

Welcome to The Patient Journey Course
Unlock the secrets to skyrocketing your case acceptance rates with our comprehensive online course. Learn how to confidently communicate with your patients, handle objections, and present treatment plans in a way that resonates with their personality type. With our proven strategies, you'll see a significant increase in your case acceptance, leading to a higher monthly income, a successful practice brand and most importantly satisfied patients. Don't let another potential case slip through your fingers
The first impression is everything, and that's especially true when it comes to patient consultations. If you want to make a good impression and increase your case acceptance rate, you need to deliver the perfect consultation. In this course, you will learn how to: - Build rapport with your patients - Ask the right questions Present your treatment plan in a clear and concise way - Overcome objections - Close the sale By the end of this course, you will be able to deliver consultations that are both informative, persuasive and fun.
Whether you're dealing with NHS or private patients, effective communication is key. Our course offers tailored strategies for both sectors, helping you navigate the presentation of both options and converting more patients to private treatment. Learn how to build trust, manage expectations, and deliver exceptional patient care, regardless of the setting.
Take the guesswork out of patient communication with our tried-and-tested frameworks and scripts. We provide you with the tools to handle any scenario, from tricky patients to complex treatment discussions. With our course, you'll never be at a loss for words again.
We believe in the power of learning from real-world examples. That's why we've included an exclusive archive of real patient journeys I have filmed (as Dental Hype) over the years, shared by successful clinicians You'll learn from their experiences, their mistakes, their highly converting tactics. These are the insider secrets you won't find anywhere else. Our courses will be available to you anytime, with unlimited access. Disclaimer: CPD Certificates will be sent after 6 months from launch upon full course module release.
Learn how to create comprehensive, understandable, and premium treatment plans that your patients will readily accept. We'll teach you how to effectively communicate the value of your services and how to actually price your treatments irrespective of what your competition is doing.

Course Curriculum
You want to build a great patient journey? It starts with great foundations. This module will teach you the building blocks of what the highest converting clinicians do, day-in day-out in their surgeries.
Want to learn how to persuade your patients effectively? To talk their language? To read their personality types? This cutting edge, psychometric framework has not been taught in dentistry before. This module will teach an efficient method to be able to read patients fast and mould your patient journey and treatment plan presentation in a way that will be help your case acceptance increase exponentially without needing to "hard sell!"
Learn the ultimate patient journey framework. Bring your patients through the six phases of dental communicative excellence. Transform your patient journey forever and create an eager waiting list of patients built on amazing word of mouth referrals. Warning - This module will change your career (and potentially your life).
"I don't know how to discuss prices with patients" - Every Dentist Ever. The most common complaint we hear with regards to treatment planning is about price. We are looking to make this complaint a myth with this module. By the end of this module we will have your treatment planning process optimised, taking your presentations from "high stress selling" to "low stress conversations" that convert high end treatment with ease.
Are you tired of constantly under-pricing your high quality work to match your local competitions prices? Do you want the confidence to be able to charge a premium? From pricing strategies and price psychology to treatment planning frameworks and presentation tips & tricks - this module has it all.
In Module 6 of our patient journey course, we dive into the intricacies of operating a mixed practice and achieving patient journey perfection within the NHS system. This module is designed to equip you with the necessary knowledge and skills to seamlessly convert NHS patients to private patients while presenting both options in a persuasive and compelling manner. We understand that navigating the complexities of the NHS system can be challenging, and our aim is to empower you with practical strategies to optimize the patient experience and facilitate a smooth transition from public to private care. Throughout this module, you will gain invaluable insights into the key factors that influence patient decisions and learn effective techniques to engage and educate them about the benefits of private healthcare. We will delve into various topics, including: 1. Understanding the NHS Patient Journey: You will explore the entire patient journey within the NHS system, from initial contact to post-treatment follow-up. By comprehending the intricacies of this process, you will be better equipped to identify opportunities for presenting private care as a valuable alternative. 2. Tailoring the Patient Experience: Creating a seamless and personalized patient experience is paramount in ensuring patient satisfaction and loyalty. We will provide you with practical tips and strategies to enhance the patient journey, including effective communication techniques, active listening, and fostering a sense of trust and rapport. 3. Presenting Private Care Options: Converting NHS patients to private patients requires a delicate balance of presenting the advantages of private healthcare while respecting the existing system. We will guide you through the process of showcasing the unique benefits of private care, emphasizing personalized attention, reduced wait times, access to advanced treatments, and the overall enhanced patient experience. 4. Overcoming Patient Objections: Addressing patient concerns and objections is a crucial aspect of the conversion process. We will equip you with proven techniques to handle objections effectively, emphasizing the value proposition of private care and highlighting the long-term benefits that patients can enjoy. By the end of this module, you will possess the tools and knowledge to navigate the challenges of operating a mixed practice successfully. You will be able to present both NHS and private care options in a persuasive and compelling manner, ultimately helping patients make informed decisions that align with their healthcare needs and aspirations.
The anxiety you face dealing with a difficult patient. The gut wrenching moment you get a complaint. We have you covered. We have multiple, step-by-step, tried and tested frameworks to not only avoid or mitigate against complaints but also turn those difficult patients into your biggest fans! Unbelievable right? You might want to hear us out.
We walk the walk in this course. You are about to see BTS footage of Dr Raabiha Maan with a myriad of different patients. Watch how she communicates, educates, handles objections, treatment plans, manages difficult patients, puts them at ease, wins their hearts, converts high end treatment with ease and has her patient returning for years to come! It's our Patient Journey Framework in action. Once you see this module, you won't practice day-to-day dentistry the same way again.
Implementation. That is what separates a "good" clinician from a "great" one! A "good" course from a "great" one! A "good" patient journey from a "great" one! You are here for a transformation so this module teaches you how to implement everything you have learnt in this course. We made this course for a reason. To help Clinicians Create a personalised, repeatable and unique patient journey that you feel confident and comfortable delivering. Your patients leave with absolute faith in you and talk about you to their friends as “the best experience in a dental practice I've ever had”. So we'll be damned if you don't go ahead and get that outcome for yourself.
Ever wondered what other clinicians patient journeys look like in real life? Never been done in any online course before ... This is our behind the scenes "Fly on the wall content" with real patients and real clinicians that we have filmed over the last 6 years. Finally understand what makes other clinicians so good and learn from what they say/do to close their patients.
Testimonials

Lorem ipsum dolor sit amet, consectetur adipiscing elit. Nullam et lacinia mi. Proin in sagittis dolor. Curabitur et quam id mauris.
“Amazing content. Really impressed/inspired by your story!”
"One of the best online courses I have purchased. Dr Rhona is an amazing teacher and really makes you feel empowered to implement all the ideas, tactics and workflows that she reveals in the course. As a practice owner, I was blown away by the efficiency at which she manages her Invisalign volume. Learning her workflows and social media strategies were worth way more than the price of admission - I was so impressed I've upgraded onto her mentorship programme so I can shadow her and learn first hand. Thank you Rhona."
“Hey Rhona! I did my first composite bonding case today! Still needs adjustments and polishing but watched your module on composite last night and it helped so much thank you!! Made the treatment flow so much better than I expected and i loved it so much! Hopefully much more to come✨”

Get started today
DentalHype © 2023
Root out friction in every digital experience, super-charge conversion rates, and optimize digital self-service
Uncover insights from any interaction, deliver AI-powered agent coaching, and reduce cost to serve
Increase revenue and loyalty with real-time insights and recommendations delivered to teams on the ground
Know how your people feel and empower managers to improve employee engagement, productivity, and retention
Take action in the moments that matter most along the employee journey and drive bottom line growth
Whatever they’re are saying, wherever they’re saying it, know exactly what’s going on with your people
Get faster, richer insights with qual and quant tools that make powerful market research available to everyone
Run concept tests, pricing studies, prototyping + more with fast, powerful studies designed by UX research experts
Track your brand performance 24/7 and act quickly to respond to opportunities and challenges in your market
Explore the platform powering Experience Management
- Free Account
- For Digital
- For Customer Care
- For Human Resources
- For Researchers
- Financial Services
- All Industries
Popular Use Cases
- Customer Experience
- Employee Experience
- Net Promoter Score
- Voice of Customer
- Customer Success Hub
- Product Documentation
- Training & Certification
- XM Institute
- Popular Resources
- Customer Stories
- Artificial Intelligence
- Market Research
- Partnerships
- Marketplace
The annual gathering of the experience leaders at the world’s iconic brands building breakthrough business results, live in Salt Lake City.
- English/AU & NZ
- Español/Europa
- Español/América Latina
- Português Brasileiro
- REQUEST DEMO
- Experience Management
- Sector Specific
- Patient Experience
- Patient Journey Mapping
Try Qualtrics for free
Your complete guide to patient journey mapping.
15 min read Healthcare organizations can increase patient retention and improve patient satisfaction with patient journey mapping. Discover how to create a patient journey map and how you can use it to improve your organization’s bottom line.
What is the patient journey?
The patient journey is the sequence of events that begins when a patient first develops a need for care. Rather than focusing on service delivery, the patient journey encompasses all touchpoints of a patient’s healthcare experience–from locating healthcare providers and scheduling appointments, to paying the bill and continuing their care after treatment.
Examining the patient journey is essential to improving the patient experience. Not all interactions a patient has with your organization are weighted the same. Gathering patient feedback and understanding perceptions all along the patient journey can help you to identify moments of truth : the touchpoints that have the biggest impact on patient loyalty.
Download eBook: The 3 steps to driving human-centered healthcare experiences
The patient journey vs. the patient experience
Unlike traditional patient experience measurement, the patient journey looks not only at service delivery but also at the steps the patient takes before and after they engage directly with your organization. It recognizes that patient interactions with a healthcare system go well beyond the walls of the medical facility itself.
What are the stages of the patient journey?
There are several stages along the patient journey. When gathering patient feedback, you should make sure to capture insights at each of these stages.
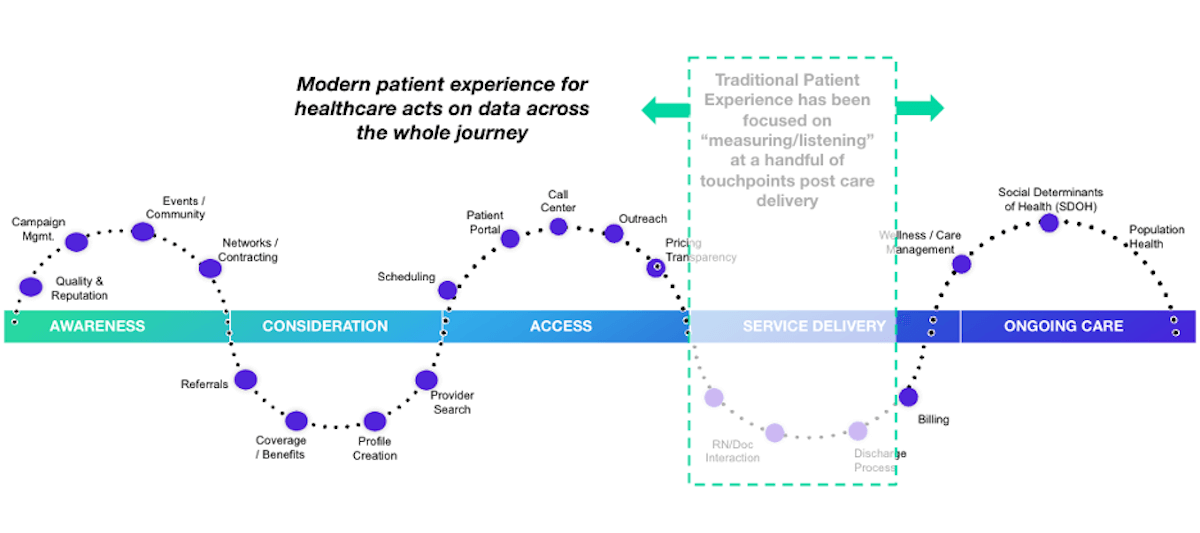
Stage 1: Awareness
The patient journey starts with awareness. In this stage, the patient identifies a need for care and begins searching for care providers. Examples of how patients learn about healthcare providers include online searches, review sites, marketing campaigns, networking, and community involvement.
Stage 2: Consideration
In the consideration stage, the patient weighs their options to determine if your health system can meet their needs. Factors patients consider include referrals, coverage and benefits, recommendations, access, and ratings and reviews. Often in this stage, patients interact with your website or social media pages or contact you via phone or email during this stage.
Stage 3: Access
The access stage is where the patient decides to schedule services with your healthcare organization. Direct patient engagement with your organization increases during this stage. You’ll engage with patients in a variety of ways including phone calls, the patient portal, text messages, and emails as part of the scheduling and new patient acquisition process.
Stage 4: Service delivery
The service delivery stage relates to the clinical care provided to your patients. Encompassed in this stage are the clinical visit itself, check-in and check-out, admission and discharge, and billing. Traditional patient satisfaction measurement centers around this stage of the patient journey.
Stage 5: Ongoing care
The ongoing care stage of the patient journey involves patient engagement that occurs after the interactions directly related to service delivery. In addition to wellness and care management, this stage may address social determinants of health and population health.
What is a patient journey map?
The best way to utilize the patient journey to enhance patient experiences is by journey mapping. A patient journey map is a visual tool that illustrates the relationship a patient has with a healthcare organization over time.
Patient journey mapping helps stakeholders to assess the patient experience from multiple perspectives. Journey maps provide a way to visualize the internal and external factors affecting patient flow and the different paths patients must take in order to reach their care goals.
What are the benefits of patient journey mapping?
Patient journey mapping can help you to visualize all of the steps patients take throughout the entire process of seeking, receiving, and continuing care. Creating a patient journey map is useful to identify pain points and gaps in care. Mapping the patient journey makes it easier to develop solutions that make a more seamless experience within your healthcare system.
Patient journey mapping benefits include:
- Creating shared ownership of the patient experience
- Refining your patient listening strategy
- Aligning your organization with a common view of the patient experience
- Measuring gaps between the intended experience for your patients versus the actual experience
- Identifying and resolving common pain points for your patients
Four types of patient journey maps
When creating a patient journey map, there are four types to consider. Each type of map has an intended purpose. You might start your patient journey mapping with only one type and incorporate the others as your efforts progress.
Current state
A current state journey map tells the story of what patients do, think, and feel as they interact with your organization today. This type of patient journey map is ideally created using patient data and observational data.
The current state journey map is best for driving incremental improvements to enhance the patient experience.
Future state
A future state patient journey map tells the story of what you want your patients to do, think, and feel as they interact with your organization in the future. This type of map should capture the ideal journey you’d like to see for your patients.
The future state journey map is an effective tool to drive strategy, align teams, and communicate your visions for new services, processes, and experiences.
Day in the life
A day in the life patient journey map illustrates what your patients do, think, and feel today, within a specific area of focus. Patient personas are particularly useful when creating day in the life maps; these are discussed in greater detail below.
This type of patient journey map is intended to capture what your patients experience both inside and outside of the healthcare system. Day in the life maps are valuable to address unmet needs and determine how and when you can better engage your patients.
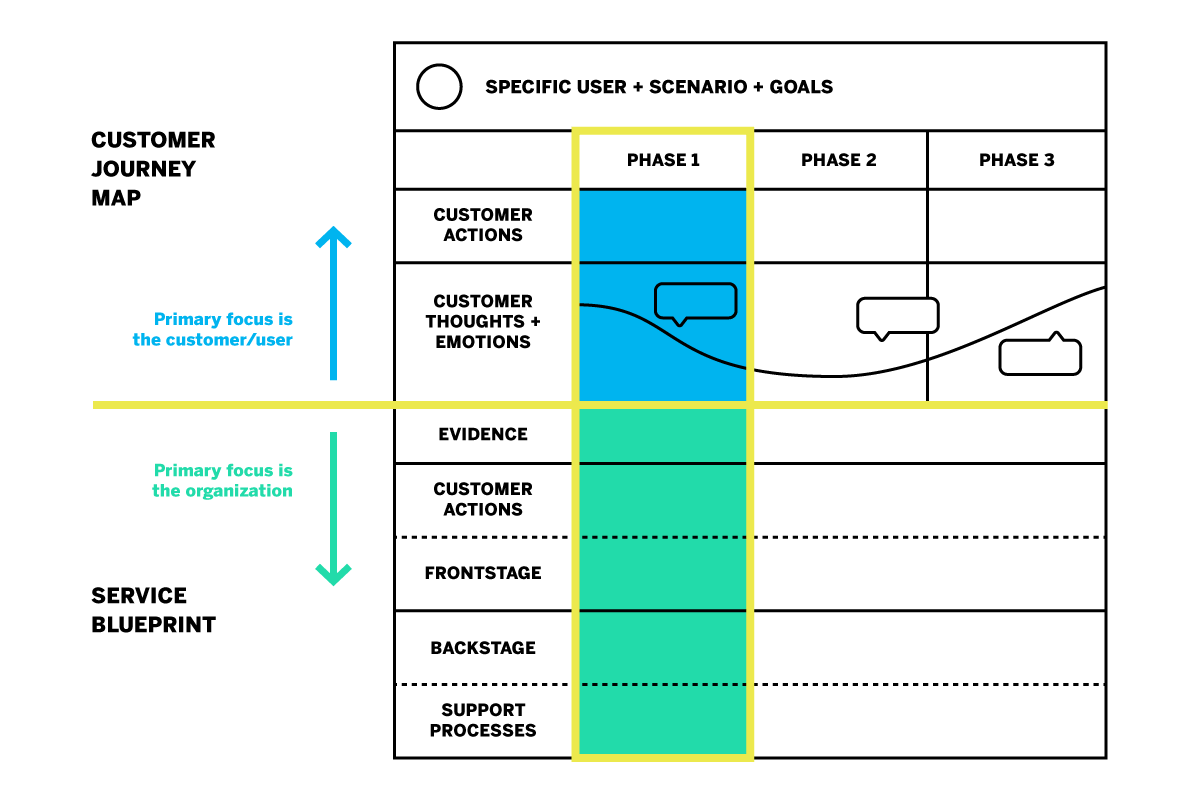
Service blueprint
A service blueprint is a simplified diagram of a current state or future state patient journey map. In the service blueprint, you add layers to illustrate the systems of people, processes, policies, and technologies surrounding each patient touchpoint.
For current state patient journey maps, the service blueprint can help to identify root causes of pain points. For future state, the service blueprint is helpful to visualize the systems or processes that can be put in place to support the intended patient experience.
How do you create a patient journey map?
Now that you know about the different types of patient journey maps and their roles in driving patient experience improvement, how do you get started on creating your own?
The most useful maps are those which can expound upon each touchpoint of the healthcare journey with operational data, such as patient demographics, as well as real patient insights and perspectives. Using a platform that can capture this data will aid significantly in your patient journey mapping process.
Patient journey mapping: getting started
Before you get started, it’s a good idea to engage individuals across all departments and include input from multiple stakeholders. Once you’re ready, follow these steps to begin creating an effective patient journey map.
Identify your target audience
What type of patient journey will you be mapping? There may be varying patient journeys within your organization; for instance, an oncology patient’s journey will look very different from that of an expectant mother. The journey of a patient with health insurance will differ from that of a patient without insurance. To map the patient journey, you’ll want to create robust patient profiles you can use to segment and track like-populations throughout the healthcare experience.
Establishing patient personas and segments
Not every patient will have the same healthcare goals. Creating patient personas based on behaviors and preferences is a good way to differentiate the needs and more clearly understand the perspectives of the unique populations you serve.
The ideal patient persona will include the following information.
- Demographic information such as age group, gender, or location
- Healthcare-specific goals, conditions, and treatments
- Healthcare-specific challenges/pain points
- Engagement patterns and expressed feedback
- How your services fit into their life
- Barriers to care
Specify a goal for the patient’s journey
The patient personas you create will all have unique goals within the care journey. The patient has a specific goal in mind when they initiate contact with your organization, whether it is treatment of symptoms, a diagnosis for chronic issues, or surgery.
Every interaction along the patient journey influences how successful the patient feels about achieving this goal. When mapping the patient journey, you’ll want to consider how the various touchpoints affect the patient’s ability to meet this goal.
Identify the patient’s steps to accomplish their target goal
This step is about how the patient views their care journey within your health system–not about the actual processes and systems your organization has in place. Effective patient journey mapping requires you to see how the patient navigates the journey through their point of view.
Omni-channel listening is a valuable strategy in this step of journey mapping. Listening to your patients across all the channels can provide a clearer picture of their perceptions and behaviors as they engage with your organization.
Some steps the patient takes may not even include your organization, but might still affect how they are interacting with you directly. For example, if a patient logs into their health insurance portal to check coverage for healthcare services, they are not engaging with your organization but this is still a part of their care journey that may feed into their interactions with your organization later on.
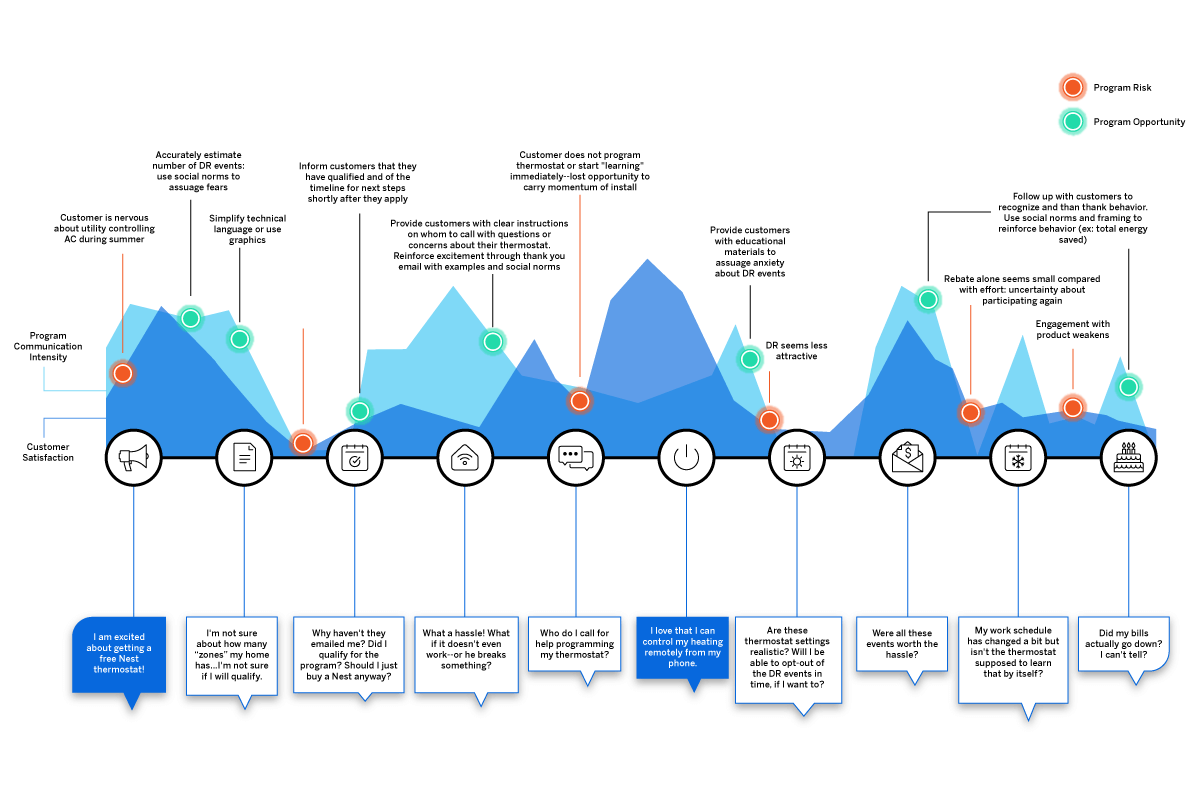
Uncover perceptions along the journey
Gather patient feedback along the touchpoints of the care journey to identify key emotional moments that may disproportionately shape attitudes. These insights shed light on what’s working and what’s not; they can also be used to highlight the moments of truth that contribute to patient loyalty.
Patient perceptions are an important piece of patient journey mapping; it will be difficult to drive action without them.
Additional tips for creating the ideal patient journey map
Patient journey mapping is a continuous process. Creating the map is the first step, but the true value is dependent upon maintaining the map as you continue to gather insights and refine processes.
This leads to the second tip: be ready to take action! You can use a patient journey map to draw conclusions about your patients’ experiences within your organization, but awareness alone will yield no benefits. The journey map is a valuable tool to be used in your wider improvement efforts.
How do you drive action using a patient journey map?
Once your patient journey mapping is complete, it’s time to put it to good use. Here are five ways patient journey maps can be used to drive action.
Identify and fix problems
The visual layout of a journey map makes it ideal to identify gaps and potential pain points in your patient journeys. This will give you a better understanding of what’s working and what’s not. It will also help you to visualize where and how improvements can be made.
Build a patient mindset
Patient journey mapping enables you to incorporate more patient-centric thinking into your processes and systems. Use your map to challenge internal ideas of what patients want or need. Invite stakeholders to navigate the touchpoints along the healthcare journey to gain perspective.
Uncover unmet patient needs
By mapping the patient journey, you can build stronger patient relationships by listening across all channels to determine where experiences are falling short or where unmet needs emerge. This enables you to look for opportunities to expand alternatives, streamline initiatives, and create new, engaging ways for your patients to share feedback.
Create strategic alignment
Utilize your patient journey map to prioritize projects or improvement efforts. It can also help you to better engage interdepartmental staff to better understand policies and work together toward patient experience goals.
Refine measurement
Patient journey mapping is a great resource to use when defining patient satisfaction metrics and identifying gaps in how you currently gather insights.
How does patient journey mapping increase your bottom line?
Patient journey mapping can increase your bottom line by laying the foundation for improved patient satisfaction and higher retention.
Organizations across all industries are looking to understand customer journeys in order to attract and retain customers by gaining deeper insights into what drives the consumer experience.
As healthcare becomes more consumer-driven, health systems must similarly map the patient journey to improve the patient experience and boost retention. The cost of patient acquisition, combined with the fact that patients are willing to shop around for the best healthcare experience, means success depends on creating the most seamless patient journey possible.
The tools for success
For the most impactful patient journey mapping experience, you’ll want the ability to link your operational and experience data to your journey map’s touchpoints. Insights about what has happened at each touchpoint, as well as why it is happening, empower you to create experiences that meet patient expectations and drive up satisfaction.
Here are some best practice considerations as you develop your patient journey mapping strategy:
- Create a shared understanding throughout your health system of how your patients interact with your organization, and you’ll know the roles and responsibilities of your different teams
- Design a unique patient journey based on multichannel, real-time feedback from the patient
- Consider the frequency with which topics emerge in feedback, as well as the emotional intensity behind them to zero in on what improvements can drive the greatest impact
- Develop empathy and collaboration between teams, working together to achieve the same outcome
- Drive a patient-centric culture by developing a shared sense of ownership of the patient experience
- Connect your operational patient data with your patient experience feedback in one system
- Leverage a closed-loop feedback system that triggers actions for immediate responses to patient concerns
Qualtrics’ XM Platform™ is designed to support all of these actions throughout the journey mapping process.
The 3 steps to driving human-centered healthcare experiences
Related resources
Patient feedback 15 min read, healthcare branding 13 min read, patient journey 10 min read, patient experience 12 min read, symptoms survey 10 min read, nurse satisfaction survey 11 min read, cahps surveys 6 min read, request demo.
Ready to learn more about Qualtrics?

transforming healthcare leadership and management
Patient Experience
Patient Experience and Service Excellence
Design and deliver more person-centred, compassionate and responsive care, about the course.
There is growing evidence that better patient experiences lead to measurably better health outcomes, enhanced patient safety and improved revenues. So today, more than ever, we must build healthcare services around the needs of patients and their families.
IHLM’s popular course on Patient Experience and Service Excellence is for progressive healthcare providers and professionals who want to design and deliver more person-centred, compassionate and responsive care.
The course has been developed by IHLM faculty in collaboration with leading patient experience experts and carefully benchmarked against the Picker Institute’s Principles of Person-Centred Care , the Beryl Institute’s Patient Experience Body of Knowledge and the Planetree Person-Centred Care Certification Criteria . It will provide you with a comprehensive understanding of this entire area of healthcare management and prepare you for future professional opportunities in the field.
Delivered via IHLM’s online learning platform and through live interactive virtual tutorials you will become part of a global community learning how to transform patient experience together.
What you’ll learn
On completion of this course you’ll be able to:
- understand what person-centred care is and set-up the systems, processes and resources needed to deliver it
- educate and support healthcare staff to become more compassionate and engaged caregivers
- collaborate with patients and caregivers to co-design more person-centred services and smoother patient journeys
- create effective systems for collecting patient experience data and acting on improvement opportunities
- evaluate and improve the emotional, clinical, functional, physical and digital dimensions of patient experience
How you’ll learn
This course is broken down into ten manageable weekly modules:
- work at your own speed through a carefully curated collection of self-paced online learning materials that include video lectures, podcasts, interviews and real-world case studies
- evidence-based research from peer-reviewed publications will help you dig more deeply into topics that really interest you
- you are not alone – you will interact with other course members, collaborate on learning activities and get direct feedback and coaching from the course leader during weekly virtual tutorials
- earn professional certification by completing weekly learning activities and mini-projects
This course should take approximately 4 – 6 hours per week. You can expect to devote about 1 – 2 hours per week to self-paced learning, 1 – 2 hours per week preparing for and participating in the webinar and 1 – 2 hours per week applying your knowledge through learning activities and mini-projects. Every webinar is recorded so you can rewatch it at any time.
Who should take this course?
This course will benefit all healthcare professionals who have an interest in person-centered care – including doctors, nurses, allied healthcare professionals and staff in administrative or managerial roles. It is an ideal course for established patient experience leaders who want to update and expand their knowledge and is also very suitable for staff who are aspiring to, or preparing for, future patient experience or service excellence roles.
About the certificates
Upon successful completion of the course you’ll receive an:
- IHLM Certificate of CPD Completion – This may be useful for course members who belong to professional bodies that have Continuing Professional Development requirements. The course has an estimated 60 hours of guided learning.
- IHLM Professional Certificate in Patient Experience and Service Excellence – This is evidence of the advanced patient experience capabilities you’ve developed during the course. The award of a professional certificate requires completion of learning activities and mini-projects during each module.
How to register
Ready to start? Just click the ‘Register now’ button at the top of this page or use the ‘Ask us a question’ button if you’d like to talk to one of our course facilitators. The fee for this course is £995 per person. If you’d like to pay in instalments you can arrange this by contacting us at: [email protected] .
We provide discounts to organisations registering 3 or more staff in the course and can also provide a customised in-house version tailored to your organisation’s specific needs.
All registrations are subject to our terms and conditions which are available here . By registering for an IHLM course you are accepting these terms and conditions and agreeing to be bound by them.
Module 1: What Is Person-Centred Care?
Gain an overview of the core concepts of patient experience and service excellence:
- how and why patients differ from other types of consumer
- why the attitudes and expectations of today’s patients are changing
- the role and importance of patient experience in healthcare quality
- what is person-centred care and how is it delivered?
Module 2: Leadership and Governance
Review the systems, structures and processes needed to develop and sustain person-centred care:
- the difficulties and challenges that leaders face in improving patient experience
- how healthcare providers build the foundations for excellence
- how to establish a patient experience office and team
Module 3: Educating, Engaging and Supporting Caregivers
Understand the fundamental role caregivers play in delivering person-centred care:
- how and why patient experience depends on employee experience
- factors affecting the motivation and engagement of caregivers
- strategies for improving caregiver well-being and reducing burnout
- how to help caregivers develop more person-centred practices and behaviours
Module 4: Using Design Thinking to Improve Patient Experience
Discover how design thinking can transform patient experience:
- what design thinking is and how it differs from other improvement methods
- what happens during each phase of the design thinking process
- qualitative techniques for observing and understanding patient experience
- using design thinking to generate solutions to patient experience issues
Module 5: Using the ‘Model for Improvement’ to Improve Experience
Use a scientific, evidence-based method to collect patient experience data and identity improvement opportunities:
- the purpose and value of patient experience data
- using the right metrics and Key Performance Indicators (KPIs)
- quantitative techniques for measuring and analysing patient experience
- using data to develop and test change ideas
Module 6: The Emotional Experience
Understand and improve the emotional experiences of patients, families and caregivers:
- what is meant by ’emotional experience’
- why the way we interact with patients matters so much
- researching and mapping patient’s emotional journeys during care
- improving patient communication using AIDET
- using HEART in service recovery
Module 7: The Clinical Experience
Discover why we must involve patients, to the extent they desire, in every decision that affects them:
- communication practices for actively involving and empowering patients
- assuring patient access to medical records and educational materials
- dealing with social, cultural and educational barriers to communication
- when and how to involve (or to limit the involvement of) family and friends
Module 8: The Functional Experience
Explore strategies for improving access to care, reducing waiting times and ensuring smooth transitions across service boundaries:
- why the functional experience is just as important as the emotional and clinical experiences
- how to identify opportunities to improve the functional experience
- analysing and redesigning the patient’s journey
Module 9: The Physical Experience
Appreciate how the design and layout of a healthcare facility affects healing and recovery:
- the role of the built environment in patient, family and visitor experience
- what the perfect healing environment looks and feels like
- evidence-based design of healthcare facilities
- standards for person-centred healthcare facilities
Module 10: The Digital Experience
Explore how digital healthcare applications can enhance or harm the patient experience:
- what is digital healthcare and how did Covid-19 accelerate its adoption?
- patient’s attitudes to and expectations of digital healthcare
- preserving and protecting patient experience during online care
- using digital health solutions to enhance patient experience

Course Leader

Benedict Stanberry
Course factfile.
- Duration: 10 weeks
- Commitment: 4-6 hours a week
- Qualification: Certificate
Location: Online
Find out more about Patient Experience and Service Excellence

More courses
Healthcare Leadership

Healthcare MBA Essentials
Our flagship course for high-potential healthcare leaders: built around the core strategic management disciplines and designed to prepare you for more senior roles and greater responsibilities.
Productivity and Value

Healthcare Operations and Patient Flow Management
This course will enable you and your healthcare organisation to achieve operational excellence by improving capacity, productivity and patient flow at every stage of care.
- Next Session: 26th June 2024

A comprehensive course for progressive healthcare providers and professionals who want to design and deliver more person-centred, compassionate and responsive care.
Quality and Safety

Patient Safety and Risk Management
Discover how to set up effective error reporting systems, lead investigations into adverse incidents, implement successful patient safety improvement projects and design safer systems of care.
Employee Experience

Healthcare Employee and Caregiver Experience
Discover how to support, engage and retain your healthcare workforce when you need them the most.
Healthcare Strategy

Healthcare Strategy, Planning and Execution
Using case studies from hospitals, clinics and healthcare systems, this programme shows you how to design and execute a strategic project or plan in a healthcare organisation.

Transforming Performance in the Operating Room
This course will enable you to accelerate your hospital’s post-pandemic recovery and implement proven strategies for transforming performance in the operating room.

High-Performance Healthcare Leadership
Aimed at first time healthcare leaders and those aspiring to their first leadership role, this programme will enable you to improve teamwork and take responsibility for people and services.
Digital Transformation

Digital Healthcare Transformation
This unique programme will benefit anyone who wants to understand the potential benefits of digital technologies in healthcare and how they can capture those benefits for their own organisation.

Healthcare Marketing and Medical Tourism
This programme provides you with practical tools for understanding patient needs and preferences, developing a marketing plan, building your healthcare brand and growing revenues.

Healthcare Financial Management, Productivity and Cost Control
This course gives you practical tools for making better financial decisions and maximising the financial performance of your healthcare organisation.

Developing and Leading Virtual Wards
This course is designed to enable healthcare teams and professionals to set-up and manage their own virtual wards or spread the virtual ward model across their health and social care economy.

Healthcare Quality and Performance Improvement
This course will enable you to master the concepts, methods and tools you need to lead successful quality improvement projects or become a quality improvement specialist.
Data Science and Analytics

Healthcare Data Analytics
This course is for anyone who wants to develop their data literacy, make more data-informed decisions and use data analytics to improve the quality and safety of care as well as the experience and satisfaction of patients.
What is a mini MBA and who is it for?
October 18, 2023
Pretty much everyone working in business or management has heard of the MBA degree. However, few healthcare leaders have the time, money or need for such a lengthy and expensive programme.
Her Majesty Queen Elizabeth II
September 8, 2022
IHLM is deeply saddened by the death of Queen Elizabeth II. Her Majesty was patron of more than 600 charities, many of them in the field of health and medical care.
Upcoming Courses
Course starts: 26 June 2024
Patient journey 101: Definition, benefits, and strategies
Last updated
22 August 2023
Reviewed by
Melissa Udekwu, BSN., RN., LNC
Today’s patients are highly informed and empowered. They know they have choices in their healthcare, which can put healthcare providers under a lot of pressure to provide solutions and meet their patients’ expectations.
Just like any customer, patients embark on a journey that begins before they ever contact the provider. This makes understanding the journey and where improvements can be made extremely important. Mapping the patient journey can help practitioners provide better care, retain a solid customer base, and ultimately identify ways to improve patient health.
- What is the patient journey?
The patient journey is best described as the sequence of experiences a patient has from admission to discharge. This includes all the touchpoints between the patient and provider from beginning to end.
The patient journey continues through consultation, where they meet the potential caregiver. That portion of the journey includes interactions with a doctor and support staff, how long they wait to be seen, and the steps taken for diagnosis and treatment.
The patient’s post-care journey includes follow-ups from the healthcare provider, post-treatment care, and billing. For example, if the patient has questions about post-surgery care or how to read their invoice, how quickly their questions are answered and their problems resolved will impact their satisfaction.
Mapping the patient journey helps healthcare providers improve patient satisfaction at every step of the way. By collecting data at each stage and conducting an in-depth analysis, providers can identify patient concerns and make the necessary improvements to meet their patient satisfaction goals.
What is another name for the patient journey?
The term “patient funnel” describes the journey patients take from first learning about a healthcare provider or healthcare product to actually making an appointment or purchase. This “funnel” can be applied to any type of business, describing the stages a customer goes through to obtain a service.
Get a demo from a Dovetail expert
Our team can give you a demo, help you choose the right plan and ensure you get the most out of Dovetail.

- Understanding the stages of the patient journey
Each stage of the patient journey is essential to a positive patient experience . Gathering and analyzing data can alert healthcare providers to potential issues throughout the journey.
Data collection at each of the following stages will give healthcare providers the information they need to make the necessary improvements:
1. Awareness
Awareness is where the patient journey begins. This is when they first research symptoms and identify the need to see a medical professional.
They may consider at-home remedies and get advice from friends, social media, or websites. Once they identify the need for a healthcare provider, they continue their research via review sites, advertising campaigns, and seeking referrals from friends and family.
Determining the way patients become aware they need healthcare and the sources they use for research is important. The data collected at this stage could suggest your organization has an insufficient social media presence, inadequate advertising, or a website in need of an update.
To remedy these shortcomings, you might consider adding informational blogs to your website, performing a social media analysis, or closely monitoring customer reviews.
This stage in the patient journey is where the patient schedules services with the healthcare provider.
This engagement is essential for acquiring new patients and retaining current patients. Patients will contact you in several ways to schedule an appointment or get information. Most will call on the first attempt to schedule an appointment.
This is a crucial touchpoint in the journey. A new patient may become frustrated and move on if they find it difficult to access your services or are placed on hold for a long period or transferred numerous times.
Patient engagement occurs in other ways, such as your online patient portal, text messages, and emails. Your patients may interact differently, so it’s important to gather data that represents their preferred means of communication. Work to make the improvements required to correct access issues and ensure efficient communication.
The care stage can include everything from your patient’s interaction with the front desk to how long they have to wait in the examination room to see a doctor.
Check-in, check-out, admissions, discharge, billing, and of course, the actual visit with the healthcare provider are other touchpoints in the care stage.
There are a couple of ways to gather and analyze this data. Most organizations choose to analyze it holistically, even if it’s collected separately. For example, you might gather data about the patient’s interaction with the front desk, the clinical visit, and the discharge process, but you may want to analyze the care segment as a whole.
4. Treatment
Treatment may be administered in the office. For example, a patient diagnosed with hypertension may have medication prescribed. That medication is the treatment. Gathering information at this stage is critical to see how your patient views the healthcare provider’s follow-up or responses to inquiries.
In most cases, treatment extends beyond the initial clinical visit. For example, a patient might require additional tests to get a diagnosis. Providing the next steps to a patient in a timely manner and letting them know the test results is crucial to patient satisfaction .
5. Long term
A satisfied patient results in a long-term relationship and referrals to friends and family. Most of the data collected at this stage will be positive since the patient is continuing to use your services.
Gathering data after the treatment stage allows you to expand on the qualities that keep patients returning for your services in the long term.
- Benefits of patient journey mapping
The patient benefits from their healthcare provider understanding their journey and taking steps to improve it. Healthcare providers also reap several benefits, including the following:
1. Efficient patient care
When they understand the patient journey, healthcare providers can provide care more efficiently and spend less time and money on unnecessary, unwanted communications.
2. Proactive patient care
Proactive patient care is aimed at preventing rather than treating disease. For example, women who are over a certain age should have an annual mammogram, smokers may be tested for lung disease, and elderly women may need a bone density study. These preventative measures can help keep disease at bay, improve health outcomes, and build trust with patients.
3. Value-based patient care
Patients don’t want to feel they are being charged unfairly for their healthcare. Focusing on the individual patient promotes satisfaction and yields positive outcomes.
The Center for Medicare and Medicaid Services (CMS) has issued recent guidelines for participants that help offset the costs of high-quality care through a reward system.
4. Retention and referrals
Patients who are happy with their journey will keep returning for healthcare, and happy patients equal voluntary referrals. Many providers offer rewards to incentify referrals.
- How to get started with patient journey mapping
Follow the steps below to start the patient journey mapping process:
Establish your patient personas
Journey mapping is a great way to identify your patient’s characteristics so that their experience can be further enhanced.
Some of the following determinations can help you pinpoint your patient’s persona and establish protocols to provide a better service:
How do your patients prefer to communicate? Are they more comfortable with phone calls, texts, or other methods?
How are most patients finding your services? Are they being referred by friends or family members, or are they seeing advertisements?
Would the patient prefer in-person communication or telecommunication?
What are the patient’s expectations of care?
This data can be complex and widespread, but it can give you the information you need to more effectively and efficiently communicate with your patients.
Understand the entire patient lifecycle
Each patient is unique. Understanding the patient lifecycle can avoid confusion and miscommunication.
To positively engage the patient, you’ll need to gather data not only about communication methods but where they are in the patient journey, their health issue, and their familiarity with the healthcare provider’s procedures and treatment options.
Understand the moments of truth
With a few exceptions, most people seek healthcare services when they are ill or have a healthcare issue. These situations can cause patients to feel stressed and anxious. It’s these moments of interaction where compassion, knowledge, and understanding can provide relief and reassurance.
When patients see their healthcare provider, they are looking for solutions to problems. It’s the provider’s opportunity to identify these moments of truth and capitalize on them.
Get the data you need
Healthcare providers can collect vast amounts of data from patients, but the data collected rarely goes far enough in analyzing and determining solutions.
Your patients have high expectations regarding personalized treatment based on data. They want personalized, easy access to medical information and records, responsive treatments and follow-up, and communication in their preferred format.
You need more than clinical data to give patients what they want. You also need personal data that sets each patient apart and ensures a tailored experience.
For example, it might be challenging for parents of small children to contact the clinic and schedule appointments at certain times of the day. As a healthcare provider, you’ll need to be aware of the best times to contact this individual and offer simple methods for scheduling appointments.
Another example is patients with physical disabilities. You can take steps to improve their access to and experience at the healthcare facility.
Encourage referrals and loyalty
Although engagement on social media and online forums is becoming more and more common, the best way for new patients to find you is through referrals. Referrals stem from satisfactory experiences and trust.

Should you be using a customer insights hub?
Do you want to discover previous research faster?
Do you share your research findings with others?
Do you analyze patient research?
Start for free today, add your research, and get to key insights faster
Editor’s picks
Last updated: 23 August 2023
Last updated: 22 July 2023
Last updated: 11 September 2023
Last updated: 10 October 2023
Last updated: 16 November 2023
Last updated: 12 October 2023
Last updated: 25 November 2023
Last updated: 3 July 2023
Last updated: 27 January 2024
Last updated: 27 November 2023
Last updated: 17 January 2024
Latest articles
Related topics, .css-je19u9{-webkit-align-items:flex-end;-webkit-box-align:flex-end;-ms-flex-align:flex-end;align-items:flex-end;display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-flex-direction:row;-ms-flex-direction:row;flex-direction:row;-webkit-box-flex-wrap:wrap;-webkit-flex-wrap:wrap;-ms-flex-wrap:wrap;flex-wrap:wrap;-webkit-box-pack:center;-ms-flex-pack:center;-webkit-justify-content:center;justify-content:center;row-gap:0;text-align:center;max-width:671px;}@media (max-width: 1079px){.css-je19u9{max-width:400px;}.css-je19u9>span{white-space:pre;}}@media (max-width: 799px){.css-je19u9{max-width:400px;}.css-je19u9>span{white-space:pre;}} decide what to .css-1kiodld{max-height:56px;display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-align-items:center;-webkit-box-align:center;-ms-flex-align:center;align-items:center;}@media (max-width: 1079px){.css-1kiodld{display:none;}} build next, decide what to build next.

Users report unexpectedly high data usage, especially during streaming sessions.

Users find it hard to navigate from the home page to relevant playlists in the app.

It would be great to have a sleep timer feature, especially for bedtime listening.

I need better filters to find the songs or artists I’m looking for.
Log in or sign up
Get started for free
Understanding the patient journey Masterclass: MDD and PTSD
Trauma has enduring effects on our mental health, social functioning, and relationships. Post-Traumatic Stress Disorder (PTSD) and a more recent diagnostic category, Complex PTSD, are indicative of this impact. This 1.5-day course draws on expertise from the Maudsley Hospital, employing interactive, case-based learning to facilitate an understanding of the perspectives of both service users and clinicians operating in this domain.
The first day commences with an exploration of PTSD's pathogenesis, followed by an expert-led session on trauma-focused and non-trauma-focused treatments. These approaches are illustrated through a simulated patient, elucidating key concepts and techniques. Later in the morning, an expert session delves into the role of sleep in PTSD, emphasizing the repercussions of disrupted sleep on well-being and offering strategies for improvement. The afternoon segment delves into the distinction between PTSD and Complex PTSD, and an in-depth grasp of the clinical interpretation of "trauma," particularly in relation to diagnostic criteria, is fostered. Throughout the day, ample question and answer sessions are interspersed to address queries arising during the presentations.
The second day initiates with an appraisal of the signs and symptoms of Major Depressive Disorder (MDD), progressing to an expert-led discussion on combination treatments for cases where Selective Serotonin Reuptake Inhibitors (SSRIs) fail to alleviate symptoms. Additionally, an expert patient leads a session, sharing their personal experiences with illness and treatment. The course concludes by affording attendees the space to reflect upon the knowledge and insights garnered throughout the program.
At the conclusion of this course, learners will have the capability to:
Major Depressive Disorder (MDD)
- Describe the typical patient journey in the diagnosis and treatment of MDD in real-world practice.
- Recognize the role of anxiety in making treatment decisions for MDD.
- Understand the decision-making process for initiating the first combination therapy.
- Comprehend the common treatments employed in MDD, encompassing both pharmacological and non-pharmacological approaches, as observed in real-world practice.
- Describe the typical patient journey in the diagnosis and treatment of PTSD within real-world practice.
- Identify the significance of factors such as trauma type, sleep, and anxiety in treatment planning.
- Grasp the role of psychological therapy in managing PTSD, contrasting its application in real-world practice with guideline recommendations.
Course schedule
Group bookings.
Discounted rates are available for group bookings. Please contact us for more information. Maudsley Learning has a full range of courses to meet the needs of your organisation. Most can be delivered to you flexibly and tailored to your requirements.
Bespoke courses
We are able to offer custom-made programs, whether digital or face to face, to meet the education and training needs of your organisation in the UK or internationally.
We value research and knowledge-sharing and will continue to contribute to the literature base on mental health education, addressing important research questions in this exciting field.
Latest news, podcasts and blogs

NHS England and Maudsley Learning collaborate to enhance mental health education for physician associates

Stress in University Students: Empowering Students to Take Control

EP7 - Professor Sir John Strang (Confessions of an English opium eater by Thomas de Quincy)
Cookie message

The Patient Journey: What it is and Why it Matters

- Share on Facebook
- Share on Twitter
- Share on LinkedIn
- Share on Email
Healthcare is under enormous pressure today.
Patient expectations about their service and experience have changed over the years. Patients have more choices about their care, and they’re more empowered with information about what they want their care experience to be. They expect you to interact with them on their terms, not yours. And with COVID-19 turning so much of our lives digital, this trend has only accelerated.
Having a robust marketing automation approach is critical to addressing these challenges in today’s environment. Meeting — and exceeding — patient expectations comes down to managing your patient’s engagement journey.
How can patient journeys improve care?
What patient journeys can do is turn the healthcare experience from a primarily reactive experience to a proactive one.
By building out journeys for your patient personas, you can close gaps in care, establishing robust preventative routines that ultimately help your patients stay as healthy as possible for as long as possible.
Engaging consumers and patients where they are builds trust and confidence that keeps patients in the system and encourages them to refer their friends and family to your practice. According to the Beryl Institute , 70% of patients will share a positive experience with others. But your bigger risk is that 76% will share a negative one. And with a negative experience, 43% of patients won’t go back to that provider, with 37% finding a different doctor altogether.
What is the patient journey?
A patient journey represents the entire sequence of events that a patient experiences within a given healthcare system or across providers, from scheduling an appointment for a regular checkup to receiving treatment for an illness or injury.
A patient journey is an ongoing process that incorporates all parts of the healthcare ecosystem, from hospitals to physicians, specialty care, and outpatient therapy.
While it is easy to think about a patient’s journey as those interactions you have with them before, during, and after an appointment, there are actually many other touchpoints that drive their overall journey. A comprehensive patient engagement strategy touches on all aspects of a patient’s relationship with a healthcare provider, including:
- Onboarding and Access
- Diagnosis and Treatment
- Adherence to Lifestyle or Behavioral Changes
- Ongoing and Proactive Health (Wellness)
- Referrals and Loyalty
How do I create the patient engagement journey?
Every single interaction with a patient is part of the patient engagement journey and a moment of truth for the health system or provider to add value.
In today’s value-based healthcare world, having that personalized experience is more important than ever. A patient engagement journey organizes those communication touchpoints and ensures you’re delivering the right information at the right time to the right person, and leveraging the appropriate communication channel. Millennials and Generation Z, for example, may be more likely to prefer a text, email, or chat to a phone call.
It’s about knowing your patients’ preferences — like that they prefer to be texted during the day while they’re at work or if they prefer an office vs. telehealth visit — and what’s going to make it easier for them, like sending automatic reminders the week and day before an appointment.
Whether it’s making sure you follow up with cardiac patients about weighing themselves daily after surgery to catch any water retention issues or asking colonoscopy patients whether or not they’ve been following post surgery protocols after discharge, it’s about continuity of care once a patient leaves the office or hospital so they have a quality outcome. From there, patients can more proactively drive their own wellness plan.
Here are important areas to focus on when creating your patient engagement journey:
Establish your patient personas
You need to know the different types of patients that are coming into your organization. You want to figure out:
- What are the most relevant needs of your patients?
- What are their communication and care preferences?
- How do they want to engage with you?
- What information do you already know about them?
To be able to craft the best possible patient experience, you first have to know more about your patients.
For example, there’s a well-known healthcare persona out there called the “Medical Mom” (which can, of course, be any individual taking care of themselves, their kids, their spouses, and may also be the caretaker for aging parents).
Let’s say this individual has three children, and they book annual physicals at their pediatrician, which happens to have offices in the same building as their own primary care physician. Wouldn’t it be nice if the office sent them one email reminder to schedule all five appointments, rather than five different emails? And when they do call, scheduling those appointments back-to-back so everyone is in and out in one afternoon?
A spreadsheet is not going to be able to do that for you. Collecting and managing the data required to drive complex, interconnected patient journeys requires more than a spreadsheet. In order to succeed, you’ll need to pay close attention to the entire patient lifecycle.
Understand the entire patient lifecycle
An appointment reminder is a great start to engaging a patient, but it’s just one event in an ongoing patient lifecycle that begins with preventative care and includes diagnostics, delivery of care, and post-operations.
For example, how many patients show up for routine blood work at their physician office and you find out they haven’t fasted for the appropriate amount of time? Sending a patient home is frustrating for them and it’s frustrating for you. If the appointment is at 2:00 PM, then that appointment reminder should have been sent at dinnertime the previous evening, reminding them that they can’t eat anything after a 6:00 AM breakfast the next morning.
You’ll want to tailor your communications based on whether the patient is new or existing, what their preferences are, and whether they have any specific or chronic health issues. From there, you need to…
Understand the moments of truth
The healthcare system is complicated, even for those who have been a part of it for decades. The key to building a great foundation for your patient engagement strategy is to put yourself in a typical patient’s shoes. Most patients don’t engage with the healthcare industry unless they’re feeling sick. That means they’re rarely at their best, and they’re not only anxious about getting better, but about the costs associated with that.
The best healthcare providers understand the moments of truth — opportunities for a positive touchpoint that can alleviate their stress and anxiety and help them get on the road to recovery. Every time you interact with a patient is an opportunity for a moment of truth, whether that be in person or via other channels of communication. It’s not only about establishing accurate moments of truth, but capitalizing on them.
It’s up to you to understand the places people need to be, how you want to communicate to them, and make every one of those touchpoints a positive experience. It doesn’t matter whether they’re physically in your office or not. Your patient engagement journey is what guides your patients to making the best possible decisions on their care so they get better.
The easier you make it for them to engage with you, the higher quality their care will be. Ultimately, you want your patients to be evangelists for your services based on their positive experiences. To do that, you’ll need to…
Get the data you need
Your patients expect personalization.
Personalization in healthcare used to mean created tailored treatment plans and clinical protocols. That’s still important, but patients expect more personalization around the entire experience, from access to communication to quality outcomes. It’s like turning on a light switch in your home: a patient just expects the light to turn on.
Personalization today means being able to see at-a-glance a patient’s healthcare record, communication preferences, and social determinants that may be impacting their overall health to give you a 360-degree picture .
To do this, you need more than clinical data.
You may have patients that constantly miss their appointments. By storing questions that go beyond health risks — say, that they’re a smoker — but to understand that they don’t have a car to get to the appointment in the first place is becoming a more important part of the process. Part of empathetic, compassionate care is understanding these environmental factors that can help patients get the care they need, whether that’s calling a Senior Shuttle, caregiver, or arranging a telehealth appointment instead.
Once you have the data, you can…
Encourage referrals and loyalty
The first place people look for a new doctor isn’t the Internet. It’s their friends and family. In an ideal world, every patient you have should be able to say, “Oh, I loved my experience with…”
Doing that starts with the technology you have. Before a patient ever comes in for treatment, you need to make sure they have a seamless experience that builds trust and encourages referrals and loyalty.
How do I get started with patient journey mapping?
It’s time to move away from the mindset to simply fill the top of the funnel with as many new potential patients and contacts with caregivers as possible. While this is still a requirement, it is just as crucial for organizations to get better at managing and growing relationships at every phase of the patient journey. Providers must engage with consumers in the marketplace to introduce them to their services of course, but it is of growing importance that they offer support throughout the entire diagnostic and treatment process.
As a Salesforce Platinum Partner with deep industry expertise, we have created a Foundation for Patient Engagement package — a complete strategy that starts with Health Cloud and facilitates a 360-degree view of the patient , as well as a comprehensive communication strategy, CTI integration, and the use cases driving patient acquisition, engagement, and loyalty.
Learn more about building your patient journey with Silverline.
From the Blog More articles about Provider

Provider Personalization in Healthcare: 6 Keys To Successful Patient Experiences

Provider Prioritize Patient Experiences with EHR CRM Integration

Provider The Future of AI for Healthcare Providers
We don't support internet explorer.
Please use Chrome, Safari, Firefox, or Edge to view this site.
- Skip to main content
- Skip to primary sidebar
- Skip to footer
- QuestionPro

- Solutions Industries Gaming Automotive Sports and events Education Government Travel & Hospitality Financial Services Healthcare Cannabis Technology Use Case NPS+ Communities Audience Contactless surveys Mobile LivePolls Member Experience GDPR Positive People Science 360 Feedback Surveys
- Resources Blog eBooks Survey Templates Case Studies Training Help center
Patient Journey Mapping: What it is, Benefits and 5 Steps to Do it

In the rapidly evolving landscape of healthcare, patient-centered care has emerged as a crucial paradigm shift. As hospitals strive to deliver exceptional patient experiences and improve outcomes, understanding the patient journey has become paramount.
A customer journey map is a powerful tool that shares patients’ path from their first encounter with a healthcare facility to their final discharge. By visualizing this complex expedition, hospitals can gain invaluable insights into patient needs, pain points, and opportunities for enhancement, thereby revolutionizing the delivery of care.
The following article delves into the significance of patient journey maps for hospitals and their importance in optimizing patient experiences, streamlining processes, and ultimately elevating the standard of healthcare.
What is a Patient Journey Map?
A patient journey is a methodology that enables the analysis of a healthcare provider’s processes and value chain but from the patient’s viewpoint. This includes their possible solutions, pain points, emotions, touchpoints and user actions throughout the journey.
The patient journey map employs visual representation to gain deeper insights into how patients engage with a healthcare facility throughout their care journey. This unique approach is an evolution of the customer journey map , tailored specifically to the healthcare context. By employing this method, healthcare providers can unravel the intricacies of patient interactions, uncovering valuable information to enhance the quality of care provided.
The concept of the Patient Journey Map mirrors that of the Customer Journey Map, seeking to uncover areas of enhancement in patient care across various healthcare providers, including hospitals, fertility centers, and more.
Just as a skilled cartographer carefully crafts a map to navigate uncharted territories, patient journey maps chart the course of a patient’s experience, revealing hidden insights, unveiling opportunities for improvement, and ultimately guiding healthcare providers toward a destination of unparalleled patient satisfaction .
What are the benefits of implementing a Patient Journey Map?
Engaging in the patient journey proves immensely valuable as it enables us to provide patients with an optimal experience, meeting the very expectations that arise when seeking healthcare services.
The emotional aspect tied to the Patient Journey Map can be profoundly impactful, considering the inherent uncertainties often associated with visiting a healthcare facility.
Considering the unique personalities, fears, behaviors, and attitudes of different patient archetypes play a pivotal role in creating a tailored and pleasant experience for them. Thus, the patient journey map becomes a valuable tool benefiting both patients and healthcare service providers.
● Enhanced Communication with Patients:
By understanding the patient journey, healthcare providers can establish effective and continuous communication throughout the entire care process, addressing any doubts or uncertainties. Keeping patients well-informed and updated through appropriate channels reinforces the quality of care provided.
● Elimination of Blind Spots:
Clear comprehension of each stage of the patient journey helps bridge the gaps between patients and services. From the initial appointment request to discharge and follow-up, identifying and addressing potential blind spots ensures consistent and satisfactory solutions tailored to each patient’s unique situation.
● Streamlined Resolution of Pain Points:
Mapping the patient journey and defining archetypes enables a deeper understanding of patient concerns, particularly identifying which aspects of the service have the most negative impact. Pain points such as waiting times, unclear explanations, lack of empathy, or impersonalized treatments can be simplified and resolved more effectively.
Learn About: Complaint Resolution
● Process Optimization:
A well-defined patient journey optimizes workflow and allows for more efficient handling of all processes. Staff members become better equipped to anticipate and address patient issues promptly, offering alternatives that instill confidence and satisfaction.
● Continuous Improvement:
Implementing a Patient Experience model involves measuring patient experiences through a feedback system . Continuously updating the database with relevant information about patient journeys and their experiences leads to ongoing improvement in response times, customer service processes, and overall service quality .
What is a Patient Persona?
The patient persona represents an imaginary profile that encapsulates potential patients’ needs, goals, illnesses, conditions, emotions, behaviors, and knowledge.
By creating patient personas, healthcare providers can enhance the accuracy and anticipation of care and diagnosis processes, ultimately improving the experience of individuals seeking healthcare services.
5 Steps to Build Your Own Patient Journey Map
1. define the experience to map:.
Before diving into the Patient Journey Map, it is crucial to determine the specific experience you intend to outline. By establishing your objectives and identifying the type of information you seek to gather and how it will be utilized, you can ensure a more efficient mapping process right from the start.
2. Identify your Ideal Patient:
The majority of data used to construct the customer patient care journey will come directly from patient-clients. Thus, a key step is identifying the patient persona, which can be singular or multiple. You must decide whether the map will encompass various patient profiles or if separate maps will be created for each target patient.
To create the patient persona(s), gather feedback directly from patients and analyze their behaviors and data. Pose questions such as:
- What initially led the patient to seek your services?
- Which competitors did they research?
- How did they discover your website or company?
- What factors differentiated your brand from others? What influenced their decision (or lack thereof) to choose your services?
- What are their expectations when interacting with your company?
- Can they articulate what they appreciate about your company and what frustrates them?
- Have they ever contacted customer service? If so, how was their experience?
Once you have defined the patient persona(s), you can identify the distinct stages of the customer journey when engaging with your company.
3. Divide the Phases of the Customer Journey:
Throughout the customer-patient care journey, patient-clients progress through several discernible stages.
Phase #1: Pre-Visit
● DISCOVERY:
The patient journey initiates with a phase characterized by learning and concern. Patients embark on their healthcare journey upon recognizing a need or developing a concern related to a health issue.
For instance, if an individual experiences symptoms associated with being overweight, they may begin researching options for scheduling an appointment with a medical specialist. At this point, potential patients discover their specific needs and commence the process of investigating suitable solutions. They may turn to the internet, seek recommendations from friends and family, or explore other avenues. During this stage, it is recommended healthcare systems should provide educational support to aid individuals on their journey of understanding.
● CONSIDERATION:
Following their research, patients reach the consideration stage, having discovered your service. At this point, they possess some knowledge about your healthcare facility’s location and offerings, leading them to believe it could meet their needs. However, patients have also explored your competitors and are contemplating multiple options.
During the consideration stage, potential patients meticulously assess the information they come across, including service descriptions, pricing, contact pages, online inquiries, and reviews. They also evaluate the ease of accessing relevant information before scheduling an appointment and the availability of operating hours, among other factors.
Phase #3: Visit
● APPOINTMENT & ENGAGEMENT:
Having gathered sufficient information and progressed through the consideration phase, the patient ultimately chooses your service. This marks their first contact with the health center, which can occur in person, over the phone, via chat, email, or other means of communication.
During this stage, the patient schedules their appointment. The company must streamline the application process and maintain effective and proactive communication. It is crucial for this phase to be completed without complications.
● SERVICE DELIVERY:
Within the visit phase is the service delivery stage, where patients interact with various service providers at the health center. From the moment the patient enters the premises, the company must ensure an exceptional service experience.
Service delivery encompasses multiple micro-moments, necessitating comprehensive attention throughout the entire journey. Every interaction matters, from the reception care and waiting times to the core service itself—meeting the patient’s objective of being evaluated by a doctor or specialist.
Phase #3: After the Visit
● RETENTION:
The Patient journey doesn’t conclude after the initial visit. A crucial third phase occurs post-encounter, where efforts should be dedicated to fostering patient retention and encouraging their return for subsequent visits. Building strategies that monitor the patient experience is essential in designing loyalty programs to ensure patients return for future services.
● RECOMMENDATION:
Part of the post-visit phase involves patient recommendations, which heavily depend on the overall patient journey experience provided by the company. If patients have had a positive service encounter, they are likely to recommend it to others, benefiting your business.
However, it is important to remember that negative experiences are equally shared, and if patients are dissatisfied, they may spread negative feedback.
Promptly addressing any negative comments is crucial to resolving issues and preventing unfavorable recommendations.
Phase #4: Identify Touchpoints
An additional vital step in mapping the customer-patient care journey is identifying the various touchpoints between the patient and the healthcare facility. These interactions occur at different stages throughout the patient journey, and understanding these touchpoints aids in developing strategies that facilitate effective communication.
- Seeking information about healthcare centers: discovering the existence of the healthcare provider and the services it offers.
Investigation:
- Reviewing patient-client feedback: researching comments and feedback from other patients about their visit experiences at the health center.
- Exploring promotions: searching for economic benefits such as discounts, promotions, and bundled service packages.
Acquisition :
- Appointment Request: Contact or visit the health center to schedule an appointment.
- Provision of Personal Data: The health center will request personal information to finalize the appointment booking.
- Appointment Confirmation: After providing the required data, the appointment for the agreed date and time is confirmed.
- Patient Reception: The patient arrives at the health center at their scheduled appointment time.
- Waiting Room: The staff guides the patient to the designated waiting area.
- Consultation: The patient’s turn to be attended by the specialist.
- Payment: The process of settling the payment for the service, which may occur at any point during the service phase, depending on the health center’s policies.
- Patient Recommendations: Patients offer positive or negative feedback about the health center and its services.
- Loyalty Program: Incentives such as offers, promotions, discounts, or a points system to encourage future visits.
Recommendation:
- Complaint: If the patient has had a negative experience, they may file a complaint with the health center.
- Online Reviews: Patients share comments or criticisms about the service by posting reviews on the internet.
4. Identify Contact Channels
Patients engage with the health center through various channels throughout the patient journey. These channels, such as the health center itself, can be physical or online, including social media, email, applications, websites, and online forms.
Identifying the most utilized contact channels at each stage of the customer-patient care journey is crucial. This allows for the development of tailored strategies for each channel, meeting patient expectations at each phase.
Working on the patient journey is crucial for healthcare providers to deliver a high-quality experience to patients. By mapping their interactions, providers gain a deeper understanding of their patient personas, allowing them better to comprehend patient needs, desires, and circumstances to provide the desired care.
You can explore Patient Experience Software to measure your patient journey. QuestionPro published a blog about it very recently!
Patient Journey Map Example
To better understand what a Patient Journey Map is, we have created this fictitious example using one of the most reputable medical institutions in the healthcare sector, the Massachusetts General Hospital, as a reference.
In this example, we have included some generic touchpoints that are usually the most common in the interaction between a hospital and a patient.
Through this example, it would be possible to visualize the points of interaction between both parties and the perception that patients have of them, which can be positive or negative. This serves as a clear indicator for making adjustments and learning from what has been done well.
The Office of Patient Experience plays a vital role in facilitating initiatives to assess and enhance the quality of care experienced by patients and their families. They are responsible for evaluating each of these touchpoints and ensuring that appropriate actions are taken.
The Mass General Hospital is a benchmark not only in terms of service level but also in the implementation of methodologies and actions that guarantee the satisfaction of their patients. A clear example of this can be seen in the results of their annual HCAHPS survey, where they score above the national average in various aspects.
Willingness to Recommend Hospital Scores below show the percentage of patients who would “definitely recommend” Mass General to their friends and family.
To see the complete study, we invite you to visit their website and learn about it.
More Examples of Patient Journey Maps
Seeking inspiration to craft your own Patient Journey Map? Your search ends here!
Explore a collection of remarkable examples from top-notch brands, unveiling their initiatives that delight customers and foster loyalty.
Get set to revolutionize your own Patient Journey!
Mass General Hospital is renowned for providing exceptional care and taking special care in understanding the perspective of its patients. They achieve this through different tools, such as satisfaction surveys, internal and external feedback, and HCAHPS surveys .
Mayo Clinic is characterized by its focus on patient satisfaction and its extensive technical deployment to gather user and prospect feedback.
Cleveland Clinic is often ranked among the best hospitals in the United States. This recognition is not only due to its incredible facilities, global expansion, and well-prepared staff but also because of its remarkable focus on the experience they provide to its patients and clients.
Singapore General Hospital is one of the largest and oldest hospitals in Singapore. It has been a major healthcare institution providing a wide range of medical services and treatments since 1821.
Johns Hopkins Medicine has long recognized the significance of a positive patient and family experience during hospitalization, which is why they maintain a specific focus on patient satisfaction to achieve an optimal experience.
How can you enhance your Patient Journey Map based on your acquired knowledge?
The insights and recommendations shared above are likely to have sparked ideas about the potential impact of these initiatives across various industries, not just healthcare.
The first crucial step is to embrace a customer-centric approach, keeping their needs and expectations at the forefront. By doing so, the actions you take will have a meaningful impact on your customers and yield multiple benefits for your business.
At QuestionPro, we offer a range of tools and features specifically designed to help you achieve this objective.
QuestionPro SuiteCX is a Customer Journey Mapping Software that simplifies the process of creating your customer journey.
With a vast selection of templates and the ability to personalize user/buyer personas while incorporating your own data, you can conduct precise visual analyses at every touchpoint throughout your patient journey.
Start delighting your customers today!
MORE LIKE THIS

AI-Based Services Buying Guide for Market Research (based on ESOMAR’s 20 Questions)
May 20, 2024
Data Information vs Insight: Essential differences
May 14, 2024
Pricing Analytics Software: Optimize Your Pricing Strategy
May 13, 2024

Relationship Marketing: What It Is, Examples & Top 7 Benefits
May 8, 2024
Other categories
- Academic Research
- Artificial Intelligence
- Assessments
- Brand Awareness
- Case Studies
- Communities
- Consumer Insights
- Customer effort score
- Customer Engagement
- Customer Experience
- Customer Loyalty
- Customer Research
- Customer Satisfaction
- Employee Benefits
- Employee Engagement
- Employee Retention
- Friday Five
- General Data Protection Regulation
- Insights Hub
- Life@QuestionPro
- Market Research
- Mobile diaries
- Mobile Surveys
- New Features
- Online Communities
- Question Types
- Questionnaire
- QuestionPro Products
- Release Notes
- Research Tools and Apps
- Revenue at Risk
- Survey Templates
- Training Tips
- Uncategorized
- Video Learning Series
- What’s Coming Up
- Workforce Intelligence
The Patient Journey
- Open Access
- First Online: 15 December 2020
Cite this chapter
You have full access to this open access chapter

- Elena Beleffi 5 ,
- Paola Mosconi 6 &
- Susan Sheridan 7
42k Accesses
2 Citations
The wide implementation of patient safety improvement efforts continues to face many barriers including insufficient involvement of all stakeholders in healthcare, lack of individual and organizational learning when medical errors occur and scarce investments in patient safety. The promotion of systems-based approaches offers methods and tools to improve the safety of care. A multidisciplinary perspective must include the involvement of patients and citizens as fundamental contributors to the design, implementation, and delivery of health services.
The patient journey is a challenging example of using a systems approach. The inclusion of the patient’s viewpoint and experience about their health journey throughout the time of care and across all the care settings represents a key factor in improving patient safety. Patient engagement ensures that the design of healthcare services are aligned with the values, the preferences, and needs of the patient community and integrates the real-life experience and the skills of the people to enhance patient safety in the patient journey.
The utmost priority to implement patient engagement is the training of patients. Therefore, training for both patients/families/advocates and health professionals is the foundation on which to build active engagement of patients and consequently an effective and efficient patient journey.
The chapter offers examples of successful training courses designed to foster strategic alliances among healthcare professionals and researchers with patients and their organizations. Training of patients constitutes the first step to develop shared knowledge, co-produced projects, and the achievement of active multilevel participation of patients for the implementation of patient safety in the patient journey.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others

Patient Experiences of Safety in Care Transitions
Top 10 interventions in paediatric patient safety.

‘The big buzz’: a qualitative study of how safe care is perceived, understood and improved in general practice
- Patient journey
- Patient engagement
- Patient empowerment
- Patient safety
- Healthcare ergonomics
- Co-production
- Knowledge creation
1 Introduction
Almost 20 years after publication “To Err is Human: Building a Better Health System” (Kohn et al. 1999), patient safety is still not widely implemented. This report from the Institute of Medicine is the milestone that constituted a turning point for improving quality of care and patient safety identifying the need to rethink healthcare delivery to provide safe, effective, and efficient care.
The barriers of implementing patient safety as a driving force for change towards more effective healthcare include multiple factors: insufficient involvement of all stakeholders contributing to the care process, lack of willingness of organizations and individuals to learn from errors and scarce investments in patient safety improvement and research.
There is a growing need to promote systems approaches to finding solutions in healthcare to improve the safety of care, the quality of healthcare delivery, patients’ health and citizens’ well-being.
The discussion paper “Bringing a Systems Approach to Health” defines the systems approach as one “that applies scientific insights to understand the elements that influence health outcomes; models the relationships between those elements; and alters design, processes, or policies based on the resultant knowledge in order to produce better health at lower cost” [ 1 ].
A multidisciplinary approach must include the involvement of citizens and patients as fundamental contributors to the design, implementation, delivery, and evaluation of health services.
This means that citizen participation plays an essential role, bringing the unique point of view of patients and family members into the debate on patient safety and quality of care.
Patients and more generally citizens, when actively and systematically engaged, bring ideas and experiences which can support a collaborative and reciprocal learning process among the healthcare stakeholders. This produces knowledge that leads to improved practices, a real knowledge creation process where the dynamic participation of all actors in healthcare systems contribute to an active learning environment where the identification, the investigation, and the planning of solutions related to health incidents is a cyclic process enabling healthcare knowledge creation.
The added value of involving patients in healthcare is, respect to other more complex interventions, a low cost opportunity to take into consideration unconventional points of view creating and building knowledge and providing original insights and ideas that otherwise would not be considered.
Health professionals and patients’ skills and knowledge are acquired through individual experience or education and transferred to the health organizations in a perspective of co-production of healthcare. It is a merging of the efforts of those who produce and those who use the solutions to address health problems. It serves to establish a strengthened and long-term relationship in terms of trust and effectiveness and to distribute the responsibilities among all stakeholders [ 2 ].
In light of these arguments, the systems approach—inspired by the fundamentals of ergonomics and human factors (HFE)—creates new alliances between healthcare and engineering, of which patient journey is a challenging example [ 3 ].
Applying the systems approach to patient safety allows the analysis of the factors that characterize the encounters and the interactions between healthcare professionals and patients during the entire course of care. The observation of possible critical issues to the individual and specific encounter between clinician and patient is crucial in widening the scope of observation and research of the entire “journey” of the patient, taking into consideration the complexity of patient, their values and needs, their preferences, the economic and social context in which they live, and language and communication issues.
These observations and research should be carried out considering the interconnections and interactions together with the components of the processes; importance should be given to the context, and to manage the complexity, the value of a holistic approach.
2 The Patient Journey
A modern health system looks to the future in the context of the challenges imposed by the real world. It must manage the gap between guidelines and health protocols and what effectively happens and how reality is perceived by patients and family members.
It is more and more necessary to bring the patient’s point of view in the analysis of the care process, in the incident reporting and analysis, in the design and implementation of solutions and guidelines in healthcare.
Vincent and Amalberti in “Safer Healthcare” (2016) [ 4 ] stated that the incident analysis should broaden the class of events having consequences on patient safety. Incidents reported from the patient’s point of view should be included in addition to those suggested by health professionals. Additionally, when analyzing an incident, it should be done in the context of the patient journey rather than a single episode.
Instead of focusing on the individual encounter, it is necessary to extend the observation timeframe by applying the examination of contributing factors to each of the encounters that compose the patient journey (temporal series of encounters with healthcare facilities, a hospital unit, a specialist visit, a primary care clinic, a home health agency), considering both the negative and positive events and the points for improvement that were revealed (Fig. 10.1 ).
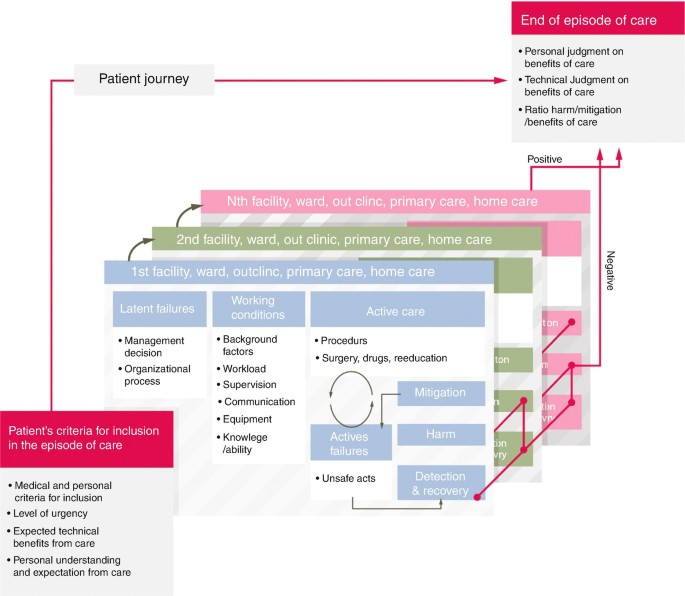
Analysis of safety along the patient journey
The adoption of this wider approach is unique in that it incorporates the patient’s perspective of safety and includes new features in the incident analysis such as asking patients to recount the episode of care, including patient and family in the investigation team when possible, asking patients the contributory factors from their point of observation and perception and involving patients and families in the reflections and comments on the disclosure process [ 4 ].
The episodes patients and families can highlight are often different from those that professionals are more accustomed to reporting. However, patients could be involved in further ways in incident reporting and assessment, and today patient-derived information constitutes a free and little used resource.
As per McCarthy’s definition, “patient journey mapping describes the patient experience, including tasks within encounters, the emotional journey, the physical journey, and the various touch points” [ 5 ]. Carayon and Woldridge define “patient journey as the spatio-temporal distribution of patients’ interactions with multiple care settings over time” [ 3 ], where at each point of touch with each healthcare service along the patient journey, the patient interacts with several system elements (task interaction, physical environment, interaction with tools and technologies, organization interaction, interaction with other organizations and other people, interaction with other people and teams within the organization) (Fig. 10.2 ).
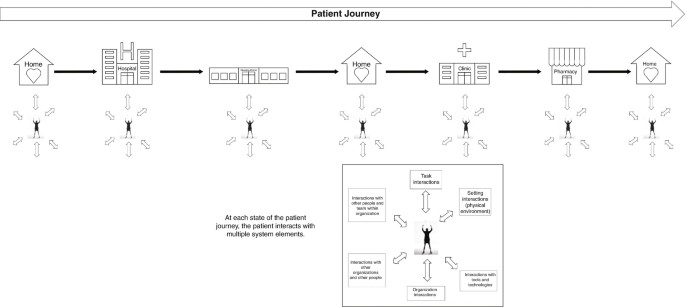
The patient journey as a set of interactions and transitions
The patient journey represents the time sequence of what happens to the patient, especially during transitions of care, in particular considering that the health professional who takes care of the patient only sees the portion of care for which he is responsible and in which he has an active role. Conversely, the patient is the only person who has a continuously active and first-hand role during their health journey. They alone are in possession of information that characterizes the entire care experience.
Moreover, when patients navigate their journey, they contact and interface with multiple work systems at several time points, where the sequence of interactions in the work systems determine the outcome experienced by patients and families, healthcare professionals, and health organizations. (Fig. 10.3 ). Each local work system is influenced by a wider socio-organizational context, which can be formal healthcare organization (such as hospital, primary care facility, nursing home) or informal (home).
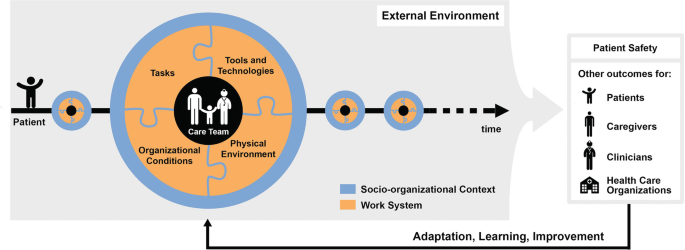
SEIPS 3.0 model: sociotechnical systems approach to patient journey and patient safety
Every point of the patient journey offers data on health outcomes and patient experience outcomes that should be used as feedback to redesign healthcare work systems in terms of adaptation, learning, improvement.
Patient’s experience represents an important resource in participatory collaborative design, especially in the patient journey where this experience is the result of multiple interactions across space and time.
3 Contextualizing Patient Safety in the Patient Journey
Many of the incidents or near-misses during healthcare are not due to serious errors, but to the combination of small failures, such as limited experience of a recently qualified doctor, use of obsolete equipment, an infection difficult to diagnose or inadequate communication within a team.
We know that the analysis of an incident requires looking back to the succession of events that have occurred and that led to the problematic episode, considering both active and latent errors, and all the aspects connected directly or indirectly. It is fundamental to examine the safety of the entire patient journey, all the encounters that make up the entire care process, to study the whole medical history of the patient in an attempt to reconstruct all the elements that characterize the “health journey”, not only from the viewpoint of the health professionals, but also from that of the patient and family.
In light of these arguments, new concepts, tools, models, and methods need to be embraced to support patient safety in the patient journey.
A significant contribution in terms of concepts, frameworks, and models is offered by Industrial and Systems Engineering, and often human factors and systems engineering (HF/SE) have an approach to include the preferences and the needs of stakeholders when designing solutions to address the critical aspects of a health process.
Human factors and ergonomics are described as “the scientific discipline concerned with the understanding of interactions among humans and other elements of a system, and the profession that applies theory, principles, data and methods to design in order to optimize human well-being and overall system performance. Practitioners of ergonomics and ergonomists contribute to the design and evaluation of tasks, jobs, products, environments and systems in order to make them compatible with the needs, abilities and limitations of people. Ergonomics helps harmonize things that interact with people in terms of people’s needs, abilities and limitations” [ 6 ].
Process models have found widespread use in drug management, visit planning, care transition, to name a few, and can offer tools and methods to investigate interprofessional and physician–patient communication, interruptions and health information handover.
Drawing from the finding of Carayon’s studies [ 3 ], the Systems Engineering Initiative for Patient Safety (SEIPS) model gives a description of five work system elements which when applied to a definite patient journey model should outline who (person) is doing what (tasks) with tool and technologies, taking into consideration the physical and organizational environment where all these activities take place. All these factors have to be examined for both patients and workers and the process analysis and modelling have to consider what patients and families/caregivers, healthcare professionals and workers actually do ( work-as-done versus work-as-imaginated ).
Patients, families, and caregivers are deeply involved in the healthcare process due to the tasks they carry out in the intermediate sectors of care between encounters. Away from direct interactions with professionals, they have to perform multiple actions requiring understanding of what behaviour to adopt, which instructions to follow, how to administer a medication and how to communicate with hospital doctors, general practitioner, and home healthcare professionals [ 3 ].
Taking into account what has been highlighted so far, one of the leading and most challenging keys to success in improving patient safety is to adopt a systems approach to patient safety which includes the patient’s perspective about their health journey throughout the time of care and across all the care settings.
This assumption highlights that patients and their families are valuable resources and can play an important role in patient safety improvement efforts. Viewing health systems as “co-producing systems”, patients can engage as partners in co-producing patient safety improvement activities individually, in groups and collectively. Individual patient and family member participation/co-production of safer care is fundamental. Equally as important is the co-management and co-governance of healthcare services, in addition to the engagement of communities in policy definition and designing activities.
In fact, patient engagement directs the design of healthcare systems towards the preferences, the values, the real-life experiences, and—not less important—the skills of the people to enhance patient safety in the patient journey.
Such a change of perspective involves multiple dimensions of interactions and relationship between patients and professionals, encompassing cooperation, dialogue and listening, trust, reciprocity and peer-to-peer work [ 2 ].
It follows that on the one hand the healthcare organizations have to demonstrate the willingness to support health professionals to effectively engage patients in the patient journey to achieve the common goal of reducing the risk of patient harm or incidents as well as the willingness to integrate patients and family members as partners into quality and safety improvement efforts. On the other hand, it is necessary to motivate and encourage patients and families/caregivers to actively participate during the individual care process for safer care as well as partner in organizational patient safety improvement efforts to ensure safer care for others.
The working group Patient and Family Involvement for the delivery of Safe and Quality Care [ 7 ] stated that the utmost priority to realize the patient involvement is the training of patients, followed by the promotion of interdisciplinary training programmes for healthcare professionals to promote patient and family engagement, the implementation of multilevel structures that allow for participatory processes by patients and smarter allocation of resources in healthcare that supports involving citizens in patient safety improvement efforts for better healthcare.
This working group was part of the activities of the “1st International Meeting about Patient safety for new generations—Florence, 31st August and 1st September 2018” organized by the Centre for Clinical Risk Management and Patient Safety, Tuscany Region—WHO Collaborating Centre for in Human Factors and Communication for the Delivery of Safe and Quality care [ 7 ].
Therefore, training for both patients/families/advocates and health professionals is a pillar on which to build active engagement of patients and consequently an effective and efficient patient journey. From this perspective, the participation of patients (i.e. representatives of patients’ associations and organizations, patient and citizen advocates) in training courses—specifically designed for this target audience of trainees and aimed to encourage co-production of care—is an essential and effective activity to co-produce a better healthcare system in terms of quality and safety of care.
Sharing a common language, promoting citizens’ and patients’ awareness of importance of co-production of care, teaching the key role that patients can play in making treatments safer (investments in health literacy), learning to work together and within a network (locally, regionally, and nationally/internationally) on priority safety and quality of care issues: these are some of the main strengths of training courses aimed to be at the basis of active engagement of patients and citizens.
Examples of successful training courses include “PartecipaSalute” and “Accademia del Cittadino” organized in Italy by Laboratory for Medical Research and Consumers Involvement of the Istituto di Ricerche Farmacologiche Mario Negri IRCCS and the Centre for Clinical Risk Management and Patient Safety, Tuscany Region. The following paragraph describes this educational experience which is specifically designed for citizens and patients to improve their knowledge and skills in patient safety and quality of care, with the aim of co-producing better healthcare services.
4 From PartecipaSalute to the Accademia del Cittadino: The Importance of Training Courses to Empower Patients
Over the last few years in the field of health and research and with regard to participation and involvement of citizens and patients, we have witnessed the transition from a paternalist to a partnership model. Individual citizens and those citizens involved in patients’ associations or groups have acquired a new role: no longer passive but actively involved in decision-making regarding health, healthcare, and research in the health field [ 8 , 9 ].
This is a progressive step-by-step process based on the recognition and implementation of the key concepts such as health literacy and empowerment. Health literacy, more properly used at individual level is defined as the capacity to obtain, read, understand, and use healthcare information in order to make appropriate health decisions and follow instructions for treatment [ 10 ]. Empowerment, more used at the community level, is a process that, starting from the acquisition of accurate knowledge and skills, enables groups to express their needs and more actively participate to request better assistance, care, and research. At this level, the availability of organized independent and evidence-based training courses is essential to allow people to be able to critically appraise and use information about the effects of healthcare interventions. Consequently, they will have the skills to participate in the multidisciplinary working groups (composed of researchers, health professionals, patient and citizen advocates, institutional representatives).
In the late 1990s, the Istituto di Ricerche Farmacologiche Mario Negri IRCCS held the first training courses of this kind focused at breast cancer associations. Some years later, within the project PartecipaSalute—a not-for-profit research project designed to foster a strategic alliance among healthcare professionals, patients, and their organizations—an ad hoc training programme for representatives of citizens’ and patients’ organizations was defined with a multimodule format [ 11 , 12 ]. This was an innovative approach, at least in the Italian setting in that period.
PartecipaSalute training programme has combined different experiences: the Mario Negri Institute IRCCS experience in collaborative research activities with patients’ associations, the Italian Cochrane Centre with the activities aimed at promoting the principles of evidence-based medicine, and Zadig long-term experience in health communication. The above promoters jointly developed the PartecipaSalute training programme on the belief that data are more important than opinions, and that every decision should be supported by well-conducted research data.
The spread of this belief to patients and citizens with the purpose of stronger involvement was a key point of PartecipaSalute training courses.
Therefore, patient, family, and community knowledge of the principles of how evidence is developed through clinical research is essential to make or support decisions in the health debate, to promote better clinical research, or to convey correct information. The strength of the PartecipaSalute programme was based on the exchange of experiences in an interactive way aimed at creating opportunities for discussion, overcoming the teacher–learner model. Each session started with an interactive discussion of a real situation—such as a screening, vaccination, therapy—and after sharing data, opinions or articles from media, evidence was presented and discussed, underlining significant methodological aspects. The programme offered the opportunity to debate the value and significance of the methodology offering critical appraisal tools. Each participant was invited to take an active part, starting from direct personal or associative experience. Table 10.1 presents the topics considered in the first three editions of the training programme. The participation was free, and different types of materials were provided including an ad hoc manual published by PartecipaSalute, copies of the PowerPoint presentation and articles.
Considering the characteristics of the programme and its modular structure, the PartecipaSalute training programme could be adapted to specific contexts. In fact, the experience of PartecipaSalute was adopted at the regional level by Regione Toscana (Centre for Clinical Risk Management and Patient Safety and the Quality of healthcare and Clinical pathways of Health Department, Tuscany Region) developing a more specific training programme called PartecipaSalute-Accademia del Cittadino (Academy of Citizen), focused on patient safety and risk management. In particular, after some modules on methods related to evidence-based medicine, uncertainties in medicine and information and communication in health, the training was mainly dedicated to regional and local activities on clinical risk management, the role of patients’ associations to improve patient safety and to support the implementation of best practices, the analysis and data of adverse events and risk assessment in terms of quality and safety in the care processes (Table 10.2 ).
The PartecipaSalute-Accademia del Cittadino joint training programme has been implemented in three editions over the last decade and has trained about 100 members of patient and citizen advocates representing 38 patients’ associations. The courses ranged from 5 to 3 modules of 2 days each in residential mode to allow participants to get to know each other and create a network of associations committed to be engaged in clinical research, quality, and healthcare safety issues.
The entire educational experience was characterized by the use of participatory training methods, based on working groups, practical exercises, lectures from experts with opportunities for discussions. As a result of this training course model, the participants were recognized as “expert patients” and were regularly involved in basic activities for promoting patient safety as auditors on significant events and helping to define policies on patient safety at the Tuscany regional level. In addition, they have participated in patient safety walkarounds in hospitals and in developing eight cartoons intended to promote the education of citizens for the prevention of the most diffused risks (such as prevention of infections, prevention of falls and handovers).
Feedback on the satisfaction on tutors, topics discussed and knowledge gained was regularly requested from participants through questionnaires distributed before and after the programme. In general, positive feedback was received; participants appreciated the interactive methods of work, the clarity of the language, and the effort to make difficult problems easy to understand. An ad hoc questionnaire was provided to the participants regarding the methodology of clinical research, always showing an improvement in the self-evaluated knowledge before and after the course. Feedback of the results of the evaluation was also shared with each participant. Most of participants reported their experience to other members of the organization. In particular, in the case of the Regione Toscana training, the possibility of immediately transferring what was learned in the course in all the activities in collaboration with the health institutions, policy makers, and health professionals—such as working groups on patient safety best practices, participation to audits, development of tools to improve health literacy—was appreciated.
Some limitations emerged from these experiences. The selection of participants is the first issue, not only because the training course is accessible to a small number of participants (in general no more than 30 participants), but also because the groups comprised of middle-aged and retired participants, with few younger ones. Additionally, there were few individual patient or family member representatives from patient associations. The majority of those representing patient associations were in managerial or leadership positions. Furthermore, it is difficult to choose between small, local, or bigger regional associations. Residential training courses also restricted the participation for geographical reasons.
The PartecipaSalute and ParteciaSalute-Accademia del Cittadino training experiences show that patients and citizens are willing to get actively involved in healthcare and the research debate. There is a real desire to improve their knowledge and skills on health and research issues and allow some general considerations regarding the active engagement of citizens representing associations and advocacy groups.
In conclusion, it is very important to invest in a process of empowerment aimed to have well-trained activists involved vigorously and constructively in the debate, design, and assessment of health and research. Switching from tokenism to active participation is necessary to effectively partner with patients and the general population to design, plan, and co-produce safer more effective healthcare, while also supporting better more patient-centred research [ 13 , 14 ].
Also, the training courses are feasible and useful, as has recently been discovered also by pharma or other groups that organize courses mainly focused on drugs and drug development, thus directing the participation of the groups more to market needs than to public health.
Furthermore, this training initiative facilitates the networking among associations in part overcoming the difficulties that derive from personalization and division among the associations representing citizens and patients.
Finally, this illustrates the importance of the design and promotion of training courses with institutions, such as the Regione Toscana, in order to be able to implement projects of real collaboration between institutions, healthcare professionals, and consumers’ and patients’ representatives.
5 Recommendations
A systemic approach to health can provide valuable models for wider implementation of patient safety. A multidisciplinary approach includes the involvement of citizens and patients as unique stakeholders in the design, implementation, delivery, and assessment of health services.
Involving patients in healthcare is an opportunity to bring uncommon points of view into policy making and to create shared knowledge between healthcare professionals and patients.
The implementation of patients’ and families’/caregivers’ perspectives in the patient journey is the golden opportunity to leverage crucial input, such as experiential knowledge, safer care, patient motivation, and trust and social cohesion into the co-production of safety solutions in healthcare. This represents a way to get closer to person-centred care, to create opportunities for patients to meet and share information and knowledge, to develop structures and policies for patient involvement at different levels (with healthcare systems, universities, and policy makers).
However, little has been done to overcome some healthcare systems barriers: the power imbalance between the doctor and patient, language differences, the lack of diffusion of non-technical skills and, last but not least, the lack of evidence about the value of patient involvement.
To be widely implemented, patient engagement in the patient journey requires courageous leadership, organizational efforts, a wider culture of safety of care, the implementation of multilevel structures for the engagement of patients and resources from smarter spending in healthcare.
Education is the landmark to integrate meaningful patient and citizen engagement in healthcare. Training of patients is the fundamental starting point to develop shared knowledge, co-produce projects, and implement an active multilevel participation of patients and families for the improvement of quality and safety of care.
Kaplan G, Bo-Linn G, Carayon P, Pronovost P, Rouse W, Reid P, Saunders R. Bringing a systems approach to health, Discussion Paper. Institute of Medicine and National Academy Engineering. 2013.
Google Scholar
Palumbo R. Contextualizing co-production of health care: a systematic literature review. Int J Public Sect Manag. 2016;29(1):72–90. https://doi.org/10.1108/IJPSM-07-2015-0125 .
Article Google Scholar
Carayon P, Wooldridge AR. Improving patient safety in the patient journey: contributions from human factors engineering. In: Smith AE, editor. Women in industrial and systems engineering. Key advances and perspective in emerging topics, Women in engineering and science, vol. 12. Cham: Springer; 2019. p. 275–99.
Vincent C, Amalberti R. Safer healthcare-strategies for the real world, vol. 5. Cham: Springer Open; 2016. p. 47–57.
Book Google Scholar
McCarthy S, O’Raghallaigh P, Woodworth S, Lim YL, Kenny LC, Adam F. An integrated patient journey mapping tool for embedding quality in healthcare service reform. J Decis Syst. 2016;25(Suppl 1):354–68. https://doi.org/10.1080/12460125.2016.1187394 .
International Ergonomics Association (IEA). Definition and domains of ergonomics. https://www.iea.cc/whats/ . Accessed 23 Dec 2019.
International Meeting about Patient safety for new medical generations—Florence, 31 Aug and 1 Sept 2018. http://iea2018.org/?page_id=4373 . Accessed 23 Dec 2019.
Castro EM, Van Regenmortel T, Vanhaecht K, Sermeus W, Van Hecke A. Patient empowerment, patient participation and patient-centeredness in hospital care: a concept analysis based on a literature review. Patient Educ Couns. 2016;99(12):1923–39. https://doi.org/10.1016/j.pec.2016.07.026 . Epub 2016 Jul 18.
Article PubMed Google Scholar
Coulter A, Ellins J. Effectiveness of strategies for informing, educating, and involving patients. Br Med J. 2007;335:24–7.
IOM. Health literacy: a prescription to end confusion. Washington DC: National Academies Press, 2004; Am J Prev Med. 2009;36(5):446–51.
Mosconi P, Colombo C, Satolli R, Liberati A. PartecipaSalute, an Italian project to involve lay people, patients’ associations and scientific-medical representatives on the health debate. Health Expect. 2007;10:194–204.
Mosconi P, Satolli R, Colombo C, Villani W. Does a consumer training work? A follow-up survey of the PartecipaSalute training programs. Health Res Policy Syst. 2012;10:27. https://doi.org/10.1186/1478-4505-10-27 .
Article PubMed PubMed Central Google Scholar
Ocloo J, Matthews R. From tokenism to empowerment: progressing patient and public involvement in healthcare improvement. BMJ Qual Saf. 2016;25:626–32. https://doi.org/10.1136/bmjqs-2015-004839 .
Chalmers I, Bracken MB, Djulbegovic B, Garattini S, Grant J, Gülmezoglu AM, Howells DW, Ioannidis JP, Oliver S. How to increase value and reduce waste when research priorities are set. Lancet. 2014;383:156–65. https://doi.org/10.1016/S0140-6736(13)62229-1 .
Download references
Author information
Authors and affiliations.
Centre for Clinical Risk Management and Patient Safety, Tuscany Region—WHO Collaborating Centre in Human Factors and Communication for the Delivery of Safe and Quality Care, Florence, Italy
Elena Beleffi
Laboratory for Medical Research and Consumers Involvement, Public Health Department, Istituto di Ricerche Farmacologiche Mario Negri IRCCS, Milan, Italy
Paola Mosconi
The Society to Improve Diagnosis in Medicine, Evanston, IL, USA
Susan Sheridan
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Elena Beleffi .
Editor information
Editors and affiliations.
London School of Hygiene and Tropical Medicine, London, UK
Liam Donaldson
Department of Hygiene and Public Health, Catholic University of the Sacred Heart, Rome, Italy
Walter Ricciardi
Italian Network for Safety in Healthcare, Florence, Italy
Riccardo Tartaglia
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Reprints and permissions
Copyright information
© 2021 The Author(s)
About this chapter
Beleffi, E., Mosconi, P., Sheridan, S. (2021). The Patient Journey. In: Donaldson, L., Ricciardi, W., Sheridan, S., Tartaglia, R. (eds) Textbook of Patient Safety and Clinical Risk Management . Springer, Cham. https://doi.org/10.1007/978-3-030-59403-9_10
Download citation
DOI : https://doi.org/10.1007/978-3-030-59403-9_10
Published : 15 December 2020
Publisher Name : Springer, Cham
Print ISBN : 978-3-030-59402-2
Online ISBN : 978-3-030-59403-9
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
The patient journey of adults with hearing impairment: the patients' views
Affiliation.
- 1 Long Term and Chronic Conditions Centre, College of Human and Health Sciences, Swansea University, Swansea, UK. [email protected]
- PMID: 21518295
- DOI: 10.1111/j.1749-4486.2011.02320.x
Objective: The term 'patient journey' refers to the experiences and processes the patient goes through during the course of a disease and its treatment. The study explores the perspectives of adults with acquired hearing impairment and to further develop the patient journey template based on the Ida model.
Design: Qualitative approach using thematic analysis and process mapping.
Setting: Support groups of people with hearing impairment.
Participants: Thirty-two adults with acquired hearing impairment from two hearing impaired groups in Wales. All were hearing aid users.
Main outcome measure: Participants worked in small groups to describe their experiences through hearing loss. These data were used to develop a template of the patients' perspective of the journey. This was then compared with the perspective of professionals, and a 'patient journey template for adults with acquired hearing impairment' was developed.
Results: This template identifies seven main phases as follows: (i) pre-awareness; (ii) awareness; (iii) movement; (iv) diagnostics; (v) rehabilitation; (vi) self-evaluation; and (vii) resolution. The study identified a number of new components. The self-evaluation component was not defined by professionals and reflects the need for patients to consider the costs, benefits and alternatives to the approach provided by audiologists. It is important for audiologists to be aware of this.
Conclusion: The study highlighted the differences and commonalities in perspectives of professionals and patients. Use of the patient journey can help clinicians to understand the unique experiences their patients go through help them to develop patient-centred treatment.
© 2011 Blackwell Publishing Ltd.
Publication types
- Comparative Study
- Aged, 80 and over
- Attitude to Health*
- Child, Preschool
- Comprehension*
- Diagnostic Self Evaluation
- Follow-Up Studies
- Middle Aged
- Patient Acceptance of Health Care / psychology*
- Patient Compliance*
- Persons With Hearing Impairments / psychology
- Persons With Hearing Impairments / rehabilitation*
- Persons With Hearing Impairments / statistics & numerical data
- Time Factors
- Wales / epidemiology
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Risk Factors
- Facts and Stats
- Communication Resources
- Blood Clot Awareness Month
- Stop the Clot, Spread the Word® Campaign Resources
- VTE E-Learning Course
- Scientific Articles
Stop the Clot®—What Every Healthcare Professional Should Know E-Learning Course
What to know.
The Centers for Disease Control and Prevention (CDC) and the National Blood Clot Alliance recently relaunched the Stop the Clot®—What Every Healthcare Professional Should Know e-learning course for healthcare providers. As one of CDC's most popular online courses, this free, self-paced e-learning course has been updated to provide current information on and best practices for identifying, treating, and managing patients who have blood clots, also known as venous thromboembolism (VTE), and other clotting disorders.
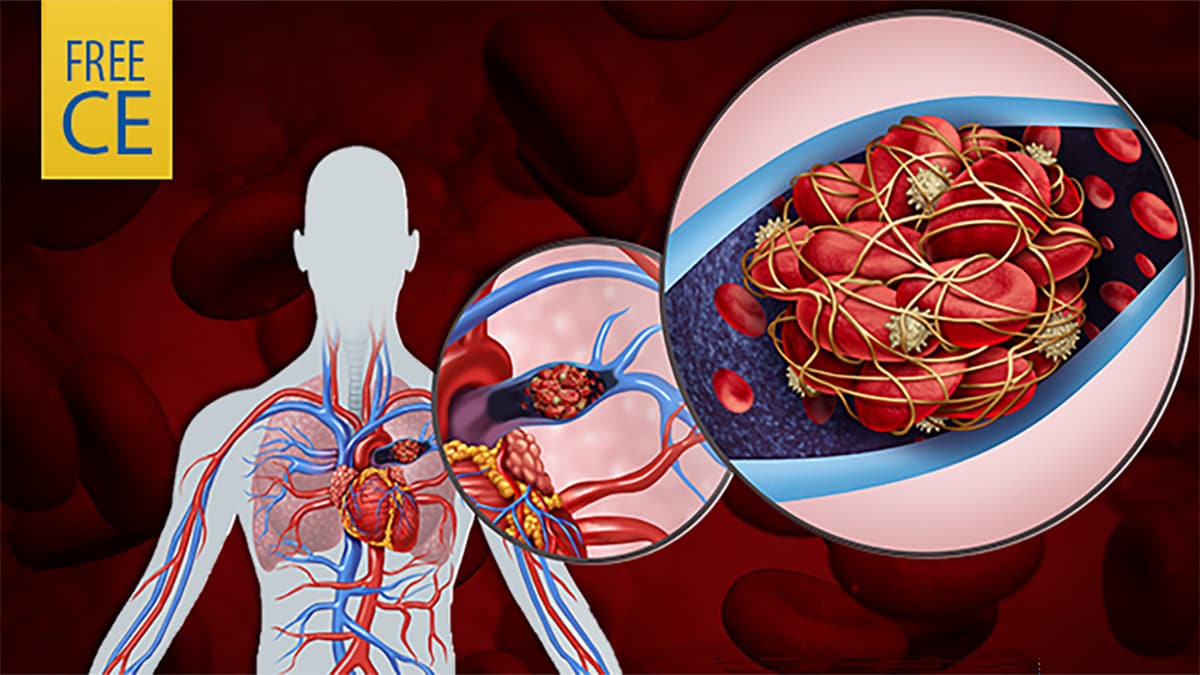
Program Description:
This course is designed to provide the most current information and clinical considerations to assess and treat patients at risk of and experiencing venous thromboembolism (VTE). It also aims to improve the ability of healthcare professionals to identify and manage these patients.
Objectives:
At the conclusion of the course, the participants will be able to:
- Explain two facts about the physiology of thrombus formation and the pathogenesis of VTE.
- Describe three risk factors for VTE.
- Describe three VTE prevention options.
- Explain three processes used in VTE diagnosis.
- Explain two VTE treatment and management options.
- Describe two possible post-VTE complications.
- Identify two key strategies for improving interprofessional care.
Target Audience:
This web-based training is intended for physicians, registered nurses, physician assistants, pharmacists, and other allied health professionals.
Continuing Education Credits:
Free continuing education (CE) credits including CME, CNE, CPE, and CEU are available after successful completion of the course.
Ready to register?
Venous thromboembolism (blood clots).
Venous thromboembolism (VTE), also known as blood clots, is an underdiagnosed and serious, but preventable medical condition.
For Everyone
Health care providers.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Patient Exp
- v.7(6); 2020 Dec
Understanding the Patient Experience: A Conceptual Framework
Patrick oben.
1 MercyOne Des Moines, Des Moines, IA, USA
The patient experience is now globally recognized as an independent dimension of health-care quality. However, although patients, providers, health-care managers, and policy-makers agree on its importance, there is no standardized definition of the patient experience. A clear understanding of the basic concepts that make up the foundation of the patient experience is more important than a statement defining the patient experience. The fundamental nature of health care involves people taking care of other people in unique times of distress. Thus, the human experience is at the very core of understanding what the patient experience is. This article reviews a framework of the basic human experience of patients as they progress from being unique, healthy individuals to a state of experiencing both disease and health-care services. This novel framework naturally leads to a basic understanding of the patient experience as a human experience of health-care services.
Introduction
Throughout the world, the patient experience is recognized as an independent dimension of health-care quality, along with clinical effectiveness and patient safety ( 1 , 2 ). Health-care organizations across the United States are focusing on how to “deliver a superior patient experience” ( 3 ). Quality is a key driver of these industry-wide changes, as are the shifts in health-care policy that have tied hospital and physician compensation to patient experience measures, the focus on patient engagement, and the emergence of the consumer mindset ( 2 , 4 ).
Despite the increasingly important role that the patient experience occupies in health-care clinical practice, research, quality improvement efforts, and policies, there is no universal understanding of what the “patient experience” is, as evidenced by the lack of a standardized definition ( 4 ). Therefore, patients, clinicians, policy makers, managers, and researchers have different interprets of the concept ( 5 ). Although this has been called the “era of the patient” ( 6 ), experts have said, “it’s no wonder that hospitals are struggling with the best way to provide it.” After all, if you can’t define what it is, you can’t provide it—and you certainly can’t measure it” ( 5 ). Thus, a clearer understanding of the patient experience will assist clinicians in improving that experience at the point of care, guide further research into the topic, and provide clear directions for quality improvement efforts and health-care policies.
There are several reasons for the lack of a formal definition or clear understanding of the patient experience. The patient experience is a multidimensional, multifaceted, and intimately connected concept with several subsections. Furthermore, framing definitions, even when concepts are well understood, is not a simple task. The Beryl Institute made a significant stride forward by providing a definition that highlights the integrated and multidimensional nature of the patient experience and the complexity of the framing task ( 4 , 7 ). They defined the patient experience as “the sum of all interactions, shaped by an organization’s culture, that influence patient perceptions, across the continuum of care” ( 7 ). This definition identifies 4 critical themes for understanding the patient experience: personal interactions, organization’s culture, patient and family perceptions, and continuum of care.
By itself, a definition is a statement that seeks to convey the understanding of a concept. The greater our understanding of the patient experience, the easier it is to frame a definition. As we continue to create a standardized definition, it is important to step back from its multidimensional nature and review its most basic concepts. One fundamental source for this concept comes from an article in the 2001 Institute of Medicine, which states, “health care is not just another service industry. Its fundamental nature is characterized by people taking care of other people in times of need and stress” ( 8 ). A central role in health care is, therefore, the humanity of both the patient and care provider throughout the process of providing health care. Both the physician and patient are people ( 9 ).
This article seeks to provide a general overview of the patient experience from the platform of who we are as human beings, whether we are patients or providers. It provides a conceptual framework that traces the patient’s virtual journey from health, to the onset of disease, and through multiple encounters with health-care services. To fully appreciate the value of this conceptual framework, awareness of 2 important elements is required. First, although the patient experience concept is multidimensional and multifaceted, the health-care experience for the individual patient is unified; it is informed by a complex combination of the patient’s personal life, as well as their own and their family’s experiences within the health-care system at all levels of care.
Second, the word “patient” is used in this article with a specific meaning. There is intense debate about replacing the word patient with consumer, users, or clients; the argument for the change is that the word “patient” conveys the idea of passivity and does not correctly describe all patient populations, especially the “well patient” seeking preventive services ( 10 , 11 ).
In this article, we use the dictionary definition of patient: “a person receiving or registered to receive medical treatment” ( 12 ). However, the additional element of “suffering,” which captures a critical element of the human experience of disease, is also incorporated. Thus, patient refers to a person suffering from a disease before and after they begin receiving or are registered to receive medical treatment.
The Experience Journey of the Patient
A recurrent and prominent theme in discussions of the patient experience is centering the patient’s perception or perspective on the health care they receive ( 7 , 13 ). Health-care providers who seek to understand the patient’s perspective of their experience will obtain a greater understanding of the patient experience. Furthermore, it is important to note that the patient’s overall health and disease experience begins before they enter the health-care system. This holistic experience from the patient’s perspective is critical for a complete understanding of their experience within the health-care organization.
Phases and landmarks of the patient experience
When a patient contacts a health-care organization, assuming they are in a basic state of health, they begin a journey that consists of 3 phases or spheres of experiences with 2 critical landmarks. These phases and landmarks of the patient experience are illustrated in Figure 1 .

A conceptual framework for understanding the patient experience. The arrows indicate the direction patients take in their journey through health-care encounters, which is hypothetically to the right of the diagram. The person moves across the continuum, indicating that the patient or user of health-care services is the same unique human being they have always been. The arrow labeled “Patient” begins in the middle, indicating the person is not always a patient and becomes one with the onset of disease. The “User” arrow indicates that the person who has a disease only becomes a user of health-care services with their first interaction with the health-care system.
- The patient, just as the provider, is a unique individual. A baseline state of health is used for the purpose of simplicity, as illustrated in the right column in Figure 1 .
- The first landmark for the individual is the beginning of a process that moves them from the first column, person, to the middle column, patient. A patient, as we have stated, is a person who is suffering from a disease, but they are still the same unique person they have been.
- The second landmark occurs when this person suffering from a disease makes their first contact with medical care services regarding this disease. They become users or consumers of these services. While they interact with health-care organizations, they continue to be the same person they were before disease onset.
Importantly, the state of disease or the role of a person as a user of health-care services is dynamic. If the disease is cured, the individual who was a patient before is restored to the experience of health and is no longer a patient.
A Continuum and Unity
As Figure 1 demonstrates, the patient remains the same person they were before the disease onset, even after they contract a disease or begin utilizing medical services. The person’s interactions with health-care providers—and not their disease or their role as consumers—are the key to understanding the fundamental nature of the patient experience.
The patient experience does not rely solely on the events that occur between themselves and health-care providers; their complex human experiences also influence their perception of the situation. For instance, while the patient seeks to understand the plan of care as the provider explains it (experience with medical services), they might also experience discomfort from their symptoms (experiences of the disease) and anxiety over making sure their kids are picked up from daycare (experiences in general life).
A journey through this continuum leads to a solid understanding of what health care currently refers to as the patient experience. As shown in Figure 1 , this experience is also a human experience of a distinct occurrence or series of events called health-care service.
The Person: The Human Experience
The first column in Figure 1 lays the foundation for understanding the person who seeks medical care from health-care providers. Understanding the humanity of patients is the critical foundation upon which any successful patient-centered experience efforts should be built. The prominent role of our humanity distinguishes health care from other service industries ( 8 ). In “Harrison’s Principles of Internal Medicine,” Jameson et al stated, “Tact, sympathy, and understanding are expected of the physician, for the patient is no mere collection of symptoms, signs disordered functions, damaged organs, and disturbed emotions. [The patient] is human, fearful and hopeful, seeking relief, help and reassurance” ( 14 ).
The patient is a human, and humanity harbors the secret to the elements of care that creates a superior patient experience. In a speech to Harvard Medical Students in 1926, Francis Peabody stated, “one of the essential qualities of the clinician is interest in humanity, for the secret of the care of the patient is in caring for the patient” ( 9 , 15 ). This statement is as valid today as it was when it was first spoken. Our interest in the humanity of our patients naturally leads us to care for the person who is suffering from an illness and seeking help from the health-care system, rather than merely managing a case or disease. The human experience is, therefore, central to the overall conceptual understanding of the patient experience.
The World Health Organization defines health as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity” ( 16 ). This definition indicates that the human experience in health and disease is multidimensional and includes physical, mental, and social dimensions. Puchalski identified a fourth, spiritual dimension; she calls compassionate care “serving the whole person—the physical, emotional, social, and spiritual” ( 17 ); research has shown this to be important to many patients ( 18 ). The social dimension emphasizes the importance of engaging not only the patient but also their families and communities ( 19 - 21 ). Needham recognizes the multinational nature of the patient experience in stating that both emotional and physical experiences must be managed, highlighting 2 out of the 4 dimensions noted above ( 22 ).
The Patient: The Experience of Illness
As noted above, this article uses the word patient to refer to a person suffering from a disease before and after they begin receiving or are registered to receive medical treatment. It has a central role in the conceptual framework of Figure 1 , as it preserves what is “distinctive about medical practice” ( 10 ) and what separates health care from many other service industries: a human being suffering from a disease seeks care from another human being who not only provides a service but also is moved with compassion and empathy for the one seeking help ( 8 ). Despite its limitations within the evolving landscape of health care, Dr. Raymond Tallis’ comment regarding replacing the word patient, to “leave it well alone” ( 10 ), seems to be echoed by most patients and providers ( 23 ).
The onset of a disease marks the critical landmark of the transition from a person who is healthy to a person suffering from a disease before or after they are registered or begin receiving medical treatment. The individual, who we assume was previously healthy, begins to experience a disease in the psychological, physical, social, and spiritual dimensions. For example, a patient with a broken bone may experience not only physical pain and sight of a possible deformity but also the fear and anxiety of lifelong loss of movement or being admitted to a hospital for the first time.
Shale describes 3 aspects of the patient experience, including physiologic experiences of illness, customer service, and lived experiences of the illness ( 24 ). The patient’s experience of an illness is a distinct aspect of their overall experience. The ultimate hope of medical care is to eliminate, reduce the impact of, or manage the varied psychological, physical, social, and spiritual experiences of illness, for both the patient and their families and communities. These distinct spheres of experiences, which simultaneously occur during every interaction between the health-care organization and the person, form the continuum of the patient’s holistic experience of care.
The Experience of Health-Care Services
Health care is, “after all, a service” ( 2 ). Patients become users or consumers of health-care services when they begin using those services, starting with their first interaction across the continuum of care. Health-care service, as a continuum of all interactions with the patient, is experienced in the same 4-dimensional sphere of human experience, that is, physically, psychologically, socially, and spiritually. The patient experience, in essence, is the human experience of health-care services. The central reason for the existence of the health-care industry is to care for the patient: to manage their physical, psychological (emotional/mental), social, and spiritual health needs as presented.
The Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) is a standardized, well-established, and extensively-validated instrument that measures the degree to which health-care services have managed to meet the aforementioned complex needs ( 13 ). The HCAHPS addresses specific aspects of interactions between the patient and the health-care organization, such as communication with doctors and nurses. The patient’s experience begins with the onset of disease, which, however, the HCAHPS cannot capture. This is because the health-care system is not responsible for the prior, varied experiences that individual patients may have experienced in their illness before seeking care for this disease state. However, when these patients are under the care of a health-care organization, the degree to which the care services meet their needs, in the context of the family and community, is the health-care service provider’s direct responsibility. The HCAHPS scores give health-care service providers a quantitative measure to assess how well they are meeting the needs of their patients, families, and communities. They can then determine areas of strengths and weaknesses and clearly plan quality improvement changes across the continuum of care so that “patients would experience care” that is safe, effective, patient-centered, timely, efficient, and more equitable” ( 8 ).
A proper, clear, and precise understanding of the patient experience will benefit the health-care industry and society in multiple aspects, including but not limited to establishing a tailored and personalized clinical bedside care, providing clear guidance for further research, stimulating consistent and sustainable improvements in medical care quality, and guiding health-care policy. The conceptual framework presented in this article, which seeks to clarify the centrality of the patient’s human experience across the continuum of care, is only the beginning point for a better overall understanding of this multidimensional, multifaceted concept. The health-care industry has not received the full benefit of the data provided by patient experience measurement tools. Given the potential impact on quality, safety, and cost of health care in general, research efforts should be made to not only create a standardized definition of the patient experience but also clarify its various components. The current methods of measurement and reporting should be improved in order to establish the best ways to incorporate the patient experience data into general health-care improvement efforts.
Author Biography
Patrick Oben is a hospitalist at MercyOne Des Moines Medical Center. He serves as the Physician Lead of the MercyOne Patient Experience unit.
Authors’ Note: No research was performed on human or animal subjects and as such approval by an Ethics Committee or Institutional Review Board was not required. Similarly, no informed patient consents were obtained as these were not required.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.

TikToker who documented journey with metastatic sarcoma dies at 31, released final video saying 'I've passed away'
TikToker Kimberley Nix, who documented her three year journey with metastatic sarcoma, has died at the age of 31.
As a final farewell, Nix published a last video on her TikTok page to her 148,000 followers saying, “If you’re seeing this message, I have passed away peacefully.”
Nix, who worked as a resident doctor, was diagnosed with palliative sarcoma cancer at 28 years old, according to her TikTok account. Since then, she's used the platform to spread awareness on sarcoma cancer, a group of cancers that begin in the bones and in soft tissues, according to the Mayo Clinic .
In her farewell video she said: "I am a resident doctor who trained in internal medical and had a beautiful life and I’m so proud of it. Those who know me know I love my pets, my husband and make up in the reverse over, my husband first and of course all of my family and friends."
"In 2021, I got the opportunity to start making TikTok videos and I never thought that these would become anything. My goal was to spread awareness about sarcoma cancer, and we have been a successful team. We have reached great heights in sarcoma awareness," she explained.
"One of the things that has been the most important for really getting to know you all better has been also sharing my own journey and through my TikTok page, I've shared my journey from the time that my disease was potentially curative ... I've shared about going through six different lines of both experimental and non experimental ... therapies," she said.
"I shared about going through the various challenges of cancer and how we overcame them and I shared about love and joy and gratitude, because in this journey being grateful with people in the little moments, those little parts of your day like that warm first sip of tea in the morning or how it feels when the snow is fresh on your face, are the most beautiful."
She also documented checking items off her bucket list — from her engagement, her wedding, to a dream trip to New York City where she had "a plush stay" that reminded her of the TV show "Gossip Girl" and saw a musical on Broadway.
Nix also enjoyed trips to the mountains, to San Francisco's wine country, and saw some of her favorite artists including Taylor Swift on her Era's Tour, Coldplay and Noah Kahan.
"Through this time my workplace, my husband’s workplace, have been so supportive of us and he’s been able to be off with me a lot of the time. I've had my parents here a lot of the time supporting me and having support is so wonderful," she said.
Nix started to cry when she spoke about her husband.
"My only sadness dying is knowing that we didn’t get to grow old together. Everything else is totally bearable because that is the only thing that really matters," she said.
In her video she said she felt "at peace" with her life and overcome with gratitude for the people in her life, enjoying everyday small moments and with her mission on TikTok.
"If following along as been helpful in any way I have achieved my goal. If sarcoma awareness is achieved, I've achieved my goal," she said.
"This community has meant the absolute world to me. I will miss you TikTok. I love you all," Nix ended her video. "Thank you so much for this amazing opportunity. I’m in happy tears because you’ve all made me find so much purpose in the end of my life."
Nix's husband, Michael MacIsaac, said in a statement on TikTok Wednesday: "My beautiful and selfless wife, my unconditional support and guiding light, and the world's purest soul, passed on today."
He said his wife faced hardship and tragedy with “grace and kindness,” “loved the unloved,” and “healed the ailing” in her life, cut too short.
“I tried to learn all I could, from the biggest inspiration I’ve ever known. Where does all your empathy come from? Your work ethic? Your ability to seize every moment? I didn’t have enough time, but a hundred lifetimes wouldn’t be enough. I’ve no idea how she crammed it all into one, short as it turned out to be,” he said.
“I’m eternally grateful to have been your husband, and am so much better off for having known you. I’m shattered into a billion pieces. I love you Kim,” he concluded his message.
In another message shared Thursday he said: "Yesterday was the worst day of my life, and somehow, thanks to some deeply cherished friends and the connectedness I felt throughout the day, we made it. Today isn’t much better, but I think we’ll make it again too."
MacIsaac said he was "overwhelmed" by the response following his wife's passing.
"You sent me your light and love from every corner of the globe. While that’s easy enough to believe — Kim accomplished the ultimate goal of leaving the world better than she found it — what I can’t believe is how many of you are concerned about me. I’m touched."
Breaking News Reporter
- Share full article
Advertisement
Supported by
First Patient Begins Newly Approved Sickle Cell Gene Therapy
A 12-year-old boy in the Washington, D.C., area faces months of procedures to remedy his disease. “I want to be cured,” he said.

By Gina Kolata
Photographs by Kenny Holston
Gina Kolata visited Kendric and his parents at the hospital in Washington, D.C., when he was having his stem cells extracted
On Wednesday, Kendric Cromer, a 12-year-old boy from a suburb of Washington, became the first person in the world with sickle cell disease to begin a commercially approved gene therapy that may cure the condition.
For the estimated 20,000 people with sickle cell in the United States who qualify for the treatment, the start of Kendric’s monthslong medical journey may offer hope. But it also signals the difficulties patients face as they seek a pair of new sickle cell treatments.
For a lucky few, like Kendric, the treatment could make possible lives they have longed for. A solemn and shy adolescent, he had learned that ordinary activities — riding a bike, going outside on a cold day, playing soccer — could bring on episodes of searing pain.
“Sickle cell always steals my dreams and interrupts all the things I want to do,” he said. Now he feels as if he has a chance for a normal life.
Near the end of last year, the Food and Drug Administration gave two companies authorization to sell gene therapy to people with sickle cell disease — a genetic disorder of red blood cells that causes debilitating pain and other medical problems. An estimated 100,000 people in the United States have sickle cell, most of them Black. People are born with the disease when they inherit the mutated gene for the condition from each parent.
The treatment helped patients in clinical trials , but Kendric is the first commercial patient for Bluebird Bio, a Somerville, Mass., company. Another company, Vertex Pharmaceuticals of Boston, declined to say if it had started treatment for any patients with its approved CRISPR gene-editing-based remedy .
Kendric — whose family’s health insurance agreed to cover the procedure — began his treatment at Children’s National Hospital in Washington. Wednesday’s treatment was only the first step. Doctors removed his bone marrow stem cells, which Bluebird will then genetically modify in a specialized lab for his treatment.
That will take months. But before it begins, Bluebird needs hundreds of millions of stem cells from Kendric, and if the first collection — taking six to eight hours — is not sufficient, the company will try once or twice more.
If it still doesn’t have enough, Kendric will have to spend another month in preparation for another stem cell extraction.
The whole process is so involved and time-consuming that Bluebird estimates it can treat the cells of only 85 to 105 patients each year — and that includes not just sickle cell patients, but also patients with a much rarer disease — beta thalassemia — who can receive a similar gene therapy.
Medical centers also have the capacity to handle only a limited number of gene therapy patients. Each person needs expert and intensive care. After a patient’s stem cells have been treated, the patient has to stay in the hospital for a month. For most of that time, patients are severely ill from powerful chemotherapy.
Children’s National can accept only about 10 gene therapy patients a year.
“This is a big effort,” said Dr. David Jacobsohn, chief of the medical center’s division of blood and marrow transplantation.
Top of the Waiting List
Last week, Kendric came prepared for the stem cell collection — he has spent many weeks in this hospital being treated for pain so severe that on his last visit, even morphine and oxycodone could not control it. He brought his special pillow with a Snoopy pillowcase that his grandmother gave him and his special Spider-Man blanket. And he had a goal.
“I want to be cured,” he said.
Bone marrow stem cells, the source of all the body’s red and white blood cells, are normally nestled in a person’s bone marrow. But Kendric’s doctors infused him with a drug, plerixafor, which pried them loose and let them float in his circulatory system.
To isolate the stem cells, staff members at the hospital inserted a catheter into a vein in Kendric’s chest and attached it to an apheresis machine, a boxlike device next to his hospital bed. It spins blood, separating it into layers — a plasma layer, a red cell layer and a stem cell layer.
Once enough stem cells have been gathered, they will be sent to Bluebird’s lab in Allendale, N.J., where technicians will add a healthy hemoglobin gene to correct the mutated ones that are causing his sickle cell disease.
They will send the modified cells back three months later. The goal is to give Kendric red blood cells that will not turn into fragile crescent shapes and get caught in his blood vessels and organs.
Although it takes just a couple of days to add a new gene to stem cells, it takes weeks to complete tests for purity, potency and safety. Technicians have to grow the cells in the lab before doing these tests.
Bluebird lists a price of $3.1 million for its gene therapy, called Lyfgenia. It’s one of the highest prices ever for a treatment.
Despite the astronomical price and the grueling process , medical centers have waiting lists of patients hoping for relief from a disease that can cause strokes, organ damage, bone damage, episodes of agonizing pain and shortened lives.
At Children’s National, Dr. Jacobsohn said at least 20 patients were eligible and interested. The choice of who would go first came down to who was sickest, and whose insurance came through.
Kendric qualified on both counts. But even though his insurance was quick to approve the treatment, the insurance payments are only part of what it will cost his family.
Chances and Hopes
Deborah Cromer, a realtor, and her husband, Keith, who works in law enforcement for the federal government, had no idea they might have a child with sickle cell.
They found out only when Deborah was pregnant with Kendric. Tests showed that their baby would have a one-in-four chance of inheriting the mutated gene from each parent and having sickle cell disease. They could terminate the pregnancy or take a chance.
They decided to take a chance.
The news that Kendric had sickle cell was devastating.
He had his first crisis when he was 3. Sickled blood cells had become trapped in his legs and feet. Their baby was inconsolable, in such pain that Deborah couldn’t even touch him.
She and Keith took him to Children’s National.
“Little did we know that that was our introduction to many many E.R. visits,” Deborah said.
The pain crises became more and more severe. It seemed as though anything could set them off — 10 minutes of playing volleyball, a dip in a swimming pool. And when they occurred, Kendric sometimes needed five days to a week of treatment in the hospital to control his pain.
His parents always stayed with him. Deborah slept on a narrow bench in the hospital room. Keith slept in a chair.
“We’d never dream of leaving him,” Deborah said.
Eventually the disease began wreaking severe damage. Kendric developed avascular necrosis in his hips — bone death that occurs when bone is deprived of blood. The condition spread to his back and shoulders. He began taking a large daily dose of gabapentin, a medicine for nerve pain.
His pain never let up. One day he said to Deborah, “Mommy, I’m in pain every single day.”
Kendric wants to be like other kids, but fear of pain crises has held him back. He became increasingly sedentary, spending his days on his iPad, watching anime or building elaborate Lego structures.
Despite his many absences, Kendric kept up in school, maintaining an A average.
Deborah and Keith began to hope for gene therapy. But when they found out what it would cost, they lost some of their hope.
But their insurer approved the treatment in a few weeks, they said.
Now it has begun.
“We always prayed this day would come,” Deborah said. But, she added, “We’re nervous reading through the consents and what he will have to go through.”
Kendric, though, is looking forward to the future. He wants to be a geneticist.
And, he said, “I want to play basketball.”
An earlier version of this article misstated the location of a lab. It is in Allendale, N.J., not Allentown.
How we handle corrections
Gina Kolata reports on diseases and treatments, how treatments are discovered and tested, and how they affect people. More about Gina Kolata
Kenny Holston is a Times photographer based in Washington, primarily covering Congress, the military and the White House. More about Kenny Holston

IMAGES
VIDEO
COMMENTS
The. Patient Journey. Course. ! Increase Conversions With Each Patient You See, Everyday, In Any Scenario, With Confidence, Authority And No Hesitation. Learn More. Communications & Case Acceptance Masterclass.
In Module 6 of our patient journey course, we dive into the intricacies of operating a mixed practice and achieving patient journey perfection within the NHS system. This module is designed to equip you with the necessary knowledge and skills to seamlessly convert NHS patients to private patients while presenting both options in a persuasive ...
Communications & Case Acceptance Masterclass.
The patient journey is a challenging example of using a systems approach. The inclusion of the patient's viewpoint and experience about their health journey throughout the time of care and across all the care settings represents a key factor in improving patient safety. ... The Importance of Training Courses to Empower Patients. Over the last ...
What is the patient journey? The patient journey is the sequence of events that begins when a patient first develops a need for care. Rather than focusing on service delivery, the patient journey encompasses all touchpoints of a patient's healthcare experience-from locating healthcare providers and scheduling appointments, to paying the bill and continuing their care after treatment.
The course has an estimated 60 hours of guided learning. IHLM Professional Certificate in Patient Experience and Service Excellence - This is evidence of the advanced patient experience capabilities you've developed during the course. The award of a professional certificate requires completion of learning activities and mini-projects during ...
The patient journey is best described as the sequence of experiences a patient has from admission to discharge. This includes all the touchpoints between the patient and provider from beginning to end. ... Check-in, check-out, admissions, discharge, billing, and of course, the actual visit with the healthcare provider are other touchpoints in ...
This 1.5-day course draws on expertise from the Maudsley Hospital, employing interactive, case-based learning to facilitate an understanding of the perspectives of both service users and clinicians operating in this domain. ... Describe the typical patient journey in the diagnosis and treatment of MDD in real-world practice.
An analysis of the patient journey revealed 3 critical needs for a more patient-centered process: (1) making the patient health goal visible; (2) instigating transparent, shared decision-making; and (3) using a closed-loop communication process. ... TeamSTEPPS Fundamentals Course: Module 3. Evidence-Based: communication. Agency for Healthcare ...
The patient journey is a challenging example of using a systems approach. The inclusion of the patient's viewpoint and experience about their health journey throughout the time of care and across all the care settings represents a key factor in improving patient safety. ... The chapter offers examples of successful training courses designed ...
In this course, you will have an opportunity to explore concepts and topics related to improving the patient experience and reducing pain points in healthcare processes through analytic and decision support frameworks. ... Then we'll examine the patient journey and what impact these trends have on this journey. Then, we will discuss the issues ...
The patient journey is a continuous process that involves every event a patient experiences over the course of their care with a particular provider or healthcare organization. Everyone who has contact with a patient can impact their patient journey. The patient journey begins when a patient decides to seek care and completes a cycle with final ...
Therefore, hospitals can significantly improve the quality of the service provided by exploring and understanding the individual patient journey [ 12 - 14 ]. Many tools may be used to measure and understand patient experience [ 15, 16 ]. Surveys are the methods mainly used to capture the patient experience and to evaluate the quality and ...
Subscribe today to gain access to this course and 230+ other courses, or get the Pro for Dentists pack to gain access to an additional 100 courses. Essentials £42. ... The aim of this course is to explain the important elements of the patient journey and enable team members to plan, create, and implement an effective patient journey handbook. ...
Abstract. Patient mapping or patient journey, a tool used to visualize the patient journey, is beneficial in understanding the patient's experience with healthcare. It highlights what contributes to good care and what does not from the patient's perspective. Additionally, the concept of the patient journey is used in the context of quality ...
INTRODUCTION. Medical researchers have long pointed to the importance of understanding the realistic picture of the patient journey: the chronological sequence of how a patient seeks and receives care from the healthcare system. 1, 2 Capturing an accurate overview of the patient journey can help identify sources of variability, evaluate why patients respond differently to the same overarching ...
Engaging consumers and patients where they are builds trust and confidence that keeps patients in the system and encourages them to refer their friends and family to your practice. According to the Beryl Institute, 70% of patients will share a positive experience with others. But your bigger risk is that 76% will share a negative one.
Therefore, hospitals can significantly improve the quality of the ser-vice provided by exploring and understanding the individual patient journey [12-14]. Many tools may be used to measure and understand patient experience [15, 16]. Surveys are the methods mainly used to capture the patient experience and to evaluate the quality and safety of ...
4. Identify Contact Channels. Patients engage with the health center through various channels throughout the patient journey. These channels, such as the health center itself, can be physical or online, including social media, email, applications, websites, and online forms.
The patient journey is a challenging example of using a systems approach. ... The chapter offers examples of successful training courses designed to foster strategic alliances among healthcare ...
The promotion of systems-based approaches offers methods and tools to improve the safety of care. A multidisciplinary perspective must include the involvement of patients and citizens as fundamental contributors to the design, implementation, and delivery of health services. The patient journey is a challenging example of using a systems approach.
Objective: The term 'patient journey' refers to the experiences and processes the patient goes through during the course of a disease and its treatment. The study explores the perspectives of adults with acquired hearing impairment and to further develop the patient journey template based on the Ida model. Design: Qualitative approach using ...
This course is designed to introduce you to the basic principles and practices of Good Clinical Practice (GCP), which are essential for conducting clinical trials and ensuring the safety and well-being of human subjects. Whether you are new to the field or seeking to refresh your knowledge, this course and its sequel courses covering the ...
Ramani Durvasula uses "journey" advisedly. A clinical psychologist in Los Angeles who treats women in emotionally abusive relationships, she recognizes how "journey" has been "eye ...
It also aims to improve the ability of healthcare professionals to identify and manage these patients. Objectives: At the conclusion of the course, the participants will be able to: Explain two facts about the physiology of thrombus formation and the pathogenesis of VTE. Describe three risk factors for VTE. Describe three VTE prevention options.
The Experience Journey of the Patient. A recurrent and prominent theme in discussions of the patient experience is centering the patient's perception or perspective on the health care they receive (7,13).Health-care providers who seek to understand the patient's perspective of their experience will obtain a greater understanding of the patient experience.
TikToker Kimberley Nix, who documented her three year journey with metastatic sarcoma, has died at the age of 31. ... my husband first and of course all of my family and friends."
A mother's calling: a journey from epilepsy patient to parent. It was 2006, a softball game in Mobile, Alabama, was in full swing, and 10-year-old Cathryn Cazalas was experiencing her first seizure. Little did she know, she would end up at Children's of Alabama five years later taking her first steps on a long road to recovery.
The U.S. Food and Drug Administration gave a green light to Elon Musk 's Neuralink to implant its brain chip in a second person, signing off on the company's proposed fixes for a problem that ...
Kendric Cromer, 12, the first commercial patient for Bluebird Bio's gene therapy to cure his sickle cell disease, in the hospital as his bone marrow stem cells were being removed for gene editing.