You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.

Pregnant Travelers

Pregnant travelers can generally travel safely with appropriate preparation. But they should avoid some destinations, including those with risk of Zika and malaria. Learn more about traveling during pregnancy and steps you can take to keep you and your baby healthy.
Before Travel
Before you book a cruise or air travel, check the airlines or cruise operator policies for pregnant women. Some airlines will let you fly until 36 weeks, but others may have an earlier cutoff. Cruises may not allow you to travel after 24–28 weeks of pregnancy, and you may need to have a note from your doctor stating you are fit to travel.
Zika and Malaria
Zika can cause severe birth defects. The Zika virus is spread through mosquito bites and sex. If you are pregnant, do not travel to areas with risk of Zika . If you must travel to an area with Zika, use insect repellent and take other steps to avoid bug bites. If you have a sex partner who lives in or has traveled to an area with Zika, you should use condoms for the rest of your pregnancy.
Pregnant travelers should avoid travel to areas with malaria, as it can be more severe in pregnant women. Malaria increases the risk for serious pregnancy problems, including premature birth, miscarriage, and stillbirth. If you must travel to an area with malaria, talk to your doctor about taking malaria prevention medicine. Malaria is spread by mosquitoes, so use insect repellent and take other steps to avoid bug bites.
Make an appointment with your healthcare provider or a travel health specialist that takes place at least one month before you leave. They can help you get destination-specific vaccines, medicines, and information. Discussing your health concerns, itinerary, and planned activities with your provider allows them to give more specific advice and recommendations.
Plan for the unexpected. It is important to plan for unexpected events as much as possible. Doing so can help you get quality health care or avoid being stranded at a destination. A few steps you can take to plan for unexpected events are to get travel insurance , learn where to get health care during travel , pack a travel health kit , and enroll in the Department of State’s STEP .
Be sure your healthcare policy covers pregnancy and neonatal complications while overseas. If it doesn’t get travel health insurance that covers those items. Consider getting medical evacuation insurance too.
Recognize signs and symptoms that require immediate medical attention, including pelvic or abdominal pain, bleeding, contractions, symptoms of preeclampsia (unusual swelling, severe headaches, nausea and vomiting, and vision changes), and dehydration.
Prepare a travel health kit . Pregnant travelers may want to include in your kit prescription medications, hemorrhoid cream, antiemetic drugs, antacids, prenatal vitamins, medication for vaginitis or yeast infection, and support hose, in addition to the items recommended for all travelers.
During Travel
Your feet may become swollen on a long flight, so wear comfortable shoes and loose clothing and try to walk around every hour or so. Sitting for a long time, like on long flight, increases your chances of getting blood clots, or deep vein thrombosis. Pregnant women are also more likely to get blood clots. To reduce your risk of a blood clot, your doctor may recommend compression stockings or leg exercises you can do in your seat. Also, see CDC’s Blood Clots During Travel page for more tips on how to avoid blood clots during travel.
Choose safe food and drink. Contaminated food or drinks can cause travelers’ diarrhea and other diseases and disrupt your travel. Travelers to low or middle income destinations are especially at risk. Generally, foods served hot are usually safe to eat as well as dry and packaged foods. Bottled, canned, and hot drinks are usually safe to drink. Learn more about how to choose safer food and drinks to prevent getting sick.
Pregnant women should not use bismuth subsalicylate, which is in Pepto-Bismol and Kaopectate. Travelers to low or middle income destinations are more likely to get sick from food or drinks. Iodine tablets for water purification should not be used since they can harm thyroid development of the fetus.
After Travel

If you traveled and feel sick, particularly if you have a fever, talk to a healthcare provider immediately, and tell them about your travel. Avoid contact with other people while you are sick.
More Information
CDC Yellow Book: Pregnant Travelers
File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file

Traveling Abroad while Pregnant: Firsthand Advice from a Pregnant Travel Addict
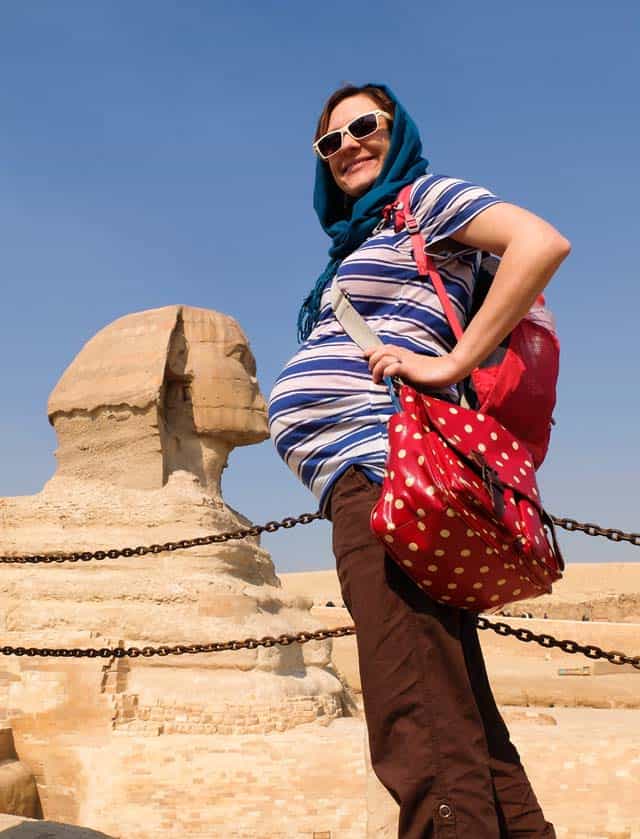
When I told people that I was planning to travel to a foreign country while 7 months pregnant, I got looked at like I was crazy. The look turned into shock when they heard I was going to a developing country: Egypt.
“Is it safe to travel while pregnant?”
“Can you fly while pregnant?”
“What if something happens???”
There are some legit concerns about traveling abroad while pregnant – but those can easily be addressed by making some smart travel choices and precautions.
This is NOT Your Last Chance to Travel
Apparently, most people believe that their lives come to a screeching halt once they have a baby. They have to travel “while they still can.” There is even a name for these pregnancy holidays – a “ babymoon .”
Fear that this is your “last chance to travel” is a terrible reason to plan a trip!!!
It is perfectly possible to travel with a baby . In some ways, traveling with a baby is even more fun (such as how you get priority treatment and meet locals easier). So don’t feel pressured to rush out and take a trip “while you still can.” There will be plenty of opportunities to travel later on.

Get the Timing Right
I am one of those unlucky women who gets hyperemesis gravidarum during pregnancy. Don’t confuse HG with morning sickness. I’m talking about puking blood because the vomit has eroded your throat. I’m talking about getting IV transfusions because I couldn’t keep water down…
So it was a bad mistake to go backpacking while 4 weeks pregnant . I ended up having to cut the trip short. It’s no fun puking all over the trail!!!
But, because this was my second pregnancy, I knew that I would probably stop puking at 6 months. So that’s when I planned my Egypt trip for.

You don’t know how you’ll feel as pregnancy progresses, so here’s what I’d recommend about planning a trip abroad:
- Go during months 6 or 7: In general, these are the best months for most pregnant women. The hormones and morning sickness have leveled off, but you aren’t so huge that you tire easily.
- Wait until the last minute to plan your trip: If possible, hold off on planning your trip until you know how you feel.
- Check refund policies: Most travel insurance policies don’t allow pregnancy as a reason for cancellation . So, be sure you understand cancellation/refund policies. Otherwise you’ll be out a lot of money if you decide to cancel the trip because you feel too crappy.
You Probably Can’t Get Travel Health Insurance while Pregnant
One of the biggest issues with traveling abroad while pregnant is that almost no travel insurance company will give coverage to pregnant women.
If something happens while on your trip, you’ll be stuck with the bill!
Consider the case of Jennifer Huculak-Kimmel and her “ million dollar baby .” The Canadian couple were on vacation in the USA when Jennifer went into premature labor. Two months in the ICU ran up a hospital bill of $950,000 – none of which was covered under her insurance policy!
I admit that the idea of being saddled with a huge hospital bill terrified me. Before going to Egypt, I intensely researched the cost of giving birth there, as well as how much a night in ICU would cost. Egypt is a poor country, so the costs weren’t too high – so I was willing to take the risk.
Know Airline Policies for Pregnant Women

Flying while pregnant is perfectly safe . The real reason that airlines put restrictions on flying while pregnant is because they are afraid you will give birth in the air.
Thus, a lot of airlines won’t let pregnant women fly after 36 weeks (or 32 weeks if you are having multiples). You may need a doctor’s note before being allowed to fly. This was the case with Air Cairo. The note had to be no more than 7 days old, so I actually had to visit a gynecologist while in Egypt – which was actually a cool part of the trip.
You can find a good breakdown on airline pregnancy restrictions here .
Choose the Right Climate
Since you are already going abroad, you might as well choose an agreeable climate! The entire reason we chose Egypt for our trip was because it was January.
While everyone else was battling snow, we were swimming in the Red Sea!
However, there is no way in hell that I’d go to Egypt in summer while pregnant. For a summer trip, I would have chosen a cooler country like Norway or gone into the mountains.

Only Plan ONE Activity Per Day
In general, I’m not the type of traveler who tries to see/do a zillion things. But I knew to take it even easier while pregnant.
I made a list of the things I absolutely wanted to do in each destination. Then planned to do just one per day. Some days we managed to do more than one thing, but only if I still felt up to it. This kept the pace relaxed so I didn't inadvertently overexert myself.
Consider the Bathroom Situation
One piece of travel advice for pregnant women which commonly gets overlooked is the bathroom situation. Since pregnancy makes you pee like crazy, this is not something which should not be overlooked.
Going to the bathroom actually ended up being the hardest part of traveling abroad while pregnant. After this ordeal, here’s what I’d recommend to other pregnant travelers:
- Make sure you can squat: Public bathrooms aren’t exactly known for their cleanliness – do you really want to sit on them? If you can’t squat over them, you are going to be in for some trouble. Squats are great exercises for preparing for childbirth anyway. 😉
- Consider a pee funnel: If you can’t squat, then get a pee funnel . This makes it possible to pee standing up.
- Map out some nicer restaurants: As is the case in many developing countries, it was very hard to find a bathroom in Egypt. The local restaurants didn’t have bathrooms (seriously!) and cafes usually only had a bathroom for men (which might just be a bucket in a corner!!!). The tourist restaurants consistently had nice bathrooms, so I mapped these out so I knew where to go to pee.
- Carry TONS of wet wipes and antiseptic gel: Once you have a baby, you’ll be carrying tons of these anyway. 🙂 For traveling abroad, these come in handy for wiping down disgusting surfaces and sanitizing your hands – don’t expect soap in every bathroom!

Budget for Luxury Transportation
Normally I’m fine taking cramped minibuses and crowded trains. But, at 7 months pregnant, I wasn’t keen about shoving into Egypt’s crowded local transportation.
It probably would have ended with me puking or passing out. Or, worse, someone banging into my stomach.
Luckily we were able to afford taxis everywhere (we used Uber to avoid haggling with the crooked taxi drivers). We took things a step further and even hired a private driver to take us between cities.
Since it was Egypt (and not, for example, Norway), it wasn’t too expensive. In developed countries, this sort of luxury travel will definitely cost more.
Even a short taxi ride each day in somewhere like Europe can add a huge amount to your travel budget. But in developed countries the public transportation won’t be as crazy. So really think about the cost vs. hassle of public transport and budget your trip accordingly.

Some Activities Will Be Off-Limits While Traveling Pregnant
In the weeks before my Egypt trip, I was Googling things like “Can you ride a camel while pregnant?”
It turns out that riding a camel is a relatively safe activity while pregnant (riding a horse, however, is not). But, to play it safe, I still decided not to ride a camel while at the pyramids.
I also had to pass on sandboarding, quad biking, and going into certain tombs (because of low oxygen levels inside). Unfortunately, it was only after I got into a jeep on our excursion into the desert that I realized that off-roading might be off-limits too! Luckily, the ride wasn't too bumpy — but I still held on tightly to prevent my stomach from getting bounced too much.

Playing It Safe with Food while Pregnant
Another major concern I had about traveling to Egypt (or any developing country) while pregnant was getting a stomach bug from tainted water or food.
Most of the time, food poisoning while pregnant isn’t particularly danger. The biggest risk is that you’ll get dehydrated.
The best thing to do is avoid food poisoning in the first place:
- Only drink safe water. I stuck to bottled water. I also have a Sawyer Mini water filter in case bottled water isn’t available.
- Remember to avoid ice cubes and juices too! Unless you know these were made with safe water, don’t drink them.
- Be cautious about street food. My doctor told me to not eat any street food. But that’s half the fun of traveling abroad! So I instead was careful about the street food I ate. I stuck with thing that were deep fried since this would have killed most bacteria. I’m vegetarian, but would have avoided all street meat regardless.
- Take probiotics the first few days. This will help your body adjust to and combat any “bad” bacteria it comes in contact with.
In case you do develop a stomach bug, the CDC says it is best to wait for it to go away on its own (if it’s severe, that’s when you’ll want to contact a doctor). You’ll need to stay hydrated while waiting for the diarrhea and vomiting to subside.
My traveler’s first aid kit is always stockpiled with electrolytes. It also has activated charcoal and other remedies for food poisoning.

Enjoy the Memories
Taking a trip while I was 7 months pregnant was by far the best decision I made – for both me and my family.
It was a much-needed break from all the pregnancy woes. For the first time in months, I stopped frantically Googling everything pregnancy related. I was able to RELAX and enjoy myself!
Even more importantly, I was able to spend some quality time with my husband and older daughter.
If I had a high-risk pregnancy, then I wouldn’t have done the trip. But for any other pregnant travel addicts who need a break from focusing on their growing baby, a trip is great for your mental health.
My only regret is that I didn’t take more photos using my bump. It would have been great to have a funny picture of my belly with a pyramid coming out of it. 🙂
Have you traveled abroad while pregnant? What tips would you add?
Image credit: squat toilet , by Maksym Kozlenko , Creative Commons Attribution-Share Alike 4.0 International license
Sharing is caring!
1 thought on “Traveling Abroad while Pregnant: Firsthand Advice from a Pregnant Travel Addict”
Pingback: Traveling Abroad while Pregnant: Firsthand Advice from a Pregnant Travel Addict – Cuddle Baby
Comments are closed.
Travelling in pregnancy
With the proper precautions such as travel insurance, most women can travel safely well into their pregnancy.
Wherever you go, find out what healthcare facilities are at your destination in case you need urgent medical attention. It's a good idea to take your maternity medical records (sometimes called handheld notes) with you so you can give doctors the relevant information if necessary.
Find out more about getting healthcare abroad .
Make sure your travel insurance covers you for any eventuality, such as pregnancy-related medical care during labour, premature birth and the cost of changing the date of your return trip if you go into labour .
When to travel in pregnancy
Some women prefer not to travel in the first 12 weeks of pregnancy because of nausea and vomiting and feeling very tired during these early stages. The risk of miscarriage is also higher in the first 3 months, whether you're travelling or not.
Travelling in the final months of pregnancy can be tiring and uncomfortable. So, many women find the best time to travel or take a holiday is in mid-pregnancy, between 4 and 6 months.
Flying in pregnancy
Flying isn't harmful to you or your baby, but discuss any health issues or pregnancy complications with your midwife or doctor before you fly.
The chance of going into labour is naturally higher after 37 weeks (around 32 weeks if you're carrying twins), and some airlines won't let you fly towards the end of your pregnancy. Check with the airline for their policy on this.
After week 28 of pregnancy, the airline may ask for a letter from your doctor or midwife confirming your due date, and that you are not at risk of complications. You may have to pay for the letter and wait several weeks before you get it.
Long-distance travel (longer than 4 hours) carries a small risk of blood clots (deep vein thrombosis (DVT)) . If you fly, drink plenty of water and move about regularly – every 30 minutes or so. You can buy a pair of graduated compression or support stockings from the pharmacy, which will help reduce leg swelling.
Travel vaccinations when you're pregnant
Most vaccines that use live bacteria or viruses aren't recommended during pregnancy because of concerns that they could harm the baby in the womb.
However, some live travel vaccines may be considered during pregnancy if the risk of infection outweighs the risk of live vaccination. Ask your GP or midwife for advice about specific travel vaccinations. Non-live (inactivated) vaccines are safe to use in pregnancy.
Malaria tablets
Some anti-malaria tablets aren't safe to take in pregnancy so ask your GP for advice.
Zika virus is mainly spread by mosquitoes found in some parts of the world. For most people it's mild and not harmful, but can cause problems if you're pregnant.
If you are pregnant, it is not recommended to travel to parts of the world where the Zika virus is present, such as parts of:
- South and Central America
- the Caribbean
- the Pacific islands
Check before you travel
It's important to check the risk for the country you're going to before you travel.
Find out more about the Zika virus risk in specific countries on the Travel Health Pro website
Car travel in pregnancy
It's best to avoid long car journeys if you're pregnant. However, if it can't be avoided, make sure you stop regularly and get out of the car to stretch and move around.
You can also do some exercises in the car (when you're not driving), such as flexing and rotating your feet and wiggling your toes. This will keep the blood flowing through your legs and reduce any stiffness and discomfort. Wearing compression stockings while on long car journeys (more than 4 hours) can also increase the blood flow in your legs and help prevent blood clots.
Tiredness and dizziness are common during pregnancy so it's important on car journeys to drink regularly and eat natural, energy-giving foods, such as fruit and nuts.
Keep the air circulating in the car and wear your seatbelt with the cross strap between your breasts and the lap strap across your pelvis under your bump, not across your bump.
Road accidents are among the most common causes of injury in pregnant women. If you have to make a long trip, don't travel on your own. You could also share the driving with your companion.
Sailing in pregnancy
Ferry companies have their own restrictions and may refuse to carry heavily pregnant women (often beyond 32 weeks on standard crossings and 28 weeks on high-speed crossings ). Check the ferry company's policy before you book.
For longer boat trips, such as cruises, find out if there are onboard facilities to deal with pregnancy and medical services at the docking ports.
Food and drink abroad in pregnancy
Take care to avoid food- and water-borne conditions, such as stomach upsets and travellers' diarrhoea . Some medicines for treating stomach upsets and travellers' diarrhoea aren't suitable during pregnancy.
Always check if tap water is safe to drink. If in doubt, drink bottled water. If you get ill, keep hydrated and continue eating for the health of your baby, even if you're not hungry.
Find out about a healthy diet in pregnancy , and foods to avoid in pregnancy .
Page last reviewed: 17 August 2022 Next review due: 17 August 2025
Health Encyclopedia
International travel while pregnant or breastfeeding, special considerations for traveling while pregnant.
Traveling during pregnancy is normal, and a lot of women do it. But it's important to think about potential problems that could come up during international travel. Also think about how you would get quality healthcare in the countries you are visiting. Get all of the vaccines you need before becoming pregnant instead of waiting to get them during pregnancy.
The American College of Obstetricians and Gynecologists says the safest time for a woman to travel is in the second trimester of her pregnancy, from 14 to 28 weeks. This is the time when you will feel your best. You are also at the lowest risk for spontaneous abortion (miscarriage) or premature labor. During the third trimester (28 to 40 weeks), many healthcare providers and midwives advise staying within a 300-mile radius of home because of potential problems, such as high blood pressure, phlebitis, and false or preterm labor. Generally, women are not allowed to travel by air after 36 weeks for domestic travel, and after 28 to 35 weeks for international travel. The decision on whether to travel and how far to travel at any time during pregnancy should be a joint decision between you and your healthcare provider.
For most pregnant women, flying does not pose a risk to the fetus from cosmic radiation. But aircrew and women who often fly may exceed radiation limits.
According to the CDC, pregnant women with the following conditions may be advised against traveling to countries that need pretravel vaccines. This list may be incomplete. So discuss your health history with your provider or midwife before planning travel:
History of miscarriage
Incompetent cervix
History of ectopic pregnancy
History of premature labor or premature rupture of membranes
History of or current placental abnormalities
Threatened miscarriage or vaginal bleeding during current pregnancy
Multiple fetuses in current pregnancy
History of pre-eclampsia, high blood pressure, or diabetes with any pregnancy
History of infertility or trouble getting pregnant
Pregnancy for the first time over the age of 35 years
Heart valve disease or congestive heart failure
History of blood clots
Severe anemia
Chronic organ system problems that need to be treated
You may also be advised against traveling to places that may have hazards. The list below may be incomplete. Talk about your travel plans with your healthcare provider or midwife before planning a trip.
Places with high altitudes
Places that have outbreaks of life-threatening food- or insect-borne infections
Places where malaria is common
Places where live-virus vaccines are needed or recommended
Healthy tips for traveling while pregnant
Here are tips for traveling while pregnant:
Try to plan ahead for any problems or emergencies that could come up before you travel. Check that your health insurance is valid while you are abroad. Also check to see whether the plan will cover a newborn, should you deliver while away. You may want to think about getting a supplemental travel and medical evacuation insurance.
Research medical facilities in your destination. Women in the last trimester of pregnancy should look for places that can manage complications of pregnancy, pre-eclampsia, and cesarean sections.
If you will need prenatal care while you are abroad, arrange for this before you leave. Talk with your healthcare provider or midwife to figure out the best way to handle this.
Know your blood type and check that blood is screened for HIV and hepatitis B in the areas you will be visiting.
Check that safe food and beverages, such as bottled water and pasteurized milk, are available at your destinations.
If flying, ask for an aisle seat at the bulkhead. This gives you the most space and comfort. If morning sickness is a problem, try to arrange travel during a time of day when you generally feel well. Seats over the wing in the midplane region will give you the smoothest ride.
Try to walk every half-hour during a smooth flight. Flex and extend your ankles often to prevent blood clots in the veins (thrombophlebitis).
Fasten your seat belt at the pelvis level, below your hips.
Drink plenty of fluids to stay hydrated. Aircraft cabins have low humidity.
Try to rest as much as possible while away. Exercise and activity during pregnancy are important but try not to overdo it.
Special considerations for traveling while breastfeeding
Breastfeeding gives babies the most nutritional start in life. It also gives them vital protection against certain infections. But traveling internationally while nursing can be challenging.
If you are breastfeeding only, you don't have to worry about sterilizing bottles or having clean water. You may get vaccines to protect against disease, depending on where you are traveling. But diseases such as yellow fever, measles, and meningococcal meningitis may be a threat to infants who can't be vaccinated at birth. Discuss this with both your healthcare provider and your infant's caregiver before you travel.
If you are feeding your baby formula, it's best to use powdered formula made with boiled water. You may also want to carry a supply of prepared infant formula in cans or ready-to-feed bottles for emergencies.
Breastfeeding helps lower the chance of your baby getting traveler's diarrhea. If you get traveler's diarrhea, drink more fluids and continue to nurse your baby.
Watch your eating and sleeping patterns, as well as your stress levels. This will affect your milk output. Drink more fluids. Stay away from alcohol and caffeine, as well as exposure to smoke.
If you are traveling without your infant, you will need to pump to maintain your milk supply. Check with TSA about transporting your milk on flights.
Medical Reviewers:
- Donna Freeborn PhD CNM FNP
- Heather M Trevino BSN RNC
- Michele Burtner CNM
- Ask a Medical Librarian Make an Appointment Interactive Tools International Travel Quiz

- Pregnancy Classes

Travel During Pregnancy
As long as there are no identified complications or concerns with your pregnancy, it is generally safe to travel during your pregnancy. The ideal time to travel during pregnancy is the second trimester . In most cases, you are past the morning sickness of the first trimester and several weeks from the third stage of pregnancy when you are more easily fatigued .
Is it safe to travel during pregnancy?
Traveling by air is considered safe for women while they are pregnant; however, the following ideas might make your trip safer and more comfortable.
- Most airlines allow pregnant women to travel through their eighth month. Traveling during the ninth month is usually allowed if there is permission from your health care provider.
- Most airlines have narrow aisles and smaller bathrooms, which makes it more challenging to walk and more uncomfortable when using the restroom. Because of potential turbulence that could shake the plane, make sure you are holding on to the seatbacks while navigating the aisle.
- You may want to choose an aisle seat which will allow you to get up more easily to reach the restroom or just to stretch your legs and back.
- Travel on major airlines with pressurized cabins and avoid smaller private planes. If you must ride in smaller planes, avoid altitudes above 7,000 feet.
- Although doubtful, the risk of DVT can be further reduced by wearing compression stockings.
The Royal College of Obstetricians and Gynaecologists and the International Air Travel Association recommend that expecting mothers in an uncomplicated pregnancy avoid travel from the 37th week of pregnancy through birth. Avoiding travel from 32 weeks through birth is recommended for women who have complicated pregnancies with risk factors for premature labor, such as mothers carrying multiples.
Risk factors that warrant travel considerations include the following:
- Severe anemia
- Cardiac disease
- Respiratory disease
- Recent hemorrhage
- Current or recent bone fractures
Traveling by Sea During Pregnancy
Traveling by sea is generally safe for women while they are pregnant; the motion of the boat may accentuate any morning sickness or make you feel nauseous all over again. There are a few considerations to make your trip safer and more comfortable:
- Check with the cruise line to ensure that there is a health care provider on board in case there are any pregnancy complications .
- Review the route and port-of-calls to identify if there is access to any medical facilities if needed.
- Make sure any medications for seasickness are approved for women who are pregnant and that there is no risk to the developing baby.
- Seasickness bands use acupressure points to help prevent upset stomach and maybe a good alternative to medication.
International Travel During Pregnancy
Traveling overseas has the same considerations that local or domestic travel has, but it also has additional concerns that you need to know about before making an international trip. The information below is provided to help you assess whether an international trip is good for you at this time:
- It is important to talk with your health care provider before you take a trip internationally to discuss safety factors for you and your baby.
- Discuss immunizations with your health care provider and carry a copy of your health records with you.
- With international travel, you may be exposed to a disease that is rare here in the United States but is common in the country you visit.
- Contact the Centers for Disease Control and Prevention at (800) 311-3435 or visit their website at www.cdc.gov to receive safety information along with immunization facts related to your travels.
- Diarrhea is a common concern when traveling overseas because you may not be used to the germs and organisms found in the food and water of other countries. This can lead to a problem of dehydration .
Here are some tips to avoid diarrhea and help keep you safe:
- Drink plenty of bottled water
- Used canned juices or soft drinks as alternatives
- Make sure the milk is pasteurized
- Avoid fresh fruits and vegetables unless they have been cooked or can be peeled (such as an orange or a banana)
- Make certain that all meat and fish has been cooked completely; if you are unsure, do not eat it
Travel Tips During Pregnancy
Whether you are going by car, bus, or train, it is generally safe to travel while you are pregnant; however, there are some things to consider that could make your trip safer and more comfortable.
- It is essential to buckle-up every time you ride in a car. Make sure that you use both the lap and shoulder belts for the best protection of you and your baby.
- Keep the airbags turned on. The safety benefits of the airbag outweigh any potential risk to you and your baby.
- Buses tend to have narrow aisles and small restrooms. This mode of transportation can be more challenging. The safest thing is to remain seated while the bus is moving. If you must use the restroom, make sure to hold on to the rail or seats to keep your balance.
- Trains usually have more room to navigate and walk. The restrooms are usually small. It is essential to hold on to rails or seat backs while the train is moving.
- Try to limit the amount of time you are cooped up in the car, bus, or train. Keep travel time around five to six hours.
- Use rest stops to take short walks and to do stretches to keep the blood circulating.
- Dress comfortably in loose cotton clothing and wear comfortable shoes.
- Take your favorite pillow.
- Plan for plenty of rest stops, restroom breaks and stretches.
- Carry snack foods with you.
- If you are traveling any distance, make sure to carry a copy of your prenatal records.
- Enjoy the trip.
Want to Know More?
- How to Treat Jet Lag Naturally During Pregnancy
Compiled using information from the following sources:
1. Planning Your Pregnancy and Birth Third Ed. The American College of Obstetricians and Gynecologists, Ch. 5. William’s Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 8.
2. Royal College of Obstetricians and Gynaecologists, Air Travel and Pregnancy (Scientific Impact Paper No. 1), https://www.rcog.org/uk, May 22, 2013.
BLOG CATEGORIES
- Pregnancy Symptoms 5
- Can I get pregnant if… ? 3
- Paternity Tests 2
- The Bumpy Truth Blog 7
- Multiple Births 10
- Pregnancy Complications 68
- Pregnancy Concerns 62
- Cord Blood 4
- Pregnancy Supplements & Medications 14
- Pregnancy Products & Tests 8
- Changes In Your Body 5
- Health & Nutrition 2
- Labor and Birth 65
- Planning and Preparing 24
- Breastfeeding 29
- Week by Week Newsletter 40
- Is it Safe While Pregnant 55
- The First Year 41
- Genetic Disorders & Birth Defects 17
- Pregnancy Health and Wellness 149
- Your Developing Baby 16
- Options for Unplanned Pregnancy 18
- Child Adoption 19
- Fertility 54
- Pregnancy Loss 11
- Uncategorized 4
- Women's Health 34
- Prenatal Testing 16
- Abstinence 3
- Birth Control Pills, Patches & Devices 21
- Thank You for Your Donation
- Unplanned Pregnancy
- Getting Pregnant
- Healthy Pregnancy
- Privacy Policy
- Pregnancy Questions Center
Share this post:
Similar post.

Pregnancy and Ice Cream

Preconception Wellness - Prepare for the Unexpected

Leg Cramps During Pregnancy
Track your baby’s development, subscribe to our week-by-week pregnancy newsletter.
- The Bumpy Truth Blog
- Fertility Products Resource Guide
Pregnancy Tools
- Ovulation Calendar
- Baby Names Directory
- Pregnancy Due Date Calculator
- Pregnancy Quiz
Pregnancy Journeys
- Partner With Us
- Corporate Sponsors
9 Tips for Traveling While Pregnant
An ob-gyn shares advice about traveling while pregnant and what you can do to stay safe..
Save this to read later.

For many, the holiday season is a time to travel and gather with family and friends. For expectant mothers, holiday travel, coupled with the ongoing challenges posed by the flu, RSV (respiratory syncytial virus), and COVID-19, can introduce a unique set of considerations and uncertainties. Traveling while pregnant may require some extra precautions to ensure their comfort and safety as well as the baby’s safety.
“For those with a low-risk pregnancy, travel is generally considered safe,” says Dr. Cassandra Simmons , division chief of General Obstetrics & Gynecology at NewYork-Presbyterian Westchester. “Most patients should feel comfortable benefiting from the positive aspects of travel during holidays — by car or by plane — and be able to enjoy their time with friends and family.”
Health Matters spoke with Dr. Simmons to learn what advice she has for people traveling while pregnant.

Dr. Cassandra Simmons
1. Check in with your doctor before traveling.
Travel is not recommended for those with certain complications, such as preeclampsia , preterm labor, or pre-labor rupture of membranes (PROM).
According to Dr. Simmons, there may be slightly higher risk associated with traveling in the first trimester (when there is a greater risk of bleeding) and the third trimester (when you’re closer to delivery). Most doctors advise a pregnant person not to fly by commercial flight after 36 weeks of pregnancy. In fact, most airlines restrict air travel for pregnant people if they are close to their due date. “As one approaches their due date, the risk of labor exists, and medical care in flight is limited or not available at all,” says Dr. Simmons.
2. Plan for unexpected situations.
Locate the closest obstetric healthcare provider and hospital, regardless of where you’re traveling. “When traveling domestically and internationally, you should ensure that there are options for obstetric care near your destination so that you have a place to go if you experience unexpected symptoms related to your pregnancy while traveling,” says Dr. Simmons.
3. Stay up to date on vaccinations.
Make sure you’re up to date on your flu and COVID-19 vaccines. If you plan to travel internationally, keep in mind that some countries require specific vaccines. While some vaccines are safe during pregnancy, others may not be. “Communicate with your provider as to what vaccines are recommended based on the country to which you plan to travel,” says Dr. Simmons.
4. Take extra precautions when traveling internationally.
It’s best to avoid areas with a high risk of infectious diseases — such as malaria or Zika, two mosquito-borne diseases. Check the Centers for Disease Control and Prevention (CDC) website for current information on countries where Zika and malaria are reported. Dr. Simmons reminds pregnant people that “the main way to mitigate risk with regard to malaria and Zika is to avoid infection altogether.”
If you absolutely must travel to areas where malaria and Zika are reported, you will need to use long-acting insect repellents that are safe for use while pregnant, like EPA-registered bug spray with DEET, picaridin, IR3535, or oil of lemon eucalyptus. Wear long-sleeved shirts and pants to protect against mosquito bites. If you’re going to a malaria-endemic area, your doctor will prescribe anti-malarial pills that are safe during pregnancy.
If you’re in a country where tap water is unsafe to drink, remember to stick with bottled water — even for things like brushing your teeth — to reduce the risk of gastrointestinal (GI) infection.
5. Wear your seat belt low and snug across your hips, not over your belly.
“For comfort and safety, avoid placing your seat belt on top of your pregnant abdomen,” says Dr. Simmons. It should be worn under your belly, just above your hips.
6. If you’re on a long flight or long car ride, get up and move often to help prevent blood clots.
During pregnancy, you are at an increased risk of developing what is called deep vein thrombosis (a blood clot in a deep vein in the body, like in the leg). Sitting for too long, as during a car or plane ride, can exacerbate blood clots. “Avoid sitting or standing in one position for extended periods,” explains Dr. Simmons. Anything you can do to improve blood flow helps. For flights, stand and walk up and down the aisle of the plane every hour. Choosing an aisle seat may make it easier to get up often. For long car rides, try and stop every hour to stretch your legs. If you can’t get up and walk around, “even calf raises in your seat help with circulation when you are sedentary during travel,” says Dr. Simmons.
“Wearing compression socks is another way to promote circulation while on a long trip,” adds Dr. Simmons. These tight-fitting socks reach up to the knees and help with blood flow and circulation.
"Most patients should feel comfortable benefiting from the positive aspects of travel during holidays — by car or by plane — and be able to enjoy their time with friends and family." — Dr. Cassandra Simmons
7. Be prepared with comfortable clothing, snacks, water, and anti-nausea medicines.
Whether you have a two-hour drive or a six-hour flight ahead of you, wear comfortable clothing and shoes. Keep snacks and water on hand as well, “to stay hydrated and keep up with the metabolic demands of being pregnant,” says Dr. Simmons. And if you’re feeling nauseous or have GI discomfort while traveling, Reglan, Dramamine, and Imodium are considered safe to take while pregnant.
8. Mask up and use hand sanitizer.
“I advise my pregnant patients to wear a mask when traveling or when in the presence of large crowds, as an added precaution for safety for themselves and their unborn babies,” says Dr. Simmons. Because COVID-19, RSV, and the flu are all airborne viruses — meaning they spread through tiny respiratory droplets in the air — wearing a mask adds a layer of protection. You may also want to ask family members, friends, and loved ones to take a COVID-19 test prior to large gatherings.
And don’t forget to wash your hands and use hand sanitizer often. Keep sanitizer handy, especially if you are traveling with young children. Keep their hands sanitized as well to help keep your family safe.
9. Upon arrival, avoid any unsafe activities.
“It’s important that you enjoy your planned activities, but try and avoid adventures that may significantly increase your risk of trauma while pregnant,” says Dr. Simmons. For example, if you’re going to an amusement park or participating in an activity that could put you at risk of falling or for sudden jerky movements (like skiing or other high-impact sports), it’s important to proceed cautiously. Stick to lower-impact exercises and sports like jogging, walking, or swimming.
Cassandra Blot Simmons, M.D. , is chief of the Division of General Obstetrics & Gynecology at NewYork-Presbyterian Westchester and NewYork-Presbyterian/Columbia University Irving Medical Center. She is also an assistant professor of obstetrics and gynecology at Columbia University Vagelos College of Physicians and Surgeons. Dr. Simmons specializes in women’s gynecological health and obstetrics care before, during, and after pregnancy.
Additional Resources
Learn more about women’s health at NewYork-Presbyterian.
At A Glance
Featured expert.
Obstetrics & Gynecology
- Women's Health
Consult an Expert
Find a Doctor or call 877-697-9355
Share This Story
Get the latest health and wellness news.
Keep in touch with NewYork-Presbyterian and subscribe to our newsletter.
- Privacy Notice
Ready Steady Baby
Travelling when pregnant.
Whether you’re doing short journeys in the car or getting on a plane for a holiday abroad, it’s important to take extra care of yourself when you’re pregnant. Making a few small changes and planning ahead will help to make sure you have a comfortable and safe journey.
Wherever you’re going, it’s a good idea to take your maternity notes with you in case you need medical help.

It’s fine to drive or be a passenger in a car while you’re pregnant.
It’s important to wear a seat belt as you normally would. Make sure the straps don’t go over your bump by:
- placing the lap strap across your hips so it fits comfortably under your bump
- placing the diagonal strap between your breasts and around your bump
Take regular breaks when driving and make sure you bring some water and snacks with you for the journey.
Going on holiday or abroad
If you’re planning a holiday, seek health advice as early as possible.
You should give some thought to where you want to go as:
- the things you may normally love, like hot sunny weather, may not be a great idea if you’re uncomfortable or finding it hard to sleep
- you shouldn’t travel to areas where there’s malaria or the Zika virus if you can avoid it
You should also consider the quality of medical care in the country you plan to visit.
Fitfortravel has more advice for pregnant travellers
Staying safe on holiday
Activities like walking and swimming are fine while you’re pregnant, but it’s not a good idea to do any activity where you might fall.
Take care to avoid coming into contact with water or food that could cause tummy upsets. Some medicines for treating diarrhoea may not be suitable in pregnancy.
Talk to your midwife if you have questions.
Travel vaccinations
You’ll need vaccinations before you travel to certain countries.
There are some vaccinations you shouldn’t have when you’re pregnant, especially in the first 3 months, so always check before you book anything.
Find out which travel vaccinations you might need
Travel insurance
Before you travel, you’ll need special travel insurance that:
- covers any medical costs
- allows you to cancel for any issues with your pregnancy
If you don’t tell your insurer you’re pregnant before you travel, your insurance may not be valid.
If you’re travelling in Europe, the European Health Insurance Card (EHIC) may allow you to use the health services in these countries.
Apply for a European Health Insurance Card
Flying while pregnant
Air travel is generally safe if you’re having an uncomplicated pregnancy.
If you have any pregnancy complications, check with your midwife or GP that there’s no medical reason to stop you flying, such as high blood pressure or a risk of deep vein thrombosis .
Most airlines won’t let you fly if you’re within about a month of your due date. Some will need a letter from your GP or midwife saying you’re fit to fly when you’re 7 months pregnant. Check with the airline before you book.
Having a comfortable flight
When travelling by plane:
- drink plenty of water as you’re much more likely to get dehydration while flying.
- take healthy snacks with you so you can follow your own eating plan
- take whatever makes you more comfortable, such as an extra pillow or warm socks
Be aware it may take you a bit longer than before to recover from jet lag.
Deep vein thrombosis
Deep vein thrombosis (DVT) is a blood clot in a deep vein in your leg, calf or pelvis.
You’re more likely to get DVT if:
- you sit for long periods of time
- do very little activity
If you’re travelling on a long-distance flight or sitting for 4 hours or more, talk to your midwife as you may need medication. F ollow your midwife or doctor’s advice.
More about deep vein thrombosis
Further information, other languages and alternative formats
Translations and alternative formats of this information are available from Public Health Scotland .
If you need a different language or format, please contact [email protected].
- Ready Steady Baby leaflet in Arabic, Polish, Simplified Chinese (Mandarin) and Ukrainian
- Ready Steady Baby leaflet in English (Easy Read)
Source: Public Health Scotland - Opens in new browser window
Last updated: 14 December 2023

Help us improve NHS inform
Your feedback has been received
Don’t include personal information e.g. name, location or any personal health conditions.
Also on NHS inform
- Travel health and vaccinations
Other health sites
- fitfortravel: Advice for pregnant women
- Institute for Health Visiting: Travelling with your baby
- Disabled Living Foundation (DLF)
- Rica: consumer research charity
- Health & Care Professions Council (HCPC)

Flying while pregnant? Here’s what you need to know

Editors note: This guide has been updated with the latest information.
During pregnancy, seemingly harmless things like eating deli meat and cleaning your cat's litter box are suddenly off-limits, along with more obvious restrictions on sports like skiing and scuba diving.
But what about "grey area" activities like flying in an airplane?
There's no single set of guidelines governing air travel during pregnancy and every airline has different restrictions, timelines and requirements. Some airlines may also require a medical certificate from a primary attending doctor or midwife for air travel during the final months of pregnancy, though even that varies, with U.S. airlines typically offering more flexibility than international carriers.
For more TPG news delivered each morning to your inbox, sign up for our daily newsletter .
In the absence of clear guidelines, TPG turned to Dr. Nithya Gopal , a board-certified OB-GYN physician and the Director of OB-GYN services at Viva Eve in New York City, for her expert recommendations on safe air travel during pregnancy.
Here's what she had to say:
Is it safe to fly when you are pregnant?
There is no evidence of adverse pregnancy outcomes due to flying, according to Dr. Gopal.
"The general consensus is that it is safest to fly in the first and second trimesters," Dr. Gopal told The Points Guy. "While the first and third trimesters tend to be when the most obstetric emergencies are going to happen, I personally become more cautious with my patients after 32 weeks because of the increased risk for premature labor and the possibility of needing urgent medical attention when you are in the sky."

The most important thing you can do, no matter how far along you are in your pregnancy, is to consult with your healthcare provider before flying.
"Any time you are planning to fly during pregnancy , you should be having that conversation," Dr. Gopal said. Your provider will be familiar with any safety precautions you should take to ensure a safe and healthy flight.
Related: Guide to flying in each trimester of pregnancy
The airline you are flying may have its own cutoff, so you will want to confirm with it beforehand whether you will be allowed to fly if you are in (or nearing) your third trimester. We've included a chart below that outlines the rules for most major airline carriers.
What can you do to stay comfortable on a flight?

When you factor in morning sickness and general pregnancy discomfort with the increased risk for blood clots that all fliers need to be aware of, flying during pregnancy can be uncomfortable even when it is deemed safe.
Dr. Gopal shared her recommendations for addressing these common issues when you take to the (baby-) friendly skies during pregnancy. Her number one tip for staying comfortable while in flight is to wear compression socks to help maintain blood flow and reduce swelling in the legs.
In addition, "I also tell my patients to get up and move at least every hour when they are on the plane," Dr. Gopal said.
To prevent clotting, "some doctors may also prescribe a low-dose aspirin," she added. "It isn't something that is recommended by the American College of Obstetricians and Gynecologists (ACOG), but it isn't harmful, either."
If it's nausea or acid reflux that ail you, there are medications generally considered safe that you can take to alleviate your symptoms. These would be the same ones prescribed by your doctor for morning sickness, so speak with your provider before your flight to ensure you have what you need at the ready.
Dr. Gopal also advises wearing loose, unrestrictive clothing (along with your seatbelt, or course) and drinking extra fluids to counteract the pressurized air in the cabin and keep you hydrated.
"Over-the-counter Gas-X may also help with bloating that can happen as a result of the pressurized air," Dr. Gopal said.
Related: What happens when a baby is born in flight?
Must you speak with your healthcare provider before flying?

Even if your pregnancy is considered low-risk, it's always a smart idea to speak with your healthcare provider before flying. "There are a number of potential risks that go along with flying during pregnancy and those risks can change from week to week and month to month, so it's important to have that honest conversation with your doctor," Dr. Gopal said.
Related: Things You Should Do Before, During and After Flying to Stay Healthy
There are certain pregnancy conditions that may make flying more risky or unadvisable. If you are hypertensive, asthmatic or prone to clotting disorders, it's even more critical to speak with your doctor before flying.
Airline policies differ, but if you need documentation, it never hurts to include enough detail to satisfy the most stringent airline requirements.
"As with many things related to air travel, it's better to be safe than sorry," Dr. Gopal said. "It's definitely worth it, and sometimes necessary, to have medical documentation from your provider's office."
A thorough medical certificate or waiver should state:
- The number of weeks of pregnancy.
- The estimated delivery date.
- Whether the pregnancy is single or multiple.
- Whether there are any complications.
- That you are in good health and fit to travel through the date of your final flight.
Additionally, the certificate should be:
- Written on official clinic or hospital letterhead if possible.
- Signed by the doctor or attending midwife.
- Be dated no later than 72 hours before the departure date.
- Be written in clear, simple English.
Carry this certificate with you on your flight. Some airlines won't ask to see it, but others will. Some airlines also may have their own documentation requirements. See the chart below to find out which airlines require it.
Airline policies for pregnant women
Bottom line.

Even though it may be deemed safe, flying during pregnancy can be uncomfortable — and it is perfectly acceptable to implement your own cutoff for flying with your baby bump in tow. The majority of the time, though, flying is perfectly safe during pregnancy, providing that you follow the guidelines of the airline and your healthcare provider. Read on to learn more about traveling before, during and after pregnancy:
- What to expect in every trimester of pregnancy
- 4 tips for planning travel while planning a pregnancy
- Babymoon boom! These are the top 10 spots for a US getaway before the baby comes
- Flying with a baby checklist
Additional reporting by Katherine Fan and Tarah Chieffi.
Appointments at Mayo Clinic
- Pregnancy week by week
Is it safe to fly during pregnancy?
Generally, air travel before 36 weeks of pregnancy is considered safe for people who aren't dealing with any pregnancy problems. Still, if you're pregnant, it's a good idea to talk with your health care provider before you fly.
Your provider might suggest that you not fly if you have certain pregnancy complications that could get worse because of air travel or that could require emergency care. Examples include a history of miscarriage or vaginal bleeding, severe anemia, and high blood pressure or diabetes that's not well controlled. If you had preeclampsia during a previous pregnancy — a condition that causes high blood pressure and extra protein in urine — flying may not be advised. The same is true if you're pregnant with twins or other multiples.
Tell your provider how far you are flying, as the length of the flight might make a difference. Also, be aware that some airlines may not allow pregnant people on international flights. Check with your airline before you make travel arrangements.
After 36 weeks of pregnancy, your health care provider may advise against flying. And some airlines don't allow pregnant people to fly after 36 weeks. The airline also may require a letter from your health care provider that states how far along in your pregnancy you are and whether flying is advised.
If your health care provider says it's okay for you to fly, and your plans are flexible, the best time to travel by air might be during the second trimester. The risks of common pregnancy emergencies are lowest during that time.
When you fly:
- Buckle up. During the trip, keep your seatbelt fastened when you are seated, and secure it under your belly.
- Drink plenty of fluids. Low humidity in the airplane could cause you to become dehydrated.
- Avoid gassy foods and drinks before you fly. Gases expand during flight, and that could make you uncomfortable. Examples of foods and drinks to avoid include broccoli and carbonated soda.
- Think about medical care. Plan for how you'll get obstetric care during your trip if you need it. Bring copies of your medical information in case you need care while you're away.
Blood clots
Air travel can raise the risk for blood clots in the legs, a condition called venous thrombosis. The risk is higher for pregnant people. Moving your legs may help prevent this problem. Take a walk up and down the aisle every hour during the flight. If you must remain seated, flex and extend your ankles from time to time. In general, it's best to avoid tightfitting clothing, as that can hinder blood flow. Wearing compression stockings can help with blood circulation during a long flight.
Radiation exposure linked to air travel at high altitudes isn't thought to be a problem for most people who fly during pregnancy. But pilots, flight attendants and others who fly often might be exposed to a level of radiation that raises concerns during pregnancy. If you must fly frequently during your pregnancy, talk about it with your health care provider.
Mary Marnach, M.D.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Allergy medications during pregnancy
- AskMayoExpert. Health considerations for air travelers: Pregnancy considerations. Mayo Clinic; 2022.
- Air Travel During Pregnancy: ACOG Practice Bulletin No. 746. American College of Obstetricians and Gynecologists. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2018/08/air-travel-during-pregnancy. Accessed Dec. 1, 2022.
- Ram S, et al. Air travel during pregnancy and the risk of venous thrombosis. American Journal of Obstetrics and Gynecology. 2022; doi:10.1016/j.ajogmf.2022.100751.
Products and Services
- Available Solutions for Prenatal Nutrition from Mayo Clinic Store
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- Ankle swelling during pregnancy
- Antibiotics and pregnancy
- Aspirin during pregnancy
- Pregnancy back pain
- Falling during pregnancy: Reason to worry?
- Fetal ultrasound
- Flu shot in pregnancy
- Headaches during pregnancy: What's the best treatment?
- Iron deficiency anemia during pregnancy: Prevention tips
- Leg cramps during pregnancy
- Pregnancy acne
- Pregnancy and fish
- Pregnancy constipation
- Pregnancy diet: Essential nutrients
- Pregnancy due date calculator
- Pregnancy exercises
- Pregnancy nutrition don'ts
- Pregnancy stretches
- Pregnancy weight gain
- Pregnant. Now What Happens?
- Prenatal testing
- Prenatal vitamins and pregnancy
- Sex during pregnancy
- Twin pregnancy
- Vaccines during pregnancy
- Vaping during pregnancy
- Working during pregnancy
- X-ray during pregnancy
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Expert Answers
- Air travel during pregnancy Is it safe
5X Challenge
Thanks to generous benefactors, your gift today can have 5X the impact to advance AI innovation at Mayo Clinic.
Tips for travelling while pregnant

Dec 16, 2019 • 8 min read

With a few pragmatic adjustments, pregnancy needn't clip your travelling wings © Tim Robberts / Digital Vision / Getty Images
Being a guidebook author and a journalist, I travel a lot for work. And for leisure; I didn’t get this job by accident. So when I became pregnant, I thought I’d make some adjustments but it never crossed my mind to stop travelling altogether. During my first pregnancy, I travelled to Côte d’Ivoire , Brazil and France , the latter on numerous occasions, including two extended research trips for Lonely Planet’s France guidebook. And it was all a breeze. In fact, with hindsight, travelling with a bump turned out to be much easier than with babies and toddlers, so my advice to future parents is make the most of it!
Disclaimer: I am fit, healthy and enjoyed a (single) trouble-free pregnancy. Were it not the case, I wouldn’t have been able to do as much. But provided you are well too, there is no reason why you should hang up your rucksack and put your passport on sabbatical until baby is old enough to fly. Overall, I found that a little planning and some minor concessions (many of which I had to make at home anyway) were all that was needed for a great trip.

Formalities
Health check: Every woman and pregnancy is different so check with your doctor or midwife that they’re happy for you to travel (mine were very supportive). They’ll also be able to advise on medications you can or can’t take and what to do about immunisations and other disease prevention (more on that in a moment).
Insurance: Policy provisions can vary depending on where you live, so it's important to check the fine print. The Association of British Insurers (ABI) recommends that you shop around to find the policy best suited to your needs and has an online tool to help you choose. Broadly speaking however, if you're European travelling in Europe, most policies will cover you if you’re enjoying a trouble-free pregnancy (as with every condition, you’ll be covered for unexpected events, not routine appointments). Just take your medical notes with you, should anything happen. But in Australia, for example, no insurance provider will cover a pregnant woman past 32 weeks (19 weeks for multiple pregnancies). Contact your insurer before you set off; travelling without insurance could be extremely costly if you were to go into labour early while abroad.
Flying: Many airlines put restrictions on pregnant women in their third trimester and the restrictions vary depending on whether you are flying long or short haul. Check the requirements before you book. In Europe, as a rule, the cut-off point is 36 weeks for a single pregnancy, 32 for twins/triplets. Once you’re past 28 weeks, some carriers ask for a letter from your doctor or midwife confirming your due date and that there are no complications with the pregnancy. Otherwise, the usual advice applies – drink plenty of fluids, move often and wear compression socks (pregnant women have a slightly higher risk of DVT, especially on long-haul flights).
Ferries and cruises: Ferry companies tend to be fairly accommodating, usually allowing pregnant women to travel well into their third trimester (restrictions vary but 32 to 38 weeks is common, sometimes with a letter from your doctor or your midwife). Cruise companies are much more restrictive however, due to lengthy periods at sea: the cut-off point is 24 weeks. Some river cruise operators lift these restrictions due to the proximity to land but this isn’t universal. Make sure you check with the operator before booking.

Malaria, zika and dengue fever prevention
This is the most delicate topic I had to deal with. Health professionals advise pregnant women not to travel to malaria-prevalent areas because pregnancy reduces the body’s immunity to the disease. If you must go, your options for prophylaxis will be more limited than usual: some drugs cannot be taken at all during pregnancy; others can only be prescribed during the last six months; others still only work on some strains of the disease (and therefore only in certain areas/countries).
As a rule, I take prophylaxis if travelling to a malaria-prevalent area such as Côte d’Ivoire (I know some travellers don’t, but that’s a debate for another article). Unfortunately, there was nothing I could take last time around, so I decided instead to go all out on prevention.
The powerful insect repellent DEET is not recommended in the first three months of pregnancy; talk to a trained medical professional about other options. Covering yourself up is key: I wore long sleeves, long trousers and closed shoes and decided to have dinner indoors in the evening rather than on balmy terraces. I also slept in an air-conditioned room; even better would have been a mosquito net on the bed, although these were surprisingly scarce in Abidjan ’s mid-range hotels. I also bought Avon Skin So Soft, having heard that it worked wonders (it is actually a moisturiser). Its properties are not scientifically proven but anecdotal evidence is plentiful, so I thought I’d give it a try. The strategy worked for me: I left Côte d’Ivoire after four days without a single bite.
In Brazil, it was dengue, not malaria, I had to think about. This was before a zika virus outbreak swept through the Americas in 2015; travellers to central and south America (and a number of other countries) will now have to worry about both, but zika in particular because of the birth defects it can cause. The US Center for Disease Control (CDC) has comprehensive information on zika, including travel advice and a map of zika prevalence and outbreaks. The CDC’s recommendation is that pregnant women and couples looking to conceive should consult a healthcare professional about the risks of travelling to areas that have reported zika transmission in the past. The ABI notes that travel insurance is likely to pay a claim if you had booked a trip to a zika-prevalent area before finding out you are pregnant or if you’d booked a trip somewhere that was subsequently declared at risk with zika.
Dengue and zika are transmitted by the same species of mosquito, the Aedes, which bites during the day as well as at night. Zika can also be sexually transmitted. There is no vaccine or prophylaxis available for either disease so prevention is key. In Brazil, I applied the same bite prevention strategy as in Côte d’Ivoire for malaria. I did get a few bites over our two-week holiday, but then I’m not sure they were mosquitoes…
There are other diseases or health concerns you may have to think about before travelling, including immunisation - whatever the issue, do speak to your doctor about it so that you can make an informed decision.

Food and drink
I’ve found the food and drink restrictions of pregnancy to be my biggest frustration (if this were Twitter, I would add #firstworldproblems). I am a real foodie and cocktails are my guiltiest pleasure – having to forego unpasteurised cheese and charcuterie (cured meats) in France and caipirinhas in Brazil was akin to punishment.
On the plus side, I found people to be endlessly accommodating. In Corsica , I had waiters running back to their kitchens to check which, if any, of their cheeses were made with pasteurised milk; in Brazil, friends plied me with plates of specially well-cooked barbecued meat; and in the south of France, a restaurant made a fuss of preparing me a non-alcoholic aperitif.
Apart from these few restrictions, I followed the same precautions as usual to minimise the risks of food poisoning: filtered or bottled water if tap water is unsafe; piping hot food; salads from places you trust. I also carried snacks (cereal bars, dried fruit or bananas) to stave off the munchies (a pregnancy novelty).
OK, so perhaps you’ll have to swap canyoning for a trek and postpone your diving course until after the baby is born, but on the whole, I found that being pregnant did not stop me from enjoying an active trip. During my research for the France guidebook, I did several hikes in Corsica and the Riviera, cycled around Nice and kayaked off Île Rousse. In Brazil, swimming, snorkelling and hiking on Ilha Grande were among the highlights of my holiday.
The only time I felt uncomfortable was on a dreadful road in Parque Nacional do Itatiaia in Brazil. Knowing we’d have to do the same in reverse the next day, I decided to walk the worst stretch instead. As with health precautions, check with your doctor or midwife if in doubt about any activity.

It may be stating the obvious but wearing comfortable clothes is essential. I wore all my usual clothes until I was about three months pregnant and regretted not having invested in a pair of maternity trousers somewhere into the 2000km I drove for my France research (plan B was unbutton and unzip the jeans while driving – not terribly glamorous).
I got it right in Brazil, however: one pair of maternity jeans, a pair of linen cropped maternity trousers, baggy low-waist shorts and plenty of dresses. Maxi/long dresses were a dream; the short dress-cum-leggings combo also worked a treat (a thicker version of the latter would be perfect for winter/colder climes).
For swimwear, think about how comfortable you will be showing your bump: ‘tankinis’ and one-piece swimming suits are great alternatives to bikinis. And if you're going somewhere cold, make sure that whatever coat you take zips over the bump – no one wants a draughty tummy.
Cultural issues
If you are showing, be prepared for people touching your bump, even strangers, especially in Mediterranean or Latin cultures. You may also encounter some disapproval about you travelling. On the other hand, you’re likely to be shown unexpected kindness and attention: we received our first baby presents in Brazil from people we had only just met.
You might also like:
Baby travel: why and where you should head afield with your infant How to pack for travel with kids Family adventure destinations
Article first published in July 2014, and last updated by Emilie Filou in December 2019
Subscribe to our Lonely Planet Kids newsletter and get 30% off your first Lonely Planet Kids book purchase.
This article was first published Jul 14, 2014 and updated Dec 16, 2019.
Explore related stories

Jul 13, 2021 • 5 min read
This first-timer's guide to France can help you narrow down the best places to go, and other top tips to make the most of your visit.

Aug 26, 2024 • 8 min read

Aug 23, 2024 • 0 min read

Aug 13, 2024 • 8 min read

Jul 31, 2024 • 5 min read

Jul 31, 2024 • 4 min read

Jun 7, 2024 • 6 min read

May 18, 2024 • 7 min read

Apr 15, 2024 • 7 min read

Mar 31, 2024 • 6 min read
- Skip to main content
- Skip to site information
Language selection
Help us to improve our website. Take our survey !
Travelling while pregnant
Find useful information and considerations to help you prepare for safe and healthy travels outside Canada while pregnant.
With careful preparation, travelling while pregnant can be safe. The decision to travel should be made in consultation with your health care professional, based on your personal health circumstances.
On this page
Before you go, while you're away, if you need help.
Medical practices, health standards and infection control measures vary from country to country. You may not have access to the same level of care, procedures, treatments and medications as you would in Canada.
You could also be at increased risk of getting an infection and/or developing severe complications from certain infections, which could also affect the fetus.
Before leaving Canada:
- consult a health care professional or visit a travel health clinic at least 6 weeks before travelling to get personalized health advice and recommendations
- check our Travel Advice and Advisories for country-specific information, including about possible health risks
- know how to seek medical assistance outside of Canada
- review the policy and the coverage it provides
- most policies do not automatically cover pregnancy-related conditions or hospital care for premature infants
- ask your insurance provider about coverage for medical care during pregnancy, giving birth and intensive care for you and your fetus or newborn
- carry a copy of your prenatal records
- talk to your health care professional about any additional items you may want to bring that are specific to your health needs
Local laws and medical services relating to pregnancy can differ from Canada. Learn the local laws, and how these may apply to you before you travel.
Pre-travel vaccines and medications
Many vaccines can be safely given during pregnancy. Due to a higher risk of more severe outcomes for you and your fetus, some vaccines are recommended specifically during pregnancy, such as tetanus-diphtheria-pertussis (DTaP) and influenza.
Don’t take medications you may still have from prior trips. Tell the health care professional about your pregnancy, or intended pregnancy, before filling any prescriptions. The decision to get any pre-travel vaccinations or medications should be discussed with your health care professional.
The decision can depend on:
- your purpose of travel (e.g., tourism, visiting friends and relatives)
- your planned destination(s)
- the length of your trip
- your risk of getting a disease
- how severe the effect of a disease would be to you and/or your fetus
- your planned activities
- any underlying medical issues and/or pregnancy-related complications
Malaria could cause major health problems for a mother and her unborn baby. A pregnant woman may want to consider avoiding travel to areas where malaria transmission occurs.
Description of malaria risk by country and preventative measures.
If you can’t avoid travelling to an area where malaria is present:
- some medications to prevent or treat malaria may not be safe during pregnancy
- take extra care to protect yourself from mosquito bites
Zika virus infection during pregnancy can pose significant risks to your fetus even if you don’t develop symptoms. While pregnant, you may want to consider avoiding travelling to a country or areas with risk of Zika virus.
Latest travel health advice on Zika virus.
If you choose to travel, take precautions to avoid infection with Zika virus:
- prevent mosquito bites at all times
- protect yourself from contact with semen, vaginal fluid and blood
- always use condoms correctly or avoid sexual contact while in countries or areas with risk of Zika virus
Learn more about Zika virus and pregnancy:
- Zika virus: Pregnant or planning a pregnancy
- Zika virus: Advice for travellers
- Pregnancy and travel (tropical medicine and travel)
Monitor your health and be prepared
Emergencies can happen at any time. Know where the nearest hospital or medical centre is while you are travelling and confirm they will accept your medical insurance.
Seek medical attention immediately if you develop any of the following symptoms while travelling:
- persistent vomiting and/or diarrhea
- dehydration
- vaginal bleeding
- passing tissue or clots
- abdominal pain, cramps or contractions
- your water breaks
- excessive swelling of face, hands or legs
- excessive leg pain
- severe headaches
- visual problems
If you develop these symptoms after your return to Canada, you should see a health care professional immediately and tell them about your recent trip.
Transportation
Always wear a seatbelt when travelling by plane or car. When using a diagonal shoulder strap with a lap belt, the straps should be placed carefully above and below your abdomen. If only a lap belt is available, fasten it at the pelvic area, below your abdomen.
If you have any medical or pregnancy-related complications, discuss with your health care professional whether air travel is safe for you.
Most airlines restrict travel in late pregnancy or may require a written confirmation from a physician. Check this with the airline before booking your flight.
During long flights, you may be at higher risk of developing blood clots, known as deep vein thrombosis (DVT). The risk of deep vein thrombosis can be reduced by:
- getting up and walking around occasionally
- exercising and stretching your legs while seated
- selecting an aisle seat when possible
- wearing comfortable shoes and loose clothing
Your health care professional may recommend additional ways to reduce your risk such as wearing compression stockings.
Always stay well hydrated while travelling.
Land travel
The risk of deep vein thrombosis can be reduced by:
- stopping the vehicle to walk around every couple of hours
Motion sickness
Certain medications used to treat nausea and vomiting during pregnancy may also be effective in relieving motion sickness.
If you think you might experience motion sickness during your trip, speak to your health care professional about the use of these medications.
Environmental and recreational risks
Some activities may not be recommended or may require additional precautions. Discuss your travel plans, including any planned or potential recreational activities with a health care professional.
High altitude
You should avoid travelling to an altitude above 3,658 metres (12,000 feet).
However, if you have a high-risk pregnancy and/or are in the late stages of pregnancy, the highest altitude should be 2,500 metres (8,200 feet).
If you have pregnancy-related complications, you should avoid unnecessary high-altitude exposure.
Keep in mind that most high-altitude destinations are far from medical care services.
Personal protective measures
Food-borne and water-borne diseases.
Eat and drink safely while travelling while travelling. Many food-borne and water-borne illnesses can be more severe during pregnancy and pose a risk to the fetus.
This can include:
- toxoplasmosis
- listeriosis
- hepatitis A and E
To help avoid food-borne and water-borne diseases:
- before eating or preparing food
- after using the bathroom or changing diapers
- after contact with animals or sick people
- before and after touching raw meat, poultry, fish and seafood
- if you’re at a destination that lacks proper sanitation and/or access to clean drinking water, only drink water if it has been boiled or disinfected or if it’s in a commercially sealed bottle
- use ice made only from purified or disinfected water
- this could cause the fetus or newborn to develop thyroid problems
- unpasteurized dairy products, such as raw milk and raw milk soft cheeses
- unpasteurized juice and cider
- raw or undercooked eggs, meat or fish, including shellfish
- raw sprouts
- non-dried deli meats, including bologna, roast beef and turkey breast
- don’t use bismuth subsalicylate (Pepto-Bismol®)
- Information on travellers’ diarrhea
Illnesses acquired from insect and other animals
Protect yourself from insect bites:
- wear light-coloured, loose clothes made of tightly woven materials such as nylon or polyester
- prevent mosquitoes from entering your living area with screening and/or closed, well-sealed doors and windows
- use insecticide-treated bed nets if mosquitoes can’t be prevented from entering your living area
- information on insect bite and pest prevention
Some infections, such as rabies and influenza, can be shared between humans and animals. You should avoid contact with animals including dogs, livestock (pigs, cows), monkeys, snakes, rodents, birds, and bats.
Information for if you become sick or injured while travelling outside Canada.
For help with emergencies outside Canada, contact the:
- nearest Canadian office abroad
- Emergency Watch and Response Centre in Ottawa
More information on services available at consular offices outside Canada.
Related links
- Immunization in pregnancy and breastfeeding: Canadian Immunization Guide
- Advice for Canadians travelling to Zika-affected countries
- Advice for women travellers
- If you get sick before or after returning to Canada
- Receiving medical care in other countries
- Travel vaccinations
- What you can bring on a plane
- Tips for healthy travel

Search Smartraveller
Advice for pregnant travellers.

If you're pregnant and planning to travel overseas, research your destination before you go. Consult your doctor and understand potential risks to you and your unborn child. Being informed about the risks will help you manage them. It will increase your chance of having a great time overseas. Explore this page to learn about:
- planning for travel during pregnancy
- medications and pregnancy
- terminating a pregnancy overseas
- going overseas to give birth
- how the Australian Government can help overseas
This page is for Australians who are pregnant, or planning to get pregnant overseas. If you're looking for information about adopting a child or engaging in surrogacy, refer to surrogacy and adoption .
Planning for travel during pregnancy
Travelling when pregnant can be challenging, but there are things you can do to stay safe and comfortable and reduce your risks.
Timing your travel
Visit your doctor or obstetrician at least 8 weeks before you go. Discuss the timing and location of your trip. Check if you're allowed to travel and if they recommend travel.
If they advise against travel, don't go. Find time to travel later, when the risk has passed.
Airlines and cruise lines have specific rules on when you can travel while pregnant. If you're having more than one baby, the rules may differ again. Most airlines won't let you fly beyond 28 weeks of pregnancy.
Ask your airline or cruise line about any rules or restrictions that could affect you while in transit.
Read more about pregnancy and travel (Victorian Government Department of Health and Human Services).
Choosing where to travel when you're pregnant
Consider the risks of going overseas, including the risks to your unborn child.
You and your baby will be more at risk in some countries. Avoid countries with poor sanitation, hygiene and medical facilities. Read the travel advisory for each country you're visiting. Note the health risks.
If the travel advisory says do not travel to that country, then do not travel at this time. You're putting yourself and your unborn child at serious risk.
Things can go wrong quickly when you're pregnant. Check how close you'll be to good medical facilities. Stay within reach of hospitals and doctors.
See a doctor before you go
See a doctor at least once before you travel. Your doctor will advise what vaccines and medications you can take when you're pregnant.
If you have a high-risk pregnancy, your doctor may advise against travel. If they advise against travel, then don't go. You're putting yourself and your unborn child at serious risk.
Most airlines will ask you to show a letter from your doctor.
Buy travel insurance to cover pregnancy
You need travel insurance.
Ask your travel insurer if your policy covers:
- pregnancy, and until what stage
- IVF pregnancy, if applicable
- pregnancy complications or premature birth while you're away
- cancellation of your trip due to pregnancy or birth issues
For cover during pregnancy, you may need to pay extra. You may need medical evidence. You may face limitations to your cover, depending on where you're going. For example, in Saudi Arabia, medical insurance won't cover pregnancy unless you're married.
Read more about travel ins urance .
Medications and pregnancy
Not all medication available over the counter or by prescription in Australia is available in other countries. Some may even be considered illegal or a controlled substance, even if prescribed by an Australian doctor.
Get the facts, before you go.
- See if your medication is legal in your destination .
- Ensure you have enough medication for your trip.
- Check with a doctor that your medication is suitable for travel.
Refer to the 'Look after your health' section on Advice for women travellers for more information. Also see our advice on travelling with medications .
Terminating pregnancy overseas (abortion)
Abortion and the law.
Abortion may be illegal in the country you're visiting.
You're subject to all local laws and penalties, including those that may appear harsh by Australian standards. Research local laws before considering an abortion.
If you're arrested or jailed for having an abortion, the Australian Government will do what it can to help you. However, we can't get you out of trouble or out of jail.
- Understand our limits. Read the Consular Services Charter .
Health care standards overseas can vary. If you choose to end your pregnancy, find a proper medical facility to help you.
Choose the safest option, not the cheapest option.
Read more about medical assistance overseas .
Medical treatment for ending a pregnancy can be costly. As with other medical procedures overseas, get a quote from the hospital first.
Find out if this procedure is covered by your travel insurance . If not, consider the cost of having this procedure overseas versus back in Australia. You may be eligible for subsidised care in Australia through Medicare.
Read more about travel insurance .
Going overseas to give birth
If you choose to give birth overseas, you'll need to check:
- healthcare costs and travel insurance
- safety and quality of care
- your budget to pay for a private hospital, if you aren't covered by the public health system via a partner or a reciprocal agreement
- any changes to your legal status, marriage and parent rights
- if you need a special visa as a medical tourist
Citizenship and passports
Giving birth overseas doesn't automatically grant your child citizenship of that country. Research local immigration and citizenship laws before you travel.
If authorities think you're planning to give birth there for visa reasons, they may refuse you entry.
In Australia
To register your child's birth with Australian authorities, you'll need to contact your state or territory registry of births, deaths and marriages (Australian Government).
Consular officials can assist with your child's passport .
There may be higher costs for processing a passport for your baby while you're overseas.
- Learn more about Australian citizenship by descent (Department of Home Affairs).
Becoming a new parent can feel overwhelming. Consider how you'll find support overseas, both practically and emotionally.
Supplies and services
Prepare ahead for how you'll travel with your new baby. Make sure you have all the medications and supplies you need.
The Australian Government can't help with medical costs or services overseas.
Learn more about medical assistance overseas .
If our travel advisory for the country in which you plan to give birth says ' do not travel ', then don't travel there. You're putting yourself and your unborn child at serious risk.
Learn more about staying safe and avoiding danger .
Consular services and pregnancy
The Australian Government is limited in how and when it can help Australians overseas.
In most cases, when you need help overseas you, or your travel insurer, must organise and pay for it.
What we can do
- We can give you a list of local medical facilities with doctors who speak English.
- We can give you a list of local lawyers who speak English.
- We can help you contact your family in Australia in an emergency.
- We can notify you when we update our travel advice for your destination . Learn more about subscriptions .
What we can't do
- We can't guarantee your safety when you travel.
- We can't pay for your bills if you need medical assistance overseas .
- We can't get you out of jail if you're arrested because you've broken a local law. Be aware laws vary greatly on abortions, medications and sex outside of marriage.
- We can't give you medical or legal advice.
Final tips before you go
Prepare before you travel:
- get medical advice, vaccinations and a health check
- know the laws about pregnancy, adoption, surrogacy and abortion overseas
- arrange adequate travel insurance and check coverage
- arrange emotional and practical support
- Read our general advice for people travelling with children .
- See information about international surrogacy .
- See information about going overseas to adopt .
- Before you go, get travel insurance that covers your pregnancy.
- See more advice on pregnancy and travel (Victorian Department of Health and Human Services).
- Read more about travelling while pregnant (CHOICE).
Related content
Information for Australians going overseas for surrogacy. Learn about types of arrangements, laws, citizenship and visas.
Many Australians adopt children from other countries. There are legal implications surrounding overseas adoptions both in Australia and in the child's country.
All travellers face risks overseas. In certain countries or cultures, women face greater risks than men and may be more vulnerable.
- Book your antenatal a course
- Make a donation
Flying when pregnant: what you need to know
Read time 6 minutes

If you’re feeling unsure about whether you can hop on that plane when you’re expecting, here’s the info.
Can I fly at one, two or three months pregnant (first trimester)?
Yes, there is no evidence that flying causes miscarriage (RCOG, 2015) . Yet as this is the riskiest time for miscarriage , just be aware that no medical help will be available if that does happen. You also might feel nauseous and exhausted, so that’s something to think about too.
Can I fly at four, five or six months pregnant (second trimester)?
Good news if you’re thinking of going away in the second trimester: it’s considered the safest time to fly (Hezelgrave et al, 2011) . That’s mainly because the risk of pregnancy-related complications, including miscarriage, is lower during the second trimester than in the first and third (Hezelgrave et al, 2011) .
Can I fly at seven, eight or nine months pregnant (third trimester)?
It’s fine to fly in the third trimester but you’re advised to do it before 37 weeks, or before 32 weeks in an uncomplicated twin pregnancy . That’s because you could go into labour any time after those dates (RCOG, 2015) .
Do still check with your specific airline before you fly though. Many airlines have restrictions on travel in advanced pregnancy (Hezelgrave et al, 2011) .
Flying when pregnant: the worries and concerns
First of all, you should know that flying is not considered harmful to you or your baby if you’re having a straightforward pregnancy.
You might feel a bit uncomfortable flying at certain stages of pregnancy. For example, you might have swollen legs, pregnancy sickness , nasal congestion (more common during pregnancy) or ear problems during pressure changes due to this congestion (RCOG, 2015) .
A change in air pressure or a decrease in humidity won’t cause your baby any harm. There is also no evidence to suggest that flying causes miscarriages, early labour or waters to break (RCOG, 2015) . If you have any health issues or pregnancy complications, discuss it with your GP or midwife before you decide to fly. They might advise you not to fly if you have:
- severe anaemia
- sickle cell disease
- significant vaginal bleeding
- a serious heart or lung condition that makes it difficult to breathe
- increased risk of going into labour before the due date
- increased chance of miscarriage or ectopic pregnancy (request an ultrasound before flying)
- previous history of ectopic pregnancy, pelvic inflammatory disease, infertility and documented tubal pathology.
(Hezelgrave et al, 2011; RCOG, 2015)
Deep vein thrombosis (DVT) when pregnant and flying
A DVT is a blood clot that develops in a deep vein in your leg or pelvis. It’s dangerous if a DVT travels to your lungs and causes a pulmonary embolism.
The risk of DVT increases when you’re flying and with longer flights because you are sitting down for a long time. You’re also at a higher risk of developing a DVT when you are pregnant and for up to six weeks after you give birth (RCOG, 2015) . Risk factors like a previous history of DVT and a high BMI can further increase your chance of developing a DVT.
Your doctor or midwife will be able to check your risk of developing DVT and advise you about flying.
How to reduce your risk of DVT
You can reduce your risk of DVT by:
- wearing loose clothing and comfy shoes
- getting an aisle seat and going for regular walks around the plane
- doing in-seat exercises every 30 minutes (ask your GP about how to do these)
- drinking plenty of water
- avoiding drinks containing alcohol and caffeine
- wearing graduated elastic compression stockings to help reduce leg swelling.
(RCOG, 2015; NHS Choices, 2016)
Flying when pregnant: general tips
- Take your hand-held pregnancy notes.
- Carry any medication in your hand luggage.
- Carry any documents confirming your due date and (if needed) that you are fit to travel. If you are 28 weeks pregnant or more, the airline you are travelling with might ask for a letter from your midwife or doctor stating your due date, that you’re in good health, have no complications and have a straightforward pregnancy.
- Carry your travel insurance documents with you too or make sure you have access to them if they’re on email.
- Carry your European Health Insurance Card (EHIC) with you if you are travelling to Europe. You can apply online for one for free .
- Seatbelt wise, it’s recommended that you strap your seatbelt reasonably tightly across the top of your thighs and then under your bump. If you need a seatbelt extension, ask cabin crew.
Travel vaccinations when pregnant – are they safe?
There’s no evidence of risk from vaccinations that contain inactivated virus, bacterial vaccines or toxoids when you’re pregnant (CDC, 2017) . However, avoid live vaccines like yellow fever because of the risk of contracting a disease that might harm your developing baby (Hezelgrave et al, 2011) .
If you need advice on specific travel vaccinations, contact your doctor or midwife. Some anti-malarial tablets are not safe to be taken during pregnancy, so consult your GP or midwife about those too (NHS Choices, 2016) .
This page was last reviewed in May 2018.
Further information
Our support line offers practical and emotional support with feeding your baby and general enquiries for parents, members and volunteers: 0300 330 0700.
We also offer antenatal courses which are a great way to find out more about birth, labour and life with a new baby.
CDC. (2017) Guidelines for vaccinating pregnant women. Available from: https://www.cdc.gov/vaccines/pregnancy/hcp/guidelines.html [Accessed 11th May 2018]
Hezelgrave NL, Shennan AH, Chappell LC. (2011) Advising on travel during pregnancy. BMJ.342. Available from: https://www.bmj.com/content/342/bmj.d2506.long [Accessed 11th May 2018]
NHS Choices. (2016) Travelling in pregnancy. Available from: https://www.nhs.uk/conditions/pregnancy-and-baby/travel-pregnant/#car-travel-in-pregnancy [Accessed 11th May 2018]
RCOG. (2015) Air travel and pregnancy. Available from: https://www.rcog.org.uk/globalassets/documents/patients/patient-information-leaflets/pregnancy/air-travel-pregnancy.pdf [Accessed 11th May 2018]
Rodger MA, Walker M, Wells PS. (2003) Diagnosis and treatment of venous thromboembolism in pregnancy. Best Pract Res Clin Haematol. 16:279-296. Available from: https://www.ncbi.nlm.nih.gov/pubmed/12763492 [Accessed 11th May 2018]
Information you can trust from NCT
When it comes to content, our aim is simple: every parent should have access to information they can trust.
All of our articles have been thoroughly researched and are based on the latest evidence from reputable and robust sources. We create our articles with NCT antenatal teachers, postnatal leaders and breastfeeding counsellors, as well as academics and representatives from relevant organisations and charities.
Read more about our editorial review process .
Related articles
Courses & workshops

In-person NCT Antenatal course

NCT Antenatal refresher course


IMAGES
VIDEO
COMMENTS
Before you book a cruise or air travel, check the airlines or cruise operator policies for pregnant women. Some airlines will let you fly until 36 weeks, but others may have an earlier cutoff. Cruises may not allow you to travel after 24-28 weeks of pregnancy, and you may need to have a note from your doctor stating you are fit to travel.
Stand up and stretch. Pregnant women are at higher risk for developing blood clots, so it's important to avoid sitting still for long periods of time. Wear loose clothes and keep the blood flowing in your legs: Whether you're flying or driving, take breaks to get up, walk around and stretch every half hour or so.
Most people can safely travel by airplane during pregnancy, but talk to your healthcare provider ahead of time to make sure you don't have any medical conditions that could cause a complication ...
Download any apps you use for renting cars and accessing boarding passes before you leave so you can easily reschedule things in the event of a last-minute cancellation. If you're flying during your third trimester, be sure to call the airline to check about the cutoff week for pregnancy travel. A note from your doctor that says you're ...
Here's my experience traveling abroad while pregnant, including to a developing country! Traveling Abroad while Pregnant: Firsthand Advice from a Pregnant Travel Addict. 1 Comment / Travel / By Diane Vukovic When I told people that I was planning to travel to a foreign country while 7 months pregnant, I got looked at like I was crazy. The look ...
Travelling in the final months of pregnancy can be tiring and uncomfortable. So, many women find the best time to travel or take a holiday is in mid-pregnancy, between 4 and 6 months. Flying in pregnancy. Flying isn't harmful to you or your baby, but discuss any health issues or pregnancy complications with your midwife or doctor before you fly.
The best time to travel is mid-pregnancy (14 to 28 weeks). During these weeks, your energy has returned, morning sickness is improved or gone, and you are still able to get around easily. ... Trimesters: The 3-month periods of time in pregnancy. They are referred to as first, second, or third. Zika: A disease caused by the Zika virus, which is ...
The American College of Obstetricians and Gynecologists says the safest time for a woman to travel is in the second trimester of her pregnancy, from 14 to 28 weeks. This is the time when you will feel your best. You are also at the lowest risk for spontaneous abortion (miscarriage) or premature labor.
Healthy tips for traveling while pregnant . Here are tips for traveling while pregnant: Try to plan ahead for any problems or emergencies that could come up before you travel. Check that your health insurance is valid while you are abroad. Also check to see whether the plan will cover a newborn, should you deliver while away.
Most airlines do allow pregnant women to fly until about a month before their due dates. Chervenak agrees: "As long as there are no known complications to pregnancy, traveling on an airplane is ...
Travel During Pregnancy. As long as there are no identified complications or concerns with your pregnancy, it is generally safe to travel during your pregnancy. The ideal time to travel during pregnancy is the second trimester. In most cases, you are past the morning sickness of the first trimester and several weeks from the third stage of ...
Keep snacks and water on hand as well, "to stay hydrated and keep up with the metabolic demands of being pregnant," says Dr. Simmons. And if you're feeling nauseous or have GI discomfort while traveling, Reglan, Dramamine, and Imodium are considered safe to take while pregnant. 8. Mask up and use hand sanitizer.
Going on holiday or abroad. If you're planning a holiday, seek health advice as early as possible. ... Flying while pregnant. Air travel is generally safe if you're having an uncomplicated pregnancy. ... Some will need a letter from your GP or midwife saying you're fit to fly when you're 7 months pregnant. Check with the airline before ...
Virgin Australia. No restrictions. Travel permitted; requires a medical certificate dated within 10 days of departure date once you reach 28 weeks. For flights longer than four hours, travel is not permitted after 36 weeks of pregnancy (32 weeks if pregnant with multiples), or within 48 hours of normal vaginal delivery.
Most airlines in the United States allow pregnant women to fly domestically in their third trimester before the 36th week. Some international flights restrict travel after 28 weeks. Flying isn't ...
If you're taking a long road trip or getting on an airplane, try to do some stretching at least every two hours. Pregnancy increases your risk for blood clots, but moving around helps keep your blood flowing normally. If you're on a plane, compression stockings can help keep blood from pooling in your legs. Make sure you add plenty of down ...
Actually, during pregnancy, you can still do many of the things you enjoyed before, including travel. Here, we want to share some tips on how to make your traveling during pregnancy more comfortable. All recommendations are based on a position statement by the European Board and College of Obstetrics and Gynaecology (EBCOG).
If you become dehydrated, it can reduce blood flow to the uterus. Exercise aloft. Your doctor may suggest you walk every half hour or so during a smooth flight. It will help keep blood flowing. In ...
Answer From Mary Marnach, M.D. Generally, air travel before 36 weeks of pregnancy is considered safe for people who aren't dealing with any pregnancy problems. Still, if you're pregnant, it's a good idea to talk with your health care provider before you fly. Your provider might suggest that you not fly if you have certain pregnancy ...
Flying: Many airlines put restrictions on pregnant women in their third trimester and the restrictions vary depending on whether you are flying long or short haul. Check the requirements before you book. In Europe, as a rule, the cut-off point is 36 weeks for a single pregnancy, 32 for twins/triplets.
You should avoid travelling to an altitude above 3,658 metres (12,000 feet). However, if you have a high-risk pregnancy and/or are in the late stages of pregnancy, the highest altitude should be 2,500 metres (8,200 feet). If you have pregnancy-related complications, you should avoid unnecessary high-altitude exposure.
See a doctor at least once before you travel. Your doctor will advise what vaccines and medications you can take when you're pregnant. If you have a high-risk pregnancy, your doctor may advise against travel. If they advise against travel, then don't go. You're putting yourself and your unborn child at serious risk.
It's fine to fly in the third trimester but you're advised to do it before 37 weeks, or before 32 weeks in an uncomplicated twin pregnancy. That's because you could go into labour any time after those dates. Do still check with your specific airline before you fly though. Many airlines have restrictions on travel in advanced pregnancy.