- Kidney stone treatment typically would be covered by health insurance. For patients covered by health insurance, out-of-pocket costs typically would consist of a doctor visit specialist copay, prescription drug copays, possibly a hospital copay of $100 or more, and coinsurance of 10% to 50% for the procedure, which could reach the yearly out-of-pocket maximum. According to the Kaiser Family Foundation[ 1 ] , the average hospital copay for outpatient surgery is $132 and for inpatient surgery is $232 .The average coinsurance rate is 17% to 18%.
- For patients not covered by health insurance, kidney stone treatment typically costs less than $500 to allow the stone to pass naturally with monitoring from a doctor, and possibly prescription medication. For example, at Southern Illinois Urology, the cost of a doctor consultation is $150 . One medicine sometimes prescribed to patients with kidney stones, Urocit-K, costs about $65 for a one-month supply at Drugstore.com. Another, Zyloprim, costs about $80 . Generic versions of some of the drugs are available for less than $20 ; for example, Drugstore.com sells 100 tablets of Allopurinol (generic Zyloprim) for $13.99 .
- Kidney stone treatment can cost from just under $10,000 to $20,000 or more for surgical removal or extracorporeal shock wave lithotripsy (ESWL). For example, at Saint Elizabeth Regional Medical Center[ 2 ] , in Lincoln, NE, a cystourethroscopy -- a kind of examination of the urinary tract using a long, flexible tube -- with removal of a kidney stone typically costs about $7,400-$12,200, not including doctor fee. At Garden City Hospital[ 3 ] , in Michigan, the full price of a surgical kidney stone removal via cystoscopy is about $8,700 -- but the hospital offers it at a discounted price of about $2,500 for uninsured patients. Fragmenting a kidney stone using ESWL typically costs about $10,700-$16,700 or more. At Baptist Memorial Health Care, in Memphis, ESWL costs about $9,870 not including the doctor fee. According to NewChoiceHealth.com[ 4 ] , the national average cost for ESWL is $17,400 -- with range from $8,300 to $35,800 .
- Some smaller kidney stones can pass naturally. After first seeking the advice of a doctor, the patient would drink at least six glasses of water per day, and use over-the-counter pain relievers -- and possibly prescription medications -- while waiting for the stone to pass. WebMD has information[ 5 ] on medications for kidney stones.
- For ESWL, the most common method of treatment for stones that are actually in the kidney (rather than the ureters or bladder), the patient is placed under local or general anesthesia and lies in either a tub of warm water or on a special cushion on a table. X-rays or ultrasound are used to locate the kidney stone, then up to 2,000 shock waves are passed through the patient to crush the stone. Typically, a day or two of hospitalization is required, and there might be pain or bleeding as fragments are passed.
- In ureteroscopy, which is often used for stones in the ureters (the tubes connecting the bladder to the kidneys), the doctor passes a flexible scope with a basket on it through the urethra, and bladder, into the ureters. The doctor grabs the stone with the basket and removes it. This typically is an outpatient procedure.
- In percutaneous nephrolithotomy/percutaneous nephrolithotripsy, which might be used for stones of a size or shape that make them impossible to remove through other methods, the patient is placed under general anesthesia. The doctor makes a small incision in the back and inserts instruments to either remove or break up the stone. A few days of hospitalization and about a week off work are required.
- The National Kidney Foundation offers overviews of ESWL[ 6 ] , ureteroscopy[ 7 ] and percutaneous nephrolithotomy/nephrolithotripsy[ 8 ] .
- Depending on the type of kidney stone, a dietician might recommend a kidney stone prevention diet[ 9 ] . Many hospitals have dieticians available, and an initial consultation can cost $100-$200 .
- Some clinics, such as the NYC Free Clinic[ 10 ] and the Clinic at Brackenridge[ 11 ] in Austin, TX, offer access to specialist care. The U.S. Department of Health & Human Services offers a tool[ 12 ] to find a federally funded health clinic.
- The American Urological Association offers a urologist locator[ 13 ] by zip code. It is important to check to make sure the doctor is board-certified by the American Board of Urology[ 14 ] .
- It is important to discuss risks with the doctor. Risks vary, depending on the treatment but can include reaction to anesthesia, infection and bleeding.
- kff.org/health-costs/report/employer-health-benefits-2012-annual-survey/
- tp.chi.acelogicus.net/nese/Default.aspx
- www.gch.org/Home.aspx?id=219&sid=1
- www.newchoicehealth.com/Directory/Procedure/136/Lithotripsy%20(Kidney%20Stone%20Re...
- www.webmd.com/kidney-stones/kidney-stones-medications
- www.kidney.org/atoz/content/lithotripsy.cfm
- www.kidney.org/atoz/content/kidneystones_Ureteroscopy.cfm
- www.kidney.org/atoz/content/kidneystones_PNN.cfm
- kidney.niddk.nih.gov/kudiseases/pubs/kidneystonediet/
- nycfreeclinic.med.nyu.edu/information-for-patients/schedule-appointment
- www.seton.net/locations/brackenridge/services
- bphc.hrsa.gov/technicalassistance/taresources/slidingscale.html
- www.urologyhealth.org/urology/findurologist.cfm
- www.abu.org/

About Virtucare
- Hospital Partnerships
- Our Doctors
What Will the ER Do For My Kidney Stones?
If you’ve ever had a kidney stone, then you know how painful they can be. Although you may decide to head to the emergency room (ER) for kidney stone relief, your experience can be more painful than the kidney stone. Long wait times, overcrowded waiting rooms and chaos. This is not what you need right now.
Before you call an ambulance for kidney stones or yell at your spouse to drive you to the ER, you should have a reasonable expectation of “what will the ER do for my kidney stones?”
As board-certified urologists who’ve been on call for the ER, allow VirtuCare experts to guide you. You don’t have to go through this painful experience alone.
Why do kidney stones hurt?
Before we discuss going to the ER for kidney stones, it helps to understand why stones hurt so much in the first place.
Kidney stones cause pain when they cause a blockage of urine in the ureter (the tube connecting your kidney to your bladder). When a stone is stuck in the ureter, it blocks the flow of urine. This causes a backflow of pressure that distends or stretches out the plumbing system of the kidneys.

Internal organ pain due to lack of blood flow, blockage or severe trauma is known as visceral pain. This is the most severe type of pain because our body is notifying us that a vital organ is “in trouble and you better get help!”
When should you go to the ER for kidney stones?
If you are experiencing any of the following symptoms, GO IMMEDIATELY TO THE EMERGENCY ROOM:
- Intolerable kidney stone pain despite prescription pain medications
- Fever > 101 F
- Mental status changes (passing out, not able to hold a conversation)
These can be signs of a urinary tract infection along with a kidney stone blockage. A kidney infection at the time of a kidney stone requires emergent drainage of your kidney (usually with a stent) to prevent sepsis or even death.
Should you go to the ER or urgent care for kidney stones?
There are situations when a kidney stone can be managed without needing a trip to the ER.
Urgent care clinics are convenient care clinics which usually accept walk-in or same day appointments. However, they are more similar to your primary care provider’s office than an ER. Provider’s can prescribe medications and order tests like your regular doctor. But, expect to have to make a separate trip elsewhere for anything other than lab tests.
So how do you decide on an urgent care vs. an ER for your kidney stone pain? It depends on how bad of shape you’re in. Again if you’re having fevers, vomiting, or intolerable pain then the ER should be your first choice for kidney stones.
As long as you’re not having any of the above serious symptoms, then an urgent care provider may be able to help you. However, realize that you’ll likely be seeing a nurse practitioner or physician’s assistant with a primary care background. You typically won’t have immediate access to a specialist if a procedure or further advice is needed.
What tests will the ER do for kidney stones?
If a kidney stone is suspected based on your history, then the ER provider will often start with blood and urine samples. They will look for microscopic blood in the urine which is a sign of a kidney stone (although blood in the urine is absent in 10% of patients). A blood count will evaluate for signs of an infection. Kidney function tests (creatinine or GFR) will make sure your kidneys are working properly.
The best imaging test is a CT scan of the abdomen and pelvis without any contrast. This is 99% accurate for detecting kidney stones. If a kidney stone is present it will be important to know the following:
- Is the kidney stone causing an obstruction or blockage?
- What size is the stone?
- Where is the stone located?
Based on these factors the ER doctor can help make a determination if you need a urology consultation now or if the evaluation can wait.
What medications will help my kidney stone pain?
A variety of intravenous medications are used for kidney stone pain. The most commonly used is ketorolac (Toradol). This is a strong NSAID (similar to ibuprofen) that is more effective than most opioids. It should be used with caution if you have acid reflux, ulcers, or kidney dysfunction.
Opioids or narcotics (hydrocodone, oxycodone, morphine, hydromorphone) are often used in combination with NSAIDS. These medications are very effective for pain relief but are also associated with nausea, vomiting and constipation.
Additionally there is an opioid epidemic in our country due to heroin and prescription pain medications. The medical community is being asked to be very cautious with the amount and frequency with which we prescribe these medications.
A safe, prescription medication called tamsulosin (Flomax) has been shown to decrease kidney stone pain and increase the likelihood of stone passage. This is a prostate medication but has been used “off-label” for years in kidney stone patients (don’t worry ladies, you won’t grow a mustache on this pill. It’s not a hormone.)
Can you use telemedicine for kidney stones?
At VirtuCare we certainly appreciate the desire to avoid the ER for kidney stones. If you are interested in using telemedicine for kidney stones here’s how we can help:
- Direct access to a specialist
Why not skip the middle-man and go right to the expert?! As board-certified urologists, managing kidney stones is our specialty. You’ll have the best counseling and care from the comfort of your home.
- Prescribe medications
Non-narcotic pain medications can be called in to the local pharmacy of your choice. Due to federal and state laws, we are unable to prescribe narcotics or opioids. So if you need oxycodone you’ll unfortunately have to go see someone in person.
The good news is that often tamsulosin and ketorolac will be enough to relieve your pain.
- Order imaging and labs
After a thorough history via telemedicine, our VirtuCare experts can send orders for labs or imaging to a local facility. We can even receive the results and follow up with you to discuss the next steps.
- Refer to surgeon
If we find a stone that is unlikely to pass (usually >5 mm in size) then we can help you find the closest and best urologist to discuss a stone removal or lithotripsy.
- Follow up visits for kidney stone prevention
Once you’ve recovered from this terrible episode, make sure to schedule a follow up visit with your VirtuCare urologist to discuss stone prevention. We will cover the latest dietary recommendations for a kidney stone diet. If necessary then a 24 hour urine collection can be ordered to perform a deep dive analysis of why you’re forming kidney stones.
With VirtuCare we offer discounted follow-up visits and annual membership plans so you can continue seeing the same urologist.
We are there for you in the moments when you need help the most!
Dr. Joe Pazona
We’re here to help..
At VirtuCare, we believe that patients deserve direct access to the experts. There should be no gatekeeper standing between you and a healthcare specialist. VirtuCare puts you in control.
Related Posts
Cremaster muscle pain: the likely cause of your achy balls, when should a woman see a urologist, how to get a telemedicine prescription, interested in learning more about a partnership with virtucare hear from one of our partners..
When to Go to the ER for Kidney Stones
When to Go to the ER
Mar 1, 2024

Kidney stones are a common and painful condition that affects millions of people each and every year. While kidney stones can often be treated at home, there are times when knowing when to go to the ER for kidney stones is necessary.
The emergency medical experts from Complete Care are here to discuss when you should go to the ER or urgent care for kidney stones and what the kidney stone ER protocol is, so you can know what to expect during your visit.
Before we go deeper on the subject, if you suspect that you have kidney stones, you should head to the ER if you have any of the following symptoms:
- Abdominal pain
- bloody urine
- Pain when urinating
- Severe pain
What is the main cause of kidney stones?
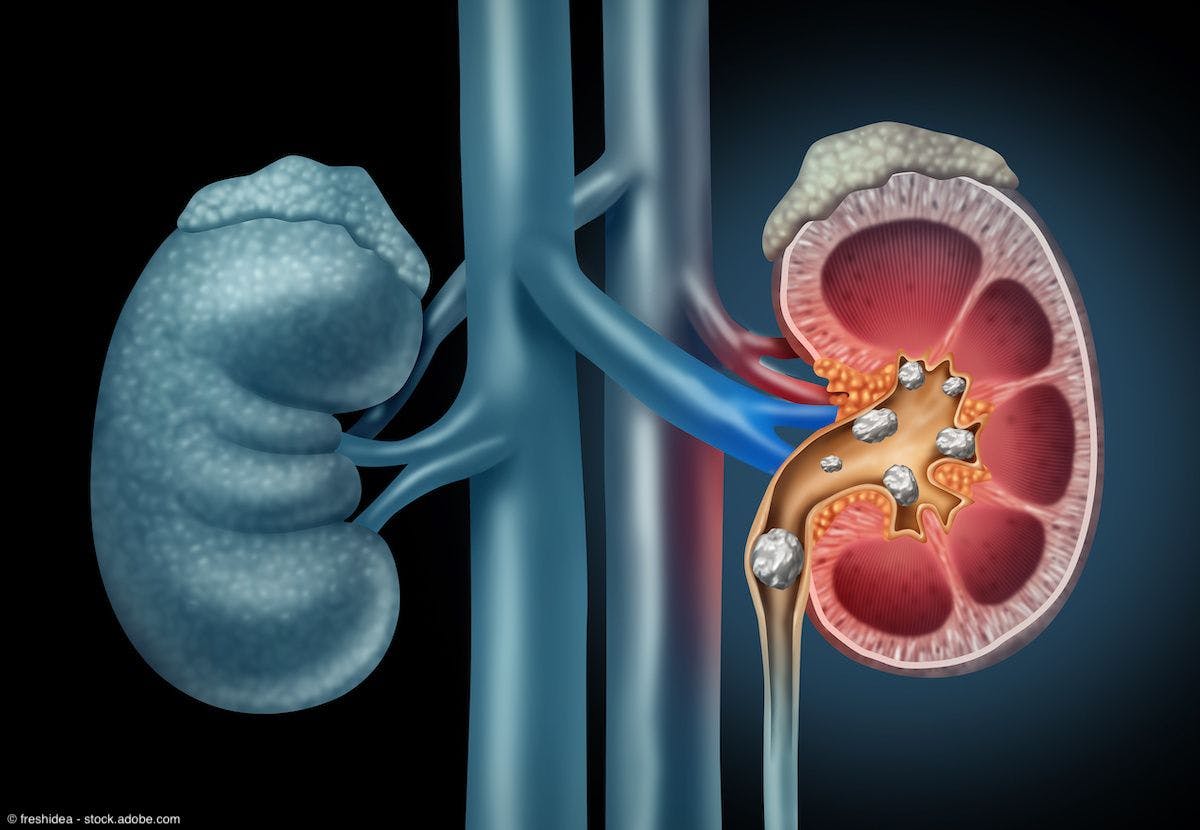
Kidney stones are hard deposits of minerals and salts that can form in the kidneys when there is an imbalance of water, salt, and mineral water in your urine. As the stones grow in size, they can lead to severe pain and other symptoms.
Kidney stones typically occur when you’re drinking less water than what your body needs, which is something many of us are guilty of. People in warmer climates who sweat more are often more susceptible as they require more water to stay hydrated. However, there are many other factors that can increase your risk of developing kidney stones, including:
- High blood pressure
- Eating a diet high in salt and sugar
- Family history
The most common type of kidney stone is made of calcium oxalate, but it can also be made of other substances such as uric acid or struvite. Kidney stones, depending on their cause and make-up, can develop over weeks or months.
Symptoms of kidney stones
How can I check myself for kidney stones? Symptoms of kidney stones most often include:
- Severe abdominal, back, or left side pain
- Severe pain in the groin or genitals
- Painful urination
- Blood in urine
- Fever and chills
- Nausea or vomiting
It’s important to note that small kidney stones can pass on their own without medical intervention, but it will not be pleasant. Passing a kidney stone can be extremely painful, even if your symptoms are mild.
How long should I wait for a kidney stone to pass?
How long a kidney stone takes to pass varies from person to person and depends on factors such as the stone’s size and location. While some stones may pass within a few days with adequate hydration and pain management, others may require medical intervention. If left untreated for too long, kidney stones can enlarge and become infected, which can pose a number of dangerous health issues.
How do you know when a kidney stone is serious?
When should you go to the ER for kidney stones? In addition to the symptoms above, you should visit the emergency room immediately if you have:
- A fever higher than 101.5 degrees Fahrenheit, as a high fever coupled with chills can be a clear sign of infection (keep reading: How does the ER treat high fever? ).
- A burning sensation when you urinate , are having difficulty urinating, or are unable to urinate at all, as this could be a sign of a blockage caused by a kidney stone.
- Cloudy, pink, or foul-smelling urine, which can be a sign that there is blood or bacteria in your urine.
- Intolerable or severe pain in your abdomen that is not relieved by over-the-counter pain medication, as this could be a sign of a larger or more complicated kidney stone that may require medical intervention (keep reading: When to go to ER for stomach pain ).
- Certain medical conditions that make passing a stone more dangerous, such as diabetes or decreased kidney function.
- A history of kidney stones and have experienced complications in the past.
If you’re unsure of whether you should go to the ER or urgent care for kidney stones, an urgent care will be able to help you manage pain and mild symptoms, whereas an emergency room will be able to handle more severe symptoms and will likely have the equipment available to provide you with a more accurate diagnosis.
Can the ER do anything for kidney stones?
Absolutely! Once you get to the emergency room, a healthcare professional will evaluate your symptoms and medical history. Kidney stone ER protocol will likely include a physical exam, blood work, and imaging tests to determine the size and location of the kidney stone, which may include an X-ray and/or a CT scan of your abdomen and pelvis. Once confirmed, you’ll be prescribed medications to help alleviate the pain and manage your symptoms as the stone passes.
In some cases where the kidney stone has grown too large, surgery may be required. When this is the case, you can be administered a non-invasive shockwave treatment procedure (lithotripsy) to remove the enlarged kidney stone or a ureteroscopy, where a small scope is used to remove the stone.
How do you prevent kidney stones from forming?
To lower your risk of kidney stones, you should drink the suggested amount of water per day. For the average adult, this should be eight 8-ounce glasses of water each day. If you live in a warmer climate or exercise often you should increase your daily water intake to stay hydrated. You can also be mindful of your salt intake and choose foods and beverages that have lower sodium levels to further reduce your risk for kidney stones.
Obesity can also raise your risk of kidney stones. If your BMI is within the obese range, you can talk to your doctor about making the changes necessary to achieve a healthy weight for your body type and lower your risk.
Experiencing painful kidney stones? Complete Care has got you covered.
Kidney stones can be a painful and uncomfortable experience, that in most cases can be treated at home. However, it’s important to know when to go to the ER for kidney stones in case you experience symptoms that are more severe. If you experience severe pain, difficulty urinating, or signs of infection, come to a Complete Care emergency room as soon as possible.
Our freestanding emergency rooms are fully equipped with digital imaging services such as X-rays and CT scans that may be necessary for determining your treatment. With our low wait times, you won’t have to deal with severe pain for long — we will get you in, out, and on the mend as soon as possible.
We have multiple locations in Texas ( Austin , Corpus Christi , Dallas/Fort Worth , East Texas , Lubbock , and San Antonio ) and in Colorado Springs that are open 24/7 to care for you and help alleviate your kidney stone symptoms. Passing a kidney stone is never fun, but it can be a lot more manageable (and a lot less scary) when you’re in our capable hands.
The BEST experience I’ve ever had medically. Hands down. I have severe anxiety when it comes to needles and came in with kidney stone pain which is spooky enough. Dr. King and her staff were so kind and patient, and got me all the scans and blood work needed while comforting me through my phobia. I’m on my second visit here, and couldn’t for better. The facility is extremely clean, quiet, and it’s a very fast trip! Little to no wait time! Front desk is extremely welcoming and did a great job! Bri N. | Satisfied Patient
More Helpful Articles by Complete Care:
- When to Go to the ER for Knee Pain
- When to Go to the ER for Sciatica Pain
- Is My Thumb Broken or Sprained?
- Exercise Safety Tips to Remember in the New Year
- Why Patients Say Complete Care is the Best Emergency Room
Share this on
- How is a ureteral stent placed?
- How is a ureteral stent removed?
- Kidney Stones FAQ
- Kidney stone myths
- Dietary prevention of kidney stones
- Letting a kidney stone pass
- Medications to help pass kidney stones
- Ureteroscopy
- Shockwave lithotripsy (ESWL)
- Percutaneous nephrolithotripsy
- Comparing ureteroscopy, shockwave lithotripsy, and percutaneous nephrolithotripsy
A reliable source of information for kidney stone patients.
The Healthcare Costs of Kidney Stones
With the increased attention on the rapidly increasing cost of healthcare , we decided to take a closer look at how much kidney stone disease costs in the United States.
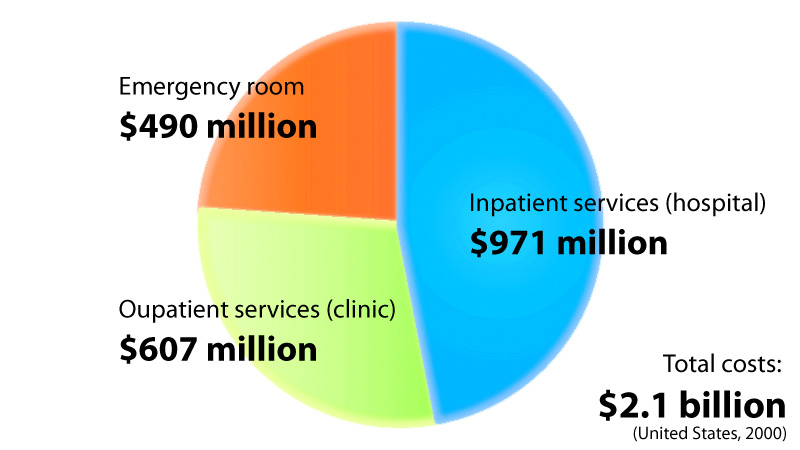
United States healthcare expenditures for kidney stone disease for the year 2000 (most recent available published data).
Underlying the costs for kidney stone treatment is how common stone disease is, with about 1 in 10 Americans experiencing a stone during their lifetime . That results in a lot of clinic and emergency room visits, trips to the operating room, and prescriptions for pain control medication. Additionally, because stone disease often afflicts working aged adults, there are also large costs incurred due to lost work hours.
Where is the money going?
About half of the healthcare expenditures for stone disease was due to inpatient hospital costs , which includes surgeries requiring hospitalizations and admissions to the hospital for stone related problems. Other costs included clinic visits, outpatient procedures, emergency room visits, radiology examinations, and prescription drugs. The estimated average healthcare cost for each stone patient for the year amounted to $6,532 dollars. This is considerably higher than the average healthcare cost of $3,308 for non-stone formers during the same year. Note that these figures refer to costs for health insurers. The “out-of-pocket” costs for an uninsured individual will be higher, sometimes significantly more.
Average cost per stone former:
$6,532 of which
18% were for prescription drugs
Cost of surgeries
About 25% of stone patients require surgical treatment each year . Of the surgical options available, percutaneous nephrolithotripsy was the most expensive approach, as measured by cost by procedure, with shockwave lithotripsy and ureteroscopy coming in second and third. The dollars figures shown below were for the year 2000 and reflects expenditures by insurance companies. Out-of-pocket costs for an uninsured patient will be higher.
Average cost of stone surgeries:
PCNL: $3,624
ESWL: $2,295
Ureteroscopy: $1,425
Costs due to lost work:
In 2000, 1% of all working age adults missed work due to a stone episode. When focusing on just stone formers, 30% of them missed work due to a stone episode, with each worker losing an average of 19 work hours over the year , or 3.1 million lost workdays for the entire working population. Estimating an average U.S. hourly wage of $24 an hour, that equates to $456 of wages lost per worker. From an employer’s standpoint, the estimated indirect costs due to stone disease was $775 million dollars a year. Unmeasured here are other potential costs, such as childcare, transportation, and lost work by family members that might be incurred during trips to the emergency room, clinic, or operating room.
Lost hours of work:
19 hours per worker
Lost wages per worker:
$456 dollars
Saigal et al, “Direct and indirect costs of nephrolithiasis in an employed population: Opportunity for disease management?” Kidney International, 2005.
Lotan and Pearle, “Economics of Stone Management”, Urologic Clinics of North America, 2007.
If you have experienced kidney stones, let us and other readers know how costs for stone treatment have personally impacted you by commenting below.
2 Leave a Reply
[…] nerkowe dotykają około 10% ludzi w świecie zachodnim, a roczne koszty opieki zdrowotnej związane z kamieniami nerkowymi w samych Stanach Zjednoczonych wynoszą ponad 2 miliardy […]
Is there anyone in the Southern Ontario area with Medullary Sponge Kidneys. I am interested in knowing if they encountered the same medical roadblocks that I have. There is a doctor in Michigan who performs a surgery that helps eleveate problems associated with MSK. Of course they do not cover the procedure in Ontario and I am not financially able to afford to pay to see this doctor on my own, or I would immediately. I just want to be able to live my life, work and be a mother who is active and able to do my daily duties. It is very frustrated to suffer and feel there is no end in sight and no way to be treated for this debilatating condition.
Find Urgent Care today
Find and book appointments for:, urgent care.
- Pediatric Urgent Care
- COVID Testing
- COVID Vaccine
Navigating Urgent Care for Kidney Stones: What to Expect and Aftercare Tips

- Kidney stones are hardened mineral deposits that can cause severe pain and complications.
- Urgent care provides prompt medical attention, diagnosis, and treatment for kidney stones.
- Aftercare and preventive measures are essential to manage kidney stones effectively.
Causes, Types, and Risk Factors of Kidney Stones
Getting diagnosed with kidney stones, treatment options, complications and emotional impact of kidney stones, when to seek urgent care for kidney stones, what to do after visiting urgent care for kidney stones, finding an urgent care for kidney stones.
- Frequently Asked Questions
Urination is the way that many minerals and salts get transported out of your body. In some cases, however, a buildup of these minerals can form stones—known as kidney stones. Anyone who has ever dealt with a kidney stone probably describes it as one of the most painful experiences of their life. This is usually because the stones became large and irritating as they traveled from the kidneys through the ureters, bladder, and urethra, reports the Kidney Foundation.
If you’re dealing with what you think could be kidney stones, urgent care can be a great option for getting a diagnosis and treatment.
At urgent care, you can expect to receive prompt medical attention from experienced healthcare professionals. They will assess your symptoms, give you pain medication if indicated, perform diagnostic tests if necessary, and determine the best course of treatment for your kidney stones. Aftercare is also an important part of managing kidney stones, and your urgent healthcare provider will be able to give you instructions on how to care for yourself at home and when to follow up with your primary care physician or urologist. If you’re not sure if you’re experiencing kidney stones, continue reading for more about the causes, symptoms, and treatment options.
Kidney stones are hardened mineral deposits that form in the kidneys and then can make their way down the ureters, into the bladder, and then out the urethra with your urine. Occasionally, a kidney stone may be too large to pass and end up getting stuck in the kidney or ureter. They can be caused by a variety of factors, according to the Kidney Foundation. Some of these factors include:
- Dehydration
- Eating a diet high in sodium, animal protein, or sugar
- Certain medical conditions, such as gout or inflammatory bowel disease
Types of Kidney Stones
There are five main types of kidney stones, according to the Urology Care Foundation. Genetics and lifestyle habits influence which type of kidney stone develops.
- Calcium oxalate stones: These are the most common type of kidney stone and are caused by a buildup of calcium and oxalate in the urine.
- Calcium phosphate stones: These stones are commonly caused by abnormalities in the urinary system.
- Cystine stones: This type of kidney stone is caused by a hereditary disorder called cystinuria. This genetic disorder causes excessive amounts of the amino acid cystine to collect in the urine.
- Uric acid stones: These stones are caused by a buildup of uric acid in the urine and are more common in people with gout.
- Struvite stones: These stones are caused by a bacterial infection in the urinary tract and can grow quickly and become quite large.
Risk Factors for Kidney Stones
Many risk factors for developing kidney stones are unavoidable. However, understanding risk factors will help you determine if your symptoms could be related to kidney stones, according to the Kidney Foundation. The largest risk factors for kidney stones include:
- Age - People between the ages of 30 and 50 are more likely to develop kidney stones according to the Urology Foundation.
- Gender - Men are more likely to develop kidney stones than women, according to the Mayo Clinic.
- Certain medical conditions - Conditions like High blood pressure and diabetes can increase the risk of kidney stones according to the Mayo Clinic.
- Family history - If someone in your family has had kidney stones, you are more likely to develop them as well, according to the Kidney Foundation.
Chances are, you may be in a great deal of pain when you arrive at the doctor's office if you suspect you have kidney stones. For this reason, a quick evaluation is necessary to get you the proper treatment. The staff at urgent care understands this and will work efficiently to determine the likelihood of kidney stones while also ruling out other potential causes of your symptoms. The Mayo Clinic outlines the most common strategies used to diagnose kidney stones, starting with a physical exam.
Physical examination and medical history
The staff at an urgent care clinic will usually start their investigation of your symptoms by doing a physical examination. This will likely involve palpating your abdomen and checking for tenderness or pain in your stomach, back, and flank areas. They will also check your vital signs, including your blood pressure, heart rate, and temperature. This will help them rule out more serious conditions while also evaluating if you have an infection.
Alongside the physical exam, the healthcare providers will also gather information from your medical history. This will include asking you questions about your symptoms—including when the symptoms began, how severe they are, and whether you have experienced similar symptoms in the past. They will also ask about any pre-existing conditions and medications you are taking.
Imaging tests (X-ray, CT scan, ultrasound)
Imaging tests are commonly used to diagnose kidney stones. X-rays are one way to detect the presence of stones—but some stones may not be visible on an X-ray. For this reason, a CT scan or ultrasound may be ordered to get a better view of the kidneys and urinary tract.
Urine and blood tests
Urine and blood tests can also help diagnose kidney stones. A urine test can detect the presence of blood or minerals that may indicate the presence of stones, according to the Mayo Clinic. Blood tests can also be used to check for signs of infection or other conditions that may be causing your symptoms.
Once a diagnosis is made, your healthcare provider can begin providing the appropriate treatment and aftercare tips to manage your symptoms and prevent future kidney stones.
There are several options available for treating kidney stones, according to the Kidney Foundation and Mayo Clinic. Your doctor will recommend the best treatment option for your specific case based on the size and location of your kidney stones, as well as your overall health.
Pain management for kidney stones
Kidney stones can be extremely painful, and managing your pain is often a top priority for both you and your medical provider. In the appropriate clinical setting, strong pain medications may be given, sometimes intravenously. Upon discharge, your doctor may recommend over-the-counter pain relievers such as ibuprofen or acetaminophen, or prescribe stronger pain medications if necessary.
Medications for kidney stones
There are several medications available that can help kidney stones pass more easily or prevent them from forming in the first place.
- Alpha-blockers (such as Alfuzosin, Doxazosin, and Terazosin) are one class of medications that can relax the muscles in the ureter, making it easier for the stone to pass.
- Diuretics are used to help flush out the stone. Your doctor may recommend purchasing these over the counter or may prescribe them to you.
- Antibiotics are also used in some cases if your healthcare provider believes that an infection is present.
Extracorporeal shock wave lithotripsy (ESWL) for kidney stones
ESWL is a non-invasive procedure that uses shock waves to break up the kidney stone into smaller pieces—thus making it easier to pass. This procedure does not require an incision and is typically performed on an outpatient basis, according to the Urology Foundation.
Ureteroscopy for kidney stones
Ureteroscopy involves inserting a small scope into the ureter to locate and manually remove the kidney stone. This procedure may be necessary for larger stones or stones that are located in a difficult-to-reach area. This procedure is also used when other techniques fail to relieve you of kidney stones, according to the Kidney Foundation.
Percutaneous nephrolithotomy (PCNL)
PCNL is a surgical procedure that involves making a small incision in the back and using a scope to locate and remove the kidney stone. Much like ureteroscopy, the Urology Foundation notes that this procedure is typically reserved for larger stones or stones that cannot be removed using other methods.
Non-urgent Treatment Options for Kidney Stones
The Mayo Clinic and the Kidney Foundation both note that drinking plenty of water and making dietary changes can help prevent kidney stones from forming and help them pass more easily if they do form. Your doctor may also recommend limiting your intake of certain foods (like processed meats, red meats, and foods high in salt, as well as alcohol, and soda) or increasing your intake of others (water, low-sodium foods, fruits, vegetables, and legumes).
Kidney stones can lead to various complications, including kidney damage and infection, according to the Mayo Clinic. If a kidney stone blocks the flow of urine, it can cause pressure to build up in the affected kidney, leading to swelling and damage. The risk of kidney damage increases if the stone is left untreated for a long time.
In some cases, kidney stones can also cause urinary tract infections (UTIs). UTIs can cause additional symptoms such as pain and burning during urination, frequent urination, and fever . If left untreated, UTIs can spread to the kidneys, leading to more severe complications.
The impact of kidney stones on patients and their families
Kidney stones can have a significant emotional and psychological impact on patients and even their families, notes the Mayo Clinic . The discomfort caused by kidney stones can be intense and debilitating, making it difficult to carry out daily activities. This can lead to feelings of frustration, helplessness, and anxiety—especially when kidney stones are recurring.
Kidney stones can also cause a financial strain , as medical bills and time off work can quickly add up. Patients may worry about the possibility of future kidney stones and the impact this can have on their quality of life and long-term finances.
Family members and caregivers also experience emotional stress as they support their loved ones through the kidney stone experience. They may feel helpless or overwhelmed by their loved one’s pain and have to adjust their life schedule to handle additional responsibilities or medical visits.
All of this underscores the importance of seeking prompt medical attention and following up with appropriate aftercare to minimize the risk of complications and support a full recovery.
In some cases, kidney stones can cause severe pain and other complications that require immediate medical attention. If you suspect that you have kidney stones, it is important to seek medical attention as soon as possible. Here are some signs to look out for, as outlined by the Mayo Clinic, that should prompt you to seek medical care immediately.
- Severe pain - Especially in your back, side, or lower abdomen. The pain may come and go in waves and may be accompanied by nausea or vomiting .
- Blood in your urine - This could be a sign that you have a kidney stone that is causing damage to your urinary tract. Blood in urine can also be a sign of a UTI or other serious conditions, so it is important to seek medical attention right away.
- The inability to urinate - This could be a sign that a kidney stone is blocking your urinary tract. If left untreated, this can lead to serious complications, including kidney damage, according to the Mayo Clinic.
- Fever - If you have a fever (above 100.4°F), along with any other symptoms of kidney stones, you should seek urgent care. A fever could be a sign that you have an infection, which can be a complication of kidney stones.
What to expect at urgent care
When you arrive at the urgent care facility for kidney stone symptoms, you can expect a prompt and thorough evaluation of your condition. The urgent care staff will evaluate you by performing a physical examination while assessing your symptoms and medical history. They then will order diagnostic tests to help ensure the proper diagnosis. Testing may include X-rays, urine tests, blood tests, ultrasounds, or CT scans. Based on the results of the examination and diagnostic testing, your urgent care staff will recommend the appropriate treatment options. Treatment options may include:
- Pain management
- Medication to help pass the stones
- Procedures to remove the stones in some cases
Your medical provider will also determine if you need referral to a specialist, such as a urologist or nephrologist. This referral may be to continue treatment or to follow up.
Insurance coverage and costs associated with urgent care for kidney stones
Urgent care costs can vary depending on your insurance coverage and what specific services are provided to you. You can check with your insurance provider to understand your coverage and any associated costs. It is important to note that you should not delay seeking medical attention if you are unsure of your insurance coverage. Some urgent care facilities may offer self-pay options or payment plans.
After receiving treatment for kidney stones at urgent care, it's important to follow any home instructions that your healthcare provider gives you. The home instructions may include instructions on how to take prescribed and over-the-counter medication, foods and drinks to avoid, how much water to drink, and when to follow up with your primary care physician or urologist. You may also be asked to filter your urine in order to capture and identify the type of stone. Follow-up evaluations are recommended by the Kidney Foundation to monitor your condition and determine if additional treatment is necessary.
Your doctor may also recommend that you undergo follow-up testing, (such as a CT scan or ultrasound) to check for any remaining stones or kidney damage.
Lifestyle Changes to Help Prevent Kidney Stones
If you have experienced kidney stones, you are probably wondering what you can do to avoid ever having them again. Although there is no guarantee that you won’t develop them again, there are some lifestyle changes you can make that can help lower your chances. The Kidney Foundation recommends:
- Drinking plenty of water to stay hydrated
- Reducing your intake of sodium and animal protein
- Increasing your intake of fruits and vegetables
Additionally, your doctor may recommend that you take calcium and vitamin D supplements, as these can help prevent the formation of kidney stones.
When to Seek Further Medical Attention
While most kidney stones can be treated at urgent care, there are some cases where further medical attention may be necessary. The Urology Foundation lists symptoms that may indicate a severe case as:
- Severe pain that is not relieved by medication
- Blood in your urine
- Difficulty urinating
- Fever and chills
- Nausea and vomiting
If you suspect that you have kidney stones, it's important to seek medical care right away. An urgent care clinic is a great option for getting fast, cost-efficient medical care. If you are experiencing any of the symptoms of kidney stones, according to the Mayo Clinic including:
- Pain or discomfort in your abdomen, back, or sides
- Painful urination
- Nausea, or vomiting
Use Solv to find an urgent care near you, by searching our directory. We can help you find an urgent care client with skilled medical providers and the testing capabilities necessary to diagnose and treat kidney stones. Once you have received care at urgent care, you can continue using Solv to book your follow-up appointments or find specialists in your area who can help you prevent future kidney stones from developing.
Frequently asked questions
What are kidney stones and how do they form, what are the types of kidney stones, what are the risk factors for developing kidney stones, how are kidney stones diagnosed, what are the treatment options for kidney stones, can lifestyle changes help prevent kidney stones, when should i seek urgent care for kidney stones, what should i do after visiting urgent care for kidney stones.
Michael is an experienced healthcare marketer, husband and father of three. He has worked alongside healthcare leaders at Johns Hopkins, Cleveland Clinic, St. Luke's, Baylor Scott and White, HCA, and many more, and currently leads strategic growth at Solv.

Dr. Rob Rohatsch leverages his vast experience in ambulatory medicine, on-demand healthcare, and consumerism to spearhead strategic initiatives. With expertise in operations, revenue cycle management, and clinical practices, he also contributes his knowledge to the academic world, having served in the US Air Force and earned an MD from Jefferson Medical College. Presently, he is part of the faculty at the University of Tennessee's Haslam School of Business, teaching in the Executive MBA Program, and holds positions on various boards, including chairing The TJ Lobraico Foundation.
Solv has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references.
- Kidney stones. (April 30, 2023) https://www.mayoclinic.org/diseases-conditions/kidney-stones/symptoms-causes/syc-20355755
- Kidney Stones. (April 30, 2023) https://www.urologyhealth.org/urology-a-z/k/kidney-stones
- Kidney stones. (April 30, 2023) https://www.kidney.org/atoz/content/kidneystones
- Kidney stones. (April 30, 2023) https://www.kidneyfund.org/all-about-kidneys/other-kidney-problems/kidney-stones
- Kidney stones. (April 30, 2023) https://www.niddk.nih.gov/health-information/urologic-diseases/kidney-stones
- Kidney stones. (April 30, 2023) https://medlineplus.gov/kidneystones.html
- Alpha-blockers: Types & Usage (April 30, 2023) https://my.clevelandclinic.org/health/treatments/22321-alpha-blockers
- medical imaging
- urgent care

Quality healthcare is just a click away with the Solv App
Book same-day care for you and your family
Find top providers near you
Choose in-person or video visits, manage visits on-the-go, related articles.

How to Treat Gout: 7 Things You Can Do to Relieve Your Gout Flare-up
Gout is a type of arthritis that happens when uric acid builds up in the blood and forms crystals in the...

UTIs and Urgent Care: Understanding the Risks, Costs, and Complicat...
A urinary tract infection (also called a “bladder infection” or “UTI”) is a common bacterial infection that can...

Plantar Warts: Why Urgent Care is a Great Option for Plantar Wart R...
Plantar warts are a common type of wart that affects the feet, and they can be painful at times, according to...

The Role of Urgent Care in Early Diagnosis and Management of Hernia...
A hernia occurs when an internal organ pushes through a weakened area of muscle. While a hernia can occur in...

Urgent Care for Knee Pain: When to Seek Medical Attention
If you're experiencing knee pain, you're not alone. Knee pain is a common issue that affects people of all ages,...

Debunking Migraine Myths: The Importance of Seeking Urgent Care for...
Migraines are recurring headaches that cause moderate to severe pain. According to the Mayo Clinic, some...

Don't Ignore the Signs: Urgent Care Options for High Blood Pressure
High blood pressure (also called hypertension) is a common condition that affects millions of people...

Don't Wait: The Importance of Urgent Care for Hemorrhoids
Hemorrhoids are a common condition that affects nearly three out of every four people, according to the Mayo...

Shedding Light On Melanoma
Melanoma is the most dangerous form of skin cancer—and it's on the rise in younger people. The Melanoma...

At-home Tips for Diabetes Self-Care
Diabetes is a chronic condition that requires careful management to prevent complications including kidney...
Related Health Concerns
Abdominal Pain
Antihistamines
Athlete's Foot
COVID-19 Vaccine
Cataract Surgery
Pinched Nerve
Sexually Transmitted Diseases
Tonsil Stones
This site uses cookies to provide you with a great user experience. By using Solv, you accept our use of cookies.
- Quick Links
- Make An Appointment
- Our Services
- Price Estimate
- Price Transparency
- Pay Your Bill
- Patient Experience
- Careers at UH
Schedule an appointment today

Comprehensive Kidney Stone Relief, Treatment & Prevention Services
Kidney stones send more than one million Americans to the emergency room every year. That doesn’t need to happen to you. If you have a kidney stone , let the experienced urology team at University Hospitals develop a personalized care path for immediate relief and help you prevent new stones from forming.
Our urologists and other kidney stone experts have many different non-invasive and minimally invasive treatment options to remove your kidney stone based on its size, location and your other health conditions. Throughout your care, our team strives to ensure your complete comfort and successful recovery.
Find Complete Relief from Your Kidney Stones
If you think you may have a kidney stone, or have suffered from them in the past, please contact the UH urology team to schedule an appointment at 216-844-3009 .
Find a Doctor
What are Kidney Stones?
Kidney stones are made of dissolved minerals, such as calcium, that crystalize in the kidney. These stones either stay in the kidney or travel down through the ureters, which are tubes that connect your kidneys with your bladder. Sometimes, if the stone is large enough, it gets stuck in the ureter and blocks urine, causing great pain. If the stone passes into the bladder, expelling it during urination can also be quite uncomfortable. Other kidney stone symptoms may include:
- Pain in the side, back and may radiate to the belly or groin
- Blood in the urine
- Cloudy or odorous urine
- Fever and chills
- Frequent urination
- Nausea and vomiting
With the advanced diagnostics needed, our urology experts conduct blood, urine and imaging tests — such as an X-ray, ultrasound or computed tomography (CT) scan — to determine the type of stone you have, its location and its size.
Based on the test results and a full medical evaluation, our specialized team of kidney stone experts will recommend kidney stone treatment options based on your unique health needs to provide the best treatment for your kidney stones and kidney stone pain.
UH Offers Unique Metabolic Evaluations for Stone Prevention
Removing stones and ensuring your comfort is our most immediate concern. However, the experts at University Hospitals conduct a complete metabolic evaluation to find out why your stone formed and how to prevent others from occurring.
A metabolic evaluation includes an analysis of the passed stone, as well as 24-hour urine collection and dietary log. In the vast majority of cases, by analyzing urine over a 24-hour period and conducting a complete health assessment, our specialists can pinpoint the cause of kidney stone formation.
Not all healthcare organizations perform a metabolic evaluation, but our team is committed to helping you avoid another painful kidney stone experience. Our specialists are highly experienced in performing metabolic evaluations, and recommend them for all our patients with kidney stones.
Improved Outcomes from Specialized Urologist Care
More than 80 percent of kidney stones pass on their own. In these situations, our primary goal is to reduce your kidney stone pain and discomfort and help it pass quickly and without injury. For more complex or larger stones, there are numerous non-invasive and minimally invasive treatments available, including:
- Cystolitholapaxy: This procedure uses a laser or other modalities to break up bladder or kidney stones.
- Shock waves or extracorporeal shock wave lithotripsy (ESWL): A non-invasive procedure, we use shock waves to break stones into smaller pieces, so they can be passed through the urine.
- Ureteroscopy: A kidney stone surgery using a tiny camera, or scope, through the urethra, our team is able to precisely locate the stone while a surgeon removes or breaks the stone into smaller pieces.
- Percutaneous nephrolithotomy (PCNL): Reserved for larger stones, this procedure to remove kidney stones uses a small incision in the back with a tube inserted to the kidney stone location. The urologist will then insert the tools through the tube to remove the stone.
- Percutaneous nephrolithotripsy (PCNL): Using the same technique as percutaneous nephrolithotomy, our urologists treat larger kidney stones, usually 2 cm or larger, by inserting tools through a tube inserted in a small incision in the back. Stones are broken up and the small fragments are then removed through the tube.
At University Hospitals, our skilled urology team operates the scopes and is responsible for every step of the process. This typically results in the faster and more precise identification of the stone, a more efficient overall procedure and better results.
Sign up for our free newsletters!
- Consumer updates newsletter
- Industry insider newsletter

ClearHealthCosts
Bringing transparency to the health care marketplace.
Kidney stone removal or lithotripsy: How much does it cost?
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
- Click to email a link to a friend (Opens in new window)
- Click to share on Reddit (Opens in new window)

(Updated 2022) Kidney stone removal, or lithotripsy , uses shock waves or lasers to break down stones in the kidney, gallbladder, or ureters. Kidney stone removal costs can vary. One of our community members shared several prices for treatment via our site , and we started a conversation focusing on both his experience and his kidney stone removal cost. Let’s call the community member Michael from the Louisville, Ky. area.
Before we start, though, I want to note that a system requiring someone like Michael to go to these lengths while he’s worrying about a serious health problem is unusual throughout the developed world. It’s pretty much only here in the United States that he would have to do this. The prices varied widely: $16,177, $9,773 or $7,642?
Also, he noted the pushback he got from seeking these prices, and adds that he succeeded this way: “I have successfully communicated to them through the analogy of having a car delivered to your house and being told that you must pay for it, but no one can tell you how much until after its delivered… and there are no returns.”
We plan to follow his journey, so check back for updates.
Michael’s experience with kidney stones
I am self-employed and my choice was down to paying for insurance or doctor bills. So I chose to forgo insurance to make sure I could afford to see my doctors.
Since that decision was made, I have had a bout of kidney stones (4 separate stones) and two surgeries… one left to go.
I told them I needed it all done before my insurance expired, but the doctors couldn’t make that happen.
I was admitted through the E.R. of a local hospital late in September and had Laser Lithotripsy done for two stones in my left kidney, the largest of which was 11mm. The approach was, I later learned, a “dusting” approach usually done for “softer” stones. I was informed only recently that the collections of stone fragments from that surgery were too small to collect. I suspect, however that they were either lost, discarded or unable to be collected as I understand that using a laser on a stone, even a soft one, breaks it into fragments. In any case, there is no analysis on record as to the actual composition of the stones.
In late December, I had another stone attack which landed me back in the E.R. with the right kidney this time having two stones, one lodged in the ureter (5mm) and one at the entrance to the ureter in the kidney (7mm). The stone pain had subsided thanks to the miracle of modern pain relief and I was able to clear-headedly discuss the plan and options with the urologist on call.
As is usual these days, the urologists are not employees of the hospital. I discussed with him the plan for treatment and together we decided to use shock wave lithotripsy which was not available in that hospital. I decided that if it was simply a matter of where I was bedded that was keeping me from the treatment that could potentially get at both stones at once (as apposed to lasering which would not allow access to both stones), then a transfer was preferable to multiple surgeries which would definitely land outside of my covered period as my insurance expired at the end of the month.
One stone left after the lithotripsy procedure
My shock wave lithotripsy (SWL) was performed and a stent was put in while I was under on the last day of the month (the soonest it could be performed) as an outpatient surgery. Unfortunately, my bones were placed in such a way that the SWL could not get past my pelvic bone to access the larger stone in my kidney. I am now left with a stone at the entrance to my right kidney that hangs like the sword of Damocles.
I had not received detailed information from my providers on these upcoming procedures that would allow me to ascertain costs. When I requested this information prior to undergoing each of the previous procedures I was told that it was impossible to know.
So, now without the excuse of “I can’t tell you how much it costs because of insurance variability”, I demanded to know the price tags… prior to getting anything done. I have had to cancel surgeries twice in order to get the information.
I am still in that process. The facilities charges are astronomical and are built around the codes that the doctors determine they will need for their surgery. Each separate code brings with it well over $1,000. So when the doctor ordered an additional code for my second operation (after I canceled the first), I started to question everything.
talk to hospital operators to find lithotripsy specialists
Here’s what I have found: Each facility has a specialist hidden within the phone system tree, and it is best to talk to the operator to find them. They are called Insurance Verification, Cost Evaluators, Financial Counselors, Cost Estimators, and possibly more as there seems to be no consistency in the industry.
If the doctors office had already scheduled you at the facility, they will have the codes the doctor sent over. If you have not been scheduled, you must get the codes from the scheduling person for your doctor. If they haven’t decided to schedule you yet, you can ask for the codes that the doctor will be using and why each code is necessary during your visit. They will likely not know, but they can get them for you… this will likely take a willingness to be persistent. I am going back to my doctor to discuss the codes chosen and exactly why each was chosen. This will cost me a doctors visit ($125), but I think it’s worth my time and $.
BTW, I found one facility that charges $2,000 less for the exact same codes… but my doctor’s office said that they don’t work at that hospital even though it is only about 6 miles away. That’s okay, because I can use another urologist in the same medical group who will, once I have squared away all of the information…. for $2k, it’s worth it.
I had trouble getting prices out of the urologists office for just their work, and finally got hold of someone in billing while on site who gave me the extension of the one person (and only one person) who does pricing. They aren’t in the phone tree, so it was a bit of a bear.
Funny thing was, their prices are very much in line with Medicaid pricing, so it’s not like they had anything to hide… they just made it difficult.
The medical codes that govern pricing
The codes that I received from talking to the scheduling nurse were the items I used to get pricing. Each code is a universal number that is applicable across all the medical universe. These are called CPT codes or “Current Procedural Terminology”. Think of them like a standard that is used so that different offices can talk to each other and be more precise. For more in-depth information about CPT codes you can find websites that discuss CPT coding as it is the basis of billing for hospitals and insurance (e.g. https://www.medicalbillingandcoding.org/intro-to-cpt/ ).[Editor’s note: Here’s our handy guide to coding .]
Strangely, the codes that I was given were all procedures that could be performed individually, but not usually together (according to the cost evaluations person at one of the hospitals that I was doing the pricing). While this was probably done so that the doctor could cover their bases in case they had to switch from one kind of procedure to another without having to request the hardware from the facility, each additional code added $1,200 – $1,800 on the low side. I determined that I would need to be very specific with my doctor and get more information on why each of these codes were necessary. Since this is an ongoing journey, I have not yet spoken with my urologist regarding the necessity of these codes.
I will include my spreadsheet. The totals given here are facility charge plus doctor charge plus $500 predicted anesthesia charge. The highlighted cells are changes that were made after initial information was given either due to the doctor adding a code (ergggh) or the facility changing their cost estimates:

I have not found a way, yet, to get prices for anesthesiologists. I have an estimate from the scheduling nurse, but I think I will have to contact the facility, find out who works there, and then call the individual offices to get prices.
My methodology for surgery pricing:
1) Get codes from doctors office… not easy, but necessary. 2) Get pricing from that office’s doctor’s billing department for the doctor’s work – get itemized pricing for each code. 3) Get pricing from facilities based off of codes from the doctor’s office – get itemized pricing for each code.
That’s it. It makes it sound easy, but the facilities do not want to give you an itemized list and in one case quoted $2K more once the codes were listed out. That same facility then quoted me regular prices and then (when pressed) gave me a 50% discount for self pay which brought it back down to the first quoted price.
I have made a list of the people I talked to at each location… none of which readily gave me a last name or a direct number to call back.
Non-surgery-related charges, and a mystery
Testing and diagnostics are sent from the doctors office to whoever it is easiest for them to send to… normally a large chain like Labcorp. When you ask how much a diagnostic or analysis will be the doctor’s office simply doesn’t know. When pressing for codes or numbers to order, they usually don’t have that either.
I was able to get into Labcorp’s public-facing website and look up tests. This allowed me to determine the limited number of tests that it could be and then a phone call to Labcorp narrowed it further to the single test for (in this case) stone analysis.
I got the CPT code from their website and I contacted a well-established lab I had run across doing my own research on kidney stones. I called them and asked for a price on that CPT code and they offered me a price of less than half the cost of Labcorp. This is where things get interesting.
I called my doctors office and let them know that I wanted my stones sent to this other lab for analysis. Gave them the address and let them know that I had already made arrangements for payment to the lab so all they had to do was send it and the order for the test.
trying to use the lower-priced provider
A day later I got a call from my doctor’s office letting me know that they can’t do that. They have a policy to only work with Labcorp (meaning they won’t do that). In the U.S., labs are not allowed to take a sample from an individual and return it to the individual under federal law. Sending my sample out of the states to a friend overseas who then submits my sample to the lab is a valid work-around, as the federal laws no longer apply.
I have recently shopped around for X-rays as well. As far as I know there isn’t the convenience of a CPT Code, but instead the designation of the area to be X-rayed. This does not correspond to the same verbiage as a CT Scan which has it’s own set of designations:
X-RAY: K.U.B (Kidneys Urinary Tract, Bladder) CT-Scan: Abdomen Pelvis
A facility again, not on my initial calling list, was half the cost.
The list is more of an assumption than a physical list that I was able to locate. “The list” was comprised of the places at which that the scheduling team at my urologists had scheduled me. I suppose I could call and ask them at which facilities they would be willing to perform surgeries or scans and I would get a pretty short list.
When it came time to do X-Ray and diagnostics pricing, I first had to get the terminology from the nurse at the doctor’s office for what kind of X-ray (or CT scan) they wanted to perform. X-rays are pretty straightforward, but CT scans can be done with or without contrast. You will need to find out if it is necessary to have contrast from your Doctor’s office, and you must get an order from them.
using the internet to find THE BEST kidney stone removal COST
Once armed with that information, I turned to the trusty Interwebs. I did a Google search for locations that are in the metropolitan area of the closest major city (which seemed like the best bet to find stand-alone centers) that performed X-ray or radiology services. This resulted in a few places to call, and so I did. I asked to speak with someone who could get me a price on an X-ray and/or CT scan. They seemed to be a lot easier to deal with than the surgery facilities when getting this information.

Thanks for being interested in my journey.
I am a self-employed computer consultant who does more research than the average person, so this isn’t totally outside of my wheelhouse. What is the most difficult is wading through the reticence I receive from these businesses to give me actual pricing _before_ they do the work.
I have successfully communicated to them through the analogy of having a car delivered to your house and being told that you must pay for it, but no one can tell you how much until after its delivered… and there are no returns.
I hope your journeys are fruitful.
Market forces simply cannot exist where there is no functioning market.
Jeanne Pinder
Jeanne Pinder is the founder and CEO of ClearHealthCosts. She worked at The New York Times for almost 25 years as a reporter, editor and human resources executive, then volunteered for a buyout and founded... More by Jeanne Pinder

- Benign Prostatic Hyperplasia
- Hormone Therapy
- Genomic Testing
- Next-Generation Imaging
- OAB and Incontinence
- Genitourinary Cancers
- Kidney Cancer
- Men's Health
- Female Urology
- Sexual Dysfunction
- Kidney Stones
- Urologic Surgery
- Bladder Cancer
- Benign Conditions
- Prostate Cancer
ER costs for treating stones, UTI vary widely
A recent study highlights huge price swings in patient charges for the 10 most common outpatient conditions-including kidney stones and urinary tract infection-in emergency rooms across the country.
The study, representing an estimated 76 million emergency department visits between 2006 and 2008, used data from the 2006-2008 Medical Expenditures Panel Survey from the Agency for Healthcare Research and Quality.
Researchers focused on adults 18 to 64 years of age, the demographic at the highest risk of facing the largest out-of-pocket charges. It excluded people 65 years of age or older because most such patients are covered by Medicare. Visits resulting in hospital admission were also excluded.
Altogether, the authors, who published their findings online in PLOS ONE (Feb. 27, 2013), looked at the total charges-medical care, tests, and treatment-for 8,303 patients, nearly half of them privately insured. The charges do not represent the amount patients or insurers reimburse providers, but rather the total charge that patients or their insurance providers are billed. Because of the complex survey design, the number of patients analyzed in the sample was weighted to provide the total estimated number of ER visits during the study time frame.
The authors found that out-of-pocket patient charges ranged from $128 to $39,408 for kidney stones and $50 to $73,502 for urinary tract infections. Of all the conditions studied, which also included sprains and strains, headache treatment, and intestinal infections, kidney stone treatment had the highest median price at $3,437.
"Our study shows unpredictable and wide differences in health care costs for patients," said senior author Renee Y. Hsia, MD, of the University of California, San Francisco.
Related Content
ER data: Urolithiasis, stone-related infection rising
Analysis bolsters expulsive therapy's cost-effectiveness

Data support shock wave lithotripsy for pediatric patients with kidney stones
Regarding patient-reported outcomes, those who underwent URS showed higher urinary symptoms, greater pain intensity, and greater pain interference at 1 week following surgery compared with those who underwent SWL.

Why kidney stones will become more prevalent over time
“The prevalence of kidney stones has increased over 80% over the last 30 years, and the epidemiology has changed such that it's beginning at a younger age now,” says Gregory Tasian, MD, MSc, MSCE.

Combo of burst wave lithotripsy and ultrasonic propulsion feasible for kidney stones
Combination treatment with burst wave lithotripsy and ultrasonic propulsion for small, asymptomatic renal stones is feasible.

Dr. Krambeck investigates efficacy of Trilogy and ShockPulse-SE lithotripters
“You have tradeoffs with every device that you use,” says Amy E. Krambeck, MD.

FDA grants orphan drug designation to ADV7103 for cystinuria
ADV7103 is currently being studied in the phase 2/3 CORAL-1 study, enrolling patients with cystinuria across centers in France and Belgium.
Alkaline water unlikely to prevent kidney stones, study finds
"While alkaline water products have a higher pH than regular water, they have a negligible alkali content–which suggests that they can't raise urine pH enough to affect the development of kidney and other urinary stones," says Roshan M. Patel, MD.
2 Commerce Drive Cranbury, NJ 08512
609-716-7777
Kidney Stone Symptoms and When to See a Doctor
Are you experiencing severe pain in your lower back? Is there blood in your urine? Do you have difficulty urinating? You may have a kidney stone, a rock-like deposit created from high levels of minerals and other substances in the urine. ( 1 , 2 ) Kidney stones can form in one or both of your kidneys, organs that remove waste from the blood and excrete urine. ( 3 )
While kidney stones have become increasingly common, with 1 in 11 people in the United States developing them, the important message is that they are treatable — and easily treated if caught early. ( 4 ) Untreated kidney stones that grow and cause complications, such as infection, fever, or blood in the urine, can be particularly dangerous.
Recognizing the symptoms associated with kidney stones is the first step to getting proper and timely care if and when you do have a stone.
You’ll Likely Feel Pain When You Have a Kidney Stone
Kidney stones can grow quietly within the kidney without causing any symptoms for months or even years, says John C. Lieske, MD , a consultant in the division of nephrology and hypertension at the Mayo Clinic in Rochester, Minnesota. However, when a stone breaks loose, it can block the ureter (the small tube that drains urine from the kidney and transports it to the bladder) and start causing a lot of pain.
The pain can be so severe that many people end up in the emergency room (ER), says Dr. Lieske, with one study finding more than one million visits to the ER in a year because of kidney stones. ( 5 )
Pain occurs because the stone is blocking the flow of urine, explains Daniel Marchalik, MD , a urologist and director of the kidney stone program at MedStar Washington Hospital Center in Washington, DC. The backup of urine makes the kidney swell, causing discomfort. “The size of the stone isn’t always important,” he says. “Even small stones can become lodged in the ureter and cause a backup of urine and severe pain.”
As the stone travels through the urinary tract, pain can shift from either side of the lower back to the abdomen and the groin, says Dr. Marchalik. Sharp, stabbing pain that comes in waves is common.
“Some women say the pain is worse than childbirth,” adds Naim Maalouf, MD , an associate professor of internal medicine at UT Southwestern Medical Center in Dallas.
Overall, symptoms tend to be similar in men and women. However, men can sometimes experience pain radiating to the tip of their penis when the stone is low in the ureter, says Marchalik.
Other Kidney Stone Symptoms, From Nausea to Cloudy Urine
In addition to pain, kidney stones can cause other symptoms: ( 6 , 7 , 8 )
- Nausea and vomiting
- A strong need to urinate
- Urinating more frequently
- Urinating small amounts
- A burning sensation or pain while urinating
- Blood in the urine — the urine will look brown, pink, or red
- Cloudy urine
- Gravel (or tiny kidney stones) in the urine
- Urine that smells bad
- Fever and chills, if you also have an infection
When and How Soon to See a Doctor if You Suspect a Stone
At the time of a first kidney stone attack, people often aren’t sure what is going on and need to be seen by a doctor to make sure the symptoms aren’t the result of a more serious problem, such as appendicitis, says Lieske.
As a general rule, you need to seek medical attention if you experience any of the following symptoms:
- Severe pain that makes sitting still or getting comfortable impossible
- Pain with nausea and vomiting
- Pain with fever and chills
- Blood in the urine
- Difficulty passing urine
- A burning sensation while urinating
If you can’t see your doctor that day, head to the ER.
“If stone pain and fever develop, go directly to the ER,” says Timothy F. Lesser, MD , a urologist at Torrance Memorial Medical Center in Torrance, California. A kidney stone with a urinary tract infection (UTI) may cause sepsis and must be treated immediately. ( 9 )
If urine is trapped behind a kidney stone that is blocking the ureter, the urine can become infected, says Seth K. Bechis, MD , a urologist at UC San Diego Health. This, in turn, can cause an infection of the kidney tissue or result in the infection spreading to the bloodstream, causing sepsis, he explains.
Additionally, over time stones can become infected and harbor bacteria, causing urinary tract infections, adds Dr. Bechis. Some people who have a history of recurrent UTIs are found to have a large stone that continuously sheds bacteria into the urine. When doctors suspect that someone has a kidney stone with a UTI, they place a tube in the ureter or kidney to drain the backed up, infected urine, says Bechis. In addition, antibiotics are given to treat infection. ( 10 )
While men are more prone to kidney stones than women, women are more likely to get UTIs, says Lieske. “So it’s not surprising that women are also more likely to get a urinary infection associated with their kidney stones,” he says.
People With a History of Kidney Stones May Sometimes Forgo the Doctor
While infection with kidney stones is a medical emergency, some people with a history of kidney stones may not always need to see a doctor, says Lieske. After an initial consultation with their physician, people who recognize their symptoms may be able to have pain medication on hand, so they can try passing the stone at home, he explains. Your doctor will likely have you drink plenty of water to help flush the stone out of your urinary tract.
Whether to use this approach “really depends on how severe the pain is and how comfortable people are with this strategy,” says Lieske. “Anecdotally, it seems that patients may have less severe pain the more kidney stone attacks they have had over the years, although this is certainly not universally true.”
Ibuprofen (Advil) can help with kidney stone pain , while a drug called tamsulosin (Flomax) may help relieve discomfort and enable you to pass the stone, notes Marchalik.
Fortunately, doctors can help you make prevention plans so you can avoid repeatedly developing stones.
Editorial Sources and Fact-Checking
Everyday Health follows strict sourcing guidelines to ensure the accuracy of its content, outlined in our editorial policy . We use only trustworthy sources, including peer-reviewed studies, board-certified medical experts, patients with lived experience, and information from top institutions.
- Kidney Stones: Symptoms and Causes. Mayo Clinic . June 3, 2022.
- Definition and Facts for Kidney Stones. National Institute of Diabetes and Digestive and Kidney Diseases . May 2017.
- How Your Kidneys Work. National Kidney Foundation .
- About USDRN. Urinary Stone Disease Research Network .
- Foster G, Stocks C, Borofsky MS. Emergency Department Visits and Hospital Admissions for Kidney Stone Disease, 2009. Healthcare Cost and Utilization Project Statistical Briefs . July 2012.
- What Are Kidney Stones? Urology Care Foundation .
- Kidney Stones. National Kidney Foundation .
- Patient Education: Kidney Stones in Adults (Beyond the Basics). UpToDate . July 2022.
- Kidney Stones. Sepsis Alliance . February 10, 2022.
- Treatment. Sepsis Alliance . March 25, 2021.
How Much Does It Cost to Go to the ER?
Treating a UTI costs $2,598, on average -- and we needed a study to tell us this.

"The health care market is not a market at all. It's a crapshoot." That's where, over 30 pages later, Time magazine's longest-ever article ended. It asked, in the course of its investigation into the industry, "Why should a trip to the emergency room for chest pains that turn out to be indigestion bring a bill that can exceed the cost of a semester of college?"
Such astronomical prices are indeed seen, according to a NIH-funded study published today in PLOS ONE: The median ER visit costs 40 percent more than what the average American pays in monthly rent. But the discrepancy in ER charges is so great, according to the study's authors , that patients have no way of knowing how much they can expect to be billed.
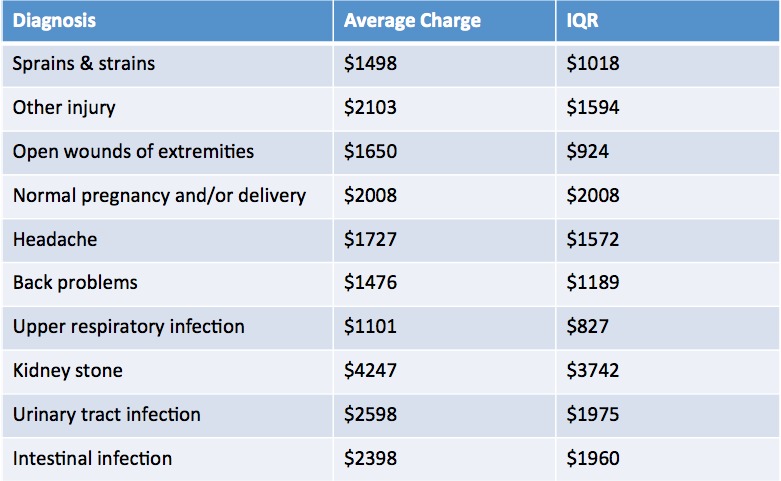
The average cost of a visit to the ER for over 8,000 patients across the U.S. was $2,168. But the interquartile range (IQR), which represents the difference between the 25th and 75th percentile of charges, was $1,957 -- meaning many patients were paying a lot more or a lot less than that. Of the top ten most common reasons for ER visits, treating kidney stones was most expensive, on average. But it was also the most variable. All of the charges -- which represent the total bill for adults 18 to 64 years old who, for simplicity's sake, came in with a single outpatient diagnosis -- followed similar patterns:
These numbers don't represent how much of the charges were ultimately covered by insurers. The researchers, did, however, also find that uninsured patients are typically charged the least, followed by privately insured patients, and finally by those on Medicaid, who saw the highest bills.
- Browse Topics
- Earn CME Credits Stroke Cardiac Trauma Pediatric Trauma Urgent Care All CME Tests
- Pathways New!
- Resources For Emergency Physicians Urgent Care Clinicians Emergency PAs & NPs Residents Groups & Hospitals

Renal Calculi: Emergency Department Diagnosis And Treatment
*new* quick search this issue.
The acute treatment of kidney stones (urolithiasis) addresses pain management and focuses on the effects of the morbidity associated with an obstructed renal system. Minimal fluid intake, resulting in decreased urine production and a high concentration of stone-forming salts, is a leading factor in renal calculi development. Radio-opaque calcareous stones account for 70% to 75% of renal calculi. Microscopic hematuria in the presence of acute flank pain is suggestive of renal colic, but the absence of red blood cells does not exclude urolithiasis. Furthermore, many inflammatory and infectious conditions cause hematuria, demonstrating the low specificity of urinalysis testing. The diagnostic modality of choice is a noncontrast computed tomography (CT); ultrasonography is preferred in pregnant patients and children. Combining opioids with non-steroidal anti-inflammatory drugs (NSAIDs) is the optimal evidence-based regimen to treat severe symptoms. Rapid intravenous (IV) hydration has not shown a benefit. Potentially life-threatening diagnoses including abdominal aortic aneurysm, ovarian torsion, and appendicitis may mimic renal colic and must be ruled out.
Case Presentations
It’s 8:30 pm and you receive a call from your chairman asking you to stop by the next morning regarding a patient you saw a few days earlier on a busy evening shift. The patient was 46 years old and complained of new-onset right flank pain for 1 day. He had no significant past medical history except chronic back pain, was on no medications, had no allergies, and was a social drinker. He had no other complaints, had stable vital signs, and his examination was only remarkable for mild CVA tenderness. You elected to treat him with oral analgesics and dipped his urine for blood. The patient had reduction of his pain with NSAIDs, and his dip showed no blood. He was discharged to home with a diagnosis of musculoskeletal back pain. The chart seemed to be in order, so why was the chairman concerned?
A 38-year-old woman presents complaining of 4 hours of left back pain. She admits to fevers, chills, and vomiting. She has a medical history of HIV and asthma. Her medications include albuterol and an HIV drug regimen. Social and surgical histories are unremarkable. She is febrile, tachycardic, and in moderate distress with a “colicky” type of presentation. She has blood drawn, urine sent for urinalysis and pregnancy test, and a noncontrast CT of her abdomen and pelvis is ordered to look for a kidney stone. You’re certain it will be positive, but you wonder if her HIV is a complicating factor.
Your last patient of the shift is a 57-year-old woman complaining of 4 hours of abdominal pain. She has a history of hypertension and hyperlipidemia. Her medications include an antihypertensive and her “high cholesterol pill.” She is noted to be restless and in mild distress with tachycardia, which you attribute to pain. Her abdomen is diffusely tender, and she has a moderate amount of blood on her urine dip. You order labs and a KUB followed by an ultrasound to rule out a kidney stone. She is medicated with morphine and is signed out to a colleague with the plan to control her pain and check her studies. When you follow up on her outcome the next morning, you are reminded that the last patient of the day does not always get the best assessment.
Introduction
Acute flank pain is a common presenting complaint to the emergency department (ED), requiring a broad differential diagnosis and work-up. Nephrolithiasis appears to be the most frequent cause of flank pain, affecting 3% to 5% of the population in industrialized countries. 1 The term nephrolithiasis is directly derived from Greek, nephros (kidney) and lithos (stone). The stone is a calculus of mineral or organic solids that can form anywhere in the urinary tract (urolithiasis) or more specifically in the ureter (ureterolithiasis). As the stone passes through the urinary tract, it can be eliminated uneventfully (asymptomatic crystalluria) or can obstruct urinary flow, causing “colicky” pain as it passes.
Renal colic is defined as severe intermittent flank pain that radiates to the groin, lower abdomen, or genitalia due to the passage of a stone through the urinary system. ( See Figure 1. ) Pain is often accompanied by nausea, vomiting, dysuria, and hematuria. A diagnosis of kidney stones can have a considerable influence on patient morbidity and healthcare costs. In a well-designed population-based data review, over 3.4 million urolithiasis patient encounters were identified from multiple national data sets, which estimated that urolithiasis had a cost of $2.1 billion per year, making it a significant health problem in the United States. 2

The acute treatment of kidney stones addresses not only adequate pain management but also focuses on the effects of partial or complete obstruction on the renal system and the time to passage of the stones. A key point in the evaluation of these patients is the need for and type of imaging study. Traditionally, these patients were evaluated with kidney, ureter, bladder (KUB) x-rays, ultrasound, or intravenous pyelogram (IVP) (excretory urography). However, the diagnostic study of choice is now noncontrast spiral CT.
In this issue of Emergency Medicine Practice , the current understanding of flank pain associated with urinary stone disease is discussed. The literature is reviewed regarding how and why stones are formed in the urinary system, what medications are best used to manage the pain and possibly enhance stone excretion, what studies can be used to evaluate the extent of disease, and what other diagnoses should be considered in patients presenting with flank pain.
Critical Appraisal Of The Literature
An extensive literature search through the National Library of Medicine’s PubMed database and review of existing guidelines was completed. The PubMed search was limited to English language clinical trials, meta-analyses, and practice guidelines over the last 10 years that included the Medical Subject Headings
(MeSH) of renal colic, flank pain, kidney calculi, or ureteral colic . This search yielded 211 articles; each of these was browsed for relevance to diagnosis and management in the hospital setting, and their references were reviewed. Relevant articles were then searched with the SciVerse Scopus database to identify additional citations of the articles. A search through The National Guideline Clearinghouse ( www.guideline.gov ) and The Cochrane Database of Systematic Reviews ( www.cochrane.org ) was also completed.
Epidemiology, Etiology, And Pathophysiology
Epidemiology.
The lifetime prevalence of kidney stone formation has been estimated at anywhere from 1% to 12%, with the probability of having a stone varying according to gender, race, age, and geographic location. 3,4 A population-based cross-sectional survey of 15,364 United States residents from 1976-1994 established a 5.2% prevalence of kidney stones, an increase from a prior prevalence of 3.8%. 5 These increasing numbers are likely due to better detection of stones due to the greater use and sensitivity of imaging studies such as the nonenhanced CT. Kidney stones typically affect men approximately 2 to 3 times more frequently than women. 2 Caucasians have the highest prevalence of kidney stones, followed by Hispanics, Asians, and Africans. 6 Incidence rates, defined as the onset of an individual’s first kidney stone, vary by age, sex, and race. For men, the incidence begins to rise after age 20 and peaks between ages 40 and 60. 1 Women have a bimodal incidence, with a second peak in incidence after age 60, believed to be due to the onset of menopause and the loss of the protective effect of estrogen. 4,7 Geographic distribution of kidney stone formation has been widely reported, with areas of hot or dry climates, such as desert or tropical areas, showing an increased prevalence. Soucie et al showed increased prevalence in the United States from north to south and west to east, with the highest prevalence being in the Southeast. 6 These studies, however, do not take into account genetic or dietary factors that may outweigh the effects of climate and geography.
There are many studies linking a particular factor to an increased risk of urinary stone formation, but no single factor can predict the likelihood of developing kidney stones. There is a general consensus that low fluid intake results in decreased urine production and a subsequent high concentration of stone-forming salts. The majority of research, however, has been focused on the unique characteristics of the different types of kidney stones, specifically calcium stones, struvite stones, and uric acid stones.
Calcium Stones
Calcium stones account for approximately 75% of all kidney stones. The most common abnormality found in patients with calcium stones is hypercalciuria. There are many medical conditions that lead to increased calcium levels, including hyperparathyroidism, 8 hypercalcemia of malignancy, 9 sarcoidosis, 10 and increased absorption of calcium from the gut, 11 among others. Medications such as thiazide diuretics have also been implicated in causing hypercalciuria. If a specific cause can be found, it can be addressed directly to prevent calcium stone formation; otherwise, it has been recommended to follow a low-salt, low-protein diet instead of a low-calcium diet, to prevent stone formation. 12
Struvite Stones
Struvite stones account for approximately 15% of all kidney stones. Formation of a struvite stone requires a combination of ammonia and alkaline urine. The ammonia is believed to come from the splitting of urea by urease, an enzyme produced by colonized bacteria. The most common urease-producing bacteria include Proteus, Klebsiella, Pseudomonas, and Staphylococcus. 13 Women or patients with anatomic abnormalities that predispose them to recurrent urinary tract infection are at an increased risk of developing struvite stones.
Uric Acid Stones
Uric acid stones account for approximately 6% of all kidney stones. Uric acid stone formation is influenced by low urine volume, low urinary pH, and hyperuricosuria, with low urine pH being the most important factor. 14 Even though the pathogenesis of low urine pH is multifactorial and not completely understood, recent research suggests that diabetes mellitus, obesity, and hypertension may be risk factors for the development of uric acid stones. 15,16
Pathophysiology
Urine is a metastable solution that contains many compounds and salts including calcium, oxalate, phosphate, and uric acid. Kidney stones form when urine becomes supersaturated with stone-forming salts. These salts precipitate out of solution and form crystals, which accumulate at anchoring sites to form a stone. ( See Figure 2. )

The concentrations of calcium, oxalate, and phosphate in urine makes it supersaturated, which would normally favor crystal formation. There are, however, inhibitory molecules in the urine that prevent
crystal formation by raising saturation levels needed for crystal formation and by reducing the rate of crystal growth and aggregation. Citrate has been shown to act as an inhibitor of both calcium phosphate and calcium oxalate stone formation. 17,18 Additionally, glycoprotein nephrocalin, Tamm-Horsfall
mucoprotein, and uropontin have been shown to inhibit crystal aggregation. 19-21 These inhibitory factors enable urine to become supersaturated before stone formation occurs.
The actual mechanism by which crystals aggregate and form stones once they have precipitated
out of solution is still not completely understood. There are several competing theories that have tried to explain this mechanism. One theory proposed by Miller et al argues that oxalate crystals damage the renal tubular epithelial cells, which in turn promotes adherence of the crystals to the epithelial cells. 22 Competing theories argue that crystals aggregate around plaque formations. Randall et al first observed plaque formations as a possible cause of renal calculi in 1937. 23 This theory has since been reexamined by Low et al, who showed that Randall’s plaques occurred in 74% of stone-formers compared to 43% of the control group. 24 Although the exact mechanism of stone formation is not understood, it can be thought of as a multifactorial process that involves the balance between high concentrations of stone-forming salts and insufficient inhibitory proteins.
The pain associated with urinary stone formation is classically called colic . This is defined as a severe intermittent or spasmodic pain typically beginning abruptly in the flank and increasing rapidly. It may also be steady and continuous, radiating to the abdomen and pelvis as the stone migrates distally. Autonomic nerve fibers serving the kidneys as well as the genital organs (testicle and ovary) are involved in pain transmission. Pain occurs due to stimulation of specialized nerve endings upon distention of the ureter, renal pelvis, or renal capsule. The location of the stone is thought to manifest a particular pattern of pain radiation. ( See Table 1. )

Each episode of pain is likely due to an stone acutely lodged in a new and more distal position in the ureter. Stones lodged in the ureter are typically found in 3 locations: the ureteropelvic junction, at the level of the iliac vessels, and the ureterovesical junction. ( See Figure 3. ) These stones also act as foreign bodies that precipitate further stasis and may lead to infection.

Differential Diagnosis
It is critical for the emergency clinician to differentiate acute flank pain caused by renal colic from other life-threatening conditions. ( See Table 2. ) It is suggested that at least half of patients with acute flank pain have no evidence of stone disease on CT, and an alternative diagnosis is often found. 25 A prospective chart review of 4000 CTs identified calculi in 28% of patients and an alternate cause of pain in 10%. 26 In another study, a review of 714 consecutive CT reports for patients presenting to an ED with acute flank pain who underwent renal stone protocol found that 455 had urolithiasis, whereas 259 were found to be without urinary stones. Significant alternate diagnoses were noted in 196 (27.4%). 27 The most common alternative diagnoses were cholelithiasis (5%), appendicitis (4%), pyelonephritis (3%), ovarian cyst (2%), renal mass (1.4%), and abdominal aortic aneurysm (AAA) with and without rupture (1.4%).
A number of disorders can cause flank pain, many of which are not associated with the urinary system. A complete differential diagnosis should consider causes of flank pain from the vascular, pulmonary, and gastrointestinal systems, among others.


Vascular Causes Of Flank Pain
Abdominal aortic aneurysm rupture and aortic dissection are catastrophic mimics that can cause flank pain. Bedside emergent ultrasound or unenhanced CT have some limitations in detecting dissection
and hemorrhage from a leaking aneurysm but may be used to detect aneurysm size, as size is the greatest predictor of which patients have the potential to rupture.
Pulmonary Causes Of Flank Pain
Pulmonary embolism and basilar pneumonia may present as acute flank pain because the lung bases approximate the area of the flank. Case reports exist for patients who underwent radiologic studies to detect a urinary tract stone, and findings were consistent with a pulmonary infarct secondary to an embolism. 28 Plain x-rays and CT scans can differentiate lung causes of acute flank pain.
Gastrointestinal Causes Of Flank Pain
Appendicitis may present with lower flank pain and can be identified by CT, which will show a fluid-filled appendix as well as findings suggestive of complications of acute appendicitis. Patients with colitis, bowel obstruction, biliary disease, and ulcers may also present with complaints of flank pain. A careful history, examination, and radiologic studies may make the differentiation.
Other Genitourinary Causes Of Flank Pain
Ectopic pregnancy and ovarian cyst/torsion must be considered along with other renal causes such as acute pyelonephritis, nephritic syndrome, papillary necrosis, and renal infarcts. Patients who present with persistent flank pain without secondary signs or evidence of calculus on CT should be scanned with contrast to rule out renal infarcts. 29
Prehospital Care
The prehospital care of a patient with acute flank pain secondary to calculus formation is primarily supportive. Because there are mimics carrying a significant mortality, providers may consider IV access and measures to alleviate excessive vomiting and pain. These should be considered especially in cases with long transport time.
Emergency Department Evaluation
Presenting history.
At triage, a patient complaining of flank pain may have a calculus, or it could be an AAA awaiting rupture. The initial evaluation of a patient with flank pain should include a complete medical history and physical examination to further differentiate kidney stones from more life-threatening diagnoses. Typical symptoms include restlessness (with the patient unable to find a position of comfort) or intermittent colicky flank pain with radiation to the lower abdomen or groin. This is often associated with nausea with or without vomiting, due to the obstruction of a hollow viscus (ureter). As the stone enters the ureter, there may be lower urinary symptoms such as dysuria, frequency, or urgency. It is important to remember that most calculi may not cause significant symptoms until they begin to descend in the urinary tract.
In a well-designed retrospective review of 235 patients, women and those with atypical symptoms and the absence of hematuria were shown to have increased length of stays, undergoing many additional
Past Medical History
Past medical history may include risk factors such as positive family history, hyperparathyroidism, renal tubular acidosis, diabetes, gout, and known anatomic anomalies such as single or horseshoe kidneys. A careful examination of medications may also increase the clinical suspicion of renal calculus. Known offenders include carbonic anhydrase inhibitors (topiramate), calcium-containing medications, and protease inhibitors such as indinavir or sulfadiazine.
Physical Examination
A complete physical examination should be conducted, beginning with vital signs. Special notice should be taken of a fever, as it may indicate occult infection. Due to the agonizing pain associated with an acute obstruction, patients may be tachycardic and tachypneic and appear pale, cool, and clammy. Hypotension or altered mental status may be indicative of urosepsis. There may be presence of acute costovertebral angle (CVA) tenderness or mild lower abdominal tenderness in some patients. Significant pain on palpation or rebound or guarding suggests a more serious intra-abdominal process and should be further investigated. The abdomen should be carefully palpated for tenderness or pulsation over the abdominal aorta. A complete genital examination should look for evidence of testicular or ovarian torsion,
epididymitis, or acute cervicitis/pelvic inflammatory disease.
Diagnostic Studies
Kidney stones represent a complex clinical problem. There are many factors to contemplate when considering what diagnostic tests should be ordered, eg, urinalysis, laboratory studies, and radiographic studies.
Urinalysis (UA) can be used to detect the presence of red or white blood cells, protein, and crystals. While microscopic hematuria in the presence of acute flank pain is highly suggestive of renal colic, stones may occur in the absence of blood. Other conditions such as ovarian masses, appendicitis, and diverticulitis may also result in hematuria due to an inflammatory process in close proximity to the ureter.
The UA has been found to be nonspecific, and false positives may occur in circumstances such as AAA, infection, or menses. 31 Luchs et al conducted a well-designed retrospective review of 950 patients that correlated urinalysis results in patients with suspected renal colic to findings on unenhanced helical
CT. 32 Their results showed the sensitivity (84%), specificity (48%), positive predictive value (72%), and negative predictive value (65%) of hematuria on microscopic urinalysis to be low, demonstrating that the presence or absence of blood on urinalysis is unreliable in determining which patients have kidney stones. While the UA is a complementary test that can be used to rule out infection, the presence or absence of red blood cells cannot be used to diagnose or exclude urolithiasis with a high degree of accuracy.
Laboratory Studies
A comprehensive metabolic evaluation is not cost-effective for all patients but should be considered in those with multiple recurrences, in pediatric patients, or in patients with significant risk factors.
These evaluations include an analysis of stone composition, 24-hour urine collections (volume, pH, urinary substrates), and a full electrolyte panel. Detailed metabolic evaluations are rarely indicated in the acute setting and should occur after the resolution of the acute event. 33
If “basic labs” are ordered, a leukocytosis may raise the suspicion for a renal or systemic infection, but in the absence of specific evidence-based recommendations, practice patterns relating to the routine use of complete blood counts (CBCs) are difficult to evaluate objectively. An assessment of renal function (blood urea nitrogen [BUN], creatinine) is warranted and may help in determining which radiologic study is ordered.
Radiographic Studies
Imaging plays a major role in the diagnosis and management of patients with acute and chronic urolithiasis, but controversy exists regarding when imaging is required and what type of imaging should be selected. Calculi composition, divided into calcareous (calcium-containing) and noncalcareous, can often dictate radiologic study selection when this information is known. ( See Table 3. ) When stone composition is unknown, however, the clinician must decide which radiographic study to order: KUB x-ray, IVP, ultrasound, or nonenhanced helical CT.

Kidney/Ureter/Bladder X-ray
Abdominal radiography of the kidney, ureter, and bladder was often used as the first step in the radiographic workup of patients with flank pain. ( See Figure 4. ) Although about 75% of stones are calcium-based and should be visible on plain film, due to varying radiographic technique and other factors,
only about 60% are found to be visible on plain films. The KUB can aid in the detection of a calcified stone, determine its location and size, and provide an assessment of bowel gas patterns and fecal debris. A study by Levine and colleagues reviewed 178 patients with acute flank pain, finding KUBs with a sensitivity of 45% to 59% and specificity of 77% in the detection of urinary tract calculi. 34 With such low sensitivities and specificities, the KUB alone is insufficient in detecting kidney stones and should always be paired with another imaging modality such as ultrasound. If a stone has previously been shown to be radio-opaque, some clinicians advocate the use of KUB in following the stone’s progression through the urinary tract.

Intravenous Pyelogram
The use of plain abdominal radiographs combined with IV urography was first described in 1923 and was the standard imaging modality for many years. Calculi are identified by their intraureteral location, and the filling defect is noted with the contrast. ( See Figure 5. ) The IVP is still used in some institutions
without availability of sonogram or CT and it is able to demonstrate the anatomy of the entire urinary tract. In a prospective study by Pfister et al in 2003, its sensitivity was 94.2% and specificity was 90.4%, which was within 5% of the results for CT. 35 The IVP assists in identification of anatomical abnormalities
of the collecting system and may detect ureteral tumors. In addition, IVP gives a rough estimation
of renal function, the degree of obstruction, and the location of calculi. Its limitations, however, have been well-documented, including its implication in contrast-induced reactions and nephrotoxicity. Although IVP was the gold standard for many years, its use has now fallen out of favor with the advent of newer imaging modalities.

Ultrasonography
Ultrasonography is the modality of choice in those who should avoid radiation (ie, pregnant patients and children). As a bedside procedure, it can often be performed quickly to look for evidence of the stone itself or for hydronephrosis as a secondary sign of the presence of a stone. 36 The stone will typically be seen as a hyperechoic structure with posterior shadowing. ( See Figure 6 .) A prospective study of 318 patients evaluating the usefulness of sonography as an initial tool in patients suspected of having kidney stones noted ultrasound has a sensitivity of 98.3% and specificity of 100%. 37 The sensitivity and specificity will vary, however, with differing equipment, skill of the operator, and patient body habitus. Additionally, in the absence of renal calculi or hydronephrosis, sonography has a limited role in diagnosis of alternate pathologies. The use of ultrasound in special populations has an American College of Radiology Appropriateness Criteria of 6 out of 10 for acute-onset flank pain and 7 for recurrent symptoms of disease. 38

Non-Enhanced Helical Computed Tomography
Non-contrast helical CT has supplanted conventional radiography and IVP in the evaluation of patients with suspected lithiasis. ( See Figure 7 .) It was introduced into clinical practice in 1989 when a single breath-hold resulted in images obtained by the helical path of the x-ray focus. The suggested CT scan window is the upper border of the body of T12 to the inferior border of the symphysis pubis using 5-mm or less cuts. 26,39 Some studies note varying section widths, such as 1.5 mm and 2.5 mm, in order to detect smaller calculi less than 3 mm. 40 It has been reported in comparative and observational studies that the unenhanced CT has a sensitivity of 94% to 100% and specificity of 92% to 100% in evaluating urinary and non-urinary flank pain. 41,42 Helical CT has the advantage of diagnosing nephrolithiasis when the stone has passed, which is missed by IVP. 43 Its sensitivity and specificity approach 100%, 44 making it the diagnostic modality of choice, when available. Computed tomography also has the added benefit of being able to make alternate diagnoses in these patients.

Several articles commented on secondary or indirect signs of calculus disease in the renal system
as visualized on CT. 42,44 These secondary signs include: perinephric stranding, ureteral dilatation, perinephric fluid, collecting system dilatation, periureteral stranding, and nephromegaly. Secondary
signs are indicative of a localized inflammatory reaction or irritation caused by the presence or passing of ureteral stones or other acute urinary obstruction. These indirect signs are thought to follow a well-defined time course corresponding to the physiologic changes caused by an acutely obstructing stone. The peak time of appearance of these secondary signs is reported to be 6 to 8 hours following obstruction, based on a study of 227 patients with stone diagnosis on CT. 44 These secondary signs increase in frequency as the duration of flank pain increases. Based on these findings, sensitivity of CT scanning may be higher during this window, 6-8 hours after onset of pain.
Despite their usefulness, CT scans are not without limitations. Because CT scans expose the patient to significant amounts of radiation and come at a considerable expense, the question can be posed: does every patient suspected of having kidney stones need a CT? A reasonable approach recommended by many clinicians is to use CT scans for initial episodes of kidney stones or if the diagnosis is unclear. 43 In contrast, Lindqvist et al performed a prospective randomized study of 686 patients and found that in patients that had complete resolution of pain with parenteral analgesics, immediate imaging with CT did not lead to reduced morbidity when compared to CT imaging done 2-3 weeks later. 45 The decision to order a CT, then, will depend on the patient characteristics and diagnostic comfort of the clinician.
Imaging Summary
Over the last several years, the diagnostic algorithm for flank pain suggestive of renal calculus has changed. For many years, IVP was the gold standard. In 1992, it was suggested that it be replaced by a KUB plain film and ultrasound. In 1993, it was suggested that the KUB and ultrasound be followed by an IVP for equivocal cases. Now, CT is the standard imaging modality, with sensitivities and specificities
approaching 100%. While CT has been found to be the most accurate technique, the combination KUB/ultrasound is an alternative with a lower sensitivity and radiation dose with good practical value. The American College of Radiology Appropriateness Criteria summarizes their recommendations for imaging in patients suspicious for stone disease and those with recurrent symptoms.38 ( See Table 4 .)

Traditionally, parenteral narcotics had been used as primary therapy for renal colic, but several studies have shown the benefits of NSAIDs, (ie, ketorolac and diclofenac) in relieving pain through prostaglandin-mediated pain pathway inhibition and decreased ureteral contractility. Caution must be observed in patients with preexisting renal insufficiency or other contraindications to NSAIDs. A Cochrane review noted that both NSAIDs and opioids can significantly relieve the pain in acute renal colic, but opioids cause more adverse effects. 46 This conclusion resulted from 20 trials in 9 countries with a total of 1613 participants. On the other hand, Safdar et al conducted a prospective double-blinded randomized controlled trial of 130 patients who presented with a clinical diagnosis 2011of acute renal colic. The patients were treated with morphine, ketorolac, or both, and it was found that a combination of morphine and ketorolac offered superior pain relief to either drug alone. 47
Clinical practice has often suggested that the use of high-dose fluids improved outcomes in patients with acute ureteral colic. An early, small study by Pak et al quantitatively assessed the effect of urinary dilution on the crystallization of calcium salts. It concluded that urinary dilution was achieved in vitro by the addition of water in amounts of 1-2 liters per day. 48 A remote prospective 5-year study of 300 patients with idiopathic calcium stone disease concluded that a large water intake results in a strong reduction of supersaturations, thus preventing recurrences. 49 A 2010 Cochrane review found no evidence for the use of fluids or diuretics for the treatment of acute ureteral colic. 50 A trial of 60 patients compared no fluids for 6 hours versus 3 liters of IV fluids over 6 hours and found no significant difference in pain at 6 hours, surgical stone removal, or manipulation by cystoscopy. 50 Therefore, the authors concluded that acute hydration has no evidence-based benefits. The earlier studies do, however, support the use of increased fluid intake to prevent recurrences of stone formation.
Some clinicians advocate the use of antimuscarinic agents, such as hyoscine butylbromide, in the treatment of kidney stones, with the belief that it may provide analgesia by inducing smooth-muscle relaxation and decreasing ureteral spasms. Holdgate et al conducted a prospective randomized
trial of 192 patients with a clinical diagnosis of acute renal colic who received morphine with and without hyoscine butylbromide. 51 They found no evidence that hyoscine butylbromide reduced opioid requirements in acute renal colic, suggesting that antimuscarinic agents should not be a part of a standard treatment regimen.
Clinically stable patients are typically given oral analgesics to treat the outpatient spontaneous passage of their kidney stones. These patients should have well-controlled pain, be without evidence of complete obstruction with hydronephrosis, have an adequate renal function reserve, and be tolerating fluids by mouth without difficulty. It is thought that most ureteral calculi smaller than 5 mm will pass spontaneously, typically within 4 weeks after the onset of symptoms. It is known that the rate of stone passage decreases as size of the stone increases. Stones larger than 7 mm may require surgical intervention. Definitive surgical treatment options include shock wave lithotripsy, ureteroscopy, or percutaneous nephrolithotomy, all of which are assessed by a urologist. Candidates for surgical management include those with persistent obstruction, failure of stone progression, or increasing or unremitting colic. 52
Special Circumstances
The diagnosis of kidney stones during pregnancy can be a challenge due to physiologic changes during
pregnancy and imaging limitations. Approximately 90% of pregnant women develop unilateral or bilateral ureteral obstruction by the third trimester, although this obstruction is asymptomatic in the majority of cases. 53 Physiologic dilation of the renal calices, pelvis, and ureter often begin in the first nettrimester, and pregnancy-induced hydronephrosis is the most common cause of dilation of the urinary tract in pregnancy and may mimic colic. 53 Establishing an accurate diagnosis calls for weighing radiation exposure to the fetus against potential complications of delayed diagnosis (infection, premature labor, renal pathology). Abdominal ultrasound should be attempted, including color Doppler ultrasound. Computed tomography is unsuitable for routine use in pregnancy, though the risk versus benefit options need to be considered.
Patients with recurrent symptoms present a clinical challenge. The likelihood of calculus as the cause of flank pain is higher, but the risks and benefits of repeated radiation exposure must be taken into consideration. A well-designed 6-year study of 5564 CTs performed for renal colic found that 96% of patients underwent 1 or 2 studies, 4% had 3 or more, and 1 patient had 18 CTs during the study period. 54 This study suggests that patients with a history of kidney stones are at an increased risk of repeat CTs and the accumulation of high-dose radiation. Although a CT may be indicated for a patient with recurrent symptoms, it should be considered judiciously.
Pediatric Patients
The formation of stones in children is dependent upon the same metabolic and anatomic factors as in adults, with the presence of infection as a contributing cause. Several differences apply to 2011kidney stones occurring in the pediatric population. ( See Table 5. ) In contrast to the adult population, boys and girls are equally affected by kidney stones. The clinical presentation is thought to be age-specific, with the typical flank pain and hematuria being more common in older children. Younger children may only show nonspecific signs of irritability and vomiting.

Pediatric patients with urinary stones are considered to be a high-risk group for developing recurrent stones. In a 2008 guideline published by the European Society for Paediatric Urology ( www.espu.org ), it was recommended that every child with a urinary stone have an outpatient full metabolic workup. 55 This workup should include a family and patient history, analysis of stone composition, a 24-hour urine collection, and blood work that may include electrolytes, BUN, creatinine, calcium, phosphorus, uric acid, albumin, and parathyroid hormone. Generally, ultrasonography should be used as a first study. Many radio-opaque stones can be identified with a simple abdominal flat-plate or KUB film. The IVP is rarely used in children. If no stone is identified but symptoms persist, a spiral CT scan is indicated.
Controversies/Cutting Edge
Intravenous contrast in the management of flank pain.
Contrast may be used in the identification of pyelonephritis or in renal or vascular conditions (tumor, mass, or cysts). The contrast is used to document stone density, location in the ureter, or other extrarenal urinary etiologies. It should be considered in the presence of secondary signs on CT without evidence of a stone.
The Cumulative Effect Of Repeat Computed Tomography Scans
Many kidney stone patients are young and undergo multiple examinations through their disease progression. A study of 356 patient encounters revealed a mean number of 2.5 scans per patient, with 10% having 5 or more scans during the study period of 10 months. 55 This study also concluded that many emergency clinicians rely on the diagnostic value of CT scans but with a limited familiarity with the potential hazards of CT-related radiation exposures. According to a 2001 report from the International Commission on Radiological Protection, a single abdominal/pelvic CT scan for suspected renal colic exposes the patient to 15 mSv. 56 Most of the data for human cancer rates caused by radiation are based on data for people exposed to the Hiroshima or Nagasaki atomic bombs or other nuclear events. It is unknown whether such data can be extrapolated to patients undergoing CT, but consideration should be given to the cumulative radiation dose of patients undergoing multiple CTs.
While CT is proven the better study in terms of diagnostic accuracy (calculus and/or secondary signs) and the identification of other diagnoses, the availability of CT in all institutions as well as the amount of radiation exposure to patients are valid concerns. Two paths have been suggested: (1) using KUB/ultrasound followed by CT if the results are negative, and (2) using CT only if there is strong suspicion of a major colic event. 35
Stones That Cannot Be Detected By Computed Tomography
Crystal deposits formed as a result of pure protease inhibitors such as indinavir are not visible on CT 2011scans. A small but well-designed 3-month study of 6 patients taking 2400 mg of indinavir reported that the calculi formed from indinavir had an attenuation that is the same or slightly higher than that of soft tissue, rendering it undetectable or barely detectable on unenhanced CT. 58 A patient with a history of use of this drug who presents with acute symptoms and secondary signs of obstruction should have a presumed diagnosis of a drug-induced stone and be managed accordingly.
Medical Expulsive Therapy
Several drugs have been suggested to enhance the spontaneous passage of ureteral calculi. These include calcium-channel blockers, steroids, and alpha-adrenergic blockers. A 2005 prospective randomized study of 210 patients compared a corticosteroid in combination with phloroglucinol, tamsulosin, or nifedipine and found that tamsulosin and a corticosteroid was the most efficacious combination. This combination resulted in stones being passed more quickly and a reduced need for analgesics. 59
Steroids are always a controversial issue. True, steroids could reduce inflammation in the urinary tract caused by a kidney stone, but are the steroids a necessary component in medical expulsive therapy (MET)? Singh et al conducted a meta-analysis of 16 studies using alpha-antagonists and 9 studies using
a calcium-channel blocker for MET and found that both drugs augmented stone expulsion rates. 60 A subgroup analysis of these trials, using adjunct medications such as steroids and antibiotics, yields a similar improvement in expulsion rates. 60 This meta-analysis seems to suggest that calcium-channel blockers or alpha-antagonists, used alone, improve expulsion rates and medications like steroids may be useful as an adjunct therapy.
The Economic Impact Of Patients With Kidney Stones In The Emergency Department
Costs and ED lengths of stay were found to be higher with stones larger than 5 mm. A retrospective
review of 574 patients in a 36,000-volume ED concluded that this likely reflected the recalcitrant nature of the pain, longer time to achieve pain control, and complications. 61 On average, the time for CT was 5-15 minutes versus KUB/ultrasound which required 20-40 minutes. 62 The indirect costs of managing these patients is higher for those receiving IVP due to room-occupation time, preparation time for contrast, and potential management of contrast-induced complications. Protocols that include the KUB/ultrasound combination are cheaper, though time-to-diagnosis is longer than that with CT alone.
Disposition
Some kidney stone patients may require admission to the hospital. ( See Table 6. ) For the remainder of patients, clear and specific discharge instructions are essential. Patients should be advised to follow up with a urologist. Although it is not the primary responsibility of the emergency clinician to determine the cause of a patient’s stones or to initiate preventive measures during acute renal colic, the patient should be educated on the availability of preventive testing and treatments.

Renal colic is one of the most severe pain syndromes commonly diagnosed and managed in the ED. While the morbidity and mortality of urolithiasis is relatively low in comparison to other conditions, these patients need to be assessed quickly for potential life-threatening mimics. In addition, they need to receive appropriate control of nausea and vomiting as well as appropriate and judicious use of analgesics. Patients who have good pain control with fluids and analgesics may be managed clinically, and imaging may not be necessary. Patients with persistent pain, concern for infection, or questionable clinical presentation should be imaged to enhance the diagnostic certainty and to rule out other etiologies of flank pain. While there is some controversy regarding the algorithm, patients may be evaluated with the KUB followed by ultrasound imaging; however, if available, CT is considered a better alternative due to its diagnostic accuracy, speed, and ability to identify alternate diagnoses. In the absence of a large stone, complete obstruction, renal failure, or sepsis, many of these patients may safely await spontaneous passage of the calculi.
Additional Resources
• American Urological Association Foundation: www.auafoundation.org , www.urologyhealth.org
• National Kidney Foundation: www.kidney.org
• Oxalosis and Hyperoxaluria Foundation: www.ohf.org
• International Kidney Stone Institute: www.iksi.org
• National Institute of Diabetes and Digestive and Kidney Disease (NIDDK) Information Clearinghouse:
www.kidney . niddk.nih.gov
Time- And Cost-Effective Strategies For Renal Calculi
If a specific etiology of calcium calculi can be identified (ie, hyperparathyroidism, hypercalcemia of malignancy, sarcoidosis, or increased calcium absorption from the gut), it can be addressed directly to prevent stone formation. However, if the cause is idiopathic, a low-salt, low-protein diet is preferred to a low-calcium diet.
- Patients with atypical symptoms often undergo unnecessary additional testing, increasing their length of stay and healthcare costs. Women, patients with atypical symptoms (such as the lack of nausea and vomiting, radiation of pain, and urinary symptoms), and patients without hematuria were found to have increased length of stays, undergoing many additional tests. Understanding that not all renal stones cause urinary symptoms and hematuria could reduce the need for additional tests and costs.
- A comprehensive metabolic evaluation is not cost-effective for all patients with urolithiasis. While not cost-effective for all patients with urolithiasis, a comprehensive metabolic evaluation should be considered for those patients with multiple recurrences, in pediatric patients, or in patients with significant risk factors. One international guideline recommended that every child with a urinary stone have a full outpatient metabolic workup. 54 The workup should include a family and patient history, analysis of stone composition, 24-hour urine collections, and a full electrolyte panel.
This method will save the patient from further CT radiation and reduce healthcare costs. Unfortunately, it is only applicable in patients with radio-opaque calculi. If the KUB is not diagnostic, a more sensitive imaging modality should be utilized.
- High-dose IV fluids are often suggested to improve outcomes in patients with acute renal colic. However, a prospective trial found no difference in the IV hydration cohort’s pain scale at 6 hours. 49 In the nonacute setting, urinary dilution can be achieved by the addition of 1-2 liters per day orally, which reduces crystallization of calcium salts and supersaturations, thereby preventing recurrences.
- Costs and ED lengths of stay that were found to be higher with stones larger than 5 mm were attributed to persistent pain, longer time period to achieve pain control, and complications. 57 Appropriate weight-based medication dosing should be administered early to hasten resolution of symptoms. Urologists should be consulted to ensure prompt follow-up for patients with renal calculi larger than 5 mm to facilitate curative surgical manipulation.
Risk Management Pitfalls For Renal Calculi
A negative UA for microscopic blood does not exclude urolithiasis. Similarly, a positive UA with red blood cells does not diagnose renal colic.
- “I was sure a renal calculus was the cause of the patient’s radiating pain, nausea, vomiting, and dysuria, but the CT of her abdomen and pelvis was negative for a kidney stone.” All stones are not visible on CT. Crystal deposits formed as a result of pure protease inhibitors such as indinavir are not appreciated on CT scans. Additionally, calculi smaller than 3 mm can be difficult to detect. If the history fits, treat as a drug-induced stone.
- “I discharged the elderly man with a previous medical history of hypertension and diabetes after he presented with severe right flank pain and microscopic hematuria. I performed a bedside ultrasound to rule out AAA and diagnosed urolithiasis. He returned to the ER 1 day later with a perforated appendicitis.” The most common alternative diagnoses of renal colic are cholelithiasis (5%), appendicitis (4%), pyelonephritis (3%), ovarian cyst (2%), and abdominal aortic aneurysm with and without rupture (1.4%). Additionally, inflammatory and infectious conditions can cause hematuria. Misdiagnosing older patients with urolithiasis can greatly increase their morbidity and mortality.
- “I assumed that my 70-year-old patient was tachycardic because of the pain from her kidney stone. She was 99.9°F orally so I didn’t bother to check a rectal temperature. I was surprised to learn that she returned with urosepsis.” Elderly febrile patients should be admitted and urology consulted. Although pain can cause tachycardia, a further workup should be initiated. Elderly patients with fever can develop altered mental status and hypotension and decompensate quickly.
A complete genital examination should be performed in patients with symptoms suggestive of renal colic. Testicular or ovarian torsion can present very similarly. Epididymitis, acute cervicitis, or pelvic inflammatory disease can also be confused with kidney stones. Remember to conduct a complete history and physical examination even if patients report similar symptoms previously and that opioids were curative.
- “I ordered an analysis of the stone composition, 24-hour urine collections (volume, pH, urinary substrates), and a full electrolyte panel for my 30-year-old patient who presented with renal colic for the first time.” A detailed metabolic evaluation is not cost-effective and is rarely indicated in the acute setting. An assessment of renal function (blood urea nitrogen and creatinine) is warranted, but further laboratory testing should be done only if indicated.
- “The majority of stones are calcium-based, so I just ordered a KUB to rule out urolithiasis.” While 70% to 75% of all stones are calcareous and radio-opaque, only 60% are visible on plain films. KUBs have a sensitivity of 45% to 59% and specificity of 77% in detecting urinary tract calculi. Thus, utilizing KUBs alone is insufficient to diagnose renal colic; KUBs should always be paired with another imaging modality.
- “A 12-week pregnant woman presented with severe right flank pain which radiated to her right lower quadrant with right costovertebral angle tenderness. It probably was renal colic, but because of the potential morbidity, I obtained a CT to make sure it wasn’t appendicitis.” Ultrasonography is the modality of choice in pregnant patients and children. The calculus itself can be seen or secondary signs of the stone such as hydronephrosis can often be visualized. Ultrasound has a reported sensitivity of 98% and a specificity of 100%, although it is dependent on the skill of the operator, adequacy of the equipment, and patient body habitus. A CT might be unavoidable for this patient; however, other modalities should be explored first.
- “My 60-kg patient with renal colic still had pain after 6 mg of morphine. I administered another 6 mg, but then she developed respiratory depression and had to be bagged.” Non-steroidal anti-inflammatory drugs relieve acute renal colic pain through prostaglandin-mediated pathways and decreased ureteral contractility. In addition, NSAIDs cause fewer adverse effects than opioids. A combination of morphine and ketorolac offers superior pain relief than either drug alone.
- “I thought his 7-mm stone would pass spontaneously and didn’t think he needed urology follow-up.” Most ureteral calculi smaller than 5 mm will pass spontaneously, typically within 4 weeks from symptom onset. Larger stones will take longer to pass. Stones larger than 7 mm usually require surgical intervention, so emergent urologic consultation is needed.
Case Conclusion
The reason your chairman wanted to see you is because less than 24 hours later, the patient you discharged came back to the ED in severe pain, febrile, vomiting, and very displeased that he had to return. A nonenhanced abdomen and pelvic CT revealed a 6-mm right ureteral stone with significant hydroureter and hydronephrosis. He was subsequently admitted to the urology service for hydration, pain management, and definitive treatment. The chairman reminded you that urine negative for blood does not rule out the presence of a calculus.
The HIV patient with back pain was medicated with ketorolac, promethazine, and IV fluids. Her labs noted a WBC count of 12, with a urinalysis positive for leukocytes and RBCs (3 per hpf). Her CT demonstrated some periureteral stranding and mild hydroureter but no evidence of a stone. Further investigation revealed that she was on indinavir, and she was properly treated for a drug-induced stone.
When you checked on the patient with abdominal pain whom you had signed out to a colleague, you found that she improved greatly with the morphine and had a fairly unremarkable KUB. A sono tech was called in, but the second physician had become busy and did not have an opportunity to reexamine her. Later, in the ultrasound suite, the patient complained of worsening abdominal and flank pain. The astute sono tech scanned her aorta and she was found to have an AAA.
Tables and Figures

Evidence-based medicine requires a critical appraisal of the literature based upon study methodology
and number of subjects. Not all references are equally robust. The findings of a large, prospective, randomized, and blinded trial should carry more weight than a case report.
To help the reader judge the strength of each reference, pertinent information about the study, such as the type of study and the number of patients in the study, will be included in bold type following the reference, where available.
- 1. Hiatt RA, Dales LG, Friedman GD, et al. Frequency of urolithiasis in a prepaid medical care program. Am J Epidemiol. 1982;115:255-265. (Epidemiologic study of over 200,000 patient questionnaires)
- Pearle MS, Calhoun EA, Curhan GC. Urologic diseases in America project: urolithiasis. J Urol. 2005;173:848-857. (Population-based data review)
- Sierakowski R, Finlayson B, Landes RR, et al. The frequency of urolithiasis in hospital discharge diagnoses in the United States. Invest Urol. 1978;15(6):438-441.
- Johnson CM, Wilson DM, O’Fallon WM, et al. Renal stone epidemiology: a 25-year study in Rochester, Minnesota. Kidney Int. 1979;16(5):624-631.
- Stamatelou KK, Francis ME, Jones CA, et al. Time trends in reported prevalence of kidney stones in the United States: 1976-1994. Kidney Int. 2003;63(5):1817-1823.
- Soucie JM, Thun MJ, Coates RJ, et al. Demographic and geographic variability of kidney stones in the United States. Kidney Int. 1994;46(3):893-899.
- Nordin BE, Need AG, Morris HA, et al. Biochemical variables in pre- and postmenopausal women: reconciling the calcium and estrogen hypotheses. Osteoporosis Int. 1999;9(4):351-357.
- Parks J, Coe F, Favus M. Hyperparathyroidism in nephrolithiasis. Arch Intern Med. 1980;140(11):1479-1481.
- Burtis WJ, Brady TG, Orloff JJ, et al. Immunochemical characterization of circulating parathyroid hormone-related protein in patients with humoral hypercalcemia of cancer. N Engl J Med. 1990;322(16):1106-1112.
- Bell NH, Stern PH, Pantzer E, et al. Evidence that increased circulating 1 alpha, 25-dihydroxyvitamin D is the probable cause for abnormal calcium metabolism in sarcoidosis. J Clin Invest. 1979;64(1):218-225.
- Breslau NA, Preminger GM, Adams BV, et al. Use of ketoconazole to probe the pathogenetic importance of 1,12-dihydroxyvitamin D in absorptive hypercalciuria. J Clin Endocrinol Metab. 1992;75(6):1446-1452.
- Borghi L, Schianchi T, Meschi T, et al. Comparison of two diets for the prevention of recurrent stones in idiopathic hypercalciuria. N Engl J Med. 2002;346(2):77-84.
- Griffith DP, Osborne CA. Infection (urease) stones. Miner Electrolyte Metab. 1987;13(4):278-285.
- Pak CY, Sakhaee K, Moe O, et al. Biochemical profile of stone-forming patients with diabetes mellitus. Urology. 2003;61(3):523-527.
- Pak CY, Poindexter JR, Adams-Huet B, et al. Predictive value of kidney stone composition in the detection of metabolic abnormalities. Am J Med. 2003;115(1):26-32.
- Sakhaee K, Adams-Huet B, Moe OW, et al. Pathophysiologic basis for normouricosuric uric acid nephrolithiasis. Kidney Int. 2002;62(3):971-979.
- Meyer JL, Smith LH. Growth of calcium oxalate crystals. II. Inhibition by natural urinary crystal growth inhibitors. Invest Urol. 1975;13(1):36-39.
- Nicar MJ, Hill K, Pak CY. Inhibition by citrate of spontaneous precipitation of calcium oxalate in vitro. J Bone Miner Res. 1987;2(3):215-220.
- Nakagawa Y, Ahmed M, Hall SL, et al. Isolation from human calcium oxalate renal stones of nephrocalcin, a glycoprotein inhibitor of calcium oxalate crystal growth. Evidence that nephrocalcin from patients with calcium oxalate nephrolithiasis is deficient in gamma-carboxyglutamic acid. J Clin Invest. 1987 Jun;79(6):1782-1787.
- Hess B, Nakagawa Y, Parks JH, et al. Molecular abnormality of Tamm-Horsfall glycoprotein in calcium oxalate nephrolithiasis. Am J Physiol. 1991;260(4 Pt 2):F569-578.
- Shiraga H, Min W, VanDusen WJ, et al. Inhibition of calcium oxalate crystal growth in vitro by uropontin: another member of the aspartic acid-rich protein superfamily. Proc Natl Acad Sci USA. 1992;89(1):426-430.
- Miller C, Kennington L, Cooney R, et al. Oxalate toxicity in renal epithelial cells: characteristics of apoptosis and necrosis.
- Toxicol Appl Pharmacol. 2000;162(2):132-141. Randall A. The origin and growth of renal calculi. Ann Surg. 1937;105:1009-1027.
- Low RK, Stoller ML. Endoscopic mapping of renal papillae for Randall’s plaques in patients with urinary stone disease. J Urol. 1997;158(6):2062-2064.
- Talner L, Vaughn M. Nonobstructive renal causes of flank pain: findings on noncontrast helical CT (CT KUB). Abdom Imaging. 2003; 28:210-216. (Chart review)
- Ather MH, Faizullah K, Achakzai I, et al. Alternate and incidental diagnoses on noncontrast-enhanced spiral computed tomography for acute flank pain. Urol J. 2009;6(1):14-18. (Chart review; 4000 reports)
- Koroglu M, Wendel JD, Ernst RD, et al. Alternative diagnoses to stone disease on unenhanced CT to investigate acute flank pain. Emerg Radiol. 2004;10:327-333. (Chart review; 714 patients)
- Amesquita M, Cocchi MN, Donnino MW. Pulmonary embolism presenting as flank pain: A case series. J Emerg Med. 2009; 20(10); 1-4. (Case reports; 3 patients)
- Tsai SH, Chu SJ, Chen SJ. Persistent flank pain without active urinary sediments. Emerg Med J. 2007; 24(6):448. (Case studies; 44 patients)
- Serinken M, Karcioglu O, Turkcuer I, et al. Analysis of clinical and demographic characteristics of patients presenting with renal colic in the emergency department. BMC Res Notes. 2008; 1:79. (Retrospective study; 235 patients)
- Bove P, Kaplan D, Dalrymple N, et al. Reexamining the value of hematuria testing in patients with acute flank pain. J Urol. 1999;162(3 pt 1):685-687. (Chart review; 267 patients)
- Luchs JS, Katz DS, Lane MJ, et al. Utility of hematuria testing in patients with suspected renal colic: correlation with unenhanced helical CT results. Urology. 2002;59:839-842.
- Parks JH, Goldfisher E, Asplin JR, et al. A single 24-hour urine collection is inadequate for the medical evaluation of nephrolithiasis. J Urol. 2002;167(4):1607-1612. (Observational study; 1142 patients)
- Levine JA, Neitlich J, Verga M, et al. Ureteral calculi in patients with flank pain: correlation of plain radiography with unenhanced helical CT. Radiology. 1997;204(1):27-31. (Retrospective review; 178 patients)
- Pfister SA, Deckart A, Laschke S, et al. Unenhanced helical computed tomography vs intravenous urography in patients with acute flank pain: accuracy and economic impact in a randomized prospective trial. Eur Radiol. 2003;13(11):2513-2520. (Prospective study; 122 patients)
- Gaspari R, Horst K. Emergency ultrasound and urinalysis in the evaluation of flank pain. Acad Emerg Med. 2005;12:1180-1185. (Prospective observational; 104 patients)
- Park SJ, Yi BH, Lee HK, et al. Evaluation of patients with suspected ureteral calculi using sonography as an initial diagnostic tool: how can we improve diagnostic accuracy? J Ultrasound Med. 2008; 27:1441-1450. (Prospective study; 318 patients)
- Baumgarten DA, Francis IR, Casalino DD. Expert Panel on Urologic Imaging. ACR appropriateness criteria® acute onset flank pain - suspicion of stone disease. [online publication]. Reston (VA): American College of Radiology (ACR); 2008. (Practice guideline)
- Türkbey B, Akpinar E, Ozer C, et al. Multidetector CT technique and imaging findings of urinary stone disease: an expanded review. Diag Interv Radiol. 2010; 16:134-144. (Expanded review)
- Jin DH, Lamberton GR, Broome DR, et al. Renal stone detection using unenhanced multidetector row computerized tomography – does section width matter? J Urol. 2009;181(6):2767-2773. (Cadaver study; 14 samples)
- Tamm EP, Silverman PM, Shuman WP. Evaluation of the patient with flank pain and possible ureteral calculus. Radiology. 2003;228(2):319-329. (Clinical radiologic review)
- Gottlieb RJ, La TC, Erturk EN, et al. CT in detecting urinary tract calculi: influence on patient imaging and clinical outcomes. Radiology. 2002;225(2):441-449. (Retrospective chart review; 867 patients)
- Ha M, MacDonald RD. Impact of CT scan in patients with first episode of suspected nephrolithiasis. J Emerg Med. 2004; 27(3):225-231. (Prospective and observational study; 365 patients)
- Varanelli MJ, Coll DM, Levine JA, et al. Relationship between duration of pain and secondary signs of obstruction of the urinary tract on unenhanced helical CT. AJR Am J Roentgenol. 2001;177:325-330. (Prospective; 227 patients)
- Lindqvist K, Hellström M, Holmberg G, et al. Immediate versus deferred radiological investigation after acute renal colic: a prospective randomized study. Scand J Urol Nephrol. 2006;40(2):119-124.
- Holdgate A, Pollock T. Systematic review of the relative efficacy of nonsteroidal anti-inflammatory drugs versus opioids for acute renal colic. BMJ. 2004;328(7453):1401. (Guideline review)
- Safdar B, Degutis LC, Landry K, et al. Intravenous morphine plus ketorolac is superior to either drug alone for treatment of acute renal colic. Ann Emerg Med. 2006;48(2):173-181.
- Pak CY, Sakhaee K, Crowther C, et al. Evidence justifying a high fluid intake in treatment or nephrolithiasis. Ann Intern Med. 1980;93(1): 36-39.
- Borghi L, Meschi T, Amato F, et al. Urinary volume, water and recurrences of idiopathic calcium nephrolithiasis: a 5-year randomized prospective study. J Urol. 1996;155(:3)839-843. (Randomized prospective study; 300 patients)
- Worster A, Richards C. Fluids and diuretics for acute ureteric colic. Cochrane Database Syst Rev. 2005;3:CD004926. (Guideline review)
- Holdgate A, Oh CM. Is there a role for antimuscarinics in renal colic? A randomized controlled trial. J Urol. 2005;174(2):575.
- Preminger GM, Tiselius HG, Assimos DG. 2007 guideline for the management of ureteral calculi. J Urol. 2007;178(6):2418-2134. (Guideline)
- Lifshitz DA, Lingeman JE. Ureteroscopy as a first-line intervention for ureteral calculi in pregnancy. J Endourol. 2002;16(1):19-22.
- Katz SI, Saluja S, Brink JA, et al. Radiation dose associated with unenhanced CT for suspected renal colic: impact of repetitive studies. AJR Am J Roetgenol. 2006;186(4):1120-1124.
- Tekgül S, Reidmiller H, Gerharz E, et al. Guidelines on paediatric urology. European Association of Urology and European Society for Paediatric Urology. Retrieved 5/22/11: http://www.uroweb.org/fileadmin/user_upload/Guidelines/Paediatric%20Urology.pdf
- International Commission on Radiological Protection. ICRP 2001 annual report. Available at: http://www.icrp.org/docs/2001_Ann_Rep.pdf. Accessed June 10, 2011.
- Broder, J, Bowen J, Lohr J, et al. Cumulative CT exposures in emergency department patients evaluated for suspected renal colic. J Emerg Med. 2007; 33:161-168.
- Blake SP, McNicholas MM, Raptopoulos V. Nonopaque crystal deposition causing ureteric obstruction in patients with HIV undergoing indinavir therapy. AJR Am J Roentgenol. 1998;171;717-720.
- Dellabella M, Milanese G, Muzzonigro G. Randomized trial of the efficacy of tamsulosin, nifedipine and phloroglucinol in medical expulsive therapy for distal ureteral calculi. J Urol. 2005;174(1):167-172.
- Singh A, Alter HJ, Littlepage A. A systematic review of medical therapy to facilitate passage of ureteral calculi. Ann Emerg Med. 2007;50(5):552-563.
- Turkcuer I, Serinken M, Karcioglu O, et al. Hospital cost analysis of management of patients with renal colic in the emergency department. Urol Res. 2010;38(1):29-33.
- Catalano O, Nunziata A, Altei F, et al. Suspected ureteral colic: primary helical CT versus selective helical CT after unenhanced radiography and sonography. AJR Am J Roentgenol. 2002;178(2):379-387.
Publication Information
Michelle R. Carter; Brad R. Green
Publication Date
July 2, 2011
Get Permission
Content You Might Be Interested In
Management of Inflammatory Bowel Disease Flares in the Emergency Department
Content you might be interested in

Price: $497/year
140+ Credits!
Get a Sample Issue
Get A Sample Issue Of Emergency Medicine Practice
1-678-366-7933, [email protected].
Connect With Us
Who We Serve
Accredited By

Endorsed By

Our Partners
- For Providers
- For Employers
- For Patients
- All Procedures
Featured Specialties
Kidney Stone Removal (PCNL)
ESTIMATED NATIONAL AVERAGE
MDSAVE NATIONAL AVERAGE
How Much Does a Kidney Stone Removal (PCNL) Cost?
Find Kidney Stone Removal (PCNL) providers near you
Search board-certified providers, compare prices, buy online, and save money.
What Our Customers Say
Browse 18 providers in these locations.
Choose your location to find Kidney Stone Removal (PCNL) providers near you.
Shop with Peace of Mind
Financing options
Promotional financing available when you pay with CareCredit. What is CareCredit?
THE MDSAVE PROMISE
We will refund your payment in full if you end up not needing your purchased procedure and do not receive care. Details
Get Care In Three Easy Steps
Compare upfront prices.
Search by procedure and location to browse local providers and compare upfront pricing.
Buy Your Procedure
Pay for your procedure online or by calling (877) 461-2491 . Or buy your procedure at the facility before your appointment is scheduled.
Receive Your Care

Follow the scheduling instructions given by your provider. Bring your voucher to your appointment.
Inspiring Stories
Thanks to [MDsave], I got the medical tests my doctor ordered, quickly, professionally, and affordably. Your personal attention and standard of care were exceptional.
–Laura from Knoxville, TN
Sign Up & Save $25
Join MDsave’s email list and get $25 off any $250+ procedure purchase. Unsubscribe at anytime.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Our Products
© Copyright 2024 MDsave Incorporated.
All Rights Reserved.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Emergency Department Revisits for Patients with Kidney Stones in California
Associated data.
Kidney stones affect nearly one in 11 persons in the United States, and among those experiencing symptoms, emergency care is common. In this population, little is known about the incidence of and factors associated with repeat emergency department (ED) visits. The objective was to identify associations between potentially mutable factors and the risk of an ED revisit for patients with kidney stones in a large, all-payer cohort.
This was a retrospective cohort study of all patients in California initially treated and released from EDs for kidney stones between February 2008 and November 2009. A multivariable regression model was created to identify associations between patient-level characteristics, area health care resources, processes of care, and the risk of repeat ED visits. The primary outcome was a second ED visit within 30 days of the initial discharge from emergent care.
Among 128,564 patients discharged from emergent care, 13,684 (11%) had at least one additional emergent visit for treatment of their kidney stone. In these patients, nearly one in three required hospitalization or an urgent temporizing procedure at the second visit. On multivariable analysis, the risk of an ED revisit was associated with insurance status (e.g., Medicaid vs. private insurance, OR 1.52, 95% CI = 1.43 to 1.61; P < 0.001). Greater access to urologic care was associated with lower odds of an ED revisit (highest quartile OR 0.88, 95% CI = 0.80 to 0.97; P < 0.01, vs. lowest quartile). In exploratory models, performance of a complete blood count was associated with a decreased odds of revisit (OR = 0.86, 95% CI = 0.75 to 0.97; P = 0.02).
Conclusions
Repeat high-acuity care affects one in nine patients discharged from initial emergent evaluations for kidney stones. Access to urologic care and processes of care are associated with lower risk of repeat emergent encounters. Efforts are indicated to identify preventable causes of ED revisits for kidney stone patients and design interventions to reduce the risk of high-cost, high-acuity, repeat care.
INTRODUCTION
Kidney stones inflict excruciating pain at least once in the lifetime of nearly one in 11 people in the United States. 1 The burden of this disease falls largely on the working-age population, 2 , 3 and the economic effect of treating patients with kidney stones is substantial. 4 The agony of stone passage is increasingly common: on a population-adjusted basis, the rate of emergency department (ED) visits for stones has nearly doubled, in parallel with the rising prevalence of stone disease. 1 , 5
ED visits for patients with kidney stones are common. 5 More than 90% of patients evaluated in EDs for stones are released after treatment. 6 , 7 However, little is known about what happens after discharge from the ED. Some patients are able to pass their stones, 8 while others require procedural intervention. While awaiting resolution, some patients experience recurrent renal colic, necessitating repeat ED visits. From the patient perspective, revisits for pain are at best inconvenient and costly. Preventing ED repeated visits is important from the policy perspective because they contribute to inefficient and potentially costly care. 9
Given this context, we sought to characterize the frequency of ED revisits in a large, all-payer cohort. We also sought identify potentially independent associations between ED revisits and both clinical and non-clinical factors. To the extent that these factors are mutable, our overarching goal was to identify potential targets for improving emergency care for patients with kidney stones.
Study Design
This was a retrospective cohort study. The institutional review boards of the University of California, Los Angeles and Duke University determined that the study design was exempt from review.
Study Setting and Population
We used data from the California State Emergency Department Database (SEDD), the California State Inpatient Database (SID), and the State Ambulatory Surgery Database (SASD), part of the Healthcare Cost and Utilization Project (HCUP) of the Agency for Healthcare Research and Quality. The SEDD data consist of a 100% sample of ED visits to nonfederal, short-term, general, and specialty hospitals that do not result in inpatient admission; ED visits resulting in admission appear in the SID ( Figure 1 ). Finally, we used the SASD to identify ED revisits that resulted in urgent ambulatory procedures (i.e., ureteral stent placement). These data include identifiers for hospitals, as well as masked patient identifiers that permit linkage of health care encounters across time, between different care settings, and between different facilities. We used the masked patient identifiers to obtain a cohort of patients initially seen and released from ED visits for stones, and then followed for outcome events in all three datasets.

SID = State Inpatient Database; SASD = State Ambulatory Surgery Database; SEDD = State Emergency Department Database.
The study population consisted of individuals who had initial ED visits for suspected kidney stones in 2008 or 2009 using the SEDD data ( Figure 1 ). We identified patients using established claims algorithms based on diagnostic codes for their visits ( Data Supplement ). 10 Patients aged younger than 18 years or older than 89 years were excluded. We excluded visits in January 2008 in order to avoid left censoring; initial visits in December 2009 were also excluded in order to permit a full 30-day window for follow up.
Our study had two aims. First, we sought to describe the incidence of and variation in ED revisits following an initial treat-and-release ED evaluations. Our primary outcome was thus a second ED visit within 30 days of an initial emergent encounter to treat a kidney stone. While some patients had multiple revisits, we only included the first revisit as an outcome event. ED revisits could appear in the SEDD, SID, or SASD, depending on outcome (i.e., hospital admission; see Study Population and Setting). The SID and SASD include an indicator for encounters originating in the ED. We used this indicator and all three datasets to identify all ED revisits for the cohort ( Figure 1 ).
Our second aim was to characterize clinical outcomes of these revisits. Since death from a kidney stone is a rare event, we instead created a composite outcome of hospital admission or urgent procedure (specifically, placement of temporizing ureteral stent or percutaneous nephrostomy tube, based on established algorithms; 10 see Data Supplement ) as a result of the revisit ( Figure 1 ). Implicitly, patients with kidney stones who are discharged from initial ED evaluations are deemed clinically suitable for outpatient follow-up. When these patients return to the ED, and then require admission or urgent procedures, these outcomes potentially represent preventable failures of care delivery. In addition, these outcomes are high-acuity, high-cost health care events, and are therefore important from both the patient and health policy perspectives.
Patient-level covariates included age, sex, and race and ethnicity as reported by HCUP. We included race and ethnicity data because important variation in the prevalence of kidney stones exists among persons from different backgrounds. 1 We included primary payer as reported by HCUP, categorizing as private payer, Medicare, Medicaid, and self-pay/other. As a proxy for socioeconomic status, we included median household income quartile as reported by HCUP. We decided to not explicitly control for comorbid conditions in this analysis for two reasons. First, identifying comorbid conditions from a single ED encounter claim is unreliable, and records from other encounters, such as outpatient clinic visits or inpatient hospitalizations, were not available for all patients in these data. Second, prior claims-based analyses of patients with kidney stones demonstrate that approximately 90% of patients with kidney stones have Charlson scores of 0 or 1, among both commercially insured and Medicare beneficiaries. 11 – 13 Weekend care may differ from weekday care, so we included a variable identifying initial weekend ED visits. Local health care system resources may also influence revisit probability. For example, limited access to urologic care in rural areas negatively affects care outcomes. 14 , 15 Therefore, we included urban-rural classification and also included the per capita density of urologists at the Federal Information Processing Standards level, grouped in quartiles, as reported in the Area Resource File.
In addition to these patient- and area-level covariates, we hypothesized that processes of care, such as diagnostic testing, could influence the probability of a revisit. Therefore, we examined associations between the probability of a revisit and specific diagnostic tests performed at the initial ED encounter. Laboratory and imaging tests were identified using Common Procedural Terminology (CPT) codes ( Data Supplement ). We created four variables denoting the receipt of diagnostic testing implicit in current guidelines. Current guidelines 16 , 17 suggest that CT scan has the highest diagnostic performance for identifying kidney stones, although renal ultrasound and plain abdominal radiography are acceptable alternatives depending on clinical context (e.g., renal ultrasound for pregnant women). Therefore, we created an indicator variable for receipt of any potentially appropriate imaging test ( Data Supplement ). Current guidelines also recommend urinalysis (for bacteriuria), assessment for signs of infection or sepsis, such as leukocytosis, and measurement of renal function. 18 For each of these three tests, we created a separate indicator variable ( Data Supplement ). Since the reliability of identifying laboratory tests in ED claims data may be uncertain, we performed several sensitivity analyses (see Data Analysis).
Data Analysis
We calculated the frequency of revisits for each baseline characteristic, and then compared these using the chi-square test. Subsequently, we modeled the binary response of a repeat visit using a generalized linear mixed model with a logit link, controlling for age, sex, race, urban-rural classification, primary payer, household income, weekend visit, and per capita urologist density, accounting for clustering of outcomes at the facility level by adding a random intercept. The rates of missing data were extremely low for these covariates (sex, age, payer, urban-rural location, weekend admission, and urologist density all <1%; race 5%), and therefore we excluded cases with missing data. We subsequently used an identical approach to model the probability of the combined outcome of hospitalization or urgent procedure as a result of the ED revisit.
We then constructed a separate generalized linear mixed model with a logit link to examine associations between the probability of an ED revisit and receipt of guidelines-based diagnostic testing at the initial visit, again controlling for age, sex, race, urban-rural classification, primary payer, household income, weekend visit, and per capita urologist density, and accounting for clustering of outcomes at the facility level. Each ED visit record reports the number of procedure codes on the claim, and not all claims for the initial visits reported procedure codes. Therefore, we designated tests as missing if the visit records reported no procedure codes. Given that the reliability of coding for diagnostic tests is uncertain in these ED data, and may vary substantially between different facilities, we elected to perform a sensitivity analysis to assess the robustness of our results. To explore the stability of the initial estimates, we created a model using only records from patients seen at facilities that reported a median of at least four procedure codes per record. This sensitivity analysis therefore limited observations to patients evaluated at facilities that consistently coded procedures, and conceptually could reduce ascertainment bias. All statistical testing was two-sided, with a Type 1 error rate set to 0.05. We used SAS version 9.2 for all analyses.
The study population consisted of 128,564 subjects who had initial treat-and-release visits to EDs for kidney stones during the study period ( Table 1 ). Among these, 61% were male and over 80% were aged between 18 and 59 years. Nearly two-thirds were white, non-Hispanic, and an additional 25% were Hispanic. More than half (58%) were privately insured.
Characteristics of Study Cohort, n (%)
Within 30 days of the initial ED visit, 13,684 (11%) subjects each had at least one additional emergent visit for treatment of their kidney stones ( Table 1 ). ED revisits were more common among younger patients. There was no difference in revisit proportions between males and females; small differences in revisits were noted across racial and ethnic groups. Revisits were lowest among subjects with private insurance and highest among Medicaid beneficiaries (10% vs. 14%, p < 0.001). Revisits were also more common in rural areas and where the local urology workforce supply was low. At the facility level, the mean revisit rate varied considerably (11%, SD ±4.7%), and more than two-thirds of EDs had repeat visit rates between 6% and 16%.
Differences in the probability of an ED revisit persisted after controlling for important covariates ( Table 2 ). ED revisits remained more likely among younger and white, non-Hispanic subjects. The odds of an ED revisit were 52% higher among Medicaid beneficiaries (OR 1.52, 95% CI = 1.43 to 1.61), as compared with those with private insurance. A high per capita density of urologists was associated with lower odds of an ED revisit (highest quartile OR 0.88, 95% CI = 0.80 to 0.97 vs. lowest quartile). There was no difference in the odds of an ED revisit when the initial evaluation occurred on the weekend.
Characteristics Associated with ED Revisit
Outcomes of Revisits
Among the 13,684 subjects who experienced ED revisits, 3,069 (29%) were either admitted to the hospital or underwent an urgent procedure as a result of the revisit. These outcomes varied substantially by clinical and non-clinical factors on multivariable analysis ( Table 3 ). As compared with young subjects, the odds of hospitalization or urgent procedures were very high among those aged at least 75 years (OR 3.90, 95% CI = 3.03 to 5.02). Females were more likely to be admitted or undergo urgent procedures than males (OR 1.82, 95% CI = 1.67 to 2.00). When subjects returned to the ED, those living in areas with the highest per capita supply of urologists were most likely to be hospitalized or undergo a procedure (OR 1.77, 95% CI = 1.38 to 2.27).
Characteristics Associated with Hospitalization or Urgent Procedure as a Result of ED Revisit
Diagnostic testing
Among the diagnostic tests recommended for the evaluation of a patient with a suspected kidney stone, only performance of a blood count was associated with the probability of an ED revisit ( Table 4 ). Patients who had a white blood cell count performed at the initial visit had 14% lower odds of experiencing an ED revisit (OR 0.86, 95% CI = 0.75 to 0.97). This association remained stable when restricting the analysis to facilities reporting a median of at least four procedure codes on each claim (OR 0.86, 95% CI = 0.76 to 0.98). In contrast, urinalysis, imaging, and assessment of renal function were not associated with the odds of an ED revisit.
Associations between performance of guideline-recommended testing and ED revisit *
We report the novel finding that up to one in nine patients requires repeat ED care within 30 days of a first ED visit for a kidney stone; among these patients, nearly one in three requires an urgent procedure or hospitalization as a result of the revisit. The probability of a repeat ED visit varies substantially among facilities. The probability of a revisit is associated with non-clinical factors, such as insurance status and local urologic health care resources. Non-use of a complete blood cell count was associated with increased risk for an ED revisit. These key findings suggest that repeat ED care is an important problem, and a potential quality of care marker for patients with kidney stones.
From the patient perspective, an ED visit for a kidney stone is a significant event, typically prompted by excruciating pain. This burden of acute disease falls primarily on a working-age population (over 80% of patients in our sample) and likely imposes substantial indirect costs, in addition to the high direct costs of emergent care. 3 , 6 Our findings suggest that after being treated and released the first time, more than 10% of patients experience additional symptoms within the next month that require an additional ED visit.
The costs of care for patients with kidney stones are substantial, and thus repeat ED visits and their sequelae are health-policy relevant. Aggregate expenditures for treating patients with kidney stones are among the greatest for any urologic condition; data from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) Urologic Diseases in America project estimated charges in excess of $10 billion annually. 4 Hospitalizations and procedures constitute the largest proportion of this spending. An important opportunity to reduce costs and improve outcomes exists, to the extent that these ED revisits and their sequelae can be reduced by optimizing care.
The hypothesis that some of these ED revisits are affected by non-clinical factors is supported by key findings from our investigation. At the ED level, revisit frequencies varied widely, with more than two-thirds of facilities falling in the range of 6% to 16% revisit probability. Insurance status was strongly associated with risk of revisits, and notably these risks were higher for patients with Medicaid or no insurance coverage, as compared to privately insured individuals. Insurance coverage may be a proxy for access to primary care, or urologic care, either of which could reduce the likelihood that a follow-up visit occurs in the ED setting. In areas with the lowest physician supply of urologists, the odds of an ED revisit were 14% higher than in areas with the highest urologist supply. We noted an intriguing association between receipt of complete blood count testing and a decreased risk of revisit. This finding must be interpreted cautiously as hypothesis-generating. A plausible clinical explanation for this association is not recognizing impending systemic infection could potentially result in an emergent revisit because of delays in treatment, such as antibiotics. Using clinical data, a recent cohort study of patients evaluated in the ED for a symptomatic stone found that leukocytosis was associated with the risk of ED revisit. 19 A 2007 guideline recommends evaluation for signs of systemic infection, 18 but no specific guidance was provided on which test(s) should be ordered, and the guideline authors rated this as Level IV evidence (i.e. expert panel opinion). This finding may also be limited by ascertainment bias. To explore the potential for ascertainment bias further, we performed a sensitivity analysis limiting the population to hospitals with relatively high frequencies of diagnostic test codes on the discharge record (median ≥4 per record). In this sensitivity analysis, the OR remained stable and statistically significant. We believe this finding should, at a minimum, prompt rigorous assessment of the clinical utility of leukocytosis in the management of acute renal colic, and its potential relationship with quality of care for these patients.
Another important consideration for interpretation of these results is the outcome of hospitalization or urgent procedure, which occurred in nearly one in three patients with second ED visits. Only 10% of patients are admitted as a result of their first ED visits, 5 – 7 and thus the second ED visit carries nearly triple the risk of hospitalization or urgent intervention. If hospitalization occurs due to poor access to urologic or primary care, or an incomplete evaluation for signs of infection, then this outcome may be potentially avoidable if different care is provided at the index visit. Alternately, hospitalization could represent a clinically appropriate escalation of best prior care, albeit the result of an inefficient, costly, and inconvenient second ED visit. Instead of a second ED visit, a more efficient and higher quality strategy would be escalation through a usual source of primary care, or through access to urologic care. Future investigations should more closely explore the role of primary care and urologic care access for the management of symptomatic kidney stone patients who are discharged from the ED.
LIMITATIONS
These data represent a single large state, and therefore may not generalize to treatment of patients with kidney stones in other areas, or nationally. The dataset lacks potentially important clinical detail, particularly with respect to clinical history, physiological information, disease severity, or indications for return. Therefore, the association between laboratory testing and revisits must be regarded as hypothesis-generating. The National Hospital Ambulatory Medical Care Survey (NHAMCS) queries whether patients were seen in the ED within 72 hours before the sampled visit, although detailed information about the reason for the prior visit is not recorded. In reports from NHAMCS, about 10% of subjects evaluated emergently for stones report prior ED visits, 5 , 6 suggesting that the revisit frequency of 11% observed in our more granular data retains validity. Some factors, such as insurance status, could change between visits; we only included data from the first visit in our analysis. Missing data could bias results, although the proportion of observations was very low. We observe variation in risk of ED revisits, hospitalizations, and urgent procedures along racial and ethnic lines; since these traits are immutable, and observed associations are likely a proxy for other factors, further investigation to understand these risk differences is warranted.
Our analysis pertains only to those patients discharged from initial ED visits, although this constitutes 90% of patients receiving emergent care for stones. 5 – 7 We used an area-level measure of socioeconomic status, which is imperfect due to heterogeneity within geographic areas. Nonetheless, our findings highlight the previously poorly described phenomenon of repeat ED visits for patients with kidney stones.
CONCLUSIONS
Our findings suggest that ED revisits are not uncommon for kidney stone patients who are initially treated and released. ED revisits are fairly likely to result in hospital admission or urgent procedures. Furthermore, observed associations between revisit risk and markers for access and quality of care suggest that mutable factors, such as care processes, may influence patient- and policy-relevant outcomes. These results should motivate efforts to identify preventable causes of ED revisits for patients with kidney stones and design interventions to reduce the risk of high-cost, high-acuity, repeat care.
Supplementary Material
Supp material, acknowledgments.
This work was initiated while Dr. Scales was a Robert Wood Johnson Foundation/VA Clinical Scholar at the David Geffen School of Medicine at UCLA.
FUNDING / SUPPORT
Dr. Scales was supported by the Robert Wood Johnson Foundation and the VA Office of Academic Affiliations through the VA/Robert Wood Johnson Clinical Scholars Program.
Dr. Mangione received support from the UCLA Robert Wood Johnson Clinical Scholars Program and the U.S. Department of Veterans Affairs (Grant #67799), the University of California at Los Angeles (UCLA), Resource Centers for Minority Aging Research Center for Health Improvement of Minority Elderly under National Institutes of Health (NIH)/NIA Grant P30-AG021684, and from NIH/National Center for Advancing Translational Sciences UCLA Clinical and Translational Science Institute Grant UL1TR000124. Dr. Mangione holds the Barbara A. Levey and Gerald S. Levey Endowed Chair in Medicine, which partially supported her work.
The Urologic Diseases in America Project is supported by grant HHSN276201200016C from the National Institute of Diabetes and Digestive and Kidney Diseases and the National Library of Medicine.
The views expressed in this article are those of the authors and do not necessarily reflect the position and policy of the United States Federal Government or the Department of Veterans Affairs. No official endorsement should be inferred.
ROLE OF THE SPONSORS:
The funding sources had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation or review of the manuscript; or decision to submit for publication. The Robert Wood Johnson Foundation and US Department of Veterans Affairs had no role in approval of the manuscript. The Executive Committee of the Urologic Diseases in America Project includes representatives from the National Institute of Diabetes and Digestive and Kidney Diseases; the Executive Committee approves project manuscripts based on technical considerations alone but otherwise has no role in the study.
* GROUP INFORMATION
The members of the NIDDK Urologic Diseases in America Project are: Mark S. Litwin, MD MPH, Department of Urology, David Geffen School of Medicine and Fielding School of Public Health, University of California, Los Angeles; Christopher S. Saigal, MD MPH, Department of Urology, David Geffen School of Medicine, UCLA and RAND Corporation; Paul Eggers, PhD, National Institute of Diabetes and Digestive and Kidney Diseases, Washington, DC; Tamara Bavendam, MD, National Institute of Diabetes and Digestive and Kidney Diseases, Washington DC; Ziya Kirkali, MD, National Institute of Diabetes and Digestive and Kidney Diseases, Washington, DC.
Prior Presentations: none
None of the authors have conflicts of interest to disclose.
How to Handle a Huge ER Bill
6 ways to avoid going into debt for your health
Mamie Laverock's Accident, Hospitalization

‘Doctors Dismissed My Mesothelioma As Fibroids’

'Dance Moms's Kelly Hyland Breast Cancer Diagnosis

10 Best Breathable Underwear Picks, Per Editors

All About Christie Brinkley's Skin Cancer

Kate Middleton's Cancer Diagnosis Timeline

All About The 2024 'Women's Health' Health Lab

Judi Dench May Be Done Acting Amid Vision Loss

Kourtney Kardashian Reveals '5 Failed IVF Cycles'

What 'Leaky Gut' Actually Means, According To RDs

Brittany Mahomes' Back Fracture: What To Know
Health Spending
- Quality of Care
Access & Affordability
- Health & Wellbeing
- Price Transparency
- Affordability
- Prescription Drugs
Emergency department visits exceed affordability threshold for many consumers with private insurance
By Hope Schwartz Twitter , Matthew Rae Twitter , Gary Claxton , Dustin Cotliar, Krutika Amin , and Cynthia Cox Twitter
December 16, 2022
Stay Connected
Get the best of the Health System Tracker delivered to your inbox.
Introduction
The high cost of emergency care may impact patients’ ability to afford treatment , with almost half of US adults reporting they have delayed care due to costs. Almost 1 in 10 Americans have medical debt , and about half of American households do not have the liquid assets to afford an average employer sponsored plan deductible. More than one third of US adults are unable to afford a $400 medical expense without borrowing.
Costs of medical emergencies present an additional financial burden on top of already costly health insurance premiums ranging $1,327 for single coverage and $6,106 for family coverage, on average, for workers with employer sponsored insurance. Variation in emergency department billing may make it difficult to predict the cost of an emergency department visit and subsequent financial liability. Recently, the No Surprises Act legislation aimed to curb unexpected emergency medical costs by prohibiting out-of-network billing for emergency services.
In this analysis, we use 2019 insurance claims data from the Merative MarketScan Commercial Database, which captures privately insured individuals with large employer health plans. We look at the total and out-of-pocket costs of emergency department visits for this group, overall and by diagnosis and severity level. We also look at which services contribute most to the costs of emergency department visits and examine regional variation in emergency department costs. Finally, we look at the demographic profile of consumers who visited the emergency department and the relationship between emergency department spending and annual spending for enrollees.
We find that enrollees spend $646 out-of-pocket, on average, for an emergency department visit. Enrollees with high annual health spending were more likely to visit the emergency department; the majority of enrollees in the top 10% of annual health care spending had at least one emergency department visit during the year. The most expensive components of most emergency department visits include evaluation and management charges, imaging, and laboratory studies, and facility fees make up 80% of the cost of visits. Cost varies by disease, visit complexity, and geographic region.
Large employer plan enrollees’ emergency department visits cost $2,453, on average, with enrollees responsible for $646 in out-of-pocket costs
On average, enrollees in large employer health plans who have an emergency department visit spend $646 out-of-pocket on the visit. There is significant variation in emergency department spending, with 25% of visits costing over $907 out-of-pocket and another quarter costing less than $128 out-of-pocket. These out-of-pocket costs for a single emergency department visit may be more than some people with private insurance can afford and, in some cases, could entirely deplete a consumer’s savings. For example, about 1-in-5 people (21%) with private insurance living in single-person households have less than $1,000 in liquid assets.
Related Content:
How does medical inflation compare to inflation in the rest of the economy?
Medical debt among new mothers
These amounts only include out-of-pocket spending required by the insurer. Before the No Surprises Act went into effect in January 2022, privately insured patients who visited the emergency department frequently had out-of-network claims on their visit, putting them at risk of providers sending them surprise balance bills. The No Surprises Act now prohibits most surprise out-of-network billing, but does not apply to ground ambulances . Any balance bill that a patient received from a provider would not appear in claims data and therefore would have been in addition to the out-of-pocket amounts shown here.
In total, enrollees and insurers paid $2,453, on average, per visit, with one quarter of visits costing $970 or less and another quarter costing $3,043 or more. All the costs described in this analysis are for the emergency department visits only, including professional services and facility fees, and do not include any spending on subsequent hospitalizations.
Facility fees contribute significantly more than professional fees to total visit cost
Emergency department bills are categorized as facility fees or professional fees. Professional fees are for services provided by clinicians, and facility fees include bills for services rendered using equipment owned by the facility, including laboratory or imaging studies. These fees are considered “overhead” for emergency departments and help facilities maintain appropriate staffing levels and technical resources. Evaluation and management charges also have a facility fee component for the equipment, staffing, and administrative resources used by the physician in their management. We find that facility fees make up 80% of total visit cost.
Evaluation and management charges make up the largest share of costs
Including both the professional fee and facility fee components of charges, the largest contributor to spending on a typical emergency department visit is the evaluation and management charge, which accounts for almost half (44%) of average visit costs. Evaluation and management charges are bills for the assessment of a patient that are not related to specific procedures or treatments provided; these services cost over $1,100 per visit, on average.
Imaging charges, including radiologist interpretation fees, make up an additional 19% of the average emergency department visit charge and cost $483, on average. The highest cost routinely performed imaging services include x-rays of the chest and CT scans of the head, chest, abdomen, and pelvis. Over half of visits (55%) include a charge for imaging services. About half of patients (49%) are charged for laboratory studies, including blood tests, which cost $230 on average. Other high cost but less common charges include surgical charges for patients with appendicitis and other conditions requiring surgery without inpatient admission, as well as ambulance charges for transport.
Heart attacks and appendicitis among the most expensive common conditions treated in the emergency department
Costs of emergency department visits depend on diagnosis. We selected nine common reasons to visit the emergency department that vary in complexity of management. More severe conditions, or those with more intervention required, are the most expensive. Of the nine specific diagnoses that we evaluated, the lower-cost diagnoses were those that generally do not require imaging or extensive treatment in the emergency department. These included upper respiratory tract infections ($1,535 total, $523 out-of-pocket), skin and soft tissue infections ($2,005 total, $572 out-of-pocket), and urinary tract infections ($2,726 total, $683 out-of-pocket). While these diagnoses can occasionally require admission to the hospital, in otherwise healthy adults they are typically evaluated with basic laboratory studies and discharged with prescriptions.
The most expensive emergency department diagnosis among those we examined is appendicitis, which, on average, costs $9,535 ($1,717 out-of-pocket) per visit. Appendicitis is almost two times as expensive as the next most expensive diagnosis we looked at, heart attack. 11% of enrollees with a diagnosis of appendicitis had surgical charges associated with their emergency department visit. Surgical costs may be included in emergency department outpatient billing because these patients are often discharged after surgery without being admitted to the hospital. In contrast, other emergency department visits requiring surgery are often admitted to the hospital and have surgical charges during their inpatient visit. Enrollees who had surgery had more expensive visits by over $2,000 compared to those who did not; however even without surgery, visits for appendicitis were almost four times as expensive as the average emergency department visit (and more than twice as expensive out-of-pocket).
Enrollees with emergency department visits have variable annual spending depending on diagnosis
In addition to the costs of the emergency department visit itself, enrollees who visit the emergency department at least once during the year have higher annual health care spending. Annual spending includes the cost of all claims for each patient in 2019, either before or after their emergency department visit. Though appendicitis was the most expensive emergency department visit among the diagnoses we analyzed, enrollees with appendicitis in 2019 incurred an average of $24,333 in additional health care spending, which was comparable to lower cost diagnoses. Enrollees with heart attacks had at least two times more annual spending than any other diagnosis ($52,993), while enrollees with upper respiratory tract infections had the lowest annual spending ($13,727).
These differences in annual costs may reflect spending both directly related and unrelated to the emergency department visit. For example, enrollees with heart attack emergency department visits may have high annual spending because of follow-up, medications, or hospitalizations after their heart attacks. However, their high annual spending may also reflect more comorbidities and higher healthcare utilization at baseline. In contrast, appendicitis, the most expensive emergency department visit, is correlated with relatively lower annual costs; unlike heart attacks, appendicitis often occurs in younger, healthier people and requires comparatively little additional post-surgical follow-up or treatment.
The most complex emergency visits are more than 6 times as expensive as the least expensive visits, but insurers pay an increasing share of the visit as complexity increases
Emergency department visits are coded by complexity during the billing process, from 1 (least complex) to 5 (most complex). Each evaluation and management charge is associated with a procedure code ranging from level 1 to level 5 (99281 to 99285), which are generated by hospital coding professionals based on the physicians’ medical note. Criteria are defined by the Centers for Medicare and Medicaid Services ( CMS ) and based on the complexity of documentation and medical decision making. Patients with level 1 complexity codes require straightforward medical decision making, with self-limited or minor presenting problems, such as rashes or medication refills. Patients with level 5 codes require high complexity medical decision making and present with life- or limb-threatening conditions, such as severe infections or cardiac arrests.
The lowest complexity visits cost $592 on average, with enrollees responsible for $205, or about one-third of the total visit cost. As visits increase in complexity, both out-of-pocket costs and costs covered by insurance increase. For the highest complexity visits, the health plan covers $3,015 on average, or eight times the cost of the lowest complexity visits. On average, patients pay $840 out-of-pocket for the highest complexity visits, which is four times their out-of-pocket costs for the lowest complexity visits.
Higher complexity visits are more expensive for multiple reasons. In general, evaluation and management charges are higher cost for more complex patients. Also, patients with more complex medical conditions generally receive more diagnostic tests, medication, and other treatment, which increases the cost of the visit. For the lowest complexity visits, evaluation and management charges account for almost half (47%) of the overall visit cost. In contrast, evaluation and management charges for the highest complexity visits account for about one-fourth (27%) of the total visit cost, with additional services including tests and treatment making up a larger share of the cost.
Emergency department costs vary by geographic region
We analyzed the top 20 metropolitan statistical areas (MSAs) by population, where data are available. Overall, the San Diego, CA area had the most expensive average ED visits ($3,761 on average). San Diego ED visits were more than twice as expensive as Baltimore, MD, the least expensive MSA in our analysis ($1,645 on average). Expensive MSAs were geographically distributed in all regions of the country including the South, West, Northeast, and Midwest. Within each MSA, there was significant variation in visit costa. For example, 25% of visits in Oakland, CA cost less than $1,236 on average, while 25% cost more than $4,436 on average.
Some variation may be based on the distribution of diagnoses in each area, with more serious or complex diagnoses leading to higher cost visits. For example, if a metro area sees higher than average volume of appendicitis, heart attacks, or other high-cost diagnoses, that would drive up regional emergency department costs.
For common diagnoses, Texas and Florida MSAs are among the most expensive
If we examine costs for specific diagnoses, we can minimize some of this variation in reasons for visits and gain a better understanding of how prices and service intensity affect the rankings. We selected two common, moderate-cost reasons for emergency department visits: low back pain and lower respiratory infections. While these visits can range in complexity and treatment required, they usually do not require hospital admission or high-cost treatment. Low back pain includes patients who present with the symptom of low back pain, regardless of diagnosis. Lower respiratory tract infection includes infectious causes of pneumonia and bronchitis. This analysis was limited to MSAs in which there were >500 cases of each diagnosis in 2019.
Visit costs for both diagnoses in Dallas, TX, Houston, TX, Fort Worth, TX, and Orlando, FL are in the top five most expensive MSAs with >500 cases. For low back pain visits, the Orlando, FL, Fort Worth, TX, Dallas, TX, and Houston, TX areas are each more than twice as expensive as the Warren, MI and Detroit, MI areas, on average. This trend is similar for lower respiratory tract infections. Within MSAs, variation in costs exist for both diagnoses. For example, for low back pain visits, there is more than a $3,000 difference between the least expensive and most expensive quarter of visits in Fort Worth, TX, Dallas, TX, and Houston, TX.
12% of large employer group enrollees went to the emergency department in 2019
We find that 12% of large group enrollees under age 65 had at least one emergency department visit in 2019, and of enrollees with emergency department visits, 80% had only one visit. 20% had more than one visit, and 7% had more than two visits. Emergency department visits were associated with higher annual health care spending, with almost half of enrollees in the top 25% of annual spending having at least one emergency department visit during the year.
We find that the average emergency department visit exceeds the threshold that some consumers can pay without borrowing, and even one emergency department visit in a year may create financial hardship for enrollees in large employer plans. For example, one quarter of emergency department visits for large employer enrollees cost over $907 out-of-pocket. Meanwhile, about 1-in-5 people with private insurance do not have $1,000 in liquid assets, and almost half of US adults report that they would not be able to pay a $500 medical bill without going into debt. Emergency department visits range significantly in cost depending on diagnosis, visit complexity, and geographic area. These variations may present challenges for consumers trying to predict the cost of their emergency department visit prior to going to the emergency department.
Several factors contribute to the variability of emergency department charges. First, unlike other forms of outpatient care including primary care or urgent care visits, emergency departments charge facility fees to offset the cost of keeping emergency departments open and staffed 24/7. These fees vary widely and are increasing at a faster rate than overall health care spending. The facility component represented 80% of total emergency department spending in our analysis. Many hospitals and health care providers consider these costs necessary given their mandate to provide emergency triage and treatment to allcomers. A second contributor to variation is that services are often billed at different complexity levels, and visits that are billed as more complex are more expensive . In some cases, even similar services are billed at different prices by different facilities. Notably, surprise out-of-network medical bills from emergency departments have contributed to high emergency costs for consumers, though the cost of any balance bills would be outside the scope of our claims data. The implementation of the No Surprises Act in January 2022 will generally curb surprise medical billing for emergency care.
As seen in non-emergency spending , we find that emergency department costs vary by geographic area. Among the most expensive MSAs in our analysis were MSAs located in Texas, Florida, California, Colorado, and New York. Interestingly, the most expensive regions for ED care do not align with the most expensive regions for overall health care spending. These comparisons suggest that our findings are not solely related to overall high health care prices in these areas and may reflect other factors including the age and medical complexity of the population or differences in local norms and practice patterns. State-level emergency department regulation may also play a role—states with higher numbers of freestanding , non-hospital affiliated emergency departments (which are associated with higher spending on emergency care) were among the most costly in our analysis.
The financial implications of visiting the emergency department vary widely. Not all the variation in total charges is reflected in out-of-pocket costs, since differences in cost by complexity level are smaller after insurance covers its portion of the bill. However, the most complex emergency department visits have four times higher out-of-pocket costs than the least complex visits. Even the least complex visits, some of which could be treated by a primary care office or urgent care center, cost an average of $205 out-of-pocket ($592 total). Given facility fees and relatively high evaluation and management charges in emergency departments, insurers and patients are paying more when receiving care for these conditions at emergency departments than they would using primary or urgent care. These lower complexity visits may represent a substantial avoidable cost to patients and the health care system at large.
High health care costs are of foremost concern for US adults, leading people to skip recommended medical treatment or delay necessary care. Even in the era of new price transparency regulation , which aims to improve consumer access to prices for elective care, emergency department consumers often do not know what testing or treatment they will need, so it is difficult to assess the costs of a visit upfront. Further, in an emergency situation, patients may not be able to choose their provider or facility if they are brought in by ambulance or otherwise unable to direct their care. Lastly, lack of availability and standardization in data may make it difficult for patients to use price transparency data in real time to make decisions about accepting tests and treatment in an emergency. The high and variable cost of emergency department visits represents an opportunity for future policy changes to protect consumers from unaffordable medical bills.
This analysis is based on data from the Merative MarketScan Commercial Database, which contains claims information provided by a sample of large employer plans. Enrollees in MarketScan claims data were included if they were enrolled for 12 months. This analysis used claims for almost 14 million people representing about 17% of the 85 million people in large group market plans (employers with a thousand or more workers) from 2004-2019. To make MarketScan data representative of large group plans, weights were applied to match counts in the Current Population Survey for enrollees at firms of a thousand or more workers by sex, age, state, and whether the enrollee was a policy holder or dependent.
Emergency department visits were flagged if an enrollee had an emergency department evaluation and management claim in the emergency department or the hospital on a given day. If an enrollee had either an emergency evaluation and management claim or another claim originating in the emergency department on the day prior to or after the flagged day, we added the previous and or following day’s outpatient spending to the visit cost. This was to capture all emergency department services for visits that may have spanned overnight or multiple days. Over half (53%) of the spending in this analysis occurred in the emergency department, with another 42% occurring in the hospital, which may occur when a patient receives a test or procedure in a location outside the emergency department during their visit.
Claims were included if they were above $100 and below the 99.5 th percentile of cost. Selected conditions were generated from a literature review of common emergency department diagnoses and defined using ICD10 codes. Enrollees were considered to have a certain diagnosis if the relevant ICD10 code appeared in the “Diagnosis 1” column in one or more claims on an emergency department visit day. While emergency department claims have up to four diagnoses, diagnoses listed in 2-4 were not used to identify relevant conditions because these diagnoses were most often incidentally found rather than related to the reason for presenting to the emergency department. For specific diagnosis definitions: Heart attack includes acute STEMI and NSTEMI, and excludes complications from prior heart attacks or angina; UTI includes acute cystitis, UTI and pyelonephritis; Kidney stone includes renal calculus in any location and renal colic; Lower respiratory infection includes pneumonia and bronchitis. Surgical charges for acute appendicitis include both open and laparoscopic surgical charges. Annual spending was defined as the total spending for each enrollee in the year 2019, which could occur before and/or after their emergency department visit depending on the time of year of the emergency department visit.
This analysis has some limitations. First, there is a chance that we could incorrectly include non-emergency outpatient care (such as a next-day, follow up primary care appointment) in our estimate of emergency department visit costs. Secondly, when accounting for annual spending, we do not control for health status prior to the emergency department visit. Therefore, the increase in annual health spending for patients who visit the emergency department for certain conditions may be because these patients are sicker and higher healthcare utilizers at baseline, rather than specific follow-up costs incurred for the emergency department visit itself. For selecting relevant diagnoses, we only include claims in which a particular diagnosis occurs as the primary diagnosis. Third, the MarketScan database includes only charges incurred under the enrollees’ plan and do not include balance billing to enrollees which may have occurred. Lastly, our findings only represent enrollees in large group employer sponsored plans and may not be generalizable to other groups.
About this site
The Peterson Center on Healthcare and KFF are partnering to monitor how well the U.S. healthcare system is performing in terms of quality and cost.
More from Health System Tracker
What are the recent trends in employer-based health coverage.
Privately insured people with depression and anxiety face high out-of-pocket costs
Looking for more data?
Find out more details about U.S. healthcare from our updated dashboard.
A Partnership Of
Share health system tracker.
How to avoid this hidden summer health risk that affects 1 in 10 Americans

Warm weather brings days at the beach, sunscreen and ... kidney stones?
Researchers say people who don't stay properly hydrated face a higher risk of these painful mineral deposits as temperatures and humidity rise in the summer. On top of that, they noted that in general people whose diet is packed with too much sodium, fat and sugar, could find themselves among the 1 in 10 Americans who will get a kidney stone in their lifetimes.
Kidney stones are formed when minerals from urine crystalize into a small stone or pebble-like mass. These stones can become lodged in the ureter, the tube connecting the kidney to the bladder. The stones sometimes cause an obstruction that makes it difficult to urinate and triggers a sharp pain in the side or lower back. Some stones pass on their own and cause little or no discomfort.
Summer is a key time to pay attention to these deposits, since there's a greater risk of kidney stones when temperatures rise and people don't stay hydrated, said Dr. Ivan E. Porter, a nephrologist at the Mayo Clinic in Jacksonville, Florida. When its hot and people sweat more but don't drink sufficient water or other fluids, those conditions "absolutely can relate to an increased risk of both stone events and stone formation," Porter said.
A 2023 study published in the American Journal of Kidney Diseases reported emergency room visits to New York state hospitals for kidney stones, urinary tract infections and other kidney injuries increased during warmer months, particularly during "transitional" months of May when weather warms and September as summer trails off.
The research suggests people likely aren't prepared when temperatures rise, said Dr. Shao Lin, a professor of environmental health at State University of New York at Albany and study co-author. The problem, she said: People spend too much time in the sun, don't drink enough water or don't turn on their air conditioner when temperatures rise.
"The human body has not yet adapted to the hot weather in May," Lin said. "People are not ready for that."
Beyond elevated risk due to heat and lack of hydration, other factors likely have accelerated the rising number of kidney stone cases. Kidney stone rates in the United States increased from 3.8% in the late 1970s to about 10% a decade ago, according to the National Kidney Foundation.
"Over the last couple of decades, where we've seen some other diseases drop off or slow down, kidney stones have not. It's continued to increase," said Dr. Timothy Averch, a urologist in Columbia, South Carolina.
Averch said warming temperatures worldwide might contribute to rising rates of kidney stones, but, he said, diets are also likely a major explanation.
"What we eat is not super healthy when it comes to kidney stones, and even some of the things we consider healthy can have a negative effect on kidney stone formation," Averch said.
What can I do to lower my risk of kidney stones?
The most important thing is to drink plenty of water or other fluids with citrate, such as lemonade or lemon juice, to stay hydrated, Averch said. Equally important is avoiding or minimizing intake of drinks that can dehydrate such as coffee and alcohol.
Doctors also recommend avoiding foods with a lot of sodium. Processed foods are often packed with sodium and should be avoided, Porter said.
"The majority of salt we get in a normal American diet does not come from the salt shaker," Porter said. "It comes from processed foods. So it's something out of a can or something out of a bag."
People also should avoid eating diets with an excess amount of animal proteins and fats. Averch cited one study from Italian researchers that showed diets heavy in animal protein led to hypercalcemia, or too much calcium in the blood.
Researchers also have busted diet myths. A few decades ago, people were advised they could be at risk for kidney stones if they drank too much milk or consumed a lot of dairy products such as cheese or yogurt. But diet studies have shown that such calcium-rich foods had the opposite effect - they reduced the risk of a type of kidney stone called calcium oxalate stones.
"Those who increased dairy intake with cheese, milk, yogurt, those patients actually had lower metabolic risk factors for stones," Porter said.
However, people who take large dosages of calcium supplements might face a higher risk, he said.
"So a diet rich in calcium is good. Calcium supplements, not so good," Porter said.
What to do if you have kidney stone symptoms
People with kidney stones might first recognize sharp pain in the lower back or side that radiates down to the groin. Others have described having a more general pain or stomachache that won't go away.
Other symptoms can include blood in the urine or a burning sensation when urinating, as well as nausea, vomiting, fever and chills.
Doctors can check whether you have a stone or might order imaging tests to determine the size of the stone. They may also order blood tests to check for signs of calcium, phosphorus and uric acid tests. Many patients are able to pass stones on their own, but some need them removed. If you've had a stone, you have a 50% risk of developing another within five to seven years, according to the National Kidney Foundation.
If you suspect you might have one, it's always better to get checked, doctors said.
"If you're not sure what that is, and never had a kidney stone before, you should probably seek medical care," Averch said.
carolina Forest ER
Photos & videos.
See all 2 photos

You Might Also Consider

Heart of Grace Home Care
6.4 miles away from carolina Forest ER
Heart of Grace is the epitome of what kind of heart we carry servicing the community. This company has the heart of grace, we're humble, we show good character, we show goodness and generosity. Your family become our family and… read more
in Home Health Care

Right at Home
9.4 miles away from carolina Forest ER
in Home Health Care, Personal Care Services

Life Line Services
John W. said "Did not know what to expect from a visit with Trish. Actually, I went with very little expectation at all. In my mind there was nothing wrong with me that I couldn't fix myself. How wrong was I? Trish is an amazing Therapist. She…" read more
in Addiction Medicine, Counseling & Mental Health, Weight Loss Centers
Location & Hours
Suggest an edit
2101 Oakheart Rd
Myrtle Beach, SC 29579
Recommended Reviews
- 1 star rating Not good
- 2 star rating Could’ve been better
- 3 star rating OK
- 4 star rating Good
- 5 star rating Great
Select your rating
Overall rating

Another 6am visit to the ER. Kidney stones this time. Check in was easy with a kiosk. Was roomed fairly quickly and meds administered in a timely fashion. All the nurses were extremely helpful. The doctor on duty even called a specialist to verify my kidneys were not going to sustain permanent injuries due the high readings we was getting. A follow up appointment will be needed to confirm. All in all, excellent staff on duty!!!

What a great alternative to going to grand Strand ER. (For my situation). I was having abdominal pain and the Urgent Care facility I was at earlier said to head over here for a CT scan. A newly constructed Emergency Care facility in Carolina Forest is beautiful. Located near Buffalo Wild Wings off 501 In Carolina Forest. Easy check in with a kiosk, was shown to a room within 5 minutes of walking through the front door, (FYI, there is an ambulance drop-off area as well), nurse hooks me up to an I.V. and the process is underway. A new process for me was the IPAD check in while I laid in the bed. A live person goes over your issues and you sign paperwork online and process your payment as well. Kinda cool. Not sure how the older generation would feel about this but it's a sign of the times. Technology changes. Anyway, I was in and out of the ER in 2 hours. This is my 1st choice over a Grand Strand hospital visit!!!
People Also Viewed

Mcleod Health Carolina Forest

McLeod Health Seacoast
Loris Community Hospital

Grand Strand Medical Center
South Strand Medical Center

Seacoast Medical Center
Carolina Health Specialists

South Strand Internists and Urgent Care

Beach Family & Urgent Care

Nicholson George B Jr MD
Browse Nearby
Restaurants
Things to Do
Chiropractors
Other Hospitals Nearby
Find more Hospitals near carolina Forest ER

COMMENTS
Kidney stone treatment can cost from just under $10,000 to $20,000 or more for surgical removal or extracorporeal shock wave lithotripsy (ESWL). ... ER visit (moved to private room quickly), pain meds, blood tests, malaria test, ECG, CT scan, moved to ward, transferred to specialist hospital via ambulance, covid tests, overnight stay, lots of ...
What tests will the ER do for kidney stones? If a kidney stone is suspected based on your history, then the ER provider will often start with blood and urine samples. They will look for microscopic blood in the urine which is a sign of a kidney stone (although blood in the urine is absent in 10% of patients).
Kidney stones are hard deposits of minerals and salts that can form in the kidneys when there is an imbalance of water, salt, and mineral water in your urine. As the stones grow in size, they can lead to severe pain and other symptoms. Kidney stones typically occur when you're drinking less water than what your body needs, which is something ...
Out-of-pocket costs for an uninsured patient will be higher. Average cost of stone surgeries: PCNL: $3,624. ESWL: $2,295. Ureteroscopy: $1,425. Costs due to lost work: In 2000, 1% of all working age adults missed work due to a stone episode. When focusing on just stone formers, 30% of them missed work due to a stone episode, with each worker ...
Certain kidney stone symptoms and changes in symptoms may indicate the need to consult with a primary care provider or visit the emergency room. You should go to the hospital or seek medical attention for these kidney stone symptoms: A sharp pain in the side, back or lower abdomen; Pain when urinating; Blood in the urine (hematuria) Fever or chills
Yes, lifestyle changes can help prevent kidney stones. These changes include drinking plenty of water to stay hydrated, reducing intake of sodium and animal protein, and increasing intake of fruits and vegetables. Your doctor may also recommend taking calcium and vitamin D supplements.
Kidney stones send more than one million Americans to the emergency room every year. If you or a loved one is in need of kidney stone relief, treatment or even kidney stone removal surgery, our urologists will develop a personalized care path to help provide you with the best care possible. ... Learn more about virtual visit. Find a Doctor. 1 ...
(Updated 2022) Kidney stone removal, or lithotripsy, uses shock waves or lasers to break down stones in the kidney, gallbladder, or ureters.Kidney stone removal costs can vary. One of our community members shared several prices for treatment via our site, and we started a conversation focusing on both his experience and his kidney stone removal cost.
Men (497 per 100,000) were more likely than women (369 per 100,000) to have an ED visit for kidney stone disease. Approximately 43 percent of all kidney stone-related ED visits were for women (table 3). However men and women had identical rates of ED visits resulting in a hospitalization (85 per 100,000).
A recent study highlights huge price swings in patient charges for the 10 most common outpatient conditions-including kidney stones and urinary tract infection-in emergency rooms across the country.
Overview You have come to the emergency department and the emergency doctor has recommended an imaging test to check for kidney stones. This summary will tell you about two types of imaging tests—a CT scan (computed tomography scan) and an ultrasound. Kidney Stones and Possible Symptoms The kidneys are bean-shaped organs that filter the waste chemicals out of your blood and make urine.
In addition to pain, kidney stones can cause other symptoms: ( 6, 7, 8) Nausea and vomiting. A strong need to urinate. Urinating more frequently. Urinating small amounts. A burning sensation or ...
The average cost of a visit to the ER for over 8,000 patients across the U.S. was $2,168. ... Of the top ten most common reasons for ER visits, treating kidney stones was most expensive, on ...
Out-of-pocket patient charges ranged from $4 to $24,110 for sprains and strains; from $15 to $17,797 for headache treatment; from $128 to $39,408 for kidney stone treatment; from $29 to $29,551 for intestinal infections; and from $50 to $73,002 for urinary tract infections. While the study was not designed to evaluate specific reasons behind ...
The lifetime prevalence of kidney stone formation has been estimated at anywhere from 1% to 12%, with the probability of having a stone varying according to gender, race, age, and geographic location. 3,4 A population-based cross-sectional survey of 15,364 United States residents from 1976-1994 established a 5.2% prevalence of kidney stones, an ...
Purchase a Kidney Stone Removal (PCNL) today on MDsave. Costs range from $12,419 to $18,863. Those on high deductible health plans or without insurance can save when they buy their procedure upfront through MDsave. Read more about how MDsave works. Search board-certified providers, compare prices, buy online, and save money.
Cost $13,000! : r/KidneyStones. Don't go to the ER! Cost $13,000! : r/KidneyStones. Don't go to the ER! Cost $13,000! I know the pain is the worst you ever felt. But I just got a $13,000 bill from the ER for going because of my Stone. It included a CT Scan and getting toradol. My insurance covered $10,000.
The acute passage of a kidney stone is the 9th most common cause of emergency room visits. Approximately 7-8% of women and 11-16% of men will have stone disease by age 70. The acute syndrome complex called renal colic implies obstruction of the collecting system or ureter, and the most common cause of obstruction is a kidney stone. Kidney stone colic is relatively constant in contrast to ...
If you have insurance and already met your deductible: The amount you'll pay varies by insurance plan. However, emergency care generally costs a lot more than urgent care. The average copay for a trip to urgent care is $40-65. And the average copay for a trip to the ER is $100-$150. The price also goes up if you have coinsurance.
Among more than 128,000 patients discharged from emergency care, 11% had at least 1 additional emergency visit for kidney stone treatment.
RESULTS. The study population consisted of 128,564 subjects who had initial treat-and-release visits to EDs for kidney stones during the study period ( Table 1 ). Among these, 61% were male and over 80% were aged between 18 and 59 years. Nearly two-thirds were white, non-Hispanic, and an additional 25% were Hispanic.
After all, medical care costs what it costs, right? ... the total cost of treatment for kidney stones in the ER ranged from $29 ... Since you can't exactly find a Groupon for your next ER visit, ...
On average, enrollees in large employer health plans who have an emergency department visit spend $646 out-of-pocket on the visit. There is significant variation in emergency department spending, with 25% of visits costing over $907 out-of-pocket and another quarter costing less than $128 out-of-pocket.
During this visit, your child's provider will do a physical exam. And they'll order an ultrasound to see inside your child's kidneys and urinary tract. ... Kidney stones larger than 5 millimeters often don't move as easily through their urinary system. Sometimes, even smaller stones won't be able to pass in your child's pee.
A 2023 study published in the American Journal of Kidney Diseases reported emergency room visits to New York state ... Kidney stone rates in the United States increased from 3.8% in the late 1970s ...
1 review and 2 photos of CAROLINA FOREST ER "Another 6am visit to the ER. Kidney stones this time. Check in was easy with a kiosk. Was roomed fairly quickly and meds administered in a timely fashion. All the nurses were extremely helpful. The doctor on duty even called a specialist to verify my kidneys were not going to sustain permanent injuries due the high readings we was getting.