissue must:
- include a statement on ethics approval and consent (even where the need for approval was waived)
- include the name of the ethics committee that approved the study and the committee’s reference number if appropriate
Studies involving animals must include a statement on ethics approval and for experimental studies involving client-owned animals, authors must also include a statement on informed consent from the client or owner.
See our editorial policies for more information.
If your manuscript does not report on or involve the use of any animal or human data or tissue, please state “Not applicable” in this section.
If your manuscript contains any individual person’s data in any form (including any individual details, images or videos), consent for publication must be obtained from that person, or in the case of children, their parent or legal guardian. All presentations of case reports must have consent for publication.
You can use your institutional consent form or our consent form if you prefer. You should not send the form to us on submission, but we may request to see a copy at any stage (including after publication).
See our editorial policies for more information on consent for publication.
If your manuscript does not contain data from any individual person, please state “Not applicable” in this section.
All manuscripts must include an ‘Availability of data and materials’ statement. Data availability statements should include information on where data supporting the results reported in the article can be found including, where applicable, hyperlinks to publicly archived datasets analysed or generated during the study. By data we mean the minimal dataset that would be necessary to interpret, replicate and build upon the findings reported in the article. We recognise it is not always possible to share research data publicly, for instance when individual privacy could be compromised, and in such instances data availability should still be stated in the manuscript along with any conditions for access.
Authors are also encouraged to preserve search strings on searchRxiv https://searchrxiv.org/ , an archive to support researchers to report, store and share their searches consistently and to enable them to review and re-use existing searches. searchRxiv enables researchers to obtain a digital object identifier (DOI) for their search, allowing it to be cited.
Data availability statements can take one of the following forms (or a combination of more than one if required for multiple datasets):
- The datasets generated and/or analysed during the current study are available in the [NAME] repository, [PERSISTENT WEB LINK TO DATASETS]
- The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
- All data generated or analysed during this study are included in this published article [and its supplementary information files].
- The datasets generated and/or analysed during the current study are not publicly available due [REASON WHY DATA ARE NOT PUBLIC] but are available from the corresponding author on reasonable request.
- Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
- The data that support the findings of this study are available from [third party name] but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of [third party name].
- Not applicable. If your manuscript does not contain any data, please state 'Not applicable' in this section.
More examples of template data availability statements, which include examples of openly available and restricted access datasets, are available here .
BioMed Central strongly encourages the citation of any publicly available data on which the conclusions of the paper rely in the manuscript. Data citations should include a persistent identifier (such as a DOI) and should ideally be included in the reference list. Citations of datasets, when they appear in the reference list, should include the minimum information recommended by DataCite and follow journal style. Dataset identifiers including DOIs should be expressed as full URLs. For example:
Hao Z, AghaKouchak A, Nakhjiri N, Farahmand A. Global integrated drought monitoring and prediction system (GIDMaPS) data sets. figshare. 2014. http://dx.doi.org/10.6084/m9.figshare.853801
With the corresponding text in the Availability of data and materials statement:
The datasets generated during and/or analysed during the current study are available in the [NAME] repository, [PERSISTENT WEB LINK TO DATASETS]. [Reference number]
If you wish to co-submit a data note describing your data to be published in BMC Research Notes , you can do so by visiting our submission portal . Data notes support open data and help authors to comply with funder policies on data sharing. Co-published data notes will be linked to the research article the data support ( example ).
All financial and non-financial competing interests must be declared in this section.
See our editorial policies for a full explanation of competing interests. If you are unsure whether you or any of your co-authors have a competing interest please contact the editorial office.
Please use the authors initials to refer to each authors' competing interests in this section.
If you do not have any competing interests, please state "The authors declare that they have no competing interests" in this section.
All sources of funding for the research reported should be declared. If the funder has a specific role in the conceptualization, design, data collection, analysis, decision to publish, or preparation of the manuscript, this should be declared.
The individual contributions of authors to the manuscript should be specified in this section. Guidance and criteria for authorship can be found in our editorial policies .
Please use initials to refer to each author's contribution in this section, for example: "FC analyzed and interpreted the patient data regarding the hematological disease and the transplant. RH performed the histological examination of the kidney, and was a major contributor in writing the manuscript. All authors read and approved the final manuscript."
Please acknowledge anyone who contributed towards the article who does not meet the criteria for authorship including anyone who provided professional writing services or materials.
Authors should obtain permission to acknowledge from all those mentioned in the Acknowledgements section.
See our editorial policies for a full explanation of acknowledgements and authorship criteria.
If you do not have anyone to acknowledge, please write "Not applicable" in this section.
Group authorship (for manuscripts involving a collaboration group): if you would like the names of the individual members of a collaboration Group to be searchable through their individual PubMed records, please ensure that the title of the collaboration Group is included on the title page and in the submission system and also include collaborating author names as the last paragraph of the “Acknowledgements” section. Please add authors in the format First Name, Middle initial(s) (optional), Last Name. You can add institution or country information for each author if you wish, but this should be consistent across all authors.
Please note that individual names may not be present in the PubMed record at the time a published article is initially included in PubMed as it takes PubMed additional time to code this information.
Authors' information
This section is optional.
You may choose to use this section to include any relevant information about the author(s) that may aid the reader's interpretation of the article, and understand the standpoint of the author(s). This may include details about the authors' qualifications, current positions they hold at institutions or societies, or any other relevant background information. Please refer to authors using their initials. Note this section should not be used to describe any competing interests.
Footnotes can be used to give additional information, which may include the citation of a reference included in the reference list. They should not consist solely of a reference citation, and they should never include the bibliographic details of a reference. They should also not contain any figures or tables.
Footnotes to the text are numbered consecutively; those to tables should be indicated by superscript lower-case letters (or asterisks for significance values and other statistical data). Footnotes to the title or the authors of the article are not given reference symbols.
Always use footnotes instead of endnotes.
Examples of the Vancouver reference style are shown below.
See our editorial policies for author guidance on good citation practice
Web links and URLs: All web links and URLs, including links to the authors' own websites, should be given a reference number and included in the reference list rather than within the text of the manuscript. They should be provided in full, including both the title of the site and the URL, as well as the date the site was accessed, in the following format: The Mouse Tumor Biology Database. http://tumor.informatics.jax.org/mtbwi/index.do . Accessed 20 May 2013. If an author or group of authors can clearly be associated with a web link, such as for weblogs, then they should be included in the reference.
Example reference style:
Article within a journal
Smith JJ. The world of science. Am J Sci. 1999;36:234-5.
Article within a journal (no page numbers)
Rohrmann S, Overvad K, Bueno-de-Mesquita HB, Jakobsen MU, Egeberg R, Tjønneland A, et al. Meat consumption and mortality - results from the European Prospective Investigation into Cancer and Nutrition. BMC Medicine. 2013;11:63.
Article within a journal by DOI
Slifka MK, Whitton JL. Clinical implications of dysregulated cytokine production. Dig J Mol Med. 2000; doi:10.1007/s801090000086.
Article within a journal supplement
Frumin AM, Nussbaum J, Esposito M. Functional asplenia: demonstration of splenic activity by bone marrow scan. Blood 1979;59 Suppl 1:26-32.
Book chapter, or an article within a book
Wyllie AH, Kerr JFR, Currie AR. Cell death: the significance of apoptosis. In: Bourne GH, Danielli JF, Jeon KW, editors. International review of cytology. London: Academic; 1980. p. 251-306.
OnlineFirst chapter in a series (without a volume designation but with a DOI)
Saito Y, Hyuga H. Rate equation approaches to amplification of enantiomeric excess and chiral symmetry breaking. Top Curr Chem. 2007. doi:10.1007/128_2006_108.
Complete book, authored
Blenkinsopp A, Paxton P. Symptoms in the pharmacy: a guide to the management of common illness. 3rd ed. Oxford: Blackwell Science; 1998.
Online document
Doe J. Title of subordinate document. In: The dictionary of substances and their effects. Royal Society of Chemistry. 1999. http://www.rsc.org/dose/title of subordinate document. Accessed 15 Jan 1999.
Online database
Healthwise Knowledgebase. US Pharmacopeia, Rockville. 1998. http://www.healthwise.org. Accessed 21 Sept 1998.
Supplementary material/private homepage
Doe J. Title of supplementary material. 2000. http://www.privatehomepage.com. Accessed 22 Feb 2000.
University site
Doe, J: Title of preprint. http://www.uni-heidelberg.de/mydata.html (1999). Accessed 25 Dec 1999.
Doe, J: Trivial HTTP, RFC2169. ftp://ftp.isi.edu/in-notes/rfc2169.txt (1999). Accessed 12 Nov 1999.
Organization site
ISSN International Centre: The ISSN register. http://www.issn.org (2006). Accessed 20 Feb 2007.
Dataset with persistent identifier
Zheng L-Y, Guo X-S, He B, Sun L-J, Peng Y, Dong S-S, et al. Genome data from sweet and grain sorghum (Sorghum bicolor). GigaScience Database. 2011. http://dx.doi.org/10.5524/100012 .
Figures, tables and additional files
See General formatting guidelines for information on how to format figures, tables and additional files.
Submit manuscript
- Editorial Board
- Manuscript editing services
- Instructions for Editors
- SNAPP Editorial Login
- Sign up for article alerts and news from this journal
Annual Journal Metrics
2022 Citation Impact 3.1 - 2-year Impact Factor 1.059 - SNIP (Source Normalized Impact per Paper) 1.128 - SJR (SCImago Journal Rank)
2023 Speed 10 days submission to first editorial decision for all manuscripts (Median) 115 days submission to accept (Median)
2023 Usage 312,456 downloads 262 Altmetric mentions
- More about our metrics
Tropical Diseases, Travel Medicine and Vaccines
ISSN: 2055-0936
- Submission enquiries: [email protected]
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
Travel medicine
- Related content
- Peer review
- Jane N Zuckerman , senior lecturer. ( j.zuckerman{at}rfc.ucl.ac.uk )
- Academic Centre for Travel Medicine and Vaccines, Royal Free and University College Medical School, London NW3 2PF
- Accepted 23 May 2002
Travel medicine is an exciting interdisciplinary specialty that has developed rapidly in response to the needs of the travelling population worldwide. International arrivals worldwide by any form of transport were around 664 million in 2000 (fig 1 ), and the World Tourist Organisation has predicted an 80% increase in travel to long haul destinations between 1995 and 2010. 1 2 Specialists in travel medicine consider diverse aspects of travel related health, including fitness to travel and the health risks of travelling in itself, as well as the implications of exposure to a variety of infectious diseases. This review highlights current topical issues in this evolving specialty.
Sources and search criteria
This article is based on information from several sources, including a review of the literature obtained from the PubMed database, clinical experience, and textbooks on the subject of travel medicine.
The development of travel medicine as a distinct discipline
The development of travel medicine as a discipline is a recent advance in itself. 4 This has been recognised in the United Kingdom by the Department of Health in its new strategy for combating infectious disease, which confirms the need for specialists in travel medicine. 5
An important organisational development has been the establishment of dedicated specialist travel health clinics in teaching hospitals and primary care (in addition to clinics operated by independent commercial groups). These provide individual pretravel risk assessments (box 1 ) and should improve services for patients, many of whom seldom seek health advice before travel. 6 The importance of providing services for patients is increasingly being recognised in relation to an increased incidence of travel related disease (box 2 )and importation of infection (fig 2 ). 7
Recent developments
Travel medicine is developing as a new specialty providing specialist travel services to meet the health needs of vastly increasing numbers of travellers
A pretravel risk assessment allows travel health related risk factors to be identified
The public health implications of the growing number of refugees and migrants from less developed to developed countries need to be fully assessed, and appropriate services need to be provided
Vector borne diseases, in particular malaria, remain an important health risk
The appropriate use of malaria standby treatment may become an option for experienced travellers
New combination vaccines that can be administered by an accelerated schedule are a welcome advance in combating infectious disease
Assessment of fitness to fly and awareness of the possible physiological and psychological impacts of air travel should be considered
The International Society of Travel Medicine and the British Travel Health Association (UK) provide information and support to health professionals who are offering travel advisory services to patients. Information from the International Society of Travel Medicine is available on the internet and includes a comprehensive and international listing of travel medicine specialists and travel health clinics. Guidelines and information relating to the discipline of travel medicine are also available from the World Health Organization, the Department of Health, and the Centers for Disease Control and Prevention, as well as from the recently formed European Travel Health Advisory Board (see additional educational resources). 8
Training in the discipline is available both nationally and internationally through certification, diploma, or masters degrees (see bmj.com). A new initiative from the International Society of Travel Medicine includes a certificate in travel medicine that encompasses a body of knowledge in travel medicine developed by an international group of travel medicine physicians.
Refugees and migrants
International migration, usually from poor countries to rich countries, is a worldwide phenomenon. Estimates put the number of migrants worldwide in 1990 in excess of 120 million, with an annual growth rate of 1.9%. 9 Net international migration contributed to 45% of the population growth in the developed world and almost 88% of the population growth in Europe in 1990-5. The number of refugees worldwide, including asylum seekers, in 2001 totalled 19.8 million. 10 Trafficking in migrants has become a lucrative illegal market.
The migration process has important health implications. Migrants often have a higher rate than other travellers of conditions such as tuberculosis, hepatitis B and C, schistosomiasis, malaria, and sexually transmitted infections (including syphilis and HIV). They also have a higher rate of non-infectious conditions such as diabetes, cardiovascular disease, malignant diseases, asthma, respiratory diseases linked to smoking, occupational diseases, and injuries, as well as psychological disorders. 11 Stress related health problems are exacerbated by changes in lifestyle, food habits, culture, and religious life. As the number of refugees and migrants grows, medical providers and travel medicine physicians need to understand and respond to the wide range of health problems they have.
Percentage increase in international arrivals between 1993 and 1997 3
- Download figure
- Open in new tab
- Download powerpoint
Pretravel risk assessment
• Detailed itinerary:
Countries and regions
Urban, rural, or jungle
Purpose of travel
Mode of travel
Type of accommodation
Duration of stay and travel
Special activities
Special needs
Special high risks
Previous travel
Available medical facilities
Detailed medical history
Concurrent medications
Personal immunisation history
Appropriate immunisations and malaria prophylaxis
Key travel related health problems
Travellers' diarrhoea
Respiratory tract infections
Hepatitis A and B
Skin infections
Sexually transmitted infections
Cases of falciparum malaria in the United Kingdom, 1990-9 5
Vector borne disease
Up to 8 in 1000 travellers in developed countries become infected with malaria, resulting in more than 10 000 cases of malaria being imported into Europe each year (fig 2 ). 12 13 Other vector borne diseases, such as dengue and yellow fever, are also increasingly important. 14
Since December 2001, following the report of six deaths possibly associated with the administration of yellow fever vaccine in elderly travellers, health professionals have expressed concern about the use of yellow fever vaccine. 15 – 17 Millions of doses of vaccine have been administered over many years, however, with a minimum risk of morbidity or mortality, and experts agree that the benefits of yellow fever vaccination outweigh the risks.
Malaria remains the single most important disease hazard facing travellers. Adherence to antimalarial chemoprophylaxis, in addition to adopting measures to avoid being bitten, is essential. Chloroquine resistant falciparum malaria is an increasing problem in Central and South America, South East Asia, Oceania, and sub-Saharan Africa. 18 Recommended prophylaxis for chloroquine resistant areas, to be discussed with the individual traveller, include mefloquine, doxycycline, and atovaquone plus proguanil (Malarone). Chloroquine continues to be recommended as prophylaxis for malaria in areas where there is no chloroquine resistance.
It is advisable for people taking mefloquine for the first time to start three weeks before departure so that if they experience side effects such as anxiety or nightmares alternative prophylactic drugs can be considered. Alternatives include Malarone one tablet daily, doxycycline 100 mg daily, dapsone plus pyrimethamine (Maloprim) one tablet weekly or chloroquine and proguanil. Malarone consists of 250 mg atovaquone and 100 mg proguanil and is of particular value for people travelling to chloroquine resistant areas. 19 Prophylaxis should be started one day before entry into an endemic area and continued for seven days after leaving it.
Guidance on antimalarial chemoprophylaxis has recently been issued by the Advisory Committee on Malaria Prevention for UK Travellers (box 3 ). Malarone, doxycycline, and mefloquine are recommended in chloroquine resistant areas. Mefloquine is recommended for travel of longer than two weeks' duration to West, Central, and East Africa and specific areas of South East Asia. Chloroquine and proguanil are recommended for travel to other areas. 20
Malaria chemoprophylaxis by continent (depending on season and area visited
The advisory committee on malaria prevention for uk travellers recommends.
North Africa and Middle East—chloroquine alone or chloroquine plus proguanil
Sub-Saharan Africa—mefloquine, doxycycline, or atovaquone plus proguanil
South Asia—chloroquine plus proguanil
South East Asia—mefloquine, doxycycline, or atovaquone plus proguanil (Indonesia and forests of Malaysia and Sarawak—chloroquine plus proguanil)
Oceania—mefloquine, doxycycline, or atovaquone plus proguanil
Latin America—mefloquine, doxycycline, or atovaquone plus proguanil
Caribbean—chloroquine plus proguanil or chloroquine alone
Malaria chemoprophylaxis regimens
Chloroquine—two tablets taken weekly starting a week before travel to endemic area and continuing for four weeks after leaving malarious area
Proguanil—one tablet daily starting a week before travel to endemic area and continuing for four weeks after leaving malarious area
Doxycycline—one tablet daily starting one day before travel to endemic area and continuing for four weeks after leaving malarious area
Atovaquone plus proguanil (Malarone)—one tablet daily starting one day before travel to endemic area and continuing for seven days after leaving malarious area
Mefloquine—one tablet weekly starting trial dose three weeks before departure if appropriate and continuing for four weeks after leaving malarious area
Standby treatment in defined circumstances may become of increasing value to travellers. Standby treatment consists of a course of antimalarial drugs that travellers to malaria endemic areas can use for self treatment if they are unable to gain access to medical advice within 24 hours of becoming unwell. The treatment kits are supplied with written instructions, and travellers must seek medical advice as soon as possible. Recently licensed agents indicated for use as standby treatment include Malarone and Riamet, which is a new fixed dose antimalarial drug containing 20 mg artemether and 120 mg lumefantrine. 21
Prevention of infectious disea
The prevention of infectious disease in travellers continues to receive substantial consideration, as an appreciable number of such diseases are now considered to be “vaccine preventable.” 22 Vaccines usually recommended for general travel include tetanus, poliomyelitis, and hepatitis A. As destinations become more diverse, with people increasingly travelling outside Europe, additions to this list include typhoid, hepatitis B, diphtheria, and rabies (box 4 ). Mandatory vaccines, for which certification is often necessary, include yellow fever and meningoccocal meningitis, as appropriate to the destination. Travellers at high risk, such as those with chronic medical problems, would benefit from vaccination against diseases such as influenza, whose seasonal prevalence differs in temperate and tropical climates, as well as pneumococcal vaccine and hepatitis B vaccine.
Vaccines for travellers
Poliomyelitis
Childhood immunisations (in date
Recommended for travel outside northwest Europe, North America, Australia, and New Zealand:
Diphtheria (travellers in close contact with the indigenous population)
Hepatitis A
Hepatitis B
Special risk
Influenza (travellers with underlying medical problems)
Japanese encephalitis (travel for more than four weeks in rural area
Meningoccocal meningitis (travellers in close contact with the indigenous population)
Pneumococcus (travellers with underlying medical problems)
Rabies (rural travel and travel more than 24 hours away from medical help)
Tick borne encephalitis (travel to forested areas of Eastern Europe)
Certificate required
Meningoccocal meningitis (travel to Saudi Arabia for purposes of a pilgrimage)
Yellow fever (travel to parts of sub-Saharan Africa and parts of Central and South America)
Rapid schedules of vaccination
Hepatitis B (Engerix B)—days 0, 7, and 21; booster at 12 months
Hepatitis A and B (Twinrix)—days 0, 7, and 21; booster at 12 months
Combination vaccines
Hepatitis A and B (Twinrix)
Hepatitis A and typhoid (Hepatyrix; ViATIM)
Diphtheria and tetanus (DT, d, Td)
Additional educational resources
Bradley DJ, Bannister B. Guidelines for malaria prevention in travellers from the United Kingdom for 2001. Commun Dis Public Health 2001;4:84-101
Department of Health. Health information for overseas travel 2001 . London: Department of Health, 2001
World Health Organization. International travel and health 2002 . Geneva: WHO, 2002
Zuckerman JN, ed. The principles and practice of travel medicine . Chichester: John Wiley & Sons, 2001
Foreign and Commonwealth Office—general travel health and safety advice www.fco.gov.uk/travel/
World Health Organization, International Travel and Health—vaccination requirements and health www.who.int/ith/ and disease outbreak reports www.who.int/disease-outbreak-news/
Centers for Disease Control and Prevention—US health information for international travel www.cdc.gov/travel
International Society of Travel Medicine—information resource for both travel medicine practitioners and travellers http://www.istm.org/
NHS resource for healthcare professionals advising travellers about how to avoid illness when travelling abroad— http://www.travax.scot.nhs.uk/
Fit for Travel—public access website provided by the NHS, which gives travel health information for people travelling abroad from the UK http://www.fitfortravel.scot.nhs.uk/
Medical care before, during, and after air travel— http://www.britishairways.com/
BMJ archive
Mortimer P. Yellow fever vaccine. BMJ 2002;324:439
Goodwin T. In-flight medical emergencies: an overview. BMJ 2000;321:1338-41
Webster G, Barnes E, Dusheiko G, Franklin I. Protecting travellers from hepatitis A. BMJ 2001;322:1194-5
Hepatitis B vaccine should also be considered for a wider range of travellers, including those who may travel to areas endemic for hepatitis B, may be exposed by virtue of their sexual practices, or may be exposed to unscreened or inadequately screened blood or blood products or inadequately sterilised medical and surgical equipment. 23
People are increasingly travelling at short notice, and the ability to provide good levels of protection within a period of four weeks is an important development. Newer combination vaccines, such as hepatitis A plus typhoid and hepatitis A plus B, provide dual protection by a single injection (box 5). This increases uptake and convenience (particularly for people with a fear of needles) and by using only one site makes another injection site available when time is short and multiple immunisations need to be considered. Rapid schedules of vaccination include monovalent hepatitis B vaccine, which can be administered according to three different schedules, and combined hepatitis A and B vaccine, which can be administered as a primary course within three weeks. 24
Other recent developments include the introduction of a quadrivalent meningoccocal meningitis vaccine to protect against the W135 strain, which has been associated with several outbreaks of disease in Saudi Arabia as well as in parts of sub-Saharan Africa. 25 Other new vaccines licensed in the United States include a vaccine against varicella. 26
The increase in air travel has led to increases in the incidence of travel related disease and the importation of infection
Credit: PETER MACDIARMID/REX
As part of the expanded programme on immunisation, under the auspices of the WHO, worldwide eradication of poliomyelitis remains a goal. The report of outbreaks of vaccine associated poliomyelitis in countries where wild poliovirus has been eliminated is, however, of concern. 27 In view of this, it would seem prudent for those travellers at particular risk—for example, those in contact with the local population, such as aid workers—to maintain levels of protection against poliomyelitis.
Aviation medicine
Health practitioners need to be aware of the health effects of reduced atmospheric pressure, transmeridian travel (causing jetlag), and motion sickness and to consider passengers' fitness to travel by air. Guidelines for medical clearance, in-flight medical emergencies, and aircraft emergency medical equipment have been reviewed. 28
The risk of transmission of respiratory diseases in association with air travel should also be considered. No case of active tuberculosis as a result of exposure during travel by air has yet been identified, but transmission of Mycobacterium tuberculosis may occur during flights of more than eight hours, as the risk of infection is related to the proximity and duration of exposure to the source patient. 29
Considerable attention has been given to travel related deep vein thrombosis. 30 31 The estimated risk of developing deep vein thrombosis after a long distance flight is between 0.1 and 0.4 per thousand of the general population. 32 Methods of preventing deep vein thrombosis, including identification of travellers with predisposing risk factors, 32 are important. All passengers, regardless of their risk, should move around in their seats and in the aircraft cabin as much as possible during the journey. Drinks containing alcohol or caffeine should be avoided before and during the flight, and water or soft drinks should be taken to reduce the effects of dehydration. Exercising the calf muscles every half hour while seated by spending a few minutes flexing and rotating the ankles is also recommended to reduce the effects of stasis.
The prophylactic use of aspirin, and in some cases subcutaneous heparin, to prevent deep vein thrombosis is under discussion. Under the auspices of the WHO, studies are planned to evaluate the risk of deep vein thrombosis associated with travelling by air. The aims of the research programme are to determine the frequency and cause of travellers' thrombosis through epidemiological studies, to identify who is at greatest risk through pathophysiological studies, and to undertake clinical studies that will focus on the effectiveness of possible preventive strategies. 33
Competing interests JNZ has been reimbursed by several manufacturers of vaccines and antimalarial prophylaxis for attending conferences and running educational programmes and has received unrestricted educational grants. JNZ is also a consultant in travel medicine to British Airways travel clinics
Details of courses in travel medicine appear on bmj.com
- World Tourist Organisation
- Lederberg J
- Department of Health
- Stringer C ,
- Chiodini J ,
- Zuckerman JN
- ↵ Travellers Omnibus Survey. London : Ipsos RSL , 1999 .
- World Health Organization
- United Nations High Commissioners for Refugees.
- Carballo M ,
- Divino JJ ,
- Steffen R ,
- Heymann D ,
- Chang G-JJ ,
- Holmes DA ,
- Penney DJ ,
- Carter IW ,
- Roberts JA ,
- Rawlinson WD
- World Health Organization 2000(b)
- Bradley DJ ,
- Bannister B
- Schlagenhauf P ,
- Zuckerman JN ,
- Dietrich M ,
- Nothdurft HD ,
- Knotloch J ,
- Vollmar J ,
- ↵ Meningococcal disease serogroup W135 WER 2001 ; 19 : 141 – 142 .
- Varicella, measles, mumps, rubella vaccine
- ↵ Progress toward global eradication of poliomyelitis, 2001. MMWR Morb Mortal Wkly Rep 2002 ; 51 : 253 – 256 . OpenUrl PubMed
- Geroulakos G
- Machin SJ ,
- Bailey-King S ,
- Mackie IJ ,
- McDonald S ,
- House of Lords
- ↵ WHO study of venous thrombosis and air travel. Weekly Epidemiological Record 2002 ; 77 : 197 – 199 . OpenUrl PubMed
Advertisement
Travel in the Time of COVID: A Review of International Travel Health in a Global Pandemic
- Tropical, Travel and Emerging Infections (LH Chen and F Norman, Section Editors)
- Open access
- Published: 04 August 2022
- Volume 24 , pages 129–145, ( 2022 )
Cite this article
You have full access to this open access article

- Gerard T. Flaherty ORCID: orcid.org/0000-0002-5987-1658 1 , 2 ,
- Davidson H. Hamer 3 , 4 , 5 , 6 &
- Lin H. Chen 7 , 8
4448 Accesses
17 Citations
1 Altmetric
Explore all metrics
Purpose of Review
This review critically considers the impact of the COVID-19 pandemic on global travel and the practice of travel medicine, highlights key innovations that have facilitated the resumption of travel, and anticipates how travel medicine providers should prepare for the future of international travel.
Recent Findings
Since asymptomatic transmission of the virus was first recognized in March 2020, extensive efforts have been made to characterize the pattern and dynamics of SARS-CoV-2 transmission aboard commercial aircraft, cruise ships, rail and bus transport, and in mass gatherings and quarantine facilities. Despite the negative impact of further waves of COVID-19 driven by the more transmissible Omicron variant, rapid increases of international tourist arrivals are occurring and modeling anticipates further growth. Mitigation of spread requires an integrated approach that combines masking, physical distancing, improving ventilation, testing, and quarantine. Vaccines and therapeutics have played a significant role in reopening society and accelerating the resumption of travel and further therapeutic innovation is likely.
COVID-19 is likely to persist as an endemic infection, and surveillance will assume an even more important role. The pandemic has provided an impetus to advance technology for telemedicine, to adopt mobile devices and GPS in contact tracing, and to apply digital applications in research. The future of travel medicine should continue to harness these novel platforms in the clinical, research, and educational arenas.
Similar content being viewed by others
International travel is not a significant risk of exposure for patients at a Midwestern United States travel clinic

COVID-19 in comparison with other emerging viral diseases: risk of geographic spread via travel
Modelling the effect of travel-related policies on disease control in a meta-population structure
Avoid common mistakes on your manuscript.
Introduction
On March 11, 2020, the World Health Organization (WHO) declared COVID-19 a pandemic. As the world faced this unparalleled global health, social, and economic emergency, the travel and tourism industries were among the most affected sectors with airplanes on the ground, hotels closed, and travel restrictions put in place around the world. International tourist arrivals fell by 74% from 2019 to 2020, with an estimated 11-fold loss in international tourism receipts compared to the 2009 global economic crisis [ 1 ]. Past travel recovery periods from the 9/11 attack in the USA (2001), SARS (2003), and the global economic crisis (2009) depressed global travel levels for periods of between 11 and 19 months. Regional variations in the recovery intervals were significant in the Americas following the 9/11 attack with protracted recovery periods of up to 42 months observed. Despite the rapid gains in scientific discovery about SARS-CoV-2, its ability to mutate and become more transmissible have complicated the world’s recovery from the pandemic.
During this historic period, travel clinics closed and staff were furloughed or reassigned to COVID-19 response. Many recommendations were developed to provide guidance on travel during the pandemic [ 2 , 3 , 4 ••, 5 , 6 , 7 •, 8 ••, 9 ]. Thoughtful reflections discussed the impact of the pandemic on travel and travel medicine, and many adaptations were made in response [ 4 ••, 10 , 11 , 12 , 13 •]. Given the resumption of travel, travel medicine providers and the travelling public should consider how this pandemic will influence the future of travel medicine.
This narrative review aims to describe some major aspects of the pandemic that affected travel, the optimization of elements of pre-travel advice that will be useful for the future, highlight game changers that helped to restart travel, key data and digital services that have altered travel medicine practice, and some travel health risks beyond COVID-19 that persist.
Literature Search Strategy
Between March 5 and May 5, 2022, the authors searched MEDLINE, Embase, and Google Scholar databases using search terms relevant to COVID-19 (e.g., “covid,” “SARS-CoV-2,” “pandemic,” “transmission,” “vaccine”) combined with search terms relevant to international travel (e.g., “travel,” “international,” “borders,” “air travel”). The search was restricted to publications in English. Evidence from recent systematic reviews, meta-analyses, and clinical trials was prioritized. The bibliographies of retrieved articles were manually searched for additional sources not yielded by the primary search. The gray literature was consulted for relevant online reports from reputable international agencies involved in travel and tourism.
Impact of COVID-19 Pandemic on International Travel
Following the turbulence experienced in 2020 and 2021, the travel and tourism industry has entered a steady though sluggish recovery phase. Despite a 4% increase in international tourist arrivals in 2021 (415 million), compared to 2020 as a whole (400 million), arrivals during the second year of the pandemic were still 72% lower than the immediate pre-pandemic year of 2019 [ 14 ]. The regions with the most robust recovery of travel volumes in 2021 were the Caribbean, Mediterranean Europe, and Central America, with further declines in arrivals observed in the Middle East and Asia–Pacific. Although there was a moderate rebound in the second half of 2021, owing to increased traveler confidence resulting from successful vaccination programs in developed countries, clearer travel protocols, and some loosening of travel restrictions [ 15 ], the pace of travel recovery remains cautious and uneven, with significant variation in mobility restrictions and vaccine uptake.
Tourism direct gross domestic product plummeted from a peak of US$ 3.5 trillion in 2019 to US$ 1.6 trillion in 2020, when many countries suspended all non-essential inbound and outbound international travel, before recovering to US$ 1.9 trillion in 2021 [ 14 ]. An increase in tourism expenditure reflected in average receipts per arrival in 2021 has been attributed to the impact of lockdown-related savings in a segment of the population, longer durations of stay, and higher transport and accommodation prices [ 14 ]. International arrivals are predicted to return to 2019 levels by 2024 at the earliest [ 14 ].
A greater public awareness of the contribution of air travel to global greenhouse gas emissions, coupled with a vocal flight shaming movement [ 14 , 16 ], inflationary pressures, and recent conflict-induced surges in fossil fuel energy prices, have further slowed the recovery in international travel. The shutdown of Russian and Ukrainian airspace since February 2022 has affected travel within Europe and imposed increased costs on long-haul travel between Europe and the Middle East and Asia–Pacific regions owing to flight detours. Lifting of travel restrictions has been a leading factor in the recovery of international travel. Despite the negative impact of further waves of COVID-19 driven by the more transmissible Omicron variant in the first quarter of 2022, modeling by the United Nations World Tourism Organization (UNWTO) anticipates gradual growth in international tourist arrivals of up to 78% in 2022, compared to 2021 [ 14 ].
Novel consumer travel trends have been recognized, which include a preference for short-haul travel and domestic staycations, greater consciousness around sustainable approaches to travel, renewed interest in rural and nature-based tourism, and a tendency towards longer, but fewer and more expensive trips [ 17 ]. Anecdotally, a pattern of “revenge tourism” has emerged in recent months, whereby travelers have combined several bucket-list destinations into a single, more complex itinerary. The marked reduction in discretionary leisure travel throughout 2020 and much of 2021 also drew attention to an emerging phenomenon of social media influencer tourism, which deserves further research [ 18 ].
Relevant Effects of COVID-19 Pandemic and Mitigation Strategies
The extreme measures adopted by national governments to limit the importation and domestic transmission of SARS-CoV-2 have divided public opinion, with some considering them too restrictive, non-evidence-based, or inconsistently applied across countries. The counterargument points to the significant additional mortality which would undoubtedly have occurred in the absence of societal lockdowns, social distancing, face mask mandates, and international travel bans. With the benefit of hindsight, it is prudent to reflect on some of the adverse collateral effects of stringent pandemic mitigation strategies, if important lessons are to be learned for future pandemics.
Harmful consequences have been attributed to national border closures, international travel restrictions, and mandatory traveler quarantine policies in relation to quality of life, well-being, and mental health [ 19 •]. Concerns have been identified regarding equity, equality, and the global distribution of burdens arising from international travel measures and the impact of border closures on family reunification when relatives were trapped in a foreign country. Specific cohorts were disproportionately affected, such as students studying abroad [ 20 ], refugees [ 21 ], and cruise ship employees [ 22 ]. Mandatory hotel quarantine was generally perceived as detrimental to the mental health of travelers, although there were perceived economic benefits to host countries at a time of diminished hotel activity. Environmental benefits accrued from improved air quality resulting from reduced vehicular traffic during lockdowns [ 23 ]. Cities that usually experience mass tourism, such as Venice in Italy, reported improvements in the quality of life of their residents [ 24 ].
This pandemic has raised awareness of the mode of transmission of respiratory viruses and the beneficial effects of mask-wearing in crowded indoor settings such as aboard commercial aircraft. There has also been a revolution in hand hygiene practices and widespread adoption of rapid antigen self-testing to guide social behavior domestically and in travel settings [ 25 , 26 ]. The long-term benefits of travel-related infection prevention remain to be fully appreciated, but there are indications that pandemic control measures were responsible for a decline in the incidence of influenza and other respiratory viruses [ 27 , 28 ], gastroenteritis [ 29 ], sexually transmitted infections [ 30 ], and dengue [ 31 ] in certain countries. Other collateral effects of the pandemic have included delays in the diagnosis of severe malaria [ 32 ], interruptions to national childhood immunization schedules [ 33 ], changing patterns of sex tourism [ 34 ], and flexible work practices, which have given rise to novel entities in travel medicine such as digital nomads and so-called workcations.
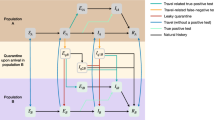
Travel-Related Transmission of COVID-19
The role of international transportation in facilitating the spread of SARS-CoV-2 has been extensively investigated. Since pre-symptomatic transmission of the virus was first recognized in March 2020 [ 35 ], efforts have been made to characterize the pattern and dynamics of transmission aboard commercial aircraft [ 36 ], cruise ships [ 37 ], rail and bus transport, and in mass gatherings and quarantine facilities (Table 1 ). Whole-genome sequencing has contributed dramatically to understanding the spread of SARS-CoV-2 among aircraft passengers [ 38 , 39 ]. An engineering simulation study from Hong Kong determined that front passengers exposed to a passenger coughing in the seat behind them had a four-fold greater infection risk than that of other passengers [ 40 ]. The risk of inhaling infected droplets from a talking passenger was broadly the same for nearby passengers. Wastewater-based epidemiology has emerged as a valuable tool for the surveillance of SARS-CoV-2 RNA and has been successfully applied in the setting of commercial aircraft and cruise ship sanitation systems as well as at mass gatherings including the Tokyo 2020 Olympic and Paralympic Games [ 41 , 42 ].
COVID-19 Mitigation and Control Measures
Pre-travel testing and airport screening protocols.
Early in the pandemic, many national guidelines included fever screening for travelers pre-departure or during transit. Some entry screening processes have also used symptom surveys and visual observations to identify potentially infected travelers. Fever scanning devices have reasonable sensitivity for detection of febrile travelers although with a relatively low positive predictive value [ 67 ]. With recognition of asymptomatic and pre-symptomatic transmission of SARS-CoV-2 and clinical studies showing that not all COVID-19 patients exhibited fevers [ 35 , 68 , 69 ], airport-based fever and symptom checklists are relatively low-yield screening strategies.
With the advent of more widely available diagnostic modalities including PCR and rapid antigen tests, pre-travel screening within 24 to 72 h of departure or even on-site pre-boarding rapid testing became feasible strategies to reduce the potential risk of infected travelers boarding flights or testing positive on arrival and thus requiring immediate isolation [ 5 ]. Pre-departure rapid antigen testing compared to PCR in Vancouver demonstrated the feasibility of using lateral flow, rapid antigen tests in the airport pre-departure [ 26 ]. The use of specially trained dogs to identify individuals with asymptomatic or mild COVID-19 may provide an additional innovative approach to detect infected travelers at airports, train stations, and other ports of embarkation [ 70 , 71 ].
Pre-travel screening has been a frequently implemented strategy to reduce the risk of SARS-CoV-2 importation. Generally, testing was required to be conducted within 72 h before departure although from October 2021 to June 2022, the USA mandated testing within a day of travel to the USA. The yield of this approach may be relatively limited. One study of German travelers, conducted between October 2020 and January 2021, found positive pre-travel tests in only 0.58% of 521 international travelers [ 72 ]. A PCR test done 2–3 days before departure may still miss an infected traveler in the incubation period that will become infectious during travel or shortly after arrival at their destination. Examples of both have occurred. Despite pre-departure negative tests, whole genome sequencing indicated inflight transmission between Dubai and Auckland based on testing performed shortly after arrival while in managed isolation and quarantine, although the pre-departure testing had been performed 4 to 5 days before departure [ 50 •]. Similarly, some travelers were found to have a high viral load (low cycle threshold value) on arrival in Spain despite negative pre-travel tests [ 54 ]. A modeling analysis of different strategies found that the risk of imported infection could be reduced by 80–90% through the use of testing on arrival and 7- or 14-day quarantine for test-negative individuals (relative to no testing) [ 73 ]. In summary, a variety of strategies have been utilized to attempt to reduce the importation of COVID-19 via international travelers, including controversial travel bans [ 74 ], pre-departure testing within 24 to 72 h, rapid testing immediately prior to travel, testing on arrival [ 75 ], and mandatory quarantine with testing and isolation of infected travelers. Some countries have mandated quarantine periods of as long as 21 days; these measures have resulted in unanticipated negative effects on the mental health, quality of life, and economic livelihood of travelers [ 19 •].
Attempts to use rigorous strategies to create COVID-19-free bubbles were successfully implemented by several countries including China, Hong Kong, New Zealand, and Australia during the first year or more of the pandemic [ 76 ]. These approaches required a multi-component approach including pre-departure testing, testing on arrival, strict mandatory quarantine with testing, and isolation of infected individuals. When successfully implemented, countries like Australia and New Zealand were able to develop COVID-19-free travel corridors. However, with the advent of the highly transmissible Omicron variant of concern in late 2021 and early 2022, SARS-CoV-2 was introduced into these previously virus-free locations, leading to local spread, although often limited by intensive local testing and control measures, especially in mainland China. Ultimately, the best available strategies to reduce the spread of COVID-19 through travel need to be deployed, but with the recognition that total containment is not possible. Data support an integrated approach with pre-travel testing, ideally within 24 h of departure or airport-based screening, masking during travel, and voluntary or mandatory quarantine on arrival with testing within 5–7 days of arrival will help to mitigate the spread of COVID-19.
Protective Efficacy of Masks and Social Distancing During Air Travel
Since recognition that SARS-CoV-2 is predominantly transmitted through respiratory droplets and small particle aerosols, face masks have become a widely used protective strategy. Observational and laboratory studies provided evidence that face masks prevent infected individuals from transmitting virus (source control) but also protect uninfected individuals from exposure to SARS-CoV-2 [ 77 ]. Similarly, a systematic review and meta-analysis found that face masks could reduce infection by as much as 85% with greater levels of protection provided by N95 or similar types of masks relative to surgical masks [ 78 ]. Good fit, mask quality, and appropriate use are all key factors influencing the degree of protection [ 78 , 79 ].
While many epidemiological studies supported the protective effectiveness of masks for reducing risk of SARS-CoV-2 infection, direct evidence from airplanes, trains, and cruise ships is relatively limited. A review of in-flight transmission described several examples where strict masking policies on flights were associated with reduced or no transmission of SARS-CoV-2 in contrast to flights where masking was optional or rare [ 80 •]. Sophisticated modeling studies have accounted for dynamic variables such as the movement of air passengers around the cabin and the variable effectiveness of masking; usage of FFP2/N95 masks reduced super-spreading events by 95–100%, while cloth masks were estimated to reduce infection rates by 40–80% [ 81 ]. The infected traveler’s overhead gasper jet and a higher backrest were mitigating factors [ 40 ]. Although prolonged masking during air travel may be uncomfortable, volunteers wearing an FFP2 protective mask showed no differences in blood oxygen saturation measurements at sea level and simulated airplane altitude (7500 ft) relative to non-mask-wearing participants [ 82 ].
Since most well-documented in-flight instances of SARS-CoV-2 transmission have involved people sitting in the same row or within two rows in front of or behind the index case [ 80 •], reduced seating density may also help to reduce risk of in-flight transmission. In addition to masking, there is evidence from community and hospital studies that maintaining a distance between individuals reduces transmission risk with increasing protective effectiveness at 1, 2, and 3 m of distance [ 78 ]. The potential protective effect of eliminating middle seat occupancy on flights was evaluated in an experimental model, which found that this approach could lead to a reduction of transmission risk of up to 57% [ 83 ]. Unfortunately, airlines need to make use of all seats in order to maximize profits and therefore no longer use this approach.
Protective Measures to Mitigate SARS-CoV-2 Spread on Cruise Ships
Cruise lines have had major problems with outbreaks (Table 1 ), which have led to careful consideration of strategies to reduce SARS-CoV-2 transmission. Many cruise ship outbreaks occurred early in the pandemic before stricter protocols were implemented by the cruise ship companies. A comprehensive analysis by the CDC of 89 voyages on 70 cruises in US water or carrying US citizens between January and April 2020 identified longer duration of travel (14- vs. 7-day voyages) as a risk factor for outbreaks [ 84 ]. In contrast, risk was lower for cruises that decreased the total number of passengers and crew members, performed testing on days 0 and 4, used daily symptom screening, isolated anyone who tested positive or developed compatible symptoms, and limited the cruise to a single port of call. Thus, a series of measures including advising full pre-cruise vaccination (ideally mandatory rather than just advised), pre-embarkation screening, daily symptom monitoring, testing on two time points shortly after departure, and effective isolation and quarantine protocols can help reduce the spread of SARS-CoV-2 on ships [ 85 ]. Data are limited on the utility of masking in this context.
Game-Changing Therapeutic Advances
Vaccines and therapeutics were developed swiftly against SARS-CoV-2 and have played a game-changing role, especially in reopening society and restarting travel. The dazzling speed with which COVID-19 vaccines were developed and rolled out generated optimism for the world to regain normalcy [ 86 , 87 , 88 , 89 ]. Although some countries initially accepted only the vaccines authorized by their national health authority, many countries have come to accept vaccines that have been issued an Emergency Use Listing by the WHO [ 90 ]. Currently the most widely available, accepted, and recognized vaccines are the mRNA vaccines and adenovirus-vectored vaccines, but the list will certainly expand as more vaccines are authorized. The emergence of SARS-CoV-2 variants has moderated some expectations for normalcy due to the “immune escape” displayed by Omicron and its subvariants [ 91 ••].
Although COVID-19 vaccination programs allowed progress where vaccinated persons can assemble and can restart travel, complications arose because of vaccine hesitancy and concerns about vaccine inequality [ 92 , 93 , 94 , 95 ]. Misinformation and conspiracy theories regarding COVID-19 fueled doubt in science, medical experts, health authorities, and governments, and exacerbated skepticism about vaccines [ 92 ]. The exploitation of social media platforms by anti-vaccine movements and the delay in responding to misinformation led to a decline in intent to receive COVID-19 vaccines [ 92 ]. Interventions continue to be needed to increase trust in vaccines and motivation to undergo vaccination, especially with the inclusion of disadvantaged groups in mind.
Along with vaccine rollouts, documentation became a new complication for travelers due to the lack of standardized recording of COVID-19 vaccines. Each country or jurisdiction developed and utilized its own system, whether in paper or digital format. Despite the long-standing worldwide recognition of the WHO International Certificate of Vaccines or Prophylaxis (ICVP), it had not been designated as a universally accepted COVID-19 vaccine record at the start of the pandemic, and WHO’s development of digital health records had progressed slowly [ 7 •]. The solution for the complex health passport issues includes the use of the ICVP in paper format along with digital apps. Specifically, a global framework needs to be developed for documentation of vaccination, testing type and results, and immunity [ 6 , 7 •].
The other game changer for travel is the therapeutics for ambulatory settings (Table 2 ). Monoclonal antibodies (currently tixagevimab-cilgavimab) for pre-exposure prophylaxis provide protection for immunocompromised travelers who may have suboptimal vaccine response, or for persons who have contraindications to COVID-19 vaccination [ 96 ••, 97 ]. Effective oral drugs have become available for treatment [ 98 , 99 , 100 , 101 ]. These oral drugs may become additional strategies for safe travel when they can serve as post-exposure prophylaxis. However, this awaits an abundant drug supply and studies supporting their use in this role.
Pandemic Preparedness: Lessons for the Future
Much has been learned during the last 2 years of the COVID-19 pandemic that can serve to prepare the world for future challenges. The capacity exists to rapidly identify and sequence new viruses, and to use this knowledge to quickly develop vaccines and diagnostic tests [ 101 , 102 ]. However, there is a need to be able to rapidly scale up testing access including the early development of highly sensitive and specific rapid diagnostic tests that can be used as point-of-care tests pre-travel and immediately post-travel. There needs to be recognition of the importance of specialized travel clinics in education, pre-travel testing, and provision of travel kits (e.g., rapid diagnostic tests and standby antiviral therapy). In addition, efforts to facilitate equitable distribution of effective vaccines and to ensure public trust in domestic and international responses to new pandemics will be a critical feature of future pandemic responses [ 102 ].
Adapting to the Pandemic: the Future of Travel Medicine
Dramatic disruption of life took hold in an attempt to contain or mitigate the impact of COVID-19, with pervasive effects on travel, travel medicine, and migrant health [ 103 , 104 ]. A survey by the International Society of Travel Medicine found that travel clinics faced a substantial reduction in their travel volume; the staff shifted their focus to other clinical activities (18%) or redeployed to other healthcare needs (13%), while the majority were involved with COVID-19 testing and screening (56%), providing vaccine information (53%), and vaccine administration (43%) [ 13 •].
The COVID-19 pandemic has expedited innovation, which must continue to be incorporated into travel medicine in the future. Travel advisories and destination requirements were improved and updated weekly, such as those of the CDC Travelers’ Health Branch, UNWTO, and International Air Transport Association [ 105 , 106 ]. The field of disease modeling has expanded impressively and provided estimates on many aspects of COVID-19. Molecular epidemiology through genome sequencing has accelerated rapidly. Worldwide, educational programs were modified to follow public health advice. Leading travel medicine educational programs transformed to successfully deliver high-quality online webinars and courses, online examinations, and an international conference using an immersive virtual reality platform [ 12 ]. Collaborators also met regularly online, overcoming the previous barrier imposed by distance and cost.
The future of travel medicine is robust. Travel-related health risks persist and concern for non-infectious diseases has increased [ 10 , 11 ]. COVID-19 has raised public awareness about the interaction of travel with cross-border infections and emerging infections, and again illustrated the role of the traveler as sentinel of infectious diseases [ 107 ]. It has also highlighted the vulnerability of the traveler with chronic medical illnesses [ 108 •]. COVID-19 is likely to remain as an endemic infection, and surveillance will be as important as prevention. COVID-19 gave an impetus to advance technology for virtual appointments, to adopt mobile devices and GPS in contact tracing, and to use digital applications in research and surveillance of other travel-related infections such as arboviral diseases and rabies [ 17 , 109 , 110 ]. The future of travel medicine should harness these new platforms in its clinical work, research, and education.
Strengths and Limitations of Review
The volume of new publications relating to COVID-19 continues to increase rapidly, making it necessary to update reviews on this subject at regular intervals. An effort has been made to draw on the most recently published sources relevant to COVID-19 and international travel in this review. Our search strategy did not include specialized social science or psychology sources, which may have contained relevant material. Our literature search was restricted to articles published in the English language, and potentially relevant studies published in other languages may therefore have been overlooked.
Conclusions
The ongoing COVID-19 pandemic has had a profound impact on the travel industry and on the experiences of the travelling public, who are now familiar with the requirements of COVID-19 vaccine certification, pre- and post-departure diagnostic testing, rapid antigen self-testing, mask wearing, and the critical importance of comprehensive travel insurance. While novel vaccines and antiviral agents have greatly reduced the risk of severe hospitalization and death, the threat of further variants that show vaccine or immune escape looms large and complicates efforts to return to a normal travel environment. Travel medicine providers have demonstrated resilience in adapting to the pandemic. Travel medicine should leverage the technological and behavioral progress of the pandemic in insulating itself against future global shocks. Future research should assess the long-term impact of the pandemic on traveler health behavior and on the practice of travel medicine.
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
World Tourism Organization. International tourism highlights, 2020 edition. UNWTO, Madrid. 2021. https://doi.org/10.18111/9789284422456 .
Wilson ME, Chen LH. Travelers give wings to novel coronavirus (2019-nCoV). J Travel Med. 2020;27(2):1–3. https://doi.org/10.1093/jtm/taaa015 .
Article Google Scholar
Chen LH, Freedman DO, Visser LG. COVID-19 immunity passport to ease travel restrictions? J Travel Med. 2020. https://doi.org/10.1093/jtm/taaa085 .
Article PubMed PubMed Central Google Scholar
•• Wilson ME, Chen LH. Re-starting travel in the era of COVID-19: preparing anew. J Travel Med 2020;27(5):taaa108. Practical guidance for travel medicine practitioners regarding the assessment of the risk of SARS-CoV-2 in the pre-travel consultation.
Chen LH, Steffen R. SARS-CoV-2 testing to assure safety in air travel. J Travel Med. 2021;28(2):taaa241.
Petersen E, Lucey D, Blumberg L, Kramer LD, Al-Abri S, Lee SS, Pinto TCA, Obiero CW, Rodriguez-Morales AJ, Yapi R, Abubakar A, Tambyah PA, Holmes A, Chen LH. COVID-19 vaccines under the International Health Regulations - we must use the WHO International Certificate of Vaccination or Prophylaxis. Int J Infect Dis. 2021;20(104):175–7. https://doi.org/10.1016/j.ijid.2021.01.039 .
Article CAS Google Scholar
• Chen LH, Petersen E, Blumberg L, Piyaphanee W, Steffen R. COVID-19 health passes: current status and prospects for a global approach. J Travel Med. 2021;28(7):taab118. https://doi.org/10.1093/jtm/taab118 . Authoritative perspective on the use of digital health passports at international borders.
•• Khatib AN, Carvalho AM, Primavesi R, To K, Poirier V. Navigating the risks of flying during COVID-19: a review for safe air travel. J Travel Med. 2020;27(8):taaa212. https://doi.org/10.1093/jtm/taaa212 . Review of the in-flight transmission risks of commercial air travel, with recommendations about the risks of flying during the pandemic.
Khatib AN, McGuinness S, Wilder-Smith A. COVID-19 transmission and the safety of air travel during the pandemic: a scoping review. Curr Opin Infect Dis. 2021;34(5):415–22. https://doi.org/10.1097/QCO.0000000000000771 .
Article CAS PubMed Google Scholar
Hatz C, Bühler S, Farnham A. The COVID-19 pandemic offers a key moment to reflect on travel medicine practice. J Travel Med. 2020;27(8):taaa149. https://doi.org/10.1093/jtm/taaa149 .
Article PubMed Google Scholar
Shlim DR, Connor BA, Taylor DN. What will travel medicine look like in the COVID-19 pandemic era? J Travel Med. 2021;28(2):taaa148. https://doi.org/10.1093/jtm/taaa148 .
Flaherty GT, Acosta RW, Visser JT, Coyle CM, Chen LH. Learning in lockdown: preparing for the inaugural virtual conference of the International Society of Travel Medicine. J Travel Med. 2020;27(8):taaa220. https://doi.org/10.1093/jtm/taaa220 .
• Acosta RW, Visser JT, Chen LH, Leggat PA, Flaherty GT. Adaptation of travel medicine practitioners to the COVID-19 pandemic: a cross-sectional survey of ISTM members. J Travel Med. 2022;taac032. https://doi.org/10.1093/jtm/taac032 . An insightful report on the response of the travel medicine community to the COVID-19 pandemic.
World Tourism Organization. Impact assessment of the COVID-19 outbreak on international tourism. 2022. Available at: https://www.unwto.org/impact-assessment-of-the-covid-19-outbreak-on-international-tourism . (last accessed 06 May 2022).
Flaherty GT, Nasir N. Reiseangst: travel anxiety and psychological resilience during and beyond the COVID-19 pandemic. J Travel Med. 2020;27(8):taaa150. https://doi.org/10.1093/jtm/taaa150 .
Flaherty GT, Holmes A. Will flight shaming influence the future of air travel? J Travel Med. 2020;27(2):taz088. https://doi.org/10.1093/jtm/taz088 .
Flaherty GT, Vyas V, Browne F. Quo vadis? Reflections on the future direction of travel medicine practice and research. IeJSME. 2021;15(1):1–4.
Mangan RM, Flaherty GT. The advent of social media influencer tourism: travel health risks and opportunities. J Travel Med. 2021;28(8):taab140. https://doi.org/10.1093/jtm/taab140 .
• Klinger C, Burns J, Movsisyan A, et al. Unintended health and societal consequences of international travel measures during the COVID-19 pandemic: a scoping review. J Travel Med. 2021;28(7):taab123. https://doi.org/10.1093/jtm/taab123 . Scoping review of empirical studies on the collateral effects, both beneficial and harmful, of international travel restrictions relating to the COVID-19 pandemic.
Hu Y, Xu CL, Tu M. Family-mediated migration infrastructure: Chinese international students and parents navigating (im)mobilities during the COVID-19 pandemic. Chin Sociol Rev. 2020.
Martuscelli PN. How are refugees affected by Brazilian responses to COVID-19? Rev Adm Pública. 2020;54:1446–57.
Google Scholar
Radic A, Lück M, Ariza-Montes A, Han H. Fear and trembling of cruise ship employees: psychological effects of the COVID-19 pandemic. Int J Environ Res Public Health. 2020;17:6741.
Zhang H, Lin Y, Wei S, et al. Global association between satellite-derived nitrogen dioxide (NO2) and lockdown policies under the COVID-19 pandemic. Sci Total Environ. 2021;761:144148.
CNN Travel. Deserted Venice contemplates a future without tourist hordes after Covid-19. 2020. Available at: https://edition.cnn.com/travel/article/venice-future-covid-19/index.html . Accessed 24 June 2022.
Barry G, McCarney C, Farrelly M, Breathnach R, Mooney C, More SJ. Rapid antigen testing for SARS-CoV-2 infection in a university setting in Ireland: learning from a 6-week pilot study. Public Health Pract (Oxf). 2022;3:100255. https://doi.org/10.1016/j.puhip.2022.100255 .
Qahtani MA, Yang CWT, Lazosky L, et al. SARS-CoV-2 rapid antigen testing for departing passengers at Vancouver International Airport. J Travel Med. 2021;28(7):taab085. https://doi.org/10.1093/jtm/taab085 .
Soo RJJ, Chiew CJ, Ma S, Pung R, Lee V. Decreased influenza incidence under COVID-19 control measures. Singapore Emerg Infect Dis. 2020;26(8):1933–5. https://doi.org/10.3201/eid2608.201229 .
Achangwa C, Park H, Ryu S, Lee MS. Collateral impact of public health and social measures on respiratory virus activity during the COVID-19 pandemic 2020–2021. Viruses. 2022;14(5):1071. https://doi.org/10.3390/v14051071 .
Article CAS PubMed PubMed Central Google Scholar
de Miguel Buckley R, Trigo E, de la Calle-Prieto F, Arsuaga M, Díaz-Menéndez M. Social distancing to combat COVID-19 led to a marked decrease in food-borne infections and sexually transmitted diseases in Spain. J Travel Med. 2020;27(8):taaa134. https://doi.org/10.1093/jtm/taaa134 .
Steffen R, Lautenschlager S, Fehr J. Travel restrictions and lockdown during the COVID-19 pandemic-impact on notified infectious diseases in Switzerland. J Travel Med. 2020;27(8):taaa180. https://doi.org/10.1093/jtm/taaa180 .
Chen Y, Li N, Lourenço J, et al. Measuring the effects of COVID-19-related disruption on dengue transmission in southeast Asia and Latin America: a statistical modelling study. Lancet Infect Dis. 2022;22(5):657–67. https://doi.org/10.1016/S1473-3099(22)00025-1 .
Schubert L, Thurnher PMM, Machold PK, Tobudic PS, Winkler PS. Pandemic-related delay of falciparum malaria diagnosis in a traveller leading to cerebral malaria. J Travel Med. 2021;28(8):taab159. https://doi.org/10.1093/jtm/taab159 .
Lee DID, Vanderhout S, Aglipay M, et al. Delay in childhood vaccinations during the COVID-19 pandemic. Can J Public Health. 2022;113(1):126–34. https://doi.org/10.17269/s41997-021-00601-9 .
Hillis A, Leavey C, Kewley S, Church S, Van Hout MC. Sex tourism, disease migration and COVID-19: lessons learnt and best practices moving forward. J Travel Med. 2020;27(7):taaa144. https://doi.org/10.1093/jtm/taaa144 .
Rothe C, Schunk M, Sothmann P, et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382(10):970–1. https://doi.org/10.1056/NEJMc2001468 .
Rosca EC, Heneghan C, Spencer EA, et al. Transmission of SARS-CoV-2 associated with aircraft travel: a systematic review. J Travel Med. 2021;28(7):taab133. https://doi.org/10.1093/jtm/taab133 .
Willebrand KS, Pischel L, Malik AA, Jenness SM, Omer SB. A review of COVID-19 transmission dynamics and clinical outcomes on cruise ships worldwide, January to October 2020. Euro Surveill. 2022;27(1):2002113. https://doi.org/10.2807/1560-7917.ES.2022.27.1.2002113 .
Article CAS PubMed Central Google Scholar
Ngeh S, Vogt F, Sikazwe CT, et al. Travel-associated SARS-CoV-2 transmission documented with whole genome sequencing following a long-haul international flight. J Travel Med. 2022. https://doi.org/10.1093/jtm/taac057 .
Speake H, Phillips A, Chong T, et al. Flight-associated transmission of severe acute respiratory syndrome coronavirus 2 corroborated by whole-genome sequencing. Emerg Infect Dis. 2020;26(12):2872–80. https://doi.org/10.3201/eid2612.203910 .
Wang CT, Xu JC, Fu SC, Chao CYH. Airborne infection risk of nearby passengers in a cabin environment and implications for infection control. Travel Med Infect Dis. 2022;47:102285. https://doi.org/10.1016/j.tmaid.2022.102285 .
Ahmed W, Bertsch PM, Angel N, et al. Detection of SARS-CoV-2 RNA in commercial passenger aircraft and cruise ship wastewater: a surveillance tool for assessing the presence of COVID-19 infected travellers. J Travel Med. 2020;27(5):taaa116. https://doi.org/10.1093/jtm/taaa116 .
Kitajima M, Murakami M, Iwamoto R, Katayama H, Imoto S. COVID-19 wastewater surveillance implemented in the Tokyo 2020 Olympic and Paralympic Village. J Travel Med. 2022;29(3):taac004. https://doi.org/10.1093/jtm/taac004 .
Moriarty LF, Plucinski MM, Marston BJ, et al. Public health responses to COVID-19 outbreaks on cruise ships - worldwide, February-March 2020. MMWR Morb Mortal Wkly Rep. 2020;69(12):347–52. https://doi.org/10.15585/mmwr.mm6912e3 .
Plucinski MM, Wallace M, Uehara A, et al. Coronavirus disease 2019 (COVID-19) in Americans aboard the Diamond Princess cruise ship. Clin Infect Dis. 2021;72(10):e448–57. https://doi.org/10.1093/cid/ciaa1180 .
Rocklöv J, Sjödin H, Wilder-Smith A. COVID-19 outbreak on the Diamond Princess cruise ship: estimating the epidemic potential and effectiveness of public health countermeasures. J Travel Med. 2020;27(3):taaa030. https://doi.org/10.1093/jtm/taaa030 .
Gravningen K, Henriksen S, Hungnes O, et al. Risk factors, immune response and whole-genome sequencing of SARS-CoV-2 in a cruise ship outbreak in Norway. Int J Infect Dis. 2022;118:10–20. https://doi.org/10.1016/j.ijid.2022.02.025 .
Khanh NC, Thai PQ, Quach HL, et al. Transmission of SARS-CoV 2 during long-haul flight. Emerg Infect Dis. 2020;26(11):2617–24. https://doi.org/10.3201/eid2611.203299 .
Choi EM, Chu DKW, Cheng PKC, et al. In-flight transmission of SARS-CoV-2. Emerg Infect Dis. 2020;26(11):2713–6. https://doi.org/10.3201/eid2611.203254 .
Eichler N, Thornley C, Swadi T, et al. Transmission of severe acute respiratory syndrome coronavirus 2 during border quarantine and air travel, New Zealand (Aotearoa). Emerg Infect Dis. 2021;27(5):1274–8. https://doi.org/10.3201/eid2705.210514 .
• Swadi T, Geoghegan JL, Devine T, et al. Genomic evidence of in-flight transmission of SARS-CoV-2 despite predeparture testing. Emerg Infect Dis. 2021;27(3):687–93. https://doi.org/10.3201/eid2703.204714 . Report of seven cases of SARS-CoV-2 in a managed isolation and quarantine setting in New Zealand.
White PF, Boland M, O’Sullivan MB, et al. Transmission of SARS-CoV-2 arising from international flights arriving in Ireland in December 2020: a descriptive analysis using national surveillance data. Public Health. 2022;204:49–53. https://doi.org/10.1016/j.puhe.2022.01.004 .
Dhanasekaran V, Edwards KM, Xie R, et al. Air travel-related outbreak of multiple SARS-CoV-2 variants. J Travel Med. 2021;28(8):taab149. https://doi.org/10.1093/jtm/taab149 .
• Hogarth F, Coffey P, Goddard L, et al. Genomic evidence of in-flight SARS-CoV-2 transmission, India to Australia, April 2021. Emerg Infect Dis. 2022;28(7):1527–30. https://doi.org/10.3201/eid2807.212466 . Epidemiologic and genomic investigation suggesting SARS-CoV-2 transmission despite mandatory mask use and pre-departure testing.
Molero-Salinas A, Rico-Luna C, Losada C, et al. High SARS-CoV-2 viral load in travellers arriving in Spain with a negative COVID-19 test prior to departure. J Travel Med. 2022;29(3):taab180. https://doi.org/10.1093/jtm/taab180 .
Fox-Lewis A, Williamson F, Harrower J, et al. Airborne transmission of SARS-CoV-2 Delta variant within tightly monitored isolation facility, New Zealand (Aotearoa). Emerg Infect Dis. 2022;28(3):501–9. https://doi.org/10.3201/eid2803.212318 .
Qiu S, Liu H, Li P, et al. Familial cluster of SARS-CoV-2 infection associated with a railway journey. J Travel Med. 2020;27(5):taaa088. https://doi.org/10.1093/jtm/taaa088 .
Benenson S, Ottolenghi M, Cohen MJ, Nir-Paz R, Oster Y. High attack rate of COVID-19 in an organized tour group of vaccinated travellers to Iceland. J Travel Med. 2021;28(8):taab157. https://doi.org/10.1093/jtm/taab157 .
Tsuchihashi Y, Yamagishi T, Suzuki M, et al. High attack rate of SARS-CoV-2 infections during a bus tour in Japan. J Travel Med. 2021;28(8):taab111. https://doi.org/10.1093/jtm/taab111 .
Amatya B, Pandey P, Dawadi S, Manandhar S. COVID-19 in fully vaccinated Everest trekkers in Nepal. J Travel Med. 2021;28(7):taab098. https://doi.org/10.1093/jtm/taab098 .
Stange M, Mari A, Roloff T, et al. SARS-CoV-2 outbreak in a tri-national urban area is dominated by a B.1 lineage variant linked to a mass gathering event. PLoS Pathog. 2021;17(3):e1009374. https://doi.org/10.1371/journal.ppat.1009374 .
Lemieux JE, Siddle KJ, Shaw BM, et al. Phylogenetic analysis of SARS-CoV-2 in Boston highlights the impact of superspreading events. Science. 2021;371(6529):eabe3261. https://doi.org/10.1126/science.abe3261 .
Yusef D, Hayajneh W, Awad S, et al. Large outbreak of coronavirus disease among wedding attendees. Jordan Emerg Infect Dis. 2020;26(9):2165–7. https://doi.org/10.3201/eid2609.201469 .
Shukla S, Khan R, Ahmed Y, Memish ZA. Conducting mass gathering events during the COVID-19 pandemic: a case study of Kumbh Mela 2021 as a potential ‘super spreader event.’ J Travel Med. 2021;28(8):taab160. https://doi.org/10.1093/jtm/taab160 .
Cuschieri S, Grech S, Cuschieri A. An observational study of the Covid-19 situation following the first pan-European mass sports event. Eur J Clin Invest. 2022;52(4):e13743. https://doi.org/10.1111/eci.13743 .
Sami S, Horter L, Valencia D, et al. Investigation of SARS-CoV-2 transmission associated with a large indoor convention - New York City, November-December 2021. MMWR Morb Mortal Wkly Rep. 2022;71(7):243–8. https://doi.org/10.15585/mmwr.mm7107a4 .
Smith-Jeffcoat SE, Pomeroy MA, Sleweon S, et al. Multistate outbreak of SARS-CoV-2 B.1.1.529 (Omicron) variant infections among persons in a social network attending a convention - New York City, November 18-December 20, 2021. MMWR Morb Mortal Wkly Rep. 2022;71(7):238–42. https://doi.org/10.15585/mmwr.mm7107a3 .
Aggarwal N, Garg M, Dwarakanathan V, et al. Diagnostic accuracy of non-contact infrared thermometers and thermal scanners: a systematic review and meta-analysis. J Travel Med. 2020;27(8):taaa193. https://doi.org/10.1093/jtm/taaa193 .
Arons MM, Hatfield KM, Reddy SC, et al. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. N Engl J Med. 2020;382(22):2081–90. https://doi.org/10.1056/NEJMoa2008457 .
Burke RM, Killerby ME, Newton S, et al. Symptom profiles of a convenience sample of patients with COVID-19 - United States, January-April 2020. MMWR Morb Mortal Wkly Rep. 2020;69(28):904–8. https://doi.org/10.15585/mmwr.mm6928a2 .
Guest C, Dewhirst SY, Lindsay SW, et al. Using trained dogs and organic semi-conducting sensors to identify asymptomatic and mild SARS-CoV-2 infections: an observational study. J Travel Med. 2022;29(3):taac043. https://doi.org/10.1093/jtm/taac043 .
Kantele A, Paajanen J, Turunen S, et al. Scent dogs in detection of COVID-19: triple-blinded randomised trial and operational real-life screening in airport setting. BMJ Glob Health. 2022;7(5):e008024. https://doi.org/10.1136/bmjgh-2021-008024 .
Schneitler S, Gülker J, Alhussein F, et al. Experiences with pre-travel diagnostic PCR testing for SARS-CoV-2: challenges and opportunities. J Travel Med. 2021;28(7):taab116. https://doi.org/10.1093/jtm/taab116 .
Dickens BL, Koo JR, Lim JT, et al. Strategies at points of entry to reduce importation risk of COVID-19 cases and reopen travel. J Travel Med. 2020;27(8):taaa141. https://doi.org/10.1093/jtm/taaa141 .
Mendelson M, Venter F, Moshabela M, et al. The political theatre of the UK’s travel ban on South Africa. Lancet. 2021;398(10318):2211–3. https://doi.org/10.1016/S0140-6736(21)02752-5 .
Layer E, Hoehl S, Widera M, et al. SARS-CoV-2 screening strategies for returning international travellers: evaluation of a rapid antigen test approach. Int J Infect Dis. 2022;118:126–31. https://doi.org/10.1016/j.ijid.2022.02.045 .
Sharun K, Tiwari R, Natesan S, Yatoo MI, Malik YS, Dhama K. International travel during the COVID-19 pandemic: implications and risks associated with ‘travel bubbles.’ J Travel Med. 2020;27(8):taaa184. https://doi.org/10.1093/jtm/taaa184 .
Czypionka T, Greenhalgh T, Bassler D, Bryant MB. Masks and face coverings for the lay public: a narrative update. Ann Intern Med. 2021;174(4):511–20. https://doi.org/10.7326/M20-6625 .
Chu DK, Akl EA, Duda S, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395(10242):1973–87. https://doi.org/10.1016/S0140-6736(20)31142-9 .
Brooks JT, Beezhold DH, Noti JD, et al. Maximizing fit for cloth and medical procedure masks to improve performance and reduce SARS-CoV-2 transmission and exposure, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(7):254–7. https://doi.org/10.15585/mmwr.mm7007e1 .
• Freedman DO, Wilder-Smith A. In-flight transmission of SARS-CoV-2: a review of the attack rates and available data on the efficacy of face masks. J Travel Med. 2020;27(8):taaa178. https://doi.org/10.1093/jtm/taaa178 . Perspective on the role of face masks in preventing transmission of SARS-CoV-2 aboard commercial aircraft.
Namilae S, Wu Y, Mubayi A, Srinivasan A, Scotch M. Identifying mitigation strategies for COVID-19 superspreading on flights using models that account for passenger movement. Travel Med Infect Dis. 2022;47:102313. https://doi.org/10.1016/j.tmaid.2022.102313 .
Sammito S, Müller GPJ, Erley OM, Werner A. Impact of in-flight use of FFP2 masks on oxygen saturation: an experimental crossover study. J Travel Med. 2021;28(4):taab018. https://doi.org/10.1093/jtm/taab018 .
Dietrich WL, Bennett JS, Jones BW, Hosni MH. Laboratory modeling of SARS-CoV-2 exposure reduction through physically distanced seating in aircraft cabins using bacteriophage aerosol - November 2020. MMWR Morb Mortal Wkly Rep. 2021;70(16):595–9. https://doi.org/10.15585/mmwr.mm7016e1 .
Guagliardo SAJ, Prasad PV, Rodriguez A, et al. Cruise ship travel in the era of coronavirus disease 2019 (COVID-19): a summary of outbreaks and a model of public health interventions. Clin Infect Dis. 2022;74(3):490–7. https://doi.org/10.1093/cid/ciab433 .
Centers for Disease Control and Prevention. Technical instructions for CDC’s COVID-19 program for cruise ships operating in U.S. waters. 2022. Available at: https://www.cdc.gov/quarantine/cruise/management/technical-instructions-for-cruise-ships.html . (last accessed 27 June 2022).
Jackson LA, Anderson EJ, Rouphael NG, et al. An mRNA vaccine against SARS-CoV-2 - preliminary report. N Engl J Med. 2020;383(20):1920–31. https://doi.org/10.1056/NEJMoa2022483 .
Polack FP, Thomas SJ, Kitchin N, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383(27):2603–15. https://doi.org/10.1056/NEJMoa2034577 .
Voysey M, Clemens SAC, Madhi SA, et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet. 2021 9;397(10269):99–111. https://doi.org/10.1016/S0140-6736(20)32661-1 . Epub 2020 Dec 8. Erratum in: Lancet. 2021 Jan 9;397(10269):98.
Sadoff J, Gray G, Vandebosch A, et al. Safety and efficacy of single-dose Ad26.COV2.S vaccine against Covid-19. N Engl J Med. 2021;384(23):2187–201. https://doi.org/10.1056/NEJMoa2101544 .
World Health Organization. COVID-19 vaccines with WHO Emergency Use Listing. 2022. Available at: https://extranet.who.int/pqweb/vaccines/vaccinescovid-19-vaccine-eul-issued . (last accessed 27 June 2022).
•• Krause PR, Fleming TR, Longini IM, et al. SARS-CoV-2 variants and vaccines. N Engl J Med. 2021;385(2):179–86. https://doi.org/10.1056/NEJMsr2105280 . Special report about the emergence of SARS-CoV-2 variants of concern and their response to currently available vaccines.
Pertwee E, Simas C, Larson HJ. An epidemic of uncertainty: rumors, conspiracy theories and vaccine hesitancy. Nat Med. 2022;28(3):456–9. https://doi.org/10.1038/s41591-022-01728-z .
Crawshaw AF, Deal A, Rustage K, et al. What must be done to tackle vaccine hesitancy and barriers to COVID-19 vaccination in migrants? J Travel Med. 2021;28(4):taab048. https://doi.org/10.1093/jtm/taab048 .
Crawshaw AF, Farah Y, Deal A, et al. Defining the determinants of vaccine uptake and undervaccination in migrant populations in Europe to improve routine and COVID-19 vaccine uptake: a systematic review. Lancet Infect Dis. 2022;S1473–3099(22):00066–74. https://doi.org/10.1016/S1473-3099(22)00066-4 .
Franco-Paredes C, Suarez JA, Henao-Martínez AF. Global COVID-19 vaccine equity should precede requiring travelers proof of vaccination. Int J Infect Dis. 2021;105:243–4. https://doi.org/10.1016/j.ijid.2021.02.061 .
•• Levin MJ, Ustianowski A, De Wit S, et al. Intramuscular AZD7442 (tixagevimab-cilgavimab) for prevention of Covid-19. N Engl J Med. 2022. https://doi.org/10.1056/NEJMoa2116620 . Phase 3 trial of the efficacy of a monoclonal antibody combination in the prevention of COVID-19.
Kotton CN. Belt and suspenders: vaccines and tixagevimab/cilgavimab for prevention of COVID-19 in immunocompromised patients. Ann Intern Med. 2022;12:M22-1026. https://doi.org/10.7326/M22-1026 .
Hammond J, Leister-Tebbe H, Gardner A, et al. Oral nirmatrelvir for high-risk, nonhospitalized adults with Covid-19. N Engl J Med. 2022;386(15):1397–408. https://doi.org/10.1056/NEJMoa2118542 .
Jayk Bernal A, Gomes da Silva MM, Musungaie DB, et al. Molnupiravir for oral treatment of Covid-19 in nonhospitalized patients. N Engl J Med. 2022;386(6):509–20. https://doi.org/10.1056/NEJMoa2116044 .
U.S. National Library of Medicine. Phase III double-blind, placebo-controlled study of AZD7442 for pre-exposure prophylaxis of COVID-19 in adult. (PROVENT). 2022. Available at: https://clinicaltrials.gov/ct2/show/NCT04625725 . (last accessed 25 June 2022).
Adashi EY, Cohen IG. SARS-CoV-2 laboratory-developed tests: integrity restored. JAMA. 2022;327(13):1229–30. https://doi.org/10.1001/jama.2022.3382 .
Nuzzo JB, Gostin LO. The first 2 years of COVID-19: lessons to improve preparedness for the next pandemic. JAMA. 2022;327(3):217–8. https://doi.org/10.1001/jama.2021.24394 .
Gobbi F, Noharet R, Abreu C, Del Mar Lago Nuñez M, Canale A, Oñorbe MF, Muñoz J, Rossanese A, Atouguia J. South Europe perspective of COVID-19 impact on travel medicine. J Travel Med. 2021;28(8):taab143. https://doi.org/10.1093/jtm/taab143 .
Hayward SE, Deal A, Cheng C, et al. Clinical outcomes and risk factors for COVID-19 among migrant populations in high-income countries: a systematic review. J Migr Health. 2021;3:100041. https://doi.org/10.1016/j.jmh.2021.100041 .
Centers for Disease Control and Prevention. COVID-19 travel recommendations by destination. 2022. Available at: https://www.cdc.gov/coronavirus/2019-ncov/travelers/map-and-travel-notices.html . (last accessed 27 June 2022).
World Tourism Organization. UNWTO/IATA Destination Tracker – Easy Travel. 2022. Available at: https://www.unwto.org/tourism-data/unwto-iata-destination-tracker-easy-travel . (last accessed 27 June 2022).
Hamer DH, Rizwan A, Freedman DO, Kozarsky P, Libman M. GeoSentinel: past, present and future†. J Travel Med. 2020;27(8):taaa219. https://doi.org/10.1093/jtm/taaa219 .
• Flaherty GT, Hession P, Liew CH, et al. COVID-19 in adult patients with pre-existing chronic cardiac, respiratory and metabolic disease: a critical literature review with clinical recommendations. Trop Dis Travel Med Vaccines. 2020;6:16. https://doi.org/10.1186/s40794-020-00118-y . Comprehensive review of the impact of COVID-19 on travellers with chronic illness.
Carrillo MA, Kroeger A, Cardenas Sanchez R, Diaz Monsalve S, Runge-Ranzinger S. The use of mobile phones for the prevention and control of arboviral diseases: a scoping review. BMC Public Health. 2021;21(1):110. https://doi.org/10.1186/s12889-020-10126-4 .
Subrata IM, Harjana NPA, Agustina KK, Purnama SG, Kardiwinata MP. Designing a rabies control mobile application for a community-based rabies surveillance system during the COVID-19 pandemic in Bali. Indonesia Vet World. 2022;15(5):1237–45. https://doi.org/10.14202/vetworld.2022.1237-1245 .
Download references
Open Access funding provided by the IReL Consortium.
Author information
Authors and affiliations.
School of Medicine, University of Galway, Galway, Ireland
Gerard T. Flaherty
School of Medicine, International Medical University, Kuala Lumpur, Malaysia
Department of Global Health, Boston University School of Public Health, Boston, MA, USA
Davidson H. Hamer
Section of Infectious Diseases, Boston University School of Medicine, Boston, MA, USA
Center for Emerging Infectious Disease Research and Policy, Boston University, Boston, MA, USA
National Emerging Infectious Disease Laboratory, Boston University, Boston, MA, USA
Division of Infectious Diseases and Travel Medicine, Mount Auburn Hospital, Cambridge, MA, USA
Lin H. Chen
Harvard Medical School, Boston, MA, USA
You can also search for this author in PubMed Google Scholar
Contributions
LHC was responsible for study conception. GTF, DH, and LHC contributed equally to the literature review and preparation of the first draft of the manuscript. All authors contributed equally to the editing of subsequent manuscript drafts. Each author read and approved the final version of the manuscript.
Corresponding author
Correspondence to Gerard T. Flaherty .
Ethics declarations
Conflict of interest.
Dr. Flaherty has received conference registration support as an Executive Board member of the Travel Medicine Society of Ireland (former) and International Society of Travel Medicine (current). Dr. Chen reports honoraria from Shoreland Inc, Valneva, Takeda, Sanofi-Pasteur, Emergent BioSolutions, and Merck. Dr. Hamer reports consulting fees and honoraria from Xenophon Strategies, Inc., Trinity Biotech, LLC, Equinox, Major League Soccer, PGA of America, Valneva, and Takeda.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Tropical, Travel and Emerging Infection
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Flaherty, G.T., Hamer, D.H. & Chen, L.H. Travel in the Time of COVID: A Review of International Travel Health in a Global Pandemic. Curr Infect Dis Rep 24 , 129–145 (2022). https://doi.org/10.1007/s11908-022-00784-3
Download citation
Accepted : 25 July 2022
Published : 04 August 2022
Issue Date : October 2022
DOI : https://doi.org/10.1007/s11908-022-00784-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Transmission
- Travel medicine
- Health passport
- Sustainable travel
- Find a journal
- Publish with us
- Track your research

- INTRODUCTION
- CASE REPORT
- ACKNOWLEDGMENTS
High-resolution esophageal manometry findings demonstrating ineffective esophageal motility with weak/failed propagation of the normal esophageal pressure wave during deglutition.
- View raw image
- Download Powerpoint Slide
WHO , 2022 . Chagas disease (also known as American trypanosomiasis). Available at: https://www.who.int/news-room/fact-sheets/detail/chagas-disease-(american-trypanosomiasis ). Accessed July 7, 2022.
- Export Citation
CDC , 2020 . Yellow Book 2020: health information for international travel. Available at: https://wwwnc.cdc.gov/travel/page/yellowbook-home-2020 . Accessed July 7, 2022.
Carter YL , Juliano JJ , Montgomery SP , Qvarnstrom Y , 2012 . Acute Chagas disease in a returning traveler . Am J Trop Med Hyg 87 : 1038 – 1040 .
- Search Google Scholar
The Global Surveillance Network of the ISTM and CDC , 2008 . The GeoSentinel Newsletter: Information for Action. Infrequent Diagnoses & Their Geographic Exposures . Atlanta, GA : Centers for Disease Control and Prevention .
Gautret P et al. , 2012 . Infectious diseases among travellers and migrants in Europe, EuroTravNet 2010 . Euro Surveill 17 : 20205 .
Villamil-Gómez WE , Echeverría LE , Ayala MS , Muñoz L , Mejía L , Eyes-Escalante M , Venegas-Hermosilla J , Rodríguez-Morales AJ , 2017 . Orally transmitted acute Chagas disease in domestic travelers in Colombia . J Infect Public Health 10 : 244 – 246 .
Yadlapati R et al. , 2021 . Esophageal motility disorders on high-resolution manometry: Chicago classification version 4.0 © . Neurogastroenterol Motil 33 : e14058 .
Forsyth CJ et al. , 2022 . Recommendations for screening and diagnosis of Chagas disease in the United States . J Infect Dis 225 : 1601 – 1610 .
Franco-Paredes C , Villamil-Gómez WE , Schultz J , Henao-Martínez AF , Parra-Henao G , Rassi A Jr , Rodríguez-Morales AJ , Suarez JA , 2020 . A deadly feast: elucidating the burden of orally acquired acute Chagas disease in Latin America —public health and travel medicine importance . Travel Med Infect Dis 36 : 101565 .
Medina-Rincón GJ , Gallo-Bernal S , Jiménez PA , Cruz-Saavedra L , Ramírez JD , Rodríguez MJ , Medina-Mur R , Díaz-Nassif G , Valderrama-Achury MD , Medina HM , 2021 . Molecular and clinical aspects of chronic manifestations in chagas disease: a state-of-the-art review . Pathogens 10 : 1493 .
Messenger LA , Miles MA , Bern C , 2015 . Between a bug and a hard place: Trypanosoma cruzi genetic diversity and the clinical outcomes of Chagas disease . Expert Rev Anti Infect Ther 13 : 995 – 1029 .
Salazar-Schettino PM et al. , 1984 . First case of megaeshophagus with positive Trypanosoma cruzi serology . Salud Publica Mex 26 : 452 – 455 .
Ocampo S et al. , 1993 . Megaesófago chagásico con serología y xenodiagnóstico positivos . Rev Mexicana Gastroenterol 58 : 36 – 38 .
Bellistri JP , Grucela A , 2014 . Chagas disease: an interesting presentation and diagnosis . Austin J Surg 1 : 1038 .
Sánchez-Guillén Mdel C , López-Colombo A , Ordóñez-Toquero G , Gomez-Albino I , Ramos-Jimenez J , Torres-Rasgado E , Salgado-Rosas H , Romero-Díaz M , Pulido-Pérez P , Pérez-Fuentes R , 2006 . Clinical forms of Trypanosoma cruzi infected individuals in the chronic phase of Chagas disease in Puebla, Mexico . Mem Inst Oswaldo Cruz 101 : 733 – 740 .
Lozano-Kasten F et al. , 1997 . Manifestaciones digestivas en la fase crónica de la enfermedad de Chagas . Cir Cir 65 : 10 – 14 .
Herbella FAM , Malafaia O , Patti MG , 2022 . New classification for esophageal motility disorders (Chicago classification version 4.0 © ) and Chagas disease esophagopathy (achalasia) . Arq Bras Cir Dig 34 : e1624 .
Vicentine FP , Herbella FA , Allaix ME , Silva LC , Patti MG , 2014 . Comparison of idiopathic achalasia and Chagas’ disease esophagopathy at the light of high-resolution manometry . Dis Esophagus 27 : 128 – 133 .
Vicentine FP , Herbella FA , Allaix ME , Silva LC , Patti MG , 2014 . High-resolution manometry classifications for idiopathic achalasia in patients with Chagas’ disease esophagopathy . J Gastrointest Surg 18 : 221 – 224, discussion 224–225 .
de Oliveira RB , Troncon LE , Dantas RO , Menghelli UG , 1998 . Gastrointestinal manifestations of Chagas’ disease . Am J Gastroenterol 93 : 884 .
Oliveira JA , Gharib AZGE , Dantas RO , 2021 . Dymptoms associated with different degrees of megaesophagus in Chagas disease . Arq Gastroenterol 58 : 491 – 494 .
Sánchez-Montalvá A , Moris M , Mego M , Salvador F , Accarino A , Ramírez K , Azpiroz F , Ruiz-de-Leon A , Molina I , 2016 . High resolution esophageal manometry in patients with Chagas disease: a cross-sectional evaluation . PLoS Negl Trop Dis 10 : e0004416 .
Pinazo MJ , Lacima G , Elizalde JI , Posada EJ , Gimeno F , Aldasoro E , Valls ME , Gascon J , 2014 . Characterization of digestive involvement in patients with chronic T. cruzi infection in Barcelona, Spain . PLoS Negl Trop Dis 8 : e3105 .
Vitton V , Andrianjafy C , Luciano L , Gonzalez JM , Padovani L , 2021 . Radio-induced esophageal motility disorders: an unrecognized diagnosis . Cancer Radiother 25 : 249 – 253 .
Chan TY , Tan PW , Tang JI , 2017 . Intensity-modulated radiation therapy for early-stage breast cancer: is it ready for prime time? Breast Cancer (Dove Med Press) 9 : 177 – 183 .
Mészáros N , Major T , Stelczer G , Jánváry L , Zaka Z , Pukancsik D , Takácsi-Nagy Z , Md JF , Polgár C , 2020 . Accelerated partial breast irradiation with 3-dimensional conformal and image-guided intensity-modulated radiotherapy following breast conserving surgery—7-year results of a phase II trial . Breast 54 : 222 – 228 .
Nagai A , Shibamoto Y , Yoshida M , Inoda K , Kikuchi Y , 2017 . Intensity-modulated radiotherapy using two static ports of tomotherapy for breast cancer after conservative surgery: dosimetric comparison with other treatment methods and 3-year clinical results . J Radiat Res (Tokyo) 58 : 529 – 536 .
Related Content
Tacaribe virus, a new agent isolated from artibeus bats and mosquitoes in trinidad, west indies, increase in size of entamoeba hartmanni trophozoites cultured on an enriched medium, two nosological forms of cutaneous leishmaniasis, experimental intrahepatic portal embolism induced by adult schistosoma mansoni, ethanol extracts of various helminths in a complement fixation test for eosinophilic lung (tropical eosinophilia).
%20CFA%20Deadline%20Proof%201.png)
- Previous Article
- Next Article
Case Report: Chagas Disease in a Traveler Who Developed Esophageal Involvement Decades after Acute Infection
- Download PDF
Travelers to Chagas disease endemic regions of Latin America may be at risk for Trypanosoma cruzi infection. We report a 67-year-old woman who screened positive for T. cruzi infection while donating blood. The patient had a history of an unusual febrile illness and marked swelling of the face sustained at age 10 after camping in northern Mexico that led to a 3-week hospitalization without a diagnosis. More than 4 decades later, rapid diagnostic tests and commercial and confirmatory serology for Chagas disease were all positive for T. cruzi infection. On evaluation, the patient described a progressive chronic cough, gastroesophageal reflux, and dysphagia for > 10 years. There was no evidence of any cardiac complications. However, esophageal manometry demonstrated significant dysmotility, with 90% of swallows being ineffective with evidence of esophageal pressurization and retrograde peristalsis in several swallows, suggesting early autonomic disruption due to Chagas disease esophagopathy. In this report, we highlight the importance of travel-related Chagas disease among travelers to endemic regions and the need to further identify potential risks of transmission among this at-risk population.
Chagas disease (CD) is a neglected tropical disease endemic in 21 Latin American countries throughout Central and South America. 1 Travelers who visit regions with high levels of endemic CD, especially with the active presence of vectors and oral transmission, could be exposed to Trypanosoma cruzi infection depending on their itinerary, purpose of travel, and activities, but very little is known about the actual risk among this population. According to the CDC’s Yellow Book 2020: Health Information for International Travel , the risk for CD is extremely low but increases if staying in poor-quality housing or ingesting food or drink products potentially contaminated with the parasite. 2 Travel-related CD has been reported in the United States, 3 Canada, 4 and certain European countries 5 but is considered a rare event. Domestic travelers within Latin America have also been found to be at risk for acquiring CD via travel-associated activities such as accidental oral consumption of the parasite. 6 We present a unique case of a traveler who developed CD with esophageal involvement decades after acute infection acquired while visiting a CD endemic region of Mexico. Transmission of CD among those visiting endemic regions is not well understood, and this report aims to bring further awareness of this risk among travelers.
A 67-year-old female with a past medical history of hypertension, hyperlipidemia, invasive ductal breast carcinoma with lumpectomy treated with aromatase inhibitor and localized intensity-modulated radiation therapy (IMRT) to the left breast (2016), left eye retinal detachment with partial blindness, gastroesophageal reflux disease (GERD), chronic dry cough, and progressive dysphagia presented to our infectious diseases clinic for evaluation of positive T. cruzi infection screening assays after routine blood donation in September 2020. She had never donated blood in the past. A complete review of systems revealed a > 10-year history of GERD with a progressively worsening dry cough that had led to coughing spells and subsequent left eye retinal detachment from extreme coughing. Investigations performed by several ear, nose, and throat specialists did not reveal the etiology of the cough, but it was thought to be from GERD. She began to develop difficulty swallowing liquids during the last 2 years along with transient sensations of food getting stuck in her esophagus. Proton-pump inhibitors and H 2 -blockers helped with reflux symptoms but had no effect on her dysphagia. She denied abdominal pain or bloating and normally had a bowel movement every 2 or 3 days, although she reported bouts of intermittent, chronic constipation (6 or more days between bowel movements) since childhood. Previous colonoscopy performed for routine surveillance of colorectal cancer was normal 2 years prior. She denied any heart palpitations, shortness of breath, substernal chest pain, lower extremity edema, irregular heartbeats, or central nervous system deficits.
The patient was born in Nashville, Tennessee and lived in a suburban setting most of her childhood and early adult life. Her mother was born in Tennessee. The patient has lived in north Florida for approximately the last 20 years in a semi-rural setting and is a retired elementary school teacher. She has not lived anywhere else in the United States. The patient denied blood transfusions in her lifetime and is not an organ donor recipient. She denied any known exposure to the triatomine vector (kissing bug) while living in Tennessee or Florida, after being shown several species of naturally occurring Triatoma preserved in resin and images from entomological keys. She did not recall ingestion of any uncooked or undercooked wild game meat and is not a hunter. She has never lived in Latin America but, after a detailed history, she described an acute febrile illness sustained at age 10 that occurred during a family camping trip in 1964. The camping trip took place in the state of Nuevo León in northern Mexico near the city of Monterrey. The family slept in pop-up tents and outdoors on the ground within a national park. She recalled being bitten by insects while camping and having welts on her body. While driving back to Tennessee, she developed high-grade fever and bilateral facial swelling. She was admitted to a university hospital in Nashville, Tennessee for 3 weeks and was treated with antibiotics. Eventually her condition improved, and the facial swelling slowly resolved. She was discharged home without a clear explanation of the etiology of her febrile illness. No other family members on the trip developed an illness. Hospital medical records from this event were not available from that time period.
On physical examination her vitals were normal. There were no abnormal findings in the oral cavity. Her lungs were clear to auscultation, and her heart rhythm was regular with normal S1 and S2 without murmur. Her abdomen was soft, nondistended, and with normal bowel sounds. Her lower extremities were without edema and the skin was without rashes. Cranial nerves were grossly intact, and no neurological deficits were noted. Rapid diagnostic testing to investigate for CD was performed in the clinic following each manufacturer’s instructions (Chagas Detect™ Plus; InBios International, Inc., Seattle, WA; DPP ® Chagas system; Chembio Diagnostic Systems, Inc., Hauppauge, NY) and was found to be reactive. Serum samples sent to two commercial reference laboratories (Weiner Chagatest ELISA recombinante v. 3.0, Quest Diagnostics laboratory, San Juan Capistrano, CA; Hemagen Chagas kit EIA, Associated Regional and University Pathologists laboratory, Salt Lake City, UT) were both reactive. Confirmatory serological testing performed at the CDC was positive for T. cruzi anti-IgG (Weiner Chagatest ELISA recombinante v. 3.0) and trypomastigote excretory-secretory antigen by immunoblot. Baseline complete blood counts and metabolic panel were within normal limits. HIV screening and Strongyloides stercoralis IgG were negative.
Further workup took place investigating both the cardiac and gastrointestinal organ systems. Chest X-ray, electrocardiogram, and transthoracic echocardiogram did not reveal any abnormalities. Cardiac magnetic resonance imaging was also performed and did not reveal any radiologic evidence of Chagasic cardiomyopathy. Esophagogastroduodenoscopy was unremarkable, with biopsies of the esophagus, stomach, and duodenum demonstrating only mild chronic gastritis with negative Helicobacter pylori testing. High-resolution esophageal manometry (HREM) revealed that 90% of swallows were ineffective, with 60% failed swallows and 30% weak swallows ( Figure 1 ). Although the esophagogastric junction (EGJ) demonstrated normal relaxation, the median integrated relaxation pressure (IRP) was in the upper limit of normal (12.6 mm Hg, normal < 15 mm Hg). The combination of 90% ineffective swallows with borderline normal median IRP was highly suggestive of an evolving achalasia or achalasia phenotype secondary to esophageal involvement of CD. Impedance analysis demonstrated complete bolus clearance in 60% of the swallows. Upper esophageal sphincter had normal tone, relaxation, and residual pressures. Multiple rapid swallow testing indicated a good peristaltic reserve, and the rapid drink challenge yielded complete EGJ/deglutitive inhibition.

Citation: The American Journal of Tropical Medicine and Hygiene 108, 3; 10.4269/ajtmh.22-0461
- Download Figure
- Download figure as PowerPoint slide
A diagnosis of ineffective esophageal motility (IEM) (based on Chicago classification version 4.0 © for high-resolution manometry 7 ), with some swallows showing esophageal pressurization and retrograde peristalsis, was made. Risks and benefits of antiparasitic treatment were discussed with the patient, who decided to undergo standard antitrypanosomal therapy and was treated with oral benznidazole (300 mg) daily divided into two separate doses for a total of 60 days. She tolerated the complete treatment and experienced fatigue, subjective low-grade fever, and headache that self-resolved after finishing the course. The patient did not develop any other systemic adverse effects such as urticarial rash. Weekly complete blood counts and metabolic panels were followed during treatment and yielded mild lymphocytic leukopenia (normal absolute lymphocyte count of 1.0–3.20 × 10 3 /μL; while on benznidazole therapy, the count was 0.36–0.97 × 10 3 /μL) and acute kidney injury (baseline creatinine was 0.9 mg/dL; while on benznidazole therapy, it was 1.09–1.37 mg/dL) that did not require cessation of benznidazole. These laboratory abnormalities self-resolved after the benznidazole treatment course. Approximately 6 months after completing treatment with oral benznidazole, the patient had not noticed any improvement in her dysphagia, but she also thinks that it has not worsened. The patient has been advised on dietary techniques and some restrictions for certain foods to avoid impaction. Other targeted treatments such as surgical intervention and possibly pharmacotherapy will be considered in the future if IEM progresses to achalasia. The patient is being followed up with infectious diseases and gastroenterology annually, including clinical monitoring of esophageal disease and possible colonic involvement.
The risks for CD among travelers residing in the United States after visiting endemic regions of Latin America have been described but are not well characterized. A traveler who spent 3 weeks in Puerto Viejo, Costa Rica developed acute infection 2 days after her trip. 3 She stayed in a cottage with wooden plank floors under a mosquito net, but a known exposure to the triatomine vector was not mentioned. She was found to have clear evidence of unilateral periorbital edema (Romaña’s sign), nonblanching rash, and one enlarged non-tender cervical lymph node. Her peripheral blood smear showed circulating T. cruzi trypomastigotes, and she was treated with the antitrypanosomal agent nifurtimox. Another case reported by the GeoSentinel network in a Canadian woman was described in 2008 after she visited rural regions of southern Mexico for 5 months. 4 In 2021, the U.S. Chagas Diagnostic Working Group provided recommendations for screening at-risk populations for CD. Travelers who have stayed in an endemic region with confirmed or suspected triatomine exposure (bite or being found within human dwelling), or have slept in a home constructed of mud, adobe, or a thatched roof, or consumed raw or unpasteurized foods/drinks that could be contaminated with T. cruzi can be considered for screening with a conditional recommendation based on low-quality evidence. 8 Travelers are advised to avoid ingesting certain fruit juices previously implicated in acute CD such as guava juice, bacaba, babaçu and palm wine, açai pulp, and raw sugar cane juice. 9
Our patient developed chronic CD with esophageal involvement ∼40 years after her acute infection while visiting rural regions of northern Mexico. The case is notable because the gastrointestinal involvement of CD is more commonly reported among those infected in the Southern Cone of South America, including regions within the Gran Chaco. 10 , 11 Certain T. cruzi discrete typing units (DTUs) are found in the Southern Cone and are known to cause gastrointestinal disease, including DTUs Tc II, Tc V, and Tc VI. 10 , 11 However, as demonstrated in this case and other cases from Mexico, gastrointestinal disease can be found in endemic regions where TcI is the dominant DTU causing human disease. 12 – 16 One seroprevalence study from the state of Puebla, Mexico revealed 16.9% ( n = 12/71) of those with CD had gastrointestinal symptoms, including 4 patients with esophageal manometry abnormalities. 15 Chagas disease esophagopathy (CDE) more commonly evolves into achalasia characterized by aperistalsis with EGJ outflow obstruction (abnormal median IRP). However, those with CDE often present with varying degrees of esophageal dysmotility seen on HREM, which is likely related to the evolution of autonomic dysregulation seen in CDE. 16 – 21 One investigation of 62 patients confirmed with chronic CD living in Spain found that 22.6% ( n = 14/62) had pathologic HREM findings consistent with CDE prior to antitrypanosomal treatment. 22 Most ( n = 13/14) were diagnosed with IEM, and 1 patient was diagnosed with fragmented peristalsis. 22 Another study in Spain revealed that 8.8% ( n = 6/67) with chronic CD had IEM after esophageal manometric testing. 23 Dysphagia is the most common and first symptom seen in CDE but may not always correlate to the degree of megaesophagus seen radiologically. 17 – 23 Regurgitation, weight loss, dyspepsia, increased thirst, chest discomfort, and cough are all associated symptoms of CDE, so a thorough review of symptoms should be undertaken in all those with serological evidence of CD. 17 – 23 One limitation of this case report is that our patient did receive a short course (6 weeks; ≈50 Gy) of IMRT for 0.4-cm invasive ductal carcinoma (TIaN0M0) in 2016 after lumpectomy. She did not experience acute radiation-induced esophagitis during this treatment or receive concomitant chemotherapy, which has been described in those who develop late-onset esophageal toxicity. 24 Limited data exist (if any) with regard to HREM findings and those with a previous history of localized IMRT to a single breast. 24 IMRT is a specialized technique that uses small photon and proton beams to precisely deliver radiation to the tumor or lumpectomy cavity to avoid or reduce exposure to surrounding tissues. 25 Late complications of IMRT are typically described locally in the breast and do not extend into deeper tissues found in the thorax. 25 – 27 Because late complications in the esophagus after receiving IMRT have not been reported, and her symptoms had already started prior to her diagnosis of left breast cancer, we think that the current clinical presentation supports CD with esophageal involvement.
In conclusion, CD among those traveling to endemic regions is likely a rare event. Our case highlights the importance of keeping CD in the differential diagnosis for travelers who may be manifesting clinical evidence of chronic disease, even decades after their return.
We thank our patient for her consent and participation in this case report. The Drugs for Neglected Diseases initiative (DNDi) is grateful to its donors, public and private, who have provided funding to DNDi since its inception in 2003. A full list of DNDi’s donors can be found at http://www.dndi.org/donors/donors/ . We also thank Susan Montgomery and the Parasitic Diseases Branch laboratory at the CDC for support and assistance with CD confirmatory serological testing.
Author Notes
Financial Support: Funding for rapid diagnostic tests was provided in part by a grant from the Mundo Sano Foundation (AWD08818). The study of the rapid diagnostic tests was conducted according to the guidelines of the Declaration of Helsinki, and approved by the University of Florida Institutional Review Board (IRB201903417) on August 29, 2020.
Authors’ addresses: Norman L. Beatty, Rodrigo F. Alcala, and Nelson A. Luque, Division of Infectious Diseases and Global Medicine, University of Florida College of Medicine, Gainesville, FL, E-mails: [email protected] , [email protected] , and [email protected] . Mark Radetic, Priti Joshi-Guske, and Eyad Alakrad, Division of Gastroenterology, Hepatology & Nutrition, Department of Medicine, University of Florida College of Medicine, Gainesville, FL, E-mails: [email protected] , [email protected] , and [email protected] . Colin J. Forsyth, Drugs for Neglected Diseases Initiative, New York, NY, E-mail: [email protected] . Davidson H. Hamer, Boston University Schools of Public Health and Medicine, Boston, MA, E-mail: [email protected] .
American Journal of Tropical Medicine and Hygiene
241 18th Street South, Suite 501
Arlington, VA 22202 USA
© 2022 The American Journal of Tropical Medicine and Hygiene
Access brought to you by:
Powered by: PubFactory
- [66.249.64.20|81.177.182.159]
- 81.177.182.159
Character limit 500 /500
Official websites use .gov
A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
Travel-Related Diagnoses Among U.S. Nonmigrant Travelers or Migrants Presenting to U.S. GeoSentinel Sites — GeoSentinel Network, 2012–2021
Surveillance Summaries / June 30, 2023 / 72(7);1–22
Please note: This report has been corrected. An erratum has been published.
Ashley B. Brown, MPH 1 ; Charles Miller, MSOR 1 ; Davidson H. Hamer, MD 2 ,3 ; Phyllis Kozarsky, MD 4 ; Michael Libman, MD 5 ; Ralph Huits, MD, PhD 6 ; Aisha Rizwan, MPH 7 ; Hannah Emetulu, MPH 7 ; Jesse Waggoner, MD 8 ; Lin H. Chen, MD 9 ,10 ; Daniel T. Leung, MD 11 ; Daniel Bourque, MD 3 ; Bradley A. Connor, MD 12 ; Carmelo Licitra, MD 13 ; Kristina M. Angelo, DO 1 ( View author affiliations )
Views: Views equals page views plus PDF downloads
Introduction, selected worldwide health event notifications, selected health event notifications in geosentinel, limitations, future directions, acknowledgments.
- Full Issue PDF
Problem/Condition: During 2012–2021, the volume of international travel reached record highs and lows. This period also was marked by the emergence or large outbreaks of multiple infectious diseases (e.g., Zika virus, yellow fever, and COVID-19). Over time, the growing ease and increased frequency of travel has resulted in the unprecedented global spread of infectious diseases. Detecting infectious diseases and other diagnoses among travelers can serve as sentinel surveillance for new or emerging pathogens and provide information to improve case identification, clinical management, and public health prevention and response.
Reporting Period: 2012–2021.
Description of System: Established in 1995, the GeoSentinel Network (GeoSentinel), a collaboration between CDC and the International Society of Travel Medicine, is a global, clinical-care–based surveillance and research network of travel and tropical medicine sites that monitors infectious diseases and other adverse health events that affect international travelers. GeoSentinel comprises 71 sites in 29 countries where clinicians diagnose illnesses and collect demographic, clinical, and travel-related information about diseases and illnesses acquired during travel using a standardized report form. Data are collected electronically via a secure CDC database, and daily reports are generated for assistance in detecting sentinel events (i.e., unusual patterns or clusters of disease). GeoSentinel sites collaborate to report disease or population-specific findings through retrospective database analyses and the collection of supplemental data to fill specific knowledge gaps. GeoSentinel also serves as a communications network by using internal notifications, ProMed alerts, and peer-reviewed publications to alert clinicians and public health professionals about global outbreaks and events that might affect travelers. This report summarizes data from 20 U.S. GeoSentinel sites and reports on the detection of three worldwide events that demonstrate GeoSentinel’s notification capability.
Results: During 2012–2021, data were collected by all GeoSentinel sites on approximately 200,000 patients who had approximately 244,000 confirmed or probable travel-related diagnoses. Twenty GeoSentinel sites from the United States contributed records during the 10-year surveillance period, submitting data on 18,336 patients, of which 17,389 lived in the United States and were evaluated by a clinician at a U.S. site after travel. Of those patients, 7,530 (43.3%) were recent migrants to the United States, and 9,859 (56.7%) were returning nonmigrant travelers.
Among the recent migrants to the United States, the median age was 28.5 years (range = <19 years to 93 years); 47.3% were female, and 6.0% were U.S. citizens. A majority (89.8%) were seen as outpatients, and among 4,672 migrants with information available, 4,148 (88.8%) did not receive pretravel health information. Of 13,986 diagnoses among migrants, the most frequent were vitamin D deficiency (20.2%), Blastocystis (10.9%), and latent tuberculosis (10.3%). Malaria was diagnosed in 54 (<1%) migrants. Of the 26 migrants diagnosed with malaria for whom pretravel information was known, 88.5% did not receive pretravel health information. Before November 16, 2018, patients’ reasons for travel, exposure country, and exposure region were not linked to an individual diagnosis. Thus, results of these data from January 1, 2012, to November 15, 2018 (early period), and from November 16, 2018, to December 31, 2021 (later period), are reported separately. During the early and later periods, the most frequent regions of exposure were Sub-Saharan Africa (22.7% and 26.2%, respectively), the Caribbean (21.3% and 8.4%, respectively), Central America (13.4% and 27.6%, respectively), and South East Asia (13.1% and 16.9%, respectively). Migrants with diagnosed malaria were most frequently exposed in Sub-Saharan Africa (89.3% and 100%, respectively).
Among nonmigrant travelers returning to the United States, the median age was 37 years (range = <19 years to 96 years); 55.7% were female, 75.3% were born in the United States, and 89.4% were U.S. citizens. A majority (90.6%) were seen as outpatients, and of 8,967 nonmigrant travelers with available information, 5,878 (65.6%) did not receive pretravel health information. Of 11,987 diagnoses, the most frequent were related to the gastrointestinal system (5,173; 43.2%). The most frequent diagnoses among nonmigrant travelers were acute diarrhea (16.9%), viral syndrome (4.9%), and irritable bowel syndrome (4.1%).
Malaria was diagnosed in 421 (3.5%) nonmigrant travelers. During the early (January 1, 2012, to November 15, 2018) and later (November 16, 2018, to December 31, 2021) periods, the most frequent reasons for travel among nonmigrant travelers were tourism (44.8% and 53.6%, respectively), travelers visiting friends and relatives (VFRs) (22.0% and 21.4%, respectively), business (13.4% and 12.3%, respectively), and missionary or humanitarian aid (13.1% and 6.2%, respectively). The most frequent regions of exposure for any diagnosis among nonmigrant travelers during the early and later period were Central America (19.2% and 17.3%, respectively), Sub-Saharan Africa (17.7% and 25.5%, respectively), the Caribbean (13.0% and 10.9%, respectively), and South East Asia (10.4% and 11.2%, respectively).
Nonmigrant travelers who had malaria diagnosed were most frequently exposed in Sub-Saharan Africa (88.6% and 95.9% during the early and later period, respectively) and VFRs (70.3% and 57.9%, respectively). Among VFRs with malaria, a majority did not receive pretravel health information (70.2% and 83.3%, respectively) or take malaria chemoprophylaxis (88.3% and 100%, respectively).
Interpretation: Among ill U.S. travelers evaluated at U.S. GeoSentinel sites after travel, the majority were nonmigrant travelers who most frequently received a gastrointestinal disease diagnosis, implying that persons from the United States traveling internationally might be exposed to contaminated food and water. Migrants most frequently received diagnoses of conditions such as vitamin D deficiency and latent tuberculosis, which might result from adverse circumstances before and during migration (e.g., malnutrition and food insecurity, limited access to adequate sanitation and hygiene, and crowded housing,). Malaria was diagnosed in both migrants and nonmigrant travelers, and only a limited number reported taking malaria chemoprophylaxis, which might be attributed to both barriers to acquiring pretravel health care (especially for VFRs) and lack of prevention practices (e.g., insect repellant use) during travel. The number of ill travelers evaluated by U.S. GeoSentinel sites after travel decreased in 2020 and 2021 compared with previous years because of the COVID-19 pandemic and associated travel restrictions. GeoSentinel detected limited cases of COVID-19 and did not detect any sentinel cases early in the pandemic because of the lack of global diagnostic testing capacity.
Public Health Action: The findings in this report describe the scope of health-related conditions that migrants and returning nonmigrant travelers to the United States acquired, illustrating risk for acquiring illnesses during travel. In addition, certain travelers do not seek pretravel health care, even when traveling to areas in which high-risk, preventable diseases are endemic. Health care professionals can aid international travelers by providing evaluations and destination-specific advice.
Health care professionals should both foster trust and enhance pretravel prevention messaging for VFRs, a group known to have a higher incidence of serious diseases after travel (e.g., malaria and enteric fever). Health care professionals should continue to advocate for medical care in underserved populations (e.g., VFRs and migrants) to prevent disease progression, reactivation, and potential spread to and within vulnerable populations. Because both travel and infectious diseases evolve, public health professionals should explore ways to enhance the detection of emerging diseases that might not be captured by current surveillance systems that are not site based.
Modern modes of transportation and growing economies have made traveling more efficient and accessible. This progress has resulted in a surge of international travel, including travel to remote destinations and lower-income countries ( 1 ). In 2019, a record 2.4 billion international tourist arrivals globally ( 2 ) were observed by the World Tourism Organization.
Four studies estimated that 43%–79% of travelers to low- and middle-income countries became ill with a travel-related health problem, some of whom needed medical care during or after travel ( 3 ). Certain groups (e.g., travelers visiting friends and relatives [VFRs] and migrants) are particularly at risk for acquiring travel-related diseases because of a lack of risk awareness, access to specialized health care and pretravel consultation, and trust in the health care system ( 4 , 5 ). In addition, travelers might introduce pathogens into new environments and populations, leading to the spread of novel and emerging infectious diseases ( 6 ). The 2019 measles outbreaks across Europe illustrated how travel and poor vaccination coverage among local populations can fuel an epidemic ( 7 ). These outbreaks resulted in the importation of measles to communities with low vaccination coverage in the United States, a country that had eliminated measles in 2000. The rapid spread of disease across international borders also was observed during the Ebola virus disease epidemic in West Africa during 2014–2016 ( 8 ) as well as during the COVID-19 pandemic ( 9 ). These events illustrate the dangers of introducing pathogens into geographic clusters of susceptible populations as well as the importance of vaccination and other preventative strategies to reduce the risk for importation and spread.
Studying illness among travelers improves case identification, clinical management, and public health prevention strategies and also helps to characterize the epidemiology of diseases and control their spread ( 10 ). Because international travel continues to increase, conducting surveillance and research regarding travel-related diseases will be instrumental in reducing global transmission. To identify travel-related diseases and facilitate rapid communication between clinicians and public health professionals globally, a surveillance system (e.g., GeoSentinel) is needed. Such connectivity can reduce the size of outbreaks while promoting the timely sharing of clinical insight regarding the diagnosis and treatment of patients.
The GeoSentinel Network (GeoSentinel) is a global, clinical-care–based surveillance and research network of travel and tropical medicine sites that monitors infectious diseases and other adverse health events that affect international travelers ( https://geosentinel.org/ ). Since its inception in 1995, GeoSentinel has remained at the forefront of travel-related sentinel surveillance and continues to refine its collection of epidemiologic data from ill travelers during and after travel.
This report describes GeoSentinel, key changes in its data collection, its successful detection of sentinel events, and future directions. This report also summarizes the data collected from migrants and returning U.S. nonmigrant travelers presenting for evaluation at a U.S. GeoSentinel site during 2012–2021. The findings in this report underscore the importance of global travel-related disease surveillance so that clinicians and public health professionals are aware of the most common travel-related illnesses and can develop improved treatment and prevention strategies.
The GeoSentinel Network
GeoSentinel is a collaboration between CDC and the International Society of Travel Medicine (ISTM) and was established in the United States in 1995 with nine U.S. sites ( 11 ). During 1996–1997, the GeoSentinel network expanded globally. GeoSentinel’s primary purpose is to coordinate multiple clinical-care–based sites that operate a global, provider-based emerging infections sentinel network, conduct surveillance for travel-related infections, and communicate and help guide public health responses ( 12 ). Sites collaborate to report disease or population-specific findings through retrospective database analyses and the collection of supplemental data to fill specific knowledge gaps.
Sites and Affiliate Members
As of December 2021, GeoSentinel comprised 71 sites in 29 countries located on six continents ( Figure 1 ). GeoSentinel sites are health care facilities led by site directors and codirectors who are medical professionals with expertise in travel and tropical medicine. GeoSentinel also includes 164 affiliate members (formerly referred to as network members) who report sentinel or unusual travel medicine cases but do not enter data into the GeoSentinel database.
Eligible Patients
Patient data can be entered into the GeoSentinel database if the patient has crossed an international border and was seen at a GeoSentinel site with a possible travel-related illness or, in the case of certain migrants, for screening purposes upon entry into their arrival country. Data from patients who develop a complication from pretravel treatments (i.e., adverse effect from vaccinations or antimalarial medication) also might be entered, even if the patients have not yet departed on their trip.
Data Collection
GeoSentinel sites use a standardized data collection form (Supplementary Appendix, https://stacks.cdc.gov/view/cdc/127681 ) to collect demographic, clinical, and travel-related information about patients and the illnesses acquired during travel. These data are collected electronically via a secure web-based data entry application based at CDC. Daily reports are generated for assistance in detecting events (i.e., unusual patterns or clusters of disease). The system emails these reports to both CDC and ISTM partners for review. If an unusual disease pattern or cluster of disease is detected, the GeoSentinel program manager sends an email to the site requesting additional information. Electronic validation is integrated into the database to reduce data entry errors and maintain data integrity. Whereas certain sites enter all travel-related cases into the GeoSentinel database, other sites only enter a convenience sample. Entry of cases into the GeoSentinel database and determination of travel association are at the discretion of the treating clinician. This activity was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy.* Ethics clearance has been obtained by sites as required by their respective institutions.
Selected Variables and Definitions
The GeoSentinel database contains information obtained from patients evaluated at GeoSentinel sites during and after international travel. The following definitions were used during the study period.
Citizen. A person who is a legally recognized national of a country.
Clinical setting. The timing of the visit related to travel.
- During travel. The trip related to the current illness is in progress. This category includes expatriates seen in their country of residence for illnesses likely acquired in that country or where the country of exposure cannot be ascertained.
- After travel. The trip related to the current illness has been completed. This category also includes expatriates who acquire an illness during travel outside their current country of residence and where the relevant exposure is related to travel.
Diagnosis and diagnosis type. Site directors choose from approximately 475 diagnoses classified as either etiologic or syndromic. A write-in option is available on the data collection form if the diagnosis is not on the list.
- Etiologic. This diagnosis type reflects a specific disease. The “diagnosis status” of etiologic diagnoses might be “confirmed” or “probable” (see Diagnosis status).
- Syndromic. This diagnosis type reflects symptom- or syndrome-based etiologies when a more specific etiology is not known or could not be determined as a result of use of empiric therapy, self-limited disease, or inability to justify additional diagnostic tests beyond standard clinical practice. The “diagnosis status” of all syndromic diagnoses is “confirmed” (see Diagnosis status).
Diagnosis status . The diagnosis is categorized in one of two ways on the basis of available diagnostic methods:
- Confirmed. The diagnosis has been made by an indisputable clinical finding (e.g., removal of larvae of tungiasis) or diagnostic test.
- Probable. The diagnosis is supported by evidence (including diagnostic testing) strong enough to establish presumption but not proof.
Expatriate. A person living in a destination with an independent residence and address and using the same infrastructure as local residents of the same economic class. Expatriates intend to remain in-country for ≥6 months and have no intention to legally change their citizenship or permanent residency status.
Main symptoms. The symptoms associated with the illness that was the reason for the clinic visit.
Migrant. A person who, at some time in their life, has emigrated from their country of birth and has previously or intends to legally change their citizenship or permanent residency status. The resident country is entered on the data collection form as the new home country.
Nonmigrant traveler. A person who is traveling for a purpose unrelated to migration.
Pretravel encounter. Any pretravel health visit or the receipt of travel-related health information.
Resident. A person who has their primary residence in a particular country.
Severity. The highest level of clinical care received for the travel-related diagnosis, including outpatient, inpatient ward, and inpatient intensive care unit (ICU) care.
Syndrome or system groupings of diagnoses. All GeoSentinel diagnoses are categorized into groups according to the type of syndrome or system affected ( Box 1 ).
Travel reason. Primary reason for travel related to the current illness ( Box 2 ).
Travel related. Designates the relation of the main diagnosis to the patient’s travel.
- Travel related. Used when the illness under evaluation, initially suspected to be travel-related, was determined to have been acquired during the patient’s travel.
- Imported infection. Used for infections acquired in the patient’s country of residence if exported to another country and then evaluated at a GeoSentinel site.
- Not travel related. Used when the illness under evaluation, initially suspected to be travel related, was determined to have been acquired before departure from or after returning to the home country.
- Not ascertainable . Used when the illness under evaluation, initially suspected to be travel related, was equally likely to have been acquired during the patient’s travel or before departing from or after returning to the residence country.
Changes to GeoSentinel Data Collection
During 2012–2021, multiple changes were made to the GeoSentinel data entry application ( Box 3 ). New fields and subfields that collect detailed information on patient types, diagnoses, and trip information were added to provide a complete profile of patients and their associated illnesses. Additional fields were added for diseases of interest to provide information (e.g., vaccination status, etiology [e.g., organism genus and species], and cause of death). Case definitions were developed for each diagnosis code, and data collection fields were refined on an ongoing basis to aid clinicians in classifying patients and diagnoses.
Internal validation is now used to ensure that data are collected uniformly and accurately among sites. The collection of diagnostic methods allows for validation of confirmed and probable cases, and quality assurance (QA) alerts prevent sites from classifying diagnoses as confirmed during data entry without required disease-specific diagnostic methods. Other QA alerts prevent the skipping of required fields as well as logical errors.
Before November 16, 2018, the variables of travel reason and exposure country (and region) were not linked to an individual diagnosis. Instances where patients had multiple unrelated diagnoses made it difficult to ascertain what information applied to which diagnosis. As a result, the data collection form and database were updated to specify travel reason and exposure country information for each individual diagnosis.
To fill knowledge gaps, enhanced surveillance projects were deployed throughout the analysis period to collect specific information about a disease or types of travelers that was not collected on the core data collection form. This included projects on antibiotic resistance for selected bacterial pathogens, rickettsioses, mass gatherings ( 13 ), rabies postexposure prophylaxis ( 14 ), planned and unplanned health care abroad ( 15 ), migrants ( 16 ), and respiratory illnesses related to COVID-19.
This report includes GeoSentinel data limited to unique patients with ≥1 confirmed or probable travel-related diagnosis who were evaluated after migration or travel at a GeoSentinel site in the United States during 2012–2021. Each patient might have multiple diagnoses. Patients must have been residents of the United States and evaluated after travel and within 10 years of migrating or returning from a trip outside of the United States. Only migrants with illnesses associated with their migration to the United States were included. The validity of diagnoses was verified by an infectious disease specialist using the diagnostic methods recorded by the sites. Descriptive analyses were performed on data from the 20 GeoSentinel sites in the United States ( Figure 2 ) with patients who met inclusion criteria. Frequencies were calculated on patient demographics (e.g., sex, age, country of birth, citizenship, and residence), travel-related information (e.g., reason for travel and country or region of exposure), diagnosis, diagnostic methods, year of illness onset, and severity of illness. Because of changes in the collection of travel-related information, a subanalysis was done on travel-related information before and after November 16, 2018. This information is reported separately. Geographic regions of exposure are classified based on modified UNICEF groupings ( https://data.unicef.org/regionalclassifications/ ). Data were managed using Microsoft Access (version 2208; Microsoft Corporation), and all analyses were performed using SAS (version 9.4; SAS Institute).
To demonstrate GeoSentinel’s ability to identify sentinel events and emerging disease patterns, three examples (i.e., dengue in Angola [2013], Zika in Costa Rica [2016], and yellow fever in Brazil [2018]) of emerging sentinel health threats that occurred during 2012–2021 are described. These health events were not limited to residents of the United States who were evaluated after travel and ≤10 years of migrating or returning from a trip outside of the United States. Therefore, these patients could be residents of any country and were seen at GeoSentinel sites both inside and outside of the United States.
During 2012–2021, a total of 198,120 unique patients were evaluated at GeoSentinel sites globally and included in GeoSentinel’s database ( Figure 3 ). Of these, 177,703 patients received at least one confirmed or probable travel-related diagnosis, of which 18,336 were reported from 20 GeoSentinel sites in the United States. Of the 17,538 patients evaluated by a clinician after travel, 17,389 were migrants or returning U.S. nonmigrant travelers to the United States, accounting for 25,973 travel-related diagnoses. The remaining 149 patients were non-U.S. residents and were excluded from the analysis. The results of migrants and returning nonmigrant travelers are reported separately.
Patient Demographics
Of the 17,389 patients who were included in this analysis, 7,530 (43.3%) were recent migrants to the United States; <1% of patients were expatriates. Of 7,527 migrants, 47.4% were female ( Table 1 ). The median age was 28.5 years (range = <19 years to 93 years), and the largest proportion of migrants was aged 19–39 years (35.9%). Of 4,672 patients with information available, 88.8% did not receive pretravel health information. Of 2,867 patients with information available on severity, a majority (89.8%) were seen as outpatients, 9.7% were seen in an inpatient ward, and <1% were seen in an ICU.
Of the 13,986 travel-related diagnoses among migrants, the most frequent were vitamin D deficiency (20.2%), Blastocystis (10.9%), latent tuberculosis (10.3%), strongyloidiasis (6.7%), and eosinophilia (5.8%) ( Table 2 ). A total of 43% of diagnoses fell into eight infectious or travel-related syndrome groupings including “other” (18.7%), gastrointestinal (15.7%), dermatological (2.0%), neurologic (1.9%), genitourinary (1.6%), febrile (1.5%), respiratory (1.5%), and musculoskeletal (<1%). No deaths or animal bites or scratches were reported ( Table 3 ).
Of the 2,614 diagnoses in the “other” grouping (Table 3), the most frequent were latent tuberculosis (55.2%), eosinophilia (30.8%), Chagas disease (3.8%), posttraumatic stress disorder (3.6%), and depression (2.9%). Of the 2,202 diagnoses in the gastrointestinal grouping, the most frequent were simple intestinal strongyloidiasis (41.6%), giardiasis (18.9%), Helicobacter pylori infection (8.4%), dientamoebiasis (6.9%), and schistosomiasis (6.5%). Of the 275 diagnoses in the dermatological grouping, the most frequent were fungal infection (42.6%), insect bite/sting (10.9%), rash of unknown etiology (10.2%), cutaneous leishmaniasis (5.8%), and leprosy (4.4%). Of the 263 diagnoses in the neurologic grouping, the most frequent were neurocysticercosis (76.8%), headache (16.4%), ataxia (1.5%), central nervous system tuberculosis (1.5%), and tuberculosis meningitis (1.1%). Of the 229 diagnoses in the genitourinary grouping, the most frequent were schistosomiasis (27.5%), chlamydia (15.3%), syphilis (11.4%), urinary tract infection (10.9%), and HIV (10.0%).
Among the 212 diagnoses in the febrile grouping (Table 3), the most frequent were malaria (25.5%), other extrapulmonary tuberculosis (13.2%), toxoplasmosis (8.0%), tuberculosis lymphadenitis (6.6%), and disseminated tuberculosis (5.2%). Malaria was diagnosed in 54 (<1%) migrants, and 88.5% did not receive pretravel health information (information available for 26 migrants). Of all species of malaria, Plasmodium falciparum was diagnosed most frequently (77.4%).
Among the 204 diagnoses in the respiratory grouping (Table 3), the most frequent was pulmonary tuberculosis (70.6%), which accounted for 68.9% of all active tuberculosis diagnoses; only 1% of migrants received a diagnosis of active tuberculosis disease. The remaining frequent diagnoses in the respiratory grouping were acute otitis media (4.9%), atypical pneumonia (3.4%), otitis externa (2.9%), and unspecified lobar pneumonia (2.9%). Of the 131 diagnoses in the musculoskeletal grouping, the most frequent were arthralgia (48.1%), trauma or injury (43.5%), osteomyelitis (1.5%), knee pain (1.5%), and sprain (1.5%).
Diagnostic Characteristics Before November 16, 2018
Among the 2,892 diagnoses with information available ( Table 4 ), the five most frequent regions of exposure were Sub-Saharan Africa (22.7%), the Caribbean (21.3%), Central America (13.4%), South East Asia (13.1%), and South Central Asia (9.2%). Among the 2,554 diagnoses with information available, the most frequent countries of exposure were Dominican Republic (7.9%), Thailand (6.5%), Haiti (6.2%), Ecuador (4.8%), and Myanmar (4.3%). Of 46 migrants with a malaria diagnosis, 89.3% were exposed in Sub-Saharan Africa (information available for 28 migrants).
Diagnostic Characteristics After November 16, 2018
Among the 2,012 diagnoses with information available (Table 4), the five most frequent regions of exposure were Central America (27.6%), Sub-Saharan Africa (26.2%), South East Asia (16.9%), the Caribbean (8.4%), and South America (7.0%). Among the 1,575 diagnoses with information available, the most frequent countries of exposure were El Salvador (11.2%), Thailand (10.7%), Honduras (9.1%), Guatemala (7.6%), and Dominican Republic (5.9%). Of seven migrants with a malaria diagnosis, all were exposed in Sub-Saharan Africa (information available for seven migrants).

Returning Nonmigrant Travelers
Among the 9,859 nonmigrant travelers returning to the United States, 55.7% were female and 75.3% were born in the United States. The median age was 37 years (range = <19 years to 96 years), and the largest proportion of nonmigrant travelers was aged 19–39 years (44.1%). Among the 8,967 patients with information available, 65.6% did not receive pretravel health information. Among the 5,884 patients with information available on severity, a majority (90.6%) were seen as outpatients, 8.4% were seen in an inpatient ward, and <1% were seen in an ICU. Approximately 1% of patients were expatriates, and 89.4% were U.S. citizens.
Of the 11,987 travel-related diagnoses of returning U.S. nonmigrant travelers (Table 3), 90.7% of diagnoses fell into nine infectious or travel-related syndrome groupings, including gastrointestinal (43.2%), febrile (16.7%), respiratory (13.0%), dermatological (8.9%), “other” (4.1%), animal bites or scratches (1.3%), genitourinary (1.4%), musculoskeletal (1.2%), and neurologic (<1%). The most frequent diagnoses (Table 2) were acute diarrhea (16.9%), viral syndrome (4.9%), irritable bowel syndrome (4.1%), campylobacteriosis (3.1%), and malaria (3.5%). Four deaths were reported, of which two were patients who received a diagnosis of severe P. falciparum malaria. Of the remaining two patients, one received a diagnosis of COVID-19 and the other received a diagnosis of acute unspecified hepatitis with renal failure.
Among the 5,173 diagnoses in the gastrointestinal grouping (Table 3), the most frequent were acute diarrhea (39.3%), irritable bowel syndrome (9.5%), campylobacteriosis (7.2%), giardiasis (5.5%), and chronic diarrhea (5.2%). Among the 2,001 diagnoses in the febrile grouping, the most frequent were viral syndrome (29.0%), malaria (21.0%), dengue (13.7%), chikungunya (6.4%), and unspecified febrile illness (5.0%). Among the 421 nonmigrant travelers with malaria of any species diagnosed, 80.8% had P. falciparum .
Among the 1,554 diagnoses in the respiratory grouping (Table 3), the most frequent were influenza-like illness (16.5%), upper respiratory tract infection (14.9%), acute bronchitis (11.9%), acute sinusitis (9.1%), and unspecified lobar pneumonia (8.4%). Among the 1,071 diagnoses in the dermatological grouping, the most frequent were insect or arthropod bite or sting (31.3%), rash of unknown etiology (8.8%), dermatitis (7.9%), skin and soft tissue infection (e.g., erysipelas, cellulitis, or gangrene [7.4%]), and superficial skin and soft tissue infection (6.0%). Among the 487 diagnoses in the “other” grouping, the most frequent were dehydration (18.7%), jet lag (17.9%), eosinophilia (11.7%), latent tuberculosis (8.8%), and anxiety disorder (7.6%).
Among the 173 diagnoses in the genitourinary grouping (Table 3), the most frequent were urinary tract infection (33.0%), schistosomiasis (11.6%), gonorrhea (9.3%), pyelonephritis (8.7%), and genital chlamydia (8.1%). Among the 142 diagnoses in the musculoskeletal grouping, the most frequent were arthralgia (19.7%), fracture (17.6%), myalgia (10.6%), trauma or injury (9.9%), and contusion (7.8%). Among the 105 diagnoses in the neurologic grouping, the most frequent were headache (26.7%), vertigo (12.4%), acute mountain sickness (10.5%), neurocysticercosis (9.5%), and dizziness (8.6%). Among the 153 diagnoses of bites or scratches, the most frequent were dog bite (50.3%), monkey bite (18.3%), other animal bite (6.5%), monkey exposure (5.9%), and dog exposure (3.9%).
Among the 9,919 diagnoses, 6,518 had information regarding travel reason ( Table 5 ). The most frequent reasons for travel were tourism (44.8%), VFR (22.0%), and business (13.4%). Among the 6,296 diagnoses with information available, the five most frequent regions of exposure were Central America (19.2%), Sub-Saharan Africa (17.7%), the Caribbean (13.0%), South East Asia (10.4%), and South America (9.4%). Among 5,920 diagnoses with information available, the most frequent countries of exposure were Mexico (12.5%), India (7.2%), Dominican Republic (5.3%), China (3.3%), and Costa Rica (3.0%).
Of 300 nonmigrant travelers with malaria, 70.3% were VFRs (information available for 232 nonmigrant travelers), and 88.6% were exposed in Sub-Saharan Africa. Of 163 VFRs with malaria, 70.2% did not receive pretravel health information (information available for 141 nonmigrant travelers), and 88.3% did not take malaria chemoprophylaxis (information available for 103 nonmigrant travelers).
Information regarding travel reason and exposure region was available for all 2,068 diagnoses (Table 5). The most frequent reasons for travel were tourism (53.6%), VFR (21.4%), business (12.3%), and missionary (6.2%). The five most frequent regions of exposure were Sub-Saharan Africa (25.5%), Central America (17.3%), South East Asia (11.2%), the Caribbean (10.9%), and South Central Asia (9.0%). Among the 1,894 diagnoses with information available, the most frequent countries of exposure were Mexico (13.2%), India (5.0%), Dominican Republic (4.2%), Philippines (3.0%), and Ethiopia (3.0%).
Of 121 nonmigrant travelers with malaria, 57.9% were VFRs and 95.9% were exposed in Sub-Saharan Africa. Of 70 VFRs with malaria, 83.3% did not receive pretravel health information (information available for 54 nonmigrant travelers), and none took malaria chemoprophylaxis (information available for three nonmigrant travelers).
Dengue in Angola, 2013
During April–May 2013, GeoSentinel sites in Canada, France, Germany, Israel, and South Africa reported 10 cases of dengue among travelers returning from Luanda, Angola. All patients had classic symptoms of dengue that included headache and joint pain and recovered without complication. Although dengue is endemic in Angola, before 2013, the last outbreak occurred during the 1980s. In the decades that followed, little was known regarding the epidemiology of dengue in Angola because of poor surveillance ( 17 ).
Although six cases of dengue had been reported to the Ministry of Health of Angola by April 1, 2013, the GeoSentinel cases, in combination with other imported cases to Portugal, were among the first indications of a large-scale outbreak. By May 31, there were 517 suspected cases and one death reported; all but two cases were in Luanda province ( 18 ). The GeoSentinel cases in Angola demonstrated that data on travelers’ adverse health events can aid in the detection of outbreaks, offering insight into the epidemiology of infectious disease in countries with suboptimal surveillance and reporting.
Zika in Costa Rica, 2016
On January 26, 2016, a GeoSentinel site in Massachusetts diagnosed dengue in a returned U.S. traveler from Nosara, Costa Rica. The patient returned to the United States with fever, rash, conjunctivitis, arthralgia, and headache; the patient also reported multiple mosquito bites. The patient was referred to a GeoSentinel site where antibody tests for Zika and dengue viruses were conducted by CDC. Plaque reduction neutralization antibody testing confirmed a diagnosis of Zika ( 19 ).
Zika virus emerged in the western hemisphere during 2014–2016 when outbreaks were reported from certain countries in the Americas and Caribbean ( 20 ). This case was the first case of Zika reported from Costa Rica, illustrating the continual geographic spread of a high-consequence pathogen. The Massachusetts GeoSentinel site detected and reported this sentinel case, and it also sent a networkwide notification, alerting clinicians to the risk for Zika in Costa Rica, a popular travel destination with no previous evidence of underlying circulation. By August 2017, a total of 1,920 cases were reported in Costa Rica, mirroring the trends of other countries in the region.
Yellow Fever in Brazil, 2018
In January 2018, a GeoSentinel site in the Netherlands reported a case of yellow fever in a Dutch man aged 46 years with recent travel to São Paulo state, Brazil. He had signs and symptoms of diarrhea, fever, headache, myalgia, and vomiting. By March 15, 2018, four additional GeoSentinel sites reported cases of yellow fever among travelers returning from Brazil, including two deaths. These five cases accounted for one half of all cases reported among international travelers to Brazil during this time. All patients were unvaccinated travelers, many of whom visited Ilha Grande ( 21 ).
Although yellow fever is endemic in Brazil, during 2016–2017 and 2017–2018, a higher incidence does not, by itself, indicate geographic expansion ( 22 ). Cases detected by GeoSentinel in early 2018 were among the first reported in newly identified regions of risk, confirming travelers as sentinels in the expansion of the outbreak and highlighting the importance of yellow fever vaccination in recommended regions ( 21 ).
GeoSentinel is the only surveillance network that operates a global, provider-based emerging infections sentinel network to conduct surveillance for travel-related infections and communicates with public health and clinical partners ( 11 ). From its inception in 1995 to 2011 ( 11 ), efforts were made to increase the size of the network, modernize data collection, and introduce internal validation to improve the quality of the data collected. Since 2012, GeoSentinel has expanded to 71 sites on six continents and has generated approximately 70 peer-reviewed publications. GeoSentinel also has undergone numerous methodologic changes aimed to improve data collection, the validity of resulting conclusions, and the provision of public health recommendations.
GeoSentinel data have been instrumental in the detection of sentinel events, as demonstrated by, but not limited to, the detection of expanded geographic area of yellow fever in Brazil ( 21 ), a large outbreak of dengue in Angola ( 17 ), and the first case of Zika in Costa Rica ( 19 ). These examples illustrate GeoSentinel’s ability to both identify emerging pathogens and communicate findings with clinicians and public health professionals around the world.
The most frequent diagnoses among migrants described in this analysis (e.g., vitamin D deficiency and latent tuberculosis) have been described elsewhere ( 23 , 24 ). Vitamin D deficiency might be because of reduced sun exposure caused by skin-covering clothing as well as low dietary intake ( 23 ). Acquisition of strongyloidiasis and latent tuberculosis might be from crowding, malnutrition, exposure to unsafe food and water, inadequate sanitation, and limited access to health care ( 25 ). Multiple presentations of Mycobacterium tuberculosis (e.g., pulmonary, extrapulmonary, lymphadenitis, disseminated, CNS tuberculoma, and meningitis) also were reported among migrants, highlighting that health care professionals should maintain a high degree of suspicion for M. tuberculosis infection among ill patients whose routine bacterial cultures do not yield a pathogen. Because the United States has the largest population of migrants in the world ( 26 ), health care professionals should continue to advocate for medical care for this underserved population, with the aim to prevent disease reactivation and subsequent spread to and within vulnerable populations.
Gastrointestinal illnesses remain a frequent cause of illness among travelers ( 27 ). In this analysis, acute diarrhea was the most frequent illness among nonmigrant travelers, accounting for 16.9% of their diagnoses. Previous studies have reported attack rates for acute diarrhea among travelers ranging from 30%–70%, most often caused by bacterial pathogens and transmitted because of poor hygiene practices in local restaurants ( 28 ). In other studies, travelers have reported not adhering to prevention practices and drinking unsafe tap water, consuming drinks with ice, eating salads, and consuming unpasteurized dairy products while abroad ( 29 ). Most acute diarrhea cases reported to GeoSentinel were of unknown etiology, illustrating the lack of use of specialized diagnostic tests or culture to determine the cause of diarrhea ( 30 ), despite the widespread availability of multiplex polymerase chain reaction tests for gastrointestinal pathogens ( 31 ), likely because the majority of cases of acute diarrhea resolve without the need for intervention ( 32 ).
Febrile illnesses were another frequent cause of illness among nonmigrant travelers in this analysis, of which viral syndromes and P. falciparum malaria were most frequent. Of nonmigrant travelers with malaria, a majority were exposed in Sub-Saharan Africa; the majority were VFRs, who infrequently received pretravel health advice or took malaria chemoprophylaxis. Inadequate pretravel preparation practices place VFRs at high risk for acquiring malaria during travel. Studies of African VFR travelers indicated they might not be able to afford health care visits, might feel unable to advocate for themselves in a health care setting, and might be culturally opposed to malaria chemoprophylaxis or other preventive measures (e.g., use of bed nets) because of concerns about offending their hosts or a low perception of risk ( 33 , 34 ). CDC recommends that all travelers going to an area where malaria is endemic take chemoprophylaxis before and during travel ( 35 ), but special considerations (e.g., improving accessibility or improving trust in the U.S. health care system) could be prioritized to ensure that VFRs are protected from malaria ( 33 , 36 ).
COVID-19 Pandemic
During 2020–2021, the number of patients presenting at U.S. GeoSentinel sites substantially decreased, mirroring worldwide declines in travel because of the COVID-19 pandemic and associated travel restrictions. Although GeoSentinel historically has been lauded for its ability to detect sentinel events in real time, GeoSentinel only retrospectively identified cases of influenza-like illness as COVID-19 among travelers who returned from China early in the pandemic. Although the outbreak began in China, a popular destination for U.S. travelers, in late 2019, U.S. GeoSentinel sites first reported COVID cases among travelers in March 2020. This lack of early identification of COVID-19 cases was likely because of three main reasons. First, daily reports were generated for assistance in detecting sentinel events, but these were simple line listings of cases and focused primarily on etiologic diagnoses; although cases of “viral illness” were reported from China to GeoSentinel as early as December 2019, these were not identified to be out of the ordinary. Surveillance systems (e.g., GeoSentinel) are most effective in detecting established etiologic illnesses, not novel pathogens ( 37 ). Second, delays in identification and available diagnostics for this novel pathogen meant that testing was not routinely available globally or at GeoSentinel sites early in the pandemic; therefore, etiologic COVID-19 diagnoses were only made retrospectively. Third, many cases of COVID-19 might have had mild symptoms similar to influenza, the common cold, and seasonal allergies, whose symptoms can be treated with over-the-counter medication. Thus, ill travelers might have opted to treat their symptoms at home and not seek health care or visited their primary care provider instead of a travel and tropical medicine site despite their recent travel.
To address these challenges, GeoSentinel has begun to explore other ways to detect and track novel pathogens more rapidly. GeoSentinel is developing automated, real-time data analytics (e.g., machine learning algorithms by likelihood of outbreak origin) to improve the ability to detect outbreaks and unusual clusters of disease together with more classical surveillance approaches ( 38 ).
The findings in this report are subject to at least six limitations. First, GeoSentinel data are not representative of all travelers. Although GeoSentinel tracks illnesses among travelers who are treated at GeoSentinel sites, data are entered at the discretion of the sites, which might lead to underreporting. Second, sites are not evenly dispersed globally and are predominantly located in Europe and North America. This pattern might reflect the travel attributes of persons from these continents. Third, GeoSentinel only collects data on ill travelers who seek care at GeoSentinel sites. The total numbers of travelers, ill travelers who do not seek care, or travelers who seek care outside of the GeoSentinel network is unknown. Thus, GeoSentinel data cannot be used to estimate risk, incidence, prevalence, or other rates because the number of well or unexposed travelers in the denominator is not known. Fourth, the United States does not have many large travel and tropical medicine centers (in comparison with Europe or Asia) and travelers, including migrants, might seek care external to the GeoSentinel network. Fifth, although changes in the information collected, methods, and the sites themselves have made data collection more robust, these changes also make the comparison of periods difficult and, in certain cases, inappropriate. Although all sites use the same standardized data collection form, data entry practices vary by site and over time. Finally, the large number of migrants reported from U.S. GeoSentinel sites might be the result of selection bias because of the migration medicine specialization of many U.S. sites. Diseases detected among migrants might be driven by routine screening on entry to the United States.
As of September 2021, GeoSentinel has incorporated research through its cooperative agreement between CDC and ISTM. This will allow GeoSentinel to conduct hypothesis-driven studies to help guide clinical and public health recommendations. Initial projects include investigation of fever of unknown etiology among travelers, neurocognitive outcomes among travelers with malaria, kinetics of human Mpox infections, and exploration of the distribution and types of antimalarial resistance using malaria genomics.
Over the past decade, GeoSentinel has contributed to the early detection of diseases among international travelers. The information about demographics, traveler types, and frequent diagnoses provides data that clinicians and public health agencies can use to improve pretravel preparedness and enhance guidance for the evaluation and treatment of ill travelers who seek medical care after international travel. The key successes and shortcomings of GeoSentinel serve as references to improve surveillance and expand the capability to detect sentinel events.
The following active members of the GeoSentinel Network contributed data from U.S. sites: Susan Anderson (Palo Alto, California); Kunjana Mavunda (Miami, Florida); Ashley Thomas (Orlando, Florida); Henry Wu (Atlanta, Georgia); Johnnie Yates (Honolulu, Hawaii); Noreen Hynes (Baltimore, Maryland); Anne Settgast, Bill Stauffer (St. Paul, Minnesota); Elizabeth Barnett (Boston, Massachusetts); Christina Coyle, Paul Kelly, Cosmina Zeana (Bronx, New York); John Cahill, Marina Rogova, Ben Wyler; (New York, New York); Terri Sofarelli (Salt Lake City, Utah). All maps were contributed by Marielle Glynn.
Corresponding author: Ashley B. Brown, Division of Global Migration and Quarantine, National Center for Emerging and Zoonotic Infectious Disease, CDC. Telephone: 678-315-3279; Email: [email protected] .
1 Division of Global Migration and Quarantine, National Center for Emerging and Zoonotic Infectious Disease, CDC; 2 Department of Global Health, Boston University School of Public Health, Boston, Massachusetts; 3 Section of Infectious Disease, Department of Medicine, Boston University Chobanian & Avedisian School of Medicine, Boston, Massachusetts; 4 Division of Infectious Diseases (Emerita), Department of Medicine, Emory University, Atlanta, Georgia; 5 J.D. MacLean Centre for Tropical Diseases, McGill University, Montreal, Canada; 6 Department of Infectious Tropical Diseases and Microbiology, IRCCS Sacro Cuore Don Calabria Hospital, Negrar, Verona, Italy; 7 GeoSentinel, International Society of Travel Medicine, Alpharetta, Georgia; 8 Department of Medicine, Emory University School of Medicine, Atlanta, Georgia; 9 Department of Medicine, Mount Auburn Hospital, Cambridge, Massachusetts; 10 Harvard Medical School, Boston, Massachusetts; 11 Division of Infectious Diseases, University of Utah School of Medicine, Salt Lake City, Utah; start highlight 12 Department of Psychology, Colorado State University, Fort Collins, Colorado; end highlight 13 Infectious Diseases, Orlando Health Medical Group, Orlando, Florida
Conflicts of Interest
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflicts of interest were disclosed.
* 45 C.F.R. part 46.102(l)(2), 21 C.F.R. part 56; 42 U.S.C. §241(d); 5 U.S.C. §552a; 44 U.S.C. §3501 et seq.
- Glaesser D, Kester J, Paulose H, Alizadeh A, Valentin B. Global travel patterns: an overview. J Travel Med 2017;24:1–5. https://doi.org/10.1093/jtm/tax007 PMID:28637267
- World Tourism Organization. Yearbook of tourism statistics, data 2015–2019, 2021 edn. Madrid, Spain: World Tourism Organization; 2021. https://www.e-unwto.org/doi/book/10.18111/9789284422487
- Angelo KM, Kozarsky PE, Ryan ET, Chen LH, Sotir MJ. What proportion of international travellers acquire a travel-related illness? a review of the literature. J Travel Med 2017;24:1–8. https://doi.org/10.1093/jtm/tax046 PMID:28931136
- Kozarsky PE, Keystone JS. VFR (visiting friends and relatives) travelers [Chapter 5]. In: Schwartz E, ed. Tropical diseases in travelers. Chichester, UK: Wiley-Blackwell; 2010: 35–44.
- Ghent A. Overcoming migrants’ barriers to health. Bull World Health Organ 2008;86:583–4. https://doi.org/10.2471/BLT.08.020808 PMID:18797611
- Findlater A, Bogoch II. Human mobility and the global spread of infectious diseases: a focus on air travel. Trends Parasitol 2018;34:772–83. https://doi.org/10.1016/j.pt.2018.07.004 PMID:30049602
- Angelo KM, Gastañaduy PA, Walker AT, et al. Spread of measles in Europe and implications for US travelers. Pediatrics 2019;144:e20190414. https://doi.org/10.1542/peds.2019-0414 PMID:31209161
- CDC, Guinea Interministerial Committee for Response Against the Ebola Virus, World Health Organization, Liberia Ministry of Health and Social Welfare, Sierra Leone Ministry of Health and Sanitation. Update: Ebola virus disease epidemic—West Africa, February 2015. MMWR Morb Mortal Wkly Rep 2015;64:186–7. PMID:25719681
- Keni R, Alexander A, Nayak PG, Mudgal J, Nandakumar K. COVID-19: emergence, spread, possible treatments, and global burden. Front Public Health 2020;8:216. https://doi.org/10.3389/fpubh.2020.00216 PMID:32574299
- Chen LH, Wilson ME. The role of the traveler in emerging infections and magnitude of travel. Med Clin North Am 2008;92:1409–32, xi. https://doi.org/10.1016/j.mcna.2008.07.005 PMID:19061759
- Harvey K, Esposito DH, Han P, et al.; CDC. Surveillance for travel-related disease—GeoSentinel Surveillance System, United States, 1997–2011. MMWR Surveill Summ 2013;62(No. SS-3):1–23. PMID:23863769
- Hamer DH, Rizwan A, Freedman DO, Kozarsky P, Libman M. GeoSentinel: past, present and future. Alpharetta, GA: International Society of Travel Medicine, Journal of Travel Medicine; 2020. https://academic.oup.com/jtm/article/27/8/taaa219/6007543
- Gautret P, Angelo KM, Asgeirsson H, et al.; GeoSentinel Network. International mass gatherings and travel-associated illness: a GeoSentinel cross-sectional, observational study. Travel Med Infect Dis 2019;32:101504. https://doi.org/10.1016/j.tmaid.2019.101504 PMID:31707112
- Gautret P, Angelo KM, Asgeirsson H, et al.; GeoSentinel Global Surveillance Network. Rabies post-exposure prophylaxis started during or after travel: a GeoSentinel analysis. PLoS Negl Trop Dis 2018;12:e0006951. https://doi.org/10.1371/journal.pntd.0006951 PMID:30422981
- Chen LH, Piyaphanee W, Diaz-Menendez M, et al. Unplanned healthcare during travel: a descriptive analysis from the GeoSentinel Network [Abstract 1398]. In: Proceedings of the American Society of Tropical Medicine and Hygiene Annual Conference; November 18, 2020; Toronto, Canada. Arlington, VA: American Society of Tropical Medicine and Hygiene.
- Barnett ED, Mccarthy A, Coyle CM, et al. Global surveillance of infectious diseases in migrants by the GeoSentinel network [Abstract 110]. In: Proceedings of the International Conference on Migration Health; October 2, 2018: Rome, Italy. Dunwoody, GA: International Society of Travel Medicine.
- Schwartz E, Meltzer E, Mendelson M, et al. Detection on four continents of dengue fever cases related to an ongoing outbreak in Luanda, Angola, March to May 2013. Euro Surveill 2013;18:20488. https://doi.org/10.2807/ese.18.21.20488-en PMID:23725977
- CDC. Ongoing dengue epidemic—Angola, June 2013. MMWR Morb Mortal Wkly Rep 2013;62:504–7. PMID:23784016
- Chen LH. Zika virus infection in a Massachusetts resident after travel to Costa Rica: a case report. Ann Intern Med 2016;164:574–6. https://doi.org/10.7326/L16-0075 PMID:26864175
- Hamer DH, Barbre KA, Chen LH, et al.; GeoSentinel Surveillance Network. Travel-associated Zika virus disease acquired in the Americas through February 2016: a GeoSentinel analysis. Ann Intern Med 2017;166:99–108. https://doi.org/10.7326/M16-1842 PMID:27893080
- Hamer DH, Angelo K, Caumes E, et al. Fatal yellow fever in travelers to Brazil, 2018. MMWR Morb Mortal Wkly Rep 2018;67:340–1. https://doi.org/10.15585/mmwr.mm6711e1 PMID:29565840
- World Health Organization. Yellow fever—Brazil. Geneva, Switzerland: World Health Organization; 2019. https://www.who.int/emergencies/disease-outbreak-news/item/18-april-2019-yellow-fever-brazil-en
- Lips P, de Jongh RT. Vitamin D deficiency in immigrants. Bone Rep 2018;9:37–41. https://doi.org/10.1016/j.bonr.2018.06.001 PMID:30591925
- Dhavan P, Dias HM, Creswell J, Weil D. An overview of tuberculosis and migration. Int J Tuberc Lung Dis 2017;21:610–23. https://doi.org/10.5588/ijtld.16.0917 PMID:28482955
- Castelli F, Sulis G. Migration and infectious diseases. Clin Microbiol Infect 2017;23:283–9. https://doi.org/10.1016/j.cmi.2017.03.012 PMID:28336382
- McAuliffe M, Triandafyllidou A, eds. World migration report 2022. Geneva, Switzerland: International Organization for Migration; 2021. https://publications.iom.int/books/world-migration-report-2022
- Leder K, Torresi J, Libman MD, et al.; GeoSentinel Surveillance Network. GeoSentinel surveillance of illness in returned travelers, 2007–2011. Ann Intern Med 2013;158:456–68. https://doi.org/10.7326/0003-4819-158-6-201303190-00005 PMID:23552375
- Conner B. Travelers’ diarrhea [Chapter 2]. In: Brunette GW, Nemhauser JB, eds. CDC yellow book 2020: health information for international travel. New York, NY: Oxford University Press; 2019.
- Stoney RJ, Han PV, Barnett ED, et al. Travelers’ diarrhea and other gastrointestinal symptoms among Boston-area international travelers. Am J Trop Med Hyg 2017;96:1388–93. https://doi.org/10.4269/ajtmh.16-0447 PMID:28719282
- Leder K, Torresi J, Libman MD, et al. ; GeoSentinel Surveillance Network. GeoSentinel surveillance of illness in returned travelers, 2007–2011. Ann Intern Med 2013;158:456–68. https://doi.org/10.7326/0003-4819-158-6-201303190-00005 PMID:23552375
- Vila J. New molecular diagnostic tools in traveller’s diarrhea. J Travel Med 2017;24(suppl_1):S23–8. https://doi.org/10.1093/jtm/taw071 PMID:28520995
- Diemert DJ. Prevention and self-treatment of traveler’s diarrhea. Clin Microbiol Rev 2006;19:583–94. https://doi.org/10.1128/CMR.00052-05 PMID:16847088
- Walz EJ, Volkman HR, Adedimeji AA, et al. Barriers to malaria prevention in US-based travellers visiting friends and relatives abroad: a qualitative study of West African immigrant travellers. J Travel Med 2019;26:tay163. https://doi.org/10.1093/jtm/tay163 PMID:30602033
- Neave PE, Behrens RH, Jones COH. “You’re losing your Ghanaianess”: understanding malaria decision-making among Africans visiting friends and relatives in the UK. Malar J 2014;13:287. https://doi.org/10.1186/1475-2875-13-287 PMID:25064713
- Tan KR, Arguin PM. Malaria [Chapter 4]. In: Brunette GW, Nemhauser JB. CDC yellow book 2020: health information for international travel. New York, NY: Oxford University Press; 2019:267.
- Volkman HR, Walz EJ, Wanduragala D, et al. Barriers to malaria prevention among immigrant travelers in the United States who visit friends and relatives in sub-Saharan Africa: a cross-sectional, multi-setting survey of knowledge, attitudes, and practices. PLoS One 2020;15:e0229565. https://doi.org/10.1371/journal.pone.0229565 PMID:32163426
- Christaki E. New technologies in predicting, preventing and controlling emerging infectious diseases. Virulence 2015;6:558–65. https://doi.org/10.1080/21505594.2015.1040975 PMID:26068569
- Dai Y, Wang J. Identifying the outbreak signal of COVID-19 before the response of the traditional disease monitoring system. PLoS Negl Trop Dis 2020;14:e0008758. https://doi.org/10.1371/journal.pntd.0008758 PMID:33001985
FIGURE 1 . GeoSentinel sites and affiliate members — GeoSentinel Network, 2012–2021*
* Sites = 71; affiliate members = 164.
BOX 1 . Syndrome and system groupings of diagnoses for surveillance — GeoSentinel Network, 2012–2021
- Adverse events to medication or vaccine
- Animal bites or scratches
- Dermatological: infectious or potentially travel related
- Dermatological: preexisting or chronic disease or comorbidity
- Febrile or systemic syndrome
- Gastrointestinal: infectious or potentially travel related
- Gastrointestinal: preexisting or chronic disease or comorbidity
- Genitourinary and STDs: infectious or potentially travel related
- Genitourinary and STDs: pre-existing or chronic disease or comorbidity
- Musculoskeletal: infectious or potentially travel related
- Musculoskeletal: pre-existing or chronic disease or comorbidity
- Neurological: infectious or potentially travel related
- Neurological: preexisting or chronic disease or comorbidity
- Other:* infectious or potentially travel related
- Other:* chronic disease or comorbidity
- Respiratory or ENT: infectious or potentially travel related
- Respiratory or ENT: pre-existing or chronic disease or comorbidity
Abbreviations: ENT = ears, nose, and throat; STD = sexually transmitted disease.
* Diseases that do not fall into system groupings.
BOX 2 . Reason for travel — GeoSentinel Network, 2012–2021
- Tourism (vacation): Includes all travel for tourism or leisure. Also includes travel that might involve visiting friends and relatives overseas if the traveler is not a first- or second-generation immigrant returning to his or her country of origin.
- ° Conference: Travel by an employed person for the purpose of attending a conference or convention
- ° Corporate or professional: Travel by an employed person for the purpose of carrying out business, attending meetings, or other work-related events
- ° Business or occupational — research: Travel by an employed person for the purpose of field work, laboratory work, or other type of academic research
- ° Business or occupational — other: Travel for the purpose of business or as part of one’s occupation but where the travel does not fit in the other specific categories of research, study, conference, or seasonal migrant work
- Seasonal or temporary work (migrant worker): Travel for the purpose of pursuing seasonal or other nonpermanent work because of economic opportunities in countries other than the person’s country of birth or place or permanent residence. These persons usually do not have any intention or permission to stay permanently in the country or region in which they are working.
- Student: Travel by a student for the purpose of study abroad, attending a student conference, research, or other educational purpose
- Migration: Main reason for travel is intent or need to resettle outside of birth country or country of secondary migration
- Providing medical care: Travel for the purpose of providing medical care
- VFR: Person is traveling from the region in which they are currently residing (usually as a migrant, expatriate, or long-term visitor) to their region of origin (e.g., a low-income country) to visit friends and relatives. This reason for travel includes persons who are travelling with a child/grandchild (second-generation VFRs) or parent and those traveling with a spouse or partner.
- Military: Main purpose is deployment to the country visited or to participate in military operations
- Missionary, humanitarian aid, volunteer, or community service: Travel to perform humanitarian work, community service, or take part in volunteer work (includes travel prompted by participation in a religious organization). If the purpose is primarily to provide health care, then the reason for travel should instead be providing medical care.
- Retirement: Travel for the purpose of retiring to a new location. Certain of these persons will be expatriates or long-term visitors.
- Planned medical care : Main purpose of travel is to obtain medical care
- Not ascertainable: Reason for travel cannot be ascertained or is unknown
Abbreviation: VFR = visiting friends and relatives.
BOX 3 . Changes to the GeoSentinel data entry application — GeoSentinel Network, 2012–2021
- Added date of illness onset
- Added preexisting conditions (e.g., HIV, cancer, or diabetes), including use of immunosuppressive drugs
- Added a requirement to mark a “primary diagnosis” if more than one diagnosis was entered
- Added new fields for diagnosis activity (active or resolved) and if diagnosed by screening
October 2015
- Modified function for “complete” records to include only those with infectious diagnoses or those that were travel related
- Added fields to capture the highest level of care required for the illness (severity), where the patient obtained pretravel information, and a write-in field for general comments
- Modified main presenting symptoms
- Updated reason for travel options
- ° Animal exposure
- ° Antibiotic taken during travel
- ° Attended mass gathering
- ° Blood or body fluid exposure
- ° Provided medical care
- ° Staying or eating in local homes
- ° Unplanned medical or dental care
- Added ability to capture diagnosis method(s)
- Created supplemental data form to collect antibiotic resistance data on nine pathogens ( Campylobacter spp., Escherichia coli , Klebsiella pneumoniae , Salmonella spp., S. enterica Typhi, S. enterica Paratyphi, Shigella spp., Staphylococcus aureus , and Streptococcus pneumoniae )
- Initiated special projects for mass gatherings and rabies postexposure prophylaxis
October 2016
- Modified main presenting symptoms and diagnostic methods
- Added ability to collect specimen type and organism genus and species
- Added geographic alerts for certain diseases (Barmah Forest virus, chronic Chagas disease, coccidioidomycosis, filariasis, malaria, paracoccidioidomycosis, Ross River virus, and schistosomiasis) that are reported from unexpected countries and regions
- Added required additional information for certain diseases, including vaccination status, etiology (e.g., organism genus and species), and cause of death
- Deployed enhanced surveillance migrant form to capture detailed information on migrants
November 2017
- Added subcategories for VFRs, identifying the VFR as the person, child or dependent, or spouse or partner
- Added option for secondary reason for travel and country of exposure for VFRs
- Added additional questions for certain diagnoses (i.e., malaria, leishmaniasis, and Zika)
- Added QA alerts to ensure that certain diagnoses meeting the case definition using the diagnosis methods to be marked confirmed
- Began collecting data for enhanced surveillance projects for rickettsioses, planned and unplanned healthcare abroad
August 2018
- Updated production database from Microsoft SQL Server 2008 to Microsoft SQL Server 2016
November 2018
- Combined supplemental migrant data collection form with main data collection form
- Updated expatriate and long-term visitor definitions and added subcategory options
- Added reason for travel, country of exposure, and region of exposure fields to each diagnosis
- Added imported infection as a travel-related option for migrants
- Added new project for respiratory illness in older travelers
October 2019
- Removed variables for primary diagnosis and patient type fields (inpatient, outpatient, tele-consult inpatient, and tele-consult outpatient)
- Removed student subchoices for travel reason field
- Added field for required medical evacuation
- Updated antibiotic resistance drug options
- Revised antibody diagnosis method to specify whether IgM or IgG
- Deployed enhanced surveillance project for respiratory illness in travelers related to COVID-19
August 2020
- Deployed enhanced surveillance project for sentinel identification of respiratory illness in travelers related to COVID-19
November 2021
- Updated COVID-19 vaccination status, including boosters
Abbreviations: IgG = immunoglobulin G; IgM = immunoglobulin M; QA = quality assurance; VFR = visiting friends and relatives.
FIGURE 2 . U.S. GeoSentinel sites* — GeoSentinel Network, 2012–2021
* Sites include Atlanta, GA (1); Baltimore, MD (2); Bethesda, MD (3); Birmingham, AL (4); Boston, MA (5); Bronx, NY (6); Bronx Lebanon, NY (7); Cambridge, MA (8); Hollywood, CA (9); Honolulu, HI (10); Miami, FL (11); New York City, NY (12); New York Northwest, NY (13); New York West, NY (14); Orlando, FL (15); Palo Alto, CA (16); Peekskill, NY (17); Salt Lake City, UT (18); Seattle, WA (19); and St. Paul, MN (20).
FIGURE 3 . U.S. nonmigrant travelers or migrants presenting to U.S. GeoSentinel sites — GeoSentinel Network, 2012–2021*
* A total of 149 non-U.S. residents were excluded from the analysis.
* Information available for 7,527 migrants and 9,852 other travelers. † Information available for 7,490 migrants and 9,793 other travelers. § Information available for 7,488 migrants and 9,841 other travelers. ¶ Information available for 4,672 migrants and 8,967 other travelers.
Abbreviations: CNS = central nervous system; ENT = ear, nose, and throat; STD = sexually transmitted disease. * The five most common diagnoses are provided for the most common travel-related syndrome and system groupings. † No deaths were observed among migrants; four deaths were observed among nonmigrant travelers.
* Information available for 2,892 diagnoses. † Five countries or regions with highest number of patient exposures. § Information available for 2,554 diagnoses. ¶ Information available for 1,575 diagnoses.
* Information available for 6,518 diagnoses. † Information available for 6,296 diagnoses. § Five countries or regions with highest number of patient exposures. ¶ Information available for 5,920 diagnoses. ** Information available for 1,894 diagnoses.
Suggested citation for this article: Brown AB, Miller C, Hamer DH, et al. Travel-Related Diagnoses Among U.S. Nonmigrant Travelers or Migrants Presenting to U.S. GeoSentinel Sites — GeoSentinel Network, 2012–2021. MMWR Surveill Summ 2023;72(No. SS-7):1–22. DOI: http://dx.doi.org/10.15585/mmwr.ss7207a1 .
MMWR and Morbidity and Mortality Weekly Report are service marks of the U.S. Department of Health and Human Services. Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services. References to non-CDC sites on the Internet are provided as a service to MMWR readers and do not constitute or imply endorsement of these organizations or their programs by CDC or the U.S. Department of Health and Human Services. CDC is not responsible for the content of pages found at these sites. URL addresses listed in MMWR were current as of the date of publication.
All HTML versions of MMWR articles are generated from final proofs through an automated process. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version ( https://www.cdc.gov/mmwr ) and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
COVID-19-associated mucormycosis: Case report and systematic review
Affiliations.
- 1 Intensive Care Unit, VM Medicalpark Samsun Hospital, Samsun, Turkey; Istinye University, Faculty of Medicine, Istanbul, Turkey. Electronic address: [email protected].
- 2 Department of Infectious Diseases, Medilife Health Group, Istanbul, Turkey. Electronic address: [email protected].
- 3 Department of Pulmonology, VM Medicalpark Samsun Hospital, Samsun, Turkey; Department of Pulmonology, Bahcesehir University Medical School, Istanbul, Turkey. Electronic address: [email protected].
- 4 Department of Infectious Diseases, Samsun Liv Hospital, Samsun, Turkey. Electronic address: [email protected].
- 5 Intern, Bahcesehir University, Medical School, Istanbul, Turkey. Electronic address: [email protected].
- 6 Department of Infectious Diseases, VM Medicalpark Samsun Hospital, Samsun, Turkey. Electronic address: [email protected].
- PMID: 34454090
- PMCID: PMC8387131
- DOI: 10.1016/j.tmaid.2021.102148
Background: Increasing number of patients with COVID-19-associated mucormycosis have been reported, especially from India recently. We have described a patient with COVID-19-associated mucormycosis and, searched and analyzed current medical literature to delineate the characteristics of COVID-19-associated mucormycosis.
Method: We reported a patient developed mucormycosis during post-COVID period. We searched literature to describe the incidence, clinical features, and outcomes of COVID-19-associated mucormycosis. Demographic features, risk factors, clinical features, diagnostic methods, treatment and outcome were analyzed.
Results: We describe a 54-year-old male, hospitalized due to severe COVID-19 pneumonia. He was given long-term, high doses of systemic steroids. He developed maxillo-fascial mucormycosis and died of sepsis. Our literature search found 30 publications describing 100 patients including present case report. The majority (n = 68) were reported from India. 76% were male. The most commonly seen risk factors were corticosteroid use (90.5%), diabetes (79%), and hypertension (34%). Also, excessive use of broad-spectrum antibiotics were noted in cases. Most frequent involvements were rhino-orbital (50%), followed by rhino-sinusal (17%), and rhino-orbito-cerebral (15%). Death was reported as 33 out of 99 patients (33,3%).
Conclusions: Steroid use, diabetes, environmental conditions, excessive use of antibiotics, and hypoxia are main risk factors. Despite medical and surgical treatment, mortality rate is high. A multidisciplinary approach is essential to improve the conditions facilitating the emergence of COVID-19-associated mucormycosis.
Keywords: COVID-19; Coronavirus; Fungal infections; Mucor; Mucormycosis.
Copyright © 2021 Elsevier Ltd. All rights reserved.
Publication types
- Case Reports
- Systematic Review
- Middle Aged
- Mucormycosis* / diagnosis
- Mucormycosis* / drug therapy
- Risk Factors
You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.
- Section 1 - Improving the Quality of Travel Medicine Through Education & Training
- Section 2 - Perspectives : Travelers' Perception of Risk
The Pretravel Consultation
Cdc yellow book 2024.
Author(s): Lin Hwei Chen, Natasha Hochberg
The pretravel consultation offers a dedicated time to prepare travelers for health concerns that might arise during their trips. During the pretravel consultation, clinicians can conduct a risk assessment for each traveler, communicate risk by sharing information about potential health hazards, and manage risk by various means. Managing risk might include giving immunizations, emphasizing to travelers the importance of taking prescribed malaria prophylaxis and other medications (and highlighting the risks of not taking them correctly), and educating travelers about steps they can take to address and minimize travel-associated risks. The pretravel consultation also serves a public health purpose by helping limit the role international travelers could play in the global spread of infectious diseases.
The Travel Medicine Specialist
Travel medicine specialists have in-depth knowledge of immunizations, risks associated with specific destinations, and the implications of traveling with underlying conditions. Therefore, a comprehensive consultation with a travel medicine expert is indicated for all international travelers and is particularly important for those with a complicated health history, anyone taking special risks (e.g., traveling at high elevation, working in refugee camps), or those with exotic or complicated itineraries. Clinicians aspiring to be travel medicine providers can benefit from the resources provided by the International Society of Travel Medicine (ISTM) and might consider specialty training and certification (see Sec. 1, Ch. 4, Improving the Quality of Travel Medicine Through Education & Training ).
Components of a Pretravel Consultation
Effective pretravel consultations require attention to the traveler’s health background, and incorporate the itinerary, trip duration, travel purpose, and activities, all of which determine health risks ( Table 2-01 ). The pretravel consultation is the best opportunity to educate the traveler about health risks at the destination and how to mitigate them. The typical pretravel consultation does not include a physical examination, and a separate appointment with the same or a different provider might be necessary to assess fitness for travel. Because travel medicine clinics are not available in some communities, primary care physicians should seek guidance from travel medicine specialists to address areas of uncertainty. The Centers for Disease Control and Prevention (CDC) Travelers’ Health website also has materials and an interactive web-tool to guide primary care physicians through a pretravel consultation.
Personalize travel health advice by highlighting likely exposures and reminding the traveler of ubiquitous risks (e.g., injury, foodborne and waterborne infections, vectorborne diseases, respiratory tract infections—including coronavirus disease 2019 [COVID-19]—and bloodborne and sexually transmitted infections). Balancing cautions with an appreciation of the positive aspects of the journey can lead to a more meaningful pretravel consultation. In addition, pay attention to the cost of recommended interventions. Because some travelers are unable to afford all the recommended immunizations and medications, prioritize interventions (see Sec. 2, Ch. 15, Prioritizing Care for Resource-Limited Travelers ).
Table 2-01 The pretravel consultation: medical history & travel risk assessment
Health background.
Past medical history
- Allergies (especially any pertaining to vaccines, eggs, or latex)
- Medications
- Underlying conditions
Special conditions
- Breastfeeding
- Cardiopulmonary event (recent)
- Cerebrovascular event (recent)
- Disability or handicap
- Guillain-Barré syndrome (history of)
- Immunocompromising conditions or medications
- Pregnancy (including trimester)
- Psychiatric condition
- Seizure disorder
- Surgery (recent)
- Thymus abnormality
Immunization history
- Routine vaccines
- Travel vaccines
Prior travel experience
- High-elevation travel/ mountain climbing
- Malaria chemoprophylaxis
- Prior travel-related illnesses
Travel Risk Assessment (Trip Details)
- Countries and specific regions, including order of countries if >1 country
- Outbreaks at destination
- Rural or urban destinations
- Season of travel
- Time to departure
- Trip duration
Reason for travel
- Education or research
- Medical tourism (seeking health care)
- Visiting friends and relatives
- Volunteer, missionary, or aid work
Travel style
- Accommodations (e.g., camping/ tent, dormitory, guest house, hostel/ budget hotel, local home or host family, tourist/ luxury hotel)
- "Adventurous" eating
- Independent travel or package tour
- Level of hygiene at destination
- Modes of transportation
- Traveler risk tolerance
- Travel with children
Special activities
- Animal interactions (including visiting farms, touring live animal markets)
- Cruise ship
- Cycling/motorbiking
- Disaster relief
- Extreme sports
- High elevations
- Medical care (providing or receiving)
- Rafting or other water exposure
- Sexual encounters (planned)
Assess Individual Risk
Traveler characteristics and destination-specific risk provide the background to assess travel-associated health risks. Such characteristics include personal health background (e.g., past medical history, special conditions, immunization history, medications); prior travel experience; trip details, including itinerary, timing, reason for travel, travel style, and specific activities; and details about the status of COVID-19 and other infectious diseases at the destination. Certain travelers also might confront special risks. Recent hospitalization for serious problems might lead to a decision to recommend delaying travel. Air travel is contraindicated for patients with certain conditions. For instance, patients should not travel by air <3 weeks after an uncomplicated myocardial infarction or <10 days after thoracic or abdominal surgery. Consult relevant health care providers most familiar with the traveler’s underlying illnesses.
Other travelers with specific risks include those who have chronic illnesses, are immunocompromised, or are pregnant. Travelers visiting friends and relatives, long-term travelers, and travelers with small children also face unique risks. More comprehensive discussion on advising travelers with additional health considerations is available in Section 3. Determine whether recent outbreaks or other safety notices have been posted for the traveler’s destination by checking information available on CDC Travelers’ Health and US Department of State websites and other resources.
In addition to recognizing the traveler’s characteristics, health background, and destination-specific risks, discuss anticipated exposures related to special activities. For example, river rafting could expose a traveler to schistosomiasis or leptospirosis, and spelunking in Central America could put the traveler at risk for histoplasmosis. Flying from lowlands to high-elevation areas and trekking or climbing in mountainous regions introduces the risk for altitude illness. Inquire about plans for specific leisure, business, and health care-seeking activities.
Communicate Risk
Once destination-specific risks for a particular itinerary have been assessed, communicate them clearly to the traveler. Health-risk communication is an exchange of information in which the clinician and traveler discuss potential health hazards for the trip and any available preventive measures. Communicating risk is one of the most challenging aspects of a pretravel consultation, because travelers’ perception of and tolerance for risk can vary widely. For a more detailed discussion, see Sec. 2, Ch. 2, . . . perspectives: Travelers’ Perception of Risk .
Manage Risk
Vaccinations.
Vaccinations are a crucial component of pretravel consultations, and the risk assessment forms the basis of recommendations for travel vaccines. Consider whether the patient has sufficient time to complete a vaccine series before travel; the purpose of travel and specific destination within a country will inform the need for vaccines. At the same time, the pretravel consultation presents an opportunity to update routine vaccines (Table 2-02) and to ensure that eligible travelers are up to date with their COVID-19 vaccinations .
Pay attention to vaccine-preventable diseases for which immunity might have waned over time or after a recent immunocompromising condition (e.g., after a hematopoietic stem cell transplant). Asking whether travelers plan to travel again in the next 1–2 years can help them justify an immunization for travel over several years (e.g., rabies preexposure, Japanese encephalitis) rather than only the upcoming trip. Provide travelers with a record of administered immunizations and instructions to follow up as needed to complete a vaccine series.
Table 2-02 The pretravel consultation: vaccines to update & consider 1
Abbreviation: HBsAg, hepatitis B surface antigen.
1 Based on Advisory Committee on Immunization Practices guidelines, current as of October 21, 2021
Malaria Prevention
Self-treatable conditions.
Despite health care providers’ best efforts, some travelers will become ill. Obtaining reliable and timely medical care during travel can be problematic in many destinations. Consequently, consider prescribing certain medications in advance to enable the traveler to treat common health problems. Box 2-01 provides a list of some of the most common situations for which travelers find self-treatment useful.
Travel health providers need to recognize conditions for which travelers might be at risk and provide information about appropriate self-diagnosis and treatment. Keys to a successful treatment strategy include sharing a simple disease or condition definition, recommending or prescribing treatment, and educating the traveler about the expected outcome of treatment. As an example, for travelers’ diarrhea, inform travelers that most symptoms can be managed with fluid replacement plus loperamide or bismuth subsalicylate; prescribe travelers antibiotics they can carry with them for use in selected cases of incapacitating diarrhea (see Sec. 2, Ch. 6, Travelers’ Diarrhea , and Sec. 2, Ch. 7 . . . perspectives: Antibiotics in Travelers’ Diarrhea—Balancing Benefit & Risk ); and tell them to seek medical attention if symptoms persist for 24–36 hours or are particularly severe.
With some activities in remote settings (e.g., trekking), the only alternative to self-treatment would be no treatment. Pretravel counseling might result in a more accurate self-diagnosis and treatment than relying on local medical care in some areas. In addition, the increasing awareness of substandard and counterfeit drugs in pharmacies in certain countries makes it important for travelers to bring quality manufactured drugs with them from a reliable supplier (see Sec. 6, Ch. 3, . . . perspectives: Avoiding Poorly Regulated Medicines & Medical Products During Travel ).
Encourage travelers to carry a travel health kit with prescription and nonprescription medications and review each traveler’s medication list for possible drug–drug interactions. More detailed information for providers and travelers is included in Sec. 2., Ch. 10, Travel Health Kits , and Section 3 has supplementary travel health kit information for travelers who have additional health needs and considerations.
Box 2-01 The pretravel consultation: self-treatable conditions
The following list includes common situations for which travelers might find self-treatment useful. The extent of self-treatment recommendations offered to travelers should reflect the remoteness and difficulty of travel and the availability of reliable medical care at the destination. Recommended self-treatment options for each of the listed diseases are provided below or in the designated sections of this text.
ALTITUDE ILLNESS: Sec. 4, Ch. 5, High Elevation Travel & Altitude Illness
HIV EXPOSURE (OCCUPATIONAL): Sec. 9, Ch. 4, Health Care Workers, Including Public Health Researchers & Medical Laboratorians
JET LAG: Sec. 8, Ch. 4, Jet Lag
MALARIA: Sec. 5, Part 3, Ch. 16, Malaria
MOTION SICKNESS: Sec. 8, Ch. 7, Motion Sickness
TRAVELERS’ DIARRHEA: Sec. 2, Ch. 6, Travelers’ Diarrhea
URINARY TRACT INFECTIONS: common among many women; carrying a prescribed antibiotic for empiric treatment can be helpful.
VAGINAL YEAST INFECTIONS: self-treatment course of patient’s preferred antifungal medication can be prescribed for people who are prone to infections, sexually active, or who might be receiving antibiotics for other reasons, including doxycycline for malaria chemoprophylaxis.
Address Special Health Risks
Travelers with underlying health conditions require additional attention to health issues related to the destination and activities. For instance, travelers with a history of cardiac disease should carry medical reports, including a recent electrocardiogram. Asthma can flare in a traveler visiting a polluted city or from physical exertion during a hike; recommend that travelers discuss with their primary care provider a plan for treatment and carry necessary medication in case of asthma exacerbation.
Instruct travelers on how to obtain travel medical insurance and direct them to resources that provide lists of reputable medical facilities at their destination (e.g., the ISTM website; the American Society of Tropical Medicine and Hygiene website; the US Department of State’s Your Health Abroad website). Advise travelers to identify any allergies or serious medical conditions on a bracelet or a card to expedite medical care in emergency situations (see Sec. 3, Ch. 4, Highly Allergic Travelers ). Section 6 provides more information on preparing for and obtaining health care abroad.
Educate to Change Behavior
The pretravel consultation provides another setting to remind travelers of basic health and safety practices during travel, including frequent handwashing, wearing seatbelts, using car seats for infants and children, safe sexual practices, and COVID-19 prevention. Organize topics into a checklist and place priority on the most serious and frequently encountered issues ( Table 2-03 and Box 2-02 ). In addition, address general issues (e.g., preventing injury, sunburn). Written information is essential to supplement oral advice and enables travelers to review the instructions from their clinic visits. CDC’s Travelers’ Health website provides educational material. By giving advice on health risks and self-treatable conditions, clinicians can minimize the traveler’s need to seek medical care while abroad and possibly help them return to good health faster.
Table 2-03 The pretravel consultation: key discussion topics
TRAVEL-ASSOCIATED RISK
DISCUSSION POINTS
Altitude illness
- Determine if the itinerary puts the traveler at risk of altitude illness.
- Discuss preventive measures (e.g., gradual ascent, adequate hydration, medications to prevent and treat).
Bloodborne pathogens
- Avoid potential exposures (e.g., injections, piercings, tattoos, shared razors).
- Inform travelers who will provide health care overseas what to do in case of needlesticks or bloodborne pathogen exposures; discuss use of HIV postexposure prophylaxis.
- See Box 2-02 for summary on sexual health recommendations for travelers.
Disease-specific counseling
- Advise travelers to prepare for exacerbations or complications from underlying disease(s).
- Remind travelers to keep medications and supplies in carry-on luggage, to keep medications in their original prescription bottles, and to carry copies of their written prescriptions.
Environmental hazards
- Advise travelers to avoid walking barefoot to reduce their chances of certain parasitic infections.
- Advise travelers to avoid wading or swimming in freshwater where where risk for schistosomiasis or leptospirosis is possible.
- Caution travelers to avoid contact with animals to reduce the potential for bites and scratches that can transmit rabies. This is particularly important advice for the parents of young children.
- Remind travelers to apply sunscreen to sun- exposed skin.
Immunizations
- Discuss indications for, effectiveness of, and adverse reactions to immunizations.
- Discuss benefit of antibody titers when past vaccine records are unavailable or unreliable, particularly for hepatitis A, measles, mumps, rubella, and varicella.
- Review routine immunizations and travel immunizations indicated for the specific itinerary and based on the traveler's medical history.
- Screen for chronic hepatitis B for people born in countries with HBsAg prevalence ≥2% (see Map 5-07 ).
Malaria, yellow fever, & other vectorborne diseases
- Define vectorborne disease risks at the destination.
- Discuss personal protective measures and recommended insect bite precautions.
- For itineraries where malaria transmission is a risk: discuss risks and benefits of malaria chemoprophylaxis and recommended chemoprophylaxis choices.
- For itineraries where yellow fever virus transmission is a risk (see Sec. 2, Ch. 5, Yellow Fever Vaccine & Malaria Prevention Information, by Country , and Sec. 5, Part 3, Ch. 16, Yellow Fever ): assess individual traveler precautions and contraindications for receiving yellow fever vaccine; discuss risks and benefits of vaccination; discuss alternatives to vaccination for travelers at increased risk for adverse events from yellow fever vaccine.
Personal safety
- Advise travelers to look for security bulletins related to their destination and consider areas to avoid.
- Discuss precautions travelers can take (including avoiding excess alcohol consumption) to minimize risk for traffic accidents, personal assault, robbery, or drowning.
- Provide information on travel health and medical evacuation insurance.
Respiratory illnesses
- Consider influenza self-treatment for high-risk travelers.
- Discuss diseases and destinations of particular concern.
Travelers’ diarrhea and other food/waterborne illnesses
- Discuss food and water safety.
- Discuss antibiotics for self- treatment, adjunct medications (e.g., loperamide), and staying hydrated.
- Recommend strategies to decrease risk of diarrhea.
Abbreviation: HBsAg, hepatitis B surface antigen
Box 2-02 The pretravel consultation: summary of sexual health recommendations for travelers
Before travel.
- Get recommended vaccinations, including those that protect against sexually transmitted infections (STIs).
- Get recommended tests for HIV and treatable STIs. Be aware of STI symptoms in case any develop.
- Obtain condoms to carry on trip.
- Consider preexposure prophylaxis medication for HIV for high-risk travelers.
- Review local laws about sexual practices and obtain contact information for medical and law enforcement services.
- If pregnant or considering pregnancy, review whether Zika virus infection is a risk at destination.
During Travel
- Use condoms consistently and correctly to decrease the risk of HIV and STIs.
- If indicated, be prepared to start taking medications for HIV postexposure prophylaxis or unintended pregnancy within 72 hours after a high-risk sexual encounter.
- Never engage in sex with a minor (<18 years old), child pornography, or trafficking activities in any country.
- Report suspicious activity to US and local authorities as soon as it occurs.
After Travel
- Avoid exposing sexual partners at home. See a clinician to get recommended tests for HIV and STIs.
- Get treatment for all diagnosed, treatable STIs.
The following authors contributed to the previous version of this chapter: Lin H. Chen, Natasha S. Hochberg
Bibliography
Freedman DO, Chen LH. Vaccines for international travel. Mayo Clin Proc. 2019;94(11):2314–39.
Hatz CFR, Chen LH. Pre-travel consultation. In: Keystone JS, Freedman DO, Kozarsky PE, Connor BA, Nothdurft HD, editors. Travel medicine, 4th ed. Philadelphia: Saunders Elsevier; 2019. pp. 25–30.
Hill DR, Ericsson CD, Pearson RD, Keystone JS, Freedman DO, Kozarsky PE, et al. The practice of travel medicine: guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2006;43(12):1499–539.
International Society of Travel Medicine. The ISTM Body of knowledge for the practice of travel medicine, revised 2017. Atlanta: International Society of Travel Medicine; 2017. Available from: www.istm.org/bodyofknowledge2
Kozarsky PE, Steffen R. Travel medicine education—what are the needs? J Travel Med. 2016;23(5):taw039.
Leder K, Chen LH, Wilson ME. Aggregate travel vs. single trip assessment: arguments for cumulative risk analysis. Vaccine. 2012;30(15):2600–4.
Leder K, Torresi J, Libman MD, Cramer JP, Castelli F, Schlagenhauf P, et al. GeoSentinel surveillance of illness in returned travelers, 2007–2011. Ann Intern Med. 2013;158(6):456–68.
Leung DT, LaRocque RC, Ryan ET. In the clinic: travel medicine. Ann Intern Med. 2018 Jan 2;168(1):ITC1–16.
Steffen R. Travel vaccine preventable diseases—updated logarithmic scale with monthly incidence rates. J Travel Med. 2018;25(1):tay046.
File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Med Case Rep

A guide to writing case reports for the Journal of Medical Case Reports and BioMed Central Research Notes
Richard a rison.
1 Presbyterian Intercommunity Hospital Health Stroke Program, Los Angeles County Medical Center, University of Southern California Keck School of Medicine, 12401 Washington Blvd, Whittier, CA 90602, USA
Case reports are a time-honored, important, integral, and accepted part of the medical literature. Both the Journal of Medical Case Reports and the Case Report section of BioMed Central Research Notes are committed to case report publication, and each have different criteria. Journal of Medical Case Reports was the world’s first international, PubMed-listed medical journal devoted to publishing case reports from all clinical disciplines and was launched in 2007. The Case Report section of BioMed Central Research Notes was created and began publishing case reports in 2012. Between the two of them, thousands of peer-reviewed case reports have now been published with a worldwide audience. Authors now also have Cases Database, a continually updated, freely accessible database of thousands of medical case reports from multiple publishers. This informal editorial outlines the process and mechanics of how and when to write a case report, and provides a brief look into the editorial process behind each of these complementary journals along with the author’s anecdotes in the hope of inspiring all authors (both novice and experienced) to write and continue writing case reports of all specialties. Useful hyperlinks are embedded throughout for easy and quick reference to style guidelines for both journals.
Introduction: the importance of case reports
Case reports are a time-honored tradition in the medical profession. From Hippocrates (460 B.C. to 370 B.C.), and even arguably further back since the papyrus records of ancient Egyptian medicine (c. 1600 B.C.) to modern day, physicians of all specialties have described interesting cases involving all specialties [ 1 , 2 ]. Published case reports provide essential information for optimal patient care because they can describe important scientific observations that are missed or undetected in clinical trials, and provide individual clinical insights thus expanding our knowledge base [ 3 ].
The publication of case reports has indeed become a standard lexicon of the medical literature. Examples abound. Few practicing physicians would not know for instance the significance and subsequent discovery of a disease whose first description in 1981 began with the title in the medical case report literature as: “A preliminary communication on extensively disseminated Kaposi’s sarcoma in a young homosexual man” [ 4 ]. There is no neurologist that I know who is unfamiliar with the disease whose description began in 1817 by James Parkinson (1755 to 1824) with the title “An essay on the shaking palsy.” [ 5 ].
Yes, both of the above-mentioned famous diseases (the acquired immunodeficiency syndrome and Parkinson’s disease) were first described in the case study format. The act of recording, discussion with colleagues, and publishing our clinical observations with patients remains essential to the art of medicine and patient care. As Osler once said “Always note and record the unusual…Publish it. Place it on permanent record as a short, concise note. Such communications are always of value.” [ 6 ].
But how and when should we do this? Early case reports were little more than personal communications between colleagues about unique and interesting patients seen in their respective medical practices. This anecdotal reporting has evolved into an accepted form of scholarly publication with the ability to rapidly disseminate knowledge to a broad medical audience [ 7 ] using the generally accepted format of a title, abstract, introduction (background), case presentation, discussion, conclusions, and references. Many biomedical journals publish case reports and provide authors with guidelines that provide instruction for acceptance criteria, content, and format and give advice on relevant patient case reports that merit publication [ 3 ].
There are already many well-written published articles on how and when to write a good case report (please see Recommended further reading section at the end). I will not re-invent the wheel, but within this editorial I hope to provide an informal guide on how and when to write a case report for BioMed Central (BMC), in particular the Journal of Medical Case Reports ( JMCR ) and BioMed Central Research Notes ( BMCRN ). The utility of the newly created Cases Database will also be discussed. Relevant and useful website links will be used throughout to allow the reader easy access to further information on BMC requirements. I also hope to impart to the reader a brief overview of case report editorial flow in both JMCR and BMCRN along with the complementary relationship between both journals. I will also give anecdotes of how I personally approach things.
Definitions
What exactly is a case report? From peer-reviewed journals to Wikipedia (and yes, I read Wikipedia like we all do) definitions are readily available and generally agreed upon. A simple online search shows the following definition from “thefreedictionary.com” [ 8 ]: “Case Report A report of a single case of a disease, usually with an unexpected presentation, which typically describes the findings, clinical course, and prognosis of the case, often accompanied by a review of other cases previously reported in the biomedical literature to put the reported case in context.” Wikipedia [ 9 ] has this to say: “In medicine, a case report is a detailed report of the symptoms, signs, diagnosis, treatment, and follow-up of an individual patient. Case reports may contain a demographic profile of the patient, but usually describe an unusual or novel occurrence. Some case reports also contain a literature review of other reported cases.” Whether one uses the above definitional references or older more classic ones [ 10 ], all are in agreement.
How to start: the patient
Things start at the bedside or in the office with the most important person involved: the patient. Patients and their stories (including from their friends, coworkers, and family) are our portal to writing the case report. Patients (both in-patients and out-patients) are assessed, we confer with colleagues, appropriate investigations then follow, and treatment if possible begins. If I encounter an in-patient on call then I follow him or her throughout his or her hospitalization and, I hope, timely discharge. The patient is then followed and reexamined in the office over the course of time to see how the clinical course evolves. I usually wait 6 months over the course of multiple visits before I actually begin to write a case report so as to allow enough time for the clinical course to play out. Of course if the patient is hospitalized with an acute and rapid illness then this time may be much shorter, but I still follow him or her with daily neurologic examinations.
Collegial discussion and the Internet: our modern day water cooler
When an interesting condition is encountered in either the hospital or the office setting, I discuss the case in person with both my local neurology colleagues and colleagues of other specialties to see if they have encountered before the clinical scenario that I am dealing with at the time. This is usually a quick face-to-face nursing station conversation. If the case is particularly challenging then I will contact my local university colleagues for their opinion (especially if an urgent transfer needs to be arranged). I then “hit the books”, or at least I used to. Nowadays I usually “hit the keyboards” which are plentiful at every hospital nursing station and in my office. Indeed, the Internet seems to have become our modern day replacement for office water cooler conversations. Since it is readily available (and free to me because I am a member of the staff) in the hospital in which I see patients and in my office, I usually start with UpToDate® [ 11 ] and then click the links to individual references. Further reading is then supplemented by both PubMed [ 12 ] (free) and Cases Database (also free) [ 13 ] (see later). If I feel that a particular patient warrants a case report, then I continue to read more and more. There are also medical list servers and medical online communities to which one can post a case with de-identified images online and petition the advice of colleagues worldwide. I use both Neurolist [ 14 ] (a membership-only service, but membership is free) and The American Academy of Neurology (AAN) for my specialty and/or subspecialties [ 15 ] (also a membership-only service, the fee of which comes out of my yearly AAN dues). Another useful list server is sermo® [ 16 ], which has free membership. Teaching grand rounds at one’s local university or hospital, poster presentations, and simple discussion with professors giving lectures at local seminars are also good (and previously “traditional”) places to start. I have always preferred an in-person encounter to discuss a case with a colleague or professor, but given the current day and age (daily workload, travel costs, time away from the office and family, and so on), I have found Internet-based discussion (keeping all patient information anonymous of course) very helpful.
The BMC series, JMCR , and BMCRN : a brief history
The BMC series is a group of open access, peer-reviewed journals that spans most areas of biological and clinical research. There are currently 65 journals in the series, including (alphabetically) BMC Anesthesiology to BMC Women’s Health. Some of these publish case reports within their respective disciplines, and some do not [ 17 ].
JMCR is an online, open access journal under BMC auspices dedicated mainly to the publication of high quality case reports, and aims to contribute to the expansion of current medical knowledge (please see specific publication criteria below). It was created and founded by Michael Kidd and colleagues in 2007 and at the time was believed to be the world’s first international medical journal devoted to publishing case reports from all clinical disciplines. In the 5 years since its launch, JMCR has published over 2000 case reports. In 2011, case reports were downloaded from the journal’s website over 1,500,000 times [ 18 ].
BMCRN is also an online, open access journal under BMC auspices publishing scientifically sound research across all fields of biology and medicine. The journal provides a home for short publications, case series, and incremental updates to previous work with the intention of reducing the loss suffered by the research community when such results remain unpublished. BMCRN began publishing case reports in 2012 and now has a dedicated section for case reports [ 19 ].
Please read on to see the complementary relationship of case reporting between the two journals, how they relate to other journals in the BMC series, and further information on editorial work flow including specific publication criteria.
Cases Database: an invaluable resource
Since the launch of JMCR in 2007 and the more recent introduction of case reports to the BMCRN , which aims to have a broader scope, BMC has acknowledged and continues to acknowledge the value of case reports to the scientific literature. To further strengthen this commitment, BMC in conjunction with Michael Kidd have developed the invaluable new resource of Cases Database, a continually updated, freely accessible database of thousands of medical case reports from multiple other publishers, including Springer, British Medical Journal, and PubMed Central. By aggregating case reports and facilitating comparison, Cases Database provides a simple resource to clinicians, researchers, regulators and patients to explore content and identify emerging trends [ 20 ].
http://www.casesdatabase.com/
I find Cases Database indispensable when I research a particular patient’s condition. It is very helpful in seeing if a particular condition has been reported before and what treatment the authors have performed. It is an invaluable resource which can be used to check and see if previous cases have been reported before and how other authors have managed their patients with similar clinical conditions. When I last checked, Cases Database had in its repository 27,915 peer-reviewed medical case reports from 250 journals (!) [ 13 ]. Cases Database is quickly becoming my first go to when reading about a patient’s condition and symptoms.
When to write a case report
How does one determine when to write an actual case report? What constitutes and what are the criteria for publication? Different journals have different criteria, but here are the criteria for JMCR and BMCRN .
JMCR [ 21 ] publishes original and interesting case reports that contribute significantly to medical knowledge. Manuscripts must meet one of the following criteria: unreported or unusual side effects or adverse interactions involving medications; unexpected or unusual presentations of a disease; new associations or variations in disease processes; presentations, diagnoses and/or management of new and emerging diseases; an unexpected association between diseases or symptoms; an unexpected event in the course of observing or treating a patient; findings that shed new light on the possible pathogenesis of a disease or an adverse effect.
http://www.jmedicalcasereports.com/authors/instructions/casereport
BMCRN [ 22 ] has somewhat different publication criteria: BMCRN considers medical case reports that describe any clinical case. Case reports submitted to BMCRN do not need to be novel, but must be authentic cases and have some educational value along with representing at least an incremental advance in the field. BMCRN will not consider case reports describing preventive or therapeutic interventions because these generally require stronger evidence.
http://www.biomedcentral.com/bmcresnotes/authors/instructions/casereport
Neither BMCRN nor JMCR will consider case reports where there are ethical concerns.
JMCR and BMCRN have the following definitions that authors should know: a single case report, two case reports, or a case series (greater than two reported cases). Both journals follow this format and accept submissions with these title structures.
I tend to classify case reports in my mind generally as follows: diagnosis-related, management-related, or both [ 10 ]. Either type should have clear and concise take-home messages and teaching points. I personally keep a stack of charts labeled “Curious Cases” on a bookshelf within my small office next to my desk which is always within my field of view at work, adhering to the “out of sight, out of mind” principle. Over the years that space has grown and, admittedly, I have cases dating back over the entire span of my years in practice (now over 13 years) which I simply have not gotten around to yet (!).
BMC editorial workflow for case reports: a brief glimpse
If a BMC Series journal editorial team considers a submitted case report unsuitable for their respective specialty journal (and now a growing list of Springer journals that BMC is now affiliated with), the authors are given the option to transfer their manuscript to BMCRN . If this option is exercised, then the BMC editorial team (usually the Case Report Section Editor for BMCRN in conjunction with the appropriate Associate Editor) determines if the manuscript is suitable for BMCRN or if it is more suitable for JMCR (based on the criteria listed above). The manuscripts will then be forwarded on to the respective Deputy and/or Associate Editors for peer review depending on which of the journals the author(s) agree(s) to. Peer reviewers are solicited (usually at least one at BMCRN and at least two at JMCR ). The peer review comments (which are open and identifiable at JMCR and blinded at BMCRN ) are then usually sent to the authors for appropriate revisions and rebuttals (unless it is felt that the manuscript should be rejected outright, at which time the editorial office sends the authors an explanatory letter). After these revisions and rebuttals have been performed, the revised manuscript and rebuttals are sent back to the respective editors for a final decision and recommendations. These decisions and recommendations are then forwarded on to the Editor-in-Chief for final approval for publication. At JMCR , manuscripts are professionally copyedited before being sent off to the production team for publication, whereas at BMCRN the authors are requested to obtain their own professional copyediting (if needed) before publication (the respective costs being reflected within the different article processing charges for both journals). When the manuscripts are published in both journals, they are in the preliminary form before being converted to the final form after production.
Author satisfaction consistently ranks high for the overall process in both journals.
The actual case report
Now let us discuss the brass tacks of writing the actual case report by going through the individual sections that will comprise the manuscript. I will present them in a sequence that matches the journals’ website requirements and provide easily accessible hyperlinks to both respective journals.
The first page of the manuscript should be a dedicated title page, including the title of the article. The title should be a clear and short description of the case with a list of the full names, institutional addresses and email addresses for all authors. There should always be at least one corresponding author who is clearly identified. Abbreviations within the title should always be avoided.
http://www.jmedicalcasereports.com/authors/instructions/casereport#formatting-title
http://www.biomedcentral.com/bmcresnotes/authors/instructions/casereport#title
I usually end the title with “…: a case report” or “…: two case reports” or “…: a case series”. I also try to avoid any puns or overly cute wording within the title and try to keep things strictly descriptive and clear. The title needs to accurately describe the case – after all, this may be all that someone reads. If a cute or clever title is used that obscures what the case is really about, then it may be even less likely that the manuscript is read.
The Abstract should be “short and sweet”. It should not exceed 350 words. Abbreviations or references within the Abstract should not be used. The Abstract should be structured into three sections: Background, an introduction about why this case is important and needs to be reported. Please include information on whether this is the first report of this kind in the literature; Case presentation, brief details of what the patient(s) presented with, including the patient’s age, sex and ethnic background; Conclusions, a brief conclusion of what the reader should learn from the case report and what the clinical impact will be. Is it an original case report of interest to a particular clinical specialty of medicine or will it have a broader clinical impact across medicine? Are any teaching points identified?
http://www.jmedicalcasereports.com/authors/instructions/casereport#formatting-abstract
http://www.biomedcentral.com/bmcresnotes/authors/instructions/casereport#abstract
I find this is the most important part because this is often all that people will read and its availability will allow easy retrieval from electronic databases and help researchers decide their level of interest in the case report. The Abstract should be a concise and condensed version of the case report and should include the same main sections of the main text and be as succinct as possible [ 3 ]. This is the last thing that I usually write as it tends to flow easily after I have invested my time in thought and writing of the manuscript.
This section is comprised of three to ten keywords representing the main content of the article. It is important for indexing the manuscript and easy online retrieval.
http://www.jmedicalcasereports.com/authors/instructions/casereport#formatting-keywords
http://www.biomedcentral.com/bmcresnotes/authors/instructions/casereport#formatting-keywords
Introduction (Background)
The Introduction ( JMCR ) or Background ( BMCRN ) section should explain the background of the case, including the disorder, usual presentation and progression, and an explanation of the presentation if it is a new disease. If it is a case discussing an adverse drug interaction the Introduction should give details of the drug’s common use and any previously reported side effects. It should also include a brief literature review. This should give an introduction to the case report from the standpoint of those without specialist knowledge in the area, clearly explaining the background of the topic. It should end with a very brief statement of what is being reported in the article.
http://www.jmedicalcasereports.com/authors/instructions/casereport#formatting-intro
http://www.biomedcentral.com/bmcresnotes/authors/instructions/casereport#background
The Introduction or Background serves as the sales pitch for the rest of the manuscript. It should be concise and salient [ 3 ] and immediately attract the reader’s attention to entice him or her to read on.
Case presentation
This should present all relevant details concerning the case. The Case presentation section should contain a description of the patient’s relevant demographic information (without adding any details that could lead to the identification of the patient); any relevant medical history of the patient; the patient's symptoms and signs; any tests that were carried out and a description of any treatment or intervention. If it is a case series, then details must be included for all patients. This section may be broken into subsections with appropriate subheadings.
http://www.jmedicalcasereports.com/authors/instructions/casereport#formatting-case
http://www.biomedcentral.com/bmcresnotes/authors/instructions/casereport#presentation
This is one of the most integral sections. The case should be described in a concise and chronological order. One should usually begin with the primary complaint, salient history (including significant family, occupational, and other social history along with any significant medications taken or allergies), followed by the physical examination, starting with the vital signs presented at the examination, along with pertinent investigations and results. There should be enough detail (but not too much) for the reader to establish his or her own conclusions about the validity. It should contain only pertinent information and nothing superfluous or confusing [ 3 ].
This is an optional section in JMCR for additional comments that provide additional relevant information not included in the case presentation, and that put the case in context or that explain specific treatment decisions.
http://www.jmedicalcasereports.com/authors/instructions/casereport#formatting-discussion
This section should evaluate the patient case for accuracy, validity, and uniqueness and compare and contrast the case report with the published literature. The authors should briefly summarize the published literature with contemporary references [ 3 ].
Although this section is optional in JMCR (and not even listed separately on the BMCRN guidelines website), I find that most authors write this section, or an expanded conclusions section incorporating the elements listed above.
I personally write a separate discussion section and conclusions section for each case report that I author.
Conclusions
This should state clearly the main conclusions of the case report and give a clear explanation of their importance and relevance. Is it an original case report of interest to a particular clinical specialty of medicine or will it have a broader clinical impact across medicine? Information should be included on how it will significantly advance our knowledge of a particular disease etiology or drug mechanism (if appropriate).
http://www.jmedicalcasereports.com/authors/instructions/casereport#formatting-conclusion
http://www.biomedcentral.com/bmcresnotes/authors/instructions/casereport#conclusions
This should be short and concise with clear take-home messages and teaching points [ 3 ].
Patient’s perspective
This section is an opportunity for patients to add a description of a case from their own perspective. The patients should be encouraged to state what originally made them seek medical advice, give a description of their symptoms, whether the symptoms were better or worse at different times, how tests and treatments affected them, and how the problem is now. This section can be written as deemed appropriate by the patients, but should not include identifying information that is irrelevant to the case reported. As medicine becomes more person-centered, the voice of the individual patient becomes even more important, both to assist in clinical decision making, and for medical education.
http://www.jmedicalcasereports.com/authors/instructions/casereport#formatting-patients
This optional section is unique to JMCR , and I believe adds an important new dimension to the traditional case report. Most authors still do not yet take advantage of this, but I hope as time goes on and more and more open access case report manuscripts are published that this section will be routinely used, not just in JMCR but also in BMCRN and all other BMC clinical journals. I recall one manuscript in particular where the patient himself was requesting publication as soon as possible because of his terminal disease. He wanted his message out there and be available to all to read before he died.
List of abbreviations
When abbreviations are used in the text they should be defined in the text at first use, and a list of abbreviations can be provided, which should precede the Competing interests and Authors’ contributions sections.
http://www.jmedicalcasereports.com/authors/instructions/casereport#formatting-abbreviations
http://www.biomedcentral.com/bmcresnotes/authors/instructions/casereport#formatting-abbreviations
Both JMCR and BMCRN publish case reports over a wide range of medical and surgical specialties, and it is important for the reader who may not be within that particular specialty to readily access a quick list of common technical abbreviations. Also, given the open access nature of both journals, please keep in mind that non-medical professionals may read the manuscript as well.
This section is compulsory for BMC. It should provide a statement to confirm that the patient has given their informed consent for the case report to be published. The written consent should not routinely be sent in along with the manuscript submission (because of patient privacy issues), but the BMC editorial office may request copies of the consent documentation at any time. The following wording is recommended: “Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.” If the individual described in the case report is a minor, or unable to provide consent, then consent must be sought from his or her parents or legal guardians. In these cases, the statement in the ‘Consent’ section of the manuscript should be amended accordingly. Please keep in mind that manuscripts will not be peer reviewed if a statement of patient consent is not present.
http://www.jmedicalcasereports.com/authors/instructions/casereport#formatting-consent
http://www.biomedcentral.com/bmcresnotes/authors/instructions/casereport#consent
In practice, I always start with written consent from the patient. If the patient is incapacitated or deceased, then I obtain consent from the patient’s next-of-kin. Once this is obtained then I place it in the patient’s chart for safe keeping. I find that most patients and family members are quite agreeable to publication as long as their details are anonymous. BMC has very clear and explicit consent criteria and consent forms in multiple languages. I always keep a consent form within my office (and carry a few in my doctor’s handbag for hospital consults) for ready access. After I have obtained consent, I place it in the patient’s chart and keep it my office.
If the patient has died, then I try to obtain consent from the patient’s next-of-kin. This is usually done via telephone or postal mail. If the deceased patient’s family is amenable (and usually they are), then I send them (I never use email when it comes to patient-identifying information) the pre-filled out consent form in their language with a return envelope and paid for postage via the postal service. If I am unable to obtain consent this way in a case involving a patient who has died, then I write in the Consent section the following: “Written informed consent could not be obtained from the deceased patient’s next-of-kin for publication of this case report and accompanying images despite all reasonable attempts. Every effort has been made to protect the patient’s identity and there is no reason to believe that our patient would have objected to publication.”
If the patient was last known to be living but untraceable (or mentally incapacitated without next-of-kin consent), then I just simply do not publish the case.
For further information, please see JMCR and BMCRN website consent section hyperlinks as listed above.
Competing interests
A competing interest exists when one’s interpretation of data or presentation of information may be influenced by a personal or financial relationship with other people or organizations. Authors must disclose any financial competing interests and should also reveal any non-financial competing interests that may cause embarrassment were they to become public after the publication of the manuscript. Authors are required to complete a declaration of competing interests. All competing interests that are declared will be listed at the end of published article. Where an author gives no competing interests, the listing should read “The author(s) declare that they have no competing interests”.
http://www.jmedicalcasereports.com/authors/instructions/casereport#formatting-competing
http://www.biomedcentral.com/bmcresnotes/authors/instructions/casereport#formatting-competing
I do not usually find any problems with competing interests in the case reports that I publish, but the section should always be completed in our era and in the spirit of complete disclosure.
Authors’ contributions
In order to give appropriate credit to each author of a paper, the individual contributions of authors to the manuscript should be specified in this section.
An ‘author’ is generally considered to be someone who has made substantive intellectual contributions to a published study. To qualify as an author one should: 1) have made substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data; 2) have been involved in drafting the manuscript or revising it critically for important intellectual content; and 3) have given final approval of the version to be published. Each author should have participated sufficiently in the work to take public responsibility for appropriate portions of the content. Acquisition of funding, collection of data, or general supervision of the research group, alone, does not justify authorship. All contributors who do not meet the criteria for authorship should be listed in an Acknowledgements section. Examples of those who might be acknowledged include a person who provided purely technical help, writing assistance, or a department chair who provided only general support.
http://www.jmedicalcasereports.com/authors/instructions/casereport#formatting-contributions
http://www.biomedcentral.com/bmcresnotes/authors/instructions/casereport#formatting-contributions
I have found over the years a trend towards multi-authored case report manuscripts by many different individuals involved in the care of a patient(s). In my setting, it is usually me, a medical student or resident, a second-opinion tertiary colleague, and/or a pathologist or radiologist (if applicable). But I also recognize that there are situations that warrant more co-authors. The above criteria though for co-authorship should always be followed, and I have seen editorial situations where peer reviewers (including Associate Editors) have questioned what they felt was excessive authorship.
Authors’ information
This section includes any relevant information about the author(s) that may aid the reader’s interpretation of the article and understanding of the standpoint of the author(s). This may include details about the authors’ qualifications, current positions they hold at institutions or societies, or any other relevant background information. Please refer to authors using their initials. Note this section should not be used to describe any competing interests.
http://www.jmedicalcasereports.com/authors/instructions/casereport#formatting-information
http://www.biomedcentral.com/bmcresnotes/authors/instructions/casereport#formatting-information
In practice, I have frankly also personally used this section to advertise my services and “tout” my certifications and subspecialties (along with any co-authors and affiliated institutions) to my surrounding local community. This has in turn given me a modest increase in business (which has been completely non-monetary to date), usually in the form of email-based queries, many of which come from patients outside of my locality.
Acknowledgements
Authors should acknowledge anyone who contributed towards the article by making substantial contributions to conception, design, acquisition of data, or analysis and interpretation of data, or who was involved in drafting the manuscript or revising it critically for important intellectual content, but who does not meet the criteria for authorship. Also included should be the source(s) of funding for each author, and for the manuscript preparation. Authors must describe the role of the funding body, if any, in the: design, collection, analysis, and interpretation of data; writing of the manuscript; and decision to submit the manuscript for publication. Please also acknowledge anyone who contributed materials essential for the study. If a language editor has made significant revision of the manuscript, I recommend that you acknowledge the editor by name, where possible. Authors may also like to acknowledge (anonymously) the patient on whom the case report is based. If a scientific (medical) writer is used, this person should be included in the Acknowledgements section, including their source(s) of funding. Authors should obtain permission to acknowledge from all those mentioned in the Acknowledgements section.
http://www.jmedicalcasereports.com/authors/instructions/casereport#formatting-acknowledgements
http://www.biomedcentral.com/bmcresnotes/authors/instructions/casereport#formatting-acknowledgements
I have had colleagues who do not want to participate in the actual writing of the manuscript or do any actual “work” who have instead preferred to be mentioned in this section only.
Authors must search for and cite published case reports that are relevant to the case they are presenting. There should be no more than 15 references usually, although BMC does publish manuscripts with more references particularly if there is an extended literature review. Unless it is of historic interest, please keep the references as contemporary as feasible (for example, within the last 5 years or so). Please avoid excessive referencing.
http://www.jmedicalcasereports.com/authors/instructions/casereport#formatting-references
http://www.biomedcentral.com/bmcresnotes/authors/instructions/casereport#formatting-references
Cover letter
This is a separate document that should be written and uploaded with the main manuscript submission. I usually write this after I have written the Abstract. The cover letter should be addressed to the Editor-in-Chief in a formal manner and include all of the authors’ contact information. It should clearly and concisely state the title of the manuscript, and why the authors feel that their case report should be published based on any already available literature on the topic at hand. From an editor’s viewpoint, the cover letter is exceptionally important as that is the first thing that he or she reads and serves as the gateway to the Abstract and then the rest of the manuscript.
BMC author academy: help for all
Both JMCR and BMCRN have a large number of non-native English-speaking authors. Since JMCR and BMCRN are both BMC publications whose editorial offices are based in England, the language of publication is of course English. The BMC author academy is a joint program by BMC and Edanz [ 23 ] aimed at equipping writers for successful publication. Their materials have been developed from training workshops that Edanz gives to researchers worldwide and are not just limited to case reports. BMC recommends Edanz for authors who want to have their manuscript edited by a native speaker of English who is a scientific expert. Edanz provides scientific editing and related services that raise the quality of manuscripts to the standard needed to be understood at peer review.
http://www.biomedcentral.com/authors/authoracademy
I find that most non-native English-speaking authors have their manuscripts reviewed informally by a native English-speaking colleague and/or friend who is usually mentioned within the Acknowledgements section. This is understandable to keep costs down. However, please be aware that poor grammar and frequent spelling mistakes can be an impediment to editorial work flow and peer review. The editorial staff for both JMCR and BMCRN are acutely aware and sensitive to this given the large number of international submissions. At both JMCR and BMCRN , submitted manuscripts with questionable grammar and spelling are returned back to the authors by the editorial staff if it is felt that the grammar and spelling mistakes would impede peer review. If these issues are minor and it is felt that they would not impede peer review, then the manuscripts are sent off to peer reviewers (when appropriate).
Final checklist and the rule of C s
After I have completed a case report, I like to run through my long-winded (but useful) “rule of Cs” which is as follows.
Is it C lear, C oncise, and C oherent? Does it C onvey your message? Have you used C ases Database to look for any previously similar reported cases, and included them, if appropriate, in your references? Have you C onferred with your C olleagues on the C ontent? Will it C ause the reader to be C urious? Did you obtain C onsent? Does it C ontain all of the necessary information? Does it C omply with BM C guidelines? Do you think that it may need C opyediting? Do your C o-authors C oncur with the C ompleted paper? C an you C ut anything unnecessary out? Are your findings likely to be a C oincidence or by C hance alone? If so, then mention this in the Discussion section. Is the writing style C onsistent? Many times I find co-authored manuscripts have different writing styles within the same paper depending on who wrote what section. There should be a C entral, C orresponding author who is in C harge and oversees all of this. Is the C ase report written in a C hronological fashion with respect to the patient’s history and C hain of events? Is there anything that can be C ut out and have it still C ontain the C ompulsory information? Is it C oncise? Have you C onveyed C uriosity for your C ase report within your C over letter to the editorial team? Remember: your C over letter is the sales pitch to the editorial team! Make it C ount! Have you used within the manuscript C opyrighted information from another source? If so, do you need and/or have permission for use? After C ompletion, wait a C ouple of days before final submission to C lear your mind and read the manuscript again to C atch any mistakes that you may have made while you were C aught up in the C ompletion of it. Are the references C ontemporary? C an it be C omprehended by the average (“ C ”) reader? Remember, both JMCR and BMCRN are open access and freely available to anyone with an Internet C onnection and C omputer. C ast as wide a net as possible and C apture your C olleagues’ and other readers’ C uriosity. And first and foremost as a C linician: was the C are of your patient C ompetent and C ompassionate? (that is, are there any ethical concerns that may preclude peer review and publication?).
Summary and parting advice
Case reporting can be fun and a lifelong hobby, both for novice and experienced authors alike. It is now integral and widely accepted within published medical literature and today’s electronic information and data-sharing age. By following the above recommended steps and general overview, I hope to encourage BMC authors to continue to write and submit manuscripts to both JMCR and BMCRN . After your manuscript is complete, please follow the rule of “Cs”, especially “ C lear, C oncise, C oherent, C onsent, C ompassion, and C ompetence”, which will be appreciated by both reviewers and editors. Do not be afraid to obtain help from native English speakers for your manuscript. Also, please adhere to deadlines and follow instructions given by the editorial office, especially regarding any revisions. Editors read many different manuscripts and the longer it takes to get back a manuscript after revisions have been requested the less fresh that manuscript is in mind. Lastly, consider volunteering as an Associate Editor and/or reviewer within your specialty for both journals. I do for both, and the experience has improved both my writing and editing skills and daily interactions with patients.
Recommended further reading
I recommend the following further instructive reading on how and when to write a case report: References [ 3 , 7 , 10 , 24 ] (the last referenced article is in German, but one should readily be able to obtain an English translation if needed through a local librarian. It is well worth reading.)
I also recommend the following instructive BMC-related editorials and commentaries concerning the modern-day importance of case reports: References 2, 18, and 19.
I thank Professor Michael R. Kidd for his valuable advice and comments on this manuscript.
- Breasted J. The Edwin Smith Surgical Papyrus. Chicago: Chicago University Press; 1930. [ Google Scholar ]
- Rison RA. Neurology case reporting: a call for all. J Med Case Reports. 2011; 7 :113. doi: 10.1186/1752-1947-5-113. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cohen H. How to write a case report. Am J Health Syst Pharm. 2006; 7 :1888–1892. doi: 10.2146/ajhp060182. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gottleib GJ, Rogoz A, Vogel JV, Friedman-Kien A, Rywlin AM, Weiner EA, Ackerman AB. A preliminary communication on extensively disseminated Kaposi’s sarcoma in a young homosexual man. Am J Dermatopathol. 1981; 7 :111–114. doi: 10.1097/00000372-198100320-00002. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Goetz CG. The history of Parkinson’s disease: early clinical descriptions and neurological therapies. Cold Spring Harb Perspect Med. 2011; 7 (1):a008862. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Thayer WS. Osler, The Teacher Sir William Osler, Bart. Baltimore: Johns Hopkins Press; 1920. pp. 51–52. [ Google Scholar ]
- Carleton HA, Webb ML. The case report in context. Yale J Biol Med. 2012; 7 :93–96. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Weblink. “ http://medical-dictionary.thefreedictionary.com/case+report ” Accessed on August 11 th , 2013.
- Weblink. “ http://en.wikipedia.org/wiki/Case_report ” Accessed on August 11 th , 2013.
- Peh WCG, Ng KH. Writing a case report. Singapore Med J. 2010; 7 (1):10. [ PubMed ] [ Google Scholar ]
- Weblink. “ http://www.uptodate.com/home ” Accessed on August 11 th , 2013.
- Weblink. “ http://www.ncbi.nlm.nih.gov/pubmed ” Accessed on August 11 th , 2013.
- Weblink. “ http://www.casesdatabase.com/ ” Accessed on August 11 th , 2013.
- Weblink. “ http://www.neurolist.com/ ” Accessed on August 11 th , 2013.
- Weblink. “ http://www.aan.com/ ” Accessed on August 11 th , 2013.
- Weblink. “ http://www.sermo.com/ ” Accessed on August 11 th , 2013.
- Weblink. “ http://www.biomedcentral.com/authors/bmcseries ” Accessed on August 11 th , 2013.
- Kidd MR, Saltman DC. Case reports at the vanguard of 21 st century medicine. J Med Case Reports. 2012; 7 :156. doi: 10.1186/1752-1947-6-156. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cabán-Martinez AJ, Beltrán WF. Advancing medicine one research note at a time: the educational value in clinical case reports. BMC Res Notes. 2012; 7 :293. doi: 10.1186/1756-0500-5-293. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Weblink. “ http://www.casesdatabase.com/about ” Accessed on August 11 th , 2013.
- Weblink. “ http://www.jmedicalcasereports.com/ ” Accessed on August 11 th , 2013.
- Weblink. “ http://www.biomedcentral.com/bmcresnotes ” Accessed on August 11 th , 2013.
- Weblink. “ http://www.edanzediting.com/ ” Accessed on August 11 th , 2013.
- Schneemann M, Ruggieri F. [Publish your case report]. [ Article in German ] Praxis ( Bern 1994 ) 2013. pp. 253–259. doi:10.1024/1661-8157/a001229. quiz 60–61. [ PubMed ]
- Case report
- Open access
- Published: 14 June 2021
Post-mortem diagnosis of imported malaria in France: a case report
- Jacques Sevestre ORCID: orcid.org/0000-0001-8020-0050 1 ,
- Caroline Bernardi 2 ,
- Morgane Gillet 2 ,
- Pascal Delaunay 1 ,
- Youta Fanjat 3 ,
- Giorgio Toni 3 ,
- Pierre Marty 1 ,
- Véronique Alunni 2 &
- Christelle Pomares 1 , 4
Malaria Journal volume 20 , Article number: 271 ( 2021 ) Cite this article
2 Citations
1 Altmetric
Metrics details
Malaria is a potentially lethal parasitic disease due to infection by Plasmodium parasites, transmitted by Anopheles mosquito vectors. Various preventative measures may be recommended for travellers who visit endemic areas. The diagnosis is generally evoked in the context of a febrile patient returning from an endemic zone. Nevertheless, symptoms and clinical signs may be difficult to interpret, and fatal cases may only be diagnosed retrospectively with laboratory techniques, specific pathological features and patient history. The present work reports a case of fatal cerebral malaria diagnosed post-mortem, along with the techniques that allowed identification of the causative agent.
Case presentation
A 29 year-old male was found dead in his rental home during a vacation in Southern France. In the absence of explainable cause, an autopsy was performed, which did not retrieve major lesions. In the context of frequent business-related travels in tropical Africa, several samples were adressed for parasitological examination. Microscopy techniques, along with immunochromatographic and molecular biology assays, led to post-mortem diagnosis of fatal cerebral malaria. It was discovered in retrospect that the patient had not used preventative measures against malaria when travelling in endemic zones, and had not been provided with proper travel medicine counseling prior to his travel.
A vast proportion of imported malaria cases reported in France concerns patients who did not use preventive measures, such as bed nets, repellents or chemoprophylaxis. Given the wide availability of prevention tools in developed countries, and the important number of declared imported malaria cases, there is no doubt traveller awareness still needs to be raised. Moreover, healthcare professionals should always question travel history in febrile patients. The authors advocate for recurrent information campaigns for travellers, and physician training for a better prevention and diagnosis of malaria cases.
Malaria is a potentially lethal parasitic disease due to Plasmodium sp . infection, transmitted by Anopheles mosquito vectors. Even though a lot of progress has been made in the battle against malaria, it still accounts for a considerable number of deaths worldwide, estimated around 440,000 in 2018 [ 1 ] Among all these casualties, an overwhelming proportion occurs in the African continent, where several Plasmodium species are endemic, with Plasmodium falciparum being the most frequent one. This species is also the main culprit for lethal malaria cases [ 1 ]. The recent progress in the fight against malaria are the result of a broad distribution of long-lasting insecticidal mosquito nets, as well as the availability of efficient diagnostic tests and treatments [ 2 , 3 ]. Most people who live in endemic areas develop a partially protective immunity (i.e. premunition) over time. However, travellers who are naïve for the parasite may develop a fatal infection [ 1 ]. Thus, preventative measures are generally enforced for travellers in malaria-endemic countries. Travel medicine specialists offer different options according to the risk level: mosquito nets, repellents and chemoprophylaxis (CP), which reduce the risk of infection [ 4 ]. Nevertheless, none of these measures ensures 100% protection. Once infection has starded, clinical signs and symptoms are nonspecific: a high temperature, headhaches, vomiting, diarrrhoea, chills, muscle pains and fatigue [ 1 ]. They may be difficult to recognize, and physicians do not always think of the possibility of a Plasmodium infection if they are not aware of the patient’s travel history. The present work report a case of post-mortem diagnosed malaria case in a man who regularly travelled in endemic zones for professional purposes.
This case study concerns a 29 year-old Caucasian male of Dutch nationality who was found dead on a rental holiday home in July 2018 in southern France. Forensic autopsy findings were notable for oedema and congestion of the brain (Fig. 1 ), and splenomegaly. In the absence of major macroscopic lesion, no conclusions were drawn from forensic examination.

Autopsic aspect of the right parietal lobe of the brain, showing oedema, with widening of the gyri and narrowing of the sulci, and congestion
Upon questioning, family members explained that the man had no known medical condition. He worked a salesman for a food industry company, and had visited many African countries for professional purposes, travelling to Benin, Gambia, Guinea, the Ivory Coast, Liberia, Mali, Niger, Tchad, Togo and Senegal in the previous year. His last trip had occured a month before his death, in Guinea, where he had spent five days. Moreover, his family explained that he reported feeling sick for the past four months, with recurrent fever, headache, nausea and diarrhoea. They also mentioned that over this four-month period during which he experienced symptoms, he had visited several general practitioners in his hometown in the Netherlands. He presented with intermittent, febrile gastrointestinal symptoms and headaches associated with great fatigue. He had been prescribed an oral course of antibiotics, which did not improve his symptoms, and common blood chemistry analysis performed three months before his death only retrieved a slight elevation of Alanine Amino-Transferase (ALAT) measured at 56 U/l (above a reference range of 0 to 41). All other parameters were within normal range. No diagnostic tests for Plasmodium infection had been prescribed.
Post-mortem, samples from various body tissues were subjected to pathological and parasitological examination. Parasitological examination was performed on peripheral blood, brain tissue and spleen samples. Microscopic examination of peripheral blood smears and dry smears from the apposition of brain and spleen tissue stained with May-Grünwald-Giemsa (MGG) retrieved numerous trophozoïtes of P. falciparum (Fig. 2 ). In peripheral blood, parasitaemia was estimated at 5%. An immunochromatographic rapid diagnostic test (RDT) (PALUTOP + 4, BioSynex, Illkirch, France) performed on peripheral blood showed positivity for Plasmodium Lactate Dehydrogenase and Histidine Rich Protein-2 antigens, which was also consistent with P. falciparum infection. Pathological examination of brain tissue stained with the Haematoxylin–Eosin-Saffron (HES) method was consistent with previous findings, revealing numerous parasitized erythrocytes in the cerebral veins lumen (Fig. 3 ). Real-time polymerase chain reaction (PCR) analysis was secondarily performed by the French National Reference Centre in Marseille, France, and confirmed the presence of P. falciparum DNA in peripheral blood samples. Altogether, these results led to a post-mortem diagnosis of fatal cerebral imported malaria.
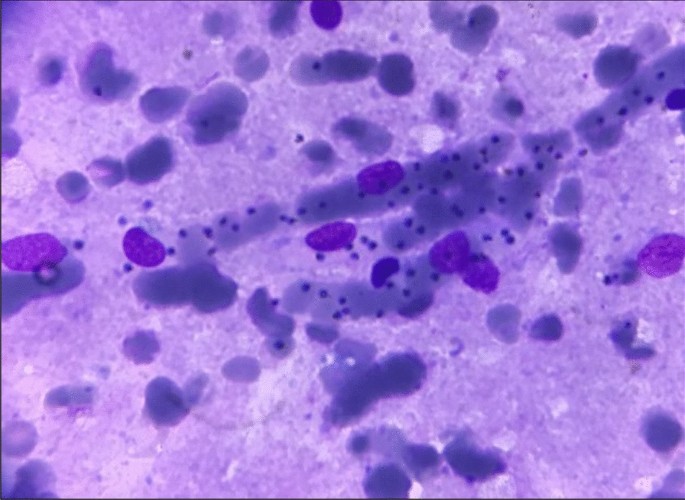
Microscopic aspect of a dry smear obtained from brain tissue apposition. Numerous trophozoïtes can be observed in the path of a small vessel (May-Grünwald-Giemsa staining, x1000)
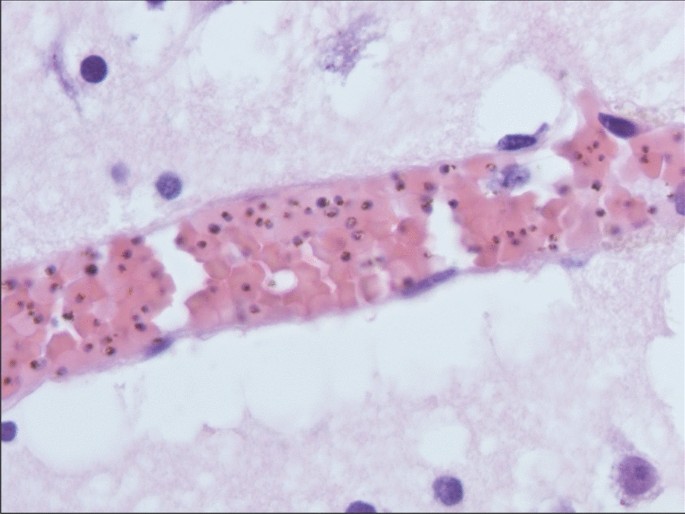
Brain parenchyma section showing intercellular oedema and venular congestion, with numerous parasitized erythrocytes. (Hematoxylin-Eosin-Saffron staining, x200)
In retrospect, it was found that this man had not been properly informed about risks regarding business travels in malaria-endemic countries. Indeed, he had not seen any travel medicine professional prior to his several travels in Africa, nor was he prescribed CP or repellents. However, he had received vaccination against yellow fever.
Discussion and conclusion
The present work reports a case of fatal cerebral imported malaria in a man who had probably been infected for months prior to this dramatic outcome. This report summarizes several features for the diagnosis of malaria, and how post-mortem investigations may lead to retrospective diagnosis of a fatal complicated form, with cerebral involvement.
Malaria is generally separated in two distinct clinical presentations: uncomplicated and severe. Uncomplicated malaria clinical signs are non-specific such as “flu-like" symptoms, fever, headaches, and also nauseas and diarrhoea [ 1 ]. Severe malaria follows uncomplicated malaria and may involve different vital functions, the most frequent being cerebral malaria, acute respiratory distress syndrome, acute kidney failure and acidosis [ 1 ]. Even when treated, cerebral malaria fatality rates may reach 10–20% in adults, highlighting the severity of this clinical form [ 1 , 5 ].
For this patient, the diagnosis of cerebral malaria was done post-mortem. In this context, examination of the brain generally reveals unspecific autopsic signs, such as oedema, congestion and petechias [ 6 , 7 ]. Techniques commonly used in clinical microbiology, such as peripheral smears and RDTs are of great aid, given the rapidity of the results and the high specificity for the diagnosis of malaria [ 8 ]. Histological findings may also orient towards a diagnosis of cerebral malaria. Histopathological features of cerebral malaria generally include vascular congestion, parasitized erythrocyte sequestration, ring trophozoïtes and the presence of malarial pigment in the small capillary vessels [ 6 , 8 , 9 ]. In this patient, gross autopsy findings were not conclusive, whereas rapid smear techniques (e.g. dry smears and thin blood smears) and RDTs quickly prompted the diagnosis of fatal cerebral malaria, which was secondarily confirmed by histopathological findings and PCR.
In France, 2,840 cases of imported malaria have been recorded in 2018 [ 10 ]. Lethal cases only occurred in a small proportion (11 cases = 0.38%) and were all due to P. falciparum infection [ 10 ]. Ten out of the 11 patients did not use proper preventative measures against malaria, whereas one patient had taken an inappropriate CP [ 10 ]. Dutch national surveillance data showed that 1,941 malaria cases were recorded between 2008 and 2015, including seven fatal outcomes, and underlined an increase in reported cases in this period of time [ 11 ].
This case tragically highlights several points that should remain etched in the mind of every medical professional. Before any travel in a malaria endemic area, traveller awareness still needs to be raised by health professionals and authorities, as almost all the imported malaria cases reported in France either did not observe chemoprophylaxis or used it inappropriately [ 4 ]. Patient information and education may considerably lower the risk of being infected during a stay in endemic zone [ 4 , 12 ]. Once travellers return from endemic areas, physicians should always consider the eventuality of malarial infection in a febrile patient, even after several months and whatever the symptoms. They should never hesitate to test patients for malaria infection, given the relative simpleness and rapidity of diagnostic techniques [ 1 ].
In this man's history, several opportunities to avoid the fatal outcome were missed. First, he was not provided with counseling by a travel medicine specialist, and no CP was initiated. Then, none of the physicians consulted by the patient after his travels were able to make a diagnosis of malaria. General practitioners should always question a possible history of travel in patients presenting with fever or unspecific signs. Indeed, in malaria-free areas, the key to securing diagnosis in febrile subjects is to unveil a history of travel in endemic regions [ 1 ].
In developed countries, travellers have an easy access to travel medicine practitioners. Furthermore, online resources for malaria prevention are generally available for physicians and travellers in developed countries [ 13 , 14 , 15 , 16 ]. An important proportion (if not all) of the imported malaria casualties could be avoided with adapted prevention.
Availability of data and materials
Not applicable.
Ashley EA, Pyae Phyo A, Woodrow CJ. Malaria. Lancet. 2018;391:1608–21.
Article Google Scholar
Nevill CG, Some ES, Mung’ala VO, Mutemi W, New L, Marsh K, et al. Insecticide-treated bednets reduce mortality and severe morbidity from malaria among children on the Kenyan coast. Trop Med Int Health. 1996;1:139–46.
Article CAS Google Scholar
McMorrow ML, Aidoo M, Kachur SP. Malaria rapid diagnostic tests in elimination settings—can they find the last parasite? Clin Microbiol Infect. 2011;17:1624–31.
Delaigue S, Signolet I, Consigny PH, de Gentile L, D’Ortenzio E, Gautret P, et al. New guidelines for the prevention of imported malaria in France. Med Mal Infect. 2020;50:113–26.
Wang W, Qian H, Cao J. Stem cell therapy: a novel treatment option for cerebral malaria? Stem Cell Res Ther. 2015;6:141.
Prat S, Desoubeaux G, Lefrancq Th, Chandenier J, Saint-Martin P. Sudden death due to cerebral malaria: a case report. J Forensic Leg Med. 2013;20:690–2.
Alunni-Perret V, Vandenbos F, Kechkekian A, Marty P, Legros F, Michiels JF, et al. Fatal cerebral malaria diagnosed after death in a French patient. Am J Forensic Med Pathol. 2010;31:269–72.
Menezes RG, Pant S, Kharoshah MA, Senthilkumaran S, Arun M, Nagesh KR, et al. Autopsy discoveries of death from malaria. Leg Med Tokyo Jpn. 2012;14:111–5.
Burel-Vandenbos F, Effa’a C, Alunni V, Cardot-Leccia N, Haudebourg J, Michiels J-F. A histologic study of brain in fatal cerebral malaria in French. Ann Pathol. 2008;28:495–7.
Rapport annuel d’activité 2019—Centre National de Référence du Paludisme. (2019) https://www.pasteur-cayenne.fr/wp-content/uploads/2020/04/2019-04-15-RA_cnr_2019_Paludisme.pdf . Accessed 25 May 2021.
de Gier B, Suryapranata FST, Croughs M, van Genderen PJJ, Keuter M, Visser LG, et al. Increase in imported malaria in the Netherlands in asylum seekers and VFR travellers. Malar J. 2017;16:60.
Sturrock HJW, Roberts KW, Wegbreit J, Ohrt C, Gosling RD. Tackling imported malaria: an elimination endgame. Am J Trop Med Hyg. 2015;93:139–44.
CDC. Malaria Information and Prophylaxis, by Country. (2019) https://www.cdc.gov/malaria/travelers/country_table/a.html . Accessed 25 May 2021.
Guidelines for malaria prevention in travellers from the UK 2019. (2019) https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/833506/ACMP_Guidelines.pdf . Accessed 25 May 2021.
SPF. Bulletin épidémiologique hebdomadaire, 19 mai 2020, n°Hors-série Recommandations sanitaires pour les voyageurs, 2020 (à l’attention des professionnels de santé). (2020) https://www.import/bulletin-epidemiologique-hebdomadaire-19-mai-2020-n-hors-serie-recommandations-sanitaires-pour-les-voyageurs-2020-a-l-attention-des-professionn.html . Accessed 25 May 2021
Zaken M van B. Vaccinations—Travel–netherlandsworldwide.nl. Dutch Ministry of Foreign Affairs (2016) https://www.netherlandsworldwide.nl/travel/vaccinations Accessed 25 May 2021
Download references
Acknowledgements
The authors wish to thank the patient’s family for accepting publication of this case report. The authors also thank Doctor Fanny VANDENBOS, Professor Jean-François MICHIELS and Professor Henri SEVESTRE for their help. The authors also warmly thank Suzanne SEVESTRE for revising the manuscript.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
Service de Parasitologie-Mycologie, Hôpital L’Archet, Centre Hospitalier Universitaire de Nice, UCA, 151 route de Saint Antoine de Giestière, 06000, Nice, France
Jacques Sevestre, Pascal Delaunay, Pierre Marty & Christelle Pomares
Laboratoire de Médecine Légale Et Anthropologie Médico-Légale, Hôpital Cimiez, Centre Hospitalier Universitaire de Nice, Nice, France
Caroline Bernardi, Morgane Gillet & Véronique Alunni
Laboratoire Central D’Anatomie Pathologique, Hôpital Pasteur, Centre Hospitalier Universitaire de Nice, Nice, France
Youta Fanjat & Giorgio Toni
Equipe 6 Virulence Microbienne Et Signalisation Inflammatoire, C3M, INSERM 1065, Nice, France
Christelle Pomares
You can also search for this author in PubMed Google Scholar
Contributions
JS participated to the parasitological diagnosis, collected the data and wrote the manuscript. CB and MG performed forensic examination and collected data. PD performed parasitological diagnosis and reviewed the paper. YF and GT performed the histopathological diagnosis. PM, VA and CP participated to the diagnosis, reviewed the manuscript and supervised the work. All authors have read and approved the final manuscript.
Corresponding author
Correspondence to Jacques Sevestre .
Ethics declarations
Ethical approval and consent to participate., consent for publication..
Written informed consent was obtained from the next of kin for publication of this case report as well as any accompanying images.
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Sevestre, J., Bernardi, C., Gillet, M. et al. Post-mortem diagnosis of imported malaria in France: a case report. Malar J 20 , 271 (2021). https://doi.org/10.1186/s12936-021-03806-y
Download citation
Received : 22 April 2021
Accepted : 07 June 2021
Published : 14 June 2021
DOI : https://doi.org/10.1186/s12936-021-03806-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Cerebral malaria
- Malaria diagnosis
- Malaria prevention
- Travel medicine
Malaria Journal
ISSN: 1475-2875
- Submission enquiries: [email protected]
- Search Menu
- Sign in through your institution
- Advance articles
- Collections
- Editor's Choice
- Supplements
- Author Guidelines
- Submission Site
- Open Access
- About Journal of Travel Medicine
- About the International Society of Travel Medicine
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Risk assessment, absolute risk measures: incidence rate, incidence density, and attack rate, additional biases and limitations of absolute risk measures in the travel medicine context, the “average traveler”, risk factor measures, interpreting risk data, risk reduction from interventions, risk perception and risk tolerance, conclusions, declaration of interests.
- < Previous
Risk Assessment in Travel Medicine: How to Obtain, Interpret, and Use Risk Data for Informing Pre‐Travel Advice
- Article contents
- Figures & tables
- Supplementary Data
Karin Leder, Robert Steffen, Jakob P. Cramer, Christina Greenaway, Risk Assessment in Travel Medicine: How to Obtain, Interpret, and Use Risk Data for Informing Pre‐Travel Advice, Journal of Travel Medicine , Volume 22, Issue 1, 1 January 2015, Pages 13–20, https://doi.org/10.1111/jtm.12170
- Permissions Icon Permissions
It has been recommended that numerical risk data should be provided during the pre‐travel consultation in order for travelers to make informed decisions regarding uptake of preventive interventions.
In this article, we review the definitions of the various risk measures, particularly as they relate to travel health, and discuss the study designs and methodological details required to obtain each measure.
Risk measures can be broadly divided into absolute risk measures (including incidence rate, attack rate, and incidence density) and risk factor measures (including relative risk, risk ratio, and odds ratio). Although there are limitations inherent to each measure, absolute risk measures estimate the baseline risk for an “average” traveler, and risk factor measures help determine whether the risks for an individual traveler are likely to be higher or lower than this average, which is determined by specific traveler and itinerary characteristics. Incremental risk considerations add additional complexity, and risk communication plus risk perception/risk tolerance have additional impact on the individual traveler's interpretation of risk measures.
Travel health practitioners should be aware of the complexities, limitations, and difficulties in understanding numerical risk data, as these factors are important in travelers' acceptance or rejection of interventions offered.
In travel medicine, data on disease risks are frequently derived from epidemiology within endemic populations. However, these data may not be relevant to travelers because of differences in past exposures, past vaccination history, specific activities undertaken, coexisting morbidities, and other factors. Dedicated research over the last few decades has provided improved information on the risks of various infections relevant for traveling populations, although uncertainties in risk magnitude remain for many diseases. 1
A recent article on risk assessment in the travel clinic concluded that “By the end of the pre‐travel consultation, it is expected travelers will have been provided with numerical data about likelihood of events happening.” 2 This begs the question: how important and comprehensible are the actual risk numbers to travelers and their providers?
Various risk measures are undoubtedly cited when discussing risks with travelers. The objectives of this article are to define terms used for risk assessment in relation to the travel medicine context, and to consider the role of risk magnitude as well as other relevant factors on decision making. This will remind providers about which study design provides which risk measure, assist with understanding of risk concepts and their potential impact on preventive risk‐based discussions, and will also help to guide the use of a common language by both travel health professionals and researchers.
Risk assessment for impending travelers is generally considered in the following sequential manner:
Estimate baseline risk for the average traveler (requires absolute risk data).
Consider specific risk factors relevant for the individual traveler that may modify the “average” risk [requires exposure, itinerary, demographic data, and comorbidity, often reflected as relative risk (RR) and odds ratio (OR) data].
Consider the role of interventions such as vaccines and prophylaxis: compare travel risks with and without the intervention and balance this against potential side effects (requires data on baseline risk as well as on effectiveness and harms of interventions).
Account for individual risk perception and risk tolerance issues, which influence the travelers' interpretation of risk measures and the likelihood they will accept or decline interventions offered.
In practice, as well as in these issues, the travelers' budget may play a decisive role in the uptake of preventive measures, and prioritization of interventions is often required.
When communicating travel risks, it is important to clarify what various risk measures tell us, including their strengths, biases, and limitations, and from which sources relevant information can be obtained (Table 1 ). Absolute risk measures are often considered optimal, and are commonly expressed as incidence rates, incidence density, or attack rates (Table 2 ). Such rates are usually measured via cohort studies. Cohort studies address a population at risk (denominator) and collect data on new cases (numerator) in a specified period of time, thus providing all necessary data to assess incidence rates (see below). However, in travel medicine, cohort studies are often very difficult to carry out for a number of reasons. Travelers are a very heterogeneous population (Table 3 ), and most diseases are rare except for conditions of syndromes such as travelers' diarrhea and respiratory infections. It is, therefore, difficult to prospectively follow up a sufficiently large group of travelers to enable collection of enough cases of individual diseases, and it is also difficult to confirm illness etiologies during trips, especially to remote areas.
Relationship between study designs and risk measures
Adapted from Ref. 11 .
Absolute and indirect risk measures
Definitions adapted from Ref. 3 .
Definition adapted from Ref. 17 .
Examples of diversity among international travelers
Incidence rates are defined as the number of new cases of disease within a specific at‐risk population, expressed per unit of time. 3 A frequently quoted example is the incidence rate of 1 influenza case per 100 travelers per month. 4 A closely related risk measurement is the incidence density, defined as the number of new cases in a specified at‐risk population per person‐time at risk. 3 An example is the estimated incidence density of hepatitis A in travelers to countries of high or intermediate risk of transmission of 3.0 to 11.0 per 100,000 person‐months abroad for all travelers and 6.0 to 28.0 per 100,000 person‐months for those presumed to be non‐immune. 5 Although the terms “incidence rate” and “incidence density” are often used interchangeably, at least theoretically, all persons at risk should be observed prospectively throughout the specified time period to calculate incidence rates, whereas individuals can be observed and/or be at risk for different periods of time for calculation of incidence densities. In many epidemiological population‐based cohort studies, the subtle difference between these measures may be irrelevant, but in the travel medicine context, as travelers have widely variable trip durations, using person‐time in the denominator has the advantage of being able to account for varying periods of travel, and consequently varying periods of risk. However, the entire period of the trip (eg, the number of days or the number of weeks of travel) is usually used, which infers that risk is considered uniform throughout. When there is no linear relationship between duration of exposure and risk, incidence density may be misleading. For example, the incidence rate of travelers' diarrhea is greatest during the first week and continuously decreases thereafter. 6 In this situation, it is therefore more useful to measure incidence rates during the initial 2 weeks of stay (corresponding to a “usual” duration of stay for most tourist travelers) or a cumulative incidence per specified time period, rather than an incidence density per 100 travel‐days or per person‐year.
Another risk measure is the attack rate, which is defined as the proportion of a specified at‐risk population that develops illness over a given time period. 3 In traditional epidemiology, attack rates are usually described in the setting of an outbreak when the population at risk following a specific exposure can be defined. It should be noted that the attack rate is not truly a rate but rather a proportion without including a specific time unit, but time can often be inferred as the period of the outbreak (often inferring a discrete short time period even if not explicitly stated). 7 In travel medicine, we generally consider the trip as being the period of risk, and define the attack rate as the proportion of people falling ill during the trip. A frequently quoted example is the attack rate for typhoid of 1 per 3,000 travelers to South Asia, which describes the risk per trip but with no duration of stay mentioned. 8
These absolute risk terms are sometimes used interchangeably in the travel medicine literature, and the difference between these measures is often subtle given they each provide risk data using event frequency, number of persons, and some indication of time factors (either a specific duration or the period of the trip, with the average duration of travel generally being a few weeks at most intercontinental destinations). However, the different information incorporated to calculate risk and the varying trip durations among individuals can give rise to apparent risk differences. As an example, among 15,180 travelers to Kenya with a mean duration of stay of 13.2 days, the incidence rate for travelers' diarrhea was 64 cases per 100 travelers per 2‐week stay, whereas the overall attack rate among the group was 54.6%. 9 Additionally, because cohort studies require follow‐up of participants over time, they are vulnerable to effects of different withdrawal rates between cases and non‐cases (attrition bias), leading to either over‐estimation of incidence rates (if there is greater drop‐out among non‐cases) or underestimation (if greater drop‐out among cases).
Although incidence measures are usually defined via prospective studies, cross sectional questionnaires which ask about newly occurring symptoms related to travel can also provide information on the frequency of medical events during a trip. The cross sectional study design is traditionally used to measure point‐prevalence, but in the travel medicine context it can instead be used to ask about new onset of travel‐related symptoms in order to provide incidence estimates. These studies are often carried out either during travel (eg, as pre‐return airport surveys) or immediately post‐travel (such as telephone interviews). Unlike cohort studies, cross sectional studies have no attrition bias, but those who have experienced relevant symptoms may be more likely to agree to participation than those who have remained well (selection bias), which could lead to an overestimation of true risk. There are also significant limitations in confirming diagnoses with this study design, which is therefore best used to assess the proportion of travelers who develop symptoms of interest rather than to define exact illness etiologies.
Another way to obtain data on travel‐associated health risks is to use notification data. The number of notified cases can be used as case numbers (numerator data), and sources such as national registries or World Tourism Organization can be used to infer the total numbers of travelers (denominator data). These data can be stratified into regions of exposure and acquisition. However, this approach is generally possible only for infections that are reportable, such as malaria, typhoid, and hepatitis A, and is most readily interpreted to infer travel‐associated risks of diseases that do not occur in the travelers' home countries. Under‐diagnosis and under‐reporting is also common leading to an underestimation of the actual number of cases, and precise details about trip itineraries may be unavailable. Additionally, different methodologies used to estimate the number of travelers result in different estimations of denominator statistics. 10
An important issue regarding the prospective cohort study design required to obtain absolute risk data in the context of travel medicine is that it often includes only individuals who have sought pre‐travel health care, who agree to be recruited, and who are followed up on return. This potentially biases results to certain types of travelers and may mean that findings cannot be generalized to populations who have not sought health care before travel. One potential way to overcome this bias would be to recruit pre‐departure at airports, but this approach is rarely feasible and would be adversely impacted on by low recruitment and follow‐up rates. Additionally, there have been no multisite cohort studies assessing illness risks in travel medicine, so we generally rely on the relatively few, often single‐site cohort studies that have been carried out among select subgroups of travelers for incidence rate/incidence density data, which again reduces generalizability. 11
Many illnesses acquired by travelers are acute and occur during and/or soon after travel. Diagnostic options are limited, particularly en route, so researchers are rarely able to confirm illness etiologies. Some trials have enlisted the collaboration of local partners in the destination countries to help confirm the cause of acute symptoms, such as recently conducted trials of patch vaccines containing heat‐labile toxin from Escherichia coli among travelers to Central America and India, 12,13 but this is an extremely expensive approach. Thus, even with dedicated prospective studies, it is difficult to generate complete data on health risks during and after the journey. This issue can be overcome to some extent for infections which are diagnosable using antibody testing, as before‐and‐after blood samples can be taken to look for seroconversion. Both symptomatic and asymptomatic infections will be detected; the asymptomatic infections may or may not be clinically relevant. Moreover, serological testing cannot be used to diagnose vaccine‐preventable diseases in the immunized traveler, as (with some notable exceptions, such as hepatitis B) serology generally cannot differentiate between antibodies induced by the vaccine and antibodies induced by exposure to the pathogen.
In addition to the difficulties in obtaining “average population” data on absolute travel risks already discussed, the generation of appropriate data on the individual traveler's risks is further complicated by the fact that the “average traveler” does not exist. Transmission of many tropical infectious diseases is influenced by seasonality, so the same duration of travel at different times of the year may be associated with different levels of infection risks (eg, higher transmission of Plasmodia during rainy season). The actual likelihood of an adverse health event is also dependent on the year, the exact place of exposure, the precise accommodation, and the activities and likely exposures of the individual, so will vary within and between trips. Furthermore, personal factors, including basic demographics (age and gender), co‐morbidities, education level, and financial status influence risk. Individual factors such as risk behavior and compliance with prophylactic measures also modify personal risks. Table 3 lists a variety of characteristics of different traveler subgroups illustrating the importance of subgroup‐specific risk information that goes beyond risk assessment in the “average traveler.” Providing the individual traveler with average risk information may significantly under‐ or overestimate this traveler's personal risk, arguably making it unadvisable to try to be too precise with actual numerical data, and highlighting the need to also incorporate individual risk factor measures.
Although recognized that each individual's probability of disease varies according to demographic, host, and itinerary characteristics, risk measures for every specific trip (all itineraries, all durations, and all activities) in every type of traveler (both genders, all ages, and all co‐morbidities) cannot be calculated. The travel medicine advisor must therefore take the best absolute risk measure (if there is one), and then decide whether the traveler sitting in front has demographic or itinerary characteristics that put him/her at higher, lower, or the same risk as this average. This requires knowledge about risk factors for certain outcomes. Such risk factors are commonly measured via RRs (or risk ratios) and ORs (Table 2 ).
RR compares the proportion or probability of an event in one group with the proportion among another group (eg, with/without a specific risk factor or with/without a specific protective intervention). 3 The rate ratio similarly compares rates of events between two groups, such as the incidence rate in a population with a specific risk (or protective factor) and without this factor. While RR is based on a ratio of two proportions, the rate ratio includes the factor time. These measures can be calculated via the study designs discussed above. An example is the difference in risks of certain illnesses among tourist travelers versus those visiting friends and relatives (VFRs). 14
The OR, which also quantifies the relationship between a risk factor and a health outcome, represents the ratio of the odds of an event occurring in one group compared with that of the odds of an event occurring in another group (eg, with/without a risk factor). 3 In contrast to the RR, the OR is based on chances rather than on proportions, so does not require information on the entire population at risk. The OR can, therefore, be calculated from all epidemiologic study designs including the less resource‐intensive case‐control study design.
Once a risk factor has been suspected or identified, both RRs and ORs allow determination of the magnitude of the risk‐modifying effect, ie, the impact of this factor in placing individuals at higher or lower risk of disease. The OR usually overestimates the true risk ratio, but the rarer the event, the more similar the OR and RR estimates will be. 15 Such risk factor identification means that, if the individual traveler has characteristics that have been shown to be associated with a disease or adverse outcome (eg, immunosuppression, elderly, VFR, and expatriate), then the “average” rate of disease acquisition or vaccine reaction should be raised or lowered according to the RR (or OR) estimates. Proportionate morbidities reported from surveillance databases (eg, GeoSentinel) also assess the relative likelihood of presenting with an illness given certain demographic or itinerary factors, and can similarly be considered as providing risk factor data. 11
It is common for research studies to report both crude and adjusted rates. The population studied may not have the same proportion of age, gender, race, destination, etc. as the entire traveling population, and as these demographic and itinerary factors may impact on health outcomes, adjusted results on RR measures provide data that take this into account. To estimate the impact of each individual risk factor “adjusted” for other possible factors in the study, statistical methods such as regression models/multivariate analysis and/or stratification are commonly applied. As with any study, methodological issues such as generalizability, bias (observer, recall, selection, attrition), residual confounders, sample size, and statistical significance need to be considered when interpreting results from studies on risk data.
If the above is not confusing enough, there is yet another layer of complexity. In discussing risk, an astute traveler may be more interested in incremental risks associated with travel than with absolute risks. In other words, the absolute risk of acquiring an illness that occurs globally may be higher, lower, or the same than if travelers stay home. Naturally this depends on the endemicity of disease, not just at their travel destination, but also in their country of origin. Typhoid vaccine recommended for a traveler from the United States going to Africa may be considered unnecessary for a traveler from India with exactly the same African itinerary, as the latter individual may actually be going from high to lower risk region. 16
Other factors of practical interest to travelers trying to decide about uptake of certain vaccines or prophylactic measures are as follows: (1) the magnitude of disease risk reduction if the intervention proceeds; (2) the severity or consequences of the illness if acquired; (3) the magnitude of potential harms from an intervention; and (4) the severity and consequences of the harms associated with the intervention. The absolute magnitude of risk reduction (also known as the risk difference) will be driven by the baseline and RRs of disease, as well as by the effectiveness of the intervention.
In public health measures directed to the general population, the benefits beyond individual protection as well as the financial aspects are relatively more important than in travel medicine, which typically concentrates on protection of the individual. Therefore, public health measures related to the effectiveness of a preventive intervention like the Number Needed to Treat (NNT), which is calculated as the number of patients who need to be treated to achieve the desired outcome for one person, is of relatively lower importance. The traveler may seek maximum protection and may be willing to accept to pay for protection against infectious diseases while from a public health standpoint, a particular intervention may be seen differently. The NNT depends both on vaccine efficacy and on the absolute risk of disease. For example, 1,000 doses of a vaccine may need to be given to avert one case of disease. Similarly, the risk of a vaccine, or treatment hazard, can be measured as the “number needed to harm”: if 5% of people get an adverse drug reaction, then on average for every 20 people you give the drug or vaccine to, one will have reaction. The spectrum of vaccine‐preventable diseases ranges from rare/high individual impact (eg, invasive meningococcal disease, rabies) to frequent/low individual impact (eg, travelers' diarrhea). In both the cases, the vaccine may appear acceptable to the traveler despite the fact that vaccine efficacy and NNT are completely different.
Given all these issues, as well as the lack of risk data for many travel‐associated adverse health outcomes, is it possible to do a pre‐travel risk assessment that will make any sense to the traveler? And how can the messages be conveyed to the average traveler in a way he/she can understand? Should absolute or incremental or RRs or all be discussed? Any numerical discussion about risk will be interpreted by travelers according to their ideas and risk perception: what some people will see as an unacceptably high risk, others will view as a risk they are prepared to accept, even given exactly the same risk data and numbers. For example, a risk of one case of an adverse reaction to a vaccine that has been given to 100,000 people, or one case of illness of 100,000 travelers, may be interpreted as a high risk by some and as negligible by others. Personality, perception, personal experiences (including past travel health), cultural factors, and differences in risk tolerance/risk aversion behaviors will have major impacts on interpretation of risk information and on the ultimate decisions travelers make, yet there has been scant research focus on these issues in the pre‐traveler context. Risk communication is also likely to have substantial influence, yet has also been understudied in travel medicine.
A theoretical example can illustrate many of the complexities: suppose that there are two vaccines which protect against disease X, and that vaccine A has twice the chance of being associated with side effects compared with vaccine B. In deciding the implications of this doubled risk, it needs to be clarified what the magnitude of absolute risk of side effects will be (eg, 1 in 10 to 2 in 10, 1 in 100 to 2 in 100, or from 1 per million to 2 per million). While the RR has doubled in all cases, the absolute risk has increased by somewhere between 1 per million and 1 in 10 (equal to 100,000 per million), depending on the scenario. One can imagine that the same numerical facts could be communicated in different ways, potentially depending on personal preferences of the health care provider. Moreover, the side effects or harms of the intervention will be balanced by the magnitude of benefit: if the side effect is a local reaction versus seizures or death, people will view doubling of the risk in entirely different ways. Risks of commission versus risks of omission may well also be viewed differently: if a vaccine has a risk of side effects (eg, death) of one in a million and the chances of being infected and dying from the disease without vaccination is also estimated at one in a million, despite the equivalent numerical risks, many clinicians and recipients will view these risks unequally and will be resistant to offering the vaccine (“first do no harm” principle).
Travel medicine has definitely progressed scientifically over the last decade, in part because of large multisite databases that have been generated, but there are distinct issues about the traveling population that add unique complexities to the risk discussion. It is unnecessary and unfeasible for practitioners to assess the quality of published studies for all travel health risks, but some awareness regarding the fact that the accuracy of absolute and relative disease measures is dependent on sound study design is important, as is understanding of common risk concepts. Additionally, recognition of the specific difficulties associated with studying travelers because of their extreme diversity and their mobility is important when citing reported risk magnitude data. While it is increasingly common to aim for an “evidence‐based” approach to decision making, the limitations even of the best study designs must be acknowledged, and travel risk data can probably at best give us an idea of the likely risk magnitude for prioritizing risk interventions. Even absolute risk measures (proportions, rates) which require labor‐intense prospective studies have numerator problems such as difficulties in obtaining accurate diagnoses during trips and denominator problems including the fact that the risks may be non‐uniform throughout the travel period, and are subject to biases. Moreover, the actual risks of many illnesses change over time, even from week to week or month to month, and it is obviously not feasible to have numerical data for each time period. Additionally, inferring risks from endemic populations may be incorrect, especially for diseases for which partial or complete immunity develops. Many studies on risks among travelers define risk factors rather than absolute risks; such risk factor data may be helpful in deciding whether an individual's risk is likely to be higher or lower than “average,” but cannot provide information about the actual magnitude of the underlying risk. There are issues of incremental risk compared with those of staying at home and issues of cumulative risk over multiple trips that add more complexity. Cost‐effectiveness and affordability issues, which are beyond the scope of this article and therefore have not been discussed in detail, are also extremely important in practical decision making.
It is important that health professionals understand risk concepts, and that risk decisions are based on the best available risk data despite the methodological limitations discussed. However, the actual decision about whether a risk is unacceptably high or acceptably low and whether or not an intervention will be accepted rely not only on risk numbers or clinical severity of outcomes, but also heavily on risk communication and—presumably even more importantly—on risk perception of both the health provider and the traveler.

This plane “crash” illustrates the risks borne by travelers (see the article by Leder et al., pages 13–20). Fortunately in this case, this plane is part of the architecture of a restaurant located on one of the beaches in Preah Sihanuk (formely known as Kampong Som), Cambodia. This beach is quite popular with tourists. Photo Credit: Eric Caumes.
The authors state they have no conflicts of interest.
Steffen R Behrens R Hill DR , et al. Vaccine preventable travel health risks: What is the evidence — what are the gaps? J Travel Med 2014 ; doi: 10.1111/jtm.12171 [Epub ahead of print].
Google Scholar
Noble LM Willcox A Behrens RH . Travel clinic consultation and risk assessment . Infect Dis Clin North Am 2012 ; 26 : 575 – 593 .
Porta M . A dictionary of epidemiology . 5th Ed. New York : Oxford University Press , 2008 .
Mutsch M Tavernini M Marx A , et al. Influenza virus infection in travelers to tropical and subtropical countries . Clin Infect Dis 2005 ; 40 : 1282 – 1287 .
Mutsch M Spicher VM Gut C Steffen R . Hepatitis A virus infections in travelers, 1988‐2004 . Clin Infect Dis 2006 ; 42 : 490 – 497 .
Angst F Steffen R . Update on the epidemiology of traveler's diarrhea in East Africa . J Travel Med 1997 ; 4 : 118 – 120 .
Gordis L . Epidemiology . 5th Ed. Philadelphia : Saunders, Elsevier , 2013 .
Greenaway C Schofield S Henteleff A , et al. Statement on international travellers and typhoid by the committee to advise on tropical medicine and travel (CATMAT) . Can Commun Dis Rep 2014 ; 40 : 60 – 70 .
Steffen R Tornieporth N Clemens SA , et al. Epidemiology of travelers' diarrhea: details of a global survey . J Travel Med 2004 ; 11 : 231 – 237 .
Behrens RH Carroll B . The challenges of disease risk ascertainment using accessible data sources for numbers of travelers . J Travel Med 2013 ; 20 : 296 – 302 .
Leder K Wilson ME Freedman DO Torresi J . A comparative analysis of methodological approaches used for estimating risk in travel medicine . J Travel Med 2008 ; 15 : 263 – 272 .
Behrens RH Cramer JP Jelinek T , et al. Efficacy and safety of a patch vaccine containing heat‐labile toxin from Escherichia coli against travellers' diarrhoea: a phase 3, randomised, double‐blind, placebo‐controlled field trial in travellers from Europe to Mexico and Guatemala . Lancet Infect Dis 2014 ; 14 : 197 – 204 .
Steffen R Cramer JP Burchard G , et al. Efficacy of a travelers' diarrhea vaccine system in travelers to India . J Travel Med 2013 ; 20 : 374 – 379 .
Angell SY Behrens RH . Risk assessment and disease prevention in travelers visiting friends and relatives . Infect Dis Clin North Am 2005 ; 19 : 49 – 65 .
Woodward M . Epidemiology: study design and data analysis . 3rd Ed. Florida : Chapman & Hall , 2013 .
Piyaphanee W Steffen R Shlim DR , et al. Travel medicine for Asian travelers—do we need new approaches? J Travel Med 2012 ; 19 : 335 – 337 .
Freedman DO Weld LH Kozarsky PE , et al. Spectrum of disease and relation to place of exposure among ill returned travelers . N Engl J Med 2006 ; 354 : 119 – 130 .
- consultation
- rejection (psychology)
- risk assessment
- attack rate
- risk perception
- travel medicine
Email alerts
More on this topic, related articles in pubmed, citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1708-8305
- Copyright © 2024 International Society of Travel Medicine
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

IMAGES
VIDEO
COMMENTS
From January 1, 2023, Travel Medicine and Infectious Disease will become a full gold open access journal freely available for everyone to access and read. All articles submitted after October 14, 2022, are subject to an article publishing charge (APC) after peer review and acceptance.Learn more about hybrid journals moving to open access. $3270
The Journal of Travel Medicine publishes cutting-edge research, consensus papers, policy papers and expert reviews in the field of travel medicine in the interface with other disciplines. Learn why it's the perfect home for your research. ... Kyasanur Forest disease in India: a case report . A 'ring in ring' skin infection in a returning ...
Travel medicine. The use of rotational thromboelastometry to guide management following Bitis nasicornis envenoming. Charles Nye, David Griffith Lalloo, Timothy Hooper. BMJ Case Reports CP Apr 2024, 17 (4) e258319; DOI: 10.1136/bcr-2023-258319 . ... Case Reports Oct 2017, 2017 bcr-2017-220959; ...
A specialized travel medicine clinic or a medical facility ... Recurrent Transient Ischemic Attacks and Stroke Due to Carotid Dissection During Air Travel: A Case Report, Cureus, (2023 ...
Travel Med Infect Dis. 2017 Mar-Apr;16:49-51. doi: 10.1016/j.tmaid.2016. ... 2 Institute of Occupational and Social Medicine, RWTH Aachen Technical University, Pauwelsstr. 30, D-52074 Aachen ... We report the case of a 12-year old American female who survived a PAM infection and propose a new drug therapy which includes the antimicrobial drug ...
Refugees, immigrants and migrants often have barriers to travel medicine. Community Advisory Boards (CAB) are a vital but underutilized tool for understanding and meeting healthcare needs and challenges, providing communities with a voice, and finding solutions. ... We report in Madrid (Spain) a case of intraventricular neurocysticercosis in a ...
Clinical characteristics and management of neurocysticercosis patients: a retrospective assessment of case reports from Europe. Dominik Stelzle and others. Journal of Travel Medicine, Volume 30, Issue 1, January 2023, taac102, ... Journal of Travel Medicine, Volume 30, Issue 1, January 2023, ...
Tropical Diseases, Travel Medicine and Vaccines welcomes well-described reports of cases that can be used for educational purposes or that describe unusual features of the disease, its treatment, transmission or control. When describing clinical cases, the authors are requested to provide written and signed consent to publish the information from the patients or their guardians; case reports ...
Travel medicine is an exciting interdisciplinary specialty that has developed rapidly in response to the needs of the travelling population worldwide. International arrivals worldwide by any form of transport were around 664 million in 2000 (fig 1), and the World Tourist Organisation has predicted an 80% increase in travel to long haul destinations between 1995 and 2010.12 Specialists in ...
The future of travel medicine should continue to harness these novel platforms in the clinical, research, and educational arenas. ... An insightful report on the response of the travel medicine community to the COVID-19 pandemic. ... Conducting mass gathering events during the COVID-19 pandemic: a case study of Kumbh Mela 2021 as a potential ...
ABSTRACT. Travelers to Chagas disease endemic regions of Latin America may be at risk for Trypanosoma cruzi infection. We report a 67-year-old woman who screened positive for T. cruzi infection while donating blood. The patient had a history of an unusual febrile illness and marked swelling of the face sustained at age 10 after camping in northern Mexico that led to a 3-week hospitalization ...
GeoSentinel also includes 164 affiliate members (formerly referred to as network members) who report sentinel or unusual travel medicine cases but do not enter data into the GeoSentinel database. ... Zika virus infection in a Massachusetts resident after travel to Costa Rica: a case report. Ann Intern Med 2016;164:574-6. https: ...
Method: We reported a patient developed mucormycosis during post-COVID period. We searched literature to describe the incidence, clinical features, and outcomes of COVID-19-associated mucormycosis. Demographic features, risk factors, clinical features, diagnostic methods, treatment and outcome were analyzed. Results: We describe a 54-year-old ...
Travel medicine must adapt to serve the changing profile of travellers, ... Effectiveness of massive testing and intensive case and contact tracing. ... 5-year intervals: 1998-2002, 2003-2007, 2008-2012 and 2013-2018). This analysis focuses on infectious diseases reports, constituting the vast majority of EuroTravNet records. Although ...
Main message. Travel medicine is a highly dynamic specialty that focuses on pretravel preventive care. A comprehensive risk assessment for each individual traveler is essential in order to accurately evaluate traveler-, itinerary-, and destination-specific risks, and to advise on the most appropriate risk management interventions to promote health and prevent adverse health outcomes during travel.
Physician passengers provided medical assistance in 48.1% of in-flight medical emergencies, and aircraft diversion occurred in 7.3%. Of 10,914 patients for whom postflight follow-up data were ...
Enterotoxigenic E. coli (ETEC) is the leading pathogen in travelers' diarrhea. 5 Common health problems among travelers include circadian desynchronosis (jet lag), sunburn, dehydration, and water‐related problems (eg, exposure to infectious agents, near‐drowning, boating, and diving accidents).
The Travel Medicine Specialist. ... No reports of travel-acquired infection; sexual activity during travel might lead to HPV and other sexually transmitted infections. Influenza: ... Rare cases have occurred, estimated at <1 case/1 million travelers to endemic countries. However, the severe neurologic sequelae and high fatality rate warrant ...
Medical tourism—people traveling abroad with the expressed purpose of accessing medical treatment—is a growing phenomenon associated with globalization. 1 This includes cheaper and more widely available air travel and cross‐border communication through the Internet, which allows medical providers from one country to market themselves to patients in another. 2 At the same time, increased ...
Introduction: the importance of case reports. Case reports are a time-honored tradition in the medical profession. From Hippocrates (460 B.C. to 370 B.C.), and even arguably further back since the papyrus records of ancient Egyptian medicine (c. 1600 B.C.) to modern day, physicians of all specialties have described interesting cases involving all specialties [1,2].
Case report. Malaria is a potentially lethal parasitic disease due to infection by Plasmodium parasites, transmitted by Anopheles mosquito vectors. Various preventative measures may be recommended for travellers who visit endemic areas. The diagnosis is generally evoked in the context of a febrile patient returning from an endemic zone.
• Difficulties confirming diagnoses for illnesses that occur during travel : Case reports/case series: Not applicable ... all activities) in every type of traveler (both genders, all ages, and all co‐morbidities) cannot be calculated. The travel medicine advisor must therefore take the best absolute risk measure (if there is one), and then ...
The Diverse Spectrum of Invasive Meningococcal Disease in Pediatric and Adolescent Patients: Narrative Review of Cases and Case Series, Infectious Diseases and Therapy, 13, 2, (251-271), (2024 ...