- Search Menu
- Sign in through your institution
- Advance Articles
- Editor's Choice
- Supplements
- Patient Perspectives
- Methods Corner
- Science for Patients
- Invited Commentaries
- ESC Content Collections
- Author Guidelines
- Instructions for reviewers
- Submission Site
- Why publish with EJCN?
- Open Access Options
- Self-Archiving Policy
- Read & Publish
- About European Journal of Cardiovascular Nursing
- About ACNAP
- About European Society of Cardiology
- ESC Publications
- Editorial Board
- Advertising & Corporate Services
- War in Ukraine
- Journals on Oxford Academic
- Books on Oxford Academic


Article Contents
Introduction, why patient journey mapping, how is patient journey mapping conducted, use of technology in patient journey mapping, future implications for patient journey mapping, conclusions.
- < Previous
Patient journey mapping: emerging methods for understanding and improving patient experiences of health systems and services
Lemma N Bulto and Ellen Davies Shared first authorship.
Conflict of interest: none declared.
- Article contents
- Figures & tables
- Supplementary Data
Lemma N Bulto, Ellen Davies, Janet Kelly, Jeroen M Hendriks, Patient journey mapping: emerging methods for understanding and improving patient experiences of health systems and services, European Journal of Cardiovascular Nursing , Volume 23, Issue 4, May 2024, Pages 429–433, https://doi.org/10.1093/eurjcn/zvae012
- Permissions Icon Permissions
Patient journey mapping is an emerging field of research that uses various methods to map and report evidence relating to patient experiences and interactions with healthcare providers, services, and systems. This research often involves the development of visual, narrative, and descriptive maps or tables, which describe patient journeys and transitions into, through, and out of health services. This methods corner paper presents an overview of how patient journey mapping has been conducted within the health sector, providing cardiovascular examples. It introduces six key steps for conducting patient journey mapping and describes the opportunities and benefits of using patient journey mapping and future implications of using this approach.
Acquire an understanding of patient journey mapping and the methods and steps employed.
Examine practical and clinical examples in which patient journey mapping has been adopted in cardiac care to explore the perspectives and experiences of patients, family members, and healthcare professionals.
Quality and safety guidelines in healthcare services are increasingly encouraging and mandating engagement of patients, clients, and consumers in partnerships. 1 The aim of many of these partnerships is to consider how health services can be improved, in relation to accessibility, service delivery, discharge, and referral. 2 , 3 Patient journey mapping is a research approach increasingly being adopted to explore these experiences in healthcare. 3
a patient-oriented project that has been undertaken to better understand barriers, facilitators, experiences, interactions with services and/or outcomes for individuals and/or their carers, and family members as they enter, navigate, experience and exit one or more services in a health system by documenting elements of the journey to produce a visual or descriptive map. 3
It is an emerging field with a clear patient-centred focus, as opposed to studies that track patient flow, demand, and movement. As a general principle, patient journey mapping projects will provide evidence of patient perspectives and highlight experiences through the patient and consumer lens.
Patient journey mapping can provide significant insights that enable responsive and context-specific strategies for improving patient healthcare experiences and outcomes to be designed and implemented. 3–6 These improvements can occur at the individual patient, model of care, and/or health system level. As with other emerging methodologies, questions have been raised regarding exactly how patient journey mapping projects can best be designed, conducted, and reported. 3
In this methods paper, we provide an overview of patient journey mapping as an emergent field of research, including reasons that mapping patient journeys might be considered, methods that can be adopted, the principles that can guide patient journey mapping data collection and analysis, and considerations for reporting findings and recognizing the implications of findings. We summarize and draw on five cardiovascular patient journey mapping projects, as examples.
One of the most appealing elements of the patient journey mapping field of research is its focus on illuminating the lived experiences of patients and/or their family members, and the health professionals caring for them, methodically and purposefully. Patient journey mapping has an ability to provide detailed information about patient experiences, gaps in health services, and barriers and facilitators for access to health services. This information can be used independently, or alongside information from larger data sets, to adapt and improve models of care relevant to the population that is being investigated. 3
To date, the most frequent reason for adopting this approach is to inform health service redesign and improvement. 3 , 7 , 8 Other reasons have included: (i) to develop a deeper understanding of a person’s entire journey through health systems; 3 (ii) to identify delays in diagnosis or treatment (often described as bottlenecks); 9 (iii) to identify gaps in care and unmet needs; (iv) to evaluate continuity of care across health services and regions; 10 (v) to understand and evaluate the comprehensiveness of care; 11 (vi) to understand how people are navigating health systems and services; and (vii) to compare patient experiences with practice guidelines and standards of care.
Patient journey mapping approaches frequently use six broad steps that help facilitate the preparation and execution of research projects. These are outlined in the Central illustration . We acknowledge that not all patient journey mapping approaches will follow the order outlined in the Central illustration , but all steps need to be considered at some point throughout each project to ensure that research is undertaken rigorously, appropriately, and in alignment with best practice research principles.

Steps for conducing patient journey mapping.
Five cardiovascular patient journey mapping research examples have been included in Figure 1 , 12–16 to provide specific context and illustrate these six steps. For each of these examples, the problem or gap in practice or research, consultation processes, research question or aim, type of mapping, methods, and reporting of findings have been extracted. Each of these steps is then discussed, using these cardiovascular examples.

Examples of patient journey mapping projects.
Define the problem or gap in practice or research
Developing an understanding of a problem or gap in practice is essential for facilitating the design and development of quality research projects. In the examples outlined in Figure 1 , it is evident that clinical variation or system gaps have been explored using patient journey mapping. In the first two examples, populations known to have health vulnerabilities were explored—in Example 1, this related to comorbid substance use and physical illness, 13 and in Example 2, this related to geographical location. 13 Broader systems and societal gaps were explored in Examples 4 and 5, respectively, 15 , 16 and in Example 3, a new technologically driven solution for an existing model of care was tested for its ability to improve patient outcomes relating to hypertension. 14
Consultation, engagement, and partnership
Ideally, consultation with heathcare providers and/or patients would occur when the problem or gap in practice or research is being defined. This is a key principle of co-designed research. 17 Numerous existing frameworks for supporting patient involvement in research have been designed and were recently documented and explored in a systematic review by Greenhalgh et al . 18 While none of the five example studies included this step in the initial phase of the project, it is increasingly being undertaken in patient partnership projects internationally (e.g. in renal care). 17 If not in the project conceptualization phase, consultation may occur during the data collection or analysis phase, as demonstrated in Example 3, where a care pathway was co-created with participants. 14 We refer readers to Greenhalgh’s systematic review as a starting point for considering suitable frameworks for engaging participants in consultation, partnership, and co-design of patient journey mapping projects. 18
Design the research question/project aim
Conducting patient journey mapping research requires a thoughtful and systematic approach to adequately capture the complexity of the healthcare experience. First, the research objectives and questions should be clearly defined. Aspects of the patient journey that will be explored need to be identified. Then, a robust approach must be developed, taking into account whether qualitative, quantitative, or mixed methods are more appropriate for the objectives of the study.
For example, in the cardiac examples in Figure 1 , the broad aims included mapping existing pathways through health services where there were known problems 12 , 13 , 15 , 16 and documenting the co-creation of a new care pathway using quantitative, qualitative, or mixed methods. 14
In traditional studies, questions that might be addressed in the area of patient movement in health systems include data collected through the health systems databases, such as ‘What is the length of stay for x population’, or ‘What is the door to balloon time in this hospital?’ In contrast, patient mapping journey studies will approach asking questions about experiences that require data from patients and their family members, e.g. ‘What is the impact on you of your length of stay?’, ‘What was your experience in being assessed and undergoing treatment for your chest pain?’, ‘What was your experience supporting this patient during their cardiac admission and discharge?’
Select appropriate type of mapping
The methods chosen for mapping need to align with the identified purpose for mapping and the aim or question that was designed in Step 3. A range of research methods have been used in patient journey mapping projects involving various qualitative, quantitative, and mixed methods techniques and tools. 4 Some approaches use traditional forms of data collection, such as short-form and long-form patient interviews, focus groups, and direct patient observations. 18 , 19 Other approaches use patient journey mapping tools, designed and used with specific cultural groups, such as First Nations peoples using artwork, paintings, sand trays, and photovoice. 17 , 20 In the cardiovascular examples presented in Figure 1 , both qualitative and quantitative methods have been used, with interviews, patient record reviews, and observational techniques adopted to map patient journeys.
In a recent scoping review investigating patient journey mapping across all health care settings and specialities, six types of patient journey mapping were identified. 3 These included (i) mapping key experiences throughout a period of illness; (ii) mapping by location of health service; (iii) mapping by events that occurred throughout a period of illness; (iv) mapping roles, input, and experiences of key stakeholders throughout patient journeys; (v) mapping a journey from multiple perspectives; and (vi) mapping a timeline of events. 3 Combinations or variations of these may be used in cardiovascular settings in the future, depending on the research question, and the reasons mapping is being undertaken.
Recruit, collect data, and analyse data
The majority of health-focused patient journey mapping projects published to date have recruited <50 participants. 3 Projects with fewer participants tend to be qualitative in nature. In the cardiovascular examples provided in Figure 1 , participant numbers range from 7 14 to 260. 15 The 3 studies with <20 participants were qualitative, 12 , 14 , 16 and the 2 with 95 and 260 participants, respectively, were quantitative. 13 , 15 As seen in these and wider patient journey mapping examples, 3 participants may include patients, relatives, carers, healthcare professionals, or other stakeholders, as required, to meet the study objectives. These different participant perspectives may be analysed within each participant group and/or across the wider cohort to provide insights into experiences, and the contextual factors that shape these experiences.
The approach chosen for data collection and analysis will vary and depends on the research question. What differentiates data analysis in patient journey mapping studies from other qualitative or quantitative studies is the focus on describing, defining, or exploring the journey from a patient’s, rather than a health service, perspective. Dimensions that may, therefore, be highlighted in the analysis include timing of service access, duration of delays to service access, physical location of services relative to a patient’s home, comparison of care received vs. benchmarked care, placing focus on the patient perspective.
The mapping of individual patient journeys may take place during data collection with the use of mapping templates (tables, diagrams, and figures) and/or later in the analysis phase with the use of inductive or deductive analysis, mapping tables, or frameworks. These have been characterized and visually represented in a recent scoping review. 3 Representations of patient journeys can also be constructed through a secondary analysis of previously collected data. In these instances, qualitative data (i.e. interviews and focus group transcripts) have been re-analysed to understand whether a patient journey narrative can be extracted and reported. Undertaking these projects triggers a new research cycle involving the six steps outlined in the Central illustration . The difference in these instances is that the data are already collected for Step 5.
Report findings, disseminate findings, and take action on findings
A standardized, formal reporting guideline for patient journey mapping research does not currently exist. As argued in Davies et al ., 3 a dedicated reporting guide for patient journey mapping would be ill-advised, given the diversity of approaches and methods that have been adopted in this field. Our recommendation is for projects to be reported in accordance with formal guidelines that best align with the research methods that have been adopted. For example, COREQ may be used for patient journey mapping where qualitative methods have been used. 20 STROBE may be used for patient journey mapping where quantitative methods have been used. 21 Whichever methods have been adopted, reporting of projects should be transparent, rigorous, and contain enough detail to the extent that the principles of transparency, trustworthiness, and reproducibility are upheld. 3
Dissemination of research findings needs to include the research, healthcare, and broader communities. Dissemination methods may include academic publications, conference presentations, and communication with relevant stakeholders including healthcare professionals, policymakers, and patient advocacy groups. Based on the findings and identified insights, stakeholders can collaboratively design and implement interventions, programmes, or improvements in healthcare delivery that overcome the identified challenges directly and address and improve the overall patient experience. This cyclical process can hopefully produce research that not only informs but also leads to tangible improvements in healthcare practice and policy.
Patient journey mapping is typically a hands-on process, relying on surveys, interviews, and observational research. The technology that supports this research has, to date, included word processing software, and data analysis packages, such as NVivo, SPSS, and Stata. With the advent of more sophisticated technological tools, such as electronic health records, data analytics programmes, and patient tracking systems, healthcare providers and researchers can potentially use this technology to complement and enhance patient journey mapping research. 19 , 20 , 22 There are existing examples where technology has been harnessed in patient journey. Lee et al . used patient journey mapping to verify disease treatment data from the perspective of the patient, and then the authors developed a mobile prototype that organizes and visualizes personal health information according to the patient-centred journey map. They used a visualization approach for analysing medical information in personal health management and examined the medical information representation of seven mobile health apps that were used by patients and individuals. The apps provide easy access to patient health information; they primarily import data from the hospital database, without the need for patients to create their own medical records and information. 23
In another example, Wauben et al. 19 used radio frequency identification technology (a wireless system that is able to track a patient journey), as a component of their patient journey mapping project, to track surgical day care patients to increase patient flow, reduce wait times, and improve patient and staff satisfaction.
Patient journey mapping has emerged as a valuable research methodology in healthcare, providing a comprehensive and patient-centric approach to understanding the entire spectrum of a patient’s experience within the healthcare system. Future implications of this methodology are promising, particularly for transforming and redesigning healthcare delivery and improving patient outcomes. The impact may be most profound in the following key areas:
Personalized, patient-centred care : The methodology allows healthcare providers to gain deep insights into individual patient experiences. This information can be leveraged to deliver personalized, patient-centric care, based on the needs, values, and preferences of each patient, and aligned with guideline recommendations, healthcare professionals can tailor interventions and treatment plans to optimize patient and clinical outcomes.
Enhanced communication, collaboration, and co-design : Mapping patient interactions with health professionals and journeys within and across health services enables specific gaps in communication and collaboration to be highlighted and potentially informs responsive strategies for improvement. Ideally, these strategies would be co-designed with patients and health professionals, leading to improved care co-ordination and healthcare experience and outcomes.
Patient engagement and empowerment : When patients are invited to share their health journey experiences, and see visual or written representations of their journeys, they may come to understand their own health situation more deeply. Potentially, this may lead to increased health literacy, renewed adherence to treatment plans, and/or self-management of chronic conditions such as cardiovascular disease. Given these benefits, we recommend that patients be provided with the findings of research and quality improvement projects with which they are involved, to close the loop, and to ensure that the findings are appropriately disseminated.
Patient journey mapping is an emerging field of research. Methods used in patient journey mapping projects have varied quite significantly; however, there are common research processes that can be followed to produce high-quality, insightful, and valuable research outputs. Insights gained from patient journey mapping can facilitate the identification of areas for enhancement within healthcare systems and inform the design of patient-centric solutions that prioritize the quality of care and patient outcomes, and patient satisfaction. Using patient journey mapping research can enable healthcare providers to forge stronger patient–provider relationships and co-design improved health service quality, patient experiences, and outcomes.
None declared.
Farmer J , Bigby C , Davis H , Carlisle K , Kenny A , Huysmans R , et al. The state of health services partnering with consumers: evidence from an online survey of Australian health services . BMC Health Serv Res 2018 ; 18 : 628 .
Google Scholar
Kelly J , Dwyer J , Mackean T , O’Donnell K , Willis E . Coproducing Aboriginal patient journey mapping tools for improved quality and coordination of care . Aust J Prim Health 2017 ; 23 : 536 – 542 .
Davies EL , Bulto LN , Walsh A , Pollock D , Langton VM , Laing RE , et al. Reporting and conducting patient journey mapping research in healthcare: a scoping review . J Adv Nurs 2023 ; 79 : 83 – 100 .
Ly S , Runacres F , Poon P . Journey mapping as a novel approach to healthcare: a qualitative mixed methods study in palliative care . BMC Health Serv Res 2021 ; 21 : 915 .
Arias M , Rojas E , Aguirre S , Cornejo F , Munoz-Gama J , Sepúlveda M , et al. Mapping the patient’s journey in healthcare through process mining . Int J Environ Res Public Health 2020 ; 17 : 6586 .
Natale V , Pruette C , Gerohristodoulos K , Scheimann A , Allen L , Kim JM , et al. Journey mapping to improve patient-family experience and teamwork: applying a systems thinking tool to a pediatric ambulatory clinic . Qual Manag Health Care 2023 ; 32 : 61 – 64 .
Cherif E , Martin-Verdier E , Rochette C . Investigating the healthcare pathway through patients’ experience and profiles: implications for breast cancer healthcare providers . BMC Health Serv Res 2020 ; 20 : 735 .
Gilburt H , Drummond C , Sinclair J . Navigating the alcohol treatment pathway: a qualitative study from the service users’ perspective . Alcohol Alcohol 2015 ; 50 : 444 – 450 .
Gichuhi S , Kabiru J , M’Bongo Zindamoyen A , Rono H , Ollando E , Wachira J , et al. Delay along the care-seeking journey of patients with ocular surface squamous neoplasia in Kenya . BMC Health Serv Res 2017 ; 17 : 485 .
Borycki EM , Kushniruk AW , Wagner E , Kletke R . Patient journey mapping: integrating digital technologies into the journey . Knowl Manag E-Learn 2020 ; 12 : 521 – 535 .
Barton E , Freeman T , Baum F , Javanparast S , Lawless A . The feasibility and potential use of case-tracked client journeys in primary healthcare: a pilot study . BMJ Open 2019 ; 9 : e024419 .
Bearnot B , Mitton JA . “You’re always jumping through hoops”: journey mapping the care experiences of individuals with opioid use disorder-associated endocarditis . J Addict Med 2020 ; 14 : 494 – 501 .
Cunnington MS , Plummer CJ , McDiarmid AK , McComb JM . The patient journey from symptom onset to pacemaker implantation . QJM 2008 ; 101 : 955 – 960 .
Geerse C , van Slobbe C , van Triet E , Simonse L . Design of a care pathway for preventive blood pressure monitoring: qualitative study . JMIR Cardio 2019 ; 3 : e13048 .
Laveau F , Hammoudi N , Berthelot E , Belmin J , Assayag P , Cohen A , et al. Patient journey in decompensated heart failure: an analysis in departments of cardiology and geriatrics in the Greater Paris University Hospitals . Arch Cardiovasc Dis 2017 ; 110 : 42 – 50 .
Naheed A , Haldane V , Jafar TH , Chakma N , Legido-Quigley H . Patient pathways and perceptions of treatment, management, and control Bangladesh: a qualitative study . Patient Prefer Adherence 2018 ; 12 : 1437 – 1449 .
Bateman S , Arnold-Chamney M , Jesudason S , Lester R , McDonald S , O’Donnell K , et al. Real ways of working together: co-creating meaningful Aboriginal community consultations to advance kidney care . Aust N Z J Public Health 2022 ; 46 : 614 – 621 .
Greenhalgh T , Hinton L , Finlay T , Macfarlane A , Fahy N , Clyde B , et al. Frameworks for supporting patient and public involvement in research: systematic review and co-design pilot . Health Expect 2019 ; 22 : 785 – 801 .
Wauben LSGL , Guédon ACP , de Korne DF , van den Dobbelsteen JJ . Tracking surgical day care patients using RFID technology . BMJ Innov 2015 ; 1 : 59 – 66 .
Tong A , Sainsbury P , Craig J . Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups . Int J Qual Health Care 2007 ; 19 : 349 – 357 .
von Elm E , Altman DG , Egger M , Pocock SJ , Gøtzsche PC , Vandenbroucke JP , et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies . Lancet 2007 ; 370 (9596): 1453 – 1457 .
Wilson A , Mackean T , Withall L , Willis EM , Pearson O , Hayes C , et al. Protocols for an Aboriginal-led, multi-methods study of the role of Aboriginal and Torres Strait Islander health workers, practitioners and Liaison officers in quality acute health care . J Aust Indigenous HealthInfoNet 2022 ; 3 : 1 – 15 .
Lee B , Lee J , Cho Y , Shin Y , Oh C , Park H , et al. Visualisation of information using patient journey maps for a mobile health application . Appl Sci 2023 ; 13 : 6067 .
Author notes
- cardiovascular system
- health personnel
- health services
- health care systems
- narrative discourse
Email alerts
Related articles in pubmed, citing articles via.
- Recommend to Your Librarian
- Advertising and Corporate Services
- Journals Career Network
Affiliations
- Online ISSN 1873-1953
- Print ISSN 1474-5151
- Copyright © 2024 European Society of Cardiology
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Root out friction in every digital experience, super-charge conversion rates, and optimise digital self-service
Uncover insights from any interaction, deliver AI-powered agent coaching, and reduce cost to serve
Increase revenue and loyalty with real-time insights and recommendations delivered straight to teams on the ground
Know exactly how your people feel and empower managers to improve employee engagement, productivity, and retention
Take action in the moments that matter most along the employee journey and drive bottom line growth
Whatever they’re are saying, wherever they’re saying it, know exactly what’s going on with your people
Get faster, richer insights with qual and quant tools that make powerful market research available to everyone
Run concept tests, pricing studies, prototyping + more with fast, powerful studies designed by UX research experts
Track your brand performance 24/7 and act quickly to respond to opportunities and challenges in your market
Meet the operating system for experience management
- Free Account
- For Digital
- For Customer Care
- For Human Resources
- For Researchers
- Financial Services
- All Industries
Popular Use Cases
- Customer Experience
- Employee Experience
- Employee Exit Interviews
- Net Promoter Score
- Voice of Customer
- Customer Success Hub
- Product Documentation
- Training & Certification
- XM Institute
- Popular Resources
- Customer Stories
- Artificial Intelligence
- Market Research
- Partnerships
- Marketplace
The annual gathering of the experience leaders at the world’s iconic brands building breakthrough business results.
- English/AU & NZ
- Español/Europa
- Español/América Latina
- Português Brasileiro
- REQUEST DEMO
- Experience Management
- Industry Specific
- Patient Journey Mapping
Your complete guide to patient journey mapping
15 min read Healthcare organisations can increase patient retention and improve patient satisfaction with patient journey mapping. Discover how to create a patient journey map and how you can use it to improve your organisation’s bottom line.
What is the patient journey?
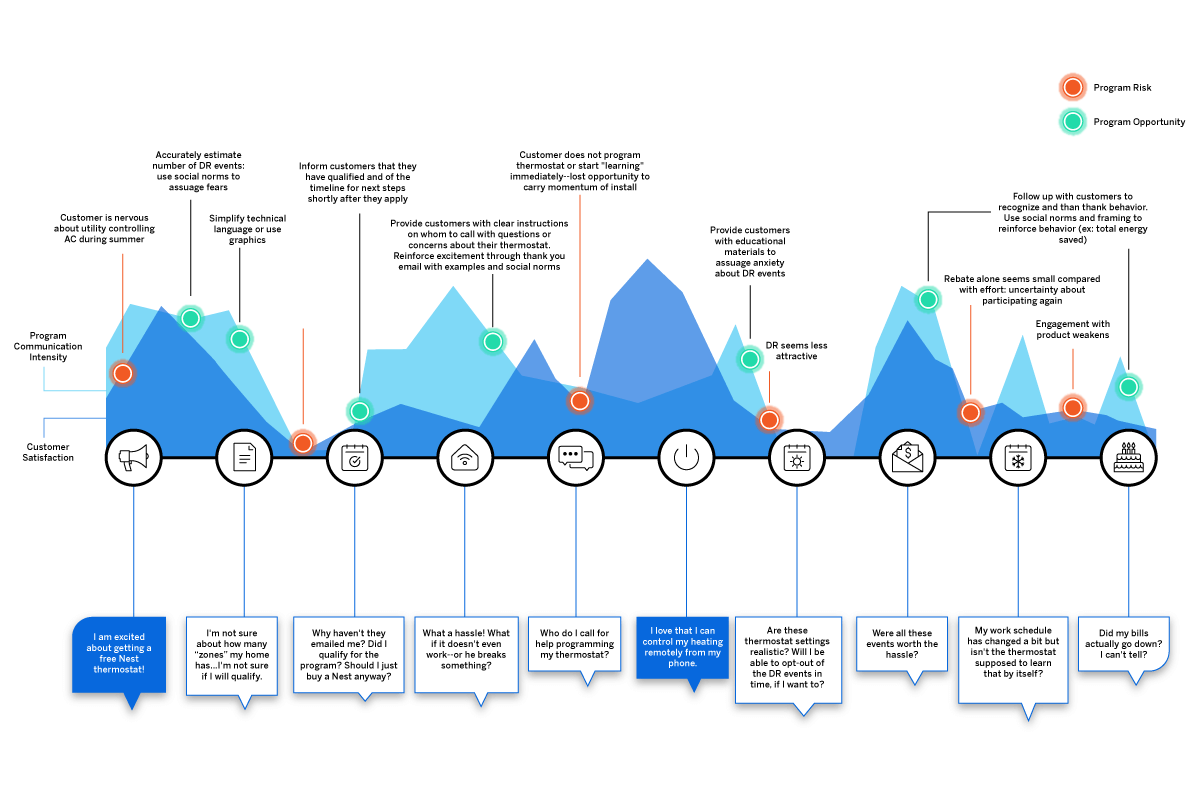
The patient journey is the sequence of events that begins when a patient first develops a need for care. Rather than focusing on service delivery, the patient journey encompasses all touchpoints of a patient’s healthcare experience–from locating healthcare providers and scheduling appointments, to paying the bill and continuing their care after treatment.
Examining the patient journey is essential to improving the patient experience. Not all interactions a patient has with your organisation are weighted the same. Gathering patient feedback and understanding perceptions all along the patient journey can help you to identify moments of truth : the touchpoints that have the biggest impact on patient loyalty.
Discover how Qualtrics can enhance the healthcare industry
The patient journey vs. the patient experience
Unlike traditional patient experience measurement, the patient journey looks not only at service delivery but also at the steps the patient takes before and after they engage directly with your organisation. It recognises that patient interactions with a healthcare system go well beyond the walls of the medical facility itself.
What are the stages of the patient journey?
There are several stages along the patient journey. When gathering patient feedback, you should make sure to capture insights at each of these stages.
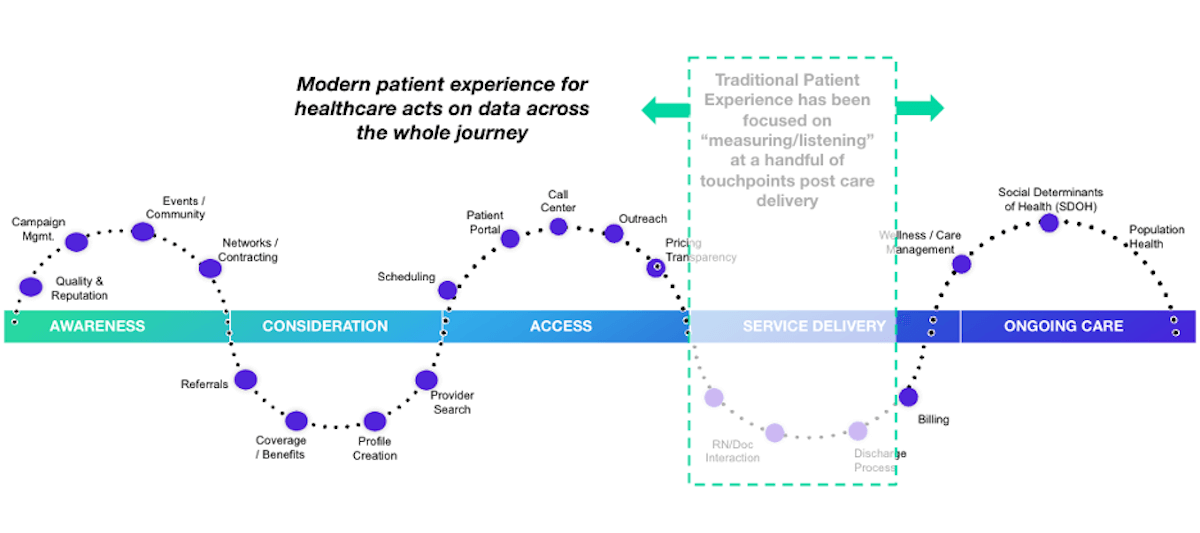
Stage 1: Awareness
The patient journey starts with awareness. In this stage, the patient identifies a need for care and begins searching for care providers. Examples of how patients learn about healthcare providers include online searches, review sites, marketing campaigns, networking, and community involvement.
Stage 2: Consideration
In the consideration stage, the patient weighs their options to determine if your health system can meet their needs. Factors patients consider include referrals, coverage and benefits, recommendations, access, and ratings and reviews. Often in this stage, patients interact with your website or social media pages or contact you via phone or email during this stage.
Stage 3: Access
The access stage is where the patient decides to schedule services with your healthcare organisation. Direct patient engagement with your organisation increases during this stage. You’ll engage with patients in a variety of ways including phone calls, the patient portal, text messages, and emails as part of the scheduling and new patient acquisition process.
Stage 4: Service delivery
The service delivery stage relates to the clinical care provided to your patients. Encompassed in this stage are the clinical visit itself, check-in and check-out, admission and discharge, and billing. Traditional patient satisfaction measurement centres around this stage of the patient journey.
Stage 5: Ongoing care
The ongoing care stage of the patient journey involves patient engagement that occurs after the interactions directly related to service delivery. In addition to wellness and care management, this stage may address social determinants of health and population health.
What is a patient journey map?
The best way to utilise the patient journey to enhance patient experiences is by journey mapping. A patient journey map is a visual tool that illustrates the relationship a patient has with a healthcare organisation over time.
Patient journey mapping helps stakeholders to assess the patient experience from multiple perspectives. Journey maps provide a way to visualise the internal and external factors affecting patient flow and the different paths patients must take in order to reach their care goals.
What are the benefits of patient journey mapping?
Patient journey mapping can help you to visualise all of the steps patients take throughout the entire process of seeking, receiving, and continuing care. Creating a patient journey map is useful to identify pain points and gaps in care. Mapping the patient journey makes it easier to develop solutions that make a more seamless experience within your healthcare system.
Patient journey mapping benefits include:
- Creating shared ownership of the patient experience
- Refining your patient listening strategy
- Aligning your organisation with a common view of the patient experience
- Measuring gaps between the intended experience for your patients versus the actual experience
- Identifying and resolving common pain points for your patients
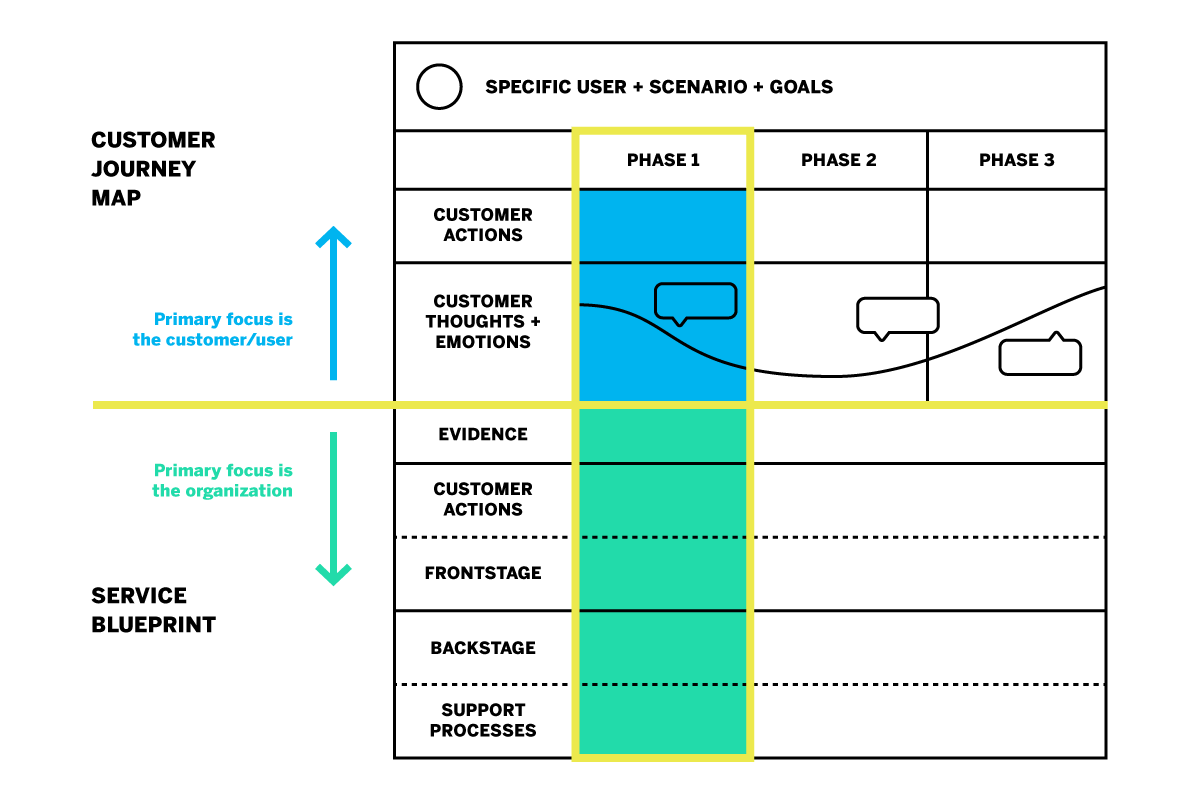
Four types of patient journey maps
When creating a patient journey map, there are four types to consider. Each type of map has an intended purpose. You might start your patient journey mapping with only one type and incorporate the others as your efforts progress.
Current state
A current state journey map tells the story of what patients do, think, and feel as they interact with your organisation today. This type of patient journey map is ideally created using patient data and observational data.
The current state journey map is best for driving incremental improvements to enhance the patient experience.
Future state
A future state patient journey map tells the story of what you want your patients to do, think, and feel as they interact with your organisation in the future. This type of map should capture the ideal journey you’d like to see for your patients.
The future state journey map is an effective tool to drive strategy, align teams, and communicate your visions for new services, processes, and experiences.
Day in the life
A day in the life patient journey map illustrates what your patients do, think, and feel today, within a specific area of focus. Patient personas are particularly useful when creating day in the life maps; these are discussed in greater detail below.
This type of patient journey map is intended to capture what your patients experience both inside and outside of the healthcare system. Day in the life maps are valuable to address unmet needs and determine how and when you can better engage your patients.
Service blueprint
A service blueprint is a simplified diagram of a current state or future state patient journey map. In the service blueprint, you add layers to illustrate the systems of people, processes, policies, and technologies surrounding each patient touchpoint.
For current state patient journey maps, the service blueprint can help to identify root causes of pain points. For future state, the service blueprint is helpful to visualize the systems or processes that can be put in place to support the intended patient experience.
How do you create a patient journey map?
Now that you know about the different types of patient journey maps and their roles in driving patient experience improvement, how do you get started on creating your own?
The most useful maps are those which can expound upon each touchpoint of the healthcare journey with operational data, such as patient demographics, as well as real patient insights and perspectives. Using a platform that can capture this data will aid significantly in your patient journey mapping process.
Patient journey mapping: getting started
Before you get started, it’s a good idea to engage individuals across all departments and include input from multiple stakeholders. Once you’re ready, follow these steps to begin creating an effective patient journey map.
Identify your target audience
What type of patient journey will you be mapping? There may be varying patient journeys within your organisation; for instance, an oncology patient’s journey will look very different from that of an expectant mother. The journey of a patient with health insurance will differ from that of a patient without insurance. To map the patient journey, you’ll want to create robust patient profiles you can use to segment and track like-populations throughout the healthcare experience.
Establishing patient personas and segments
Not every patient will have the same healthcare goals. Creating patient personas based on behaviours and preferences is a good way to differentiate the needs and more clearly understand the perspectives of the unique populations you serve.
- Demographic information such as age group, gender, or location
- Healthcare-specific goals, conditions, and treatments
- Healthcare-specific challenges/pain points
- Engagement patterns and expressed feedback
- How your services fit into their life
- Barriers to care
Specify a goal for the patient’s journey
The patient personas you create will all have unique goals within the care journey. The patient has a specific goal in mind when they initiate contact with your organisation, whether it is treatment of symptoms, a diagnosis for chronic issues, or surgery.
Every interaction along the patient journey influences how successful the patient feels about achieving this goal. When mapping the patient journey, you’ll want to consider how the various touchpoints affect the patient’s ability to meet this goal.
Identify the patient’s steps to accomplish their target goal
This step is about how the patient views their care journey within your health system–not about the actual processes and systems your organisation has in place. Effective patient journey mapping requires you to see how the patient navigates the journey through their point of view.
Omni-channel listening is a valuable strategy in this step of journey mapping. Listening to your patients across all the channels can provide a clearer picture of their perceptions and behaviours as they engage with your organisation.
Some steps the patient takes may not even include your organisation, but might still affect how they are interacting with you directly. For example, if a patient logs into their health insurance portal to check coverage for healthcare services, they are not engaging with your organisation but this is still a part of their care journey that may feed into their interactions with your organisation later on.
Uncover perceptions along the journey
Gather patient feedback along the touchpoints of the care journey to identify key emotional moments that may disproportionately shape attitudes. These insights shed light on what’s working and what’s not; they can also be used to highlight the moments of truth that contribute to patient loyalty.
Patient perceptions are an important piece of patient journey mapping; it will be difficult to drive action without them.
Additional tips for creating the ideal patient journey map
Patient journey mapping is a continuous process. Creating the map is the first step, but the true value is dependent upon maintaining the map as you continue to gather insights and refine processes.
This leads to the second tip: be ready to take action! You can use a patient journey map to draw conclusions about your patients’ experiences within your organisation, but awareness alone will yield no benefits. The journey map is a valuable tool to be used in your wider improvement efforts.
How do you drive action using a patient journey map?
Once your patient journey mapping is complete, it’s time to put it to good use. Here are five ways patient journey maps can be used to drive action.
Identify and fix problems
The visual layout of a journey map makes it ideal to identify gaps and potential pain points in your patient journeys. This will give you a better understanding of what’s working and what’s not. It will also help you to visualise where and how improvements can be made.
Build a patient mindset
Patient journey mapping enables you to incorporate more patient-centric thinking into your processes and systems. Use your map to challenge internal ideas of what patients want or need. Invite stakeholders to navigate the touchpoints along the healthcare journey to gain perspective.
Uncover unmet patient needs
By mapping the patient journey, you can build stronger patient relationships by listening across all channels to determine where experiences are falling short or where unmet needs emerge. This enables you to look for opportunities to expand alternatives, streamline initiatives, and create new, engaging ways for your patients to share feedback.
Create strategic alignment
Utilise your patient journey map to prioritise projects or improvement efforts. It can also help you to better engage interdepartmental staff to better understand policies and work together toward patient experience goals.
Refine measurement
Patient journey mapping is a great resource to use when defining patient satisfaction metrics and identifying gaps in how you currently gather insights.
How does patient journey mapping increase your bottom line?
Patient journey mapping can increase your bottom line by laying the foundation for improved patient satisfaction and higher retention.
Organisations across all industries are looking to understand customer journeys in order to attract and retain customers by gaining deeper insights into what drives the consumer experience.
As healthcare becomes more consumer-driven, health systems must similarly map the patient journey to improve the patient experience and boost retention. The cost of patient acquisition, combined with the fact that patients are willing to shop around for the best healthcare experience, means success depends on creating the most seamless patient journey possible.
The tools for success
For the most impactful patient journey mapping experience, you’ll want the ability to link your operational and experience data to your journey map’s touchpoints. Insights about what has happened at each touchpoint, as well as why it is happening, empower you to create experiences that meet patient expectations and drive up satisfaction.
Here are some best practice considerations as you develop your patient journey mapping strategy:
- Create a shared understanding throughout your health system of how your patients interact with your organisation, and you’ll know the roles and responsibilities of your different teams
- Design a unique patient journey based on multichannel, real-time feedback from the patient
- Consider the frequency with which topics emerge in feedback, as well as the emotional intensity behind them to zero in on what improvements can drive the greatest impact
- Develop empathy and collaboration between teams, working together to achieve the same outcome
- Drive a patient-centric culture by developing a shared sense of ownership of the patient experience
- Connect your operational patient data with your patient experience feedback in one system
- Leverage a closed-loop feedback system that triggers actions for immediate responses to patient concerns
Qualtrics’ XM Platform™ is designed to support all of these actions throughout the journey mapping process.
Related resources
Nursing shortages 13 min read, healthcare branding 13 min read, patient feedback 13 min read, patient experience: your complete guide 12 min read, symptoms survey 10 min read, quality improvement in healthcare 11 min read, nurse satisfaction survey 11 min read, request demo.
Ready to learn more about Qualtrics?
The 1-2-3 Guide to Patient Journey Mapping [Template Inside]
by Gaine Solutions | Feb 28, 2024 | Healthcare , Life Sciences , Master Data Management

Patient journeys in today’s healthcare landscape are complex, spanning a number of platforms, systems, touchpoints, and interactions. As patients engage with healthcare providers through diverse channels, both digital and physical, the need for a structured and comprehensive approach to managing the patient journeys is evident. Patient journey mapping is the solution.
Patient journey mapping creates a high-level and holistic view of the patient journey that empowers healthcare providers to make the most informed and impactful decisions possible about how to enhance operations and care.
In this guide, we’ll walk step-by-step through the process of creating and implementing a patient journey map that drives better performance results and patient outcomes for your healthcare organization.
Key Takeaways:
- Patient journey mapping is crucial for understanding and enhancing the patient experience.
- Patient journey mapping leads to improved patient satisfaction, better clinical outcomes, and increased operational efficiency.
- Developing a patient journey map requires clear objectives, a cross-functional team, and data-driven approaches to gaining insight.
- Improvement strategies should be developed for each critical moment and touchpoint, with changes implemented and continuously monitored for effectiveness over time.
What is Patient Journey Mapping and Why Is It Important?
Patient journey mapping is the process of creating a detailed visualization of a patient’s healthcare journey, from initial contact through treatment and follow-up care, identifying every touchpoint along the way. This methodical approach helps healthcare providers see the care process from the patient perspective, including the highs, lows, and gaps in the patient experience.
The example below is from the U.S. Department of Veteran Affairs, and shows how intricate and complex the patient journey is once it’s mapped completely. This drives home the importance of documenting the journey visually in order to see it in a holistic way.
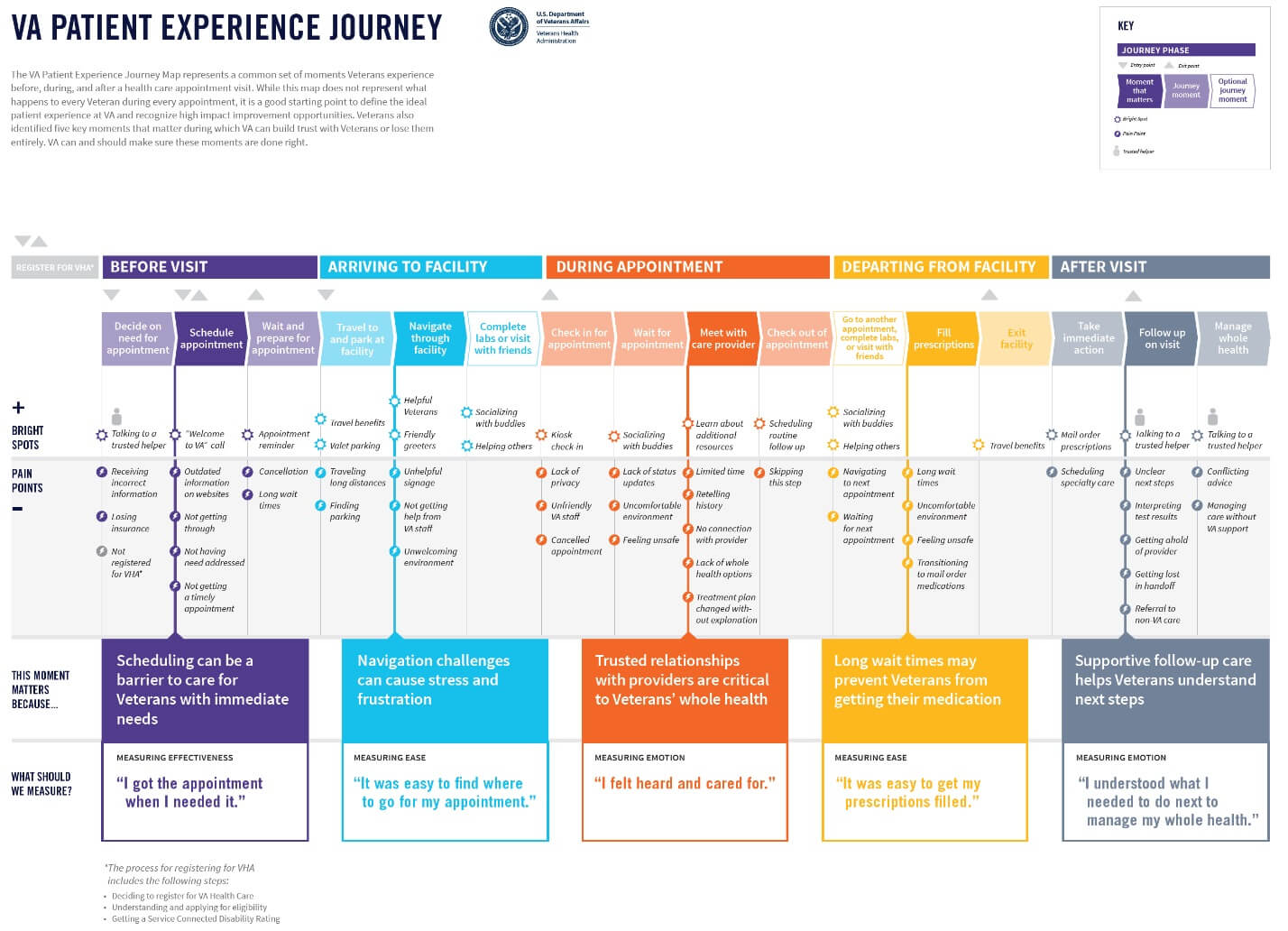
Image Source
When done effectively, patient journey mapping is a valuable tool driving more seamless, integrated, and patient-centered care. Journey mapping also helps healthcare organizations make informed decisions about where to allocate resources, how to streamline operations, and ways to personalize care to meet the unique needs of each patient.
In the end, the benefits of patient journey mapping are threefold:
- Improved Patient Satisfaction : Enhances the overall patient experience by addressing specific needs and preferences, leading to higher satisfaction rates.
- Better Clinical Outcomes : Identifies opportunities for early intervention and personalized care plans, contributing to improved health results.
- Increased Operational Efficiency : Streamlines healthcare processes by pinpointing inefficiencies and redundancies, leading to more effective use of resources.
It leads to 360-degree improvements that enhance clinical, administrative, and operational aspects of both the healthcare system and the patient experience. In the next section, we’ll walk through the steps you can take to develop a patient journey map for your organization.
Your Step-by-Step Patient Journey Mapping Template
1. identify the goals and scope of your map.
Begin by d eve loping a clear vision of what you aim to achieve through patient journey mapping. Whether it’s to enhance patient satisfaction, streamline healthcare delivery, or identify gaps in service, setting specific objectives will direct your mapping efforts. During this step, you should also determine the scope of your map (i.e. whether it focuses on a particular service line or the entire healthcare experience).
2. Gather a Cross-Functional Team
Assemble a team that represents a broad spectrum of roles within your organization, including clinicians, administrative staff, IT professionals, and cust ome r service representatives. Diverse perspectives ensure a holistic view of the patient journey, capturing insights from every facet of patient interaction.
3. Map the Patient Touchpoints
Systematically list every interaction point between the patient and your healthcare system. This includes digital touchpoints like website visits, appointment scheduling portals, and social media interactions, as well as physical touchpoints like clinic visits, phone calls, and direct mail communication. Mapping these touchpoints requires a detailed understanding of the patient’s path through your system, from initial awareness through treatment and follow-up care.
4. Collect and Analyze Data
Leverage diverse data sources to understand patient experiences at each touchpoint. Collect patient feedback through cha nne ls like surveys, interviews, and comment cards. Analyze staff insights and review operational data. Look for patterns in behavior and satisfaction levels, and identify bottlenecks or pain points in the patient journey.
Having a centralized data management platform in place is crucial for this step—it provides a central repository for the data you collect as part of your patient journey mapping exercise, while also giving you seamless access to historical data in one location.
5. Visualize the Journey
Develop a visual representation of the patient journey. Use flowcharts, storyboards, or diagrams to depict the sequence of touchpoints and the patient’s experience at each stage. This visualization should be from the patient’s perspective, highlighting critical interactions, emotions, and decision points.
Tools like customer journey mapping software can facilitate this process, but even simple graphical tools or whiteboards can be effective.
6. Identify Moments of Truth
Highlight key moments in the journey that significantly impact the patient’s perception of care—things like first contact, diagnosis communication, wait times, and billing support. These are opportunities to make a lasting impression on the patient, and identifying them allows your team to prioritize areas for immediate improvement or innovation.
7. Develop Improvement Strategies
For each critical moment and touchpoint, evaluate what’s working effectively as well as areas for potential improvements. Call out specific gaps and pain points that may exist for the patient at every stage on your journey map. Then, brainstorm how to resolve them.
This may happen by introducing new technologies, optimizing existing processes, providing additional training for your staff, enhancing communication strategies, and more.
8. Implement Changes
Prioritize the identified improvements based on their potential impact and feasibility. Create a detailed implementation plan, assigning clear responsibilities and deadlines. Ensure there is a mechanism for tracking progress and measuring the impact of these changes on the patient experience and other goals and objectives you set at the start of the process.
9. Monitor and Adjust
Establish a continuous feedback loop to monitor the effectiveness of implemented changes. Use patient feedback, staff input, and performance metrics to assess progress. Be prepared to make iterative adjustments to your strategies based on this feedback, fostering a culture of continuous improvement.
Putting it All Together
Embarking on patient journey mapping is more than a strategic exercise—it’s a commitment to elevating the standard of care through a deep understanding of the patient’s experience. It represents a pivotal shift toward a more empathetic, patient-centric approach in healthcare, where decisions are informed by the nuanced needs and experiences of those we serve.
Gaine’s Coperor platform is a scalable, ecosystem-wide master data management solution designed for the unique challenges of the healthcare and life sciences industries. It creates a single source of data truth within an organization that makes initiatives like journey mapping possible. Learn more here or start your real-time Coperer demo today.
Opt-in with Gaine for More Insight
Great welcome to the mdm a-team you may unsubscribe at any time., more articles like this.
- Case Studies
- Contracting
- Credentialing
- Data Governance
- Data Quality
- Data Science
- Health Plans
- Interoperability
- Life Sciences
- Master Data Management
- Network Adequacy
- Network Management
- Next-Gen MDM
- Provider Data Management
- Provider Groups
- Provider Network
- Provider Network Management
- Uncategorized

Understanding the Coperor™ Health Data Management Platform

Data-Driven Healthcare: Unveiling the Path to Enhanced HEDIS and Star Quality Metrics

Demystifying HEDIS and Star Ratings: Challenges & Best Practices for Providers.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Process mapping the...
Process mapping the patient journey: an introduction
- Related content
- Peer review
- Timothy M Trebble , consultant gastroenterologist 1 ,
- Navjyot Hansi , CMT 2 1 ,
- Theresa Hydes , CMT 1 1 ,
- Melissa A Smith , specialist registrar 2 ,
- Marc Baker , senior faculty member 3
- 1 Department of Gastroenterology, Portsmouth Hospitals Trust, Portsmouth PO6 3LY
- 2 Department of Gastroenterology, Guy’s and St Thomas’ NHS Foundation Trust, London
- 3 Lean Enterprise Academy, Ross-on-Wye, Hertfordshire
- Correspondence to: T M Trebble tim.trebble{at}porthosp.nhs.uk
- Accepted 15 July 2010
Process mapping enables the reconfiguring of the patient journey from the patient’s perspective in order to improve quality of care and release resources. This paper provides a practical framework for using this versatile and simple technique in hospital.
Healthcare process mapping is a new and important form of clinical audit that examines how we manage the patient journey, using the patient’s perspective to identify problems and suggest improvements. 1 2 We outline the steps involved in mapping the patient’s journey, as we believe that a basic understanding of this versatile and simple technique, and when and how to use it, is valuable to clinicians who are developing clinical services.
What information does process mapping provide and what is it used for?
Process mapping allows us to “see” and understand the patient’s experience 3 by separating the management of a specific condition or treatment into a series of consecutive events or steps (activities, interventions, or staff interactions, for example). The sequence of these steps between two points (from admission to the accident and emergency department to discharge from the ward) can be viewed as a patient pathway or process of care. 4
Improving the patient pathway involves the coordination of multidisciplinary practice, aiming to maximise clinical efficacy and efficiency by eliminating ineffective and unnecessary care. 5 The data provided by process mapping can be used to redesign the patient pathway 4 6 to improve the quality or efficiency of clinical management and to alter the focus of care towards activities most valued by the patient.
Process mapping has shown clinical benefit across a variety of specialties, multidisciplinary teams, and healthcare systems. 7 8 9 The NHS Institute for Innovation and Improvement proposes a range of practical benefits using this approach (box 1). 6
Box 1 Benefits of process mapping 6
A starting point for an improvement project specific for your own place of work
Creating a culture of ownership, responsibility and accountability for your team
Illustrates a patient pathway or process, understanding it from a patient’s perspective
An aid to plan changes more effectively
Collecting ideas, often from staff who understand the system but who rarely contribute to change
An interactive event that engages staff
An end product (a process map) that is easy to understand and highly visual
Several management systems are available to support process mapping and pathway redesign. 10 11 A common technique, derived originally from the Japanese car maker Toyota, is known as lean thinking transformation. 3 12 This considers each step in a patient pathway in terms of the relative contribution towards the patient’s outcome, taken from the patient’s perspective: it improves the patient’s health, wellbeing, and experience (value adding) or it does not (non-value or “waste”) (box 2). 14 15 16
Box 2 The eight types of waste in health care 13
Defects —Drug prescription errors; incomplete surgical equipment
Overproduction —Inappropriate scheduling
Transportation —Distance between related departments
Waiting —By patients or staff
Inventory —Excess stores, that expire
Motion —Poor ergonomics
Overprocessing —A sledgehammer to crack a nut
Human potential —Not making the most of staff skills
Process mapping can be used to identify and characterise value and non-value steps in the patient pathway (also known as value stream mapping). Using lean thinking transformation to redesign the pathway aims to enhance the contribution of value steps and remove non-value steps. 17 In most processes, non-value steps account for nine times more effort than steps that add value. 18
Reviewing the patient journey is always beneficial, and therefore a process mapping exercise can be undertaken at any time. However, common indications include a need to improve patients’ satisfaction or quality or financial aspects of a particular clinical service.
How to organise a process mapping exercise
Process mapping requires a planned approach, as even apparently straightforward patient journeys can be complex, with many interdependent steps. 4 A process mapping exercise should be an enjoyable and creative experience for staff. In common with other audit techniques, it must avoid being confrontational or judgmental or used to “name, shame, and blame.” 8 19
Preparation and planning
A good first step is to form a team of four or five key staff, ideally including a member with previous experience of lean thinking transformation. The group should decide on a plan for the project and its scope; this can be visualised by using a flow diagram (fig 1 ⇓ ). Producing a rough initial draft of the patient journey can be useful for providing an overview of the exercise.
Fig 1 Steps involved in a process mapping exercise
- Download figure
- Open in new tab
- Download powerpoint
The medical literature or questionnaire studies of patients’ expectations and outcomes should be reviewed to identify value adding steps involved in the management of the clinical condition or intervention from the patient’s perspective. 1 3
Data collection
Data collection should include information on each step under routine clinical circumstances in the usual clinical environment. Information is needed on waiting episodes and bottlenecks (any step within the patient pathway that slows the overall rate of a patient’s progress, normally through reduced capacity or availability 20 ). Using estimates of minimum and maximum time for each step reduces the influence of day to day variations that may skew the data. Limiting the number of steps (to below 60) aids subsequent analysis.
The techniques used for data collection (table 1 ⇓ ) each have advantages and disadvantages; a combination of approaches can be applied, contributing different qualitative or quantitative information. The commonly used technique of walking the patient journey includes interviews with patients and staff and direct observation of the patient journey and clinical environment. It allows the investigator to “see” the patient journey at first hand. Involving junior (or student) doctors or nurses as interviewers may increase the openness of opinions from staff, and time needed for data collection can be reduced by allotting members of the team to investigate different stages in the patient’s journey.
Data collection in process mapping
- View inline
Mapping the information
The process map should comprehensively represent the patient journey. It is common practice to draw the map by hand onto paper (often several metres long), either directly or on repositionable notes (fig 2 ⇓ ).
Fig 2 Section of a current state map of the endoscopy patient journey
Information relating to the steps or representing movement of information (request forms, results, etc) can be added. It is useful to obtain any missing information at this stage, either from staff within the meeting or by revisiting the clinical environment.
Analysing the data and problem solving
The map can be analysed by using a series of simple questions (box 3). The additional information can be added to the process map for visual representation. This can be helped by producing a workflow diagram—a map of the clinical environment, including information on patient, staff, and information movement (fig 3 ⇓ ). 18
Box 3 How to analyse a process map 6
How many steps are involved?
How many staff-staff interactions (handoffs)?
What is the time for each step and between each step?
What is the total time between start and finish (lead time)?
When does a patient join a queue, and is it a regular occurrence?
How many non-value steps are there?
What do patients complain about?
What are the problems for staff?
Fig 3 Workflow diagram of current state endoscopy pathway
Redesigning the patient journey
Lean thinking transformation involves redesigning the patient journey. 21 22 This will eliminate, combine and simplify non-value steps, 23 limit the impact of rate limiting steps (such as bottlenecks), and emphasise the value adding steps, making the process more patient-centred. 6 It is often useful to trial the new pathway and review its effect on patient management and satisfaction before attempting more sustained implementation.
Worked example: How to undertake a process mapping exercise
South Coast NHS Trust, a large district general hospital, plans to improve patient access to local services by offering unsedated endoscopy in two peripheral units. A consultant gastroenterologist has been asked to lead a process mapping exercise of the current patient journey to develop a fast track, high quality patient pathway.
In the absence of local data, he reviews the published literature and identifies key factors to the patient experience that include levels of discomfort during the procedure, time to discuss the findings with the endoscopist, and time spent waiting. 24 25 26 27 He recruits a team: an experienced performance manager, a sister from the endoscopy department, and two junior doctors.
The team drafts a map of the current endoscopy journey, using repositionable notes on the wall. This allows team members to identify the start (admission to the unit) and completion (discharge) points and the locations thought to be involved in the patient journey.
They decide to use a “walk the journey” format, interviewing staff in their clinical environments and allowing direct observation of the patient’s management.
The junior doctors visit the endoscopy unit over two days, building up rapport with the staff to ensure that they feel comfortable with being observed and interviewed (on a semistructured but informal basis). On each day they start at the point of admission at the reception office and follow the patient journey to completion.
They observe the process from staff and patient’s perspectives, sitting in on the booking process and the endoscopy procedure. They identify the sequence of steps and assess each for its duration (minimum and maximum times) and the factors that influence this. For some of the steps, they use a digital watch and notepad to check and record times. They also note staff-patient and staff-staff interactions and their function, and the recording and movement of relevant information.
Details for each step are entered into a simple table (table 2 ⇓ ), with relevant notes and symbols for bottlenecks and patients’ waits.
Patient journey for non-sedated upper gastrointestinal endoscopy
When data collection is complete, the doctor organises a meeting with the team. The individual steps of the patient journey are mapped on a single long section of paper with coloured temporary markers (fig 2 ⇑ ); additional information is added in different colours. A workflow diagram is drawn to show the physical route of the patient journey (fig 3 ⇑ ).
The performance manager calculates that the total patient journey takes a minimum of 50 minutes to a maximum of 345 minutes. This variation mainly reflects waiting times before a number of bottleneck steps.
Only five steps (14 to 17 and 22, table 2 ⇑ ) are considered both to add value and needed on the day of the procedure (providing patient information and consent can be obtained before the patient attends the department). These represent from 13 to 47 minutes. At its least efficient, therefore, only 4% of the patient journey (13 of 345 minutes) is spent in activities that contribute directly towards the patient’s outcome.
The team redesigns the patient journey (fig 4 ⇓ ) to increase time spent on value adding aspects but reduce waiting times, bottlenecks, and travelling distances. For example, time for discussing the results of the procedure is increased but the location is moved from the end of the journey (a bottleneck) to shortly after the procedure in the anteroom, reducing the patient’s waiting time and staff’s travelling distances.
Fig 4 Workflow diagram of future state endoscopy pathway
Implementing changes and sustaining improvements
The endoscopy staff are consulted on the new patient pathway, which is then piloted. After successful review two months later, including a patient satisfaction questionnaire, the new patient pathway is formally adopted in the peripheral units.
Further reading
Practical applications.
NHS Institute for Innovation and Improvement ( https://www.institute.nhs.uk )—comprehensive online resource providing practical guidance on process mapping and service improvement
Lean Enterprise Academy ( http://www.leanuk.org )—independent body dedicated to lean thinking in industry and healthcare, through training and academic discussion; its publication, Making Hospitals Work 23 is a practical guide to lean transformation in the hospital environment
Manufacturing Institute ( http://www.manufacturinginstitute.co.uk )—undertakes courses on process mapping and lean thinking transformation within health care and industrial practice
Theoretical basis
Bircheno J. The new lean toolbox . 4th ed. Buckingham: PICSIE Books, 2008
Mould G, Bowers J, Ghattas M. The evolution of the pathway and its role in improving patient care. Qual Saf Health Care 2010 [online publication 29 April]
Layton A, Moss F, Morgan G. Mapping out the patient’s journey: experiences of developing pathways of care. Qual Health Care 1998; 7 (suppl):S30-6
Graban M. Lean hospitals, improving quality, patient safety and employee satisfaction . New York: Taylor & Francis, 2009
Womack JP, Jones DT. Lean thinking . 2nd ed. London: Simon & Schuster, 2003
Cite this as: BMJ 2010;341:c4078
Contributors: TMT designed the protocol and drafted the manuscript; TMT, MB, JH, and TH collected and analysed the data; all authors critically reviewed and contributed towards revision and production of the manuscript. TMT is guarantor.
Competing interests: MB is a senior faculty member carrying out research for the Lean Enterprise Academy and undertakes paid consultancies both individually and from Lean Enterprise Academy, and training fees for providing lean thinking in healthcare.
Provenance and peer review: Not commissioned; externally peer reviewed.
- ↵ Kollberg B, Dahlgaard JJ, Brehmer P. Measuring lean initiatives in health care services: issues and findings. Int J Productivity Perform Manage 2007 ; 56 : 7 -24. OpenUrl CrossRef
- ↵ Bevan H, Lendon R. Improving performance by improving processes and systems. In: Walburg J, Bevan H, Wilderspin J, Lemmens K, eds. Performance management in health care. Abingdon: Routeledge, 2006:75-85.
- ↵ Kim CS, Spahlinger DA, Kin JM, Billi JE. Lean health care: what can hospitals learn from a world-class automaker? J Hosp Med 2006 ; 1 : 191 -9. OpenUrl CrossRef PubMed
- ↵ Layton A, Moss F, Morgan G. Mapping out the patient’s journey: experiences of developing pathways of care. Qual Health Care 1998 ; 7 (suppl): S30 -6. OpenUrl
- ↵ Peterson KM, Kane DP. Beyond disease management: population-based health management. Disease management. Chicago: American Hospital Publishing, 1996.
- ↵ NHS Modernisation Agency. Process mapping, analysis and redesign. London: Department of Health, 2005;1-40.
- ↵ Taylor AJ, Randall C. Process mapping: enhancing the implementation of the Liverpool care pathway. Int J Palliat Nurs 2007 ; 13 : 163 -7. OpenUrl PubMed
- ↵ Ben-Tovim DI, Dougherty ML, O’Connell TJ, McGrath KM. Patient journeys: the process of clinical redesign. Med J Aust 2008 ; 188 (suppl 6): S14 -7. OpenUrl PubMed Web of Science
- ↵ King DL, Ben-Tovim DI, Bassham J. Redesigning emergency department patient flows: application of lean thinking to health care. Emerg Med Australas 2006 ; 18 : 391 -7. OpenUrl CrossRef PubMed
- ↵ Mould G, Bowers J, Ghattas M. The evolution of the pathway and its role in improving patient care. Qual Saf Health Care 2010 ; published online 29 April.
- ↵ Rath F. Tools for developing a quality management program: proactive tools (process mapping, value stream mapping, fault tree analysis, and failure mode and effects analysis). Int J Radiat Oncol Biol Phys 2008 ; 71 (suppl): S187 -90. OpenUrl PubMed Web of Science
- ↵ Womack JP, Jones DT. Lean thinking. 2nd ed. London: Simon & Schuster, 2003.
- ↵ Graban M. Value and waste. In: Lean hospitals. New York: Taylor & Francis, 2009;35-56.
- ↵ Westwood N, James-Moore M, Cooke M. Going lean in the NHS. London: NHS Institute for Innovation and Improvement, 2007.
- ↵ Liker JK. The heart of the Toyota production system: eliminating waste. The Toyota way. New York: McGraw-Hill, 2004;27-34.
- ↵ Womack JP, Jones DT. Introduction: Lean thinking versus Muda. In: Lean thinking. 2nd ed. London: Simon & Schuster, 2003:15-28.
- ↵ George ML, Rowlands D, Price M, Maxey J. Value stream mapping and process flow tools. Lean six sigma pocket toolbook. New York: McGraw Hill, 2005:33-54.
- ↵ Fillingham D. Can lean save lives. Leadership Health Serv 2007 ; 20 : 231 -41. OpenUrl CrossRef
- ↵ Benjamin A. Audit: how to do it in practice. BMJ 2008 ; 336 : 1241 -5. OpenUrl FREE Full Text
- ↵ Vissers J. Unit Logistics. In: Vissers J, Beech R, eds. Health operations management patient flow logistics in health care. Oxford: Routledge, 2005:51-69.
- ↵ Graban M. Overview of lean for hospital. Lean hospitals. New York: Taylor & Francis, 2009;19-33.
- ↵ Eaton M. The key lean concepts. Lean for practitioners. Penryn, Cornwall: Academy Press, 2008:13-28.
- ↵ Baker M, Taylor I, Mitchell A. Analysing the situation: learning to think differently. In: Making hospitals work. Ross-on-Wye: Lean Enterprise Academy, 2009:51-70.
- ↵ Ko HH, Zhang H, Telford JJ, Enns R. Factors influencing patient satisfaction when undergoing endoscopic procedures. Gastrointest Endosc 2009 ; 69 : 883 -91. OpenUrl CrossRef PubMed Web of Science
- ↵ Del Rio AS, Baudet JS, Fernandez OA, Morales I, Socas MR. Evaluation of patient satisfaction in gastrointestinal endoscopy. Eur J Gastroenterol Hepatol 2007 ; 19 : 896 -900. OpenUrl CrossRef PubMed Web of Science
- ↵ Seip B, Huppertz-Hauss G, Sauar J, Bretthauer M, Hoff G. Patients’ satisfaction: an important factor in quality control of gastroscopies. Scand J Gastroenterol 2008 ; 43 : 1004 -11. OpenUrl CrossRef PubMed Web of Science
- ↵ Yanai H, Schushan-Eisen I, Neuman S, Novis B. Patient satisfaction with endoscopy measurement and assessment. Dig Dis 2008 ; 26 : 75 -9. OpenUrl CrossRef PubMed Web of Science
Nursing and the Patient Journey
- First Online: 22 September 2023
Cite this chapter

- Barbara Sassen ORCID: orcid.org/0000-0001-8354-7885 2
557 Accesses
Patient mapping or patient journey, a tool used to visualize the patient journey, is beneficial in understanding the patient’s experience with healthcare. It highlights what contributes to good care and what does not from the patient’s perspective.
Additionally, the concept of the patient journey is used in the context of quality of care to refer to the path a patient takes through the healthcare system. By viewing the journey from the patient’s perspective, the effectiveness and efficiency of care can be improved by eliminating ineffective or unnecessary treatments. This can lead to a redesign of the patient’s journey with the goal of increasing patient satisfaction and improving the quality of care. Achieving this requires healthcare providers to align care with the patient’s perceptions, preferences, and expectations.
Understanding the patient experience within the healthcare system is important particularly using patient journey mapping. This involves mapping out the process a patient goes through, from diagnosis to discharge, to identify areas for improvement and to make care more efficient and effective. The focus should be on activities valued by patients to improve patient satisfaction. Process mapping is also used to optimize care processes, but it often lacks a patient-centered approach. The text emphasizes the importance of incorporating patient satisfaction into medical protocols, guidelines, and ethical standards. A care continuum is also preferable from a patient perspective, where care providers maintain continuous contact with their patients to avoid gaps in care and ensure effective care outcomes.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as EPUB and PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Bate P, Robert G. Experience-based design: from redesigning the system around the patient to co-designing services with the patient. Qual Saf Health Care. 2006;15:307–10. https://doi.org/10.1136/qshc.2005.016527 . (This is based on mapping a consecutive series of ‘touch points’ between the patient and the service where patient experience is actively shaped).
Article PubMed PubMed Central Google Scholar
Elliss-Brookes L, McPhail S, Ives A, Greenslade M, Shelton J, Hiom S, et al. Routes to diagnosis for cancer—determining the patient journey using multiple routine data sets. Br J Cancer. 2012;107:1220–6.
Article CAS PubMed PubMed Central Google Scholar
Gregory M. A possible patient journey: a tool to facilitate patient-centered care. New York, NY: Thieme Medical Publishers; 2012.
Google Scholar
McCarthy S, O’Raghallaigh P, Woodworth S, Lin Lim Y, Kenny LC, Adam F. An integrated patient journey mapping tool for embedding quality in healthcare service reform. J Decis Syst. 2016;25:354–68. Published online: 16 Jun 2016. https://doi.org/10.1080/12460125.2016.1187394 .
Article Google Scholar
Trebble TM, Hansi N, Hydes T, Smith MA, Baker M. Process mapping the patient journey: an introduction. BMJ. 2010;341:c4078. https://doi.org/10.1136/bmj.c4078 .
Article PubMed Google Scholar
Download references
Author information
Authors and affiliations.
University of Applied Sciences, Utrecht, The Netherlands
Barbara Sassen
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Barbara Sassen .
Rights and permissions
Reprints and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Sassen, B. (2023). Nursing and the Patient Journey. In: Improving Person-Centered Innovation of Nursing Care. Springer, Cham. https://doi.org/10.1007/978-3-031-35048-1_26
Download citation
DOI : https://doi.org/10.1007/978-3-031-35048-1_26
Published : 22 September 2023
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-35047-4
Online ISBN : 978-3-031-35048-1
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
- Open access
- Published: 20 October 2023
Navigating the facilitation journey: a qualitative, longitudinal evaluation of ‘Eat Walk Engage’ novice and experienced facilitators
- Gillian Harvey 1 , 2 ,
- Sarah Collyer 1 ,
- Prue McRae 3 , 4 ,
- Sally E. Barrimore 5 ,
- Camey Demmitt 6 ,
- Karen Lee-Steere 3 , 7 ,
- Bernadette Nolan 8 &
- Alison M. Mudge 3 , 9
BMC Health Services Research volume 23 , Article number: 1132 ( 2023 ) Cite this article
932 Accesses
7 Altmetric
Metrics details
The Promoting Action on Research Implementation in Health Services (PARIHS) and integrated-PARIHS (i-PARIHS) frameworks position facilitation as an overarching strategy to enable implementation. In the revised i-PARIHS framework, facilitation is operationalised through a multi-level model with novice, experienced and expert facilitators working together in a network structure to build facilitation knowledge and skills along a continuum. To date, there has been limited evaluation of this facilitation model in practice, which is the aim of the study reported here.
A descriptive, qualitative longitudinal study was undertaken to track a team of four novice and two experienced facilitators involved in facilitating the implementation of an intervention known as ‘Eat Walk Engage’ to improve multidisciplinary team delivery of age-friendly care principles in hospital. Over an 18-month period, repeat interviews were conducted to explore the learning, development, and evolving roles of novice facilitators and the roles of the experienced facilitators in providing support and mentoring. Interview data were analysed using a descriptive qualitative approach and findings were interpreted in collaboration with the participating facilitators.
The findings demonstrated experiential learning in both the novice and experienced facilitator groups as they enacted their roles in practice. The novice facilitators progressively transitioned to becoming more experienced facilitators and the experienced facilitators became increasingly expert, in line with the i-PARIHS concept of a facilitation journey from novice to expert. Strategies to support this development included a staggered approach to learning, regular meetings between the experienced and novice facilitators, reflective writing and informal peer support and networking. However, the roles were not without challenge and these challenges changed over time, from a more specific focus on the demands of the facilitator role to concerns about embedding and sustaining improvements in practice.
Conclusions
Within a network of peers and a mentored relationship with more experienced facilitators, individuals who are new to an implementation facilitator role can transition along a continuum to become experienced facilitators. Building implementation facilitation capability in this way takes time and requires tailored support and mentorship using a mix of structured and flexible approaches incorporating opportunities for reflection to support individual and group learning.
Peer Review reports
Contribution to the literature
The i-PARIHS framework proposes a networked model of novice, experienced and expert facilitators. This study is one of the first empirical evaluations of the i-PARIHS facilitation model in practice.
The study demonstrates that a facilitation network, where less experienced facilitators have a mentored relationship with more experienced facilitators, supports experiential learning and development of facilitation ‘know-how’. In turn, facilitator roles can evolve over time, from a specific project to a wider organisational focus.
Facilitation is a dynamic process and journey. A combination of formal and informal strategies helps to structure and support facilitator learning and development.
Facilitation is a resource-intensive implementation strategy. Future research could investigate when and how facilitation produces an acceptable return on investment.
Facilitation is positioned as an overarching implementation strategy, with a focus on enabling others to implement innovations and improvements in practice, as opposed to telling, directing, or using persuasion to encourage change [ 1 ]. It encompasses facilitator roles and facilitation strategies that are aligned with a philosophy of enabling and empowering others to act. It has been adopted as an approach to implementation across a broad range of initiatives in health care in different settings, different countries and for different interventions [ 2 ]. These facilitation approaches are often underpinned by the Promoting Action on Research Implementation in Health Services (PARIHS) and integrated-PARIHS frameworks [ 3 , 4 , 5 ], which explicitly position facilitation as the active agent for implementation, unlike many other implementation theories, frameworks, and models. Facilitators can be external or internal to the organisational setting and use a wide range of discrete implementation strategies, combining and tailoring these to the specific implementation initiative and context in which they are working [ 6 ]. Enacting the role involves a combination of so-called ‘hard and soft’ skills, including project management, problem solving, stakeholder engagement, relationship building, communication, teamwork, negotiation, and evaluation (see Table 1 ).
Facilitation in the PARIHS and i-PARIHS frameworks
The original PARIHS framework proposed that the successful implementation of evidence into practice was a function of the interplay between the nature of the evidence to be implemented, the context where implementation was occurring and the way in which the process was facilitated [ 3 ]. The development of PARIHS was informed by experiential knowledge of working as facilitators of quality improvement and practice development, where the emphasis was on embedding change at a local level through enabling participation, engagement, and ownership of the changes to be implemented [ 3 ].
In response to application, evaluation, and critiques of the PARIHS framework over several years [ 12 , 13 , 14 , 15 ], the framework was revised to the i-PARIHS framework, with a more explicit focus on operationalising the facilitation construct [ 5 , 16 ]. This involved a more detailed description of facilitation roles and functions and a facilitator’s ‘toolkit’ to support facilitation activities at the level of an implementation project [ 16 ]. i-PARIHS recognises the complex nature of facilitation, encompassing a broad range of discrete implementation strategies (including, for example, interactive education, audit and feedback, quality improvement methods, reminder systems), and identifies the experiential development of knowledge and skills to fulfil the role. It proposes a network of facilitators with a continuum of expertise from novice to experienced and expert facilitators whereby facilitators who are new to the role are developed, mentored, and supported by facilitators who are more experienced [ 9 ]. As such, novice facilitators embark on an experiential journey to build their skills, confidence, and ability in the role, typically starting off facilitating a defined implementation project within a local setting. As their knowledge, skills, and confidence build, they move to work at a wider organisational level and may develop, mentor, and support a new set of novice facilitators, in turn guided and supported by an expert facilitator, who is generally external to the organisation. In this way, a network of facilitators is established, and facilitation capability is expanded within an organisation.
As transition along the facilitation continuum occurs, additional skills and knowledge are required, such as influencing and negotiating skills to address organisational level barriers to implementation (for example, time for clinical staff to participate in implementation projects or educational programs to support acquisition of new knowledge and skills) and political skills to understand the wider policy environment (with associated levers or mandates for change) in which implementation is taking place. The i-PARIHS framework illustrates this multi-level model of facilitation within a spiral of contextual levels, each exerting different influences on implementation and requiring a different focus from a facilitator perspective (see Fig. 1 ). Table 2 summarises the typical role and activities that the different facilitator roles would be undertaking.
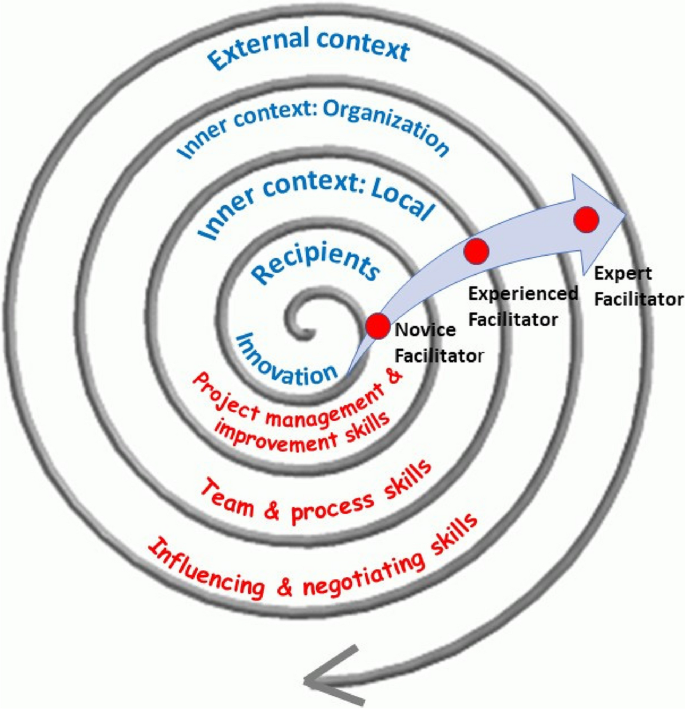
Levels of facilitation focus and activity
There has been limited evaluation of the facilitation journey proposed in the i-PARIHS framework, particularly in terms of how facilitators acquire skills and build expertise over time. As illustrated in Table 1 , previous studies have identified the types of activities that facilitators undertake and related knowledge and skill requirements. However, having a taxonomy of facilitation activities is not the same as being able to apply them in practice. As Ritchie and colleagues note, this requires tacit knowledge and processes in place to support experiential learning [ 11 ]. In their recently published study, informed by the i-PARIHS framework, the authors examined an external expert facilitator working with two novice facilitators and identified 21 techniques that were used by the expert to transfer implementation facilitation skills. These encompassed a range of cognitive, psychosocial, self-learning and structural learning supports, encompassing both active (providing information, modelling, and coaching) and participatory methods [ 11 ].
The current study aims to build further understanding of the development of facilitation ‘know-how’ by following the longitudinal journeys of four novice facilitators over an 18-month period. The specific objectives of the paper are to:
Assess the learning, development, and evolving role of novice facilitators in the implementation of a complex inpatient intervention ‘Eat Walk Engage’.
Explore the roles of the two experienced facilitators supporting and mentoring the novice facilitators.
Compare the theoretical model of facilitation (informed by i-PARIHS) with what happened in practice.
The eat walk engage intervention
Eat Walk Engage (EWE) is a hospital ward-based programme developed to improve multidisciplinary team delivery of age-friendly care principles (adequate nutrition and hydration, early regular mobility, and meaningful cognitive and social activities) to reduce hospital-associated complications in older inpatients [ 17 , 18 ]. The implementation component of EWE is underpinned by the i-PARIHS framework and involves a trained novice site facilitator working with a local multidisciplinary work group to implement the intervention.
Following initial pilot testing and refinement of EWE, a hybrid effectiveness-implementation cluster randomised trial—the Collaborative for Hospitalized Elders: Reducing the Impact of Stays in Hospital (CHERISH)—was undertaken between October 2016 and May 2017 to evaluate implementation of EWE in four hospitals. Implementation involved a local site (novice) facilitator (one for each hospital) establishing and facilitating a ward-based multidisciplinary work group to implement EWE within their own setting. The novice facilitators were allocated 16 h per week to undertake the role and received support from 2 experienced facilitators who had been responsible for the development and prior testing of EWE. These experienced facilitators (AM, PM) were clinician researchers (with backgrounds in general medicine and physiotherapy) employed within one of the hospitals and were principal investigators for the overall evaluation study. The experienced facilitators' time commitment totalled 24 h per week to provide project management, external facilitation across the project sites, and mentoring and support of the novice facilitators. Initial group training was delivered by the experienced facilitators over 4 half-days, guided by the i-PARIHS facilitator’s toolkit [ 16 , 19 ]. Thereafter, the experienced and novice facilitators all met together for monthly mentoring sessions in the form of half-day face-to-face peer group meetings. Informal individual telephone and email support was provided on an as needed basis between meetings. The experienced facilitators also visited each ward that was implementing EWE before and during the implementation period to meet key stakeholders and participate, alongside the novice facilitator, in the multidisciplinary work group meetings. This included providing one on one support as required for particular activities (e.g. reflecting on local context, undertaking observational audits). External advice for the experienced facilitators was provided via a project implementation steering group, which included other experienced and expert facilitators (GH, IB, AY), along with a consumer representative.
Details of the study and its effect of a significant reduction in hospital-associated delirium have been published previously [ 20 , 21 ]. The accompanying process evaluation paper [ 22 ] documents how the implementation of EWE occurred across the four different hospital settings and identifies the multiple strategies that novice facilitators used to facilitate 45 discrete improvements in care. This paper focuses on the experiences of the novice and experienced facilitators, including their perceived learning and development, as they enacted their roles to support the implementation of EWE.
A descriptive qualitative longitudinal design was applied to track the novice and experienced facilitators supporting the implementation of EWE.
Participants and data collection
Participants were four novice site facilitators (NFs 1–4) and two experienced facilitators (EF1 and EF2). The novice facilitators were mid-level health professionals from allied health (dietetics and occupational therapy) and nursing backgrounds, who were recruited from within the hospital. Most had previous involvement in quality improvement, patient safety and/or clinical guideline initiatives and shared the part-time facilitator role with another clinical or project role within the same hospital, which was separate from the CHERISH study. The experienced facilitators also had previous experience in implementation, quality improvement and facilitation. All 6 facilitators (novice and experienced) were female. Semi-structured interviews with novice ( n = 4) and expert ( n = 2) facilitators were conducted (by GH) at 3 time points over an 18-month period: early, mid, and post-implementation (Table 3 ). Each interview lasted 45–60 min and was conducted face to face. Participants were offered the opportunity to review their individual transcription for verification purposes. Verbal consent was given, and interviews were recorded and transcribed verbatim.
Data analysis
Transcripts were analysed using a descriptive qualitative approach [ 23 ]. Transcripts were read multiple times by two of the authors, one who was a member of the implementation steering group (GH) and a second researcher who was external to the implementation study and process evaluation (SC). Content analysis was used to code data, group codes into categories and subsequently identify four major themes [ 24 ]. Analysis was conducted using MAXQDA Analytics Pro 2020 20.4.0. The team of novice and experienced facilitators were engaged in reviewing and interpreting the emergent findings.
Ethical approval
The evaluation was approved by the Human Research Ethics Committee of the Royal Brisbane and Women’s Hospital (HREC15/QRBW/95) and Queensland University of Technology. Interviews were audio recorded with informed consent.
Across the 18-month period of following the novice facilitators, changes were apparent in key aspects of the role, reflecting experiential learning and progression along the facilitation journey. These changes are discussed in relation to 4 themes: enactment of the facilitator role; learning about the role; strategies to support learning and development; and challenges encountered. Key findings relating to these themes at the different time-points of study are summarised in Table 4 .

Enacting the role
Having come into the facilitator role from mid-level allied health and nursing backgrounds, often with some experience in quality improvement, clinical guideline and patient safety initiatives, expectations of what the facilitator role would involve did not always match with the reality. For some novice facilitators, this was influenced by previous experience of project management and an expectation that facilitation would be a project management type role.
I’ve been involved in previous [health service] projects and projects are very different from the way in which this program is run and the principles behind it. I think going into it I probably had expected it to be more project like and utilising probably more concrete project management skills and for some more clearly defined timeframes for key markers of accomplishment, I guess you’d say, but I think in fact that mindset has changed quite considerably. [NF4]
Once in the facilitator role, expectations began to change as the novice facilitators recognised the importance of a more organic approach empowering others to take ownership of the implementation process.
I guess my view has changed and something that has changed in my thinking is I’m not the strategy and I’m not going to be fixing things, I’m building capacity on the wards. …. so working out what other people need to do or who to talk to, to get something happening rather than telling people what they need to do, if that makes sense? [NF3]
This involved a considerable amount of initial work to build connections and relationships, identify potential supporters and generally understand the “ lay of the land ” [NF3]. Novice facilitators engaged in a range of activities to support this groundwork, including one-on-one meetings with key individuals, informal coffee catch-ups and spending time in the implementation context to observe and shadow typical clinical activity.
Around 6 months into the role, novice facilitators appeared more confident and comfortable with the flexible nature of the facilitation role, compared to what they had originally expected and could see that it would lead to more sustainable change in the longer-term.
… I’m able to kind of step away from that project manage-y kind of feeling about … ticking off this and this and this and that and ‘we’ve done that and we’ve done that’. You have to have an element, I suppose, of some organisation in with it but it’s more flexible and it can be fluid and I’m trying to put it back to others as well, to take some of that ownership [NF1]
However, the extent to which they were facilitating ward-based work group meetings without one of the experienced facilitators present was variable. For example, one novice facilitator had not yet facilitated any meetings on her own, whereas another had done all but one without the presence of the experienced facilitator. From the experienced facilitator perspective, the novice facilitators had required more support than originally anticipated, including training in interpreting and presenting data, and on-site meeting support.
I feel like we’re investing a lot in facilitator support but they’re responding really well to that and I think if we didn’t they would be at sea so I think it’s been critical to have that really quite - you know, a lot of hand holding early on and then giving them a lot more autonomy as time has gone by. [EF2]
As the novice facilitators became increasingly confident, the experienced facilitators were able to move towards providing less directive input.
At the beginning, it was much more directive, or content driven, and then it very rapidly became – you know, so the last four meetings have really not been us talking, it’s been them talking. [EF1]
By the completion of the study, the novice facilitators reflected on how their expectations of a facilitator role had changed significantly over time, in terms of becoming less structured, more patient with the pace of progress and recognising that they needed to be in it for the long term to achieve the desired changes in care. As novice facilitators grew in confidence, it was also clear to see that they were moving from working solely at the inner context level to greater involvement at the organisational context level, building new relationships and engaging in wider discussions, partly due to the deliberate strategy of the experienced facilitators.
We really pushed, and supported, and mentored, a lot [ into the] organisation context rather than the ward context – challenging, and actually needed quite a lot of support, but actually managed really well. [EF1]
Learning about the role
As they started out in the role, novice facilitators began to develop insights into what the role involved and the implications in terms of their own learning and development. For some, this involved becoming clearer about the distinction between facilitation and management:
I guess probably the biggest area I will be learning or getting some more knowledge and skills and learning I think will be that concept of facilitation versus sort of management ….. I think that’s going to be really interesting and really good, to have those skills and learn those skills … but I can foresee initially it’s going to be hard to bite my tongue, so to speak [NF2]
Similarly, other novice facilitators talked about accepting the need for greater flexibility and patience in guiding or nudging people along “ so that they think they have done it all by themselves ” [NF1]. One novice facilitator described this as requiring a degree of intuition, accompanied by reflection to build skills and confidence.
I think you have to be a little bit intuitive to some degree to be able to go with it but still be going - having that feedback loop for yourself and for your own professional practice that you know you’re going in the right direction because that’s where the confidence needs to come from as well because it is very organic... [NF4]
Whilst the initial training had helped novice facilitators to prepare for the role, they recognised that this would probably need to be re-visited once implementation projects were underway and issues and challenges presented in real-time. In terms of their role within the wider project, novice facilitators described themselves as working at the inner context level – the middle of the i-PARIHS spiral [NF3] – and relying on the experienced facilitators to function at the wider organizational context level.
Novice facilitators described learning about themselves, the facilitator role, and the facilitation process over time. After the first 6 months or so, they recognised a range of improvements in terms of their skills and knowledge, including how to read group dynamics more accurately, managing group processes and conflict, learning how to pace activities, negotiating without coming across as too directive, knowing what facilitation approaches to use when and the importance of engaging with key stakeholders such as the Nurse Unit Manager.
I feel like I’ve come a long way from six months ago, mostly I think just in terms of being able to engage at a variety of different levels and being a little bit more sensitive to the needs of the various groups on the ward. …. I have a better understanding of how to go in softly I guess and, yeah I guess use different techniques for different individuals to gain and build relationships and get their opinions and try and see where their aims for the ward would kind of drive things. [NF4]
Evidence of the enabling focus of facilitation was clear in the way that one of the novice facilitators described the skill of “ giving that sense of accomplishment back to the staff ” [NF1], citing an example where they had helped to get the meal delivery times to the ward changed.
I think one of the things to learn is not taking the glory for this, so presenting back at the next meeting and …. saying ‘this is what the team came up with. This is what the team, as a team, was able to influence and change. This is the outcome’. [NF1]
Encouraging the identified ward champions and team members to take ownership of implementation became more apparent as the novice facilitators gained knowledge, skills, and confidence in the role and moved away from a directive, project management style of affecting change.
The way they interact at their working group meetings is much more ‘tell me what you think. Tell me how you think this would work’ rather than ‘you need to do this’. [EF1]
Strategies to support learning and development
Both formal and informal strategies were in place to support learning and development of the novice facilitators, including monthly face-to-face meetings for the 4 novice facilitators with the experienced facilitators and weekly telephone support. The way in which the experienced facilitators worked with the novice facilitators was “practice-based support” [NF4], which was helpful and pragmatic.
I would say like one of the things I really have liked about working with [the two experienced facilitators] is that …. they’re a bit more down to earth where I tend to really get - that perfectionist in me comes out …. I guess it helps to decrease my nervousness around that because they are pretty easy to work with and they have a bit more of a laid-back style. …. You know, they’re realistic so I think that that’s been really good and helpful so from that point of view it’s been wonderful. [NF1]
The experienced facilitators deliberately adopted this approach, based on their experience of an earlier pilot study of the EWE intervention. This informed their decision to adopt a staggered approach to learning rather than conducting a period of intense training at the start of the project.
We started with some nice, structured tasks ‘okay, go and interview ten patients and come back and put it together’ and how would we display it? … then they were starting to get to know the environment and then we started introducing the key concepts of facilitation, like engaging and measuring and assessing and things. That worked much better. [EF2]
Alongside the more structured learning mechanisms, a growing sense of teamwork and peer support amongst the novice facilitators was apparent and was helping to building skills and confidence.
We usually kind of send out emails to each other like ‘help’ if we have a problem and that’s been really good. I think that’s really nice, to have the other facilitators around the same stage as where I’m at because you can bounce ideas off each other or … just knowing you’re not the only one that has that question. [NF1]
These structured and unstructured opportunities for reflection and learning continued to be centrally important throughout the 18 months of the study, helping the novice facilitators to extend and solidify their learning. Novice facilitators referred to the benefits of learning from hearing each other’s examples of things that had worked well or not so well. Additionally, the novice facilitators had reflective journals ( the little pink book – NF2) which they used in different ways to record thoughts, reminders, notes from mentoring meetings or key events.
I probably don’t use it as much as some of them do. I don’t write a daily entry, or whatever, I tend to write when I have a key interaction, so a real leverage moment, I guess you’d call it. [NF4] I wasn’t sure how to use this book initially but what I’ve changed it into is each week, on a Thursday or Friday, I just write down the three big -- couple of big things of what’s happened that week or what I’ve spent my time doing that week and then things to follow up for the next week or query people to talk to. [NF3]
Regular novice facilitator and experienced facilitator meetings were viewed by both parties as critically important, providing a safe space for bidirectional learning, sharing, support, mentoring and debriefing. Although the experienced facilitators “ didn’t anticipate quite so much face to face, peer to peer support”, they believed it was an “incredibly valuable” component of the facilitation model [EF2].
One morning a month we spend three hours all together and we obviously learn more about their context and their recipients […] we learn all sorts of things from them and can reflect on how we’ve done things in different settings […] I think we’re becoming much better facilitators just by watching other people learn as well. [EF2]
Challenges encountered
Starting out in the facilitator role, the types of challenges encountered by the novice facilitators included getting the local implementation working groups established, setting up communication structures and balancing flexibility and project management. Additionally, for some of the novice facilitators, they had to juggle the half-time novice facilitator role with another position, such as a clinical or project responsibility, which meant learning how to manage their time effectively. Concerns were also raised about the need to engage with staff beyond the immediate work group they were responsible for facilitating, particularly where this involved communicating with senior medical staff.
I’ve been getting quite a few questions from some consultants [about the study design]. I feel like my skills are improving in responding to them and not being scared of them when they go … ‘Why are you doing this study like this?’ I feel a bit more confident now and I think that’ll only improve now with [experienced facilitator’s] backing [NF3]
Challenges continued to be faced over time, although they changed in nature as the focus shifted from how the novice facilitator carried out the role to concerns about embedding and sustaining improvements in practice. Concerns related to issues such as staff turnover, maintaining momentum, demonstrating achievements, and convincing others of the value of facilitator roles to support implementation. Novice facilitators commented on a need for ongoing facilitation support as progress appeared to stall or fall back when they were less present on the ward, particularly when other key roles such as the Nurse Unit Manager or ward champions had changed. However, it was difficult to convince some key decision makers of the importance of investing in facilitation roles.
…. they’re not real keen to fund a facilitator because they keep thinking of it as a project officer. I’ve had a meeting with our [senior manager] and tried to explain it to her …. she just doesn’t get it. Like I cannot explain it to her in a way that she understands. [NF1]
Reflecting on problems related to embedding and sustaining change, novice facilitators reinforced the need to engage key champions, both those with an official role in the implementation project and others more widely in the ward and organizational environment. The experienced facilitators also highlighted an important contribution of facilitating communication between individuals and teams responsible for delivering care.
We just come across ward after ward that has no mechanism of daily communication between disciplines, at all, and that has no common picture of what they’re trying to achieve […] That’s so much of what the facilitator, you know, tries to do, and give them permission to talk to each other and come up with shared meaning. (EFs1 & 2]
In this study, we set out to examine how novice facilitators learn and develop knowledge and skills, informed by the i-PARIHS conceptualisation of a mentored journey that is supported by more experienced facilitators. The findings illustrate how, over an 18-month period, the novice facilitators progressively transitioned from novice to more experienced facilitators, consistent with the i-PARIHS proposed facilitation model [ 25 ]. They typically changed from a project management or task-focused approach to a more enabling way of working. They established and encouraged interdisciplinary teams to take ownership of implementing the intervention, and gradually moved from a ward facing to an organisational focus. Throughout this journey, novice facilitators displayed learning about themselves, about the facilitator role and the facilitation process.
The support and input from experienced facilitators were critical to supporting the development process of the novice facilitators. The experienced facilitators, building on their previous experience of facilitation and the development of the EWE intervention, used varying strategies and approaches to meet the individual learning and support needs of the novice facilitators. The methods adopted by the experienced facilitators reflect the findings of the earlier study by Ritchie and colleagues, highlighting the use of so-called ‘active’ and ‘participatory’ techniques to transfer implementation facilitation skills [ 11 ]. Initially the experienced facilitators used more directive and structured approaches, modelling, teaching, and imparting knowledge. As the program progressed, they provided scaffolding for the novice facilitators’ learning and development by exposure to increasingly complex tasks, and gradually encouraging greater autonomy. The pace and timing of moving from a more to less directive approach varied according to the support needs and confidence of individual novice facilitators. For example, some were accompanied by the experienced facilitator for several implementation work group meetings, whereas others were not. This finding is consistent with Heron’s conceptualisation of the facilitator role, whereby facilitators and the groups they are working with operate along a continuum from directive to non-directive facilitation, with corresponding variations in the level of group autonomy [ 26 ]. Other studies of implementation facilitation similarly demonstrate that the process used by external facilitators is fluid, evolves over time and is dependent on the stage of the project [ 8 , 10 ]. The experienced facilitators recognised and adapted to the needs of the novice facilitator in the current study, providing them with a higher degree of support than they had initially envisaged. As others have noted, the experienced facilitator role was heavily support-oriented [ 27 ] and involved emotional support, debriefing, reflecting, problem solving and normalising the challenges faced by novice facilitators.
Alongside the provision of information, coaching and role modelling, the participatory methods identified in Ritchie and colleagues’ research [ 11 ] were critically important. Regular, face to face support between experienced facilitators and novice facilitators emerged as an essential element of the facilitation model in practice. It helped decrease novice facilitators’ feelings of isolation, and provided a supportive environment for debriefing, discussion, and reflection on experiences. Structured opportunities for reflection, including reflective writing, have been shown to contribute to facilitator learning and effectiveness [ 28 ]. The peer relationships and network between the novice facilitators also emerged as an important element in the development of their knowledge, skills, and confidence. It enabled sharing and learning from each other’s experiences, including coping with negative experiences they encountered and providing a safe space to manage their frustrations. In turn, the novice facilitators encouraged networking and team building in their facilitation role at the project level through identifying and engaging key stakeholders and champions and employing strategies to share ownership of EWE with those involved in implementation. However, this proved time-consuming and challenging due to factors such as staff turnover and other local or organisational priorities.
Reflecting on the facilitation continuum and the facilitation roles proposed in the i-PARIHS framework, the study provides initial support for the idea of a mentored facilitation journey from novice to expert. In particular, the findings highlight the importance of role modelling, adopting a team approach and creating a supportive network, which are key concepts within the i-PARIHS facilitation model. Although i-PARIHS proposes three levels of facilitator, in this study, the focus was mainly on novice and experienced facilitator roles, with some expert facilitator mentoring provided through an implementation steering committee. The novice facilitators demonstrated evidence of transitioning to experienced facilitators within the 18-month timeframe of study. Similarly, the experienced facilitators continued to develop their knowledge and expertise through mentoring and working alongside the novice facilitators. This suggests that the i-PARIHS model of facilitation should be interpreted flexibly depending on the nature and scale of the implementation project, and the existing experience and skills of the facilitators.
The findings provide a preliminary indication of the time and support needed to transition from novice to experienced facilitator, bearing in mind that the four novice facilitators studied were experienced health professionals, purposefully recruited for the role of novice facilitator. Combined with the extensive mentoring and support required from the experienced facilitators, it is evident that facilitated complex interventions in acute care are resource, time, and support intensive. However, as the facilitation network develops and matures, there is potential for it to function as a self-organising community of practice [ 29 ], which could off-set some of the resource requirements for mentoring and support.
The interview findings further illuminate the findings of the process evaluation [ 22 ], which reports the multiple and diverse activities of the facilitators and the teams they were supporting, and the outcome evaluation [ 21 ], which showed significantly reduced delirium and promising improvements in other outcomes, consistent with the program logic. However, further research is required to measure the impact of facilitation and address the question of whether facilitation produces an acceptable return on investment, particularly over the mid to long term in a changing context, reinforcing a need for greater use of health economics evaluation within implementation research [ 30 ]. A final observation relates to the gender of the facilitators studied in this research, all of whom were female. There is an emerging interest in sex and gender issues in knowledge translation [ 31 ] and this could be an area for further consideration within future research on implementation facilitation.
Limitations
The current study involved a small sample, with only 2 experienced facilitators and 4 novice facilitators working within a multi-site complex intervention programme. However, this allowed for careful attention to be given to the implementation facilitation across differing contexts. Additionally, no interviews were conducted with the experienced facilitators at time-point 1, although the experienced facilitators were encouraged to reflect on the total period of implementation during their interviews and the data collected were suitably representative and rich. Lastly, data collection consisted of semi-structured interviews only. While this was beneficial in gathering rich descriptions of the facilitators’ experience, we did not objectively assess changes in the novice facilitators’ knowledge, skills, or confidence levels. Future research could seek to implement more objective measures of these elements.
Within a network of peers and a mentored relationship with experienced facilitators, the novice facilitators followed in this study transitioned along the facilitation continuum to become experienced facilitators. In moving to a more experienced level, novice facilitators developed their knowledge, skills, and confidence in the role, learning both from each other and from more experienced facilitators. Building implementation facilitation capability in this way takes time and requires tailored support and mentorship using a mix of structured and flexible approaches incorporating opportunities for reflection to support individual and group learning.
Availability of data and materials
The datasets generated and analysed in this research are not publicly available in accordance with local ethics approval but are available from the corresponding author on reasonable request.
Harvey G, Lynch E. Enabling Continuous Quality Improvement in Practice: The Role and Contribution of Facilitation. Front Public Health. 2017;5:27.
Article PubMed PubMed Central Google Scholar
Cranley LA, et al. Facilitation roles and characteristics associated with research use by healthcare professionals: a scoping review. BMJ Open. 2017;7:e014384.
Kitson A, Harvey G, McCormack B. Enabling the implementation of evidence based practice: a conceptual framework. Qual Health Care. 1998;7:149–59.
Article CAS PubMed PubMed Central Google Scholar
Rycroft-Malone J, Kitson A, Harvey G. Ingredients for change: revisiting a conceptual framework. Qual Saf Health Care. 2002;11:174–80.
Harvey G, Kitson A. PARIHS revisited: from heuristic to integrated framework for the successful implementation of knowledge into practice. Implement Sci. 2016;11:33.
Dogherty EJ, Harrison MB, Graham ID. Facilitation as a role and process in achieving evidence-based practice in nursing: a focused review of concept and meaning. Worldviews Evid Based Nurs. 2010;7(2):76–89.
PubMed Google Scholar
Stetler CB, Legro MW, Rycroft-Malone J, Bowman C, Curran G, Guihan M, Hagedorn H, Pineros S, Wallace CM. Role of "external facilitation" in implementation of research findings: a qualitative evaluation of facilitation experiences in the Veterans Health Administration. Implement Sci. 2006;1:23.
Bidassie B, et al. Key components of external facilitation in an acute stroke quality improvement collaborative in the Veterans Health Administration. Implement Sci. 2015;10:1–9.
Article Google Scholar
Kitson AL, Harvey G. Methods to Succeed in Effective Knowledge Translation in Clinical Practice. J Nurs Scholarsh. 2016;48(3):294–302.
Article PubMed Google Scholar
Baloh J, Zhu X, Ward MM. Types of internal facilitation activities in hospitals implementing evidence-based interventions. Health Care Manage Rev. 2018;43(3):229.
Ritchie MJ, Parker LE, Kirchner JE. From novice to expert: methods for transferring implementation facilitation skills to improve healthcare delivery. Implement Sci Commun. 2021;2:1–14.
Rycroft-Malone J, et al. An exploration of the factors that influence the implementation of evidence into practice. J Clin Nurs. 2004;13:913–24.
Helfrich C, et al. A critical synthesis of literature on the promoting action on research implementation in health services (PARIHS) framework. Implement Sci. 2010;5:82.
Seers K, et al. Facilitating Implementation of Research Evidence (FIRE): an international cluster randomised controlled trial to evaluate two models of facilitation informed by the Promoting Action on Research Implementation in Health Services (PARIHS) framework. Implement Sci. 2018;13:137.
Rycroft-Malone J, et al. A realist process evaluation within the Facilitating Implementation of Research Evidence (FIRE) cluster randomised controlled international trial: an exemplar. Implement Sci. 2018;13:138.
Harvey G, Kitson A. Kitson, Implementing Evidence-Based Practice in Healthcare: A facilitation guide. Oxon: Abingdon; 2015.
Book Google Scholar
Mudge A, McRae P, Cruickshank M. Eat Walk Engage: an interdisciplinary collabroative model to improve care of hospitalized elders. Am J Med Qual. 2015;30:5–13.
Mudge AM, et al. Multidisciplinary quality improvement programme for older patients admitted to a vascular surgery ward. Intern Med J. 2020;50(6):741–8.
Hunter SC, et al. Experiences of using the i-PARIHS framework: a co-designed case study of four multi-site implementation projects. BMC Health Serv Res. 2020;20:573.
Mudge AM, et al. CHERISH (collaboration for hospitalised elders reducing the impact of stays in hospital): protocol for a multi-site improvement program to reduce geriatric syndromes in older inpatients. BMC Geriatr. 2017;17:11.
Mudge AM, et al. Effect of a Ward-Based Program on Hospital-Associated Complications and Length of Stay for Older Inpatients: The Cluster Randomized CHERISH Trial. JAMA Intern Med. 2022;182(3):274–82.
Mudge AM, et al. Implementing a ward-based programme to improve care for older inpatients: process evaluation of the cluster randomised CHERISH trial. BMC Health Serv Res. 2023;23:668.
Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. 2000;23(4):334–40.
Article CAS PubMed Google Scholar
Colorafi KJ, Evans B. Qualitative Descriptive Methods in Health Science Research. Health Environ Res Des J. 2016;9(4):16–25.
Google Scholar
Kitson A, Harvey G. Getting started with facilitation: the facilitator’s role. In: Implementing Evidence-Based Practice In Healthcare. Routledge; 2015. p. 70–84.
Chapter Google Scholar
Heron J. The Facilitator’s Handbook. London: Kogan Page; 1989.
Lessard S, et al. External facilitators and interprofessional facilitation teams: a qualitative study of their roles in supporting practice change. Implement Sci. 2015;11:1–12.
Olmos-Ochoa TT, et al. Reflective writing: a tool to support continuous learning and improved effectiveness in implementation facilitators. Implement Sci Commun. 2021;2:98.
Lave J, Wenger E, Situated Learning. Legitimate peripheral participation. Cambridge: University of Cambridge Press; 1991.
Barnett ML, et al. Collaborating with health economists to advance implementation science: a qualitative study. Implement Sci Commun. 2020;1:82.
Gogovor A, et al. Sex and gender analysis in knowledge translation interventions: challenges and solutions. Health Res Policy Syst. 2020;18:108.
Download references
Acknowledgements
We acknowledge all the participants who engaged in the Eat Walk Engage program.
The study was funded by a Queensland Accelerate Partnership Grant with contributions from the Queensland Department of Science, Information Technology, Innovation and the Arts; Queensland University of Technology; the Australian Centre for Health Services Innovation; and the Metro North and Sunshine Coast Hospitals and Health Services. Professor Mudge was supported by a Metro North Clinician Research Fellowship. The funders had no role in the conduct, analysis or interpretation of the study or writing the manuscript.
Author information
Authors and affiliations.
Caring Futures Institute, Flinders University, Adelaide, Australia
Gillian Harvey & Sarah Collyer
Australian Centre for Health Services Innovation, Queensland University of Technology, Brisbane, Australia
Gillian Harvey
Royal Brisbane and Women’s Hospital Department of Internal Medicine and Aged Care, Brisbane, Australia
Prue McRae, Karen Lee-Steere & Alison M. Mudge
Queensland University of Technology Institute of Health and Biomedical Innovation, Brisbane, Australia
The Prince Charles Hospital, Brisbane, Australia
Sally E. Barrimore
Caboolture Hospital, Caboolture, Queensland, Australia
Camey Demmitt
University of Queensland Faculty of Health and Behavioural Sciences, Brisbane, Australia
Karen Lee-Steere
Queensland Health, Birtinya, Australia
Bernadette Nolan
University of Queensland Faculty of Medicine, Brisbane, Australia
Alison M. Mudge
You can also search for this author in PubMed Google Scholar
Contributions
GH conceived the study. AM, PMc and GH contributed to the initial study protocol. GH conducted the data collection and GH and SC undertook the initial data analysis. All authors contributed to interpretation of the data to inform the drafting of the manuscript. GH and SC drafted the manuscript and all authors reviewed and approved the manuscript.
Corresponding author
Correspondence to Gillian Harvey .
Ethics declarations
Ethics approval and consent to participate.
The evaluation was approved by the Human Research Ethics Committee of the Royal Brisbane and Women’s Hospital (HREC15/QRBW/95) and Queensland University of Technology. Interviews were audio recorded with written informed consent. All the methods included in this study are in accordance with the declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Harvey, G., Collyer, S., McRae, P. et al. Navigating the facilitation journey: a qualitative, longitudinal evaluation of ‘Eat Walk Engage’ novice and experienced facilitators. BMC Health Serv Res 23 , 1132 (2023). https://doi.org/10.1186/s12913-023-10116-3
Download citation
Received : 08 June 2023
Accepted : 04 October 2023
Published : 20 October 2023
DOI : https://doi.org/10.1186/s12913-023-10116-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Facilitation
- Implementation
- Facilitator development
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]

- Patient Journey Mapping
by Tanya Gadsby | Nov 17, 2012 | Graphic Recording , Patient Journey Mapping
UPDATE Jan. 2021: Learn more about the journey mapping process here!
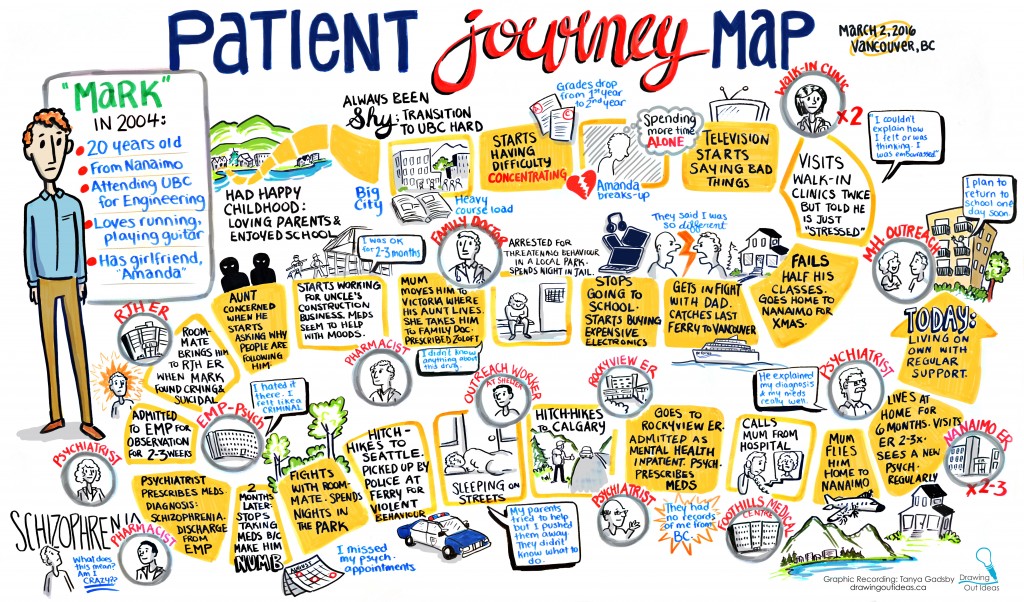
Many organizations get locked into one way of doing business and it never changes year to year, despite advances in technology or changes in customer needs. It’s important for an organization to map out their process of providing service to customers and identify any road blocks or bottlenecks along the way. This leads to improved efficiency and cost savings.
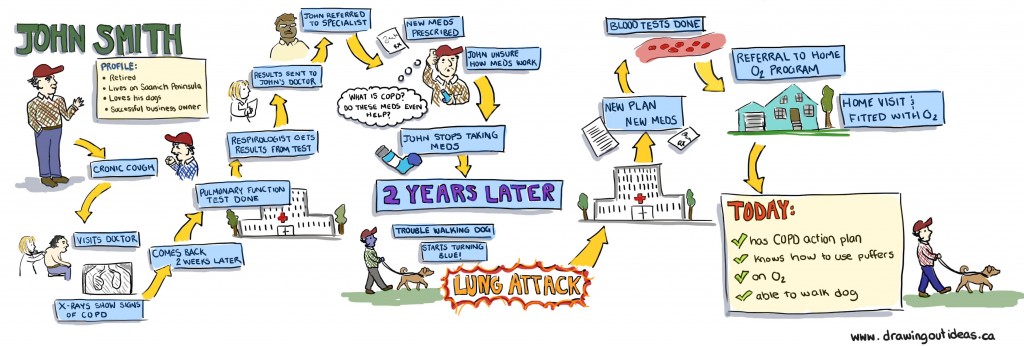
A fictional Patient Journey Map for COPD.
Journey mapping is used in a variety of industries, including healthcare. Patient Journey Mapping brings together physicians, health professionals, and patients for a day-long session of mapping the patient experience. The focus is the patient and plotting their healthcare path through diagnosis, treatment, discharge home, and back again. As the patient journey is mapped, gaps in care are identified and wait times highlighted.
Graphic recording the journey ensures clear communication, especially when dealing with highly complex processes and with many people providing input. Creating a visual map is crucial in maintaining the group’s focus in order to thoroughly map the journey. It’s also important that patients feel they can express their personal stories in a safe environment where their voice is being heard. Graphic recording helps ensure patients feel validated by seeing their words displayed clearly through images. Graphic recording also captures the tone of what’s being said (or not said!).
Once the mapping is complete, it’s easy to send the digital version of the map to other health professionals during the validation process to ensure nothing has been missed.

TANYA GADSBY
Creative Director + Graphic Facilitator
[email protected]
- Augmented reality
- Conference in a box
- Engagement Walls
- Explainer Videos
- Fuselight Team
- Graphic Facilitation
- Graphic Recording
- Hybrid Meetings
- Infographics
- Interactive Graphic Recording
- Journey Maps
- Live Drawing
- Live illustration
- Meeting Engagement
- Online meetings
- projection mapping
- Rich Pictures
- Sketchnotes
- Time-lapse Animation
- Uncategorized
- Virtual Graphic Recording
- Virtual meetings
- Visual Maps
- Visual note-taking
- Visual Notes
- Whiteboard Animation
- Whiteboard Videos
- Zoom Tech Host
LATEST POSTS

Engagement Walls: connecting ideas and people
Mar 7, 2024

The Power of Rough Sketches: Unlocking Creativity During Early Brainstorming
Sep 19, 2023

What’s in a look? Animation styles for explainer videos
Apr 25, 2023
Cookies on NHS Jobs
We've put some small files called cookies on your device to help us make improvements to our site.
To improve our site we'd also like to use cookies which will send information to Google Analytics. You can read more about our cookies before you choose.
Peripatetic Patient Journey Facilitator
The Shrewsbury and Telford Hospital NHS Trust
This job is now closed
Job summary
We are excited to announce a rare opportunity to join our wonderful team! We have a permanent vacancy within our patient journey department
This Peripatetic Patient Journey Facilitator role will be based at The Princess Royal Hospital, Telford and cross site working may be required. You will need to be flexible and provide additional support to the areas where demand exceeds usual activity or where their is annual leave or short/long term absences.
The Peripatetic Patient Journey Facilitators is to facilitate the SAFER Red2Green approach and also to assist the wards with daily discharges.
SAFER Red2Green aims to value patient time and improve flow by reducing delays in a patient's hospital journey.
We are therefore seeking a keen individual with a 'can-do' attitude who is able to work flexibly alongside the Patient Flow team to progress the patient's journey.
The successful candidate will need to be dynamic, proactive and personable. You will need to use great communication skills to be the main point of contact relating to the discharge of patients on ward areas, linking in with social care, therapy services for example. It is important that you use your organisational skills to ensure tasks are completed timely and any concerns are escalated. Ideally, you should have an understanding of SAFER Red2Green approach and the different pathways to ensure the patients' journey is progressed in a timely manner.
Main duties of the job
To provide flexible cover in the event there is a vacant Patient Journey Facilitator post or there is long/short term absence in the team, or to support another Patient Journey Facilitator due to high level of discharges and to work flexibly across the wards as required.
Daily update of database to ensure patients are discharged in a timely manor. Whilst actively seeking to ensure that all patients are managed through their pathway. Where this is not likely to be met; to proactively take steps to ensure that patients investigation and treatment schedules are brought back within target.
To understand the pathway of each individual patient ; monitoring their progress and ensuring timely intervention is achieved.
Attend daily board rounds, and identify the patients who require the support of social services, Pathway Zero or any other support service's to facilitate discharge.
Ensure the accuracy of the information entered on the Computerised SEMA system and that PSAG Boards are updated followed with plans and actions.
The Patient Journey Facilitator's (PJF) role is vital in supporting the wards to ensure patients are discharged from hospital in a safe and timely manner. There are currently 10 PJF supporting the wards across the two sites and are supported by the Medicine Flow Co Ordinators and Service Manager.
The PJF's sit within the Medicine and Emergency Care Division - Patient Flow, along with the Medicine Flow Co-ordinators and Operational Managers and provide support to the medical wards in respect to the patients' journey and their discharge process.
This is a very busy and proactive role, where no two days are the same. The Peripatetic Patient Journey Facilitator role is very diverse. You will work very closely with a range of multi-disciplinary teams (clinical and non clinical) to ensure that the patient's pathway and planned discharge runs smoothly and effective.
Date posted
05 October 2023
Agenda for change
£22,816 to £24,336 a year per annum
Working pattern
Reference number.
223-PPJ-270
Job locations
The Princess Royal Hospital
Apley Castle
Job description
Job responsibilities.
For full duties and responsibilities please refer to the attached document entitled Job Description.
Person Specification
Qualifications.
- 5 GCSE's / O Levels Grade 9 - 4 including English Language and Mathematics
- Medical Terminology
- Extensive experience of working within a health care environment
- Data Collection and Validation
- Understanding of SAFER / Red2Green and Patient Pathways
- MS Office applications
- Fully PC Literate
- Evidence of knowledge of Medical Terminology
- Advanced keyboard skills
- Ability to work to tight deadlines
- Hospital IT Systems
Key Competenacies and Behaviours
- Excellent Communication Skills
- Ability to work on own Initiative
- Experience of working under pressure and to tight deadlines
Disclosure and Barring Service Check
This post is subject to the Rehabilitation of Offenders Act (Exceptions Order) 1975 and as such it will be necessary for a submission for Disclosure to be made to the Disclosure and Barring Service (formerly known as CRB) to check for any previous criminal convictions.
Certificate of Sponsorship
Applications from job seekers who require current Skilled worker sponsorship to work in the UK are welcome and will be considered alongside all other applications. For further information visit the UK Visas and Immigration website (Opens in a new tab) .
From 6 April 2017, skilled worker applicants, applying for entry clearance into the UK, have had to present a criminal record certificate from each country they have resided continuously or cumulatively for 12 months or more in the past 10 years. Adult dependants (over 18 years old) are also subject to this requirement. Guidance can be found here Criminal records checks for overseas applicants (Opens in a new tab) .
Employer details
Employer name, employer's website.
http://www.sath.nhs.uk/ (Opens in a new tab)

For questions about the job, contact:
Clinical Flow Coordinator
Shelbey Fenton-Cook
01743261000
Supporting documents
Privacy notice.
The Shrewsbury and Telford Hospital NHS Trust's privacy notice (opens in a new tab)
- Services overview
- Accreditation & Standards
- Education: Improvement Academy
- Performance & Outcomes Service
- Member organisations
- Member insights
- Member resources
- Become a member organisation
- Assessor Portal
- Become an Assessor
- News & insights
- Our partnerships
- Conferences
- Honours and awards
- Join our team

Introduction to Patient Journey Mapping
One of the most important Design Thinking tools, Patient Journey Mapping, is a human-centred approach to process problem solving.
- Understand the fundamentals of using a patient-centred journey mapping approach;
- Identify and understand key patient segments (personas) and develop a detailed patient journey for a specific segment;
- Learn how patient journey mapping helps you get deeper insights into patient needs, behaviour, experience, motivation and desired outcomes;
- Understand how patients navigate their end-to-end journey and identify where you may be falling short, where silos exist, and interaction points can improve;
- Identify the moments, metrics and outcomes that matter to patients and their care network.
- Clinical managers and medical heads of departments
- Surgical and procedural team leaders
- Directors of patient safety
- Patient safety officers
- Frontline clinicians who provide care and services to patients.
ACHS acknowledges the traditional owners of country throughout Australia and pays its respect to the ongoing living cultures of Aboriginal people.
- Improvement Academy
- News & Insights

Understanding A Patient Journey
Most client histories begin before a person realizes they have a hearing loss and extend long after their final visit to a hearing care professional. By understanding the journey people with hearing loss go through on their path to rehabilitation, professionals can better address their clients’ experiences and collaborate with them for better outcomes.
A Patient Journey assists hearing care professionals in understanding their client’s point of view and recognizing where they are on their journey. It supports students and clinicians in mapping the rehabilitation journey and can be used as a starting point for understanding the complex phases and numerous milestones of hearing loss.
A Patient Journey is based on the Transtheoretical Model — also known as the Stages of Change. The model has six stages (Pre-contemplation, Contemplation, Preparation, Action, Maintenance, and Relapse) and intervention strategies for each to help people move to the next stage. The model was developed in the 1970s through studies examining people who were able to quit smoking on their own versus those who required further treatment to change their behavior.
Patient journeys
The term “patient journey” has been used extensively in the medical field to describe the touchpoints between patients, medical professionals, and stakeholders. The emphasis is usually on how patients proceed through a care system such as a hospital or clinic.
A Patient Journey maps the internal stages of change a person goes through from the realization of hearing loss to successful rehabilitation and management of their hearing loss. Understanding how a typical patient journey may look creates a richer context for the interaction between the client and professional and allows the professional to provide the most appropriate support at the right time.
Traditional medical model
Patient journeys are typically part of the treatment protocol in the medical model. In this model, the approach to gathering information is physician-centered and focuses on problems and symptoms. Clients are not encouraged to share their stories. In the medical model, the professional is the expert and is responsible for what takes place during the appointment. They diagnose the problem, determine a solution, and advise how to proceed with treatment.
In the medical model, the patient intake interview is an exchange of information about the patient's specific illness. Clinicians see and define the journey from the medical point of view. When did the problem start? What are the symptoms? What the medical model does not take into account is that people come into the appointment with unique experiences, social environments, communication needs, and cultural backgrounds.
Toward a person-centered model
One of the most important characteristics of the person-centered approach is that the interaction between the clinician and client is perceived as a partnership. In this case, the hearing care professional is the expert in the field of audiology and the client is the expert in their own experience with hearing loss. In this more responsive model, professionals engage the client in a dialogue that respects their point of view.
According to Miller and Rollnick, motivational interviewing can facilitate behavior change by helping clients to explore and resolve their ambivalence about adopting or ceasing a behavior.
A Patient Journey provides a basis for understanding the client's story and incorporating motivational interviewing in the appointment to empower clients to become joint decision-makers in their treatment plans.
Benefits of a person-centered approach
Abdel-Tawab and Roter found that person-centered consultations took only one minute longer than physician-centered consultations but resulted in a threefold increase in client satisfaction and greater adherence to treatment. The quality of client outcomes is inextricably tied to the ability of the hearing care professional to listen to the client's perspective and to explore their readiness and motivation for treatment — in other words, to provide person-centered care based on an understanding of the client’s individual patient journey.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.14(7); 2022 Jul

Empowering Patients: Promoting Patient Education and Health Literacy
Pradnya brijmohan bhattad.
1 Cardiovascular Medicine, Saint Vincent Hospital, University of Massachusetts Chan Medical School, Worcester, USA
Luigi Pacifico
Patients are generally keen to understand and obtain more information about their medical conditions. There exists a need to develop updated and thorough yet concise patient education handouts and to encourage healthcare providers (HCPs) to use uniform patient education methods.
A thorough review of literature on patient education material was performed prior to starting the study. A comparison with different resources regarding the appropriateness of patient education was done. Educating HCPs to effectively use patient educational materials incorporated into the electronic health record system, including electronic methods, such as the use of a patient portal, to help educate patients.
Strategies were formulated to reduce the amount of processing and attending time required for fetching appropriate materials and lead to fast, efficient, and effective patient education. To improve the physical and psychosocial wellbeing of a patient, personalized patient education handouts, in addition to verbal education by the HCPs, augment the betterment of patient care via shared decision making and by improving patient satisfaction and health literacy.
Introduction
Patients are often eager to understand and know more about their medical conditions and health situation, and educating them with the most relevant, current, consistent, and updated information helps patients and their families significantly in the medical care and decision-making process [ 1 ].
Patients need formal education on the disease condition; they need to know their ailment, understand their symptoms, be educated on the diagnostics, appropriate medication use, and should be taught when to call for help. Several patient education handouts for various conditions are available, and there exists a need to assess which one is better suited for a particular disease/condition encountered and provides concise information. Patient education materials help educate the patients on their health conditions, improves their health literacy, and enhances and promotes informed decision-making based on the most current and updated medical and clinical evidence as well as patient preference [ 2 ].
The aim of this study was to develop updated patient education handouts and materials in addition to verbal counseling of the patients to help them understand the disease condition, diagnostic studies, proper advice on medications, and when to call for help. And to encourage healthcare providers (HCPs) to use uniform patient education materials.
The objectives of this study are 1) the implementation of quality improvement techniques of Plan-Do-Study-Act (PDSA) cycles on patient education in clinical settings; 2) to enhance the delivery of patient education and create awareness amongst the HCPs regarding the importance of patient education and improved health literacy; 3) to verify if patient education handouts have the minimum necessary information that patient should know; 4) to compare patient education handouts from databases integrated in the electronic health record (EHR) with standard patient education database websites like the Centers for Disease Control and Prevention website, and MedlinePlus® site to make sure that they have the minimum necessary information; and 5) to educate and encourage HCPs on the use of appropriate patient education articles in the EHR and utilize an electronic patient portal for patient education, help transition the patient education to an electronic form, and increase efficacy and consistent patient education.
Materials and methods
A comprehensive review of the patient education materials on the most common medical ailments in various clinical settings was performed. We compared the existing patient education database integrated in the EHR with the standard resources such as the CDC, MedlinePlus via retrospective chart study format to ensure the minimum necessary information is available.
A comparison of existing educational material was completed by analyzing other patient education materials from resources such as UpToDate (the basics/beyond the basics), MedlinePlus, US National Library of Medicine of NIH, CDC, and the US Department of Health and Human Services to ensure that effective, most updated, current, and evidence-based information is provided to the patients from the educational materials.
Search words were incorporated to help search for the educational articles in the existing EHR by the title of the article. Educational materials studied were relevant to the common medical ailments in various clinical settings. The patient handouts were made available in such a way that these should be able to be sent either through an electronic patient portal or printed out.
HCPs were educated in a session with pre- and post-lecture survey qualitative and quantitative questionnaires. The impact of these interventions was further assessed by pre- and post-intervention surveys after educating the HCPs.
Uniform updated patient education handouts were created after comparing them with standard resources. A pre-test survey questionnaire was obtained to discuss with HCPs regarding the current knowledge and practices of the usage of patient education handouts and the understanding of EHR to utilize uniform and standardized patient education handouts. After educating the HCPs, their knowledge regarding the use of EHR to effectively use patient education handouts was tested in a post-test survey questionnaire. After completion of the pre and post-test survey questionnaire by HCPs, analysis of the data performed (Figures (Figures1 1 - -20 20 ).

HCPs - healthcare providers

"Do you feel that attending and processing times required for fetching appropriate educational articles will be reduced if standard materials are outlined?"

“Do you think that efficient patient education is effective in creating and improving adherence to treatment, medication compliance, and for improving overall patient health?”

Quality improvement (QI), problem-solving, and gap analysis
QI techniques, including PDSA cycles, to improve patient education implemented in various clinical settings [ 1 ].
Reasons for Action
There is a need for updated and uniform patient education materials in addition to verbal counseling of the patient to help them understand the disease condition, diagnostic studies, proper advice on medications, and when to call for help, thereby enhancing health literacy. There exists several patient education materials for various ailments, and the need to assess which one is better suited for a disease condition and contains concise information.
Initial State
We reviewed the available patient education material from the patient education database integrated in the EHR, and compared it with current standardized resources such as MedlinePlus, US National Library of Medicine of NIH, CDC, and the US Department of Health and Human Services. A thorough review of literature on patient education material was performed prior to starting the study.
We compared more than one source regarding the appropriateness of patient education, most specifically, how to use the medications and when to call for help. The quality of educational materials regarding disease education, diagnostics education, education on medication use, and education on when to call for help was assessed. The resources described above were utilized for comparison.
Gap Analysis
A graph of the gap analysis is displayed in Figure Figure21 21 below.

Solution Approach
It was noticed that the educational materials were available only in printed format. Enrolling patients on the electronic patient portal helps send educational materials to the patient as a soft copy in a faster and more efficient electronic format.
Higher attending and processing time is required for fetching appropriate materials due to the unavailability of exact materials and using non-updated educational materials. Therefore, creating an index of educational articles on commonly encountered medical situations and ensuring that these articles are current and updated might make the process more efficient.
There is a very limited time availability to impart specific educational elements with the limited appointment times. Appropriately detailed educational materials can be sent to the patient via a patient portal even after the patient encounter has ended. For patients with limited technology/computer use, educational materials can be mailed if they're missed during the encounter.
Inadequate educational methods were utilized; thus, incorporating educational articles from resources other than the databases in the existing EHR, and using the index of educational articles on commonly encountered medical situations were applied.
Inefficient usage of the operational capacity of EHR for patient education, using database integrated in the EHR, and lack of training were identified. As a result, HCPs were trained on using educational materials for their patients in an efficient manner, and patient education was prioritized.
Rapid Experiment: Plan-Do-Study-Act Cycle
Plan: Plan to use appropriate patient education material from several sources made available in the index of the educational articles.
Do: Counsel and verbally educate the patients, along with providing educational materials. Obtain a verbal read-back from the patients about how to use medications and when to call for help.
Study: Use the teach-back method to make patients explain back the information provided in their own words to see if they understood the disease, diagnostics, medication use, and when to call for help to improve health literacy.
Act: If a patient has questions, address them appropriately and if need be, set up a follow-up appointment.
Actions Taken
An index of educational materials relevant to the common medical ailments in various clinical settings was created. This index of educational materials was to guide HCPs in choosing appropriate and relevant articles in an efficient, quick, and timely manner for patients in various clinical settings. Effective use of patient educational materials in the database incorporated into the EHR, including electronic methods such as the use of the patient portal to help educate patients, was promoted. Alternate resources other than those from the database in the existing EHR were utilized. Educational materials in printed format were made available for patients with limited technology access. The amount of time required for fetching appropriate materials was reduced by creating and referencing to an index for commonly encountered medical situations.
Efficient and faster patient education was imparted with reduced processing and attending time required. Prioritized health education to improve health literacy. Efficient usage of operational capacity of database integrated in the EHR was undertaken to improve health literacy. HCPs were trained to use patient education materials efficiently.
What Helped
Fast, efficient, and effective patient education helped patients and their families significantly in medical care and shared decision-making based on the most current and updated clinical evidence and patient preference. Creating an index of educational materials relevant to the medical conditions commonly encountered thereby reduced the amount of processing and attending time required for fetching appropriate materials. Effectively using patient educational materials in the database incorporated into the EHR, including electronic methods such as the use of a patient portal to help educate patients, using soft copy (electronic-copy) reduced requirement of printed materials. Correction of misconceptions that patients may have helped improve health literacy.
What Went Well
Helping engage, encourage, and empower the patients in participating in their own health care and treatment decisions. Enhanced patient satisfaction and better outcomes (for instance, educating a patient on osteopenia encouraged them to continue/start the vitamin D supplementation, participate in regular exercise, healthy diet preferences, and health promotion).
What Hindered
High HCP turnover rate with changing schedules hindered consistent use of patient education materials. Insufficient number of HCPs trained for patient education.
What Could Improve
Incorporating educational materials in the video format for patients who do not wish to read or talk about their health situations. Enhanced training of all the HCPs for effective and efficient use of patient education resources to allow consistency in effective patient education.
Personalized patient education engages, encourages, and empowers patients in participating in their own health care and treatment decisions and leading to better outcomes, decreased need for excess diagnostic testing, and enhanced patient satisfaction [ 3 , 4 , 5 ]. This needs motivation on the part of the resident doctors, nurse practitioners, physician assistants, physicians, and the allied staff.
The Advisory Committee on Training in Primary Care Medicine (ACTPCMD) recommends that Health Resources & Services Administration’s (HRSA) Title VII, Part C, Section 747 and 748 education and training programs should prepare students, faculty, and practitioners to involve patients and caretakers in shared medical decision-making which can happen well with better patient education process [ 6 ].
We as HCPs should cultivate good habits amongst ourselves to ensure patients know about their condition and treatment well. This will help increase medication and treatment compliance amongst patients and enhance the physician-patient relationship to a higher level.
Conclusions
To improve the physical and psychosocial well-being of a patient, personalized patient education materials, in addition to verbal education by the HCPs, augment the betterment of patient care via shared decision making and by improving patient satisfaction. There is a need to reiterate that HCPs understand patients' concerns and provide effective patient education and counseling for effective health care delivery.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
For More Information
* required field

How It Works
A. Navigate Patient Journey's website and fill out our submission form. Other options include CALLING us at 305-799-6765 , sending a WHATSAPP message, or using the CHAT feature on our website.
- A. CALL: Our 24/7/365 customer service answers your questions. We connect you to a qualified healthcare provider based on your needs.
- A. EMAIL: Your inquiry is sent directly to a qualified healthcare provider based on your needs.
- B. CHAT: Our customer service is avaible to answers your questions Mon-Sun 8:00am - 6:00pm EST. We connect you to a qualified healthcare provider based on your needs.
B. We will set up a video call with a qualified and certified specialist who will guide you, answer all your questions and eventually perform the procedure(s) you are looking for (no intermediaries). We have found this video call to be the most effective way to get to know each other, answer all your questions and eventually move forward. There is NO COST or commitment on your part for having this video call.
C. After all your medical questions have been addressed, you will receive a quote from the doctor tailored to your specific needs for your approval. Once approved, you will choose a date for your procedure.
- A. Unlike other countries, where post-procedure care might be arranged in a recovery home, all hotel lodging provided meets or exceeds the health and safety standards required by our healthcare provider network.
D. You will also receive a list of suggested hotels near the clinic or hospital where your procedure(s) will be performed. This way you can directly book your lodging with your chosen hotel.
E. We will arrange for a private car to pick you up at the airport when you arrive to Costa Rica, and then back to the airport when you return home. The driver will speak your language.
F. You need to book your own flight to Costa Rica. You will most likely have to fly to San Jose, Costa Rica (airport code: SJO). There may be some cases in which you would fly to Liberia, Costa Rica (airport code: LIR), but we would know this ahead of time so you can book your flight to the right airport.
G. A personal local nurse/companion can be arranged if patient so desires (associated costs will be provided for your approval).
H. Patients will have access to a large network of post-procedure clinics, hospitals and rehab centers upon their return home.
I. Health provider(s) will remain readily available to patients after they have left Costa Rica for any question and/or concerns.
Patient Journey is not an intermediary between patients and healthcare providers in Costa Rica. We connect you directly. Your treatment plan estimate will be the same whether you connect through Patient Journey or directly to any healthcare provider in Costa Rica, who is part of the Patient Journey Network of Healthcare Providers. We have done all the work for you. You'll save days, weeks, months of research...and our services do not cost you a penny!
Healthcare Providers
Your care will be provided by highly educated, trained, experienced and specialized healthcare providers.
Dentists, doctors, nurses and support staff
Studied and trained at the best universities and hospitals in the USA and throughout the world. Click here to learn more about our healthcare providers. Click here to learn more about our healthcare providers. Who are they? Who are they?
Multilingual doctors and support staff
You'll feel right at home because all your communication needs will be met.
Your healthcare is the focal point.
1:2 nurse to patient ratio vs 1:10 on average in most countries.
World-Class Healthcare System
Health care.
Ranked 2nd best healthcare system in the world by Global Health Intelligence
Ranked healthiest country in Latin America
Tico Times/Bloomberg.
Consistent high-quality services
Every doctor and medical facility in the Patient Journey network carries the ProMed (Costa Rica's Health Chamber) seal of approval.
Ideal geographic location
Short, direct flights available from many US cities.
Highest medical standards
Medical facilities that meet the highest medical standards in the world ( Joint Commission International accredited).
Open access
Access to procedures and treatments that may not be accessible where you live due to local, regional or national laws/regulations.
State Of The Art Facilities And Technology
Hospitals and clinics that meet the highest medical standards in the world.

Portfolio Dashboard

Procedures And Treatments
Every dental need is offered, below a few examples:
- Full mouth restoration "All on 4" "All on 6"
- Dental implants
- Dental veneers
- Pediatric dentistry
- Dental resins
- Crown lengthening
Every medical need is offered, below a few examples:
- Orthopedic (knee, hip, etc)
- General surgery
- Otolaryngology (ear)
- Dermatology
- Preventive medical check-ups
Every plastic and cosmetic procedure is offered, below a few examples:
- Breast implants and explants
- Liposuction/Liposculpture
- Gluteal augmentation
- Mentoplasty
- Rhinoplasty
- Hair transplant
Significant Savings
50-70% savings versus your cost at home.
Your Health Insurance Policy May Cover Part Or All Of The Costs Associated With Your Medical Treatment
If your medical procedure is covered at home by your insurance policy, it's very likely it is also covered in Costa Rica as an "out-of-network" provider. You have the right to ask your insurance provider.
You Are Protected
Hospitals, clinics and doctors carry medical liability insurance policies for your protection.
In the remote chance a complication occurs with your treatment, you are protected.

ProMed - An added layer of safety and security.
ProMed is Costa Rica’s health chamber, created exclusively to ensure that international patients visiting Costa Rica receive consistent, high-quality medical and dental services from its members. Patient Journey ONLY offers healthcare providers who carry the ProMed seal of approval.
An extra layer of protection.
You can purchase medical travel insurance that will pay for any unforeseen financial needs during or after your medical treatment trip. IMPORTANT: Covid-19 insurance is mandatory, click here for details.
Costa Rica Is Safe, Modern And Ideally Located
Costa Rica history facts
- Gained independence on September 15th, 1821.
- Slavery abolished in 1824 (The US did it in 1865) & a democracy since 1848 (The US in 1796).
- The Army was abolished in 1948.
- Women were given the right to vote in 1950 (The US in 1920).
International airports
- Costa Rica has two modern international airports: The largest, Juan Santamaría Airport (SJO) and Daniel Oduber Airport (LIR).
- International airports have an expedited immigration process (average immigration and baggage process time at arrival is 25 minutes).
- Short-direct flights available from many US cities.
- Many major airlines fly to Costa Rica.
- Most world citizenships don't require an entry visa to visit Costa Rica, your passport may be all you need.
- Where is Costa Rica?
Rehab Services Right After Surgery and When You Return Home When You Return Home
Rehab options are available for you to use right after your surgery..
You'll be able to start your rehab immediately and before you return home. [ ... ]
Insurance coverage
Your own insurance policy has a rehab network you can tap into. [ ... ]
US-based rehab network
Other rehab centers.

Recovery In Paradise Is An Option
Post-procedure recovery is possible at a beach or mountain resort; it depends on your condition and only with your doctor's approval.
Chat With Us
We have a full time team ready to serve you!
You can also reach us at: (305)799-6765.
1 (305) 799-6765 .--> We look forward to speaking with you!
Thank you for reaching out!
Thank you for contacting us.
We will get back to you within the next 24 hours or less.
Visit our Network of Healthcare Providers and so much more. We are here to help you!
Cookie cleared. Re-run demo
HealingUS Communities

What are 5 Engaging Recovery Group Activities to Foster Healing and Connection?
- Post author: Healing Us
- Post published: May 28, 2024
- Post category: Blog
Recovery groups are crucial forums for people to access support, educate each other, and contribute to recovery. Such groups are usually involved in various activities that help to create a bond and advance recovery . Using activities can significantly facilitate the healing process by supplementing recovery groups with tools, insights, and a sense of community for the participants. These are five group activities that can be useful during the recovery process.
Story Sharing Circles
Story-sharing circles are one of the most useful recovery group activities that encourage members to tell their stories. This activity fosters openness and transparency and is an important part of the healing process. Participants can confront their problems from a different point of view and become less lonely in their everyday lives.
How It Works:
- Preparation: Make arrangements in a comfortable space where everyone can sit in a circle.
- Guidelines: Set the right boundaries for respectful listening and confidentiality so everyone feels safe.
- Sharing: Each participant takes turns telling his or her story. They can give details about their recovery, their achievements, or their current struggles.
- Feedback: It is recommended that after each story is told the group should offer support, ask questions, or share similar experiences so that the listener can relate to the stories.
- Empathy and Understanding: It is possible to develop empathy and group understanding by listening to the stories of other members.
- Emotional Release: Disclosing personal information may help an individual to release suppressed emotions.
- Community Building: It is also an educative activity as learners discover that they are not alone in their troubles.
Art Therapy Sessions
Art Therapy is one type of recovery group activity that can also help promote healing and express oneself. Engaging in creative activities offers the participants a space to express their emotions and experiences without necessarily having to do so verbally, which may be beneficial, especially to those who are not expressive about their emotions.
- Materials: Provide a variety of art supplies such as paints, markers, clay, and paper.
- Theme: Set a theme or message that the group will be focusing on for the meeting, such as “Recovery story” or “Hope”.
- Creation: Give them enough time to make their artwork and encourage them to focus on the process rather than the end product.
- Sharing: At the end of the art-making, have participants present their creations and discuss what it represents to them.
- Self-Expression: Art therapy offers a crucial service by being a place of self-expression and helping to deal with complex emotional experiences.
- Stress Reduction: Engaging in creative activities reduces stress and promotes relaxation.
- Insight and Reflection: Art-making and the sharing of artworks also provide avenues for self-reflection and learning about their recovery process.
Mindfulness and Meditation Practices
Practicing mindfulness and meditation techniques during the process of recovery groups can enhance participants’ self-awareness and emotional intelligence. These practices are very beneficial in managing stress, anxiety, and cravings which are likely to be experienced during the process of recovery from addiction.
- Guided Meditation: Start with a short guided meditation to bring the participants into a relaxed state.
- Mindfulness Exercises: The first mindfulness practices to be adopted are mindful breathing , body scan, and mindful walking, among others.
- Discussion: End the practice with a discussion about the participants’ experiences. They will then be asked to explain how mindfulness and meditation support recovery.
- Stress Reduction: The practice of mindfulness and meditation helps to nullify stress and create a sense of overall composure.
- Emotional Regulation: These practices assist people in learning better emotional regulation skills that are essential for the recovery process.
- Enhanced Focus: Mindfulness exercises can enhance the ability to concentrate and maintain attention, which is useful for both personal and professional purposes.
Group Activities and Games
Incorporating fun and engaging group activities and games into recovery group sessions will help bring together the participants and will assist in developing trust among them. These activities can also provide a much-needed break from the more intense components of recovery work, promoting a balanced approach to healing.
- Icebreakers: Begin with icebreaker activities to facilitate introduction and relationship-building among the participants.
- Team-Building Games: Organize team-building games that involve communication and collaboration, like trust falls, group puzzles, or board games that participants have to play together.
- Reflection: After the games, facilitate a discussion about what participants learned and how they can apply these lessons to their recovery journey.
- Trust and Connection: Team-building games can build trust and strengthen connections among group members.
- Fun and Relaxation: Having fun is an alternative to the work-oriented elements of the recovery process.
- Skill Development: These activities can assist participants in obtaining vital skills such as communication, cooperation, and problem-solving.
Journaling and Reflection Exercises
Journaling and reflection exercises are valuable recovery group activities that encourage introspection and personal growth. Writing about their thoughts, feelings, and experiences can provide clarity and insight, helping individuals make sense of their recovery journey.
- Prompts: Provide journaling prompts related to recovery, such as What are your biggest challenges and how are you overcoming them? or Write a letter to your future self.
- Writing Time: Offer the participants time to complete their journal entries and to be as truthful as possible.
- Sharing: Provide a context for participants to bring their journal entries and share them with the rest of the group if they wish to do so.
- Discussion: Conduct a discussion about the themes and insights that emerged from the journaling exercise.
- Self-Reflection: Journaling promotes self-reflection and can help individuals better understand their thoughts and emotions.
- Emotional Release: Self-expression through writing can be therapeutic, providing emotional release and relief.
- Personal Growth: Daily journaling can help personal development and growth as people can be able to monitor their progress and chart the future.
1. Why are recovery group activities important in the healing process?
Recovery group work is invaluable when it comes to helping participants recover and rebuild relational bonds within the group. These activities are beneficial since they allow people to express themselves and discover more about their experiences while at the same time being able to bond well with others. The participants can complement their healing process with tools, ideas, and social support through such activities as sharing life story circles, art therapy, mindfulness events, group tasks and games, and journaling.
2. How do recovery group activities benefit participants?
Taking part in recovery group activities provides a plethora of advantages for members. These activities foster identification with members of the group, encourage the expression of feelings, contribute towards feelings of belonging and support for fellow members, act as stress busters, and help to relax the spirit. Thus, actions such as painting, meditation, and writing assignments give patients a chance to transform and learn about their healing process.
3. How can individuals and facilitators incorporate recovery group activities effectively ?
Facilitators as well as individuals can apply Recovery Group Activities whereby one has to identify the needs of the recovery group members. The key here is to ensure that the participants feel at ease and are encouraged through their energetic involvement in various activities. Teachers’ interventions should define the goals and procedures of each exercise, promote participation, and support the sharing of ideas within the group. For that reason, another way of making sessions energetic is to include as many activities as possible that may suit the participants’ interests and preferences.
It is crucial to offer meaningful and entertaining recovery group activities that would help clients develop trusting relationships with other members of the recovery group. Story-sharing circles, art therapy sessions, mindfulness and meditation practices, group activities and games, and journaling and reflection exercises each offer unique benefits that can enhance the recovery process. By incorporating these activities into recovery group sessions, facilitators can create a supportive and dynamic environment that promotes healing, connection, and personal growth.
Whether you’re a facilitator looking to enrich your recovery group sessions or an individual seeking new ways to engage in your recovery journey, these activities can provide valuable tools and insights. It’s important to appreciate the power of recovery group activities to transform the healing process and build a stronger, more connected community.
Take the next step in your journey with HealingUS . Join us in supporting healing and connection through engaging recovery group activities.
Please Share This Share this content
- Opens in a new window X
- Opens in a new window Facebook
- Opens in a new window Pinterest
You Might Also Like

Are There Non-Profit Sober Living Homes?

Am I an Alcoholic?

Find Free Recovery Group Meetings Near You
Contact info.
- CFC Loud N Clear Foundation
- Headquarters 260 Casino Drive, Farmingdale, NJ
- Ocean County: 508 Hooper Avenue, Toms River, NJ
- N. Monmouth County: 109 Freneau Ave, Matawan, NJ
- Email: [email protected] Opens in your application
- Opens in a new tab

- Life stories
- Women of Childbearing Age
- Our company
Our Science
Reflections on winning the made with patients award: our journey in parkinson's disease.

With immense pride and humility, UCB’s Patient Engagement Council for Parkinson’s Research (PECPR) initiative has been selected as a winner of the second edition of the Made with Patients Awards. “Made with Patients” is the first global award celebrating innovators in patient engagement. Hosted by Patient Engagement for Medicine Development (PFMD), the award recognizes outstanding contributions across medicine development, MedTech, digital health sectors, and more. It recognizes over two years of dedicated work in Parkinson’s by UCB and our partners, Parkinson’s Foundation and Parkinson’s UK.
For UCB, this also serves as a moment to reflect on our ongoing mission to transform care for those living with Parkinson’s.
The Challenges for Patients The journey for patients with Parkinson’s is fraught with challenges, beginning with the often prolonged and complex diagnostic process. The odyssey from first symptoms to diagnosis can be a harrowing experience for patients and their families, marked by uncertainty and frustration.
Once a diagnosis is made, the road doesn’t get much easier. Current treatments primarily focus on managing symptoms1 without truly altering the disease's relentless progression. While these treatments provide necessary relief, they represent a compromise, not a victory, in the battle against Parkinson’s.
“The experience with the PECPR demonstrates that patients can make an impactful contribution to prioritization, planning, and programming of research. The Council created an open and constructive atmosphere attributing equal weight to the views of everyone participating. PECPR being awarded the Made with Patients award further encourages industry and patient organizations to see us for who we are,” said Marc van Grieken, Parkinson’s patient advocate.
The Path Less Trodden At UCB, we have dared to challenge the status quo, driven by a belief that patients deserve more than symptomatic relief. This paradigm shift demands innovation, courage, and an unwavering commitment to scientific excellence. Our vision extends beyond the current landscape of treatment, aiming to pioneer therapies that can slow down or even halt the progression of these debilitating conditions.
The Importance of Partnership Central to our approach is the principle of partnership, particularly the involvement of patients at every stage of drug development. This collaborative ethos is reflected in our alliances with industry leaders and research institutions, which amplify our capabilities and accelerate our progress towards transformative treatments.
Our partnership philosophy extends to include the most critical stakeholders of all—the patients themselves. From the early stages of research through to clinical trials and beyond, we integrate the patient voice into every facet of our work. We aim to work as true trusted partners with patients. This patient-centric approach not only enriches our understanding but ensures that our innovations truly meet the needs of those we serve.
“It is critical to the Parkinson’s Foundation to engage people with Parkinson’s as partners in everything we do. We are proud to be part of this council which puts the voice of people living with the disease at the forefront,” said John Lehr, President and Chief Executive Officer, Parkinson’s Foundation.
“Parkinson's UK is immensely proud of its longstanding partnership with UCB, Parkinson's Foundation, and the Parkinson's patient community. Our collaboration via the PECPR, showcases how industry, patient organisations and the patient community can work together towards positively impacting research for the benefit of the Parkinson's community,” said Nikul Bakshi, Research Involvement Manager, Parkinson’s UK.
Looking Forward The path to a new treatment paradigm is long and fraught with challenges, but the Made with Patients Award serves as a beacon of encouragement, illuminating our way forward. It is a testament to the dedication of our teams and more importantly, the patients who have been involved in PECPR, including those who are no longer with us. This award serves as a reminder of the lives we strive to improve, and a spur to continue our pursuit of excellence.
Leave a Comment
By submitting your personal data, you agree with UCB's Data Privacy Policy . Furthermore, for more information on the terms of use of this website please visit our Legal Notice, accessible here .
Enter the characters shown in the image.
Our Company
- Sustainability
- Health of the Planet
- Disclosure of payments
- Digital Business Transformation
- Ethical Business Practices
- Our positions
- Disease Areas
- Drug discovery
- Capabilities
- R&D locations
Clinical Studies
- Innovation is
UCB Worldwide
Our products.
- Press Releases
- Our stories
- UCB equity story
- UCB financials
- UCB Governance
- UCB shareholders
- ESG overview
- Download center
- HCP Overview
- Dermatology
- Women of childbearing age
- Immune to the impossible
- Current studies
- Clinical studies index
- General information
- Data Transparency Policy

IMAGES
VIDEO
COMMENTS
Patient journey mapping has an ability to provide detailed information about patient experiences, gaps in health services, and barriers and facilitators for access to health services. This information can be used independently, or alongside information from larger data sets, to adapt and improve models of care relevant to the population that is ...
Build a patient mindset. Patient journey mapping enables you to incorporate more patient-centric thinking into your processes and systems. Use your map to challenge internal ideas of what patients want or need. Invite stakeholders to navigate the touchpoints along the healthcare journey to gain perspective.
Research shows that providers feel ill-equipped to use patient-reported experience information to improve patient care. 22 Garnering an understanding of experience through journey mapping is a more recent development in methodology and application to health care. 17 The present study introduces (1) a set of methods to be considered to advance ...
1. Identify The Goals and Scope of Your Map. Begin by developing a clear vision of what you aim to achieve through patient journey mapping. Whether it's to enhance patient satisfaction, streamline healthcare delivery, or identify gaps in service, setting specific objectives will direct your mapping efforts.
Process mapping enables the reconfiguring of the patient journey from the patient's perspective in order to improve quality of care and release resources. This paper provides a practical framework for using this versatile and simple technique in hospital. Healthcare process mapping is a new and important form of clinical audit that examines how we manage the patient journey, using the ...
Patient journey mapping is a comprehensive discipline that traces a patient's entire healthcare journey, from initial symptoms to treatment and beyond. Understanding this journey is imperative for pharmaceutical companies, enabling them to address challenges and optimize patient-centric solutions.
In this review, patient journey mapping is viewed as a patient-oriented project that has been undertaken to better understand barriers, facilitators, experiences, interactions with services and/or outcomes for individuals and/or their carers and family members as they enter, navigate, experience and exit one or more services in a health system ...
According to the authors, the main arguments in favor of this method are: 1. Improving continuity of care. 2. Better communication - including identifying patient expectations. 3. Continuous improvement - the collection and use of patient data on their journey helps develop a culture of continuous improvement. 4.
Abstract. Patient mapping or patient journey, a tool used to visualize the patient journey, is beneficial in understanding the patient's experience with healthcare. It highlights what contributes to good care and what does not from the patient's perspective. Additionally, the concept of the patient journey is used in the context of quality ...
The novice facilitators progressively transitioned to becoming more experienced facilitators and the experienced facilitators became increasingly expert, in line with the i-PARIHS concept of a facilitation journey from novice to expert. ... patient safety and/or clinical guideline initiatives and shared the part-time facilitator role with ...
The most important part of preparing for a patient journey mapping session is creating as safe a space possible for people to open up about personal experiences. These experiences may be difficult or traumatic, or it may be the first time people are being asked to share feedback about their care. The more welcoming and well planned the space, the better able people can open up and share their ...
By understanding the patient journey, audiologists can address the entire patient experience and collaborate with patients to gain better outcomes. Abstract The concept of a patient journey provides a framework for understanding the complex phases and numerous milestones of life with hearing loss from the perspective of the patient. This understanding can facilitate patient-centered care ...
Patient Journey Mapping brings together physicians, health professionals, and patients for a day-long session of mapping the patient experience. The focus is the patient and plotting their healthcare path through diagnosis, treatment, discharge home, and back again. ... Tanya has been working as a graphic facilitator and graphic recorder since ...
The Patient Journey Facilitator's (PJF) role is vital in supporting the wards to ensure patients are discharged from hospital in a safe and timely manner. There are currently 10 PJF supporting the wards across the two sites and are supported by the Medicine Flow Co Ordinators and Service Manager. The PJF's sit within the Medicine and Emergency ...
Introduction to Patient Journey Mapping. Member price: $500.00 | Price: $555.00. Online. 23 Jul 2024 - 27 Aug 2024, 11AM - 2PM. Register now. One of the most important Design Thinking tools, Patient Journey Mapping, is a human-centred approach to process problem solving.
A Patient Journey is based on the Transtheoretical Model — also known as the Stages of Change. The model has six stages (Pre-contemplation, Contemplation, Preparation, Action, Maintenance, and Relapse) and intervention strategies for each to help people move to the next stage. The model was developed in the 1970s through studies examining ...
Practice Facilitation. Practice facilitation is an approach to supporting improvement in primary care practices that focuses on building organizational capacity for continuous improvement. Practice facilitators are specially trained individuals who work with primary care practices to make meaningful changes designed to improve patients' outcomes.
Identify your patients' biggest pain-points Map out the end -to-end patient journey so you can identify the biggest gaps and opportunities for •improvement Understand how you can remove siloes and harmonise •disparate systems Learn how you can start drawing up a service •blueprint Understand how you can apply these learnings across
Apply to Patient Journey Facilitator jobs now hiring on Indeed.com, the worlds largest job site.
Introduction. Patients are often eager to understand and know more about their medical conditions and health situation, and educating them with the most relevant, current, consistent, and updated information helps patients and their families significantly in the medical care and decision-making process [].Patients need formal education on the disease condition; they need to know their ailment ...
ProMed - An added layer of safety and security. ProMed is Costa Rica's health chamber, created exclusively to ensure that international patients visiting Costa Rica receive consistent, high-quality medical and dental services from its members. Patient Journey ONLY offers healthcare providers who carry the ProMed seal of approval.
Recovery groups are crucial forums for people to access support, educate each other, and contribute to recovery. Such groups are usually involved in various activities that help to create a bond and advance recovery.Using activities can significantly facilitate the healing process by supplementing recovery groups with tools, insights, and a sense of community for the participants.
Whole Health facilitators are trained to offer: Introduction to Whole Health: An educational and experiential course that introduces participants to Whole Health and offers time for self-care and self-exploration through the completion of a Personal Health Inventory. Taking Charge of My Life and Health: This facilitated group program centers ...
Lack of a significant association between CSPAM and PAM scores and change in CSPAM scores suggest that modifying staff beliefs alone is less likely to influence patient self-management, requiring co-production between patients and staff. Background Patient self-management, measured by the Patient Activation Measure (PAM), is associated with reduced healthcare utilisation and better health ...
6 Continuous Learning. The field of patient advocacy is ever-evolving, and as a mid-career professional, committing to continuous learning is crucial. Stay abreast of new healthcare trends, attend ...
Impact. Patient journey mapping is a rapidly growing approach for better understanding how people enter, experience and exit health services. This type of methodology has significant potential to inform new, patient centred models of care and facilitate clinicians, patients and health professionals to better understand gaps and strategies in health services.
Adapt customer journey mapping for different functions to help decision-making for successful project and service delivery. Gain an in-depth understanding of your diverse customers. Identify the broken processes and gaps in your customer interactions. Adopt a customer-centric view of your systems, beyond siloes.
29-May-2024. With immense pride and humility, UCB's Patient Engagement Council for Parkinson's Research (PECPR) initiative has been selected as a winner of the second edition of the Made with Patients Awards. "Made with Patients" is the first global award celebrating innovators in patient engagement. Hosted by Patient Engagement for ...
Meet Alejandra Saitas. 60-year-old Alejandra has been an avid runner since 1994, participating in multiple marathons and triathlons. She and her husband, also an elite runner, traveled to Tokyo in April to run the city's marathon together. After crossing the finish line, she later celebrated her accomplishment at dinner with friends.
At our health center, Spanish-speaking patients were more likely to complete screening mammography compared to patients with English proficiency (53% vs 31% in 2022). To understand this pattern and barriers and facilitators to breast cancer screening, we conducted a mixed methods rapid assessment survey as part of a quality improvement initiative.