Appointments at Mayo Clinic
Foot swelling during air travel: a concern, what causes leg and foot swelling during air travel.
Leg and foot swelling during air travel is common. It's usually harmless. The most likely reason for it is sitting for a long time without moving during a flight.
Sitting with the feet on the floor for a long time causes blood to pool in the leg veins. The position of the legs while seated also increases pressure in the leg veins. This plays a role in swelling by causing fluid to leave the blood and move into the surrounding soft tissues.
A dangerous blood clot called deep vein thrombosis (DVT) sometimes causes leg swelling. But the risk of getting DVT on an airplane is very low for healthy people, especially on flights that last under four hours. In general, the chance of getting DVT starts to rise on flights over 12 hours.
You can reduce foot and leg swelling, and lower your risk of blood clots, by wearing compression stockings on a long flight. The stockings apply pressure to the lower legs.
If you notice swelling in one leg that doesn't go away or starts within two weeks of a long flight, get a health care checkup right away. The swelling might be a symptom of DVT or another condition that needs treatment. If you have a higher risk of blood clots, talk with a member of your health care team before you fly.
John M. Wilkinson, M.D.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.

From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Hand swelling during exercise: A concern?
- Clarke MJ, et al. Compression stockings for preventing deep vein thrombosis in airline passengers (review). Cochrane Database of Systematic Reviews. 2021; doi:10.1002/14651858.CD004002.pub4.
- Douketis JD, et al. Prevention of venous thromboembolism in adult travelers. https://www.uptodate.com/contents/search. Accessed June 27, 2023.
- Blood clots and travel: What you need to know. Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/dvt/travel.html. Accessed June 27, 2023.
- AskMayoExpert. Health considerations for air travelers. Mayo Clinic; 2022.
- Jong EC. Jet health. Travel and Tropic Medicine Manual. Elsevier; 2017. https://www.clinicalkey.com. Accessed June 27, 2023.
- Smith CC. Clinical manifestations and evaluation of edema in adults. https://www.uptodate.com/contents/search. Accessed June 27, 2023.
- The effect of compression stocking on leg edema and discomfort during a 3-hour flight: A randomized controlled trial. European Journal of Internal Medicine. 2019; doi:10.1016/j.ejim.2019.01.013.
- Nishmura N, et al. Gravity-induced lower-leg swelling can be ameliorated by ingestion of α-glucosyl hesperidin beverage. Frontiers in Physiology. 2021; doi:10.3389/fphys.2021.670640.
- Wilkinson JM (expert opinion). Mayo Clinic. July 4, 2023.
Products and Services
- Available Compression Products from Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Mitral valve clip to treat mitral regurgitation: Bob's story
- Mitral valve overview
- Chronic sinusitis
- Cold urticaria
- Compression bandaging
- Mitral valve regurgitation
- Myocarditis
- Robotic heart surgery treats mitral regurgitation: Ed's story
- Scleroderma
- Symptom Checker
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Foot swelling during air travel A concern
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.

10 Ways to Avoid Swollen Feet and Ankles During Travel
Cramped seats, salty snacks, and long periods of sitting are a recipe for uncomfortable swelling. But these expert tips can help you prevent discomfort and deal if you experience the condition.
When you fly, you're trapped in a tiny seat in an enclosed area without much room to move — so it’s no wonder you may land with swollen feet. And although leg and foot swelling during air travel is common and typically harmless, per the Mayo Clinic , it can still put an uncomfortable damper on your travel plans.
Luckily, there are things you can do to prevent it. Here, three doctors share their tips on how to avoid swollen feet and ankles during air travel and what you can do if you do experience some swelling.
Why Do Your Feet Swell When You Fly?
It comes down to inactivity during flights, says Lauren Wurster, a doctor of podiatric medicine and an Arizona-based podiatrist and spokesperson for the American Podiatric Medical Association (APMA) . “The longer you are sitting still, the more gravity pulls fluid down to your feet and ankles,” she explains. “Also, the position you are sitting in, with your legs bent, increases the pressure on the veins and increases swelling.”
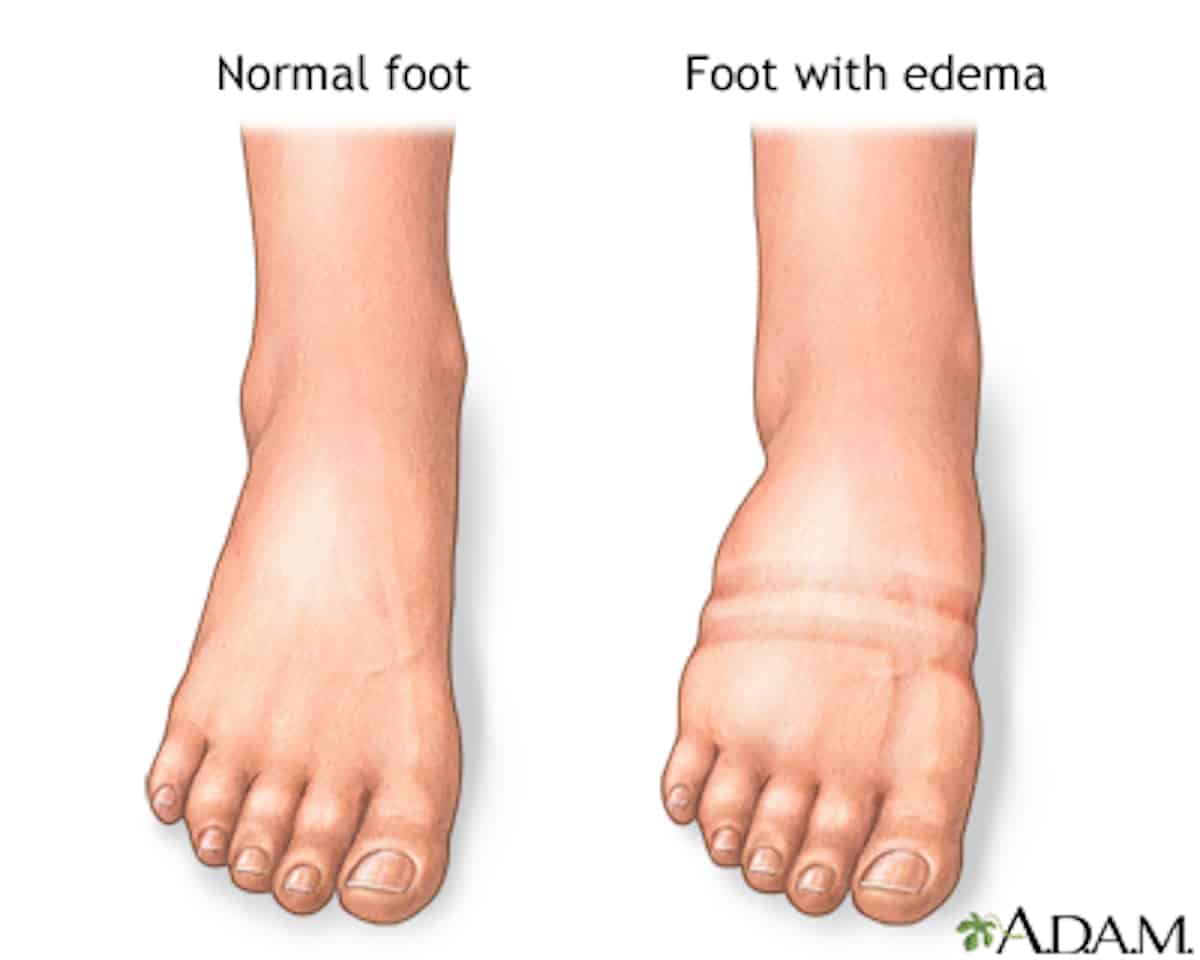
When sitting, the muscles that help pump fluid out of your legs are not active, says Timothy Ford , a doctor of podiatric medicine and an associate professor in the department of orthopedics at the University of Louisville School of Medicine. As a result, blood may pool in your feet, leading to swelling, medically known as edema.
Travel day habits can also contribute to feet swelling, says Todd Taylor, MD , an associate professor at Emory University’s department of emergency medicine. “As we travel, we tend to eat in restaurants, eat snacks, and consume other processed foods high in salt. This will raise our salt level in our body, increasing the fluid and again contributing to dependent edema [leg swelling].”
Finally, Dr. Wurster notes, there are certain health conditions that can cause swelling in your legs or feet regardless of your altitude, including heart, liver, thyroid, and kidney conditions; pregnancy; and venous insufficiency. (That said, if minor swelling occurs only during air travel, it’s more likely due to the lack of mobility in your legs than an underlying medical concern.)
Fortunately, there are steps you can take to reduce the likelihood of leg swelling during travel and potentially reduce swelling when it happens. Read on for the experts’ tips.
10 Ways to Prevent Swollen Feet During Travel
1. drink water throughout your travels.
Even though it might feel counterintuitive to add more fluids to your body when it’s retaining fluid, the Cleveland Clinic notes that drinking more water can help clear your system of excessive sodium, which contributes to fluid retention . Drink plenty of water the day before and the day of the trip so that you don't start out dehydrated. Bring a big bottle of water with you on the plane, and refill it as needed to stay hydrated. Another plus to drinking a lot of water: It’ll motivate you to get up and walk to the bathroom when nature calls.
2. Watch Your Diet and Avoid Salty Foods
Avoid salt as much as possible on the day of and even the day before. Salt can cause you to retain fluid, notes the Mayo Clinic , which can make your feet swell even more.
3. Reach for a Pair of Compression Socks
Your flight day outfit should include compression socks that reach up to your knees. “I really love this one as they are really effective,” says Dr. Taylor. And these days, they don’t have to be boring! Endurance athletes use compression socks during and after racing, so you can find cool colors and patterns. The APMA also offers a list of its approved socks and hosiery . “Avoid normal socks that constrict above the ankle," suggests Ford.
4. Stretch Your Legs on Long Flights
If possible, get up to walk the aisle every hour or so, especially on flights over two hours, recommends Dr. Ford. Standing or walking to the bathroom can get your blood flowing and help combat swelling.
5. Give Your Feet a Seated Workout
Even when you can't get up and walk around, you can work the muscles in your feet. Point your toes up and down, then side to side to get your feet moving. The focus here is flexing the muscles in your feet, calves, and legs to get them engaged after a long period of inactivity, says Wurster.
6. Stow Bags Overhead to Maximize Legroom
If your feet are fighting for space with your carry-on bags, they'll be cramped even more into awkward positions that cut off the blood supply. Store your bags overhead.
7. Don't Cross Your Legs
Your circulation is already slower when you're sitting for hours, so don't cut it off even more by crossing your legs. ( Past research has also suggested crossing the leg at the knee results in a significant increase in blood pressure for people with hypertension.)
8. Shift Positions Regularly While Seated
The position of your legs when you are seated increases pressure in your leg veins, explains the Mayo Clinic, so don’t stay locked in one position for too long. Wurster advises shifting your seated position frequently to avoid being in one position for too long.
9. Elevate Your Feet to Help Blood Flow Return
Keeping your legs raised can help improve circulation, per the Cleveland Clinic . Wherever possible, try to raise your legs and feet; if there's no one next to you, stretch out and prop your feet up across the seats.
10. Opt for Comfy and Practical Footwear
Ford recommends wearing slip-on shoes on travel days because “they can be removed easily and allow you to massage your feet or exercise your feet." A foot massage could help stimulate blood flow — just be conscious of your neighbors. (This might be one tip to save for a road trip rather than a crowded plane.)
How to Reduce Swelling in Feet After Travel
Once you’ve landed, you can use a lot of the same tools to reduce swelling after your travel: “Stay hydrated, move around, and wear compression socks,” says Wurster. “Also, be mindful of what you're eating and avoid foods too high in sodium because that can also add to further swelling.”
If you can’t move around, elevating your legs after traveling can also help, says Taylor. Use gravity to your advantage and prop your feet up to help your circulation move that blood around. For those who can manage it, the Cleveland Clinic recommends a yoga pose called Viparita Karani, where you lay with your back on the ground perpendicular to a wall and then press your legs up against the wall. (Steer clear of this pose if you’re living with uncontrolled high blood pressure, glaucoma , congestive heart failure , kidney failure, or liver failure, though.)
When Should You See a Doctor About Swollen Feet and Legs?
“Usually, the swelling isn't serious and will improve with activity after the flight lands,” says Wurster. “However, in long periods of travel and with people with certain risk factors, the swelling can be a sign of a blood clot in the calf, also known as a deep vein thrombosis . This can be very serious if not treated appropriately.”
Wurster and Taylor say any of these red flags would be a reason to go to the nearest emergency department for an evaluation:
- Severe leg swelling
- One leg bigger than the other
- Swelling, pain, redness, and warmth to one of the calves
- Shortness of breath
MORE TIME TO TRAVEL
Explore new places and savor new tastes
Swollen Ankles When Flying: 8 Questions and Answers
Have you ever gotten off a plane, looked down at your swollen legs after flying — and become alarmed at their size?
Rest assured. It’s usually not a serious problem if it is time-limited.
Swollen ankles, feet, and legs are common among travelers—especially older ones. With aging, many people tend to experience leg and foot swelling due to excess fluid buildup in the tissues.
“Edema” is the medical term for this condition. Colloquially, some people call them “flight feet.”
Although temporary, swollen legs can be more than unattractive.
Depending on the extent of the swelling, you may experience discomfort from the stretching of your skin, or have a tough time getting your shoes back on (if you’ve taken them off during a flight).
This post may contain affiliate links. This means that I may receive compensation if you click a link, at no additional cost to you. For more information, please read my privacy and disclosure policies at the end of this page.
Jump ahead to...
QUESTIONS AND ANSWERS ABOUT SWOLLEN ANKLES WHEN FLYING

What causes leg swelling when you’re flying?
The amount of legroom on flights seems to be constantly shrinking.
And depending on the placement of your seat and the pattern of turbulence, it can be difficult to get up and stretch, especially on long-haul flights (four hours or more) or lights-out overnight flights across the ocean.
Being seated in one fixed position in a cramped space for a long period of time causes fluid to leave the blood and move into surrounding tissues.
Is swelling more prevalent with age?
Aging makes many things more complicated, including leg swelling.
Older people are prone to experience more significant swelling and tightness after long flights than younger people for a variety of age-related reasons.
For example, their veins don’t circulate blood as well as they used to, and they are more likely to be taking certain prescribed medications (e.g., blood pressure-lowering medications like calcium channel blockers).

What can you do to prevent swollen ankles when flying?
There are a number of common sense ways to prevent or reduce swollen legs and ankles on long flights:
- Maintain a healthy body weight,
- Seek out flights and seats with more legroom, when possible,
- Limit salt intake on the day of and during the flight (I always wonder why airlines offer pretzels and salted peanuts with drinks),
- Keep hydrated and avoid excessive alcohol intake,
- Avoid caffeine intake as well, and while it may seem counterintuitive, try to increase water intake,
- Opt for loose, non-binding clothing and shoes that easily slip off (I love this pair of Skechers because they are lightweight and easy to get on an off),
- Wear compression stockings (see below),
- Remove your shoes when it’s safe to do so,
- Avoid keeping your legs crossed for long periods of time,
- Wiggle your toes and move your legs in circles during the flight, and tighten and loosen your leg muscles,
- To improve blood flow, several airlines recommend pulling each knee to your chest and holding it there for 15 seconds, repeating this up to 10 times (CDC, Clots During Travel , accessed 10/17/23).
- Get up, move, and walk up and down the aisle several times during the flight (your bladder will thank you, too).
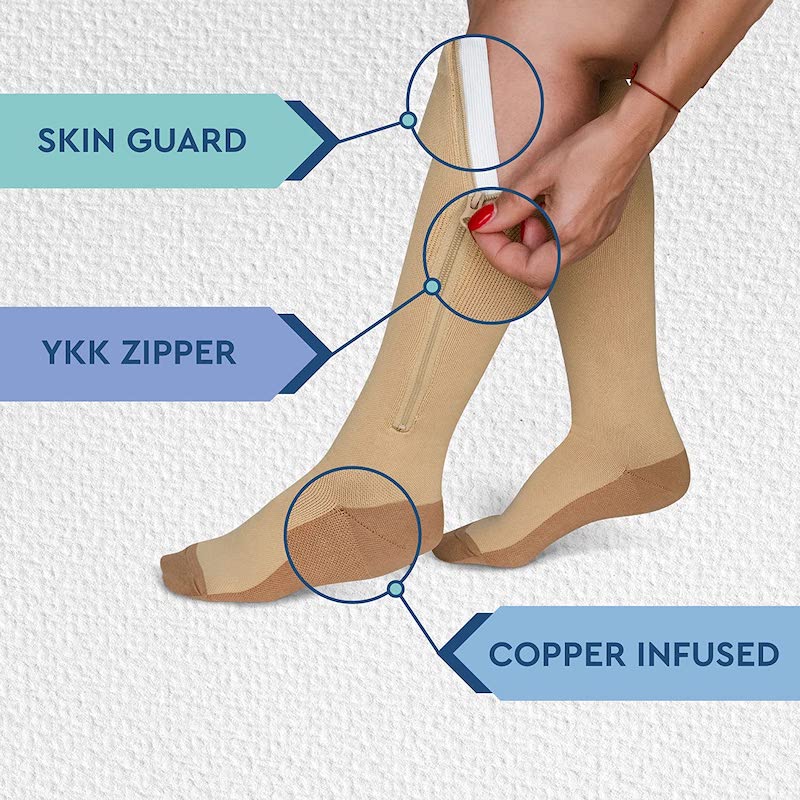
What do I need to know about compression socks for swollen ankles when flying?
A systematic Cochrane literature review looked at the effects of wearing compression socks on flights of at least four hours duration.
It concluded with high certainty that the use of compression socks had a substantial impact on lowering the incidence of symptomless DVT and lower certainty evidence that it reduced edema of the lower legs.
Healthline describes three different types of compression socks:
- Graduated compression socks, usually prescribed by a healthcare professional
- Nonmedical support hosiery (intended to provide support and improve circulation), widely available in stores and online
- Anti-embolism stockings , also prescribed by a professional, are intended to prevent DVT .
Although compression socks aren’t likely to pose problems for most individuals, wearers do need to be cautious of potential skin problems (burning, chafing, bruising, and broken skin) that can lead to infections and any signs of impaired circulation on a long flight.
Getting them on can be challenging too, but practice makes perfect. Doctors recommend getting used to them by wearing them for a few hours at first and gradually increasing the time you wear them.
We recently learned about zip-up compression socks that take the pain out of trying to get them on and off. Another alternative is to ask your spouse or travel companion for help.
Does recent surgery increase the risk of DVTs?
Evidence suggests that long-distance air travel post-surgery (e.g., hip and knee replacements) can increase the risk of leg blood clots.
Therefore, it is essential for travelers to consult their physician concerning how soon after surgery they can safely fly and what precautions they should take to minimize the risk of DVT when they do.
In general or orthopedic surgery settings, research on the efficacy of graduated compression socks has been shown to be a literal lifesaver.
A meta-analysis of 19 studies involving 1681 individuals found them effective in lowering the risk of DVT in hospitalized patients. More effectiveness research needs to be conducted on outpatients.
Is the use of aspirin recommended to prevent blood clots?
An article in AFAR notes that there is no available data to suggest that travelers take aspirins to prevent blood clots on long-haul flights.
However, taking into account an individual patient’s health history and risk factors (e.g., gastrointestinal bleeding), some doctors might recommend its use or prescribe an anticoagulant drug to prevent blood clots. As noted above, the risk of DVT may be elevated after recent surgery.
But it is always advisable to check with your physician before taking aspirin before flying.
If your legs swell after flying, what can you do afterward?
- If your legs, ankles or feet are swollen after getting off the plane, it’s wise to take off your shoes and elevate your legs (above your heart) to lessen the swelling.
- It also could be useful to soak your legs in lukewarm water, or gently massage them once you get to your destination.
- Try to minimize eating foods with excessive salt until you see the swelling of your ankles and/or legs go down.
Is leg swelling dangerous?
According to a recent publication from the Mayo Clinic , swelling caused by inactivity during travel (e.g. on planes or long car rides) is usually harmless .
When to seek medical attention for leg swelling
However, it is prudent to seek medical attention if you experience any of the following, especially if the swelling is frequent and persistent:
- Swelling that is red or warm to the touch (this could be a sign of a clot),
- Pain, tenderness or swelling only in one leg (as opposed to both),
- Any chest pain associated with swelling, and
- Swelling that doesn’t dissipate after several hours of activity.
- Mayo Clinic: What causes leg and foot swelling during travel?
- Healthy Advice: Preventing DVT when traveling
- Medline Plus: Foot, leg and ankle swelling
- PubMed: Prevention of edema, flight microangiopathy and venous thrombosis in long flights with elastic stockings
- Medical News Today: What can cause socks to leave marks on legs?
- Centers for Disease Control: Clots During Travel
A Mini-Guide to Compression Socks
What to look for when buying compression socks.
- Make sure they offer the correct amount of compression recommended by a healthcare professional
- Find your correct size to ensure a good fit (including calf width); most vendors provide sizing guides
- Choose breathable, moisture-wicking materials
- Read the return policy in case the compression socks don’t fit or aren’t comfortable
- To maintain them at their best, wash them in a mesh laundry bag and let them air-dry
- Remove them at bedtime and never weak them to sleep
Benefits of Compression Socks
- Reduce pain, swelling and inflammation
- Help prevent fluids from pooling in the feet and ankles
- Promote increased flow toward the heart
- Help prevent blood clots and embolisms
Lily Trotter Wide-Calf Compression Socks for Women

The Lily Trotter line of socks comes in a number of great looks and sizes.
The idea of designed compression socks may sound like an oxymoron but women no longer have to sacrifice fashion for fitness. These athletic support socks are made with graduated compression measured at 15-20 mmHg.
READ MORE OR PURCHASE
Hi Clasmix Medical Grade Compression Socks for Men & Women

These knee-highs offer graduated compression at 20-30 mmHg and come in a variety of sizes and colors.
With more than 40,000 ratings, they are a best seller on Amazon.
Jobst Unisex Relief Stockings

These medical grade 20-30 mmHg compression socks come with a closed-toe style that offers a roomy toe allowance for those who want extra wiggle room.
They also come in an open-toe version for even more toe room and in graduated compression at 30-40 mmHg.
Also on MoreTimeToTravel:
Ever find a rash around your ankles when traveling in warm climates or taking long walks? Read on:
Golfers Vasculitis: A Common But Often Misdiagnosed Boomer Travel Malady
Save to Pinterest!!
Similar Posts

The sharing economy has changed the face of travel
In a phenomenon dubbed the “sharing economy” or “peer-to-peer marketplace,” Americans are traveling in ways that were virtually unheard of a decade ago.

Traveling with Friends: Always popular but on the upswing
Traveling with friends is nothing new but because of the confluence of demographics and economics, it’s a phenomenon that appears to be gaining popularity across all age groups

Lounge Review: Airspace Lounge at JFK Terminal 5
You have to look hard to find the Airspace Lounge at JFK airport in NYC. The only lounge in Terminal 5 is tucked in a space at its far end, across from Gates 24 and 25.

How to tag your bag…and give it personality
I wrote this short piece about how to tag your bag a while ago for the Chicago Tribune that seems to have stood the test of time. It’s still important to tag it, especially if you are planning holiday travel! Fire-engine red and royal blue may be the new black, but it’s still pretty tough…

Foolproof Tips For Fighting Jet Lag
Experiencing jet lag is almost inevitable after most long haul flights but there are some simple ways to minimize the effects.

Take the MTA Bus: Best Senior Travel Bargain in NYC
You might have called me a bus snob. I hadn’t used an MTA bus in NYC since my college days. But after depending on city buses exclusively last week, I’ll tell you why I prefer them.
20 Comments
Excellent article! This just became an issue with me. Now I swear by compression socks and re-hydration products in addition to lots of water.
I’m curious…what kind of re-hydration products do you use?
Maintaining a healthy body weight is probably the one piece of advice that may be difficult to achieve on the fly—so to speak. 😉 I’ve definitely noticed that it’s harder to slip my shoes back on after a flight.
Yes, that’s a battle to be waged on the ground!:-)
Maintaining a healthy body weight is most important. My feet and ankles used to swell on long road trips, so I began stopping every hour or so to walk around to prevent this. Now I can do a 6 hour drive with one stop and my ankles don’t swell at all.
My doctor told me there’s usually no worry if both of your ankles swell. The time to be concerned is if only one side is swollen because it could be a sign of something else more serious like a blood clot.
Good advice from your doc! Congratulations on your weight loss. You’re more fit to travel!
Very helpful, thank you. It happened to me once on a cruise and just recently on a 4-hour fight. For me getting my feet above my heart always works. That and loads of water. –MaryGo
People make the mistake of thinking that cruises are sedentary but most travelers do far much more walking and standing than they usually do.
Your timing is epic. This has never happened to me before except just a few days ago. We took a red eye from Kauai (used miles, you take what you can) I noticed that both of my feet were swollen in the car on the way home. Kind of freaked me out! Since is was an overnight flight, I only got up once. I also crossed my legs a great deal. I won’t let this happen again.
You look like a leg-crosser!;-)
Great article Irene! I’m a huge believer in compression socks and wear them on all flights. I even use them for trade-shows or all day walking they make a big difference.
You are one of the few. Many people dread putting them on.
So far — knock on wood — I’ve been lucky and never had swollen ankles. I always drink a lot of water on flights, and, of course, that means I make multiple trips to the toilet, which lets me stretch a bit. And in most planes I’m too tall to be able to cross my legs, so I don’t do that either. Thanks for the tips, though. I suppose it’s just a matter of time till this starts happening to me too on long flights!
I think genetics makes some people more prone than others. You may be among one of the lucky ones!
What a great article people often avoid writing about these things as they think they are not interesting. Will bookmark for our next flight great tips to help stop the cursed swollen ankles.
Hope it helps!
My sister-in-law always gets swollen ankles on even a relatively short flight (3-1/2 hours) but not on much longer road trips of several hundred kilometres. She does everything possible – excercises; walking, elevation of legs, etc. – but nothing works. She said that as soon as she comes back home the swelling goes down. I was a bit dubious, until this happened to me also. Long car trips cause a little edema, but a 33-4 hour flight has my ankles and feet hugely swollen, and staying like that for days and days. When I came home, all of the swelling had gone by the next morning. So, I’m not sure that it has a great deal to do with inactivity.
“Being seated in one fixed position in a cramped space for a long period of time causes fluid to leave the blood and move into surrounding tissues.”
This is more likely to occur in a plane than a car because there is less space and opportunity to move around. It’s important to wiggle your toes, move your feet, and stand up and walk around, whenever possible.
How can you keep hydrated when every small bottle of water costs £2. You cannot take any water onto the plane for”security ” reasons
Most airlines provide beverage service with water. You can also purchase a large bottle of water after you pass through security.
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Notify me of followup comments via e-mail
Save my name, email, and website in this browser for the next time I comment.
Free shipping over $75 USD
Get the most effective travel essentials here.

Learn about our story and our products.

- Try FLIGHTFŪD We're currently experiencing turbulence

Your carry on baggage
Free US Shipping on Orders $39+
Before you take off, we think you may also love this.

Water Bottle
- Try FLIGHTFŪD
- Swelling When Traveling? Here’s Why It Happens + What to Do
Jet lag , bloating , and a reduced immune system are all unfortunate but well-known side effects of travel.
But there’s another common and equally annoying side effect: swelling.
If you’re a frequent flyer, you’ve likely been a victim of swelling at some point. Swollen feet after a long flight, swollen face after the loss of sleep , or swollen fingers from the heat of a tropical destination have probably happened to you before.
Swelling happens to us all differently, and it can be hard to predict when and where it will happen. This article will cover why swelling when traveling happens and 10 ways to prevent or treat it on your next trip.
Article Guide
Why does swelling happen when you travel, the effects of swelling on your body and your health, how to prevent swelling when traveling, where does swelling happen when traveling, the best ways to relieve swelling when traveling.
Swelling, also called edema, happens when fluids in the body pool in certain areas, causing them to become temporarily larger.
Sometimes swelling is mild and may go away on it’s own in a few hours. Other times it can be uncomfortable and lead to other problems.
While swelling can happen to the body anytime, traveling puts your body through specific conditions that trigger it.
To prevent swelling, we need to understand why it happens when we travel. These are the main travel related causes of swelling in the body.
#1. Swelling from Flying
Swelling is most common for travelers when they are flying.
Those long hours spent sitting in your cabin chair causes blood to pool into your feet and ankles, also known as gravitational edema.
It happens when you are in an upright position for a long time, but aren’t moving.
The result is swollen feet that may even make wearing shoes uncomfortable.
The lower air pressure and humidity inflight also promotes dehydration, which causes your body to retain water and swell.
Read More : Does Flying Dehydrate You? Your Guide to Air Travel Hydration
#2. Your Body Adjusting to a Sudden Change in Climate
Another common cause for swelling while traveling is that your body has to adjust to a sudden change in temperature and climate.
If you aren’t used to hot or humid climates, or you’re flying from winter into a tropical place, swelling in the limbs can happen.
It can affect any body part, from the face, hands, feet, arms or legs to your fingers and toes. This explains why so many travelers find it difficult to remove their rings during and after a trip to a warm-weather destination.
#3. Changes in Diet from Travel
One of the challenges of travel (and why FLIGHTFUD exists!) is that access to high-quality, healthy foods is so limited in airports and on most flights.
While most airlines are improving their food options, historically, airplane food is known to be sodium-filled and made from unhealthy ingredients that can make you bloated and feel swollen in both the face and tummy.
Most people eat more healthfully at home then they do when traveling partially because of the lack of access to nutrient-rich foods. So your diet when you’re going places tends to differ from your normal eating patterns.

This can cause swelling as your digestive system and cells attempt to deal with the onslaught of nutrient-depleted, carbohydrate-heavy travel options.
Plus, if the cuisine in your destination is saltier or heavier than your usual diet, your body will retain water and the dreaded face swelling can happen.
Generally, swelling is harmless and not life-threatening.
Most travelers and frequent flyers will experience mild swelling at some point on their travels. Once relieved, they can go on enjoying their trip as usual.
But sometimes swelling can lead to other issues.
Foot and ankle swelling can make wearing your shoes unbearable, and in some cases it can be uncomfortable to walk for days.
In extreme cases, the swelling can become a serious condition.
If swelling doesn’t go down within a few days after a flight, you seek medical attention. In rare cases, it can even lead to blood clotting. Thankfully, this is very rare and there are loads of ways you can prevent swelling from becoming serious, or from happening at all.
The best way to deal with swelling is to avoid it in the first place.
Here are some key tips on how to lower your chances of experiencing this unfavorable part of travel.
#1. Stay Hydrated

Cabin air on your flight is dryer than the Sahara desert, because it needs to be.
The dry air can lead to dehydration than you’d think.
Among keeping other crucial bodily processes running smoothly, water is vital to keeping your blood circulation from slowing, which is a culprit of swelling.
Since dehydration is such a prevalent travel side-effect that leads to so many other impaired bodily processes and symptoms, it’s crucial to stay hydrated and drink plenty of water before and during your flight.
This is why we developed Flight Elixir as a drink mix . We could have made it in any other form, but we wanted to encourage travelers to stay hydrated.
Ideally, you’ll drink the equivalent of 1, 8-oz glass of water for each in-flight hour.
Once at your destination, keep your Travel Water Bottle on hand so you can stay hydrated and can track how much water you’re drinking.
#2. Wear Loose Clothing
Besides being incredibly uncomfortable, wearing tight clothing, especially jeans or anything that constricts your mid-section, can impair blood circulation which is necessary for keeping fluids flowing in your body and preventing swelling.
This can lead to swelling in the lower body.
Skip the jeans and restrictive clothing and opt for joggers, leggings, or loose-fitting pants to avoid this. Tight shoes and socks should be avoided as well.
#3. Avoid Salty Food
Airplane food is notorious for being salty and just not very healthy overall.
You don’t have to go on a food strike while you fly, but it’s wise to avoid stopping at the convenience store on your way through the airport to grab even more salty snacks. In flight, this means avoiding the peanuts, chips, and pretzels that are commonly given on-board.
While in your destination, it may be harder to say no to the cuisine. After all, a big part of travel is trying new food! But it does pay to be mindful of what you eat, and try to avoid mindlessly snacking.
#4. Drink Alcohol Wisely
One of the best parts about flying is that you can sit back, relax, and order a drink. And we’re realistic. We’re not going to tell you to avoid the inflight indulgences.
Just be aware that alcohol dehydrates your body, which is the main reason you might experience a headache when you overindulge the night before. In response, your body may also react by retaining fluids.
Alcohol depresses the nervous system as well, which can make you more likely to fall asleep in a bad sitting position in-flight after a few drinks, which may cause ankle and foot swelling.
So while we’re not saying you have to skip the wine, definitely consume your spirits wisely inflight (and in general).
Drink in moderation, and drink an extra glass of water for each drink.
It doesn’t hurt to ensure you’re drinking your Flight Elixir as well; with coconut water crystals for electrolytes and vitamins to support your body while you travel, we’ve stacked it with the ingredients you need to help you balance your body.
#5. Come Prepared
Travel can be hard on the body . It promotes dehydration, impairs circulation and exposes you to pollutants which have negative health impacts.
Boost your body’s immunity and function by bringing your own micronutrient supplements.
We’ve created our own all-in-one Flight Elixir made to support the body’s specific needs during travel, with ingredients such as papaya for bloating and indigestion and goji berry, which dilate blood vessels promoting optimal circulation and blood flow.
Another supplement to consider bringing is probiotics, which promote gut health. This will help lessen the impacts of swelling from the foreign food. Omega-3 is also known to be an effective anti-inflammatory to reduce swelling and pain.
Swelling can happen anywhere on the body depending on the cause.
Flying usually leads to swelling in the ankles and feet, while a new travel diet can lead to swelling in the stomach and face. If the weather or change in climate is the cause of swelling, it can happen anywhere in the body, from the neck, limbs, or even hands.
If you do experience swelling during your travels, there are a few ways to find relief quickly. Here are some key tips on what to do if you start to swell.
#1. Stretch and Change Positions
If you feel your ankles and feet swelling in the airplane cabin, try to stretch it out before it gets worse.
Start by rolling your ankle around in a circular motion, extend your legs and stretch, then change positions.
It also helps to continue changing positions and stretching frequently until landing. This keeps blood circulation up, and prevents it from pooling into the lower body again.
#2. Go for Walks in the Airplane Cabin
If you feel the onset of swelling coming, get up and go for a walk.
Even in the flight cabin when there’s limited space, just going for a short walk to the bathroom or down the aisle and back will help.
Walking helps to bring back proper blood circulation, which stops the swelling from getting worse.
#3. Do Cardio
If you find yourself swelling during your trip because of hot weather or from the foreign cuisine, opt for some cardio.
Swimming is a great counter to swelling, so is hiking and jogging.
If the swelling is too painful to do those, going for a brisk walk also works. Exercise helps improve blood flow giving relief from swelling. Plus, the salt your body loses from sweating helps to release excess fluids your body may be holding onto.
#4. Elevate the Limbs
Elevating the swollen body parts will help drain the extra fluid pooled into that area.
If possible, elevate the swollen limb above the heart, on a chair or cushion in bed. If swelling persists, you can elevate the limb overnight while sleeping.
#5. Use Compression Socks
If you are a frequent flyer who often experiences swelling, it may be worth it to get compression socks.
These help to both prevent and relieve swelling. If you find your feet and ankle swelling mid-flight, slip on the compression socks and they’ll safely help to push the extra fluid out of the ankle and foot.
Sarah Peterson
Sarah Peterson is the co-founder and head of marketing at FLIGHTFŪD. She's a travel health expert and after having visited 20+ countries as a digital nomad and flying every 4-6 weeks for business, she became passionate about empowering others to protect their bodies on the go.
Hi Patrick! We discussed via email, but in case anybody else has experienced this problem, we definitely recommend visiting a doctor who specializes in circulatory issues. Circulation can become impaired when you fly and left unchecked, issues can become more serious.
Sounds more like a dvt / a blood clot. Get to a US doctor ASAP
Greetings, I just flew from Bali had a stop over in Istanbul went into Los Angeles and now into Puerto Vallarta. It’s been 5 days and I have my left arm swollen and dark blue as perhaps a capillary broke. I’ve gone to the doctor here in Puerto Vallarta and it seems my pulse and my blood flow is good and although the swelling has lessened it’s still numb tingly and discolored. I understand you’re not positions and not legally entitled to give that advice but what do you suggest I should do? Thank you for your time, Blessings to you and your loved ones sincerely Patrick
Leave a comment
Explore more.
- Healthy Travel
- things to do
- Travel Destinations
- travel essentials
- Where to eat
- where to stay
Popular posts

Featured product
FLIGHT CHECK IN
Check into the VIP News Room. Stay up to date on all flight changes.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Guidelines for Flying With Heart Disease
Air travel is generally safe for heart patients, with appropriate precautions
- Pre-Flight Evaluation
Planning and Prevention
During your flight.
If you have heart disease, you can fly safely as a passenger on an airplane, but you need to be aware of your risks and take necessary precautions.
Heart conditions that can lead to health emergencies when flying include coronary artery disease (CAD) , cardiac arrhythmia (irregular heart rate), recent heart surgery, an implanted heart device, heart failure , and pulmonary arterial disease.
When planning air travel, anxiety about the prevention and treatment of a heart attack on a plane or worrying about questions such as "can flying cause heart attacks" may give you the jitters. You can shrink your concern about things like fear of having a heart attack after flying by planning ahead.
Air travel does not pose major risks to most people with heart disease. But there are some aspects of flying that can be problematic when you have certain heart conditions.
When you have heart disease, air flight can lead to problems due to the confined space, low oxygen concentration, dehydration, air pressure, high altitude, and the potential for increased stress. Keep in mind some of these issues compound each other's effects on your health.
Confined Space
The prolonged lack of physical movement and dehydration on an airplane may increase your risk of blood clots, including deep vein thrombosis (DVT) or pulmonary embolism (PE) . One of the biggest risks for people with heart disease who are flying is developing venous thrombosis.
These risks are higher if you have CAD or an implanted heart device, such as an artificial heart valve or a coronary stent. And if you have an arrhythmia, a blood clot in your heart can lead to a stroke.
One of the biggest risks for people with heart disease who are flying is developing an arterial blood clot or venous thrombosis.
Low Oxygen and Air Pressure
The partial pressure of oxygen is slightly lower at high altitudes than at ground level. And, while this discrepancy on an airplane is typically inconsequential, the reduced oxygen pressure in airplane cabins can lead to less-than-optimal oxygen concentration in your body if you have heart disease.
This exacerbates the effects of pre-existing heart diseases such as CAD and pulmonary hypertension .
The changes in gas pressure in an airplane cabin can translate to changes in gas volume in the body. For some people, airplane cabin pressure causes air expansion in the lungs. This can lead to serious lung or heart damage if you are recovering from recent heart surgery.
Dehydration
Dehydration due to cabin pressure at high altitude can affect your blood pressure, causing exacerbation of heart disease. This is especially problematic if you have heart failure, CAD, or an arrhythmia.
If you experience stress due to generalized anxiety about traveling or sudden turbulence on your flight, you could have an exacerbation of your hypertension or CAD.
Pre-Flight Health Evaluation
Before you fly, talk to your healthcare provider about whether you need any pre-flight tests or medication adjustments. If your heart disease is stable and well-controlled, it is considered safe for you to travel on an airplane.
But, if you're very concerned about your health due to recent symptoms, it might be better for you to confirm that it's safe with your healthcare provider first before you book a ticket that you may have to cancel.
Indications that your heart condition is unstable include:
- Heart surgery within three months
- Chest pain or a heart attack within three months
- A stroke within six months
- Uncontrolled hypertension
- Very low blood pressure
- An irregular heart rhythm that isn't controlled
If you've had a recent heart attack, a cardiologist may suggest a stress test prior to flying.
Your healthcare provider might also check your oxygen blood saturation. Heart disease with lower than 91% O2 saturation may be associated with an increased risk of flying.
Unstable heart disease is associated with a higher risk of adverse events due to flying, and you may need to avoid flying, at least temporarily, until your condition is well controlled.
People with pacemakers or implantable defibrillators can fly safely.
As you plan your flight, you need to make sure that you do so with your heart condition in mind so you can pre-emptively minimize problems.
While it's safe for you to fly with a pacemaker or defibrillator, security equipment might interfere with your device function. Ask your healthcare provider or check with the manufacturer to see if it's safe for you to go through security.
If you need to carry any liquid medications or supplemental oxygen through security, ask your healthcare provider or pharmacist for a document explaining that you need to carry it on the plane with you.
Carry a copy of your medication list, allergies, your healthcare providers' contact information, and family members' contact information in case you have a health emergency.
To avoid unnecessary anxiety, get to the airport in plenty of time to avoid stressful rushing.
As you plan your time in-flight, be sure to take the following steps:
- Request an aisle seat if you tend to need to make frequent trips to the bathroom (a common effect of congestive heart failure ) and so you can get up and walk around periodically.
- Make sure you pack all your prescriptions within reach so you won't miss any of your scheduled doses, even if there's a delay in your flight or connections.
- Consider wearing compression socks, especially on a long trip, to help prevent blood clots in your legs.
If you have been cleared by your healthcare provider to fly, rest assured that you are at very low risk of developing a problem. You can relax and do whatever you like to do on flights—snack, read, rest, or enjoy entertainment or games.
Stay hydrated and avoid excessive alcohol and caffeine, which are both dehydrating. And, if possible, get up and walk for a few minutes every two hours on a long flight, or do leg exercises, such as pumping your calves up and down, to prevent DVT.
If you develop any concerning issues while flying, let your flight attendant know right away.
People with heart disease are at higher risk for developing severe complications from COVID-19, so it's especially important for those with heart disease to wear a mask and practice social distancing while traveling.
Warning Signs
Complications can manifest with a variety of symptoms. Many of these might not turn out to be dangerous, but getting prompt medical attention can prevent serious consequences.
Symptoms to watch for:
- Lightheadedness
- Dyspnea (shortness of breath)
- Angina (chest pain)
- Palpitations (rapid heart rate)
- Tachypnea (rapid breathing)
To prepare for health emergencies, the U.S. Federal Aviation Administration mandates that supplemental oxygen and an automated external defibrillator (AED) is on board for passenger airplanes that carry 30 passengers or more. Flight crews receive training in the management of in-flight medical emergencies and there are protocols in place for flight diversions if necessary.
A Word From Verywell
For most people who have heart disease , it is possible to fly safely as long as precautions are taken. Only 8% percent of medical emergencies in the air are cardiac events, but cardiac events are the most common in-flight medical cause of death.
This means that you don't need to avoid air travel if you have stable heart disease, but you do need to take precautions and be aware of warning signs so you can get prompt attention if you start to develop any trouble.
Hammadah M, Kindya BR, Allard‐Ratick MP, et al. Navigating air travel and cardiovascular concerns: Is the sky the limit? Clinical Cardiology . 2017;40(9):660-666. doi:10.1002/clc.22741.
Greenleaf JE, Rehrer NJ, Mohler SR, Quach DT, Evans DG. Airline chair-rest deconditioning: induction of immobilisation thromboemboli? . Sports Med. 2004;34(11):705-25.doi:10.2165/00007256-200434110-00002
American Heart Association. Travel and heart disease .
Ruskin KJ, Hernandez KA, Barash PG. Management of in-flight medical emergencies . Anesthesiology. 2008;108(4):749-55.doi:10.1097/ALN.0b013e31816725bc
Naqvi N, Doughty VL, Starling L, et al. Hypoxic challenge testing (fitness to fly) in children with complex congenital heart disease . Heart. 2018;104(16):1333-1338.doi:10.1136/heartjnl-2017-312753
By Richard N. Fogoros, MD Richard N. Fogoros, MD, is a retired professor of medicine and board-certified in internal medicine, clinical cardiology, and clinical electrophysiology.

NICOLE POWELL-DUNFORD, MD, MPH, JOSEPH R. ADAMS, DO, MPH, AND CHRISTOPHER GRACE, DO, MPH
Am Fam Physician. 2021;104(4):403-410
Related Letter to the Editor: Helping Adults With Dementia Travel by Air
Author disclosure: No relevant financial affiliations.
Air travel is generally safe, but the flight environment poses unique physiologic challenges such as relative hypoxia that may trigger adverse myocardial or pulmonary outcomes. To optimize health outcomes, communication must take place between the traveler, family physician, and airline carrier when there is any doubt about fitness for air travel. Travelers should carry current medications in their original containers and a list of their medical conditions and allergies; they should adjust timing of medications as needed based on time zone changes. The Hypoxia Altitude Simulation Test can be used to determine specific in-flight oxygen requirements for patients who have pulmonary complications or for those for whom safe air travel remains in doubt. Patients with pulmonary conditions who are unable to walk 50 m or for those whose usual oxygen requirements exceed 4 L per minute should be advised not to fly. Trapped gases that expand at high altitude can cause problems for travelers with recent surgery; casting; ear, nose, and throat issues; or dental issues. Insulin requirements may change based on duration and direction of travel. Travelers can minimize risk for deep venous thrombosis by adequately hydrating, avoiding alcohol, walking for 10 to 15 minutes every two hours of travel time, and performing seated isometric exercises. Wearing compression stockings can prevent asymptomatic deep venous thrombosis and superficial venous thrombosis for flights five hours or longer in duration. Physicians and travelers can review relevant pretravel health information, including required and recommended immunizations, health concerns, and other travel resources appropriate for any destination worldwide on the Centers for Disease Control and Prevention travel website.
Air travel has become increasingly popular over time, despite decreases during the COVID-19 pandemic, with 1.1 billion total passengers in 2019 and most Americans having flown at least once in the past three years. 1 Air travel is generally safe, but especially for the aging U.S. population, the flight environment poses unique physiologic challenges, particularly relative hypoxia, which may trigger adverse myocardial or pulmonary outcomes. To optimize health outcomes, communication must take place between the traveler, family physician, and airline carrier when any doubt occurs about fitness for air travel. Travelers should carry current medications in their original containers as well as a list of their medical conditions and allergies and should adjust timing of medications as needed based on time zone changes. Travelers should also consider available medical resources at their travel destinations and layover locations. Family physicians and travelers can review relevant pretravel health information, including required and recommended immunizations, health concerns, and other travel resources appropriate for any destination worldwide at https://wwwnc.cdc.gov/travel/destinations/list .
Pulmonary Conditions
By law, U.S. commercial aircraft cannot exceed a relative cabin altitude of 8,000 feet (2,438 m) because of the potential for significant hypoxia above this altitude. 2 Most passengers exposed to this environment will have a partial pressure of arterial oxygen (Pao 2 ) of 60 to 65 mm Hg (7.98 to 8.64 kPa), corresponding to 89% to 94% peripheral oxygen saturation (Spo 2 ), which may compromise cardiovascular or pulmonary disease in affected travelers. 3 Neither reassuring pulse oximetry nor reassuring forced expiratory volume in one second has been found to predict hypoxemia or in-flight events for patients with pulmonary conditions. 3
The nonstandardized Hypoxia Altitude Simulation Test, administered and interpreted by pulmonologists, can be used to determine specific in-flight oxygen requirements for patients with pulmonary complications or those for whom safe air travel remains in doubt. Typically, the Hypoxia Altitude Simulation Test comprises breathing 15% fraction of inspired oxygen for 20 minutes, with pulse oximeter and blood gas measurements taken before and after testing. 4 – 6 Patients with a Hypoxia Altitude Simulation Test Pao 2 less than 50 mm Hg (6.65 kPa) at any point during the test require supplemental oxygen in flight, whereas those with a Pao 2 greater than 55 mm Hg (7.32 kPa) do not. Pao 2 measurements falling between 50 and 55 mm Hg are considered borderline and may necessitate further testing with activity. 5 Given that the test itself incurs some risk and may not be available to all travelers, family physicians can counsel patients who are unable to walk 50 m (164 ft) or those whose usual oxygen requirements exceed 4 L per minute not to fly. 3 , 4 , 7 , 8
Patients with oxygen requirements less than 4 L per minute can be counseled to double their usual flow rate while flying. 8
Commercial airline carriers usually permit the use of personal Federal Aviation Administration–approved portable oxygen compressors, but carriers require travelers to give from 48 hours to one month's notice before flight when they are requesting the use of compressed oxygen. 9
Table 1 lists indications for which further assessment (e.g., Hypoxia Altitude Simulation Test, ability to walk 50 m) is warranted, including previous respiratory difficulties while flying, severe lung disease, recent or active lung infections, any preexisting oxygen requirements or ventilatory support, or if less than six weeks have passed since hospital discharge for acute respiratory illness. 3 Patients who have undergone an open-chest lung procedure should defer travel for two to three weeks, must not have any recent or residual pneumothorax, and should be assessed for supplemental oxygen needs. 10
Cardiac Conditions
Travelers with underlying cardiac conditions should use airport assistance services such as wheelchairs and baggage trolleys to decrease myocardial oxygen demand. 9 Although most cardiac conditions are safe for flight, some require additional consideration. Travelers with minimally symptomatic, stable heart failure may safely fly, but medication adherence is critical. 9 , 11 Patients with stable angina should be assessed for oxygen needs if they become short of breath after walking 50 m , and they should not fly following any recent medication changes that have not demonstrated clinical stability beyond that medication's half-life. 7 , 11
Patients with unstable angina, new cardiac or pulmonary symptoms, or recent changes in medication without appropriate follow-up should not fly until stable, particularly for medication changes that could impact blood pressure or coronary reserve. 11 Travelers with recent myocardial infarction at low risk should defer air travel for three to 10 days postevent 11 – 15 ( Table 2 11 ) . Low-risk patients who required percutaneous transluminal coronary angioplasty may fly after three days as long as they are asymptomatic. 9 Travelers who have had coronary artery bypass grafting or an uncomplicated open-chest procedure should wait to fly until they are 10 days postprocedure. 7 , 11
Many implantable-cardioverter defibrillators are compatible with standard airport security. 9 The Transportation Security Administration recommends that travelers with pacemakers, defibrillators, or any other implanted metal device request pat-down screening instead of using a walk-through metal detector. 16 For travelers with pacemakers and implantable-cardioverter defibrillators, a two-day flight restriction following uncomplicated placement is appropriate. 11 It is prudent for all cardiac patients to travel with a copy of their most recent electrocardiography results and a preflight graded exercise test, which may aid in assessment and management in case of an event during flight. 9 In patients with hypertension, medication compliance is especially important because aircraft noise and other travel-related stress may provoke blood pressure elevations. 17 Travel in patients with moderately controlled hypertension is not a contraindication, but airline travel for those with uncontrolled hypertension requires shared decision-making and clinical judgment.
Ear, Nose, and Throat Conditions
Trapped gases and sinus air-fluid levels can cause significant pain for the patient with ear, nose, and/or throat conditions. Adult patients with symptomatic rhinosinusitis or allergic rhinitis may benefit from oxymetazoline (Afrin) and/or pseudoephedrine to prevent ear blockage during descent. 18 No evidence suggests that antihistamines or decongestants are beneficial in children with sinusitis, 19 and these medications should not be used to hasten an early clearance for flight in any age group. Flight within 36 hours of otitis media resolution is generally safe. 20 Equalizing pressure on descent can also be accomplished in adults with frequent swallowing, chewing gum or food, or by generating pressure against a closed mouth and glottis. In young children and infants, upright bottle feeding or pacifier use can achieve similar effects. 21
Patients who have undergone jaw fracture repair should defer flying for at least one to two weeks, and jaw wiring should be temporarily replaced with elastic bands in case of emesis. 18 Transdermal scopolamine is effective in preventing air sickness , 22 and alternatives such as first-generation antihistamines may also be useful. Patients who elect to take scopolamine should be counseled on adverse effects of drowsiness, blurry vision, dry mouth, or dizziness. 22 Individuals who are prone to air sickness should refrain from alcohol use during flight and in preflight and should eat smaller, lighter meals. 18 The expansion of trapped gas at altitude may cause severe tooth pain in patients with caries beneath fixed restorations. Travelers with hearing aids should bring extra batteries and all accessories and may need to adjust their volume levels to offset background noise.
Diabetes Mellitus
In addition to carrying all medications, travelers with diabetes requiring insulin should request appropriate meals and consider checking blood glucose levels at intervals during longer flights. 23 Bringing snacks or other food can assist those with tenuous diabetes management in the event of layovers or delays. Insulin requirements may change based on the direction of travel and crossing time zones, which may entail lost or gained hours. Even if it is not part of the patient's normal regimen, fast-acting insulin, ideally with a pen device, should be considered for all travelers during flight due to its flexibility and responsiveness. 23 When traveling east, if the day is shortened by two or more hours, it may be necessary to give less insulin on the first day at the destination. When traveling west, if the day is extended by two or more hours, it may be necessary to give more insulin on the first day at the destination. Blood glucose should be checked at least 10 hours after the first-day dose to allow for further adjustments. Travelers can return to their normal insulin regimen on day 2 at their destination. A comprehensive public access resource for medical professionals addressing insulin adjustment for the air traveler is available through the Aerospace Medical Association. 23
Gastrointestinal Conditions
For travelers with recent intra-abdominal procedures, trapped gas expansion could disrupt sutures and cause rebleeding. Travelers should wait until 24 hours have passed and any bloating has resolved following laparoscopic abdominal procedures or colonoscopy. 7 , 10 Travelers should wait one to two weeks after open abdominal surgery. 10 Patients with active gastrointestinal problems, including hematemesis, melena, or obstruction, should not fly. 24
Hematologic Conditions
A baseline anemia may predispose travelers to syncope given the relative hypoxia of the flight environment. Caution should be exercised for travelers with a hemoglobin level below 8.5 g per dL (85 g per L), and some authorities recommend not advising flight for any travelers with levels below 7.5 g per dL (75 g per L). 7 Young, otherwise healthy patients with chronic anemia may be more tolerant of relative hypoxia, especially if their hemoglobin level is greater than 7.5 g per dL. 24 For the traveler with sickle cell anemia, sickling crisis during flight is unlikely 24 ; however, flight should be delayed for 10 days following an acute crisis, and patients with sickle cell anemia who have received a recent transfusion should not fly if hemoglobin levels are less than 7.5 g per dL. 24
Although deep venous thrombosis (DVT) is not caused by the flight environment itself, DVT is a concern for people who sit for extended periods or have risk factors. 25 Incidence of DVT reaches up to 5.4% in high-risk groups flying an average of 12.4 hours. 26 Compression stockings can prevent asymptomatic DVT and superficial venous thrombosis in flights lasting five hours or longer. 27 Table 3 lists recommendations for DVT prophylaxis for travelers who are at low, moderate, and high risk for DVT. 11 The baseline recommendations for each group include staying hydrated, avoiding alcohol to prevent dehydration, walking at least 10 to 15 minutes in each two hours of travel time, and performing isometric exercises while seated. 11 When indicated for high-risk travelers, including those with reduced mobility, low-molecular-weight heparin (e.g., 40 mg of subcutaneous enoxaparin [Lovenox]) on the day of and day after travel is appropriate for anticoagulation. 28
Psychiatric and Intellectual Disability Conditions
Passengers with mental or intellectual disabilities often benefit from a traveling companion because physiologic stresses of flight and the chaotic nature of busy airports may be especially challenging aspects of travel for these groups. 9 Prescription anxiolytics may alleviate travel anxiety, but a test dose is highly encouraged before flight. 9 Service or emotional support animals can be used for a variety of mental health conditions; an article in American Family Physician provides information about considerations for documentation for emotional support animals. 29 See the U.S. Department of Transportation website for current guidelines regarding the use of these animals during air travel. 30
Neurologic Conditions
Passengers predisposed to stress-related headaches and severe migraines should always carry abortive medications. Travelers with uncontrolled vertigo are not good candidates for flight. Patients prone to syncope should remain well-hydrated and be cautioned to avoid alcohol or quickly standing from a seated position. One small study suggests that people who have epilepsy with a history of flight-related seizures and a high baseline seizure frequency are likely to have a seizure after flying. 31 The Aerospace Medical Association recommends that patients with uncontrolled or poorly controlled seizures should not fly. 32 A safe amount of time permitted before flight following a seizure has not been established, but clinical judgment and the presence of a knowledgeable chaperone should factor into any medical recommendation. Although some airline carriers allow patients to fly 72 hours after a stroke, 7 the Aerospace Medical Association recommends waiting one to two weeks. 32
Obstetric Conditions
Background radiation associated with the flight environment does not pose a special hazard for most pregnant air travelers; however, the Federal Aviation Administration recommends informing aircrew or frequent flyers about health risks of radiation exposure. 33 Because a lack of in-flight medical resources may jeopardize safety of the mother and neonate, patients with an uncomplicated singleton pregnancy should generally not fly beyond 36 weeks of estimated gestational age 7 , 24 , 33 , 34 and those with a multiple gestation not beyond 32 weeks . 7 , 34 Body imaging scanners are safe for security screening during pregnancy. 34 , 35 Postpartum travelers are at moderate risk for DVT and should wear compression stockings and perform isometric exercises during flight. 11 Travelers who have undergone an uncomplicated cesarean delivery are generally safe for flight within one to two weeks. 10
Ophthalmologic Conditions
Passengers with severe visual impairment may benefit from having a traveling companion. Xerophthalmia may be exacerbated in the low humidity of the airplane cabin, and lubricating eye drops are advisable. Cataracts and clinically stable glaucoma are not contraindications to flight; however, any retinal detachment interventions should restrict flight for at least two weeks. 36 Open-globe eye surgery should delay air travel for up to six weeks, and travel recommendations should be made in conjunction with an ophthalmologist. 36
Orthopedic Conditions
Because of expansion of trapped air at altitude, all fixed casts should be bivalved. 7 , 37 Some airlines do not permit air casts of any kind, but if they are used, a small amount of air should be released to prevent any limb compression that occurs as a result of trapped gas expansion. Elastic bandages can be added to a bivalved cast and can be loosened as tolerated. The Transportation Security Administration recommends that passengers with prosthetic limbs should avoid metal detector screening and should be screened with alternative measures. 16 Individuals with significantly decreased mobility should consider wheelchairs and the use of travel companions. Passengers with low back pain and other mobility-limiting conditions can request seating near the front to reduce walking; however, business and first-class seating is an additional cost.

Urologic Conditions
Foley catheters and other inflatable balloons are compatible with flight; however, they should be filled with liquid for air travel, given the previously described expansion of trapped gas at altitude.
Special Considerations for Children
Healthy, term neonates should not fly for at least 48 hours after birth but preferably one to two weeks. 21 Infants younger than one year with a history of chronic respiratory problems since birth should be evaluated by a pulmonologist before air travel. 3
Other Air Travel Considerations
Jet lag occurs as a result of desynchronization between an individual's internal circadian rhythm and the external environment's time zone. 38 , 39 Jet lag is worse for eastward rather than westward travel. 40 Measures for prevention include ensuring enough sleep before travel, timing light exposure using sunglasses, avoiding alcohol, and eating at appropriate times after arriving at the destination. Timed melatonin is highly effective at treating jet lag, 41 and prescription hypnotic-sedative medications may also work in controlling sleep loss. 38
Self-contained underwater breathing apparatus (SCUBA) divers should not fly within 12 hours of a dive because of the concern for decompression sickness or life-threatening arterial gas embolism. 42
The airplane cabin does not inherently pose greater risk for infection than any other close contact, but respiratory viral pathogens are the most commonly transmitted infections. 43 Because of the ongoing COVID-19 pandemic, the Centers for Disease Control and Prevention (CDC) recommends delaying travel until the individual is fully vaccinated because traveling increases the chance of getting and spreading COVID-19. For patients not fully vaccinated who must travel, it is important to follow the CDC's recommendations for unvaccinated people. Check for evolving guidelines on the CDC's website. 44
Patients with breast cancer who have had surgery may fly without risking new or worsening lymphadenopathy. 45
A comprehensive discussion of in-flight emergencies is beyond the scope of this article. See the American Family Physician article on in-flight emergencies for more details. 46
This article updates a previous article on this topic by Bettes and McKenas . 37
Data Sources: A PubMed, Cochrane database, Essential Evidence Plus, ACCESSSS, and ECRI search occurred in April and May 2020 and April and May 2021 using search terms aviation medicine, travel medicine, commercial flight, air travel, and fitness to fly. The Aerospace Medical Association's website resource, Medical Considerations for Airline Travel, was searched in its entirety. The Handbook of Aviation and Space Medicine, Fundamentals of Aerospace Medicine, and Aviation and Space Medicine were reviewed for clinically relevant chapters.
The authors acknowledge Rachel Kinsler, USAARL Research Engineer, for her thoughtful review of this manuscript.
The views, opinions, and/or findings contained in this report are those of the authors and should not be construed as an official Department of the Army position, policy, or decision, unless so designated by other official documentation. Citation of trade names in this report does not constitute an official Department of the Army endorsement or approval of the use of such commercial items.
Airlines for America. Air travelers in America: annual survey. Accessed May 1, 2021. https://www.airlines.org/dataset/air-travelers-in-america-annual-survey/#
14 Code of Federal Regulations §25.841—pressurized cabins. Accessed May 1, 2021. https://www.govinfo.gov/app/details/CFR-2012-title14-vol1/CFR-2012-title14-vol1-sec25-841
- Ahmedzai S, Balfour-Lynn IM, Bewick T, et al.; British Thoracic Society Standards of Care Committee. Managing passengers with stable respiratory disease planning air travel. Thorax. 2011;66(suppl 1):i1-i30.
Respiratory disease. In: Green N, Gaydos S, Hutchinson E, et al., eds. Handbook of Aviation and Space Medicine . CRC Press; 2019:329–333.
Dine CJ, Kreider ME. Hypoxia altitude simulation test. Chest. 2008;133(4):1002-1005.
- Matthys H. Fit for high altitude: are hypoxic challenge tests useful? Multidiscip Respir Med. 2011;6(1):38-46.
Bagshaw M. Commercial passenger fitness to fly. In: Gradwell DP, Rainford DJ, eds. Ernsting's Aviation and Space Medicine . 5th ed. CRC Press; 2016:631–640.
Josephs LK, Coker RK, Thomas M; BTS Air Travel Working Group; British Thoracic Society; Managing patients with stable respiratory disease planning air travel. Prim Care Respir J. 2013;22(2):234-238.
Rayman RB, Williams KA. The passenger and the patient inflight. In: DeHart RL, Davis JR, eds. Fundamentals of Aerospace Medicine . 3rd ed. Lippincott Williams & Wilkins; 2002:453–469.
Aerospace Medical Association. Surgical conditions. May 2003. Accessed May 1, 2021. http://www.asma.org/asma/media/asma/Travel-Publications/Medical%20Guidelines/Surgical-Conditions.pdf
- Smith D, Toff W, Joy M, et al. Fitness to fly for passengers with cardiovascular disease. Heart. 2010;96(suppl 2):ii1-ii16.
- Thomas MD, Hinds R, Walker C, et al. Safety of aeromedical repatriation after myocardial infarction: a retrospective study. Heart. 2006;92(12):1864-1865.
Roby H, Lee A, Hopkins A. Safety of air travel following acute myocardial infarction. Aviat Space Environ Med. 2002;73(2):91-96.
- Zahger D, Leibowitz D, Tabb IK, et al. Long-distance air travel soon after an acute coronary syndrome: a prospective evaluation of a triage protocol. Am Heart J. 2000;140(2):241-242.
- Cox GR, Peterson J, Bouchel L, et al. Safety of commercial air travel following myocardial infarction. Aviat Space Environ Med. 1996;67(10):976-982.
Transportation Security Administration. Frequently asked questions. Accessed May 1, 2021. https://tsa.gov/travel/frequently-asked-questions
- Steven S, Frenis K, Kalinovic S, et al. Exacerbation of adverse cardiovascular effects of aircraft noise in an animal model of arterial hypertension. Redox Biol. 2020;34:101515.
Aerospace Medical Association. Ear, nose, and throat. May 2003. Accessed May 1, 2021. https://www.asma.org/asma/media/asma/Travel-Publications/Medical%20Guidelines/Ear-Nose-and-Throat.pdf
Shaikh N, Wald ER, Pi M. Decongestants, antihistamines and nasal irrigation for acute sinusitis in children. Cochrane Database Syst Rev. 2014;(10):CD007909.
- Pinto JA, Dos Santos Sobreira Nunes H, Soeli Dos Santos R, et al. Otitis media with effusion in aircrew members. Aerosp Med Hum Perform. 2019;90(5):462-465.
Aerospace Medical Association. Travel with children. May 2003. Accessed May 1, 2021. https://www.asma.org/asma/media/asma/Travel-Publications/Medical%20Guidelines/Travel-With-Children.pdf
Spinks A, Wasiak J. Scopolamine (hyoscine) for preventing and treating motion sickness. Cochrane Database Syst Rev. 2011;(6):CD002851.
Aerospace Medical Association. Diabetes. May 2003. Accessed May 1, 2021. http://www.asma.org/asma/media/asma/Travel-Publications/Medical%20Guidelines/Diabetes.pdf
Passenger fitness to fly. In: Green N, Gaydos S, Hutchinson E, et al., eds. Handbook of Aviation and Space Medicine . CRC Press; 2019:263–266.
Watson HG, Baglin TP. Guidelines on travel-related venous thrombosis. Br J Haematol. 2011;152(1):31-34.
Possick SE, Barry M. Evaluation and management of the cardiovascular patient embarking on air travel. Ann Intern Med. 2004;141(2):148-154.
- Clarke MJ, Broderick C, Hopewell S, et al. Compression stockings for preventing deep vein thrombosis in airline passengers. Cochrane Database Syst Rev. 2021;(4):CD004002.
Gavish I, Brenner B. Air travel and the risk of thromboembolism. Intern Emerg Med. 2011;6(2):113-116.
Tin AH, Rabinowitz P, Fowler H. Emotional support animals: considerations for documentation. Am Fam Physician. 2020;101(5):302-304. Accessed May 1, 2021. https://www.aafp.org/afp/2020/0301/p302.html
U.S. Department of Transportation. U.S. Department of Transportation announces final rule on traveling by air with service animals. December 2, 2020. Accessed May 1, 2021. https://www.transportation.gov/briefing-room/us-department-transportation-announces-final-rule-traveling-air-service-animals
Trevorrow T. Air travel and seizure frequency for individuals with epilepsy. Seizure. 2006;15(5):320-327.
Hastings, JD; Aerospace Medical Association. Medical guidelines for airline travel: air travel for passengers with neurological conditions. September 2014. Accessed May 1, 2021. http://www.asma.org/asma/media/asma/Travel-Publications/Medical%20Guidelines/Neurology-Sep-2014.pdf
ACOG Committee opinion no. 746: air travel during pregnancy. Obstet Gynecol. 2018;132(2):e64-e66.
Royal College of Obstetricians and Gynaecologists. Air travel and pregnancy: scientific impact paper no. 1. May 2013. Accessed May 1, 2021. http://www.asma.org/asma/media/asma/Travel-Publications/Medical%20Guidelines/RCOG-Pregnancy-and-Air-Travel-Scientific-Impact-Paper.pdf
Harvard Medical School. Are full-body airport scanners safe? June 2011. Accessed May 1, 2021. https://www.health.harvard.edu/diseases-and-conditions/are-full-body-airport-scanners-safe#:~:text=he%20authors%20begin%20with%20an,the%20biological%20effects%20of%20radiation
Aerospace Medical Association. Ophthalmological conditions. May 2003. Accessed May 1, 2021. http://www.asma.org/asma/media/asma/Travel-Publications/Medical%20Guidelines/Ophthalmological-Conditions.pdf
Bettes TN, McKenas DK. Medical advice for commercial air travelers. Am Fam Physician. 1999;60(3):801-808. Accessed May 1, 2021. https://www.aafp.org/afp/1999/0901/p801.html
Aerospace Medical Association. Jet lag. May 2003. Accessed May 1, 2021. https://www.asma.org/asma/media/asma/Travel-Publications/Medical%20Guidelines/Jet-Lag.pdf
Choy M, Salbu RL. Jet lag: current and potential therapies. PT. 2011;36(4):221-231.
- Waterhouse J, Reilly T, Atkinson G, et al. Jet lag: trends and coping strategies. Lancet. 2007;369(9567):1117-1129.
Herxheimer A, Petrie KJ. Melatonin for the prevention and treatment of jet lag. Cochrane Database Syst Rev. 2002;(2):CD001520.
Divers Alert Network. February 1, 2017. Accessed May 11, 2021. https://dan.org/alert-diver/article/flying-after-pool-diving-2/
Mitchell GW, Martin GJ. Chapter 19 Infectious diseases. In: Davis JR, Johnson R, Stepanek J, et al. Fundamentals of Aerospace Medicine . 4th ed. Lippincott Williams & Wilkins; 2008:432–446.
Centers for Disease Control and Prevention. Domestic travel during COVID-19. Updated April 27, 2021. Accessed April 30, 2021. https://www.cdc.gov/coronavirus/2019-ncov/travelers/travel-during-covid19.html
Co M, Ng J, Kwong A. Air travel and postoperative lymph-edema—a systematic review. Clin Breast Cancer. 2018;18(1):e151-e155.
Hu JS, Smith JK. In-flight medical emergencies. Am Fam Physician. 2021;103(9):547-552. Accessed April 30, 2021. https://www.aafp.org/afp/2021/0501/p547.html
Continue Reading

More in AFP
More in pubmed.
Copyright © 2021 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

- Northern Ireland
- Hurling & Camogie
- GAA Fixtures & Results
- Personal Finance
- Holidays & Travel
- Food & Drink
- Irish Language
- Entertainment
- Opens in new window
Ask the GP: Is it safe for me to fly with swollen legs?

Q: MY husband has pitting oedema and the doctor says there is no cure. Is this the case, and is it safe for him to take a long flight with this condition?
A: OEDEMA is the medical term for swelling that’s caused by fluid retention. Pitting oedema means that if you apply pressure to the swollen area, then an indent will remain for a few seconds (with non-pitting oedema, applying pressure will not cause any lasting indentation – and this has different underlying causes).
The swelling itself is caused by an increase in the amount of fluid, known as lymph, present in the interstitial space – the area outside of blood vessels and around the cells which make up our tissue.

Review: Cailíní tells the story of a family’s world on the brink of change

Bobby Storey funeral ‘undermined confidence in lockdown more than minister disputes’
The fluid is essentially blood that has been filtered of blood cells by the capillary walls it has pushed through.
There are a number of conditions that cause this build-up of fluid, such as heart failure, cirrhosis of the liver, kidney disease and disorders of the veins that return blood to the heart – varicose veins (swollen veins), for example.
I am going to assume that the oedema you describe is of the lower legs.
The most common cause of bilateral leg oedema (swelling in both legs) is when the body has trouble sending blood from veins back to the heart.
This is usually due to severe varicose veins – the blood vessels are grossly widened and so there is less pressure on the blood to flow in the right direction. So blood, rather than coursing along a relatively narrow vessel back toward the heart, is only indolently flowing, almost like water in a canal rather than a fast river.
Varicose veins are also often so wide they have no effective valves that would otherwise control blood flow in the correct direction.
In the absence of detailed knowledge of your husband’s medical history, it is necessary to consider whether the pitting oedema is a result of the side-effects of medications he may be taking – most commonly a group of drugs called calcium channel blockers, which are prescribed for high blood pressure.
These medicines cause sodium retention, which inevitably leads to a build-up of fluid.
Your GP will have taken these details into account before making his prognosis, and will also have excluded causes such as heart failure, kidney disorders and deep vein thrombosis (blood clots in deep veins).
If your GP has not recommended any specific precautions, I would assume your husband is safe to take a long flight; it is, however, essential that he wears full-length compression stockings to guard against the swelling worsening in his legs.
He should also walk along the aisle in the plane once every two hours and stay well hydrated.
Seek the advice of the GP again before the flight, in case there are aspects that have not been revealed to me, and ask about the right compression stockings.
A prescription is not essential – your pharmacist will be able to provide this hosiery.

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 06 January 2022
Travelling with heart failure: risk assessment and practical recommendations
- Stephan von Haehling 1 , 2 ,
- Christoph Birner 3 , 4 ,
- Elke Dworatzek 5 , 6 ,
- Stefan Frantz 7 ,
- Kristian Hellenkamp 1 ,
- Carsten W. Israel 8 ,
- Tibor Kempf 9 ,
- Hermann H. Klein 10 ,
- Christoph Knosalla ORCID: orcid.org/0000-0002-8127-5019 6 , 11 , 12 ,
- Ulrich Laufs ORCID: orcid.org/0000-0003-2620-9323 13 ,
- Philip Raake 14 , 15 ,
- Rolf Wachter 1 , 2 , 13 &
- Gerd Hasenfuss 1 , 2
Nature Reviews Cardiology volume 19 , pages 302–313 ( 2022 ) Cite this article
39k Accesses
6 Citations
165 Altmetric
Metrics details
- Heart failure
- Patient education
Patients with heart failure are at a higher risk of cardiovascular events compared with the general population, particularly during domestic or international travel. Patients with heart failure should adhere to specific recommendations during travel to lower their risk of developing heart failure symptoms. In this Review, we aim to provide clinicians with a set of guidelines for patients with heart failure embarking on national or international travel. Considerations when choosing a travel destination include travel distance and time, the season upon arrival, air pollution levels, jet lag and altitude level because all these factors can increase the risk of symptom development in patients with heart failure. In particular, volume depletion is of major concern while travelling given that it can contribute to worsening heart failure symptoms. Pre-travel risk assessment should be performed by a clinician 4–6 weeks before departure, and patients should receive advice on potential travel-related illness and on strategies to prevent volume depletion. Oxygen supplementation might be useful for patients who are very symptomatic. Upon arrival at the destination, potential drug-induced photosensitivity (particularly in tropical destinations) and risks associated with the local cuisine require consideration. Special recommendations are needed for patients with cardiac implantable electronic devices or left ventricular assist devices as well as for those who have undergone major cardiac surgery.
Patients with heart failure (HF) are recommended to schedule a specialist consultation for pre-travel risk assessment 4–6 weeks before departure.
Preparation for travel requires special considerations in patients with HF, including the choice of destination, availability of medical resources and strategies to prevent volume depletion.
Most patients with HF can travel when medically stable; patients with a ground-level oxygen saturation ≤90% or those in NYHA class III–IV might need an on-board medical oxygen supply.
All medication and important documents should be stored in carry-on luggage.
Volume depletion and dehydration are important considerations requiring meticulous attention with regards to medication adjustment and fluid intake.
Patients with implantable cardiac devices might require extra time at security checkpoints and additional documents; for some patients, remote monitoring of implantable cardiac devices might be useful.
Similar content being viewed by others

Evaluating the “holiday season effect” of hospital care on the risk of mortality from pulmonary embolism: a nationwide analysis in Taiwan
The role of cardiac rehabilitation in improving cardiovascular outcomes
Variation in community and ambulance care processes for out-of-hospital cardiac arrest during the COVID-19 pandemic: a systematic review and meta-analysis
Introduction.
Domestic and international travel are associated with increased health risks, with 20–70% of individuals reporting health issues during their travels 1 . During international travel, 1–5% of individuals seek medical attention and the rate of death among travellers is 1 in 100,000, with cardiovascular disease being the most frequent cause of death 1 . Trauma, particularly from motor vehicle accidents, is another major cause of death while travelling 1 . Health-care providers are frequently approached by patients for advice on how to prepare for travel or to determine whether travelling is advisable at all. General practitioners can provide information to healthy individuals but specialist consultation is of benefit for patients with underlying illnesses such heart failure (HF) 2 . Indeed, many patients with HF intend to travel for business or leisure. Although some guidance has been published 3 , a systematic overview of recommendations for patients with HF planning to travel is not yet available. In this Review, we aim to provide clinicians with recommendations for preparatory measures before travel to inform and educate patients with HF. We discuss factors that might increase the risk of HF symptom development, such as local climate, air pollution levels and altitude levels, and provide specific guidance for patients with a cardiac implantable device and those who have undergone major surgery.
Which patients with HF can travel safely?
To date, guidance on travel recommendations for patients with HF is limited. In general, patients with NYHA class I–III HF who are stable should be able to travel safely 4 . However, patients with NYHA class III HF who are planning to travel by air should be advised to consider on-board medical oxygen support. Patients with NYHA class IV should not travel; however, if travel is unavoidable, on-board oxygen and medical assistance should be requested. A patient with an oxygen saturation rate >90% at ground level usually will not require medical oxygen during flight 5 . An overview of whether travelling is advisable for different classes of HF 6 , 7 is provided in Box 1 . An overview of contraindications for air travel in patients with cardiovascular diseases is provided in Box 2 .
Box 1 Travel recommendations for patients with heart failure
Chronic stable heart failure
NYHA class I–II: travel advisable, if patient is stable
NYHA class III: travel advisable, if patient is stable; consider use of on-board medical oxygen during air travel
NYHA class IV: travel not advisable; if travel is unavoidable, on-board oyxgen and medical assistance are required
Acute heart failure decompensation
Travel not advisable until at least 6 weeks after discharge and rehabilitation, if patient is stable
Ventricular assist device implantation
Travel advisable after hospital discharge and rehabilitation, if patient is stable
Heart transplantation
Not advisable until at least 1 year after transplantation surgery, if patient is stable
Implantable cardioverter–defibrillator or cardiac resynchronization therapy implantation
Not advisable until at least 2 weeks after discharge, if patient is stable
Box 2 Contraindications for air travel in patients with cardiovascular disease
Myocardial infarction (ST-elevation or non-ST-elevation myocardial infarction) within the previous 2 weeks
Unstable angina without further diagnostics and treatment
Percutaneous coronary angioplasty within the previous 2 weeks; in patients who have undergone uncomplicated percutaneous coronary intervention, shorter time frames might be acceptable
Cardiac surgery or interventional valve therapy within the previous 3 weeks
NYHA class IV heart failure or any decompensated heart failure
Untreated arrhythmias (ventricular or supraventricular)
Eisenmenger syndrome
Uncontrolled pulmonary artery hypertension
Pneumothorax (such as after major cardiac surgery)
Choice of destination
The choice of destination for travel can have important health implications for patients with HF, particularly when travelling abroad. Considerations include the local climate, air pollution levels, altitude levels, the season upon arrival, the distance and time for travelling, jet lag, and vaccines required.
Effects of transitioning climates on HF
Individuals who transition through climates different to the one they reside in (such as someone living in the arctic travelling to a tropical island) are at an increased health risk. In general, people living in warmer regions tend to be most vulnerable to cold weather and, conversely, those residing in a cold climate are most sensitive to heat 8 . Exposure to extreme heat has been associated with increased morbidity and mortality from heat exhaustion and heat stroke 9 , 10 . Maintenance of homeostasis during hot weather requires an increase in cardiac output; heat tolerance is impaired when cardiac output cannot be increased to meet the requirements of heat loss. Numerous medications that are frequently prescribed for individuals with HF can also increase susceptibility to heat stroke, including loop diuretics, serotonic antidepressants, angiotensin-converting enzyme inhibitors and proton-pump inhibitors 11 , 12 , 13 . Colder temperatures are less likely to have effects on cardiovascular health but have been associated with increased morbidity among patients with respiratory disease 14 . Patients with HF should be advised to choose either spring or autumn for international travel to avoid travelling during extremities in weather and to adjust medications that can contribute to volume depletion. Appropriate clothing is required for the site of departure, the destination and for the journey itself. Given the challenges in contacting a patient’s primary care physician if the patient is in a different country or continent, distant travel destinations might only be advisable for patients who are well-informed about their medication regimen, dietary restrictions and exercise limitations.
Endemic diseases
The need for immunization for travel depends on the destination. In general, the status of routine vaccinations, such as the diphtheria, measles–mumps–rubella, pertussis, tetanus and varicella vaccines, should be checked before travelling abroad. For all patients with HF, vaccines are required for pneumococcal disease, influenza and coronavirus disease 2019 (COVID-19). Other destination-dependent vaccines are provided in Table 1 .
Air pollution and HF
Air pollution can be measured by the air quality index, which integrates measures for the five main air pollutants: ground-level ozone, particulate matter, carbon monoxide, sulfur dioxide and nitrogen dioxide. An air quality index value of 0–50 indicates good air quality, 51–100 indicates moderately polluted air, >100 indicates an unhealthy level of air pollution and >300 designates a hazardous environment 15 . Particulate matter (PM) of ≤10 µm (PM 10 ) or ≤2.5 µm (PM 2.5 ) in diameter are linked with increased cardiopulmonary mortality 16 , 17 as well as with an increased risk of hospitalization for HF 18 and death 19 . The pathophysiological mechanisms underlying this increased risk remain elusive. Accumulating evidence points towards a crucial role of PM-induced systemic oxidative stress 20 and endothelial dysfunction 21 in the development of arterial vasoconstriction and elevated systemic blood pressure 22 . In addition, PM-induced pulmonary vasoconstriction results from increases in pulmonary and right ventricular diastolic filling pressures, which affect right ventricular performance 22 . Given that the effects of air pollutants on cardiovascular performance and outcomes can occur within hours or days of exposure 23 , patients with HF should be advised to avoid travelling to locations with high levels of air pollution.
Altitude-induced hypoxia and HF
Patients with HF are more susceptible to the physiological changes induced by high altitude exposure than the general population 24 . During air travel, cabin pressure is required to be no less than the barometric pressure at an altitude of 2,438 m (8,000 ft), which is classified as an intermediate altitude 25 (Fig. 1a ). Cabin pressures usually remain higher than this altitude, particularly during long-haul flights 26 . Travel to high altitude locations that are >2,500 m above sea level triggers physiological acclimatization processes within the cardiocirculatory and pulmonary systems 27 , 28 (Fig. 1b ). These processes are initiated by a gradual decrease in barometric pressure, which in turn lowers the partial pressure of oxygen in inspired air. Hypobaric hypoxia leads to a fast increase in respiratory rate and tidal volume 29 , which leads to respiratory alkalosis and hypoxic diuresis 30 . Hypoxia induces pulmonary vasoconstriction and eventual pulmonary hypertension, an important trigger for high altitude pulmonary oedema 31 . To compensate for the lower arterial oxygen content, heart rate and stroke volume are increased via activation of the sympathetic nervous system 26 , 32 , 33 , 34 . Together, these physiological adaptations limit the exercise capacity of patients with HF and make them prone to cardiac decompensation. However, studies that assessed simulated altitude-induced hypoxia in patients with NYHA class III–IV HF showed that high altitude was not associated with angina, arrhythmia, or ischaemia 35 , 36 and that the degree of the reduction of maximum work capacity was dependent on the individual’s exercise tolerance at sea level 35 . The ESC and other professional societies recommend that the assessment of safety of high altitude exposure for patients with HF should depend on their functional capacity (that is, NYHA class) at sea level 35 , 37 . Furthermore, certain drugs that are prescribed to patients with HF can further interfere with the physiological adaptation processes at high altitudes. For example, angiotensin-converting enzyme inhibitors and angiotensin receptor blockers can reduce renal erythropoietin production, thereby hampering the compensatory rise in haematocrit mediated by altitude-induced hypoxia 38 . Therefore, diuretic therapy should be tailored to the individual to account for clinical signs of dehydration (such as through hypoxic diuresis) or fluid gain 39 . Finally, anaemia reduces oxygen delivery, and muscle loss (present in patients with sarcopenia or cachexia) reduces maximal physical workload and time to fatigue; patients with these conditions in addition to HF need to have special considerations when planning to travel to high altitude locations. To summarize, travel to destinations at an intermediate altitude (~2,000 m) is safe for patients with HF who have good exercise tolerance at sea level.
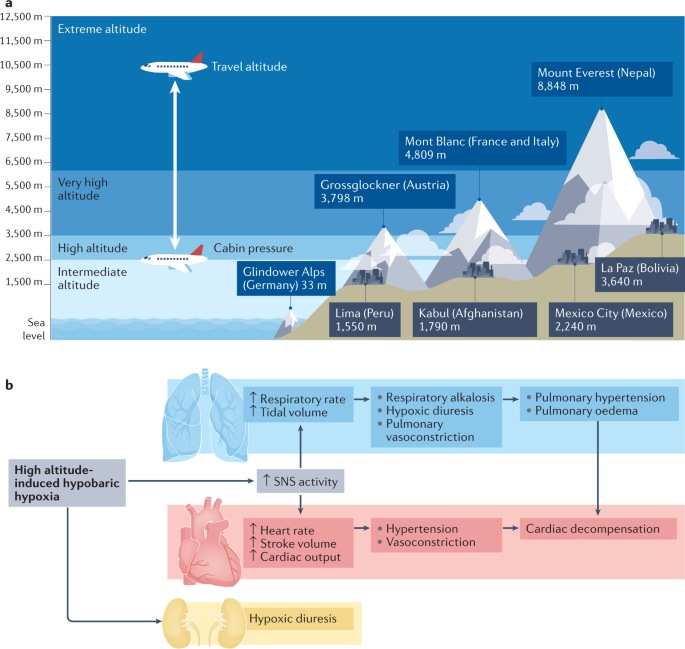
a | Definitions of height and examples of mountains and cities at different altitudes. Most aircraft fly at approximately 10,000–12,000 m (33,000–42,000 ft) above sea level, with the cabin pressurized to an equivalent of 2,438 m (8,000 ft). b | High altitude-induced hypobaric hypoxia leads to an increase in respiratory rate and tidal volume, which promotes respiratory alkalosis, hypoxic diuresis, pulmonary vasoconstriction and, ultimately, pulmonary hypertension and pulmonary oedema. Compensatory mechanisms of this hypoxia include increases in heart rate and stroke volume via activation of the sympathetic nervous system (SNS). Together, these changes can limit exercise capacity and promote cardiac decompensation.
Seasonal variations and HF
Hospitalizations owing to worsening HF show intriguing seasonality, with a substantial decline during warmer periods and an increase during colder periods 18 , 40 , especially in older patients 41 . Temperature had the greatest (inverse) correlation with hospitalizations for HF among other causative environmental factors such as humidity, precipitation or irradiation 16 . Skin cooling has been shown to increase vascular resistance 42 and plasma noradrenaline concentration 43 , which might lead to HF decompensation. Beyond neurohumoural activation and haemodynamic stress, respiratory infections, which peak during the colder months, can precipitate and aggravate HF symptoms 41 . Furthermore, vitamin D insufficiency during winter has also been linked to worsening HF 44 . Interestingly, the effect of seasonal variability on health is more prominent in elderly people and winter hospitalization is associated with both poorer short-term and long-term prognosis 41 . These observations suggest that patients with more severe HF (and worse prognosis) are prone to decompensation during winter and that these patients and older patients with more advanced disease should be advised to avoid travelling to colder regions. Of note, a study from Norway reported that the Christmas winter period was associated with the highest rates of excess all-cause and cardiovascular deaths 45 . Overall, appropriate clothing and heating strategies need to be carefully selected for optimal stabilization of body core temperatures, vitamin D levels should be measured before departure and supplemented if required, and vaccines against influenza and pneunococcal disease should be administered 40 (Table 1 ).
Preparing to travel
Any patient with a history of HF should seek medical consultation before departure, particularly when travelling overseas or when leaving for a long period. Women are generally more likely to seek pre-travel medical advice than men 46 and are also more likely to have travel-related worries 47 . A cross-sectional national survey found that a low perceived need was among the main causes for avoiding medical care, often because patients expected their illness or symptoms to improve over time 48 . For patients with HF, travel preparation should include a specialist consultation approximately 4–6 weeks before departure. This consultation should follow a structured and sequenced approach, which should involve risk assessment (including an evaluation of medical history and travel itinerary), interventions required before departure (including physical examination or setting up of remote monitoring for cardiac implantable devices) and focused education on topics such as medications and factors that can lead to volume depletion. For example, the presence of anaemia might cause lightheadedness, angina or loss of consciousness, particularly during flights 49 , 50 . Medication regimens should be optimized before departure and patients with iron deficiency should be considered for repletion therapy. Suggestions for topics to cover during this consultation are summarized in Box 3 .
Box 3 Recommendations for pre-travel assessment
Risk assessment
Full medical history (current medications, immunization history, history of surgeries or device implantation, immune status, allergies, pregnancy or breast feeding)
Previous travel experience (particularly to the same destination) or risk tolerance
Travel itinerary (destination, mode of travel, travel distance, season, air pollution levels, potential jet lag, clothing required and altitude)
Activities planned (such as adventure sports or hiking, mass gatherings)
Type of accommodation
In-office interventions
Physical examination, electrocardiogram tracing, biochemistry analysis (plasma levels of creatinine, ferritin, glucose, glycated haemoglobin, N-terminal pro-B-type natriuretic peptide, potassium, sodium, transferrin saturation, thyroid-stimulating hormone, vitamin D and urea, estimated glomerular filtration rate, and lipid profile and liver function tests), full blood count (to identify potential anaemia), exercise test and/or transthoracic echocardiography
Set up remote monitoring of implanted devices
Administration of immunizations (routine vaccines include measles–mumps–rubella, tetanus–diphtheria–pertussis, coronavirus disease 2019 (COVID-19), pneumococcal disease and influenza as well as any destination-specific vaccine that might be needed for diseases such as hepatitis A or yellow fever) or malaria chemoprophylaxis (if required)
Strategies to prevent or treat traveller’s diarrhoea (food and water precautions, oral rehydration, treatment with loperamide and bismuth subsalicylate, and antibiotic self-treatment options for severe diarrhoea)
Focused education before travel
Medical kit and documents required during travel: personal health kit (medication, device information or medical records), evacuation and health insurance
Location of medical facilities at destination
Education on heart failure medication adjustment (to avoid dehydration and volume overload), cardiac device handling, telemonitoring and factors that contribute to volume depletion (excess alcohol, coffee or salt intake; traveller’s diarrhoea)
Patients with a cardiac implanted device should avoid strong electromagnetic fields
Travel-related illnesses: altitude illness, traveller’s thrombosis, bloodborne and sexually transmitted diseases, transportation-associated illnesses, respiratory infections, rabies and other animal-associated illness, and skin conditions and wounds
Personal protection for vector-borne disease (if at risk)
Risk assessment and medication adjustment
As mentioned in the previous section, pre-travel risk assessment should consider the type and duration of travel, the travel destination, and the medical history of the patient. Typical health emergencies that patients with HF might encounter during travel are listed in Table 2 . Patients should be advised that provision of incomplete medical information during a cardiac emergency might increase the risk of death. Any accompanying travellers need to know where to find important documents (Box 4 ) in case of an emergency. Given the difficulty in obtaining prescription drugs in a different country as well as the different brands of drugs having varying strengths in different countries, extra medication should be brought on the trip. Importantly, some over-the-counter drugs might be legal in the patient’s home country but illegal elsewhere (such as certain analgesics).
Box 4 Medication and documents required during travel
Sufficient medication for the whole journey (consider bringing extra drugs in case of unforeseen delays in returning home)
Medication to be kept in carry-on luggage for flights (in case of loss of luggage or emergency)
Photocopy of last prescription
Insurance card
Patient identification card
List of diagnosed health conditions and prescribed medicines
Last discharge letter from hospital
Device interrogation print-out
List of names and phone numbers of cardiologist and other relevant clinicians
Remote device monitoring
Remote monitoring is recommended by the ESC and other professional societies for patients with cardiac implantable devices such as pacemakers, implantable cardioverter–defibrillators (ICDs) and implantable cardiac monitors 51 , 52 , 53 . Most remote monitoring systems use a transmitter (base station) placed in the vicinity of the implanted device, with information sent via an internet connection to a remote monitoring service. Alternatively, alerts can be activated after events that trigger an immediate remote transmission (for example, after ICD shock, detection of ventricular tachyarrhythmias or signs of lead failure). Given that travelling is usually associated with increased physical activity levels, daily remote monitoring might be useful for the detection of events such as arrhythmias, HF decompensation or device malfunction (Box 5 ).
Box 5 Travel-related activities and related cardiac events reported via remote monitoring
Sports (such as swimming and diving)
Arrhythmias (atrial fibrillation, ventricular tachyarrhythmia or premature ventricular contractions)
Heart failure decompensation
Damage to the implanted cardiac lead (fracture or insulation failure)
Cardiac device compression with loss of function (during diving)
Stay in high altitude
Eating out (higher intake of sodium) and alcohol consumption
Reduced adherence to medication
Arrhythmias
Travel by aircraft
Electromagnetic interference with cardiac electronic device
Travel by train or ship
Special considerations
Patients who have undergone recent surgery.
Major cardiac surgery ranges from minimally invasive approaches to complete sternotomy. The Canadian Cardiac Society guidelines on air travel recommend that patients with a haemoglobin level <9 g/dl who have undergone coronary artery bypass graft surgery should be advised against air travel 54 ; recommendations for travel in patients with HF who have undergone coronary artery bypass graft surgery should perhaps be even more conservative. These patients should be advised not to travel by air until intrathoracic gas resorption is completed given that gas expands when air pressure is reduced with increasing altitude (the Boyle law) 4 . Gas resorption usually takes 3–10 days after surgery. Any air remaining in the pericardial space or in the thoracic cavity can expand by up to 60%, which might be dangerous and painful 4 . Indeed, the Aerospace Medical Association guidelines state that pneumothorax is an absolute contraindication to air travel and advocate an interval of 2–3 weeks before flying after thoracic surgery 5 . Furthermore, patients who have had a recent operation are in a state of increased oxygen consumption owing to the trauma of surgery, possible presence of sepsis and increased adrenergic outflow. A 2017 study compared complication rates between ground and air travel 5–25 days after pulmonary resection 55 . Air travel was as safe as ground travel if the chest tubes were removed after the absence of ongoing air leak and an output <300 ml over 24 hours combined with adequate pain medication and an active ambulation schedule.
Patients with LVADs
Left ventricular assist devices (LVADs) are increasingly implanted as a bridging strategy while patients wait for heart transplantation or as a permanent therapy for end-stage HF. Patients in either category can travel by air if medically stable and rehabilitation measures have been performed 56 . Box 6 lists precautions before and during travel for patients with an LVAD.
Box 6 Considerations before and during travel for patients with an LVAD
Considerations before departure
Approval should be sought from the responsible left ventricular assist devices (LVAD) centre, including an airline information letter (templates from LVAD manufacturer)
Closest LVAD centres within the travel destination should be located as possible emergency contacts
All LVAD-related equipment needs to be stored in carry-on luggage with handling advice and emergency contact information attached and batteries should be fully charged before departure
The size and weight of the equipment should be checked to ensure that it can be carried on board the plane and the airport and airline need to be informed about the LVAD before arrival to the airport
Considerations during travel
Flight attendants and other personnel need to be informed about the LVAD and the location of the emergency information card
Patients need to maintain fluid intake to avoid low flow alarms from the LVAD pump
For flights longer than 2 hours, support stockings should be considered
Considerations while en route
Departure from home.
Patients with HF or ischaemic heart disease need to take extra caution on the way to and from the departure point, such as an airport or train station, given the multitude of stressors: commotion, a delay or any last-minute changes to the train or flight, and lifting of heavy luggage, all of which can increase physical and mental exertion and risk of myocardial ischaemia 57 , 58 . As such, travel planning should include estimation of psychological stressors and physical loads as well as a plan for any emergencies (Table 2 ). Pre-planned assistance with luggage or transport by wheelchair at the point of departure might reduce pre-travel stress and physical exhaustion.
Dehydration and fluid intake
Patients with HF are susceptible to volume depletion during travel given that fluid intake, lifestyle and diuretics are tuned precisely to maintain a state of euvolaemia 59 (Fig. 2 ). A hypovolaemic state adversely affects cardiac and renal function, aggravates HF symptoms, and might interfere with the efficacy of HF medications. Fluid loss, caused by changes in temperature, diet (higher salt intake) or as a consequence of traveller’s diarrhoea, might occur during the flight.
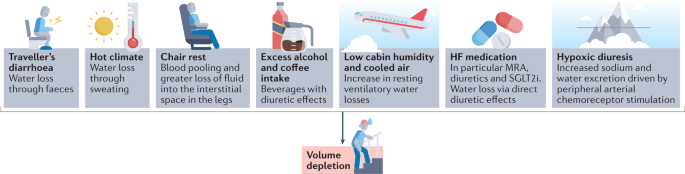
A vast array of factors contributes to volume depletion in patients with heart failure (HF) and require medication adjustment and increased fluid intake. MRA, mineralocorticoid receptor antagonists; SGLT2i, sodium–glucose cotransporter 2 inhibitor.
On board a plane, the low cabin humidity and cooled air can increase resting ventilatory water losses by approximately 200 ml per hour 60 . In addition, chair rest immobilization for 4 hours can decrease plasma volume by approximately 6% as a result of blood pooling and greater loss of fluid within the interstitial space in the legs 60 . Urinary output is often normal or only slightly reduced 61 . Sodium-free, alcoholic or caffeine-containing drinks consumed during the flight can promote diuresis and might further increase fluid loss. Furthermore, arrival to a hot and dry climate can result in loss of fluid through sweating and breathing by up to 1.2 l per day independently of physical activity 62 .
Apart from air travel and a transition in climate, acute diarrhoea is the most common illness in individuals travelling from resource-rich to resource-limited regions of the world 63 , 64 . Traveller’s diarrhoea usually occurs 4–14 days after arrival and results from bacterial (>90% of cases), viral and parasitic infections 64 . Approximately 10–40% of travellers to high-risk regions in Asia, Africa, and South and Central America experience diarrhoea during their travels 64 . Patients should be educated on food and water safety to prevent ingestion of pathogens. Cardiac dysfunction and HF management and treatment strategies, such as fluid restriction, diuretic therapy and renin–angiotensin–aldosterone system (RAAS) inhibitors, also increase the risk of diarrhoea-related complications in patients with HF during (temporal) hypovolaemia 63 , 64 .
Signs and symptoms of volume depletion and dehydration-associated electrolyte or acid–base disorders include fatigue, exercise intolerance, weight loss, increase in heart rate, muscle cramps, weakness, postural dizziness, abdominal pain, low urine volume, low blood pressure, lethargy and confusion. On the basis of invidualized risk assessment, patients should be advised to increase fluid intake by 0.5–1 l per day and to avoid alcohol or excessive coffee consumption during long-haul flights and hot weather. In case of signs and symptoms of volume depletion, therapy with diuretics, mineralocorticoid receptor antagonists and sodium–glucose cotransporter 2 inhibitors should be stopped or reduced for a day or longer until symptoms have resolved and body weight has returned to normal 65 . In case of postural or symptomatic hypotension, therapy with RAAS inhibitors and angiotensin receptor blocker–neprilysin inhibitors should be reduced or discontinued until symptoms have resolved; patients who experience postural or symptomatic hypotension require medical evaluation.
In a hot environment, patients with HF are advised to restrain from strenuous activity to avoid increased fluid loss. In case of uncomplicated traveller’s diarrhoea, patients need to increase fluid intake with oral rehydration solutions and monitor body weight and urinary output to avoid dehydration. Given that patients with HF are at an increased risk of complications, an antimotility agent (loperamide) and an antibiotic (azithromycin or rifaximin) can be prescribed for self-treatment 63 , 64 .
Venous thromboembolism
The risk of deep venous thrombosis (DVT) is greatly increased in patients with incident HF according to data from the ARIC cohort 66 and a systematic review 67 . The term ‘economy class syndrome’ has been used to describe the venous complications caused by cramped seating conditions 68 . The risk of DVT or pulmonary embolism is increased during travel that is >4 hours in duration, most probably owing to the associated immobility that is a key component of the Virchow triad of hypercoagulability, stasis and endothelial injury. Travelling in general (>4 hours in the preceding 8 weeks) is associated with a twofold increase in the risk of venous thrombosis 69 . This risk seems to be similar regardless of the mode of transportation (airplane, bus or train) 67 . The overall absolute incidence of symptomatic venous thromboembolism (VTE) in healthy individuals within the first month after a flight lasting >4 hours is approximately 1 in 4,600 flights and increases by 18% for each additional 2 hours in flight duration 2 , 70 . Importantly, the risk of VTE in individuals with pro-thrombotic risk factors, such as chronic HF, is substantially higher than in the general population. A 2021 meta-analysis found that patients with chronic HF were at an increased risk of VTE (risk ratio 1.57, 95% CI 1.34–1.84) 71 . A window seat compared with an aisle seat has been associated with a twofold greater risk of VTE or a sixfold greater risk in individuals with a BMI of >30 kg/m 2 (ref. 72 ).
Strategies to prevent VTE include appropriate loose clothing, frequent walks, calf muscle exercises, use of elastic compression stockings and adequate hydration 73 . Leg exercises have been shown to improve popliteal venous flow during prolonged immobility in seated individuals 74 . Furthermore, a systematic review of 11 randomized trials that included 2,906 individuals revealed the benefits of compression stockings (15–30 mmHg) on reducing the incidence of asymptomatic DVT and, with less evidence, of leg oedema 75 .
The evidence for thromboprophylaxis to prevent VTE during travel is very limited. The LONFLIT-3 study 76 randomly assigned 300 individuals at high risk of flight-related VTE to receive aspirin, enoxaparine (a low-molecular-weight heparin) or no prophylaxis. In total, 4.8% of patients in the control group were diagnosed with asymptomatic DVT compared with 3.6% in the aspirin group and 0% in the enoxaparine group. The authors of this small study concluded that one dose of enoxaparine might be an important option for individuals at high risk of DVT during long-haul flights 76 . Of note, specific studies of thromboprophylaxis during long-haul travel in patients with HF are lacking.
Medical emergencies during air travel
Patients with HF can travel by air if their condition is stable (Box 1 ). Commercial airplanes are required to carry basic emergency medical equipment according to regulations of the Federal Aviation Administration (FAA) in the USA and the European Aviation Safety Agency (EASA) in Europe 77 . Commercial aircrafts travelling from Europe to the USA have to meet both FAA and EASA requirements and, thus, must carry on board an external automated defibrillator, a saline infusion system and a bag-valve mask resuscitator 77 .
Data on on-board medical emergencies are sparse owing to the lack of international registries 78 . According to the available data provided by the airline Lufthansa, which contains details on approximately 20,000 on-board medical events from 2000 to 2011, cardiac emergencies accounted for 43% of on-board incidents 77 . Reported medical issues included circulatory collapse, high blood pressure, chest symptoms and dehydration 47 . On-board treatment included blood pressure management in 76% of incidents, drug administration in 54%, oxygen delivery in 48%, blood glucose measurement in 9%, monitoring of oxygen saturation in 6% and use of an automated external defibrillator in 6% 77 .
Considerations at the destination
Dietary considerations.
Dietary intake of fluids, sodium, potassium and alcohol during travel should be guided by current ESC recommendations for the management of patients with HF 3 , 79 . According to the guidelines, fluid restriction of 1.5–2.0 l per day might be considered in patients with severe HF to relieve symptoms and congestion 80 . When travelling to hot and dry destinations, an additional intake of 0.5–1.0 l per day of non-alcoholic drinks is recommended. Patients at risk of volume overload or on moderate-to-high doses of diuretics should be advised to regularly check their body weight. In case of body weight changes, patients can adjust doses of diuretics and the amount of fluid intake for a few days until body weight has normalized. Controlling sodium intake is important for patients at risk of hyponatraemia and for the management of oedema, although evidence showing the effects of sodium intake on HF outcomes is scarce 3 . During travel, increased consumption of foods high in salt can adversely affect sodium and volume balance and thereby exacerbate HF symptoms by causing fluid retention. Patients with HF and cardiorenal syndrome and/or treated with RAAS inhibitors are at increased risk of hyperkalaemia 81 . In patients with advanced chronic kidney disease (estimated glomerular filtration rate <30 ml/min/1.73 m²), a daily sodium intake of <3 g is recommended 81 . These patients should also be aware that certain foods, such as fresh fruits, juices, vegetables and milk products, contain high amounts of potassium.
Drinking habits also change during vacation. Moderate-to-heavy alcohol consumption is associated with increased risk of supraventricular arrhythmias, especially atrial fibrillation, and high blood pressure 82 , 83 . Therefore, increased intake of alcoholic beverages might aggravate HF symptoms and promote volume overload. Alcohol intake should be limited to two units per day for men with HF, one unit for women with HF, or no intake if alcohol has caused or contributed to the individual’s HF, as recommended by the ESC 3 .
Drug-induced photosensitivity
Numerous classes of drugs commonly used for the treatment of patients with HF have been associated with photo-induced, cutaneous drug eruptions, which are adverse effects that occur as a result of the exposure to a drug (and its presence in the skin) and ultraviolet or visible radiation 84 . Box 7 provides an overview of drugs that have been linked with drug-induced photosensitivity. Amiodarone can cause drug-induced photosensitivity in >50% of treated patients 84 . The typical presentation of this adverse effect is a burning and tingling sensation in sun-exposed skin, with associated erythema. Amiodarone induces a distinctive blue–grey pigmentation on sun-exposed sites in 1–2% of patients, particularly after long-term sun exposure. Another prototypical drug class associated with photosensitivity is thiazide diuretics, which includes hydrochlorothiazide 85 . Thiazide diuretics can trigger a variety of photosensitive eruptions, including an exaggerated sunburn reaction, dermatitis and a lichenoid eruption.
Various factors, such as time of day, season, geographical location, altitude and weather conditions, can affect the amount of ultraviolet radiation exposure 86 . In general, patients with HF should be advised to seek shade when outside, in particular around midday, and to keep in mind that radiation can be stronger when reflected by water, sand or snow. Patients in areas with high sun exposure should wear clothing that protects as much of the body as possible as well as sunglasses and broad-brimmed hats. Broad-spectrum sunscreens with a sun protection factor of 30 or higher are recommended 86 .
Box 7 Medications linked to drug-induced photosensitivity 80
Angiotensin-converting enzyme inhibitors
Ramipril, enalapril and quinapril
Angiotensin receptor blockers
Candesartan, irbesartan, losartan, olmesartan, telmisartan and valsartan
Anti-arrhythmic drugs
Amiodarone and dronedarone
Anti-depressant drugs
Citalopram, clomipramine, escitalopram, fluoxetine, fluvoxamine, imipramine, paroxetine, sertraline, St. John’s wort and venlafaxine
Antimicrobial drugs
Anti-fungals, anti-malarials, anti-tuberculous drugs, anti-retrovirals, β-lactams, fluoroquinolones, nalidixic acid, sulphonamides and tetracyclines
Calcium channel blockers
Amlodipine, diltiazem and nifedipine
Bumetanide, furosemide, indapamide, thiazides and triamterene
3-Hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitors
Atorvastatin, pravastatin and simvastatin
Non-steroidal anti-inflammatory drugs
Ampiroxicam, celecoxib, diclofenac, ibuprofen, indomethacin, ketoprofen, meclofenamide, nabumetone, naproxen, oxaprozin, piroxicam, sulindac and tiaprofenic acid
Psychotropic drugs
Anti-psychotic drugs (aripriprazole, chlorpromazine, clozanine, flupenthixol, haloperidol, olanzapine, risperidone and thioridazine) and anxiolytics (alprazolam and chlordiazepoxide)
Considerations for drivers
Driving regulations for individuals with HF take into account the severity of HF (NYHA class plus left ventricular ejection fraction) 54 . In the European Union, individuals with NYHA class I–III HF but not those with NYHA class IV HF are permitted to drive private vehicles. Patients with HF should ensure that they are permitted to drive in their travelling destination by accessing country-specific driving regulations online.
Considerations for patients with ICDs
Electromagnetic interference.
Many patients with HF are fitted with cardiac implantable electronic devices (CIEDs; namely ICDs), cardiac resynchronization therapy devices or pacemakers. These devices might be subject to electromagnetic interference (EMI) if exposed to a strong electromagnetic field (Table 3 ). Exposure of the device to EMI can result in device failure (loss of anti-bradycardia pacing with the risk of asystole), switch to asynchronous mode (pacing at a preset rate independent of intrinsic rhythm with the risk of inducing arrhythmias, including ventricular fibrillation), inappropriate tracking (atrial oversensing leading to rapid, irregular ventricular pacing) and in the inappropriate detection of ventricular tachyarrhythmias by ICDs, potentially with inappropriate shock therapy. High-voltage lines above trains, for example, have a strong electromagnetic field but the patient is shielded when inside the train. In trams or underground trains, electric motors can be located under the seat, whereas in cars and motorbikes, the only relevant source of EMI is the ignition system. Patients with a cardiac implantable device should be careful not lean over an unshielded, running motor.
Metal detectors at airport security checkpoints do not interfere with CIEDs 87 , 88 . However, patients with ICDs should be advised to have their device card ready to show to airport personnel before walking through the security checkpoint. To minimize the risk of interference, patients should move through metal detector gates at normal walking speed and should not linger. Hand-held scanners should not affect CIED functionality 89 but patients should ask personnel to move the wand over the device quickly and only once.
Magnets are not allowed in carry-on luggage and thus cannot be used to remedy inappropriate device activity on airplanes. EMI inside airplanes is rare but has been reported, for example, in association with electronic chair handles. Finally, cosmic radiation is approximately 100-fold higher during air travel, which increases the risk of radiation-induced EMI (for example, power-on reset).
Conclusions
The list of considerations for patients with HF embarking on national or international travel is extensive. Patients should be aware of an increased risk of cardiovascular events during their travels, which can be reduced with meticulous pre-travel risk assessment, physical examination, therapy adjustment and education. Pre-travel risk assessment should involve research into the local climate, air pollution levels, the distance and time for travelling, potential jet lag and altitude. En route, patients with HF should avoid volume depletion caused by extended chair rest, low cabin humidity and cooled air, excess alcohol or coffee intake, drugs with diuretic effects, hypoxia or traveller’s diarrhoea. Upon arrival at the destination, drug-induced photosensitivity and the health effects of local foods and beverages require consideration. Special recommendations are needed for patients after implantation of cardiac rhythm devices or LVADs as well as for patients who have undergone major cardiac surgery.
Ryan, E. T. & Kain, K. C. Health advice and immunizations for travelers. N. Engl. J. Med. 342 , 1716–1725 (2000).
Article CAS PubMed Google Scholar
Freedman, D. O., Chen, L. H. & Kozarsky, P. E. Medical considerations before international travel. N. Engl. J. Med. 375 , 247–260 (2016).
Article PubMed Google Scholar
Jaarsma, T. et al. Self-care of heart failure patients: practical management recommendations from the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 23 , 157–174 (2021).
Smith, D. et al. Fitness to fly for passengers with cardiovascular disease. Heart 96 (Suppl. 2), ii1–ii16 (2010).
PubMed Google Scholar
Aerospace Medical Association. Medical considerations for airline travel: surgical conditions (ASMA, 2021).
Dharmarajan, K. et al. Trajectories of risk after hospitalization for heart failure, acute myocardial infarction, or pneumonia: retrospective cohort study. BMJ 350 , h411 (2015).
Article PubMed PubMed Central Google Scholar
Alba, C. et al. Complications after heart transplantation: hope for the best, but prepare for the worst. Int. J. Transpl. Res. Med. 2 , 022 (2016).
Article Google Scholar
Curriero, F. C. et al. Temperature and mortality in 11 cities of the eastern United States. Am. J. Epidemiol. 155 , 80–87 (2002).
De Blois, J. et al. The effects of climate change on cardiac health. Cardiology 131 , 209–217 (2015).
Kenny, G. P., Yardley, J., Brown, C., Sigal, R. J. & Jay, O. Heat stress in older individuals and patients with common chronic diseases. CMAJ 182 , 1053–1060 (2010).
Bouchama, A. & Knochel, J. P. Heat stroke. N. Engl. J. Med. 346 , 1978–1988 (2002).
Faunt, J. D. et al. The effete in the heat: heat-related hospital presentations during a ten day heat wave. Aust. N. Z. J. Med. 25 , 117–121 (1995).
Sommet, A., Durrieu, G., Lapeyre-Mestre, M., Montastruc, J. L. & Association of French PharmacoVigilance Centres. A comparative study of adverse drug reactions during two heat waves that occurred in France in 2003 and 2006. Pharmacoepidemiol. Drug Saf. 21 , 285–288 (2012).
McCormack, M. C. et al. Colder temperature is associated with increased COPD morbidity. Eur. Respir. J. 49 , 1601501 (2017).
AirNow. Air Quality Index (AQI) basics. AirNow https://airnow.gov/index.cfm?action=aqibasics.aqi (2019).
Miller, K. A. et al. Long-term exposure to air pollution and incidence of cardiovascular events in women. N. Engl. J. Med. 356 , 447–458 (2007).
Pope, C. A. Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. JAMA 287 , 1132–1141 (2002).
Article CAS PubMed PubMed Central Google Scholar
Escolar, V. et al. Impact of environmental factors on heart failure decompensations. ESC Heart Fail. 6 , 1226–1232 (2019).
Shah, A. S. et al. Global association of air pollution and heart failure: a systematic review and meta-analysis. Lancet 382 , 1039–1048 (2013).
Barregard, L. et al. Experimental exposure to wood-smoke particles in healthy humans: effects on markers of inflammation, coagulation, and lipid peroxidation. Inhal. Toxicol. 18 , 845–853 (2006).
Törnqvist, H. et al. Persistent endothelial dysfunction in humans after diesel exhaust inhalation. Am. J. Respir. Crit. Care Med. 176 , 395–400 (2007).
Wold, L. E. et al. Cardiovascular remodeling in response to long-term exposure to fine particulate matter air pollution. Circ. Heart Fail. 5 , 452–461 (2012).
Tofler, G. H. & Muller, J. E. Triggering of acute cardiovascular disease and potential preventive strategies. Circulation 114 , 1863–1872 (2006).
Higgins, J. P., Tuttle, T. & Higgins, J. A. Altitude and the heart: is going high safe for your cardiac patient? Am. Heart J. 159 , 25–32 (2010).
US Office of the Federal Register. Code of Federal Regulations: Title 14 aeronautics and space, part 25.841 (US Government Printing Office, 1986).
Seccombe, L. M. & Peters, M. J. Physiology in medicine: acute altitude exposure in patients with pulmonary and cardiovascular disease. J. Appl. Physiol. 116 , 478–485 (2014).
Imray, C., Booth, A., Wright, A. & Bradwell, A. Acute altitude illnesses. BMJ 343 , d4943 (2011).
Bärtsch, P. & Gibbs, J. S. Effect of altitude on the heart and the lungs. Circulation 116 , 2191–2202 (2007).
Jones, J. G., Bakewell, S. E., Heneghan, C. P., Jones, S. E. & Snape, S. L. Profound hypoxemia in pulmonary patients in airline-equivalent hypoxia: roles of VA/Q and shunt. Aviat. Space Env. Med. 79 , 81–86 (2008).
Sawka, M. N., Convertino, V. A., Eichner, E. R., Schnieder, S. M. & Young, A. J. Blood volume: importance and adaptations to exercise training, environmental stresses, and trauma/sickness. Med. Sci. Sports Exerc. 32 , 332–348 (2000).
Cheung, S. S. et al. Ventilatory chemosensitivity, cerebral and muscle oxygenation, and total hemoglobin mass before and after a 72-day mt. Everest expedition. High Alt. Med. Biol. 15 , 331–340 (2014).
Hughson, R. L., Yamamoto, Y., McCullough, R. E., Sutton, J. R. & Reeves, J. T. Sympathetic and parasympathetic indicators of heart rate control at altitude studied by spectral analysis. J. Appl. Physiol. 77 , 2537–2542 (1994).
Vogel, J. A. & Harris, C. W. Cardiopulmonary responses of resting man during early exposure to high altitude. J. Appl. Physiol. 22 , 1124–1128 (1967).
Heistad, D. D., Abboud, F. M. & Dickinson, W. Richards Lecture: circulatory adjustments to hypoxia. Circulation 61 , 463–470 (1980).
Agostoni, P. et al. Effects of simulated altitude-induced hypoxia on exercise capacity in patients with chronic heart failure. Am. J. Med. 109 , 450–455 (2000).
Negrao, C. E. & Middlekauff, H. R. Adaptations in autonomic function during exercise training in heart failure. Heart Fail. Rev. 13 , 51–60 (2008).
Parati, G. et al. Clinical recommendations for high altitude exposure of individuals with pre-existing cardiovascular conditions: a joint statement by the European Society of Cardiology, the Council on Hypertension of the European Society of Cardiology, the European Society of Hypertension, the International Society of Mountain Medicine, the Italian Society of Hypertension and the Italian Society of Mountain Medicine. Eur. Heart J. 39 , 1546–1554 (2018).
Pratt, M. C. et al. Effect of angiotensin converting enzyme inhibitors on erythropoietin concentrations in healthy volunteers. Br. J. Clin. Pharmacol. 34 , 363–365 (1992).
Swenson, E. R. Carbonic anhydrase inhibitors and high altitude illnesses. Subcell. Biochem. 75 , 361–386 (2014).
Stewart, S., Keates, A. K., Redfern, A. & McMurray, J. J. V. Seasonal variations in cardiovascular disease. Nat. Rev. Cardiol. 14 , 654–664 (2017).
Stewart, S., McIntyre, K., Capewell, S. & McMurray, J. J. Heart failure in a cold climate. Seasonal variation in heart failure-related morbidity and mortality. J. Am. Coll. Cardiol. 39 , 760–766 (2002).
Hayward, J. M., Holmes, W. F. & Gooden, B. A. Cardiovascular responses in man to a stream of cold air. Cardiovasc. Res. 10 , 691–696 (1976).
Westheim, A. et al. Haemodynamic and neurohumoral effects of cold pressor test in severe heart failure. Clin. Physiol. 12 , 95–106 (1992).
Barnett, A. G., de Looper, M. & Fraser, J. F. The seasonality in heart failure deaths and total cardiovascular deaths. Aust. N. Z. J. Public Health 32 , 408–413 (2008).
Moholdt, T. Excess mortality at Christmas due to cardiovascular disease in the HUNT study prospective population-based cohort in Norway. BMC Public Health 21 , 549 (2021).
Schlagenhauf, P. et al. Sex and gender differences in travel-associated disease. Clin. Infect. Dis. 50 , 826–832 (2010).
McIntosh, I. B., Power, K. G. & Reed, J. M. Prevalence, intensity, and sex differences in travel related stressors. J. Travel Med. 3 , 96–102 (1996).
Taber, J. M., Leyva, B. & Persoskie, A. Why do people avoid medical care? A qualitative study using national data. J. Gen. Intern. Med. 30 , 290–297 (2015).
Aerospace Medical Association. Medical considerations for airline travel: anemia (ASMA, 2021).
Roig, E. et al. Disabling angina pectoris with normal coronary arteries in patients undergoing long-term hemodialysis. Am. J. Med. 71 , 431–434 (1981).
Brignole, M. et al. 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: the Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Eur. Heart J. 34 , 2281–2329 (2013).
Dubner, S. et al. ISHNE/EHRA expert consensus on remote monitoring of cardiovascular implantable electronic devices (CIEDs). Ann. Noninvasive Electrocardiol. 17 , 36–56 (2012).
Slotwiner, D. et al. HRS Expert Consensus Statement on remote interrogation and monitoring for cardiovascular implantable electronic devices. Heart Rhythm 12 , e69–e100 (2015).
Simpson, C. et al. Canadian cardiovascular society consensus conference. Assessment of the cardiac patient for fitness to drive and fly – executive summary. Can. J. Cardiol. 20 , 1313–1323 (2004).
Google Scholar
Cassivi, S. D. et al. Safety of air travel in the immediate postoperative period after anatomic pulmonary resection. J. Thorac. Cardiovasc. Surg. 153 , 1191–1196.e1 (2017).
MyLVAD Foundation. 10 Tips for traveling with an LVAD. MyLVAD https://www.mylvad.com/patients-caregivers/discuss-connect/forums/1048-10-tips-traveling-lvad (2011).
Kupper, N., Denollet, J., Widdershoven, J. & Kop, W. J. Cardiovascular reactivity to mental stress and mortality in patients with heart failure. JACC Heart Fail. 3 , 373–382 (2015).
Strike, P. C. & Steptoe, A. A systematic review of mental stress-induced myocardial ischaemia. Eur. Heart J. 24 , 690e703 (2003).
Mullens, W. et al. The use of diuretics in heart failure with congestion - a position statement from the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 21 , 137–155 (2019).
Greenleaf, J. E., Rehrer, N. J., Mohler, S. R., Quach, D. T. & Evans, D. G. Airline chair-rest deconditioning: induction of immobilisation thromboemboli? Sports Med. 34 , 705–725 (2004).
Greenleaf, J. E., Shvartz, E., Kravik, S. & Keil, I. C. Fluid shifts and endocrine responses during chair rest and water immersion in man. J. Appl. Physiol. 48 , 79–88 (1980).
Better, O. S. Impaired fluid and electrolyte balance in hot climates. Kidney Int. Suppl. 21 , S97–S101 (1987).
CAS PubMed Google Scholar
Riddle, M. S. et al. Guidelines for the prevention and treatment of travelers’ diarrhea: a graded expert panel report. J. Travel Med. 24 (Suppl. 2), S57–S74 (2017).
Steffen, R., Hill, D. R. & DuPont, H. L. JAMA patient page. Traveler’s diarrhea. JAMA 313 , 108 (2015).
Rosenstock, J. & Ferrannini, E. Euglycemic diabetic ketoacidosis: a predictable, detectable, and preventable safety concern with SGLT2 inhibitors. Diabetes Care 38 , 1638–1642 (2015).
Fanola, C. L. et al. Incident heart failure and long-term risk for venous thromboembolism. J. Am. Coll. Cardiol. 75 , 148–158 (2020).
Trujillo-Santos, A. J., Jiménez-Puente, A. & Perea-Milla, E. Association between long travel and venous thromboembolic disease: a systematic review and meta-analysis of case-control studies. Ann. Hematol. 87 , 79–86 (2008).
Czuprynska, J. & Arya, R. Annotation: travel and thrombosis. Br. J. Haematol. 188 , 838–843 (2020).
Cannegieter, S. C., Doggen, C. J., van Houwelingen, H. C. & Rosendaal, F. R. Travel-related venous thrombosis: results from a large population-based case control study (MEGA study). PLoS Med. 3 , e307 (2006).
Kahn, S. R. et al. Prevention of VTE in nonsurgical patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141 (Suppl. 2), e195S–e226S (2012).
Xu, T. et al. Heart failure is associated with increased risk of long-term venous thromboembolism. Korean Circ. J. 51 , 766–780 (2021).
Schreijer, A. J., Cannegieter, S. C., Doggen, C. J. & Rosendaal, F. R. The effect of flight-related behaviour on the risk of venous thrombosis after air travel. Br. J. Haematol. 144 , 425–429 (2009).
Dusse, L. M. S., Silva, M. V. F., Freitas, L. G., Marcolino, M. S. & Carvalho, M. D. G. Economy class syndrome: what is it and who are the individuals at risk? Rev. Bras. Hematol. Hemoter. 39 , 349–353 (2017).
Hitos, K., Cannon, M., Cannon, S., Garth, S. & Fletcher, J. P. Effect of leg exercises on popliteal venous blood flow during prolonged immobility of seated subjects: implications for prevention of travel-related deep vein thrombosis. J. Thromb. Haemost. 5 , 1890–1895 (2007).
Clarke, M. J., Broderick, C., Hopewell, S., Juszczak, E. & Eisinga, A. Compression stockings for preventing deep vein thrombosis in airline passengers. Cochrane Database Syst. Rev. 9 , CD004002 (2016).
Cesarone, M. R. et al. Venous thrombosis from air travel: the LONFLIT3 study–prevention with aspirin vs low-molecular-weight heparin (LMWH) in high-risk subjects: a randomized trial. Angiology 53 , 1–6 (2002).
Graf, J., Stüben, U. & Pump, S. In-flight medical emergencies. Dtsch. Arztebl Int. 109 , 591–602 (2012).
PubMed PubMed Central Google Scholar
Goodwin, T. In-flight medical emergencies: an overview. BMJ 321 , 1338 (2000).
McDonagh, T. A. et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 42 , 3599–3726 (2021).
Seferovic, P. M. et al. Clinical practice update on heart failure 2019: pharmacotherapy, procedures, devices and patient management. An expert consensus meeting report of the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 21 , 1169–1186 (2019).
Kalantar-Zadeh, K. & Fouque, D. Nutritional management of chronic kidney disease. N. Engl. J. Med. 377 , 1765–1776 (2017).
Hindricks, G. et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur. Heart J. 42 , 373–498 (2021); erratum 42, 507 (2021); erratum 42, 546–547 (2021).
Tasnim, S., Tang, C., Musini, V. M. & Wright, J. M. Effect of alcohol on blood pressure. Cochrane Database Syst. Rev. 7 , CD012787 (2020).
Drucker, A. M. & Rosen, C. F. Drug-induced photosensitivity: culprit drugs, management and prevention. Drug Saf. 34 , 821–837 (2011).
Blakely, K. M., Drucker, A. M. & Rosen, C. F. Drug-induced photosensitivity-an update: culprit drugs, prevention and management. Drug Saf. 42 , 827–847 (2019).
US Food and Drug Administration. The Sun and your medicine (FDA, 2015).
Kolb, C. et al. Do airport metal detectors interfere with implantable pacemakers or cardioverter-defibrillators? J. Am. Coll. Cardiol. 41 , 2054–2059 (2003).
Copperman, Y., Zarfati, D. & Laniado, S. The effect of metal detector gates on implanted permanent pacemakers. Pacing Clin. Electrophysiol. 11 , 1386–1387 (1988).
Jilek, C. et al. Safety of screening procedures with hand-held metal detectors among patients with implanted cardiac rhythm devices: a cross-sectional analysis. Ann. Intern. Med. 155 , 587–592 (2011).
Download references
Acknowledgements
This Review is the result of a cooperation under the umbrella of the Study Group 10 (heart failure) of the German Cardiac Society. S.v.H. has received research funding from the German Center for Cardiovascular Research (DZHK). T.K. has received research funding from the German Heart Research Foundation and is supported by the German Research Foundation (Clinical Research Unit KFO311). R.W. has received research support from the German Center for Cardiovascular Research (DZHK).
Author information
Authors and affiliations.
Department of Cardiology and Pneumology, University of Göttingen Medical Center, Göttingen, Germany
Stephan von Haehling, Kristian Hellenkamp, Rolf Wachter & Gerd Hasenfuss
German Center for Cardiovascular Research (DZHK), Partner Site Göttingen, Göttingen, Germany
Stephan von Haehling, Rolf Wachter & Gerd Hasenfuss
Department of Internal Medicine II, University Hospital Regensburg, Regensburg, Germany
Christoph Birner
Department of Internal Medicine I, Klinikum St. Marien, Amberg, Germany
Institute of Gender in Medicine, Charité – Universitaetsmedizin Berlin, Corporate Member of Freie Universität Berlin and Berlin Institute of Health, Berlin, Germany
Elke Dworatzek
German Centre for Cardiovascular Research (DZHK), Partner Site Berlin, Berlin, Germany
Elke Dworatzek & Christoph Knosalla
Department of Internal Medicine I, University Hospital Würzburg, Würzburg, Germany
Stefan Frantz
Klinik für Innere Medizin, Kardiologie, Diabetologie and Nephrologie, Evangelisches Klinikum Bethel, Bielefeld, Germany
Carsten W. Israel
Department of Cardiology and Angiology, Hannover Medical School, Hannover, Germany
Tibor Kempf
Helios Klinikum Warburg, Idar–Oberstein, Germany
Hermann H. Klein
Department of Cardiothoracic and Vascular Surgery, German Heart Center Berlin, Berlin, Germany
Christoph Knosalla
Charité–Universitätsmedizin Berlin, corporate member of Freie Universität Berlin, Humoldt–Universität zu Berlin and Berlin Institute of Health, Berlin, Germany
Klinik und Poliklinik für Kardiologie, Universitätsklinikum Leipzig, Leipzig, Germany
Ulrich Laufs & Rolf Wachter
Department of Cardiology, Angiology and Pneumology, Heidelberg University Hospital, Heidelberg, Germany
Philip Raake
German Center for Cardiovascular Research (DZHK), Partner Site Heidelberg/Mannheim, Heidelberg, Germany
You can also search for this author in PubMed Google Scholar
Contributions
S.v.H. wrote the article. All the authors researched data for the article, contributed to discussion of content, and reviewed and edited the manuscript before submission.
Corresponding author
Correspondence to Stephan von Haehling .
Ethics declarations
Competing interests.
S.v.H. has been a paid consultant for and/or received honoraria payments from AstraZeneca, Bayer, Boehringer Ingelheim, BRAHMS, Chugai, Grünenthal, Helsinn, Hexal, Novartis, Pharmacosmos, Respicardia, Roche, Servier, Sorin, and Vifor and has received research funding from Amgen, Boehringer Ingelheim and IMI. T.K. has been a paid consultant for and/or received honoraria payments from AstraZeneca, Bayer, Boehringer Ingelheim, Bristol Myers Squibb, Novartis, Pharmacosmos, and Vifor and has received research support from Vifor. P.R. has been a paid consultant for and/or received honoraria payments from Abbott, AstraZeneca, Bayer, BDI, Biotronik, Conventus Congressmanagement & Marketing GmbH, CTI GmbH, Daiichi-Sankyo, Deutsche Gesellschaft für Kardiologie, Diaplan, Edwards, Elisabeth-KH Essen, Heart Institute GmbH, Herzzentrum Leipzig, Kelcon, Medizinische Ausstellungs- und Werbegesellschaft Wien, Medtronic, Novartis and Vifor. R.W. has been a paid consultant for and/or received honoraria payments from AstraZeneca, Bayer, BMS, Boehringer Ingelheim, CVRx, Daiichi, Medtronic, Novartis, Pfizer, Pharmacosmos and Servier. R.W. has received research support from Boehringer Ingelheim, Bundesministerium für Bildung und Forschung, Deutsche Forschungsgemeinschaft, European Union and Medtronic. G.H. has been a paid consultant for and/or received honoraria payments from AstraZeneca, Bayer, Berlin Chemie, Boehringer Ingelheim, Corvia, Impulse Dynamics, Novartis, Servier, Springer and Vifor. All other authors declare no competing interests.
Additional information
Peer review information.
Nature Reviews Cardiology thanks Biykem Bozkurt, Tiny Jaarsma and Simon Stewart for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
von Haehling, S., Birner, C., Dworatzek, E. et al. Travelling with heart failure: risk assessment and practical recommendations. Nat Rev Cardiol 19 , 302–313 (2022). https://doi.org/10.1038/s41569-021-00643-z
Download citation
Accepted : 01 November 2021
Published : 06 January 2022
Issue Date : May 2022
DOI : https://doi.org/10.1038/s41569-021-00643-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Heart failure with preserved ejection fraction: diagnosis, risk assessment, and treatment.
- Stephan von Haehling
- Birgit Assmus
- Johann Bauersachs
Clinical Research in Cardiology (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
What to Know Before Traveling With Lymphedema
This side effect of breast cancer treatment can impact your travel plans.
Traveling With Lymphedema
A common side effect of breast cancer treatments is a condition called lymphedema , in which lymph fluid builds up and creates an uncomfortable swelling. This happens because lymph nodes have been removed to check for cancer or because they were cancerous, and after the surgery is complete, the body loses some of its ability to move lymph fluid through the area. Chemotherapy and radiation therapies can also damage lymph nodes, which are an important part of the body's immune system.
Dr. Roman Skoracki, division chief for oncologic reconstructive surgery at the Ohio State University Wexner Medical Center, explains that the body uses lymph fluid to monitor for infections. Lymph fluid, which results from cellular processes, "moves from the extremities to the core in unidirectional flow," he says. The muscles of the body act as sort of pumps to help move the fluid along until it hits a cluster of lymph nodes. "This is the whole point of the system," Skoracki says. "The fluid gets filtered and examined in the lymph nodes. It's the immune system's way of surveying the entire body constantly."
[See: 7 Innovations in Cancer Therapy .]
These clusters of nodes are scattered throughout the body, with most people having anywhere from 20 to 40 nodes in the axilla area – the armpit – and that's the source of the problem for most cases of breast cancer-related lymphedema.
For many breast cancer patients , some lymph nodes in this region may be removed as part of their treatment , and this can create a stopping point for that fluid as it tries to clear the body. "The fluid continues to get produced and collected and moves up the extremities. But then it hits a dead-end" when it reaches the axilla area, Skoracki says. "That's where it starts to swell like a traffic jam, where the cars pile up," and fluid can back up down the arm.
Most people have enough redundancy in the system that the fluid can find another way to get around the blockage, but according to The Memorial Sloan Kettering Cancer Center, about 15 to 25 percent of patients who've undergone an axillary lymph node dissection will develop lymphedema. The National Cancer Institute reports patients who've had sentinel node biopsies have a 5 to 17 percent risk of developing lymphedema.
A Patient's Guide to Breast Cancer
Elaine K. Howley Aug. 9, 2019

This development can create real problems for these patients, as lymphedema can negatively impact daily life . Cases of breast cancer-related lymphedema typically occur in the arm on the same side where the cancer was, and in severe cases of lymphedema, limb functionality may be reduced. The swelling and heaviness of the limb that are the hallmark symptoms can progress to a point where the limb becomes less usable. But long before that, even formerly simple activities like flying to another city can become problematic.
Although there's currently no cure for lymphedema, there are several ways to manage it, and if you're getting ready for a trip – particularly one that involves air travel – you'll want to make sure you're on top of your lymphedema management routine. One of the most common ways of controlling the condition is the use of compression garments. Typically shaped like a tight sleeve and worn along the arm where the lymphedema has developed, these garments squeeze the tissues in the affected limb and prevent fluid from building up.
Dr. Richard Klein, section chief for plastic and reconstructive surgery at Orlando Health Aesthetic and Reconstructive Surgery Institute, says that when traveling, "the most important thing is anyone who's had lymph nodes removed … if they fly, they wear a sleeve even if they don't have a [lymphedema] diagnosis." That's because the conditions inside the standard commercial airliner can cause swelling. "In an airplane, the air is pressurized to the equivalent of about 8,000 feet. The altitude can trigger an episode in someone with lymphedema and exacerbate the condition."
[See: Breast Pain? Stop Worrying About Cancer .]
According to an airline travel guide prepared by the National Lymphedema Network, this happens because "changes in fluid production in the tissues occur when the external pressures exerted on the limb are changed. Diminished pressure in the airplane cabin will result in a decrease in the fluid moved in to the lymphatic system. The fluid will remain in the extracellular spaces and an exacerbation of lymphedema may result."
To help prevent this, Klein says, "the most important thing is applying pressure to the limb." And lymphedema patients should visit with their lymphedema therapist before and after a flight to remove as much fluid from the limb as possible. "Lymphedema care is not only the garment. Doing manual lymphatic drainage and getting the fluid out is also important. The garment isn't going to get the fluid out, but it's going to prevent it from coming back," he says.
In addition to wearing your compression sleeve, Klein recommends that anyone who's had lymph nodes removed watch their salt intake prior to a flight, as salt can cause the body to retain more fluid than it normally does, which can lead to a worsening of the lymphedema.
Can Exercise Help With My Breast Cancer?
Elaine K. Howley June 29, 2017

And depending on where you're headed, you may need to be mindful of the limb and how it's responding to local conditions. If you're traveling to Denver, for example, where the elevation is more than a mile up, wear your sleeve and stay vigilant for changes in the limb. Similarly, if you're headed somewhere hot and humid, you may experience more swelling than if you go to Alaska.
Because hot, humid conditions can cause blood vessels to dilate and move more fluid into the affected limb, keeping cool is important for lymphedema patients. In a blog post for the NLN, lymphedema therapist DeCourcy Squire offers tips for staying cool . "Drink lots of water, even more than you do in the winter, to help keep yourself well hydrated. This makes it easier for your body to regulate its temperature. Even if salty foods don't normally affect your swelling, they may be more likely to in the summer. For crunchy snacks, go for fresh raw vegetables instead of potato chips." And when it comes to clothing, selecting loose or free-flowing garments can help keep you cooler.
[See: The 10 Best Diets for Healthy Eating .]
And if you're headed somewhere to enjoy the great outdoors, be sure to remember your insect repellent and sunblock. Insect bites and sunburn can both increase swelling from lymphedema, as the immune system attempts to clear the damage to the skin.
The bottom line, says Kate Howell, a doctor of physical therapy and certified lymphedema therapist with Peltz and Associates Physical Therapy in Santa Rosa, California, is that lymphedema patients must "constantly pay attention. You always want to be acting prophylactically. Once you have it, it's got to be on your radar and you can't ignore it. Lymphedema is a marathon with no end. You need to figure out how you can manage it," and following your doctor or lymphedema therapist's recommendations can help you keep traveling and doing all the other things you want to do.
Best Hospitals for Cancer
Hospital Ranking information as of August 29th, 2017
Tags: breast cancer , cancer , patients , patient advice , Travel
Most Popular
Patient Advice

health disclaimer »
Disclaimer and a note about your health ».

Your Health
A guide to nutrition and wellness from the health team at U.S. News & World Report.
You May Also Like
How to find the best spinal surgeon.
Elaine K. Howley May 6, 2024
Finding the Best Orthopedic Surgeon
Elaine K. Howley May 3, 2024
Does Medicare Cover Ozempic?
Paul Wynn May 2, 2024
Is Mifepristone Safe?
Payton Sy May 1, 2024
Health Screening Tests Women Should Have
Angela Haupt and Gretel Schueller May 1, 2024

Doctors That Women Should See
Vanessa Caceres and Gretel Schueller May 1, 2024
How to Find the Best OB-GYN for You
Elaine K. Howley and Gretel Schueller May 1, 2024

Early Miscarriage Symptoms
Claire Wolters April 30, 2024

11 Tips for Your First Mammogram
Elaine K. Howley April 29, 2024

Osteoporosis, Osteoarthritis, Osteopenia
Payton Sy April 29, 2024

Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Hosted content
- BMJ Journals More You are viewing from: Google Indexer
You are here
Should i stay or should i go pulmonary embolism and air travel.
The global increase in air travel, with over 3.97 billion people traveling by air each year, and the ageing population, increase the number of those with an illness who wish to travel (1). Even more, in countries like Greece with hundreds of islands, health professionals are frequently asked to assess a patient’s fitness to fly. Doctors can receive advice and guidance mainly from two sources: the IATA passenger medical clearance guidelines (2) and the Aerospace Medical Association in which the British Thoracic Society’s recommendations for air travel (3) are suggested. Many respiratory conditions can affect a passenger’s fitness to fly with pulmonary embolism being the most debatable (3). A major question that respiratory physicians frequently have to answer, mostly with visitors from overseas who need to be repatriated following diagnosis of pulmonary embolism, is about the right time to “fly with a clot”. The British Thoracic Society guidelines recommend against airline travel during the first four weeks following pulmonary embolism (3). On the other hand, in the IATA medical guidelines published in 2018 it is suggested that patients can fly 5 days after an acute pulmonary embolism episode, if they receive anticoagulation and their PaO2 is normal on room air (2). Although there is little scientific evidence to support the above mentioned recommendations, the huge difference in the suggested period can really confuse healthcare professionals. Moreover, asking patients-tourists to remain in a travel destination one month more than scheduled, launches their cost of stay and many times they are proven unable to follow this recommendation. In our opinion, one size does not fit all. The 4-week period seems too long for a patient with pulmonary embolism severity index I or II, no evidence of right ventricular dysfunction on an imaging test, negative laboratory biomarkers on presentation (low risk patient) and a normal PaO2 on room air (4). On the other hand, the 4-week period and even more the 5-day period may be too short for a patient with pulmonary embolism severity index III-V, evidence of right ventricular dysfunction on an imaging test and positive laboratory biomarkers on presentation (intermediate high risk patient), who has a significantly higher mortality rate during the first thirty days even without traveling (4). Thus, we believe that the risk of flying after being diagnosed with pulmonary embolism is not the same for all patients and in every case we should take into consideration the risk stratification on presentation and the PaO2 level. Further carefully designed studies taking into account risk stratification will give the answer to the tough question “should I stay or should I go” after pulmonary embolism.
References The World Bank. Air transport, passengers carried. https://data.worldbank.org/indicator/IS.AIR.PSGR Date last accessed: December 7, 2018. International Air Transport Association. Medical manual 11th edition. https://www.iata.org/publications/Documents/medical-manual.pdf 2018 Ahmedzai S1, Balfour-Lynn IM, Bewick T, Buchdahl R, Coker RK, Cummin AR, Gradwell DP, Howard L, Innes JA, Johnson AO, Lim E, Lim WS, McKinlay KP, Partridge MR, Popplestone M, Pozniak A, Robson A, Shovlin CL, Shrikrishna D, Simonds A, Tait P, Thomas M; British Thoracic Society Standards of Care Committee. Managing passengers with stable respiratory disease planning air travel: British Thoracic Society recommendations. Thorax. 2011 Sep;66 Suppl 1:i1-30. Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D, Galiè N, Gibbs JS, Huisman MV, Humbert M, Kucher N, Lang I, Lankeit M, Lekakis J, Maack C, Mayer E, Meneveau N, Perrier A, Pruszczyk P, Rasmussen LH, Schindler TH, Svitil P, Vonk Noordegraaf A, Zamorano JL, Zompatori M; Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014 Nov 14;35(43):3033-69, 3069a-3069k.
Conflict of Interest
FREE US STANDARD SHIPPING ON ORDERS $200+
Lymphedema Risk During Air Travel
February 24, 2017
If you have had lymph node surgery such as an axillary lymph node dissection (ALND) or sentinel lymph node biopsy (SLNB) and/or radiation therapy as a part of your breast cancer treatment then you are at risk for breast cancer related lymphedema (BCRL). According to the National Cancer Institute, as many as 56% of women who undergo breast cancer surgery develop lymphedema within two years post-surgery, but the risk remains up to 30 years later [ 1 ]. Women who undergo ALND have a lifetime risk of up to 50% and women who undergo SLNB have a lifetime risk of 6% [ 2 ].
When traveling it’s important to be aware of travel-related risk factors that can exacerbate the condition and cause the onset of lymphedema or an increase in existing swelling. When traveling by air, the decreased pressure that is experienced within the cabin can give rise to increased swelling . The National Lymphedema Network recommends the use of compression garments to “provide external pressure on the extremity to adequately support favorable resorption and decrease the potential for fluid accumulation in the tissue”[ 3 ]. Wearing compression garments during air travel reduces lymphedema swelling risk by “First, resorption of fluid at the capillary level is enhanced due to the compression. Seconds, the garment or bandages stimulate the lymphatic system, via the muscle pump, and uptake of extracellular fluid increases, helping to prevent exacerbation of lymphedema” [ 3 ]. There are additional aspects of air travel that may exacerbate lymphedema risk or swelling. The sedentary nature of travel causes blood and lymphatic circulation to slow, standing, moving around the cabin and moving the affected limb frequently can help increase lymphatic fluid circulation and reduce swelling risk.
It is important to take into consideration that wearing compression garments in route can be just as important in avoiding swelling. When in route to the airport or if traveling by car or train it is best to avoid carrying or lifting heavy luggage and/or bags with shoulder straps with the affected or at-risk arm. Heavy bags can increase muscle stress, while bags with shoulder straps can create a tourniquet by impeding lymphatic circulation -- both of which can exacerbate swelling.
If you think you may be at-risk for lymphedema or have existing swelling, it is important to be properly fitted for a compression garment by your doctor, physical, occupational or lymphedema therapist prior to hitting the road.
Download Lymphedema Risk During Air Travel PDF
- #risk reduction
- #white paper
- Search Please fill out this field.
- Manage Your Subscription
- Give a Gift Subscription
- Newsletters
- Sweepstakes
If you click on links we provide, we may receive compensation.
- Travel Products
- Trends + Deals We Love
10 TikTok-approved Packing Essentials That Flight Attendants Won’t Travel Without — From $10
Best of all, everything is under $50.
:max_bytes(150000):strip_icc():format(webp)/IMG_9861-28adc25e5c9643fa9f55e077a316c3f4.jpg)
Travel + Leisure / Tyler Roeland
Flight attendants, by nature, are highly seasoned travelers, and are therefore brimming with untapped knowledge on how to make your time in the sky (and on the road) all the more enjoyable. Thankfully, many of them have taken to TikTok to share their treasure trove of tips and tricks for optimized packing — and we took notes.
We dove into flight attendant TikTok to discover exactly what they bring along when prioritizing comfort, functionality, and safety, and many of their top picks are available at Amazon. From supportive travel pillows and cushions , to portable door locks and even a compact humidifier for dry nights, these are the 10 products airline workers won’t travel without — all under $50.
Clarks Calla Ease Loafer Flat
Comfy shoes are pivotal for long travel days, and nobody knows this to be true more than flight attendants. If you’re looking for a slightly more stylish option than your favorite pair of running sneakers, take it from one airline worker on TikTok that these cushy loafers from Clarks are a top-notch selection for spending extended time on your feet thanks to the foam-cushioned insoles, a long-lasting 100 percent leather exterior, and thick, sturdy outsoles. Plus, right now you can score these shoes for up to 58 percent off in one of the four neutral colors.
Zzrui Upgraded Portable Door Stopper Wedge Alarm
Whether you’re staying in a hotel alone or with a group of friends, it never hurts to come prepared with additional safety measures, and flight attendants swear that this portable door wedge alarm is exactly what you need to feel secure. Simply turn it on and place the device against the door before you head to sleep, and if any pressure is applied it will emit a blaring noise to scare away intruders. One flight attendant shared that they prefer to use one for the primary door of their room and another for any potential adjoining rooms.
HotLogic Mini Portable Electric Lunch Box
It’s no secret that the food in airports isn’t necessarily top notch. To avoid paying for overpriced food, flight attendants on TikTok rave about the HotLogic lunch box, a portable oven that heats up pre-packed meals or dinner. You can easily stow it in your carry-on or hotel room without having to turn to a cheap microwave that won’t evenly heat your food. And not only has it earned a stamp of approval from countless airline workers, but it has also racked up more than 32,800 five-star ratings at Amazon after travelers revealed that it “changed” their “layover eating life.”
AceMining Portable Door Lock
This best-selling safety device has made it into numerous TikToks from flight attendants who swear by the added protection it provides to hotel room doors, and for just $15, it’s a no-brainer addition to your carry-on the next time you travel. The compact lock is easy to use: Just close your door around the metal attachment and insert the second piece into the frame once the door is closed. Not only does this act as additional security, but it also stops housekeeping from entering if you’re hoping to get some extra shut eye in the morning. It’s durable, packable, and well-suited for a wide range of doors — so long as they open inwards.
Jisulife Mini Portable Humidifier
Air travel can be incredibly drying to the skin (especially during long-haul flights), but this portable humidifier is here to transform your next hotel stay — and flight attendants swear by it . The slim and packable device offers up to seven hours of use thanks to its rechargeable battery, and it instantly adds moisture to the air when placed into any cup of water. It’s quiet, easy to use, and a game-changer for both your skin and sinuses.
Twelve South AirFly SE Bluetooth Wireless Transmitter
Gone are the days of using airline-issued earbuds with the help of the flight attendant-approved AirFly Bluetooth Wireless Transmitter. This pocket-sized device can be plugged into your plane seat and connects to up to two pairs of wireless headphones at once, eliminating the unnecessary tangle of cords while allowing you to watch a movie with your seatmate. You can easily control the volume directly from the device, and it even boasts more than 20 hours of battery life on a single charge. It’s really no wonder that flight attendants love it for longer flights when they’re off duty.
Tessan Power Strip
There’s generally a finite number of outlets available in any given hotel room, so one flight attendant on TikTok recommended this compact power strip as a simple solution to ensure that every device has access to a charge. They shared that they love being able to “plug everything in in one spot” so they don’t have to “worry about finding plugs all over the room.” And with three outlets and three USB ports, everything from your laptop to your e-reader can stay fully charged at all times. Plus, the extension cord provides easy access to hard-to-reach plugs.
J Pillow Travel Pillow
Nothing makes sleeping on a flight more difficult than your head continuously lolling around, which is why flight attendants point to the thoughtfully designed J-Pillow as their favorite hack for restful sleep. This pillow gets tucked around the back of your neck much like a traditional travel pillow, while under-chin support adds another layer of comfort and security for longer trips. It keeps your head, neck, and chin well-cushioned so you won’t awaken with discomfort or stiffness once you touch down. Plus, it comes with a convenient case that can be snapped onto your luggage or tucked into your carry-on bag.
Ergonomic Innovations Donut Pillow
Sitting for long hours during an international flight is never going to be truly comfortable, but one flight attendant promises that this memory foam donut pillow is the best way to upgrade your experience without splurging on a first class ticket. This best-selling cushion is designed to alleviate pressure from your tailbone and back, resulting in a significantly more pleasant travel day. The donut shape evenly distributes body weight, leading to less need for adjustment throughout your flight, and it’s so lightweight that you’ll hardly notice it in your carry-on. You may not be able to use it during take off, but when you’re high in the sky, this pillow will make even the firmest airplane seats feel cushy.
Gasince Handheld Mini Fan
No matter what time of year it is, you should always be prepared for the possibility that your airplane cabin is much warmer than you’d prefer. Because of this, flight attendants suggest always packing a small handheld fan for your travels — in particular, this rechargeable option that’s fitted with a stable base that sits right on your tray table. The portable device boasts up to 13 hours of running time on a single charge so you can even use it overnight in toasty hotel rooms. Plus, you can choose from three speeds to keep you comfortable on the go.
Love a great deal? Sign up for our T+L Recommends newsletter and we’ll send you our favorite travel products each week.
Shop More T+L-Approved Picks
:max_bytes(150000):strip_icc():format(webp)/Im-Picky-About-TK-Im-a-Snob-about-TK-Here-Are-the-TK-Comfy-Shoes-I-Swear-By-tout-64144b437f664ef991dd5636392a7568.jpg)
Related Articles

IMAGES
VIDEO
COMMENTS
Answer From John M. Wilkinson, M.D. Leg and foot swelling during air travel is common. It's usually harmless. The most likely reason for it is sitting for a long time without moving during a flight. Sitting with the feet on the floor for a long time causes blood to pool in the leg veins. The position of the legs while seated also increases ...
Summary. It is very common for a person's ankles to swell during or after flying. This is often due to a buildup of fluid known as edema. Swollen ankles due to edema are often harmless and the ...
4. Stretch Your Legs on Long Flights. If possible, get up to walk the aisle every hour or so, especially on flights over two hours, recommends Dr. Ford. Standing or walking to the bathroom can get ...
Remove your shoes when it's safe to do so, ... Evidence suggests that long-distance air travel post-surgery (e.g., hip and knee replacements) can increase the risk of leg blood clots. ... According to a recent publication from the Mayo Clinic, swelling caused by inactivity during travel (e.g. on planes or long car rides) is usually harmless.
If you feel the onset of swelling coming, get up and go for a walk. Even in the flight cabin when there's limited space, just going for a short walk to the bathroom or down the aisle and back will help. Walking helps to bring back proper blood circulation, which stops the swelling from getting worse. #3. Do Cardio.
In-flight actions. While preparation is important, making smart choices in-flight also helps mitigate swelling. Move your body. Resist the urge to stay in your seat for the duration of your flight. While it may be easy to get lost in movies, books or a deep sleep, your feet and ankles will feel much better if you walk the aisle a few times once ...
Air travel is generally safe for heart patients, with appropriate precautions. If you have heart disease, you can fly safely as a passenger on an airplane, but you need to be aware of your risks and take necessary precautions. Heart conditions that can lead to health emergencies when flying include coronary artery disease (CAD), cardiac ...
Patients with unstable angina, new cardiac or pulmonary symptoms, or recent changes in medications without appropriate follow-up should not fly until stable. 11. C. Consensus/expert opinion ...
Air travel is known as the safest way of transportation. ... and high reactivity could lead to hypoxia-related diseases such as high-altitude pulmonary edema. ... Lendeckel F, Grimminger F, Seeger W, et al. Air travel can be safe and well tolerated in patients with clinically stable pulmonary hypertension. Pulm Circ. 2011; 1:239-43. doi: 10. ...
The most common cause of bilateral leg oedema (swelling in both legs) is when the body has trouble sending blood from veins back to the heart. This is usually due to severe varicose veins - the ...
Not withstanding these numerous causes, the exacerbation of leg edema during travel can be controlled and limited. Thankfully, there are many tips to avoid the swelling and complications that result from air travel: You can sit in an aisle seat; it can help to stretch out your legs. The emergency row, although it comes with more responsibility ...
Lymphedema and Travel. If you have had any surgical procedure that has affected your lymph nodes, travel-related activities may be of concern. During travel, there can be many physical stresses that can affect a body part that is at risk for developing lymphedema. The demand on the lymph system may cause extra swelling for long periods, perhaps ...
Bringing oxygen along. Patients with severe pulmonary hypertension may need portable oxygen because they have a weakened heart that has trouble delivering oxygen to the rest of the body. Their ...
Air travel was as safe as ground travel if the chest tubes were removed after the absence of ongoing air leak and an output <300 ml over 24 hours combined with adequate pain medication and an ...
Sitting immobile on long plane flights or car, train or bus rides can slightly increase a normal person's risk of blood clots in the legs, but associated medical issues usually contribute to it. If someone has peripheral artery disease (PAD) or a history of heart failure, the clot risk increases. Recent surgery, older age and catheters in a ...
According to an airline travel guide prepared by the National Lymphedema Network, this happens because "changes in fluid production in the tissues occur when the external pressures exerted on the ...
The term is often used interchangeably with peripheral artery disease - or PAD - and can include the narrowing of the blood vessels that deliver blood to your legs and arms. The disease ...
The British Thoracic Society guidelines recommend against airline travel during the first four weeks following pulmonary embolism (3). On the other hand, in the IATA medical guidelines published in 2018 it is suggested that patients can fly 5 days after an acute pulmonary embolism episode, if they receive anticoagulation and their PaO2 is ...
Air travel has allowed people to journey long distances and stay connected to loved ones in far away places. Individuals that have sustained a brain injury may wonder when they can fly again and what safety precautions to consider before flying. ... if you're currently experiencing swelling, headaches or any other issues, it is highly ...
Wearing compression garments during air travel reduces lymphedema swelling risk by "First, resorption of fluid at the capillary level is enhanced due to the compression. Seconds, the garment or bandages stimulate the lymphatic system, via the muscle pump, and uptake of extracellular fluid increases, helping to prevent exacerbation of ...
The total incidence of pulmonary embolism reached 4.77 cases per million passengers for distances greater than 10,000 km (6200 mi). Figure 1. Incidence of Pulmonary Embolism According to Distance ...
Flight attendants are taking to TikTok to share their favorite travel essentials, and they're all available at Amazon this spring. Shop comfy neck pillows, loafers with arch support, air ...