
Complications After Dental Treatment
- More Information |
Complications after a dental procedure that include swelling and pain, dry socket, osteomyelitis, bleeding, and osteonecrosis of the jaw comprise another set of urgent dental problems that require prompt attention.
Swelling and pain
Swelling is common after certain dental procedures, particularly tooth removal (extraction) and periodontal surgery. Holding an ice pack—or better yet, a plastic bag of frozen peas or corn (which adapts to the shape of the face)—to the cheek can prevent much of the swelling. Ice therapy can be used for the first 18 hours. Cold should be held on the cheek for 25-minute periods every hour or two. If swelling persists or increases after 3 days or if pain is severe, an infection may have developed, and the person should contact the dentist.
Pain after a dental procedure can be moderate to severe. People can take various pain relievers.
Dry socket (alveolitis)
A dry socket (exposure of the bone in the socket, causing delayed healing) may develop after a lower back tooth has been extracted and the normal blood clot in the socket is lost. Typically, discomfort lessens for 2 or 3 days after the extraction and then suddenly worsens, sometimes accompanied by an earache. Although the condition goes away by itself after 1 to 2 weeks, a dentist can place a dressing soaked with an anesthetic in the socket to eliminate the pain. The dentist replaces the dressing every 1 to 3 days until no more pain is felt after the gauze has been left out for a few hours. Alternatively, dentists often use a commercial dressing that does not need to be removed and that contains an antimicrobial and a pain reliever in addition to an anesthetic. Nonsteroidal anti-inflammatory drugs (NSAIDs) may be taken by mouth if additional pain relief is needed.
Dry sockets are much more common among people who smoke. If at all possible, people should not smoke for several days before and after the extraction is done. Women (especially those taking oral contraceptives) also have a high rate of developing dry socket.
Osteomyelitis
Osteomyelitis is an infection of the bone and is usually caused by bacteria. When osteomyelitis occurs in the mouth, it typically occurs as an infection of the lower jaw. People usually have a fever, and the affected area is tender and swollen. Doctors or dentists use an x-ray to make the diagnosis. People with osteomyelitis need to take antibiotics for an extended period of time.
Osteonecrosis of the jaw
Osteonecrosis of the jaw is a disorder that involves bone death of areas of the jawbones after exposure of the jawbone through the gum tissue. The disorder usually causes pain, loosening of teeth, and a discharge of pus. The disorder may occur after
Tooth extraction
Radiation therapy to the head and neck (osteoradionecrosis)
Use of bisphosphonate drugs in high doses or for long periods
osteoporosis for shorter periods of time.
Treatment typically involves scraping away some of the damaged bone (debridement), taking antibiotics by mouth, and using antibacterial mouth rinses.
Bleeding after a tooth is removed is common. Bleeding in the mouth may appear worse than it is because a small amount of blood may mix with saliva and appear to be more blood than is actually present. Usually, the bleeding can be stopped by keeping steady pressure on the surgical site for the first hour, normally by having the person bite down on a piece of gauze. People may have to repeat the process two or three times. Keeping the gauze (or a tea bag) steadily in place for at least an hour is important. Most problems with bleeding occur because the person frequently removes the pack to see whether the bleeding has stopped. If bleeding continues for more than a few hours, the dentist should be notified. The dentist may need to clean out the bleeding area and surgically close it with stitches (sutures).
More Information
The following English-language resource may be useful. Please note that THE MANUAL is not responsible for the content of this resource.
Mouth Healthy: This resource provides information on oral health, including nutrition and guidance on selecting products that carry the American Dental Association's seal of approval, as well as advice on how to find a dentist and when to see one.

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
- Cookie Preferences

JuniorDentist.com
Oral Care Tips by a Dentist
Enlargement of Lymph Nodes and their related Dental Conditions
February 19, 2020 by Dr. Varun Pandula 8 Comments
Lymphatic System comprises of Lymph nodes in the Facial region which are related to the Oral cavity and are enlarged due to infection of the particular region. Palpation of Lymph nodes helps in Provisional Diagnosis of oral conditions. The Lymph nodes should be checked for tenderness, mobility, enlargement and consistency while performing a Examination. Facial Lymph nodes are divided into three groups – Infaorbital or Maxillary Lymph nodes, Mandibular lymph nodes and buccinator lymph nodes. From these groups the lymph nodes which are relevant to oral cavity are preauricular, submandibular, submental and cervical lymph nodes.
- How to palpate and Examine Head and Neck Lymphnodes
The Lymphatic drainage of the Oral cavity is further divided into Regional nodes and deep cervical nodes based on their position.

Regional Lymph Nodes and their drainage :
- Parotid node on top of the parotid gland which drains into these nodes
- Submandibular nodes located on the lateral wall of the submandibular gland, the cheek region drains into this along with the upper lip, lower lip, maxillary sinus along with upper and lower teeth, the floor of mouth, two thirds of the tongue, vestibule and the gums.
- Buccal Nodes are located on the buccinator muscle over the cheek and transport the lymph collected in the submandibular nodes.
- Submental Nodes are located below the chin in the submental triangle, the tip of the tongue, floor of anterior part of mouth, incisors, the central part of the lower lip and skin on chin drain into these nodes.
- Superficial cervical nodes are located on the external jugular vein and drain the skin over the angle of the mandible along with skin covering the parotid gland.
Palpation of Lymphnodes and its Provisional diagnosis:
- Submental Lymphnodes Enlargement : Infection to Anterior teeth
- Submandibular Lymphnodes Enlargement : Infection of Mandibular Molars
- Angle of mandible lymphnodes Enlargement : Tonsillar infection
- Palpable and Tender Lymphnodes with Fever and swelling : Acute infection
- Palpable Lymphnode with no pain : Chronic infection
- Hard fixed lymph node with stone like consistency : Malignancy
- Nontender and Matted Lymphnodes : Tuberculosis
Palpation of Lymphnodes is a very integral part of Diagnosis and to decide the treatment plan after other diagnostic tests to determine the source of infection.
August 3, 2022 at 4:57 am
Are you aware of any dental conditions that would cause swelling in the lyphatic system in the body of the mandible?
August 16, 2022 at 8:09 am
The swelling of the Sub Mandibular glands can be caused to something as simple as a Mouth Ulcer, tooth abscess or some systemic conditions like Tuberculosis. So it will be difficult to identify a condition just based on swollen Lymph Node, other symptoms should also be taken into consideration to come to a proper diagnosis.
April 13, 2023 at 4:48 am
I would like to know if there is a remedy for hardened lymph nodes? I have one under my lower right jaw area that has acted as a blockage on that side. The onnly thing that i have found that reduces the lymph nodes size is eating only fruit for many weeks. This is not sustainable while in a physical job. The acids accumulated have caused damage to the teeth but i dont see the point in getting any dental work done until the root cause is remedied. Regards, mark
April 14, 2023 at 2:20 pm
Lymph nodes enlargement is usually caused due to an underlying disease, so getting rid of the underlying condition can help solve the problem of enlarged lymphnodes. The nodes under the lower right jaw area is drained into from these regions – cheek, upper lip, lower lip, maxillary sinus along with upper and lower teeth, the floor of mouth, two thirds of the tongue, vestibule and the gums.
So if you are suffering from – Tonsilitis, Sinusitis or any chronic ailment related to any of the above regions it can lead to your Lymph nodes being enlarged.
April 27, 2023 at 12:24 pm
I have much dental work. More porcelain than teeth. I have bilateral lyphodemia and I’m thinking the swelling might be due to dental work. Is that possible for dental root canals could harbor infection somewhere and cause this symptoms of swelling in legs??
May 1, 2023 at 6:20 am
Swelling is legs is an highly unlikely outcome of re-infected root canals but bilateral Lymphedema can be a cause of Prolonged Chronic Infected teeth.
September 8, 2023 at 9:57 pm
If you had a headache and one left side sore, tender occipital node on the same side as dental work done three days prior to remove and old crown and clean out some decay in an area around a molar with a precious root canal, would you assume a connection between the two and would you contact the dentist? There is no fever present. Just one tender occipital node and a head ache and some still aching teeth three days post dental work. Thanks.
September 17, 2023 at 8:04 am
Usually an occipital Lymph node is enlarged in Mandibular teeth infections, it usually comes down in a couple of days post treatment of the affected tooth.
Leave a Reply
Your email address will not be published. Required fields are marked *
Notify me of follow-up comments by email.
Notify me of new posts by email.
- Financing Available
- Emergency Dentist
- Sedation Dentistry

7 Dental Reasons for Swollen Lymph Nodes You Must Address ASAP With A Lymph Nodes Dentist
When your body is actively fighting an infection or disease, your lymph nodes can swell in response. These tiny, bean-shaped glands play a vital role in your immune system, helping your body to recognize, fight, and filter out bad bacteria, viruses, and other harmful invaders. While illnesses like the cold and flu can trigger swelling, dental problems can also lead to lymph node inflammation. Let’s dive in and take a look at 7 dental reasons for lymph node swelling, and why a lymph nodes dentist consult is needed ASAP to prevent complications.
Identifying Dental Conditions That Inflame Your Oral Lymph Nodes
If you have untreated dental conditions such as an infected tooth or gum disease, harmful bacteria can spread to the lymph nodes in the oral cavity and trigger an immune response. This can lead to swelling in the lymph nodes located below the lower jaw, under the jawline, on the sides of the neck, behind the ears, and under the chin. Dental ailments that can cause this type of swelling include:
1. Swollen Gums - Gingivostomatitis: this is a painful oral infection that causes blisters and canker sores in and around the mouth. It can develop from not flossing and brushing enough, and generally having poor oral hygiene. Seeing a lymph node dentist can help diagnose this kind of oral infection, and they may recommend antibiotics or minor oral surgery as treatment.
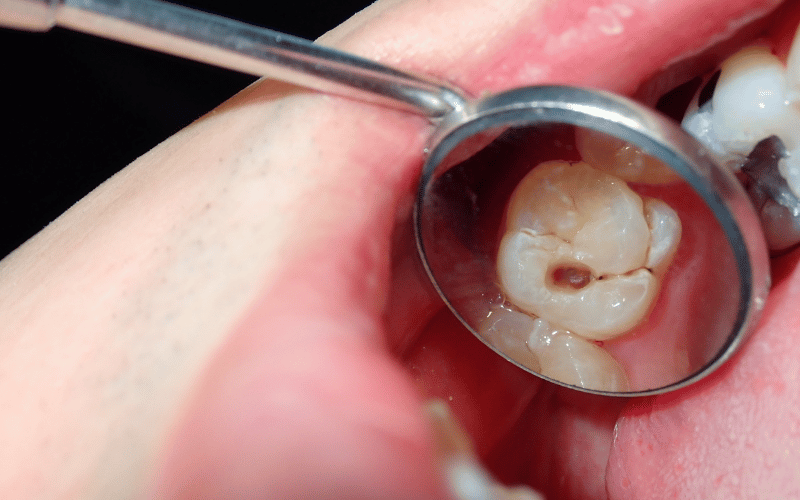
2. Untreated Cavities: a cavity is a decayed or damaged part of a tooth, which develops when bacteria break down your tooth enamel and create a hole. If left untreated, the cavity will grow and eventually cause pain, infection, and even tooth loss. If an infection sets in, the lymph nodes near the affected tooth can swell, as your immune system tries to combat the infection. Prompt dental attention is required to save the tooth and to prevent infection from spreading.
3. Dental Abscesses: dental abscesses are highly concerning to a lymph node dentist due to their potential for serious complications. These pockets of pus are caused by bacterial infections and are often accompanied by severe pain, swelling, and discomfort in the affected tooth and surrounding gums. If a dental abscess is left untreated, the infection can spread to the surrounding tissues, resulting in tooth loss, and even systemic health issues.
4. Canker Sores: these are small, painful sores that develop inside the mouth. You can identify them by their round/oval shape, white or yellowish center, and their red borders. Factors such as stress, injury to the mouth, certain foods, hormonal changes, and immune system problems can trigger development. Seek treatment if they don’t go away within 1-2 weeks and are accompanied by swollen lymph nodes.
5. Oral Thrush: this is a fungal infection that occurs in the mouth, caused by an overgrowth of yeast. The symptoms include painful, creamy white lesions on the tongue, inner cheeks, and roof of the mouth, that sometimes bleed when scraped. A lymph node dentist can treat these with anti-fungal medications, such as oral rinses or lozenges.
6. Periodontal Disease: if you have a severe form of gum disease, you may experience localized inflammation in the gums. If periodontitis is left untreated and unmanaged, this can lead to swollen lymph nodes over time.
7. Post-Dental Recovery: when receiving dental procedures like tooth extractions or root canals, you may develop temporary inflammation in the surrounding tissues, causing your lymph nodes to swell. This is not an issue in itself unless the swelling persists or is accompanied by other symptoms well past the expected recovery time.
Have Persistent Swelling? Get A Lymph Node Dentist Consult ASAP!
A lymph nodes dentist consult is a must if you have persistent swelling in your lymph nodes, and believe that dental issues are the cause. This is because infections from dental ailments can spread to other areas of the body, cause sepsis (a life-threatening infection), lead to complications such as bone loss and tooth loss, or may even create ongoing damage to the surrounding teeth and gums.
Book in with us here at Family, Implant, and Cosmetic Dentistry , and we’ll give you an accurate diagnosis of what’s going on, and provide you with a tailored treatment plan that combats the underlying dental ailment, and prevents future complications.
Let’s get your health back on track by scheduling a consultation today.
Your Road Map to Dental Implants For Front Teeth - Top 5 Strategies for A Successful Stunning Smile
Do dental implants hurt the procedure and timeline overview.
You can use the form below to ask questions and submit appointment requests or cancellations.
Choose Office Location Location: Brandon Location: Lakeland Location: Riverview
How did you hear about us? Google Bing Facebook Yelp Referral Other
Ask Us About Our Complimentary Implant Consultations & Seminars!

From same-day dental emergencies to long term oral care, our highly trained Brandon, FL and Lakeland, FL dental teams are ready to create a positive dental experience for you.
Patient Resources
- New Patient Health History
- Financial Policy
- HIPAA Disclosure
- Consent for Photographs, Consultation & Local Anesthetic
- Records Release From Another Dentist
(813) 684-7888 Dental Emergency: (813) 684-7888 Ext 2 10847 Boyette Rd. Riverview, FL 33569 View Directions
Office Hours
(863) 249-0205 Dental Emergency: (863) 249-0205 Ext 2 6419 Florida Ave S. Suite 105 Lakeland, FL 33813 View Directions
(813) 684-7888 Dental Emergency: (813) 684-7888 Ext 2 787 W. Lumsden Rd, Brandon, FL 33511 View Directions
Copyright © 2022 Family, Implant & Cosmetic Dentistry — All rights reserved | Terms and Conditions | Privacy Policy
Website by Digital Space Marketing
24/7 Online Scheduling

614-568-4021
845 polaris pkwy, westerville, oh 43082.

- Meet Dr. Hanul Oh
- Testimonials
- Exams & Cleanings
- Emergency Dentistry
- Dental Sealants
- Fluoride Varnish
- Mouth Guards
- Oral Cancer Screening
- Dental Implants
- Tooth Extractions
- Dental Crowns
- Dental Bridges
- Bone Grafting
- Root Canal Therapy
- Dental Implant Restorations
- Teeth Whitening
- Dental Veneers
- Tooth Colored Fillings
- IV Sedation
- Oral Sedation
- Nitrous Oxide Sedation
- Office Fees
- Dental Savings Plan
Can Dental Problems Trigger Swollen Lymph Nodes?

By Westar Dental
Our bodies are intricate systems where every part is interconnected, and often, a problem in one area can manifest as symptoms elsewhere. Dental problems, for instance, can have far-reaching effects beyond your oral health. One intriguing connection is between dental issues and swollen lymph nodes. In this article, we’ll explore the causes, symptoms, prevention, and management of swollen lymph nodes related to dental problems.
Understanding Swollen Lymph Nodes
Lymph nodes are small, bean-shaped structures scattered throughout the body, playing a crucial role in our immune system. When your body detects an infection or injury, lymph nodes may become enlarged or swollen as they work to fight off the problem.
Dental Issues and Swollen Lymph Nodes: The Connection
Dental problems can sometimes lead to swollen lymph nodes, and understanding this connection is crucial for maintaining oral and overall health. Here are several key points explaining the relationship between dental issues and swollen lymph nodes:
Infection and Inflammation:
When you have a dental infection, such as a tooth abscess or gum disease, harmful bacteria can spread beyond the affected area. This can trigger an inflammatory response in your body, leading to swollen lymph nodes. Lymph nodes are part of your immune system, and when they detect an infection, they become enlarged as they work to fight off the invading bacteria.
Location Matters:
The location of the swollen lymph nodes can provide valuable information. Swollen lymph nodes in the neck or jaw area are often associated with dental issues in the nearby oral cavity. For example, an infected tooth or gum problem on one side of your mouth can cause lymph nodes on that side of your neck to swell.
Systemic Impact:
Dental infections and swollen lymph nodes can have systemic effects on your body. An untreated dental infection can potentially lead to the bacteria entering your bloodstream, increasing the risk of more severe health issues. Timely dental care and addressing oral infections can help prevent such complications.
Pain and Discomfort:
Swollen lymph nodes due to dental problems can cause discomfort. You may experience pain or tenderness in the affected area, making eating, speaking, or even turning your head challenging. Ignoring these symptoms can worsen the underlying dental issue, so seeking dental care is essential.
Diagnosis and Treatment:
If you notice swollen lymph nodes in your neck or jaw, especially if they are accompanied by dental discomfort or signs of infection like a fever, it’s crucial to consult with a dentist. They will perform a thorough examination, which may include dental X-rays, to identify the source of the problem. Once the dental issue is diagnosed, appropriate treatment, such as antibiotics, dental procedures, or periodontal therapy, can be administered to address both the dental problem and the swollen lymph nodes.
Preventing Dental-Related Swollen Lymph Nodes
Prevention is always better than cure. Maintaining good oral hygiene is key to preventing dental problems leading to swollen lymph nodes. Here are some tips:
- Regular Dental Check-ups
Schedule regular visits to your dentist for check-ups and cleanings. This helps identify and address dental issues before they worsen.
- Brush and Floss Daily
Brush your teeth at least twice daily and floss once daily to remove food particles and plaque, preventing tooth decay and gum disease.
- Use Antiseptic Mouthwash
Antiseptic mouthwash can help reduce the bacteria in your mouth, lowering the risk of infections.
- Maintain a Balanced Diet
Eating a balanced diet rich in fruits and vegetables can boost your immune system and promote oral health.
- Avoid Smoking and Excessive Alcohol
Both smoking and excessive alcohol consumption can harm your oral health. Quitting or reducing these habits can improve your overall well-being.
Managing Swollen Lymph Nodes
When you’re dealing with swollen lymph nodes caused by dental issues, it’s essential to take the right steps to manage and alleviate this discomfort. Here are several key points to help you manage swollen lymph nodes associated with dental problems:
Seek Dental Evaluation:
The first and most crucial step is to consult a dentist for a thorough evaluation. If necessary, your dentist will examine your oral cavity, perform X-rays, and identify the dental problem causing the swollen lymph nodes. Once the source of the issue is determined, your dentist can recommend appropriate treatment.
Address the Dental Problem:
Treating the underlying dental problem is essential for resolving swollen lymph nodes. Whether it’s a tooth abscess, gum infection, or other oral issue, your dentist will recommend the appropriate dental procedures or treatments. This may include root canal therapy , tooth extraction, periodontal treatment, or antibiotics to clear the infection.
Maintain Excellent Oral Hygiene:
Good oral hygiene is key to preventing dental problems and their associated complications, including swollen lymph nodes. Brush your teeth at least twice a day with fluoride toothpaste, floss daily to remove plaque and food particles, and rinse with an antimicrobial mouthwash to keep your mouth clean and healthy. Regular dental check-ups and cleanings are also crucial for maintaining optimal oral health.
Follow Dental Aftercare Instructions:
If you undergo dental procedures to address the underlying issue, you must follow your dentist’s aftercare instructions diligently. This may include taking prescribed medications, practicing good oral hygiene, and attending follow-up appointments. Proper aftercare helps ensure a successful recovery and reduces the risk of complications.
Manage Discomfort:
Swollen lymph nodes can be uncomfortable. Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help alleviate pain and reduce inflammation. Ensure you follow the recommended dosage instructions and consult your dentist or healthcare provider if the discomfort persists or worsens.
Stay Hydrated and Rest:
Adequate hydration and rest are essential for your body’s natural healing process. Drink plenty of water to stay hydrated, and give your body the rest it needs to recover from dental procedures or infections. A well-rested body is better equipped to combat infections and reduce inflammation.
Monitor Progress:
Keep an eye on the progress of your swollen lymph nodes as you undergo dental treatment. They should gradually decrease in size and discomfort as the dental issue resolves. If there is no improvement or if the swelling persists, consult your dentist promptly for further evaluation.
Your oral health is intricately connected to your overall well-being, and dental problems can have wide-ranging effects, including triggering swollen lymph nodes. Recognizing the signs and addressing dental issues promptly is crucial for preventing complications and maintaining good health.
Remember, maintaining good oral hygiene through regular dental check-ups, proper brushing and flossing, and a healthy lifestyle can go a long way in preventing dental problems and the associated swollen lymph nodes. And if you ever experience persistent or painful swelling of lymph nodes, don’t hesitate to consult a dentalcare professional for a thorough evaluation and appropriate treatment.
Take care of your dental health, and your entire body will thank you for it.
Q1: Can dental problems lead to swollen lymph nodes elsewhere in the body?
A1: While dental problems primarily affect the head and neck region, severe infections can theoretically lead to swollen lymph nodes in other areas, although this is less common.
Q2: Are swollen lymph nodes always a sign of a serious problem?
A2: Swollen lymph nodes can be a sign of various issues, from mild infections to more serious conditions. If you have persistent swollen lymph nodes, it’s advisable to seek medical evaluation to determine the underlying cause.
Q3: Can swollen lymph nodes go away on their own?
A3: Swollen lymph nodes can resolve on their own if they are caused by a minor infection. However, if they persist or are accompanied by concerning symptoms, medical attention is necessary.
Q4: Can good oral hygiene prevent all dental-related issues?
A4: While good oral hygiene significantly reduces the risk of dental problems, it cannot eliminate all potential issues. Regular dental check-ups are essential for early detection and treatment.
Related Articles

Effective Tips For Eliminating Coffee Stains From Your Teeth
Lymphomas: What Your Dental Visit Can Reveal
Medically Reviewed By Colgate Global Scientific Communications

When you’re in the dental chair for a routine visit, you may be thinking, “I hope I don’t have any cavities” and, “I love how clean my teeth feel after I’m done.”
The last thing you’re probably thinking about is cancer.
Sometimes a routine dental checkup can uncover lymphoma, a type of cancer, before other signs are even present. And while a cancer discovery is not welcomed, early detection is.
About Lymphoma
Lymphoma is a cancer of the body's immune system. There are two types: Hodgkin's lymphoma and non-Hodgkin's lymphoma. It can show up at any age, but chances increase as you age. According to the American Cancer Society , non-Hodgkin's lymphoma is one of the most common cancers diagnosed in the United States. Roughly 4 percent of all cancers found are non-Hodgkin's lymphoma.
Two Types of Lymphoma: What's the Difference?
The key difference between Hodgkin's and non-Hodgkin's lymphoma is the type of white blood cells, also known as lymphocytes it involves. According to the Mayo Clinic , this determination requires a microscope. If a specific cell called Reed-Sternberg is seen, the diagnosis is Hodgkin's lymphoma. If not, it's non-Hodgkin's lymphoma.
Signs and Symptoms
Healthy white blood cells travel in your body through the lymphatic system within clusters of lymph nodes. Many times, lymphomas are discovered when people find painless swelling in areas near lymph nodes. These can include swelling in the armpits, groin, abdomen, and neck.
Other symptoms can include:
- Extreme fatigue
- Night sweats
- Difficulty breathing
- Unexplained weight loss
- Mouth sores, swelling, and pain
Dental Detectives
Sometimes a routine dental checkup can be critical in revealing signs of lymphoma before other symptoms occur. Swollen glands are usually painless and may go unnoticed until they are examined by a medical professional. So, when your dental professional sweeps his or her hands down your neck during an oral cancer screening, they're checking for swollen lymph nodes in your neck.
According to a review in eCancer Medical Science , oral cavity lymphomas are the third most common malignancy in oral cancers. The oral lymphoma symptoms such as ulcerations, pain, swelling, and loose teeth can often be mistaken for other conditions such as periodontal disease, which is why it's essential to have routine oral health appointments that include oral cancer screenings.
The disease type and stage will determine lymphoma treatment. Some of the more slow-growing cases will only require blood work and symptom control. If it's a more aggressive type of lymphoma, radiation, chemotherapy, immunotherapy, targeted drug therapies, and a bone marrow transplant are possible treatments. The goal is to destroy the cancer cells and achieve remission of the disease.
As with many cancers, early detection of lymphoma is best. While you wouldn't normally dream of connecting lymphoma and teeth, it's essential to keep up with your regular health and dental checkups. Make sure your dental appointment includes an oral cancer screening.
This article is intended to promote understanding of and knowledge about general oral health topics. It is not intended to be a substitute for professional advice, diagnosis or treatment. Always seek the advice of your dentist or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment.
ORAL HEALTH QUIZ
What's behind your smile?
Take our Oral Health assessment to get the most from your oral care routine
2.3 billion
people worldwide suffer from tooth decay
Related Articles

What Causes A Swollen Gum Around One Tooth?

Is Indemnity Dental Insurance Right For You?

What a Lump on the Jawline Could Indicate

What Is Tooth Bonding?
Related products.

Colgate ® Total Pro-Shield Spearmint Mouthwash
Colgate Total 12HR Pro-Shield Mouthwash provides 12-hour germ protection after eating and drinking for fresh breath.

Colgate ® Total Mouthwash for Gum Health
Colgate Total Gum Health mouthwash is a germ-fighting formula that forms a protective shield along the gum line and protects against bacteria for fresh breath.

Colgate ® Cavity Protection Toothpaste
Colgate Cavity Protection Toothpaste with Fluoride, Great Regular Flavor helps strengthen teeth enamel every time you brush your teeth.

Colgate ® Whitening + Charcoal Toothpaste
Colgate Total Whitening + Charcoal toothpaste gently removes stains and fights against cavities, plaque and gingivitis while preventing new stains and tartar buildup.

Helping dental professionals

Get the best of your oral health routine and take it to the next level with expert advice, recommendations, products and solutions and special offers.
- Whiter teeth
- Protect your gums
- Kids oral health
- Fighting cavities
- Reduce tooth sensitivity
- Protect enamel
- Reduce plaque
- Better Breath
- Reduce Tartar
Thank you for joining!
We’re excited to have you as a part of our Colgate Community. Your first newsletter is on its way to you now!
- Oral Health
- Oral Health Check
- Product Match
- ColgateProfessional.com
- Shop.Colgate.com</b>"> Shop.Colgate.com
- Terms of Use
- Privacy Policy
- Terms of Sale
- Cookie Consent Tool
- Do Not Sell My Personal Information
- Skip to main content
- Skip to header right navigation
- Skip to after header navigation
- Skip to site footer

Ask the Dentist
Health Begins in the Mouth | Dr. Mark Burhenne
Every product I recommend meets my rigorous safety and testing standards. When you buy through links on my website, I may earn a small commission which helps offset the costs of running this website. Learn more →
Pain After Dental Work: Types, Recovery Time, & Pain Relief
Get Dr. B’s Dental Health Tips
1. jaw muscle fatigue, 2. pulpitis, 3. referred myofacial pain, 4. dry socket pain, 5. soft tissue injury pain, 6. dental implant pain, 7. gum graft surgery pain, 9. tooth sensitivity, how to prevent pain after a dental visit, how to relieve pain after dental work.
The number one reason people put off going to the dentist is a fear of pain . This can greatly damage your oral health and lead to many more problems down the road.
Some pain after a dental visit is to be expected, while other types of pain after dental work may require follow-up care.
You may wonder if your jaw pain or referred pain in your ears, eyes, or other areas of the face is normal, rare, or cause for alarm.
The most common types of pain after a dental visit include:
Common causes of pain after dental work are poor procedure, pre-existing inflammation, very large cavities, and irritation of TMD (TMJ pain).
People who struggle with teeth grinding/clenching are generally at the highest risk for postoperative pain.
IF YOU PURCHASE A PRODUCT USING A LINK BELOW, WE MAY RECEIVE A SMALL COMMISSION AT NO ADDITIONAL COST TO YOU. READ OUR AD POLICY HERE .
How long does pain after dental work last.
The majority of pain after dental treatment should go away in 1-2 days. For wisdom tooth surgery, pain may last closer to 1-2 weeks. If you have TMJ pain after dental work, it may take months for the pain to go away.
Typically, I recommend asking the dentist who will perform your procedure what kind of pain you should expect afterwards.
In addition, understanding what kind of pain to expect helps you know when your dental problems are cause for a follow-up visit.
Questions to ask your dentist include:
- Will I feel stabbing pain?
- Should I expect a sore mouth?
- Will my teeth be sensitive to hot or cold?
- Should my recovery pain make it hard to perform daily tasks, or is it more likely to simply be annoying or minor?
If you experience pain outside of what your dentist describes as expected, call him or her to find out the next steps. If procedures have been performed poorly or if you have additional issues that must be corrected professionally, you may end up having to get a follow-up procedure.
Free weekly dental health advice in your inbox, plus 10 Insider Secrets to Dental Care as a free download when you sign up

What it is: Jaw muscle pain after dental work, like a filling or root canal, is muscle soreness caused by having the mouth open for a long time. People that grind their teeth a lot are more susceptible to this condition because their temporomandibular joint is already strained.
What it feels like: The jaw muscles give out, much like your leg muscles when running until you can hardly stand. Your muscles may feel tired, exhausted, and shaking, which produces pain.
How it happens: The mouth stays open for an extended period of time, exhausting the muscles of the jaw.
Your dentist may notice when this is happening during a procedure because you won’t be able to keep your mouth open and have accompanying muscle spasms. You may believe you’re holding your mouth open, even when you aren’t.
How to fix it: If you know you have TMJ problems, ask your dentist for a bite block. A bite block is a small rubber block that does not force your jaw open but allows it to stay open without jaw muscle exhaustion. The block does the work for you.
How long should jaw muscle fatigue last? Jaw muscle pain after dental work is most common for longer procedures, like root canals, and can last for several days.
What it is: Pulpitis is inflammation of the sensitive inner layer, or pulp, of the tooth.
What it feels like: Pulpitis causes sensitive teeth , painful when exposed to hot or cold. It can also cause generalized toothache and may eventually lead to an abscess if left untreated. This painful condition will usually be concentrated to the tooth your dentist worked on during the procedure.
The pain of pulpitis after dental work is similar to the pain you develop from extensive tooth decay.
There are two types of pulpitis: reversible pulpitis and irreversible pulpitis. If you have reversible pulpitis, you probably don’t feel pain unless something actually touches your affected tooth. Irreversible pulpitis feels more consistent and hurts worse.
How it happens: Even a simple filling can cause pulpitis. Aggressively prepping and drilling of the tooth can cause pulpitis. Your dentist also may have used a lot of air after drilling in the tooth, which can cause tooth pain to be generated from the filled area of the tooth.
Rarely, a careless dentist may actually nick the nerve, leading to greater sensitivity and pain.
However, your dentist may find that a cavity is deeper and more extensive than originally thought, requiring the tooth be drilled into the nerve area. This would require a root canal.
Working on a cracked or chipped tooth may also cause pulpitis.
How to fix it: Reversible pulpitis can go away if the inflammation goes down, but your dentist will probably need to examine and correct the damage if possible. Irreversible pulpitis, once the inflammation reaches a certain point, requires a root canal or tooth extraction .
How long should pulpitis last? Pulpitis pain in a specific tooth several days after a dental procedure necessitates another visit to the dentist. Neither type of pulpitis is likely to go away on its own.
What it is : Any dental procedure may result in referred facial pain. This is pain that may affect the eye socket, ears, or other facial areas.
What it feels like: Referred myofacial pain may feel like an earache or other persistent pain in areas associated with the teeth, but outside of the mouth.
How it happens: This happens when nerves are inflamed or irritated by dental work but send pain throughout other nerves nearby. It can feel like a knotted muscle and will probably interfere with your sleep.
There’s no way to predict or prevent referred pain after a dental visit.
How to fix it : While this type of pain is very common, it’s also one that will require intervention from your dentist or oral surgeon.
Common ways to treat referred myofascial pain include trigger point injections and physical therapy.
How long should referred myofacial pain last? Referred myofacial pain after dental work probably won’t go away without further treatment.
What it is: Dry socket is bone pain that results from loss of the blood clot in a tooth socket after tooth extraction. This pain after dental visits is usually associated with more extensive oral surgery (like after wisdom teeth removal ).
What it feels like: Dry socket pain is deep, sore pain that radiates from your tooth socket up and down the same side of your face.
The pain receptors in bone are very sensitive, which is why this condition hurts so much.
Dry socket pain sometimes radiates up to the ear and may also cause worsened breath or unpleasant taste in the mouth. Other symptoms include headache and, on occasion, fever from a resulting infection.
How it happens: If the blood clot from your tooth extraction falls out before the 4-day mark after tooth extraction, you will probably develop dry socket. It’s most likely 2-3 days after your tooth is removed.
Any sucking motion in the mouth, like drinking through a straw or aggressive mouthwash swishing increases your chances of losing the blood clot over your exposed bone.
How to fix it: Dry socket that happens in the first 1-2 days after extraction will probably need to be corrected by your dentist or oral surgeon. Most of the time, he or she can use dry socket paste to relieve your pain and protect the exposed area so it has time to heal.
In severe cases, you may need bone graft material or surgical foam to support the healing process. This is most necessary for people with thinning bone (like those with advanced periodontal disease).
If your clot falls out between day 3-4, the pain is likely to clear up on its own without intervention. However, it’s always a good idea to contact your dentist/oral surgeon to find out what s/he would suggest.
Home remedies for dry socket pain may include over-the-counter anti-inflammatory medications, cold compress, salt water rinse, clove oil, and/or honey.
How long should dry socket pain last? Dry socket is typically painful for 7-10 days after tooth extraction. Patients with advancing gum disease may experience pain for several weeks.
What it is: Nicking the gums or tongue during a dental procedure will likely cause trauma in the mouth, resulting in soft tissue pain.
What it feels like: Injury of soft tissue typically results in throbbing pain that’s sensitive to touch, like when you chew food. It will probably also cause pain when you eat hot foods.
Anytime the tongue is harmed at all can be very painful. It’s one of the reasons your dentist discourages eating food that requires a lot of chewing following a procedure that requires anesthetic.
How it happens: Some people may inadvertently bite their tongues during a dental procedure, which will produce pain in the days following the procedure as the tongue heals. The gums may be nicked by dental instruments.
Gums will also feel pain after procedures where they are purposefully incised, such as removal of an impacted wisdom tooth.
Burning your mouth with hot foods shortly after a procedure can also cause pain.
A biopsy usually does not cause a lot of pain, but there is the possibility of soft tissue involvement, which can cause pain as it heals.
How to fix it: Be very cautious eating after dental work where your mouth and tongue are numbed. Use a salt water rinse, clove oil, benzocaine, or another toothache home remedy to correct the pain.
How long should soft tissue injury pain last? Soft tissue pain should last 3 days or fewer, although it can open your body up to infection. The tongue is very sensitive and takes a while to heal, which can take 2-3 weeks.
If you develop an infection from this type of injury, your dentist will probably prescribe an antibiotic.
Numbness in the tongue, lips, and jaw (known as paresthesia) is normal for a few hours after many types of dental procedures. However, if it lasts much longer, it may be permanent. If this happens, talk to your dentist right away.
What it is: When you get a dental implant , you’ll have soreness in the days following the procedure.
What it feels like: Implant pain is inflammation in the bone, like dry socket, and bone pain is very generalized. It can refer, run up and down the jaw, and is very achy, which is the nature of bone pain.
The pain receptors in bone are one of the most sensitive types of pain receptors in the body.
How it happens: Some post-op pain should be expected after an implant, but it’s usually less than the pain of having a tooth pulled.
How to fix it: This type of pain after a dental visit should go away without any sort of intervention. Just be aware of this before your implant, and call your dentist if the pain persists for more than a few days.
How long should dental implant pain last? Dental implant pain usually lasts about 2-3 days.
What it is: If you have receding gums that have progressed to exposing sensitive dentin (or bone), your dentist may suggest you have gum graft surgery.
What it feels like: Pain after gum graft surgery can be significant, with a combination of bone pain and gum pain in two different parts of the mouth. Expect the pain to be generalized and somewhat severe for several days.
How it happens: In gum graft surgery, your gums are purposefully “injured” in the process of correcting gum recession. Because dentin was exposed, you’ll also have bone pain as a result of increased contact between dental instruments and bone.
How to fix it: This pain should be expected after gum graft surgery. Your oral surgeon should recommend pain relievers or give you a prescription for one. Let him or her know if the pain lasts longer than a week and doesn’t subside.
How long should gum graft surgery pain last? Gum graft surgery pain typically lasts a week or less.
What it is: Trismus is a spasm of the jaw muscles, causing the mouth to remain tightly closed.
Trismus is sometimes called lockjaw, although it’s not the same “lockjaw” as a tetanus infection.
What it feels like: With trismus, your jaw muscles will spasm and close the mouth tightly. You can expect pain from the tensed muscles and possibly some tooth sensitivity from grinding.
Soreness and tenderness in the lower jaw are also symptoms of trismus.
How it happens: The needle used to inject local anesthetic may go through the muscle when a dentist is working on your lower teeth.
This doesn’t usually produce pain immediately following the procedure. But in 2-3 days following the procedure or injection, the muscle may stiffen, making it hard to open your mouth.
The condition will always be on the same side as the injection site, but it is fairly rare. You could also have it on both sides if you’re having your wisdom teeth out, though that’s even more rare.
How to fix it: Trismus is a condition your dentist should help you treat. He or she may prescribe a soft foods diet, physical therapy or massage, a jaw-stretching device, and/or muscle relaxers and pain relieving medication.
How long should trismus last? Trismus should last 2 weeks or less.
What it is: Tooth sensitivity may happen after dental procedures like a teeth cleaning or even a dental crown . Anytime tooth enamel or gums are worked on, sensitivity can result.
What it feels like: Tooth sensitivity is generalized soreness when teeth are exposed to very hot or very cold foods or drinks.
How it happens: Tooth sensitivity is a normal pain to expect after any dental procedure. It happens because the sensitive tissues of the teeth and gums have been agitated during normal dental care.
This is more likely during a root planing and scaling , a deep teeth cleaning performed during gum disease treatment.
In some cases, a dental filling is too high and can cause sensitivity (usually on just one side of the mouth).
How to fix it: Tooth sensitivity from a dental procedure should go away on its own, but you can try a salt rinse or benzocaine for relief. If you know you struggle with sensitivity after normal procedures like cleanings at your check-ups, try tips for making your cleanings less painful .
If you got a dental filling that is too high and interferes with your bite, you’ll need to go back to the dentist to resolve the sensitivity.
How long should tooth sensitivity last? Tooth sensitivity caused by dental work should go away in 2-3 days.
While some pain is to be expected after most dental procedures, there are a few steps you can take to prevent it before it starts.
To prevent pain after dental work:
- Eat an anti-inflammatory diet. Eating anti-inflammatory foods before you go to the dentist can be helpful in reducing how much pain you experience afterwards.
- Treat your TMD/TMJ before any procedure. If you’re more susceptible to jaw pain, try giving your muscles some light stretching and more rest before you go into a dental procedure.
- Ask for a bite block. To give your jaw muscles a break, you can request a bite block be used during your procedure to minimize muscle pain afterwards.
- Deal with bruxism (grinding) issues before your procedure. Grinding your teeth is likely to trigger pain after dental work. Treating that ahead of time will go a long way in helping you have a quick recovery.
- Deal with infection before having a cavity restored. Your doctor may give you antibiotics before having a root canal or dental filling . The less infection and smaller the abscess near a cavity, the less pain you’re likely to experience after having it fixed.
- Ask for a break in the middle of a long procedure. If your mouth has to be opened wide for several hours, asking ahead of time for a break in the middle is one way to prevent extra jaw muscle pain.
- Relax! Stress can cause a number of pain-inducing conditions like dental anxiety, muscle aches, and even some extra tooth grinding. Practice mindfulness and rest in the days leading up to your procedure. You might even try some CBD for dental anxiety if you know you’re nervous before your dental work. Using weighted blankets, noise-canceling headphones, or working with a therapy dog helps to provide some calm from the anxiety that many people feel before dental work.
Prevention is always your best tool for preventing tooth pain. In general, a large majority of dental work can be avoided by addressing dental health on a regular basis.
To prevent dental problems that require restorative procedures:
- Practice good oral hygiene. Use an electric toothbrush , a remineralizing toothpaste , and scrape your tongue at least twice every day. Never skip flossing. Good oral care is key to good oral health!
- Eat a tooth-friendly diet . Foods can cause or prevent/reverse cavities . Focus on nutrient-dense foods with minimal processing, sugar, and acid content.
- Don’t ignore signs of periodontal disease. Gum disease is incredibly common, especially after the age of 60. It’s associated with dozens of comorbid health conditions — don’t ignore it. Talk to your dentist about bleeding gums .
- See your dentist every 6 months. Dental health care is a huge part of your overall health. Bi-yearly dental appointments are important because teeth cleanings and regular exams can prevent small problems before they become big.
- Address sleep-disordered breathing . Sleep-disordered breathing (SDB), like that seen in sleep apnea, is a problem for countless reasons — one of which is poor oral health. SDB is associated with bad breath , TMJ, and weakened tooth enamel, among other issues.
For pain relief after dental work:
- Eat an anti-inflammatory diet. A diet high in plant-based foods , essential fatty acids, high-antioxidant foods, and foods with plenty of trace minerals reduce all-body inflammation . Inflammation is the root cause of most pain. Popular anti-inflammatory diets include the keto diet , Paleo diet, Mediterranean diet, or Whole30.
- Try a turmeric supplement. Turmeric is one of nature’s most potent natural pain relievers . Turmeric even outperforms some non-steroidal anti-inflammatory drugs used for pain and may treat postoperative pain.
- Rest and ice your jaw. If TMJ pain is your biggest issue, do what you can to relax your jaw before and after the procedure. Use an ice pack to reduce swelling and calm muscle inflammation. Avoid having dental work performed at a dental school , as the procedures done there usually take longer.
- Try THC or CBD. Both major compounds in marijuana, THC and CBD, are powerful pain relieving agents .
- Drink ice-cold coconut water. Coconut water can help to replenish electrolytes that you may lose during wisdom teeth removal recovery . Drinking it ice cold may reduce inflammation and soft tissue pain.
- Take an over-the-counter painkiller like ibuprofen. Ibuprofen is generally considered the best pain reliever for tooth pain . You may also try acetaminophen (Tylenol). I recommend patients follow the 3-3-3 method: 3 ibuprofen, 3 times a day, for 3 days after dental work.
- Take pain medications prescribed by your dentist. Opioids like Tylenol-3, Vicodin (Lortab; acetaminophen with hydrocodone), and Percocet (acetaminophen with oxycodone) may be used for dental pain. These are not prescribed as often as they used to be due to the opioid epidemic. Your dentist is unlikely to prescribe these pain medications except in extreme cases.
Should my teeth hurt after a cleaning?
If you’ve waited years to get a cleaning, your hygienist might need to do a full scaling and root planing to clear your teeth of plaque.
After that, your roots will be very clean — but they’ll be sensitive to cold for 1-2 weeks.
Is it normal to have tooth pain after a filling?
Metal fillings tend to cause pain more easily than plastic fillings, but plastics can cause pain in their own way, too.
There are two types of pain from a filling that would send you back to the dentist, though.
Aching and cold sensitivity around a filled tooth that lasts more than 3 days may be a sign of pulpitis. Pulpitis can be reversible or irreversible. The latter would, unfortunately, require a root canal or tooth extraction.
That’s why you should always get cavities filled once they’re small but have passed the point of reversal. The larger the cavity, the bigger your chance to develop pulpitis.
The second reason a filling could cause pain longer than a couple of days is a filling that’s too high. A tall filling may mess with your bite.
How do you know this has happened? You’d notice cold sensitivity and some aching about 2-3 days after getting the filling, and the pain would not get better over time.
How do you know if you have an infection after dental work?
- Bad taste in the mouth
- Toothache or new hot/cold tooth sensitivity
- Gum swelling
- Swollen jaw
- Swelling of the lymph nodes or neck
If you think you have developed an infection after dental work, talk to your dentist immediately. References
- Watzl, B. (2008). Anti-inflammatory effects of plant-based foods and of their constituents. International journal for vitamin and nutrition research, 78 (6), 293-298. Abstract: https://pubmed.ncbi.nlm.nih.gov/19685439/
- Chrysohoou, C., Panagiotakos, D. B., Pitsavos, C., Das, U. N., & Stefanadis, C. (2004). Adherence to the Mediterranean diet attenuates inflammation and coagulation process in healthy adults: The ATTICA Study. Journal of the American College of Cardiology, 44 (1), 152-158. Abstract: https://pubmed.ncbi.nlm.nih.gov/21139128/
- Sun, J., Chen, F., Braun, C., Zhou, Y. Q., Rittner, H., Tian, Y. K., … & Ye, D. W. (2018). Role of curcumin in the management of pathological pain. Phytomedicine, 48 , 129-140. Abstract: https://pubmed.ncbi.nlm.nih.gov/30195871/
- Takada, Y., Bhardwaj, A., Potdar, P., & Aggarwal, B. B. (2004). Nonsteroidal anti-inflammatory agents differ in their ability to suppress NF-κB activation, inhibition of expression of cyclooxygenase-2 and cyclin D1, and abrogation of tumor cell proliferation. Oncogene, 23 (57), 9247. Abstract: https://pubmed.ncbi.nlm.nih.gov/15489888/
- Agarwal, K. A., Tripathi, C. D., Agarwal, B. B., & Saluja, S. (2011). Efficacy of turmeric (curcumin) in pain and postoperative fatigue after laparoscopic cholecystectomy: a double-blind, randomized placebo-controlled study. Surgical endoscopy, 25 (12), 3805-3810. Abstract: https://pubmed.ncbi.nlm.nih.gov/21671126/
- Mack, A., & Joy, J. (2000). MARIJUANA AND PAIN . Full text: https://www.ncbi.nlm.nih.gov/books/NBK224384/
- Bailey, E., Worthington, H. V., van Wijk, A., Yates, J. M., Coulthard, P., & Afzal, Z. (2013). Ibuprofen and/or paracetamol (acetaminophen) for pain relief after surgical removal of lower wisdom teeth. Cochrane Database of Systematic Review s, (12). Full text: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD004624.pub2/full
About Mark Burhenne, DDS
I’m on a mission to empower people everywhere with the same evidence-based, easy-to-understand dental health advice that my patients get. You can read my story here. I have been a dentist in private practice for 35 years. I graduated from the Dugoni School of Dentistry in San Francisco, CA in 1987 and am a member of the American Academy of Dental Sleep Medicine (AADSM), Academy of General Dentistry (Chicago, IL), American Academy for Oral Systemic Health (AAOSH), and Dental Board of California.

Dr. Mark is the author of the best-selling book 8-Hour Sleep Paradox
CALL 727-467-2759 to Make Your Appointment with Dr. José F. Lázaro Today!
- Meet the Doctor
- Oral Surgery
- Dental Implants
- Wisdom Teeth Removal
- Bone Grafting
- Bio Active Modifiers
- Sinus Augmentation
- Cone Bean Computer Tomography (CBCT) Scan
- Surgical Procedures to Aid Orthodontic Treatment
- Testimonials
Infection Signs to Watch for After Oral Surgery

Signs You May Have a Fractured Tooth

Tips for Managing Anxiety before Oral Surgery

Oral Surgery Recovery Includes Watching for Infection Signs
Surgical procedures bear the risk of infections during recovery, and oral surgery is no exception. Patients undergo oral surgery for different reasons. It could be a root canal, bone grafting, tooth extraction, or corrective jaw surgery. With advancements in dental health technology, infection control practices are at their best. However, your wound could still get infected during or after surgery. After oral surgery, take the necessary measures to ensure that your wound is not infected because the resulting complications will be more painful. To properly take care of your wound, you should be aware of what to watch out for and follow post-care guidelines from your dentist.
Signs of Infections
Immediately after surgery, expect some numbness, bleeding, pain and swelling. However, these should not last long. The signs below indicate unusual occurrences in your mouth, and you should seek medical help immediately.
Pain on the tooth area, neck or jaw that does not cease after medication
Increasingly swelling face, jaw or gums
Persistent fever
Bleeding for more than a day
Emitting pus or redness from the area
Swollen neck lymph nodes
Excessive pain when opening your mouth or jaw
Difficulty in breathing
How to Prevent Infections after Oral Surgery
Avoid Physical Activity
Purpose to spend the next day or two after surgery resting. If you are feeling drowsy after the procedure, it is because they put you on sedatives. Do not engage in any activity that requires concentration, like driving.
What’s more, do not engage in heavy lifting or any activity that puts pressure on the tooth area to avoid bleeding. If you prefer to spend your day sleeping, keep your head elevated by adding extra pillows.
Stick by Your Surgeons Aftercare Instructions
The surgeon will give you instructions on how to take care of your wound. If you get home and are not sure of the instructions given, call the facility for an update. To successfully prevent infections after oral surgery, you must adhere to the instructions provided. For example, you might be told not to brush or use mouth wash for two days but to rinse your mouth with warm salty water after meals to dislodge food particles. As much as you want to maintain oral hygiene, brushing your teeth after the procedure brings you complications. Therefore, follow the instructions given.
Be Informed
Information is power, and when it comes to oral surgery recovery, you need to know what to look out for. You will be told that bleeding and swelling is expected, but where do you cut the line. If you get home and the incision site is still bleeding, bite a folded dump gauze to stop the flow. If your face is still swollen, apply ice on the swollen side for about 30 minutes until it goes down. What’s more, if you are experiencing pain, take the prescribed pain killers. If any of the above symptoms persist or you experience any other unusual signs, contact your dentist promptly.
Do Not Skip Your Antibiotics
Depending on the type of oral surgery you will get, your dentist will prescribe antibiotics before or after the surgery. The antibiotics are meant to prevent the bacteria in your mouth from infecting the wound. Therefore, finish the dosage as prescribed. While some symptoms like bleeding and pain are usual after oral surgery, make sure to contact your surgeon if they seem excessive. In addition, ensure to attend all your follow up appointments even if you feel like you have healed. Only your surgeon can give you a clean bill of health and wean you off medications and appointments after confirming your wound is healing well.
Dr. José Lázaro
Related posts.

FAQs About Sedation Dentistry

The Top 3 Reasons Your Jaw Clicks

What are the Implications of Infected Teeth on My Oral Health and Wellbeing?
Comments are closed.
Can Dental Problems Cause Swollen Lymph Nodes?
When you’re starting to feel a little sick, you may notice some swelling on the sides of your neck. Those tiny lumps feel soft and tender to the touch and may even hurt a little. These are called lymph nodes. Swollen lymph nodes are common and are a good sign. The swelling in these lumps is one of your body’s reactions to illness or infection.
When your lymph nodes get swollen, it means your immune system is working to clear away infection and viruses or bacteria. These swollen lumps act like filters that help your body get rid of cells or foreign matter that passes through your lymph fluid and are located throughout your body in the jaw, arms, groin, abdomen, and legs.
The lymph nodes that swell up are the ones located closest to the area of the infection or illness. For example, the most common cause of swollen lymph nodes in the neck is an upper respiratory infection. Lymph nodes can swell up with pretty much any kind of infection, including dental issues.
Dental Issues That Can Swell Your Lymph Nodes
Tooth infections.
A tooth infection is a pocket of infection and pus that develops because of a bacterial infection in the mouth. They are most commonly formed because of untreated dental cavities, a traumatic injury to the teeth, or even a poorly performed dental procedure. One of the symptoms of these kinds of infections, other than swelling of the face and toothache, is swollen lymph nodes in the jaw or neck.
It is crucial to catch them quickly because, in some cases, the infection can spread to other parts of the body. If the bacterial infection from an untreated tooth infection spreads to the neck, jaw, or brain, it can become life-threatening. The best way to prevent tooth infections is to practice good oral hygiene and be aware of the symptoms.
Canker Sore
A canker sore is an open mouth ulcer or sore, typically inside the lips or cheeks. They’re usually white or yellow and surrounded by inflamed soft tissue, and are really painful. Canker sore and swollen lymph nodes usually go hand in hand. Canker sores can have many causes like a virus or vitamin or mineral deficiency. Still, it’s always better to visit your dentist and let them examine it.
Get The Oral Health Assistance You Need
Dental problems are very delicate; they can lead to more significant issues within your body. If you notice anything unusual on your mouth, it’s better to visit a dentist as soon as possible, like canker sore and swollen lymph nodes. If you’re looking for a dentist in Knoxville, TN, look no further than Jim Erpenbach DDS.
Dr. Erpenbach is a founding member of the American Academy of Oral Systemic Health and an accredited member of the Academy of Biomimetic Dentistry. He is a compassionate dentist who thrives on giving his patients conservative care and high-quality service. If you want to receive unparalleled care from the best dentist in Knoxville, TN, contact the best today.

ONLINE SCHEDULING AND VIRTUAL CONSULTS AVAILABLE

11941 West Sunrise Blvd. Plantation, FL 33323
(954) 787-1695
- Why Choose Us
- Meet Dr. Rizvi
- Meet Dr. Calero
- Meet Dr. McCall
- Meet Our Team
- Office Tour
- Our Happy Patients
- New Patient Forms
- New Patients: What to Expect
- Financial Options
- Testimonials
- Ozone Therapy
- Laser Treatment
- Sleep Apnea
- Perio Protect
- Saliva Testing
- SMART Safe Mercury Removal
- Biological Dentistry
- Porcelain Veneers
- Teeth Whitening
- Kör® Whitening
- Porcelain Crowns
- Dental Implant
- All-on-4 Implants
- Full Or Partial Dentures
- Porcelain Bridges
- Invisalign® Plantation
- Six Month Smiles®
- Dental Emergency
- Oral Cancer Screening
- Guided Biofilm Therapy
- Periodontal Therapy
- Laser Bacterial Reduction
- Scaling & Root Planing
- Teen’s Dentistry
- Adult’s Dentistry
- Ortho Screenings
- Composite Fillings
- Test Drive Your Smile
- What is Digital Smile Design
- Why Choose Us For Your Digital Smile Design?
- Itero® Element 5D Scanner
- Intra-oral Camera
- Fotona Laser Technology
- Hard Tissue Laser
- Extractions
- Oral Surgery
- Root Canals
- Bone Grafting
- Oral Sedation Plantation
- Pain Free Sedation Plantation
- Sleep Study Test
- Facial Esthetics

Are Swollen Lymph Nodes Linked to Dental Conditions?

By My Dentist For Life Of Plantation
Swollen lymph nodes can be a sign of various health issues. But did you know they can also be related to dental conditions?
When they swell, it’s usually a sign that your body is fighting off an infection or dealing with another health issue. While many people associate swollen lymph nodes with illnesses like the flu or throat infections, they might be surprised to learn that dental conditions can also be a significant factor.
Dental infections, gum diseases, and other oral health issues can lead to swollen lymph nodes, signaling that something is amiss in your mouth. Understanding this connection is vital for effective diagnosis and treatment. In this blog, we’ll delve into how dental problems can cause swollen lymph nodes, the symptoms to watch for, and what you can do to prevent and treat these issues.
Let’s uncover the link between your oral health and swollen lymph nodes to help you maintain overall wellness.
Understanding Lymph Nodes
Lymph nodes are small, bean-shaped glands. They are part of the lymphatic system, which helps fight infections and maintain fluid balance. Found throughout the body, they play a crucial role in your immune response.
Causes of Swollen Lymph Nodes
Swollen lymph nodes, or lymphadenopathy, often signal that your body is fighting an infection. Common causes include:
- Infections: Bacterial, viral, or fungal infections can cause swelling.
- Immune System Disorders: Conditions like lupus or rheumatoid arthritis.
- Cancer: Certain cancers, such as lymphoma, can cause enlarged lymph nodes.
Dental Infections and Swollen Lymph Nodes
Dental conditions can indeed lead to swollen lymph nodes. Here’s how:
- Tooth Abscess: An abscessed tooth, a pocket of pus caused by infection, can lead to swollen nodes. It often causes pain and requires immediate treatment.
- Gum Disease: Gingivitis and periodontitis, caused by bacteria, can lead to inflammation and swollen nodes. Good oral hygiene is key to prevention.
- Oral Infections: Other oral infections, like canker sores or oral thrush, can also cause lymph node swelling. A dentist in Plantation can help diagnose and treat these conditions.
Symptoms and When to Seek Help
Recognizing symptoms early can make a big difference. Look for:
- Persistent Swelling: If nodes remain swollen for more than a few weeks.
- Pain and Tenderness: Painful nodes can indicate a serious infection.
- Fever: A fever alongside swollen nodes may require medical attention.
- Night Sweats or Weight Loss: These symptoms can be signs of more serious conditions.
Diagnosis and Treatment
Proper diagnosis is crucial for effective treatment. Here’s what to expect:
- Medical History: Your doctor will take a detailed medical and dental history.
- Physical Examination: They will examine your swollen nodes and look for signs of dental issues .
- Diagnostic Tests: Blood tests, imaging, or a biopsy may be needed.
Treatment depends on the underlying cause:
- Antibiotics: For bacterial infections.
- Antiviral or Antifungal Medications: For viral or fungal infections.
- Dental Treatment: Addressing dental issues, such as filling a cavity or treating gum disease, can reduce lymph node swelling.
Preventive Measures
Prevention is always better than cure. Here are some tips:
- Maintain Good Oral Hygiene: Brush twice a day, floss regularly, and use mouthwash.
- Regular Dental Check-ups: Visit your dentist regularly for cleanings and check-ups.
- Healthy Diet: Eat a balanced diet rich in vitamins and minerals.
- Stay Hydrated: Drink plenty of water to keep your mouth healthy.
Swollen lymph nodes can be linked to dental conditions. Recognizing the signs and seeking prompt treatment can prevent complications. Maintain good oral hygiene and visit your dentist regularly to keep your smile and your lymph nodes healthy.
By understanding the connection between dental health and swollen lymph nodes, you can take proactive steps to ensure overall well-being. Stay informed, stay healthy, and don’t ignore those swollen glands—they might be telling you more than you think.
Related Articles
Is It Possible to Reverse Cavities Without a Dentist? Uncover the Truth
What to Do If You Lose an Adult Tooth: Immediate Steps and Long-term Solutions

Why You Shouldn’t Miss Your Dental Checkups and Cleanings?
Request an appointment.
" * " indicates required fields
- Swollen lymph nodes
On this page
Preparing for your appointment.
To diagnose what might be causing your swollen lymph nodes, your doctor may need:
- Your medical history. Your doctor will want to know when and how your swollen lymph nodes developed and if you have any other signs or symptoms.
- A physical exam. Your doctor will also want to check lymph nodes near the surface of your skin for size, tenderness, warmth and texture. The site of your swollen lymph nodes and your other signs and symptoms will offer clues to the underlying cause.
- Blood tests. Certain blood tests may help confirm or exclude any suspected underlying conditions. The specific tests will depend on the suspected cause, but most likely will include a complete blood count (CBC). This test helps evaluate your overall health and detect a range of disorders, including infections and leukemia.
- Imaging studies. A chest X-ray or computerized tomography (CT) scan of the affected area may help determine potential sources of infection or find tumors.
- Lymph node biopsy. Your doctor may have you undergo a biopsy to secure the diagnosis. He or she will remove a sample from a lymph node or even an entire lymph node for microscopic examination.
More Information
- Chest X-rays
- Complete blood count (CBC)
- Needle biopsy
Swollen lymph nodes caused by a virus usually return to normal after the viral infection resolves. Antibiotics are not useful to treat viral infections. Treatment for swollen lymph nodes from other causes depends on the cause:
- Infection. The most common treatment for swollen lymph nodes caused by a bacterial infection is antibiotics. If your swollen lymph nodes are due to an HIV infection, you'll receive specific treatment for that condition.
- Immune disorder. If your swollen lymph nodes are a result of certain conditions, such as lupus or rheumatoid arthritis, treatment is directed at the underlying condition.
- Cancer. Swollen nodes caused by cancer require treatment for the cancer. Depending on the type of cancer, treatment may involve surgery, radiation or chemotherapy.

From Mayo Clinic to your inbox
If your swollen lymph nodes are tender or painful, you might get some relief by doing the following:
- Apply a warm compress. Apply a warm, wet compress, such as a washcloth dipped in hot water and wrung out, to the affected area.
- Take an over-the-counter pain reliever. These include aspirin, ibuprofen (Advil, Motrin, others), naproxen (Aleve) or acetaminophen (Tylenol, others). Use caution when giving aspirin to children or teenagers. Though aspirin is approved for use in children older than age 2, children and teenagers recovering from chickenpox or flu-like symptoms should never take aspirin. Talk to your doctor if you have concerns.
- Get adequate rest. You often need rest to aid your recovery from the underlying condition.
If you have swollen lymph nodes, you're likely to start by first seeing your family doctor. When you call to set up your appointment, you may be urged to seek immediate medical care if you're experiencing severe symptoms such as difficulty breathing or swallowing.
Here's some information to help you get ready for your appointment.
What you can do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, ask if you need to do anything in advance.
- List any symptoms you've been experiencing, and for how long. Among other symptoms, your doctor will want to know if you've had flu-like symptoms, such as a fever or sore throat, and may ask whether you've noticed changes in your weight. Include on your list every symptom, from mild to severe, that you've noticed since your lymph nodes began to swell.
- Make a list of all recent exposures to possible sources of infection. These may include travel abroad, hiking in areas known to have ticks, eating undercooked meat, being scratched by a cat, or engaging in high-risk sexual behavior or sex with a new partner.
- Make a list of your key medical information, including other conditions you're being treated for and the names of the medications that you're taking. Include every prescription and over-the-counter (OTC) drug you use, as well as any vitamins and supplements.
- List questions to ask your doctor.
For swollen lymph nodes, some basic questions to ask your doctor include:
- What's causing my symptoms?
- What are other possible causes for my symptoms?
- What kinds of tests do I need?
- What treatment do you recommend?
- How quickly will I start to feel better?
- Am I contagious? How can I reduce the risk of infecting others?
- How can I prevent this from happening in the future?
- I have these other health conditions. Do I need to change the treatments I've been using?
- Is there a generic alternative to the medicine you're prescribing for me?
- Do you have any brochures or other printed material that I can take with me? What websites do you recommend?
What to expect from your doctor
Your doctor is likely to ask you a number of questions, such as:
- What are your symptoms?
- When did you first begin experiencing symptoms?
- Have your affected lymph nodes gotten larger over time?
- Are your affected lymph nodes tender?
- Have you been experiencing a fever or night sweats?
- Have you lost weight without trying?
- Do you have a sore throat or difficulty swallowing?
- Have you experienced any difficulty breathing?
- Have your bowel habits changed?
- What medications are you currently taking?
- Have you recently traveled to another country or to tick-inhabited regions? Did anyone who traveled with you get sick?
- Have you recently been exposed to new animals? Were you bitten or scratched?
- Have you recently had sex with a new partner?
- Do you practice safe sex? Have you done so since you became sexually active?
- Do you smoke? For how long?
What you can do in the meantime
While you wait for your appointment, if your swollen nodes are painful, try easing your discomfort by using warm compresses and an over-the-counter (OTC) pain reliever, such as ibuprofen (Advil, Motrin IB, others) or acetaminophen (Tylenol, others).
January 10, 2024
- Fletcher RH. Evaluation of peripheral lymphadenopathy in adults. https://www.uptodate.com/contents/search. Accessed Sept. 3, 2019.
- Jameson JL, et al., eds. Enlargement of lymph nodes and spleen. In: Harrison's Principles of Internal Medicine. 20th ed. The McGraw-Hill Companies; 2018. https://accessmedicine.mhmedical.com. Accessed Sept. 3, 2019.
- Lymphadenopathy. Merck Manual Professional Version. https://www.merckmanuals.com/professional/cardiovascular-disorders/lymphatic-disorders/lymphadenopathy#. Accessed Sept. 3, 2019.
- Papadakis MA, et al., eds. Lymphangitis and lymphadenitis. In: Current Medical Diagnosis & Treatment 2019. 58th ed. McGraw-Hill Education; 2019. https://accessmedicine.mhmedical.com. Accessed Sept. 3, 2019.
- American Cancer Society. Lymph nodes and cancer. https://www.cancer.org/cancer/cancer-basics/lymph-nodes-and-cancer.html. Accessed Sept. 3, 2019.
- Symptoms & causes
- Doctors & departments
- Diseases & Conditions
- Swollen lymph nodes diagnosis & treatment
- Parts of the immune system
Associated Procedures
Products & services.
- A Book: Mayo Clinic Family Health Book
- Newsletter: Mayo Clinic Health Letter — Digital Edition
CON-XXXXXXXX
5X Challenge
Thanks to generous benefactors, your gift today can have 5X the impact to advance AI innovation at Mayo Clinic.
1507 W Yosemite Ave Manteca, CA 95337
Call for an Appointment:
Valley Oak Dental Group
Swollen lymph nodes can appear all over your body and are typically a sign that your body is trying to fight something off. In many cases, swollen lymph nodes may appear when you go through dental issues. The lymph nodes could swell up on the neck or the back of the head. The swelling is typically temporary, especially when you’ve recently gone through dental issues.
Learn about some of the dental causes of swollen lymph nodes, your treatment options, and when to seek a dentist for professional help. The sudden appearance of a swollen gland may seem alarming, but knowing the direct connection will help you feel better until the swelling goes away.
Swollen Gums
One of the more basic ways your lymph nodes may swell from mouth issues is from swollen gums. Swollen gums can occur for a number of reasons. Improper tooth care, like a lack of adequate brushing or flossing can lead to gum diseases like gingivitis.
As the bacteria builds up, your body may try to fight off the bacteria and you could have swollen lymph nodes as a result. One of the best treatments for swollen gum issues is a dental cleaning. A professional can clean deep inside the gums to remove excess bacteria build-up. With less bacteria to fight, swollen lymph nodes will go down.
Swollen gums could also occur from mouth trauma. Mouth injuries could result in damaged and swollen gums. As the injury heals, your lymph nodes may swell. The nodes could stay swollen until after the gums have healed. Monitor the shape and size until they fully go away.
Infected Gums
Some swelling gums may be advanced beyond basic swelling and include deep infections. One of the more common infections that will cause lymph node swelling is a root infection like an abscess. If a tooth or gum abscess occurs, then you could run into major health issues. Lymph nodes will swell to help and fight the infection, but a dental treatment is often needed.
One of the main dental treatments to consider is a root canal. A root canal will treat the infection directly, prevent the loss of your teeth, and can reduce any pain inside your mouth. Swelling lymph nodes is one of the key signs of a root infection, but is often paired with physical pain or issues like sensitive teeth.
Post-Dental Treatments
In some cases, you may notice swollen lymph nodes after visiting the dentist. The swelling is typically normal and attributed to procedures beyond just a basic cleaning. For example, if you had any dental work done like fillings, crowns, or root canals, the swelling lymph nodes could be a sign that your body is directing more blood flow to repair and heal your mouth.
A dentist can give you information on the lymph nodes, including the average time before the swelling goes down. If swelling persists for longer periods of time, then you may need to contact your primary care doctor for a follow-up and lymph node exam. In some cases, you may need to do blood work to check blood counts or signs of other issues.
Mouth Sores
Sometimes, you will develop sores on the inside of your mouth. The sores could appear on the inside of your cheeks or the gums. The sores are typically known as canker sores, although there are some other varieties. You will notice the pain associated with the sore as the area feels very tender and raw.
When a sore develops, you may also notice swollen lymph nodes. This swelling is a common symptom of mouth sores and may go unnoticed when compared to the pain inside your mouth. A canker sore may take a couple of weeks to go away, and the swelling will typically follow the same trajectory.
The sores could appear inside of your mouth for a number of reasons. Some of the more common issues associated with dentistry include mouth infections, food allergies, and vitamin deficiencies. Vitamin deficiencies can also cause dental problems. For example, a vitamin D deficiency may cause issues like weak jaw bones and gum disease.
Bring up the frequency of any canker sores to a dentist. Not only can they examine the sore and provide a pain relief gel, but they can help rule out any dental issues that may be the direct cause of the problem. If a dental issues does appear, then the dentist will guide you through a treatment option to reduce sores and prevent swelling lymph nodes.
For more information on mouth issues and swollen lymph nodes, contact our office at Valley Oak Dental Group . We will help treat your mouth with the utmost care and can help you get through any oral issues you may have. Our dentists will take your swollen lymph nodes into accounts during the diagnosis and treatment of any dental conditions.
Search Post
Recent Posts

4 Reasons Diet Soda Is Just as Bad for Your Teeth as Regular Soda

Tooth Problems Associated With Swollen Lymph Nodes

5 Reasons to Choose a Dental Membership Plan Over Dental Insurance
Valley Oak Dental Group offers a variety of experienced dentists for your convenience. Get all your dental care in Manteca, CA with us.

Office Hours
Monday 8:00 am - 5:00 pm
Tuesday 6:00 am - 7:00 pm
Wednesday 8:00 am - 8:00 pm
Thursday 6:00 am - 5:00 pm
Friday 6:00 am - 5:00 pm
Every 3rd Saturday 8:00 am - 4:00 pm
Sunday Closed
Oral Surgery Hours Click Here
© 2024 Content, including images, displayed on this website is protected by copyright laws. Downloading, republication, retransmission or reproduction of content on this website is strictly prohibited.
Terms of Use | Privacy Policy | Disclaimer | Accessibility | HIPAA Website Built by BROADPROXIMITY
Top Family, Cosmetic and Implant Center In 537 Amherst St, Nashua, NH 03063
CALL US: (603) 882-3885
- Meet The Team
- Office Tour
- Tooth Extraction
- Custom Mouth Guards
- Dental Fillings
- Dental Inlays Onlays
- Dental Crown
- Dental Bridges
- Dental Implants
- Teeth Whitening
- Dental Veneers
- Dental Bonding
- Single Tooth Dental Implants
- Implant Supported Dentures
- Mini Dental Implants
- Guided Implant Placement
- Cad Cam Dental Restorations
- TMJ Disorders
- Snoring Therapy
- Sedation Dentistry
- Root Canal Treatment
- Endodontic Retreatment
- Pediatric Dentistry
- Interceptive Orthodontics for Children
- Dental Emergencies
- Crown Bridge Inlay Onlay
- Denture Partial Delivery
- Scaling And Root Planing
- Root Canal Therapy
- Soft Tissue Graft
- Implant Surgery Treatment
- Wisdom Teeth Removal
- Prophy Cleaning
- Fluoride Treatment
- Sealant Placement
- Pulp Treatment
- First Visit
- Practice Policies
- Delta Dental
- Blue Cross Blue Shield
- GEHA Dental Insurance Plan
- Guardian Dental
- Laser dentistry
- Digital Dentures
- Leica Microscope
- OP3D CT Scan
- 3Shape TRIOS Scanner
- SprintRay 3d printer
- Oral Health And Wellness
- Early Dental Care
- Tooth Eruption And Shedding
- Brush Timer
- Financial Options
- Read Our Reviews
- Pay My Bill Online
Pay My Bill
Request Appointment
Tooth Infection Swollen Lymph Nodes and Treatment
By Advanced Family Dentistry
February 6, 2024.
Picture this: you wake up one morning with a throbbing toothache. As the pain intensifies, you notice something else—swollen lymph nodes under your jaw on one side. What could be causing these symptoms? Could it be a tooth infection? The answer is yes! In this blog post, we will dive deep into the world of tooth infections and swollen lymph nodes, exploring their symptoms, causes, treatment options, and prevention tips.
Understaing Tooth Infections and Swollen Lymph Nodes
Bacteria can enter a tooth through a cavity, crack, or other dental problems, leading to tooth infections. The infection has the potential to spread to the tissues in the vicinity and even impact the lymph nodes.
Bad dental hygiene is one of the main causes of tooth infections. When we don’t regularly brush and floss, plaque accumulates on our teeth, giving dangerous bacteria a place to grow. These microorganisms have the ability to pierce the tooth’s enamel and induce an infection.
Did you know that approximately 10 to 20 percent of all lymph node enlargements are due to dental infections such as tooth abscesses? This alarming figure underscores the significant impact tooth infections can have on our health, particularly when it comes to swollen lymph nodes.
Swollen lymph nodes, also known as lymphadenopathy , refer to the enlargement of lymph nodes, which are small, bean-shaped structures found throughout the body. These nodes play a crucial role in the immune system, serving as filters that trap and destroy harmful substances like bacteria, viruses, and abnormal cells.
Symptoms of a Tooth Infection Swollen Lymph Nodes
- Toothache: A persistent pain, throbbing, or sensitivity in a specific tooth is a telltale sign.
- Swollen lymph nodes: Look for lumps under your jaw or neck, usually on the same side as the aching tooth. They might be tender or painful to the touch.
- Fever: A low-grade fever, especially if accompanied by chills, can indicate the body fighting infection.
- Facial swelling: In some cases, swelling might extend to your cheek or jaw, causing discomfort and asymmetry.
- Gum tenderness or redness: Inflammation around the infected tooth and its surrounding gums is a common symptom.
- Difficulty chewing or swallowing: Pain or discomfort while using your mouth can be another clue.
- Bad breath or a foul taste: The presence of bacteria and pus can lead to unpleasant odors.
- Spread of infection: The bacteria can travel to other parts of your body, causing serious health risks.
- Abscess formation: A painful collection of pus that requires immediate intervention.
- Bone damage: Untreated infections can erode the jawbone, potentially requiring complex treatments.

Causes of Tooth Infections Swollen Lymph Nodes
That nagging toothache isn’t just a nuisance; it could be a silent alarm for a brewing storm within your body. Swollen lymph nodes, those pea-sized lumps under your jaw or neck, often point to infection, and in up to 30% of cases, tooth infections are the culprit. Understanding the link between these two seemingly unrelated symptoms is crucial for safeguarding your oral and overall health.
- Cavities: Untreated cavities allow bacteria to infiltrate deeper tooth layers, leading to infection and inflammation.
- Gum Disease: This progressive disease weakens gum tissue, creating pockets where bacteria thrive and trigger infection.
- Cracked or Chipped Teeth: These openings serve as gateways for bacteria to invade the inner tooth, causing infection.
- Improper Dental Work: Faulty fillings, crowns, or root canals can harbor bacteria and lead to infection.
- Dental Injuries: Trauma to the tooth can damage nerves and blood vessels, increasing infection risk.
Your lymph nodes act as tiny filters, trapping bacteria and debris from nearby tissues. When a tooth infection flares up, the lymph nodes in your head and neck go on high alert, swelling as they work overtime to contain the invaders. This swelling is their way of signaling the immune system to fight the infection.
While tooth infections are a major cause, swollen lymph nodes can also stem from other head and neck issues, like:
- Ear infections
- Tonsillitis
Don’t Wait: Signs You Need Professional Help
Ignoring these signs can lead to severe complications, so be vigilant:
- Persistent toothache or sensitivity
- Tender, swollen lymph nodes under your jaw or neck
- Fever, especially with chills
- Facial swelling
- Gum redness or pus
- Difficulty chewing or swallowing
- Bad breath or foul taste
Treatment Options for Tooth Infections Swollen Lymph Nodes
Reducing inflammation and treating the underlying cause of the infection are the usual treatments for tooth infections and enlarged lymph nodes. It is imperative that you seek immediate dental care if you think you may have a tooth infection in order to avoid more complications.
Root canal therapy is a popular tooth infection treatment option. In order to stop reinfection, the infected pulp inside the tooth must be removed during this procedure and sealed. If a root canal is not an effective treatment for the infection, extraction may be required in certain cases.
Your healthcare provider may prescribe antibiotics to directly treat the infection or suggest over-the-counter pain relievers to reduce the swelling and discomfort associated with swollen lymph nodes. Rinses with warm saltwater can also aid in the healing and soothing of sore gums.
Prevention Tips for Avoiding Tooth Infections Swollen Lymph Nodes
It is essential to practice good oral hygiene in order to avoid swelling lymph nodes and tooth infections. The following advice will help you maintain the health of your gums and teeth:
- Brush twice a day: Ensure that you spend at least two minutes each time thoroughly cleaning your teeth with fluoride toothpaste. Remember to wash your tongue as well.
- Floss every day: Brushing may not be able to reach areas between your teeth where food particles and plaque are present. Regular flossing can help.
- Use mouthwash: To eliminate bacteria that cause oral infections, rinse your mouth with an antiseptic mouthwash after brushing and flossing.
- Schedule routine dental visits: Make an appointment for a dental examination at least twice a year to ensure thorough cleaning and early identification of any possible problems.
- Maintain a healthy diet and cut back on sugary drinks and foods, as they can aggravate tooth decay. Rather, choose nutrient-dense foods like dairy, whole grains, fruits, vegetables, and lean meats.
- Steer clear of tobacco use: Gum disease, which can result in tooth infections, is increased by smoking or chewing tobacco.
- Protect Your Teeth During Sports Activities: When playing contact sports, wearing mouthguards lowers the risk of injury or trauma that could result in an infection.
Good oral hygiene habits, such as brushing twice a day with fluoride toothpaste and flossing frequently, are the first line of defense against dental infections. It is crucial to schedule routine cleanings and exams at Advanced Family Dentistry Nashua in order to identify any early indications of decay and treat them before they worsen.
Yes, any type of tooth infection, from a small cavity to a severe abscess, can trigger swollen lymph nodes.
With proper treatment, they usually subside within a few days to a week.
Seek immediate medical attention if the nodes are large, painful, red, or accompanied by fever or facial swelling.
Warm compresses and rest can offer comfort. However, they don’t treat the underlying infection.
Untreated, they can signal a serious underlying infection and lead to complications.
Antibiotics treat bacterial infections, and if the swollen nodes are due to a tooth infection,
Related Articles
The Importance of Early Dental Care: Why Your Child Needs a Pediatric Dentist

Step-By-Step Guide On Preventing Tooth Decay

How a Professional Deep Cleaning Treats Gum Disease
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Oral Maxillofac Pathol
- v.21(1); Jan-Apr 2017
Benign reactive lymphadenopathy associated with submandibular gland enlargement during orthodontic treatment
Rohan pulgaonkar.
Department of Orthodontics, Army College of Dental Sciences, Secunderabad, Telangana, India
Prasad Chitra
Zama moosvi.
1 Department of Oral Pathology, Army College of Dental Sciences, Secunderabad, Telangana, India
Lymphadenopathy may be caused due to various reasons, most common being infections, neoplasms and immunologic disorders. Considering the frequent use of biomaterials in dentistry, it is not uncommon to find allergic reactions in the oral mucosa. Delayed-type hypersensitivity is one mechanism of allergy, which may manifest as either contact stomatitis or rarely present as only lymphadenopathy. An unusual case of unilateral submandibular gland swelling with associated lymphadenopathy during orthodontic treatment is reported. The processes followed in the differential diagnosis of the condition have been elucidated. Delayed hypersensitivity as a possible causative factor has been discussed. The article highlights the possibility of such conditions manifesting at any time during orthodontic therapy.
INTRODUCTION
Lymphadenopathy is the term used to describe the clinical sign of swelling of the lymph nodes. Lymphadenitis is the pathologic term for inflammation of the lymph nodes. When enlarged lymph nodes are detected, a cause has to be determined by careful medical history, thorough physical examination, judicious selection of laboratory tests and if necessary, a lymph node biopsy.[ 1 ] In general, there are two mechanisms of lymphadenopathy - hyperplasia and infiltration. The former occurs in response to immunologic or infectious stimuli, and the later is the result of infiltration by various cell types including cancer cells, lipid cells or glycoprotein-laden macrophages. When this occurs, lymph nodes may be detected clinically.[ 2 ]
Lymphadenopathy is a common clinical presentation. The cervical lymph nodes show a frequent tendency for enlargement considering their drainage from the oral cavity which houses the teeth communicating with the external environment. Cervical lymphadenopathy is often reactive and usually due to bacterial, viral infections, dental infections and surgical procedures in the head and neck region. Causes of cervical lymphadenopathy in a patient with other signs of systemic infection, trauma to oral structures or dental infections are easy to diagnose.[ 3 ] Difficulty arises when lymphadenopathy is the only clinical finding in an otherwise healthy patient. A spectrum of serious illness then come to act as differential diagnosis such as lymphomas, AIDS and malignancy in any other part of the body. Cervical lymphadenopathy is also seen in many oral surgical procedures; however, it is seen very rarely following orthodontic treatment.
Orthodontic materials such as monomer containing acrylic resins and nickel-containing stainless steels have been known to cause allergies in individuals. Autopolymerized methacrylate resins have shown greater leaching effects as compared to heat-cured resin. Among the metals used in orthodontics, nickel is one of the most common causes of contact dermatitis and produces more allergic reactions than all other metals combined. Nickel is also a primary component of orthodontic wires used for aligning of teeth.[ 4 , 5 , 6 ]
Unpolymerized resins have shown to cause varying effects when exposed to the oral environment, ranging from irritant contact dermatitis to neuropathy. Some studies have also shown methacrylate components to cause genetic and cellular damage. These leached monomers act as low-molecular weight molecules and penetrate the oral mucosa and lead to delayed type of hypersensitivity reactions. The antigens formed migrate to the regional lymph nodes through carrier system and present to the T-lymphocytes which undergo clonal expansion. This results in a localized inflammatory reaction on secondary exposure to the antigen, which can be in the form of a lymph node enlargement.[ 7 ]
Submandibular gland enlargement may be due to nonneoplastic causes such as mumps, sialadenitis, Sjogren's syndrome, cysts, infections and neoplasms of the salivary glands, lymphomas or any metastatic masses. Obstructive sialadenitis due to stones may account for approximately half of benign salivary gland disorders. On the other hand, salivary glands tumors are relatively rare and constitute 6% of all head and neck tumors. Various diagnostic methods such as fine-needle aspiration cytology, incisional biopsy, ultrasonography, computed tomography and magnetic resonance imaging are employed in the diagnosis of their etiology. Fine-needle aspiration cytology (FNAC) is a commonly used method for preoperative diagnosis of salivary gland swellings/mass before opting for the surgical route.[ 8 ]
The case report presented herewith is of a benign cervical lymphadenopathy and submandibular gland enlargement occurring in concurrence with orthodontic therapy.
CASE REPORT
A 13-year-old girl reported to the Department of Orthodontics and Dentofacial Orthopaedics, Army College of Dental Sciences, Secunderabad, with the chief complaint of forwardly placed upper front teeth and spacing [Figures [Figures1a, 1a , ,2a 2a and and3a 3a ].

(a) Pretreatment photographs, (b) frontal photograph with left-side swelling

(a) Pretreatment oblique lateral photograph, (b) oblique photograph with left side swelling

(a) Pretreatment intraoral photographs, (b) normal intraoral appearance during the onset phase
A full set of records needed for treatment planning were obtained which included:
- Study models
- Lateral cephalogram
- Orthopantomogram (OPG)
- Intraoral periapical (IOPA) X-rays of all the anterior teeth
- Extraoral and intraoral photographs.
Analysis of the records showed the patient to be a skeletal Class II malocclusion with a deficient mandible which necessitated functional orthopedic therapy with the “Twin-Block appliance”[ 9 , 10 , 11 ] to aid in mandibular advancement enabling correction of the sagittal skeletal discrepancy initially. The case would be reassessed for further dental treatment after completion of the functional phase. The functional appliance was a two-piece type with separate upper and lower components fabricated in heat-cured acrylic resin. Retention was obtained with stainless steel ball end clasps [ Figure 4 ].

“Twin-Block” functional appliance used in the patient
The patient reported with a diffuse swelling measuring approximately 40 mm in height and 53 mm in length on the left side of the face in the submandibular region after a period of 40 days [Figures [Figures1b 1b and and2b]. 2b ]. Case history revealed that the swelling developed over a period of 3 days with no signs of any respiratory tract infection or fever. On extraoral examination, a single, diffuse nonmovable swelling was observed in the left submandibular region which was nontender on palpation and firm in consistency. Intraoral examination showed no lesions, ulcerations or any tooth-related anomaly [ Figure 3b ]. Moreover, the oral hygiene status of the patient was also good. Bimanual palpation of the submandibular gland showed a normal gland texture. Salivary gland duct evaluation showed no abnormality with no history of “meal time syndrome.” Salivary flow tests were done, and results were within normal limits. Lymph node examination of the body in general was carried out to rule out generalized lymphadenopathy. The only positive clinical finding was a slight reduction in mouth opening owing to the swelling present in the region. A provisional diagnosis of reactive lymphadenopathy was made.
The functional therapy was immediately discontinued. Diagnostic IOPAs of the developing second molar regions as well as an OPG were recorded [ Figure 5 ]. The patient was advised investigations including a complete blood picture, ultrasonographic (USG) evaluation of the left submandibular gland region [ Figure 6 ] and a FNAC. The blood reports were nonspecific with the only significant finding being a mildly elevated erythrocyte sedimentation rate. USG scan revealed that the left submandibular gland was slightly enlarged as compared to the right with altered echotexture and increased vascularity on color Doppler. Enlarged cervical lymph nodes were noted at Levels I mainly and few in Level II and III during USG examination, with the largest one measuring 2.3 cm × 1.0 cm. Acid-fast bacillus smear and Mantoux test were done to rule out tuberculosis, and the test results were negative. Microscopic evaluation of the FNAC from left submandibular gland revealed few cells. It contained mostly blood and occasional salivary gland acini which were inadequate for diagnosis.

No relevant findings evident on orthopantomogram examination

Ultrasound of left submandibular gland
A final diagnosis of reactive lymphadenopathy with submandibular gland sialadenitis was given. After discussion with an oral surgeon, a period of observation without using any medication and temporary discontinuation of the appliance was decided on. The patient reported to the clinic 3 days later without any swelling which was surprising considering its size on initial presentation. As a matter of precaution, orthodontic appliance therapy was temporarily halted for another 3 weeks. The patient started wearing the removable functional appliance after completion of the period of observation. Treatment progressed smoothly with no further recurrence in symptoms.
Lymphadenopathy is a term that describes an abnormality in either size, consistency or number of lymph nodes. It can be broadly classified as either generalized or localized. Generalized lymphadenopathy requires the involvement of at least two or more noncontiguous areas while localized involves only one area.[ 3 ]
There are various causes for lymphadenopathy ranging from infections, immunologic disorders, malignancies, drug reactions, etc.,[ 2 ] [ Table 1 ]. The most common cause for submandibular lymphadenopathy is infections of the head, neck, sinuses, ears, eyes, scalp and pharynx. Less common causes for submandibular lymphadenopathy include malignancies or immunologic disorders such as Sjogren's syndrome. Drug hypersensitivity uncommonly is also a cause for submandibular lymphadenopathy. Similarly, hypersensitivity to dental biomaterials can also cause allergic manifestations.[ 12 ]
Causes of lymphadenopathy

All dental biomaterials release substances into the oral cavity to a varying degree. The biological reactions between dental biomaterials and the oral mucosa can take place at a local level or far from the site of contact. Most components of these materials are of low-molecular weight. By acting as haptens and combining with body proteins, they may form complete antigens capable of inducing sensitization of immunologically competent cells. Methyl methacrylate (MMA) is a widely used monomer in dentistry and has been reported to cause various abnormalities such as irritation to skin, eyes and mucous membranes, allergic dermatitis, stomatitis, asthma, neuropathy, disturbances of central nervous system, liver toxicity and fertility problems. Thus, the monomer from the MMA acts as a hapten sensitizing the T-lymphocytes which in turn undergo clonal expansion leading to lymphadenopathy.[ 7 ]
Delayed hypersensitivity reactions (Type IV) hypersensitivity is involved in the pathogenesis of many autoimmune and infectious disorders. It may also be caused by foreign antigens such as chemicals and heavy metals. Contact dermatitis and stomatitis are an important form of delayed-type hypersensitivity. The reaction time take in delayed hypersensitivity reactions can vary from 48 to 72 h up to 21–28 days.[ 13 ]
The vascularity and semi-permeability of the oral mucosa allow the easy penetration of the monomer that is leached out of the orthodontic appliance into the underlying tissues and blood vessels which in turn can lead to a possible delayed hypersensitivity reaction that may manifest either as contact stomatitis or as lymphadenopathy. The present case did not show any infective, immunologic or neoplastic cause for the lymphadenopathy which was ruled out by doing a series of investigations based on a diagnostic algorithm for the lymphadenopathy.
There are various causes for submandibular gland enlargement as listed in Table 2 . Allergic reactions are an established cause for gland enlargement as listed by the WHO.[ 14 ] A study conducted by Kamogashira et al .[ 15 ] involving the use orthodontic appliances in rats showed submandibular and sublingual gland swelling. However, no human studies are available to corroborate the same till date.
Causes of submandibular gland enlargement

We can deduce from this that the leaching of monomer from the appliance might have caused a delayed-type hypersensitivity reaction which caused the enlargement of the submandibular gland.
This paper presents a unique first of its kind situation involving orthodontic therapy causing this unexpected condition. Dentists need to be aware of the possibility of lymphadenopathies and salivary gland enlargement occurring in conjunction with orthodontic procedures and undertake preventive methods to avoid such circumstances.
In a study done by Bural et al .[ 16 ] it was established that the effects produced by leaching of the monomer can be minimized by immersion of the appliance for 1–2 h in boiling water before the final delivery. Hence, it is recommended to follow these simple, yet important steps before insertion of dental appliances to avoid the possibility of leaching monomer and subsequent hypersensitivity reactions.
Delayed-type hypersensitivity can manifest as contact stomatitis or lymphadenopathy or even rarely salivary gland enlargement. Materials used in orthodontic appliances may possibly leach over a period of time and can cause delayed hypersensitivity reactions. Hence, it is important for dental professionals to be aware of this possibility and follow proper procedures to minimize the leaching of monomers after insertion of the appliance.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.
Cervical lymphadenopathy in the dental patient: a review of clinical approach
Affiliation.
- 1 Division of Oral Medicare, University of Medicine and Dentistry of New Jersey, 110 Bergen Street, D-860, Newark, NJ 07101, USA. [email protected]
- PMID: 15954248
Lymph node enlargement may be an incidental finding on examination, or may be associated with a patient complaint. It is likely that over half of all patients examined each day may have enlarged lymph nodes in the head and neck region. There are no written guidelines specifying when further evaluation of lymphadenopathy is necessary. With such a high frequency of occurrence, oral health care providers need to be able to determine when lymphadenopathy should be investigated further. Although most cervical lymphadenopathy is the result of a benign infectious etiology, clinicians should search for a precipitating cause and examine other nodal locations to exclude generalized lymphadenopathy. Lymph nodes larger than 1 cm in diameter are generally considered abnormal. Malignancy should be considered when palpable lymph nodes are identified in the supraclavicular region, or when nodes are rock hard, rubbery, or fixed in consistency. Patients with unexplained localized cervical lymphadenopathy presenting with a benign clinical picture should be observed for a 2- to 4-week period. Generalized lymphadenopathy should prompt further clinical investigation. This article reviews common causes of lymphadenopathy, and presents a methodical clinical approach to a patient with cervical lymphadenopathy.
- Arthritis, Rheumatoid / complications
- Bacterial Infections / complications
- Cat-Scratch Disease / complications
- Dental Care for Chronically Ill*
- Diagnosis, Differential
- Drug Hypersensitivity / complications
- Head and Neck Neoplasms / complications
- Lupus Erythematosus, Systemic / complications
- Lymphatic Diseases / blood
- Lymphatic Diseases / etiology*
- Lymphatic Diseases / pathology
- Medical History Taking
- Neck* / pathology
- Respiratory Tract Infections / complications
- Sjogren's Syndrome / complications
- Toxoplasmosis / complications
- Tuberculosis, Lymph Node / diagnosis
- Virus Diseases / complications
Swollen Jaw Symptoms, Causes, and Treatment

In this article
When to Seek Medical Help
If you are experiencing pain in your jaw, swollen gums, or difficulty chewing, consult a dentist or doctor. If you have a fever or if the pain worsens over time, seek medical attention as soon as possible.
In some cases, an infection in the mouth may cause swelling. Antibiotics or a simple dental procedure can usually treat this. However, you may need surgery if you experience severe pain and swelling that does not go away after 2 weeks of treatment.
If you have additional symptoms with a swollen jaw, speak to a doctor rather than a dentist.
Can Jaw Swelling Cause Complications?
A common complication associated with jaw swelling is difficulty swallowing or breathing. 21 This can lead to choking and aspiration pneumonia if the person cannot clear the food from the throat.
8 Potential Causes of Swelling in the Jaw and Neck
There are several causes of swelling in the jaw and surrounding areas. It’s important to recognize your symptoms to determine whether the cause is severe.
1. Viral infections
Viral infections, such as those that cause mononucleosis or the flu, often cause lymph nodes in the neck to swell. 1 If you experience these swollen glands, a virus could be causing them.
Symptoms
You may also experience other symptoms, such as:
- Sore throat
If you have these symptoms and swollen lymph nodes that don’t improve after a few days, speak to your doctor. They will check that the infection is not something more severe like an abscess.
Antibiotics do not work for viral infections. Antiviral medications, however, help the body fight off harmful viruses by easing symptoms and shortening the length of an infection.
2. Tonsillitis
Tonsillitis is an inflammation of the tonsils. The tonsils are two small, oval-shaped organs at the back of the throat. They help fight infection in the mouth and throat. Bacteria usually cause tonsilitis. 2

Symptoms of tonsillitis include:
- Swollen lymph nodes in the neck
- Difficulty swallowing food or drink (dysphagia)
- Ear pain (otalgia)
- Bad breath (halitosis)
- Nausea and vomiting
Healthcare providers usually prescribe antibiotics to prevent the bacterial infection from spreading. Surgeons may need to remove your tonsils if they become severely infected, or if your tonsils keep getting re-infected.
3. Thyroid Nodules
The thyroid gland is a butterfly-shaped organ in the neck, just below the larynx. It produces hormones that help regulate metabolism and control how quickly the body uses energy. The thyroid gland also makes hormones that affect the body’s sensitivity to other hormones.

Thyroid nodules are small lumps that form on the thyroid gland. They can be cancerous or benign (not cancerous). Most thyroid nodules are benign. 6
Symptoms may include:
- A lump in the neck
- A tickling sensation in the throat
Benign nodules can be treated with medication or surgery if they cause discomfort or other problems. Malignant nodules must be treated with surgery, radiation therapy, and/or chemotherapy. 7
4. Strep Throat
Streptococcal pharyngitis, also known as strep throat, is a bacterial infection caused by group A beta-hemolytic streptococcus bacteria that results in tonsil swelling.
The infection usually starts with a sore throat and a fever and can impact surrounding areas, like the jaw. Left untreated, it can lead to complications such as rheumatic fever and kidney damage.
Common symptoms of strep throat include: 8
- Pain when swallowing
- Swollen tonsils, sometimes with pus or white patches
- Tiny, red spots on the roof of the mouth (petechiae)
The most common treatment for this condition is antibiotics. Doctors typically prescribe penicillin or amoxicillin to treat the infection. 9 It is important to finish the entire course of antibiotics to prevent the infection from returning.
Approximately 1.2% of people will be diagnosed with cancer of the oral cavity and/or pharynx at some point in their life. 10
Oral cancer usually starts in the cells lining the inside of the mouth and throat. It can also affect parts of the voice box, tonsils, and other nearby tissues.
Oral cancer is typically caused by tobacco or alcohol abuse, but it can also be caused by human papillomavirus (HPV) infection and certain types of herpes virus infections. 11
Other types of cancer that may cause swelling in the head and neck area include throat and thyroid cancer. If cancer from other areas spreads to the lymph nodes, the lymph nodes can also become swollen.
Symptoms vary depending on the type of cancer but may include: 12
- Red or white patches
- Pain, tenderness, or numbness in the mouth or lips
- A sore or irritation that doesn’t go away
- A lump, rough spot, crust, or small sore area that doesn’t go away
- Difficulty moving the tongue or jaw while chewing, swallowing, or speaking
First, a doctor will conduct a physical examination. They may order X-rays or other imaging tests to identify the location and size of the tumor.
Oral cancer treatment depends on the location, size, and whether it has spread to lymph nodes or other parts of the body. Treatment can include surgery, radiation therapy, chemotherapy, immunotherapy, or a combination.
6. Tooth Abscess
A tooth abscess results from bacteria entering your tooth and creating a pocket of pus, which can cause swelling around your gums. This can be attributed to gum disease, broken teeth, trauma or injury to the teeth, and big cavities.

Symptoms may include: 13
- Intense, throbbing tooth pain
- Pain that radiates outwards toward the ear, jaw, and neck
- Red and swollen gums
Abscessed teeth are a serious condition. If left untreated, the infection can spread to the surrounding areas, including the jawbone and surrounding teeth and soft tissues. If you suspect you have an abscessed tooth, visit a dentist as soon as possible.
Treatment involves draining the abscess of pus and administering antibiotics.
7. Pericoronitis
Pericoronitis is a condition that arises when the gum tissue surrounding a newly erupting tooth becomes inflamed. This condition commonly occurs when wisdom teeth come in, specifically when the teeth do not have enough room to erupt from the gums. 14

The condition can lead to extensive damage to the teeth, jaw, and mouth if left untreated.
Symptoms may include: 15
- Redness or swelling of the gums
- Pus or drainage
- Severe pain around the back teeth
- Difficulty opening your mouth
Chronic pericoronitis symptoms may include:
- Temporary achiness around the back teeth
- A bad taste
Treatment involves removing the tissue flap or wisdom tooth.
8. Lyme Disease
Lyme disease is a bacterial infection that spreads through the bite of infected ticks.
Symptoms may include: 18
- A characteristic “bulls-eye” rash at the site of the tick bite
- Flu-like illness
- Muscle aches
- Swelling or redness
A short course of oral antibiotics, such as doxycycline or amoxicillin, cures most cases of early Lyme disease. 19 For more complicated cases, Lyme disease is usually successfully treated with additional antibiotics. 20
Listen In Q&A Format
Newmouth podcast.

Why Do I Have Swelling Around My Jaws or Neck?
The human jaw is an integral part of the body. It has many functions, including chewing and speaking. The jaw is connected to the skull and can be affected by diseases, trauma, and other serious health conditions.
Jaw and neck swelling can be symptoms of many conditions, such as an infection, injury, or inflammation. Certain medications may also cause swelling in these areas.
Speak to your doctor or dentist if you experience other symptoms or they don’t resolve themselves after a few days.
Share this article
Related pages.

Swollen Tonsils - Symptoms, Causes & Treatments
Medically Reviewed by Khushbu Gopalakrishnan

Why Does My Throat Hurt on One Side When I Swallow?
by Caroline Bonin
10 min read

What Does Throat Cancer Feel Like? Symptoms, Risk Factors & Treatment
Medically Reviewed by Erica Anand

Tonsil Stones: Causes, Symptoms & Treatment

Pain When Swallowing: Causes, Relief, and Treatment
Medically Reviewed by Elena Borrelli

White Spots in the Throat: Are They a Sign of Early-Stage Throat Cancer?
Medically Reviewed by Nandita Lilly
- Mayo Clinic. “ Mononucleosis ,” 2020.
- Mayo Clinic. “ Tonsillitis ,” 2022.
- Cleveland Clinic. “ Swollen Lymph Nodes ,” 2022.
- Mayo Clinic. “ Swollen lymph nodes: symptoms and causes ,” 2021.
- Mayo Clinic. “ Swollen lymph nodes: diagnosis and treatment ,” 2021.
- American Thyroid Association. “ Thyroid Nodules ,” n.d.
- American Cancer Society. “ Treatment of Thyroid Cancer, by Type and Stage ,” 2021.
- Centers for Disease Control and Prevention. “ Strep Throat: All You Need to Know ,” 2022.
- Cleveland Clinic. “ Strep Throat ,” 2019.
- National Cancer Institute. “ Cancer Stat Facts: Oral Cavity and Pharynx Cancer ,” n.d.
- American Cancer Society. “ Risk Factors for Oral Cavity and Oropharyngeal Cancers ,” 2021.
- American Dental Association. “ Oral Cancer ,” n.d.
- American Dental Association. “ Abscess (Toothache) ,” n.d.
- Kwon, Gloria, et al. “ Pericoronitis” StatPearls, 2022.
- Cleveland Clinic. “ Pericoronitis ,” 2022.
- Centers for Disease Control and Prevention. “ Symptoms of ME/CFS ,” 2021.
- Centers for Disease Control and Prevention. “ Treatment of ME/CFS ,” 2021.
- Centers for Disease Control and Prevention. “ Signs and Symptoms of Untreated Lyme Disease ,” 2021.
- Centers for Disease Control and Prevention. “ Erythema migrans rash ,” 2022.
- National Institute of Allergy and Infectious Diseases. “ Lyme Disease Antibiotic Treatment Research ,” 2018.
- Health Direct. “ Toothache and swelling ,” 2022.

Cookies on GOV.UK
We use some essential cookies to make this website work.
We’d like to set additional cookies to understand how you use GOV.UK, remember your settings and improve government services.
We also use cookies set by other sites to help us deliver content from their services.
You have accepted additional cookies. You can change your cookie settings at any time.
You have rejected additional cookies. You can change your cookie settings at any time.
Monkeypox cases confirmed in England – latest updates
Latest updates on cases of monkeypox identified by the UK Health Security Agency (UKHSA).

UKHSA has published the latest epidemiological overview for the ongoing monkeypox outbreak.
Thursday 1 September 2022
Monkeypox case linked with travel to west africa identified.
UKHSA has confirmed that an individual has been diagnosed with monkeypox linked to recent travel to West Africa.
Preliminary genomic sequencing conducted by UKHSA indicates that this case does not have the current outbreak strain circulating in the UK. The individual has been admitted to the High Consequence Infectious Disease ( HCID ) unit at the Royal Liverpool University Hospital in line with standing advice from the Advisory Committee on Dangerous Pathogens ( ACDP ).
Contact tracing of close contacts of the individual is underway. So far, no further linked cases have been identified.
Dr Sophia Maki, Incident Director, UKHSA , said:
We are working to contact the individuals who have had close contact with the case prior to confirmation of their infection, to assess them as necessary and provide advice. UKHSA and the NHS have well established and robust infection control procedures for dealing with cases of imported infectious disease and these will be strictly followed and the risk to the general public is very low. We remind everyone who is planning to travel to West and Central Africa to be alert for the symptoms of monkeypox and to call 111 if you have symptoms on your return.
The ACDP has previously advised that importations of monkeypox directly from West Africa as well as cases caused by Clade I of the virus should still be classified as HCIDs as we cannot predict their characteristics.
Tuesday 30 August 2022
Tuesday 23 august 2022.
UKHSA has published the latest epidemiological overview for the ongoing monkeypox outbreak.
Tuesday 16 August 2022
Tuesday 9 august 2022.
UKHSA has published the latest epidemiological overview for the ongoing monkeypox outbreak.
It shows that as of 8 August 2022, there are 2,914 confirmed and 103 highly probable monkeypox cases in the UK: 3,017 in total. Of these, 2,883 are in England.
A breakdown of cases by upper tier local authority has also been published today.
Data will now be published once a week on Tuesdays.
Dr William Welfare, Incident Director at UKHSA , said:
While the most recent data suggests the growth of the outbreak has slowed, we continue to see new cases every day. While anyone can get monkeypox, the majority of monkeypox cases in the UK continue to be in gay, bisexual and other men who have sex with men, with the infection being passed on mainly through close contact in interconnected sexual networks. Please continue to be aware of symptoms, including rashes and blisters, particularly if you have recently had a new sexual partner.
Friday 5 August 2022
It shows that as of 4 August 2022, there are 2,768 confirmed and 91 highly probable monkeypox cases in the UK: 2,859 in total. Of these, 2,730 are in England.
It also includes a breakdown of cases in England by region, which demonstrates that a high proportion of cases are in London.
Further epidemiological data and additional analysis can be found in UKHSA ’s regular monkeypox technical briefings .
Tuesday 2 August 2022
It shows that as of 1 August 2022, there are 2,672 confirmed and 87 highly probable monkeypox cases in the UK: 2,759 in total. Of these, 2,638 are in England.
Further epidemiological data and additional analysis can be found in UKHSA ’s regular monkeypox technical briefings .
Friday 29 July 2022
It shows that as of 28 July 2022, there are 2,469 confirmed and 77 highly probable monkeypox cases in the UK: 2,546 in total. Of these, 2,436 are in England.
It also includes a breakdown of cases in England by region, which demonstrates that a significant majority of cases are in London.
Further epidemiological data and additional analysis can be found in UKHSA ’s regular monkeypox technical briefings .
Tuesday 26 July 2022
Up to 25 July 2022, there were 2,367 confirmed and 65 highly probable monkeypox cases in the UK: 2,432 in total.
To expand the UK’s capability to detect monkeypox cases, some NHS laboratories are now testing suspected monkeypox samples with an orthopox polymerase chain reaction ( PCR ) test (orthopox is the group of viruses which monkeypox is part of). Since 25 July 2022, the monkeypox case definition recognises those who are orthopox-positive as highly probable cases, and those who test positive on a monkeypox PCR test as confirmed cases.
Dr Sophia Makki, National Incident Director at UKHSA , said:
Monkeypox cases continue to rise, with the virus being passed on predominantly in interconnected sexual networks. Before you have sex, go to a party or event, check yourself for monkeypox symptoms, including rashes and blisters. If you have monkeypox symptoms, take a break from attending events or sex until you’ve called 111 or a sexual health service and been assessed by a clinician. Vaccination will further strengthen our monkeypox response and so we urge all those who are eligible for the vaccine to take it up when offered. It will help protect yourself and others you have had close contact with. While the infection is mild for many, it can cause severe symptoms and hospitalisation in some. Please remember that the vaccine may not provide complete protection against monkeypox, so it is still important to be alert for the symptoms of monkeypox and call 111 or a sexual health clinic if you develop any. The NHS will provide the vaccine to those eligible, so please wait until you are contacted.
Friday 22 July 2022
It shows that as of 21 July 2022, there were 2,208 confirmed cases in the UK. Of these, 2,115 are in England.
UKHSA has also published its fourth technical briefing on the ongoing monkeypox outbreak today. The briefing is based on figures from 20 July 2022. So far, the evidence suggests that transmission continues to occur primarily within interconnected sexual networks. Currently we are not seeing significant levels of transmission outside of these networks, but we continue to monitor for changes.
The most recent data suggests that the growth of the outbreak may have slowed. This means that we continue to identify new infections but at a more stable rate.
Dr Meera Chand, Director of Clinical and Emerging Infections at UKHSA , said:
While anyone can catch monkeypox, the majority of monkeypox cases in the UK continue to be in gay, bisexual and other men who have sex with men ( MSM ), with the infection being passed on mainly through close contact between people in interconnected sexual networks. Before you go to a party or event, check yourself for monkeypox symptoms, including rashes and blisters. If you have monkeypox symptoms, take a break from attending events or sex until you’ve called 111 or a sexual health service and been assessed by a clinician. It can take up to 3 weeks for symptoms to appear after being in contact with someone with monkeypox, so stay alert for symptoms after you have skin to skin or sexual contact with someone new.
UKHSA will continue to publish regular technical briefings as the response to the outbreak continues.
Tuesday 19 July 2022
Ukhsa procures more than 100,000 additional vaccine doses and updates close contact guidance as monkeypox cases rise to 2,137.
It shows that as of 18 July 2022, there were 2,137 confirmed cases in the UK. Of these, 2,050 are in England.
UKHSA guidance for close contacts of a confirmed monkeypox case has been updated. This means close contacts won’t need to isolate at home if they don’t have symptoms.
The change is being implemented in response to latest data showing that a relatively small number of close contacts have gone on to develop monkeypox and a lack of evidence of transmission outside of close intimate or sexual contact, now that more epidemiological information is available. It means the latest guidance is proportionate to the latest transmission risks identified and is in line with advice from the WHO , other European countries and the CDC .
For category 2 and category 3 close contacts we now recommend people:
- contact NHS 111 or a sexual health clinic if they develop a fever or any of the other symptoms described below
- avoid skin to skin contact with others, such as hugging and kissing
- refrain from sexual or intimate contact
- avoid international travel if possible; travel insurance may also not be valid for people advised not to travel
- let health or dental facility staff know they’re a close contact before attending for health or dental care
For category 3 close contacts:
- we recommend avoiding close contact with children aged under 5 years, pregnant women and those who have an impaired immune system
- if they work with children aged under 5 years, pregnant women or those who have an impaired immune system, UKHSA or their employer might inform them if they need to take time off – this decision will be based on a personalised clinical assessment
A smallpox vaccine is still being offered to close contacts with higher risk exposure on a case by case basis.
Trained health protection teams carry out detailed clinical assessments of each case to inform their recommendations and categorisation.
Dr Merav Kliner, Deputy Incident Director at UKHSA , said:
We have now passed over 2,000 confirmed cases of monkeypox in the UK, and the outbreak continues to grow. Based on the growing evidence of how the monkeypox virus is being passed on in this outbreak, close contacts will no longer have to isolate for 21 days unless they develop symptoms. While our advice on isolation is changing, monkeypox is still a serious public health challenge, and we urge contacts to take a break from any activities or events involving skin to skin contact, including sex, hugging and kissing to reduce the risk of the virus being passed on unknowingly. Stay alert to symptoms and call a sexual health clinic if you become unwell. Thank you to all contacts who have isolated already in response to this outbreak. We understand that isolation can be difficult but this was a necessary precaution whilst our knowledge of the outbreak was limited.
In response to the ongoing monkeypox outbreak, UKHSA has procured more than 100,000 additional doses of the smallpox vaccine enabling more people to be vaccinated to prevent infection and limit transmission of the virus.
Additional doses will arrive from the manufacturer, Bavarian Nordic, this month, with the remainder expected by September.
The UK previously procured nearly 30,000 doses, enabling the NHS to begin rollout of the vaccine programme to individuals who are most likely to acquire the virus.
While anyone can get monkeypox, the majority of cases in the UK continue to be in gay, bisexual and other men who have sex with men ( GBMSM ), with the infection being passed on mainly through close contact between people in interconnected sexual networks.
An individual’s eligibility for vaccination is detailed in the UKHSA vaccination strategy which was endorsed by the Joint Committee on Vaccination and Immunisation ( JCVI ).
The vaccine will be offered to some GBMSM who are more likely to acquire the virus, with eligibility based on a number of factors, similar to the criteria used to assess those eligible for HIV pre-exposure prophylaxis ( PrEP ), even if they are already living with HIV.
Health and Social Care Secretary Steve Barclay said:
Monkeypox is a rare and usually mild disease that does not spread easily between people, but we are taking action to help further manage the outbreak in the UK by procuring over 100,000 additional doses of vaccine. The NHS is already contacting those eligible for the vaccine, and I would urge people to take up the offer as soon as they are contacted. In the meantime, please contact a sexual health clinic if you notice any unusual rashes or lesions. I am hugely grateful to the fantastic sexual health staff and 111 call handlers for working hard to keep the current outbreak under control.
Dr Gayatri Amirthalingam, Head of Immunisation at UKHSA , said:
These additional doses mean that we are in an even stronger position to bring the current monkeypox outbreak under control, ensuring those most likely to acquire the virus are protected from infection. We would like to thank our colleagues in sexual health services for all their hard work in rolling out the vaccination programme. Although most cases of monkeypox in the current outbreak are mild, severe illness can occur in some people, so it is important we use the available vaccine to reach groups where transmission is occurring. Anyone can get monkeypox and we continue to urge anyone with a rash with blisters, or any other monkeypox symptoms, to take a break from events, meeting with friends or having sexual contact. Instead, stay at home and contact 111 or your local sexual health service for advice.
The NHS is already rolling out the vaccine to those who are more likely to acquire the virus, including healthcare workers in specialist roles and in clinics where exposure to monkeypox is highest.
The NHS is contacting GBMSM who are eligible for the vaccine.
Friday 15 July 2022
It shows that as of 14 July 2022, there were 1,856 confirmed cases in the UK. Of these, 1,778 are in England.
Full guidance on semen testing for monkeypox for clinicians has been published.
The evidence relating to the transmission of monkeypox through semen is limited at the present time. In line with the World Health Organization’s ( WHO ) guidance, UKHSA is now advising people to use condoms for 12 weeks after infection. This is a precaution to reduce the risk of spreading the virus to a partner.
We continue to advise those with monkeypox to not have sex while symptomatic and while lesions are present.
Tuesday 12 July 2022
It shows that as of 11 July, there were 1,735 confirmed cases in the UK. Of these, 1,660 are in England.
Friday 8 July 2022
It shows that as of 7 July, there were 1,552 confirmed cases in the UK. Of these, 1,482 are in England.
Tuesday 5 July 2022
As of 4 July, the total number of monkeypox cases in the UK is 1,351 .
Dr Meera Chand, Director of Clinical and Emerging Infections at UKHSA , said:
As of July 2022, the current outbreak clade of monkeypox is no longer classified as a high consequence infectious disease ( HCID ) , following review by the Advisory Committee on Dangerous Pathogens ( ACDP ) and agreement by the UK 4 nations public health agencies.
This does not alter the public health response or measures taken to control monkeypox, but relates to which clinical pathways are used in the NHS.
This decision has been taken because the current outbreak does not meet the criteria for a high consequence infectious disease, which is defined as having a high mortality rate and a lack of available interventions.
We have had no reported deaths from monkeypox in the UK and we have vaccine available for higher risk contacts, healthcare workers who are caring for and who are due to start caring for a patient with confirmed monkeypox, and a new vaccination programme for those who are most at risk.
Future importations of monkeypox directly from West Africa as well as cases caused by the Congo basin clade of the virus will still be classified as HCIDs as we cannot predict their characteristics.
UKHSA is now working to adapt case and contact management using the growing body of evidence about the outbreak. The majority of contacts of cases will no longer be contacted every day following their initial notification and will instead be provided with contact details to approach if they develop symptoms.
This change has been made in light of the emerging evidence about disease severity, meaning that suspected cases do not need to be rapidly transferred to hospital.
NHS England is due to set out details on how eligible people can get vaccinated shortly. People are advised not to come forward for the vaccine until contacted.
Friday 1 July 2022
UKHSA has published the latest data report on monkeypox in the UK.
As of Thursday 30 June, there are 1,235 confirmed cases in the UK.
Wendi Shepherd, monkeypox incident director at UKHSA , says:
The monkeypox outbreak continues to grow. Our investigations and information from confirmed cases continue to show that the overwhelming majority of cases are in gay, bisexual or other men who have sex with men. This weekend, let’s enjoy Pride safely – before you go to any events or parties, check yourself for blister-like spots and rashes. Please don’t attend if you have monkeypox symptoms or feel unwell. If you have a rash or blisters, stay at home, phone a sexual health clinic, and get tested. Please be vigilant for any monkeypox symptoms in the coming weeks – especially if you are having sex with someone new. To assist with our contact tracing, we encourage everyone to ensure they exchange contact details with sexual partners, to help us limit further transmission where cases occur.
Anyone can get monkeypox and it can spread from person to person through:
- touching clothing, bedding or towels used by someone with the monkeypox rash
- touching monkeypox skin blisters or scabs (including during sex)
- the coughs or sneezes of a person with the monkeypox rash
We have been advising event organisers throughout the outbreak. See the latest guidance for organised events and mass gatherings .
Tuesday 28 June 2022
As of Sunday 26 June, there are 1,076 confirmed cases in the UK.
This report is published every Tuesday and Friday.
Dr Sophia Makki, Incident director at UKHSA said:
The monkeypox outbreak in the UK continues to grow, with over a thousand cases now confirmed nationwide. We expect cases to continue to rise further in the coming days and weeks. If you are attending large events over the summer or having sex with new partners, be alert to any monkeypox symptoms so you can get tested rapidly and help avoid passing the infection on. Currently the majority of cases have been in men who are gay, bisexual or have sex with men. However, anyone who has had close contact with an individual with symptoms is also at increased risk. If you are concerned that you may have monkeypox, don’t go to events, meet with friends or have sexual contact. Instead, stay at home and contact 111 or your local sexual health service for advice. We are grateful to all the people who have come forward so far for testing and to assist us with our contact tracing.
Tuesday 21 June 2022
UKHSA is now publishing a regular data report on monkeypox in the UK.
The report will be published every Tuesday and Friday.
Dr Sophia Makki, Incident Director at UKHSA , said:
We continue to see a steady increase in monkeypox cases. We’re reminding everyone to be aware of the symptoms of monkeypox, particularly if you’ve recently had new or multiple sexual partners, to help prevent further spread and protect others. If you have a rash with blisters, or any other monkeypox symptoms, don’t go to events, meet with friends or have sexual contact. Instead, stay at home and contact 111 or your local sexual health service for advice. Please contact the clinic ahead of your visit and avoid close contact with others until you’ve been reviewed by a clinician.
Monday 20 June 2022
From this week, UKHSA will be moving to a twice-weekly schedule for reporting monkeypox case numbers in the UK.
Updated case data will be published on Tuesdays and Fridays beginning on Tuesday 21 June.
Friday 17 June 2022
The UK Health Security Agency ( UKHSA ) has detected 46 additional cases of monkeypox in England, 3 additional cases in Scotland and 1 in Wales.
This brings the total number confirmed in the UK to 574, as of 16 June.
There are currently 550 confirmed cases in England, 16 in Scotland, 2 in Northern Ireland and 6 in Wales.
Anyone can get monkeypox, particularly if you have had close contact, including sexual contact, with an individual with symptoms. Currently most cases have been in men who are gay, bisexual or have sex with men.
Contact a sexual health clinic if you have a rash with blisters and you’ve been either:
- in close contact, including sexual contact, with someone who has or might have monkeypox (even if they’ve not been tested yet) in the past 3 weeks
- to West or Central Africa in the past 3 weeks
Dr William Welfare, Incident Director at UKHSA , said:
As case numbers of monkeypox continue to rise and with many summer events and festivals ahead, we’re reminding people to be aware of the symptoms of monkeypox, particularly if you’ve recently had new or multiple sexual partners, to help prevent further spread and protect others. If you have a rash with blisters, or any other monkeypox symptoms, don’t go to events, meet with friends or have sexual contact. Instead, stay at home and contact 111 or your local sexual health service for advice. Please contact the clinic ahead of your visit and avoid close contact with others until you’ve been seen by a clinician. UKHSA is working closely with partners across the country, including event organisers and venues, to raise public awareness of monkeypox symptoms so everyone has a safe, happy and healthy summer.
Wednesday 15 June 2022
The UK Health Security Agency ( UKHSA ) has detected 52 additional cases of monkeypox in England, one additional case in Scotland and one in Wales.
This brings the total number confirmed in the UK to 524, as of 14 June.
There are currently 504 confirmed cases in England, 13 in Scotland, 2 in Northern Ireland and 5 in Wales.
- in close contact, including sexual contact, with someone who has or might have monkeypox (even if they’ve not been tested yet) in the past 3 weeks.
- to West or Central Africa in the past 3 weeks.
Monday 13 June 2022
The UK Health Security Agency ( UKHSA ) has detected 104 additional cases of monkeypox in England.
This brings the total number confirmed in the UK to 470, as of 12 June.
There are currently 452 confirmed cases in England, 12 in Scotland, 2 in Northern Ireland and 4 in Wales.
UKHSA publishes first monkeypox technical briefing
The UK Health Security Agency ( UKHSA ) has published its first technical briefing on the ongoing monkeypox outbreak. The briefing shares UKHSA analysis with other public health investigators and academic partners.
This first publication includes updated epidemiological data, with evidence from anonymised detailed interviews with patients which are helping us to understand transmission and to determine how to target interventions.
Of the cases interviewed, 81% were known to be London residents and 99% were male. The median age of confirmed cases in the UK was 38 years old.
152 cases participated in more detailed questionnaires. In this data, 151 of the 152 men interviewed identified as gay, bisexual, or men who have sex with men, or reported same sex contact. Recent foreign travel, within 21 days prior to symptom onset, was reported by 75 cases, with 59 of these reporting travel within Europe.
We also share preliminary assessment of the genomic differences between the outbreak virus and previous monkeypox viruses. In any emerging infection outbreak we assess the virus or bacteria for any changes. We will be working to investigate the significance of the mutations identified so far to determine if they will have any impact on the virus’ behaviour
Dr Meera Chand, Director of Clinical and Emerging Infections, UKHSA said:
We are working, both in the UK and together with global partners, to progress the investigations that we need to help us better understand the virus, its transmission and the best use of mitigations such as vaccines and treatments. We use the new data rapidly to inform the public health response and we continue to work to reduce transmission. We are grateful to all those who have come forward for testing and the patients who continue to help us understand the outbreak through participating in studies and investigations.
UKHSA has identified a number of aspects of this outbreak which require further investigation. We will release the results of our ongoing investigations in subsequent technical briefings – these will be published regularly.
Friday 10 June 2022
The UK Health Security Agency ( UKHSA ) has detected 43 additional cases of monkeypox in England, one additional case in Scotland and one additional case in Wales.
This brings the total number confirmed in the UK to 366, as of 9 June.
There are currently 348 confirmed cases in England, 12 in Scotland, 2 in Northern Ireland and 4 in Wales.
Wednesday 8 June 2022
The UK Health Security Agency ( UKHSA ) has detected 18 additional cases of monkeypox in England, and one additional case in Scotland.
This brings the total number confirmed in the UK to 321, as of 7 June.
There are currently 305 confirmed cases in England, 11 in Scotland, 2 in Northern Ireland and 3 in Wales.
Anyone can get monkeypox, particularly if you have had close contact, including sexual contact, with an individual with symptoms. People who are gay or bisexual and men who have sex with men remain disproportionately affected.
Tuesday 7 June 2022
Monkeypox designated a notifiable disease.
Monkeypox is to be listed as a notifiable disease in law from 8 June 2022.
Legislation has been laid today (7 June 2022) which will make monkeypox a notifiable infectious disease under the Health Protection (Notification) Regulations 2010 from 8 June 2022.
This means all doctors in England are required to notify their local council or local Health Protection Team ( HPT ) if they suspect a patient has monkeypox. Laboratories must also notify the UK Health Security Agency ( UKHSA ) if the monkeypox virus is identified in a laboratory sample.
Wendi Shepherd, monkeypox incident director at UKHSA , said:
Rapid diagnosis and reporting is the key to interrupting transmission and containing any further spread of monkeypox. This new legislation will support us and our health partners to swiftly identify, treat and control the disease. It also supports us with the swift collection and analysis of data which enables us to detect possible outbreaks of the disease and trace close contacts rapidly, whilst offering vaccinations where appropriate to limit onward transmission.
Full guidance about reporting notifiable diseases and causative organisms can be found on GOV.UK.
It is important anyone concerned they may have symptoms of monkeypox feels able to access healthcare and clinical advice immediately.
To enable this, The National Health Service (Charges to Overseas Visitors) Regulations 2022 have been amended making the diagnosis and treatment of monkeypox, and suspected monkeypox, exempt from charges for all overseas visitors.
Monday 6 June 2022
The UK Health Security Agency ( UKHSA ) has detected 73 additional cases of monkeypox in England, 2 additional cases in Scotland and 2 in Wales.
This brings the total number confirmed in the UK to 302, as of 5 June.
There are currently 287 confirmed cases in England, 10 in Scotland, 2 in Northern Ireland and 3 in Wales.
Friday 3 June 2022
The UK Health Security Agency ( UKHSA ) has detected 15 additional cases of monkeypox in England and 3 in Scotland.
This brings the total number confirmed in England to 214, as of 2 June.
There are currently 8 confirmed cases in Scotland, 2 in Northern Ireland and 1 in Wales, taking the UK total to 225.
Anyone can get monkeypox. Currently most cases have been in men who are gay, bisexual or have sex with men, so it’s particularly important to be aware of the symptoms if you’re in these groups.
Thursday 2 June 2022
The UK Health Security Agency ( UKHSA ) has detected 11 additional cases of monkeypox in England.
This brings the total number confirmed in England to 199, as of 1 June.
There are currently 5 confirmed cases in Scotland, 2 in Northern Ireland and 1 in Wales, taking the UK total to 207.
Wednesday 1 June 2022
The UK Health Security Agency ( UKHSA ) has detected 5 additional cases of monkeypox in England and 1 in Scotland.
This brings the total number confirmed in England to 188, as of 31 May.
There are currently 5 confirmed cases in Scotland, 2 in Northern Ireland and 1 in Wales, taking the UK total to 196.
A further epidemiological update on the current outbreak using data up to 30 May has been published.
Tuesday 31 May 2022
Eleven new monkeypox cases identified in england.
The latest cases, as of 30 May, bring the total number confirmed in England since 7 May to 183.
There are currently 4 confirmed cases in Scotland, 2 in Northern Ireland and 1 in Wales, taking the UK total to 190.
The risk to the UK population remains low, but we are asking people to be alert to any new rashes or lesions, which would appear like spots, ulcers or blisters, on any part of their body.
Although this advice applies to everyone, the majority of the cases identified to date have been among men who are gay, bisexual and men who have sex with men, so we are asking these people in particular to be aware of the symptoms, particularly if they have recently had a new sexual partner.
You should call NHS 111 or a sexual health centre immediately if you have a rash with blisters. Do not go to a sexual health clinic without contacting them first. Stay at home and avoid close contact with other people until you’ve been told what to do.
Dr Ruth Milton, Senior Medical Advisor at UKHSA , said:
The risk to the general public from monkeypox is still low, but it’s important that we work to limit the virus being passed on. We remind people that they should be alert to new spots, ulcers or blisters on any part of their body. If anyone suspects they might have these, particularly if they have recently had a new sexual partner, they should limit their contact with others and contact NHS 111 or their local sexual health service as soon as possible, though please phone ahead before attending in person.
UKHSA health protection teams are contacting people considered to be high-risk contacts of confirmed cases and are advising those who have been risk assessed and remain well to isolate at home for up to 21 days.
Monday 30 May 2022
Seventy-one additional monkeypox cases identified in england.
The UK Health Security Agency ( UKHSA ) has detected 71 additional cases of monkeypox in England.
The latest cases, as of 29 May, bring the total number confirmed in England since 7 May to 172.
There are currently 4 confirmed cases in Scotland, 2 in Northern Ireland and 1 in Wales, taking the UK total to 179.
You should call NHS 111 or a sexual health centre immediately if you have a rash with blisters and either, you:
have been in close contact with someone who has or might have monkeypox (even if they have not been tested yet) in the past 3 weeks
have been to West or Central Africa in the past 3 weeks
are a man who has sex with men
Tell the person you speak to if you have had close contact with someone who has or might have monkeypox, or if you’ve recently travelled to central or west Africa.
Do not go to a sexual health clinic without contacting them first. Stay at home and avoid close contact with other people until you’ve been told what to do.
Additionally, today, UKHSA has published guidance principles agreed across all 4 UK nations on how to effectively limit transmission of monkeypox and limit onward transmission when cases are identified.
This includes advice and protocols for those testing positive for monkeypox, their close contacts and anyone involved in their treatment or care, including healthcare workers. The principles are already in use in response to the outbreak, and today’s publication confirms the UK’s aligned response.
Dr Ruth Milton, Senior Medical Advisor at UKHSA , said:
We are continuing to work closely with our colleagues in Scotland, Wales and Northern Ireland to ensure we are aligned in our approach to reducing the risk of transmission of monkeypox in the UK. We are reminding people to look out for new spots, ulcers or blisters on any part of their body. If anyone suspects they might have these, particularly if they have recently had a new sexual partner, they should limit their contact with others and contact NHS 111 or their local sexual health service as soon as possible, though please phone ahead before attending in person. This will help us to limit the virus being passed on.
UKHSA health protection teams are contacting people considered to be high-risk contacts of confirmed cases and are advising those who have been risk assessed and remain well to isolate at home for up to 21 days.
UKHSA has also purchased over 20,000 doses of a safe smallpox vaccine called Imvanex (supplied by Bavarian Nordic) and this is being offered to identified close contacts of those diagnosed with monkeypox to reduce the risk of symptomatic infection and severe illness.
Friday 27 May 2022
Sixteen additional monkeypox cases identified in england.
The UK Health Security Agency ( UKHSA ) has detected 16 additional cases of monkeypox in England.
The latest cases, as of 26 May, bring the total number confirmed in England since 7 May to 101.
There are currently 3 confirmed cases in Scotland, one in Wales and one in Northern Ireland, taking the UK total to 106.
You should contact a sexual health clinic immediately if you develop a rash or lesions – though please phone ahead before attending in person.
Dr Susan Hopkins, Chief Medical Adviser, UKHSA , said:
We are continuing to promptly identify further monkeypox cases in England through our extensive surveillance and contact tracing networks, our vigilant NHS services, and thanks to people coming forward with symptoms. We are asking people to look out for new spots, ulcers or blisters on any part of their body. If anyone suspects they might have these, particularly if they have recently had a new sexual partner, they should limit their contact with others and contact NHS 111 or their local sexual health service as soon as possible, though please phone ahead before attending in person.
Thursday 26 May 2022
Eight additional monkeypox cases identified in england.
The UK Health Security Agency ( UKHSA ) has detected 8 additional cases of monkeypox in England.
The latest cases, as of 25 May, bring the total number confirmed in England since 7 May to 85.
There are 3 confirmed cases in Scotland, one in Wales and one in Northern Ireland, taking the UK total to 90.
The risk to the UK population remains low, but we are asking people to be alert to any new rashes or lesions on any part of their body.
Although this advice applies to everyone, a notable proportion of the cases identified to date have been among men who are gay, bisexual and men who have sex with men ( MSM ), so we are asking these people in particular to be aware of the symptoms, particularly if they have recently had a new sexual partner.
You should contact a sexual health clinic immediately if you develop a rash or lesions – please phone ahead.
We are continuing to promptly identify further monkeypox cases in England through our extensive surveillance and contact tracing networks, our vigilant NHS services, and thanks to people coming forward with symptoms. If anyone suspects they might have rashes or lesions on any part of their body, particularly if they have recently had a new sexual partner, they should limit their contact with others and contact NHS 111 or their local sexual health service as soon as possible, though please phone ahead before attending in person.
Wednesday 25 May 2022
Seven additional monkeypox cases identified in england.
UKHSA has detected 7 additional cases of monkeypox in England
The latest cases bring the total number confirmed in England since 7 May to 77, as of 24 May.
Public Health Scotland confirmed on Monday it had identified one monkeypox case, taking the total cases identified in the UK to 78.
As of 24 May, no cases have been identified in Wales or Northern Ireland. Despite further cases being detected, the risk to the UK population remains low.
Anyone with unusual rashes or lesions on any part of their body should immediately contact NHS 111 or their local sexual health service – please phone ahead before attending in person.
A notable proportion of the cases identified to date have been among people who are gay, bisexual and MSM , so we are asking these groups in particular to be aware of the symptoms, particularly if they have recently had a new sexual partner.
We are continuing to promptly detect new monkeypox cases through our extensive surveillance network and NHS services. If anyone suspects they might have rashes or lesions on any part of their body, particularly if they have recently had a new sexual partner, they should limit their contact with others and contact NHS 111 or their local sexual health service as soon as possible – though please phone ahead before attending in person.
In addition, UKHSA has purchased supplies of a safe smallpox vaccine (Imvanex, supplied by Bavarian Nordic) and this is being offered to close contacts of those diagnosed with monkeypox to reduce the risk of symptomatic infection and severe illness.
Tuesday 24 May 2022
Fourteen more cases of monkeypox identified by ukhsa.
The UK Health Security Agency ( UKHSA ) has detected 14 additional cases of monkeypox in England.
The latest cases bring the total number of cases confirmed in England since 7 May to 70, as of 23 May.
Public Health Scotland confirmed on Monday it had identified one monkeypox case, taking the total cases identified in the UK to 71.
As of 23 May, no cases have so far been identified in Wales or Northern Ireland.
Despite further cases being detected, the risk to the UK population remains low.
Anyone with unusual rashes or lesions on any part of their body should immediately contact NHS 111 or their local sexual health service.
A notable proportion of the cases identified to date have been among people who are gay, bisexual and men who have sex with men, so we are asking these groups in particular to be aware of the symptoms.
We are continuing to promptly identify further monkeypox cases in England through our extensive surveillance and contact tracing networks, our vigilant NHS services and thanks to people coming forward with symptoms. If anyone suspects they might have rashes or lesions on any part of their body, particularly if they have recently had a new sexual partner, they should limit their contact with others and contact NHS 111 or their local sexual health service as soon as possible – though please phone ahead before attending in person.
UKHSA health protection teams are contacting people considered to be high-risk contacts of confirmed cases and are advising those who have been risk assessed and remain well to isolate at home for up to 21 days. In addition, UKHSA has purchased supplies of a safe smallpox vaccine (called Imvanex, supplied by Bavarian Nordic) and this is being offered to identified close contacts of someone diagnosed with monkeypox to reduce the risk of symptomatic infection and severe illness.
Monday 23 May 2022
Thirty-six more cases of monkeypox identified by ukhsa.
The UK Health Security Agency ( UKHSA ) has detected 36 additional cases of monkeypox in England.
The latest cases bring the total number of monkeypox cases confirmed in England since 7 May to 56.
The virus does not usually spread easily between people, but it can be passed on through close person-to-person contact or contact with items used by a person who has monkeypox, such as clothes, bedding or utensils. Monkeypox is usually a self-limiting illness and most people recover within a few weeks.
While the current outbreak is significant and concerning, the risk to the UK population remains low.
Anyone with unusual rashes or lesions on any part of their body, especially their genitalia, should immediately contact NHS 111 or their local sexual health service.
A notable proportion of cases detected have been in gay and bisexual men, so UKHSA continues to urge this community to be alert to monkeypox symptoms.
People should notify clinics ahead of their visit and can be assured their call or discussion will be treated sensitively and confidentially.
Alongside reports of further cases being identified in other countries globally, we continue to identify additional cases in the UK. Thank you to everyone who has come forward for testing already and supported our contact tracing efforts – you are helping us limit the spread of this infection in the UK. Because the virus spreads through close contact, we are urging everyone to be aware of any unusual rashes or lesions and to contact a sexual health service if they have any symptoms. A notable proportion of recent cases in the UK and Europe have been found in gay and bisexual men so we are particularly encouraging these men to be alert to the symptoms.
UKHSA health protection teams are contacting people considered to be high-risk contacts of confirmed cases and are advising those who have been risk assessed and remain well to isolate at home for up to 21 days. In addition, UKHSA has purchased supplies of a safe smallpox vaccine (called Imvanex) and this is being offered to identified close contacts of someone diagnosed with monkeypox to reduce the risk of symptomatic infection and severe illness.
We continue to engage with partners across the sector to ensure people are aware of the signs and symptoms and what action to take.
The vaccination of high-risk contacts of cases is underway. As of 10am on 23 May 2022, over 1,000 doses of Imvanex have been issued, or are in the process of being issued, to NHS Trusts. There remain over 3,500 doses of Imvanex in the UK.
Friday 20 May 2022
Eleven more cases of monkeypox identified by ukhsa.
The latest cases bring the total number of monkeypox cases confirmed in England since 6 May to 20.
The infection can be passed on through close contact or contact with clothing or linens used by a person who has monkeypox.
However, the virus does not usually spread easily between people and the risk to the UK population remains low.
Anyone with unusual rashes or lesions on any part of their body, especially their genitalia, should contact NHS 111 or call a sexual health service if they have concerns.
We continue to engage with partners across the sector at pace to deliver training webinars about monkeypox to clinicians to increase knowledge and awareness of this infection which is unusual in clinical settings in the UK. The first of these was hosted earlier this week by British Association for Sexual Health and HIV ( BASHH ) and was attended by over 900 people.
A notable proportion of early cases detected have been in gay and bisexual men and so UKHSA is urging this community in particular to be alert.
Monkeypox is usually a mild self-limiting illness, spread by very close contact with someone with monkeypox and most people recover within a few weeks.
Dr Susan Hopkins, Chief Medical Adviser, UKHSA , said:
We anticipated that further cases would be detected through our active case finding with NHS services and heightened vigilance among healthcare professionals. We expect this increase to continue in the coming days and for more cases to be identified in the wider community. Alongside this we are receiving reports of further cases being identified in other countries globally. We continue to rapidly investigate the source of these infections and raise awareness among healthcare professionals. We are contacting any identified close contacts of the cases to provide health information and advice. Because the virus spreads through close contact, we are urging everyone to be aware of any unusual rashes or lesions and to contact NHS 111 or a sexual health service if they have any concerns. Please contact clinics ahead of your visit and avoid close contact with others until you have been seen by a clinician. A notable proportion of recent cases in the UK and Europe have been found in gay and bisexual men so we are particularly encouraging them to be alert to the symptoms and seek help if concerned. Clinicians should be alert to any individual presenting with unusual rashes without a clear alternative diagnosis and should contact specialist services for advice.
Initial symptoms of monkeypox include fever, headache, muscle aches, backache, swollen lymph nodes, chills and exhaustion.
A rash can develop, often beginning on the face, then spreading to other parts of the body including the genitals.
The rash changes and goes through different stages – it can look like chickenpox or syphilis, before finally forming a scab which later falls off.
Wednesday 18 May 2022
Two more cases of monkeypox identified by ukhsa.
The UK Health Security Agency ( UKHSA ) has detected 2 additional cases of monkeypox, one in London and one in the South East of England.
The latest cases bring the total number of monkeypox cases confirmed in England since 6 May to 9, with recent cases predominantly in gay, bisexual or men who have sex with men ( MSM ).
The 2 latest cases have no travel links to a country where monkeypox is endemic, so it is possible they acquired the infection through community transmission.
The virus spreads through close contact and UKHSA is advising individuals, particularly those who are gay, bisexual or MSM , to be alert to any unusual rashes or lesions on any part of their body, especially their genitalia, and to contact a sexual health service if they have concerns.
Monkeypox has not previously been described as a sexually transmitted infection, though it can be passed on by direct contact during sex. It can also be passed on through other close contact with a person who has monkeypox or contact with clothing or linens used by a person who has monkeypox.
The 2 new cases do not have known connections with previous confirmed cases announced on 16, 14 and 7 May.
UKHSA is working closely with the NHS and other stakeholders to urgently investigate where and how recent confirmed monkeypox cases were acquired, including how they may be linked to each other.
The virus does not usually spread easily between people. The risk to the UK population remains low.
Anyone with concerns that they could be infected with monkeypox is advised to contact NHS 111 or a sexual health clinic. People should notify clinics ahead of their visit. We can assure them their call or discussion will be treated sensitively and confidentially.
Monkeypox is a viral infection usually associated with travel to West Africa. It is usually a mild self-limiting illness, spread by very close contact with someone with monkeypox and most people recover within a few weeks.
These latest cases, together with reports of cases in countries across Europe, confirms our initial concerns that there could be spread of monkeypox within our communities. UKHSA has quickly identified cases so far and we continue to rapidly investigate the source of these infections and raise awareness among healthcare professionals. We are particularly urging men who are gay and bisexual to be aware of any unusual rashes or lesions and to contact a sexual health service without delay if they have concerns. Please contact clinics ahead of your visit. We are contacting any identified close contacts of the cases to provide health information and advice.
Clinicians should be alert to individuals presenting with rashes without a clear alternative diagnosis and should contact specialist services for advice.
Initial symptoms of monkeypox include fever, headache, muscle aches, backache, swollen lymph nodes, chills and exhaustion. A rash can develop, often beginning on the face, then spreading to other parts of the body including the genitals.
The rash changes and goes through different stages, and can look like chickenpox or syphilis, before finally forming a scab, which later falls off.
16 May 2022
Four more cases of monkeypox indentified by ukhsa.
The UK Health Security Agency ( UKHSA ) has detected 4 additional cases of monkeypox, 3 in London and one linked case in the North East of England.
The 4 new cases do not have known connections with the previous confirmed cases announced on 14 May and the case announced on 7 May .
Investigations are underway to establish links between the latest 4 cases, who all appear to have been infected in London. All 4 of these cases self-identify as gay, bisexual or other men who have sex with men ( MSM ).
Currently, common contacts have been identified for 2 of the 4 latest cases.
There is no link to travel to a country where monkeypox is endemic, and exactly where and how they acquired their infections remains under urgent investigation, including whether they have further links to each other.
Those patients needing medical care are all in specialist infectious disease units at the Royal Free Hosptial, Royal Victoria Infirmary in Newcastle upon Tyne and Guys’ and St Thomas’. The individuals have the West African clade of the virus, which is mild compared to the Central African clade.
These latest cases mean that there are currently 7 confirmed monkeypox cases in the UK, diagnosed between 6 and 15 May.
Due to the recent increase in cases and uncertainties around where some of these individuals acquired their infection, we are working closely with NHS partners to identify if there may have been more cases in recent weeks, as well as international partners to understand if similar rises have been seen in other countries.
The virus does not spread easily between people and the risk to the UK population is low. However, the most recent cases are in gay, bisexual and other MSM communities, and as the virus spreads through close contact, we are advising these groups to be alert to any unusual rashes or lesions on any part of their body, especially their genitalia, and to contact a sexual health service if they have concerns.
Anyone with concerns that they could be infected with monkeypox is advised to make contact with clinics ahead of their visit. We can assure them their call or discussion will be treated sensitively and confidentially.
This is rare and unusual. UKHSA is rapidly investigating the source of these infections because the evidence suggests that there may be transmission of the monkeypox virus in the community, spread by close contact. We are particularly urging men who are gay and bisexual to be aware of any unusual rashes or lesions and to contact a sexual health service without delay. We are contacting any potential close contacts of the cases to provide health information and advice.
14 May 2022
Two additional cases of monkeypox identified in london.
Two individuals have been diagnosed with monkeypox in London, the UK Health Security Agency ( UKHSA ) has confirmed.
The cases live together in the same household. They are not linked to the previous confirmed case announced on 7 May . Where and how they acquired their infection remains under investigation.
Monkeypox is a rare viral infection that does not spread easily between people. It is usually a mild self-limiting illness and most people recover within a few weeks. However, severe illness can occur in some people.
The infection can be spread when someone is in close contact with an infected person, however, there is a very low risk of transmission to the general population.
One of the cases is receiving care at the expert infectious disease unit at St Mary’s Hospital, Imperial College Healthcare NHS Trust, London. The other case is isolating and does not currently require hospital treatment.
As a precautionary measure, UKHSA experts are working closely with the individuals and NHS colleagues and will be contacting people who might have been in close contact to provide information and health advice.
People without symptoms are not considered infectious but, as a precaution, those who have been in close proximity to the individuals are being contacted to ensure that, if they do become unwell, they can be treated quickly.
Dr Colin Brown, Director of Clinical and Emerging Infections, UKHSA , said:
We have confirmed 2 new monkeypox cases in England that are not linked to the case announced on May 7. While investigations remain ongoing to determine the source of infection, it is important to emphasise it does not spread easily between people and requires close personal contact with an infected symptomatic person. The overall risk to the general public remains very low. We are contacting any potential close contacts of the case. We are also working with the NHS to reach any healthcare contacts who have had close contact with the cases prior to confirmation of their infection, to assess them as necessary and provide advice. UKHSA and the NHS have well established and robust infection control procedures for dealing with cases of imported infectious disease and these will be strictly followed.
Professor Julian Redhead, medical director at Imperial College Healthcare NHS Trust, said:
We are caring for a patient in our specialist high consequence infectious diseases unit at St Mary’s Hospital. All of the necessary infectious control procedures have been followed and we are working closely with UKHSA and NHS England.
A rash can develop, often beginning on the face, then spreading to other parts of the body, particularly the hands and feet.
The rash changes and goes through different stages before finally forming a scab, which later falls off.
Monkeypox case confirmed in England
The UK Health Security Agency ( UKHSA ) can confirm an individual has been diagnosed with monkeypox in England.
The patient has a recent travel history from Nigeria, which is where they are believed to have contracted the infection, before travelling to the UK.
Monkeypox is a rare viral infection that does not spread easily between people. It is usually a mild self-limiting illness and most people recover within a few weeks. However, severe illness can occur in some individuals.
The infection can be spread when someone is in close contact with an infected person; however, there is a very low risk of transmission to the general population.
The patient is receiving care at the expert infectious disease unit at the Guy’s and St Thomas’ NHS Foundation Trust, London.
As a precautionary measure, UKHSA experts are working closely with NHS colleagues and will be contacting people who might have been in close contact with the individual to provide information and health advice.
This includes contacting a number of passengers who travelled in close proximity to the patient on the same flight to the UK. People without symptoms are not considered infectious but, as a precaution, those who have been in close proximity are being contacted to ensure that if they do become unwell they can be treated quickly. If passengers are not contacted then there is no action they should take.
It is important to emphasise that monkeypox does not spread easily between people and the overall risk to the general public is very low. We are working with NHS England and NHS Improvement (NHSEI) to contact the individuals who have had close contact with the case prior to confirmation of their infection, to assess them as necessary and provide advice. UKHSA and the NHS have well established and robust infection control procedures for dealing with cases of imported infectious disease and these will be strictly followed.
Dr Nicholas Price, Director NHSE High Consequence Infection Diseases (airborne) Network and Consultant in Infectious Diseases at Guy’s and St Thomas’, said:
The patient is being treated in our specialist isolation unit at St Thomas’ Hospital by expert clinical staff with strict infection prevention procedures. This is a good example of the way that the High Consequence Infectious Diseases national network and UKHSA work closely together in responding swiftly and effectively to these sporadic cases.
Initial symptoms include fever, headache, muscle aches, backache, swollen lymph nodes, chills and exhaustion. A rash can develop, often beginning on the face, then spreading to other parts of the body. The rash changes and goes through different stages before finally forming a scab, which later falls off.
Share this page
The following links open in a new tab
- Share on Facebook (opens in new tab)
- Share on Twitter (opens in new tab)
Updates to this page
Added latest update.
Added further information regarding semen testing and condom use.
Added latest udate.
First published.
Related content
Is this page useful.
- Yes this page is useful
- No this page is not useful
Help us improve GOV.UK
Don’t include personal or financial information like your National Insurance number or credit card details.
To help us improve GOV.UK, we’d like to know more about your visit today. Please fill in this survey (opens in a new tab) .

IMAGES
VIDEO
COMMENTS
Complications after a dental procedure that include swelling and pain, dry socket, osteomyelitis, bleeding, and osteonecrosis of the jaw comprise another set of urgent dental problems that require prompt attention.
Can Dental Issues Cause Swollen Lymph Nodes? Yes! There is evidence that suggests that there may be a link between swollen lymph nodes and dental issues such as gum disease or cavities. The bacteria from these conditions can enter the bloodstream and travel to other parts of the body, resulting in swelling of the lymph nodes around the infected ...
Lymphatic System comprises of Lymph nodes in the Facial region which are related to the Oral cavity and are enlarged due to infection of the particular region. Palpation of Lymph nodes helps in Provisional Diagnosis of oral conditions. The Lymph nodes should be checked for tenderness, mobility, enlargement and consistency while performing a ...
I had a routine dental cleaning on Friday of last week; a few hours after the appointment, I noticed a sharp pain associated with a little "lump" on the bottom of my lingual frenulum; basically some raised skin under the tongue, resting on the floor of my mouth. I also noticed some slight swelling in my right submandibular lymph node.
A lymph nodes dentist consult is a must if you have persistent swelling in your lymph nodes, and believe that dental issues are the cause. This is because infections from dental ailments can spread to other areas of the body, cause sepsis (a life-threatening infection), lead to complications such as bone loss and tooth loss, or may even create ...
Explore the connection between dental issues and swollen lymph nodes. Learn how oral health impacts your overall well-being, and discover tips for prevention and management.
Swollen glands are usually painless and may go unnoticed until they are examined by a medical professional. So, when your dental professional sweeps his or her hands down your neck during an oral cancer screening, they're checking for swollen lymph nodes in your neck.
Learn more about swollen lymph nodes, including possible causes and treatments your doctor may recommend.
Find out when to worry about swollen lymph nodes, when you should call a doctor, and the tests the care team may use to evaluate suspected cancer.
Pain after dental work is often an expected part of recovery. Pain relief methods can reduce discomfort. Some types of dental pain require a follow-up visit.
Increasingly swelling face, jaw or gums. Persistent fever. Bleeding for more than a day. Emitting pus or redness from the area. Swollen neck lymph nodes. Excessive pain when opening your mouth or jaw. Difficulty in breathing. How to Prevent Infections after Oral Surgery. Avoid Physical Activity.
So you've describe several symptoms of grinding. Why it could seem like a swollen lymph node is the constant muscle contractions in the head and neck from grinding all night which leads to muscular fatigue, headaches, and knots in the muscles. Pain usually radiates the sides and back of head and neck and worst at night or in the morning.
The lymph nodes that swell up are the ones located closest to the area of the infection or illness. For example, the most common cause of swollen lymph nodes in the neck is an upper respiratory infection. Lymph nodes can swell up with pretty much any kind of infection, including dental issues.
Discover how dental conditions can cause swollen lymph nodes. Learn about symptoms, treatments, and prevention to maintain overall health.
Treatment Swollen lymph nodes caused by a virus usually return to normal after the viral infection resolves. Antibiotics are not useful to treat viral infections. Treatment for swollen lymph nodes from other causes depends on the cause: Infection. The most common treatment for swollen lymph nodes caused by a bacterial infection is antibiotics. If your swollen lymph nodes are due to an HIV ...
Explore the intricate relationship between cavities and swollen lymph nodes. Learn about dental fillings, root canals, and when to consult a dental professional.
Swollen lymph nodes may appear when you go through dental issues. Learn more about why and what you can do to protect your health.
Discover symptoms and treatment options for tooth infections swollen lymph nodes. Learn how to manage this dental issue effectively.
The cervical lymph nodes show a frequent tendency for enlargement considering their drainage from the oral cavity which houses the teeth communicating with the external environment. Cervical lymphadenopathy is often reactive and usually due to bacterial, viral infections, dental infections and surgical procedures in the head and neck region.
Abstract Lymph node enlargement may be an incidental finding on examination, or may be associated with a patient complaint. It is likely that over half of all patients examined each day may have enlarged lymph nodes in the head and neck region. There are no written guidelines specifying when further evaluation of lymphadenopathy is necessary. With such a high frequency of occurrence, oral ...
If you have these symptoms and swollen lymph nodes that don't improve after a few days, speak to your doctor. They will check that the infection is not something more severe like an abscess.
Initial symptoms include fever, headache, muscle aches, backache, swollen lymph nodes, chills and exhaustion. A rash can develop, often beginning on the face, then spreading to other parts of the ...