- ACS Foundation
- Diversity, Equity, and Inclusion
- ACS Archives
- Careers at ACS
- Federal Legislation
- State Legislation
- Regulatory Issues
- Get Involved
- SurgeonsPAC
- About ACS Quality Programs
- Accreditation & Verification Programs
- Data & Registries
- Standards & Staging
- Membership & Community
- Practice Management
- Professional Growth
- News & Publications
- Information for Patients and Family
- Preparing for Your Surgery
- Recovering from Your Surgery
- Jobs for Surgeons
- Become a Member
- Media Center
Our top priority is providing value to members. Your Member Services team is here to ensure you maximize your ACS member benefits, participate in College activities, and engage with your ACS colleagues. It's all here.
- Membership Benefits
- Find a Surgeon
- Find a Hospital or Facility
- Quality Programs
- Education Programs
- Member Benefits
- Coding, Billing, and Payment
- E/M Coding and Billing Res...
- Split-Shared EM Visits

Reporting Split/Shared E/M Visits in 2024
Beginning January 1, 2024, the Centers for Medicare & Medicaid Services (CMS) will implement a new split (or shared) evaluation and management (E/M) billing policy for E/M visits provided in part by a physician and in part by a nonphysician practitioner (NPP). The billing provider for such visits will be the physician or NPP who furnished the “substantive portion” of the visit. CMS defines “substantive portion” to mean more than half of the total time spent by the physician or NPP performing the split/shared visit or the substantive part of the medical decision making (MDM) during the split/shared visit.
A split/shared visit is an E/M visit in a hospital or other facility setting that is performed in part by both a physician and an NPP who are in the same group practice. A split/shared E/M visit may be provided to a new or established patient for an initial or subsequent visit.
No. This new split/shared E/M visit reporting policy applies only to those furnished in a facility setting. In a nonfacility setting, such as a physician’s office, different reporting rules apply when an NPP provides some or all of an E/M visit and the physician bills for the visit. This type of E/M visit is referred to as an "incident-to" service.
Medicare defines an NPP as a nurse practitioner, physician assistant, certified nurse specialist, or certified nurse midwife. All of these practitioners may independently report E/M services if they are legally authorized and qualified to furnish an E/M service in their state. NPPs who care for Medicare patients in a facility must enroll in the Medicare program to bill for the services they provide.
CMS has yet to provide a definition of "same group" at this time, but has indicated that a physician and an NPP must work jointly to furnish all of the work related to the E/M in circumstances when a split/shared visit is appropriately billed. If a physician and NPP are in different groups, the physician and NPP would be expected to bill independently and only for the services each fully furnishes.
CMS has adopted the following Current Procedural Terminology (CPT ® ) guidelines for reporting a split/shared E/M visit:
If the physician or other QHP 1 performs a substantive portion of the encounter, the physician or other QHP may report the service. If code selection is based on total time on the date of the encounter, the service is reported by the professional who spent the majority of the face-to-face or non-face-to-face time performing the service. For the purpose of reporting E/M services within the context of team-based care, performance of a substantive part of the MDM requires that the physician(s) or other QHP(s) made or approved the management plan for the number and complexity of problems addressed at the encounter and takes responsibility for that plan with its inherent risk of complications and/or morbidity or mortality of patient management. By doing so, a physician or other QHP has performed two of the three elements used in the selection of the code level based on MDM. If the amount and/or complexity of data to be reviewed and analyzed is used by the physician or other QHP to determine the reported code level, assessing an independent historian’s narrative and the ordering or review of tests or documents do not have to be personally performed by the physician or other QHP because the relevant items would be considered in formulating the management plan. Independent interpretation of tests and discussion of management plan or test interpretation must be personally performed by the physician or other QHP if these are used to determine the reported code level by the physician or other QHP. 2
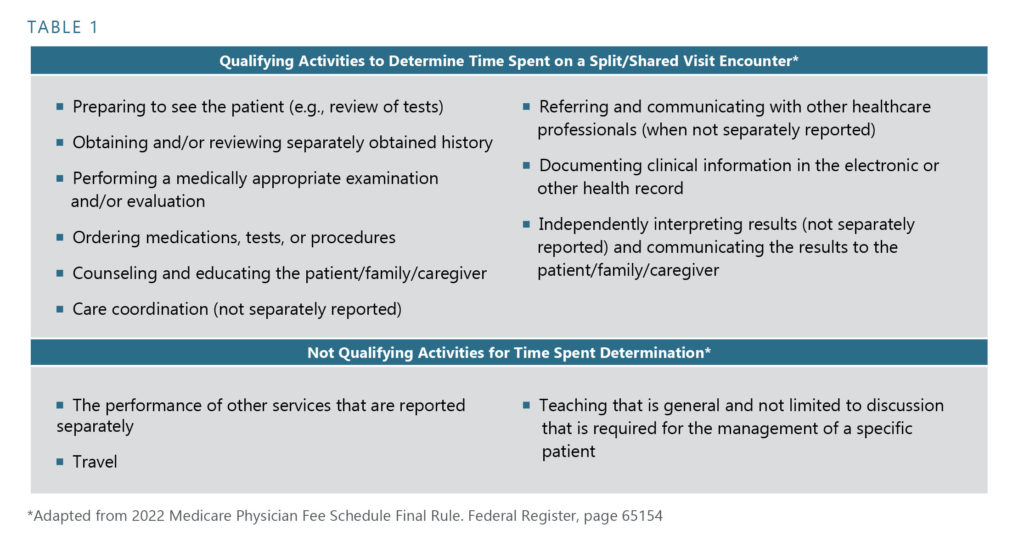
CMS relies on the list of activities included in CPT E/M Guidelines that count toward total time for purposes of who reports the split/shared visit and for the level of code selected. Based on these guidelines, physician/NPP time includes the following activities:
- Preparing to see the patient (such as review of tests)
- Obtaining and/or reviewing separately obtained history
- Performing a medically appropriate examination and/or evaluation
- Counseling and educating the patient/family/caregiver
- Ordering medications, tests, or procedures
- Referring and communicating with other health care professionals (when not separately reported)
- Documenting clinical information in the electronic or other health record
- Independently interpreting results (not separately reported) and communicating results to the patient/family/caregiver
- Care coordination (not separately reported)
Physician/NPP time does not include the following activities:
- Performance of other services that are reported separately
- Teaching that is general and not limited to discussion that is required for the management of a specific patient
No. For all split/shared E/M visits, only one of the practitioners must have face-to-face (in-person) contact with the patient, but it does not necessarily have to be the practitioner who performs the substantive portion and bills for the visit. When reporting a split/shared visit using total time, the substantive portion could be provided entirely with or without direct patient contact and will be determined based on the proportion of total time, not whether the time involves direct or in-person patient contact.
Yes. If code selection is based on total time on the date of the encounter, the service is reported by the physician/NPP who spent the majority of time performing the service.
CMS has not yet released specific documentation requirements for reporting a split/shared E/M visit. However, it is best practice that the medical record identify the two practitioners who performed the split/shared visit, the activities each practitioner performed, and the time spent by each practitioner. In addition, the individual who performed the substantive portion—and therefore bills the visit—must sign and date the medical record. CMS has emphasized that, although any member of the medical team may enter information into the medical record, only the reporting provider may review and verify notes made in the record by others for the services the reporting clinician furnishes and bills.
The new split/shared E/M visit guidelines indicate that performance of a substantive part of the MDM requires that the physician or NPP who will bill the visit made or approved the management plan for the number and complexity of problems addressed at the encounter and takes responsibility for that plan with its inherent risk of complications and/or the morbidity or mortality of patient management. By doing so, a physician or NPP has performed two of the three elements used in the selection of the code level based on MDM.
Yes. CMS requires that HCPCS modifier –FS ( Split or shared E/M visit ) be appended to the facility claims for split/shared E/M visits, no matter if the physician or NPP bills for the visit. This modifier does not apply to incident-to office visits.
No. Critical care E/M services (e.g., CPT codes 99291-99292) are reported based solely on time. MDM is not a component of these CPT codes.
Please note that the reporting details above are suggestions only and should not be construed as official coding/billing rules.
1 CPT, in general, refers to NPPs as other qualified healthcare professionals (QHPs). With respect to reporting split/shared services in a facility setting, NPPs and other QHPs are synonymous.
2 2024 CPT Codebook, pg. 6.
All specific references to CPT codes and descriptions are © 2023 American Medical Association. All rights reserved. CPT is a registered trademark of the American Medical Association.
- Advertise with TH
- Improving Your HCAHPS Scores
- Comanagement
- Evidence-Based Medicine
- Growing Your Practice
- Health Care Redesign/Reform
- Observation
- Practice Management
- Quality Improvement
- Technology/Electronic Health Record
- Working With Other Specialties
- Addiction Medicine
- Anticoagulation
- Cardiac Care
- Critical Care
- Delirium/Dementia
- End-of-Life Care
- Glycemic Control
- Infectious Disease
- Pain Management
- Pneumonia/COPD
- Perioperative Care
- Psychiatric Care
- Download Coding Report
- Handoffs/Transfers
- Post-Acute Care
- Readmissions
- Moving Towards Unit-Based Care
- Unclogging the hospital
- Unit-Based Care
- CME/Meetings
- Compensation
- Malpractice
- Recertification
- Recruiting/Retention
- Satisfaction/Burnout
- Schedule/Workload
- Survey Articles
- Reports for sale
- Survey Overview
- Email Alerts
- Past Issues
- Privacy Policy & Terms of Use
Split visit billing rules for physicians and NPs/PAs
Who gets to bill?

IN NOVEMBER 2021 , the Centers for Medicare and Medicaid Services (CMS) set off a bombshell with new rules governing how physicians and NPs/PAs can bill split hospital visits. The rules took effect this Jan. 1, just two months after they were finalized.
Groups with physician-NP/PA teams were left scrambling to figure out how to implement the new rules. The group led by Sushamma Brimmer, MD, regional hospitalist medical director for the Northeast Texas Region of CHRISTUS Health, with two campuses, is a case in point.
“For us, it’s still a work in progress,” says Dr. Brimmer, speaking in mid-December. “Right now, I’m working with the finance and coding departments to try to figure this out, and I’m not sure there’s a best way to handle it. But I do know that we have to come up with something that won’t terribly affect our workflow.” Like hospitalist leaders and administrators around the country, Dr. Brimmer spent the last weeks of 2021 in meetings with her physicians and NPs/PAs, trying to figure out options to meet the new rules.
“We have to come up with something that won’t terribly affect our workflow.” ~ Sushamma Brimmer, MD CHRISTUS Health
Those options may come down to having doctors spend more time performing (and documenting) split visits with NP/PA teams or letting NPs/PAs bill more visits at 85% of the physician fee schedule. Some group members don’t much like either option.
What the new rules say For years, physicians and NPs/PAs have been submitting bills for split (or shared) visits under physicians’ names and ID numbers for 100% of the allowable physician fee—as long as doctors perform a “substantive portion” of the visit. (Otherwise, NPs/PAs bill under their own names and ID numbers at 85% of the allowable fee.) Medicare, however, has never provided any real oversight of that billing. Further, it’s never spelled out what a “substantive portion” of a visit really means, other than saying that doctors can’t just rubber-stamp the care that NPs/PAs provide and capture the visit at 100%.
That’s now changed. In its proposed rule last year, the CMS said “substantive” would consist of having to perform more than 50% of the time it took for the entire visit; only the provider spending that 50+% time could bill it. But in response to very loud concerns—after all, tracking time in the hospital has been used only for critical care and prolonged services, never for admissions and subsequent inpatient care or ED visits—the CMS in its final rule decided to make 2022 a transitional year.
For this year only, doctors and NPs/PAs can determine who bills a shared visit by using either that more-than-50% time gauge—or physicians will be considered to be providing a substantive portion of the visit if they perform one of three key visit components (history, exam or medical decision-making) in its entirety.
“More transparency and visibility for NPs/PAs could be a good thing.” ~ Michael L. Powe American Academy of Physician Assistants
That “entirety” language is also brand new. Up to now, doctors and NPs/PAs have both been able to contribute to all visit components and still bill at 100%. As for 2023, when this transitional year ends? As the final rule currently stands, the CMS will crack down and allow only time of more than 50% to determine billing.
Another change this year and going forward: Previously, the CMS had no idea if a visit being billed at 100% under a physician’s name was actually provided by two different clinicians. Now, all shared visit bills must come with a new modifier—FS-Split—to tip the agency off and allow it to track those claims.
A move toward more transparency What’s behind the changes? According to Michael L. Powe, vice president, reimbursement and professional advocacy for the American Academy of Physician Assistants, Medicare has come to recognize that, in certain encounters, NPs/PAs may often perform the lion’s share of the care. If that’s the case, the CMS would rather pay only 85% of charges, not the 100% that groups may have been billing up until now.
Also, says Mr. Powe, the CMS is looking for transparency about physician-NP/PA teams, as well as the ability to collect data (through the new modifier) on visits NPs/ PAs contribute to.
“We never know with these visits who does what and how health care teams contribute to quality, patient satisfaction and care outcomes,” he says. “We’re never able to track the productivity of NPs/PAs or the revenue they generate because of billing mechanisms like shared billing.” When visit claims don’t accurately reflect the actual level of care NPs/PAs provide, he adds, NPs/PAs can look less important to their organizations.
“At what point will doctors decide they no longer want to work in a team pair?” ~ Heather Miles, CPC St. Dominic Hospital
“If you don’t really understand their impact in health care,” says Mr. Powe, “you can’t determine how to most efficiently utilize the members of health care teams going forward.”
Mr. Powe is also waiting to see what changes this transitional year brings. “More transparency and visibility for NPs/PAs could be a good thing,” he says. He also believes that, given the new visit component requirements, some doctors may choose to bill fewer shared visits—and NPs/ PAs in the hospital may start submitting more bills at 85%.
Making team care less attractive? In Jackson, Miss., Heather Miles, CPC, is the practice administrator for the hospital medicine department at St. Dominic Hospital. She also administers the billing and documentation of her hospital’s neurology and palliative care departments, both of which utilize NPs/PAs.
In their current model, the NP/PA-hospitalist teams at St. Dominic share documentation, with physicians billing on more acute cases and NPs/PAs managing less acute care. “It’s the physicians’ call on how often they want to add an addendum and capture the charge,” Ms. Miles points out. “That’s the benefit of a true ‘split-share’ environment in which the team shares the work.”
Like Mr. Powe, she thinks the revised rules could spur more non-split NP/PA bills at 85%, and she worries about that potential hit to her hospital’s revenue.
But she has other concerns. Two years ago, the hospital medicine department decided to change the NP/PA contracts so those advanced providers could share in the productivity bonuses the physicians receive when they meet their RVU threshold on split visits. Currently, the bonuses are divided 75%-25% between the doctors and the NPs/PAs.
“It makes more financial sense for physicians to see new patients of their own instead of doing several split visits.” ~ Timothy Capstack, MD Adfinitas Health
“That provided a great deal of satisfaction for our advanced practice providers,” says Ms. Miles. Now, she worries that generating more bills at 85% will drive competition over RVUs between the doctors who work with NP/ PA teams and the NPs/PAs themselves.
Or if physicians working with NPs/PAs want to continue billing 100% and safeguard a higher number of RVUs, they may have to do more work during shared visits than just providing an appropriate addendum.
“At what point,” Ms. Miles asks, “will doctors decide they no longer want to work in a team pair?” Currently, only 40% of the physicians in her group choose to work on a team with an NP/PA. In response to the new billing rules, she’s concerned that the ranks of hospitalists who want to work solo may grow, even though the hospitalists rely on their NP/PA teams to help manage their census.
The case for practicing autonomously Hospitalist Timothy Capstack, MD, was the lead author of an influential study on how groups use NPs/PAs that appeared in the October 2016 issue of the Journal of Clinical Outcomes Management.
In that research, Dr. Capstack found that his private group in Maryland—compared to an employed hospitalist group working in the same hospital—had the same outcomes with lower costs by using what the article called an “expanded PA” care model. Compared to the other group, his program relied on a much higher PA-to-physician staffing ratio, with physician-PA pairs seeing considerably more patients per day than its comparator.
Dr. Capstack’s group has now rebranded as Adfinitas Health, a private hospitalist group with about 200 physicians and 200 NPs/PAs serving in 15 hospitals and 50 post-acute care settings across six states. (Dr. Capstack is partner and clinical integration director.) Given that the group’s number of NPs/PAs has kept pace with that of doctors, it’s clear that NPs/PAs are still key to the program’s care model. Because the group relies on their ability to practice autonomously, NPs/PAs undergo extensive training and onboarding when they’re hired.
The extensive use of NPs/PAs is a selling point for hospital clients, Dr. Capstack says. “We’ve found a receptive environment,” he points out. “We’re more affordable because our salary needs are so much lower than groups staffed entirely by physicians. Hospitals have to offset less of our costs.”
Sometimes, doctors in his group do find it medically necessary to split a visit with an NP/PA, and “we’ll of course spend as much time as we need to,” he says. But many NP/PA visits are billed at only 85%, which Dr. Capstack says makes sense for his group.
“It takes a fair amount of time for the physician to earn that additional 15%,” he notes. “If it’s not clinically necessary, it makes more financial sense for physicians to see new patients of their own instead of doing several split visits. We don’t count on split visits for a big chunk of our reimbursement.” While the new billing rule will have some impact on him and his colleagues, he adds, “it probably won’t get to us as much as it might affect other groups that have different billing structures.”
How to assign RVUs Alissa M. Clough, MD, is president of Inpatient Physician Associates, a private hospitalist group in Lincoln, Neb., that covers two Bryan Health hospitals. To figure out what her group wants to do to get ready for the revised rules, Dr. Clough has put in hours with representatives of her group’s billing company as well as her hospitals’ director of medical informatics and operations director.
Until now, her group—with 38 physicians and 30 NPs/ PAs—has billed about 90% of its claims for NP/PA team care as split visits at 100%. Going forward, she’s not sure how many of those claims may start being billed at only 85%, or what impact that change could have on group revenue. (See “ An opportunity in open ICUs? “)
“The physicians may just go see more patients” as in Dr. Capstack’s group, Dr. Clough says. “In the end, we may not worry about the 15%.”
But that raises logistical and accounting challenges, she says, such as how to make sure the RVUs being billed at 85% under the NPs/PAs get assigned to the physicians who supervise them. That RVU assignment for physicians is also top of mind for Dr. Brimmer in Texas.
“One option may be to put all the RVUs generated by NP/PA billing at 85% into a bucket, then divide them among all the physicians who work with NPs/PAs,” says Dr. Brimmer. “That would assume that all those doctors use NPs/ PAs pretty evenly.” She adds that productivity accounts for as much as 25% of physicians’ income in her group.
In Nebraska, Dr. Clough and her colleagues are also trying to figure out what EHR and documentation changes are needed to accommodate the new billing rules. “Most of our shared billing right now is for admissions,” she points out. To meet the new rule’s component requirements for billing a shared visit at 100%, her group is reviewing how best to document in attestations that physicians are indeed providing the substantive portion of medical decision-making or of whichever component they choose to complete.
“Our physicians already do this, but has that been documented in a manner that complies with this new rule?” Dr. Clough says. “We’re working on adding some Epic SmartPhrases and a hard stop to make sure doctors document the assessment and plan within the attestation.” She also thinks that “physicians will have to do a bit more documentation and be more diligent about making sure the assessment and plan are on every attestation we do.”
Weighing component options According to Dr. Capstack in Maryland, the visit component that doctors opt to complete to meet the new rule will be based in part on the particular patient they’re treating. (Again, according to the new rules, physicians’ ability to document a note component in its entirety and bill a split visit will no longer be an option in 2023.) But in terms of being efficient with physician time in split visits this year, “I’m guessing that documenting the interval history might be the way to go,” he says. “That would be less cumbersome than medical decision-making, which makes up the bulk of the progress note.”
In Texas, Dr. Brimmer is also weighing options around the various visit components. While she is certainly sensitive to physicians’ time and productivity needs, she’s also concerned about NP/PA job satisfaction.
“If we have to structure split visits in a way that NPs/PAs can’t bring anything to the table in terms of their clinical thinking, I’m worried they’ll feel like a scribe,” Dr. Brimmer says. “That concerns me. I definitely respect and value our advanced practice clinicians, and the last thing I want to do is lose them.”
For at least the first quarter this year, Dr. Brimmer adds, she and her colleagues may not make major changes. Instead, “we may just let the chips fall where they may, then make whatever changes we need.”
Mr. Powe from the AAPA points to another unknown: what definitive guidance Medicare administrative contractors (MACs) might put out about the revised rules and how much variation among MACs there will be. In the meantime, his biggest concerns are about 2023, when the rules are slated to change—and split billing may be based exclusively on time.
If that’s the case for 2023, “it may be necessary for the CMS to have some discussions with various professional groups about that,” he says. Dr. Clough in Nebraska agrees.
“We’re going to take this a year at a time,” she says. As for the drastic changes slated for 2023, “I’m going to hope that the Society of Hospital Medicine and other groups will continue to work toward solutions that benefit all parties. I worry about the strain on groups from only time-based coding for all shared visits.”
Phyllis Maguire is Executive Editor of Today’s Hospitalist
An opportunity in open ICUs?
WHEN IT COMES to the CMS’ revised rules for split billing, the possible impact on billing new and subsequent inpatient visits—and on hospitalist workflow—are getting most of the attention. But the new rules include other changes that should be on hospitalists’ radar.
“Shared critical care billing could have some advantages.” ~ Alissa M. Clough, MD Inpatient Physician Associates
For one, NPs/PAs and physicians for the first time can now submit split bills for some services in skilled nursing facilities. That change may not have much of an impact because two providers aren’t usually engaged in SNF visits.
But here’s another first: Physicians and NPs/PAs can now submit split bills for critical care services, and that’s a big deal for hospitalists who work with NPs/PAs in open ICUs. Inpatient Physician Associates in Lincoln, Neb., a private hospitalist group that covers two Bryan Health hospitals, does just that, says president Alissa M. Clough, MD.
“Shared critical care billing could have some advantages, and I’m excited about it,” Dr. Clough says. “Now, we’ll be able to get credit for both physicians’ and NPs/PAs’ time, which should boost our payments.” While her group’s NPs/PAs may start billing additional non-critical care services at 85%, the gains or added RVUs that group members may see in split critical care billing could offset that lost revenue.
Critical care services, of course, are billed according to time, so the new split billing rules in the ICU pose some logistical and template challenges. According to Dr. Clough, she and her colleagues aren’t sure yet how to best capture the time element for each provider.
But “we may have to revise the critical care note—and we’ll need some kind of pop-up or alert to make sure physicians enter both their time and that of the associate,” she says. Her group plans to lean on its Epic resources to make documenting time spent providing critical care for split bills more seamless.
“Whatever alert we go with, it has to be built in so time is tracked for every shared ICU visit,” Dr. Clough notes. “It can’t be user-dependent.”
How many NPs/PAs bill independently?
It remains to be seen how new CMS rules on split billing that took effect Jan. 1 may change the number of hospitalist NPs/PAs who are billing independently.
For an idea of what billing statistics have looked like up to now, the “2020 State of Hospital Medicine Report” published by the Society of Hospital Medicine offers a great snapshot. For hospitalist groups that treat only adults, 83.3% reported employing NPs/PAs, a percentage that varies widely by region. Close to 94% of groups in the East, for instance, use NPs/PAs, but that’s true for only a bare majority (50.8%) in the West.
As for how those programs bill the work of their NPs/PAs, 17.4% said that NPs/PAs bill independently, while almost twice as many—31.6%—bill their work as shared services under a collaborating/supervising physician’s provider number. However, an even larger percentage—42.9%—use a combination of both independent and shared services billing. A much smaller group (8.1%) reported that NPs/PAs don’t provide billable services or at least don’t submit service charges to payers.
Other stats from the 2020 report on NPs/PAs:
• Among different employment models, 88.3% of multistate hospitalist management companies said they employ NPs/PAs, which is true for only 40% of private multispecialty or primary care groups.
• Private multispecialty/PCP groups have the highest percentage of NPs/PAs billing services independently: 26.7%.
• Among NPs/PAs employed by hospitals, health systems or integrated delivery systems, only 10.5% of NP/PA services are independently billed.
Published in the January/February 2022 issue of Today’s Hospitalist
RELATED ARTICLES MORE FROM AUTHOR

How many hospitalists work with NPs/PAs?

How to get hospital at home up to scale

Study: Big benefits from oncology comanagement
I think APPs are much better utilized in specialty (particularly proceduralists) groups. While the doc is doing procedures, the NP/PA can see the floor consults and put in some preliminary orders. General hospital medicine, in my opinion, can and should be managed by physicians only. I know the APPs are typically utilized for lower acuity follow ups and H&P/Consults during call shifts. However, it is nice to have some lower acuity visits during the day and most days that I’m on call, it’s faster for me to just see the patient, put in orders and note myself.
On-line Only

I am “JUST” the hospitalist

Writing retreats build community among academic hospitalists

Throughput innovations: one hospital’s solutions to improve length of stay

How much paid time off do hospitalists get?

A doctor’s struggle for patient care

Flexible scheduling: smoother workflow, happier doctors?

Matching shift-start times to workflow

Different strengths, skills, personalities

Making the most of scheduling software

Seasonal staffing

Covid News Updates

Are hospitalists more or less satisfied than when they started in...
Featured articles.

Treating stroke: this year’s headlines

A look at average shift lengths for hospitalists

What type of shift do hospitalists work?

What are health systems doing to attract and retain nurses?

Tearing down barriers to mental health resources

How’s it going with the new E/M inpatient coding changes?
- Privacy Policy and Terms of Use
Observation care: Is it still stressing you out?
License for Use of "Physicians' Current Procedural Terminology", (CPT) Fourth Edition
End User/Point and Click Agreement: CPT codes, descriptions and other data only are copyright 2009 American Medical Association (AMA). All Rights Reserved (or such other date of publication of CPT). CPT is a trademark of the AMA.
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials including but not limited to CGS fee schedules, general communications, Medicare Bulletin , and related materials internally within your organization within the United States for the sole use by yourself, employees, and agents. Use is limited to use in Medicare, Medicaid, or other programs administered by the Centers for Medicare & Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
This product includes CPT which is commercial technical data and/or computer data bases and/or commercial computer software and/or commercial computer software documentation, as applicable which were developed exclusively at private expense by the American Medical Association, 515 North State Street, Chicago, Illinois, 60610. U.S. Government rights to use, modify, reproduce, release, perform, display, or disclose these technical data and/or computer data bases and/or computer software and/or computer software documentation are subject to the limited rights restrictions of DFARS 252.227-7015(b)(2)(June 1995) and/or subject to the restrictions of DFARS 227.7202-1(a)(June 1995) and DFARS 227.7202-3(a)June 1995), as applicable for U.S. Department of Defense procurements and the limited rights restrictions of FAR 52.227-14 (June 1987) and/or subject to the restricted rights provisions of FAR 52.227-14 (June 1987) and FAR 52.227-19 (June 1987), as applicable, and any applicable agency FAR Supplements, for non-Department Federal procurements.
AMA Disclaimer of Warranties and Liabilities.
CPT is provided "as is" without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. AMA warrants that due to the nature of CPT, it does not manipulate or process dates, therefore there is no Year 2000 issue with CPT. AMA disclaims responsibility for any errors in CPT that may arise as a result of CPT being used in conjunction with any software and/or hardware system that is not Year 2000 compliant. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CGS or the CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
CMS Disclaimer
The scope of this license is determined by the AMA, the copyright holder. Any questions pertaining to the license or use of the CPT must be addressed to the AMA. End Users do not act for or on behalf of the CMS. CMS DISCLAIMS RESPONSIBILITY FOR ANY LIABILITY ATTRIBUTABLE TO END USER USE OF THE CPT. CMS WILL NOT BE LIABLE FOR ANY CLAIMS ATTRIBUTABLE TO ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION OR MATERIAL CONTAINED ON THIS PAGE. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information or material.
This license will terminate upon notice to you if you violate the terms of this license. The AMA is a third party beneficiary to this license.
POINT AND CLICK LICENSE FOR USE OF "CURRENT DENTAL TERMINOLOGY", ("CDT")
End User License Agreement
These materials contain Current Dental Terminology, Fourth Edition (CDT), copyright © 2002, 2004 American Dental Association (ADA). All rights reserved. CDT is a trademark of the ADA.
THE LICENSE GRANTED HEREIN IS EXPRESSLY CONDITIONED UPON YOUR ACCEPTANCE OF ALL TERMS AND CONDITIONS CONTAINED IN THIS AGREEMENT. BY CLICKING BELOW ON THE BUTTON LABELED "I ACCEPT", YOU HEREBY ACKNOWLEDGE THAT YOU HAVE READ, UNDERSTOOD AND AGREED TO ALL TERMS AND CONDITIONS SET FORTH IN THIS AGREEMENT.
IF YOU DO NOT AGREE WITH ALL TERMS AND CONDITIONS SET FORTH HEREIN, CLICK BELOW ON THE BUTTON LABELED "I DO NOT ACCEPT" AND EXIT FROM THIS COMPUTER SCREEN.
IF YOU ARE ACTING ON BEHALF OF AN ORGANIZATION, YOU REPRESENT THAT YOU ARE AUTHORIZED TO ACT ON BEHALF OF SUCH ORGANIZATION AND THAT YOUR ACCEPTANCE OF THE TERMS OF THIS AGREEMENT CREATES A LEGALLY ENFORCEABLE OBLIGATION OF THE ORGANIZATION. AS USED HEREIN, "YOU" AND "YOUR" REFER TO YOU AND ANY ORGANIZATION ON BEHALF OF WHICH YOU ARE ACTING.
- Subject to the terms and conditions contained in this Agreement, you, your employees, and agents are authorized to use CDT-4 only as contained in the following authorized materials and solely for internal use by yourself, employees and agents within your organization within the United States and its territories. Use of CDT-4 is limited to use in programs administered by Centers for Medicare & Medicaid Services (CMS). You agree to take all necessary steps to ensure that your employees and agents abide by the terms of this agreement. You acknowledge that the ADA holds all copyright, trademark and other rights in CDT-4. You shall not remove, alter, or obscure any ADA copyright notices or other proprietary rights notices included in the materials.
- Applicable Federal Acquisition Regulation Clauses (FARS)\Department of Defense Federal Acquisition Regulation Supplement (DFARS) Restrictions Apply to Government use. Please click here to see all U.S. Government Rights Provisions .
- ADA DISCLAIMER OF WARRANTIES AND LIABILITIES. CDT-4 is provided "as is" without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. No fee schedules, basic unit, relative values or related listings are included in CDT-4. The ADA does not directly or indirectly practice medicine or dispense dental services. The sole responsibility for the software, including any CDT-4 and other content contained therein, is with (insert name of applicable entity) or the CMS; and no endorsement by the ADA is intended or implied. The ADA expressly disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon notice to you if you violate the terms of this Agreement. The ADA is a third-party beneficiary to this Agreement.
- CMS DISCLAIMER. The scope of this license is determined by the ADA, the copyright holder. Any questions pertaining to the license or use of the CDT-4 should be addressed to the ADA. End users do not act for or on behalf of the CMS. CMS DISCLAIMS RESPONSIBILITY FOR ANY LIABILITY ATTRIBUTABLE TO END USER USE OF THE CDT-4. CMS WILL NOT BE LIABLE FOR ANY CLAIMS ATTRIBUTABLE TO ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION OR MATERIAL COVERED BY THIS LICENSE. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information or material.
The license granted herein is expressly conditioned upon your acceptance of all terms and conditions contained in this agreement. If the foregoing terms and conditions are acceptable to you, please indicate your agreement by clicking below on the button labeled "I ACCEPT". If you do not agree to the terms and conditions, you may not access or use the software. Instead, you must click below on the button labeled "I DO NOT ACCEPT" and exit from this computer screen.

Stay Connected
People With Medicare
- 888.739.7039
- Client Portal
- Business and Practice Valuations
- Clinical Workforce Optimization
- Co-Sourcing/Interim Services
- CPT Solutions | Physician Fee Schedule
- Governance and Compliance
- Executive Governance
- Fair Market Value and Commercial Reasonableness
- Mergers and Acquisitions
- Physician Affiliation and Needs Assessment
- Provider Affiliation and Optimization
- Tools and Technology Solutions
- Provider Needs Assessment
- Total Rewards
- Compensation Benchmarking
- Compensation Design
- Physician Compensation Design
- Living Wage
- Workforce and Performance Analytics
- Performance Analytics and Advisory Services
- Workforce Insights360™
- Advanced Practice Providers
- Academic Medical Centers
- For-Profit Health Care
- Health Plans
- Hospitals and Health Systems
- Integrated Delivery Systems
- Medical Groups
- Pediatric Health Care Organizations
- C3 Nonprofit Consulting Group
- Associations
- Foundations
- Higher Education
- Research Institutes
- Service and Charitable Organizations
- Health Care Management and Executive Compensation Survey
- Health Plan Management and Executive Compensation Survey
- Physician Executive Compensation Survey
- Medical Group Executive Compensation Survey
- Benefits Practices in Health Care Organizations Survey
- Endowment and Foundation Investment Staff Compensation Survey
- Physician Compensation and Productivity Survey
- Medical Group Compensation and Productivity Survey
- Physician and APP CPT Work RVU Benchmark Study
- Physician and APP On-Call Compensation Survey
- Hospital-Based Physician and APP Work Effort Practices Survey
- Advanced Practice Provider Compensation and Productivity Survey
- Advanced Practice Provider Leadership and Organizational Survey
- Health Care Staff Compensation Survey
- Workforce Metrics Benchmark Survey
- Registered Nursing Compensation Survey
- Meet Our Leadership
- Career Opportunities
- Why Choose SullivanCotter
- Working at SullivanCotter
2022 Physician Fee Schedule: Understanding Changes to Split/Shared Visits
Download full article.
Each year, the Centers for Medicare and Medicaid Services (CMS) incorporates changes in policy, regulations and requirements for billing under the Medicare Physician Fee Schedule (PFS). These changes are often adopted by commercial payers.
On November 2, 2021, CMS released the final rule for the 2022 PFS that included changes to split/shared visits scheduled to go into effect on January 1, 2022. The proposed changes included some important considerations related to the conditions for submitting split/shared visits for reimbursement and have the potential to alter the existing workflow of physicians and advanced practice providers (APPs) related to billing for split/shared encounters.
While some changes took effect in 2022, a number of the most impactful changes to split/shared billing were delayed to January 1, 2024. The 2023 PFS final rule indicates CMS’ desire to make significant changes to split/shared visits while allowing organizations time to prepare.
Split/Shared Visits
According to the Medicare Claims Processing Manual Publication #100-04:
“A split/shared E/M visit is defined by Medicare Part B payment policy as a medically necessary encounter with a patient where the physician and a qualified non-physician provider each personally perform a substantive portion of an evaluation and management (E/M) visit face-to-face with the same patient on the same date of service. A substantive portion of an E/M visit involves all or some portion of the history, exam or medical decision-making key components of an E/M service. The physician and the qualified NPP must be in the same group practice or be employed by the same employer.”
Split/shared E/M visits are only applicable in the hospital inpatient and hospital outpatient departments using provider-based billing and emergency room sites of service for all professional encounters currently except for critical care services, procedures, or time-based codes (e.g., prolonged service time).
What is Changing?
The 2022 final rule included several changes that are designed to reflect current clinical practice, recognize APPs’ evolving role as members of the care team, reduce duplication of services and clarify the conditions of payment for these types of services. 1,2 These changes were implemented beginning in 2022 with additional changes identified for implementation in 2024. The most significant change is moving the split/shared visit from an E/M and medical decision-making based attribution to a time-based attribution. Under the current medical decision-making rubric, split/shared visits are typically billed by physicians, assuming specific conditions of collaboration have been met (e.g., face to face encounter, contributing to the evaluation, management or medical decision, employed by the same group or employer). In 2022, changes include the allowance of time-based accounting for a split/shared visit where “the practitioner who provides the substantive portion of the visit (more than ½ of the total time spent) would bill for the visit.” In 2022 and 2023, split/shared visits can be submitted using the current medical decision-making methodology or the new time-based methodology. Other changes applicable in 2022 include the ability for critical care services to be reported as split/shared, and the requirement that a new billing modifier be added for all shared visits. A survey performed by SullivanCotter of National APP Advisory Council (NAAC) members found that 54% of organizations were still using split shared billing. 3
The greatest impact on split/shared visit billing is set to occur in 2024 when all shared visits must be billed using the time-based methodology where the practitioner who provides the substantive portion of the visit (“more than ½ of the total time spent”) bills for the visit1. In 2022 and 2023, the impact of the split/shared change will likely be modest but will allow organizations time to better understand the degree of split/shared billing that occurs within their organizations through the shared visit modifier requirement.
In 2024, the impact on attributed wRVUs for physicians and APPs providing services in the inpatient setting could be significant. The time-based methodology will require physicians to have greater than 50% of the time spent with a patient in order to bill and receive wRVU attribution. Because of this change, in 2024, the same patient volume using current split/shared workflows could result in an increase in reported APP wRVUs and a corresponding decrease in reported physician wRVUs. This change could also result in an overall decrease in professional collections (to account for the 15% difference in Medicare physician and APP reimbursement levels for the same service).
When accounting for time, CMS identified these specific activities: 2
- Preparing to see the patient (for example, review of tests).
- Obtaining and/or reviewing separately obtained history.
- Performing a medically appropriate examination and/or evaluation.
- Counseling and educating the patient/family/caregiver.
- Ordering medications, tests, or procedures.
- Referring and communicating with other health care professionals (when not separately reported).
- Documenting clinical information in the electronic or other health record (Note: CMS has stated it may be helpful for each individual to document their own participation in the medical record in order to determine the substantive time).
- Independently interpreting results (not separately reported).
- Communicating results to the patient/family/caregiver.
- Care coordination (not separately reported).
A hospitalized patient with a diagnosis of pneumonia is being cared for by the hospital medicine team composed of a physician and an APP. On hospital day 2, the APP sees the patient in the morning and spends 25 minutes with the patient performing a focused history and physical, reviewing the morning labs and providing patient education related to the course of treatment with the patient and their family. Based on a detected decrease in lung sounds during the lung exam, the APP orders a chest x-ray. Later in the day, the physician and the APP spend an additional 10 minutes together to make afternoon rounds and review the chest x-ray findings, make changes in treatment, and meet with the patient to review the chest x-ray results (35 minutes in total for the APP and 10 minutes total for the physician).
The hospital medicine team bills the encounter as 99233 (subsequent hospital care level 3). Under the historical medical decision-making approach, this could be billed by the physician as a split/shared visit (assuming all of the other criteria were met) or by the APP (paid at 85% of the allowed amount for Medicare patients).
Under the time-based billing approach, the visit could only be billed by the APP as the APP provided the majority of the encounter (35 out of 45 minutes or 78% of the total time spent in the encounter). As the physician would not receive wRVU or reimbursement credit for this visit using this methodology, this could impact credited physician productivity and, for organizations using productivity-based compensation models, both physician and APP compensation.
Current care delivery models should be reevaluated when developing a strategy to transition to time-based billing for split/shared visits. It is important to design an effective and transparent workflow that allows for top-of-licensure operation and minimizes any competition for credit. With changes imminent, organizations can take the following steps to prepare:
- Assess the current state of split/shared billing at your organization.
- Evaluate current care team composition and work responsibilities to determine the optimal team composition and anticipated wRVU attribution impact to ensure that providers are efficient and optimally utilized.
- Assess the impact on specific patient workflows (e.g., new patients, established patients, discharges) where split/shared visits are utilized today.
- Identify types of encounters that could be performed solo by the APP thus allowing physician to see other patients.
- Consider if modifications to physician and APP compensation arrangements are needed to ensure financial sustainability and regulatory compliance. Be aware these changes may influence the reported wRVU and compensation per wRVU 2023 survey report data.
1. Calendar Year (CY) 2022 Medicare Physician Fee Schedule Final Rule. Published November 2, 2021. Retrieved from https://www.cms.gov/newsroom/fact-sheets/calendar-year-cy-2022-medicare-physician-fee-schedule-final-rule
2. RIN 0938-AU42 Medicare Program; CY 2022 Payment Policies under the Physician Fee Schedule and Other Changes to Part B Payment Policies. Published November 19, 2021. Retrieved from https://www.federalregister.gov/d/2021-23972
3. National APP Advisory Council – Fall 2022 Pulse Survey
Contact Us to Learn More
- Insights & Events
About McDermott
- Firm Overview
- Vision & Values
- Our Approach
- Justice, Diversity, Equity & Inclusion
- Pro Bono & Community Service
CMS Finalizes Changes to Clarify Physician and NPP “Split (or Shared)” Billing Policy
- CMS Finalizes Changes to Clarify Physician and NPP “Split ...
On November 2, 2021, the Centers for Medicare & Medicaid Services (CMS) issued the calendar year (CY) 2022 Medicare Physician Fee Schedule (MPFS) final rule which, among other policy and regulatory changes, finalized regulations codifying CMS requirements for billing for “split (or shared)” evaluation and management (E/M) visits under the MPFS. Split (or shared) visits are E/M visits provided in part by both physician and non-physician practitioners (NPPs) and are now defined at 42 CFR § 415.140. NPPs generally include nurse practitioners, physician assistants and clinical nurse specialists, and are also known outside of the Medicare program by other names, such as advanced practice practitioners. The finalized regulations generally reflect prior CMS guidance for billing “split/shared” visits, but also incorporates changes from the historical guidance that introduce new opportunities and restrictions on providing what are now known as split (or shared) visits.
Medicare reimburses services paid under the MPFS and furnished by NPPs at 85% of the rate paid when a physician furnishes the same service. Under CMS regulations, when a patient visit is performed in part by a physician and in part by a NPP in a physician office setting, the physician is permitted to bill for the visit under their own NPI and receive the higher Medicare payment rate. These services are considered to be services furnished “incident to” a physician’s professional services and must meet other Medicare requirements for “incident to” services. CMS regulations have not historically addressed services furnished in part by a physician and in part by an NPP in the facility setting ( e.g. , hospitals and skilled nursing facilities (SNFs)). Instead, CMS relied solely on guidance found in the Medicare Claims Processing Manual (MCPM) to establish requirements for coverage and payment of such services. In May 2021, in response to a petition submitted under the US Department of Health and Human Services’ Good Guidance Practices Regulation, CMS withdrew the MCPM sections specifically addressing split (or shared) visits and indicated that CMS would reissue the guidance as proposed regulations.
For dates of service on or after January 1, 2022, the new finalized regulations specify the requirements that must be met in order for a physician or NPP to bill a split (or shared) visit in a hospital, SNF or other facility setting. The final rule expands the clinical scenarios under which a healthcare professional can bill for services performed in part by another practitioner but also imposes restrictions on which performing practitioners can bill for the split (or shared) visit. While the finalized regulations provide the circumstances under which a physician or NPP may bill for professional services furnished to patients in a facility setting, this regulation addresses only services furnished in the facility setting and paid under MPFS. It does not appear to apply to facility services payable under a separate payment system ( i.e. , for hospitals, under the outpatient prospective payment system, or for SNFs, under the SNF prospective payment system).
In addition to clarifying when split (or shared) visits may be billed to Medicare, the finalized regulations modify CMS’s policy and permit physicians and NPPs to bill for split (or shared) visits for both new and established patients, critical care services and certain E/M visits in a SNF. In issuing the new rules, CMS indicated that prior guidance had been interpreted as limiting split (or shared) visit billing to established patients and prohibited billing for split (or shared) visits involving critical care services or in SNFs. The new regulations also define “split (or shared) visit” as E/M visits performed in part by a physician and NPP in institutional settings for which “incident to” payment is not available. This definition is intended to distinguish between the policy applicable to services furnished “incident to” the professional services of a physician in a physician office setting and the policy applicable to services furnished in a facility setting.
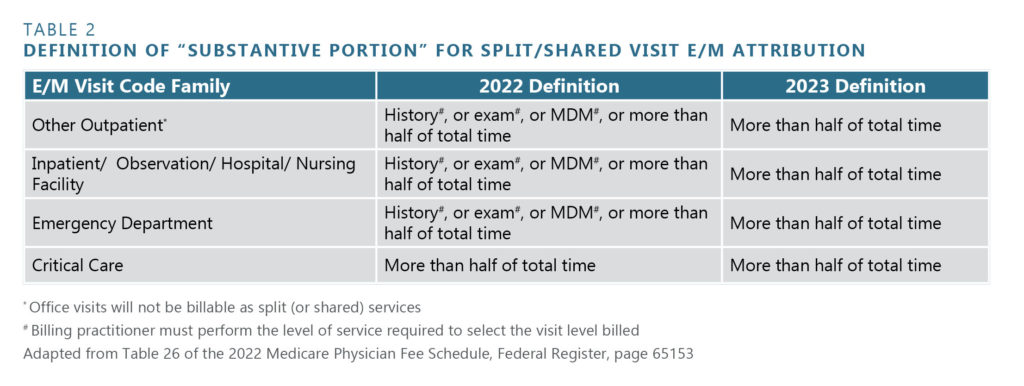
In the final rule, CMS established which of the physician or NPP performing a split (or shared) visit can bill Medicare for the visit. This is an important concept because the visit is paid at a higher rate if the physician submits the claim rather than the NPP. Historically, in determining whether a physician or an NPP may bill for a split (or shared) visit, either the physician or the NPP could bill for the service as long as the billing practitioner performed a “substantive portion” of the visit. In the final rule, CMS codified its policy as proposed and, effective January 1, 2023, will utilize time as the key factor in determining whether the physician or the NPP performed the substantive portion of the visit. CMS finalized its proposal to limit the billing practitioner to the individual who performed more than 50% of the visit. In response to concerns raised from commenters, CMS provided a one-year transitional period that will permit either time or the provision of one of three key components of the visit (history, exam or medical decision-making) to be considered a “substantive portion” of the visit. If performing a key component of the visit is utilized, the practitioner who bills the visit must perform that component in its entirety. For critical care services, which are time-based codes, the physician or NPP must provide more than half of the total time in order to bill for the visit.
CMS also finalized a list of activities that may count toward the total time of the E/M visit for purposes of determining the provider who performed the substantive portion of the visit. Under the final rule, documentation in the medical record must identify both professionals who performed the visit, and the individual who performed the substantive portion (and bills for the visit) must sign and date the medical record. CMS clarified that for all split (or shared) visits, while one of the practitioners must have face-to-face (in-person) contact with the patient, the face-to-face contact does not necessarily need to be with the practitioner who performs the substantive portion and bills for the visit.
CMS also finalized the rule to provide important clarifications to its policy and to permit either a physician or an NPP to bill for split (or shared) visits for both new and established patients and for initial or subsequent visits. This expands the availability of split (or shared) visit billing in the facility setting.
Under its previous policy, CMS did not permit healthcare professionals to bill for split (or shared) visits for critical care services or for E/M visits in a SNF. In the proposed rule, CMS proposed to permit healthcare professionals to bill for split (or shared visits) that are critical care services. CMS also proposed to expand split (or shared) visit billing to permit E/M visits to be furnished by a physician and a NPP in a SNF setting. CMS finalized both these proposals in the final rule. However, CMS also proposed to clarify that no other E/M visit can be billed for a patient on the same date as critical care services are furnished when the services are furnished by the same professional (or professionals) in the same specialty and group. In light of significant public comments, CMS did not adopt this limitation as proposed. Rather, the final rule provides that an E/M service can be billed for a patient on the same day as critical care services as long as the physician documents that (1) the E/M service was provided prior to the critical care service (when the patient did not require critical care), (2) the E/M service is medically necessary, (3) the E/M service is separate and distinct from the critical care services, and (4) the E/M service does not include any elements of the critical care services furnished later in the day. The critical care services must be reported using modifier -25 on the claim.
Under previous guidance, a physician and an NPP had to be in the “same group” in order to bill for a split (or shared) visit. In the proposed rule, CMS declined to define “same group” for purposes of the new split (or shared) visit billing rule and sought comments on how to define same group. The final rule retains the requirement that split (or shared) visits must be performed by a physician and NPP who are in the same group, although, consistent with the proposed rule, CMS declined to adopt a definition for a “group.” Commenters agreed with CMS that appropriately defining a “group” in the context of split (or shared) visits is a complex issue. Although CMS considered several options, including using the definition under the Stark Law or considering practitioners under the same billing tax ID number to be the same group, CMS declined to adopt a definition of “group.” This determination is important because if the two practitioners are determined not to be in the same group, neither practitioner will be able to bill for the visit, assuming neither performed a complete E/M visit. As it currently stands, providers will need to determine how to ensure that physicians and NPPs are practicing in the “same group” to bill for split (or shared) visits without explicit guidance from CMS.
CMS made it clear in the final rule that it will not pay for partial E/M visits. CMS also finalized its proposal to create a claim modifier that is mandatory for split (or shared) visits. This modifier will allow CMS to identify services furnished in part by NPPs and will allow for more targeted review of services furnished by physicians and NPPs. CMS did not provide the specific modifier that will be required.
The following chart summarizes the previous guidance and the finalized revisions to CMS’s policy for split (or shared) visits in the final rule:
PRACTICAL IMPLICATIONS
CMS finalized significant changes to its long-standing policy on billing for split (or shared) visits in the facility setting. The changes provide both new opportunities for billing such visits, including for new patients, services in SNFs and critical care visits, but also restrict the reimbursement opportunity for services that are performed primarily by NPPs. In light of the new regulations, providers utilizing the split (or shared) billing concept, or who may do so in the future, should review the changes and ensure that their split (or shared) billing policies are consistent with the new rules.
Providers should begin considering how to track and document the time physicians and NPPs each spend furnishing services to patients. While this is consistent with the updated CPT guidance for E/M services, ensuring services meet the time requirements will also be important to the extent providers contemplate relying on the split (or shared) visit regulations to bill for services that are performed jointly by physicians and NPPs. While CMS has provided a one-year transition period for full implementation of the component of the rules governing how to evaluate whether a split (or shared) visit should be billed under the NPI of the physician or the NPI of the NPP who shared in furnishing services as part of the visit, this flexibility will end effective January 1, 2023. In addition, the medical record documentation and claim modifier requirements may necessitate modifications to longstanding documentation and billing practices for physicians and NPPs who furnish services in facility settings. Providers also should consider establishing and memorializing the definition of “same group” that will be used to determine which physicians and NPPs can jointly furnish services billed under the split (or shared) billing rules.
Stay Connected
Emily jane cook.
Partner | Los Angeles
Caroline Reignley
Partner | Washington, DC
You are using an outdated browser. Please upgrade your browser or activate Google Chrome Frame to improve your experience.

- The PYA Way
- Pay Invoice

The CMS 2023 Proposed Rule: Questions Unanswered on Split (or Shared) Visits
Public comments on the rule close september 6.
In early July 2022, the Centers for Medicare & Medicaid Services (CMS) released the 2023 Proposed Rule, which addressed split (or shared) visits. A split visit is an evaluation and management (E/M) service performed jointly between a physician and an advanced practice provider (APP) and is billed under the physician’s National Provider Identifier (NPI) at 100% of the Medicare Physician Fee Schedule (MPFS), rather than 85% if it were billed under the APP’s NPI. To bill for a split visit, the following requirements must be satisfied:
- The physician and APP must be employed by the same group practice (i.e., same Tax ID), or the APP must be an expense to the physician practice through, for example, a lease arrangement.
- The service must be performed in a facility setting as opposed to an office setting (review the incident to [1] requirements for an office setting).
- The visit requires a substantive portion to be performed by both the physician and APP.
CMS is providing a 60-day public comment period on the 2023 Proposed Rule, which closes on September 6, 2022. This PYA insight will provide more clarity on how split and shared visits are addressed in the 2023 Proposed Rule.
2022 CMS Policy
Before diving into the CMS 2023 Proposed Rule, it is important to mention the definition of a “substantive portion” was revised by CMS in calendar year (CY) 2022. CMS introduced a change that further defined a “substantive portion” as more than half of the total time of the visit, meaning the visit should be billed under the provider who performs more than 50% of the total time counted for the visit. Time relevant to split visits is defined in the 2022 Final Rule consistent with the 2021 E/M Guidelines and, notably, is not relevant to the 1995/1997 E/M guidelines. To allow for a transition period, CMS stated physicians could alternatively meet the level of one of the key components (history, exam, or medical decision-making [MDM]) to support selecting the physician, as opposed to the APP, as the billing provider. Prior to 2022, CMS defined the physician documentation requirement of a “substantive portion” as all or some portion of the history, exam, or MDM key components of an E/M service.
The changes finalized in the CY2022 Final Rule created significant internal process and revenue challenges for provider organizations. Effectively, more work and documentation from the physicians were expected for the same or less reimbursement. Fortunately, due to the feedback and comments from the public after the Final Rule was published, CMS is proposing a delay to the implementation of the revised definition of the substantive portion in the 2023 Proposed Rule until CY2024, to allow a smoother conversion.
Specifically, the Proposed Rule states:
We are amending § 415.140 by adding to paragraph (a) “and 2023” after the phrase “For visits other than critical care visits furnished in calendar year 2022.” Therefore, the proposed paragraph would specify, for visits other than critical care visits furnished in calendar years 2022 and 2023, substantive portion means one of the three key components (history, exam, or MDM) or more than half of the total time spent by the physician and NPP performing the split (or shared) visit.
However, in the newsroom post of the 2023 MPFS fact sheet, CMS defines a substantive portion of a visit by any of the following elements:
- Performing a physical exam
- Making a medical decision
- Spending time (more than half of the total time spent by the practitioner who bills the visit)
These two descriptions are inconsistent with each other and with the 2022 Final Rule. Again, the 2022 Final Rule stated the physician had to meet the level of one key component. This guidance does not state that, but it also does not clarify what it means. If CMS is saying physicians can return to pre-2022 requirements and document a portion of the history, exam, or MDM to meet the requirement of billing provider selection, that should be confirmed and clarified in Final Rule verbiage. Additionally, the industry would applaud that finalization. However, if CMS is, in fact, requiring one of the three key components be met for the physician to be selected as the billing provider, there is a conflict in the guidelines.
2023 E/M Guideline Changes
The dilemma with the substantive portion definition guidance provided for 2023—if the expectation is for the key component to be fully documented by the physician—is it does not align with the new 2023 E/M guideline requirements. Unlike the 1995/1997 E/M guidelines, the 2023 guidelines [2] require only a medically appropriate history and/or examination. The extent of the history and exam is not an element in the selection of an E/M service in the inpatient setting. Therefore, the only key component with a defined level is the MDM. This creates confusion for providers trying to perform split visits compliantly, while also implementing the simplified 2023 E/M guidelines in their documentation practices.
It would be an additional administrative burden for providers to consider the 1995/1997 E/M guidelines [3] when performing split visits in CY2023; therefore, it is important to get this clarified.
- Due to the conflicting guidance provided by CMS, we recommend organizations comment prior to the September 6 deadline to request this clarification and include their recommendations for a solution.
Additional Impact Considerations
wRVU Attribution
Because the CY2022 change creates a significant time burden on the physician, it is expected that some visits previously performed as a split visit will be performed only by the APP and billed under the APP’s NPI number at 85% of the fee schedule. Many organizations attribute work relative value units (wRVUs) generated by split visits to the “Billing Provider;” and under the current requirements, the physician is usually designated, which awards the physician wRVU credit for the visit. If the APP becomes designated as the Billing Provider by performing a substantive portion (or all) of the visit, the APP would by default be awarded all the wRVU credit for the visit. The reason for this anticipated shift is due to the common understanding that APPs generally spend more time with the patient than the physician. The physician’s contribution is expertise and quality assurance, elevating the level of care overall; time is less of a factor. The immediate impact of this change is the involved physicians’ wRVU credit would significantly decrease.
- Organizations that utilize a production-based incentive program will need to consider this change and how wRVUs associated with split visits are allocated among the contributing providers and adjust the accounting of personally performed services of the physician accordingly.
- Organizations should communicate this impact on compensation design and other downstream impacts, such as discouraging team-based care approaches, to CMS during the comment period.
Revenue Impact
As noted above, if the APP, rather than the physician, is designated as the Billing Provider for split visits, organizations will receive 15% less Medicare revenue for visits previously reimbursed at 100% of the fee schedule. This shift could result in significant loss of revenue for some specialties.
- The financial impact of this change will need to be analyzed, and organizations should develop a proactive plan for addressing the revenue decrease.
- The anticipated revenue impact on your organization should be communicated to CMS in the comment period.
Billing Processes
As part of the CY2022 Final Rule, CMS required a modifier be appended to all split visits for tracking purposes. After the Final Rule was published, modifier “FS” was designated to indicate split visits.
- Billing systems should be updated with the new FS modifier and processes developed to ensure the modifier is applied to all split visits.
- Robust internal auditing processes will need to be implemented to ensure split visits follow CMS requirements. The new FS modifier will make it easier for organizations and CMS to identify split visits for auditing purposes.
CY2023 Proposed Rule and Comment Period
CMS still believes adjusting the definition to be more than half of the total time—and not based on MDM or the key components—is the right direction to go. However, the delay in the CY2022 rule will allow time to consider feedback and comments from interested parties, so it can determine whether there is a necessity for additional changes to policy.
We highly encourage providers to offer comments to CMS regarding what they believe satisfies physician involvement during a split visit to bill at 100% of the MPFS, as well as the impact of the impending shift to a time-based approach to team-based care, reimbursement, and the need to overhaul physician compensation design to address physician personally performed services now allocated in APP billing data and reimbursed at 85% of prior reimbursement.
If you would like assistance with the 2023 MPFS Proposed Rule, or any matter involving valuation, strategy and transactions, or compliance, one of our executive contacts would be happy to assist. You may email them below, or call (800) 270-9629.
https://www.cms.gov/newsroom/fact-sheets/calendar-year-cy-2023-medicare-physician-fee-schedule-proposed-rule
https://public-inspection.federalregister.gov/2022-14562.pdf
[1] https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/r1764b3.pdf
[2] https://www.ama-assn.org/system/files/2023-e-m-descriptors-guidelines.pdf
[3] https://www.cms.gov/outreach-and-education/medicare-learning-network-mln/mlnedwebguide/downloads/97docguidelines.pdf
Executive Contacts
Thanks for reaching out. You can contact me at 404-266-9876.
Thanks for reaching out. You can contact me at 800-270-9629.

- Privacy Overview
- Strictly Necessary Cookies
This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
Strictly Necessary Cookie should be enabled at all times so that we can save your preferences for cookie settings.
If you disable this cookie, we will not be able to save your preferences. This means that every time you visit this website you will need to enable or disable cookies again.

The 2022 CMS Split/Shared Visit Rules and the Anticipated Impacts
The 2022 Split/Shared Visit rule changes may create disruption to wRVU credit, physician and APP compensation, and overall revenue generated.
When many executives read reviews of the 2022 Medicare Physician Fee Schedule (MPFS) Final Rule , most focused on the additional 3.75% decrease in the Medicare conversion factor and the impact that determination would have on revenues. This focus is understandable considering the noteworthy 2021 increases in wRVU credit for many E/M and CPT codes and the subsequent monumental increases in production-based physician and advanced practice provider (APP) compensation for many specialties because of it – without a commensurate increase in professional services revenue.
The Split/Shared Visit rule changes included in the 2022 MPFS Final Rule could generate a similarly devastating disruption of wRVU credit, physician and APP compensation, and organizational revenue for hospital-generated professional services in many specialties.
WHAT PROMPTED THE 2022 MPFS FINAL RULE SPLIT/SHARED VISIT CHANGES?
CMS previously defined the parameters for Split/Shared Visits in the Medicare Claims Policy Manual (Sections 30.6.1(B), 30.6.12, and 30.6.13(H)). When the Manual provisions were withdrawn on May 9, 2021 in response to petition, CMS indicated that it would update and clarify requirements through rulemaking. The 2022 MPFS presented that opportunity and the parameter changes are now codified in CMS Regulation § 415.140.
WHAT ARE THE 2022 MPFS FINAL RULE SPLIT/SHARED VISIT CHANGES?
1) definition of the split/shared visit.
The 2022 MPFS Final Rule defines a split (or shared) visit as “an E/M visit in a facility setting that is performed in part by a Physician and an NPP who are in the same group.” [NPP = nonphysician practitioner]
“Facility setting” is equated to an “institutional setting” in the Final Rule. According to the referenced regulation (§ 410.26(b)(1)), institutions are limited to hospitals and skilled nursing facilities (SNFs). The 2022 MPFS Final Rule added SNFs as a permitted location for Split/Shared Visits – with the impression that there would be close coordination and collaboration of care within groups providing care under these circumstances.
The 2022 MPFS Final Rule also clarified that the Split/Shared Visit scenario does not apply to the office setting. “Incident to” billing requirements would apply to office locations of care.
2) BILLING PROVIDER
The 2022 MPFS Final Rule requires that the Split/Shared Visit encounter be billed under the provider who performed “the substantive portion” of the encounter. In the Final Rule, CMS intended to define the “substantive portion” of the encounter as being more than half of the total time dedicated to the patient encounter. The total time determination is defined similarly to the 2021 office-based coding requirements and is delineated in Table 1. Split/Shared Visit encounters can currently be billed under the involved physician as long as the physician’s “substantive” participation in the encounter was accurately documented in the medical record.
In response to public comment, CMS modified the effective date for implementing the intended “total time” definition as the sole determinant for “substantive portion” purposes and granted a transition year to allow a smoother conversion. “Total time” dedicated to the encounter will be the sole determinant effective January 1, 2023. For the CY2022 transition year, CMS will accept performance of history, exam, medical decision-making, or time spent as criteria – with the caveat that the billing provider must have performed the entirety of one of these first three elements to the degree that the visit billing level requires. Since critical care codes are based solely on time spent, dedicating more than half of the total time spent is the lone criterion effective January 1, 2022. The applicable determinants are summarized in Table 2.
In addition, the individual ascertained to be the “Billing Provider” is required to be the one that signs and dates the encounter document. The encounter document must clearly indicate the physician and APP involved in the patient’s care and their roles in that care – this includes the individual time and/or effort dedicated to the encounter in sufficient detail to justify the “Billing Provider” determination.
3) CLAIM SUBMISSION
In CY2022, Split/Shared Visit encounter claims must be annotated by a specific modifier – regardless of the provider type that the encounter is billed under. This permits identification and tracking of these encounters – something that was not able to be done in the past without performing manual record review. CMS felt that adding this identification factor would be important for ensuring program integrity (interpreted to imply that these claims can now actually be tracked and audited). After the Final Rule was published, MGMA reported that the designated modifier will be “FS.”
4) APPLICABLE ENCOUNTERS
The Split/Shared Visit criteria apply to new or established patients, initial and subsequent visits, critical care services, and prolonged services. Split/Shared Visit criteria could previously only be applied to “established” patient encounters.
WHAT IMPACTS WILL THE 2022 MPFS FINAL RULE SPLIT/SHARED VISIT CHANGES HAVE?
In many hospital and SNF environments, APPs traditionally perform most of the time intensive aspects of Split/Shared Visit encounters. After all, this is one of the “values” of APP utilization in hospital settings – maximizing effective patient care delivery while efficiently minimizing dedicated physician time. Employed provider networks verify this is the case for many specialties, including hospital medicine. As a result, the above outlined changes create several important consequences.
1) WORKLOAD ATTRIBUTION/PRODUCTION-BASED PROVIDER COMPENSATION
Many employed provider networks directly attribute wRVUs generated by Split/Shared Visits to the “Billing Provider.” Under current circumstances, the “Billing Provider” is generally the physician as that designation allows “full” reimbursement for the professional services rendered to the patient by the care delivery team. Awarding all wRVU credit for Split/Shared Visits to the physician risks the perception that the physician is compensated for services that were not “personally performed” – a situation that is not fully aligned with Stark laws and regulations. One justification for the practice has been directly linking correlations with “incident to” scenarios. The distinction of Split/Shared Visits from office-based “incident to” circumstances in the 2022 MPFS places this justification in jeopardy.
Further, if the APP becomes the designated “Billing Provider” by performing the “substantive portion” of the encounter based on total time spent, the APP would, by the above default, be awarded all of the wRVU credit for these encounters. Awarding the physician these wRVUs would be very difficult to justify, as the physician did not perform a “substantive portion” of the encounter by definition. The immediate impact of this change is that the involved physicians’ wRVU credit would plummet – with serious consequences in production-based compensation models.
Consider the following options to address this new circumstance:
- If maintaining a production-based incentive remains an organizational imperative, create a teambased productivity incentive that pools earned wRVUs and distributes them equally among the involved physicians and APPs according to service or participation FTE. This option recognizes and promotes team member contributions to the overall group dynamics and successes while eliminating individual attribution issues and personally performed services concerns.
- If maintaining a production-based incentive remains an organizational imperative, create a mechanism to distribute wRVUs associated with Split/Shared Visits among the contributing individuals. This requires the ability to identify the individuals involved in each patient’s care and determining a fair distribution methodology. A 50/50 distribution methodology fully promotes a team-centered approach – although some organizations prefer to distribute according to the level of effort expended. This latter approach is more complex but more readily achievable with the new documentation requirements, i.e., how much of total time each participant dedicated to the encounter.
- If maintaining a production-based incentive is not an organizational imperative, consider eliminating the productivity component for shift-based providers, such as hospitalists, and incentivize nonproductivity elements like hospital clinical quality metric performance, committee participation, discharge summary completion, and others. Additional base income can be generated by covering more shifts and the individuals and the entire team can be incentivized to accomplish objectives that are actually within their sphere of influence.
2) MEDICARE REVENUE
As previously noted, most organizations designate the physician as the “Billing Provider” under current circumstances. This allows revenue generation at the lesser of 80% of the actual charge or at the fee schedule Amount for the services – essentially at 100% of anticipated revenue for the professional services rendered. hen an APP is the “Billing Provider,” revenue generation is at the lesser of 80% of the actual charge or at 85% of the fee schedule amount for the services – with the latter method predominating. The anticipated shift in “Billing Provider” designation noted above could result in the organization receiving 15% less revenue for the same volume and types of rendered professional services – and result in a significant loss of revenue for some specialties. This eventuality should be planned for, analyzed, and proactively addressed.
3) AUDITING ENCOUNTERS
Under current circumstances, payers do not require definitive identification of Split/Shared Visit encounters. This situation will change for submitted Medicare claims starting January 1, 2022. In the past, some organizations internally identified Split/Shared Visits in order to audit compliance and/or adjust workload attribution parameters. Some utilized a mechanism in which the physician was designated as the “Billing Provider” and the APP was designated as the “Rendering (or Service) Provider.” This system simultaneously identified the visit type and the involved physician and APP. These organizations often used this structure to not only audit encounters and ensure compliance with visit documentation requirements but also to individually attribute wRVU workload credit (often awarding a 50/50 split to promote true teambased function and performance). Others attached an internally derived modifier that was not reported externally to payers in order to identify these visits for internal audit purposes.
As alluded to above, CMS’ new requirement for adding a defined modifier to claims submitted for these visits allows them to be targeted for CMS audits. Developing or revising an internal audit process to ensure compliance with participation and documentation requirements would seem to be advisable.
Organizations need to be aware of the presence and potential impact of the new CMS Split/Shared Visit Requirements and proactively intervene to mitigate adverse consequences. With every challenge comes opportunity – and this challenge is no exception. Please feel free to contact HSG for analyses or assistance With any of these new issues – particularly the impact on physician and APP compensation models.
Related Physician Compensation Thought Leadership
The authors.

Terrence R. McWilliams, MD, FAAFP
Split/Shared Billing: 2024 Medicare Physician Fee Schedule Final Rule
On November 2, 2023, the Centers for Medicare & Medicaid Services (CMS) issued the calendar year 2024 Medicare Physician Fee Schedule Final Rule. Within it, CMS announced it will be adopting the American Medical Association (AMA) definition of “substantive portion” for split/shared evaluation and management (E&M) inpatient visits so that the split/shared policy aligns with CPT guidelines.
The 2024 CPT E&M guidelines indicate the following:
- A split/shared encounter is one in which a physician and other qualified healthcare professional (QHP) act as a team in providing care for the patient, working together during a single E&M service.
- The split/shared visit guidelines are applied to determine which professional may report the service. If the physician or other QHP performs a substantive portion of the encounter, the physician or other QHP may report the service.
Accordingly, per the final rule, the definition of substantive portion will be more than half of the total time spent by the physician and nonphysician practitioner (NPP) performing the split/shared visit, or a substantive part of the medical decision-making (MDM) as defined by CPT.
- The most notable change is that CMS no longer allows the documentation of history or exam in its entirety as a measure of determining which provider performed the substantive portion, since these are not included in the E&M split/share CPT code definitions.
- One key exception to the final rule definition change concerns critical care visits. Critical care visits do not use MDM, only time. As such, for critical care visits, the substantive portion will continue to mean more than half of the total time spent by the physician and NPP performing the split/shared visit.
CMS has finalized the policy for 2024 to alleviate administrative challenges that would otherwise burden practices investing time and resources in preparing for potential policy changes that are repeatedly postponed. However, CMS has emphasized that billing under the physician for split/shared visits must include documentation for how the physician participated in the care management plan, including whether they made or approved the plan for the number and complexity of problems and take responsibility for the plan and its inherent risk of complications.
It is worth noting that CMS received a variety of feedback on finalization of the policy. Some commentors requested that CMS withdraw the substantive portion policy altogether while others asked that it continue the current policy to allow use of the three key components (history, time, MDM) or time to determine who bills for the visit. Industry reaction notwithstanding, the substantive portion policy is here to stay in 2024.
ECG can provide strategies to help your organization be proactive in addressing the regulatory changes of the final rule.
Visit our Center for Split/Shared Success for continuing updates and advice.
Center for Split/Shared Success
Edited by: Matt Maslin
Published December 27, 2023
Related Services
- Provider Compensation Planning
- Provider Valuation
- Revenue Cycle
- Service Line Solutions
You Might Also Like
APP Compensation Planning Trends: Responding to Current Market Dynamics
Academic Compensation Planning Trends: Responding to Current Market Dynamics
Trends from ECG’s 2022 Pediatric Subspecialty Physician and APP Compensation Survey and Planning for 2023
Major Changes to Split/Shared Billing Affect Advanced Practice Providers and Physicians
6 key effects of the split/shared billing changes..
The 2022 Medicare Physician Fee Schedule Final Rule included major changes to the treatment of split/shared billing for advanced practice providers (APPs) and physicians. After a one-year delay, these changes are to go into effect in 2024. A split/shared visit is defined as “an E/M visit in a facility setting that is performed in part by a Physician and an NPP who are in the same group.” It is billed based on which provider performed the “substantive portion” of the service. For non-critical care split/shared visits in 2023, a substantive portion is considered “all or some portion of the history, exam or medical decision-making key components of an E/M service.” However, beginning January 1, 2024, a substantive portion is more specifically defined as greater than 50% of the time spent on the encounter.
The core consideration is that much of the work credited to the physicians in the past will not meet the “more than half of the total time” criteria. Therefore, the credit will go to APPs, and reimbursement will be at the APP rate of 85%. The purpose of the change appears to be to align reimbursement and productivity better with the provider that primarily provided the service.
Read about how the 2022 Medicare Physician Fee Schedule Final Rule affects split/shared visits
5 Facts to Remember with Split/Shared Visits
- Applicable only in hospitals and skilled nursing facilities (SNFs), not in an office setting
- Must be billed with a specific modifier
- Previously only applied to established patient encounters
- Now applicable to new or established patients, initial and subsequent visits, critical care services, and prolonged services
- A modifier identifies the physician and APP that delivered care for the split/shared services
The split/shared billing change most heavily affects practices where APPs perform a large portion of the work from a time perspective (e.g., hospitalists, critical care, cardiology). In many cases, we expect up to 90% of production to shift to the APPs, with the remaining cases primarily being higher complexity cases.
The November 2021 regulations declined to define same group , creating ambiguity over the applicability of split/shared billing in the context of a physician and APP that do not practice under the same Tax-ID number. Instead, CMS will monitor the split/shared bills submission and determine if it will later define the term group . If a physician and APP are part of different groups, they would be unable to split/share billing for services rendered by both where the physician or APP did not independently complete a billable service; the physician or APP would bill only for the service that they performed.
This regulatory change will have a number of effects on both practice operations and economics. Impacted practices should proactively consider and address the effects of regulatory changes on compensation methodologies to ensure efficiency.
We summarize the operational and economic effects in the following sections.
Key Effect #1: Changes in billing and coding practices
Practices must develop a methodology for quickly and easily determining whether a service should be billed under the physician or an APP.

Key Effect #2: Revenue decreases
Due to the fact that billing under an APP reduces reimbursement, revenue decreases can be expected for any service line that relies heavily on the use of APPs starting in 2024.
Key Effect #3: Work RVU attribution
Work RVU (wRVU) attribution for compensation purposes, which will be both wRVU productivity of individual physicians and APPs as well as comparability to both historical data and survey benchmarks.
Key Effect #4: Incentivizes physicians, not APPs
A potential incentive for a physician to perform work that is more appropriate for an APP, reducing efficiency and the growth of APP utilization.
Key Effect #5: Compensation changes
By changing the level of services personally performed by physicians versus APPs, physician compensation may decrease, and APP compensation may increase.
Key Effect #6: Physician and APP compensation structure changes
The following changes to physician and APP compensation structures could occur:
- Alignment with the new wRVU attribution structure
- Shift to salary or time/shift-based compensation
- Shift to team-based compensation models
- APP supervision may become a more significant portion of total physician compensation
- APP productivity-based compensation may grow in popularity
We recommend proactive action to ensure a smooth transition to the new split/shared visit regulations. It is important to review contracts (of both physicians and APPs) to determine which may result in increased or decreased compensation due to changes in wRVU attribution. A sample of past claims should be reviewed to get a sense of the potential impact of the change in split/shared visit rules. Prospectively, it will be key to establish a process to track the actual time spent by each provider during an encounter that could be subject to split/shared visit billing rules. This will ensure compliance with new billing rules in 2024 and can be used to analyze the potential impacts on revenue and physician and APP wRVU productivity before the new billing rules are in effect.
Request a Call to Evaluate Options
Co-authored with Gunnar Bedford , an associate in Hancock Daniel’s Richmond office. Last updated May 2, 2023.

Related Insights
Get your macra house in order: how to plan for & mine your own specialty data, ehr documentation integrity risks: ten ways to stay compliant, will providers be reimbursed for telehealth services, cms issues 2023 physician fee schedule final rule.
The conversion factor will decrease by 4.5%.
Front-End Patient Collections: Where the Rubber Meets the Road
Employee incentive programs in an era of change, professional services agreements as an alternative to employment: a contemporary option for alignment and integration, managing financial risk through a value-based clinical care delivery system, beyond borders: telemedicine’s vital role in healthcare transformation.
Telemedicine bridges the gap in access to healthcare for rural communities.
Healthcare Cybersecurity – Where are You Vulnerable?
Is there a looming physician shortage and what does it mean, collections guarantee or stipend that is the question.
What's the best way to staff your ER?
It’s Always a Good Time to Clean Up Your Vendor Contracts
Contracts can renew automatically without permission or approval.
2019: New Year, New Physician Fee Schedule, and New Opportunities for Your Practice
Macra and mips in physician practice valuations, revenue cycle: the devil is in the details, case study: leveraging technology during a pandemic, do hospitals that employ their physicians need a community need assessment, reassessing value in hospital-based subsidy arrangements.
Evaluate and document the value of your service provider.
The Next Stage of Evolution in Physician Practice Transactions: Can hospitals compete with private equity in attracting physician group deals?
Preparing for telemedicine: 5 ways to minimize claims denials, mitigating risk when migrating from one emr to another, increase operational efficiency through scheduling options, procare portal, coker interviews ahla president rob niccolini, coker group has added brandt jewell as a senior vice president to lead their physician services group, cms announces new options for macra participation, 5 fatal it vendor contract mistakes.
Prevent devastating consequences that can adversely impact the company.
Key Issues and Guidance for Hospitals and Medical Groups during the COVID 19 Pandemic
Coker elevates talent with 2024 team member promotions.
Promotions are effective April 1, 2024.
Achieve Quality Improvement through IT Integration
Understanding value-based compensation models.
How should physician compensation models evolve with the shift toward value?
Is Your Healthcare IT Up To Par? Why IT Assessments are Beneficial
Vendor selection and negotiating ehr vendor contracts, provider compensation in rural markets: top 5 lessons learned, direct to employer contracting arrangements: a response to rising premiums and compromised care, conflict management and successful leadership, compensation best practices for physician enterprises, leadership development and succession planning, understanding call pay compensation methods.
Structure call coverage arrangements to comply with regulations.
The Keyword for Hospitals: Track Documentation of Physician Community Need Before Recruiting Physicians
Five steps to building a "macra ready" physician compensation, covid-19 telehealth privacy and security concerns, hospital-physician disengagement – say that again, the effect of the election on the healthcare industry, let’s talk about why qualitative information matters in your physician needs assessment.
The medical community's input and health system leadership can be vital to a comprehensive physician needs assessment.
MACRA Implementation Webinar Series
Strategic planning video series: set mile markers along the road.
90% of organizations fail to execute their strategies successfully.
Benchmarking to Perfection
The importance of a cmo: it's a big job, artificial intelligence (ai) in healthcare: how is it changing healthcare and what are the ramifications, overcoming obstacles with performance improvement for critical access hospitals.
Actionable solutions for rural health leaders.
The Year in Review
Covid-19 pandemic exposes vulnerabilities in healthcare organizations (part 3), covid-19 pandemic exposes vulnerabilities in healthcare organizations (part 1), lawmakers grapple with artificial intelligence regulation as popularity and utilization grow.
ChatGPT could improve providers' productivity
Coker Group has added Alex Kirkland as a Vice President to Expand Financial Advisory and Physician Enterprise Services
Five tips to keep your data safe, ehr ease of use - does it exist and how do we define it, physicians in practice: ways to align and remain independent.
Corporate entities now employ 3 out of 4 physicians.
Where's the Value in Physician Practice Valuations?
Covid-19 pandemic exposes vulnerabilities in healthcare organizations (part 2), address community need with physician income guarantee arrangements.
Physician income guarantees are not just good for the physician.
Next Generation MSOs: Strategies to Grow beyond Traditional Practice Management Services
Does the corporation’s compliance program work in practice, too little not too late, enhance your executive compensation model to improve retention and recruitment, revenue and quality integrity: a comprehensive approach to coding, compliance, and clinical documentation, physician compensation governance: building a good foundation, is your risk analysis thorough and accurate.
A gap analysis does not provide a comprehensive view of security processes.
Developing Management Services Organizations for Private Practices: The Newest Version of Strength in Numbers?
Post-merger integration: the key to value creation in healthcare transactions, the icd-10 freeze is over: 2017 icd-10-cm/pcs coding updates and the impact on clinical documentation improvement, use a checklist to track documentation of community need, patient access, 2018 updates to macra, avoiding four common pitfalls in revenue cycle management, onc temporarily relaxes compliance deadlines related to the cures act, how the cy 2022 pfs final rule affects split/shared visits and critical care services.
On May 3, 2021, CMS withdrew provisions for split/shared E/M visits and critical care services from the Medicare Claims Processing Manual IOM
Understanding and Preventing Physician Burnout
Interim management solutions: take time to pursue the right hire, fair market value: assessing compensation arrangements in the healthcare industry, interim management: allow your organization time to find expert leadership, achieving and maintaining a high performing revenue cycle, revenue cycle management – look out for the red flags, “cio-on-demand” – an innovative approach to meet interim cio needs, up, up, and away inflation, shortages, and the impact on business valuation analyses.
A thorough review of each revenue and expense line item is required.
Just When You Think You’ve Heard It All: CMS’s Proposal for an E/M Makeover
Smoothing the rough spots in patient flow in outpatient practices, trinity hunt partners establishes healthcare advisory platform with investment in coker.
Trinity Hunt will work closely with Coker’s skilled team to facilitate expansion.
Navigating the New Normal of a Post-Pandemic World
Navigating the documentation of community need, cybersecurity tips, it assessments: an essential initiative, challenges of clinical documentation, "mu" will soon be "mips": why and what do you need to know, cyber criminals are targeting telemedicine visits, the intersection of compliance and fair market value: are you sure your arrangements coincide, don’t write-off timely filing denials.
Practice administrator recovered over $60,000 in unpaid claims that would have otherwise been written off.
The Importance of the Provider Onboarding and Recruiting Process

CMS Makes Major Change to Split/Shared Rule for 2024
- November 2, 2023

Recent Posts
Oig issues recommendations for short stay admissions, oig semiannual report to congress, 2023 medicare improper payments data, new requirements for hospital price transparency in 2024, ready to discuss your project with us, hbe advisors llc.
- 3597 E Monarch Sky Lane Suite F240 Meridian, ID 83646
- (208) 319-0074
- [email protected]
- Executive Team
Web Design Boise by Thrive
Compliance with Medicare’s updated 2024 split (or shared) visit policy
[author: Elin Baklid-Kunz*]
Compliance Today (May 2024)
Split (or shared) visits—the current term used by the Center for Medicare & Medicaid Services (CMS)—allow non-physician practitioners (NPPs) and physicians who work for the same employer/entity to share patient visits on the same day by billing the combined work under the physician’s National Provider Identifier (NPI) and receive 100% of the Medicare Physician Fee Schedule (MPFS), or the NPP’s NPI for reimbursement of 85% of the MPFS.
In the 2024 MPFS Final Rule, CMS revised the definition of “substantive portion” of a split (or shared ) visit to reflect the revisions made by the American Medical Association’s (AMA) Current Procedural Terminology (CPT) Editorial Panel. [1] CMS removed history and exam from the definition of substantive portion and adopted the determination of medical decision making (MDM) as defined by CPT as the provider who “made or approved the management plan.”
There are two ways for providers to meet the guidelines, and the billing provider is determined by the provider who performs:
more than half of the total time, or
a substantive part of the MDM as defined by CPT (except for critical care visits, which use time only and are not MDM).
The revised policy is somewhat unexpected, as CMS has several times delayed a proposed policy that “whichever of the providers who spends the most time” would bill the service.
While there are many articles for providers on how to be compliant going forward, for auditors and providers facing retrospective audits, things are a little bit more confusing—specifically for auditors working in the legal space who frequently perform audits based on the different guidelines in effect for the different dates of service. For example, an auditor may be asked to review evaluation and management (E/M) services where the scope also includes compliance with split (or shared) services from 2021 to 2024. This would be a challenge with the different guidelines for split (or)shared services with different rules based on 2021 and prior, 2022 to 2023 new policy and transition, and 2024 revisions. To complicate this further, AMA had major revisions to the CPT Documentation Guidelines for outpatient office visits (CPT 99202–99215) in 2021 and for the remainder of E/M services in 2023 that impacts how E/M services are documented and reviewed.
Background Medicare’s split (or shared) visits—2021 and prior
Prior to 2002, the role of NPPs and the appropriate billing practices related to the services they provided in the facility setting were not clearly defined. Typically, NPPs such as nurse practitioners and physician assistants—also referred to as qualified healthcare practitioners (QHP) by the AMA—would assist physicians in the hospital with rounding or seeing patients in the emergency room, and these services were billed under the physicians’ NPIs. While certain documentation requirements applied, they were not clearly defined and varied by payer.
In October 2002, CMS Transmittal 1776 introduced Medicare’s payment policy for split (or shared) E/M visits. [2] However, the full definition was introduced in Transmittal 808 in January 2006; it updated CMS Internet Only Manual: Medicare Claims Processing Manual (MCPM) Publication 100-04, Chapter 12, Section 30.6.1.H Split/Shared E/M Visit. (This section has since been removed): [3]
A split/shared E/M visit cannot be reported in the SNF [skilled nursing facility]/NF [nursing facility] setting. A split/shared E/M visit is defined by Medicare Part B payment policy as a medically necessary encounter with a patient where the physician and a qualified NPP each personally perform a substantive portion of an E/M visit face-to-face with the same patient on the same date of service. A substantive portion of an E/M visit involves all or some portion of the history, exam or medical decision making key components of an E/M service. The physician and the qualified NPP must be in the same group practice or be employed by the same employer. The split/shared E/M visit applies only to selected E/M visits and settings (i.e., hospital inpatient, hospital outpatient, hospital observation, emergency department, hospital discharge, office and non facility clinic visits, and prolonged visits associated with these E/M visit codes). The split/shared E/M policy does not apply to consultation services, critical care services or procedures.
This allowed physicians to be reimbursed at 100% of the MPFS, although the NPP may have done most of the work if the physician performed and documented a face-to-face portion on the same calendar day.
These regulations remained in effect until CMS removed the MCPM sections related to split (or shared) E/M visits on May 26, 2021, [4] preparing for the revised payment rules, which were published in the 2022 MPFS Final Rule in November 2021. [5] It should also be noted that with the removal of the guidelines and until CMS published the final rule, CMS stated that “the agency will limit review.”
Revised policy and CMS transition period 2022–2023
Both 2022 and 2023 are considered transition years before CMS revised the policy for 2024; however, the major changes were effective in 2022.
With the revised policy—effective on January 1, 2022—split (or shared) E/M visits can only be performed in the facility setting (i.e., hospital inpatient/outpatient and emergency room); they can no longer be performed in an office setting, such as place of service 11. Prior to 2022, split (or shared) services were allowed in the office setting if incident-to were also met. [6] CMS added SNF E/M visits to services that can be split (or shared) except for SNF E/M visits that are required to be performed in their entirety by a physician; however, NF visits remained not billable as split (or shared) services.
Also new for 2022 was the addition of critical care services to E/M services that may be performed as split (or shared) and a new modifier -FS, which is required on Medicare claims to indicate the services were split (or shared) E/M visits.
For 2022, there were two ways for providers to meet the guidelines for billing split (or shared)—determined by the provider who performed the “substantive portion” of the visit—which was further defined as the provider who:
Performed more than half of the total time of the visit, or
Fully performed one of the three key components, history exam, or MDM.
The exception was critical care services, which must meet the “greater than 50%” definition of substantive portion. Perhaps the biggest change for 2022 was that time can now include non-face-to-face time.
The 2022 MPFS Final Rule also contained a separate definition for the “substantive portion” for 2023: whichever providers spend the most time would bill the service. However, the implementation of billing only based on time spent was delayed until at least December 31, 2024.
This new payment policy and the substantive portion are codified in 42 C.F.R. § 415.140 : [7]
Split (or shared) visit means an evaluation and management (E/M) visit in the facility setting that is performed in part by both a physician and a nonphysician practitioner who are in the same group, in accordance with applicable law and regulations such that the service could be billed by either the physician or nonphysician practitioner if furnished independently by only one of them. Substantive portion means more than half of the total time spent by the physician and nonphysician practitioner performing the split (or shared) visit, or a substantive part of the medical decision making except as otherwise provided in this paragraph. For critical care visits, substantive portion means more than half of the total time spent by the physician and nonphysician practitioner performing the split (or shared) visit.
Prior to 2022, AMA updated their office/outpatient E/M visits guidelines for 2021, allowing providers to select the level of office visits based on the amount of time spent with the patient or the level of MDM. [8] For coding purposes, history and physical exam documentation were eliminated, and total time was updated to include non-face-to-face time personally spent by the provider or NPP, but not other clinical staff. Non-face-to-face time includes activities such as preparing to see the patient, ordering procedures, etc.
It should also be noted that the AMA introduced a split (or shared) visit definition in the CPT manual for the first time in 2021. Although CMS did not adopt the CPT definition, the CPT time guidelines can be used. CPT defines the specific activities, which can be found in the E/M guidelines section of the CPT book.
Documentation
Documentation for split (or shared) visits should follow the guidelines for any E/M service and must support the combined service level reported on the claim. Both providers should personally document their portion of the visit separately in the medical record, as documentation should clearly indicate the services provided by each individual. If time is used for the level, the documentation should include time spent by each provider.
Prior to the 2022 changes, the documentation requirements for split (or shared) visits were focused on ensuring the physician performed and documented a face-to-face encounter with the patient on the same day as the NPP.
The policy then requires the provider who bills the service to perform a “substantive” component, starting with 2022. The new definition of substantive means the provider must document one of the components in its entirety, such as history, exam or MDM, or bill based on time.
Then, for 2024, since history or exam are no longer relevant for coding purposes, the billing provider must document the MDM in its entirety or bill based on time.
Medicare’s conditions of payment require that the documentation in the medical record identify the physician and NPP who performed the visit, and that the billing provider who is performing the substantive portion must sign and date the medical record. [9] For billing purposes, starting with 2022, the designated modifier -FS must be included on the claim to identify that the services are split (or shared).
As for any medical record documentation, it is important to avoid copy-and-paste errors, by ensuring that documentation is unique to each patient encounter and avoiding copying and pasting information from previous encounters. Each encounter should reflect the specific details of that visit. Providers should exercise caution with canned statements.
For example, it is not uncommon to see attestation statements when reviewing split (or shared) services, and often these statements are not sufficient. For example: “I, the attending emergency medicine physician, provided a substantive portion of the care of this patient. I personally performed the medical decision making in its entirety, in addition to components of the history and physical exam, for this encounter.”
This statement alone would not likely pass a payer audit if the medical record also does not contain documentation of what the physician actually performed.
Billing based on time
Before 2023, in the facility setting (2021 for office visits), providers could use time as the determining factor for E/M services by documenting total time, the content of the counseling or coordination of care, and documentation that more than half of the time was spent on counseling or coordination of care. (i.e., “20 minutes of the 30-minute visit spent counseling the patient on . . .”). This is often referred to as using “time based counseling or coordination of care” and was eliminated in 2023 when CPT expanded the 2021 documentation guidelines where visits are based on total time or MDM, to apply to all EM visit codes (except critical care services). [10]
The biggest change with time, however, is allowing “non-face-to-face” time spent on the same date to be used for split (or shared) visits as long as one of the practitioners has face-to-face (in-person) contact with the patient. It does not necessarily have to be the physician or the NPP who performs the substantive portion and bills for the visit. The substantive portion can be entirely with or without direct patient contact and is determined by the proportion of total time—not whether the time involves patient contact.
Examples of non-face-to-face time include time preparing to see the patient, reviewing test results, or discussing the patient’s care with other providers. For example, activities that cannot be counted include traveling and teaching.
It is essential that each provider documents their distinct time in the medical record. And when two or more providers jointly meet with or discuss the patient, only the time of one individual should be counted. For example:
If the NPP sees a hospital patient in the morning and spends 10 minutes, and the physician follows up later the same calendar day with a 15-minute visit, the physician may report the service based on time. The total time for the visit would be 25 minutes, and the provider who spent more than 50% of the visit—the physician—can report the service.
If, in the same situation, the physician and NPP met together for five additional minutes (beyond the 25 minutes) to discuss the patient’s treatment plan, that overlapping time could only be counted once for purposes of establishing total time and who provided the substantive portion of the visit. The total time would be 30 minutes, and the physician would bill for the visit since they spent more than half of the total time (20 of 30 total minutes).
This captures the main intent behind the split (or shared) service, as it allows the NPP to see patients while the physician may be in surgery or otherwise unavailable. The physician would then see the patient later in the day, such as more complex patients who need the physician’s experience. The split (or shared) rules were not designed to encourage physicians to simply stop by to see the patient to capture the additional 15% in revenue or only sign off on the medical records after the NPP visit. However, it should be noted that CMS— in the 2024 Final Rule—specifically stated: “We note that the policy is not about whether the physician’s expertise is ‘necessary’ for the visit but rather whether the physician or the NPP should bill for the service when each of them are performing part of an E/M visit.” [11]
Compliance with split (or shared) E/M visits
Many of the recent overpayments, audits, Civil False Claims Act, and even criminal cases instituted by the federal and state agencies overseeing the Medicare and Medicaid programs involve allegations of improper billing for “incident-to” services and split (or shared) services.
One example is the recent False Claims Act case against TeamHealth, who settled for $48 million in 2021. The realtors alleged that TeamHealth engaged in a scheme to defraud Medicare by overbilling for services provided by NPPs by submitting claims for reimbursement for services performed by NPPs but using physicians’ NPIs, which inflated their reimbursement rate. The relators alleged that TeamHealth covered up this practice by characterizing NPP services as split (or shared) E/M services. [12]
To prepare for potential increased audit scrutiny, if your practice employs NPPs, any E/M audit should include services performed split (or shared) as well as services performed incident-to.
Practices should consider the following steps for compliance:
Understand current policy : Familiarize yourself with Medicare and CPT guidelines for split (or shared) E/M visits. See Figure 1.
Payer difference : Query payers to understand their policy for split (or shared) visits.
Perform baseline audit : Assess your compliance by performing a baseline audit.
Educate providers : If discrepancies or issues are identified, provide feedback to the involved providers and educate them on Medicare and other payers’ specific guidelines.
Implement corrective actions : If necessary, implement corrective actions to address any identified issues. This may include additional training for providers or improvements to documentation processes. It may include changes to workflows and roles affected by the revisions for 2024.
Monitor compliance : Establish an ongoing monitoring process to ensure ongoing compliance with Medicare guidelines for split (or shared) E/M visits. Regularly audit sample documentation to identify and address any issues promptly. A checklist can be used to help with this.
Stay informed : Keep abreast of any updates or changes to Medicare guidelines. Medicare policies can change, and staying informed will help ensure ongoing compliance. And make sure to monitor updates from your Medicare administrative contractors, as we can expect additional information based on the revised policy.
Last, remember that the new modifier -FS will make it easier for Medicare to monitor claims and ensure that providers are correctly billing for split (or shared) E/M services.
Understand the different timelines and guidelines for auditing split (or shared) visits: 2021 and prior, 2022–2023 new and transition and 2024 revisions.
Use an auditor reference tool to help with retrospective audits.
The Centers for Medicare & Medicaid Services only allow split (or shared) visits in the facility setting (i.e., hospital, emergency room) starting with calendar year 2022; however, Current Procedural Terminology is silent on location and may be allowed in the office setting.
Time for split/shared service may include both face-to-face and non-face-to-face activities.
Perform a baseline audit to ensure compliance with Medicare’s updated split (or shared) visit policy.
*Elin Baklid-Kunz is a Healthcare Consultant at KUNZ LLC in Orlando, Fl.
1 Centers for Medicare & Medicaid Services, CY 2024 Payment Policies Under the Physician Fee Schedule and Other Changes to Part B Payment and Coverage Policies; Medicare Shared Savings Program Requirements; Medicare Advantage; Medicare and Medicaid Provider and Supplier Enrollment Policies; and Basic Health Program, 88 Fed. Reg. 78,818 (Nov. 16, 2023), https://www.federalregister.gov/documents/2023/11/16/2023-24184/medicare-and-medicaid-programs-cy-2024-payment-policies-under-the-physician-fee-schedule-and-other .
2 Centers for Medicare & Medicaid Services, “New/Revised Material – Effective Date: July 1, 2001, Implementation Date: October 25, 2002,” Transmittal 1776, Change Request 2321, October 25, 2002, https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/Downloads/R1776B3.pdf .
3 Centers for Medicare & Medicaid Services, “Nursing Facility Service (Codes 99304 – 99318),” CMS Manual System, Pub 100–04 Claims Processing, Transmittal 808, Change Request 4246, January 6, 2006, https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R808CP.pdf .
4 Centers for Medicare & Medicaid Services, “Release: CMS Notice Regarding Split (or Shared) Evaluation and Management Visits and Critical Care Services from May 26, 2021, through December 31, 2021,” May 26, 2021, https://www.cms.gov/files/document/enf-instruction-split-shared-critical-care-052521-final.pdf .
5 Medicare Program; CY 2022 Payment Policies Under the Physician Fee Schedule and Other Changes to Part B Payment Policies; Medicare Shared Savings Program Requirements; Provider Enrollment Regulation Updates; and Provider and Supplier Prepayment and Post-Payment Medical Review Requirements, 86 Fed. Reg. 64,996 (Nov. 19, 2021), https://www.govinfo.gov/content/pkg/FR-2021-11-19/pdf/2021-23972.pdf .
6 Medicare Program; CY 2022 Payment Policies Under the Physician Fee Schedule and Other Changes to Part B Payment Policies.
7 § 415.140 Conditions for payment: Split (or shared) visits, up to date as of March 11, 2024, https://www.ecfr.gov/current/title-42/chapter-IV/subchapter-B/part-415/subpart-C/section-415.140 .
8 American Medical Association, “CPT® Evaluation and Management (E/M) Office or Other Outpatient (99202–99215) and Prolonged Services (99354, 99355, 99356, 99417) Code and Guideline Changes,” January 1, 2021, https://www.ama-assn.org/system/files/2019-06/cpt-office-prolonged-svs-code-changes.pdf .
9 42 C.F.R. § 415.140 Conditions for payment, Split (or shared) visits.
10 American Medical Association, “CPT® Evaluation and Management (E/M) Code and Guideline Changes,” January 1, 2023, https://www.ama-assn.org/system/files/2023-e-m-descriptors-guidelines.pdf .
11 Centers for Medicare & Medicaid Services, CY 2024 Payment Policies Under the Physician Fee Schedule and Other Changes to Part B Payment and Coverage Policies.
12 United States of America, ex rel. Caleb Hernandez & Jason Whaley, Relators v. Team Health Holdings INC., Team Finance, L.L.C., Team Health INC., & Ameriteam Services, L.L.C., Case 2:16-cv-00432-JRG, (E.D. Tex. Nov. 12, 2018).
13 Medicare & Medicaid Services, CY 2024 Payment Policies Under the Physician Fee Schedule and Other Changes to Part B Payment and Coverage Policies; Medicare Shared Savings Program Requirements; Medicare Advantage; Medicare and Medicaid Provider and Supplier Enrollment Policies; and Basic Health Program, 88 Fed. Reg. 78,818 (Nov. 16, 2023), https://www.federalregister.gov/documents/2023/11/16/2023-24184/medicare-and-medicaid-programs-cy-2024-payment-policies-under-the-physician-fee-schedule-and-other .
14 American Medical Association, CPT Professional 2024 (Chicago, IL: American Medical Association, 2023).
15 Medicare and Medicaid Services, CY 2023 Payment Policies Under the Physician Fee Schedule and Other Changes to Part B Payment and Coverage Policies; Medicare Shared Savings Program Requirements; Implementing Requirements for Manufacturers of Certain Single-dose Container or Single-use Package Drugs To Provide Refunds With Respect to Discarded Amounts; and COVID–19 Interim Final Rules, 87 Fed. Reg. 69,904 (Nov. 18, 2022), https://www.federalregister.gov/documents/2022/11/18/2022-23873/medicare-and-medicaid-programs-cy-2023-payment-policies-under-the-physician-fee-schedule-and-other .
16 American Medical Association, “CPT® Evaluation and Management (E/M) Code and Guideline Changes.”
17 Medicare Program; CY 2022 Payment Policies Under the Physician Fee Schedule and Other Changes to Part B Payment Policies.
18 Centers for Medicare & Medicaid Services, 1997 Documentation Guidelines for Evaluation and Management Services , accessed March 25, 2024, https://www.cms.gov/outreach-and-education/medicare-learning-network-mln/mlnedwebguide/downloads/97docguidelines.pdf ; Centers for Medicare & Medicaid Services, 1995 Documentation Guidelines for Evaluation and Management Services , accessed March 25, 2024, https://www.cms.gov/outreach-and-education/medicare-learning-network-mln/mlnedwebguide/downloads/95docguidelines.pdf .
19 American Medical Association, CPT Professional 2022 (Chicago, IL: American Medical Association, 2021).
20 Centers for Medicare & Medicaid Services, “Release: CMS Notice Regarding Split (or Shared) Evaluation and Management Visits and Critical Care Services from May 26, 2021, through December 31, 2021.”
21 American Medical Association, CPT Professional 2021 (Chicago, IL: American Medical Association, 2020).
22 American Medical Association, “CPT® Evaluation and Management (E/M) Office or Other Outpatient (99202–99215) and Prolonged Services (99354, 99355, 99356, 99417) Code and Guideline Changes.”
23 Centers for Medicare & Medicaid Services, “Nursing Facility Service (Codes 99304 – 99318).”
[ View source .]
Latest Posts
- [Event] Healthcare Research Compliance Academy - September 9th - 12th, Las Vegas, NV
- [Event] Healthcare Privacy Compliance Academy - September 9th - 12th, Las Vegas, NV
- [Event] Healthcare Basic Compliance Academy - September 9th - 12th, Las Vegas, NV
- [Event] Healthcare Basic Compliance Academy - August 19th - 22nd, Washington, DC
- [Webinar] Mending the Fence: How State Privacy Laws are Closing the Gap on Health Consumer Privacy - June 18th, 12:00 pm - 1:30 pm CT
See more »
Refine your interests »
Written by:

PUBLISH YOUR CONTENT ON JD SUPRA NOW
- Increased visibility
- Actionable analytics
- Ongoing guidance
Published In:
Health care compliance association (hcca) on:.

"My best business intelligence, in one easy email…"
Climate change funding talks stuck ahead of COP29 summit
- Medium Text

GETTING THE NUMBER RIGHT
Deciding who should pay.
Sign up here.
Reporting by Kate Abnett; Editing by Josie Kao
Our Standards: The Thomson Reuters Trust Principles. New Tab , opens new tab
Thomson Reuters
Kate Abnett covers EU climate and energy policy in Brussels, reporting on Europe’s green transition and how climate change is affecting people and ecosystems across the EU. Other areas of coverage include international climate diplomacy. Before joining Reuters, Kate covered emissions and energy markets for Argus Media in London. She is part of the teams whose reporting on Europe’s energy crisis won two Reuters journalist of the year awards in 2022.
Business Chevron

China issues rare earth regulations to further protect domestic supply
China has unveiled a list of rare earth regulations aimed at protecting supplies in the name of national security, laying out rules on the mining, smelting and trade in the critical materials used to make products from magnets in electric vehicles to consumer electronics.

Need a good bill splitting app? Here are our recommendations

Spending time with friends is always a treat, but it can get awkward when it comes to divvying up the expenses. However, there's no need to stress about the math and logistics of everyone paying their share, as technology can take care of it. Whether it's something as straightforward as a dinner bill or a bit more complex, like a vacation with multiple expenses involved, apps can help you keep track of costs, figure out who owes what and easily facilitate paying someone back.
Plus, many of these apps are great options to help split your regular expenses, like rent or utilities.
Watch this video to see how apps can help you split the bill with friends.
Easily split payments
You're probably already using a payment app like PayPal, Venmo , Zelle or CashApp. These apps are great for getting paid or paying someone back but often require you to do the math to determine exactly what's due and by whom.
However, in November 2023, Venmo introduced Venmo Groups to make splitting expenses among a group of people easier. According to the company, the feature reduces "the need for spreadsheets" by automatically calculating who owes what.
Splitwise is another useful app for splitting costs, not only between friends or roommates but when what's due isn't a 50/50 split. The app has options such as splitting a total by percentages or shares. Plus, you can connect your third-party payment app, such as PayPal or Venmo, to make the payment.
Whichever payment route you choose, it works best when everyone involved in the transaction has the app. So, find the one that works best for you and your situation.
Uncomfortable Conversations: Did you get stuck splitting the dining bill unfairly?
Always be careful when sending money on apps, and always, always, always double (or triple!) check that you're sending it to the correct person. Once a payment is sent, it usually can't be unsent.
Reviewed-approved iPhone accessories
Purchases you make through our links may earn us and our publishing partners a commission.
Reviewed helps you find the best stuff and get the most out of what you already own. Our team of tech experts test everything from Apple AirPods and screen protectors to iPhone tripods and car mounts so you can shop for the best of the best.
- A rugged iPhone case: Casekoo Crystal Clear Protective Case
- A top wireless charger: Yootech Wireless Charger
- Our favorite screen protector: Ailun Glass Screen Protector
- The best portable battery pack: Mophie Powerstation Plus
- Durable phone car holders: Beam Electronics Phone Holder
- An iPhone tripod we love: Aureday Phone Tripod
- The best USB-C cable: Anker 6 Foot USB-C Cable, Pack of 2
Columbus United FC visits Children’s Hospital at Piedmont
COLUMBUS, Ga. (WTVM) - Members of the Columbus United FC made a trip to the Children’s Hospital at Piedmont Columbus Regional on Thursday.
On Wednesday night, Columbus United FC beat Tallahassee SC, 3-1, securing a home playoff game on July 6. The team was back in Columbus to visit with patients less than a day later.
“At difficult times, it’s good to have a happy feeling around. It’s a blessing to be able to come here, see their smiles and pass out signatures,” said Columbus United FC centre-back Damean Dominguez.
A percentage of ticket sales to Saturday’s game with Pensacola FC will go to the Piedmont Bill and Olivia Amos Children’s Hospital. The new Piedmont Bill and Olivia Amos Children’s Hospital will open this fall and is the only freestanding children’s hospital in the region.
This Saturday’s match begins at 7 ET at Kinnett Stadium.
Copyright 2024 WTVM. All rights reserved.

UPDATE: 2 dead after incident at Lee County creek

Baby unaccounted for after mother dies in house fire; 2 detained

Alabama Power explains how 20-degree rule impacts air conditioning

Woman killed in Phenix City house fire

Georgia Power expands Income-Qualified Discount
Latest news.

Former ‘Bama standout named to 2024 USA Basketball Men’s Select Team

Dejounte Murray traded from Atlanta Hawks to Pelicans, reports say

Former Auburn standout named to 2024 USA Basketball Men’s Select Team

Columbus United FC visits Children's Hospital at Piedmont

IMAGES
VIDEO
COMMENTS
and can bill for the split or shared E/M visit. Definition of Split or Shared Visit. A split or shared visit is an E/M visit that both a physician or NPP in the same group perform in a facility setting, and in accordance with applicable law and regulations, either the physician or NPP can bill the service if they provide it independently.
Billing Split (or Shared) Visits in 2022-2023. What didn't change for split (or shared) E/M visits is that they are still leveled using the 1995 or 1997 Documentation Guidelines for Evaluation and Management Services through the end of 2022. What did change for split (or shared) E/M visits is the selection of the billing provider.
Reporting Split/Shared E/M Visits in 2024. Beginning January 1, 2024, the Centers for Medicare & Medicaid Services (CMS) will implement a new split (or shared) evaluation and management (E/M) billing policy for E/M visits provided in part by a physician and in part by a nonphysician practitioner (NPP). The billing provider for such visits will ...
Specifically, for CY 2024, for purposes of Medicare billing for split (or shared) services, the definition of "substantive portion" means more than half of the total time spent by the physician and NPP performing the split (or shared) visit, or a substantive part of the medical decision making as defined by CPT ®," per the 2024 final rule.
6. Applicable modifiers for split/shared visits. The new HCPCS Level II modifier FS Split (or shared) evaluation and management visit must be included on the claim to identify that the service was a split/shared visit for services furnished on or after Jan. 1, 2022. A breakdown of these requirements for billing a split/shared visit is provided ...
The total time would be 30 minutes, and the physician would bill for the visit since they spent more than half of the total time (20 of 30 total minutes). To bill as a split or shared subsequent hospital service, the billing practitioner reports CPT code 99232 if basing the coding on time.
What the new rules say. For years, physicians and NPs/PAs have been submitting bills for split (or shared) visits under physicians' names and ID numbers for 100% of the allowable physician fee—as long as doctors perform a "substantive portion" of the visit. (Otherwise, NPs/PAs bill under their own names and ID numbers at 85% of the ...
No, a split (or shared) visit cannot be billed for visits furnished in a NF setting. We revised our regulation at 42 CFR § 415.140 to define a split (or shared) visit as an E/M visit in a facility ... minutes have been spent), and may bill 99292 for each additional 30-minute time increment completed. April 7, 2022
Specifically, CMS' split/shared visit rule has required that a physician perform only some portion of the E/M visit in order to bill that service under the physician's NPI. Thus, the practice received full payment for the visit rather than the 85% of the Physician Fee Schedule rate paid for services billed under an NPP's NPI. In the Final ...
To bill split (or shared) subsequent hospital service, the billing practitioner reports CPT® code 99232 if basing the coding on time. If not using time, bill CPT ®codes 99231-99233 as meets the key component level on which the coding is based. Modifier -FS (split/ shared E/M visit) must be appended to the E/M CPT® code on the claim
Split/shared visits may be submitted with physician's PTAN as long as the following conditions are met: ... (Note: Medicare clarifies that incident-to billing is not allowed for new patient visits). If services do not meet the CMS incident to guidelines, submit the charges under the NPP name and National Provider Identifier (NPI) number.
Split/shared visits can be billed by either time (more than 50 percent of visit spent) or medical decision making (MDM) (substantiative portion). This distinction created confusion about how to document time versus a substantive portion. ... In addition, for split/shared billing, there are no restrictions about the type of patient seen (new or ...
The greatest impact on split/shared visit billing is set to occur in 2024 when all shared visits must be billed using the time-based methodology where the practitioner who provides the substantive portion of the visit ("more than ½ of the total time spent") bills for the visit1. In 2022 and 2023, the impact of the split/shared change will ...
Specifically, for CY 2024, for purposes of Medicare billing for split (or shared) services, the definition of "substantive portion" means more than half of the total time spent by the physician and NPP performing the split (or shared) visit, or a substantive part of the medical decision-making as defined by CPT. Page 476 CY 2024 Final Rule
In the proposed rule, CMS proposed to permit healthcare professionals to bill for split (or shared visits) that are critical care services. CMS also proposed to expand split (or shared) visit billing to permit E/M visits to be furnished by a physician and a NPP in a SNF setting. CMS finalized both these proposals in the final rule.
As part of the CY2022 Final Rule, CMS required a modifier be appended to all split visits for tracking purposes. After the Final Rule was published, modifier "FS" was designated to indicate split visits. Billing systems should be updated with the new FS modifier and processes developed to ensure the modifier is applied to all split visits.
Get answers to your coding and billing questions for these E/M visits. In the 2023 Medicare Physician Fee Schedule (MPFS) final rule, the Centers for Medicare & Medicaid Services finalized its split/shared visits policy.The Medicare policy was established under 2022 rulemaking, however, CMS postponed enforcing its definition of "substantive portion" until 2024.
The 2022 Split/Shared Visit rule changes may create disruption to wRVU credit, physician and APP compensation, ... that the billing provider must have performed the entirety of one of these first three elements to the degree that the visit billing level requires. Since critical care codes are based solely on time spent, dedicating more than ...
On November 2, 2023, the Centers for Medicare & Medicaid Services (CMS) issued the calendar year 2024 Medicare Physician Fee Schedule Final Rule. Within it, CMS announced it will be adopting the American Medical Association (AMA) definition of "substantive portion" for split/shared evaluation and management (E&M) inpatient visits so that ...
The 2022 Medicare Physician Fee Schedule Final Ruleincluded major changes to the treatment of split/shared billing for advanced practice providers (APPs) and physicians. After a one-year delay, these changes are to go into effect in 2024. A split/shared visit is defined as "an E/M visit in a facility setting that is performed in part by a ...
The 2024 Medicare Physician Fee Schedule Final Rule was released today. In a shocking turn of events, CMS announced in the Final Rule they will be adopting the 2024 AMA definition of substantive portion for split (or shared) visits. Specifically, CMS stated, "we are finalizing a policy that reflects a revised definition of "substantive portion" […]
Facility E/M visits, including split (shared) visits are still leveled using 1995 or 1997 guidelines as the new table of risk in CPT guidelines only apply to E/M office visits (CPT 99202-99215 ...
Split/Shared Visit Guidelines: Physician and APP must be part of same billing group practice. for a shared visit. for a shared visit. for a shared visit. Applies to E&M services only. Does NOT apply to procedures. Both the physician and APP must personally evaluate the patient on the same day.
These instructions are referred to as Medicare's Split/Shared Visit Policy. The policy is one of three billing options for NPPs: NPPs own provider number receiving 85 percent of the MPFS amount. Incident-to the physician receiving 100 percent of the MPFS. Split/shared service receiving 100 percent of MPFS.
A bipartisan data privacy bill is splitting House Republicans and pitting the chair of the powerful House Energy and Commerce Committee against House GOP leadership. House Energy and Commerce Commi…
BONN, June 13 (Reuters) - With just five months to go before this year's U.N. climate summit, countries cannot agree on the size of a global funding bill to help the developing world fight climate ...
Watch this video to see how apps can help you split the bill with friends. Easily split payments You're probably already using a payment app like PayPal, Venmo , Zelle or CashApp.
The new Piedmont Bill and Olivia Amos Children's Hospital will open this fall and is the only freestanding children's hospital in the region. This Saturday's match begins at 7 ET at Kinnett ...