- FOR PROFESSIONALS
- PATIENT PORTAL
- TELETHERAPY
We have beds available!

How To Help Someone Having a Bad Trip, According to Medical Professionals
When someone takes a psychoactive substance like a hallucinogen or cannabis , they often experience a trip. A trip is a set of hallucinations and other psychological symptoms that come from using a substance. Some psychoactive trips can be pleasant, but others lead to troubling experiences and mental status changes. If a loved one uses a drug and has a bad trip, it’s important to know how to help the person through the ordeal.
What Are the Signs of a Bad Trip, and How Can They Be Avoided?
Signs of a bad trip are very subjective based on what the person is hallucinating and if they perceive it as concerning, scary, dangerous, or otherwise uncomfortable. Common signs of a trip, which may be bad for some, include :
- Hallucinations
- Intensified sensory experiences
- Changes in awareness of time
Risk factors have been identified for bad trips, especially those related to psilocybin (shrooms). Researchers have found that mental health symptoms like neurosis make a person more likely to have a bad trip.
When to Seek Medical Attention
If ever in doubt whether someone is having a bad trip, contact poison control at 1-800-222-1222 or by chat here .
However, some symptoms warrant a call to 911. If you or a loved one experience any of these symptoms, call 911 immediately. You will not get in trouble for saving someone’s life, even if you have been taking drugs yourself:
- Increased heart rate
- Increased blood pressure
- Increased breathing rate
- Excessive sweating
- Being a danger to oneself or others
Step-by-Step Instructions on How To Help Someone Experiencing a Bad Trip
The most important ways you can help someone overcome a bad trip are calmly supporting them throughout the trip and calling for help when necessary.
Step One: Recognize That the Person Is Having a Bad Trip
The first step in overcoming a problem is identifying it. If a person has a bad trip, having someone else there to realize there is a problem is vital.
Step Two: Make Sure the Person Is in a Safe Place
Having a bad trip can be very scary. The person may feel out of control physically and mentally. Ensure they are in a place where they can work through their trip safely.
Step Three: Calmly Explain to the Person Why They Are Feeling the Way They Do
A person having a bad trip may not remember taking a substance and be unaware they are on a trip. Calmly reminding the person that they took a drug and are in a safe place while going through its effects can help keep them calm.
Step Four: Stay With the Person During the Trip
Being a source of safety and staying with the person through their bad trip can help keep them physically and mentally safe during the experience.
Step Five: Protect Others
Upsetting hallucinations during trips can make a person a danger to themselves and others. Make sure the person experiencing the trip stays calm and stays away from others, for their safety.
Step Six: Seek Help if Needed
Despite your best efforts, sometimes a person having a bad trip may become a danger to themselves or others or have physical symptoms like a fever that require medical attention. The best thing you can do at that time is to call 911 and refer the person to medical experts who can help them through the rest of the trip.
How Long Will a Bad Trip Last (By Drug Type)?
An unpleasant experience with a drug usually lasts just as long as a good experience. However, a trip can last different lengths depending on the drug taken.
- What can happen during a bad trip? Many different things can happen during a bad trip. Often, the person has troubling hallucinations. However, other symptoms like fever, fast heart rate or panic can also occur.
- What to do if someone has a panic attack? If someone has a panic attack while on a bad trip, you should try your best to calm and reassure them that they are safe. If they remain agitated and you fear they are a danger to themselves or others, you should seek emergency medical attention and call 911.
- What to do if someone becomes overheated and dehydrated? If a person becomes overheated or dehydrated, you should call 911. The person may need intravenous fluids or medical assistance to get their temperature back to normal.
If you or someone you love struggles with substance misuse and has a bad trip, this may be a sign of addiction. Contact our intake experts at The Recovery Village today to learn how we can help.

National Institute on Drug Abuse. “ What are marijuana’s effects? ” July 2020. Accessed September 25, 2022.
National Institute on Drug Abuse. “ Hallucinogens .” November 2021. Accessed September 25, 2022.
Drugs.com. “ Ketamine .” Accessed September 25, 2022.
Drugs.com. “ Bath Salts .” Accessed September 25, 2022.
Drugs.com. “ Mescaline .” Accessed September 25, 2022.
Drugs.com. “ Synthetic Cannabinoids (Synthetic Marijuana, Spice, K2) .” Accessed September 25, 2022.
Drugs.com. “ MDMA (Ecstasy/Molly) .” Accessed September 25, 2022.
Drugs.com. “ Psilocybin (Magic Mushrooms) .” Accessed September 25, 2022.Barrett, Frederick S.; Johnson, Matthew W.; Griffiths, Roland R. “ Neuroticism is associated with challengi[…]psilocybin mushrooms .” Personality and Individual Differences, June 7, 2017. Accessed September 25, 2022.
The Recovery Village aims to improve the quality of life for people struggling with substance use or mental health disorder with fact-based content about the nature of behavioral health conditions, treatment options and their related outcomes. We publish material that is researched, cited, edited and reviewed by licensed medical professionals. The information we provide is not intended to be a substitute for professional medical advice, diagnosis or treatment. It should not be used in place of the advice of your physician or other qualified healthcare providers.
We can help answer your questions and talk through any concerns.
What It's Like to Trip on DMT

How to Set an Intention for Your Drug Trip
What is dmt, how do people make, buy, and use dmt, how mixing mushrooms and mdma affects your body and brain, what is it like to take dmt, some pointers for not overdoing it on party drugs if it’s been a while, can you use dmt for medical purposes, why and how does dmt naturally occur in our bodies, people are using ketamine at home to escape their pandemic reality, are there any new developments in the scientific study of dmt, one email. one story. every week. sign up for the vice newsletter..
By signing up, you agree to the Terms of Use and Privacy Policy & to receive electronic communications from Vice Media Group, which may include marketing promotions, advertisements and sponsored content.

Using ‘trip killers’ to cut short bad drug trips is potentially dangerous
Professor of Neuropharmacology, University of Central Lancashire
Disclosure statement
Colin Davidson has previously received funding from the National Institute on Drug Abuse (NIH, USA) and the European Community for projects related to stimulant drug abuse and novel psychoactive compounds respectively. He is currently a paid consultant with the Defence Science Technology Laboratory (MOD) working on new psychoactive compounds.
University of Central Lancashire provides funding as a member of The Conversation UK.
View all partners
As interest in psychedelics has grown, so has interest in ways to end a bad trip. Recent research reveals that people are giving potentially dangerous advice on social media on how to stop a trip that is less than pleasurable.
Psychedelics cause changes in a person’s perception of reality. One of the earliest descriptions of a psychedelic experience in western literature can be found in Aldous Huxley’s 1953 book The Doors of Perception . Huxley describes mostly beautiful visions while tripping on mescaline.
And then there were the Beatles seeing “tangerine trees” and “marmalade skies” and “a girl with kaleidoscope eyes”.
The last few years have seen a resurgence of illicit use, not only of established psychedelics, such as LSD and magic mushrooms (psilocybin), but also of the novel psychoactive substances that are psychedelics, such as AMT, 5-MeO-DALT, mCPP and methoxetamine.
There is also renewed interest in studying these drugs as treatments for mental health conditions, such as post-traumatic stress disorder (PTSD) and depression. Even a single dose of these drugs appears to have long-term therapeutic effects.
But not all trips are pleasurable. Research shows that if someone is in a bad mood or depressed then they are more likely to have a bad trip , as are people who take too high a dose.
This sort of experience might include extreme fear, time standing still and mood swings. Very high doses of LSD can also cause agitation, vomiting, high blood pressure, hyperthermia and other nasty side-effects. But at regular doses, psychedelics are relatively safe .
To mitigate against bad trips, people will often take the drug in a relaxing and safe environment, and they might include a friend, or “trip sitter” to look after them for the duration of the trip. This was a common practice in the 1960s among people taking psychedelics.

Trip killers
More recently, though, some psychedelic users have been turning to “trip killers” to end a bad trip. These are drugs that can either block the direct effects of the psychedelic or simply reduce the anxiety associated with a bad trip.
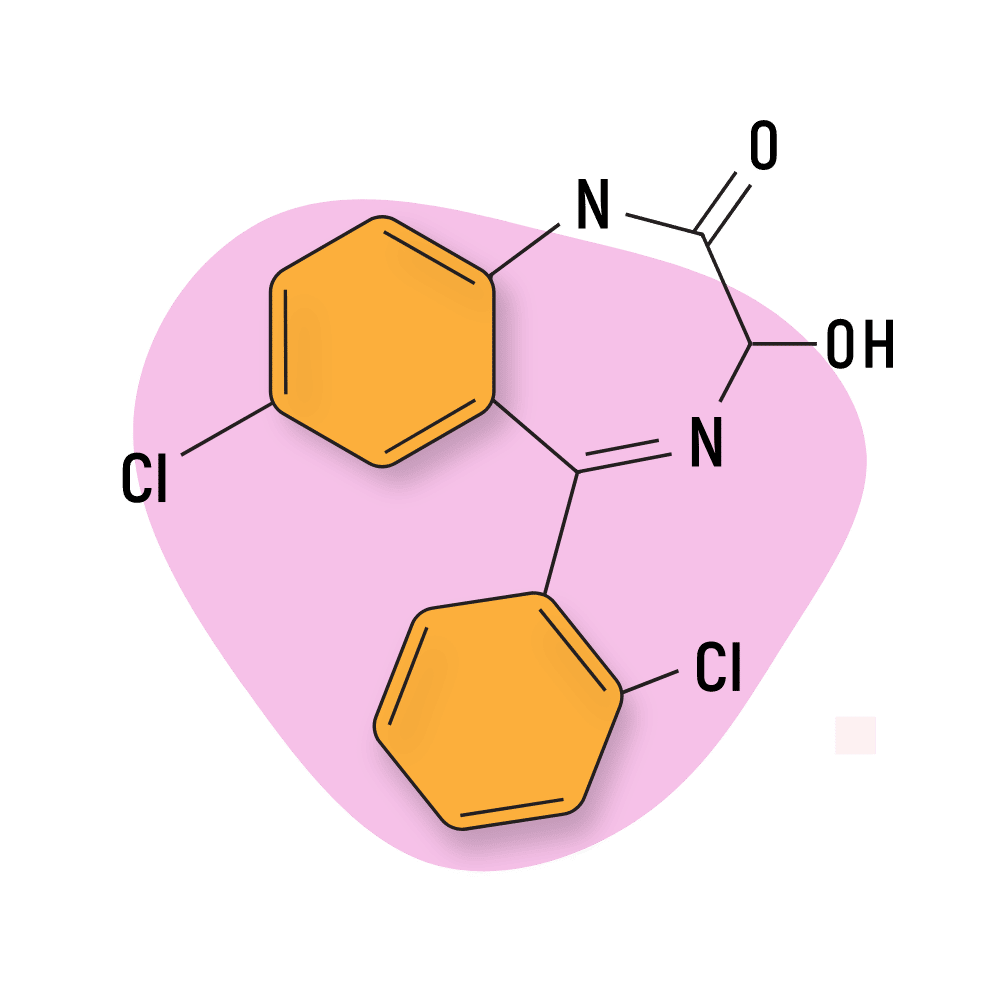
Few clinical studies have examined trip killers, but one has found that ketanserin – a drug used to treat high blood pressure – reverses the psychedelic effects of LSD.
A recent article in the Emergency Medical Journal analysed posts on Reddit about trip killers. The researchers found 128 threads with 709 posts from 2015 to 2023.
Trip killers were discussed most often for LSD (235 posts), magic mushrooms (143 posts) and MDMA (21 posts). The most commonly suggested trip killer was Xanax (an anxiolytic) followed by quetiapine (an antipsychotic), trazodone (an antidepressant) and diazepam (an anxiolytic). Alcohol, herbal remedies, opioids, antihistamines, sleep medication and cannabinoids were barely mentioned.
Receptor blocking
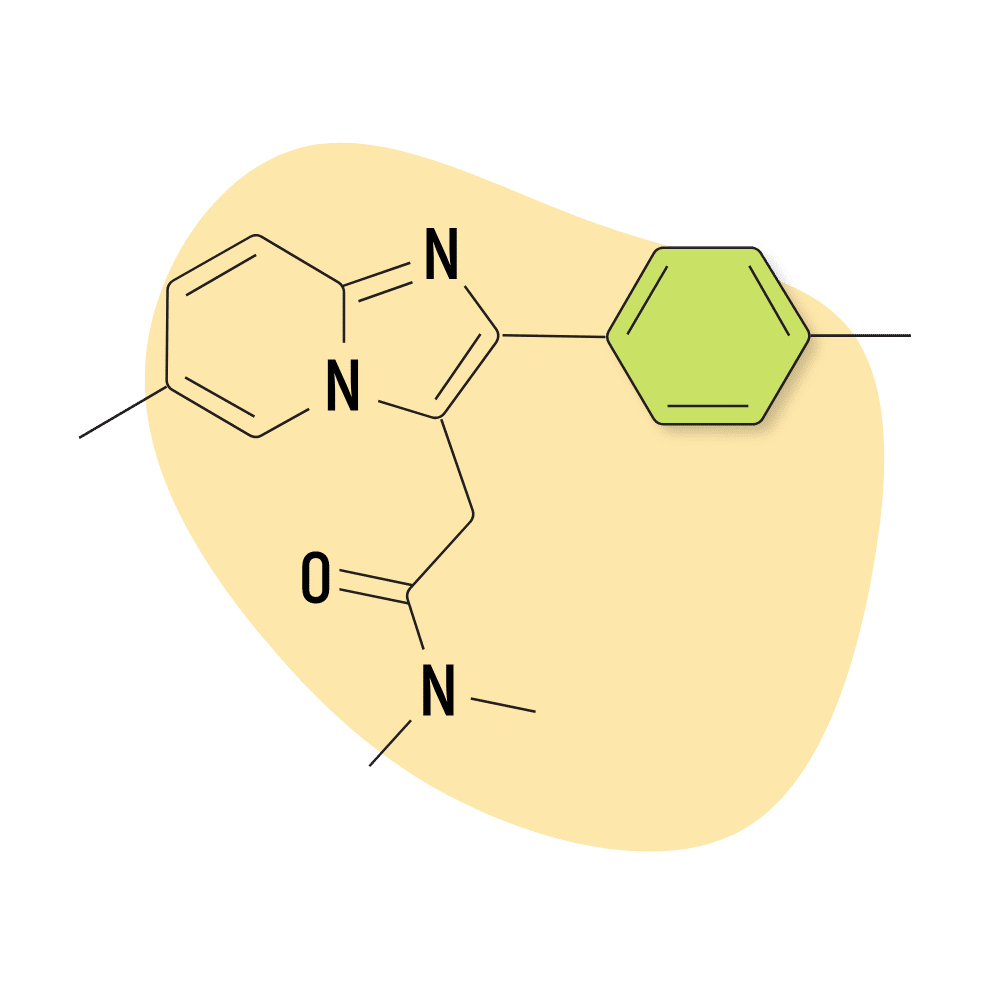
LSD and magic mushrooms create their effects by activating certain proteins in the brain. These are called 5-HT2A receptors and are usually activated by the neurotransmitter serotonin (5-HT). There are 14 known 5-HT receptors, but psychedelics have specific activity at only the 5-HT2A subtype.
To kill a trip then, one simply has to give the drug user another drug that blocks (rather than activates) the 5-HT2A receptor. Many prescription drugs can do this and they tend to be antipsychotic drugs .
Quetiapine from the list above is one popular example, while another antipsychotic, olanzapine, was mentioned in 14 posts in that study. Similarly, the atypical antidepressants trazodone and mirtazapine also block the 5-HT2A receptor.
One can think of these trip killers as working in the same way that naloxone would be used for heroin or fentanyl overdose. These drugs activate mu opioid receptors in the brain, while naloxone blocks these receptors. Naloxone is therefore used to treat life-threatening respiratory depression from opioid overdose.
Another option for the psychedelics would be to decrease the anxiety associated with the trip by taking anxiolytics, such as benzodiazapines – alprazolam (Xanax) and diazepam (Valium) being the most popular in the posts analysed above. These would also help the drug taker to fall asleep.
Some of the trip-killing drug doses suggested in the Reddit posts were high. For example, quetiapine was suggested to be used at 25mg to 600mg, but clinical guidance for these drugs suggests a single dose of up to 225mg.
The doses suggested on Reddit for alprazolam are 0.5mg to 4mg but the clinically suggested maximum dose is usually 2mg to 3mg. Four milligrams could cause low blood pressure, oversedation and respiratory depression. Unfortunately, benzodiazepines are also highly addictive and can lead to overdose deaths.
People who turn up at A&E suffering from a bad trip or overdose of a psychedelic will be reassured in a calm environment. If that doesn’t work, they are likely to be given an antipsychotic or low-dose benzodiazepine, at a clinically advised dose.
Read more: A brief history of drug-fuelled combatants
- War on Drugs
- Psychedelics
- Richard Nixon

Research Fellow – Magnetic Refrigeration

Centre Director, Transformative Media Technologies

Postdoctoral Research Fellowship

Social Media Producer

Dean (Head of School), Indigenous Knowledges
Trip Killers: How To Stop an Acid Trip
Occasionally, a psychedelic trip can take a turn for the worse. This group of “trip killer” drugs are used by experienced trip sitters and medical professionals to stop the trip in its tracks.
What Are Trip Killers?
1. alprazolam (xanax), 2. lorazepam (ativan), 3. diazepam (valium), 4. clonazepam (klonopin), 5. zolpidem (ambien), 6. quetiapine (seroquel), 7. olanzapine (zyprexa) , how long do trip killers take to kick in, psychedelics that have trip killers, psychedelics that don’t have trip killers, 1. are you in over your head, 2. are you or those around you at risk, 3. do you need to sober up asap, who shouldn’t use benzodiazepine-based trip killers, 1. the “bad trip”, 2. you or your trip sitter realize it’s time for a trip killer, 3. you enter “the placebo effect”, 4. the trip killer begins to take effect, 5. the trip comes to an end , 6. you feel almost sober, 1. sourcing the trip killers responsibly, 2. get the dose right, set (mindset), final word: using trip killers .
In most cases, “a bad trip” is just your mind’s way of showing you factors in your past or present life that need to be confronted and dealt with. However, in some cases, a bad trip can become nightmarish to the point that it may put yourself or others in danger.
In these situations, it may be beneficial to have some form of a trip killer on hand to get you out of the negative headspace and effectively “kill” the trip.
Let’s delve into what trip killers are, when to use them, explore the risks, and discuss what to expect when you use one halfway through a psychedelic journey.
Trip killers are substances that help mellow out or block the effects of psychedelic substances. They “bring you back to reality” when a trip takes a dark turn.
Trip killers are taken with the intent to end a psychedelic trip. There is no one substance that will help end a psychedelic experience, and not all trip killers are effective for all psychedelics — you have to use the right trip killer depending on what substance you’re using.
The most common trip killers are benzodiazepines, but other drugs, such as certain antipsychotic medications, can also be effective.
Just as it’s important to know the right dose of the psychedelic you’re using, it’s important to take the right dose of trip killers too. Some of these substances are exceptionally potent and should be taken with great care.
Trip killers are a last resort and should only be used when the effects of a bad trip start to become dangerous to oneself or others.
Ideally, people who are at risk of such an experience will be under the supervision of a trained psychedelic facilitator who can help walk the user through the challenging visions they may be receiving. In many cases, the bad trips are where most of the benefits of psychedelics derive from — so stopping them in their tracks should be avoided if possible.
Top 7 Trip Killers
By far, the most effective and commonly used trip killers are benzodiazepine drugs . We’ll look at these substances first because they offer the strongest and fastest-acting way to end a psychedelic experience.
Benzodiazepines aren’t for everyone; some people should avoid them entirely. In these cases, there are other options available (keep reading).
It’s important to note that benzodiazepines can be dangerous, especially if mixed with other sedative drugs or alcohol. They’re also notoriously addictive. Taking benzos habitually doesn’t end well for anybody.
For now, let’s take a look at the most common trip killers:
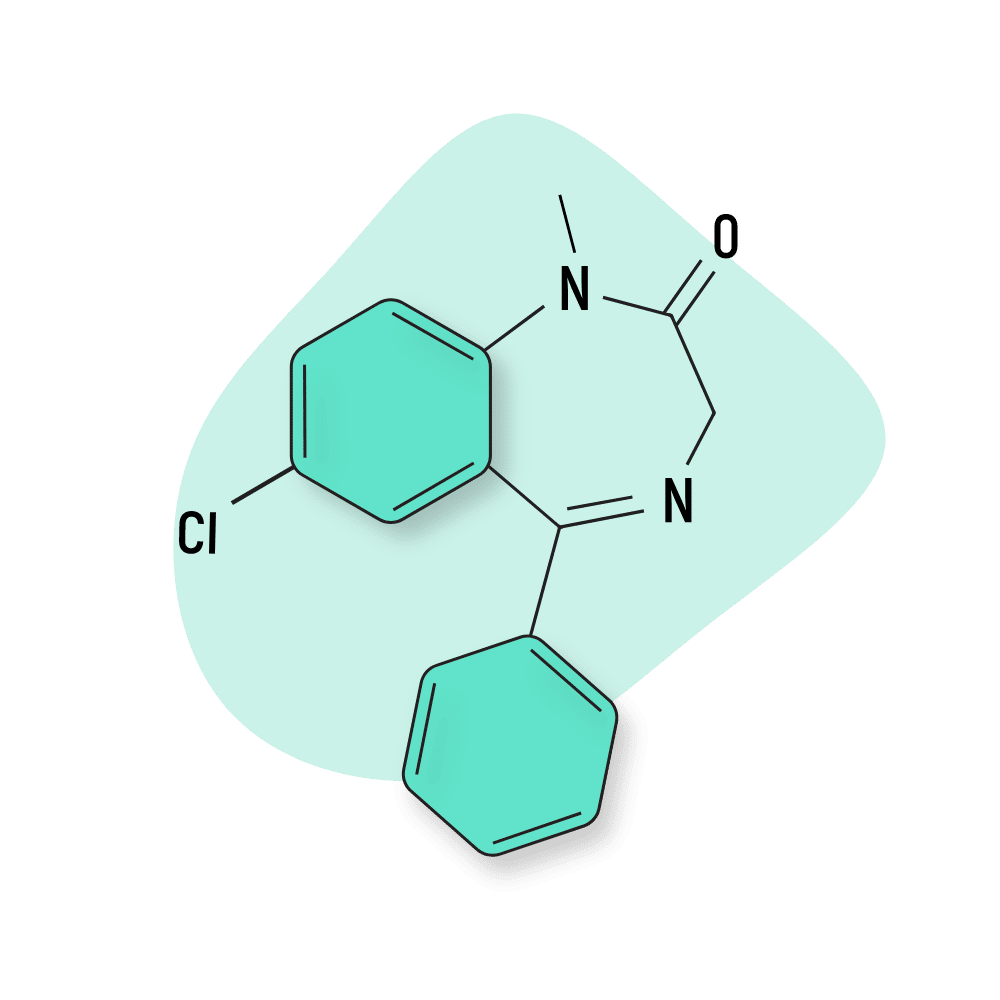
Alprazolam is one of the fastest-acting trip killers in the benzodiazepine family — but it’s also one of the shortest-lasting. The effects of Xanax, although fast-acting, only last for around four to six hours.
Xanax is a favored trip killer among psychonauts purely because of its fast-acting nature. It’s designed for people to use at the first sign of an anxiety attack to stop it in its tracks.
The effects of alprazolam start to kick in within 15 minutes or so and reach peak effects in as little as 45 minutes.
Xanax does have a habit of wiping your memory, in a sense. When consumed with other substances or at too high a dose, it can make you black out and lose all memory of the previous night.
When you consume Xanax as a trip killer, you should be prepared to lie down and get some rest. When you awake, you may have an extremely blurry memory and struggle to recall anything about the experience. This can be a positive or negative point, depending on what you want to achieve from the psychedelic trip.
Lorazepam is considered an intermediate-acting benzodiazepine. This means it won’t kick in quite as fast as something like Xanax — but the effects last for over eight hours. This is a better option for long-lasting psychedelics, such as DOX compounds, 2CX compounds , or other amphetamine psychedelics .
Lorazepam is great for getting you out of a bad trip, but it may cause drowsiness to the point you fall asleep. This can be a plus since it allows you to rest easy after a bad experience, but it does put a complete halt on your psychedelic experience.
Diazepam isn’t as fast-acting as lorazepam and alprazolam, but it is one of the longest-lasting of the popular benzodiazepine trip killers. The effects of diazepam can last for over 12 hours.
It’s reported that this trip killer takes “too long” to take effect when swallowed in pill form. However, the onset of effects can be sped up significantly by chewing the drug, so it can be sublingually absorbed under the tongue.
Diazepam works great to get you out of a nightmarish thought loop, but it doesn’t have the same effect as lorazepam and alprazolam in the aspect of drowsiness. Many people report that taking diazepam during a bad trip helps them calm down without completely removing the psychedelic effects of the drug.
Clonazepam is considered the slowest-acting of the benzodiazepine trip killers. It can take between one and four hours after taking it to reach peak levels in the blood. Of course, this can be sped up by chewing the pill and allowing it to absorb sublingually.
Although clonazepam takes a long time to kick in, the effects can last up to 12 hours, and the half-life is also long, standing at around 40 hours — meaning it won’t be cleared from the body for a couple of days.
This is the least popular of the common benzodiazepine trip killers, but it’s often one of the easiest to get hold of (depending on where you live). Some like Klonopin for its euphoric nature, which many other benzodiazepines don’t have.
Zolpidem is classified as a Z-drug — which is a group of compounds that exert benzodiazepine-like effects but have an entirely different structure.
These drugs work in much the same way as benzos and are also considered useful as trip killers. But there’s one catch — these drugs tend to be much more sedative than their benzodiazepine cousins. People who take Ambien to stop a trip will almost always fall asleep shortly after. You may or may not remember the experience the following morning.
While Z-drugs carry a lower risk than most benzodiazepines, there’s still a great deal of risk associated with their use. Getting the dose right, avoiding mixing with other depressants, and only using if you’ve been approved by a doctor are still key elements for using these substances safely.
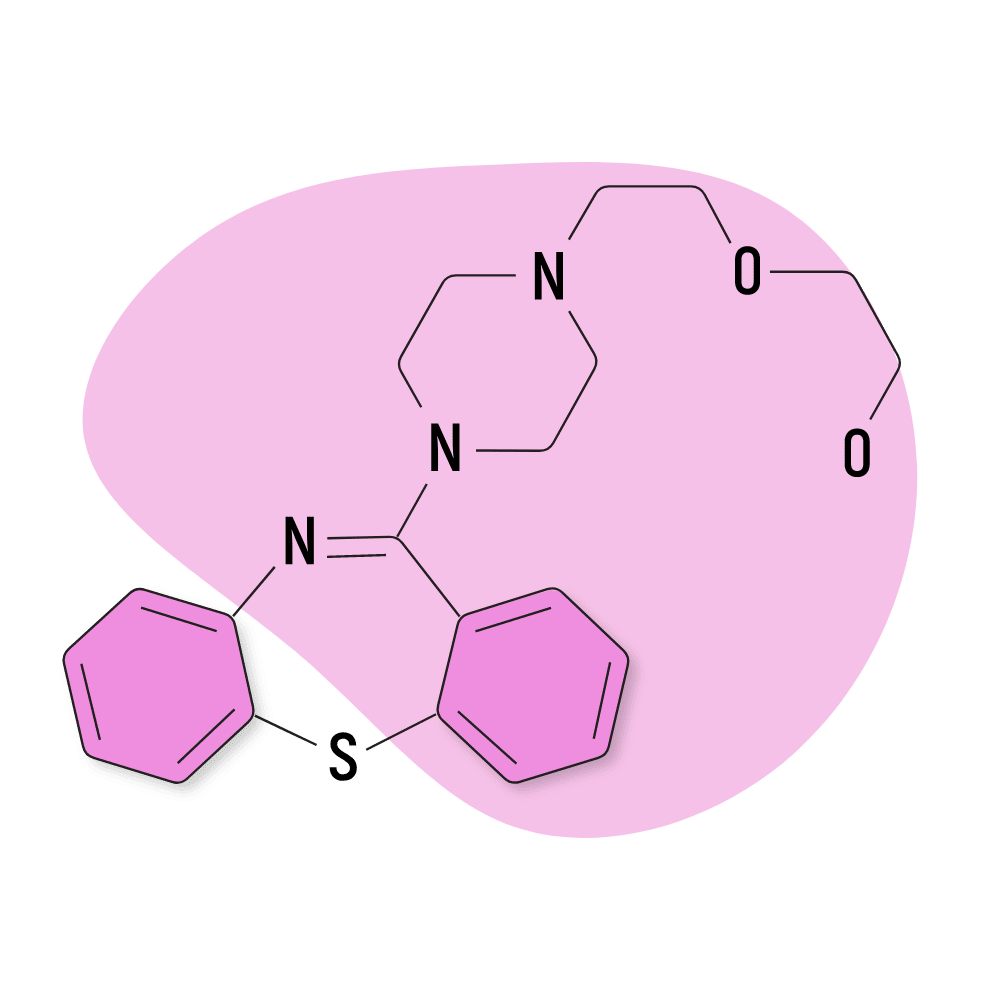
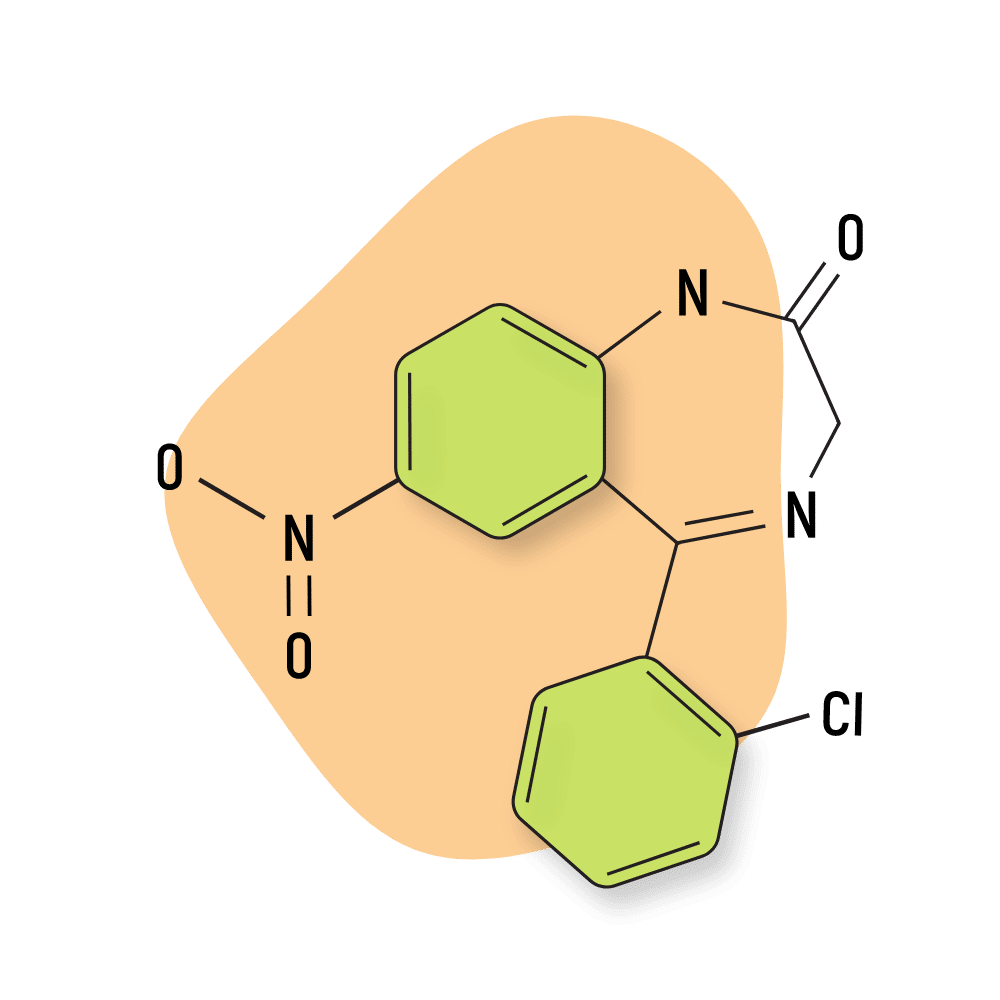
Although nowhere near as popular as benzos, another common option is antipsychotics like quetiapine (Seroquel).
Antipsychotic medications treat psychosis. People with schizophrenia, bipolar disorder, severe depression, and Alzheimer’s are often prescribed these.
Quetiapine is classified as an atypical antipsychotic. It differs from typical antipsychotics because it produces fewer extrapyramidal symptoms and has a lower risk of tardive dyskinesia. In simpler terms, it produces fewer side effects than typical antipsychotics, such as the inability to sit still, muscle contractions, tremors, and stiff muscles.
Antipsychotics are the best trip killers for people that can’t use benzodiazepines or Z-drugs.
Seroquel typically takes 20 to 60 minutes to kick in when consumed sublingually at a dose of around 25–50 mg.
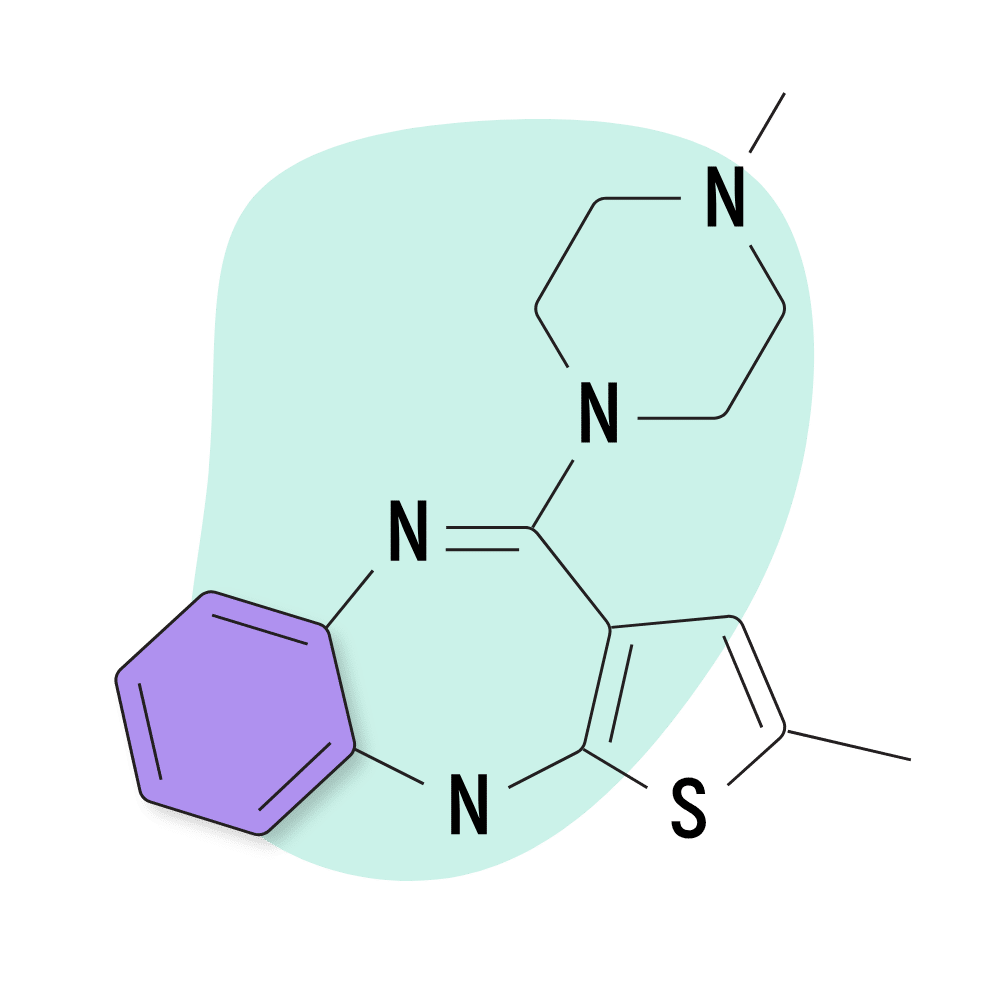
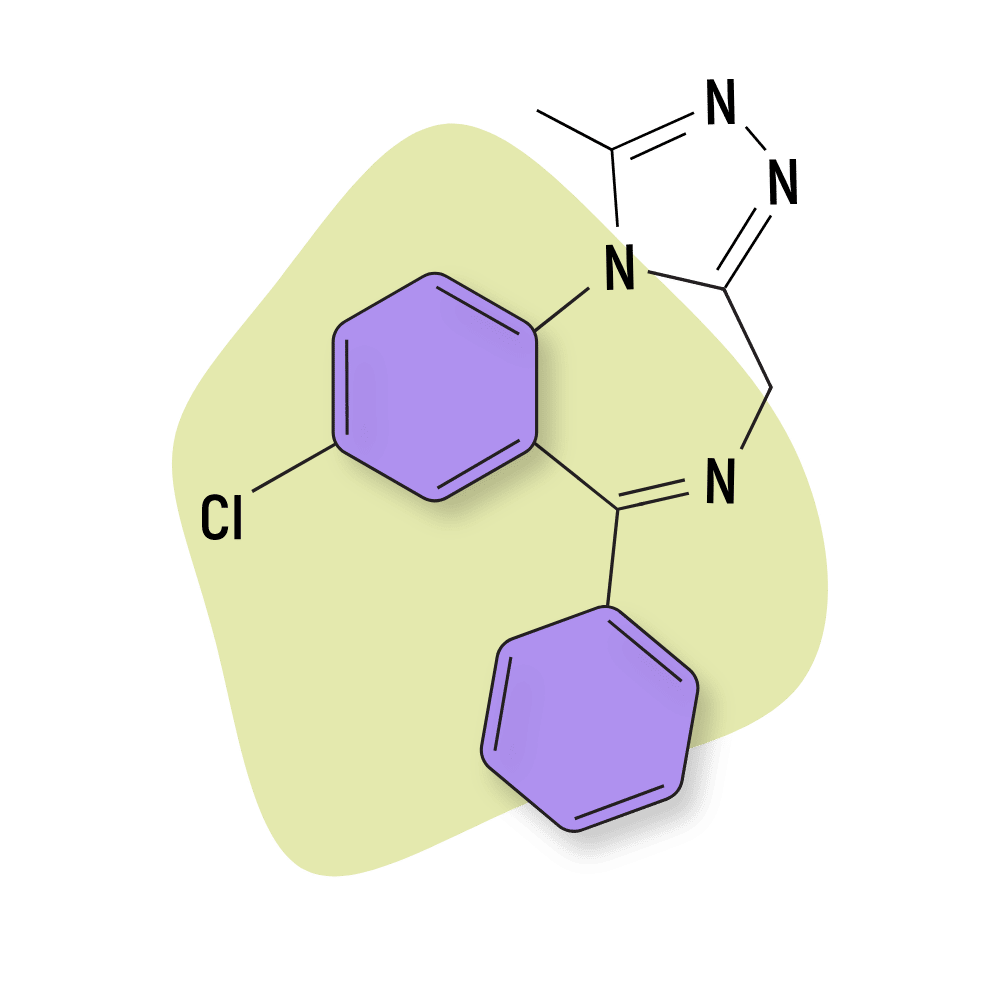
Olanzapine is another atypical antipsychotic reported to be effective in dulling the effects of psychedelics. This compound has a particularly high affinity for the 5HT2A receptor and is, therefore, better for killing the trips from tryptamine-based psychedelics like LSD, psilocybin, or DMT.
Zyprexa is less effective for dopaminergic or NMDA-based psychedelics such as the psychedelic amphetamines (MDMA, MDA, cathinones) or arylcyclohexylamines (PCP, ketamine, and others).
Olanzapine usually takes around 30 minutes to kick in at a 10–20 mg dose.
How Do Trip Killers Work?
Benzodiazepines such as diazepam or lorazepam (or other sedative anxiolytics) are usually the substances a doctor will administer if you’re submitted to the hospital due to signs of psychosis from consuming too much of a psychedelic substance.
These drugs work similarly to those for someone with a panic or anxiety attack. They have anxiolytic, sedative, and relaxant properties that all work to reduce anxiety levels and negative thought loops.
More specifically, benzodiazepines kill the trip by amplifying the activity of GABA in the brain. GABA is a neuroinhibitor — which means it reduces brain activity.
When we’re anxious, the inhibitory effects of GABA result in a dramatic reduction in anxiety levels. We think less, care less about our problems and feel more calm and relaxed. In higher doses, this causes full-on sedation.
The same concepts apply to psychedelic experiences. Paranoia, anxiety, and fear responses experienced during the psychedelic state can all be muted by dulling brain activity with GABA-boosting drugs.
Antipsychotic trip killers work a little bit differently. These drugs work as serotonin and dopamine antagonists (blockers). The exact mechanism is still not fully understood, but the leading theory is that certain antipsychotics reverse the effects of psychedelics by blocking the 5-HT2A receptors.
5-HT2A is one of the main receptor sites on which psychedelics such as LSD and psilocybin work. Some, but not all, psychedelic substances bind to these receptors to induce their psychedelic effects.
Every trip killer is different — some kick in quickly (10–20 minutes); others take an hour or more.
Here are some of the average onset times for the four most popular benzo-based trip killers listed above.
These refer to the oral onset time of these drugs. It’s not a good idea to smoke, inject, or snort benzodiazepines for any reason.
- Alprazolam (Xanax): 10–20 minutes
- Lorazepam (Ativan): 20–45 minutes
- Diazepam (Valium): 1–2 hours
- Clonazepam (Klonopin): 45–60 minutes
When Do Trip Killers NOT Work?
Trip killers don’t work on every psychedelic substance. Benzodiazepines and antipsychotic medications are effective for standard, serotonin-based psychedelics such as LSD and psilocybin. However, there are a few substances that don’t have any effective trip killers.
Always educate yourself on any substance before using it. You should know how much to take, what to expect during the trip, and onset times and duration. You should also know whether there’s an effective trip killer for it.
Psychedelic trips from some of the most commonly used psychedelics can be stopped by the use of benzodiazepines or antipsychotic medications.
These are the most prevalently used and have the most research surrounding them, though trip killers likely work on more substances than the ones listed below.
Here’s a list of commonly used psychedelic substances that do have effective trip killers:
- LSD (lysergic acid diethylamide) (and other lysergamide psychedelics )
- Psilocybin (the active compound in magic mushrooms )
- 4-AcO-DMT (synthetic shrooms)
- 5-MeO-DMT (the active compound in bufo toad venom )
- N,N-DMT (the active ingredient in ayahuasca )
- 2C-B (and other 2C psychedelics )
- NBOMes (N-bombs)
- Synthetic Cathinones (Bath Salts)
- MDMA (and other MDXX psychedelics )
- Mescaline (the active compound in Peyote & San Pedro cactus)
Some psychedelic substances do not have trip killers. Not all psychedelics affect the brain in the same way; therefore, trip killers, such as benzodiazepines, will not end all psychedelic experiences.
For example, many dissociative drugs like PCP or ketamine work via the NMDA receptors in the brain. The psychedelic trips these drugs produce appear to be unaffected by benzodiazepines. Making matters worse, most dissociatives are also considered sedatives — which are notoriously dangerous to mix with benzodiazepines.
Other substances, such as salvinorin A from salvia or any of the deliriant hallucinogenics, don’t diminish after taking benzodiazepines or Z-drugs. There are no effective trip killers for these substances.
If you plan on consuming any of the substances listed below, be warned that you have no option but to ride the experience out naturally. Never consume a substance that you’re not comfortable with.
It’s a good idea to have a trip sitter around that you trust who can help you through a difficult experience should it arise.
Here are some of the more common psychedelic substances that do not have effective trip killers:
- Datura (a hallucinogenic flower from the nightshade family)
- Brugmansia (commonly known as angel’s trumpet)
- Phencyclidine (and other arylcyclohexylamines )
- Ketamine (and other dissociatives )
- Grayanotoxins (found in Rhododendron flowers)
- Xenon gas or nitrous oxide gas
- Salvia divinorum

When Should You Use a Trip Killer?
Preferably, you should never consume a trip killer. A “bad trip” can often unlock a door that will show you traits in our personality (our “ shadow ”) or traumas and aspects in life that we need to heal in order to live a better life.
A typical “bad trip” is often a lesson containing vital information we can use to work on ourselves and get over mental blocks that reduce our quality of life. Using a trip killer to end an experience like this may be counterintuitive. Doing so could close “the door” that leads to healing.
Many experienced psychonauts swear off ever needing to consume trip killers to end a trip because they believe every vision has value. However, trip killers definitely have their place. You should always be safe rather than sorry and never bite off more than you can chew in terms of set, setting, and dosage. End the trip if you feel you’re in over your head.
As long as you use psychedelics responsibly , you’ll likely never need a trip killer. Proper dosing is the best way to ensure this, but having your frame of mind and setting fit for a psychedelic trip is also important. This way, if a bad trip occurs, you have the strength to deal with it.
Sometimes, we don’t get it right. A “bad trip” can spiral out of control into a nightmarish event that can be truly traumatic. When this happens, you and the others around you could be at risk.
People who swear off trip killers may have experienced a challenging trip but may not have had a truly terrifying one. It may never happen, but it could occur at any time, so it’s always wise to have some form of trip killer available.
A nightmarish loop of events during a trip can seem to last forever, and in some, it can lead them to cause harm to themselves or others. This is rare but not unheard of. Trip killers can be a lifesaver for those who find themselves trapped in such a situation.
In our opinion, trip killers should be a part of every psychonaut’s tool kit. You should strive never to use them, but they should be readily available in case a trip takes a dark turn that you feel you can’t benefit from or work through without putting yourself or others at risk.
No matter how responsible you are when planning a psychedelic trip, there are times when circumstances come up that are outside your control. You think you have the day to sit and trip, but suddenly something comes up (family emergency, etc.), and you need to be sober ASAP.
Even though a trip killer won’t make you feel “normal,” it’ll speed up the process and make you more clear-headed than you would be without it.
Some people should avoid benzodiazepine-based trip killers at all costs . This section outlines who should not take these types of trip killers and what they can use instead.
Although most psychedelics aren’t addictive, benzos definitely are. Anyone with an addictive personality or who has had a past dependence on benzos or similar substances should avoid using these as trip killers.
Benzos have some of the longest-lasting, worst, and most savage withdrawals of any substance on the planet.
Withdrawal symptoms can last for months. If you become addicted and prolong the use of these substances, quitting cold turkey isn’t an option. Simply quitting after prolonged benzo abuse can be life-threatening due to the body seizing up.
In simple terms: don’t use benzo-based trip killers if there’s a chance you’ll get addicted to them.

What To Expect When You “Kill” a Trip
As I’ve mentioned, trip killers aren’t an instant solution. You’re not going to magically become sober as soon as the pill touches your tongue. The onset time and experience will vary depending on the type of trip killer consumed, the dosage taken, the psychedelic consumed, and how far into your trip you are.
That being said, I can give you a rough idea of what happens when consuming a benzodiazepine trip killer during a bad experience.
Let’s paint a hypothetical picture.
A few hours after consuming your chosen psychedelic, you enter an area of dark and disturbing thoughts somewhere in your subconscious mind. At first, tell yourself, “It’s okay; it’s just the psychedelic messing with my brain.”
After a while, you start to convince yourself that this is, in fact, real, and you begin to sink into nightmarish thought loops.
If the situation starts to get out of hand, a trip killer might be employed to bring you back to some semblance of reality.
You chew one milligram of Xanax in the hope that the sublingual absorption will allow it to take effect quickly.
Although unpleasant, the acrid taste of the trip killer in your mouth relieves you. You associate the taste with the trip coming to an end. When you swallow your saliva, you feel a wave of calm rush over you because you know that this nightmare will all be over soon.
About 15 to 30 minutes later (depending on the trip killer consumed), you notice a wave of relaxation come over you. Any feelings of anxiety and panic start to wash away as the drug begins to take effect.
Not only do the dark thought loops start to diminish, but you also start to feel as though you don’t care about much of anything at all. You become emotionless and calm. You may or may not continue to experience hallucinations, but none of them seem to steal your attention.
If you’re not laying down already, you’ll probably seek out somewhere to post up and relax for a while as your muscles start to feel weak.
One hour after taking the trip killer, your hallucinations have likely died down substantially, and you feel much more rational and level-headed. You may even regret taking the trip killer — if you were in this head space originally, perhaps you wouldn’t have had such a terrifying experience.
Two to three hours after ingesting the trip killer, you feel more or less sober (depending on the psychedelic you consumed). Most of the effects of the psychedelics have worn off, and if you’re not already asleep, you’re probably feeling pretty drained and ready for some zzz’s.
You’ll be emotionally and physically exhausted by this time, and you’ll likely reach for a bottle of water and a hefty snack to restore the energy lost throughout the ordeal.
Safety Aspects to Consider When Using Trip Killers
There are a few things to consider when purchasing and adding trip killers to your psychedelic tool kit. The most effective trip killers — benzodiazepines — are restricted in terms of sale and use. This can make it difficult to legally purchase these drugs, which is where our first safety aspect stems.
If you cannot obtain trip killers (benzos) in a legal way — via prescription from a doctor — the level of risk goes up substantially.
The most popular benzodiazepines for recreational use are Valium (diazepam) and Xanax (alprazolam). These can be obtained on the black market, but it’s not recommended.
Illegal vendors distributing Valium and Xanax don’t necessarily consider the consumer’s best interest. Several samples of these substances have contained drugs such as fentanyl (an extremely dangerous synthetic opioid).
Clandestine drug manufacturers use tablet molds that produce exact replicas of the prescribed Xanax and Valium tablets. Criminals produce pills with these molds that look the same but contain a cocktail of potentially life-threatening substances. Whether you’re tripping or not, taking one of these pills at any time may pose a serious health risk.
Basically, unless you’re getting your drugs from a pharmacy, you can never be sure the drugs you’re using are safe.
If you absolutely have to purchase “trip killers” from the black market, you must test them using — at the minimum — a fentanyl test kit. We cannot stress this enough.
You can also buy benzo test kits to help identify what adulterants may be contained in your pills.
You should check your benzos before you need them. You’re not going to have time to test them for safety if using them as a trip killer.
Another safety aspect to consider is, of course, dosage. Getting the correct dosages for each substance is critical to avoid overdosing . However, you also need to consume enough of the substance to kill a trip.
Several individual drugs fall under the benzodiazepine classification; although similar, the required dosage for each differs.
It’s important to note that your weight, gender, and familiarity with the drug will affect the exact dose. A heavier person that regularly consumes benzos will need a far larger dose than a small-framed person that has never tried the substance before.
Below I’ve listed the recommended dosages of the four most popular trip killers based on first-hand reports and prescribed dosage guides. However, you should take these numbers with a grain of salt and do your own research outside before consuming anything to kill a trip. These substances can be dangerous.
- Alprazolam (Xanax): 0.5 to 1 mg
- Lorazepam (Ativan): 0.5 to 1.5 mg
- Diazepam (Valium): 5 to 10 mg
- Clonazepam (Klonopin): 1 to 1.5 mg
As you can see, the recommended dosages for killing a trip vary and depends on where you are on your trip.
Again, I can’t stress this enough — everyone’s required dosage will be different because of a variety of factors. Unfortunately, your required dose will be something you’ll have to find out through experience. Just be aware that trip killers of this nature don’t work immediately, so don’t keep dosing if you don’t experience any trip-calming effects right away . This is how overdoses occur.
How To Minimize the Risk of a Bad Trip
Trip killers should only be used in an emergency when a trip takes a dark turn that could harm you or others around you. It’s best to avoid trip killers at all costs, and these steps can also help you have the best trip possible.
Preparation is key. If you’ve experimented with psychedelics before, you must have heard of set and setting.
The set is the frame of mind you’re in. When consuming psychedelic substances, you should never be in a negative, anxious, or unstable state of mind. Entering a trip with negative thoughts in your head is a surefire way to a nightmarish trip.
It’s important to relax your body and mind before entering a trip. This can be done by simply putting yourself in a good headspace by recalling a positive memory or experience. Practicing meditation and/or yoga can also help you relax into a positive state of mind.
The setting is the space you’ll experience the trip in. The setting is extremely important in psychedelics and will help you stay in the right “set.” Playing relaxing music, putting beautiful pictures around you, and lighting a few candles can make the setting more relaxed and inviting.
Many people also like to trip out in nature. This is a fantastic way to do it; however, several variables can affect your trip.
If you head out into nature for a psychedelic trip, ensure it’s in a safe area with no foot traffic. Make sure the weather is good, and there are no external factors that may “freak you out.” The last thing you want is bad weather (a storm, for example) or a stranger entering your space — this will likely lead to a bad experience.
Another way to ensure a smooth trip is to have an object nearby that means something to you. This object helps connect you to the physical world and can get you back on course if your trip dives into a dark place . Simply holding the object and looking at it may just be enough to snap you back to reality.
This technique is definitely something to try before resorting to the use of trip killers.
Trip killers may be an important part of the psychonaut’s tool kit. Hopefully, you will never need to use them, and you should strive to work through difficult experiences rather than chemically halt them.
However, if you have a truly terrifying psychedelic experience, they will help you get back to reality as quickly and safely as possible.
The most popular and effective trip killers are benzodiazepines or Z-drugs, but some antipsychotic medications are also effective and a good alternative for people with addictive personalities.
When sourcing trip killers, it’s important to test their purity. Several drugs on the black market are contaminated with fentanyl — an extremely dangerous synthetic opioid that’s similar to morphine but much stronger. This drug can be life-threatening, so it’s of paramount importance that any drug sourced on the black market is tested thoroughly.
Regardless of whether you have trip killers available, you should always practice safe psychedelic use. Ensuring that your set and setting are perfect before a trip helps mitigate the risk of a bad trip occurring. As we said, you should never need to use a trip killer, but they should be available as an absolute last resort.
How to Make DMT: 3 Separate Methods (N,N,DMT & 5-MeO-DMT)
Can Psychedelics Help With Problem Solving?
The Mind’s Theatre: Psychedelics & Dreams
What is the psilocybin cup (cup winners & strongest strains 2021 & 2022).

How to Make Ayahuasca: Step-by-Step Guide

Where Does Ketamine Come from?
Subscribe for more psychedelics 🍄🌵.
This will close in 20 seconds
How to cope with a ‘bad trip’ or high when using drugs
If you or a friend is experiencing a ‘bad trip’ you can use this advice to navigate the complex and distressing feelings it may bring up.
Written by spunout
Fact checked by experts and reviewed by young people.
People will often use drugs like mushrooms , LSD , MDMA , cannabis and ketamine to feel a sense of euphoria, excitement and wonder. Users will often report that they feel more sociable, find the world around them more fascinating and feel more connected to the universe and others around them when high on certain drugs.
But the feelings caused by recreational drug use are not always positive. The effect a drug will have on you can be difficult to predict, particularly when it comes to psychedelics. Sometimes, users may find themselves feeling panicked, depressed and paranoid during a drug high. This is often referred to as a ‘bad trip’.
What is a ‘bad trip’?
A ‘trip’ is a term used to refer to a drug high. It is most often associated with psychedelic drugs, such as mushrooms and LSD, and may include effects like visual hallucinations or ‘visuals’. The act of being on a trip is called ‘tripping’. Some users also report tripping while taking drugs such as MDMA and ketamine. These drugs can have some psychedelic properties, though they are not typically called psychedelics.
Bad trips are most often associated with psychedelics. It is possible to experience negative emotional side effects with a lot of drugs, even ones that aren’t typically considered to produce a ‘trip’. If you or someone you know is experiencing a bad trip, here are a few ways you can minimise how unpleasant the experience is.
Ensure the person tripping is physically safe
Before proceeding with harm reduction advice, it is important to make sure that the person in question is physically safe. You can use this guide to determine whether a person is experiencing a drug emergency .
When in doubt, it is always best to seek the advice of a medical professional, and to be totally honest with this professional about what the person has taken and how much they have taken.
Being high on drugs will often impair a person’s judgement. In some cases, drugs may also interfere with depth perception, making falls more likely. To minimise the chance of accident or injury, keep the person tripping away from high places, bodies of water, traffic or other physical dangers.
Take the person to a calm, safe environment
If the person experiencing a bad trip is not already in a safe, controlled environment, such as their home or the home of a friend, try to bring them to a place that is peaceful and quiet.
Loud, public settings such as festivals can be difficult to tolerate when under the influence of drugs such as psychedelics. If you are in a public place, you should bring the person tripping to a quieter spot to help them feel more calm. Try to avoid leaving the person on their own.
Some music festivals will have welfare tents or areas where you can bring people who are having a bad trip. The HSE operates welfare tents at some Irish music festivals with on-site volunteers, as do some harm reduction organisations such as Help Not Harm and PsyCare Ireland .
Stay hydrated
It is a good idea to get some water for a person experiencing a bad trip and advise them to take slow sips. They do not need to chug massive amounts of water in a short period of time, taking sips of water is best. Gentle hydration can help with feelings of nausea, and can help to rehydrate the person if they have vomited during the course of their high.
Talk about how you are feeling during your bad trip
If you are experiencing a bad trip, try to be as open as possible about how you are feeling with a trusted friend or loved one. Sharing your experiences can reduce the distress you may feel and may help pull you out of whatever emotional spiral you are experiencing.
If you are caring for someone having a bad trip, gently ask them how they are, and tell them it is okay for them to share and that you would be happy to listen to them. Telling them that it is okay and that you would be happy to listen may help them feel less self-conscious about opening up.
Equally, try not to push someone to speak if they don’t feel comfortable doing so. It is best to just let them know you are here for them and let them make their own choice.
All trips are temporary
It can be helpful to remember, or to remind someone you are caring for, that a drug high will eventually wear off. Drugs can influence the perception of time, so it is easy while experiencing a bad trip to worry that the trip will last an inordinately long time, or will never subside. Reassure the person you are taking care of that what they are feeling will not last forever and that the high will eventually wear off.
Avoid self-medicating
It may be tempting to use other drugs, such as cannabis or alcohol , while experiencing a bad trip, as you may assume that these substances will help you calm down. Introducing more drugs is risky, as how drugs interact with each other isn’t always very predictable, especially if the person having a bad trip has already taken multiple substances, such as mixing LSD and MDMA .
Benzodiazepines (better known by brand names such as Xanax or Valium) are not capable of stopping a psychedelic trip, despite what some myths may suggest. If you present to a doctor or paramedic, they may give you this kind of medication to help you calm down. Introducing prescription drugs should only be done under medical supervision. If you have been prescribed a drug such as a benzodiazepine, only ever use it as indicated by your prescribing physician.
Try some grounding techniques
If you find yourself distressed or panicking while high on drugs, using grounding techniques can help prevent you from getting too overwhelmed by your emotions.
One type of grounding technique called the 54321 technique and relates to the five senses. If you feel like you would not get distressed by thinking too much about your surroundings, you can try these steps:
- First, look around and pick out five things that you can see. In a living room, you might pick a carpet, a television, a mug, a gaming console and a plant. It can help to say each item out loud.
- Look for four things you can touch. This could be the feeling of clothes against your skin, or the grass under your feet, depending where you are. You can reach out and touch an object nearby and think about the sensation.
- Acknowledge three things you can hear. Try to focus on things outside of your body, such as the rumbling of a nearby train track, the sound of an extraction fan and the caw of a bird.
- Think of two things you can smell. If you are at home, you may be able to smell the scent of shampoo on your hair or the lingering smell of whatever you cooked for lunch. Outdoors or at a festival, you may smell grass or the smell of food being cooked at a food stall.
- Think of one thing you can taste; this could be the lingering taste of something you recently ate or drank. Alternatively, if you have a piece of gum, you could take the chance to chew a piece and focus on the taste and sensation
Use breathing exercises
There are also a number of breathing techniques that are useful for anxiety in general that may help a person experiencing a bad trip:
- ‘Box breathing’, or square breathing, involves taking deep breaths (that cause both your chest and stomach to move) and timing your breathing. To do this, inhale through your nose for four seconds, hold your breath for four seconds without exhaling, and then slowly exhale for four seconds. Repeat until you feel more centred.
- Another technique is the 4-7-8 technique. This involves inhaling through the nose for four seconds, holding your breath for seven seconds and then exhaling through the mouth for eight seconds.
Stick together and implement a buddy system
A person having a bad trip is in a vulnerable position and should not be left alone. The gentle presence of another person can help them feel less afraid, while they may be inclined to panic if left by themselves. If you are having a bad trip, it may be tempting to run off by yourself, but it is always better to let a friend know how you are feeling and ask them to come with you.
Can a bad trip be avoided?
It is impossible to guarantee that you will not have a bad trip or drug experience, but some pre-planning can minimise the likelihood of it happening.
Some people who use psychedelics report introspective experiences while tripping such as confronting a past trauma . A good thing to consider before taking psychedelics is whether you feel prepared to deal with something like this should it arise, and what supports you might turn to if it does. If you do not feel emotionally prepared for that possibility, or feel like you do not have a support system, it may be better to avoid taking psychedelics or drugs in general.
If you do decide to use drugs, it is always advised to take them in a safe and controlled environment such as your home, especially if you have never taken a certain drug before. It is likely better to take drugs with others you trust around you as opposed to alone, so that you can ask for help should you need it.
In the case of psychedelics, some people recommend taking them with a ‘trip sitter’, a person who has used psychedelics before and who will remain sober during the course of your trip to monitor you if anything should go wrong.
Planning a trip
There are some steps you can take to make your drug taking experience as safe and pleasant as possible:
- Reflect on your mindset at the time and make sure you are in the right headspace to take psychedelics.
- Choose a calm environment, such as your home or a wide open space such as a garden.
- Avoid taking drugs alone and instead do them with people you trust.
- If you are new to taking psychedelics, take a low dose so that you are not too overwhelmed by the intensity.
- Make a plan of how you might spend your time during your trip.
- Minimise the need to venture into busy areas; ensure you have adequate food and water before starting and try not to have any reason to leave the safe, familiar space you have decided to trip in. Having snacks, water, a colouring book or other supplies on hand before your trip can help with this.
- Figure out before your trip who you will call or what you will do in the event of an emergency. Find out more about how to cope with a drug emergency here .
Support services
- Drugs.ie : Online information and support for drug and alcohol use. Includes a national directory of drug and alcohol services
- HSE Drugs, Alcohol, HIV and Sexual Health Helpline: Freephone 1800 459 459
- You can contact Youth Information Chat , an online service that can put you in touch with Youth Information Officers based all around the country, for more general information
- You can also contact the HSE’s Drug and Alcohol Helpline on freephone at 1800 459 459 if you want to discuss your cocaine use
Feeling overwhelmed and want to talk to someone?
- Get anonymous support 24/7 with our text message support service
- Connect with a trained volunteer who will listen to you, and help you to move forward feeling better
- Free-text SPUNOUT to 50808 to begin
- Find out more about our text message support service
If you are a customer of the 48 or An Post network or cannot get through using the ‘50808’ short code please text HELLO to 086 1800 280 (standard message rates may apply). Some smaller networks do not support short codes like ‘50808’.
Related articles

Staying sesh safe with drug harm reduction
If you or those around you choose to use drugs, you should try to be aware of harm reduction advice.

Harm reduction advice for when you are using drugs
If you choose to use drugs, you can reduce the risks to your health by following simple harm reduction advice.

Signs that your relationship with drug use is problematic
People take drugs for many reasons, such as to relax or to socialise. However, sometimes drug use can become problematic.
Our work is supported by

Let’s Talk About Bad Trips: Separating Difficult from Traumatic
Bad trips are a polarizing concept in psychedelics. acknowledging that they exist - and knowing how to work with them - can be healing..

Want to start a war on social media? Post something like this: “Bad trips exist.”
As somebody who has worked in the psychedelic space for years now and has supported many, many people during their trips, it’s time to come out of the closet and say it: people can be harmed by psychedelics, and bad trips exist.
But allow me to define the term “ bad trip ,” because the vague phrase has become too polarized to be meaningful.
When I talk about bad trips, I’m not talking about the harrowing, painful journeys to the underworld from which we return raw and exhausted, with some important piece of our healing work having been catalyzed.
When I talk about bad trips, I mean the trips that register in the body as a trauma or injury to the nervous system. And that is not , in fact, the same thing as a difficult trip.
What happens when we deny this truth is that we inadvertently alienate those who have had traumatic or harmful experiences. These people have endured a trauma, and are now being told that they have not.
So let’s talk about traumatic trips: The psychedelic experiences that leave us injured. Thankfully, they are rare.
I’m not just speaking from my observations as a clinician, but also from personal experience: I had a traumatic psychedelic experience on ayahuasca many years ago. I was decidedly “not okay” afterwards and required much time and support to recover.
Despite the shock and injury to my nervous system, I eventually used psychedelics again. In fact, in the eight or so years that have passed since the traumatic trip, I have openly supported the legalization of psychedelics, and have built two businesses centered around empowering people to heal with psychedelics.
I have also taken sabbaticals from my practice to work in other countries as a psychedelic facilitator. I am now a lead educator in the country’s first training program for psilocybin facilitators to be licensed by Oregon’s Higher Education Coordinating Commission (HECC). I’m a ketamine prescriber, and I train other prescribers in the use of ketamine for treating chronic pain and mood disorders. I lead and run intensive healing retreats. I’ve also taken my own fair share of mind altering substances in a variety of sets, settings, and time zones.
All of which is to say: I am no newcomer to the world of psychedelics.
And yet I cannot swallow the field’s echo-chamber-like mantra that “there is no such thing as a bad trip .” In fact, I find the rabidity with which some of my fellow cosmonauts deny the existence of bad trips to be rather disconcerting. In the more-than-one heated debate I’ve had about this topic, I’ve noticed certain patterns – or myths, if you will – around the topic of traumatic trips. I address each one here.
Myth: Bad Trips Only Happen When the Set and Setting Are Improper
If the word “only” didn’t appear in the above sentence, it would be true. In my experience in working with hundreds of patients who have used psychedelics – and in administering psychedelics myself – I’ll say that the vast majority of traumatic trips happen when the environment is not safe, calm, and supportive.
When we talk about set and setting in psychedelic harm reduction , we mean two things: (1) the person’s mindset when they took the drug, and (2) their physical environment. If somebody had just had an argument with their spouse before taking LSD, for example, that’s their set. If they were at a noisy, crowded music festival, that’s the setting. Perhaps unsurprisingly, the majority of bad trips happen when individuals on drugs feel overwhelmed in a noisy, chaotic setting like that of a concert or party. Drug-drug interactions are also often at play during difficult trips, for example, when people combine alcohol with psychedelics.
When people insist a little too strongly that, “There’s no such thing as a bad trip, if the set and setting are right,” I feel uneasy. It’s perhaps like asking a rape survivor, “Yeah, but what were you wearing?” (If you think the analogy of a bad trip and rape is too far of a reach, you luckily have never had a traumatic trip.)
There are other factors in psychedelic harm reduction that influence the outcomes. These include the substance being used, the dosage taken, and the people you’re with.

The night of my traumatic trip was the third of a three-night ayahuasca ceremony. I was there with my then-partner. I liked the other people attending. I trusted the facilitators completely and knew they were well trained and highly esteemed by their colleagues. The medicine was pure. The environment was soothing and well contained. The music was beautiful. The first half of the third ceremony was trippy, strange, and lovely.
After I drank my second dose of the brew, however, I was decidedly NOT OKAY. I will not describe the experience here, but I will say two things about it: (1) I felt like my nervous system was being gang raped, repeatedly, and (2) I can now absolutely understand why people with psychosis sometimes choose to die by suicide.
The facilitators of the circle took care of me, pulling me out of the ceremony space and letting me try to calm down outside. Somebody stayed with me at all times until I vomited up the salt water they gave me to drink.
There’s one factor of harm reduction we don’t discuss enough: dose. It’s possible that the second cup of ayahuasca I drank that night contained more voltage than my nervous system could handle – that it was too much, too fast, and too hard for me.
The Influence of Neuroticism
Aside from the environment, another factor that can predict bad trip potential is neuroticism. Neuroticism is one of the “Big Five” traits thought to collectively form the full picture of personality.
People who score high on neuroticism tend to overthink things, typically have a hard time relaxing, and may feel irritated in noisy settings or stressful situations. These folks are often described as “high strung.”
At least two studies have shown that people who score high on neuroticism scales are more likely to have a challenging psychedelic trip than those who score lower. [1] , [2] The theory behind this is that if a neurotic’s negative thoughts or feelings arise during a psychedelic trip, the person might get pulled into an amplification spiral of their own negativity.
But does that mean it’s somebody’s fault that if they tend towards neurosis and they have a bad trip? Aren’t psychedelics supposed to help heal negativity? What does it mean that the same drugs that help soothe negative thoughts and feelings can also make us feel worse? (Let a neurotic chew on that one.)
Once again, we could very easily slip into the territory of victim blaming if we are not mindful.
While writing this article, I took the Big Five Personality Test online. I scored in a higher-than-average percentile for negative emotionality (neuroticism). That may explain why grumpy cat is one of my heroes and why my friend Greg refers to me as “a female Larry David.” It could also explain why I’m one of the unlucky few who have had a traumatic psychedelic trip. (Side note: I also scored pretty high on open mindedness, so that could explain why got into psychedelics in the first place.)
Myth: Bad Trips Are Actually Just Difficult Experiences That Haven’t Been Integrated
I continue to stay in this field because traumatic trips are, indeed, exceedingly rare, and because the healing gains people typically experience from psychedelics are unparalleled by any other intervention I’ve found.
Working regularly with patients in non-ordinary states of consciousness, I see that the most challenging experiences are often the most rewarding. Drawing from my previous experiences in volunteering with the Zendo Project and White Bird , I teach my students the tenants of “trip sitting.”
As one of the Zendo principles states: difficult is not necessarily bad. Note that the phrase is not “difficult is not bad,” but rather, “ difficult is not necessarily bad. ” In other words, difficult can sometimes be bad.
Another layer to this argument is that if you wait long enough, the bad experience will prove itself to be good. This does, indeed, happen to many people after their challenging journeys. Yet there is a difference between suggesting this to a bad trip survivor and insisting that “everyone gets the trip they need.”
Many of my new-age peers have become allergic to the word “bad,” especially within the context of bad trips. “Is anything really bad?” I’m often asked. The argument here, as I understand it, is that with every cloud there comes a silver lining, and that silver lining might just hold a very valuable teaching for us.
I admit that my own traumatic trip gave me a lesson: It taught me that there is indeed such a thing as a bad trip. Another gift was that my bad trip helped me to better understand, validate, and support others who have been harmed by psychedelics. Another lesson was this: my bad trip was an amplifier of the toxic positivity that I see running rampant in the psychedelic field.
In fact, a patient once confessed to me, “I’m just so mad at her” – her being ayahuasca – “but everyone in the group is so in love with Great Grandmother that if I say one bad thing about her, it’ll be like heresy.” I noticed that he was clenching his jaw and only breathing into the upper part of his chest. I leaned forward, looked him in the eye, and said: “Tell me exactly what you think about that bitch – you won’t offend me.”
By the end of the hour, he had raged, wept, and laughed. His breath was reaching his abdomen and his jaw was relaxed. The client messaged me some days later, saying, “That was so healing for me just to be heard, to be able to say mean things without being afraid somebody would cancel me. Thank you.”
Perhaps for this client, “the medicine” was to be heard without anybody trying to stop him from expressing anger. Maybe the bad trip was just part of the arc that took him to that finale. I don’t know.
Myth: There’s No Such Thing as Bad
There’s that old story about the Zen master, whose son got a new horse. “What good luck!” The neighbors said. “We’ll see,” said the master. One day the son was thrown from the horse and broke his leg. “How terrible!” Said the neighbors. “We’ll see,” said the master. Then the country went to war, and the army came to recruit soldiers. Because the young man’s leg was broken, they army didn’t take him to battle. “How good!” said the neighbors. “We’ll see,” said the Zen master. Perhaps there is no good or bad.
What I’ve always found lacking in this story about the Zen master was the voice of his son – the one who actually fell from the horse.
Is a bad trip like falling from a horse? It absolutely can be. Yet something about the “you just haven’t integrated it yet, there’s gold there” argument feels like a dismissive bypass. Let us consider other situations in which we could apply such a statement:
- After getting food poisoning and vomiting for hours
- After taking penicillin and breaking out in a full body rash
- After going on a horrible date
- After surviving a sexual assault
- After your child has been diagnosed with a life-threatening illness
- After losing a loved one to cancer
- After surviving a terrible accident that has resulted in disability
- After your cat has been run over by a car
- After losing a house to foreclosure

Would we really tell the people in the above hypothetical situations that there was no such thing as bad shellfish? No such thing as a bad drug reaction or a bad date? No such thing as rape? No such thing as a bad diagnosis, a bad prognosis? Or how about just a bad day? Or something as non-threatening as a bad movie, a bad haircut, or a bad parking job? Would we really tell somebody whose child just died to avoid using the word “bad” to describe her condition?
Perhaps it is true that none of these things are bad, and that all of them are blessings in disguise. But would we really get righteous about it on social media, the way some of us do about denying bad trips?
And what’s so bad about saying “bad,” anyway? Must everything truly be a blessing? (The neurotic writing this article needs to know.)
I’d also like to share the story of Becks. Becks was a 24-year-old female patient of mine with anorexia nervosa who did MDMA-assisted psychotherapy to heal from PTSD (post-traumatic stress disorder) rooted in childhood sexual abuse.
In a follow-up visit, Becks told me that the MDMA-assisted therapy session (done with an underground provider) had done wonders for her. She was getting much more mileage out of her weekly therapy sessions. She was now remembering things she had repressed previously, and she was able to stay present when the memories arose.
Becks had also forgiven herself. She explained that without realizing it, she had blamed herself for what happened to her when she was a child, punishing herself through self-denigrating thoughts, food restriction, and high-risk drinking. Her MDMA-assisted therapy session helped her identify this pattern and realize that she didn’t deserve the blame or the punishment. Having forgiven herself, Becks was now sleeping better at night, eating when she was hungry, and avoiding alcohol. Clearly, much healing had occurred for her.
Yet Becks felt discouraged and worried. “I don’t think I’m doing it right,” she told me while pulling at the rings on her fingers.
“Why’s that?” I asked.
“Well,” she explained, “I know I’m supposed to get to this place where I feel like the trauma was a blessing – and that hasn’t happened.”
“You think you’re supposed to get to a place where you think that being repeatedly molested as a child is a blessing? ” I asked her.
“Yes,” she said with a defeated sigh as she looked at her shoes.
“Where’d you get that idea?”
Her head snapped up to look at me, breathless, huge-eyed. And then she burst out laughing. The laughter turned to tears. She sobbed and babbled something about a podcast she’d heard. Then she laughed some more. Her face lit up and the color returned to her cheeks.
“Becks, was being molested by your stepbrother every night a blessing?” I asked her.
“No, it was a fucking horrible nightmare that I wouldn’t wish on my worst enemy,” she declared.
“Okay,” I said, “and is it possible that it was a fucking horrible nightmare and that you still get to heal and have a happy adult life starting right now?” I asked.
“ Fuck yeah,” she said. And the look on her face told me she believed it.
(This, by the way, is what happens when you go to a doctor who scores high on neuroticism scales: We acknowledge and celebrate that life might be a fucked up mess sometimes, and that we can still heal even if we don’t buy into toxic positivity.)
(Also: I do have patients who come to see their traumas as gifts. It truly is a powerful and important step in their healing. But let’s not assume that healing cannot happen in other forms. Everyone’s path is different and valid.)
Myth: Talking About Bad Trips Is Going to Harm the Psychedelic Movement
On the day I graduated from medical school, I took an oath to First, Do No Harm . Sometimes, First, Do No Harm means doing the uncomfortable thing or saying what others don’t want to hear. In this case, it means acknowledging that there are risks to using psychedelic substances, and a traumatic trip is one of those risks.
Every therapy, every medicine, every experience comes with risks and benefits. One risk of taking vitamin C is that too much can cause diarrhea. One risk of antibiotics is that they can lead to vaginal yeast infections. One risk of using acetaminophen (paracetamol) is that it’s hard on the liver. One risk of eating a vegan diet is that it can deplete vitamin B12 stores and subsequently trigger depression. One risk of a life-saving surgery is that it can result in a lethal infection. And so forth.
Psychedelic medicines also come with their risks, and the risk of a traumatic trip should be on that list. Admittedly, it should be in small letters, towards the bottom of the list, next to the words “very rare when used in therapeutic contexts.” But traumatic trips are, in fact, “a thing.” They’re part of the fine print.
As far as I know, bad trips have not been reported in any of the clinical trials on psychedelics – but keep in mind that we haven’t had too many people go through the clinical trials as compared to the number of folks doing psychedelics “in the wild.” Bad trips may have also been down-played in the trials as “dysphoria” or “agitation” by the researchers.
Are the possible risks of psychedelic medicines worth wagering for the potential benefits? The answer to that question can only be answered on a case-by-case basis – as with any intervention.
For me personally: The healing engendered by psychedelics has far outweighed and more than redeemed the harm I’ve endured. Every time I take a psychedelic medicine now, I understand that I am taking a risk, and I make the clear, informed decision to proceed – or not to proceed, depending on the circumstance.
When I advocate for the destigmatization and legalization of psychedelics, furthermore, I don’t just act out of love for the movement: I act out of love for my patients.
What’s going to injure the psychedelic movement even more than a level-headed discussion about traumatic trips is the harm that may be caused by denying them.
How to Talk to a Bad Trip Survivor
So, what should we say to a survivor of a traumatic trip? Anything but: “There’s no such thing as a bad trip.”
If somebody tells you they’ve endured a bad trip, treat them as if they’d just told you that they survived an accident, an assault, or another kind of shock. Offer them comfort and support. Listen. Don’t ask them to prove the truth of what they say happened.
Essentially: treat them as you would treat the survivor of any kind of experience that was too much, too hard, and/or too fast for their mind, body, or spirit.
Remember that the word “trauma” does not refer to the distressing event itself, but rather to the resulting emotional and neurological response. Trauma can harm a person’s sense of Self, their sense of safety, their ability to navigate relationships, and their ability to regulate their emotions. Trauma, in other words, is injury to the nervous system that ripples outward. (To be clear: Trauma does not mean simply feeling uncomfortable or offended, as some people mistakenly use it.)
Even if integration of the experience would be helpful for the survivor – and might even help them stop using the term “bad trip” to describe it – that cannot happen at the beginning. The first thing the bad trip survivor likely needs is to know that they are safe now . The nightmare has ended, and they are loved and supported by trustworthy people who care.
How can we help others feel safe? By our presence. By regulating our own breath. By listening. By letting them know that we believe them. By showing empathy. By making them soup, gifting them a massage, or offering to pick their kids up from school. By being kind.
Even if the traumatic trip was the result of poor planning, improper set and setting, or other user error, hold your tongue for now. Think of how you might react if a friend was in a terrible car accident that resulted from driving when they were overly tired.
Think of how you might respond if a child dragged a chair to the kitchen counter and climbed atop it to try and reach the off-limits cookie jar sitting high up on a shelf – only to tumble backwards and slam onto the floor. Would you shout, “Well, that’s what you get for climbing on the chair!” while the poor kiddo cried on the linoleum? I hope not. I hope you would sit by their side, hug them, and stroke their hair. Once you felt their breathing return to normal and the smile return to their face – and not a second sooner – might you ask, “Honey, remember what we said about climbing on the furniture?”
Healing From My Bad Trip
It took me almost eight years to feel like I had fully integrated my bad trip. Curiously, what helped me complete the arc from wound to health was a peyote ceremony.
What prolonged my healing was people insisting that there was no such thing as a bad trip. I heard this line in my ayahuasca circle, at psychedelic conferences, on social media, on podcasts, and in books. The experience-denying and victim-blaming made me feel angry and alone.
Another factor that delayed my full recovery was peer pressure. Buckling to the well-intentioned insistence of friends, I returned to the ayahuasca circle (and other psychedelic circles) sooner than I truly wanted to. This meant that I was taking medicines with a mindset of doubt and fear, which resulted in several dysphoric, confusing, and terrifying journeys that only compounded the injury.
I was fortunate to find a healer who believed in bad trips and who confirmed that I was not fully in my body. Through regular sessions, I was able to return. While my therapist hadn’t had much psychedelic experience herself, she at least believed me. That allowed us to start from a place of trust and not from a place of defensiveness. I also took a break from psychedelics and instead cultivated gentler, more predictable health-affirming practices like singing and going to the gym.
Years after the experience, I read about the concept of “too much, too hard, too fast” in a book about psychedelic facilitation. I felt a surge of heat rush to my face as I read the words; hot tears filled my eyes. I hadn’t made it up. It had happened to me. I wasn’t weak, or stupid, or crazy. But why was the truth so hard for other people to accept?
I’m grateful to my own stubborn will to get better – to that spark within me that keeps me seeking out people, places, and things that can help me heal, grow, and learn.
There was, indeed, some good that came from my bad trip on ayahuasca all those years ago. The seams of that horrific shroud were sewn with golden thread. I am grateful for the blessings gleaned.
I am also grateful to my unconditionally supportive family, friends, and partner, and to Grandfather Peyote for helping me weave the blessings into my life and pull back the heavy curtain.
I had a bad trip, and that’s okay.
And you know? Considering that I’m a neurotic, I’m pretty proud of myself for saying so.
Follow your Curiosity
[1] Barrett FS, Johnson MW, Griffiths RR. Neuroticism is associated with challenging experiences with psilocybin mushrooms. Pers Individ Dif. 2017 Oct 15;117:155-160. doi: 10.1016/j.paid.2017.06.004 .
[2] Petter Grahl Johnstad (2021) The Psychedelic Personality: Personality Structure and Associations in a Sample of Psychedelics Users, Journal of Psychoactive Drugs, 53:2, 97-103, DOI: 10.1080/02791072.2020.1842569
You may also be interested in:

Mental Health

Harm Reduction

Self-Discovery


What Exactly Is a “Bad Trip”? Dangers of Hallucinogens

A broad category of drugs used recreationally falls under the heading of hallucinogens. Most of these drugs can result in a pleasant experience of unusual perceptual and sensory experiences. Colloquially, taking hallucinogens is known as “tripping.” Taking these drugs regularly increases your risk of a bad trip.
What Is a Bad Trip?
A bad trip is an unpleasant experience while using hallucinogens, though some users even report bad trips when using marijuana, which is not typically categorized as a hallucinogen. During a bad trip, users may experience extreme psychological distress. Externally, a bad trip might look like someone destroying a room, crying for extended periods of time or seeming unresponsive to external stimuli.
Hallucinogens That Can Cause a Bad Trip
There are two basic categories of hallucinogens: classic and dissociative . Drugs in both categories can cause a bad trip at times. There’s no specific way to determine which way a trip will go, though there are risk factors that can make a trip more likely to go bad. If you want to avoid adverse reactions, you should avoid using:
- LSD: LSD , also known as acid, is a well-known and powerful hallucinogenic drug. Its psychedelic effects are often depicted in movies and media.
- DMT: Dimethyltryptamine, also known as psilocybin or magic mushrooms, is another powerful psychedelic. Many people report experiencing a bad trip while using mushrooms.
- MDMA: “Molly” or ecstasy is best known as a party drug. While bad trips are uncommon, they can occur on MDMA when paired with dehydration and too much partying.
- Salvia divanorum: Salvia, a plant commonly found throughout southern Mexico and in Central and South America, is a short-acting and potent psychedelic. Users often report feeling terrified when experiencing a bad trip on salvia due to the heightened experience.
- Peyote: A small, spineless cactus that contains mescaline, this drug is used in some indigenous practices in the United States. When brewed into a tea or other liquid, trips can last for 12 hours or more.
- Ketamine: Users may mention falling into a K-hole, which is a reference to a bad trip on ketamine and describes a near-complete disassociation from reality and a trance-like state.
- Marijuana: Paranoia and anxiety are often reported side effects of using weed , which can fall under the heading of a bad trip.
Studies are ongoing as to the efficacy of using psychedelics as part of a treatment plan for depression, anxiety and trauma. Talk to your mental health provider before you consider using any drug as a treatment option.
Signs and Symptoms of a Bad Trip
No two bad trips are the same, even when experienced by the same person taking the same drug. However, some of the most commonly reported bad trip symptoms include:
- Time dilation, or the sense that time isn’t passing
- Negative thought spirals
- Extreme paranoia and emotional distress
- Sudden mood swings with extreme responses
- Frightening or horrifying hallucinations and delusions
If you’re with someone who’s taken a hallucinogenic, keep any eye out for the signs of a bad trip. If the symptoms are prolonged or accompany dangerous behaviors, call 911 for help managing the symptoms.
Risks and Dangers Associated With Bad Trips
The risks and dangers you might experience with a bad trip can vary depending on the drug you take. Classic hallucinogens create visual and audio hallucinations and can make your feel sensations that aren’t real. The effects usually start as you metabolize the drug , which can be within 20 minutes. Some trips last as long as 12 hours or more, while others can be short, intense 15-minute trips.
When taking classic hallucinogens, you may feel your heart race, nausea and overloaded sensory responses. Colors may appear brighter, and you may lose track of time. Most people will experience a loss of appetite while on the drug, along with dry mouth and increases in blood pressure , breathing rate and temperature. During a good trip, you might have a spiritual experience and feel very relaxed. During a bad trip, excessive sweating, panic, paranoia and psychosis can be a problem.
Dissociative drugs can also cause numbness and disorientation, two relatively benign side effects when you’re in control that can be very dangerous during a bad trip. If you experience acute intoxication with a dissociative drug, you may also experience memory loss, panic, anxiety, seizures, psychotic symptoms, amnesia, breathing troubles and other side effects.
These short-term effects can be dangerous during a bad trip. If you’re experiencing mood swings, panic and numbness, you might not notice if you cause yourself an injury. Panic and paranoia combined could create a cocktail of bad decisions and no trust in the people around you to help.
Long-Term Effects of Bad Trips
Although rare, there are other risks associated with bad trips that could leave you with chronic health conditions, including:
- Persistent psychosis: A series of continuing mental problems that often include visual disturbances, disorganized thinking, paranoia and mood changes, even when not actively taking a hallucinogenic drug.
- Hallucinogen persisting perception disorder (HPPD): HPPD can create symptoms often associated with PTSD, where the person has flashbacks to things experienced while using a hallucinogen. You might experience visual or audio hallucinations or notice more general visual disturbances. Flashbacks can happen with little to no warning and persist for more than a year after the last time you tripped.
- Speech problems: Speech problems following hallucinogen use may involve slurred speech, slow speech, agitated speech and difficulty putting together sentences.
- Memory loss: Both short- and long-term memory loss may be side effects of a bad trip. You may forget what happened during the trip and have trouble with short-term memory for some time after using.
- Weight loss: Uncontrolled weight loss can be a long-term side effect of hallucinogen use. Drugs like LSD and mushrooms disrupt hunger cues, which may cause an unhealthy level of weight loss.
- Depression and suicidal thoughts: During and after a bad trip, there’s a risk of depression and suicidal thoughts. The anxiety caused by a bad trip can lead to negative thinking even after the drug passes through your system.
Some hallucinogens may also come with a risk of addiction; PCP is one example. Behavioral therapies and medication can be used to help people improve the symptoms of many of these side effects.
How to Prevent and Manage a Bad Trip
You can’t always prevent a bad trip. You can stay hydrated, only use hallucinogens in a low-stimulation space with company and avoid mixing drugs with any other substances, including alcohol. You should avoid hallucinogens if you’re not in a good mood as negative thoughts can spiral, causing a bad trip. But, even if you take all the appropriate precautions, you can still have a bad trip.
There are medications available that may help stymie a bad trip, but you’ll need to seek medical attention, as these medications are prescription-only.
Share This Story, Choose Your Platform!
Related posts.

What Are Pressed Pills?

Can Teletherapy Be Used for Addiction Treatment?
Does Gabapentin Cause Weight Gain?

Is It Dangerous to Mix Antibiotics with My Medications?
855-908-0047.

© All rights reserved. • Sunlight Recovery Center
Are You In An Emergency?
Spontaneous tripping — causes?
- Counseling and Psychological Services (CPS) (Morningside)
- Medical Services (Morningside)
- Counseling Services (CUIMC)
- Medical Services (CUIMC)
Cite this Response
Alice! Health Promotion. "Spontaneous tripping — causes?." Go Ask Alice!, Columbia University, 06 Jul. 2018, https://goaskalice.columbia.edu/answered-questions/spontaneous-tripping-causes. Accessed 26, Jun. 2024.
Copy Citation
Alice! Health Promotion. (2018, July 06). Spontaneous tripping — causes?. Go Ask Alice!, https://goaskalice.columbia.edu/answered-questions/spontaneous-tripping-causes.
Dear Alice,
I want to know what it is when you spontaneously trip without dropping tabs or anything. I've never had any drugs except marijuana. It is weird. I know that tripping is an induced psychosis, so am I psychotic or what? I was seeing a shrink and will be going back into treatment next semester. I think substance use is boring and a complete copout on life. I've made a lot of discoveries without needing to trip. Why does this happen? Tell me what you know.
Signed, Gandhi admirer
Dear Gandhi admirer,
Non-drug-induced mind-altering moments are a mouthful to say, but they do in fact exist! Researchers have noted that many trips can actually occur in response to certain common substances (such as antibiotics) and mental illnesses, which may be some potential explanations for what you're experiencing. Interestingly, marijuana has also been found to produce an effect on the mind similar to psychosis. If these spontaneous trips are interfering with your daily activities, it might be good to talk with a health care provider to see if something else is happening that may be causing these experiences.
Tripping refers to experiencing drug-induced symptoms of psychosis (such as hallucinations and delusions) which commonly occur after taking psychotomimetic substances; these drugs are capable of producing an effect on the mind similar to a psychotic state and include substances such as lysergic acid diethylamide (LSD), ketamine, and even marijuana. This response typically occurs in those already vulnerable to psychotic disorders. These symptoms aren't just a result of taking substances; they’re also possible during withdrawal and from prior substance abuse (referred to as substance-induced psychotic disorder). It’s worth noting that a history of drug use (particularly early and heavy use of marijuana or stimulants) is also associated with the development of schizophrenia, a disorder that includes psychosis as a symptom.
All of that said, it’s entirely possible that someone without a history of substance use or mental illness experiences hallucinations spontaneously — that is, they feel the symptoms without having taken any substances or a diagnosable mental health condition. The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) attributes this to a great deal of negative stress. For those experiencing or prone to mental illness, the amount of stress that leads to hallucination is less than those who are not at risk. Additionally, research shows that hallucinations may be impacted by a number of variables, such as age (teenagers and young adults dealing with hormonal changes in the brain during puberty), genetics, trauma, or physical illness or injury. This is particularly relevant if the hallucinations aren’t associated with other cognitive, emotional, or behavioral disruptions and don’t compromise personal, social, or occupational function. While hallucinations can be associated with mental illnesses or disorders, they aren't always, especially if the person experiencing the hallucination is aware of it at the time.
However, it's also possible that this tripping feeling you're experiencing may be attributed to psychosis, which is a symptom of a number of mental and physical illnesses. During psychosis, a person has a difficult time differentiating between reality and their own thoughts and perceptions. Psychotic states often consist of hallucinations and delusions — hallucinations involve seeing, hearing, or feeling things that aren’t there, while delusions are the presence of strong beliefs inconsistent with the person’s culture and are unlikely to be true. Psychotic symptoms are most known for being associated with illnesses such as schizophrenia, depression, bipolar disorder, and autism spectrum disorder. They’re also common among those with diseases such as Alzheimer’s, Parkinson’s, traumatic brain injury, and HIV. According to the DSM-5, psychosis differs from a psychotic episode, which is an experience in which the individual doesn’t know that they’re experiencing symptoms of psychosis, or is, in other words, having a break from reality.
With this information in mind, you may take some time to reflect: do your symptoms interfere with your ability to perform tasks like completing schoolwork, performing at work, or engaging in relationships? If so, a health care provider will be able to assist you in evaluating your trips and suggesting next steps. They may ask about family history, check your vital signs, and conduct tests to determine what condition, if any, could be causing these trips. In the end, only a professional can tell you whether your trips are a result of a drug you have taken in the past, a tendency toward mental illness, or an active imagination.
Here's hoping that this response — while only the t(r)ip of the iceberg – is helpful!
Additional Relevant Topics:
Is what i’m feeling nirvana or burn out from lsd use, 'shrooms and lsd used to treat body dysmorphic disorder, effects of marijuana on libido and fertility.

Photo by Gravity Images/Getty
How to have a safe psychedelic trip
A psychedelic experience can be deeply rewarding, but also carries real risks. here’s how to avoid a bad trip.
by Christian Jarrett + BIO
is the editor of Psyche. A cognitive neuroscientist by training, his books include The Rough Guide to Psychology (2011), Great Myths of the Brain (2014) and Be Who You Want: Unlocking the Science of Personality Change (2021).
Edited by Sam Dresser
Listen to this Guide.
Need to know
Humans have consumed substances with consciousness-altering properties for millennia. Traditional societies used them in healing rituals, initiation ceremonies and to make contact with the gods and the dead, among other practices. Today they are known as psychedelics, and include the naturally occurring compounds psilocybin (found in ‘magic mushrooms’), DMT and mescaline; the hallucinogenic tea Ayahuasca, used by indigenous peoples in the Amazon basin; and the hallucinogenic shrub iboga, found in West Africa.
Synthetic hallucinogenic compounds, most famously LSD, emerged in the 20th century. The synthetic ‘party drugs’ MDMA (also known as ecstasy) and ketamine (used in medicine as an anaesthetic) are not technically classified as psychedelics, but they also produce consciousness-altering effects and are often considered under the same broad umbrella as the classic psychedelics.
In the industrialised West, psychedelic substances, especially LSD and magic mushrooms, burst on to the scene in the 1950s and ’60s with intense research interest in their therapeutic potential. However, an establishment backlash began in the late-1960s as the drugs became associated with the counterculture movement and opposition to the Vietnam War. Fermenting the eventual clampdown, the psychedelics-researcher-turned-evangelist Timothy Leary exhorted American youth to ‘turn on, tune in, drop out’. Tales spread of ‘bad trips’ and associated suicides, and the field of psychedelic research fell silent for decades.
We are now living through what’s been described as a ‘psychedelic renaissance’ that began in the 1990s. Research groups around the world, notably at Imperial College London and Johns Hopkins University in Baltimore, have been pumping out studies uncovering the neural basis of the drugs’ effects and exploring their apparent therapeutic benefits, especially when used as an adjunct to psychotherapy.
Research trials suggest that, when used as part of psychotherapy, the benefits of psychedelics include, but are not limited to, alleviating depression and anxiety (including for people who have not benefited from other forms of therapy or drug treatment), tackling longstanding symptoms of post-traumatic stress disorder, treating addiction, and calming existential distress in people with terminal illnesses.
Superior trial outcomes correlate with participants’ reports of having a mystical or transcendent experience during their psychedelic session. In fact, many people who take a psychedelic drug describe the experience as among the most personally meaningful of their lives. Many are changed by their trip, displaying greater open-mindedness, humility and feelings of connectedness with humanity and the wider world.
Although they can lead to subjectively similar experiences, different psychedelic drugs exert their effects in the brain via different mechanisms. For instance, psilocybin, mescaline and LSD act principally via the 5-HT2A receptor system (5-HT, also known as serotonin, is a neurotransmitter involved in mood and perception), whereas DMT acts on the 5-HT2A system and sigma-1 receptors involved in neuronal signalling. Meanwhile, ketamine interacts with another brain chemical called glutamate by blocking the NMDA receptors that this neurotransmitter usually binds with.
At a global level, psychedelic drugs have in common that they increase levels of entropy in the brain by allowing for communication between neural regions that don’t usually interact, and reducing the activity of a group of neural areas known collectively as the ‘default mode network’, which is involved in self-conscious thought. It’s believed that these neural changes lead to ‘ego dissolution’ and facilitate the mystical feelings of oneness and transcendence that are common to many trips.
The upsurge in research interest in psychedelic drugs and reports of their transcendent, life-changing effects have led to a steady flow of newspaper stories documenting their potential, and the publication of a spate of popular books about psychedelics. As curiosity about these drugs and their beneficial effects continues to grow, it raises the question of whether it’s possible for individuals to take these substances safely – and, if so, how?
Safety and legality issues
There are certain physical and mental health conditions that make it inadvisable to experiment with psychedelics, including heart problems and a history of psychosis or bipolar disorder. Antidepressant or antipsychotic medication could also interact unpredictably with the psychedelic. ‘Chronically, SSRIs [a form of antidepressant] may reduce the effect of psychedelics while other antidepressants may have other effects. But at this point there’s just not enough known about the effect of other psychoactive drugs on psychedelics,’ explains Sandeep Nayak, a psychiatrist at Johns Hopkins who has trained as a facilitator in psychedelic research studies.
‘If you have underlying mental health concerns or are experiencing depression, anxiety, or any medical issues, talk to a psychedelic-friendly therapist or doctor before taking substances,’ advises Sara Gael, director of harm reduction at the Multidisciplinary Association for Psychedelic Studies (MAPS) in the United States.
Even if you are fully fit and healthy, experts unanimously say that it’s a bad idea to take a psychedelic drug on your own, especially if it’s your first time. Ben Sessa is a psychiatrist, based in the United Kingdom, who has been researching the therapeutic effects of psychedelics for more than 15 years. He rejects the framing of the question in terms of whether it is possible to have a safe trip. ‘It’s like: “Is a knife safe or dangerous?”, it’s a ridiculous question. It’s about risk/benefit analysis.’ But he, like others, warns against journeying solo.
‘There are more risk factors [on your own] because there isn’t somebody there to manage your feelings or your behaviour,’ he says. ‘More importantly, you could be disorientated, and try to get in your car and drive away. Anything from the most benign behaviour – going online and buying 200 kg of avocados – to much more dangerous, there’s nobody who is not high who is able to temper your behaviour and make sure things are okay.’ Psychedelics have a profound effect on cognition, perception and coordination and you should take care to be in a physically safe, controlled environment. You should not plan to be driving, walking in traffic, be in high places or other dangerous environments which require you to be alert and coordinated.
Ideally you should identify an experienced and trusted guide or therapist to work with you before, during and after your psychedelic experience. Many cities in the US, Europe and elsewhere have psychedelics societies and these can be a good place to begin your search for a guide. At a minimum, make sure you are with a trusted and competent friend to keep you as safe as possible for the duration of the drug’s effects (consider, for instance, that the mind-altering effects of LSD can typically last up to 12 hours).
Another glaring practical issue is that, in most jurisdictions around the world, psychedelic drugs are illegal and if you are caught in possession, you will face criminal charges. This also has important implications for sourcing drugs safely. Françoise Bourzat, who has worked as a psychedelics guide in California for decades and is the author of the book Consciousness Medicine (2019), says that to source the drugs you will have little option other than to rely on word of mouth. ‘Always test your drugs,’ adds Gael. ‘Test kits are available on the DanceSafe website.’
If you decide to go ahead and it’s your first time, it’s sensible to start out with a weaker dose and, as mentioned, to pay due attention to the duration of the drug’s effects. The PsychonautWiki community encyclopaedia has information on dosing, duration and other practical issues.
However, even if you take these practical precautions, other experts urge an even more cautious stance. ‘I can’t and don’t endorse the use of psychedelics outside of research settings,’ says Nayak.
Fortunately, the physiological risks from the classic psychedelics are low to zero. ‘LSD and psilocybin are virtually inert physically – they have very low physical toxicity profiles so there are minimal physical risks,’ says Sessa. ‘They’re also not moreish,’ he explains. ‘You can see this in animal trials, they won’t repeatedly self-administer psychedelic drugs, they’ll take a single dose and then just largely ignore options to redose. So, the risk of addiction to psychedelics is low. Taking MDMA repeatedly long-term can be more harmful, but studies show that the physical risks go down after stopping.’
The main risks are psychological, and this is why preparation is so important. As safety guidelines for psychedelics trials from Johns Hopkins University put it: ‘The most likely risk associated with hallucinogen administration is commonly known as a “bad trip” and is characterised by anxiety, fear/panic, dysphoria, and/or paranoia.’
The most effective way to minimise the risk of a bad trip occurring is to prepare well. The Johns Hopkins advice is for guides and therapists to discuss the broad range of psychological effects that can be experienced under the influence of a psychedelic, including out-of-body sensations, the evocation of powerful memories, distortions to time and space, and feelings of oneness with the world, to name but a few. It’s also important to pay due attention to what Leary called ‘set and setting’. Most relevant to the preparation phase, ‘set’ describes the mindset and intention you bring to the psychedelic journey, and an experienced guide will work on this with you. The ‘setting’ refers to the physical, social and cultural environment in which the user takes a psychedelic drug.
‘Are you entering the experience with a certain need in your life? Do you want to explore something? Do you need healing? Do you have an emotional relationship that is problematic, burdened by childhood issues?’ asks Bourzat. ‘Do you want to be connected more with spirits or explore your relationship with nature? You don’t have to have a pathology to have an experience, but it’s a good idea to know why you’re doing it. What are you looking for in the journey? That’s the preparation.’ Other basic aspects of preparation, she adds, include writing a journal and preparing the body by fasting and avoiding alcohol.
The journey
Researchers have known about the importance of the ‘setting’ in the psychedelic experience for decades . In a series of studies published in 1960, Robert Hyde, a doctor at Boston Psychopathic Hospital, spent three years observing how the effects of LSD varied in different contexts. For instance, in the second year of his research, volunteers were treated as ‘research objects’ and given structured tasks to complete, whereas in the final year, the experience involved more chance for relaxation and personal support from and rapport with the researchers. Needless to say, the final year was generally associated with positive psychedelic experiences whereas the second year led to more unpleasant outcomes.
If you take a hallucinogenic drug at a party, even the attitude – the ‘set’ – of your friends could influence the ‘setting’ and thereby make a difference to your own experience. A field study in 2002 found that, on the rare occasions when people taking MDMA/ecstasy at parties reported bad experiences, this usually coincided with the user’s friends having pessimistic expectations or concerns about the trip. ‘A sense that another user, particularly a friend or acquaintance who is part of the collective, is not having a pleasant experience may have a deleterious effect on the group as a whole,’ the researchers said.
When it comes to a more formal, guided psychedelic journey, Bourzat explains that the setting is literally where the journey is happening: ‘What is the location? Who is sitting with you? Who is helping? What is the expertise and style of the guide? It also includes the length of time … What is guiding the work? Is it nature? Is it someone singing for you? Is there music playing? Is it quiet? All these different elements create the setting.’
She adds that commonsense steps to take include ensuring that the room is comfortable with soft furnishings and that any music is conducive to a pleasant experience. ‘I wouldn’t play rock and roll or house music. It should be expansive, not just classical but also more contemporary, or new age or tribal, African, Tibetan – anything ambient that’s conducive to introspection,’ says Bourzat.
If you have any frightening experiences or difficult overwhelming emotions, the usual advice is to surrender to these rather than trying to suppress them or run away from them. ‘Whether the disturbance consists of frightening illusions or internal imagery, difficult thoughts and feelings about some past or present personal issue, or anxiety related to a radical change in sense of self (eg, temporary loss of self-identity), the volunteer is encouraged to mentally surrender to the experience, trusting that her or his usual state of consciousness will return when the drug effects resolve,’ state the safety guidelines from Johns Hopkins University.
Integration
Following your psychedelic journey, it’s critical that you process the meaning of your experience with a guide or therapist. This ‘integration’ should take place during the two to three months after your experience. ‘When people take drugs recreationally, like just go to a festival and take LSD and then go home, that’s where they tend to run into problems because there’s a lack of integration of the experience,’ says Sessa.
One of the key aims of integration, Bourzat explains, is to carry the beneficial aspects of the psychedelic journey into everyday life. ‘If someone had a beautiful experience of nature, and in the journey they experienced beautiful birds, a meadow, then I would say you actually need to do that in your life. You need to cultivate that experience, and maintain that goodness that you connected with in the journey,’ she says. ‘Or say someone connected with a loved one they had lost, and felt love and tenderness and dealt with unfinished business in the journey, then I would suggest some ritual in real life – writing to the deceased person or beginning a journal and making that part of their life.’
Gael notes that integration therapists have different approaches and backgrounds. It’s important to find a guide or therapist whom you trust and who is nonjudgmental. ‘One helpful resource for finding integration support is the Psychedelic Support [network],’ she says.
Key points – How to have a safe psychedelic trip
- Remember that psychedelic substances are illegal in most jurisdictions.
- If you have physical or mental health issues, speak to a sympathetic doctor before experimenting with psychedelics. People with a history of psychosis or bipolar disorder are usually not allowed to participate in psychedelic research trials because they face heightened risks.
- Ensure you are in a physically safe, controlled environment. Always start with a low dose.
- Don’t take psychedelic drugs on your own. Find an experienced guide or therapist whom you trust.
- Use word of mouth at psychedelic societies and elsewhere to source psychedelic substances safely, and use online testing kits to ensure their quality. Alternatively, for greater safety, consider signing up to a research trial conducted at a university.
- Remember the importance of set and setting. Work with a guide who will help you prepare for your psychedelic journey, sit with you during the experience, and conduct integration with you for several weeks or months afterwards.
The main safety challenges confronting anyone who wishes to experiment with psychedelics stem from their illegality, meaning that there is no formal regulation of the training of psychedelic guides, nor is there a reliable way to source the drugs safely. Many researchers in the field, including Sessa, have been campaigning for drug-law reforms for decades. ‘The current situation is a total practical folly and extremely dangerous, utterly immoral and totally unpoliceable,’ he says. ‘It’s putting our heads in the sand and not addressing the fact that many people will take these drugs. It’s like the prohibition era in the States but on a much larger scale. The only way to control potentially dangerous drugs is through appropriate regulation. Imagine if scuba diving were outlawed – people would still do it, but now there were would be poor training, poor equipment and loads of people dying.’
Until the laws are changed, and outside of a research environment, the best route to a safe experience lies in finding a suitably trustworthy and experienced guide – someone who is vouched for by others. And it’s key that this guide will work with you before and after your psychedelic journey.
‘There’s lots of underground therapists in this country and elsewhere, these so-called healer/shaman/guru-type people who will quite happily take you down to Totnes and take four grand off you and take you into their yurt and give you a bag of mushrooms, but they won’t give you the other stuff; they won’t do the preparation and they won’t do the integration, so people are left hanging high and dry,’ says Sessa. ‘I always say to people who’ve found a so-called shaman or healer: “Ask this guy if he will see you for three weeks before and three weeks afterwards, and I bet he won’t.” That’s the bit that’s missing, not only from recreational use, but also from underground use.’
Until the laws change, signing up to a research trial is probably the least risky way to experience a psychedelic trip. These are being conducted at various research institutions around the world, principally: the University of Bristol, Imperial College London, Newcastle University and Manchester University in the UK; and at Johns Hopkins University in the US.
Links & books
Erowid is a US-based organisation that provides ‘reliable, nonjudgmental information about psychoactive plants, chemicals, and related issues’.
Bluelight is an ‘international, online, harm-reduction community committed to reducing the harms associated with drug use’.
The Multidisciplinary Association for Psychedelic Studies (MAPS) is a US-based ‘non-profit research and educational organisation that develops medical, legal, and cultural contexts for people to benefit from the careful uses of psychedelics and marijuana’.
DanceSafe is a public health organisation, founded in California, that provides ‘a nonjudgmental perspective to help support people who use drugs in making informed decisions about their health and safety’.
PsychonautWiki is a ‘community-driven online encyclopaedia that aims to document the field of psychonautics in a comprehensive, scientifically grounded manner’.
The Psychedelic Renaissance (2nd ed, 2017) by Ben Sessa is an excellent introductory textbook that describes the cultural history of psychedelics, and is the most up-to-date review of contemporary work in the field.
Consciousness Medicine: Indigenous Wisdom, Entheogens, and Expanded States of Consciousness for Healing and Growth (2019) by Françoise Bourzat with Kristina Hunter is a ‘comprehensive guide to the safe and ethical application of expanded states of consciousness for therapists, healing practitioners, and sincere explorers’.
How to Change Your Mind: What the New Science of Psychedelics Teaches Us About Consciousness, Dying, Addiction, Depression, and Transcendence (2018) by Michael Pollan is a ‘brilliant and brave investigation into the medical and scientific revolution taking place around psychedelic drugs – and the spellbinding story of his own life-changing psychedelic experiences’.

How to use ‘possibility thinking’
Have you hit an impasse in your personal or professional life? Answer these questions to open your mind to what’s possible
by Constance de Saint Laurent & Vlad Glăveanu
The nature of reality
How to think about time
This philosopher’s introduction to the nature of time could radically alter how you see your past and imagine your future
by Graeme A Forbes

How to control your gambling
What’s fun at first can all too easily get out of hand. Learn the warning signs and use these tips to rein things in
by Luke Clark

Call Us: 720-796-4785
Click to download our Free Psilocybin Sourcing Guide
Register for Free Weekly Q&A: 6/26/24 4:00 PST
Register for Free Q&A: 6/26/24 4:00 PST
What is a Bad Trip and Why are They Important?
- Jimmy Nguyen
Those of you who have endured a psychedelic experience understand their potential to heal the mind, body, and spirit. You also probably had a very entertaining time while exploring these states of altered consciousness. However, many of you are equally nervous about the probability of becoming transfixed in what has been termed a “bad trip ” .
If you or someone you know has experienced a bad trip, this article will help you understand what you went through. But before we go any further, let’s break down what a bad trip really is, why they are important, and how to navigate one.
What is a Bad Trip?
Unfortunately, the War on Drugs in America has created a lot of misinformation when it comes to psychedelics, particularly with regards to the bad trip. You may have heard rumors that even one experience with lysergic acid diethylamide (LSD) can make you perpetually trip or permanently insane. Scare tactics like these have been used over the past several decades to demonize psychedelics and deter their use.
Though these myths are untrue, it is important to note that individuals predisposed to mental illness, such as schizophrenia and bipolar disorder, may have adverse effects from a psychedelic experience, including psychosis, and that proper mental health screening should be conducted before engaging in any psychedelic activity.
So what defines a bad trip? A bad trip refers to a challenging or difficult experience while being under the influence of a hallucinatory substance such as psilocybin mushrooms, LSD, ayahuasca, or even cannabis. Although it is common for occasional unpleasantness, such as nausea or bewilderment, to occur temporarily during a psychedelic experience, bad trips are defined by prolonged or seemingly uncontrollable episodes.
During these experiences, symptoms can range from unpleasant to traumatic, with some experiencing anxiety, paranoia, resurfacing of repressed memories, or overwhelming stress. Physical discomforts, such as an upset stomach, sweating, overheating, or soreness may also occur.
To be clear, “good” and “bad” are arbitrary labels we assign to our experiences. And generally, people use “bad” to describe discomfort or pain. But like a weightlifter who endures temporary discomfort to build muscle, so too can a psychedelic explorer endure a bad trip to receive long-term benefits. The caveat is that the user must prepare in advance of the experience , exercise safety during, and take care of the body and mind well after. And just like the weightlifter, results do not happen overnight.
What is the Likelihood of Having a Bad Trip?
It is often difficult to predict if you will have a bad trip. In actuality, it’s not really a question of if, but when, as bad trips are actually unavoidable milestones in the psychedelic journey. When you do experience one, it may be comforting to know that you are not alone and that adverse effects are temporary.
According to the Journal of Psychopharmacology , a study surveyed 1993 psilocybin users. Of this, 39% labeled the experience one of the most challenging of their lives. However, 84% of the total participants stated that this challenge was a positive experience in the long term. What’s more is that the study concluded that risky behavior or enduring psychological distress is extremely low when psilocybin was given to screened, prepared, and supported participants.
Not only does this mean that bad trips are generally safe, but it further supports our belief that bad trips, though difficult to endure, are actually the most crucial part of the psychedelic experience as they result in the positive mental, physical, and spiritual growth we all desire.
Why Bad Trips Are Important
If you ask someone experienced in psychedelics if they’ve had a bad trip, an overwhelming majority would say yes. This matters because it suggests that discomfort is part of the psychedelic journey. You are typically not in control of the events or outcome of a psychedelic experience, thus putting you outside of your comfort zone.
This often results in opening up and exploring your fears, anxieties, and analyzing unwanted aspects of our personalities. This experience is accompanied by a series of mental, physical, and emotional triggers and releases.
Bad trips are misunderstood experiences that have a misguided social context. Many of these “bad” trips can actually lead to prolonged mental and physical healing. Though healing isn’t always comfortable, it is necessary to make a significant change in your life.
Healing requires confronting the traumas and pain that limit our lives to truly embrace and love all the facets, both the light and the shadow, the “good” and “bad” parts of ourselves. Like a lobster that molts its shell each year to grow larger, the psychedelic experience, particularly bad trips, can provide a venue to undergo this challenging, yet vital evolution.
This isn’t to say that you should be specifically seeking bad trips. These difficult trips are most common for inexperienced users and those who did not adequately prepare. A higher dosage is typically related to an increase in adverse reactions, so proper dosage and preparation are key. Psychedelic Passage offers guidance on dosage and preparation through our trip sitting program .
Even the most seasoned psychonaut has a chance of experiencing a taxing psychedelic experience. Ironically, if you are equipped with the framework to work through these difficult experiences, they turn out to be very rewarding. If you happen to undergo a “bad” trip, these 10 tips may help you navigate the trip , mitigate risks, and stay safe during these stressful episodes.
What Should I Do If I’m Currently Having a Bad Trip?
This is a great question, and thankfully, it’s not too late to take the edge off of your discomfort. While we always maintain the position that proper preparation is most important , there are certainly some tips you can use to make a bad trip more pleasant.
Ideally, with adequate preparation, you are in the presence of a guide or trip sitter who is knowledgeable in harm reduction and altered states of consciousness. This individual should be well prepared to help you safely and smoothly navigate a “bad” trip.
The number one thing to keep in mind is that it is temporary—you aren’t stuck like this, you will return to your normal self with time. That said, we’ve put together a list of 10 tools to help you safely navigate a bad trip , which you can find here.
I’ve Recently Had a Bad Trip. Now What Do I Do?
First off, congratulate yourself for having the strength to endure a challenging and taxing experience. We understand how wild and confusing that process can be. Now the real work can begin for you to use the experience of a bad trip to positively affect your life—this work is known as psychedelic integration .
Fortunately, we are smack dab in the middle of the psychedelic renaissance where support and integration services are more available than they have ever been. If you are preparing for an upcoming experience, you may want to seek the guidance of a trip facilitator.
And if you feel a lasting negative effect from taking psychedelics or want to discuss your trip in-depth to gain further insight, book a consultation to speak with our guides and trip sitters who are also integration specialists, have first-hand experience, and can help you integrate these powerful, profound events.
Looking for a professionally supported in-person psychedelic experience?
Take the first step and book a consultation call with us today. We'll walk you through every step of the process after getting to know you and your unique situation.
Related posts

What are the Long-Term Effects of Psychedelic Use?
If you were to do a Google search on the long-term effects of psychedelics, you may quickly see words like damaging, physical harm, disturbances, and

Can Psilocybin Mushroom Strain Predict Effect Differences?
Psilocybin mushrooms, commonly known as “magic mushrooms,” have been integral to human cultures for centuries, revered for their profound psychedelic properties. In recent times, a

At Psychedelic Passage, we offer professional 1-on-1 guidance and companionship on your journey of healing. We simply can't sit back and let Americans continue to sit in silent suffering trying to battle mental health issues within a broken health care system, all while knowing that effective alternatives exist. We stand for the sacred, at-home, ceremonial use of psychedelics for consciousness exploration, which we believe to be a fundamental human right.
Everything you need to know about how our service works
See the questions most of our clients ask
All you need for proper preparation, integration and ceremony
Sign up for our newsletter and get our free psilocybin sourcing guide
We only send you what you need to know to use psychedelics for your healing journey.

- Website by SQ & TWD
- Privacy Policy
- Terms of Use
- © Psychedelic Passage. All rights reserved
DISCLAIMER: Psychedelic Passage does not provide psychoactive or controlled substances. Many controlled substances are illegal. The illegal use of a controlled substance may result in criminal consequences. Using controlled substances outside of the lawful supervision of a medical professional may also result in serious health complications including death. We are not licensed therapists, counselors, or medical professionals. We are not spiritual guides or scientists. We are a harm reduction company. Please use your discretion and consult a medical professional to ensure our services meet your needs. Any referrals to third parties that we may provide are informational, for your convenience only, and based on the criteria you provide to us. You are solely responsible for making a selection of a practitioner or other service and determining whether he/she/they are appropriate for you. No referral is an endorsement or recommendation of the practitioner or their services. Please conduct your due diligence on any practitioner you use. We do not provide referrals to “underground” (illegal) psychedelic services. Any information received through our services should be considered for educational purposes and not be misconstrued as medical or legal advice. Please use your discretion and consult with a medical professional to ensure our services meet your needs.
1312 17th St PMB 71622 Denver, CO 80202
Search for anything like: microdosing, dosage, integration
Download Our Free Psilocybin Sourcing Guide!
For harm-reduction purposes, we provide links to online psilocybin vendors, local stores, delivery services, and spore vendors for growing your own medicine at home.
Congratulations! We've sent the sourcing guide to your inbox.
You can now close this window.
Get Your Free Psilocybin Sourcing Guide!
Just tell us where to send it…
- VIRTUAL PROGRAM
- Call 24/7: 877-505-4673 TAP TO CALL

- Hallucinogens and Tripping
- Addiction Blog
Table of Content
- Signs and Symptoms
- Risk Factors
- Success Stories
- Short and Long Term Effects
- Affects on the Body
- Types of Treatment
- Our Treatment Process
- Benefits of Seeking Treatment
- Begin Your Treatment Journey
- Drug Addiction Treatment
Education efforts on substance abuse tend to leave out one important class of drugs: hallucinogens. Although humanity has used them for various purposes for thousands of years, the average person understands them poorly, and research is still revealing new and surprising information about them. What do hallucinogens do, and how dangerous are they? This guide will give you the information you need to understand hallucinogens and tripping, as well as the consequences of abusing this class of drug.
What Are Hallucinogens?
Simply put, hallucinogens are drugs that cause the user to have hallucinations. These hallucinations represent an extreme distortion in how the person perceives reality and the stimuli in the world around them. They may see anything from subtle visual and auditory changes to heavily warped representations of their surroundings, and may even visualize things that are not there at all. Hallucinogens also alter emotion and cognition, producing intense emotions from extreme euphoria to debilitating terror depending on a variety of factors.
What Are the Types of Hallucinogens?
Schedule i vs. schedule ii hallucinogens, what is tripping, what to do when someone is having a bad trip, can you overdose on hallucinogens, are hallucinogens addictive, how is a hallucinogen addiction treated, choose gateway foundation for hallucinogen addiction treatment.
“Hallucinogen” is an umbrella term that covers three separate categories of drug. Each category possesses a certain set of effects that determine how people use them, as well as different levels of relative safety.
1. Psychedelics
Psychedelics are the most commonly known hallucinogen and are a staple of pop culture. When people wonder what hallucinogens do, they’re usually asking about psychedelics. The origin of the term springs from the Greek words “psyche,” meaning “soul” or “mind,” and “delein,” meaning “to manifest.” This alludes to the idea that psychedelics bring out hidden elements and visions from the recesses of the human mind. Proponents of psychedelics believe they have the power to unlock divine or otherwise spiritually profound experiences. Psychedelics are further classified into two categories: serotonergic psychedelics and serotonin releasers.
Serotonergic Psychedelics
Serotonergic psychedelics are known as the “classic” psychedelics. Their method of action modifies the normal transmission of serotonin within the central nervous system (CNS). Serotonin is responsible for a multitude of functions in the body, including mood balance and sensory perception. It is often referred to as the “happy chemical” due to its influence on feelings of happiness and well-being.
Lysergic acid diethylamide, more commonly known as LSD or acid, is an illegal semi-synthetic drug famous for causing extreme distortion of sensory perception as well as hallucinations. It is partially derived from a fungus called ergot, which grows on certain grains. LSD activates serotonin receptors and stimulates serotonin production. The receptors affected are those that help us perceive and interpret the world, and LSD causes them to filter out less stimuli, leading to overstimulation. This overstimulation produces significant changes in cognition, perception, attention and emotional state.
LSD was originally created in 1938 as a way to treat respiratory depression, and its hallucinogenic properties were discovered through accidental absorption into the skin. During the 1960s, it became popular for recreational use. In 1967, the Drug Enforcement Administration (DEA) classified it as a Schedule I drug, and its popularity has decreased since.
2. Psilocybin
Psilocybin is a hallucinogen found in certain types of “magic mushrooms.” This Schedule I substance is used recreationally for the euphoria and distortion of the senses it induces. Psilocybin doesn’t always cause the user to have full-fledged hallucinations. Typically, it changes the way people perceive people and objects that are actually present in the environment. The hallucinogenic effects of this substance usually take under 30 minutes to begin after ingestion and may last around four to six hours.
Psilocybin is most commonly brewed into a tea or used in the preparation of a food item, as its flavor is quite bitter and unpleasant. Some psilocybin comes in capsules filled with the powder of dried and crushed mushrooms. Psilocybin has a wide range of potency, which depends on factors including:
- Mushroom species
- Origin and growing conditions
- Period of harvest
- Fresh or dried state
One thing many people don’t realize is that dried mushrooms are significantly more potent than fresh ones. This fact may lead to inexperienced individuals taking too much and having negative experiences.
3. Mescaline and Peyote
Mescaline is the active ingredient found in the fruit and seeds present on the outside of the peyote cactus. When using peyote for its hallucinogenic effects, people gather and dry the fruit or seeds. They can be eaten or brewed into a tea, as well as ground into powder for capsules similar to those made from psilocybin mushrooms. The pure form of mescaline, mescaline sulfate, can be synthesized in a lab environment, resulting in a crystalline white product.
Mescaline produces an altered state of consciousness that many people report as being euphoric and dream-like, which can last for around 10 to 12 hours. Mescaline has been used by many indigenous peoples as a religious sacrament for thousands of years and is one of the oldest psychedelics known. In these cases, the hallucinogenic experience is purposely extended for multiple days.
Serotonin Releasers
The other broad category within psychedelics is serotonin releasers. This class includes “club drugs” such as MDMA . The effects of hallucinogens in this category include:
- Feelings of openness
- Increased empathy
- Feelings of general love
- Increased self-awareness
- Mild auditory and visual distortions
The mild hallucinogenic effect in combination with the emotional effects of serotonin release are often viewed as enhancements to social and music experiences.
2. Dissociatives
Dissociative drugs can be very dangerous. They create visual and auditory distortion like psychedelics, but they are also accompanied by the sensation of floating and feeling detached from reality or one’s body. Dissociatives frequently cause:
- Impaired motor function
- Memory loss
The effects of dissociatives are very unpredictable and some users end up feeling them for days after ingesting the substance.
Phencyclidine (PCP) or “ angel dust ” is a street drug sold as a powder to be dissolved in water. It is sometimes dissolved in alcohol, typically with disastrous results. PCP was developed in the 1920s as an anesthetic, and its ability to eliminate pain is one of its more dangerous aspects when used recreationally. It contributes to a sense of invincibility that leads users to take extremely dangerous actions, such as jumping out of windows or walking into traffic.
The effects of PCP often include feelings of euphoria combined with distortions in the perception of light, color, sound and touch as well as time. PCP has many surprising street names, including:
- Embalming fluid
- Killer weed
- Rocket fuel
- Super grass
Ketamine , developed in 1962 , started out as an anesthetic. However, its hallucinogenic effects precipitated its use as a recreational drug. Ketamine produces a sensation of floating and dissociation, which typically lasts only an hour or less, but other effects that alter the senses, as well as judgment and coordination, can last for up to 24 hours.
If someone takes a large dose of ketamine, they may enter what is known as a “K-hole.” This state occurs when the user is almost completely sedated, and people describe it as having a near-death or out-of-body experience.
Dextromethorphan (DXM), also called “robo,” is one dissociative hallucinogen most people don’t realize is highly accessible to those who want to abuse it. Its cough-suppressing capabilities make it a common ingredient in a variety of “extra strength” over-the-counter cough syrups and cold medications. At low dosages, DXM may create low-grade visual distortions and have a mild stimulant effect. At high doses, it displays the same dissociative effects of hallucinogens like Ketamine and PCP. DXM is especially popular among teens and young adults because it is relatively easy to obtain.
3. Deliriants
Deliriants are the least desirable of hallucinogens for recreational use. Rather than inducing a semi-lucid state like psychedelics do, deliriants cause a state of delirium. People under the influence of deliriants may do things like:
- Have complete conversations with imaginary people.
- Finish a complex task like getting dressed only to find that they never actually started the action.
- Be unable to recognize themselves in a mirror.
These effects tend to evoke feelings of fear and panic rather than the pleasurable experience most people are seeking when they use hallucinogens.
DPH (Benadryl)
The most common deliriant is diphenhydramine (DPH), which is used as an antihistamine in the popular medication Benadryl. When taken outside the recommended dosage, DPH has extreme sedation and deliriant effects. People who take too much Benadryl frequently report having vivid and terrifying hallucinations akin to bad nightmares.
The DEA labels most hallucinogens as controlled substances . Schedule I drugs are those determined to meet the following criteria:
- High potential for abuse.
- No accepted medical use in treatment in the United States.
- Lack of accepted safety for use of the substance even under medical supervision.
Schedule I hallucinogens include psilocybin, LSD and mescaline. Most hallucinogens fall under Schedule I.
Schedule II substances are described in the following terms:
- High potential for abuse
- Currently accepted for use in medical treatment in the United States
- Can lead to severe psychological or physical dependence
PCP is a Schedule II drug.

Someone on a trip will experience emotional changes as well, affecting how they feel about themselves, others and the world at large. These changes may be perceived as positive or negative, based on several unpredictable variables.
Good Trips vs. Bad Trips
People take hallucinogens with the intent to have a positive experience. A positive hallucinogenic experience is marked by a pleasant dream-like state, enjoyable perceptual distortions and in some cases spiritual realizations. A person will come out of a good trip feeling fulfilled, whether recreationally or on a deeper level.
Bad trips are comparable to nightmares. In a bad trip, visual and auditory distortions are frightening and may take the shape of monsters or more abstractly frightening entities. A bad trip induces fear and often panic, which can cause people to feel like the world is ending or that they are in imminent danger. A bad hallucinogenic experience creates paranoia and a feeling of losing one’s mind, which is often more than enough to keep people from trying this class of drugs again.
Being around someone who is having a bad trip can be a stressful situation whether or not you are also consuming hallucinogens. Here are five tips you can use to help someone who is having a bad trip.
1. Don’t Panic
Remaining rooted in reality is one of the best ways to help someone on a bad trip. The person is likely agitated and paranoid, which makes them highly sensitive to the cues of the people around them. Remaining calm throughout the ordeal will help keep the tripping person’s fear from escalating and may help them calm down.
2. Reaffirm Safety
One of the worst parts of a bad trip is the feeling of danger and impending doom. The person may feel that something or someone is “out to get them” and reminding them that they are in a safe place with people who care about them can help reduce their disorientation and paranoia.
3. Try Breathing Exercises
As panic sets in, a tripping person might start hyperventilating, leading to further negative physical effects like rapid heart rate and high blood pressure. If you can, get the person to participate in some simple exercises to help regulate breathing and calm them down.
4. Offer Water
Giving the person a glass of cold water can help in two ways. For one, panicking over a bad trip can increase dehydration, creating physical symptoms that make the trip even worse. Additionally, having to hold onto a glass of water and coordinate the action of drinking can force the person to focus more on reality instead of continuing down the rabbit hole of a bad trip.
Psychedelics are not inherently toxic and do not cause overdoses in the way most people think of them. Taking a large dose of psychedelics is not likely to harm organs through inherent toxicity, and will simply result in an extreme, uncontrollable trip that can easily turn bad. However, hallucinogens can cause people to act in dangerous and erratic ways that may lead to life-threatening injuries.
Dissociative and deliriant drugs, on the other hand, can be extremely dangerous if taken in overdose quantities. For instance, the effects of a ketamine overdose include:
- Respiratory depression
- Hypotension
- Bradycardia
- Heart attack
For this class of hallucinogens, an overdose can be fatal if the person doesn’t receive medical care in time.
They can be, although psychedelics are not known to cause physical dependence. LSD, for example, does not cause compulsive drug-seeking behavior and is therefore not considered addictive in the traditional sense. However, continued use does result in tolerance, and the person using it will eventually have to take more and more to achieve the desired effect. This is highly dangerous given how unpredictable all hallucinogens can be.
Other types of hallucinogens such as PCP and ketamine can be highly physically addictive and produce common symptoms of addiction such as headaches, drug cravings and severe sweating upon cessation of the drug. Regardless of the category, one of the long-term effects of hallucinogens is addiction.
Like other types of addiction, addiction to hallucinogens can be treated at multiple levels of care. Depending on the severity of the addiction and the presence of other issues such as mental illness or abuse of multiple drugs, a person can receive effective treatment in these formats.
1. Residential Treatment
Residential drug rehab centers are an effective option for people who are struggling with a dual diagnosis or abusing multiple substances at the same time. The structured and supportive environment eliminates the opportunity to relapse and provides the most rigorous level of treatment.
2. Partial Hospitalization

3. Outpatient Treatment
For people who have been abusing hallucinogens only and have not developed severe drug-seeking symptoms, outpatient treatment can be highly effective. These programs offer many of the same treatment methods available in residential and partial hospitalization programs on a flexible part-time basis. They are ideal for people who need addiction treatment but can’t give up responsibilities like work, school or childcare.
4. Therapy and Support
For any addiction treatment program to be successful, it must include robust offerings of therapy and support groups. To overcome addiction and begin on the path to a successful recovery, individuals have to get to the root of underlying issues that contributed to the development of their substance abuse problems.
Each individual may benefit from therapy differently. Those who have trouble identifying and processing their emotions can benefit greatly from dialectical behavioral therapy (DBT). People whose addiction arose as a result of a traumatic event or traumatic circumstances can benefit from trauma-informed therapy .
Processing one’s addiction and recovery in groups is essential for helping people realize they are not alone. Interacting with peers who understand the issues at hand is beneficial in building a support network for treatment and beyond. A good addiction treatment program will also offer family therapy to help inform and support the family system in recovery. Having multiple clinical services is a hallmark of an effective treatment program.
Although hallucinogen addiction is relatively rare, it can be just as devastating as addiction to other substances — especially if the substance being abused is a dissociative or a deliriant. Gateway Foundation understands the importance of using evidence-based treatment to combat all addictions, and we offer a wide variety of therapy options for those who are struggling with hallucinogen and other addictions.
If you or someone you care about is abusing hallucinogens, Gateway Foundation can help. Our team of experts is ready to create a personalized addiction treatment plan that addresses the unique needs and circumstances of each individual. Reaching out for help can feel frightening, but the long-term effects of hallucinogens make it imperative to seek treatment as soon as possible. To learn more about the programs and services available at Gateway Foundation, call us at 877.505.4673 or contact us online . Our knowledgeable and compassionate representatives are ready to answer your questions and get you or your loved one started on the path to recovery from hallucinogen addiction.
Gateway Foundation
Gateway Foundation is a recognized leader in evidence-based addiction treatment proven to get results. Our experts in Addiction Medicine—including highly educated clinical and medical professionals and expert psychiatrists and nurses—deliver care that never stops. For over 50 years, Gateway Foundation has been helping individuals and their families recover from addictions and behavioral health issues and is the only provider that covers the entire state of Illinois with 16 facilities from the Wisconsin Border to the Kentucky Border. Gateway has specific programs focusing on substance use disorders, trauma, depression, anxiety, and other co-occurring issues. We’re licensed by the state of Illinois and accredited by the Joint Commission. We are in-network with all the major commercial insurance plans. Gateway Foundation: Addiction medicine, saving lives.
Summer Substance Use Among Youth
Violence, Substance Abuse and Mental Illness

Addiction Destroys Dreams, We Can Help
The New York Times
Magazine | my adventures with the trip doctors, my adventures with the trip doctors.
By MICHAEL POLLAN MAY 15, 2018
The researchers and renegades bringing psychedelic drugs into the mental health mainstream.
The Health Issue
Guided explorations.
By MICHAEL POLLAN
By SULEIKA JAOUAD
Machine Medicine
By ABRAHAM VERGHESE
Critical Care
By KIM TINGLEY
By MICHAEL POLLAN Illustrations by CHRISTOPH NIEMANN MAY 15, 2018
M y first psilocybin journey began around an altar in the middle of a second-story loft in a suburb of a small city on the Eastern Seaboard. On this adventure I would have a guide, a therapist who, like an unknown number of other therapists administering psychedelics in America today, must work underground because these drugs are illegal. Seated across the altar from me, Mary (who asked that I use a nickname because of the work she does) began by reciting, with her eyes closed, a long and elaborate prayer derived from various Native American traditions. My eyes were closed, too, but now and again I couldn’t resist peeking out for a glance at my guide: a woman in her 60s with long blond hair parted in the middle and high cheekbones that I mention only because they would, in a few hours, figure in her miraculous transformation into a Mexican Indian.
I also stole a few glances at the scene: the squash-colored loft with its potted plants and symbols of fertility and female power; the embroidered purple fabric from Peru that covered the altar; and the collection of items arrayed across it, including an amethyst in the shape of a heart, a purple crystal holding a candle, a bowl containing a few squares of dark chocolate, the personal “sacred item” that Mary had asked me to bring (a little bronze Buddha a friend brought me from Tibet) and, set squarely before me, an antique plate holding the biggest psilocybin mushroom I had ever seen.
The crowded altar also held a branch of sage and a stub of palo santo, a fragrant wood that some Indians in South America burn ceremonially, and the jet-black wing of a crow. At various points in the ceremony, Mary would light the sage and the palo santo, using the crow’s wing to “smudge” me with the smoke — guiding the spirits through the space around my head.
The whole scene must sound ridiculously hokey, not to mention laced with cultural appropriation, yet the conviction Mary brought to the ceremony, together with the aromas of the burning plants and the spooky sound of the wing pulsing the air around my head — plus my own nervousness about the journey in store — cast a spell that allowed me to suspend my disbelief. Mary trained under one of the revered “elders” in the psychedelic community, an 80-something psychologist who was one of Timothy Leary’s graduate students at Harvard. But I think it was her manner, her sobriety and her evident compassion that made me feel sufficiently comfortable to entrust her with, well, my mind.
As a child growing up outside Providence, R.I., Mary was an enthusiastic Catholic, she says, “until I realized I was a girl” — a fact that would disqualify her from ever performing the rituals she cherished. Her religiosity lay dormant until, in college, friends gave her a pot of honey infused with psilocybin for her birthday; a few spoonfuls of the honey “catapulted me into a huge change,” she told me the first time we met. The reawakening of her spiritual life led her onto the path of Tibetan Buddhism and eventually to take the vow of an initiate: “ ‘To assist all sentient beings in their awakening and enlightenment.’ Which is still my vocation.”
And now seated before her in her treatment room was me, the next sentient being on deck, hoping to be awakened. She asked me to state my intention, and I answered: to learn whatever the “mushroom teachers,” as she called them, could teach me about myself and about the nature of consciousness.
Psychedelic therapy, whether for the treatment of psychological problems or as a means of facilitating self-exploration and spiritual growth, is undergoing a renaissance in America. This is happening both underground, where the community of guides like Mary is thriving, and aboveground, at institutions like Johns Hopkins, New York University and U.C.L.A., where a series of drug trials have yielded notably promising results.
I call it a renaissance because much of the work represents a revival of research done in the 1950s and 1960s, when psychedelic drugs like LSD and psilocybin were closely studied and regarded by many in the mental health community as breakthroughs in psychopharmacology. Before 1965, there were more than 1,000 published studies of psychedelics involving some 40,000 volunteers and six international conferences dedicated to the drugs. Psychiatrists were using small doses of LSD to help their patients access repressed material (Cary Grant, after 60 such sessions, famously declared himself “born again”); other therapists administered bigger so-called psychedelic doses to treat alcoholism, depression, personality disorders and the fear and anxiety of patients with life-threatening illnesses confronting their mortality.
That all changed in the mid-’60s, after Timothy Leary, the Harvard psychologist and lecturer turned psychedelic evangelist, began encouraging kids to “turn on, tune in and drop out.” Silly as that slogan sounds to our ears, a great many kids appeared to follow his counsel, much to the horror of their parents. The drugs fell into the eager embrace of a rising counterculture, influencing everything from styles of music and dress to cultural mores, and, many thought, inspired the questioning of adult authority that marked the “generation gap.” “The kids who take LSD aren’t going to fight your wars,” Leary famously claimed. In 1971, President Nixon called Leary, who by then had been drummed out of academia and chased by the law, “the most dangerous man in America.” That same year, the Controlled Substances Act took effect; it classified LSD and psilocybin as Schedule 1 drugs, meaning that they had a high potential for abuse and no accepted medical use; possession or sale became a federal crime. (MDMA, which was still being used therapeutically, was not banned until 1985, after it became popular as a party drug called Ecstasy.) Funding for research dried up, and the legal practice of psychedelic therapy came to a halt.
But beginning in the 1990s, a new generation of academics quietly began doing psychedelics research again, much of it focusing on people with cancer. Since then, several dozen studies using psychedelic compounds have been completed or are underway. In a pair of Phase 2 psilocybin trials at Hopkins and N.Y.U., 80 cancer patients, many of them terminal, received a moderately high dose of psilocybin in a session guided by two therapists. Patients described going into their body and confronting their cancer or their fear of death; many had mystical experiences that gave them a glimpse of an afterlife or made them feel connected to nature or the universe in a way they found comforting. The studies, which were published in The Journal of Psychopharmacology in December 2016, reported that 80 percent of the Hopkins volunteers had clinically significant reductions in standard measurements of depression and anxiety, improvements that endured for at least six months.
Other, smaller studies of psilocybin have found that one, two or three guided sessions can help alcoholics and smokers overcome their addictions; in the case of 15 smokers treated in a 2014 pilot study at Hopkins, 80 percent of the volunteers were no longer smoking six months after their first psychedelic session, a figure that fell to 67 percent after a year — which is far better than the best treatment currently available. The psychedelic experience appears to give people a radical new perspective on their own lives, making possible a shift in worldview and priorities that allows them to let go of old habits.
Yet researchers believe it is not the molecules by themselves that can help patients change their minds. The role of the guide is crucial. People under the influence of psychedelics are extraordinarily suggestible — “think of placebos on rocket boosters,” a Hopkins researcher told me — with the psychedelic experience profoundly affected by “set” and “setting” — that is, by the volunteer’s interior and exterior environments. For that reason, treatment sessions typically take place in a cozy room and always in the company of trained guides. The guides prepare volunteers for the journey to come, sit by them for the duration and then, usually on the day after a session, help them to “integrate,” or make sense of, the experience and put it to good use in changing their lives. The work is typically referred to as “psychedelic therapy,” but it would be more accurate to call it “psychedelic-assisted psychotherapy.”
Though the university researchers seldom talk about it, much of the collective wisdom regarding how best to guide a psychedelic session resides in the heads of underground guides like Mary. These are the people who, in many cases, continued to do this work illicitly, long after the backlash against psychedelics during the 1960s ended most research and therapy. But their role in the current renaissance is an awkward one, as I discovered early this spring when I sat in on the nation’s first certificate program for aspiring psychedelic guides.
On a Friday afternoon in late March, 64 health care professionals of various stripes — doctors, therapists, nurses, counselors and naturopaths — gathered in Namaste Hall at the California Institute of Integral Studies (C.I.I.S.), a school of psychology and social sciences in San Francisco, to begin their training to become legal psychedelic therapists. To be admitted to the program, an applicant must have a professional medical or therapy license of some kind, and most of the trainees — whose average age looked to be about 45 and whose number included nine psychologists, nine psychiatrists and four oncologists — had enrolled in this certificate program in the belief that psychedelic drugs like psilocybin and MDMA, administered with the proper support and guidance, hold the potential to revolutionize mental health treatment. The career path might not be clear or straight yet, but these people want to be ready to lead that revolution when it arrives — which may be sooner than we think.
It quickly became clear that the reason most of the people in the room were willing to devote the time (five weekends and one full week over nine months) and the money ($7,800) to be certified as a graduate of the program is that they’d been persuaded — often by personal experience — of the therapeutic potential of these compounds. As Manish Agrawal, a rugged 48-year-old oncologist who practices in Maryland, told me, with a sardonic lift of an eyebrow, “You don’t do something like this because you read a magazine article.”
The drugs at the center of the therapy being taught — still classified by the government as Schedule 1 — cannot be used in the training, a limitation that both students and instructors lamented. (C.I.I.S. plans to petition the F.D.A. for permission to give psilocybin and MDMA to students in future trainings.) And while most of the faculty was drawn from the ranks of therapists who work in sanctioned clinical trials of psilocybin and MDMA, because so much of the relevant experience belongs to guides who have been working underground, the program draws on the wisdom of these people too. Though the program’s explicitly stated intention is to train guides to work in the world of legal psychedelic therapy, that world (apart from the handful of clinical trials) doesn’t quite exist yet, while the psychedelic underground beckons right now.
Janis Phelps, a psychologist and C.I.I.S. administrator who established and directs the program, forthrightly confronted the issue in her introductory remarks to the class Friday evening. “We are training you to be aboveground therapists,” she emphasized. “If you are thinking of working underground” — she later told me a strenuous effort had been made to weed out such people — “you need to think about that. Because we want you to be aboveground, F.D.A.-approved therapists. Everyone engaged in this research is squeaky clean.”
She looked out over the room of aspiring guides. “So I invite you into the tensions of the field as it now exists.”
Bill Richards, clinical director of the psychedelics-research program at Johns Hopkins and the author of “Sacred Knowledge: Psychedelics and Religious Experiences,” is one of the few surviving links between the first and second waves of sanctioned psychedelic research in America. A jovial, goateed psychologist in his 70s with an infectious cackle, Richards led off the weekend’s instruction on Saturday morning. Working at the Maryland Psychiatric Research Center at Spring Grove in the 1970s, Richards and his colleagues successfully treated alcoholics, cancer patients and people suffering from depression with LSD until 1976, when research at the center shut down. “How can this ever have been illegal?” Richards likes to say. “It’s as if we made entering Gothic cathedrals illegal, or museums, or sunsets!”
When research with psilocybin resumed in the 1990s, Johns Hopkins recruited Richards because of his long experience guiding patients during a high-dose psychedelic experience. Today’s researchers work with psilocybin and MDMA because a session tends to be shorter than with LSD and because the words carry much less political baggage. Since the ’60s, LSD has been associated in the public mind with the counterculture and with stories, true or not, of people jumping off buildings thinking they could fly, blinding themselves by staring at the sun or landing themselves in the emergency room after psychotic episodes. MDMA and psilocybin are less well known and don’t seem to have the same associations. (Also, the fact that psilocybin is “natural” — derived from a mushroom — seems to count in its favor.) Richards has trained many of the guides now working in clinical trials not only at Hopkins but also at N.Y.U. and at Imperial College London.
In his PowerPoint presentation, Richards laid out what has become the standard protocol for aboveground psychedelic therapy, and the role of the guide at each of the three principal stages of “the journey.” First comes a series of preparation sessions, in which volunteers are told what to expect, asked to set an intention (to quit smoking, say, or confront their fear of death) and offered a set of “flight instructions” for the journey ahead. These generally advise surrendering to the experience, whatever it brings and however disturbing it might become. (“Trust, let go, be open” is one mantra he recommends, or, borrowing from John Lennon, “Turn off your mind, relax and float downstream.”) If you feel as if you are “dying, melting, dissolving, exploding, going crazy, etc. — go ahead.” Richards stressed how important it is for the guide to quickly establish a rapport with volunteers, so that during the session “they can let themselves ‘die’ or go crazy — that requires an awful lot of trust!” Because the patients’ ego defenses are likely to be disabled by the drug, it’s crucial that they feel safe.
The second stage is the journey itself. Richards showed a slide of the Hopkins treatment room, decorated to look like the office of a psychiatrist with an interest in Eastern religion and indigenous peoples, with shelves holding large-format art books and spiritual tchotchkes, including a Buddha and a large ceramic mushroom. The volunteer stretches out on a couch and puts on eyeshades and headphones to encourage an inward journey free of distraction. (Richards has put together a playlist consisting mainly of classical compositions arranged to support and structure the experience.) Two guides, typically one male, the other female, sit with the volunteer for the duration but say very little, allowing the journey to unfold according to its own logic. Mostly the guide is present to offer a comforting hand if the journeyer is struggling, jot down anything she has to say and generally keep an eye on the volunteer’s physical well-being while she is roaming her psychic landscape. Because it is the drug and the mind that drive the journey and not the therapist, the guide’s role calls for an unusual degree of humility, restraint and patience — the sessions can last for hours. (No snoozing or checking of email; meditating, however, is O.K.) Richards describes the session as the “ pièce de résistance ” of the work, “in which you’re focused intensely on one human being as if that’s all that exists in the world. It’s a great way to get exhausted!”
The last stage is integration, which typically takes place the following day. Here the guide helps the volunteer make sense of what can be a confusing and inchoate experience, underscoring important themes and offering ideas on how to apply whatever insights may have emerged to the conduct of the volunteer’s life. The challenge, as Richards put it, is to help the volunteer transform “flashes of illumination” (he’s quoting Huston Smith, the late scholar of religion) experienced during the trip “into abiding light” — into a new, more constructive way to regard your self and situation.
It is sometimes said that in the last few decades psychiatry went from being brainless — relying on talk therapies oblivious to neurobiology — to being mindless — relying on drugs, with little attention to the contents of consciousness. If psychedelic-assisted therapy proves as effective as early trials suggest it might, it will be because it succeeds in rejoining the brain and the mind in a radical new therapeutic paradigm: using not just a chemical but the powerful mental experience it can occasion, given the proper support, to disrupt destructive patterns of thought and behavior.
Such a new approach couldn’t come at a better time for a field that is “broken,” as Tom Insel, head of the National Institute of Mental Health until 2015, told me bluntly. Rates of depression (now the leading cause of disability worldwide, according to the W.H.O.) and suicide are climbing; addictive behavior is rampant. Little has changed, meanwhile, in psychopharmacology since the introduction of SSRI antidepressants in the late 1980s. This may explain why prominent figures in the psychiatric establishment are voicing support for psychedelic research. Addressing a conference on psychedelic science in Oakland last spring, Insel and Paul Summergrad, a former president of the American Psychiatric Association, offered encouragement to the psychedelic researchers in the audience, with Insel singling out for praise “the novel approach here” — the way the psychedelic therapist combines pharmacology and psychotherapy to create a single transformative experience.
Psychedelic therapy as the idea is now understood was developed by a group of researchers working in Saskatchewan in the mid-1950s, including the psychiatrists Abram Hoffer, Humphry Osmond (who, in 1957, coined the word “psychedelic,” which loosely translates from the Greek as “mind manifesting”) and their frequent collaborator and muse, a brilliant amateur therapist named Al Hubbard. After both conducting and participating in a great many mescaline and LSD sessions — at the time it was routine for scientists to test drugs on themselves — the researchers observed how variable the experience could be, depending on circumstance and mind-set. In those days, no one knew how best to administer these strange new compounds; the need for a guide wasn’t immediately apparent. Some early scientists in white coats bearing clipboards dosed volunteers in a hospital room with white walls and fluorescent lights. Very often, the volunteers would then be left alone. Researchers didn’t yet understand that the psychedelic experience is not foreordained by the chemical but rather is “constructed” in the mind from an unpredictable mix of expectation, memory, the contents of the unconscious and a variety of environmental factors.
Beginning in the late 1950s, as the researchers began to better grasp the many factors at work, they began to work more consciously with set and setting (though the words wouldn’t be used for another few years), bringing music and images into a treatment room they made comfy and emphasizing the role of a guide. Shamans have known for thousands of years that a person in the depths of a trance or under the influence of a hallucinogenic plant like ayahuasca or peyote can be readily manipulated with the help of certain words, cues, special objects or music. They understand intuitively how the suggestibility of the human mind during an altered state of consciousness can be harnessed as an important resource for healing — for breaking destructive patterns of thought and proposing new perspective in their place. One of the Canadian group’s key contributions to psychedelic therapy was to introduce the tried-and-true tools of shamanism, or rather the Westernized version of it that, to one degree or another, most of today’s psychedelic guides still practice, whether working aboveground or below — though the tools of shamanism play a larger role in the underground.
Before my own psychedelic journey, I met and interviewed more than a dozen such guides, many of them trained by the therapists who were using psychedelics in their practices before they became illegal and decided that, rather than give up a tool they had found to be effective, they would continue to work underground, at substantial personal risk. (Beginning in 1971, possession or sale of most psychedelic drugs was punishable by a prison sentence.) One such therapist was a Bay Area Jungian psychologist named Leo Zeff, perhaps the best-known underground guide of his generation; before his death in 1988, he claimed to have “tripped” 3,000 patients and helped train 150 underground guides, many of whom are still at work.
My travels through the psychedelic-therapy underground convinced me that while the community is obviously far-flung and heterogeneous and has its complement of charlatans, many guides are professionals who share an approach and even a code of conduct. In 2010, a “wiki” for guides appeared on the internet — a collaborative website where individuals could share documents and together create new content — where, for a time, the community appeared to be codifying the rules and standards of the profession. (The site has since vanished or moved.)
On the website, I found a draft charter for would-be guides — “to support a category of profound, prized experiences becoming more available to more people” — as well as links to printable forms for legal releases, ethical agreements and medical questionnaires. (“We don’t have very good insurance,” one guide told me. “So we’re very careful.”) There was also a link to a thoughtful “Code of Ethics for Spiritual Guides,” which acknowledges that “participants may be especially open to suggestion, manipulation and exploitation.” The code stresses that it is incumbent upon the guide to disclose all the psychological and physical risks. (Compared with other psychoactive compounds, psychedelics have low toxicity and are nonaddictive. The risks are primarily psychological: In some people, they can produce short-term anxiety and paranoia and, in rare cases, psychotic episodes. In the current clinical work, an estimated 1,000 volunteers have received psilocybin without a single serious adverse event.) The code also requires that the guide obtain consent, guarantee confidentiality, protect the safety of participants at all times, “safeguard” against ambition and self-promotion and accommodate clients “without regard to their ability to pay.”
Relative to the way guiding is practiced in the aboveground clinical trials (and taught at C.I.I.S.), the underground guides I interviewed, and eventually worked with, take a somewhat more active role in choreographing the experience, bringing into the “ceremony,” as they’re apt to call it, such traditional elements as incense, tobacco and sage smoke, rattles, the singing of icaros (sacred songs) and chanting of prayers.
“There are now two distinct lineages,” I was told by an underground guide with 35 years of experience, who asked me to use a family name, Michelle. “In the Western medical model, the guide is taught never to ‘get ahead of the medicine’ ” — that is, he or she aims for a noninterventionist, back-seat role during the session, and because these are foremost scientific trials, sticks to a standardized protocol in order to minimize the number of experimental variables in play. Many underground guides find this needlessly confining.
“The journey should be customized to each person,” Michelle said. “The idea of playing the same music for everyone makes absolutely no sense.” Instead, she might choose a comforting piece to support someone struggling with a challenging trip, or put on something “chaotic and disassembling” to help break down another client’s defenses. “A healer is not just a sitter. She does stuff.” Many underground guides have traveled extensively in Mexico, Brazil and Peru to study with traditional healers; Michelle believes psychedelic therapy still has much to learn from the “earth peoples” who have made use of psychedelic plants and fungi in their healing ceremonies for thousands of years. She feels the work she does offers more scope for “creativity and intuition” than the rote clinical techniques being taught aboveground allow.
I would have preferred to have my own guided psilocybin session aboveground in the reassuring confines of a medical institution, but the teams at Hopkins and N.Y.U. weren’t currently working with so-called healthy normals (do I flatter myself?) — and I could lay claim to none of the serious mental problems they were studying. I wasn’t trying to fix anything big — not that there wasn’t room for improvement. Like many people in late middle age, I had developed a set of fairly dependable mental algorithms for navigating whatever life threw at me, and while these are undeniably useful tools for coping with everyday life and getting things done, they leave little space for surprise or wonder or change. After interviewing several dozen people who had undergone psychedelic therapy, I envied the radical new perspectives they had achieved. I also wasn’t sure I’d ever had a spiritual experience, and time was growing short. The idea of “shaking the snow globe” of my mental life, as one psychedelic researcher put it, had come to seem appealing.
In Mary, I had found an underground guide with whom I felt comfortable. Mary’s approach, in terms of dosage, also happened to approximate the aboveground experience, though she worked with whole mushrooms rather than the capsules of synthetic psilocybin used in the university trials.
“The mushroom teachers help us to see who we really are,” Mary said, as we sat across the altar from each other. “They bring us back to our soul’s purpose for being here in this lifetime.” By now I was inured to the New Age lingo. I was also impressed, and reassured, by Mary’s professionalism. In addition to having me consent to the standard “agreements” (bowing to her authority for the duration; remaining in the room until she gave me permission to leave; no sexual contact), she had me fill out a detailed medical form, a legal release and an autobiographical questionnaire that resulted in 15 pages of writing it took me the better part of a day to complete. All of which made me feel I was in good hands, even when those hands were flapping a crow’s wing around my head.
On my tongue, the dried mushroom, which was easily four inches long and had a cap the size of a golf ball, was as parched as desert sand and tasted like earth-flavored cardboard, but alternating each bite with a nibble of chocolate helped me get it down. We chatted quietly for 20 minutes or so before Mary noticed that my face was flushed and suggested I lie down and put on eyeshades. As soon as Mary put on the first song — an insipid New Age composition by someone named Thierry David (an artist thrice nominated, I later learned, in Zone Music Reporter’s category of Best Chill/Groove Album) — I was immediately propelled into a nighttime urban landscape that appeared to have been generated by a computer.
I was experiencing synesthesia, in which one sense gets crosswired with another, so that sound was creating visual space, and what I took to be David’s electronica conjured a depopulated futuristic city, with each note giving rise to another soft black stalagmite or stalactite that together resembled the high-relief soundproofing foam used to line recording studios. I moved effortlessly through this digital nightscape as if within the confines of a dystopian video game. Though the place wasn’t particularly frightening and had a certain sleek beauty, I hated being in it and wished to be somewhere else, but it went on and on, seemingly forever. I asked Mary to please play something else, and though the mood shifted with the new music, I was still stuck — trapped — in this sunless computer world. Why, oh why, couldn’t I be outside?
This could easily take a terrifying turn, it occurred to me, and with that a dim tide of anxiety began to build. Recalling the flight instructions, I told myself there was nothing to do but let go and surrender to the experience. Relax and float downstream. I realized I was no longer captain of my attention, able to direct it this way or that and change the mental channel at will. No, this was more like being strapped into the front car of a cosmic roller coaster, its heedless headlong trajectory determining moment by moment what would appear in my field of awareness.
Actually, that’s not entirely true: All I had to do was remove my eyeshades, and reality, or at least something loosely based on it, would re-present itself. This is what I now did, partly to satisfy myself that the world still existed but mostly because I badly needed to pee. Sunlight and color flooded my eyes, and I drank it in greedily, surveying the room for the welcome signifiers of nondigital reality: walls! Windows! Plants! But this reality appeared in a new aspect: jeweled with morning light, every beam of it addressed to my eyes. I got up carefully from the mattress, and Mary took me by the elbow, geriatrically, and together we made the long journey across the loft to the bathroom. I avoided looking at her, uncertain what I might see in her face or betray in mine.
After producing the most spectacular crop of diamonds, I made my unsteady way back to the mattress and lay down. Mary, speaking softly, asked if I wanted “a booster.” I sat up to receive another mushroom, for a total of about four grams. Mary was kneeling next to me, the mushroom in her upturned palm, and when I finally looked up into her face, I saw she had turned into María Sabina, the Mazatec curandera whom I had read about. Sixty years ago, Sabina gave psilocybin mushrooms to R. Gordon Wasson, supposedly the first Westerner to try them, in a dirt-floored basement of a thatch-roofed house in the remote mountains of Oaxaca. Mary’s hair was now black; her face, stretched taut over its high cheekbones, was anciently weathered; and she was wearing a simple white peasant dress. I took the desiccated mushroom from the woman’s wrinkled brown hand and looked away as I chewed; I didn’t think I should tell Mary what had happened to her.
When I put my eyeshades back on and lay down, I was disappointed to find myself back in computer world, but something had changed, no doubt a result of the stepped-up dose. Whereas before I navigated this landscape as myself, taking in the scene from a perspective recognizable as my own, with my attitudes intact (highly critical of the music, for instance), now I watched as that familiar self began to fall apart before my eyes, gradually at first and then all at once.
“I” now turned into a sheaf of little papers, no bigger than Post-its, and they were being scattered to the wind. But the “I” taking in this seeming catastrophe had no desire to chase after the slips and pile my old self back together. No desires of any kind, in fact. And then I looked and saw myself out there again, but this time spread over the landscape like paint, or butter, thinly coating a wide expanse of the world with a substance I recognized as me.
But who was this “I” that was able to take in the scene of its own dissolution? Good question. It wasn’t I, exactly. Here the limits of our language become a problem: In order to completely make sense of the divide that had opened up in my perspective, I would need a whole new first-person pronoun. For what was observing the scene was a vantage and mode of awareness entirely distinct from my accustomed self. Where that self had always been a subject encapsulated in this body, this one seemed unbounded by any body, even though I now had access to its perspective. That perspective was supremely indifferent, unperturbed even in the face of what should have been an unmitigated personal disaster. The very category “personal,” however, had been obliterated. Everything I once was and called me, this self six decades in the making, had been liquefied and dispersed over the scene. What had always been a thinking, feeling, perceiving subject based in here was now an object out there. I was paint!
Lots of other things happened in Mary’s room, and in my head, during the course of my journey that day. I gazed into the bathroom mirror and saw the face of my dead grandfather. I trudged through a scorched desert landscape littered with bleached bones and skulls. One by one appeared the faces of the people in my life who had died, relatives and friends and colleagues whom, I was being told, I had failed properly to mourn. I beheld Mary transformed once again, this time into a ravishing young woman in the full radiance of youth; she was so beautiful I had to turn away.
At one point Mary put on one of Bach’s unaccompanied cello suites. It was the suite in D minor, a spare, infinitely sad piece that I’d heard many times before, often at funerals. But this time was different, because I heard it in my egoless, nondual state of consciousness — though “heard” doesn’t do justice to what transpired between Bach’s notes and me. The preposition “between” melted away. Losing myself in the music became a kind of rehearsal for losing myself, period. I let go of the rope of self and slipped into the warm waters of this ineffable beauty — Bach’s sublime notes, I mean, drawn from a cello’s black well of space by Yo-Yo Ma’s mournful bow as it surfed across its strings. I became identical to the music, a word that doesn’t begin to describe the power of what these unearthly vibrations were, or explain how they somehow lifted up and carried me beyond the reach of all suffering and regret.
The sovereign ego, with all its armaments and fears, its backward-looking resentments and forward-looking worries, was simply no more, and there was no one left to mourn its passing. And yet something had succeeded it: this bare, disembodied awareness, which gazed upon the scene of the self’s dissolution with benign indifference. I was present to reality but as something other than my usual self. And although there was no self left to feel, exactly, there was a feeling tone, and that was calm, unburdened, content. There was life after the death of the ego.
The Sunday-morning session at C.I.I.S. began with great anticipation — the speaker was Ralph Metzner, who worked with Timothy Leary at Harvard and is regarded as one of the wise elders in the psychedelic community.
Metzner is in his 80s now, and stepping up to the microphone in his newsboy’s cap, he seemed frail. For much of his presentation, he read from one of his books — something about the soul and the six archetypal paths through this life. It wasn’t until the Q. and A. that things got interesting.
A student who identified himself as a psychotherapist asked Metzner to talk about psychedelics, a subject he hadn’t yet mentioned. With that gentle nudge, Metzner proceeded to veer wildly off message, exposing the tensions that Janis Phelps alluded to Friday night but that had been absent from the weekend’s presentations thus far. “These are drugs that psychotherapists unanimously feel could improve psychotherapy,” Metzner began, “but their use is illegal. What does that tell you? Something about the society we live in!”
Metzner paused — and then jumped. “There is a vast underground network of psychedelic therapy, you know — vast. Larger than the approved uses of psychedelic therapy.” He went on: “It’s an underground culture, and underground cultures are good, in fact they can be lifesaving.” Phelps, her porcelain complexion reddening, stood up, taking a step toward the lectern to solicit another question, but Metzner wouldn’t be deterred. Declaring that we were in the midst of a spiritual emergency in this country, he told the students we have these “fantastically promising medicines that can cure all sorts of ills, and yet doctors can’t get them.”
Metzner’s voice rose. “We don’t have to accept that!” The eminent professor seemed to be inviting his flock to engage in a collective act of civil disobedience. This he likened to the underground in Germany, where he grew up, during the war: “There were German families who took in Jewish families and hid them in their closets.” He voiced impatience with the pace of scientific research and federal approval, “at a time of civilizational collapse,” when we have these medicines that we know work and could help our society right now. “It doesn’t need to be proven over and over again. When there’s a plague, you don’t go through double-blind placebo-controlled studies! It’s a plague!”
Finally it fell to Bill Richards to stand up and gently remind the students that while the pace of progress might be frustrating, “we have a path forward” — the path of sanctioned clinical trials leading to approval of psychedelic therapy. He pointed out that the researchers on this path had so far found federal regulators to be remarkably open and receptive. “So let’s go forward as scientist-warriors and do what we can in the aboveground world. I think we can make a significant impact.”
The students I spoke to afterward clearly shared Metzner’s sense of urgency and frustration, but they rejected his apparent invitation to join the underground. In their view, Metzner was looking backward, to a dark age when the underground served as the saving ark of psychedelic therapy. But that dark age was drawing to a close, they believed. A generation or two younger than Metzner, these people were looking resolutely forward — to a time, not too distant they thought, when the F.D.A. would approve the therapeutic use of psilocybin and MDMA and make them available to doctors to prescribe to their patients. This was the future they had signed up for when they enrolled in the course.
One student in the class, a psychiatrist who had participated in psychedelic therapy in South America for decades, told me after the session that she was now fully committed to the legal road. “I’ve had a secret life for 30 years,” she said. “I damn well want this opportunity to unify my life. Because of this class, I have a way to talk openly to people about psychedelics for the first time.” She voiced deep respect for Metzner but believed the time had come to make a choice. “I don’t want to lose the history or the knowledge we’ve gained from the underground work. But the professionals in this room have decided to put our time and credentials into furthering the legal use of these medicines.” Doing so, she said, “demands being beyond reproach so as not to endanger the work and the path that has been set out.”
Manish Agrawal, the Maryland oncologist, expressed the general sentiment in an email he sent me after Sunday’s session. He shared Metzner’s “frustration that this therapy isn’t available for my patients today, and many will suffer and die without access to this therapy. Ralph really pushed me to feel the injustice of that.” He went on: “But everyone senses how close we are,” and doesn’t want to jeopardize that by following Metzner off the legal route. Agrawal left San Francisco determined to find a way to incorporate psychedelic therapy in his oncology practice.
The day after my journey, I was grateful for the opportunity to return to Mary’s room for a couple of hours of “integration.” Without it, people might be tempted to dismiss their psilocybin journeys as simply a “drug experience,” put it in that handy box and throw it away; this has no doubt been the fate of a great many psychedelic trips. Yet though it is true that a chemical started me on this journey, it is also true that everything that I experienced I experienced: These are events that took place in my mind, psychological facts that were neither weightless nor evanescent. But I needed help making sense of them and putting them to use.
That I could survive the dissolution of my ego and its defenses was surely something to be grateful for, and we talked at length about this. What a remarkable gift: to learn that we can let go of so much — the desires, fears and defenses of a lifetime! — without suffering complete annihilation. This might not come as a surprise to Buddhists or serious meditators, but it was news to me, who had never felt anything but identical to my ego. Could it be that there is another ground on which to plant our feet? For the first time, I began to understand what the volunteers in the cancer-anxiety trials were telling me — how it was that a single psychedelic journey granted them a perspective from which the very worst life can throw at us could be regarded objectively and accepted with equanimity. I had been given a glimpse of that liberating perspective.
“That alone seems worth the price of admission,” Mary offered, and I had to agree. I also realized that I never would have achieved that perspective had Mary not guided me, creating a space where I felt safe enough to let go of my accustomed self and its usual defenses.
Yet 24 hours later, my old ego was back in uniform and on patrol, so what long-term good was that beguiling glimpse of a loftier perspective? Mary suggested that, having had a taste of a different, less defended way to be, I might learn to relax the ego’s trigger-happy command of my reactions to people and events. “Now you have had an experience of another way to react — or not react. That can be cultivated.” She suggested meditation as one way to do that.
Many researchers believe that the experience of “ego dissolution” that I had in Mary’s room can disrupt destructive patterns of thought and behavior and open us to new perspective from which to view death or addiction or depression. This was understood back in the 1950s and ’60s, when psychiatrists working with psychedelics sometimes described it as “therapy by self-transcendence.”
If the ego can be said to have an address, it would probably be in something called the default mode network, a high-level hub in the brain linking the frontal cortex to older centers of memory and emotion. The D.M.N. appears to be involved in a range of operations related to our sense of self, like rumination, time travel (contemplating the past and future), theory of mind (the ability to impute mental states to others) and the so-called autobiographical self: It helps us integrate whatever’s happening to us now with the story of who we are, thereby giving us an abiding sense of a self that is consistent over time. Neuroscientists recently began imaging the brains of people on psilocybin or LSD, and they were surprised to find that, rather than increasing brain activity, as you might expect, the drugs radically quieted traffic in the D.M.N. In particular, when volunteers report the experience of ego dissolution, their brain imaging shows a precipitous drop in D.M.N. activity.
Taking this network temporarily offline may allow the whole system to “reboot,” in the words of Robin Carhart-Harris, a pioneering neuroscientist who has done extensive work imaging tripping brains at Imperial College London. The “loosening of cognition” that results, he says, is especially helpful to people suffering from the varieties of mental stuckness, including depression, addiction, anxiety and obsession.
All these conditions, as Alison Gopnik, a professor of psychology at Berkeley, points out, may share an etiology. “There are a range of difficulties and pathologies in adults, like depression, that are connected with the phenomenology of rumination, and an excessively narrow, ego-based focus,” says Gopnik, whose research explores the consciousness of children, which she believes bears a similarity to psychedelic consciousness. “You get stuck on the same thing, you can’t escape, you become obsessive, perhaps addictive. It seems plausible to me that psychedelic experience could help get us out of those states, create an opportunity in which the old stories of who we are might be rewritten.”
Just how soon might psychedelic-assisted psychotherapy be available aboveground, to the many people who stand to benefit from it? Before the F.D.A. approves a new medicine, the drug must survive testing for safety and efficacy in a three-stage sequence of trials, each of them involving a larger sample and more rigorous methods. When researchers recently brought to the F.D.A. the results of Phase 2 clinical trials of cancer patients who were given psilocybin and MDMA, they were stunned by the positive response of the regulators. Regulators told them they could move forward to Phase 3 with MDMA, the last step before F.D.A. approval. The F.D.A. is still considering when psilocybin trials can move into Phase 3. The agency wouldn’t comment on drugs in the approval process, but a researcher who attended one of these meetings told me the regulators seemed untroubled by the illicit status of the drugs in question or by the unique challenges of controlling studies of psychedelics. These meetings took place before a Trump-appointed F.D.A. commissioner was sworn in; it remains to be seen how the Justice Department under Jeff Sessions would respond to F.D.A. approval of psychedelics. The researchers felt heartened by the F.D.A.’s response. The message the scientists took away from the meeting was that they should raise their sights and not limit themselves to treating cancer patients, but rather test the drugs on the much larger population of patients suffering from major depression.
Thus encouraged, the Multidisciplinary Association for Psychedelic Studies (MAPS), a nonprofit that has been working for federal approval of psychedelics since 1986, will begin Phase 3 trials of MDMA-assisted psychotherapy this summer for the treatment of post-traumatic stress disorder, involving more than 200 volunteers at 16 sites in the United States, Canada and Israel. Later this year, pending F.D.A. approval, two Phase 3 trials of psilocybin — one for the treatment of major depression and the other for “psychospiritual distress” in cancer patients — are expected to get underway at Hopkins, N.Y.U. and a half-dozen other sites around the country.
Phase 3 trials, which typically involve hundreds of subjects at dozens of sites, can cost tens of millions of dollars — a cost ordinarily borne by the big pharmaceutical companies that stand to profit from approval. But Big Pharma has not demonstrated significant interest in psychedelics, and it’s not hard to see why: Psychedelic therapy is a rather square peg to fit into the round hole of psychopharmacology as we now know it. Patents on the molecules in question — LSD, psilocybin and MDMA — have long since expired (psilocybin comes from a common mushroom); the drugs, if approved, don’t need to be taken more than a few times; and as the C.I.I.S. program recognizes, psychedelic-assisted psychotherapy is a novel hybrid of pharmacology and talk therapy, making it uncharted territory for a pharmaceutical industry organized around the selling of pills.
But the obstacle of funding Phase 3 trials appears to have been recently surmounted. The Psychedelic Science Funders Collaborative (P.S.F.C.), a new Bay Area-based consortium of philanthropists including the hippie-soap entrepreneur David Bronner, the author and tech investor Timothy Ferriss and other donors both in and out of the tech community, has helped raise more than $63 million in charitable contributions, an amount that could be sufficient to complete the trials. The two main beneficiaries of these funds will be MAPS and Usona Institute, a nonprofit medical-research organization that is sponsoring forthcoming psilocybin trials. Rebekah Mercer, the Trump funder behind Cambridge Analytica and Breitbart, is also a donor to MAPS.
There is at least one corporation betting that psychedelic therapy will soon become a business. Founded in London by George Goldsmith, a health care industry consultant, and Ekaterina Malievskaia, a physician, Compass Pathways aims to become the world’s first psychedelic pharmaceutical company. (The couple, who are married, were inspired to expand access to psilocybin after Malievskaia’s college-age son was successfully treated by an underground guide with the drug for a debilitating case of depression.) Compass aims to be much more than a drug company, however. The company is developing a complete treatment package — consisting of a training program for therapists; protocols for orchestrating the entire experience; and the medicine itself — that it hopes to sell to health care institutions and national health services, first in Europe and then in the United States.
Its initial therapeutic target is treatment-resistant depression (patients who have failed to respond to at least two previous treatments); after an advisory process with the European Medicines Agency (the E.U.’s drug-regulating body), it has decided to conduct trials in eight to 10 sites across Europe. It is also in discussions with the F.D.A. to organize trials here. According to Goldsmith, Compass has already raised $13 million from investors in the United States and Europe, many of them from the tech community (Peter Thiel is an investor) but also institutional investors in the health care sector.
Phase 3 trials will take at least three years, but access to psychedelic therapy could come sooner than that. Under “expanded access” or “compassionate use” programs, patients who stand to benefit from therapies still deemed experimental can gain access to them before trials are complete. In the case of MDMA, this could happen as soon as 2020.
That tantalizing possibility is very much on the minds of the C.I.I.S. students. On the flight home, Manish Agrawal and his oncology partner Paul Thambi began planning how to talk to their colleagues about the idea of adding psychedelic therapy to their practice, and where in their offices they might create a treatment room. Did they plan to hire guides to conduct the sessions? Perhaps, they said, but the weekend had left them both convinced this was work they very much wanted to do themselves.
“We don’t die well in this country,” Agrawal told me during a lunch break at the weekend course. “And we have pretty limited tools to help people deal with their fear. Prozac doesn’t work. The issue isn’t depression; it’s facing your mortality.” The oncologists’ commitment to training as psychedelic guides is notable; they would most likely be able to prescribe psilocybin once it’s approved without years of experience, a prospect that concerns some of the underground guides I interviewed. “Just because you have the ability to prescribe,” one guide told me, “doesn’t mean you have the wisdom to guide the experience.”
In the wake of the weekend’s high hopes, I couldn’t help wondering what the brave new world of legal psychedelic therapy might mean for guides like Mary and Michelle. I had heard some grumbling in the community about the limitations of the C.I.I.S. training, and the bitter twist that the psychedelic guides with the deepest experience could be excluded in favor of newly credentialed guides with no real-world experience whatsoever.
But Michelle said she is busier than ever. Mary, too, anticipates that federal approval of psychedelic medicine would bring more people to her door, especially those without an obvious pathology — the curious, the spiritual seeking and the legions of run-of-the-mill neurotics who already fill therapists’ offices. How many of them will want to try a guided psychedelic journey once they hear about it?
“I don’t think it’s going to hurt me at all,” Mary told me. “If anything, it will allow me to do even more than I do.” Was she worried about a crackdown if psychedelic therapy suddenly becomes fashionable? The work was too important to let that stop her. “I need to find a way to continue to protect myself, as I help people find their soul’s purpose in this lifetime, to help them awaken.”
This article is adapted from “How to Change Your Mind: What the New Science of Psychedelics Teaches Us About Consciousness, Dying, Addiction, Depression, and Transcendence,” published by Penguin Press. Read the book review here .
Sign up for our newsletter to get the best of The New York Times Magazine delivered to your inbox every week
Michael Pollan is a longtime contributing writer for the magazine. His most recent article was about the Obama administration’s record on food and farming issues . Pollan is the author of eight books, including “The Omnivore’s Dilemma,” “In Defense of Food” and “The Botany of Desire”; parts of all three appeared in the magazine.
More in this issue
The prisoners who care for the dying and get another chance at life, how tech can turn doctors into clerical workers, trying to put a value on the doctor-patient relationship, more on nytimes.com.
Advertisement
Wondering How to Kill a Trip? Some People Use Trip Killer Drugs
A neurologist walks you through the ins and outs of trip killers—pharmaceuticals and over-the-counter drugs people use to halt a trip..
Article by console.log(""); console.log("author name"); console.log(""); Dr. Aly Aziz .author-bio * {display: unset !important;} Published on February 09, 2024 Updated February 14, 2024
Trip day. You’ve prepped all week, tied up loose ends the morning of, and have the following day off to reflect on today’s anticipated breakthrough psychedelic experience. Dose measured: Check. Music playlist ready: Check. Stove is off: Check. The last thing you’d want during your deep subconscious dive is anything that would kill a trip. Here we go.
Everything’s going well so far… until it isn’t. It starts with a tinge of unease. Exactly why or what of you don’t know. Then the paranoia starts—and escalates: “Did I take too much? Did I check on the stove? What’s that pain in my chest? A heart attack! Wait, what did I just see ? Is the STOVE OFF?” One irrational thought loops into another until your mind spirals into a maddening dark abyss. That trip killer you didn’t want? Man, could you use one to pull you back from the unfolding hellish psychedelic nightmare.
Experienced psychonauts, guides, and sitters are well-versed in techniques to help steer themselves and others during a “bad trip.” Most welcome the unwanted subconscious contents to rise into awareness because it is in those repressed memories and feelings where true healing takes place in the long run. However, there can be a point where the sheer terror and panic triggered for some becomes counter-productive at best and downright dangerous at worst. Such situations beckon for a drug intervention—a trip killer. But is using another drug to quell your trip safe?
READ: 5 Biggest Reasons People Have a “Bad Trip”
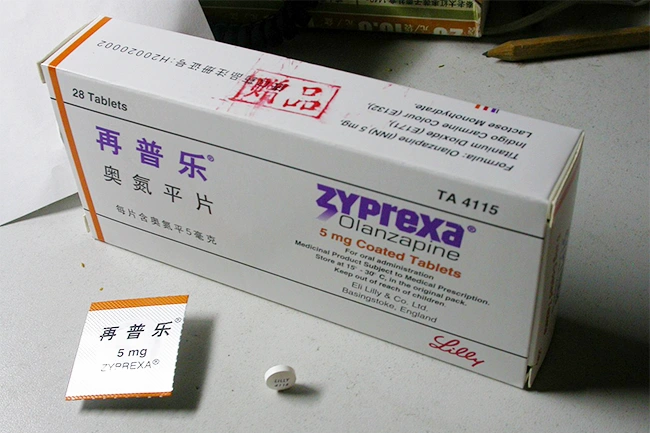
So, What is a “Trip Killer?”
A “trip killer” is usually an anti-anxiety or anti-psychotic pharmaceutical drug that people take in an attempt to halt a psychedelic experience in its tracks. People use trip killers for mushrooms, acid , and other classical psychedelics. And some drugs are more ubiquitous than others: A review of popular online forums suggests that anti-psychotics, such as olanzapine and quetiapine, are popular drugs used as trip killers. Both drugs are second-generation anti-psychotics—second-generation antipsychotics have fewer side effects compared to their first-generation predecessors. Benzodiazepines or “benozos” (eg. Xanax, Valium, Ativan, Klonopin), are also touted as trip killers. All benzos have a similar mechanism of action, but they differ in how fast, how intensely, and for how long they act on the brain. If you visit an emergency room for a bad trip, you are given these same prescription drugs (in addition to a calm, supportive environment).
The Basics Second-generation anti-psychotics and benzodiazapines (anti-anxiety drugs) are the two most commonly used trip killer medications. They’re used in the emergency room, and more commonly, in the psychedelic underground.
Are there over-the-counter trip killers?
At home, many people turn to more accessible over-the-counter drugs to try to quell a trip—like Benadryl or other medications that seem calming. Some may try alcohol or cannabis products to quell the intensity. But, while these products may be more accessible, it doesn’t mean that they’re inherently safe to mix with psychedelics. There is not a lot of real-world hard data; no scientists in white coats at the bench looking at the blood of hundreds of people mixing psychedelics and “trip-killers” and measuring the effects. All we have to go on is the online posts of users and their experiences mixing.
Even an easily accessible over-the-counter product, any drug used in excess, is an absolute no-no. Remember the Benadryl challenge? The TikTok challenge where people recorded themselves taking a pack of twelve tabs at once (way above the recommended dose) to induce hallucinations. It resulted in the death of a teen and hospitalizations for many until the manufacturer had to step in.
How to Grow Shrooms Bundle
Take both of our courses and save $90.
When it comes to mixing alcohol, cannabis, and other over-the-counter drugs (yes, even Tylenol) with psychedelics, just remember that mixing any drug with a psychedelic may:
- a) alter how your body metabolizes the psychedelic itself,
- b) how the psychedelic interacts with the attempted trip-killer,
- c) compound the side effects if you have taken a combination of trip-killers.
All in all, the general advice for any trip-taker using trip-killers is to start low (as in low dose), go slow (take another dose spaced apart), and have a trip-sitter along with your trip-killer. Oh, and if you ever end up in the emergency room, please tell the doctor everything you took (psychedelics, trip-killers, and any other medications you are on), so they don’t give you something that worsens your specific situation.
READ: Set and Setting: Here’s How to Prepare Your Mind & Space Before Using Psychedelics
To end or mitigate a psychedelic drug experience, some people use another substance as a "trip-killer." A recent study found hundreds of Reddit posts on trip-killers like benzodiazepines, & relatively few posts mentioned the potential harms. #MedicalNews https://t.co/RjduDAo7eI pic.twitter.com/Rfhcd5NWaP — JAMA (@JAMA_current) January 31, 2024
How Do “Trip Killer” Drugs Work?
There are scientific reasons why drugs like olanzapine and benzodiazepines can stop a bad trip. To make sense of it, it’s important to understand how our brains work and how psychedelics change how we see things. We’ll start with a simple question: Why do we have a brain?
The answer is relatively straightforward. The chief function of our brain is to perceive the environment (our setting), so that we can engage with it. The billions of nerve cells (neurons) and their trillions of connections in our brain are constantly being bombarded by information from our external and internal senses. The old understanding of the brain’s modus operandi —its particular way of doing something—suggested that our brain is a receiver to all of the informational bombardment. Let’s use sight as an example. Think of a camera taking a picture of the world. Our eyes receive the reflected light from whatever is in our field of vision; that light is transmitted into electrical signals within our brain, and our mind “sees” the world in front of us. Our “internal camera” is constantly taking a picture every milli-second and updating the movie of the world. This old paradigm of our brain as a passive receiver is not what the new neuroscience teaches us.
A New Way of Thinking
The new paradigm: our brains are active prediction machines. What does this mean? Let’s try an exercise. Read to the end of this paragraph, then try this: Close your eyes and imagine you are gazing at a grand colorful forest on an early Autumn morning. Shades of golden brown leaves are all around you. Dead tree stumps covered in mushroom fruiting bodies crowd your feet. Go ahead.
Welcome back. If each reader drew their imaginings above, I wager they’d look similar. But where did the information your mind’s eye conceived of a few moments ago come from? There was no external informational bombardment. You predicted a model of a forest in your mind, from your past experience of what such a forest would look like. Believe it or not, you are making this exact kind of prediction in real time with countless bits of information coming into your brain from all your senses. Your brain is continuously predicting a model of the world as you look around your environment. As new information enters your brain through the senses, that model is updated to minimize prediction errors.
Let’s use another example to show what we mean by minimizing prediction errors. Say you are now actually in a forest and lean against a tree for a breather. Something catches your attention: There’s a faint dark greenish object against the backdrop of the forest floor—but you can’t make out exactly what it is. Your brain subconsciously—and involuntarily—predicts what this greenish object could be. Is it an apple, leaf, frog, or a green plastic toy soldier (the ones you’d get by the bagful for a dollar in the 80s)? It can’t be all of those things. What do you do next? You move in for a closer look; you take action to minimize prediction error. And as you approach the mystery green object, it moves a few inches away from you. In that moment, your brain subconsciously processes the probabilities. Apples don’t jump, and neither do toy soldiers (you know this from past experience). The wind may have blown a leaf? The object moves again, and this time, you’re confident there is no accompanying breeze. You look closer and see a pair of eyes on the green object. The subconscious prediction machinery sends a message to your awareness of the most likely possibility: You are “seeing” a green frog.
The above example is a microcosm of what your brain is doing with continuous input from all of your senses. It is predicting a model of the world, and you act in a manner to reduce prediction errors. The exact mechanisms involved and the neurochemistry of it all require a detailed review of Predictive Processing and Neuronal Networks—let’s leave that for the textbooks.
Psychedelics and the Brain
Now, how do psychedelics—specifically the classical psychedelic such as LSD, “magic” mushrooms, mescaline, ayahuasca —fit into this new, prediction paradigm? For starters, psychedelics widen the sensory gates for more information to arrive to your brain. Second—and importantly—they loosen or relax the networks involved in the brain’s predictive machinery. As a result, our perceptions (the generative models of the external and internal world discussed above) are altered.
Under the influence of classical psychedelics, green apples are seen as frogs; the paintings in your home feel alive. Third—and why they are used in a clinical setting—is that they also loosen your sense of self. In clinical depression, for example, the leading theory is that psychedelics loosen those hard-wired patterns of belief about your negative sense of self, so that you are more open to therapeutic change. It’s important to note here that the majority of the healing potential of psychedelics is not solely due to the trippiness for those few hours under the influence, but how well the user has prepared before the trip and how well they integrate the experience days, weeks or months after the trip.
Unfortunately for some who are susceptible, the loosening of external reality and of the self leads to panic and paranoia, which, if not tempered, may lead to self-harm and harm to others around the trip taker. In such situations, some self-manage by using drugs to kill the trip before they go off the edge, or for a few days after to dampen the anxiety and insomnia.
Your Brain on Trip Killers
So, what exactly is going on in the neurons of your brain during a trip? And how do trip killers such as olanzapine and benzos work? For starters, your brain uses chemicals called neurotransmitters to communicate electrical activity between neurons. Neurotransmitters are released from one nerve cell (pre-synaptic nerve cell) and traverse the space between nerve cells called a synapse to dock on the receptors of the receiving nerve cell (post-synaptic nerve cell). Think of a neurotransmitter acting like a key with the receptor as its lock. See the figure below.

Psychedelics such as LSD and magic mushrooms mimic the action of the key on specific receptors on nerve cells. Others, like MDMA, flood the synapse with the brain’s native neurotransmitter to exert its effects. The end result is a change in the brain’s networks to a non-ordinary state of perception and consciousness—the trip.
Olanzapine—Trip Killer used in Emergency Rooms and Popular Culture Alike
Olanzapine acts like a bouncer at the door; it directly stops the action of classical psychedelics from binding at the receptor. Less receptor binding means less altered brain networks, which means less trippiness. Less trippiness means less possibility of paranoia, anxiety, and hallucinations. Most users take between five and 10 mg of Olanzapine to kill a trip, which is a typical dose prescribed by doctors (up to 20 mg per day). However, there are reports of some taking 50 mg! Like any other drug, the more you take, the more likely of unwanted side effects. Olanzapine is no different. The higher you go, the more chances of delirium (what you are trying to avoid in the first place), irregular heartbeat, uncontrollable movements, and exceptionally high fever. In extreme ingestions, you could wind up damaging your heart, liver, and kidneys—or worse, end up in a coma.
Another note of caution with Olanzapine or other anti-psychotic drugs: Emergency room doctors may administer such drugs to quell a psychedelic trip, but the anti-psychotic may be less safe to mix with other substances. A recent FDA drug safety surveillance database cited the combined use of Olanzapine with MDMA with an associated increased risk of death. However, the data on mixing the two is scant, so proceed with caution. Yet, even with classical psychedelics, it’s best to take olanzapine with the help of a provider’s care. Taking prescription medications that are not your own can be risky.
Safety Note Limited research suggests that mixing olanzapine with MDMA might have hazardous effects. Similarly, there’s little information available about mixing “trip killers” with novel psychedelics, like 2C-B. Yet, even with classical psychedelics like mushrooms and LSD, it’s best to take olanzapine with the help of a provider’s care. Taking prescription medications that are not your own can be risky.
Does Xanax Kill A Trip? All About Benzodiazepines
What about benzodiazepines (benzos)? While olanzapine is the most popular drug of choice, according to online reviews, its effects are not felt immediately when taken by mouth. On the other hand, benzos can reduce anxiety within minutes; in fact, they are used as stand-by emergency medications in the myriad of clinical studies on psychedelics in world-class institutions being done around the world.
Benozs work differently on neurons compared to anti-psychotics. They are not bouncers at the door. Rather, they act more like a trigger to a sprinkler system on the dance floor. By binding to a receptor called GABA-A on nerve cells, benzos increase the ability of the brain’s major inhibitory neurotransmitter, GABA (Gamma-AminoButyric Acid), to bind at the GABA-A receptor. As an inhibitory neurotransmitter, GABA has a calming effect on the nervous system. When more GABA binds, more “water” in the sprinkler system is released to kill or calm down the excited party in the neurons. The end result is less neuron firing, which, like olanzapine, leads to less altered brain networks and less anxiety. Like olanzapine, too much of a benzo, and you’re asking for trouble.

Potential Risks of Benzodiazepines as Trip Killers
I cannot stress enough how careful you have to be when considering the use of benzodiazepines as trip killers, especially if you intend to use benzos continuously for days after. First and foremost, take too much at one time, and you may not be able to breathe. Benzodiazepines can cause respiratory depression; they affect the part of your brain that controls automatic breathing. If you can’t breathe, you kill the ultimate trip: life.
Second, long-term use of benzos leads to tolerance and dependence. If you have had issues with previous substance abuse or dependence, please re-consider. Abruptly stopping long-term use of benzos can be deadly, and the withdrawal side effects (eg. insomnia, headaches, anxiety, panic attacks, palpitations) would make you wish you’d never gone down the road of using them in the first place. There are several types of benzodiazepines, with Alpralazam (Xanax) the most popular as it exerts its effect potently within a few minutes. Others, such as diazepam (Valium), take a bit longer to kick in but are also effective in quelling anxiety and paranoia.
While antipsychotics and benzodiazepines have to be taken with care, mixing them with other substances—not including psychedelics—is definitely not recommended. Alcohol, cocaine, cannabis, and opiates can magnify side effects when mixed with Olanzapine and/or benzos (and whatever psychedelic you took). Cocaine and opiates can also increase your risk of deadly overdose due to stress on the heart and respiratory depression. If you or someone you are sitting for takes a trip-killer, loses consciousness, and is not rousable, has difficulty breathing, having chest discomfort, it may be the time to alert paramedics.
Comment by u/Outside-Act-3243 from discussion in LSD
Freaking out? Tips for a Safe(r) Psychedelic Journey
Trip killers aside, the pillars of a safe psychedelic experience remain the same: set and setting . This is true whether your journey is a gentle nudge or a deep plunge. A healthy mindset and safe setting (including a trusted sitter or guide) may prevent the need for a pharmacological trip-killer. The following few suggestions are the basis for anyone looking for a positive experience.
Set (mindset):
- If you are already in an anxious or negative state of mind (we’ve all had those days), consider postponing your trip for another day.
- Relax a few days before leading up to and including trip day. Whether it be meditation, journaling, nature walks, art, music—whatever gets you in a relaxed state of mind.
- If you are using it for a therapeutic purpose, discuss the intention of your trip with your guide, along with planned strategies to navigate difficult aspects of the trip.
- Eat healthy, exercise, and sleep well before trip day. The state of your physical body affects the state of your mind.
- Avoid any other psychotropic drugs before and during your trip, including caffeine.
- Keep the day after your trip relatively free from any obligations. Self-reflection is a foundational piece of your integration. You may also want that day to recover physically.
Setting:
- Ensure that the physical space is ideal for a psychedelic trip. If indoors, a private area with a comfortable soft spot to lie down with blankets and access to a bathroom is a minimum. If outdoors, natural calm scenery (forest, beach, park) is best. Do not traverse heights, as your sense of balance and visual perception may not be 100%.
- Music can turn your positive trip into a transformative experience. Avoid tracks that are heavy on lyrics, and time your playlist such that there are calm tracks during the come-up, alternating intense and calm tracks at the peak, then calm tracks once more when you come down.
- If you’re with a group, make sure a trusted friend or family member is nearby to help you navigate a difficult part of the trip. Ensure you have a safe method to go home (DO NOT DRIVE if you are under the influence of a psychedelic).
- Have access to water during your trip and light snacks after your trip.
- Turn off your electronic devices and try to minimize the possibility of any interruptions (take care of any obligations for the day).
Valeriani G., Corazza O., Bersani F.S., Melcore C., Metastasi A., Bersani G., Schifano F. Olanzapine as the ideal “trip terminator”? Analysis of online reports relating to antipsychotics’ use and misuse following occurrence of novel psychoactive substance-related psychotic symptoms. Human Psychopharmacology . 2015. Jul;30(4):249-54.
Griffin III C.E.G., Kaye A.M., Bueno F.R., Kaye A.D. Benzodiazepine Pharmacology and Central Nervous System—Mediated Effects. The Ochsner Journal . 2013. 13(2): 214-23.
Cohen I.V., Makunts T., Abagyan R., Thomas K. Concomitant drugs associated with increased mortality for MDMA users reported in a drug safety surveillance database. Nature: Scientific Reports. 2021(11):5997.
Yates G, Melon E. Trip-Killers: a concerning practice associated with Psychedelic use. Emergency Medicine Journal . 2024;41:112-113
Enjoyed this article on how to kill a trip?
“Tripping can be fun, magical, and even transcendental, but it can also be profoundly sad and challenging, filled with tears and confusion,” writes author Michelle Janikian. She walks you through how to survive a bad trip while it’s happening.
In the psychedelic community, we often hear “bad trips don’t exist,” but that’s simply not true. Dr. Erica Zelfand walks you through how to heal after a traumatic journey.
Wow, that was crazy. Now what? Maybe you tripped balls at a music festival, had the time of your life, and never thought about it again. Maybe you took some shrooms with your best friend last weekend while camping, and you don’t know what to make of all the uncomfortable feelings that are still bubbling up. Here’s how to make sense of your last trip.
The information above does not substitute for professional medical advice. If you are considering the use of any substances mentioned, it is best to consult your medical professional to avoid unnecessary harm. Individuals react to psychotropic drugs differently depending on many factors, including the presence of pre-existing disease (eg. kidney disease, liver disease), and prescribed drugs you may be taking. Consult your doctor if you are considering using any of the above, especially if you are using it for the first time.
In the event of an emergency, please dial local emergency services. For mental health services related to substance abuse in the U.S., please dial the Substance Abuse and Mental Health Services Administration National Helpline at +1 (800) 662-4357.

DoubleBlind is a trusted resource for news, evidence-based education, and reporting on psychedelics. We work with leading medical professionals, scientific researchers, journalists, mycologists, indigenous stewards, and cultural pioneers. Read about our editorial policy and fact-checking process here.
DoubleBlind Magazine does not encourage or condone any illegal activities, including but not limited to the use of illegal substances. We do not provide mental health, clinical, or medical services. We are not a substitute for medical, psychological, or psychiatric diagnosis, treatment, or advice. If you are in a crisis or if you or any other person may be in danger or experiencing a mental health emergency, immediately call 911 or your local emergency resources. If you are considering suicide, please call 988 to connect with the National Suicide Prevention Lifeline.

How to Take Shrooms
How much shrooms should a beginner take, preparing for your first mushroom trip we've got you..

Lykos Therapeutics Highlights the Not-For-Profit to For-Profit Pipeline in Psychedelics
The multidisciplinary association for psychedelic studies, or maps, recently rebranded their public benefit corporation to lykos therapeutics, which is slated to bring us pharmaceutical mdma in 2024..

Art + Culture
Snow raven sings like the animals do , doubleblind met up with siberian singer snow raven to discuss how she embodies birds, reindeer, and other wild beasts from the arctic—all in the name of bringing the shamanic sounds of the sakha people to the world..
June 22, 2024
Should Next-Generation Psychedelics Skip the Trip?
Companies attract venture funding for redesigned psychedelic drugs
By Mark Peplow

Psilocybin mushrooms.
Juris Kraulis/Alamy Stock Photo
When Boston-based biotech Seaport Therapeutics launched in April with $100 million in venture funding, it joined a growing cadre of biotech companies that are fine-tuning psychedelic drugs to treat a range of mental health problems. These ‘next-generation psychedelics’ aim to overcome some of the limitations of using classical psychedelics as therapeutic drugs for conditions such as depression and substance use disorder.
In May, Gilgamesh Pharmaceuticals, another company working on next-generation psychedelics, announced that it would collaborate with pharma giant AbbVie to develop new therapies for psychiatric disorders. Gilgamesh will receive an up-front payment of $65 million from AbbVie, with the potential for up to $1.95 billion in fees and milestone payments, a clear sign of the growing interest in this area.
Classical psychedelics — including psilocybin, found in ‘magic mushrooms’; dimethyltryptamine (DMT), the active ingredient in the South American psychoactive brew ayahuasca; and the 1960s counterculture stalwart lysergic acid diethylamide (LSD) — are already being tested as mental health treatments. “This was very much fringe science even five years ago,” says Sam Banister, co-founder and chief scientific officer of Psylo, a biotech with labs in Sydney, New South Wales, Australia, and Boulder, Colorado, working on next-generation psychedelics. “Now you have billions of dollars of funding pouring into these initiatives and literally hundreds of companies developing psychedelics.”
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing . By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
The resurgent interest in psychedelics is partly driven by huge unmet need. The World Health Organization estimates that about 280 million people worldwide have depression, yet the most common antidepressants — selective serotonin reuptake inhibitors (SSRIs) such as Prozac (fluoxetine) — often show limited efficacy. Investor interest has also been buoyed by the recent success of Spravato (esketamine), a single enantiomer of the anesthetic ketamine, which induces trance-like states. The drug won US Food and Drug Administration (FDA) approval for treating depression in 2019, and last year racked up $689 million in sales for Johnson & Johnson.
But the psychoactive effects of such compounds pose some major challenges. It can be difficult to find a reliable placebo for a blinded clinical trial, for example — there’s no way a patient can mistake a sugar pill for a dose of LSD. And patients typically need close supervision for many hours while under the influence of the drugs, making it burdensome, expensive and impractical for many patients.
To avoid these problems, some companies are tweaking psychedelic drugs to induce shorter or milder ‘trips’ that will not require such intensive patient oversight from clinicians. Others, including Seaport, are redesigning the molecules to erase their psychedelic effects altogether while retaining their treatment efficacy. “Some patients are terrified when they go through these trips, and it’s not something they ever want to do again,” says Aaron Koenig, chief medical officer at Boston-based biotech Delix Therapeutics.
Although some researchers argue that a psychedelic experience is essential for a long-term improvement in mental health, nobody knows for sure whether it will be possible to retain therapeutic benefit while avoiding the trip. “That’s the billion-dollar question of the field,” says Andrew Kruegel, CSO and co-founder of Gilgamesh.
Banister notes that biotechs working on next-generation psychedelics all seem to be pursuing distinct strategies to fine-tune their molecules. “Every company in this space, as far as I can tell, is taking quite a different approach,” he says. In part, that may reflect the lack of scientific consensus about the role of the psychedelic trip in the classical drugs’ therapeutic effects. But it also demonstrates the breadth of opportunity in an area that has seen relatively little pharmaceutical progress since the SSRIs of the 1980s and 1990s.
Psychedelics are a broad and somewhat ill-defined class of compounds. The psychoactive effects of these drugs, including hallucinations and feelings of dissociation from the body, vary dramatically depending on the compound and the dose. “It ranges from feeling a buzz similar to having a cup of coffee to a full-blown LSD experience where you’re shaking hands with God,” says Jesper Kristensen, a medicinal chemist at the University of Copenhagen, whose spinout company Lophora is developing next-generation psychedelics.
Many psychedelics share similar molecular structures. Most activate a serotonin receptor called 5-HT 2A , which seems to be crucial to their effects. Ketamine, in contrast, is an antagonist of the N -methyl-D-aspartate (NMDA) receptor, a common target for anesthetics.
For all psychedelic agents, the sector is booming. “We have identified nearly 150 drug development programs based on different types of psychedelic drugs,” says Jasparam Kaur, a senior business analyst at Roots Analysis, a market research company headquartered in Chandigarh, India. A recent report by Roots calculates that companies in this area have collectively raised over $3.5 billion since 2017 and estimates the market for therapeutic psychedelics could grow to $6.7 billion by 2030.
One of the leading companies working on classical psychedelics is Lykos Therapeutics in San Jose, California. It has completed two phase 3 trials using 3,4-methylenedioxymethamphetamine (MDMA) in drug-assisted psychotherapy to treat post-traumatic stress disorder (PTSD) and has an Investigational New Drug application pending with the FDA. (MDMA is not considered a classical psychedelic, but it is often treated as such.)
Close behind Lykos is Compass Pathways in London, which is testing psilocybin in two phase 3 trials for treatment-resistant depression; and Mind Medicine, a New York-based biotech that unveiled positive phase 2b results in March for its LSD D-tartrate compound MM120 in treating generalized anxiety disorder. Compass and Mind Medicine have both received FDA ‘breakthrough therapy’ designations for these drugs.
“I am excited about the therapeutic possibilities of these substances, but I think there’s a lot of hype,” cautions Robert Malenka at Stanford University. Much of the science underpinning these approaches remains unknown, and, he adds: “The actual evidence of therapeutic efficacy is relatively limited.”
There are also questions about their cost effectiveness, given that patients require close supervision by psychotherapists during the drug experience. “In Australia, the cost per patient of MDMA or psilocybin therapy is likely to be around AUS$20,000 to AUS$30,000 for a treatment course lasting several months [US$13,000 to US$20,000],” says Banister.
Psilocybin faces similar challenges because a therapeutic trip can last for eight hours. This is partly because the drug must first be metabolized in the body to form psilocin, the compound that targets the 5-HT 2A receptor.
Cybin, a biopharmaceutical company headquartered in Toronto, has shortened that trip with its psilocybin analog CYB003, which does not require metabolic activation in the liver and intestines. To fine-tune the drug, the company also replaced some of the molecule’s hydrogen atoms with its heavier isotope deuterium , which slows its metabolic breakdown. The result of this tinkering is a more manageable psychedelic experience: although it still requires psychological support, the trip lasts for only 4–6 hours.
Cybin has completed a phase 2 trial of CYB003 for major depressive disorder, using a lower dose than classical psilocybin. In March, the company unveiled data showing that CYB003 achieved strong antidepressant effects that were more durable than those of SSRIs. “After four-and-a-half months, we are seeing the vast majority of patients still responding and staying in remission,” says Amir Inamdar, Cybin’s chief medical officer. CYB003 has breakthrough therapy designation from the FDA and is due to start a phase 3 trial in the next few months, assisted by $150 million raised in March.
Cybin’s pipeline also includes CYB004, an analog of DMT. When given intravenously, DMT itself is rapidly metabolized and causes an intense trip that lasts less than 20 minutes, which may be too brief to be an effective therapy. In contrast, a single intravenous injection of CYB004 produces a 90-minute trip, and Cybin is about to start recruiting patients to a phase 2 trial of the drug to treat generalized anxiety disorder.
Another problem is that some classical psychedelics also activate the 5-HT 2B receptor, which is expressed in heart tissue and can cause long-term cardiac problems. Kristensen’s company Lophora aims to solve that with its lead compound LPH-5, a phenylethylamine derivative with an extra molecular ring that makes it less flexible. LPH-5 has a 60-fold higher selectivity for 5-HT 2A over 5-HT 2B .
Lophora plucked LPH-5 from a large library of analogs, similar but not identical compounds, that the company has screened against various receptors. Other experiments in rats suggest that it could have a persistent and robust antidepressant effect, and the company is now preparing for a phase 1 trial of LPH-5 for treatment-resistant depression, which will use electroencephalogram readings and other measures to assess the drug’s effects. Kristensen expects that a therapeutic dose will not induce a trip in humans, based on experiments that involve measuring head-twitching behavior in mice, a good proxy for their psychoactive effects in humans.
Other companies are confident that they can further reduce or even erase those effects without losing therapeutic efficacy. Gilgamesh, for example, is taking that approach with ketamine, DMT and psilocybin. In the case of ketamine, says Kruegel, the dissociative side effects require that the subjects remain under supervision. So Gilgamesh designed a ketamine analog called GM-1020 that has no dissociative effects (distortions in sight, sound and feelings of detachment) and that also has better oral bioavailability than ketamine itself. After completing a phase 1 trial last year, the company began dosing patients with GM-1020 in a phase 2 trial for major depressive disorder in March. “The hope is that the psychoactive effects will be limited enough that this can eventually be taken at home,” says Kruegel.
Gilgamesh has been using machine learning algorithms to study videos of mice in head-twitch experiments, to accurately quantify the animals’ movements. They are also using Neuropixels probes to directly monitor how hundreds of individual neurons respond to the drugs, offering a much higher resolution than conventional electroencephalograms.
Gilgamesh is also working on GM-2505, a 5-HT 2A agonist that is structurally related to psilocybin and DMT. GM-2505 completed a phase 1 trial late last year and should enter phase 2 for major depressive disorder this year. Its psychedelic effect lasts 60 to 90 minutes — long enough for patients to “explore the altered state of consciousness that might be needed for long-term durable efficacy,” Krugel says, yet within a timeframe that is manageable for healthcare systems. “Personally, I believe that the hallucinogenic effects are an important component, as multiple hallucinogenic compounds have demonstrated durable, transformational changes from a single dose in human studies,” he adds.
Nevertheless, the company is also screening non-hallucinogenic drug candidates for their neuroplastic effects. Neuroplasticity is the brain’s ability to grow and reconfigure its synaptic circuits, and the company hopes that its ‘neuroplastogen’ compounds will retain the efficacy of classical psychedelics while eliminating their hallucinogenic effects. “If it has efficacy, even if it’s not remission after a single dose, the uptake of such a therapy would be much higher,” says Kruegel. “It could be taken with no monitoring, at home, as often as needed, just like any other pharmaceutical.”
Such non-hallucinogenic psychedelic analogs could also be safely taken by patients with schizophrenia or dementia, says Kurt Rasmussen, CSO at Delix. A phase 1 trial of Delix’s DLX-001, a neuroplastogen molecule related to both MDMA and DMT, has shown that it is non-hallucinogenic in people. In rodents, DLX-001 and other neuroplastogens in Delix’s pipeline can stimulate the regrowth of damaged dendritic spines, key structures that help to connect neurons. Animal experiments also show that DLX-001activates 5-HT 2A , but not the cardiac-risk-related 5-HT 2B , and the drug is on course for a phase 2 trial for major depression in 2025.
Delix’s Boston neighbor Seaport is also developing neuroplastogens, along with other compounds, to treat depression and anxiety disorders. “Our particular play is based on the notion that you don’t need a psychedelic trip experience to gather the beneficial effects of these psychedelic agents,” says founder and board chair Steve Paul.
One of the company’s preclinical antidepressants is a non-hallucinogenic LSD analog called SPT-348. LSD itself is a 5-HT 2A agonist, but there is a lot of variation between patients in how quickly it is metabolized in the liver, making it challenging to determine the optimal dose. So Seaport has tethered its LSD analog to a novel drug delivery system called Glyph that helps the drug to circumvent the liver. The drug is attached via a linker to a triglyceride, which is absorbed through the gastrointestinal lymphatic system just like dietary fats and passes directly into the bloodstream before breaking down to release the drug.
Classical psychedelic drugs are challenging to blind with a placebo in a clinical trial, but SPT-348 should be able to avoid that difficulty. “Since we don’t have a psychedelic experience, the idea is you could do a real placebo-controlled trial, which I think is helpful,” says Paul.
In Australia, Psylo has made extensive use of computational modeling to study how hundreds of millions of different molecules fit into the crucial 5-HT 2A receptor and designed thousands of potential drug candidates based on the results. Its non-hallucinogenic lead compound PSYLO-100X is not derived from any classical psychedelic, and Banister prefers to call it “psychedelic adjacent.” The company is still carrying out toxicology studies on the compound, but Banister is hopeful that it will enter a phase 1 trial next year.
Banister notes that regulators have become much more receptive to supporting clinical trials involving psychedelic drugs in recent years, as more evidence emerges that these therapies might help patients. “We’ve seen an enormous growth in mental disorders, exacerbated by the COVID-19 pandemic,” said Steffen Thirstrup, chief medical officer at the European Medicines Agency, during an online Q&A session on 7 May. “I believe psychedelics deserve a second chance.”
In the next couple of years, many of these companies’ clinical trials may begin to answer that crucial question of whether psychedelic drugs can deliver therapeutic benefit without the trip. Positive results could mark a major advance in neuropharmacology. “If it works, the reward there is tremendous,” Kruegel says.
This article is reproduced with permission and was first published on June 3, 2024.
Mexican cartels offering pricey VIP package for migrants trying to get into US
CIUDAD JUÁREZ, Mexico − The tunnel is dark and narrow. Toxic gases rise from the dank water. Insects scurry along the sides, rattlesnakes wait, coiled. Rodents lurk along the water’s edge.
Yet this drainage network that reaches from Ciudad Juárez into El Paso, Texas, is one of the most sought-after routes for patrons of a VIP migration package offered by Mexican cartels to those with the money to pay for it.
The tunnel route costs at least $6,000, according to interviews with top Mexican state authorities, federal law enforcement officials from both sides of the border and migrants waiting to cross in encampments along the Rio Grande. Ricardo, a migrant smuggler, said he has charged as much as $15,000.
Everything in this underground world functions by a code the cartels give their VIP customers, often delivered by cellphone, that identifies which cartel “travel agency” a migrant is working with so everyone from local police to rival criminal syndicates knows not to harass them.
Investigation: Hacked data reveals which US gun sellers are behind Mexican cartel violence
Heightened U.S. security along the 2,000-mile border with Mexico and fewer legal pathways to come north have been an economic boon for Mexican criminal organizations. Instead of fixing a broken immigration system, the U.S. government is outsourcing migration policy to criminal groups, some experts say, increasing practices of corruption.
“The migrant,” said Blanca Navarrete, director of the migrant advocacy nonprofit, Integral Human Rights in Action, “is the one to pay the price for that lack of action.”
A joint investigation by Mexican and U.S. authorities has discovered that one Juárez-based cartel, La Linea, has been smuggling at least 1,000 migrants through the tunnels into El Paso every month, according to a senior Mexican official.
Experts predict the return on investment of trafficking humans has eclipsed that of trafficking drugs.
“Criminals have shifted from their primary business, which was drug trafficking,” said Arturo Velasco, head of the anti-kidnapping unit at the Chihuahua attorney general’s office. “Now 60 to 70% of their focus is migrant smuggling.
“A kilo of cocaine might bring in $1,500, but the risk is very high. The cost-benefit of trafficking a person is $10,000, $12,000, $15,000.”
Velasco says he has seen the pressure − and with it, opportunity − grow in the past two years, after economies around the world gutted by the COVID-19 pandemic led people to migrate in search of work. Natural disasters driven by climate change and violence also have spurred Latin Americans to leave their countries.
A draft study by the Autonomous University of Ciudad Juárez, expected to be published later this year, estimates record-breaking payments made to migrants in Mexico by family members in the U.S.
“Remittances in cities like Ciudad Juárez have doubled to nearly $90 million per trimester so far in 2024,” said Ines Barrios de la O, an immigration specialist at the college. That is up from between $40 million to $60 million in the border town in 2015, she said.
“Migrants walk around with a price on their heads,” she said, “desperate to cross, scared for their lives.”
'Everyone is in on it'
For the VIP transit to work, key people must be in on the action. Interviews with migrants and government officials suggest the system relies on an already established flow of bribes that reach from high-level Mexican immigration bureaucrats to the city’s municipal police.
“Corruption in Juárez, or in any other Mexican border city, must be in collusion with authorities,” said Oscar Hagelsieb, a former assistant special agent in charge of the U.S. Homeland Security Investigations unit in Ciudad Juárez who now runs a security consulting firm in El Paso.
Velasco said investigations by his office have found that Mexican National Guard and immigration authorities turn migrants over to cartels and sell migration permits that allow people to legally transit through the country.
“We know of federal law enforcement that traffic migrants,” Velasco said. “From inside shelters, they, along with officials from the National Institute of Migration, send information on people and then, outside, these people are abducted by criminal groups.”
Requests for comment sent to the National Guard by phone and messaging app were not returned. The National Institute of Migration declined to comment.
Local police abduct migrants for profit as well, Velasco said. And they are a crucial part of the migrant smuggling operations in Juárez networks in the city.
In Juárez, municipal police Chief Cesar Omar Muñoz Morales denied the allegations of corruption, saying it’s “difficult and complicated” to “address things that are not formally documented.”
“It’s tough to respond to your question when there are no formal complaints for our department to follow up on,” Muñoz said. He described his department as clean and efficient, adding, “We’re doing the best we can.”
Velasco, however, confirmed that police officers are kidnapping migrants, who are then held in safe houses − in one case, just feet from the homes of one officer − until they come up with the amount they agreed to pay the cartel before starting their journey.
State investigators documented municipal police participating in kidnapping of migrants arriving at the Juárez International Airport. This year, that has resulted in several shootouts between government and rival human smuggling groups, which has turned the airport area into the latest turf war for organized crime.
The migrant smuggler who spoke with USA TODAY confirmed that municipal police play an integral role for his organization as well, including transporting migrants from the safe houses to the tunnels.
“They load people onto their trucks, and they care for them so that another cartel doesn’t abduct them,” Ricardo said.
The officers not only bring clients to drain entrances, he said, but they provide cover for him and his fellow smugglers to head into El Paso. For this service, Ricardo said, he pays a police commander nearly $600 a migrant.
“It’s millions of pesos in extortions, and everyone is in on it,” said Tony Payan, director of the U.S.-Mexico Center at Rice University who has written a book about the political situation in Juárez.
“In other words,” Payan said, “it’s an extortion force.“
The promise of a bus ride, free of hassles
Ciudad Juárez is at the heart of tensions of migration and immigration policy.
Last year, El Paso recorded 427,000 encounters with Border Patrol authorities, the most of any sector along the southern U.S. border.
Migrants come to the city from all over the globe. Some, like the Chinese, pay exorbitant fees of up to $75,000 for the VIP packages, according to Ricardo.
Others fall short or run out of money and find themselves among hundreds camping on the banks of the Rio Grande.
There they say they feel like hostages, stuck between a desire to stay away from criminal groups yet within reach of the U.S. Standing between them and their destination are hundreds of Texas National Guards members in Humvees and in helicopters hovering above.
Andrés, a 25-year-old Venezuelan, naps in a sleeping bag in an area he knows as “no-man’s land.” Nearby, others sleep on flattened cardboard boxes.
One recent afternoon, Andrés, who asked to be identified by only his first name, recounted how he came north on the promise of a “VIP package” advertised on social media. The package described crossing through the Darien Gap on a horse, he recalled, followed by a bus ride, free of hassles.
He navigated his trip through his cellphone, communicating with a chain of regional cartel representatives starting in his hometown, Caracas, all the way to the northern Mexican state of Chihuahua.
Everything went as planned until he reached Juárez, Andrés said. By then, he had paid half of the $15,000 fee to the cartel, but he had no money to cover the other half. As a result, his cartel travel agency stopped responding.
His family loaned him $750 to pay for a code provided by local criminal groups.
It’s especially helpful, he said, when he needs to cross the street next to the Río Grande, where his camp is located.
As Andrés sat on the banks of the river, he pointed to men in pickups with high-powered weapons. Below, on a highway, municipal police cars drove up and down. All had demanded his code, he said.
Andrés was growing desperate. He saw his only option as jumping over, or crawling through, the concertina wire between him and the United States. Then he would make a dash past Texas National Guardsmen and into the arms of U.S. immigration authorities.
Down the road, in central Juárez, Ricardo talks about the promising future his job has provided. In just five years, he has gone from being a low-level guide to managing 15 migrant smugglers. He said he smuggles about 50 migrants a month into the U.S. and gets paid thousands of dollars per person.
Much like the people he brings through the storm drains, he, too, has a dream.
“I want to buy my mother a car, a house, everything,” he said. “In fact, construction is already underway."
This article is published in partnership with the Puente News Collaborative, a bilingual nonprofit newsroom, convener and funder whose mission is to provide high-quality news and information about the U.S.-Mexico border. Alfredo Corchado is executive editor and correspondent for the collaborative.
- Click here - to use the wp menu builder
CEO to ride-along with Werner truck driver on 1200 mile trip

A C-suite executive will spend a week on a truck with a Werner truck driver in order to learn more about life on the road.
National Association of Truck Stop Owners (NATSO) President and CEO Lisa Mullings joined Werner truck driver Jennifer Evans on a week-long, 1200 mile trip that left out of Joilet, Illnois on Monday, June 24.

NATSO describes the trip as a “unique safety collaboration between the travel center industry and its professional truck driving customers.”
The trip will include stops at truck stops and travel centers to provide Mullings with a better understanding of the OTR lifestyle.

Evans has driven for Werner since 2003 and has achieved 1.3 million safe miles.
“Truck stops and travel centers serve as the home away from home for more than 3 million professional truck drivers,” said NATSO President and CEO Lisa Mullings. “By experiencing life on the road through the eyes of a professional truck driver, I have an incredible opportunity to help our industry meet the unique needs of the truck driving customer. Providing drivers with safe and secure places to stop and rest is the No. 1 priority of our industry. By ensuring a positive experience for truck drivers, we can help to ensure that commercial drivers remain in this critical profession while spurring others to consider a career as a professional driver.”
“We are excited to collaborate with NATSO, as this initiative will provide invaluable real-world feedback from professional drivers to enhance the safety and overall experience at truck stops nationwide,” said Werner’s Vice President of Safety and Compliance, Jaime Hamm. Jennifer Evans’ unique insights as a female professional driver will add exceptional value and a unique perspective on the road.”
NATSO is a trade group representing America’s travel plaza and truck stop industry.
Get the hottest daily trucking news

This Week in Trucking
Former wwe star arrested while working as love’s security guard, bus driver at fault but won’t be charged for collision with big rig that killed 17, rcmp says, wife of trucker killed in crash with deported driver calls for “more accountability on the truckers”, new york state dot to switch to mile-based exit numbering, jarring dashcam shows truck plummeting down embankment after car’s sudden stop for deer, video shows crash that got gravel hauler cited for ‘careless driving in a construction zone’, four-wheeler causes load shift in desperate attempt to make exit, trucker pays the price when box truck driver just forgets how to drive for a second.
Former Michigan police chief is sentenced to prison for stealing drugs on the job
A former michigan police chief is being sentenced to more than three years in prison for stealing drugs on the job.

HARTFORD, Mich. (AP) — A former Michigan police chief who admitted stealing drugs from her department was sentenced Monday to more than three years in prison.
Circuit Court Judge Kathleen Brickley said Tressa Beltran tarnished the image of law enforcement.
“The reverberations from what you did will carry on long after,” the judge said.
Beltran resigned as police chief in Hartford in southwestern Michigan in 2023, six months after investigators searched department offices. She admitted stealing prescription drugs, especially hydrocodone, from a disposal box.
Beltran pleaded guilty to drug possession and using a computer to commit a crime. She was accused of selling drugs and using her influence to extort others for drugs.
“I am trying to make myself better, and I do think that putting me in prison is not the answer. But I’m just sorry,” Beltran told the court.
She will be eligible for parole after roughly 3 1/2 years in prison.

Thousands without power across mid-Michigan

Sheriff’s office looking for missing, vulnerable person

Crews respond to house fire in Bay City

12-year-old boy’s death at camp ruled a homicide

Tuscola Co. woman wins $500K on scratch-off
Latest news.

Judge blocks Michigan’s abortion waiting period, 2 years after voters approved abortion rights

Tree destroys cabin at Michigan camp, trapping counselor in bed for 90 minutes

Detroit Pistons fire coach Monty Williams after one season that ended with NBA's worst record

Lions sign Jake Bates, United Football League kicker who hit 3 FGs of at least 60 yards this season
- Election 2024
- Entertainment
- Newsletters
- Photography
- Personal Finance
- AP Investigations
- AP Buyline Personal Finance
- AP Buyline Shopping
- Press Releases
- Israel-Hamas War
- Russia-Ukraine War
- Global elections
- Asia Pacific
- Latin America
- Middle East
- Election Results
- Delegate Tracker
- AP & Elections
- Auto Racing
- 2024 Paris Olympic Games
- Movie reviews
- Book reviews
- Financial Markets
- Business Highlights
- Financial wellness
- Artificial Intelligence
- Social Media
Biden plans to head to Camp David to prepare for June 27 debate with Trump
President Joe Biden talks with Air Force Col. Angela Ochoa, Commander, 89th Airlift Wing, as he arrives at Andrews Air Force Base, Md., on Marine One Monday, June 10, 2024. (AP Photo/Manuel Balce Ceneta)
- Copy Link copied
WASHINGTON (AP) — After back-to-back trips to Europe, President Joe Biden plans to head to Camp David next week to prepare for his first 2024 debate with former President Donald Trump , hunkering down at the woodsy Maryland hideaway that has hosted many similar cram sessions in the past.
Biden spent most of last week in France marking the 80th anniversary of D-Day . He goes to Italy on Wednesday for a summit of the Group of Seven industrialized nations and then straight to Los Angeles for a weekend fundraiser featuring Hollywood superstars George Clooney and Julia Roberts.
All that travel has left Biden little time to devote to preparation for the June 27 debate. A second faceoff is set for Sept. 10.
A person with knowledge of the president’s plans, who insisted on anonymity to more freely discuss them, suggested Biden could spend the better part of a week at Camp David getting ready for the first debate.
But others involved in the planning said Monday that details were still being worked out, including how many days Biden would devote to prep. They said exactly where he’d be doing it, at Camp David or elsewhere, had not been finalized.
Camp David, located in the Catoctin Mountains northwest of Washington, is no stranger to presidents prepping for the debate stage. Presidents Jimmy Carter and Ronald Reagan went there to ready themselves for debates during their reelection campaigns, as did George H.W. Bush before a debate in 1992.
What to know about the 2024 Election
- Democracy: American democracy has overcome big stress tests since 2020. More challenges lie ahead in 2024.
- AP’s Role: The Associated Press is the most trusted source of information on election night, with a history of accuracy dating to 1848. Learn more.
- Read the latest: Follow AP’s complete coverage of this year’s election.
President Barack Obama visited Camp David before his final debate with Republican Mitt Romney in 2012. Biden himself used the presidential retreat to prepare for his State of the Union address in February.
In a memo released to coincide with the one-month mark prior to the debate, Jen O’Malley Dillon, chair of Biden’s reelection campaign, wrote that the president will aim to go on the offensive and push Trump to talk about how his three appointees to the Supreme Court helped overturn Roe v. Wade, and how he could further undermine abortion rights in a second term.
Biden also wants Trump to discuss his “attacks” on U.S. democracy and promotion of political violence and an economic agenda that Biden’s team says will furnish the rich with tax cuts while imperiling funding for Social Security, O’Malley Dillon wrote.
Trump, meanwhile, has been eager to debate Biden, challenging him to a faceoff “anytime, anyplace.”
At one point Trump suggested that the president join him for a debate outside the lower Manhattan courthouse where the presumptive Republican nominee was on trial for 34 felony counts in a case involving hush money payment to a porn actor. Trump’s campaign set up an empty lectern at several of his rallies to underscore the message.
While Trump participated in more traditional debate prep in previous races — with his former friend-turned-critic Chris Christie playing the role of Hillary Clinton in 2016 — his team insists that this time around he will be eschewing the kind of formal preparation expected from Biden.
“President Trump takes on numerous tough interviews every single week and delivers lengthy rally speeches while standing, demonstrating elite stamina,” said Trump senior adviser Jason Miller.
Associated Press writer Jill Colvin contributed to this report from New York.

'Ozempic Face': The new cosmetic concern you should be aware of
The diabetes drug may help shed the pounds, but for some an unexpected consequence is sagging skin....

Injectable medication semaglutide, better known by the brand names WeGovy and Ozempic, was developed to help manage Type 2 diabetes, but it’s dominated headlines because of its dramatic weight loss effect and droves of celebrity fans.
Oprah, Sharon Osbourne and Rebel Wilson have all spoken candidly about the benefits, but whisperings about so-called 'Ozempic Face' took off after the effects of rapid weight loss began to show on some celebrity faces, leaving them looking drawn and gaunt.
"After extreme weight loss, skin can see reduced levels of elastic and collagen," explains aesthetic surgeon and founder of Dr Glyn MediSpa, Dr Glyn Estebanez. "Both are essential components for the structural integrity of the face and without it we see increased signs of ageing like sagging skin and wrinkling. A significant loss of volume in the face can also make facial features appear more pronounced," says Dr Glyn.
"My lower face and neck looks droopy now and I still have some stubborn pockets of fat, so I’m looking for treatments to sort this out"
WeGovy user Amelia has been taking the drug for 8 weeks and lost 10% of her body weight, but was struck with how quickly her facial appearance changed: "My lower face and neck looks droopy now and I still have some stubborn pockets of fat, so I’m looking for treatments to sort this out," she tells me.
"There are several non-surgical ways to treat ‘Ozempic Face’," says Dr Salenna Zimri, founder of Skin Doctor Clinics, "From skin regenerating lasers to precise filler placement." This aesthetic concern is now being addressed by doctors through innovative skin tightening procedures, restoring patients' confidence and appearance.

There are treatments that have skyrocketed as a result, including ultrasound therapy, and advanced dermal fillers. The growing popularity of these treatments highlight the medical community's response to addressing the unique challenges posed by 'Ozempic epidemic'. While we don't endorse the use of Ozempic, we recognise that concerns about sagging skin are widespread beyond this issue. If you're worried about skin laxicity or simply curious about available options, we've compiled a list of the most popular and effective treatments on the market right now...
Thermal Lifting
Sofwave is a needle-free, non-invasive skin treatment that gives an instant lifting effect. "The device is placed on the face and delivers ultrasound waves to the mid-dermis layer of the skin," says Dr Saleena. These microscopic vibrations create controlled, precise thermal injuries 1.5mm under the skin’s surface to stimulate the body’s natural healing response. Although it’s non-invasive, patients can feel significant heat on the skin, which is minimised by numbing cream. “The heat generated by the energy also triggers the production of new collagen and elastin fibres, which help to tighten and firm the skin over time,” Saleena tells us. Expect to see improvements in skin texture and firmness, and a lifting effect, over 12 weeks and results can last up to a year.
Sessions start from £1295 up to £2500 for full face and neck. Skin Doctor Clinics
Sculpting Injectables
"After significant fat loss we focus on replacing volume where it’s needed," says Dr Glyn. This is done with carefully injected soft tissue hyaluronic acid fillers like Juvéderm or Restylane. "These plump the skin and support areas like the cheek and tear trough, to give skin a smoother, even-toned appearance."
Particular types of filler, including Sculptra and Ellanse, contain ingredients to stimulate skin’s natural collagen production. And sometimes taking a two-pronged approach to sagging skin by combining fillers with collagen synthesising ingredients is necessary for the most natural result. "Bio-stimulators don’t volumise the face instantly, unlike traditional fillers," says Dr Saleena. "Instead, they stimulate fibroblasts in our skin to produce more collagen. This improves the quality of skin and helps with laxity." It’s not a permanent solution but many people will notice results lasting 12-24 months.
Prices start from £340 per treatment. Prima Aesthetics
Stimulating Collagen
Some are addressing the side effects of rapid weight loss with non-surgical treatments like Exion. Combining radio-frequency and targeted ultrasound in one, "this non-invasive technology targets skin laxity by gently heating problem areas to stimulate the skin’s natural collagen, hyaluronic acid and elastin production - key components for plump, healthy-looking skin," explains aesthetic doctor, Dr Wassim Taktouk.
A comfortable treatment with zero downtime, Exion is used on the face and body to tighten and rejuvenate sagging skin. Much like Sofwave, Exion utilises heat from ultrasound waves to induce thermal injury on the skin’s underlying tissues but it differs slightly by incorporating radiofrequency energy adding further micro-injuries to the dermis. Skin is left plumped, smoothed and significantly tighter. Benefits are noticeable from three months post-treatment but a course of 3-6 sessions is recommended to see maximum results.
Prices start from £300 per session. Dr Wassim Taktouk
More June Digital Edition 2024

Editor’s Letter: June-July 2024

10 Luxury travel minis to take on your next trip
'sport isn't the only part of my identity' jazmin sawyers on how fashion helped overcome her olympics setback.

Game, Set and Match: In Conversation with Paige Lorenze

Keep Calm and Carry On: Hand Luggage Essentials

Paris To Provence: Your Guide To Making The Most Of The Olympics in Paris This Summer

The Radar: The OOO Edition

My Fashion Fantasy: Nicky Hilton on escaping to Maui, her favourite Roman restaurant and where to shop

IMAGES
VIDEO
COMMENTS
It is called a trip because the sensations that a psychedelic ( hallucination-causing) drug causes can be so strange that it feels as if you are in a whole different world. A bad trip, also sometimes called a bad acid trip, occurs when the trip a psychedelic drug causes is negative. Bad trips can lead to excessive fear, agitation or emotionally ...
Step Six: Seek Help if Needed. Despite your best efforts, sometimes a person having a bad trip may become a danger to themselves or others or have physical symptoms like a fever that require medical attention. The best thing you can do at that time is to call 911 and refer the person to medical experts who can help them through the rest of the ...
What It's Like to Trip on DMT. Everything to know about the hallucinogenic "spirit molecule"—common side effects include seeing aliens and finally connecting with the universe. MH. by ...
There are two important and easy actions to avoid having a bad trip: − 1) Abstain from recreational drug use ultimately to be safe against the risks of a bad trip and the long-term effects of drug use − 2) Avoid taking medications referred to as "trip killers" such as benzodiazepines (e.g., diazepam or lorazepam) or antipsychotics (e.g ...
Some of the trip-killing drug doses suggested in the Reddit posts were high. For example, quetiapine was suggested to be used at 25mg to 600mg, but clinical guidance for these drugs suggests a ...
1. Alprazolam (Xanax) Alprazolam is one of the fastest-acting trip killers in the benzodiazepine family — but it's also one of the shortest-lasting. The effects of Xanax, although fast-acting, only last for around four to six hours. Xanax is a favored trip killer among psychonauts purely because of its fast-acting nature.
A 'trip' is a term used to refer to a drug high. It is most often associated with psychedelic drugs, such as mushrooms and LSD, and may include effects like visual hallucinations or 'visuals'. The act of being on a trip is called 'tripping'. Some users also report tripping while taking drugs such as MDMA and ketamine.
Drug-drug interactions are also often at play during difficult trips, for example, when people combine alcohol with psychedelics. ... Another gift was that my bad trip helped me to better understand, validate, and support others who have been harmed by psychedelics. Another lesson was this: my bad trip was an amplifier of the toxic positivity ...
A bad trip on drugs can be a highly unpleasant and distressing experience. What this looks or feels like for you can vary somewhat from person to person. Side effects of hallucinogenic drug intoxication may be mild, moderate, or intense in nature. Side Effects And Symptoms Of A Bad Trip On Drugs. A bad trip on drugs may be identified by a ...
The risks and dangers you might experience with a bad trip can vary depending on the drug you take. Classic hallucinogens create visual and audio hallucinations and can make your feel sensations that aren't real. The effects usually start as you metabolize the drug, which can be within 20 minutes. Some trips last as long as 12 hours or more ...
Tripping refers to experiencing drug-induced symptoms of psychosis (such as hallucinations and delusions) which commonly occur after taking psychotomimetic substances; these drugs are capable of producing an effect on the mind similar to a psychotic state and include substances such as lysergic acid diethylamide (LSD), ketamine, and even ...
Find an experienced guide or therapist whom you trust. Use word of mouth at psychedelic societies and elsewhere to source psychedelic substances safely, and use online testing kits to ensure their quality. Alternatively, for greater safety, consider signing up to a research trial conducted at a university.
A psychedelic experience (known colloquially as a trip) is a temporary altered state of consciousness induced by the consumption of a psychedelic substance (most commonly LSD, mescaline, psilocybin mushrooms, or DMT). [citation needed] For example, an acid trip is a psychedelic experience brought on by the use of LSD, while a mushroom trip is a psychedelic experience brought on by the use of ...
The most popular psychedelic substances include shrooms and LSD and are typically the suspects responsible for bad trips. Generally, psychedelics cause clouded judgment and impairment, hallucinations, and paranoia. As a result, individuals may believe untrue things and may act in strange ways.
What is a Bad Trip? Unfortunately, the War on Drugs in America has created a lot of misinformation when it comes to psychedelics, particularly with regards to the bad trip. You may have heard rumors that even one experience with lysergic acid diethylamide (LSD) can make you perpetually trip or permanently insane.
Initiate use in the presence of an experienced and trusted guide to help you understand your trip. Purchase the drugs from a trusted source if possible. Choose a safe, peaceful place to hang out. Start with only a small amount. Stay in the company of trusted friends. Stick to one substance at a time.
It is often referred to as the "happy chemical" due to its influence on feelings of happiness and well-being. 1. LSD. Lysergic acid diethylamide, more commonly known as LSD or acid, is an illegal semi-synthetic drug famous for causing extreme distortion of sensory perception as well as hallucinations.
People often use drugs in order to feel good. However, sometimes, a person who is using hallucinogens or other drugs can experience a condition known as a "bad trip," sometimes referred to as a "psychedelic crisis." The phrase "bad trip" is sometimes used to describe a situation where using the drug creates an intensely negative psychological response. 1
The study, "Trip-killers: a concerning practice associated with psychedelic drug use," was published in Emergency Medicine Journal on Dec. 19. It was announced in a news release the same day ...
The drugs at the center of the therapy being taught — still classified by the government as Schedule 1 — cannot be used in the training, a limitation that both students and instructors lamented.
Most users take between five and 10 mg of Olanzapine to kill a trip, which is a typical dose prescribed by doctors (up to 20 mg per day). However, there are reports of some taking 50 mg! Like any other drug, the more you take, the more likely of unwanted side effects. Olanzapine is no different.
A trip sitter—sometimes known as a sober sitter, spotter, or co-pilot—is a term used by recreational or spiritual drug users to describe a person who remains sober to ensure the safety of the drug user while they are under the influence of a drug; they are especially common with first-time experiences or when using psychedelics, dissociatives and deliriants.
In contrast, a single intravenous injection of CYB004 produces a 90-minute trip, and Cybin is about to start recruiting patients to a phase 2 trial of the drug to treat generalized anxiety disorder.
CIUDAD JUÁREZ, Mexico − The tunnel is dark and narrow. Toxic gases rise from the dank water. Insects scurry along the sides, rattlesnakes wait, coiled. Rodents lurk along the water's edge ...
The trip will include stops at truck stops and travel centers to provide Mullings with a better understanding of the OTR lifestyle. Evans "Truck stops and travel centers serve as the home away from home for more than 3 million professional truck drivers," said NATSO President and CEO Lisa Mullings.
She admitted stealing prescription drugs, especially hydrocodone, from a disposal box. Beltran pleaded guilty to drug possession and using a computer to commit a crime.
WASHINGTON (AP) — After back-to-back trips to Europe, President Joe Biden plans to head to Camp David next week to prepare for his first 2024 debate with former President Donald Trump, hunkering down at the woodsy Maryland hideaway that has hosted many similar cram sessions in the past.. Biden spent most of last week in France marking the 80th anniversary of D-Day.
WeGovy user Amelia has been taking the drug for 8 weeks and lost 10% of her body weight, but was struck with how quickly her facial appearance changed: "My lower face and neck looks droopy now and ...