Understanding Patient Visit Average (PVA) and How It Can Help Your Practice | Carepatron

By Jamie Frew on Jun 20, 2024.
Fact Checked by Ericka Pingol.
%2520and%2520how%2520it%2520can%2520help%2520your%2520practice%2520business%2520large.jpeg)

Exploring Patient Visit Average (PVA)
A clinic's Patient Visit Average (PVA) refers to the average number of appointments a patient has attended within your practice over a specific time period and understanding its functions can help you significantly elevate your quality of care. Tracking your PVA can aid in improved clinical outcomes amongst patients, ensure that you're effectively evaluating your performance, and identifying any outliers of client care.
PVA is a vital component of healthcare, as well as practice management software, and allows you to grow and provide the highest quality of service to clients, without compromising on quality across operations. We understand that this can be a bit tricky to initially wrap your head around, which is why we're here to help you get started.
Conducting a health check on your practice
Primary care physicians, mental health professionals, family physicians, fitness coaches—regardless of what you practice, you need to conduct regular health checks to monitor performance and assess your operations for strengths and weaknesses. With the right software, you can do this at a reduced cost, and through a completely paperless method. You can catch warning signs before it's too late, and maintain processes that you excel at!
Here are the numbers that matter:
Total new patients visits
The first aspect that you'll need to check is the number of total new patient visits. You can count this on your client list or on the software that handles your electronic health records and patient data. Generally, this number should be increasing, as it indicates growth and the need for expansion within your practice. If this number is beginning to decline, then this is clearly indicated that further evaluation is needed!
Total repeating patient visits
PVa serves as a quantifier of patient retention. Measuring the number of patients who continue to return is a good way to evaluate client loyalty and the retention value of your business.
Total revenue
Naturally, you'll also want to check on the revenue of your practice to ensure that your expenses don't outweigh your positive cashflows. After all, you are a business, and will need to make a profit to stay afloat!
Calculating and using patient visit average (PVA)
PVA numbers are vital to measuring performance and improving operations within your business. Calculating PVA is a straightforward process that provides valuable insights into your practice's performance. The formula for PVA is:
PVA = (Total number of appointments) / (Number of unique patients)
PVA can be measured within different time periods, with each one providing valuable insight for you to incorporate into your investment and business decisions. For instance, a 3-month report can provide snapshots into your growth, with a 12-month report doing the same, but also evaluating and identifying loyal clients and your retention rate. Lifelong performance reports, of PVAs over the years, can supply with you the richest, most accurate information, in regard to how long clients have been with you.
Using PVAs, you can assess what is normal, and what needs specific improvements unique to your practice. You can ensure you're continuously providing the best care possible, without sacrificing clinical aspects, and you can prevent declines before they start snowballing.
PVAs are not just statistics, but rather, are a measure of growth and are a valuable asset and crystal ball into the longevity of your practice. Even though getting more patients is good, keeping loyal customers come back for subsequent visits is better, and PVA lets you know how many you have.
Example of patient visit average (PVA)
To put PVA numbers into perspective, it may help for us to illustrate an example within Dr. Smith's chiropractic clinic. You can work out the patient visit average, and know to set the right prices for your practice at ease.
For example, Dr. Smith had 400 patients visit his clinic in the last month. He had 30 new patients book appointments with him in the same period. If we divide his total number of appointments this month (400) by the number of unique patients this month (30), his PVA number would be 13.3. Simply put, the average patient returns approximately 13 times to visit Dr. Smith and access his services.
PVAs aren't complicated, and they certainly don't have to be with the right tracking and record-keeping processes in place! Naturally, this can take some time to work out, especially if evaluating patients over longer periods, such as 12 months, however, the maths required isn't difficult. Many practice management software work to automatically calculate this for you, which is a solid win-win for developing your business.
How does tracking PVA help your practice business?
PVA provides immeasurable value to your practice business, as you can assess those who are the acute type, or specifically, those who may not return after a certain number of visits. Sometimes, these are referred to as ‘emergency factor patients', and identifying these individuals through an email or message can help you return them to your regular client list .
Offering new treatments or plans may work towards them becoming regulars, which is always a plus! You can continue strengthening and building professional relationships, as well as earn higher revenue.
Communication goes a long way, with PVAs contributing towards higher clinical outcomes and greater growth sustainability within your practice. The numbers don't lie, and simply by evaluating this statistic, you can identify strengths and weaknesses to elevate the quality of your business and attract more clients. What's not to like?
Top five tips to increase your patient visit average
Now that you know all about patient visit averages, it's important that you're aware of the top five tips and tricks that work towards increasing them. You can reduce waitlists, and increase loyalty amongst patients without compromising on quality. Doing so will also allow you to generate higher revenue and promote greater healthcare solutions within your practice, which is always welcome.
Here's what you can do:
Provide a plan at the end of your patient's session
Patients need to feel that you understand their concerns and queries, have taken them into account, evaluated them, and are using your expertise to the fullest by creating a productive plan that works to improve their condition. Always supply clients with a direct plan that addresses homework and tangible things to work on, as well as future directions. This supports patient education, too.
Book the next appointment in advance
Consider offering services in bundles or package deals to encourage patients to book multiple appointments in advance. Clearly relay to your patients that you run treatment plans and not session-by-session experiences.
This way, your patients can commit to programs that will demonstrate results, with greater accountability and consistency when it comes to their health. This also increases the chance of patients returning to your practice, which will significantly increase PVAs.
If you're transparent with your clients from the start, this shouldn't ever be an issue!
Implement a loyalty program
Want to keep your patients coming back for more? Try setting up a loyalty program. Implementing a loyalty program can be a powerful strategy to increase PVA and foster long-term relationships with your clients.
Start by offering rewards for a certain number of visits, such as a discount on future services or a complimentary treatment after a set number of appointments. This not only incentivizes repeat visits but also demonstrates your appreciation for your patients' loyalty. Make sure to communicate the benefits of the loyalty program clearly and regularly remind patients of their progress towards rewards.
All in all, a well-designed loyalty program is a great way to show some love to your patients and encourage more frequent visits.
Align staff with your PVA plan
Getting your team on board with your PVA goals is super important. Make sure that you and your staff are all on the same page when it comes to healthcare plans and your patient. Clients can interpret things very differently, and so you want to make sure that the odd comment from fellow healthcare professionals doesn't send the wrong impression.
Start by having a team meeting to chat about what PVA is and why it matters. Make sure everyone understands how their role impacts the patient's experience and the overall PVA. Encourage open communication and brainstorm ideas on how to improve PVA together. Regular check-ins can help keep everyone focused and address any issues that pop up. Remember, when your team is in sync, your patients will notice the difference!
Set goals and work towards increasing results
Setting clear PVA goals for your team can really amp up your game. Start by figuring out your current PVA and decide where you want it to be. It can help to set, measure, record, and display each member of staff's PVA numbers, as this can work as effective motivation and encouragement towards elevating the quality of care of your business.
In addition, break down the big goal into smaller, achievable targets and assign them to your team members. Make sure to track progress regularly and celebrate the wins, no matter how small. Use setbacks as learning opportunities to tweak your approach.
When your team sees their progress, it'll boost their motivation and drive better results for your practice.
Final thoughts
Although PVAs may be unfamiliar territory to you, they're a surefire way to track and monitor your performance and boost growth within your practice. You can identify weaknesses to improve as well as the strengths to emphasize and focus on to increase business value for current and prospective clients. You can evaluate and treat warning signs before they spiral, and ensure that your business is healthy and thriving across all aspects—from patient care to administrative operations.
Best of all, PVAs don't have to be complicated and are an easy way to elevate the status of your practice. Start tracking your PVA numbers now, and start your practice on the journey of improvement.
Get Carepatron for free today to create a lifetime's worth of better patient outcomes.
.png)
Further reading:
- The future of healthcare: Value creation through next-generation business models
- How to Start a Healthcare Business: The Ultimate Guide
Related Articles
.jpeg)
Join 10,000+ teams using Carepatron to be more productive
This site works best with JavaScript enabled.
What is a Patient Visit Average (PVA)?
A Patient Visit Average is the average number of appointments a patient has with your clinic over a given period of time. Physiotherapist, clinic owner, and business coach, Andrew Zacharia, explains why tracking this number will improve your patient care.
Andrew Zacharia , PhysioFit Adelaide · 12 April, 2021

As health professionals, numbers aren’t always our strong suit. Even if they are, many of us believe numbers should not play a role in healthcare at all… But before you close this article, hear me out! I want to help explain how keeping better track of business metrics can improve the mentoring of your team and, ultimately, better care and outcomes for your clients.
I have been calculating my clinic’s Patient Visit Average (PVA) for roughly 5 years. This is also sometimes known as the Client Visit Average or CVA.
I just import the data from Cliniko into my own spreadsheets. Then, I set up calculations for the PVA by dividing the total number of appointments by the number of new patients in the system over the same period.
I used to track this as a quarterly and year number as well as over a practitioner's lifetime within my clinic to get an indication for what is common or normal within our clinic, and find out what may be an outlier in client care.
Cliniko has just made this easier by allowing you to automate the PVA calculation (you can find this in the Practitioner Performance Report).
What is a Patient Visit Average?
A Patient Visit Average is the average number of appointments a patient has with your clinic over a given period of time.
It is the total number of appointments a practitioner (or clinic as a whole) sees divided by the amount of new clients within the same time period.

(total number of appointments)/(number of new clients)
An important distinction is that this does not reflect how many appointments a client attends per injury. Rather, it is an average of the overall appointments attended throughout the period selected (regardless of how many different pains or injuries they have reported).
For example: If Client A attends 8 appointments within your clinic for their lower back pain in a 12 month period, the PVA will be 8. If Client B attends 3 appointments for their niggly shoulder and 6 appointments for a sprained ankle over that same period of time, the PVA will be 9.
When is Patient Visit Average meaningful?
Time frame is an important factor in how you interpret the results of your PVA. In general, more is usually better...
Within my business, I run a weekly performance report but noting the PVA over 7 days is of no worth at all, because it’s not enough time to provide the info I’m looking for. However, when running performance reports for 3-month, 6-month or 12-month periods, as well as the lifespan of the clinic itself, the results become much more meaningful.
A 3-month and 6-month performance report will give you a good indication of the number of visits on average per episode of pain or injury. This is because you are much more likely to have one episode of care in these periods, rather than a client returning numerous times. (Although not impossible, it would be very unfortunate if someone did have 3 or 4 different injuries in half a year!)
A 12-month performance report will indicate how many appointments, on average, a client has with you in a single year. This may be valuable to note and will likely include longer periods of care or numerous episodes of care.
A lifelong performance report, covering a number of years, will give you the truest form of Patient Visit Average, which is how many appointments a client has with you, on average, over a lifetime.
Each of these periods of time may provide very different PVAs, so it is important to keep that in mind when interpreting your results.
The type of services you offer or populations you work with may also impact the numbers represented by the Patient Visit Average. For example: A physiotherapy clinic may have a PVA of 10 in a 12-month period. A podiatry clinic offering skin and nail care may have a PVA of 5 or 6. And a speech pathology or occupational therapy clinic working with a child on a specific skill or function may have a PVA of 30, 40 or even 50+ in a single year depending on the needs and frequency of therapy.
Finally, the last consideration is the number of years a practitioner has spent at your clinic. A new graduate or new team member will likely see a higher proportion of new clients in their first 12 months, resulting in a lower PVA relative to team members who have been with you for several years.
As a team member passes the 24-month mark, it is much easier to compare data across the board as even returning clients don’t skew the averages too far at that stage.
It is important to keep in mind that because of all of these factors, there is no “Benchmark Patient Visit Average” in healthcare, just the reflection of what is occurring within your clinic.
How can monitoring Patient Visit Average help your team members and clients?
The PVA shows you what is occurring within your clinic. When you compare these numbers over a similar period of time, we can get an indication for what is common or normal within our clinic and what may be an outlier in client care.
Here is an example where PVA could be used to help our team members improve client care and outcomes. (Please remember to run this through the filter of time periods, types of clients, and number of years a practitioner has been with your clinic).
SCENARIO: The average clinic PVA after 12 months is 8.
- Experienced Practitioner PVA is 10
- New Graduate 1 has a PVA of 7
- New Graduate 2 has a PVA of 3
What we can see here is there is a different standard of care amongst the Experienced Practitioner, New Graduate 1, and New Graduate 2. As a mentor to young health professionals, I wouldn't compare either of the new graduates to the Experience Practitioner. Instead, I see this as a call to open up a conversation with New Graduate 2 around areas they may be struggling with, lacking knowledge or practice in, or needing further opportunities to improve.
In this case, I would not be comparing New Graduate 1 and New Graduate 2 to the Experienced Practitioner, asking them to improve their PVA to 10. That is too numbers-driven and forgetting client care completely. I may not even be too concerned with New Graduate 1’s PVA of 7 given they are 12 months into their career and should continue to upskill and improve. I’m looking at New Graduate 2’s client care. I want to find out more about this practitioner’s story. What I am looking for is what is occurring with this practitioner that is so different to the client care and client experience when compared to everyone else in our clinic.
In the past, opportunities that have risen from these types of conversations are:
- A lack of self-confidence from the practitioner.
- Uncertainty or self-doubt with explaining conditions or the plan ahead to clients
- Seeing complex cases where they simply need help with learning more about the assessments and management of certain conditions.
- Not having the knowledge in a specific area of client care such as acute pain management or exercise prescription.
- Opportunities to improve the soft skills of communication, goal setting, rapport building, and client-therapist alliance.
- Projecting their own beliefs such as financial concerns or poor time management, believing clients may not be able to afford their appointments or believe they are too busy to attend, without discussing these concerns with the client themselves.
Working on, and making improvements to, these areas results in clients receiving the best care possible. This creates better outcomes for the client, and more raving fans for our clinic.
It also means fewer clients are heading down the sad route of being lost within our medical system, getting prescribed pain medications, being referred off for unneeded surgeries, or progressing towards persistent pain conditions.
These are such important aspects of learning and growth for all practitioners (not just new graduates), and I truly do believe these conversations hold the power to improve the lives of our clients…and it can all start with monitoring this little stat we call PVA!
Keep reading

How to onboard new team members for long-term success
In this guest post, Andrew Zacharia shows us how his team at PhysioFit Adelaide welcomes new practitioners and nurtures healthy working relationships that last for years.

The 4 considerations for going into business with a friend
There is a large debate in the business world about whether or not you should go into business with someone you’re currently friends with. Clinic Mastery's Peter Flynn outlines the things you should consider before choosing a friend as a business partner.

Cliniko is now a fully endorsed partner of the Australian Physiotherapy Association
Run your practice with confidence, knowing that Cliniko is recognised as an industry leader, equipped with the tools you need to manage your practice and give your patients the attention they deserve.
- Doctors, Clinics & Locations, Conditions & Treatments
- Patients & Visitors
- Medical Records
- Support Groups
- Help Paying Your Bill
- COVID-19 Resource Center
- Locations and Parking
- Visitor Policy
- Hospital Check-in
- Video Visits
- International Patients
View the changes to our visitor policy
View information for Guest Services
New to MyHealth?
Manage Your Care From Anywhere.
Access your health information from any device with MyHealth. You can message your clinic, view lab results, schedule an appointment, and pay your bill.
ALREADY HAVE AN ACCESS CODE?
Don't have an access code, need more details.
Learn More about MyHealth Learn More about Video Visits
MyHealth for Mobile
Get the iPhone MyHealth app Get the Android MyHealth app
WELCOME BACK
Cost estimator.
Better manage your health care with the Cost Estimator tool. The online tool offers an intuitive way to estimate your out-of-pocket cost of care for common exams, procedures, tests, and services, empowering you to make informed financial decisions about your treatment.
If you have any questions, please call the Financial Counseling department at 844-498-2900 .
If your medical services are scheduled for a Tri-Valley location, please call 925-534-6457 .
Note: Our online Cost Estimator tool currently supports a limited number of health services that are mandated to meet regulatory requirements. Stanford Health Care is working diligently to increase the number of shoppable services included in our tool.
Estimate your out-of-pocket cost of care for common services
By using the Cost Estimator tool, you confirm: I understand that this is an estimate based on charges for typical hospital and professional services. Should I elect to have this procedure performed at Stanford Health Care, I acknowledge that any final bill may vary from this estimate for many reasons, among them: my medical condition, length of hospital admission, unknown circumstances or complications, final diagnosis, and recommended treatment ordered by my physician(s). I acknowledge that my actual insurance benefits may be different than shown in this estimate. Prior to any medical service, I know that I may contact our Financial Counseling for a personalized estimate at 844-498-2900 .
Why Stanford Health Care
Whether you are seeking primary care for a wellness check-up, or specialized care for a complex condition, you can trust us for high-quality, innovative services. In fact, U.S. News & World Report has honored us as one of the nation’s top hospitals.
Our doctors and nurses combine expertise and compassion to understand your unique health needs and to personalize a precise care plan specifically for you.
QUICK LINKS
- Health Insurance Plans
- Financial Counseling
- Financial Assistance
How to Read Your Bill
Billing Process Explained
Tips for Organizing Your Bill
Pricing Transparency
Billing Glossary
Billing FAQs
Insurance FAQs
Guide to Understanding Healthcare Prices
Insurance Glossary
NPI and Tax ID

Average Revenue per Patient Visit
Boost patient experience and your bottom line by automating patient cost estimates, payer underpayment detection, and contract optimization in one place.
What is Average Revenue per Patient Visit
Average Revenue per Patient Visit (ARPV) is a key metric in healthcare revenue cycle management that measures the average amount of revenue generated per patient visit. This metric is calculated by dividing the total revenue generated by the number of patient visits during a specific period of time. ARPV is an important metric because it provides insight into the financial performance of a healthcare organization. By tracking ARPV over time, healthcare providers can identify trends and make informed decisions about pricing, reimbursement, and resource allocation. ARPV can also be used to compare the financial performance of different healthcare providers. For example, if two providers have similar patient volumes but one has a higher ARPV, it may indicate that the higher-performing provider is more efficient or has better pricing strategies. Overall, ARPV is a valuable metric for healthcare revenue cycle management because it provides a clear picture of the financial health of a healthcare organization and can help guide decision-making to improve revenue generation.
How to calculate Average Revenue per Patient Visit
Average Revenue per Patient Visit is calculated by dividing the total revenue generated by the number of patient visits during a specific period. To calculate this metric, healthcare organizations need to track the total revenue generated from all sources, including insurance payments, patient payments, and other revenue streams. They also need to track the number of patient visits during the same period, which includes both new and returning patients. Once the total revenue and the number of patient visits are determined, the average revenue per patient visit can be calculated by dividing the total revenue by the number of patient visits. This metric is useful in evaluating the financial performance of healthcare organizations and identifying areas for improvement in revenue cycle management.
Best practices to improve Average Revenue per Patient Visit
Best practices to improve Average Revenue per Patient Visit are:
1. Accurate and Timely Documentation: Accurate and timely documentation of patient visits is crucial to ensure that all services provided are captured and billed correctly. This includes documenting all procedures, tests, and treatments provided during the visit.
2. Upcoding and Downcoding: Upcoding and downcoding can have a significant impact on the Average Revenue per Patient Visit. Upcoding refers to billing for a higher level of service than what was actually provided, while downcoding refers to billing for a lower level of service. It is important to ensure that the coding accurately reflects the services provided.
3. Charge Capture: Charge capture is the process of capturing all billable services provided during a patient visit. This includes ensuring that all procedures, tests, and treatments are captured and billed correctly.
4. Denial Management: Denials can have a significant impact on the Average Revenue per Patient Visit. It is important to have a robust denial management process in place to identify and address denials in a timely manner.
5. Patient Collections: Collecting patient payments at the time of service can help improve the Average Revenue per Patient Visit. This includes verifying insurance coverage and collecting any copays or deductibles at the time of the visit.
6. Staff Training: Staff training is crucial to ensure that all staff members are aware of the importance of accurate and timely documentation, charge capture, and denial management. This includes providing ongoing training and education to staff members.
7. Technology: Technology can play a significant role in improving the Average Revenue per Patient Visit. This includes using electronic health records (EHRs) to capture and document all services provided during a patient visit, as well as using revenue cycle management software to streamline billing and collections processes.
Overall, improving the Average Revenue per Patient Visit requires a comprehensive approach that includes accurate and timely documentation, charge capture, denial management, patient collections, staff training, and technology. By implementing these best practices, healthcare organizations can improve their revenue cycle management and ultimately improve their financial performance.
Average Revenue per Patient Visit Benchmark
The industry standard benchmark for Average Revenue per Patient Visit varies depending on the type of healthcare facility and the services provided. For example, hospitals typically have a higher benchmark than physician practices due to the complexity and cost of services provided.
It is important for healthcare organizations to regularly monitor their Average Revenue per Patient Visit benchmark and compare it to industry standards to identify areas for improvement and optimize revenue cycle performance. By analyzing this metric, organizations can identify opportunities to increase revenue, improve patient satisfaction, and enhance overall financial performance.
How MD Clarity can help you optimize Average Revenue per Patient Visit
Revenue cycle software can significantly improve the Average Revenue per Patient Visit metric by streamlining the billing and coding process. With the help of advanced software, healthcare providers can easily identify any coding errors or missed charges, which can lead to a significant increase in revenue per patient visit.
Moreover, revenue cycle software can also help providers to identify any trends or patterns in patient behavior, which can help them to optimize their billing and coding processes. By analyzing patient data, providers can identify the most profitable services and procedures, and focus on providing those services to increase revenue per patient visit.
If you're looking to improve your Average Revenue per Patient Visit metric, then it's time to consider implementing revenue cycle software. MD Clarity's revenue cycle software is designed to help healthcare providers streamline their billing and coding processes, and optimize their revenue cycle management. Book a demo today to see firsthand how MD Clarity's revenue cycle software can improve your revenue cycle metrics.
Get paid in full by bringing clarity to your revenue cycle
Related metrics, dispute resolution rate.
Learn how to improve your healthcare revenue cycle management with our guide on Dispute Resolution Rate. Calculate, benchmark, and optimize for success.
Average Patient Liability
Learn about Average Patient Liability in healthcare revenue cycle management. Discover how to calculate, improve, and benchmark performance. Read now!
Subscribe to the

Healthcare Clarified newsletter
Get the latest insights on RCM and healthcare policy in your inbox
How to Calculate Your Ideal Patient Load
Here's a quick lesson on how to figure out how many patients your clinic should see each day. Click here to learn more about ideal patient loads, here.

Get the latest news and tips directly in your inbox by subscribing to our monthly newsletter
As a rehab therapy provider, the strength of your clinic’s revenue stream depends mainly on the number of patients you see each day—and the dollar amount you receive for each one of those visits. So naturally, if you want to increase your clinic’s revenue, you mostly likely will need to increase the volume of patients you treat.
But how do you figure out how many patients you should be seeing each day—in other words, your ideal patient load? Before you break into a flashback-induced cold sweat—hey, word problems were never my mathematical forte, either—take a deep breath and relax. When you break it all down, it’s actually pretty simple to come up with a ballpark patient volume target. As pediatric practice administrator Brandon Betancourt explains in this blog post, there are four main steps to calculating your clinic’s perfect patient quantity:
1. Determine your practice cost.
This is the total dollar amount of all your practice’s expenditures, including operating costs (e.g., rent, utilities, equipment, supplies, and fees) and employee salaries and benefits. Let’s say your operating costs come to $300,000 and your salary costs total $200,000. Thus, your total practice cost is $500,000.
2. Calculate the average payment per patient encounter.
As Betancourt writes, a simple method of determining this figure is to add up all of your encounters for the year and divide that number by your net receivables. For example, if your practice brought in $600,000 in total receivables with 6,000 encounters, then your average payment per encounter would be $100.
3. Count the number of days per year you worked (or will work).
For simplicity’s sake, let’s say your practice is open five days a week all year. That means you have approximately 260 working days. Please note that this number may fluctuate based on vacation time or holidays.
4. Figure out your breakeven point.
Now that you have all of the necessary values, you can plug them in to calculate the number of patients you’ll need to see each day in order to break even for the year. First, divide your practice cost by your average payment per visit to determine the total number of patients you’ll need to see for the year. In our example, this would be:
$500,000 / $100 = 5,000 patients
Now, assuming that your practice is open 260 days a year, you can use the following equation to determine the number of patients you’ll need to treat each day to offset your costs:
5,000 / 260 = 19.23 patients (round up to 20 to be safe)
Keep in mind that this is a very basic method of calculating a healthy patient load for your practice. There are other factors at play, and an experienced accountant can help you plan for those. Still, this is a good exercise to give you an idea of what you should shoot for as far as patient volume.
Have you figured out your practice’s ideal patient load? What advice do you have for others who are trying to come up with this number? Share your thoughts in the comment section below.
Related posts

FAQ: What is a MOG Gym?

FAQ: How Are PT Services Billed?


A Trilogy of Billing Blunders: Overbilling, Misbilling, and Underbilling

Learn how WebPT’s PXM platform can catapult your practice to new heights.

- Industry News
- Access and Reimbursement
- Law & Malpractice
- Coding & Documentation
- Practice Management
- Patient Engagement & Communications
- Billing & Collections
- Staffing & Salary
A Metric to Quantify the Cost of Patient Visits
What is time-driven activity based cost accounting and how does it help your practice understand the cost of seeing a patient?
One of my favorite questions to ask is “how much does it cost to see a patient?” I know it's a generic question, but it is a starting point for today’s medical practice. Understanding the cost of doing business is essential with value based and other payment models emerging.
The simple way to start is to identify total visits (all E&M codes) for a period and divide by total expenses (typically without the physician). If you have 6,250 annual visits as a solo provider and your total costs are $365,761, the cost per visit is $58.52. You can then decide to break this down further for new patients vs. established patients. Or you could chose to identify costs per total relative value unit, tRVU.
There are other options as well. Eventually you will want to break the cost idea into smaller, workable parts.
One of the most interesting approaches is to identify how much it costs for each category of care provided in the patient visit cycle (e.g., check in, triage, provider time, follow up, and check out). You can look at the cost associated with the triage area: Vital signs, questions on prescriptions, documentation for the visit, and the like. Let’s assume that it takes 10 minutes for this to occur.
If you are paying the medical assistant $15.00 an hour and there is a $2.00 additional cost per hour for benefits, the total cost per minute needs to be calculated. At 2,080 hours worked per year, the total cost at $17.00 per hour would be $35,360. The total minutes worked would be $124,800. The cost per minute is $0.28. The cost for triage is $2.80 just for time. Add in the direct cost for supplies and allocate costs for space and equipment, and it adds up. If this process is done for each category of service in the cycle you gain a better understanding of the cost for the visit. Once this is understood, you can begin to ask if there are activities done at the time by the right individual and is it worth the cost of doing that activity. Further, is it best to do that activity at that time.
This approach is called time-driven activity based cost accounting (TBABC). It may seem like a lot of work but in our experience an exercise of this nature creates an awareness that results in improving the management of the patient visit cycle. The improved management of that flow produces several options for management to consider.
First, the support is more efficient for the provider which allows the provider to spend more valuable time with the patient, either relationship building or specific to the treatment plan development. More efficiency may lead to seeing one additional patient per day for that provider, which will net at current Medicare rates additional income of ~$18,000 with very little expense. Better control of staff time leads to reduction in overtime. Better control of all times contributes to all getting out of the office on time, which leads to a better work-life balance.
Step one is to accept that there is a need to understand the cost of providing service to the patient. Once a basic understanding is arrived at, taking a page for other industries, utilizing TDABC, as initially complex as it may seem is an effort that produces some important results.
17 inches: Health care lessons from a college baseball coach
You can't keep widening the plate.

Asset Protection and Financial Planning
Asset protection attorney and regular Physicians Practice contributor Ike Devji and Anthony Williams, an investment advisor representative and the founder and president of Mosaic Financial Associates, discuss the impact of COVID-19 on high-earner assets and financial planning, impending tax changes, common asset protection and wealth preservation mistakes high earners make, and more.

Physician flexibility: Bamboo or oak?
How we cope with adversity will ultimately determine our mental and physical health.

Avoiding Claims Denials in Your Practice
Physicians Practice® spoke with Terry Blessing III, Senior Vice President of Client Development at VisiQuate, about how practices can work to reduce the likelihood of encountering denied claims.

Patients share the blame
Patients aren't blameless in the current state of health care in America.

Medical practice valuations
Historically, valuations were largely considered the total earnings of the owner, whereas investors focus on the profits of the business as a basis for valuation.
2 Commerce Drive Cranbury, NJ 08512
609-716-7777


The 3 Metrics You Must Measure If You Want To Achieve Massive Growth In Your Practice
by Dr Matt | Apr 8, 2013 | Business | 1 comment

We all know the importance of getting check ups. As practitioners we are always encouraging our patients to come in for their regular check ups, whether it be for their spine, brain or other body systems.
How often do we do check ups on our business to see how successful it is? If your business is in a steep decline this will often be apparent through falling patient numbers and revenue.
But if the decline is gradual you may not see the warning signs until it is too late. Taking some time to give your business a check up will help you catch and correct deficiencies before they become major problems. The good news is that the check up need not be painful and onerous. Some simple calculations can give you the information you need.
Likewise, doing a health check on your practice is important even if it is doing well. While you may be doing things right, you may be able to find areas that could be improved to make your business even better.
So how do you go about doing a health check on your practice?
Firstly decide what period of time you are going to do your check-up over. I would suggest doing a monthly checkup to start with. If you keep these figures you can chart any change in your practice over time. If this is your first time, do monthly calculations for the last 6 months (or longer or shorter as you desire).
Secondly you need some numbers. These numbers are your practices “vital signs”. You should be able to get these easily from your practice management software. If not, consider our Icon Practice software ( for more details click here ). They are the raw numbers, in this case, for the last month. If you are doing this for the first time, get monthly totals for the last six months.
The numbers you want are:
- Total new patients visits,
- Total patient visits (including new patient visits),
- Total revenue (also called income), with and without stock sales if possible.
These raw numbers alone can give you some good information. Generally more new patients and more patient visits is a good thing. Like wise more revenue is a good thing also.
You can do some things with these numbers though to give you a window into the efficiency of your practice.
How well are you retaining your patients?
We all know that patients who fail to complete their course of care are more likely to have a poorer outcome than those who do complete. Those who have been in practice for some time will also know that patients often have other priorities, often financial, that discourage them from completing care. Your patient retention is a measure of how well you educate your patients of the importance of continuing their care.
What you need is an easy way to measure you patient retention. This is done with a simple statistic called the patient visit average (PVA). To calculate your PVA, take the total number of patient visits including new patient visits over the period you are measuring and divide it by the number of new patient visits for the period you are measuring.
PVA = Total visits/New patient visits
This tells you how many visits on average your patients have in your practice. The older your practice, the higher this figure will tend to be, as you have patients having maintenance care, and patients returning after a break in their care.
For people practising physical treatments such as chiropractors, myotherapists, osteopaths and physiotherapists, a PVA between 1 and 3 is very poor, and you can be sure your patients are not getting the most from their care. 4-6 is poor and could be improved. 6-8 is probably average. 8-12 is good, and above 12 is good number for your patients. This takes into account that patients don’t just need symptoms relief, but also rehabilitative care to support their system through ligament and soft tissue remodelling.
How much does a patient visit bring into the practice?
You might be inclined to simply quote the value you charge for your consultation as your revenue for each visit. However this doesn’t take into account concession and no-charge visits, or stock sales. If you calculate how much you actually make per visit, you might be in for a nasty, or pleasant, surprise.
The average visit value (AVV), will tell you the revenue that you bring in for each visit on average. To calculate it, take the total revenue for the period and divide it by the total visits for the period. You can either use the revenue figure with and without stock.
AVV = Total revenue/Total visits
An AVV (excl stock) that is way below your consultation charge indicates that you are providing a lot of discounted consultations. You may need to revise your discounts policy. Alternatively, a figure higher than your average consultation may indicate that your PVA is too low. Check the PVA for confirmation.
The AVV (incl stock) compared to AVV (excl stock) can give you an insight into how well you are marketing your stock. If the two figures are close, then you are not selling much stock to your patients, and vice versa.
Your total average patient revenue.
Having worked out your average visit value and your patient visit average, you can now easily calculate the total patient revenue (TPR). This is how much an average patient brings into the practice over their lifetime.
This figure is important as you can use it to work out how much you can spend to acquire a new patient. In theory as long as you are bringing in more per patient than you are spending to acquire one, then you are on a winner. In truth it is more complex than this, however it give you an idea of how you are doing.
To calculate the TPR multiply the patient visit average by the average visit value.
TPR = PVA x AVV
Combining and interpreting the information.
With these 3 basic calculations we have taken your raw practice figures and used them to give you a deeper insight into how well your practice is running.
Your patient visit average gives you an insight into how well you are educating your patients about the importance of their care. Low figures may indicate you need to spend some time improving the skills of yourself or your staff on patient education. Or focus on improving your office procedures to ensure patients don’t slip through the cracks and drop out of care.
You average visit value lets you know what you are actually earning on average for a patient visit, and can give you insight into how well your are marketing any stock you sell in your practice. It may also indicate a need to look at your discounts policy.
Finally, the total patient revenue is the amount each patient will spend in the practice on average. You can use it to guide your marketing decisions by telling you how much you can spend to acquire a patient. In some marketing circles this is referred to as the Life Time Value (LTV) of a client.
I would recommend calculating this information monthly and recording the results so you can chart the information. Over time you would like to see all of these figures increasing. Decreasing figures are a cause for concern and indicate a need to reassess you office procedures, and possibly seek outside help.
Our Icon Practice software can provide you with these figures over whatever period you set with a few clicks of the mouse. Click here for more information and to start your free trial.
Related Posts
Making the right decision in your practice can be a daunting task. Our new infographic…

The biggest challenge that we find when we are working with clients is motivating the…

Besides referrals, online marketing is one of the best ways to attract new patients. However…
Great information!!
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
More Patients More Revenue More Often

Take advantage of the new patient opportunities that exist for your practice.

Want More Useful Tips, Trick and Advice on How to Market Your Practice Online?
Head over to Practice Unleashed, our online community and training centre. For a small monthly fee you can get access to the latest news, how to courses and ask our advice on your marketing systems. You can even try some courses for free.

- Register Now
How to Measure Your Practice
If you have ever been to a sporting event and have arrived after the contest has started, one of the first questions most people ask is, “What’s the score? Who’s winning?”
It’s natural to find out “what the score is?” But. have you ever asked this question in your practice? “What’s the score? How are we doing?” I’m talking about taking an objective look at your practice not an emotional, intuitive evaluation although those can be helpful.
To many times after a sporting contest you hear, “We played great, but we lost.” Those sentiments may be true but the final outcome is what shows up in the wins and loss column.
Objectively, you can learn a lot from the score and the statistics from the game to show you how you performed in certain areas and what needs to be done to improve the performance so that next time a win is recorded.
Would you agree that when you drive a car it is helpful to look at the dashboard as part of your driving procedure? You can see how fast you are going, how much gas is left, the RPM’s of the engine, the temperature of the engine, the direction you are going, how many miles are on the car and other items such as warning lights and controls that help you on your journey.
Your practice has a dashboard that provides you information and directs you as to what questions need to be asked to make sense of the data and “what the score is.”
This dashboard provides numbers as to how your practice is performing. Common statistics to track include: Number of office visits, New Patients, Collections, and Services over a certain time periods. You can track many more statistics but for the purpose of this article we will use these as the foundation. These are the most important numbers to look at as they can give you a ‘snapshot’ of your practice or “what’s the score?”
These numbers can be daily, weekly, monthly, quarterly or yearly for comparison. Of course comparing year to year also shows your trends, up or down.
Tracking these numbers allows you to take a temperature of your practice to see how it is doing.
With these statistics you can perform some calculations to see how you are doing and see how you are trending. Mostly it provides you a framework as to what questions you need to ask about your practice.
- OFFICE VISITS – Office visits are how many people came in for services.
- NEW PATIENTS – New Patients are people who are new to your practice.
- COLLECTIONS – Collections are what you bring into the practice as income whether across the desk in cash, check or credit card, or in the mail or automatically deposited in your account from third party or private payers.
- SERVICES – Services are the dollar amount charged for services rendered.
- With these numbers you can perform some simple calculations to mine out more information. The easiest are services per visit and collections per visit. You take the amount of services for a given period and divide that number by the number of office visits giving you the average service per visit.
- SERVICES DOLLAR AMOUNT/ AMOUNT OF VISITS = Services per visit
- AMOUNT OF VISITS
- The same with collection’s, take the total collections and divide by the total number of visits for the same period and you will see your average collection per visit.
- COLLECTION DOLLAR AMOUNT/AMOUNT OF VISITS = Collections per visit
This is important as you can compare the collection per visit to the services. If you had a 100% cash practice, theoretically the collections and services should be the same, providing patients are not running balances. If there is a vast difference you must ask why? Perhaps there are lots of write offs due to contracted rates. You may have a significant amount of personal injury or workers compensation cases and that money will come later. The question you must ask and know is how much of the services do you expect to collect? This statistic allows you to formulate the right questions and get the right answers.
With these four statistics you can also calculate some indicators of performance. The first is called patient visit average (PVA). You take the total number of office visits for a period and divide that number by the amount of new patients for the same period.
AMOUNT OF VISITS/NEW PATIENTS = Patient Visit Average
Theoretically it is the average amount of patient visits a new patient will receive over their lifetime. This number is misleading but does provide a number or indicator of effectiveness and what type of practice do you really have. Is it a pain relief practice primarily or a wellness practice.
The number gives you an indicator of effectiveness. If you are great at obtaining new patients but they are not staying, it give you a reason to ask why and to look at your communication, your procedures and your experience you are providing patients.
The last calculation can also give you an indicator of your effectiveness and it’s called case average. You take the amount of collections over a given period and divide by the number of new patients.
AMOUNT OF COLLECTIONS/NEW PATIENTS = Case Average
This will give you an average of how much each new patient is worth over their lifetime. Once again it is misleading but gives you and indicator that you can compare. If each year your case average goes up as it should you can compare each year to the previous to see trends and of course ask questions.
These simple statistical indicators give you a snap shot of your practice. This is a starting point and not the end-all. There are other things you can look at that can be very helpful such as cost-per-visit. You take your total overhead for a period and divide that amount by the number of office visits.
TOTAL PRACTICE OVERHEAD/TOTAL OFFICE VISITS = Cost per visit
This will tell you how much your overhead is for someone to walk through your door as a patient. [quote_right]This is a powerful number as you know how much it cost you when you give away care and when you compare it to your collections per visit. [/quote_right]
Anything worthwhile is worth tracking. You can take your collections and break them down. How much is cash? How much is insurance checks? How much is personal injury or workers comp? You can even take insurance and break it down to PPO and HMO.
Statistics tell you how you are performing. They tell you what questions to ask and where to look. They can give you indicators for predicting what resources are needed in the future. They can help you evaluate to see if your practice is working or not and what areas need attention.
It is essential and practical to keep track of your practice performance. Anything you do in practice is worth tracking and evaluating. Remember, record breakers are record keepers.
This article is from the soon to be released book, The Hole In Your Practice. Learn from the greatest practitioner in the world and the habits they cultivate each and every day.
Go to: www.holeinyourdiploma.com
There you can download the Hole In Your Diploma Book for FREE and sign up for the FREE mentor ship program where successful chiropractors will share their journey from chiropractic college to new in practice to successful practice and what keeps their passion fueled today. Yes there is a hole in your diploma and a hole in your practice and the good news is it can be fixed.
RELATED ARTICLES MORE FROM AUTHOR

The Top Chiropractic Podcasts Every Chiropractor Should Be Listening To In 2019

ChiroLux Plus Portable Table (Unboxing & REVIEW)

Chiropractic Care Is Contributing Toward A 50 Percent Reduction In Opioid Prescriptions Issued In The United States According to Yale Study

InShot Mobile Video App Review

Vertebral Subluxation: Where do you stand?

Core Values, Purpose and Your Mindset with Dr. Matt Hubbard

- Medical Insurance Billing
- Radiation Oncology Medical Billing
- Dermatology Insurance Billing
- Gastroenterology Insurance Billing
- Holistic Billing Services
- Medical Billing
- Dermatology
- Gastroenterology
- Radiation Oncology
- Acupuncture
- 800-959-1906
What Is the Lifetime Value of a Patient? (+ Why It Matters To Your Medical Practice)
December 21, 2021 by Antonio Arias, MBA, CHBME
Topics: Revenue Cycle Management , Practice Management
Do you know how much your patients are individually, or as a whole, contributing to your revenue cycle ? On the other hand, are you aware of how much your medical practice is spending to retain or acquire patients? Both the financial input and output for each patient can provide insight into your medical practice’s bottom line and help you gain a better understanding of your practice’s relationship with your patients. Keep reading to learn how to calculate the lifetime value of a patient, and why it matters to your practice.
Quick Links:
What is patient lifetime value, why is patient lifetime value important to your medical practice, how to calculate the lifetime value of a patient.
- 3 Tips for Improving Lifetime Value of a Patient (and Keeping It High)
As the name might suggest, patient lifetime value (PLV) is the total worth of a patient to a medical practice over the course of their relationship. Sometimes referred to as customer lifetime value, or CLV for short, this metric reveals how much it costs your practice to acquire new patients and how much it costs to retain existing patients. Understanding—and increasing—the patient lifetime value of current patients can be a beneficial avenue to drive growth at your medical practice .
Patient lifetime value is vital to your medical practice because it helps you understand your marketing scope and secure your financial future. When you’ve established what the lifetime value of a patient is at your medical practice, you’ll have a solid idea of how much you want to spend on that relationship—hint, you don’t want to spend more than they’re contributing to your revenue cycle.
Knowing the lifetime patient value at your medical practice is also necessary for evaluating the status of your bottom line. Your patients are the whole reason your medical practice exists, so it’s essential to know and anticipate how much revenue they generate at your medical practice while you’re serving them.
Once you’ve calculated the patient’s lifetime value for your medical practice, you can use that information to further enhance the patient’s relationship with your office; for example, the CLV metric can help you:
- Refine your marketing strategy by understanding which types of patients are most valuable to you; with this information, you can emphasize patient acquisition strategies that target your best patients
- Boost loyalty in new patients and retain current ones by investing in your practice’s most valuable patients with the insight gained from calculating their CLV
- Learn which touchpoints in the patient’s journey get the most engagement and grow your medical practice upon expanding those channels or develop new propositions
Leveraging your patients’ lifetime values can help you deliver a better patient experience and result in a stronger relationship with your patients.

In order to calculate the lifetime value of a patient at your medical practice, you’ll need three pieces of information:
- Average visit value of the patient: This is the total value of all patient visits over a period of time (for example, one year), divided by the number of visits in that period
- Average visit frequency: To gather this figure, divide the number of visits to your medical practice in that same time period (one year) by the number of individual patients over the same period
- Patient value: You’ll calculate the average practice visit frequency multiplied by the average visit value
- Average patient lifespan: What is the average length of time a patient continues seeing you?
PLV = patient value X average patient lifespan
The resulting answer reveals how much you can reasonably expect the average patient to spend at your medical practice over the course of their relationship to your practice .
3 Tips for Improving Lifetime Value of a Patient (+ Keeping It High)
Ready to boost the lifetime value of your patients? Try the following tips:
1. Utilize Patient Satisfaction Surveys
Your medical practice wouldn’t exist without patients, whether new or returning. Do you know how they perceive your medical practice? Of course you’re delivering high quality care, but what if there are some inconveniences to the patient that could be easily resolved but which you don’t know about? Utilizing patient satisfaction surveys can help you measure the impact of your medical practice on the members of your community.
By gathering and considering patient feedback and then implementing new initiatives at your practice, you demonstrate how much value you put into your patients. If a patient notes that the scheduling system could be better streamlined, then adding some grease to that wheel would illustrate that your practice listens to the needs of patients and you’ll build loyalty in the relationship.
2. Boost Patient Engagement
When patients are more engaged with your medical practice—and, in turn, their own medical health journey—they’re more likely to stay with you instead of finding another practice that they feel might better serve them. One way to boost patient engagement is to develop and disseminate patient education resources .
These types of material are vital to a well-rounded practice that values its relationship with the patient because they help inform and empower the patient. When a patient is given literature from their trusted provider, the patient learns more about their diagnosis, condition, treatment plan, and furthers their own understanding. Further, they can use this information to do more research, if needed. This can lead to a healthy dialogue between patient and provider and the patient feels valued by the medical practice.

3. Partner with a Medical Billing Firm
When you let a team of qualified medical billing experts handle your medical billing and coding, you remove a significant frustration from your daily operations. This lets you and your team get back to what matters most: addressing the specific needs of the patient and delivering the best care for them.
Turn to the experts at NCG Medical for medical billing, revenue cycle management, and more to streamline your practice and optimize your operations. Outsourcing your medical billing can tremendously improve your practice in terms of internal and external efficiency. A medical billing firm can equip your practice with 24/7 reporting via analytics, for example, or can act as an in-house electronic health records (EHR) expert. In doing so, the outsourcing service can help ensure that incentive program adherence doesn’t drag your team’s time away from patients.
With NCG Medical , you’ll gain a team of experts in your corner who can help navigate the worlds of medical billing, healthcare software, and more! Contact us today to learn how we can make your practice more efficient, enable better patient access, and ensure you give the most effective care.
Related Posts
What is a patient care policy (+ how to write one).
October 31, 2022
If you’ve never heard of a patient care policy before, then you might ask yourself if your medical practice needs another piece of business writing. The answer is yes, it’s a good ...
What Is a Hospitalist? (+ Medical Billing Tips for This Specialty)
July 26, 2022
While some areas of medicine aren’t apparent in their titles—such as a nephrologist, who deals with the study of kidneys—other areas give a better starting point for understanding ...
HIE Time: Why the Stock Market is Paying Attention to Medical Billing
June 27, 2017
No matter the makeup of your investment portfolio, most financial experts advise everyday investors against paying heed to the day-to-day whims of the stock market. (Whereas ...
Subscribe to Our Blog
Stay in-the-know on trends, best practices, and news affecting the medical billing industry!
- Our Products
- Speak with Techsperts
- 1402 Edgewater Drive • Suite 101
- Orlando, FL 32804
- [email protected]

The Drummond Certified™ certification seal is for software solutions which have been tested and certified for complete and modular electronic health records (EHR) testing under the Drummond Certified program.

Journal of Urgent Care Medicine
Practice Management
Understanding Your Cost Per Patient
Urgent message: Assessing the true cost per patient is key to determining which pricing model will generate the most revenue for an urgent care center.
JORDAN TODD RICE, MD A cost-per-patient analysis may not work for every urgent care center owner, but this article is intended to give JUCM readers the basic tools they need to understand the formulas. It can also serve as a baseline for discussions with urgent care center staff, executives, managers, clinicians, and owners.
The goal of the exercise is to help urgent care providers better understand key elements of patient costs so they can determine which pricing model will best serve their organizations, be they for-profit, nonprofit, a single urgent care center or a practice with multiple locations.
How do operators of urgent care centers truly break down the cost for providing care to a single patient for primary care, urgent care or Workers’ Compensation services?
- How can the operator of an urgent care center do a true cost/benefit analysis to find out if it makes sense to switch to a single payment from payors rather than traditional fee-for-service reimbursement?
- How can and will paperless and digital systems affect the answers to the previous two questions?
Overcoming Accounting Obstacles One of the biggest challenges in calculating cost per patient is getting information from an urgent care center’s accounting and practice management systems. This is the most difficult task because such systems are great for generating information about pricing and revenue but not set up to provide costs, unless the Relative Value Unit (RVU) option is switched on. Some providers thought that the advent of all-in-one systems and single databases combing practice management (billing, scheduling, claims follow-up, etc.) and an electronic medical record would make the task easy to accomplish. In fact, automation helps practices do better charge capture, speeds up patient visits (after the normal 3- to 6-month learning curve for the switch from paper to paperless) and may even automate coding. It does not, however, compute the true cost per patient.
The other obstacle is the accounting program. Virtually every transaction in every category can be seen in an urgent care practice’s Chart of Accounts, but calculating the cost of each transaction is not as easy as you might think. For example, if your practice has a 401 (k) plan or your employees pay a portion of their health insurance, is that a true “cost” that needs to be factored into the computation of average cost?
Finally, an urgent care practice must be able to differentiate types of payors and services. For example, if your practice is a hybrid that provides both primary care and urgent care services, payors typically pay the same amount regardless of the type of visit. The main differentiators for most states and payors are factors such as the type of provider (some payors discount a physician extender visit by as much as 15%), use of “s” codes for a particular facility (fee-for-service or global fee) and whether a service was rendered “after hours” compared with the hours of an average practice. All of these factors affect reimbursement and cost, assuming that physician extenders are paid less than MDs and DOs. Even the place of service can affect reimbursement, but it usually does not impact cost. The same is true for treating Workers’ Compensation cases or providing occupational medicine services. The reimbursement levels may be higher or lower than those for a non-work-related injury, but the cost should be relatively similar for treating a 10-cm laceration, an aggravated left ankle sprain, or carpal tunnel syndrome, which is now becoming more and more common outside of the workplace because of the advent of home computers, pads, tablets, and even smartphones.
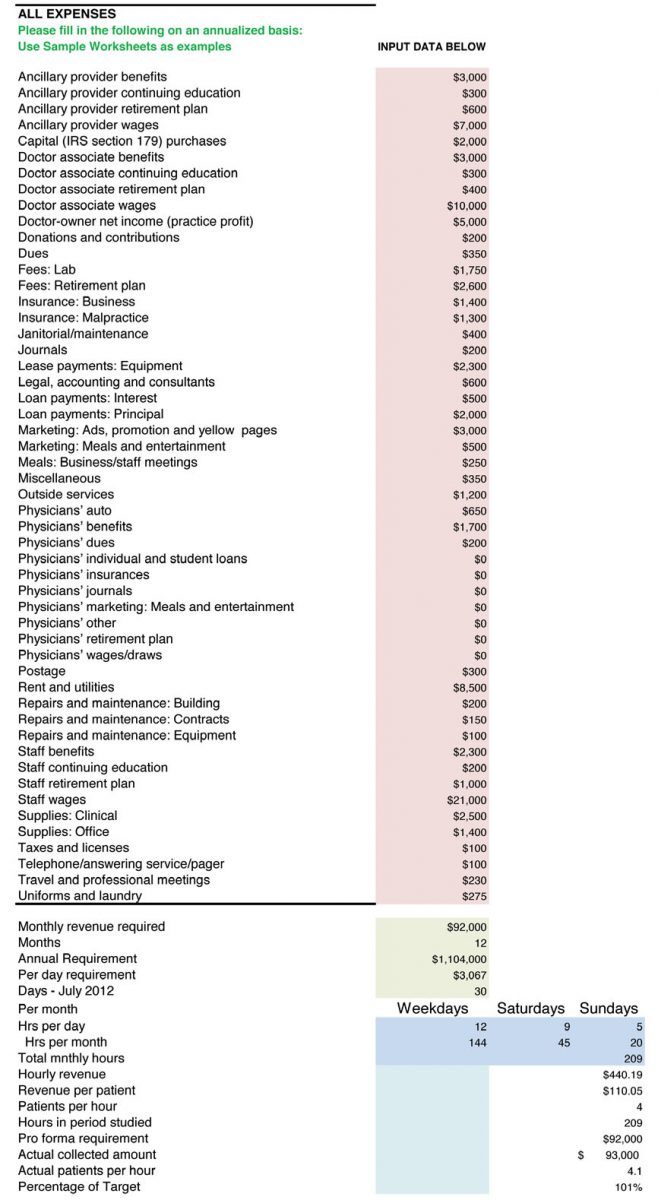
Thus we need to focus on cost only and in this case we will look across the board. Table 1 is a typical chart of accounts for an urgent care practice by category.
Your urgent care practice may have more or less accounts, but the ones listed are typical whether you have one office or 50.
For simplicity, let’s assume that for June 2011, the total for the accounts shown in Table 1 was $100,000. In a very unsophisticated model, we would simply take the number of patients for the month and divide that into $100,000 to get the cost per patient. If the practice saw 50 patients per day for 30 days in June, the total number of patients seen that month would have been 1,500. The cost per patient, then, would be $66.66 ($100,000 divided by 1,500). Net revenue of $120,000 from the 1,500 patients (understanding that most billings would be collected in June, some in July, and the remainder in August) would result in net profit of $20,000.
The collected amount per patient would be $80 and the profit per patient, in our simplistic model, would be $14.34. Continuing with our simplistic example, if a payor were to offer the practice a global fee of $90 per patient, which would typically encompass all services, including on-site laboratory, x-ray, electrocardiography (ECG), spirometry and most other patient costs, the practice would then receive a profit of $24.34 per patient. That is one reason that practices receiving global fees use digital technology for x-rays, ECG, and spirometry and send most laboratory work out to be processed. There are also savings to be had on the billing and collection side because global fees don’t get rejected, don’t have to be re-filed, and co-pays are received at the time of service, so there is little patient follow-up in terms of collections.
Real-World Complications Why, then, do simple cost-per-patient calculations not work in the real world? The factors involved are myriad, some which we’ve already discussed. One issue is how payroll is processed. In a traditional medical model, employees and clinicians are paid every 2 weeks. Some urgent care practices pay employees weekly, whereas others pay twice a month, and others even pay clinicians daily.
Clearly, when employees are paid every 2 weeks, there will be three pay periods in several months every year, which skews costs tremendously. Also, many insurance premiums are paid quarterly, semi-annually or even annually. That, too, affects month-to-month costs. Other factors include benefits payments, such as 401 (k) or retirement contributions, which may happen every pay period, monthly, or annually. Utility, water, sewer, and other costs also fluctuate from month to month. In Maine and Oregon, heating costs may sky rocket in mid-winter, whereas Arizona and Florida may have high cooling costs from mid-spring to mid-fall. Water and sewer costs tend to fluctuate less, but even they can go up and down. Therefore, it might make sense to do computations for your urgent care practice using quarterly, semi-annually, or even annual numbers.
If our model urgent care center has $1.2 million in true costs and 18,000 patients, the cost per patient would be the same: $66.66. But what if the center’s costs were actually $1.4 million and it had only 17,000 patients? Now the cost zooms to $82.35 per patient. Conversely, if the center only had $1 million in costs and 20,000 patients, the cost per patient would be only $50. Again, ANY additional revenues above this would be profits (or surplus for non-profit urgent care centers).
Now, let’s do some addition and subtraction from revenues for your urgent care center. Do you sell products for weight loss or durable medical equipment, or do your physicians dispense drugs? If so, those services usually are not paid by fee-for-services or global contracts. Laboratory services and x-rays typically are included in a global fee, but they usually are separate fees for a payor. Do you bill separately for them? The same question applies to Healthcare Common Procedure Coding System items, which are reimbursed and may be a “carve out” paid in addition to a global fee, depending on the individual contract. Cash-only services such as allergy testing, home sleep studies (elective), Holter or event monitoring are revenue. But their costs should be separated from the equation to compare fee-for-service and global fees and truly understand your actual cost per patient.
Understanding a Cost Benefit Analysis Spreadsheet Next, let’s look at how a cost benefit analysis spreadsheet works. A typical one that includes all costs is available in the Resources section of UCA’s Members Only portal, Uconnect (http://uconnect.ucaoa.org), and can be downloaded for free. A screenshot of what typical data entry looks like is shown in Figure 1.
Please note that annualized numbers were used in our example for the reasons we previously mentioned. There are too many expenses that are not paid on a monthly basis, and payroll can skew the numbers from month to month. What is key is to understand that each provider uses different resources, some of which are reimbursed and some are not. Once again, x-rays could be a profitable venture, but you have to understand the true cost of each x-ray. What is the cost of the unit? Is it leased or purchased? How much developer or fixer does it take if you use plain film for 100 or 1,000 x-rays? Is there a maintenance contract on the development unit? How about on the x-ray tube and collimator?
What cost benefit analysis does is permit the operator of an urgent care center operator to know the exact cost per x-ray, based on ALL costs against ALL revenues. In fact, I have worked with owners of urgent care centers who insisted they made money with a particular payor on a three-view ankle x-ray. But when we looked at all costs, including the cost for the room (rented or owned facility), personnel and over-reads if required, many times those x-rays were costing money not producing revenue. Even digital units have costs associated with them other than just the lease or amortized purchase price, such as the price of replacement cassettes, DVDs, maintenance, and replacement tubes.
The Impact of Variation in Reimbursement The hardest part of determining cost per patient is factoring into the equation varying reimbursements. Unless your urgent care center accepts cash only, you may be receiving 100 different reimbursements for a three-view ankle x-ray. Medicare, Medicaid, Indian Health Service, Tri-Care and some Federally Qualified Health Center fees are all under the Centers for Medicare & Medicaid Services (CMS) umbrella, but each will have a different reimbursement level. And even that number can be affected by the clinician on duty and whether that individual was a physician extender or a physician, for whom discounts of between 10% and 15% might apply. Figure 2 illustrates this computation, focusing on one insurance company.
For our example, we used fictitious numbers and a fictitious payor and chose an arbitrary reimbursement of $35 for a three-view ankle x-ray for Delta employee. From there, we included all costs involved with taking three x-rays. Note that we added every possible cost. Most are inputted as an annual cost and then we worked backward to the cost per x-ray. We can do this working off the annual number or the monthly number. The spreadsheet includes ALL costs for the facility and takes into consideration the total amount of space for x-rays, including the development room, x-ray storage, x-ray room, and operator area. If you pay for over-reads and they are not reimbursed separately or directly by a payor, then that needs to be included. We added all costs associated with the x-ray unit (assuming a lease, in this case), such as maintenance, fixer, developer, film, and any other direct costs. We also added in 15% (every center will be different) for billing and administration to collect and bill for the service. So, after looking at our sample $35 payment and subtracting these expenses, we came out with a profit of $1.64 per three-view ankle x-ray for this particular insurance company.
The same cost can be used when negotiating global fees. You simply need to look at the total number of x-rays you do for that particular payor over a period of time (1 year is safe) and interpolate the same costs minus some administration and billing, because they will be lower. If you receive a global fee of $150, for example, and one out of three patients has an x-ray and the average cost of that x-ray is $33.36, that equals a cost of $11.12 per patient under the global fee. This same calculation can be done for all payors and all x-rays your center offers and for which it bills. This is true of in-house laboratories.
A lot of work? Absolutely! There is no easy way to do a cost benefit analysis. It takes time and effort and requires a complete knowledge of true costs and actual reimbursements net of any write-offs, charge-offs, collection fees, and any other factors that will affect the actual cash that goes into the center’s bank account.
Understanding RBRVS Now we turn to Resource-Based Relative Value Units (RBRVS). Why are these helpful to your practice, if your practice management system allows you to use them? This is a neutral system used by CMS, HMOs, and many payors to determine how much money providers should be paid. All procedures (CPTs) are assigned a base value, which is influenced by three factors: physician work (52%), practice expense (44%), and malpractice expense (4%). The value for a particular CPT code is then further adjusted by a geographic factor because it clearly costs more to deliver services in New York and San Francisco than it would in small towns where there are no physician shortages. And finally, there is an annual conversion factor.
A debate about the issue of payment for effort-based medicine versus outcomes-based medicine is beyond the scope of this article. Reimbursement for urgent care services traditionally has been done based on our efforts and not the actual outcomes because urgent care providers usually do little follow up and are the largest referral source in all of medicine, save the emergency department. An argument can be made for reimbursing hybrid urgent care centers for outcomes-based medicine, but the focus of this article is understanding costs. And costs based on RBRVS can be a helpful indicator of what it should cost to provide a particular procedure coded via CPT for conditions from urinary tract infection, to ankle sprain, to upper respiratory infection.
Weighing Fee-for-Service Versus Global Fees Once you understand the cost per patient for your urgent care center, you can start evaluating whether fee-for-service is better than global fees on a payor-by-payor basis. In other words, the center will have to absorb the cost per x-ray, which will ONLY be affected on the global fee basis (because it is part of the global fee), but the actual cost per x-ray to the center should be a bit lower because there is less administration and the payment is stable from patient to patient. Yes, the comparison between fee-for-service and global fees is apples to organs, but in the end, the issue is which generates more profit or surplus (for non-profits). This article has not addressed hospital-based centers that have a facility fee and professional component, because a global fee for both typically is precluded by regulatory issues at the state and federal level. Physicians employed by a hospital-owned center may want to consider comparing global fees with fee for service. Again, such calculations can take a lot of time and one center may have a global fee with Medicaid but a fee-for-service arrangement with Blue Cross Blue Shield, for example. However, without calculating the true cost per patient, no urgent care center can be in a position to properly to make a case that an insurance company or CMS is underpaying for its providers’ services.
This primer offers basic tools for starting the process of identifying your urgent care center’s cost per patient. More information is available from the following resources to help providers further refine the process:
- http://www.sjsu.edu/faculty/watkins/cba.htm
- http://management.about.com/cs/money/a/CostBenefit.htm
- http://www.mindtools.com/pages/article/newTED_08.htm
- http://www.archives.gov/federal-register/publications/faqs.html
- http://www.physicianpractice.com/rvu/content/article/1462168/1867117
- ← High-Risk Conditions Presenting as Back Pain (Part 2)
- Atypical Appendicitis in the Older Patient →
- Clinical Feature Articles
- Case Reports
- Orthopedic Case Report
- Clinical Image Challenges
- Web Exclusive Images Challenges
- Abstracts in Urgent Care
- JUCM Webinars Archive
- Letters from the Editor-in-Chief
- From the UCA CEO
- Practice Management Articles
- Perspectives
- Occupational Medicine
- Revenue Cycle Management
- Developing Data
- Web Exclusive Articles
- Buyer’s Guide
- Author Bios
- Author Instructions
- Submit An Article
- Individual Articles
- Full Issue PDFs
Remember Me
Lost your password?
Username or E-mail:
Simplify Scheduling With This Patient Volume Calculator
Every physician walks a tightrope between scheduling enough patients to cover costs and overbooking to the point of burnout.
On one hand , running a medical practice is expensive. When you consider all of the various expenses related to running a medical practice—rent, insurance, employee salaries, software, equipment etc.—you understand why it’s imperative to get enough paying patients walking through your doors.
On the other hand , overbooking patients can very quickly lead to physicians feeling overworked and burned out, which is a serious problem. In 2017, 42 percent of physicians said they experienced burnout—and that number was the same for both self-employed physicians and physicians working at larger practices.
So the problem you face is one of balance:
Lean too far one way and you’ll be facing overwhelming costs and the threat of closing your practice.
Lean too far the other way and you’ll soon find yourself too tired to get through your days and serve your patients.
What you need is a tool to help you examine the specific details of your practice and financial needs, in order to determine exactly how many patients you need to see every day to walk that tightrope.
Fortunately, that’s exactly what you’ll find right here.
Understanding Elements of the Patient Load Equation
Now that you’ve seen the tool, you might be curious about the different elements that go into the equation.
The truth is, every physician’s ideal patient load is different because it depends on specific numbers that are unique to individual practices. Each of those numbers—which we’ll cover in-depth—all add up to one question: How much money do you need to bring in?
The three factors in the patient load equation are:
Practice Cost
Patient Value
Days Worked
How Much Does Your Practice Cost?
This is a broad element of the equation, but it’s the best place to start figuring out how much money you need to bring in. To find this number, add up any expense related to running your practice, including things such as:
Building costs, e.g., rent, utilities and property insurance.
Medical supplies and equipment (including software, such as EHRs or practice management systems).
Office supplies.
Salaries and benefits for you and your employees.
Liability insurance.
Essentially, what you need for this step is an annual expense report. Here’s an example:
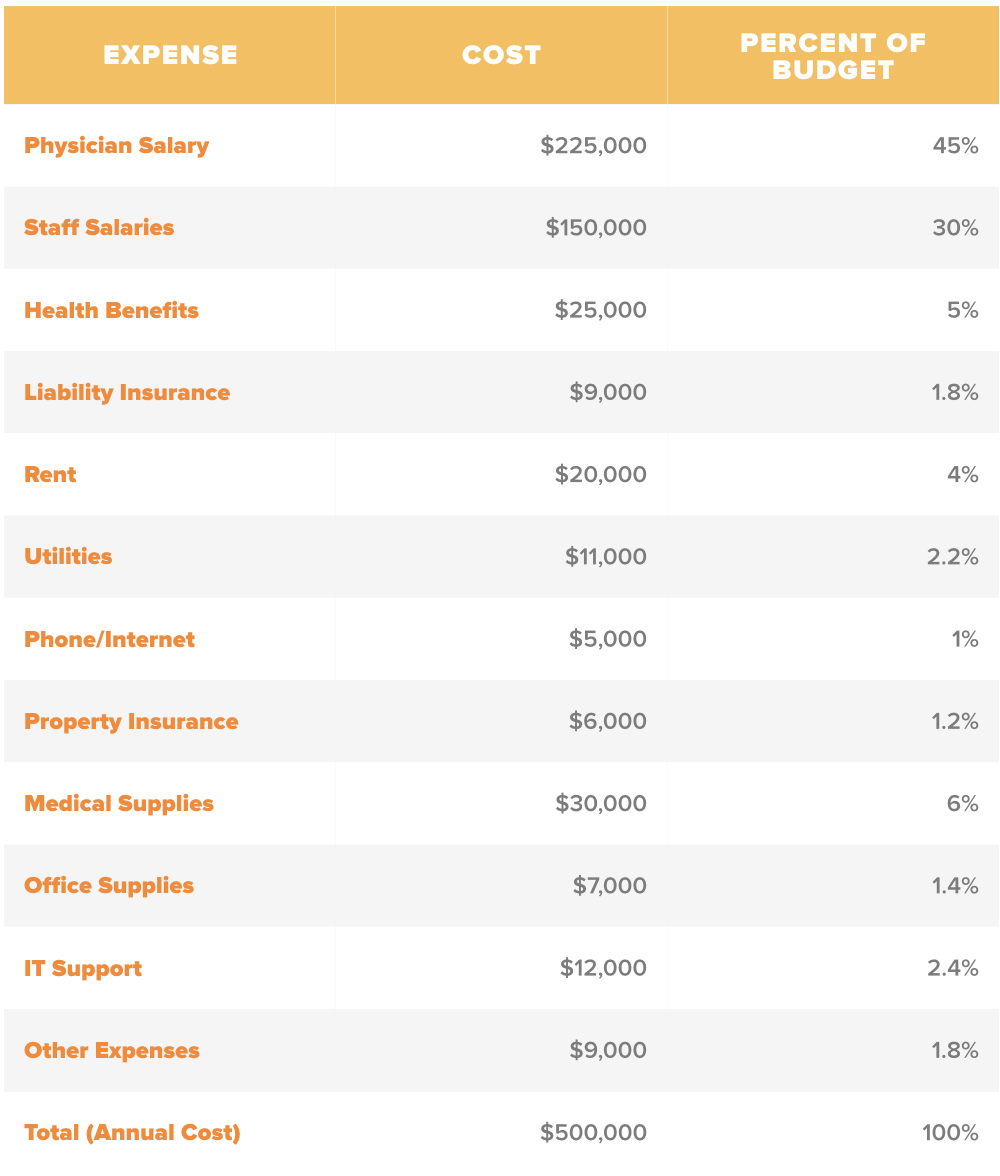
In the example expense report, the total cost of running this practice is (conveniently) $500,000. Yours could be (and in fact probably is) an entirely different number, but that’s OK. We’re just using this sample as an easy number to work with.
SOFTWARE HACK: This is a lot to tally up, but hopefully, you’re already using either a general business accounting system or a medical-specific accounting system —if not, you absolutely should be. With either of these systems, you can access a yearly expense report through your general ledger.That’ll tell you everything you need to know for this step of the patient load equation.
Once you find the grand total of all your business expenses, you’ll move on to the next part of the patient volume calculator.
How Much Does Each Appointment Bring In?
The next step is to figure out how much you bring in after every individual patient encounter. Because this varies depending on things like patient insurance coverage or treatments, it’s best to find an average amount instead of trying to pinpoint it exactly.
The process for finding this number will vary depending on the type of practice—specifically, inpatient versus outpatient.
For inpatient practices, you’ll want to find your net receivables for the year, then divide by the total number of appointments you saw in the same year.
So, let’s say our example physician from above had 10,000 patient encounters in 2017 and their total net receivables amounted to $1,000,000. Their revenue per patient encounter would be:
$1,000,000 / 10,000 patient encounters = $100 per patient encounter
For outpatient practices, you’re looking for the amount your practice billed for and collected, less any payer adjustments.
SOFTWARE HACK: If you’re using medical billing software , revenue cycle management software or a third-party biller, you should be able to find your average revenue per patient encounter fairly easily.
After that, there’s one more piece of information to collect.
How Much Do You Work in a Year?
Finally, in order to calculate your breakeven point and determine how many patients you need to see per day in order to make a certain amount of money, you have to know how many days you’re going to work.
This, just like every other aspect of this equation, differs widely from physician to physician. You’ll need to take into consideration the holidays on which your practice is closed, weekends, business trips (such as continuing education or conferences) and personal vacations.
SOFTWARE HACK: Using dedicated HR software with time and attendance tracking and payroll features will make defining paid time off and observed holidays easier for your employees. It will also help you keep track of how many days you worked so that you can easily find this factor of the equation whenever you need it.
For our example, let’s assume the physician takes weekends off and only observes Federal holidays. That means out of 365 days in a year, they’ll see patients on about 250 days.
Putting It All Together
So now that we know all three factors of the equation for our example physician, here’s what the calculation looks like:
Practice cost = $500,000
Patient value = $100
Days worked = 250
Step 1: Divide practice cost by the average amount of money each patient encounter brings in. This will tell you how many patients you need to see in a year.
$500,000 / $100 = 5,000 patients/year
Step 2: From there, use the number of days you’ll work in a year to determine how many patients you need to see every day.
5,000 / 250 = 20 patients/day
And viola! Now we know that our example physician needs to see at least 20 patients every day that they’re open in order to cover all of their business expenses.
Next Steps: How to Manage Your Patient Volume
Once you’ve answered the question of how many patients you should be seeing, you’ll be looking at one of three scenarios:
You’re seeing more patients than you need to
You’re not seeing enough patients to cover costs
You’re right on track
If you find yourself in category number one, you’re probably feeling overworked and overwhelmed. To help alleviate some of the stress of dealing with too many patients, we suggest you consider either a dedicated patient scheduling system or a broad-featured practice management solution . Both can help provide additional control over scheduling and communication so that your patients arrive more prepared and your appointments go by quicker.
If you find yourself in category number two, you have two options.
You can cut costs in order to stay within your budget. Medical accounting software can provide more insight and control over your expenses should you decide to go that route.
You can try to attract more patients to your practice. A customer relationship management (CRM) system that’s specific to the medical industry is a great way to go. Also, tools such as patient engagement software and patient portals can help improve existing patient experiences, which could result in a better online reputation for your practice and an influx of new patients.
If you find yourself in category number three , you’re doing great—don’t change a thing! Unless, of course, you want to grow your practice or streamline your processes. In which case, you may find our Medical Needs Cycle particularly helpful.
And of course, if you have any other questions about medical software to help your practice thrive, you can reach out to our team of advisors for customized recommendations to fit your exact needs.
- Skip to main content
- Skip to primary sidebar
- Skip to footer
Savvy Calculator
Savvy Calculator is a free online tool of calculations.
Cost Per Visit Calculator
About cost per visit calculator (formula).
The Cost Per Visit Calculator is a tool used to calculate the cost per visit based on the total cost and the number of visits. It provides a straightforward way to determine the average cost incurred per visit, allowing individuals or organizations to analyze and manage their expenses effectively.
The Cost Per Visit (CPV) is calculated using the following formula:
CPV = Total Cost / Number of Visits
- Total Cost represents the overall cost incurred.
- Number of Visits represents the total number of visits made.
Explanation: The formula divides the total cost by the number of visits to obtain the average cost per visit. By calculating the CPV, individuals or organizations can gain insights into the financial implications of each visit.
For example, if the total cost is $1,000 and there have been 50 visits, the calculation would be as follows:
CPV = $1,000 / 50 = $20
This means that the average cost per visit is $20. It provides a clear understanding of the expenses incurred on average during each visit.
The Cost Per Visit Calculator is a valuable tool for financial analysis and decision-making. It allows individuals or organizations to evaluate the financial feasibility of their operations, budget effectively, and compare costs across different periods or activities.
By using the calculator, users can easily input the total cost and the number of visits to obtain the cost per visit. This information can be useful in various scenarios, such as healthcare institutions assessing the average cost of patient visits or businesses evaluating the average expenses incurred per customer interaction.
Overall, the Cost Per Visit Calculator simplifies the process of determining the average cost per visit, enabling individuals and organizations to monitor and manage their expenses efficiently, make informed financial decisions, and optimize resource allocation.
- Privacy Policy
- Terms and Conditions
Patient Lifetime Value Calculator
What is patient lifetime value.

How is PLV Used for the Valuation of Marketing Campaigns?
Marketing campaigns can end up costing a lot of money, especially if you don’t set a budget or understand the true cost of acquiring patients for your practice. Not every lead turns into a new patient, and some leads aren’t meant to become patients. In these cases, it’s better to cut your losses early instead of spending more trying to convince a new patient when they aren’t committed to your practice in the first place.
Using the PLV formula above shows you the average financial outcomes of a lead. Some patients will earn you more, and some will earn less. But for those that earn more, you can mitigate the costs of those that earn less. In fact, the quality of the lead will affect the financial outcome. We can usually put patients in one of these categories:
Positives – With inbound marketing, such as Google Ads and SEO, you typically have a higher quality of lead. These are patients that come to you, so you know they’re highly interested in visiting your practice.
Negatives – When you spend a lot of time or money trying to acquire a new lead, you may end up spending more than what you’ll see returned when the patient finally visits your practice. This is more common with lead generation campaigns, mailers, and in-person events.
We offer a free calculator that can help you quickly and easily determine the Patient Lifetime Value for your practice. All you have to do is enter in the average value for each line:
First-Time Patient Visit Revenue – How much do you earn from the first time a patient visits your practice?
Recurring Visit Revenue – How much do you earn from every subsequent visit for that patient?
Average Visits per Year – How many times will that patient visit you in one year?
Average Number of Years – How many years will that patient visit your practice?
The calculator will then work the formula for you to determine your individual Patient Lifetime Value. You can run this calculator as many times as you like to find the PLV for all the different services you offer or the types of patients you encounter at your practice.
Marketing Done Right is a leading digital marketing agency located in Cleveland, Ohio. We work with medical practices of all kinds throughout the United States to bring in new patients and turn them into lifelong visitors. Please contact us today to learn more about our services. If you’d like a free local marketing audit, please do so below:
- Privacy Policy
- Terms & Conditions
- Cookie Policy

Knowing how your services are valued is key to understanding and improving your productivity.
ANNE C. KANTNER, MD, FAAP, FACP
Fam Pract Manag. 2023;30(2):4-8
Author disclosure: no relevant financial relationships.

Although the use of value-based payment models is growing, 1 the most common payment method in physicians' employment contracts is still a base salary plus a production bonus based largely on relative value units (RVUs). 2 RVUs reflect a physician's volume of work and level of effort in treating patients. The more RVUs a physician generates, the more income the practice (and the physician) should receive.
Knowing the RVUs assigned to different types of services allows physicians to understand how their productivity is measured. And knowing their RVUs per visit and per year allows physicians to understand how they compare to their peers. They can then assess whether they need to see more patients, work more efficiently, or change key processes such as billing and coding to better reflect the amount of work they are doing.
The four questions outlined in this article can help physicians get started in understanding and improving their RVUs.
Knowing the work RVUs assigned to different types of services can help you understand how your productivity is being measured.
Work RVUs vary depending on the work and effort required; for example, a 99212 has 0.70 work RVUs while a 99214 has 1.92 work RVUs.
To improve your total work RVUs per year, you may need to work more efficiently so you can see more patients, improve your coding practices to capture the full value of your work, or offer more high-value services, such as procedures or transitional care management.
1. WHAT ARE RVUS?
RVUs are part of the Resource-Based Relative Value Scale (RBRVS), which Medicare and other payers have used for decades to determine payment for physician services. RVUs are just one of three components that factor into the payment calculation. 3 The other two components are geographic practice cost indices (GPCIs), which adjust RVUs to reflect regional differences in the cost of physician services, and a conversion factor (CF), which is the dollar amount by which total, geographically adjusted RVUs are multiplied to arrive at the payment amount for a given service. (See “ How payment for a service is calculated. ”)
Total RVUs are the sum of three types:
Work RVUs , which reflect the physician's work, including mental effort, decision making, technical skills, physical effort, stress related to patient risk, and amount of time spent,
Practice expense RVUs , which reflect the clinical and nonclinical labor costs and practice expenses,
Malpractice RVUs , which reflect the liability insurance costs.
The remainder of this article will focus on work RVUs because they are a key measure of physician productivity. Work RVUs for common services in primary care are listed at the end of this article. For example, a 99214 established patient evaluation and management (E/M) office visit has 1.92 work RVUs, a “Welcome to Medicare” visit has 2.6 work RVUs, and a 99223 initial hospital visit (admission) has 3.5 work RVUs.
HOW PAYMENT FOR A SERVICE IS CALCULATED
Relative value units (RVUs) are just one of three components that factor into physician payment under the Resource-Based Relative Value Scale:
Total RVUs , which is the sum of work RVUs, practice expense (PE) RVUs, and malpractice RVUs,
Geographic practice cost indices (GPCIs), which adjust RVUs to reflect regional differences in the cost of physician services,
A conversion factor (CF), which is the annually updated dollar amount by which total, geographically adjusted RVUs are multiplied to arrive at the payment amount for a given service.
Payments are calculated as follows:
[(Work RVUs x Work GPCI) + (PE RVUs x PE GPCI) + (Malpractice RVUs x Malpractice GPCI)] x CF = Payment amount
2. WHAT ARE YOUR WORK RVUS?
If you are an employed physician, you likely receive productivity reports from your employer, but you may not be in the habit of looking at them closely or you may not know what to do with the information. A helpful report should provide you with the following individualized data:
Annualized work RVUs (projected total if you continue to generate the same amount of work for the rest of the fiscal year),
Number of visits,
Annualized number of visits,
Types of visits you are seeing (such as preventive care visits, E/M visits, hospital visits, and Medicare wellness visits),
A breakdown of your E/M visits (i.e., what percentage are coded as level 1, 2, 3, 4, or 5).
If you are expected to meet a goal for work RVUs, you should receive your data on a regular and predictable basis — e.g., monthly, bimonthly, or quarterly — allowing you to analyze the data and make adjustments in scheduling, coding, or practice efficiency to meet the goal. Waiting until the end of the fiscal year to distribute a finalized report does not allow physicians enough time to make effective changes.
Data should be accurate, trustworthy, and presented to physicians in a user-friendly way. Practices should have a contact person who understands the information well and can answer physicians' questions or investigate discrepancies should they arise.
If your employer does not provide you with a productivity report, or does not provide it in a timely manner, ask for it. Most EHRs and practice management systems capture the required data and can generate customizable reports.
You can estimate your work RVUs on your own using the process described in the physician example .
HOW TO CALCULATE WORK RVUS PER VISIT AND PER YEAR: AN EXAMPLE
Dr. Smith is a family physician in a physician-owned outpatient practice. He sees an average of 10 patients per session, or 20 visits per day, and his average work RVUs are 1.69 per visit. Out of 260 total workdays per year, Dr. Smith has 40 days for vacation, continuing medical education, holidays, etc., leaving 220 workdays per year. That means he averages 4,400 visits and 7,436 work RVUs per year, which puts him well above the 50th percentile in national benchmarks but below the 90th percentile.
Here's the method used to estimate his work RVUs:
First, list the types of visits in an average session, assign work RVUs to each visit, and add the values to get the total work RVUs per session.
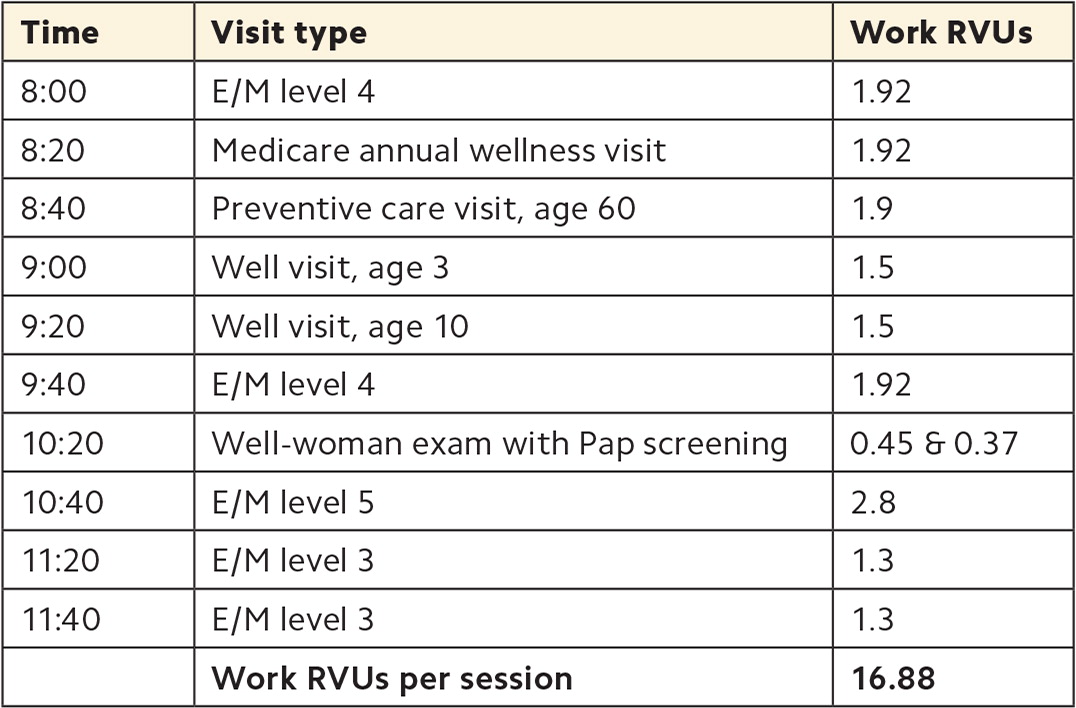
Next, complete the following calculations:
Work RVUs per session ÷ Visits per session = Work RVUs per visit
16.88 ÷ 10 = 1.69
Workdays per year x Visits per day = Visits per year
220 x 20 = 4,400
Visits per year x Work RVUs per visit = Work RVUs per year
4,400 x 1.69 = 7,436
3. HOW DO YOUR WORK RVUS COMPARE TO BENCHMARKS
Practices should establish work RVU benchmarks at the beginning of the fiscal year and include them in productivity reports so physicians can see whether they are meeting work RVU goals. Practices may use internal data to set benchmarks, comparing you to your peers, or they may rely on national benchmarks from external sources. Benchmarks should be specialty-specific, but they may differ for inpatient versus outpatient practice, new versus established physicians, and physician-owned practices versus practices owned by hospital or health systems.
For example, according to data from the Medical Group Management Association, for family medicine physicians in physician-owned outpatient practices, the 50th percentile is 5,945 annual work RVUs and the 90th percentile is 9,063. 4 Meanwhile, for those in hospital-owned or health-system-owned outpatient practice, the 50th percentile is 4,715 annual work RVUs and the 90th percentile is 7,451. One possible reason for the difference is that physician-owned practices may be more likely to reward productivity, while practices owned by a hospital or health system may be more likely to use straight salary compensation.
4. HOW CAN YOU INCREASE YOUR WORK RVUS?
If your work RVUs are below goal, there are several ways you may be able to increase them. Start by examining the following factors.
Visit volume . To assess whether low patient volume is contributing to low work RVUs, identify how many patients you see per day. A 2018 survey by the Physicians Foundation found an overall average of 20.2 patients per day across all specialties. 5 According to data from the American Academy of Family Physicians, family physicians average 84 patient encounters per week — 63 in the office, 12 e-visits, seven in the hospital, and two in nursing homes or house calls. 6 What ultimately matters is the benchmark your group is using. If your visit volume is too low, that does not necessarily mean that you need to work longer each day, but you may need to work more efficiently in order to see more patients. For example, you may need to delegate more tasks to your team, or you may need to address a high no-show rate.
Visit levels . Identify what percentage of your E/M visits are level 1 through 5, and compare this distribution to that of your peers. If your practice cannot provide this data, you can use national benchmarks derived from Centers for Medicare & Medicaid Services data (see this FPM worksheet , which has been updated with 2021 data). If you find that you are billing a higher percentage of lower-level visits than your peers, you will need to either see more patients to achieve the same overall work RVUs or investigate other issues. For example, it could be that your billing, coding, and documentation practices are inefficient, leading to under-coding or missed coding.
High-value visits . Identify which high-value visits you frequently provide, and which ones you should be providing. (See the list of work RVUs for different visit types on page 7 .) For example, new patient visits have higher work RVUs than established patient visits, so if you've closed your panel to new patients, this could be affecting your work RVUs. Many procedures are also valued highly, so you may want to consider expanding your scope of practice by adding skin procedures, joint aspirations and injections, treadmill stress tests, etc. Transitional care management visits and Medicare annual wellness visits are also higher-value services. Consider whether you can provide these to patients who need them, and how your care team can assist with the workload.
Visit lengths . Track your visit lengths for various visit types to see whether you need to adjust your scheduling practices. Adjusting visit duration in your scheduling template can allow you to see more patients per day or per session to meet your work RVU goals. For example, a physician who has a goal of 30 work RVUs per day and averages 1.3 work RVUs per visit (the equivalent of an established-patient, level 3 office visit) would need to see 23 patients per day. In an eight-hour workday, that would allow for an average of 20-minute visits. Note that time-based billing became easier following the 2021 E/M coding changes and now includes the physician's total time spent on the day of the visit (not only face-to-face time but also pre-visit planning, coordination of care after the visit, and other physician activities).
WORK RVUS FOR COMMON VISIT TYPES
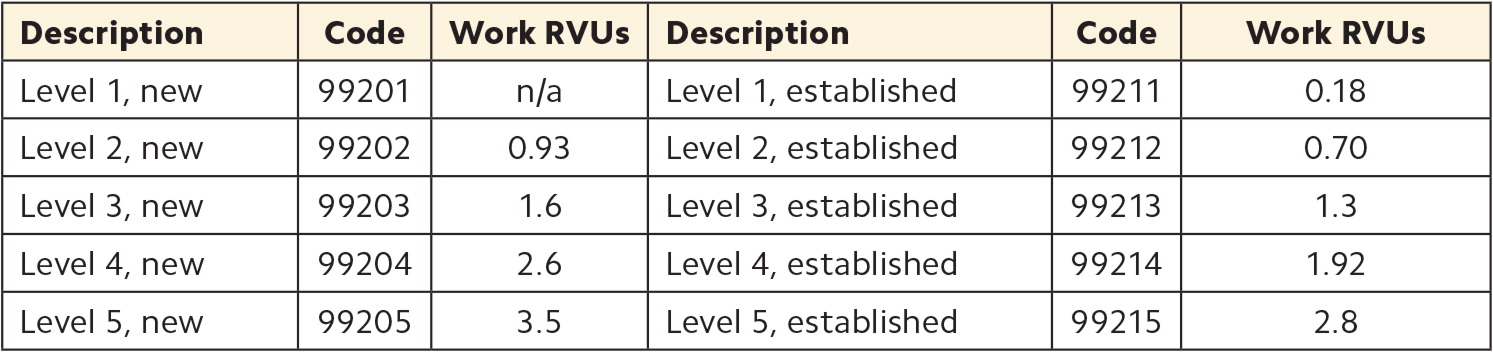
FOCUSING ON WHAT YOU CAN CONTROL
Some aspects of physician productivity are beyond your control. For example, you can't really control whether your schedule is full every day or what level of care your patients need. However, it's still beneficial to understand the factors that are affecting your work RVUs so you can assess your performance and make the case for what you need, such as more clinical support staff or a second exam room. Improving productivity isn't just about working harder, but working smarter and identifying changes in practice operations and efficiency that will actually make a difference.
Johnson K, Rittenhouse D. From volume to value: progress, rationale, and guiding principles. Fam Pract Manag . 2023;30(1):5-7.
Singleton T, Miller P. Employment and contract considerations for family physicians in the era of COVID-19. Fam Pract Manag . 2021;28(1):11-16.
What are relative value units? AAPC. Updated June 21, 2022. Accessed Jan. 27, 2023. https://www.aapc.com/practice-management/rvus.aspx
Medical Group Management Association. DataDive provider compensation: 2022 report based on 2021 data; 2022. https://www.mgma.com/data/data-reports/2022-mgma-data-dive-provider-comp-report
- 2018 survey of America's physicians. The Physicians Foundation and Merritt Hawkins. September 2018. Accessed Jan. 27, 2023. https://physiciansfoundation.org/physician-and-patient-surveys/the-physicians-foundation-2018-physician-survey
Slideshow: a week in the life of a family physician. FPM . 2020. Accessed Jan. 27, 2023. https://www.aafp.org/pubs/fpm/multimedia/slideshows/fp-hours-compensation.html
Continue Reading
More in FPM
More in pubmed.
Copyright © 2023 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

IMAGES
VIDEO
COMMENTS
Example of patient visit average (PVA) To put PVA numbers into perspective, it may help for us to illustrate an example within Dr. Smith's chiropractic clinic. You can work out the patient visit average, and know to set the right prices for your practice at ease. For example, Dr. Smith had 400 patients visit his clinic in the last month.
A Patient Visit Average is the average number of appointments a patient has with your clinic over a given period of time. It is the total number of appointments a practitioner (or clinic as a whole) sees divided by the amount of new clients within the same time period. PVA =. (total number of appointments)/ (number of new clients)
To calculate the cost of donated services, multiply the market value of the services by the allocation rate, and then divide by the number of units of service provided (e.g., $10,000 x .20 ÷ ...
For example, if you have the capacity to provide 5,280 visits per year and your panel visit rate is 2.5 visits per patient per year, then your right-sized panel is 2,112 patients — or 1,584 ...
If you have any questions, please call the Financial Counseling department at 844-498-2900. If your medical services are scheduled for a Tri-Valley location, please call 925-534-6457. Note: Our online Cost Estimator tool currently supports a limited number of health services that are mandated to meet regulatory requirements. Stanford Health ...
Average Revenue per Patient Visit is calculated by dividing the total revenue generated by the number of patient visits during a specific period. To calculate this metric, healthcare organizations need to track the total revenue generated from all sources, including insurance payments, patient payments, and other revenue streams.
To calculate your clinic's PVA, obtain patient data from the following two statistic reports: Clinic Statistics: a summary breakdown of total visits per practitioner; New Patients: a list of all new patient profiles created within a timeframe . PVA (Patient Visit Average) Total Visits / Total New Patients . Overview:
Determine your practice cost. This is the total dollar amount of all your practice's expenditures, including operating costs (e.g., rent, utilities, equipment, supplies, and fees) and employee salaries and benefits. Let's say your operating costs come to $300,000 and your salary costs total $200,000. Thus, your total practice cost is ...
If you have 6,250 annual visits as a solo provider and your total costs are $365,761, the cost per visit is $58.52. You can then decide to break this down further for new patients vs. established patients. Or you could chose to identify costs per total relative value unit, tRVU. There are other options as well.
Enter the Total Office Visits (OV's) during the last 12 months. Step 3 In order to get your CDA, divide the number on Step 1 by the number on Step 2. Your CVA is: How to calculate your Profit Per Patient Visit (PPV) Take your CVA above, and subtract your CDA. Your PPV is: Cost per Visit Calculation Name of Office: Name of Provider:
Cost per member or per patient, per month; Cost per clinician FTE; Cost per administrative staff person; Cost per patient per encounter/visit; Cost per accreditation standard or element; Another way to standardize results is to report them in standardized dollars (e.g., 2012 dollars).
To calculate your PVA, take the total number of patient visits including new patient visits over the period you are measuring and divide it by the number of new patient visits for the period you are measuring. PVA = Total visits/New patient visits. This tells you how many visits on average your patients have in your practice.
If you don't know how to calculate cost per patient visit, here's how to calculate it. Take your monthly overhead expense (excluding any personal expenses you run through your company such as car payments, etc.) and divide it by the number of office visits you see in a month. For example, if your monthly overhead runs $15,000 and you see ...
With these four statistics you can also calculate some indicators of performance. The first is called patient visit average (PVA). You take the total number of office visits for a period and divide that number by the amount of new patients for the same period. AMOUNT OF VISITS/NEW PATIENTS = Patient Visit Average.
Do you think that it could be improved? Imagine this - let's say your average reimbursement is $83/visit currently. What if with the correct direction and a strong billing team that number increased $3/visit to $86/visit? At face value that may not seem like much. But let's say you treat 150 visits/week. That would be an increase in ...
In order to calculate the lifetime value of a patient at your medical practice, you'll need three pieces of information: Average visit value of the patient: This is the total value of all patient visits over a period of time (for example, one year), divided by the number of visits in that period. Average visit frequency: To gather this figure ...
The cost per patient, then, would be $66.66 ($100,000 divided by 1,500). Net revenue of $120,000 from the 1,500 patients (understanding that most billings would be collected in June, some in July, and the remainder in August) would result in net profit of $20,000. The collected amount per patient would be $80 and the profit per patient, in our ...
Practice cost = $500,000. Patient value = $100. Days worked = 250. Step 1: Divide practice cost by the average amount of money each patient encounter brings in. This will tell you how many patients you need to see in a year. $500,000 / $100 = 5,000 patients/year.
By calculating the CPV, individuals or organizations can gain insights into the financial implications of each visit. For example, if the total cost is $1,000 and there have been 50 visits, the calculation would be as follows: CPV = $1,000 / 50 = $20. This means that the average cost per visit is $20. It provides a clear understanding of the ...
For example, a provider who sees 20 patients per day, 210 days per year, with an average of three visits per patient per year, could manage a panel of 1,400 patients. By increasing capacity to 25 ...
Average Number of Years - How many years will that patient visit your practice? The calculator will then work the formula for you to determine your individual Patient Lifetime Value. You can run this calculator as many times as you like to find the PLV for all the different services you offer or the types of patients you encounter at your ...
Annual Visit Plan. Hypertension, diabetes, and hyperlipidemia: once every six months with labs. Asthma and allergies: once a year. Physical exam: as needed, but at least once every two years ...
Next, complete the following calculations: Work RVUs per session ÷ Visits per session = Work RVUs per visit. 16.88 ÷ 10 = 1.69. Workdays per year x Visits per day = Visits per year. 220 x 20 ...