

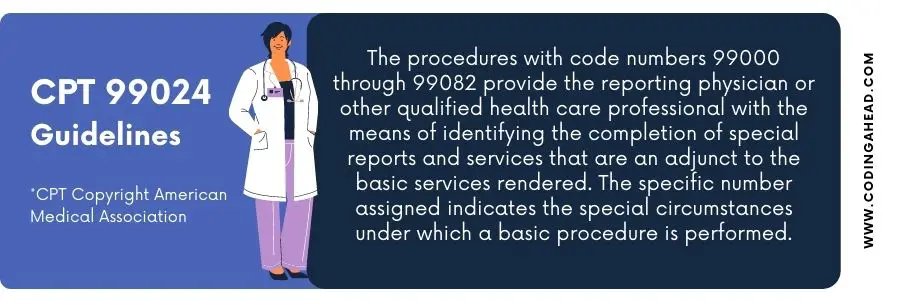
99024 CPT Code (2023) | Description, Guidelines, Reimbursement, Modifiers & Examples
The current procedural terminology (CPT) describes the postoperative follow-up visit with the 99024 CPT code.
Description Of The 99024 CPT Code
CPT code 99024 usually comprises the surgical package to designate that the provider did perform an evaluation and management service during a postoperative period for reasons related to the original procedure.
Official description CPT code 99024: “Postoperative follow-up visit, normally included in the surgical package, to indicate that an evaluation and management service was performed during a postoperative period for a reason(s) related to the original procedure . “
The provider performs an E/M examination during the global surgical period for surgery; the patient already had gone through it before.
The global surgical package, also called global surgery, includes all the compulsory services generally supplied by a surgeon before, during, and after a procedure.
Medicare payment for a surgical procedure consists of preoperative and intra-operative.
The provider typically performs the postoperative services or associates of the same group with the same specialty.
Billing Guidelines
While submitting the postoperative follow-up visit, first understand the usage of the 99024 CPT Code.
It is a Medicare bundled code with zero relative value units (RVUs). And it has no fee on the Medicare Physician Fee Schedule (MPFS); CMS is interested in collecting this information.
Medicare may reimburse bundled code, but not when the provider has performed the service.
Because government insurance pays for the service in advance, it is suitably interested in whether the provider performs it.
Thorough postoperative care minimizes the risk of surgery problems, including pain, helps manage the side effects of the procedure, and supports recovery.
There are some general guidelines for postoperative period billing.
The same provider executes a distinct procedure or evaluation and management service during a postoperative period.
The coder or biller may use two modifiers to simplify billing for visits and other methods in the postoperative period of a surgical procedure but not included in the payment for the surgical procedure.
Modifier 79 narrates the process (unrelated) or service by the same physician during a postoperative time.
The health professional may need to indicate that a function or service furnished during a postoperative period was unrelated to the original procedure.
A new postoperative period begins when someone bills the irrelevant method. Modifier 24 is represented as (unrelated evaluation and management service by the same physician during a postoperative period).
The physician may need to indicate that he provides the assessment and management service during an unrelated procedure’s postoperative period.
An E/M service billed with modifier 24 medical notes must support that the service is irrelevant to the postoperative care of the technique.
The CPT 99024 , when performing an evaluation and management service during a global period , is related to the procedure for which the patient is in the worldwide period. It applies to services with 10–and 90–day global periods.
Some have viewed the reporting of this code as optional because it is not associated with any payment.
Knowing those who practice (in Florida, Kentucky, Louisiana, Nevada, New Jersey, North Dakota, Ohio, Oregon, and Rhode Island) is essential.
When it is appropriate, the Centers for Medicare and Medicaid Services (CMS) require CPT 99024 in those states.
While submitting the postoperative follow-up visit (CPT 99024), one must report these visits through the normal process for filing a claim.
The coder or biller should submit provider, patient, and date-of-service information for claim submission.
The postoperative visit (CPT 99024) does not need to link the related 10–day or 90–day global code, and it is not essential to add any modifiers.
The provider should follow standard Medicare billing requirements to determine that he provided the visits and correctly used the code.
Notably, the Centers for Medicare & Medicaid Services (CMS) may use the collected data to revalue surgery CPT codes.
Therefore, providing complete and precise information about postoperative visits is critical.
Correct usage of postoperative follow-up CPT 99024 is also applied in teaching hospitals and to services provided by residents. Moreover, the provider must be present during postoperative follow-up visits in the primary or critical portions of the service.
The reporting requirement dictates using the 99024 CPT code for all postoperative visits in the global package, not just office visits .
CMS states it in its Global Surgery Data Collection Requirement. Reporting the 99024 CPT code for all postoperative follow-up visits is mandatory.
But it must be during the global period, regardless of the postoperative care setting.
The CPT code 99024 for postoperative care will help ensure surgeons are reimbursed sufficiently for all their work.
And help postoperative physician visits achieve better health results for patients
Billing Examples
The following are examples of when the 99024 CPT code can be used.
A 44 – year old patient was seen in the provider’s office five days ago with a 2.5 – cm laceration to the right anterior side of the wrist. An intermediate layered closure was performed ( CPT code 12031 ).
The same patient now presents with redness, swelling, and drainage to the sutured area. The final diagnosis was infected laceration.
The coder correctly gives the following CPT code, in this case, 99024 CPT code Postoperative Follow-Up Visit, Included Surgical Package, E&M Performed.
The modifier is not acceptable because all services go under the code assigned.
In the second example, a 56 – year old male patient was seen in the provider’s office 30 days ago for permanent sterilization or contraception ( CPT 55250 ).
The same patient again visits the provider’s office to confirm the complete sterilization in the semen test. There is no reason for the visit to sterilize (ICD – 10 CM code Z30.2).
After reviewing the previous surgical data and current medical notes, the coder suggests CPT code 99024 as a postoperative follow-up visit and diagnosis code Z30.2.
Similar Posts
How to use cpt code 67880.
CPT code 67880 describes a procedure known as construction of intermarginal adhesions, median tarsorrhaphy, or canthorrhaphy. This article will cover the description, official description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information and billing examples. 1. What is CPT Code 67880? CPT 67880 is a code used to describe a surgical procedure…
How To Use CPT Code 45386
CPT 45386 describes the procedure of colonoscopy with transendoscopic balloon dilation. This article will cover the official description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information and billing examples. 1. What is CPT Code 45386? CPT 45386 is used to describe a specific procedure called colonoscopy with transendoscopic balloon dilation. This procedure…
How To Use cpt 11313
cpt 11313 describes the shaving of epidermal or dermal lesions that are single lesions with a diameter over 2.0 cm. This article will cover the description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information, and examples of cpt 11313. 1. What is cpt 11313? cpt 11313 is a code used to describe…
How To Use CPT Code 27520
CPT 27520 describes the closed treatment of a patellar fracture without manipulation. This article will cover the description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information and billing examples. 1. What is CPT Code 27520? CPT 27520 can be used to describe the closed treatment of a patellar fracture without manipulation. This…
How To Use CPT Code 99195
CPT 99195 is a therapeutic phlebotomy procedure used to remove venous blood from a patient to reduce the number of red blood cells or treat high levels of iron or potassium in the blood. This article will cover the description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information, similar codes, and examples…
How To Use CPT Code 77401
CPT 77401 describes the technical component of a procedure in which radiation treatment is delivered using superficial and/or ortho voltage, per day. This article will cover the description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information, similar codes and billing examples. 1. What is CPT Code 77401? CPT 77401 can be used…
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
The Importance of CPT® 99024

CPT 99024 — Postoperative follow-up visit, normally included in the surgical package, to indicate that an evaluation and management service was performed during a postoperative period for a reason(s) related to the original procedure.
Procedure Values
When the value of any procedure is determined, the number of global postoperative encounters that typically follow that procedure is taken into consideration. For example, the value of CPT 10140 (Incision and drainage of hematoma, seroma or fluid collection) was determined considering one postoperative visit within the 10-day global period is typically performed. Generally speaking, when more postoperative encounters typically follow a procedure, a higher procedure value is calculated.
What Determines “Typical”?
The Relative Value Update Committee (RUC), with professional society representation, provides input regarding what is typical. Determining how many postoperative encounters typically follow a procedure is also based upon the frequency of CPT 99024 submission following a procedure.
The Problem
There are providers who are not submitting CPT 99024 when they should be. In the 2019 Medicare Part B Physician Fee Schedule Proposed Rule, the Centers for Medicare and Medicaid Services (CMS) published its concern that postoperative global visits are occurring so infrequently that CMS may lower the values associated with procedures that carry a postoperative global period. In their mindset, if the global visit isn’t occurring, it should not be included in the value of the procedure. This can lead to the value of our procedures being reduced.
What Can We Do?
The most important thing that we can do right now is to submit CPT 99024 every time a qualifying postoperative global encounter is performed. Even though this code does not carry any value, the analysis described above shows that CMS uses CPT 99024 submission rates to make important decisions. A low volume of submission has led CMS to believe that these services are not being provided, and that can have a negative impact on the value of procedures we perform.
Dr. Lehrman operates Lehrman Consulting, LLC, is a consultant to the APMA Health Policy and Practice Department, serves as an expert panelist on Codingline , and is a Certified Professional Coder. Follow him on Twitter @DrLehrman .
References:
- Department of Health and Human Services Centers for Medicare & Medicaid Services 42 CFR Parts 405, 410, 411, 414, 415, and 495 [CMS-1693-P] RIN 0938-AT31 Medicare Program; Revisions to Payment Policies under the Physician Fee Schedule and Other Revisions to Part B for CY 2019; Medicare Shared Savings Program Requirements; Quality Payment Program; and Medicaid Promoting Interoperability Program
- 2022 CPT Professional. Current Procedural Terminology (CPT®) is copyright 1966, 1970, 1973, 1977, 1981, 1983-2021 by the American Medical Association. All rights reserved. CPT is a registered trademark of the American Medical Association (AMA).
Related posts:

Jeffrey D. Lehrman, DPM, FASPS, MAPWCA, CPC, CPMA
Subscribe to the intellicure blog.
You May Also Like …

What Doctors Wish Patients Knew About Prior Authorization
May 21, 2024
Maybe if I’d let patients read this article, I could have discussed the issue with my patients honestly, rather than just running away from it.

Pneumatic Compression Devices Are in the Spotlight for 2024 Audits
May 13, 2024
Check out the article by Knicole Emanuel in Today’s Wound Clinic: Pneumatic Compression Devices Are in the Spotlight for 2024 Audits.

CMS Explains its 2024 Value-Based Care Strategy
May 9, 2024
CMS ALWAYS tell us what they are going to do before they do it. Then they do it, and we are surprised.
- Health Policy
Global Surgery Data Collection and Reporting for Postoperative Care
In 2017, the Centers for Medicare and Medicaid Services (CMS) finalized a policy, required by the Medicare Access and CHIP Reauthorization Act (MACRA), in which some physicians that provide 10- and 90-day global services would be required to report information on the number of postoperative visits they provide.
Who is required to report postoperative care information?
Practitioners in 9 states, Florida, Kentucky, Louisiana, Nevada, New Jersey, North Dakota, Ohio, Oregon and Rhode Island , are required to report data on every postoperative visits furnished during the global period of specified procedures.
While this policy only affects practitioners in the above listed states who belong to groups of 10 practitioners or more. ASPS encourages all surgeons to report each postoperative visit to CMS.
What will need to be reported? And how will it be reported?
Practitioners who meet requirements and perform any of the surgical CPT codes that have been identified will report postoperative visits using CPT code 99024 , (postoperative follow-up visit, normally included in the surgical package, to indicate that an evaluation and management service was performed during a postoperative period for a reason(s) related to the original procedure) for each postoperative evaluation and management visit they provide within the global period. This includes every facility visit (inpatient, outpatient, observation) as well as office visits.
The specified procedures have been identified as those that are furnished by more than 100 practitioners and are either nationally furnished more than 10,000 times annually or have more than $10 million in annual allowed charges. Please see below for a complete list of procedures that must follow the new guidelines.
Why is it important to participate?
This is a mandatory policy for some surgeons. Currently there is no penalty for not participating, however, there is the possibility of future payments being withheld if data is not routinely shared. It is important to report because incomplete reporting means incomplete and inaccurate data and can result in reduced global codes and values.
How will Plastic Surgeons be affected?
Plastic Surgeons who bill the following codes may be impacted:
*For a complete list of all surgical CPT codes that require reporting of postoperative visits, please click here .
- Centers for Medicare & Medicaid Services: www.cms.gov
- Contact CMS: [email protected]
- Contact ASPS: (847) 228-9900 or [email protected]
More Resources
- Are You Ready to Report 99024 for Global Post-Op Visits?
- Frequently Asked Questions

- Become a Member
- Renew Membership
- Medical Staffs
- Resolutions
- Nominations
- Practice Management Tools
- Reimbursement Assistance
- Legal Resources
- Confidential Line
- Practice Transformation
- Health Law Library
- Continuing Medical Education
- On-Demand Webinars
- Policy Library
- Membership Dashboard
- Member Benefits
- Organizational Structure
- Discussion Forums
- Legislative Hot List
Coding Corner: The global period – post-op pain management and more
CPR’s “Coding Corner” focuses on coding, compliance, and documentation issues relating specifically to physician billing. This month’s tip comes from G. John Verhovshek, the managing editor for AAPC, a training and credentialing association for the business side of health care.
Question: We are an orthopedic practice with a pain management/anesthesiologist as part of our group. Our orthopedist performs the surgical procedure, and the practice then schedules follow-up pain management with the anesthesiologist. We have received denials from payors citing that the anesthesiologist/pain management visit is included as part of the global surgical procedure. Can you explain the components of the global period and provide clarity on what is included in it?
Answer: The global period, or global surgical package, is a reimbursement convention that bundles all care typically related to surgical service into a single payment.
CPT® defines the surgical package as including the operative procedure itself, as well as:
- Local infiltration, metacarpal/metatarsal/digital block, or topical anesthesia
- Subsequent to the decision for surgery, one related evaluation and management encounter on the date immediately prior to or on the date of the procedure (including history and physical)
- Immediate postoperative care, including dictating operative notes and talking with the family and other physicians
- Writing orders
- Evaluating the patient in the post-anesthesia recovery area
- Typical postoperative follow up care
The Centers for Medicare & Medicaid Services (CMS), which devises Medicare rules, defines the global period to include:
- Preoperative visits after the decision is made to operate. For major procedures, this includes preoperative visits the day before the day of surgery. For minor procedures, this includes preoperative visits the day of surgery
- Intraoperative services that are normally a usual and necessary part of a surgical procedure
- All additional medical or surgical services required of the surgeon during the postoperative period of the surgery because of complications, which do not require additional trips to the operating room
- Follow-up visits during the postoperative period of the surgery that are related to recovery from the surgery
- Post-surgical pain management by the surgeon
- Supplies, except for those identified as exclusions
- Miscellaneous services, such as dressing changes; local incision care; removal of operative pack; removal of cutaneous sutures, staples, lines, wires, tubes, drains, casts, and splints; insertion, irrigation, and removal of urinary catheters; routine peripheral intravenous lines; nasogastric and rectal tubes; and changes and removal of tracheostomy tubes
The following services are never bundled, per CMS, and may be billed separately during the global period:
- Initial consultation or evaluation of the problem by the surgeon to determine the need for major surgeries. This is billed separately using the modifier “-57” (Decision for surgery). This visit may be billed separately only for major surgical procedures.
- Services of other physicians related to the surgery, except where the surgeon and the other physician(s) agree on the transfer of care. This agreement may be in the form of a letter or an annotation in the discharge summary, hospital record or ambulatory surgical center record.
- Visits unrelated to the diagnosis for which the surgical procedure is performed, unless the visits occur due to complications of the surgery
- Treatment for the underlying condition or an added course of treatment, which is not part of normal recovery from surgery
- Diagnostic tests and procedures, including diagnostic radiological procedures
- Clearly distinct surgical procedures that occur during the postoperative period, which are not re-operations or treatment for complications
- Treatment for postoperative complications requiring a return trip to the operating room (OR). An OR, for this purpose, is defined as a place of service specifically equipped and staffed for the sole purpose of performing procedures. The term includes a cardiac catheterization suite, a laser suite and an endoscopy suite. It does not include a patient’s room, a minor treatment room, a recovery room or an intensive care unit (unless the patient’s condition was so critical there would be insufficient time for transportation to an OR).
- If a less extensive procedure fails, and a more extensive procedure is required, the second procedure is payable separately.
- Immunosuppressive therapy for organ transplants
- Critical care services (CPT® codes 99291 and 99292) unrelated to the surgery where a seriously injured or burned patient is critically ill and requires constant attendance of the physician
Count the days
When a global package begins and ends depends on the type of procedure or service being reported.
- A “minor” procedure is assigned a 0- or 10-day global period. A 0-day global means there is no preoperative period and no postoperative days. That is, the global package applies for one day only (the day of the procedure or service).
- A 10-day global has no preoperative period and a 10-day postoperative period. This means the global package applies for 11 days (the day of the procedure or service and for 10 days following).
- “Major” procedures have a 90-day global period. They are more resource-intensive than minor procedures and require a longer patient recovery. The global package for a major procedure begins one day before the procedure and includes the day of service and 90 days thereafter (total 92 days).
Global periods for all CPT® codes may be found using AAPC coder or other encoder software, or in the CMS Physician Fee Schedule Relative Value File. In addition to “000,” “010,” and “090” day global periods, you may also see indicators “XXX” (global period does not apply), “ZZZ” (add-on code), “YYY” (global period determined by payer) and “MMM” (maternity).
Separate services
Note that when reporting separately any service or procedure during the global period, as allowable per the CMS rules described, above, you may have to apply specific modifiers. Examples include modifier 57 Decision for surgery , modifier 58 Staged or related procedure or service by the same physician or other qualified healthcare professional during the postoperative period , or any of several others. To learn more about these modifiers and when to apply them, see “ Your Quick Guide to the Global Surgical Package .”
Finally, note that CMS defines “post-surgical pain management by the surgeon” as part of the global package. But some providers may prefer that this care be provided by another provider. For example, in the question above, an anesthesiologist is brought into the practice to provide postoperative pain management. Because this care is part of the global package, however, the anesthesiologist cannot bill separately for these services. In other cases, a provider may contract postoperative care work to a different provider. For example, an orthopedic surgeon may pay an anesthesiologist “per patient” to manage post-operative pain.

Download the new CMADocs app!
CMA's new mobile app lets you connect with your colleagues and engage with CMA content! Download the "CMADocs" app today from the Apple or Google Play app stores for daily news updates, events calendar, resource library and more.
Latest News
Trivia Tuesday Week 1: And the winner is...
May 24, 2024
Congratulations to John Maher, M.D., this week’s winner of CMA's Trivia Tuesday challenge, successfully answering the w...
CMA urges Blue Shield to rescind recently announced modifier 25 policy
CMA said the new modifier 25 payment cuts are duplicative and unjustified, urging the payor to rescind the recently ann...
Medi-Cal assigns reimbursement rates to 12 hernia repair service codes
May 23, 2024
The California Department of Health Care Services recently announced it has updated the reimbursement rates for ventral...
House committee passes extension of federal telehealth flexibilities
On May 8, 2024, the U.S. House of Representatives Committee on Ways and Means unanimously passed legislation that would...
In historic action, CA Democratic and Republican parties urge voters to support Protect Access to Care Initiative
May 22, 2024
In a demonstration of broad, bipartisan support, both the California Democratic Party and the California Republican Par...
Join PHC's Health Equity Leadership Summit to gain valuable insights on the role of chief health equity officers
Physicians for a Healthy California is excited to announce that Reggie Tucker-Seeley Sc.D., Sc.M., Principal of Health ...
Trivia Tuesday: Test your CMA knowledge for a chance to win a Starbucks gift card!
May 17, 2024
Get ready to test your knowledge and compete with CMA members for a chance to win CMA’s new weekly Trivia Tuesday chall...
DWC to address ongoing e-filer errors
May 15, 2024
The Division of Workers’ Compensation (DWC) has announced plans to reduce e-filing practices that result in repeated ...
Governor's health care funding cuts highlight urgency of Protect Access to Healthcare ballot initiative
May 14, 2024
In his May Revision to the budget, the Governor proposes to maintain the provider rates that became effective on
CMA marks Mental Health Awareness Month with call to pass AB 2164
During Mental Health Awareness Month, the California Medical Association (CMA) is urging legislators to pass Assembly B...
Big legal victory! Health plans drop challenge to retroactive enforcement of law requiring payment for COVID-19 services
After losing at the trial court level, the California Association of Health Plans (CAHP) has dropped its appeal in a la...
Present and future CMA leaders invited to leadership development session on June 18
May 13, 2024
CMA members are invited to a virtual leadership development session hosted by past CMA president Ted Mazer, M.D. on Jun...
Save the Date: Join the 36th Annual Virtual Conference on Physicians’ Well-Being on July 19
May 10, 2024
The Riverside County Medical Association is presenting the 36 th Annual Virtual Conference on Physicians’ Well-Being, ...
Nominations open for 2024-25 CMA councils and committees
May 09, 2024
CMA is seeking recommendations for physicians who are interested in and willing to serve on its standing
Blue Shield to significantly cut reimbursement of E/M services billed with modifier 25 and will no longer pay consult codes
May 08, 2024
Effective July 14, 2024, Blue Shield will no longer reimburse for face-to-face consultation services. Additionally, the...
Medicare trustees warn of access threat, CMA urges H.R. 2474 passage
A report released by the Medicare trustees on Monday warned that the failure of Medicare to provide physician payments ...
HHS finalizes rule expanding access to care for Dreamers
May 06, 2024
The U.S. Department of Health and Human Services finalized a rule on Friday to expand Affordable Care Act eligibility t...
CMA to co-host webinar on joining the California Data Exchange Framework
May 02, 2024
CMA is co-hosting a free webinar with Bamboo Health and Manifest Medex on May 22, 2024, for practices who want to learn...
CalHealthCares loan repayment program earns praise at congressional hearing for addressing provider shortages in underserved areas
In testimony to congress, Dr. Galvez emphasized the critical role of programs like CalHealthCares
Support PHC on Big Day of Giving, May 2
May 01, 2024
On the Big Day of Giving (Thursday, May 2), please join us in uplifting PHC’s work and service by donating to support e...
AI in health care webinar now available for free download
Recently, CMA hosted a webinar with Joshua Tamayo-Sarver, M.D., Ph.D., Vice President of Innovation for Vituity, on art...
Physician practices still struggling with fallout from Change cyberattacks, latest AMA survey finds
Physician practices are still in crisis and continue to experience issues with multiple operations due to the Change He...
LAST CALL: Registration for the CMA HIT Summit closes TOMORROW
April 30, 2024
If you plan to join us next week in San Francisco for the 2024 CMA HIT Summit— "Health IT in the Safety Net"— registrat...
Medi-Cal Rx implements utilization management criteria for Code 1 diagnosis restricted drugs
Effective April 30, 2024, DHCS has turned on claim utilization management edits for Reject Code 80 – Diagnosis Code D...
New health care worker minimum wage takes effect June 1; IPAs and small physician practices exempt
On June 1, 2024, a new state law takes effect that phases in minimum wage increases for health care workers.

Office of Health Care Affordability sets spending growth target
After months of discussion, the OHCA board approved a statewide health care spending target starting at 3.5% for 2025 a...
CMS signals additional prior auth reforms for Medicare Advantage, prescription drugs
April 26, 2024
CMS recently suggested that the agency may implement additional prior authorization reforms in the Medicare Advantage p...
Voter signatures submitted to qualify CMA’s initiative for the November ballot
April 25, 2024
The California Medical Association and the Coalition to Protect Access to Care, a broad and diverse group of health car...
FTC votes to ban noncompete agreements for most employees
April 24, 2024
The FTC this week finalized a rule to ban noncompete clauses, which are particularly harmful for underserved communit...
64,000 Medi-Cal patients affected by expiration of Partnership HealthPlan’s contract with Dignity Health
April 23, 2024
CMA recently learned that Partnership HealthPlan of California’s contract with Dignity Health expired as of March 31, 2...
Saturday, April 27, is Drug Take Back Day
April 22, 2024
Saturday, April 27, 2024, is National Prescription Drug Take Back Day, when hundreds of locations throughout California...
PHC study reveals critical need to support women physicians of color
PHC has published a new study that presents crucial insights into the factors contributing to burnout and attrition amo...
New survey about ongoing impacts of Change Healthcare cyberattack: Respond by Wednesday, April 24
April 19, 2024
AMA is asking physician practices to take a follow-up survey to assess the current level of service disruption and fina...
CMA's 50th Legislative Advocacy Day: A success for physician advocacy
April 18, 2024
CMA recently celebrated a milestone with its 50th Legislative Advocacy Day, held on April 10, 2024, in Sacramento.
#CMAVoices: Share your story about prior authorization
April 17, 2024
CMA urges physicians to continue to share stories about the harms of prior authorization delays.
Last chance: PSLF income-driven repayment account adjustment deadline is April 30
The U.S. Department of Education extended the deadline for borrowers to consolidate commercial FFEL or Perkins loans in...
Tell your legislators to support AB 2164 to reduce stigma for physicians who seek mental health care
Contact your legislator TODAY and consider sharing your personal experiences or stories about the importance of seeking...
Just Added: Oracle Health’s Michelle Flemmings joins CMA HIT Summit to share industry insights on the future of AI in health care
April 16, 2024
The California Medical Association (CMA) and HealthTech 4 Medicaid (HT4M) are excited
Free CME: Webinar to look at AI and its implications on autonomy, cyber security and patient care
April 15, 2024
CMA is hosting a free CME webinar that will look at the evolving landscape of AI within health care.
DWC implements update to workers' compensation physician fee schedule
The California California Division of Workers’ Compensation recently published a notice that updates the Official Med...
Reminder: Temporary funding support available to physician practices affected by Change Healthcare cyberattack
On Feb. 21, 2024, Change Healthcare, a subsidiary of the UnitedHealth Group Optum unit, experienced a cyber-attack caus...
New mailing addresses for Blue Shield of California Promise Claims and Disputes
On April 1, 2024, Blue Shield of California Promise Health Plan announced that new mailing addresses are now in effect ...
AMA survey finds cyberattack continues to threaten the viability of physician practices
April 12, 2024
AMA has released informal survey findings showing the ongoing, devastating impact of the Change Healthcare cyberattac...
New updates to CMA’s California Physician’s Legal Handbook
An invaluable resource unlike any other, the California Physician’s Legal Handbook (CPLH) is designed to equip health c...
PHC now accepting nominations for the 2024 Health Equity Leadership Awards
Physicians for a Healthy California is now accepting nominations for its annual Health Equity Leadership Awards, which ...
Save the Date: 2nd Annual Health Equity Leadership Summit will be July 11-12 in Sacramento
The second annual Physicians for a Healthy California Health Equity Leadership Summit will take place July 11-12, 2024,...
CMA’s 2nd Annual HIT Summit featured on PopHealth Podcast
HealthTech 4 Medicaid (HT4M) founder and executive director Adimika Arthur, MPH, recently appeared on the PopHealth Po...
Protecting your cyber security: Tips from the experts
The health care sector faces significant cybersecurity risks, exemplified by incidents like the Change Healthcare cyber...
- Newsletters
- FAC Articles
Need a Good Acronym and Abbreviation Reference?

Find-A-Code Articles, Published 2023, September 12
Documenting and reporting postoperative visits.
by Aimee L. Wilcox, CPMA, CCS-P, CST, MA, MT Sep 12th, 2023
CPT® 99024 was introduced by the American Medical Association (AMA) with an effective reporting date of January 1, 2013. The associated code description is as follows:, 
“Postoperative follow-up visit, normally included in the surgical package, to indicate that an evaluation and management service was performed during a postoperative period for a reason(s) related to the original procedure”
To fully understand this code description, one must also understand the definition of the global surgical package, which CPT® describes as:
Of note, Medicare published their own definition of the global surgical package (see Chapter 12, Section 40.1 of the Medicare Claims Processing Manual-Pub. 100–04), which differs from the CPT® surgical package. The surgical package policy applied to an individual claim is determined by the patient’s insurance company’s published policies.Payers without published policies must adhere to the CPT® guidelines.
Prior to 2017, pre/postoperative services with a zero-dollar charge, were not submitted on claims. Because of this, a proper analysis of the quality and quantity of services that make up a global surgical package was not possible, as there was a deficit in the data that showed postoperative services. In 2015, Medicare proposed a change in the global surgical package to return all surgical procedures to a zero-day global period to promote a more accurate valuation of surgical services through coding data. However, Section 523(a) of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) (Pub. L. 114–10, enacted April 16, 2015) added section 1848(c)(8)(A) of the Act, prohibited the Secretary from implementing this change.
Instead, on January 1, 2017, Medicare required specific large provider groups, identified by them, to report via claim, all preoperative and postoperative services provided during the global surgical period. Although the requirement was only specific to certain large provider groups and not all Medicare providers, all Medicare contracted providers were encouraged to do likewise. This policy was strategic to facilitate a more accurate valuation of more than 4,000 surgical procedures assigned a 0, 10, or 90-day global period.
Each surgical procedure is assigned either a 0, 10, or 90-day global period; however, according to the global surgical package, the day of the procedure is considered bundled into the procedure for 0-day and 10-day global periods, which means technically the 10-day global period is actually an 11-day global period (day of the procedure and the 10 days following the procedure). For 90-day global periods, which are considered to be major surgical procedures, the day prior to the surgery, the day of the surgery, and 90 days following the surgery, are included in the global period, essentially making a 90-day global period actually a 92-day global period.
Preoperative services performed on the day of a 0-day or 10-day surgical procedure are bundled into the procedure itself. As an example, let’s review the following patient scenario:
Scenario: A patient has an appointment to have their nails trimmed in the office. The physician documents a history related to the patient’s chronic conditions and how they impact his ability to trim his own nails, examines the patient’s nails, and determines there are 8 that need to be trimmed. The provider documents the procedure where the nails are trimmed, including the method used, the nails trimmed, and the outcome and any instructions on nail care to the patient.
Code: 11721 - Debridement of nail(s) by any method(s); 6 or more is reported but not anEvaluation and Management (E/M) service code. The reason being, is that this was a scheduled procedure and all of the history and exam were related to why the patient has the condition, needs the service performed, and the actual performance of the service, all of which are considered the preoperative workup included (bundled) into the service itself.
Same Day Surgeries
Currently, there are 1,190 surgical procedures with a zero-day global period, 468 surgical procedures with a 10-day global period, and 3,743 major surgical procedures with a 90-day global period. Code 99024 is used to report postoperative services, beginning with any postoperative care provided on the day of the surgery (after the surgery has been performed) and each visit thereafter, where postoperative care is provided through the end of the assigned global period. For same day surgeries (SDS), that means all care related to admitting the patient, postoperative care up until discharge, and inclusive of the discharge services. The same applies to admission and discharge services, as well as inpatient E/M services provided to a patient in the inpatient hospital setting. Facilities who accurately report all postoperative services with 99024 during the global period would also report 99024 for any admission and discharge services, instead of the usual CPT codes for those services, and all are bundled into the surgical package, unless specific surgical or patient care for other conditions or complications is provided that is beyond what is covered in the surgical package.
However, it should be noted that if the surgeon is billing for Evaluation and Management services, during the global period, that are unrelated to the surgical procedure and global period, and the documentation supports the clear distinction of these services, the provider may report the E/M service with modifier 24 to specify it is a distinct and separately billable service provided during the global period.
Splitting Surgery and Postoperative Care
Occasionally, the surgeon who performs the surgery is not available to perform the preoperative and postoperative care. This can be because pre and postoperative services are provided in a different state than the surgeon resides and the patient has returned home after surgery to get postoperative care by their own physician, or another reason exists. Be sure to check individual payer policies related to splitting the surgical global package components to ensure coverage, medical necessity, documentation requirements, and modifier use for reporting claims.
When the global surgical package is split between providers for Medicare beneficiaries, each provider will report the surgical CPT code and the modifier that applies to the services they are providing and in the narrative box on the claim, will provide the details of the services and service dates they are providing to the patient. Novitas, and other Medicare Administrative Contractors (MACs) have provided published documents to review this process in detail.
Documentation
Clear documentation is very important in ensuring accurate reimbursement for services rendered, whether for the entire global surgical package or when it has to be split between providers. An operative report that clearly describes the pre/postoperative diagnosis, name of the procedure, and the details of how it was performed, is a must have for claims submission and medical necessity. Likewise, each postoperative report should contain language that indicates the patient is presenting for a postoperative visit, including the postoperative date (e.g., POD#7, status post day 7) and the surgical procedure they had done, including the date the procedure was performed. This facilitates proper coding for the global period and an accurate reflection of postoperative care provided to the patient following surgery.
Additionally, be sure to document any postoperative care, such as:
- Patient complaints, symptoms, or complications directly related to the surgical procedure.
- Examination of the patient, especially the body area or organ system impacted by surgery.
- Medications or treatments that have been prescribed, including pain management.
- Follow-up testing or imaging ordered to check the patient’s status after surgery.
- Any conditions, symptoms, or treatments that are unrelated to the surgical procedure that may qualify for appending modifier 25 to the E/M service.
Separately Reportable E/M Service on the Day of a Postoperative Visit by the Same Provider
When a postoperative visit turns into an E/M service for an unrelated condition, the provider may be eligible for payment if the documentation supports a separately, identifiable E/M service as well as the postoperative visit service. Providers often combine these two services in a single report; however, to ensure accurate payment and reduce confusion that may occur during an audit, we recommend either documenting the postoperative care first and in the same note, just separated from it, document a complete E/M service note as well for the unrelated problem. Providers may also choose to simply document two separate reports, one for the postoperative visit and another for the separately identifiable E/M service on the same date. To ensure the E/M service is paid, when the documentation qualifies the service, report modifier 24 (unrelated E/M by the same physician during the postoperative period) with the E/M service code to clarify it is an unrelated service. If supporting documentation is requested by the payer, be sure to send both reports, the postoperative note and the E/M service note for clarity.
Of note, there is no NCCI edit between 99024 and E/M service codes indicating that if both a postoperative visit and an unrelated E/M service are performed on the same day by the same physician/provider, they may be reported on the same claim; however, be sure to append modifier 24 to the E/M service code to instruct the payer that the provider documentation supports unbundling the E/M service from the global period for payment.
References/Resources
About aimee l. wilcox, cpma, ccs-p, cst, ma, mt.

Documenting and Reporting Postoperative Visits. (2023, September 12). Find-A-Code Articles. Retrieved from https://www.findacode.com/articles/documenting-reporting-postoperative-visits-37422.html
Article Tags (click on a tag to see related articles)
Thank you for choosing Find-A-Code, please Sign In to remove ads.

- Introduction
- Conclusions
- Article Information
Data set linkage to determine primary care provider (PCP) utilization shown. HRR indicates hospital referral region; PC, primary care.
Early primary care provider (PCP) follow-up significantly reduced 30-day readmission following open TAA repair if a postoperative complication occurred. In comparison, early PCP follow-up was not associated with a significant difference in readmission rates among patients undergoing ventral hernia repair, whether or not a complication occurred.
Patients determined to be at the highest risk for readmission following open thoracic aortic aneurysm repair achieved the greatest benefit from having their procedure performed in a region with high primary care use.
See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
Brooke BS , Stone DH , Cronenwett JL, et al. Early Primary Care Provider Follow-up and Readmission After High-Risk Surgery. JAMA Surg. 2014;149(8):821–828. doi:10.1001/jamasurg.2014.157
Manage citations:
© 2024
- Permissions
Early Primary Care Provider Follow-up and Readmission After High-Risk Surgery
- 1 Division of Vascular Surgery, Department of Surgery, University of Utah School of Medicine, Salt Lake City
- 2 Section of Vascular Surgery, Dartmouth-Hitchcock Medical Center, Lebanon, New Hampshire
- 3 The Dartmouth Institute for Health Policy and Clinical Practice, Hanover, New Hampshire
Importance Follow-up with a primary care provider (PCP) in addition to the surgical team is routinely recommended to patients discharged after major surgery despite no clear evidence that it improves outcomes.
Objective To test whether PCP follow-up is associated with lower 30-day readmission rates after open thoracic aortic aneurysm (TAA) repair and ventral hernia repair (VHR), surgical procedures known to have a high and low risk of readmission, respectively.
Design, Setting, and Participants In a cohort of Medicare beneficiaries discharged to home after open TAA repair (n = 12 679) and VHR (n = 52 807) between 2003 to 2010, we compared 30-day readmission rates between patients seen and not seen by a PCP within 30 days of discharge and across tertiles of regional primary care use. We stratified our analysis by the presence of complications during the surgical (index) admission.
Main Outcomes and Measures Thirty-day readmission rate.
Results Overall, 2619 patients (20.6%) undergoing open TAA repair and 4927 patients (9.3%) undergoing VHR were readmitted within 30 days after surgery. Complications occurred in 4649 patients (36.6%) undergoing open TAA repair and 4528 patients (8.6%) undergoing VHR during their surgical admission. Early follow-up with a PCP significantly reduced the risk of readmission among open TAA patients who experienced perioperative complications, from 35.0% (without follow-up) to 20.4% (with follow-up) ( P < .001). However, PCP follow-up made no significant difference in patients whose hospital course was uncomplicated (19.4% with follow-up vs 21.9% without follow-up; P = .31). In comparison, early follow-up with a PCP after VHR did not reduce the risk of readmission, regardless of complications. In adjusted regional analyses, undergoing open TAA repair in regions with high compared with low primary care use was associated with an 18% lower likelihood of 30-day readmission (odds ratio, 0.82; 95% CI, 0.71-0.96; P = .02), whereas no significant difference was found among patients after VHR.
Conclusions and Relevance Follow-up with a PCP after high-risk surgery (eg, open TAA repair), especially among patients with complications, is associated with a lower risk of hospital readmission. Patients undergoing lower-risk surgery (eg, VHR) do not receive the same benefit from early PCP follow-up. Identifying high-risk surgical patients who will benefit from PCP integration during care transitions may offer a low-cost solution toward limiting readmissions.
At the time of discharge after high-risk surgery, patients are routinely counseled to follow-up with their primary care provider (PCP) as well as the surgeon who performed their procedure. Aside from representing a tradition in surgical practice, patients and physicians presume that early follow-up with the PCP represents an opportunity to address problems that may emerge during the care transition from inpatient to outpatient settings. Early PCP follow-up after admission for high-risk medical conditions, such as heart failure or pneumonia, has been demonstrated 1 , 2 to lower the risk of hospital readmission, helping to validate this practice.
However, the value added by a PCP visit after surgical discharge has been debated for several reasons. First, PCPs may believe that a visit after surgical discharge is unnecessary because issues arising soon after surgery are likely related to the operation and would be best addressed by the surgical team. Second, elderly patients, often debilitated following major surgery, may not be willing to make additional office visits or will not be adherent to them, especially if the visits seem unlikely to add value. 3 Finally, in a health care environment increasingly focused on efficiency, more than 6.9 million major cardiovascular operations are performed annually, translating into increasing costs associated with scheduling routine PCP follow-up visits. 4
Patients undergoing open thoracic aortic aneurysm (TAA) repair have one of the highest documented readmission rates of any major cardiovascular operation commonly performed among Medicare beneficiaries. 5 Accordingly, these procedures have been selected as a potential target for nonreimbursement for readmissions. Within this high-risk population, we examined whether early PCP follow-up visits in addition to surgical follow-up was associated with lower rates of readmission. We examined this question among individual patients undergoing open TAA repair, as well as across hospital referral regions, for patients with and without complications sustained during their index surgical admission. In addition, a control group consisting of patients undergoing uncomplicated elective ventral hernia repair (VHR) was used to compare the benefit of early PCP follow-up among patients undergoing a common lower-risk surgical procedure.
We used the Centers for Medicare & Medicaid Services Medicare Provider Analysis and Review database to study patients undergoing open TAA repair and open VHR between January 1, 2003, and November 30, 2010. International Classification of Diseases, Ninth Revision procedure codes were used to identify patients who underwent open repair of nonruptured open TAA repair as well as open VHR from the Part A Medicare claims data set. In addition to procedural codes for open TAA repair and VHR, each patient was required to have a diagnosis code for TAA and nonobstructed/nongangrenous ventral hernia.
Because our analysis was focused on readmission, patients who underwent surgery were excluded from analysis if they died during their index admission or if they were discharged home with hospice care. To evaluate outpatient visits, Part B Medicare claims were linked to inpatient denominator files for patients undergoing open TAA repair and VHR from January 1, 2003, to November 30, 2010. Part B claims for evaluation and management services were used to examine outpatient visits with PCPs following discharge from the index hospitalization and were captured using Current Procedural Terminology codes 99201 through 99205, 99211 through 99215, 99241 through 99245, 99301 through 99303, 99311 through 99313, 99321 through 99345, and 99347 through 99350. The final date for 30-day patient follow-up was December 30, 2010. Our study protocol was approved by the Dartmouth Institutional Review Board.
Our main exposure variable was patient evaluation by a PCP within 30 days of hospital discharge after elective open TAA repair and VHR. A PCP was defined as a health care worker who was not a member of the surgical team, which included primary care physicians as well as nurse practitioners and/or physician assistants. The PCP visit needed to occur before the date of any readmission. We included all evaluations by PCPs that were performed in an outpatient clinic setting as well as within the patient’s home.
The primary outcome for the study was 30-day readmission following discharge after surgery. Readmission was defined as a readmission to any hospital within 30 days of discharge from the index hospitalization for the open TAA repair or VHR procedure. Only the first readmission during the first 30 days postoperatively was examined. Transfers to and from another hospital and admissions for rehabilitation were not counted as readmissions.
Prior work 5 , 6 has established that patients who have undergone open TAA repair or VHR and developed complications during their surgical admission are at higher risk for readmission after surgery. Therefore, analysis of our primary outcome was stratified across patients who had and those who had not experienced any major complication during their index hospitalization. Following open TAA repair, major perioperative complications were defined as renal failure, cardiopulmonary failure, major gastrointestinal complication, spinal cord ischemia, and stroke or major cerebrovascular complication. Major perioperative-related complications following VHR were defined as gastrointestinal injury, accidental laceration, or cardiopulmonary failure.
To examine the usefulness of primary care access at population-based levels, regional primary care use measures were identified from the Dartmouth Atlas of Healthcare across the 307 nationwide Hospital Referral Regions (HRRs). 7 Primary care use was defined as the percentage of Medicare beneficiaries in each HRR who had at least one ambulatory visit to a primary care provider per calendar year between 2003 and 2007. Regional primary care use data for all nationwide HRRs were then linked to patient-level data from the Medicare Provider Analysis and Review Part A claims data set using unique Centers for Medicare & Medicaid Services hospital identifiers ( Figure 1 ).
For patient-level PCP visit analyses, a 20% sample of Medicare beneficiaries from the entire open TAA repair cohort was available, whereas a 100% sample of Part B claims was used for VHR and the regional-level analyses ( Figure 1 ). We started by using unadjusted analyses to compare the rates of readmission between patients who were and those who were not seen by a PCP within 30 days following discharge. Crude analyses of patient variables and outcome measures were performed using χ 2 tests for categorical variables, unpaired, 2-tailed t tests for continuous variables that were normally distributed, and Wilcoxon signed-rank tests for nonnormally distributed data. We then conducted stratified analyses to examine the effect of major complications on readmission. Potential interactions (effect modifiers) between variables were explored using both stratification techniques and multivariate analysis. In addition, we conducted a sensitivity analysis to investigate whether readmission rates varied by whether PCP follow-up occurred less than or equal to 14 days or greater than 14 days later.
In our regional analyses, we compared readmission rates across nationwide HRRs. 8 Our numerator for these calculations was the number of patients readmitted after open TAA repair and VHR, and the denominator was the number of patients undergoing each procedure. We divided all regions into terciles of primary care use and compared regional readmission rates across the terciles of primary care use. To examine the effect of individual patient-level covariates within these regional strata, we conducted stratified analyses based on patient-level probabilities of readmission. Readmission probability scores were calculated based on variables associated with readmission probability scores (log [ρ/(1 − ρ)]) and then used to match patients within models. Patients were matched using nearest-neighbor matching techniques, based on having a low, medium, or high probability for readmission.
Risk-adjusted logistic regression models were constructed to estimate the association between patient- and regional-level primary care use with subsequent risk of readmission. These models controlled for baseline patient demographic variables for age (continuous and categorical variables), sex, race, urgency of admission (elective, urgent, or emergent), and comorbidity score using the Charlson comorbidity index. In addition, regression models and stratified analyses were designed to control for whether patients experienced a major postoperative complication. These models accounted for clustering of patient-level outcomes within hospitals and within hospital referral regions.
P < .05 (2-sided) was considered to be significant for all statistical tests and models, and Bonferroni correction was used to control for multiple comparisons. 9 Stata, version 11.0 (StataCorp), statistical software was used for all analyses.
We identified 12 679 patients who underwent open TAA repair and 52 807 patients who underwent VHR between 2003 and 2010 ( Figure 1 ). The characteristics of the patients, stratified by PCP follow-up, are reported in Table 1 . Among the 20% sample of our entire open TAA repair cohort (2437 available for analysis), we found that 1847 patients (75.8%) had PCP follow-up within 30 days after discharge, whereas 5840 (11.1%) patients had early PCP follow-up after VHR. Follow-up occurred a median of 12 days following discharge for open TAA repair and a median of 11 days for VHR. Compared with patients without 30-day follow-up, patients who attended a follow-up visit with a PCP were less likely to have experienced a renal or pulmonary complication after open TAA repair but more likely to have a bowel injury complication after VHR ( Table 1 ).
The characteristics of patients undergoing open TAA repair and VHR, stratified by regional levels of primary care use, are also reported in Table 1 . Patients who underwent either open TAA repair or VHR in regions with low primary care use were significantly older ( P < .05) compared with those in regions with higher use. Patients undergoing open TAA repair in regions with low primary care use had higher rates of renal and pulmonary postoperative complications. In comparison, patients undergoing VHR in regions with low primary care use had shorter lengths of stay and a lower rate of bowel injury complications.
Among patients with Part B claims available for analysis, a total of 538 (22.1%) patients who underwent open TAA repair and 4927 (9.3%) patients who underwent VHR were readmitted within 30 days after surgery. Readmissions occurred a mean (SD) of 11.0 (7.9) days after discharge, and patients spent 6.3 (7.8) days in the hospital once readmitted. Compared with patients who had no early follow-up care, patients who visited a PCP within 30 days were significantly less likely to be readmitted following open TAA repair (19.7% vs 28.0%; P < .001), whereas there was no benefit associated with early PCP follow-up for patients undergoing VHR (9.4% vs 9.3%; P = .77).
For patients undergoing open TAA repair, the presence of a postoperative complication significantly modified the association between PCP follow-up and 30-day readmission ( Figure 2 ). Patients who had experienced any major postoperative complication following open TAA repair received a significantly greater benefit from early PCP follow-up on risk of readmission (20.4% with follow-up vs 35.0% without follow-up; P < .001) compared with patients who experienced an uncomplicated postoperative hospital course (19.4% with follow-up vs 21.9% without follow-up; P = .31). In comparison, the presence of a complication did not significantly change the association between PCP follow-up and readmission for patients undergoing VHR repair ( Figure 2 ). These associations were sustained regardless of PCP follow-up before or after 14 days.
The association between 30-day primary care follow-up and readmission for patients undergoing open TAA repair and VHR were confirmed in risk-adjusted logistic regression models accounting for patient comorbidities and stratified by whether perioperative complications occurred ( Table 2 ). In the open TAA repair models, early PCP follow-up when a complication occurred was associated with a 47% decrease (odds ratio [OR], 0.53; 95% CI, 0.37-0.75; P < .001) in the likelihood of being readmitted within 30 days ( Table 2 ). In comparison, early PCP follow-up did not significantly reduce the risk of readmission among VHR patients with or without perioperative complications ( Table 2 ).
To further explore the association between outpatient primary care follow-up with risk of readmission following open TAA repair and VHR, we assessed the variation in primary care use within 307 nationwide HRRs. A total of 7441 beneficiaries underwent open TAA repair and 29 796 beneficiaries underwent VHR between 2003 and 2007 and had their claims data linked to rates of primary care use at the HRR level for the corresponding years. As displayed in Figure 1 , patients were then stratified into 3 equally sized groups based on regional rates of primary care use, classified as low (range, 60%-74%), medium (range, 75%-80%), and high (range, 81%-90%).
After stratifying patients by regional level of primary care use, we found that open TAA repair undertaken in regions with high primary care use was associated with a significant reduction in 30-day readmission compared with regions with low primary care use (19.6% vs 23.3%; P = .04). Moreover, readmission following open TAA repair was significantly lower in regions with high vs low primary care utilization when a complication occurred (20.6% vs 25.5%; P = .03), but was not significantly lower when patients had an uncomplicated hospital course 19.1% vs 22.0%; P = .12). In comparison, we found no significant difference in readmission rates among patients undergoing open VHR in regions with high vs low primary care use (9.2% vs 9.1; P = .18), regardless of whether a perioperative complication occurred.
The results of the region comparisons were confirmed in logistic regression models that controlled for patient demographics and complications. Adjusted models demonstrated an 18% lower likelihood of readmission (OR, 0.82; 95% CI, 0.71-0.96; P = .02) when open TAA repair was undertaken in regions with high compared with low primary care use, whereas no significant difference in readmission risk was found when VHR was undertaken in regions with high vs low primary care use (OR, 1.0; 95% CI, 0.91-1.10; P = .92). Furthermore, readmission rates following open TAA repair varied across patient strata categorized as being at low, medium, or high risk for readmission using risk scores. Among patients classified as being at low or medium risk for readmission, there was no significant difference between readmission rates following open TAA repair in regions with low vs high primary care use ( Figure 3 ). However, patients estimated to be at high risk for readmission following open TAA repair had a significant reduction in readmission rates (21.5% high vs 32.6% low; P = .02) when procedures were undertaken in regions with high vs low primary care use.
Hospital readmissions for high-risk medical and surgical patients are common, and these events impose a significant economic effect on our health care system. Our study demonstrates that early follow-up with a PCP after high-risk surgery, such as open TAA repair, especially among patients who have a complicated hospital course, is associated with a lower risk of hospital readmission. Furthermore, we show that regional- and patient-level use of primary care services among Medicare beneficiaries is similarly correlated with the risk of 30-day readmission following open TAA repair. In comparison, our data indicate that early PCP follow-up after a lower-risk surgery, such as VHR, does not reduce the risk of readmission. These findings suggest that ensuring access to primary care follow-up for high-risk surgical patients and coordinating outpatient services during transitions of care may be an effective strategy to limit readmissions.
The transition from inpatient to outpatient care is a critical stage for patients hospitalized with a wide range of complex medical and surgical conditions. Transitional care includes many critical processes, such as communication between inpatient and outpatient providers, reconciliation of medications, coordinating outpatient services, and ensuring that patients follow up with appropriate PCPs. 10 Deficits in communication and/or the transfer of information between hospital physicians and outpatient PCPs is estimated to affect the quality of care and outcomes in more than 25% of discharged patients. 11 As such, the Patient Protection and Affordable Care Act of 2010 12 established a variety of transition care programs to improve quality among vulnerable patients. 10 Improving the components of transitional care can significantly reduce readmission rates among patients with high-risk medical conditions. 13 This includes high-risk medical patients randomized to comprehensive hospital discharge programs, which have been shown 14 , 15 to significantly reduce readmissions among those receiving coordinated follow-up appointments and medicine reconciliation. Finally, it was shown 1 that among patients hospitalized for heart failure complications, early follow-up with outpatient PCPs after discharge significantly reduced 30-day readmissions.
In terms of preventing readmission, it remains unknown whether the benefits associated with outpatient follow-up after high-risk medical discharge extend to patients undergoing high-risk surgical procedures. Presuming that these benefits would extend to patients with aortic aneurysm disease has face validity because many clinical characteristics are shared by these patients, including chronic obstructive pulmonary disease, diabetes mellitus, stroke, renal insufficiency, and congestive heart failure. These conditions are common in both high-risk populations, are all independently associated with an increased risk of readmission, and may be exacerbated by surgical stress during the perioperative period. 16 In comparison, patients undergoing lower-risk surgery experience less physiological stress during the perioperative period, which may reduce the likelihood that coexisting medical conditions will be exacerbated during the recovery period. 17
We hypothesize that for patients undergoing high-risk surgery, follow-up with PCPs is a means by which complications or errors in discharge planning can be recognized before they escalate into larger problems. For example, a minor surgical site infection could be diagnosed and treated early with antibiotics, or treatment with a critical medication that was omitted from the discharge instructions could be restarted before the patient experienced an adverse clinical event. As our data show, most primary care follow-up occurred within 2 weeks after hospital discharge, allowing the opportunity for PCPs to implement these types of prophylactic measures in a clinic setting and avoid a preventable readmission.
It remains to be determined how triage should be conducted to select outpatient primary care services for surgical patients. As health care policy migrates toward capitated services, the relevant issue to address is whether all high-risk patients should be directed to primary care follow-up or whether there should be a targeted approach limited to patients most likely to benefit from primary care follow-up. Our study suggests that a good starting point is identifying patients undergoing surgical procedures associated with a high risk of readmission and focusing on those experiencing major complications during the postoperative course. Systems that identify and risk-stratify patients based on events during their postoperative hospital course can be used to ensure that individuals at high risk for readmission are targeted for primary care follow-up. This practice could be integrated as part of a coordinated transition care program using electronic health records, which have been shown 13 to be effective for preventing readmissions among high-risk medical patients. As the mandate to reduce health care costs and improve the quality of care for surgical patients is upon us, transitional care programs, such as the ones described here, may prove to be effective in reducing readmission rates.
Our study has several limitations. First, primary care use was determined retrospectively from claims and our data were observational. Differences in outcomes between primary care use groups may be confounded by unmeasured socioeconomic variables and other factors that can influence access to care. However, Medicare beneficiaries are provided similar health care benefits, and use of outpatient services is determined by providers and health care referral networks. Second, although the use of 100% denominator Medicare claims was a reliable data set for longitudinal assessment of readmissions rates, it is not possible to accurately ascertain the cause of postsurgical readmissions from administrative data. It will be important to determine the causes of readmissions, such as infectious or cardiopulmonary complications, to plan future quality improvement initiatives. Third, the precise temporal association and mechanism by which visiting a PCP lowers the risk of readmissions remains undefined. Addressing this question, however, will likely delineate the processes of care that are important in avoiding readmission of surgical patients. Finally, although open TAA repair and VHR were used as examples of high- and low-risk surgical procedures, respectively, these procedures may not adequately reflect the effect of early PCP follow-up care on readmission risks for other surgical patients. It will be important to evaluate the role of early PCP follow-up in transitions of care for other common surgical conditions.
Routine follow-up with a PCP after high-risk surgery was associated with a lower likelihood of 30-day readmission, particularly among patients with a complicated postoperative course. This association was evident both in patient- and regional-level assessment of primary care integration in the discharge process, and patients at the highest risk for readmission appear to receive the greatest benefit from early outpatient primary care services. Low-risk surgical patients, however, may not receive a benefit from this routine practice. Ensuring primary care follow-up for high-risk surgical patients may be an effective, low-cost mechanism to limit readmissions.
Accepted for Publication: October 25, 2013.
Corresponding Author: Benjamin S. Brooke, MD, PhD, Division of Vascular Surgery, Department of Surgery, University of Utah School of Medicine, 30 N 1900 E, Ste 3C344, Salt Lake City, UT 84132 ( [email protected] ).
Published Online: June 25, 2014. doi:10.1001/jamasurg.2014.157.
Author Contributions: Dr Brooke had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Brooke, Stone, Cronenwett, Goodney.
Acquisition, analysis, or interpretation of data: Brooke, Stone, Nolan, DeMartino, MacKenzie, Goodman.
Drafting of the manuscript: Brooke, Goodney.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Brooke, Nolan, DeMartino, MacKenzie, Goodney.
Obtained funding: Goodney.
Administrative, technical, or material support: Stone, Goodman.
Study supervision: Stone, Cronenwett, DeMartino.
Conflict of Interest Disclosures: None reported.
Funding/Support: Dr Goodney is supported by Career Development Award K08 HL05676 from the National Heart, Lung, and Blood Institute and a Society of Vascular Surgery Foundation award. Dr Goodman is supported in part by the Robert Wood Johnson Foundation.
Role of the Sponsor: The sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts

- For Ophthalmologists
- For Practice Management
- For Clinical Teams
- For Public & Patients
Museum of the Eye
- Managing Your Practice
- Managing Your Practice Topics
- Emergency Preparedness and Cybersecurity
- Practice Forms Library
- Practice Management News & Advice
- Lean Management
- Video Library
- My Green Doctor
- Ophthalmology Job Center
- Benchmarking & Salary Tools
- Academy Consultations
- Consultant Directory
- Coding Topics
- Ask the Coding Experts
- Cataract Surgery
- Codequest Events
- Coding for Injectable Drugs
- EM Documentation
- Ophthalmic Coding Specialist (OCS) Exam
- Savvy Coder
- Submit an Instruction Course
- Codequest Courses
- Mid-Year Forum
- Webinar Recordings
- Upcoming Webinars
- IRIS Registry
- Merit-Based Incentive Payment
- Medicare & MIPS
- Promoting Interoperability
- Improvement Activities
- Avoid a Penalty
- Medicare Participation Options
- Medicare Advantage Plans
- New Medicare Card
- Provider Enrollment, Chain and Ownership System (PECOS)
- Membership Benefits
- Renew/Pay Dues
- AAOE Membership
- AAOE Board of Directors
- Practice Views
- AAOE Content Committee
- Volunteer Opportunities
- For Practice Management /
- Ask the Coding Experts /
Insurance Changes During Global Period
Narrow your results, select code type, select topic.
- Cataract/Anterior Segment
- Coding Competency
- Coronavirus
- Oculofacial
- Pediatric/Strabismus
- Revenue Cycle Management
- Telemedicine
- Testing Services
- Trauma Coding
Select Category
About Our Coding Experts
About Our Coding Experts
Our expert staff have decades of combined experience, covering all aspects of coding and reimbursement.
John T. McAllister, MD Secretary, Federal Affairs
Michael X. Repka, MD, MBA Medical Director, Government Affairs
Joy Woodke, COE, OCS, OCSR Director, Coding and Reimbursement
Matthew Baugh, MHA, COT, OCS, OCSR Manager, Coding and Reimbursement Heather H. Dunn, COA, OCS, OCSR Manager, Coding and Reimbursement
Ask the Experts!
Email [email protected]
Note: Coding regulations and edits can change often. Academy coding advice is based on current information. Visit aao.org/coding for the most recent updates. Information provided by our coding experts is copyrighted by the American Academy of Ophthalmology and intended for individual practice use only.
- Mark Complete
All content on the Academy’s website is protected by copyright law and the Terms of Service . This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
- About the Academy
- Jobs at the Academy
- Financial Relationships with Industry
- Medical Disclaimer
- Privacy Policy
- Terms of Service
- Statement on Artificial Intelligence
- For Advertisers
FOLLOW THE ACADEMY
Medical Professionals
Public & Patients
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- EFORT Open Rev
- v.7(3); 2022 Mar 1

Large variation in timing of follow-up visits after hip replacement: a review of the literature
Mattia loppini.
1 Department of Biomedical Sciences, Humanitas University, Pieve Emanuele, Milan, Italy
2 IRCCS Humanitas Research Hospital, Rozzano, Milan, Italy
5 Fondazione Livio Sciutto Onlus, Campus Savona – Università degli Studi di Genova, Savona, Italy
Francesco Manlio Gambaro
Rob g h h nelissen.
3 Landelijke Registratie Orthopedische Implantaten (Dutch Arthroplasty Register), ’s Hertogenbosch, The Netherlands
4 Department of Orthopaedics, Leiden University Medical Center, Leiden, The Netherlands
Guido Grappiolo

- The study investigated the existing guidelines on the quality and frequency of the follow-up visits after total hip replacement surgery and assessed the level of evidence of these recommendations.
- The review process was carried out according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. Additional works were retrieved by direct investigation of the available guidelines of the most important orthopedic societies and regulatory agencies.
- The current systematic review of the literature resulted in zero original papers, four guidelines for routine follow-up and three guidelines for special cases. Concerning the quality of evidence behind them, these guidelines were not evidence based but drafted from expert consensus.
- The most important finding of this review is the large variation of recommendations in the follow-up schedule after total hip arthroplasty and the lack of evidence-based indications. Indeed, all the above-reported guidelines are the result of a consensus among experts in the field (level of recommendation class D ‘very low’) and not based on clinical studies.
Introduction
Total hip arthroplasty (THA) is one of the most frequent and successful surgeries performed in the orthopedic field, nevertheless, a clear consensus on post-surgical management still lacks ( 1 ). The need to define a clear protocol to manage patients after THA stems from a number of reasons such as the early identification of complications and the assessment of the right timing for a possible revision surgery. The latter aspect ensues due to the fact that prosthetic hip implants have a limited lifespan, which a recent review by Evans et al. has estimated to be around 20 years for 75% of patients and 25 years for 56% ( 2 ).
The gap of knowledge that the present review attempts to fill resides in the lack of clear indications regarding the follow-up visits schedule after THA. Indeed, this heterogeneity in terms of timing, number and nature of the visits following the discharge from the hospital still nowadays is not aligned with clear, evidence-based indications ( 3 ).
The main aim of the follow-up visits is to detect the asymptomatic failure of the hip prosthesis. The diagnosis of asymptomatic failure can prevent extensive surgery such as the full revision of the acetabular component instead of the liner exchange to manage the wear and complications such as periprosthetic fractures due to severe bone reabsorption and/or gross loosening. If the THA failure presents symptomatically, the patient either self-refers (45%) or is referred by the general practitioner (19%) or is referred from other hospitals (16%) or from the emergency room (7.5%) ( 4 ). On the other hand, only routine follow-up is able to identify the asymptomatic failures and these account for 9% of the total amount of failures ( 5 ). According to these data, the vast majority of current revisions are late surgeries. However, early THA revision surgeries (e.g. only revision of a worn-down liner) can provide better outcomes with lower complication rates because they can be a less extensive and non-acute procedure. In fact, complex revisions of THA have been found to cost up to 1.5 times more than the hospital and physician resources of routine revisions ( 5 ). Another reason behind performing routine follow-up is that the latter is able to identify not only asymptomatic failure but also slightly symptomatic patients, which symptoms are often not promptly correlated with the prosthetic implant. In addition, the traditional follow-up with scheduled outpatient visits represents an issue not only from the cost-effectiveness point of view but also for patient compliance. Indeed, only 61% of patients show up at follow-up visits at 1 year after surgery and that number drops even more at 2 years reaching 36% ( 6 ). This balance between the need to identify asymptomatic (radiographic) failures of THA (i.e. preventing more extensive revision surgery) and a cost-effective medical practice results in a vast heterogeneity regarding the proper schedule of follow-up visits after THA.
Materials and methods
The review process was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (flow chart in Fig. 1 ) ( 7 ). Literature research was carried out by two independent authors (M L and F M G) through August 2020 on PubMed, Google Scholar and Scopus databases with the following Medical Subject Headings: follow-up and total hip replacement. Additional information was retrieved from most recent publicly available guidelines of orthopedic societies and regulatory agencies such as the Food and Drug Administration (FDA), the Arthroplasty Society of Australia (ASA), Scientific Committee on Emerging and Newly Identified Health Risk (SCENIHR), British Orthopedic Association (BOA), Medicines and Healthcare Products Regulatory Agency (MHRA) and the National Institute of Health 1997 (NIH), Netherlands Orthopaedic Association 2018, American Association of Hip and Knee Surgeons (AAHKS) 2019 and the American Academy of Orthopedic Surgeons 2017 (AAOS). In order to judge the relevance of a study, the following inclusion criteria were adopted: information from original papers, an orthopedic society guideline or a regulatory agency recommendation, the inclusion of information on duration and frequency of the follow-up visits after THA and information in either English, German or Italian language. As the systematic review of the literature did not find any original paper, no quantitative or qualitative assessment could be performed. Therefore, only a qualitative analysis of guidelines retrieved from orthopedic societies and regulatory agencies’ websites was carried out. The latter was performed by means of the Grading of Recommendations Assessment, Development and Evaluation (GRADE).

PRISMA chart flow depicting the studies inclusion process after careful literature review.
The current systematic review of the literature resulted in zero original papers, four guidelines for routine follow-up ( 8 , 9 , 10 , 11 ) and three guidelines for special cases such as metal-on-metal (MoM) THA or small head size ( 5 , 12 , 13 ). Concerning the quality of evidence behind them, these guidelines were not evidence based but drafted from expert consensus. Therefore, the level of recommendation according to GRADE was of Class D (i.e. ‘very low’) ( 14 ).
Definition and content of follow-up
The typical surveillance program for THA includes follow-up visits composed of an interview with an orthopedic surgeon that performs a clinical assessment and, by means of an imaging tool, also a radiological assessment.
The inclusion of radiographic imaging during a routine follow-up visit after THA has been a matter of debate since it adds cost to the surveillance program. On one side, since the use of patient-reported outcomes alone is not able to assess a hip prosthesis state during a routine follow-up visit, the hip X-ray is suggested ( 15 ). On the other side, concerns on the ability of conventional radiographic imaging to effectively recognize THA failure have been raised ( 16 ). But even if plain radiography has some intrinsic limitations for the diagnosis of THA failure, it remains the first-step imaging technique and when inconclusive or doubtful, it can be followed by a more accurate tool such as a CT scan ( 17 ).
A further aspect to be acknowledged concerns the first visit after a THA procedure, since some guidelines ( 11 ) define the latter as the first meeting between the patient and the surgeon after the procedure typically occurring after a few weeks when the wound check and a general assessment are performed. Whereas other guidelines ( 9 , 10 ) do not include this meeting as part of the follow-up schedule.
Current guidelines for routine follow-up
The systematic review of the literature and the content of orthopedic societies websites demonstrated only five clearly described recommended schedules of THA follow-up visits. Large variability on the recommendation for frequency and duration of follow-up is present ( Table 1 ). For that matter, some guidelines only state that regular follow-up visits are important but do not specify frequency and duration during follow-up: the NIH consensus 1997 ( 18 ) and the AAOS guidelines 2017 ( 19 ).
Current guidelines for routine follow-up after THA.
AAHKS, American Association of Hip and Knee Surgeons; AOA, Australian orthopaedic association; ASA, Arthroplasty Society of Australia; BOA, British orthopedic association; NOA, Netherlands Orthopedic Association.
Furthermore, three orthopedic societies recommend a follow-up schedule based on a first visit within the first year after the operation, followed by a second visit around the seventh year and then a visit every 3–5 years. These recommendations are from the BOA guidelines 2012 ( 10 ), the Netherlands Orthopaedic Association 2018 ( 9 ) and the Arthroplasty Society of Australia 2019 ( 8 ). The guidelines of the BOA are justified since the majority of revision occurs 7 years after the first implant and early detection of aseptic loosening may prevent periprosthetic fracture. The latter has increased mortality and costs associated with revision surgery in an acute situation ( 20 ). Instead, the Netherlands Orthopaedic Association guidelines present a similar rationale behind their schedule of follow-up by underlining the risk of missing asymptomatic silent osteolysis or loss of function, which increases the risk of periprosthetic fracture after an in-house fall with devastating consequences. Finally, the Arthroplasty Society of Australia gives a similar justification of their recommendation warning orthopedic surgeons to be aware that despite most aseptic loosening being symptomatic, some may present with an insidious development, hence the need for a clinical and radiological review of all THA in an attempt to identify these ‘silent problems’ allows timely intervention.
The AAHKS 2019 ( 11 ) suggests a similar protocol compared to the three mentioned above, with a further recommended visit at the fifth year from surgery.
Current guidelines for follow-up in special cases
In some guidelines, a general schedule of follow-up visits (both frequency and duration) is missing, although precise recommendations on radiographic follow-up exist for high-risk patients ( Table 2 ). This risk assessment is based on both patient-specific and implant-specific factors.
Distribution of patient- and implant-specific factors in the current guidelines.
ASA, Arthroplasty Society of Australia; BOA, British Orthopedic Association; CKD, chronic kidney disease; FDA, Food and Drug Administration; MHRA, Medicines and Healthcare Products Regulatory Agency; SCENIHR, Scientific Committee on Emerging and Newly Identified Health Risk.
For example, the FDA guidelines ( 21 ) suggest regular follow-up visits (i.e. every 1–2 years) for MoM hip implants with certain risk factors (i.e. bilateral implants, the presence of small femoral heads (≤44 mm), female sex, patients receiving high doses of corticosteroids, with evidence of renal insufficiency, with immunosuppression, with suboptimal alignment of device components, with suspected metal sensitivity, BMI >40 and patients with high levels of physical activity).
While SCENIHR in 2014 ( 12 ) has released a statement suggesting yearly follow-up visits for all patients with MoM prostheses, small femoral head size and female gender, in addition, it recommends performing blood cobalt measurements (normal value range 2–7 μg/L) at follow-up visits.
In the United Kingdom, the annual report of MHRA 2017 ( 13 ) recommends the need for a more stringent follow-up schedule for MoM implants, younger patients and more active patients. Even more, for these patients, it is recommended to have an annual follow-up for the first 5 years then every 2 years until the tenth year and every 3 years thereafter.
As per the ASA guidelines ( 8 ), high-risk patients are defined as all patients with newly designed implants with limited long-term clinical results, younger patients, those with MoM articulation and total hip implants with small head sizes (≤36 mm) ( 22 ). For these patients, follow-up is recommended at yearly intervals with radiographs.
As for the latter, concerning new prosthetic implants, most guidelines also suggest a more stringent schedule of follow-up visits.: the BOA also recommends yearly radiographic follow-ups until the fifth year then every 2 years until the tenth year and then every 3 years.
The most important finding of this review is the large variation of recommendations on the follow-up schedule after THA as well as the lack of evidence-based recommendations of these follow-ups. Although, all reported guidelines are the result of a consensus among experts in the field (level of recommendation class D ‘very low’) with a rationale on the recommendation but not based on evidence from clinical studies.
Current guidelines do not recommend more than one follow-up visit (including radiographs) within the first year and one follow-up visit (including radiographs) between 2 and 10 years after surgery. Nevertheless, the assessment of a temporal sequence of radiographs plays a critical role in the early (asymptomatic) detection of failure of an implant. Although the pathophysiology of aseptic loosening is not completely understood, the main underlying mechanism is represented at radiographs by periprosthetic osteolysis induced by implant particles (e.g. liner wear). The latter usually have a diameter ranging from 0.2 to 10 μm ( 23 ), which induces an inflammatory process involving a variety of cells, eventually leading to aseptic loosening of the implant. This process results in visible radiological signs that the trained orthopedic surgeon can promptly identify at a radiograph. The identification of these radiological signs is facilitated when a temporal sequence of radiographs of the patient (e.g. hip etc) are present. Hence, the need of performing a schedule of regular follow-ups including radiological imaging is needed to detect subtle radiological changes. In particular, the temporal sequence of radiographs is most important during the first 2 years after hip prothesis implantation, since most implant migration occurs in this time window ( 24 ). This concept is supported by Mjöberg who in his ‘theory of early loosening of hip prothesis’ states that loosening is likely to begin at an early stage due to either insufficient initial fixation or an early loss of fixation ( 25 ). It should be noted that migration at radiographs is measured with an (in)accuracy of 4–12 mm. For that matter, radiostereometric analysis (RSA) is a highly accurate method to determine migration and wear of the prosthetic implant, with an accuracy of 0.1 mm in three dimensions ( 26 , 27 ). The advantage of the highly accurate RSA technique is that implants which are at risk for late failure can be detected within 1–2 years of follow-up ( 28 , 29 , 30 ). Data from these RSA studies on prosthesis migration within the first 2 years may support performing sequential radiographs during this time window, in order to detect early aseptic loosening. Nevertheless, further studies evaluating evidence of the use of normal radiographs, preferably using machine learning algorithms, are needed to support the importance of sequential series of hip radiographies for early detection of implant fixation problems.
Another interesting finding of this review is that a more stringent follow-up was recommended in high-risk patients, although each guideline defined ‘high-risk’ patients differently, making comparison difficult. The latter may be responsible for some of the large variation on the recommendation of follow-up visits after THA. Patient-related variables which determine to some extent timing of follow-up visits are younger age, female sex and high activity sport level. Indeed, according to the ASA and MHRA guidelines ( 8 , 13 ), younger patients require a more stringent follow-up, consisting of a yearly visit. While implant-specific variables which are associated with the timing of follow-up are the use of MoM prosthesis, the use of new prosthesis and the small size of the femoral head.
The large variation of recommendations in the follow-up schedule after THA observed by the current study is reflected by the lack of recommendations among the most relevant worldwide regulatory agencies in the medical field. Indeed FDA ( 21 ), the European Medicines Agencies ( 31 ) and the National Institute of Health and Care Excellence ( 32 ) only stress the importance of follow-up after THA without specifying its exact duration and frequency.
In addition, the frequency of follow-ups after a THA intervention is a matter that concerns the medical area as well as the socio-economic one. Indeed, in order to improve the efficiency of national healthcare systems, a cost-effectiveness analysis strictly depends on regional, economic and social aspects ( 33 ) therefore contributing to the heterogeneity observed in the current study.
Already in late 90’, an attempt was made to improve the cost-effectiveness of the radiographic follow-up visits for patients who had hip replacement surgery. It was theorized that a system in which trained medical staff would review routine radiographs in order to decide if a face-to-face visit was needed. This system would have allocated outpatient follow-up visits only to patients at risk of THA failure. More recently, this concept has been further developed in what has been defined as the ‘virtual clinic’. This system determines who should be offered a face-to-face appointment based on routine radiographs and questionnaires (Oxford hip or knee score), reviewed by a consultant orthopedic surgeon ( 34 ).
To investigate the efficacy of the virtual clinic to detect potential implant failure, a recent study compared the traditional outpatient visits with radiographs and questionnaires related to revision symptoms without patient contact. The results showed a substantial agreement between the two, especially for TKA (81%) and to a lower extent also for THA (69%) suggesting that the virtual clinic is a valid alternative to face-to-face visits ( 35 ). A similar study that randomized THA patients to either the traditional follow-up system based on routine outpatient visits (including radiographs) or to a questionnaire- and radiograph-based remote follow-up found that no patients who had a potential failure were missed by the remote follow-up ( 36 ). Recently during the coronavirus disease 2019 pandemic, some surgeons of BOA employed virtual follow-ups by using telephone consultations for patients unable to attend their routine THA postoperative visits. Although 63% of patients were satisfied by the ‘virtual’ appointment, 75% of patients would prefer to have their next appointments face-to-face. The latter may be related to the population of 70 years and older and the unfamiliarity with technology like electronic questionnaires. Although this may also be related to accessibility and internet density, which can be different between countries ( 37 ), it could not be related to the confidence a physical examination and face-to-face explanation give to a patient. The latter also stresses the importance of general guidelines which have to be patient specific. The main limitations of this review are represented by the limited number of guidelines and no clinical studies which report on the topic of recommendation of radiographic follow-up and the ambiguity of the definition of post-surgical follow-up. For that matter, most guidelines do not include the first visit after surgery as part of the schedule of visits, which is in our opinion important in order to compare subsequent future radiographs. Another limitation stems from the study design of the current review. In fact, after performing a systematic review of the literature and retrieving zero original papers, we could only analyze guidelines from orthopedic societies and regulatory agencies.
Conclusions
- The follow-up schedule after THA is nowadays arbitrary organized based on consensus among experts and not on evidence.
- Current guidelines do not recommend more than two radiographs 10 years after surgery.
- In certain guidelines, more stringent follow-up was recommended in high-risk patients, but the definition of ‘high risk’ was very heterogeneous among them.
- There is a clear need to develop data-based recommendations for clinical and radiographic follow-up after hip replacement.
ICMJE Conflict of Interest Statement
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Funding Statement
This work did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
- [email protected]
- (813) 940-SURG (7874)

Post-Operative Follow-Up Visits
This past week our practices made adjustments to our post-operative visit protocols. Our standard process pre-COVID-19 is seeing patients in the clinic within two weeks following low-risk, uncomplicated cholecystectomies, appendectomies, hernia repairs, and the like. However, with the COVID-19 outbreak, we felt standardizing follow-up visits via telehealth with visits by telephone versus in-person clinic visits, would be the right thing to do for several reasons:
First, the telephonic follow-up visit reduces the risk of exposure to COVID-19 at a time when the patient’s immune system is working hard to heal from surgery.
Second, for some patients, the drive to the clinic can mean an extended period in the car which may be inconvenient and uncomfortable.
Third, managing follow-up visits with patients by telephone also reduces risk of exposure for our surgeons, advanced practice providers, and office staff, who must remain in good health to be of service to others in each community we serve.
Now, when our office administrators call our patients to schedule a post-op follow-up visit with the surgeon or advanced practice provider, they first screen to ensure the patient is a candidate for a telehealth visit versus an in-person clinic appointment. According to Rae Samhoury, our Director of Practice Operations, this new follow-up option has been positive, “The telephonic appointments are going well. We’ve received great responses from both the providers and the clinical staff from offering this type of follow-up option.”
“As we continue to innovate as an organization, perhaps telehealth will become part of how we routinely conduct follow-up visits for low-risk patients,” says Dr. Mit Desai, Founder and CEO of The Surgicalist Group. “We continue monitoring the process, making adjustments when necessary to best serve our communities.”
Previous Post An Alternative Model of Surgical Staffing
Next post taking care of yourself, related posts.

Raising the Standard of Care for Surgical Patients
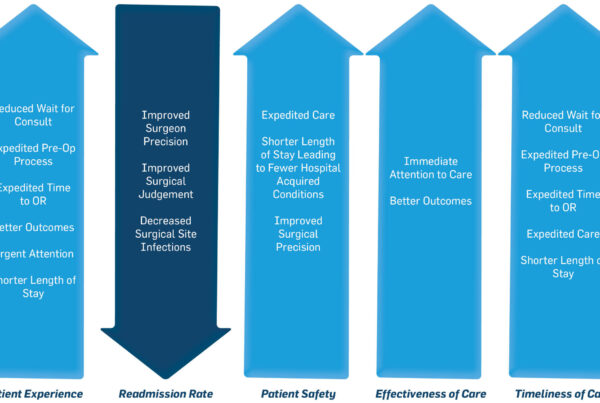
- For Hospitals
- For Surgeons
- For Patients
- News & Insights
- Terms of Use
- Privacy Policy
- Patient Privacy
Copyright©2020 - The Surgicalist Group - All Rights Reserved
- Case Studies
- Press Releases
- (813) 940 7874
Privacy Overview

IMAGES
VIDEO
COMMENTS
99024 - Postoperative follow-up visit, normally included in the surgical package, to indicate that an evaluation and management service was performed during a postoperative period for a reason(s) related to the original procedure. Applies to surgeries with 90 and 10 day global periods. Indicates that a required postoperative visit has been ...
Minor procedures are relatively simple and may have either a 0-day or 10-day global period. A 0-day global means there is no pre-operative period and no post-operative days. That is, the global package applies for one day, only (the day of the procedure or service). A 10-day global has no pre-operative period and a 10-day post-operative period.
Postoperative Visits: The Importance of CPT 99024. Current Procedural Terminology (CPT) code 99024 is defined as a "postoperative follow-up visit, normally included in the surgical package, to indicate that an evaluation and management service was performed during a postoperative period for a reason (s) related to the original procedure."1.
The current procedural terminology (CPT) describes the postoperative follow-up visit with the 99024 CPT code. Description Of The 99024 CPT Code CPT code 99024 usually comprises the surgical package to designate that the provider did perform an evaluation and management service during a postoperative period for reasons related to the original procedure. Official description CPT...
Procedure Values. When the value of any procedure is determined, the number of global postoperative encounters that typically follow that procedure is taken into consideration. For example, the value of CPT 10140 (Incision and drainage of hematoma, seroma or fluid collection) was determined considering one postoperative visit within the 10-day ...
Code 99024 captures services normally included in the surgical package, indicating an evaluation and management (E/M) service was performed during a postoperative (post-op) period for a reason (s) related to the original procedure. Note: Codes that are striked through were deleted for 2018 and no longer apply.
Reporting Related E/M Services During Global You may report related E/M services during the global period with 99024 Postoperative follow-up visit, normally included in the surgical package, to indicate that an evaluation and management service was performed during a postoperative period for a reason(s) related to the original procedure. There ...
Resources. Centers for Medicare & Medicaid Services: www.cms.gov. Contact CMS: [email protected]. Contact ASPS: (847) 228-9900 or [email protected]. Physicians that provide 10- and 90-day global services would be required to report information on the number of postoperative visits they provide.
4. Follow-up visits during the post-operative period of the surgery that are related to recovery from the surgery 5. Post-surgical pain management by the surgeon 6. Supplies, except for those identified as exclusions 7. Miscellaneous services, such as dressing changes, local incision care, removal of operative pack, removal of
Answer: CPT code 99024 should only be reported for post-operative visits that would not reported otherwise because it is delivered during the global period even though it meets all the other the requirements for E/M visits. Therefore, CPT code 99024 should only be reported with the place of service (POS) code 02 for a post-operative visit that ...
Follow-up visits during the postoperative period of the surgery that are related to recovery from the surgery; Post-surgical pain management by the surgeon; Supplies, except for those identified as exclusions; Miscellaneous services, such as dressing changes; local incision care; removal of operative pack; removal of cutaneous sutures, staples ...
by Aimee L. Wilcox, CPMA, CCS-P, CST, MA, MT Sep 12th, 2023. CPT® 99024 was introduced by the American Medical Association (AMA) with an effective reporting date of January 1, 2013. The associated code description is as follows:, "Postoperative follow-up visit, normally included in the surgical package, to indicate that an evaluation and management service was performed during a ...
When your ob-gyn sees a traditional Medicare patient after a surgery, you will need to report 99024 (Post-operative follow-up visit, normally included in the surgical package, to indicate that an evaluation and management service was performed during a post-operative period for a reason[s] related to the original procedure) for each routine ...
The global period for these codes will be 0, 10, or 90 days. Note: not all contractor-priced codes have a "YYY" global surgical indicator. Sometimes the global period is specified as 000, 010, or 090. While codes with "ZZZ" are surgical codes, they are add-on codes that you must bill with another service.
Importance of Postoperative Follow-Up for Patient Outcome. Attentive care is vital to favorable outcomes in medicine. This is particularly important for the surgical patient, for whom preoperative preparation, good inpatient care, and home postoperative recovery support are essential for optimal outcomes. In the management of many types of ...
Importance Follow-up with a primary care provider (PCP) in addition to the surgical team is routinely recommended to patients discharged after major surgery despite no clear evidence that it improves outcomes.. Objective To test whether PCP follow-up is associated with lower 30-day readmission rates after open thoracic aortic aneurysm (TAA) repair and ventral hernia repair (VHR), surgical ...
Answer: The global period should continue per the original insurance payment. You should not bill for related office visits and medically necessary tests or procedures would not need modifiers. The new insurance would not be aware of the previous surgery and would deny services billed with any additional modifiers.
In addition, the traditional follow-up with scheduled outpatient visits represents an issue not only from the cost-effectiveness point of view but also for patient compliance. Indeed, only 61% of patients show up at follow-up visits at 1 year after surgery and that number drops even more at 2 years reaching 36% . This balance between the need ...
Caution: CPT ® includes 99024 (Postoperative followup visit, normally included in the surgical package, to indicate that an evaluation and management service was performed during a postoperative period for a reason[s] related to the original procedure) for related postoperative visits within the global period. Although your orthopedist is ...
First, the telephonic follow-up visit reduces the risk of exposure to COVID-19 at a time when the patient's immune system is working hard to heal from surgery. Second, for some patients, the drive to the clinic can mean an extended period in the car which may be inconvenient and uncomfortable. Third, managing follow-up visits with patients by ...
of deferral of the first follow-up visit at 1 week. Methods: Randomized Controlled Trial was conducted at a tertiary eye care hospital, with 848 patients enrolled for the study. Patients meeting the inclusion criteria were selected. Their pre-operative and post-operative data was collected and the patients were divided into groups based on the type of cataract surgery and the postoperative ...
Purpose To compare the postoperative outcomes and management of uncomplicated cataract surgery seen on postoperative day 0 (POD0) versus postoperative day one (POD1). Methods A retrospective cohort study of patients who followed up within 0-14 days of their uncomplicated surgery (current procedural terminology code 66984) from December 2018 to March 2020. Those who had perioperative ...
While this section addresses "procedures" considered as part of the post-procedure work, it fails to address the issue of post surgical evaluation and management services. Subsection D of Chapter I addresses evaluation and management (E/M) services, but only focuses on the E/M services performed "on the same date of service as a procedure ...