
Travel Vaccines and Advice for Sierra Leone

Despite its beauty, Sierra Leone has remained mostly uninfluenced by tourist activities. Much of the country is still undiscovered.
The country’s coastline, is only one of its many attractive landscapes. The Loma Mountains in the north have dense rain forests and volcanoes nestled in rolling hills.
In Freetown vibrant houses perched on stilts remain from when freed slaves relocated to the country’s Western shores.
On This Page: Do I Need Vaccines for Sierra Leone? Other Ways to Stay Healthy in Sierra Leone Do I Need a Visa or Passport for Sierra Leone? What Is the Climate Like in Sierra Leone? How Safe Is Sierra Leone? Is the Food Safe in Sierra Leone? Going to Banana Island What Should I Take to Sierra Leone? U.S. Embassy in Sierra Leone
Do I Need Vaccines for Sierra Leone?
Yes, some vaccines are recommended or required for Sierra Leone. The CDC and WHO recommend the following vaccinations for Sierra Leone: typhoid , hepatitis A , polio , yellow fever , chikungunya , rabies , hepatitis B , influenza , COVID-19 , pneumonia , meningitis , chickenpox , shingles , Tdap (tetanus, diphtheria and pertussis) and measles, mumps and rubella (MMR) .
See the bullets below to learn more about some of these key immunizations:
- Typhoid – Food & Water – Shot lasts 2 years. Oral vaccine lasts 5 years, must be able to swallow pills. Oral doses must be kept in refrigerator.
- Hepatitis A – Food & Water – Recommended for most travelers.
- Polio – Food & Water – While there is no active polio transmission in Sierra Leone, it is vulnerable for outbreaks. Considered a routine vaccination for most travel itineraries. Single adult booster recommended.
- Yellow Fever – Mosquito – Required for arriving travelers from ALL countries. Recommended for all travelers over 9 months of age.
- Chikungunya – Mosquito – Few cases reported since 2016. Increased risk for those who may be in more rural areas.
- Rabies – Saliva of Infected Animals – High risk country. Vaccine recommended for long-term travelers and those who may come in contact with animals.
- Hepatitis B – Blood & Body Fluids – Recommended for travelers to most regions.
- Influenza – Airborne – Vaccine components change annually.
- COVID-19 – Airborne – Recommended for travel to all regions, both foreign and domestic.
- Pneumonia – Airborne – Two vaccines given separately. All 65+ or immunocompromised should receive both.
- Meningitis – Direct Contact & Airborne – Given to anyone unvaccinated or at an increased risk, especially students.
- Chickenpox – Direct Contact & Airborne – Given to those unvaccinated that did not have chickenpox.
- Shingles – Direct Contact – Vaccine can still be given if you have had shingles.
- Polio – Food & Water – Considered a routine vaccination for most travel itineraries. Single adult booster recommended.
- TDAP (Tetanus, Diphtheria & Pertussis) – Wounds & Airborne – Only one adult booster of pertussis required.
- Measles Mumps Rubella (MMR) – Various Vectors – Given to anyone unvaccinated and/or born after 1957. One time adult booster recommended.
See the table below for more information:
Specific Vaccine Information
- Typhoid – Typhoid, caused by Salmonella Typhi, spreads via contaminated food and water, especially in areas with poor sanitation. Protect yourself by practicing good hygiene and safe food habits. Vaccination can significantly reduce the risk of typhoid infection, especially when traveling to endemic areas.
- Hepatitis A – Hepatitis A is a highly contagious liver infection caused by the hepatitis A virus, typically spreading through contaminated food or water, or close contact with an infected person. Symptoms can include fatigue, nausea, stomach pain, and jaundice. The hepatitis A vaccine is a safe and effective shot that provides immunity against the virus, usually given in two doses.
- Yellow Fever – Yellow fever is a serious, potentially fatal viral disease transmitted by mosquitoes, characterized by fever, jaundice, and bleeding. The yellow fever vaccine, given as a single injection, offers effective, long-lasting immunity against the virus and is crucial for travelers to and residents of endemic areas in Africa and South America.
- Chikungunya – Chikungunya, spread by infected mosquitoes, can be prevented through mosquito bite prevention and vaccination. The chikungunya vaccine is considered the best form of protection.
- Rabies – The rabies virus is a deadly threat that spreads through bites and scratches from infected animals. Preventing rabies involves timely vaccination, avoiding contact with wildlife and seeking immediate medical attention if bitten. The rabies vaccine is instrumental in developing immunity and safeguarding against this fatal disease.
- Hepatitis B – Hepatitis B, a liver infection spread through bodily fluids, poses a significant health risk. Safe practices help, but vaccination is the ultimate safeguard. It prompts the immune system to produce antibodies, ensuring strong and persistent protection.
- Measles, Mumps, Rubella (MMR) – Measles, mumps, and rubella are contagious viral infections, causing various symptoms and complications. To prevent them, vaccination is key. The MMR vaccine, given in two doses, safeguards against all three diseases and helps establish herd immunity, reducing the risk of outbreaks.
Yellow Fever in Sierra Leone
Yellow fever vaccination is required for entry to Sierra Leone. All travelers over the age of nine months must show proof of vaccination upon arriving in the country. Vaccination is also recommended by the CDC and WHO to keep travelers protected against the virus.
Malaria in Sierra Leone
Malaria is widespread in Sierra Leone. Antimalarials are recommended for all travelers to the country. Atovaquone, doxycycline, mefloquine and tafenoquine are often given to travelers to Sierra Leone. Malaria parasite are resistant to chloroquine in the region. Be sure to consult with a travel health specialist on which antimalarials are best for your itinerary and health situation.
Proof of yellow fever vaccination is required for entry to Sierra Leone.
The CDC also says that the Zika virus is a risk in Sierra Leone. This virus can cause serious birth defects. It is recommended that pregnant women, or women planning to become pregnant, should not travel to Sierra Leone.
Typhoid vaccination is highly recommended for travelers to Sierra Leone. Individuals who visit friends or relatives or go to rural areas are at greater risk and should be immunized.
Ebola struck Sierra Leone in July of 2014. The outbreak claimed more than 700 lives.
In March 2016, the World Health Organization declared Sierra Leone Ebola-free.
To find out more about these vaccines, see our vaccinations page. Ready to travel safely? Book your appointment either call or start booking online now.
Other Ways to Stay Healthy in Sierra Leone
Prevent bug bites in sierra leone.
To ward off bug bites, follow CDC advice: wear long clothing, use screens, and remove standing water. Opt for EPA-registered repellents with DEET, picaridin, or OLE for protection. If bitten, wash the area, avoid scratching, and apply remedies. Seek medical help for severe reactions.
Food and Water Safety in Sierra Leone
Abroad, practice food safety by avoiding street vendors, washing hands thoroughly, and choosing well-cooked meals. Opt for bottled or canned drinks with unbroken seals. Prevent travelers’ diarrhea by practicing hand hygiene, skipping raw foods, and dining at reputable establishments.
Infections To Be Aware of in Sierra Leone
- African Tick-Bite Fever – ATBF, transmitted by ticks in sub-Saharan Africa, can be prevented by wearing protective clothing, using insect repellent, and checking for ticks. For additional protection, inquire about available options from healthcare experts before traveling to affected areas.
- Dengue – Dengue fever is a mosquito-borne illness with symptoms ranging from mild to severe, including high fever and pain. The CDC emphasizes prevention through avoiding mosquito bites by using repellents and removing standing water. Treatment focuses on symptom relief and hydration, avoiding certain pain relievers that can worsen bleeding risks.
- Ebola – Ebola, a deadly virus, can be prevented through rigorous hand hygiene and avoiding infected individuals, both are crucial in halting its transmission.
- Lassa Fever – Lassa fever, caused by the Lassa virus, spreads via rodents and human-to-human transmission. Although no vaccine is licensed yet, prevention entails strict hygiene, rodent control, and healthcare safety measures.
- Marburg Hemorrhagic Fever – Marburg Hemorrhagic Fever (MHF) spreads through contact with infected animals and individuals, necessitating stringent protective measures. Safe burial practices, healthcare infection control, and community education are pivotal in reducing MHF transmission risks.
- Schistosomiasis – Schistosomiasis is a parasitic infection transmitted through contaminated water. Avoiding contact with infected water sources and using protective clothing can reduce the risk of infection. Seeking medical evaluation promptly if symptoms such as fever and fatigue manifest enables timely diagnosis and treatment, preventing complications and promoting recovery.
- Zika – Zika, a mosquito-borne virus, spreads through mosquito bites, sexual contact, and from mother to child during pregnancy. Preventive measures include using repellent, practicing safe sex, and removing mosquito breeding sites.
Do I Need a Visa or Passport for Sierra Leone?
All U.S. citizens must have a visa before visiting Sierra Leone. If you do not have a visa, you will be denied entry.
Sources: Embassy of Sierra Leone and U.S. State Department
Your passport must be valid for at least 6 months following your expected date of arrival. Proof of yellow fever immunization is also required for entry.
What Is the Climate Like in Sierra Leone?
Sierra Leone is, for the most part, humid year-round. The country’s hottest season is from November through around April. During this time, travelers can expect a slight drop in humidity, but a spike in temperatures. Near the coast, breezes from the Atlantic offer a slight drop in temperature. March is considered the peak of the dry, hot season.
From December to January, dry dust storms from the Sahara blow through most of the country.
November and May are considered “wet months.” Travelers should expect a moderate amount of rainfall during this time.
- Freetown – In this coastal town, the temperatures tend to be relatively cooler than other major cities in Sierra Leone. Freetown experiences frequent rainfall.
- Kenema – Located in the South Sierra Leone, the climate is tropical and rainfall is present for most of the year. The dry season here has little impact on the climate.
- Makeni – Located in the center of Sierra Leone, this city experiences weather like Kenema to the South and Freetown to the West. But, this area experiences less rainfall.
How Safe Is Sierra Leone?
Sierra Leone is widely regarded as one of the poorest countries in the world. With this poverty comes an increase in crime rates.
Freetown is seen as the safest destination in the country. But, even in Freetown, night time wandering is not recommended. If you decide to travel from Freetown, the trip should be made in the daylight as run-ins with bandits are not uncommon.
If you are headed to border areas pay attention to your surroundings and never travel alone if you can help it. For instance, the border to Liberia is considered unstable.
Is the Food Safe in Sierra Leone?
Most dishes in Sierra Leone are spicy, plant-based and served with rice. Vegetable, meat and nut stews are common. Local dishes include: okra stew, cassava bread, coconut cake and pepper soup.
More impoverished areas in the country will have poor hygiene practices. It is best to stick to restaurants that are recommended for serving quality food on a consistent basis.
Although street food may smell tempting, cooking food outdoors increases the likelihood of your meal becoming contaminated.
All travelers to Sierra Leone should bring a travelers’ diarrhea kit , typhoid and hepatitis A vaccinations.
Going to Banana Island
Avoid an embarrassing stop, over 70% of travelers will have diarrhea., get protected with passport health’s travelers’ diarrhea kit .
Banana Island is a beautiful place in Sierra Leone that tourists like to visit because of its clear waters and white sandy beaches. People can do fun activities there, like swimming, snorkeling, and diving to see different types of colorful fish and sea animals. They can also go fishing with local fishermen, who use traditional methods to catch fish.
Banana Island is also a good place to relax and unwind because it is a quiet and peaceful island. Visitors can take a guided tour to learn about the island’s history and culture, or walk around and explore. There are also small guesthouses and lodges on the island where people can stay and experience island life.
Banana Island is a great place to visit if you like being near the ocean, want to try new things or want to relax in a beautiful setting.
What Should I Take to Sierra Leone?
Consider packing the following items, regardless what time of year you plan on traveling to Sierra Leone:
- Either a rain poncho or a light rain jacket – Prepare for any expected or unexpected rainfall.
- Bug spray or insect repellent – The high level of humidity across the country attracts mosquitoes, among other insects.
- Long sleeved shirts and pants – Coverage of the arms and legs further reduces your chances of being bitten by mosquitoes.
- Light and airy, yet relatively conservative clothing – The temperatures are manageable, but humidity can make it feel much warmer than it is.
U.S. Embassy in Sierra Leone
The U.S. Embassy urges travelers to register with the State Department before traveling to Sierra Leone.
Travelers also must make an appointment at the embassy for all non-emergency services including: routine passport application and renewals and notary signings.
U.S. Embassy Freetown Southridge, Hill Station Freetown, Sierra Leone Tel: (232) 99-105-000 Emergency after hours: (232) 99-905-029 Email: [email protected]
Ready to start your next journey? Call us at or book online now !
Customer Reviews
Passport health – travel vaccines for sierra leone.

- Records Requests
- Passport Health App
- Privacy Center
- Online Store
Security Alert May 17, 2024
Worldwide caution, update may 10, 2024, information for u.s. citizens in the middle east.
- Travel Advisories |
- Contact Us |
- MyTravelGov |
Find U.S. Embassies & Consulates
Travel.state.gov, congressional liaison, special issuance agency, u.s. passports, international travel, intercountry adoption, international parental child abduction, records and authentications, popular links, travel advisories, mytravelgov, stay connected, legal resources, legal information, info for u.s. law enforcement, replace or certify documents.
Before You Go
Learn About Your Destination
While Abroad
Emergencies
Share this page:
Sierra Leone
Travel Advisory July 31, 2023
Sierra leone - level 2: exercise increased caution.
Reissued with obsolete COVID-19 page links removed.
Exercise increased caution in Sierra Leone due to crime and civil unrest .
Country Summary: Violent crimes, such as robbery and assault, occur frequently in Sierra Leone, especially in Freetown. Local police often lack the resources to deal effectively with serious criminal incidents.
Demonstrations and protests occur in Sierra Leone and on occasion have resulted in violence.
If traveling outside the Freetown peninsula, make all efforts to complete your travel during daylight hours due to increased safety hazards at night. The U.S. Embassy is unable to provide emergency services to U.S. citizens outside of Freetown at night as U.S. government employees are prohibited from traveling outside the capital after dark.
Read the country information page for additional information about travel to Sierra Leone.
If you decide to travel to Sierra Leone:
- Do not physically resist any robbery attempt.
- Do not display signs of wealth, such as expensive watches or jewelry.
- Use caution when walking or driving at night.
- Always carry a copy of your U.S. passport and visa (if applicable). Keep original documents in a secure location.
- Enroll in the Smart Traveler Enrollment Program ( STEP ) to receive Alerts and make it easier to locate you in an emergency.
- Follow the Department of State on Facebook and Twitter .
- Review the Country Security Report for Sierra Leone.
- Prepare a contingency plan for emergency situations. Review the Traveler’s Checklist .
- Visit the CDC page for the latest Travel Health Information related to your travel.
Embassy Messages
View Alerts and Messages Archive
Quick Facts
1 page per stamp.
Yellow Fever.
Embassies and Consulates
U.S. Embassy Freetown Southridge, Hill Station Freetown, Sierra Leone Telephone: (+232) 99-105-000 Emergency after-hours telephone: (+232) 99-905-029 Email: [email protected]
Destination Description
Learn about the U.S. relationship to countries around the world.
Entry, Exit and Visa Requirements
A valid passport and visa are required for travel to Sierra Leone. Visitors to Sierra Leone are required to show their International Certificates of Vaccination (yellow card) upon arrival at the airport with a record of vaccination against yellow fever.
Visit the Embassy of the Republic of Sierra Leone’s website for the most current visa information.
The U.S. Department of State is unaware of any HIV/AIDS entry restrictions for visitors to or foreign residents of Sierra Leone.
Find information on dual nationality , prevention of international child abduction and customs regulations on our websites.
Safety and Security
Areas outside Freetown lack basic services. Travel outside the capital after dark is not allowed for U.S. Embassy officials and should be avoided by all travelers. Emergency response to vehicular and other accidents ranges from slow to nonexistent.
Crime: Crime is widespread in Sierra Leone. U.S. citizens have experienced armed mugging, assault, and burglary. Petty crime and pick pocketing of wallets, cell phones, and passports are very common, especially on the ferry to and from Lungi International Airport, as well as in bars, restaurants, and nightclubs in the Lumley Beach and Aberdeen areas of Freetown.
Demonstrations occur frequently. They may take place in response to political or economic issues, on politically significant holidays, and during international events.
- Even demonstrations intended to be peaceful can turn confrontational and possibly become violent.
- Avoid areas around protests and demonstrations.
- Check local media for updates and traffic advisories.
International Financial Scams: See the Department of State and the FBI pages for information on scams.
Internet romance and financial scams are prevalent in Sierra Leone. Scams are often initiated through Internet postings or profiles, or by unsolicited emails and letters. Scammers almost always pose as U.S. citizens who have no one else to turn to for help. Common scams include:
- Romance/Online dating
- Money transfers
- Lucrative sales
- Gold purchase
- Contracts with promises of large commissions
- Grandparent/Relative targeting
- Free Trip/Luggage
- Inheritance notices
- Work permits/job offers
- Bank overpayments
Victims of Crime: U.S. citizen victims of sexual assault should first contact the U.S. Embassy at (232) (99) 105 500. Report crimes to the local police at (232) (76) 692 830.
Remember that local authorities are responsible for investigating and prosecuting the crime.
See our webpage on help for U.S. victims of crime overseas.
- help you find appropriate medical care
- assist you in reporting a crime to the police
- contact relatives or friends with your written consent
- explain the local criminal justice process in general terms
- provide a list of local attorneys
- provide our information on victim’s compensation programs in the U.S.
- provide an emergency loan for repatriation to the United States and/or limited medical support in cases of destitution
- help you find accommodation and arrange flights home
- replace a stolen or lost passport
Domestic Violence: U.S. citizen victims of domestic violence are encouraged to contact the Embassy for assistance.
Tourism: The tourism industry is unevenly regulated, and safety inspections for equipment and facilities do not commonly occur. Hazardous areas and activities are not always identified with appropriate signage, and staff may not be trained or certified either by the host government or by recognized authorities in the field. In the event of an injury, medical treatment is typically available only in or near major cities and there are few medical specialists in country able to treat complicated medical conditions. First responders are generally unable to access areas outside of major cities and are not trained to provide urgent medical treatment. U.S. citizens are encouraged to purchase medical evacuation insurance .
Local Laws & Special Circumstances
Criminal Penalties: You are subject to local laws. If you violate local laws, even unknowingly, you may be expelled, arrested, or imprisoned.
Furthermore, some laws are also prosecutable in the United States, regardless of local law. For examples, see our website on crimes against minors abroad and the Department of Justice website .
Arrest Notification: If you are arrested or detained, ask police or prison officials to notify the U.S. Embassy immediately. See our webpage for further information.
Exports: Sierra Leone's customs authorities enforce strict regulations concerning the export of gems and precious minerals, such as diamonds and gold. All mineral resources, including gold and diamonds, belong to the State, and only the Government of Sierra Leone can issue mining and export licenses. The National Minerals Agency (NMA) can provide licenses for export, while the agency’s Directorate of Precious Minerals Trading is responsible for Kimberly Process certification of diamonds. For further information on mining activities in Sierra Leone, contact the Ministry of Mines and Mineral Resources , or see the Department of State’s annual Investment Climate Statement .
The Embassy has received reports in recent years of U.S. citizens investing in Sierra Leone who have been victims of fraud, often in the mining industry. Examples of fraud include advance-fee schemes where individuals have approached U.S. citizens urging them to purchase diamonds directly from Sierra Leone. The U.S. Embassy cannot interfere or intervene in any legal disputes, including those related to precious minerals. Please be aware that the U.S. Embassy cannot conduct checks on potential local partners.
Photography: Travelers must obtain official permission to photograph government buildings, airports, bridges, or official facilities including the Special Court for Sierra Leone and the U.S. Embassy.
Dual Nationals: U.S. citizens who are also Sierra Leonean nationals must provide proof of payment of taxes on revenue earned in Sierra Leone before being granted clearance to depart the country.
Faith-Based Travelers: See our following webpages for details:
- Faith-Based Travel Information
- International Religious Freedom Report – see country reports
- Human Rights Repor t – see country reports
- Hajj Fact Sheet for Travelers
- Best Practices for Volunteering Abroad
LGBTI Travelers: Consensual sexual relations between men are criminalized in Sierra Leone. Although the U.S. Embassy is not aware of any recent prosecutions for consensual sexual activity between men, such activity is illegal and penalties can include imprisonment. While there is no explicit legal prohibition against sexual relations between women, lesbians of all ages can be victims of “planned rapes” initiated by family members in an effort to change their sexual orientation.
See our LGBTI Travel Information page and section 6 of our Human Rights report for further details.
Travelers with Disabilities: The law in Sierra Leone does not prohibit discrimination against persons with disabilities and offers no specific protections for such persons. Social acceptance of persons with disabilities in public is as prevalent as in the United States. Expect accessibility to be limited in public transportation, lodging, communication/information, and general infrastructure throughout the country. Rental, repair, replacement parts for aids/equipment/devices, and service providers, such as sign language interpreters, are not available.
Students: See our Students Abroad page and FBI travel tips.
Women Travelers: Rape, including spousal rape, is illegal in Sierra Leone and punishable by up to 15 years in prison. However, rape is common and indictments are rare. Domestic violence is illegal and punishable by a fine of up to five (5) million leones ($943) and up to two years in prison. However, domestic violence is common and police are unlikely to intervene.
Female genital mutilation/cutting (FGM/C) is widespread in Sierra Leone. The government imposed a moratorium on practicing FGM/C as an emergency health response to the Ebola outbreak, and the moratorium remains in place, but the prohibition is not actively enforced.
See our travel tips for Women Travelers.
Please visit the Embassy’s COVID-19 page for more information about COVID-19 in Sierra Leone.
Medical facilities and services in Sierra Leone are severely limited. The standard of care, including basic medical services such as imaging or blood tests, is much lower than that of the United States.
For emergency services in Sierra Leone, dial 117.
Ambulance services are:
- not widely available and training and availability of emergency responders may be below U.S. standards.
- not present throughout the country or are unreliable in most areas.
- not equipped with state-of-the-art medical equipment.
- not staffed with trained paramedics and often have little or no medical equipment.
Injured or seriously ill travelers may prefer to take a taxi or private vehicle to the nearest major hospital rather than wait for an ambulance.
We do not pay medical bills. Be aware that U.S. Medicare/Medicaid does not apply overseas. Most hospitals and doctors overseas do not accept U.S. health insurance.
Medical Insurance: Make sure your health insurance plan provides coverage overseas. Most care providers overseas only accept cash payments. See our webpage for more information on insurance providers for overseas coverage. Visit the U.S. Centers for Disease Control and Prevention for more information on type of insurance you should consider before you travel overseas.
We strongly recommend supplemental insurance to cover medical evacuation.
Always carry your prescription medication in original packaging, along with your doctor’s prescription. Check with the Sierra Leone’s Federal Office of Public Health to ensure the medication is legal in Sierra Leone.
Vaccinations: Be up-to-date on all vaccinations recommended by the U.S. Centers for Disease Control and Prevention.
Further health information:
- World Health Organization
- U.S. Centers for Disease Control and Prevention (CDC)
Air Quality: Visit AirNow Department of State for information on air quality at U.S. Embassies and Consulates.
The U.S. Embassy maintains a list of doctors and hospitals . We do not endorse or recommend any specific medical provider or clinic.
Water Quality:
- In many areas, tap water is not potable. Bottled water and beverages are generally safe, although you should be aware that many restaurants and hotels serve tap water unless bottled water is specifically requested. Be aware that ice for drinks may be made using tap water.
- Many cities in Sierra Leone, such as Kabala, are at high altitude. Be aware of the symptoms of altitude sickness and take precautions before you travel. Visit the U.S. Centers for Disease Control and Prevention website for more information about Travel to High Altitudes.
Adventure Travel:
- Visit the U.S. Centers for Disease Control and Prevention website for more information about Adventure Travel.
General Health:
The following diseases are prevalent:
- Yellow Fever
- Travelers’ Diarrhea
Use the U.S. Centers for Disease Control and Prevention recommended mosquito repellents and sleep under insecticide-impregnated mosquito nets. Chemoprophylaxis is recommended for all travelers even for short stays.
Visit the Centers for Disease Control and Prevention website for more information regarding specific issues in Sierra Leone.
Air Quality:
- Air pollution is a significant problem in several major cities in Sierra Leone. Consider the impact seasonal smog and heavy particulate pollution may have on you and consult your doctor before traveling if necessary.
- Infants, children, and teens
- People over 65 years of age
- People with lung disease such as asthma and chronic obstructive pulmonary disease (COPD), which includes chronic bronchitis and emphysema;
- People with heart disease or diabetes
Travel and Transportation
Road Conditions and Safety: Most main roads in Freetown are navigable, but narrow and often have potholes. There is limited roadside assistance in-country and it is often difficult to find adequate fuel for longer journeys. Serious accidents are common, especially outside of Freetown, where the relative lack of traffic allows for greater speeds. Nighttime travel should be avoided.
Traffic Laws: International road signs and protocols are not routinely observed in Sierra Leone. In the event of a traffic accident, you should follow all police instructions. Large mobs often form at the scene of an accident and threaten the safety of the driver. You should go to the nearest police station for safety, even in the smallest of accidents.
Public Transportation: Public transport (bus or group taxi) is erratic, unsafe, and not recommended. U.S. Embassy officials are prohibited from using public transportation or taxis.
Motorcycle taxis are ubiquitous in Freetown and are often the cause of serious accidents. The U.S. Embassy strongly advises against utilizing these motorcycles. Pick pocketing is common in public taxis and mini-buses.
See our Road Safety page for more information.
Visit the website of Sierra Leone’s national tourist office and national authority responsible for road safety.
Aviation Safety Oversight: As there is no direct commercial air service to the United States by carriers registered in Sierra Leone, the U.S. Federal Aviation Administration (FAA) has not assessed the government of Sierra Leone’s Civil Aviation Authority for compliance with International Civil Aviation Organization (ICAO) aviation safety standards. Further information may be found on the FAA’s safety assessment page.
Maritime Travel: Mariners planning travel to Sierra Leone should also check for U.S. maritime advisories and alerts. Information may also be posted to the U.S. Coast Guard homeport website , and the NGA broadcast warnings.
For additional travel information
- Enroll in the Smart Traveler Enrollment Program (STEP) to receive security messages and make it easier to locate you in an emergency.
- Call us in Washington, D.C. at 1-888-407-4747 (toll-free in the United States and Canada) or 1-202-501-4444 (from all other countries) from 8:00 a.m. to 8:00 p.m., Eastern Standard Time, Monday through Friday (except U.S. federal holidays).
- See the State Department’s travel website for the Worldwide Caution and Travel Advisories .
- Follow us on Twitter and Facebook .
- See traveling safely abroad for useful travel tips.
For additional IPCA-related information, please see the International Child Abduction Prevention and Return Act (ICAPRA) report.
Travel Advisory Levels
Assistance for u.s. citizens, sierra leone map, learn about your destination, enroll in step.

Subscribe to get up-to-date safety and security information and help us reach you in an emergency abroad.
Recommended Web Browsers: Microsoft Edge or Google Chrome.
Check passport expiration dates carefully for all travelers! Children’s passports are issued for 5 years, adult passports for 10 years.
Afghanistan
Antigua and Barbuda
Bonaire, Sint Eustatius, and Saba
Bosnia and Herzegovina
British Virgin Islands
Burkina Faso
Burma (Myanmar)
Cayman Islands
Central African Republic
Cote d Ivoire
Curaçao
Czech Republic
Democratic Republic of the Congo
Dominican Republic
El Salvador
Equatorial Guinea
Eswatini (Swaziland)
Falkland Islands
France (includes Monaco)
French Guiana
French Polynesia
French West Indies
Guadeloupe, Martinique, Saint Martin, and Saint Barthélemy (French West Indies)
Guinea-Bissau
Isle of Man
Israel, The West Bank and Gaza
Liechtenstein
Marshall Islands
Netherlands
New Caledonia
New Zealand
North Korea (Democratic People's Republic of Korea)
Papua New Guinea
Philippines
Republic of North Macedonia
Republic of the Congo
Saint Kitts and Nevis
Saint Lucia
Saint Vincent and the Grenadines
Sao Tome and Principe
Saudi Arabia
Sint Maarten
Solomon Islands
South Africa
South Korea
South Sudan
Switzerland
The Bahamas
Timor-Leste
Trinidad and Tobago
Turkmenistan
Turks and Caicos Islands
United Arab Emirates
United Kingdom
Vatican City (Holy See)
External Link
You are about to leave travel.state.gov for an external website that is not maintained by the U.S. Department of State.
Links to external websites are provided as a convenience and should not be construed as an endorsement by the U.S. Department of State of the views or products contained therein. If you wish to remain on travel.state.gov, click the "cancel" message.
You are about to visit:
- Company History
- Mission Statement
- Philippines
- South Africa
- Afghanistan
- American Samoa
- Antigua and Barbuda
- British Virgin Islands
- Burkina Faso
- Canary Islands
- Cayman Islands
- Central African Republic
- Christmas Island
- Cocos (Keeling) Islands
- Cook Islands
- Cote d'Ivoire
- Democratic Republic of the Congo
- Dominican Republic
- Easter Island
- El Salvador
- Equatorial Guinea
- Falkland Islands
- Faroe Islands
- French Guiana
- French Polynesia
- Guinea-Bissau
- Liechtenstein
- Madeira Islands
- Marshall Islands
- Netherlands
- New Caledonia
- New Zealand
- Norfolk Island
- North Korea
- North Macedonia
- Northern Mariana Islands
- Palestinian Territories
- Papua New Guinea
- Pitcairn Islands
- Puerto Rico
- Republic of the Congo
- Saint Barthelemy
- Saint Helena
- Saint Kitts and Nevis
- Saint Lucia
- Saint Martin
- Saint Pierre-et-Miquelon
- Saint Vincent and the Grenadines
- Sao Tome and Principe
- Saudi Arabia
- Sierra Leone
- Sint Eustatius
- Solomon Islands
- South Georgia and the South Sandwich Islands
- South Korea
- South Sudan
- Switzerland
- Trinidad and Tobago
- Turkmenistan
- Turks and Caicos Islands
- U.S. Virgin Islands
- United Arab Emirates
- United Kingdom
- United States
- Wake Island
- Western Sahara
- Travel Vaccines
- Travel Health Consultations
- Travellers’ Diarrhea Kits
- Dengue Fever Prevention
- Malaria Prevention
- Chikungunya Prevention
- Zika Prevention
- Ebola Virus
- Yellow Fever
- Hepatitis A
- Japanese Encephalitis
- Hepatitis B
- Tickborne Encephalitis (TBE)
- Tetanus-Diphtheria-Pertussis
- Measles-Mumps-Rubella
- Influenza (Flu)
- Blood Tests
- Vitamin Injections
- Physician Referral Program
- London Bridge Clinic
- London – Euston Travel Clinic

Travel Vaccines and Advice for Sierra Leone

Despite its beauty, Sierra Leone has remained mostly uninfluenced by tourist activities. Much of the country is still undiscovered.
The country’s coastline, is only one of its many attractive landscapes. The Loma Mountains in the north have dense rainforests and volcanoes nestled in rolling downs.
In Freetown vibrant houses perched on stilts remain from when freed slaves relocated to the country’s Western shores.
Do I Need Vaccines for Sierra Leone?
Yes, some vaccines are recommended or required for Sierra Leone. The National Travel Health Network and Centre and WHO recommend the following vaccinations for Sierra Leone: COVID-19 , hepatitis A , hepatitis B , typhoid , cholera , yellow fever , rabies , polio and tetanus .
See the bullets below to learn more about some of these key immunisations:
- COVID-19 – Airborne – Recommended for all travellers
- Hepatitis A – Food & Water – Recommended for most travellers to the region, especially if unvaccinated.
- Hepatitis B – Blood & Body Fluids – Recommended for travellers to most regions.
- Tetanus – Wounds or Breaks in Skin – Recommended for travelers to most regions, especially if not previously vaccinated.
- Typhoid – Food & Water – Jab lasts 3 years. Oral vaccine lasts 5 years, must be able to swallow pills. Oral doses must be kept in refrigerator.
- Cholera – Food & Water – Recommended for travel to most regions.
- Yellow Fever – Mosquito – Required for arriving travellers from ALL countries. Recommended for all travellers over 9 months of age.
- Rabies – Saliva of Infected Animals – High risk country. Vaccine recommended for long-stay travellers and those who may come in contact with animals.
- Polio – Food & Water – Recommended for travel to some regions. Single adult booster recommended.
See the tables below for more information:
Proof of yellow fever vaccination is required for entry to Sierra Leone.
The NaTHNaC also says that the Zika virus is a risk in Sierra Leone. This virus can cause serious birth defects. It is recommended that pregnant women, or women planning to become pregnant, should not travel to Sierra Leone.
Ebola struck Sierra Leone in July of 2014. The outbreak claimed more than 700 lives.
In March 2016, the World Health organisation declared Sierra Leone Ebola-free.
To find out more about these vaccines, see our vaccinations page. Ready to travel safely? Book your appointment either ring or start booking online now .
Do I Need a Visa or Passport for Sierra Leone?
A visa is required for all travel to Sierra Leone. Passports must have at least six months validity. Proof of yellow fever vaccination is required to enter the country. If you do not have proof of vaccination, you may be vaccinated on site, quarantined or returned to your previous location.
Sources: Embassy of Sierra Leone and GOV.UK
What is the Climate Like in Sierra Leone?
Sierra Leone is, for the most part, humid year-round. The country’s hottest season is from November through around April. During this time, travellers can expect a slight drop in humidity, but a spike in temperatures. Near the coast, breezes from the Atlantic offer a slight drop in temperature. March is considered the peak of the dry, hot season.
From December to January, dry dust storms from the Sahara blow through most of the country.
November and May are considered wet months. Travellers should expect a moderate amount of rainfall during this time.
- Freetown – In this coastal town, the temperatures tend to be relatively cooler than other major cities in Sierra Leone. Freetown experiences frequent rainfall.
- Kenema – Located in the South Sierra Leone, the climate is tropical and rainfall is present for most of the year. The dry season here has little impact on the climate.
- Makeni – Located in the centre of Sierra Leone, this city experiences weather like Kenema to the South and Freetown to the West. But, this area experiences less rainfall.
How Safe Is Sierra Leone?
Sierra Leone is widely regarded as one of the poorest countries in the world. With this poverty comes an increase in crime rates.
Freetown is seen as the safest destination in the country. But, even in Freetown, night time wandering is not recommended. If you decide to travel from Freetown, the trip should be made in the daylight as run-ins with bandits are not uncommon.
If you are headed to border areas pay attention to your surroundings and never travel alone if you can help it. For instance, the border to Liberia is considered unstable.
Is the Food Safe In Sierra Leone?
Most dishes in Sierra Leone are spicy, plant-based and served with rice. Vegetable, meat and nut stews are common. Local dishes include: okra stew, cassava bread, coconut cake and pepper soup.
More impoverished areas in the country will have poor hygiene practices. It is best to stick to restaurants that are recommended for serving quality food on a consistent basis.
Although street food may smell tempting, cooking food outdoors increases the likelihood of your meal becoming contaminated.
All travellers to Sierra Leone should bring a traveller’s diarrhoea kit and receive cholera , typhoid and hepatitis A vaccinations.
Camping With the Wildlife of Tiwai Island
Gola Forest National Park is the best opportunity to get up close with wildlife. At one point of entry to the park sits Tiwai Island, where 11 primate species, exotic butterflies and pygmy hippos live.
Local groups offer weekend excursions that involves canoeing, hiking, animal tracking and visits to local communities for a full cultural experience.
What Should I Take to Sierra Leone?
Consider packing the following items, regardless what time of year you plan on travelling to Sierra Leone:
- Either a rain kagoul or a light rain jacket – Prepare for any expected or unexpected rainfall.
- Insect spray or insect repellent – The high level of humidity across the country attracts mosquitoes, among other insects.
- Long sleeved shirts and trousers – Coverage of the arms and legs further reduces your chances of being bitten by mosquitoes
- Light and airy, yet relatively conservative clothing – The temperatures are manageable, but humidity can make it feel much warmer than it is.
Embassy of the United Kingdom in Sierra Leone
If you are in Sierra Leone and have an emergency (for example, been attacked, arrested or someone has died) contact the nearest consular services. Contact the embassy before arrival if you have additional questions on entry requirements, safety concerns or are in need of assistance.
British High Commission Freetown 6 Spur Road Freetown Freetown Sierra Leone Telephone: +232 (0) 78200190 Emergency Phone: +232 (0) 76780713 Email: [email protected]
Ready to start your next journey? Ring us up at or book online now !
On This Page: Do I Need Vaccines for Sierra Leone? Do I Need a Visa or Passport for Sierra Leone? What Is the Climate Like In Sierra Leone? How Safe Is Sierra Leone? Is the Food Safe In Sierra Leone? Camping With the Wildlife of Tiwai Island What Should I Take to Sierra Leone? Embassy of the United Kingdom in Sierra Leone

- Privacy Policy
- Automatic Data Collection Statement
Sierra Leone Travel Restrictions
Traveler's COVID-19 vaccination status
Traveling from the United States to Sierra Leone
Open for vaccinated visitors
COVID-19 testing
Not required
Not required for vaccinated visitors
Restaurants
Not required in public spaces.
Sierra Leone entry details and exceptions
Documents & additional resources, ready to travel, find flights to sierra leone, find stays in sierra leone, explore more countries on travel restrictions map, destinations you can travel to now, dominican republic, netherlands, philippines, puerto rico, switzerland, united arab emirates, united kingdom, know when to go.
Sign up for email alerts as countries begin to open - choose the destinations you're interested in so you're in the know.
Can I travel to Sierra Leone from the United States?
Most visitors from the United States, regardless of vaccination status, can enter Sierra Leone.
Can I travel to Sierra Leone if I am vaccinated?
Fully vaccinated visitors from the United States can enter Sierra Leone without restrictions.
Can I travel to Sierra Leone without being vaccinated?
Unvaccinated visitors from the United States can enter Sierra Leone without restrictions.
Do I need a COVID test to enter Sierra Leone?
Visitors from the United States are not required to present a negative COVID-19 PCR test or antigen result upon entering Sierra Leone.
Can I travel to Sierra Leone without quarantine?
Travelers from the United States are not required to quarantine.
Do I need to wear a mask in Sierra Leone?
Mask usage in Sierra Leone is not required in public spaces.
Are the restaurants and bars open in Sierra Leone?
Restaurants in Sierra Leone are open. Bars in Sierra Leone are .

Sierra Leone launches Online Travel Portal to Manage Passenger
by dsti_v2 | Jul 5, 2023 | COVID19 | 0 comments

Travel.Gov.Sl is Sierra Leone’s official travel registration portal for passengers arriving at or departing from Freetown International Airport. The ICT Covid-19 Response PIllar manages the site which processes travel authorisation and assists the Surveillance Pillar with contact tracing during the COVID-19 pandemic.
The Government of Sierra Leone has reopened its national airspace to commercial flights after air, land, and sea borders were closed on March 22, 2020. Public health and aviation officials agree that one key way to build traveler confidence and continue to flatten the coronavirus curve is with increased testing.
Sierra Leone’s travel protocols effective July 22, 2020, require all passengers to apply for a travel permit from Travel.Gov.Sl . To receive permission to travel in or out of the country, each passenger must provide the following: A negative COVID-19 PCR lab test result issued no longer than 72hours before departure, proof of payment for a COVID-19 PCR test in Sierra Leone, and a completed public health locator form. Children ages two years old and younger are exempt from testing. Travel.Gov.Sl is the one-stop-shop that will process all requirements and issue travel authorizations.
Travel.Gov.Sl is available 24/7. Passengers can register and pay for their tests online and through mobile money. They can order a regular or premium test, with the latter offering appointment flexibility.
Since the COVID-19 outbreak in Sierra Leone the Directorate of Science, Technology, and Innovation as the lead of the ICT Pillar of the National Covid-19 Emergency Response has worked with various Ministries, Departments, and Agencies, Local ICT experts and development partners to deploy digital tools to improve the fight against the coronavirus. Fix Solutions , a technology company has played a leading role in the design and deployment of the travel web application.
From drones for surveillance during lockdowns to an e-pass solution to ease travel restrictions , and a COVID-19 Self-Check SMS and USSD Mobile Application ; DSTI continues to champion Sierra Leone’s commitment to national innovation.
#TECHAGAINSTCOVID19 COVID-19 COVID-19 E-PASS FOR ESSENTIAL TRAVEL DSTI SIERRA LEONE
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Recent Posts
- Forging Future Frontiers: UNICEF Sierra Leone Country Rep, Rudolf Schwenk Visits DSTI Sierra Leone
- General Procurement Notice: Digital Connectivity in Schools
- Bridging Digital Divides: ISDB, Unicefsl and Sierra Leone’s Bold Stride To Connect 11,000 Schools to The Internet
- Sierra Leone Joins Global Digital Public Infrastructure Ecosystem For The Launch Of The 50in5 Campaign
- Sierra Leone Joins Global Dpi Ecosystem For The Launch Of The 50in5 Campaign
Recent Comments
We’re sorry, this site is currently experiencing technical difficulties. Please try again in a few moments. Exception: request blocked
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 13 March 2024
Last-mile delivery increases vaccine uptake in Sierra Leone
- Niccolò F. Meriggi ORCID: orcid.org/0000-0002-6757-1284 1 , 2 , 3 ,
- Maarten Voors ORCID: orcid.org/0000-0001-5907-3253 2 ,
- Madison Levine 4 ,
- Vasudha Ramakrishna 5 ,
- Desmond Maada Kangbai 6 ,
- Michael Rozelle 2 ,
- Ella Tyler 2 ,
- Sellu Kallon 2 , 7 ,
- Junisa Nabieu 2 ,
- Sarah Cundy 8 &
- Ahmed Mushfiq Mobarak ORCID: orcid.org/0000-0002-1916-3438 9
Nature volume 627 , pages 612–619 ( 2024 ) Cite this article
4739 Accesses
2 Citations
159 Altmetric
Metrics details
- Developing world
Less than 30% of people in Africa received a dose of the COVID-19 vaccine even 18 months after vaccine development 1 . Here, motivated by the observation that residents of remote, rural areas of Sierra Leone faced severe access difficulties 2 , we conducted an intervention with last-mile delivery of doses and health professionals to the most inaccessible areas, along with community mobilization. A cluster randomized controlled trial in 150 communities showed that this intervention with mobile vaccination teams increased the immunization rate by about 26 percentage points within 48–72 h. Moreover, auxiliary populations visited our community vaccination points, which more than doubled the number of inoculations administered. The additional people vaccinated per intervention site translated to an implementation cost of US $33 per person vaccinated. Transportation to reach remote villages accounted for a large share of total intervention costs. Therefore, bundling multiple maternal and child health interventions in the same visit would further reduce costs per person treated. Current research on vaccine delivery maintains a large focus on individual behavioural issues such as hesitancy. Our study demonstrates that prioritizing mobile services to overcome access difficulties faced by remote populations in developing countries can generate increased returns in terms of uptake of health services 3 .
Similar content being viewed by others

Safety outcomes following COVID-19 vaccination and infection in 5.1 million children in England

A meta-analysis on global change drivers and the risk of infectious disease
Post-COVID conditions following COVID-19 vaccination: a retrospective matched cohort study of patients with SARS-CoV-2 infection
By 10 March 2022, more than a year after COVID-19 vaccines arrived on the market, 80% of the populations living in high-income countries had received at least one dose compared with only 15% of the people in low-income countries. As of 20 November 2023, only 33% of the population in Africa had received at least the first dose of a COVID-19 vaccine 1 . Low rates of vaccination keep many countries in Africa vulnerable to the threat of disease recurrence and a renewed possibility of costly lockdowns capable of undermining employment, income generation and food security 4 . Low vaccination coverage also raises the hazard of new subvariants emerging that puts the entire world at risk 5 .
To understand why vaccination rates remain low, we assembled data on vaccination beliefs, hesitancy and access from several countries in late 2021 (ref. 6 ). Nationally representative data from Sierra Leone revealed that obtaining access to a COVID-19 vaccine required the average person in Sierra Leone to travel three and a half hours each way to the nearest vaccination centre at a cost that exceeds 1 week of wages 2 . This finding motivated the design of an intervention we implemented in March–April 2022 in partnership with the Sierra Leone Ministry of Health and Sanitation (MoHS) and the international non-governmental organization (NGO) Concern Worldwide. The primary aim of this intervention was to take vaccine doses and nurses to administer vaccines to remote, rural communities, preceded by seeking permission and community mobilization. A cluster randomized controlled trial (RCT) across 150 communities showed that the vaccination rate in treatment villages increased by about 26 percentage points in response to this intervention. In addition, large numbers of people from neighbouring communities showed up to receive vaccines at our temporary clinics. In villages that received the intervention, the average number of people vaccinated increased from about 9 people pre-intervention to 55 people within the intervention period of about 2–3 days, at a cost of $33 per person vaccinated.
These results suggest that low vaccination rates are related to deficiencies in access and that a cost-effective intervention is capable of overcoming that deficiency. The Sierra Leone MoHS operates a network of peripheral health units (PHUs), but a significant proportion of people in Sierra Leone—particularly those in inaccessible rural areas—live outside the 5-km catchment area of any PHU. As such, interventions such as the one we conducted in communities outside PHU catchment areas are necessary to ease the burden of access.
This result carries broader implications for global public health. The child mortality rate in Sierra Leone was 10.5% in 2021 (ref. 7 ), as many children die from preventable diseases that immunizations and other simple interventions could address. The situation is almost as acute in neighbouring Guinea and Liberia. By contrast, efforts at community engagement in Bangladesh, including simple acts of taking maternal and child health interventions to rural populations, contributed to increasing the infant vaccination rate from 1% in the early 1980s to more than 70% within 10 years 8 . Populations in remote areas of West Africa have proven more challenging to reach, but our intervention with COVID-19 vaccination serves as a proof of concept that it may be similarly possible to tackle the high rates of child mortality in West Africa by cost-effectively delivering simple health interventions to rural populations. In fact, bundling multiple health interventions together would further reduce the cost of delivery per person treated given the high fixed transportation costs of reaching each remote community.
These results are relevant for donors and international pharmaceutical companies who have cited cases of unused vaccines in Africa reaching expiration dates 9 to explain why low-income countries did not receive adequate supplies of vaccine doses early in the pandemic 10 , 11 . Our implementation efforts taught us that the Sierra Leone MoHS needed to engage in ‘learning by doing’ to develop new distribution systems to reach remote populations with those doses. But it is a catch-22 situation: the required experimentation is only possible once a steady and dependable supply of vaccine doses is made available.
To benchmark our results against other vaccination strategies, we conducted a comprehensive literature review that identified 235 distinct interventions in 144 RCT studies that used information, nudges, community engagement, social signalling and non-financial and financial incentives to increase vaccination rates across many settings around the world. More than one third of these interventions produced null effects. Here our access intervention produced a larger percentage point effect size than 223 (95%) of the treatments reviewed. This result is not surprising because vaccinating the first 50% of the population in remote parts of low-income countries requires solving the fundamental problem of access, which we address. Once access issues are addressed, misinformation and hesitancy may loom large in the effort to vaccinate the last 20% of the population of high-income countries who stubbornly hold out, and this is the target of the bulk of the literature. Even in high-income settings, access constraints were relevant in the earliest phase of COVID-19 vaccine delivery 12 .
This finding implies that we may need to further emphasize access interventions if we are to increase the global vaccination rate and improve vaccine equity. Guidelines from the Centers for Disease Control and the World Health Organization (WHO) highlight the importance of ‘bringing services closer to the people’, and our RCT is a proof of concept that such approaches can increase vaccination rates rapidly and cost-effectively, even under difficult circumstances in the most remote communities. The mobile delivery concept has produced large effects in HIV testing 13 . Rigorously demonstrating effectiveness in vaccine delivery is crucial given the persistent low rates of vaccination in low-income countries. Our literature review revealed thousands of studies on vaccine hesitancy and misinformation, but only a handful on vaccine supply and access, with a clear bias in favour of high-income contexts. This imbalance is emblematic of a wider debate on the relative importance of individual-specific behavioural factors versus systemic deficiencies in limiting the diffusion of welfare-improving technologies among low-income populations 14 . Prominent behavioural scientists have recently acknowledged our excessive focus on individual behavioural peculiarities (‘i-frame’) at the expense of systemic solutions (‘s-frame’) 15 .
Context and research design
We conducted a pre-registered cluster RCT in 150 rural villages in Sierra Leone. We first mapped all PHUs where the MoHS was offering COVID-19 vaccines together with the catchment areas of a PHU, which is defined by the MoHS as the 5-mile (about 8-km) radius around each PHU. We then compiled a list of all communities situated outside these catchment areas and randomly selected 150 communities from this list. Overall, 100 communities were randomly assigned to receive the intervention and the other 50 were assigned to the control group. During March and April 2022, a research team first visited all communities to conduct a village population listing and a baseline survey. Immediately afterwards, mobile vaccination teams coordinated by the MoHS visited the 100 villages assigned to the intervention for 2–3 days per village (Supplementary Fig. 1 ).
On the first day of the intervention, a social mobilization team—trained and supervised by the MoHS—organized a conversation with all village leaders, including the town chief, mammy queen, town elders, the youth leaders and religious leaders, and any other important stakeholders including the paramount and section chiefs if they were available (step 1; Fig. 1a ). Members of the social mobilization team we employed were previously vetted and trained by ministry staff and commonly engaged for short-term projects such as vaccination campaigns. This cadre is referred to as MoHS volunteers because they are paid per-diem against project work and not a regular salary per a civil servant. The mobilization team explained the purpose of the visit, answered questions about the available vaccines and asked leaders for their cooperation in encouraging eligible community members to take the COVID-19 vaccine.
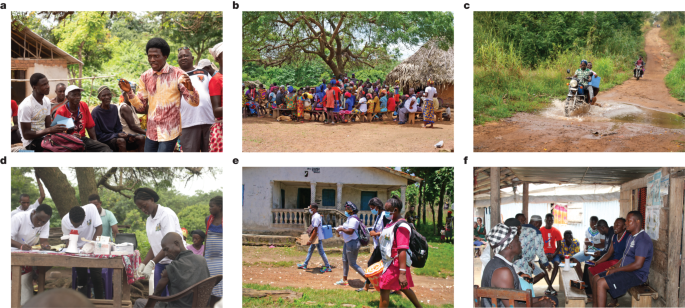
a – f , Representative photographs of the steps taken by the vaccination teams in each village for the mobile vaccination clinic. a , Step 1. A social mobilization team from the MoHS organizes a meeting with village leaders. b , Step 2. Social mobilizers convene a community meeting to talk directly with all village residents about vaccine efficacy and safety, the importance of getting vaccinated, address villagers’ questions and concerns, and the location and timing of the mobile vaccination site. c , Step 3. MoHS staff bring vaccine doses and staff to the village. d , Step 4. MoHS staff set up a 48–72 h mobile vaccine clinic in a central location in the village. e , Step 5a. Social mobilizers provide vaccine information to community members in private during door-to-door visits. f , Step 5b. Social mobilizers target social groups at fixed spots in and around the villages. Photographs in a – f reproduced with permission from Concern Worldwide.
Social mobilizers then asked leaders to convene a community meeting that same evening (when people return home from farms) to allow mobilizers to talk directly with all village residents about vaccine efficacy and safety, the importance of getting vaccinated, and to address villagers’ questions and concerns. This process (step 2; Fig. 1b ) ended with social mobilizers explaining the location and timing of the mobile vaccination site that they were about to set up.
Vaccine doses, nurses to administer vaccines and MoHS staff who could register the vaccinated were brought into the community either the same evening or early the next morning (step 3; Fig. 1c ). The vaccine doses and staff often travelled on motorbikes or on boats given the difficult terrain they had to traverse to reach these remote communities. Once the team was in place, the temporary vaccination site started operating in a central location in the village (step 4; Fig. 1d ). Villages in our sample were small, with houses closely clustered; therefore, walking distances to the vaccination site were short. The vaccination site remained operational from sunrise to sunset over the next 2–3 days, which enabled people to visit when convenient. Nurses and registration staff remained stationed at the temporary clinic while the mobilizers continued to provide vaccine information to various community members (step 5).
We randomized the exact nature of these additional step-5 mobilization activities. Half the treatment villages were randomized into an individualized door-to-door campaign (step 5a; Fig. 1e ), whereby social mobilizers went to 20 randomly selected structures to privately discuss any concerns about that vaccine that the household residents had and to encourage them to visit the vaccination site. The other 50 treatment communities were randomized into small-group outreach (step 5b; Fig. 1f ), whereby mobilizers targeted social groups who gathered at fixed spots in and around the villages (for example, groups of farmers in fields, mosque attendees or women collecting water). Social mobilizers engaged the group to have joint conversations about the vaccines. There was equipoise about whether individualized or small-group outreach would be more successful in persuading people to get vaccinated, so we tested both strategies.
Effects on COVID-19 vaccination rate
Our primary outcome was verified adult vaccine uptake, which was measured using a respondent-level question on whether the person took a COVID-19 vaccine of any type, checked against their vaccination card (if consented). This measure provided us with a site-level count of vaccine doses administered.
To calculate a village-level vaccination rate, we first enumerated the population in all 150 treatment and control villages. Such community census lists typically do not exist in Sierra Leone. Our research team therefore walked to all structures in every village to tally the number of households (39 on average, s.d. = 23), and the number of individuals living in those households (29,588 individuals across the 150 villages, or about 197 people per village).
The population of these villages was on average 22.3 years old, 26.5% of households were headed by women and 64.5% of people lived in a household of 6 or fewer people. Only 20.1% lived in a household where the household head had any form of formal schooling, and about 86.1% lived in a household where the head was primarily engaged in farming. Respondent characteristics were well balanced across the treatment groups (Extended Data Table 2 ) except for the following: the baseline vaccination rate; the proportion of households employed in agriculture; the proportion of households that own a radio; the proportion of women breastfeeding; and the proportion that owns land. Although an overall F -test did not reject the equality of means across the full set of outcomes, we added these covariates in part of our analysis below.
Figure 2 shows that at baseline, the average vaccination rate in villages assigned to the control group (control villages) was 6.2% compared with 9.5% in villages that received treatment (treatment villages) (ordinary least squares (OLS) regression, difference = 0.035, s.e. = 0.014, P = 0.015, n = 12,096). After intervention, the vaccination rate increased to 30.2% in treatment villages. We report effects from linear regression specifications of the intent-to-treat effect with randomization fixed effects and heteroscedasticity-robust standard errors clustered at the village level in Extended Data Table 3 (see the section ‘Statistical analysis’ in the Methods ). The intent-to-treat effect was 26 percentage points (OLS regression, s.e. = 0.018, P < 0.001, n = 12,096). The results remained qualitatively similar (OLS regression, 25 percentage points, s.e. = 0.019, P < 0.001, n = 12,096) when covariates for respondent characteristics were added that were imbalanced at baseline (such as vaccination status) or when we aggregated the data up to the village level (OLS regression, 28 percentage points, s.e. = 0.025, P < 0.001, n = 150).
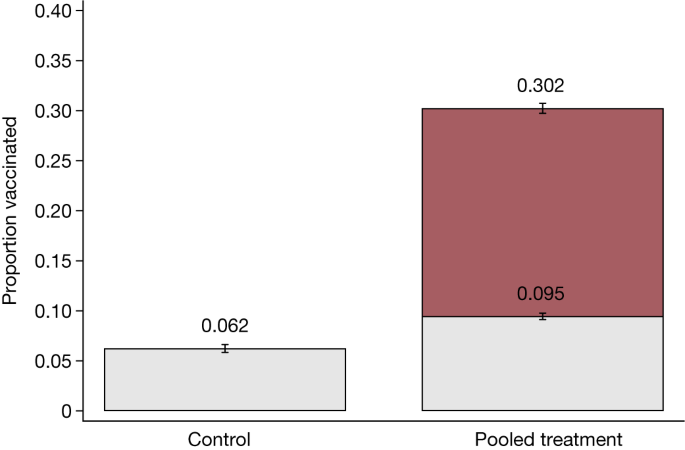
The proportion of vaccinated adults that were enumerated during the census before and at the end of the study in control villages and pooled treatment villages. The analysis includes the 12,096 people (aged >18 years) in 150 villages. Data are presented as the mean ± s.e.m. In the control group, 6% were vaccinated at baseline, whereas 9.5% were vaccinated in treatment groups. At endline, 30% were vaccinated. The intent-to-treat treatment effects estimated using OLS and including randomization block fixed effects and heteroscedasticity-robust standard errors clustered at the village level are provided in Extended Data Table 3 .
This increase in the vaccination rate is an underestimate of the total number of vaccines administered over those 2–3 days, as it does not include vaccines given to migrant returnees and others from nearby villages. The average uptake also masks considerable heterogeneity among villages. In 2 out of the 100 treatment villages, there was no increase in vaccination rate because the village authorities either dissuaded villagers from getting vaccinated or refused permission for the intervention to take place, which causing the intervention to essentially fail at step 1 (Fig. 1a ). By contrast, the full distribution of vaccination rates displayed in Supplementary Fig. 2 shows that in 5 villages, more than 50% of adults enumerated in the community census were vaccinated during the course of our intervention. A similar large degree of variation was evident from the total count of immunizations set per village (Supplementary Fig. 3 ).
Effects on total vaccination count
Many of the people who attended our temporary clinics to receive a vaccine were not enumerated during the community census. These additional people fell into one of three categories: residents of other nearby villages (who heard about the clinic and were interested in taking advantage of the easy access to a vaccine); recent migrant returnees who were not present during the village listing; and others—such as high-frequency commuters—not captured in the census. For these auxiliary populations, we do not have a denominator and can therefore not estimate a vaccination rate. We can, however, provide results on vaccination counts.
At baseline, there were on average about 5 people vaccinated in control villages and about 9 people in treatment villages (OLS regression, difference = 3.57, s.e. = 1.51, P < 0.021, n = 150). Figure 3 shows that after the intervention was implemented over the subsequent 2–3 days, the number of vaccinated individuals increased to about 55 people on average per treatment site, which is a 6-fold increase. This is the full effect of our mobile vaccination drive. Among individuals vaccinated who were not enumerated in the census, 53% (12–13 people per treatment community) were visitors who came from nearby villages to get vaccinated, whereas the remaining 47% (11–12 people) included short-term, circular commuters or migrant returnees who were not present on the day of the census and could not be matched to our listing records, as well as individuals whose ‘community of origin’ was unknown. The intent-to-treat regression estimates with heteroscedasticity-robust standard errors and additional covariates are included in Extended Data Table 4 . In total, the teams vaccinated 4,771 people aged 12 years or above. Of these, 39% received a Johnson & Johnson vaccine, 29% Pfizer, 17% Sinopharm and 16% received AstraZeneca. A variety of vaccine types was administered because there was no steady supply of any specific type of vaccine dose in Sierra Leone when this intervention was conducted. Therefore, we had to make use of the vaccines available in the Ministry of Health stocks in any given week.
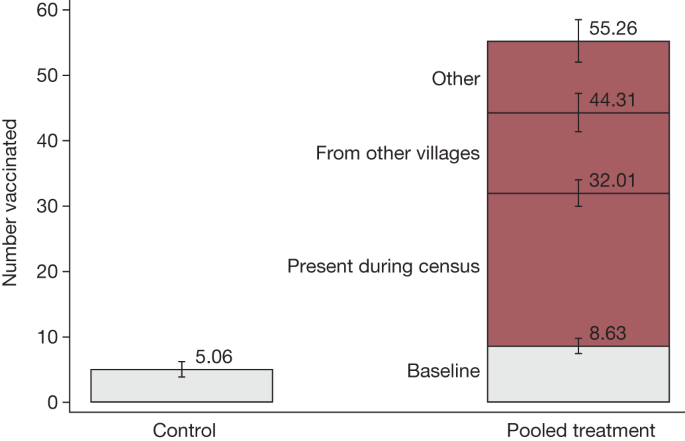
The number of the people vaccinated before and by the end of the study. Data are presented as the mean ± s.e.m. The analysis includes 150 villages. In the control group, on average five people were vaccinated, whereas in treatment villages, this was nine people. Treatment increased the count to 55 people, including 22–23 individuals who were enumerated during the census group, 12–13 people from nearby villages and 11–12 short-term, circular commuters or migrant returnees who were not present on the day of the census and could not be matched to our listing records, as well as individuals whose community of origin was unknown. The intent-to-treat treatment effects estimated using OLS and including randomization block fixed effects and heteroscedasticity-robust standard errors are provided in Extended Data Table 4 .
Effects of home visits
Both types of mobilization activities implemented in step 5 had similar effects on the vaccination rate. The evidence on whether the door-to-door or small-group activities were more effective was mixed. When we compared across communities, the door-to-door programme increased the adult vaccination rate by about 29 percentage points compared with 23 percentage points in villages assigned to the small-group mobilization activities ( t -test, difference = 6 percentage points, P = 0.014, n = 12,096; see column 1 in Extended Data Table 1 ). However, when we studied individual households randomly assigned to a visit against those who are not within door-to-door villages, we did not detect any differential uptake. In these 50 villages, up to 20 randomly selected structures were visited for a private or semi-private conversation with residents about the vaccine and to encourage them to visit the temporary clinic. The random selection of structures enabled us to report experimental results on the effects of receiving this extra nudge on the propensity to receive a vaccine. We interpret this activity as a ‘demand-side treatment’, in that the visit and conversation provides that resident an opportunity to discuss their concerns or questions about vaccines in private, which could be useful to overcome potential hesitancy. Column 3 in Extended Data Table 1 shows that this extra effort did not generate additional demand beyond the effect of our ‘supply side’ activities to enhance vaccine access. The adult vaccination rate at the end of the vaccination programme among those who received the home visit by mobilizers was not different from those who did not receive the extra nudge points (OLS regression, difference = –0.01, s.e. = 0.019, P = 0.543, n = 3,760). Social mobilizers received extensive training and close supervision, but the lack of impact from this additional demand-generating activity on vaccine uptake may reflect low effort by social mobilizers. Within-village spillovers may also dampen these individual treatment effects. Unfortunately, we lack data on distances and other channels of interactions among households to formally test this measure. However, this type of spillover may be small owing to the relatively short time interval between the home visits and the vaccine drive.
We do not have an equivalent analysis of the individual effect of the small-group treatment because that was not randomized within villages. Moreover, the enumerators were not able to exactly track which households participated in the small-group sessions.
Although our vaccine access intervention significantly raised the vaccination rate, it was also clear that we remained far short of reaching the WHO goal of near-universal uptake. We collected individual-level data in all treatment villages after the intervention from both vaccine takers and non-takers. These data can shed some light on why and how our access intervention was more or less successful for certain types of people.
Meeting attendance
Step 2 of our intervention (Fig. 1b ) was to organize a community-wide meeting to inform all village residents about the vaccine clinic. The field team registered which community members attended that meeting, and 41% of households participated in these meetings. Overall, 44% of those who chose to attend the meeting subsequently chose to get vaccinated. One cannot impose any causal interpretation to this correlation because people who were already interested in getting vaccinated may have been the ones who chose to attend the meeting.
We can make a slightly stronger inference by examining the subset of people who stated in our baseline survey that they were unwilling to receive a vaccine (Extended Data Table 5 ). Within this subgroup, 53.8% of those who attended meetings ultimately took the vaccine, whereas the vaccination rate was only 14.4% among those who did not attend. Even within the converse subgroup (those who stated at baseline that they were willing to take the vaccine), meeting attendance was strongly predictive of subsequent vaccine uptake: 64.6% vaccination rate among attendees and 39.4% among non-attendees.
These are not causal estimates, but the size and direction of these correlations suggest that the information shared in the meeting, and the answers that were provided to the community’s questions, are unlikely to have dissuaded people from getting vaccinated. These correlations—combined with our team’s on-field experience—suggest that holding these meetings was helpful and form a necessary part of any access intervention. Encouraging greater attendance in meetings in any future replications would probably be a good idea.
Vaccination knowledge and trust
We also collected data on another intermediate outcome in a subset of villages: people’s knowledge and attitudes regarding the COVID-19 vaccine. Figure 4 shows that the treatment improved people’s knowledge about vaccines (OLS regression, difference = 0.11 points, s.e. = 0.044, P = 0.019, n = 817). The change in knowledge implies that our intervention was not solely about improving access. That is, the community interactions and the information we shared were also relevant parts of the intervention package. However, there was no significant change in people’s beliefs about vaccine efficacy (OLS regression, difference = 0.097, s.e. = 0.074, P = 0.197, n = 686). Using a 95% confidence interval (CI), we can reject that our treatment increased beliefs about vaccine efficacy by more than 12 percentage points. The effect on beliefs about the safety of vaccines is not statistically precise (OLS regression, difference = 0.131 points, s.e. = 0.070, P = 0.069, n = 686)—we can neither rule out a null effect nor a 27 percentage point effect. The null effects in OLS regressions on the sources that people trust the most for receiving health information were more precisely estimated: community health clinics (OLS regression, difference = 0.013, s.e. = 0.059, P = 0.828, n = 817, 95% CI upper bound = 0.13); the MoHS (difference = 0.011, s.e. = 0.025, P = 0.682, n = 817, 95% CI upper bound = 0.06); media (OLS regression, difference = –0.028, s.e. = 0.047, P = 0.553, n = 817, 95% CI upper bound = 0.07); social media (OLS regression, difference = –0.002, s.e. = 0.004, P = 0.555, n = 817, 95% CI upper bound = 0.006); or family and friends (OLS regression, difference = –0.026, s.e. = 0.022, P = 0.242, n = 817, 95% CI upper bound = 0.018). Extended Data Tables 6 and 7 provide the associated regression estimates. Note that because this is an exploratory exercise in which we test treatment effects across several outcomes, the tables report the false discovery rate (FDR)-adjusted q values to adjust for multiple hypothesis testing.
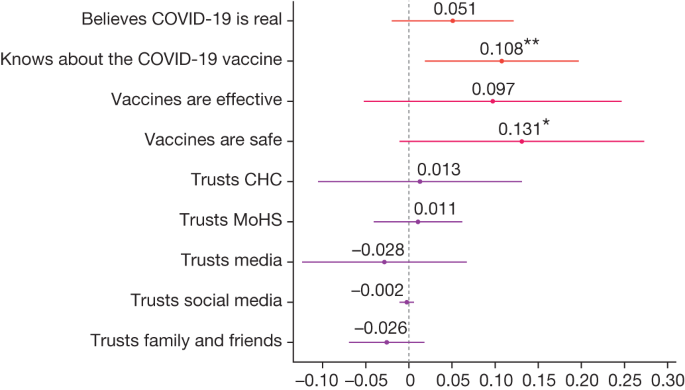
Intent-to-treat estimates of community treatment assignment for each outcome listed on the y axis. Treatment effects were estimated using OLS and included randomization block fixed effects and heteroscedasticity-robust standard errors clustered at the village level. Each dot is labelled with the exact coefficient (to three decimal places) and significance at the ***1,**5 and *10 per cent critical level. Bars represent 95% CIs of treatment estimates. The analysis includes 45 villages and 817 households surveyed at endline for which we observed complete randomization blocks. Associated regression results are provided in Extended Data Tables 6 and 7 , including corresponding sample sizes. Reported estimates do not correct for multiple hypothesis testing. The Extended Data tables report the associated FDR-adjusted q values. The survey measures for the ‘Believes COVID-19 is real’ comes from the survey question: “Do you believe that COVID-19 exists in the world?” (yes or no). ‘Knows about the COVID-19 vaccine’ comes from the survey question: “Do you know about the COVID-19 vaccine/marklate?” (yes or no). ‘Vaccines are effective’ is 1 if respondents completely agree with the statement: “Vaccines are effective.” ‘Vaccines are safe’ is 1 if respondents completely agree with the statement “How much do you agree with this statement: vaccines are safe.” Trust in sources of information are from a multiple-select question: “Who do you most trust getting information about COVID-19?” (community health clinic (CHC), MoHS, media (news, TV), social media (Facebook, among others), family and friends, among others).
Heterogeneity across demographic groups
Figure 5 shows the differences in treatment effect for specific demographic subgroups. Extended Data Table 8 and Supplementary Table 1 provide associated regression results. The treatment effect was 7 percentage points larger for men than for women (OLS regression, difference = –0.067, s.e. = 0.016, P < 0.001, n = 12,096), and 12 percentage points larger for the >55 years age group compared with the 18–24 years age group (OLS regression, difference = –0.122, s.e. = 0.028, P < 0.001, n = 12,096). We cannot reject the null hypothesis that there is no difference in treatment effects across education (OLS regression, difference = –0.003, s.e. = 0.018, P = 0.864, n = 12,096, 95% CI upper bound = 0.032), land ownership (OLS regression, difference = 0.038, s.e. = 0.035, P = 0.268, n = 2,674, 95% CI upper bound = 0.11) or food security status (OLS regression, difference = –0.006, s.e. = 0.032, P = 0.865, n = 2,674, 95% CI upper bound = 0.06), and can rule out large effect sizes.
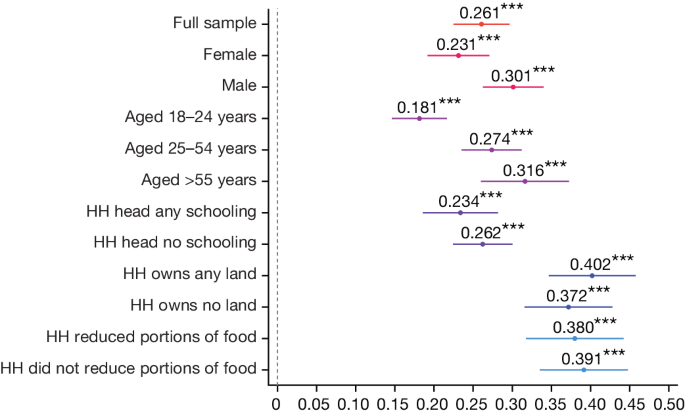
Intent-to-treat estimates of the vaccination rate of the pooled treatment groups for each subgroup listed on the y axis. Treatment effects were estimated using OLS and included randomization block fixed effects and heteroscedasticity-robust standard errors clustered at the village level. Each dot is labelled with the exact coefficient (to three decimal places) and significance at the ***1, **5 and *10 per cent critical level. Bars represent 95% CIs of treatment estimates. The dependent variable is the vaccination status of adults at the end of the study enumerated during the census. Sex, age and schooling data are from the census. Land ownership and food insecurity are from the baseline sample. Associated treatment estimates and associated sample size for each subgroup are provided in Extended Data Table 8 . The indicator for ‘HH head any schooling’ indicates whether the household (HH) head had schooling above the primary level. The ‘HH owns any land’ indicates whether the household owns land. The ‘reduced portions of food’ statements indicate whether any household member had reduced food portions during the previous week.
Comparison with other vaccination efforts
As shown in Extended Data Table 3 , the intervention increased vaccination rates by about 26 percentage points. Although such an increase seems substantial, this is the gain off a very low base rate: just 6–9.5% were vaccinated at baseline. Another relevant benchmark is our percentage point effect size and how that compares with other vaccination campaigns evaluated in the literature.
We conducted a literature review of vaccination strategies that have been evaluated using RCTs (see the section ‘Literature review of vaccination uptake RCT studies’ in the Methods ). The Methods provides inclusion criteria for this review. We identified 144 different published RCT studies that report the results of 235 distinct interventions.
These interventions varied across multiple dimensions, spanning time, space and strategy, often as part of the same study with multiple components. For clarity and brevity, we identified five major intervention ‘families’, which could be further fragmented into more granular intervention ‘types’. The families into which interventions were sorted were education, community actions, communications, incentives, and healthcare improvement and worker training. Among the 144 relevant studies, only 3 focused on the essential theme of vaccine access in a low-income context, and none of them were centred on COVID-19 vaccines 16 , 17 , 18 .
Supplementary Fig. 5 demonstrates the heterogeneity of effect sizes across these 235 different treatments (effect size range of –6 to 50 percentage points). Of all treatments reviewed, 35% had no significant effect on vaccine uptake. Perhaps unsurprisingly, owing to the variety of incentive types and sizes, the incentives group was strongly positively skewed, accounting for five out of the top ten effect sizes overall. However, the highest median effect size was among educational interventions (median = 6.25) 19 , 20 .
The intervention we conducted in Sierra Leone—whereby mobile health teams visited remote communities for 48–72 h to ease access burden—produced a larger percentage point effect size than 223 (95%) of the treatments reviewed.
Supplementary Table 2 provides details of the intervention approach used in each study. The majority of these studies were conducted in high-income settings (83%). Many of the vaccination campaigns evaluated were nudges and reminders by text messages, telephone or mailings (50%). Nudges are inexpensive, but often produce small or null effects. Other strategies involved visiting parents to educate them about the benefits of childhood immunization (25%) or sending community health workers (5%). Others offered direct financial incentives against a verified vaccination (9%).
Of special interest were recent studies that attempted to promote COVID-19 vaccinations. A study in Sweden 21 offered monetary rewards of $24 to receive a COVID-19 vaccine, and this increased the vaccination rate by an extra 4 percentage points (from 72 to 76%). A financial incentive of $10–50 combined with other nudges in the United States did not produce any effect 22 . City-wide and state-wide lotteries offering financial rewards in the United States 23 , 24 produced small or negative effects. Text-based reminders in the United States 25 , 26 and defaulting people into a vaccination appointment in Italy (so that they are forced to opt out) 27 increased vaccination rates between 0 and 3.5 percentage points.
Cost-effectiveness relative to other strategies
Sending text message reminders or running city-wide lotteries are relatively inexpensive to implement, whereas delivering vaccines to remote areas is costly. It is therefore useful to compare not just percentage point effect sizes but also the cost of administering various programmes per vaccinated individual. Moreover, we chose to work in the most remote areas not covered by the Sierra Leone MoHS vaccination programmes precisely because they are too far away even from PHUs. We collected detailed cost data on our programme to compute this metric and compared it to other studies that provide such cost information (see the section ‘Literature review of vaccination uptake RCT studies’ in the Methods ).
The total costs of our intervention to reach 100 villages was $156,023.5, or approximately $1,560 per village. This included all travel, administration and management and supervision costs, but excluded the cost of the vaccine doses, which were provided to Sierra Leone by the COVAX programme for free. This translates to a cost per dose administered of about $33.
Extended Data Table 9 provides a detailed breakdown of the fixed and variable components of our implementation costs. Of the $33, around 27% ($9) was fixed costs of training project staff and 73% ($23) was variable costs. The most expensive category (38% or $12.50) was transportation to these remote villages, which included the cost of renting vehicles and fuel. Salaries and subsistence allowances for the social mobilization and vaccination teams accounted for another one quarter of the total costs.
To conduct this intervention again at larger scale, the variable costs would need to be repeated, but not the fixed costs of training. At scale, the cost of this intervention would therefore approach about $23 per person vaccinated. The wide availability of a cadre of staff known as Ministry of Health volunteers—individuals already vetted by the ministry and available to work as mobilizers on special projects against per-diems—increases the potential for scaling this project nationwide in Sierra Leone. One potential challenge of replicating this project to other countries is to find trained staff who can take on that mobilization role.
Note that here we are looking at cost-effectiveness from the perspective of the planner (that is, the government) and do not consider the costs imposed on households. Depending on context, meeting attendance can be inconvenient or costly. In our context, villages are small. On average, people had to walk less than a couple of hundred metres to attend the meetings. Also, to minimize the inconvenience, meetings were held in the early evenings after people returned from their farms. As a result, the opportunity cost of time was low for most participants of the meeting.
Figure 6 provides the cost per vaccinated person in year 2000 US dollars for the subset of studies in Supplementary Table 2 that reported sufficiently detailed cost information for us to be able to compute this metric. Of the 235 different treatments identified in our literature review, only 33 (14%) directly stated the cost of the intervention per successfully administered vaccination. Furthermore, of these 33 interventions, 7 did not report a cost specific to the treatment group, but only the overall cost averaged over all groups of the study. In total, 57% of the vaccination campaigns exceeded our $33 benchmark. The mean value in Fig. 6 is $83 (s.d. = 132), even after excluding the most expensive approach.
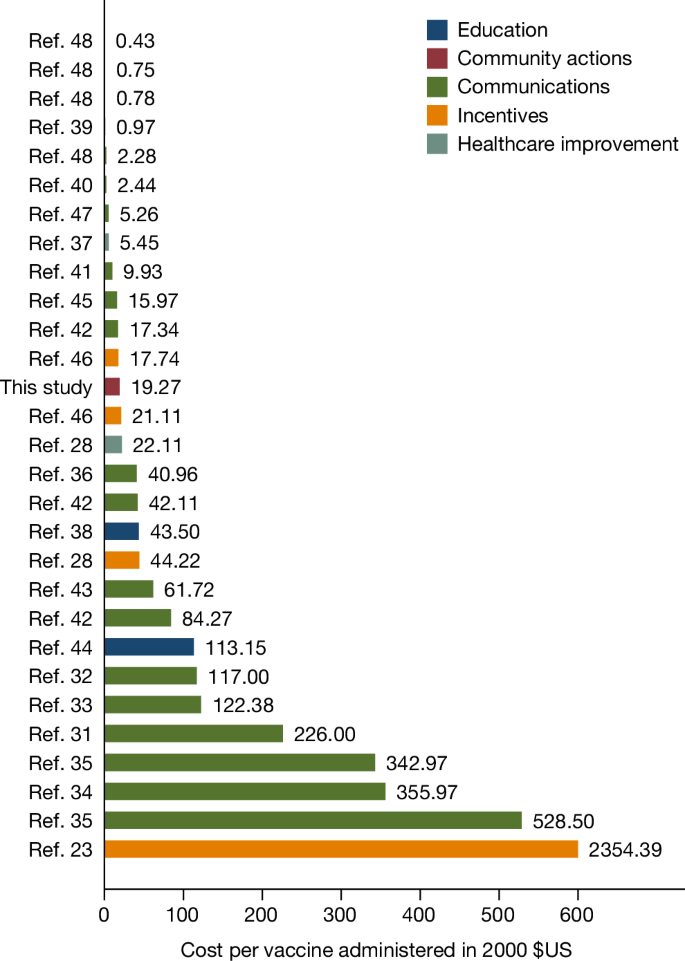
The cost per vaccination administered (in year 2000 US dollars, calculated using inflation data sourced from the US Bureau of Labor Statistics). These are treatments from studies included in Supplementary Table 2 that explicitly provided information about the cost of the intervention per vaccine actually administered. This cost specifically refers to the intervention and does not include the cost of the vaccine itself. Studies that did not unequivocally state the cost of the intervention per vaccinated person were not included. The colour of each bar indicates the broad type of intervention. The cost per person vaccinated in our study was $32.70, which is approximately $19.27 in 2000 US dollars. The mean value in this figure is $83 (s.d. = 132) after excluding the most expensive approach. References 23 , 28 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 are cited in this figure.
A study in rural India 28 pursued a similar strategy to ours by setting up measles vaccination clinics. That treatment cost $75 (in 2022 dollars) per vaccine administered, but adding an incentive for the parents to bring their children to the clinic lowered the cost to $38 per child vaccinated. The only other COVID-19 vaccine study in our review to provide cost information 21 offered $24 as a financial incentive to get vaccinated in Sweden. Unfortunately, that study did not report costs of other components of the programme, such as the cost of administering the incentive programme, verifying individual-specific vaccination information in the administrative records, sending two text message reminders, among others.
Our findings showed that a simple last-mile vaccine intervention tripled vaccination rates within 48–72 h. In addition, auxiliary populations showed up to take advantage of these mobile vaccination centres, which more than doubled vaccination counts. Our intervention, despite being delivered in highly remote locations, is cost-effective relative to other efforts that aim to increase vaccination rates.
Policy implications
Vaccine equity remains an important policy goal 10 . Vaccination rates are severely lagging among rural populations in Africa. Therefore, achieving equity requires us to devise an effective strategy to reach this population. Our study provides some guidance on how to formulate that strategy.
The most immediate and direct implication of our results is for the government of Sierra Leone to replicate and expand this cost-effective programme to reach the 59% of the country’s population who reside in similar remote, rural areas outside PHU coverage. The largest expense of our intervention was the transport cost of reaching remote communities; therefore, an obvious implication is that we should bundle COVID-19 vaccines with other necessary mother, infant and child health interventions that can be simultaneously delivered on the same trip 3 . Such an approach could substantially reduce costs per person treated. However, this would still be expensive for a resource-constrained MoHS to launch at scale, and international partners must provide support. A recent study in rural Western Kenya 29 demonstrates that such integrated approaches, combining HIV testing with other preventive health services such as bed nets and water filters, can be successfully implemented.
We have begun building the necessary coalition to implement such a bundling strategy to improve the cost-effectiveness and scalability of this last-mile-delivery intervention. The Sierra Leone MoHS has prioritized HPV vaccination for girls aged 10–12 years, and routine immunizations (DTP, measles, polio) for children aged 0– 6 years to bundle with any further COVID-19 vaccine delivery. It is reasonable to wonder whether COVID-19 vaccine distribution is a high-priority investment given the low incidence of COVID-19 in Africa. However, as the experience in India from April 2021 shows, new COVID-19 variants have the capability to devastate public health systems in developing countries 30 . Health infrastructure in a typical country in Africa is even more fragile than it is in India. If we pay the transport cost to take a bundle of health interventions to these remote communities, COVID-19 vaccines could easily be an element of that bundle.
The other direct implication is to replicate such a programme in neighbouring countries with similar last-mile delivery challenges. The majority of people in sub-Saharan Africa live in rural areas 7 , so overcoming access challenges through such initiatives holds enormous potential for both achieving vaccine equity and maximizing global coverage.
Our study showed that low-income countries need to experiment with creative ideas to overcome logistical challenges, such as setting up temporary clinics and sending both vaccine doses and nurses to remote locations on motorcycles. A broader implication for international development partners and pharmaceutical companies is that they need to facilitate and underwrite such experimentation by making vaccine doses and budgets readily available to allow ministries of health to learn what approaches work best in a given context. Local institutions need to engage in ‘learning by doing’, which is impossible without a reliable supply of vaccines and incentives for staff to tinker with new, innovative ideas.
Study limitations
The intervention we implemented had two important limitations. The $33 cost (per person vaccinated) varied substantially across villages because the number of individuals per village that we managed to vaccinate varied (the vaccination rate ranged from 0 to 69%). Village leaders did not allow us to conduct the intervention at all in 2 of the 100 treatment villages, which inflates the overall average cost of our intervention. Any replication should try to identify early the villages where such refusals might occur and find ways to avoid having the entire vaccination team travel there.
Second, we observed large cross-team variation in performance. Supplementary Fig. 4 shows that some of our teams administered more than twice as many vaccines as other teams (the number of vaccines administered ranged from 0 to 146 per village, mean = 48, s.d. = 31, median = 42). Some of these differences could be due to differences in village characteristics, but our implementation experience suggests that variability in team effort also played a part. Providing good performance incentives to teams could improve the cost-effectiveness of this strategy. Given that a large proportion of the expense of the intervention is the cost of travelling to the remote village, we should strategize to ensure that we maximize the vaccination rate within the 48–72 h window once we get there.
Ethics approval
We received Institutional Review Board (IRB) approval from the Sierra Leone Ethics and Scientific Review Committee (SLERC 20220210), Yale University (2000031541) and Wageningen University (WUR 20220222). The research protocol was pre-registered at the ISRCTN Registry (study identifier ISRCTN17878735 ). All study participants completed informed consent.
The study was implemented in close collaboration between the researchers, the Government of Sierra Leone’s Expanded Programme on Immunization (EPI) at the MoHS, their National COVID-19 Emergency Response Centre and Concern Worldwide (an international NGO who partners with MoHS on health projects). This collaboration came together because all partners had the joint goal of addressing barriers to vaccine adoption in rural Sierra Leone. Although all partners are responsible for the research design, only the Ministry of Health team was responsible for actually distributing and administering vaccines. We had a memorandum of understanding in place to govern this collaboration.
Village study sample
To determine the sample size, we ran a power calculation assuming a 5% significance level with 80% power. We assumed an intra-cluster correlation of 0.15 as decisions to take a vaccine are probably highly correlated within a village. Average village populations are 2,480 people. We assumed an eligible population of 50% and a baseline vaccination rate of 2.5%. Based on the treatment effects reported in the literature for similar studies, we took a conservative approach and set our expected minimum detectable effect at 0.05. We oversampled slightly and the final design included 150 communities across the three treatment groups in a 1:1:1 ratio.
We chose study sites in collaboration with the MoHS. We started with the 2015 Sierra Leone census, which contains data on 20,659 communities in 166 chiefdoms across 16 districts. We selected 7 largely rural districts (Koinadugu, Falaba, Karene, Kambia, Tonkolili, Bombali and Port Loko), limiting the sample to 8,784 communities in 54 chiefdoms. We then restricted our sampling frame to communities that, according to the 2015 census, had no health clinic within 5 miles (about 8 km) of the community centre, the standard PHU catchment area (Extended Data Table 10 ), resulting in 1,849 communities. From this list, we excluded very small communities that contained fewer than 19 structures and communities for which latitude and longitude were missing. The final sampling frame consisted of 420 communities located in 49 chiefdoms and 7 districts. Within each district, we then matched communities on the following strata: (1) the share of the population that was immunized; (2) the age of the population; (3) literacy levels; and (4) the distance from the closest clinic. This allowed us to identify communities that had the most similar characteristics within a district and used this to assign the most similar communities to one of the treatment groups and establish comparable ‘triplets’. This resulted in 106 triplets in total. We then randomly selected 50 triplets using district as a blocking variable. The final list included 9 triplets each for Koinadugu and Falaba districts, 8 triplets for Karene district and 6 triplets each for Port Loko, Tonkolili, Kambia and Bombali districts.
Randomization
Randomization to vaccine access treatments.
Within each of the 50 triplets, we randomized villages into control, door-to-door and small-group treatment groups. This resulted in 50 villages assigned to control, 50 to door-to-door and 50 to small group (Supplementary Fig. 1 ). The sample was well balanced on observable characteristics (the F- statistic at the bottom of Extended Data Table 2 is small and not significant).
Household-level random assignment to door-to-door treatment
Within the villages randomly assigned to the door-to-door treatment group, we randomly selected up to 20 residential structures from the community census list to receive a visit from the social mobilization team.
Data collection
Community census listing and baseline survey.
Before any intervention activities took place, the research team implemented a community census to enumerate all households in all 150 villages. The research team went door to door to each residential structure and asked how many households resided in the structure. They then interviewed each household head to create a roster of those who ‘eat from the same pot; and reside under the same roof for at least the past 9 months (aside from newborn babies).’ For each household member, enumerators asked about the sex, age and vaccination status. The total census includes N = 29,588 people. Migrant household members who were temporarily away on the day of the visit would have been missed from this listing.
Next, the research team randomly selected a sample of 20 households per village from the households listed in the census to conduct a short (baseline) survey with the household head to record household characteristics (age, sex and education), access to land and food security. The total baseline sample included N = 2,240 respondents.
Exit and endline surveys
After the interventions were implemented, the research team conducted an exit survey of those who received a vaccine at each mobile vaccination clinic. The survey recorded the vaccination status verified using visual inspection of the vaccination card, as well as age and sex.
During the exit survey, enumerators also recorded where people came from and their district and village name (if different from the implementation site). To assess between-village spillovers, we then matched the names of reported villages back to our list of control villages. Using a hard match on district names and then a Levenshtein distance metric to match village names, allowing for a string distance of 2, we found only 8 matches. Using a more conservative cut-off of 1, no overlap was found. Our within-sample spillovers were small or non-existent owing to the large physical distance between pairs of sample villages. The minimum straight-line distance between project treatment and control villages was 8.5 miles (13.7 km), which would take at least 2–3 h to traverse by foot. Any spillover benefits largely accrued to others who were not part of the experimental pool.
For a subsample, the research team conducted a follow-up survey to capture knowledge of COVID-19 and COVID-19 vaccines as well as trust in various sources of information. We used data from 878 respondents in 45 villages for which we observed triplets (that is, where we had information on all treatment groups and a 1:1:1 ratio). We collected data from a total of 105 villages (50 control, 30 door-to-door and 25 small-group treatment group villages); however, only for 45 villages did we observe all three treatment groups and therefore provide a clean comparison. Respondents in this subsample of villages were highly similar to those in the overall sample. An overall F -test did not reject the equality of means: P = 0.668 (Extended Data Table 10 ).
In treatment villages, these questions were part of the exit survey and implemented 1 day after intervention activities were completed. In control villages, households were visited only once. From a design perspective, we would have ideally captured outcomes at both baseline and endline in each village. It was, however, highly unlikely that these remote places would have been visited by other health personnel from the MoHS or NGOs in the 5-day period between baseline and endline, or that a large number of people would have incurred the cost of visiting the community health clinic for receiving a COVID-19 vaccine. In addition, the costs of revisiting communities in these remote locations are high (the largest line item on the budget relates to transportation costs; Extended Data Table 9 ). We verified that there was no vaccination drive conducted during this period. Furthermore, we use the fact that our baseline survey was conducted over a few weeks across communities to inspect the temporal trends in the data. A simple regression of baseline vaccination rates on the date of the baseline survey did not reveal any trend. This reduces the concern that our choice to not revisit control villages affects the conclusions we draw.
Research assistants were blinded with respect to treatment groups and study hypothesis.
Intervention details
Timeline of activities.
The research team collaborated closely with the Ministry of Health vaccination team. Both the team of vaccinators and social mobilizers from the MoHS and enumerators in charge of the survey received extensive training on implementation protocols. Only those individuals who were considered proficient after examination were retained for implementation or data collection. Within each village the teams followed several steps outlined below (see Supplementary Fig. 1 for further details). On day 1–2, the research team implemented census listing and baseline surveys described above. On days 3–5, the social mobilizer team engaged in small-group and door-to-door mobilization, the MoHS performed a vaccination drive and the research team conducted exit surveys in treatment villages. On day 6, the research team implemented endline surveys.
Social mobilization
The MoHS trained community mobilizers on COVID-19 vaccine safety and efficacy, vaccine types and availability. All mobilizers were trained on how to respond to questions and to counter any misinformation about COVID-19. They were also trained on WHO-recommended safe practices relating to COVID-19 and were instructed to maintain social-distancing protocols and to wear masks when social distancing could not be guaranteed. Additional masks were made available for free for community members.
Community social mobilizers arrived at the village before the mobile vaccination teams. The community mobilizer engaged with local community leaders, including the town chief, section chief, paramount chief, mammy queen, town elders, youth leaders, community health officers, imams, and any other relevant authorities, to seek permission to organize a village information session. The information session took place at a central location, often the community centre or any other convenient location amenable to safe COVID-19 practices.
At the information session, the mobilizer informed community members about COVID-19, available vaccines and evidence about the safety and efficacy of vaccines in preventing transmission and severe illness. People were also informed about the mobile vaccination team and operating procedures during the vaccination drive. They encouraged participants to spread this message to other members of the community not present during the meeting.
In two treatment villages, the MoHS vaccination team did not receive permission from village authorities to conduct the vaccination drive.
Door-to-door campaign
In 50 of the 100 villages randomly selected for treatment, community mobilizers approached up to 20 structures randomly selected from the census list, after the group information session was completed. The proportion of each community assigned to treatment therefore varied with the population of the community. In four small communities, all structures were assigned. Owing to logistical complexities and costs, in some communities, mobilizers did not include highly remote village structures (more than 15 min walk from the village centre). This excluded a total of 10 structures (including 40 people aged ≥12 years). Social mobilizers met in private with residents and delivered the same information as was presented at the community meeting. In addition, they addressed people’s concerns in private. If the individuals were immediately convinced to get vaccinated, the social mobilizer would guide them to the vaccination site before moving on to the next household. Neighbours not assigned to receive a home visit were present during the information session in a few cases. In 75% of the communities, these ‘compliance issues’ were limited to representatives of three or fewer control households, and the majority of communities had no non-compliance of this kind.
Small-group mobilization
In the other 50 treatment villages, after the group information session, social mobilizers searched for small groups of people around the village to converse with. Such groups included women washing clothes around the river, individuals gathered at the ataya (tea) shops, residents playing a game of draughts, groups of people around the mosque or church or farm, or residents gathered near the town chief’s house. Social mobilizers repeated the same information presented during the community information session. If people inside the small group had already taken the vaccine before this second session, they were invited to talk about their experience. After the session, if residents wanted to take the vaccine, the social mobilizer would guide them to the vaccination site before moving on.
Mobile vaccination drive
Vaccines were transported in approved cool boxes or vaccine carriers appropriate for transportation to remote locations. In each treatment village, the MoHS mobile vaccination teams worked with community leaders to select a suitable venue for the vaccination drive. The venue was chosen with the following requirements in mind: it needed to accommodate a waiting area (with some shelter); an arrival and check-in area where patient information can be gathered, maintaining confidentiality; a space for clinical assessment and vaccine administration, including vaccine preparation, maintaining patient confidentiality, privacy and social distancing; an area and system for post-administration observation of patients.
Individuals below 12 years of age were excluded from vaccinations. MoHS teams determined on-site whether a person deemed ‘at risk’ (for example, pregnant or suffering from severe disease) would also be excluded. After the vaccine was administered, recipients were asked to remain in close proximity to the vaccination team for a minimum of 15 min in the event that they experienced any unexpected side effect.
Vaccine teams were compliant with MoHS requirements for the storage, preparation, administration and disposal of the vaccine and associated materials. They followed infection prevention and controls and checked the eligibility of people to be vaccinated using the patient checklist.
Mobile teams adhered to MoHS guidelines on informed consent to receive COVID-19 vaccination, ensuring it was taken only by people with the mental capacity to consent to the administration of the vaccines, and taken freely, voluntarily and without coercion. Participants were allowed to withdraw consent at any time.
All vaccine teams received training on vaccinations, including the management of adverse events following immunization. All such events had to be reported using national reporting systems to the MoHS.
Statistical analysis
To estimate the impact of the intervention on the adult vaccination rate (Extended Data Table 3 ), we estimated intent-to-treat effects using OLS on individual-level data as follows:
where Y i , j is the vaccination status of individual i , in village j , T pooled is the village assignment to either door-to-door or small-group treatment groups, α k is a vector of randomization block fixed effects (that is, triplet) and ϵ i , j are heteroscedasticity-robust standard errors clustered at the village level. We estimated effects using a linear estimator (OLS) that accounts for high dimensional fixed effects 49 . In additional analyses, we added to the right-hand side of this equation Y i , j ,bl , the baseline vaccination status, and X j , the vector of covariates that were unbalanced at baseline. We also estimated equation ( 1 ) at the village level and for each group, by estimating both β 1, j T door to door and β 2, j T small group for the door-to-door and small-group treatment groups, respectively (Extended Data Table 1 ).
To estimate the vaccination count (Extended Data Table 4 ), we estimated a village - level intent-to-treat effect using OLS on village-level data as follows:
where Y j is the number of people vaccinated in village j , T pooled is the village assignment to either door-to-door and small-group treatment groups, α k is a vector of randomization block fixed effects (that is, triplets) and ϵ j is the heteroscedasticity-robust standard error. We estimated equation ( 2 ) for several types of respondents. That is, those who were part of the village census, migrants, returnees and those not present during census, and those from other villages, and added X j , a vector of covariates that were unbalanced at baseline.
To assess the individual-level effect of the door-to-door campaign, we restricted our sample to the 50 villages assigned to the door-to-door campaign (that is, T door to door = 1), and estimated intent-to-treat effects using OLS as follows:
where Y i , s is the vaccination status of individual i in structure s (hut or house), T door to door is the individual-level assignment to receive a visit by the social mobilization team to a structure, α j is a vector of randomization block fixed effect (that is, the village) and μ i , s is the heteroscedasticity-robust standard error clustered at the structure level.
For the survey-based outcomes on COVID-19 vaccine knowledge and trust, we estimated equation ( 1 ), replacing the dependent variable with the survey responses described above, using the subsample of 45 villages where this dataset was collected and we had data on the full randomization blocks.
For our analysis of the treatment effects by subgroup, we estimated equation ( 1 ) separately for men, women, various age groups (18–24 years, 25–54 years and >55 years), and sample splits based on whether the household head had any schooling, owns any land or reduced portions of food. To test for differences across subgroups, we estimate equation ( 1 ) and interact the subgroup variable with treatment.
In the results presented in Extended Data Tables 6 and 7 , we also adjusted for the fact that we conducted multiple tests on the same dataset by implementing FDR corrections and report the FDR q values 50 . We also report the bootstrapped P value 51 to account for regressions with a small number of clusters.
Literature review of vaccination uptake RCT studies
We conducted a literature review of articles in PubMed published between 1 January 2000 and 7 January 2023 using the search terms ‘(vaccin*[Title/Abstract] OR immun*[Title/Abstract]) AND additional search term [Title/Abstract]) AND (Randomized Controlled Trial[Publication Type])’, with the following additional search terms: ‘access’; ‘community-based’; ‘cost effect*’; ‘demand’; ‘hesitant’; ‘incentive*’; ‘intervention*’; ‘mobile’; ‘nudge*’; ‘rural’; and ‘supply’. These searches returned 3,615 unique articles. We screened out articles that were not related to vaccine uptake or that did not use a RCT, which reduced the sample to 141 articles. We appended a further 20 relevant studies that were identified by snowballing and rejected 17 papers that did not have a control group, did not report the percentage-point change in vaccine uptake or did not include a test statistic. The final list of 144 articles comprises 234 distinct interventions for which we can report a percentage-point change relative to a control group (Supplementary Table 2 ). Of these, 33 interventions (14%) reported information about the cost of the intervention per vaccine administered. This cost specifically refers to the cost of implementing the intervention and does not include the cost of the vaccine itself. Studies that did not unequivocally state the cost of the intervention per vaccinated person were not included in our cost-effectiveness comparisons. Two studies reported the cost in currencies other than US dollars 52 , 53 , and these costs were converted to the US dollar equivalent for the year the study was published, using exchange rate data from the respective countries’ national statistics agencies. We did not analyse publication bias.
Deviations from pre-registered hypotheses
We pre-registered our research protocol and hypotheses at the ISRCTN registry (study ISRCTN17878735 ).
We report on our main hypothesis in Fig. 2 and Extended Data Table 3 . In addition to reporting on our main pre-registered outcome (adult vaccination rate), we also report on the total immunizations given per vaccination site because many more people showed up to our temporary clinics from neighbouring villages or were not present during the pre-intervention census, and we had not anticipated this. Figure 3 and Extended Data Table 4 therefore report on the count of all individuals (aged 12 years and above) who visited our clinics to receive a vaccination. This metric is necessary to correctly compute the cost-effectiveness.
The heterogeneity analysis reported in Fig. 5 , in which we analysed whether vaccination rates differ by age, sex, schooling and wealth variables, was not pre-specified and followed heterogeneity tests that are common in the vaccine literature 54 .
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.

Data availability
The primary survey data forming part of this study were collected using SurveyCTO software (v.2.81). These de-identified datasets are available in the Harvard Dataverse at https://doi.org/10.7910/DVN/PRXF5Z .
Code availability
All analysis for this paper was conducted using Stata SE 17. Replication files and de-identified data are available in the Harvard Dataverse at https://doi.org/10.7910/DVN/PRXF5Z .
Mathieu, E. et al. Coronavirus (COVID-19) vaccinations. Our World in Data https://ourworldindata.org/covid-vaccinations (2020).
Mobarak, A. M. et al. End COVID-19 in low-and middle-income countries. Science 375 , 1105–1110 (2022).
Article ADS PubMed Google Scholar
Partapuri, T., Steinglass, R. & Sequeira, J. Integrated delivery of health services during outreach visits: a literature review of program experience through a routine immunization lens. J. Infect. Dis. 205 , S20–S27 (2012).
Article PubMed PubMed Central Google Scholar
Egger, D. et al. Falling living standards during the COVID-19 crisis: quantitative evidence from nine developing countries. Sci. Adv. 7 , eabe0997 (2021).
Article ADS CAS PubMed PubMed Central Google Scholar
Oehler, R. L. & Vega, V. R. Worldwide vaccine inequality threatens to unleash the next COVID-19 variant. Int. J. Infect. Dis. 123 , 133–135 (2022).
Solís Arce, J. S. et al. COVID-19 vaccine acceptance and hesitancy in low-and middle-income countries. Nat. Med. 27 , 1385–1394 (2021).
DataBank, World Development Indicators (The World Bank, accessed 1 December 2023); https://databank.worldbank.org/source/world-development-indicators .
Asadullah, M. N., Savoia, A. & Mahmud, W. Paths to development: is there a Bangladesh surprise? World Develop. 62 , 138–154 (2014).
Article Google Scholar
Global Biopharma CEO/Top Executives COVID-19 Media Briefing . IFPMA (7 September 2021); https://www.youtube.com/watch?v=qA7oos7sU8Y .
Ye, Y. et al. Equitable access to COVID-19 vaccines makes a life-saving difference to all countries. Nat. Hum. Behav. 6 , 207–216 (2022).
Ramachandran, R., Ross, J. S. & Miller, J. E. Access to COVID-19 vaccines in high-, middle-, and low-income countries hosting clinical trials. JAMA Netw. Open 4 , e2134233 (2021).
Kulle, A.-C., Schumacher, S. & von Bieberstein, F. Mobile vaccination units substantially increase COVID-19 vaccinations: evidence from a randomized controlled trial. J. Public Health https://doi.org/10.1093/pubmed/fdad213 (2023).
Sharma, M., Ying, R., Tarr, G. & Barnabas, R. Systematic review and meta-analysis of community and facility-based HIV testing to address linkage to care gaps in sub-Saharan Africa. Nature 528 , S77–S85 (2015).
Mobarak, A. M. & Saldanha, N. A. Remove barriers to technology adoption for people in poverty. Nat. Hum. Behav. 6 , 480–482 (2022).
Article PubMed Google Scholar
Chater, N. & Loewenstein, G. The i-frame and the s-frame: How focusing on the individual-level solutions has led behavioral public policy astray. Behav. Brain Sci. 46 , e147 (2022).
Ateudjieu, J. et al. Tracking demographic movements and immunization status to improve children’s access to immunization: field-based randomized controlled trial. JMIR Public Health Surveill. 8 , e32213 (2022).
Sengupta, P. et al. Evaluation of a community-based intervention to improve routine childhood vaccination uptake among migrants in urban slums of Ludhiana, India. J. Public Health 39 , 805–812 (2017).
Habib, M. A. et al. Community engagement and integrated health and polio immunisation campaigns in conflict-affected areas of Pakistan: a cluster randomised controlled trial. Lancet Global Health 5 , e593–e603 (2017).
Usman, H. R. et al. Randomized controlled trial to improve childhood immunization adherence in rural Pakistan: redesigned immunization card and maternal education. Trop. Med. Int. Health 16 , 334–342 (2011).
Andersson, N. et al. Evidence-based discussion increases childhood vaccination uptake: a randomised cluster controlled trial of knowledge translation in Pakistan. BMC Int. Health Hum. Rights 9 , S8 (2009).
Campos-Mercade, P. et al. Monetary incentives increase COVID-19 vaccinations. Science 374 , 879–882 (2021).
Chang, T., Jacobson, M., Shah, M., Pramanik, R. & Shah, S. B. Financial Incentives and Other Nudges do not Increase COVID-19 Vaccinations Among the Vaccine Hesitant. National Bureau of Economic Research (October 2021); https://www.nber.org/papers/w29403 .
Milkman, K. L. et al. A citywide experiment testing the impact of geographically targeted, high-pay-off vaccine lotteries. Nat. Hum. Behav. 6 , 1515–1524 (2022).
Lang, D., Esbenshade, L. & Willer, R. Did Ohio’s vaccine lottery increase vaccination rates? A pre-registered, synthetic control study. J. Exp. Pol. Sci. https://doi.org/10.1017/XPS.2021.32 (2022).
Dai, H. et al. Behavioural nudges increase COVID-19 vaccinations. Nature 597 , 404–409 (2021).
Rabb, N. et al. Evidence from a statewide vaccination RCT shows the limits of nudges. Nature 604 , 404–409 (2022).
Tentori, K. et al. Nudging covid-19 vaccine uptake by changing the default: a randomized controlled trial. Med. Decis. Mak. 42 , 837–841 (2022).
Banerjee, A. V., Duflo, E., Glennerster, R. & Kothari, D. Improving immunisation coverage in rural India: clustered randomised controlled evaluation of immunisation campaigns with and without incentives. BMJ 340 , c2220 (2010).
Lugada, E. et al. Rapid implementation of an integrated large-scale HIV counseling and testing, malaria, and diarrhea prevention campaign in rural kenya. PLOS ONE 5 , e12435 (2010).
Article ADS PubMed PubMed Central Google Scholar
Islam, S., Islam, T. & Islam, M. R. New coronavirus variants are creating more challenges to global healthcare system: a brief report on the current knowledge. Clin. Pathol. https://doi.org/10.1177/2632010X221075 (2022).
Dini, E. F., Linkins, R. W. & Sigafoos, J. The impact of computer-generated messages on childhood immunization coverage. Am. J. Prev. Med. 18 , 132–139 (2000).
Krieger, J. W., Castorina, J. S., Walls, M. L., Weaver, M. R. & Ciske, S. Increasing influenza and pneumococcal immunization rates: a randomized controlled study of a senior center–based intervention. Am. J. Prev. Med. 18 , 123–131 (2000).
Winston, C. A., Mims, A. D. & Leatherwood, K. A. Increasing pneumococcal vaccination in managed care through telephone outreach. Am. J. Manag. Care 13 , 581–588 (2007).
Szilagyi, P. G. et al. Effectiveness of a citywide patient immunization navigator program on improving adolescent immunizations and preventive care visit rates. Arch. Pediatr. Adolesc. Med. 165 , 547–553 (2011).
Szilagyi, P. G. et al. A randomized trial of the effect of centralized reminder/recall on immunizations and preventive care visits for adolescents. Acad. Pediatr. 13 , 204–213 (2013).
O’Leary, S. T. et al. Effectiveness and cost of bidirectional text messaging for adolescent vaccines and well care. Pediatrics 136 , e1220–e1227 (2015).
Busso, M, Cristia, J. & Humpage, S. Did you get your shots? Experimental evidence on the role of reminders. J. Health Econ. 44 , 226–237 (2015).
Yoo, B.-K. et al. Cost effectiveness analysis of Year 2 of an elementary school-located influenza vaccination program–Results from a randomized controlled trial. BMC Health Serv. Res. 15 , 511 (2015).
Herrett, E. et al. Text messaging reminders for influenza vaccine in primary care: a cluster randomised controlled trial (TXT4FLUJAB). BMJ Open 6 , e010069 (2016).
Regan, A. K., Bloomfield, L., Peters, I. & Effler, P. V. Randomized controlled trial of text message reminders for increasing influenza vaccination. Ann. Fam. Med. 15 , 507–514 (2017).
Kempe, A. et al. Centralized reminder/recall to increase immunization rates in young children: how much bang for the buck? Acad. Pediatr. 17 , 330–338 (2017).
Hurley, L. P. et al. RCT of centralized vaccine reminder/recall for adults. Am. J. Prev. Med. 55 , 231–239 (2018).
Yokum, D., Lauffenburger, J. C., Ghazinouri, R. & Choudhry, N. K. Letters designed with behavioural science increase influenza vaccination in Medicare beneficiaries. Nat. Hum. Behav. 2 , 743–749 (2018).
Powell-Jackson, T., Fabbri, C., Dutt, V., Tougher, S. & Singh, K. Effect and cost-effectiveness of educating mothers about childhood DPT vaccination on immunisation uptake, knowledge, and perceptions in Uttar Pradesh, India: a randomised controlled trial. PLOS Med. 15 , e1002519 (2018).
Szilagyi, P. et al. Effect of state immunization information system centralized reminder and recall on HPV vaccination rates. Pediatrics 145 , e20192689 (2020).
Yue, M., Wang, Y., Low, C. K., Yoong, J. S.-Y. & Cook, A. R. Optimal design of population-level financial incentives of influenza vaccination for the elderly. Value Health 23 , 200–208 (2020).
Kawakatsu, Y., Oyeniyi Adesina, A., Kadoi, N. & Aiga, H. Cost-effectiveness of SMS appointment reminders in increasing vaccination uptake in Lagos, Nigeria: a multi-centered randomized controlled trial. Vaccine 38 , 6600–6608 (2020).
Gurfinkel, D. et al. Centralized reminder/recall for human papillomavirus vaccination: findings from two states—A randomized clinical trial. J. Adolesc. Health 69 , 579–587 (2021).
Correia, S. REGHDFE: Stata module to perform linear or instrumental-variable regression absorbing any number of high-dimensional fixed effects. Statistical Software Components S457874, Boston College Department of Economics https://ideas.repec.org/c/boc/bocode/s457874.html (2017).
Anderson, M. L. Multiple inference and gender differences in the effects of early intervention: a reevaluation of the Abecedarian, Perry Preschool, and Early Training projects. J. Am. Stat. Assoc. 103 , 1481–1495 (2008).
Article MathSciNet CAS Google Scholar
Cameron, A. C., Gelbach, J. B. & Miller, D. L. Bootstrap-based improvements for inference with clustered errors. Rev. Econ. Stat. 90 , 414–427 (2008).
Yue, M. et al. Optimal design of population-level financial incentives of influenza vaccination for the elderly. Value Health 23 , 200–208 (2020).
Lazarus, J. V. et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 27 , 225–228 (2021).
Article CAS PubMed Google Scholar
Download references
Acknowledgements
Funding support for this research was provided by Weiss Asset Management, the Dutch Research Council (NWO) (VI.Vidi.191.154), UKRI and the International Growth Centre (SLE - 21148). We are indebted and thankful to study participants for giving their time; O. Sawaneh, A. Turray and our team of enumerators for excellent research assistance; J. W. Ansumana, A. K. Kemoh, N. S. Kamara, T. Boima and the wider team the MoHS of the Government of Sierra Leone; the district organization officers for the districts we went to (A. S. Conteh, A. Sesay, J. Kalokoh, M. Sesay, L. Mansaray, I. Bangura, D. Kanu and A. D. D. Sesay); and the team at Concern Worldwide, Yale Research Initiative on Innovation and Scale (Y-RISE) and the International Growth Centre.
Author information
Authors and affiliations.
International Growth Centre, Freetown, Sierra Leone
Niccolò F. Meriggi
Wageningen University and Research, Wageningen, The Netherlands
Niccolò F. Meriggi, Maarten Voors, Michael Rozelle, Ella Tyler, Sellu Kallon & Junisa Nabieu
Centre for the Study of African Economies, Department of Economics, University of Oxford, Oxford, UK
University of Illinois, Urbana, IL, USA
Madison Levine
Boston University, Boston, MA, USA
Vasudha Ramakrishna
Ministry of Health and Sanitation, Freetown, Sierra Leone
Desmond Maada Kangbai
University of Sierra Leone, Freetown, Sierra Leone
Sellu Kallon
Concern Worldwide, Freetown, Sierra Leone
Sarah Cundy
Yale University and Y-RISE, New Haven, CT, USA
Ahmed Mushfiq Mobarak
You can also search for this author in PubMed Google Scholar
Contributions
N.F.M., A.M.M., M.V., S.C. and D.M.K. conceptualized the project. V.R. and M.L. curated the data. V.R., M.L., E.T., M.R. and M.V. undertook formal analyses. N.F.M., A.M.M. and M.V. acquired funding. N.F.M., M.L., M.R., S.C., S.K. and J.N. performed the investigations. N.F.M., A.M.M., M.V., V.R. and M.L. designed the methodology. N.F.M. and M.V. administrated the project. M.L., V.R., S.K., J.N. and M.R. supervised the work. All authors validated the findings. V.R., E.T., M.V. and M.R. visualized the data. A.M.M. and M.V. wrote the first draft, with all authors contributing to writing, and all authors contributed to the review and editing of the paper.
Corresponding authors
Correspondence to Niccolò F. Meriggi or Ahmed Mushfiq Mobarak .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Peer review
Peer review information.
Nature thanks Jake Bowers and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data figures and tables
Supplementary information, supplementary information, reporting summary, peer review file, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Meriggi, N.F., Voors, M., Levine, M. et al. Last-mile delivery increases vaccine uptake in Sierra Leone. Nature 627 , 612–619 (2024). https://doi.org/10.1038/s41586-024-07158-w
Download citation
Received : 13 September 2022
Accepted : 01 February 2024
Published : 13 March 2024
Issue Date : 21 March 2024
DOI : https://doi.org/10.1038/s41586-024-07158-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Mobile delivery of covid-19 vaccines improved uptake in rural sierra leone.
- Alison Buttenheim
- Harsha Thirumurthy
Nature (2024)
Massive public-health experiment sends vaccination rates soaring
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Sierra Leone Receives Additional Support for Access and Effective Vaccines Deployment
WASHINGTON, June 8, 2021 — The World Bank approved an $8.5 million grant in additional financing to support affordable and equitable access to COVID-19 vaccines in Sierra Leone. The funds will provide upfront financing to help purchase and deploy coronavirus vaccines, and to strengthen relevant health systems necessary for a successful deployment and to prepare for future pandemic outbreaks.
The additional resources will also support the costs of expanding activities of the parent project— Sierra Leone COVID-19 Emergency Preparedness and Response Project —under the Coronavirus disease Strategic Preparedness and Response Program. It will complement the resources from the COVID-19 Vaccines Global Access (COVAX) Advanced Market Commitment (AMC) Facility to jointly vaccinate close to a quarter of the country’s population by the end of 2021.
“These additional funds present an opportunity for us as a Government to strengthen our response to the pandemic, and to broaden the implementation of the Coronavirus vaccine rollout,” said Hon. Austin Demby, Minister of Health and Sanitation for Sierra Leone . “Now the work of translating available funds into vaccinations and COVID-19 prevention and care activities go into high gear. As a Ministry, we continue to look forward to our strong collaboration with the World Bank as we collectively work to improve health outcomes for the people of Sierra Leone.”
The Sierra Leone COVID-19 Emergency Preparedness and Response Project was approved by the World Bank on April 2, 2020, filling critical financing gaps identified due to the new emergency preparedness and response needs created by the global pandemic. The first $7.5 million International Development Association (IDA) grant was to help strengthen Sierra Leone’s response to the outbreak and further reinforce national systems for public health preparedness.
“Given the importance of limiting the spread of COVID-19 to improve health outcomes and support economic recovery, providing access to vaccines will be crucial to accelerate economic and social recovery for Sierra Leone,” said Gayle Martin, World Bank Country Manager for Sierra Leone . “This additional financing comes at a critical time and will respond to critical needs for financing the COVID-19 vaccine deployment to scale up and build on ongoing efforts for health systems strengthening in the country.”
The project has significantly contributed to reducing the case fatality rate from 6% in May 2020 to 2.1% in February 2021 by strengthening health systems. It procured an assortment of essential local drugs needed to treat COVID-19 patients, and continues to support the strengthening of the country’s laboratory systems with the provision of vital laboratory supplies to all designated laboratories across the country. Furthermore, it has helped improve electronic data reporting with over 90% of routine data collected at district level on District Health Information Software (DHIS2).
The project also procured quantities of essential medicines, equipment, PPEs, testing kits, and consumables. Sierra Leone now has the capacity to perform rapid COVID-19 testing, with results being declared within 72 hours of taking samples. A functional grievance redress system was established with a significant number of reported cases resolved.
The World Bank , one of the largest sources of funding and knowledge for developing countries, is taking broad, fast action to help developing countries respond to the health, social and economic impacts of COVID-19. This includes $12 billion to help low- and middle-income countries purchase and distribute COVID-19 vaccines, tests, and treatments, and strengthen vaccination systems. The financing builds on the broader World Bank Group COVID-19 response , which is helping more than 100 countries strengthen health systems, support the poorest households, and create supportive conditions to maintain livelihoods and jobs for those hit hardest.
Sierra Leone
- Sierra Leone COVID-19 Emergency Preparedness and Response Project
- The World Bank in Sierra Leone
- The World Bank in Africa

How to get vaccines to remote areas? In Sierra Leone they’re delivered by foot, boat or motorbike
Postdoctoral Research Fellow, University of Oxford
Disclosure statement
Niccolò Francesco Meriggi receives funding from Weiss Asset Management, UKRI and the International Growth Centre.
University of Oxford provides funding as a member of The Conversation UK.
View all partners
In Sierra Leone almost 59% of the population live in remote, rural areas. Roads may be non-existent or in bad condition, making it very difficult for rural dwellers to access healthcare. This is one of the key reasons why COVID-19 vaccination rates in the country are low.
During an innovative vaccine programme mobile vaccine clinics were dispatched to the furthest parts of the country, sometimes on motorcycles and boats. The results showed COVID-19 vaccination rates tripled in three days.
Development Economist Niccolò F. Meriggi tells Nadine Dreyer about the programme’s potential to become a blueprint for future healthcare delivery in the country and other remote regions in Africa.
Why are vaccination rates low in Sierra Leone?
By 10 March 2022, more than a year after COVID-19 vaccines arrived on the market, 80% of people living in high-income countries had received at least one dose. In stark contrast, only 15% of people had been vaccinated in low-income countries.
Fast-forward to November 2023 and still only 33% of the population in Africa had received at least their first dose of a COVID-19 vaccine.
The hardships Sierra Leoneans face are typical of the obstacles people in low-income countries have to overcome to access healthcare.
In the early days of the COVID-19 vaccination campaign in Sierra Leone, it took the average Sierra Leonean living in a rural community three-and-a-half hours each way to the nearest vaccination centre.
Things improved as more clinics started offering the vaccine, but the cost of reaching clinics remained high and, in many cases, prohibitive. In Sierra Leone 60% of the rural population live on less than US$1.25 a day. Getting to a clinic would cost more than one week’s wages.

How did this vaccine drive tackle the problem?
A team of researchers designed a COVID-19 vaccination drive that was implemented in March and April 2022 by the Ministry of Health and Sanitation and their technical partner Concern World Wide, an international humanitarian agency.
The primary aim of this intervention was to take vaccine doses and nurses to administer vaccines to remote, rural communities, preceded by seeking permission and community mobilisation.
At the time, only 6% to 9% of the adults who took part in the programme were already immunised.
Just over 20,000 Sierra Leoneans, living in 150 rural towns outside the country’s national clinic network, took part in the vaccination campaign.
The first step was to approach village leaders including the chief and the mammy queen, the most important woman in the village. Youth and religious leaders were also consulted. They were briefed about the purpose of the visit and the vaccination team answered questions about the available vaccines.
The leaders were asked for their cooperation in encouraging eligible community members to take the COVID-19 vaccine.
That evening, when labourers returned home from farms, the health team talked directly to all villagers about vaccine efficacy and safety and the importance of getting vaccinated. They also addressed villagers’ questions and concerns.
Finally, vaccine doses and healthcare workers arrived at the villages to administer the doses. Some travelled on motorbikes or on boats because of the lack of any road access.
This last-mile vaccine intervention tripled vaccination rates within three days in treated communities.

Large numbers of people from neighbouring communities also showed up to receive vaccines at the temporary vaccination sites.
Looking forward
These results suggest that people who live far from clinics are less likely to seek healthcare and that last mile delivery is a cost-effective intervention capable of overcoming that problem.
The intervention cost in this campaign was US$33 per person vaccinated. This approach proved 76% more cost-effective than other vaccination campaigns.
Transport accounted for a large share of the costs, so the cost-effectiveness of last mile delivery can be increased by offering a “bundle” of health products. The bundle could include routine child immunisation, as well as human papillomavirus and malaria vaccines, combined with other important health supplies such as deworming tablets, vitamin A supplements, oral rehydration solutions and chlorine for drinking water.
The World Health Organization reported that between 2020 and 2021, 5.42 million people died of COVID-19.
Other estimates put the death toll for the same period at 14.83 million , which is 2.74 times higher.
Developing cost-effective strategies to make vaccines easily accessible to everyone, everywhere, is the most promising solution to prevent future pandemics. This blueprint could also be used to address obstacles to other life-saving medical care.
The research team has since been awarded funds from the International Growth Centre and the Social Science Research Council through its Mercury Project. These grants will be used to expand the model in this paper to a bundle of health products and services, including additional vaccines (HPV and Malaria) and maternal and child health interventions, and further explore its feasibility and cost-effectiveness
- Sierra Leone
- COVID-19 vaccination
- Health challenges Africa

Chief Operating Officer (COO)

Technical Assistant - Metabolomics

Data Manager

Director, Social Policy

Head, School of Psychology
- Skip to main content
- Skip to "About this site"
Language selection
Search travel.gc.ca.
Help us to improve our website. Take our survey !
COVID-19: travel health notice for all travellers
Sierra Leone travel advice
Latest updates: Editorial change
Last updated: May 23, 2024 08:00 ET
On this page
Safety and security, entry and exit requirements, laws and culture, natural disasters and climate, sierra leone - exercise a high degree of caution.
Exercise a high degree of caution in Sierra Leone due to crime.
Back to top
Political situation
The political situation in the country remains tense since the June 2023 elections.
On November 26, 2023, there were violent clashes between security forces and armed groups in Freetown.
The political situation remains volatile. Further clashes or civil unrest cannot be ruled out.
Border areas
Be vigilant in border areas. The area bordering Liberia has been highly unstable in the past. There is a high level of trans-border military, militia and criminal activity in the border area with Guinea.
Crime occurs throughout the country.
Pickpocketing and purse snatching frequently occur in the main cities.
Armed robberies, carjackings and residential burglaries have occurred in foreigners’ homes. Burglars do not hesitate to use violence. There is a heightened risk of serious crime after dark.
- Avoid walking alone, particularly at night
- Don’t display any signs of affluence in public
- Don’t leave your valuables or bags unattended
Demonstrations
Demonstrations occur occasionally. Even peaceful demonstrations can turn violent at any time. They can also lead to disruptions to traffic and public transportation.
- Avoid areas where demonstrations and large gatherings are taking place
- Follow the instructions of local authorities
- Monitor local media for information on ongoing demonstrations
There have been commercial and Internet fraud attempts through email originating from Sierra Leone.
Overseas fraud
Tourist facilities
Tourist facilities are extremely limited. When possible, check the level of security at hotels, lodges or any other type of accommodation before booking your stay.
Plan carefully any travel outside the capital. In remote regions, tourist facilities are almost non-existent.
Certain essential services are lacking, and water and gas shortages occur from time to time.
You should always maintain sufficient supplies of food, water and other essentials.
Telecommunications
Telecommunications can be unreliable, particularly in remote areas.
Public transportation
Local transportation services between Freetown (or Lungi) International Airport and Freetown are available by:
None of those options is risk-free. You should plan to land early enough in the day so that you can arrive at your destination before nightfall. Arrange for transportation prior to arrival.
Public transportation (bus or group taxis) is poorly maintained and generally unsafe.
Road safety
Other than the main roads, from Freetown to Makeni or to Bo, roads are in poor condition and rarely paved outside Freetown.
Road conditions deteriorate significantly during the rainy season.
You should only undertake land travel outside Freetown in a four-wheel-drive vehicle. You should rent a car with a hired driver, as overland travel can be hazardous.
You should not travel after dark, as it is particularly dangerous. There are no operating traffic lights, and most roads are unlit.
Poor driving habits, overloaded vehicles, pedestrians and roaming animals pose a hazard.
You may encounter difficulties at roadblocks and checkpoints, including requests for payments.
We do not make assessments on the compliance of foreign domestic airlines with international safety standards.
Information about foreign domestic airlines
Every country or territory decides who can enter or exit through its borders. The Government of Canada cannot intervene on your behalf if you do not meet your destination’s entry or exit requirements.
We have obtained the information on this page from the Sierra Leonean authorities. It can, however, change at any time.
Verify this information with the Foreign Representatives in Canada .
Entry requirements vary depending on the type of passport you use for travel.
Before you travel, check with your transportation company about passport requirements. Its rules on passport validity may be more stringent than the country’s entry rules.
Regular Canadian passport
Your passport must be valid upon entry.
Passport for official travel
Different entry rules may apply.
Official travel
Passport with “X” gender identifier
While the Government of Canada issues passports with an “X” gender identifier, it cannot guarantee your entry or transit through other countries. You might face entry restrictions in countries that do not recognize the “X” gender identifier. Before you leave, check with the closest foreign representative for your destination.
Other travel documents
Different entry rules may apply when travelling with a temporary passport or an emergency travel document. Before you leave, check with the closest foreign representative for your destination.
Useful links
- Foreign Representatives in Canada
- Canadian passports
Tourist visa: required Business visa: required Student visa: required
eVisa application - Sierra Leone Immigration Service
Children and travel
Learn more about travelling with children .
Yellow fever
Learn about potential entry requirements related to yellow fever (vaccines section).
Relevant Travel Health Notices
- Global Measles Notice - 13 March, 2024
- COVID-19 and International Travel - 13 March, 2024
- Polio: Advice for travellers - 6 May, 2024
This section contains information on possible health risks and restrictions regularly found or ongoing in the destination. Follow this advice to lower your risk of becoming ill while travelling. Not all risks are listed below.
Consult a health care professional or visit a travel health clinic preferably 6 weeks before you travel to get personalized health advice and recommendations.
Routine vaccines
Be sure that your routine vaccinations , as per your province or territory , are up-to-date before travelling, regardless of your destination.
Some of these vaccinations include measles-mumps-rubella (MMR), diphtheria, tetanus, pertussis, polio, varicella (chickenpox), influenza and others.
Pre-travel vaccines and medications
You may be at risk for preventable diseases while travelling in this destination. Talk to a travel health professional about which medications or vaccines may be right for you, based on your destination and itinerary.
There is a risk of hepatitis A in this destination. It is a disease of the liver. People can get hepatitis A if they ingest contaminated food or water, eat foods prepared by an infectious person, or if they have close physical contact (such as oral-anal sex) with an infectious person, although casual contact among people does not spread the virus.
Practise safe food and water precautions and wash your hands often. Vaccination is recommended for all travellers to areas where hepatitis A is present.
Yellow fever is a disease caused by a flavivirus from the bite of an infected mosquito.
Travellers get vaccinated either because it is required to enter a country or because it is recommended for their protection.
- There is a risk of yellow fever in this country.
Country Entry Requirement*
- Proof of yellow fever vaccination for travellers from all countries.
Recommendation
- Vaccination is recommended.
- Contact a designated Yellow Fever Vaccination Centre well in advance of their trip to arrange for vaccination.
- Discuss travel plans, activities, and destinations with a health care professional.
- Protect yourself from mosquito bites .
About Yellow Fever
Yellow Fever Vaccination Centres in Canada * It is important to note that country entry requirements may not reflect your risk of yellow fever at your destination. It is recommended that you contact the nearest diplomatic or consular office of the destination(s) you will be visiting to verify any additional entry requirements.
Measles is a highly contagious viral disease. It can spread quickly from person to person by direct contact and through droplets in the air.
Anyone who is not protected against measles is at risk of being infected with it when travelling internationally.
Regardless of where you are going, talk to a health care professional before travelling to make sure you are fully protected against measles.
Hepatitis B is a risk in every destination. It is a viral liver disease that is easily transmitted from one person to another through exposure to blood and body fluids containing the hepatitis B virus. Travellers who may be exposed to blood or other bodily fluids (e.g., through sexual contact, medical treatment, sharing needles, tattooing, acupuncture or occupational exposure) are at higher risk of getting hepatitis B.
Hepatitis B vaccination is recommended for all travellers. Prevent hepatitis B infection by practicing safe sex, only using new and sterile drug equipment, and only getting tattoos and piercings in settings that follow public health regulations and standards.
Malaria is a serious and sometimes fatal disease that is caused by parasites spread through the bites of mosquitoes.
Malaria is a risk to travellers to this destination. Antimalarial medication is recommended for most travellers to this destination and should be taken as recommended. Consult a health care professional or visit a travel health clinic before travelling to discuss your options. It is recommended to do this 6 weeks before travel, however, it is still a good idea any time before leaving. Protect yourself from mosquito bites at all times:
- Cover your skin and use an approved insect repellent on uncovered skin.
- Exclude mosquitoes from your living area with screening and/or closed, well-sealed doors and windows.
- Use insecticide-treated bed nets if mosquitoes cannot be excluded from your living area.
- Wear permethrin-treated clothing.
If you develop symptoms similar to malaria when you are travelling or up to a year after you return home, see a health care professional immediately. Tell them where you have been travelling or living.
In this destination, rabies is commonly carried by dogs and some wildlife, including bats. Rabies is a deadly disease that spreads to humans primarily through bites or scratches from an infected animal. While travelling, take precautions , including keeping your distance from animals (including free-roaming dogs), and closely supervising children.
If you are bitten or scratched by a dog or other animal while travelling, immediately wash the wound with soap and clean water and see a health care professional. In this destination, rabies treatment may be limited or may not be available, therefore you may need to return to Canada for treatment.
Before travel, discuss rabies vaccination with a health care professional. It may be recommended for travellers who are at high risk of exposure (e.g., occupational risk such as veterinarians and wildlife workers, children, adventure travellers and spelunkers, and others in close contact with animals).
Polio (poliomyelitis) is an infectious disease that can be prevented by vaccination. It is caused by poliovirus type 1, 2 or 3. Circulating vaccine-derived poliovirus 2 (cVDPV2) is present in this country. Polio is spread from person to person and through contaminated food and water. Infection with the polio virus can cause paralysis and death in individuals of any age who are not immune.
Recommendations:
- Be sure that your polio vaccinations are up to date before travelling. Polio is part of the routine vaccine schedule for children in Canada.
- One booster dose of the polio vaccine is recommended as an adult .
Coronavirus disease (COVID-19) is an infectious viral disease. It can spread from person to person by direct contact and through droplets in the air.
It is recommended that all eligible travellers complete a COVID-19 vaccine series along with any additional recommended doses in Canada before travelling. Evidence shows that vaccines are very effective at preventing severe illness, hospitalization and death from COVID-19. While vaccination provides better protection against serious illness, you may still be at risk of infection from the virus that causes COVID-19. Anyone who has not completed a vaccine series is at increased risk of being infected with the virus that causes COVID-19 and is at greater risk for severe disease when travelling internationally.
Before travelling, verify your destination’s COVID-19 vaccination entry/exit requirements. Regardless of where you are going, talk to a health care professional before travelling to make sure you are adequately protected against COVID-19.
Safe food and water precautions
Many illnesses can be caused by eating food or drinking beverages contaminated by bacteria, parasites, toxins, or viruses, or by swimming or bathing in contaminated water.
- Learn more about food and water precautions to take to avoid getting sick by visiting our eat and drink safely abroad page. Remember: Boil it, cook it, peel it, or leave it!
- Avoid getting water into your eyes, mouth or nose when swimming or participating in activities in freshwater (streams, canals, lakes), particularly after flooding or heavy rain. Water may look clean but could still be polluted or contaminated.
- Avoid inhaling or swallowing water while bathing, showering, or swimming in pools or hot tubs.
Cholera is a risk in parts of this country. Most travellers are at very low risk.
To protect against cholera, all travellers should practise safe food and water precautions .
Travellers at higher risk of getting cholera include those:
- visiting, working or living in areas with limited access to safe food, water and proper sanitation
- visiting areas where outbreaks are occurring
Vaccination may be recommended for high-risk travellers, and should be discussed with a health care professional.
Travellers' diarrhea is the most common illness affecting travellers. It is spread from eating or drinking contaminated food or water.
Risk of developing travellers' diarrhea increases when travelling in regions with poor standards of hygiene and sanitation. Practise safe food and water precautions.
The most important treatment for travellers' diarrhea is rehydration (drinking lots of fluids). Carry oral rehydration salts when travelling.
Typhoid is a bacterial infection spread by contaminated food or water. Risk is higher among children, travellers going to rural areas, travellers visiting friends and relatives or those travelling for a long period of time.
Travellers visiting regions with a risk of typhoid, especially those exposed to places with poor sanitation, should speak to a health care professional about vaccination.
There is a risk of schistosomiasis in this destination. Schistosomiasis is a parasitic disease caused by tiny worms (blood flukes) which can be found in freshwater (lakes, rivers, ponds, and wetlands). The worms can break the skin, and their eggs can cause stomach pain, diarrhea, flu-like symptoms, or urinary problems. Schistosomiasis mostly affects underdeveloped and r ural communities, particularly agricultural and fishing communities.
Most travellers are at low risk. Travellers should avoid contact with untreated freshwater such as lakes, rivers, and ponds (e.g., swimming, bathing, wading, ingesting). There is no vaccine or medication available to prevent infection.
Insect bite prevention
Many diseases are spread by the bites of infected insects such as mosquitoes, ticks, fleas or flies. When travelling to areas where infected insects may be present:
- Use insect repellent (bug spray) on exposed skin
- Cover up with light-coloured, loose clothes made of tightly woven materials such as nylon or polyester
- Minimize exposure to insects
- Use mosquito netting when sleeping outdoors or in buildings that are not fully enclosed
To learn more about how you can reduce your risk of infection and disease caused by bites, both at home and abroad, visit our insect bite prevention page.
Find out what types of insects are present where you’re travelling, when they’re most active, and the symptoms of the diseases they spread.
There is a risk of chikungunya in this country. The risk may vary between regions of a country. Chikungunya is a virus spread through the bite of an infected mosquito. Chikungunya can cause a viral disease that typically causes fever and pain in the joints. In some cases, the joint pain can be severe and last for months or years.
Protect yourself from mosquito bites at all times. There is no vaccine available for chikungunya.
- In this country, risk of dengue is sporadic. It is a viral disease spread to humans by mosquito bites.
- Dengue can cause flu-like symptoms. In some cases, it can lead to severe dengue, which can be fatal.
- The level of risk of dengue changes seasonally, and varies from year to year. The level of risk also varies between regions in a country and can depend on the elevation in the region.
- Mosquitoes carrying dengue typically bite during the daytime, particularly around sunrise and sunset.
- Protect yourself from mosquito bites . There is no vaccine or medication that protects against dengue fever.
Animal precautions
Some infections, such as rabies and influenza, can be shared between humans and animals. Certain types of activities may increase your chance of contact with animals, such as travelling in rural or forested areas, camping, hiking, and visiting wet markets (places where live animals are slaughtered and sold) or caves.
Travellers are cautioned to avoid contact with animals, including dogs, livestock (pigs, cows), monkeys, snakes, rodents, birds, and bats, and to avoid eating undercooked wild game.
Closely supervise children, as they are more likely to come in contact with animals.
Lassa fever is a risk in this country.
Lassa fever is caused by a virus carried by rodents. Humans get sick when they inhale or come into close contact with feces, saliva, or urine of infected rodents or the blood or bodily fluids of infected humans.
Lassa virus can be very serious. Avoid rodents and rodent-infested areas.
Mpox (monkeypox) is a risk in this country. It is a viral disease that can cause serious illness in some circumstances. Risk is generally low for most travellers.
Mpox spreads in 3 ways:
- from animals to humans through direct contact or by eating or preparing undercooked meat of infected animals or coming into contact with an infected animal's body fluids
- from person to person through close contact, including direct contact with the skin lesions, blood, body fluids, or mucosal surfaces (such as eyes, mouth, throat, genitalia, anus, or rectum) of an infected person
- through direct contact with contaminated objects such as bedding and towels, or by sharing personal objects used by an infected person
Follow recommended public health measures and avoid contact with animals such as rodents and primates to help prevent getting or spreading the infection.
Person-to-person infections
Stay home if you’re sick and practise proper cough and sneeze etiquette , which includes coughing or sneezing into a tissue or the bend of your arm, not your hand. Reduce your risk of colds, the flu and other illnesses by:
- washing your hands often
- avoiding or limiting the amount of time spent in closed spaces, crowded places, or at large-scale events (concerts, sporting events, rallies)
- avoiding close physical contact with people who may be showing symptoms of illness
Sexually transmitted infections (STIs) , HIV , and mpox are spread through blood and bodily fluids; use condoms, practise safe sex, and limit your number of sexual partners. Check with your local public health authority pre-travel to determine your eligibility for mpox vaccine.
Tuberculosis is an infection caused by bacteria and usually affects the lungs.
For most travellers the risk of tuberculosis is low.
Travellers who may be at high risk while travelling in regions with risk of tuberculosis should discuss pre- and post-travel options with a health care professional.
High-risk travellers include those visiting or working in prisons, refugee camps, homeless shelters, or hospitals, or travellers visiting friends and relatives.
HIV (Human Immunodeficiency Virus) is a virus that attacks and impairs the immune system, resulting in a chronic, progressive illness known as AIDS (Acquired Immunodeficiency Syndrome).
High risk activities include anything which puts you in contact with blood or body fluids, such as unprotected sex and exposure to unsterilized needles for medications or other substances (for example, steroids and drugs), tattooing, body-piercing or acupuncture.
Medical services and facilities
Medical facilities are extremely limited and only offer basic services.
Ambulance services are available, but access could be limited.
In the event of a serious illness or accident, medical evacuation will be necessary. Medical transport is very expensive and payment is often required up front.
Medicines are scarcely available.
Make sure you get travel insurance that includes coverage for medical evacuation and hospital stays.
Travel health and safety
You must abide by local laws.
Learn about what you should do and how we can help if you are arrested or detained abroad .
Precious metals
You need a licence, issued by the Ministry of Mines and Mineral Resources, to export precious minerals. This includes diamonds and gold.
Seek legal advice before engaging in commercial transactions involving precious minerals. Penalties for smuggling or illegally exporting diamonds include imprisonment.
Photography
Taking photographs of airports, government installations, official buildings and bridges is prohibited, and laws are strictly enforced. These areas may not be clearly marked or defined. If in doubt, do not take pictures.
2SLGBTQI+ travellers
The laws of Sierra Leone prohibit sexual acts between individuals of the same sex.
2SLGBTQI+ travellers should carefully consider the risks of travelling to Sierra Leone.
Travel and your sexual orientation, gender identity, gender expression and sex characteristics
Carry your identification and vehicular documentation with you.
You must carry an international driving permit.
International Driving Permit
Dual citizenship
Dual citizenship is legally recognized in Sierra Leone.
If you are a Canadian citizen, but also a citizen of Sierra Leone, our ability to offer you consular services may be limited while you're there. You may also be subject to different entry/exit requirements .
Travellers with dual citizenship
International Child Abduction
The Hague Convention on the Civil Aspects of International Child Abduction is an international treaty. It can help parents with the return of children who have been removed to or retained in certain countries in violation of custody rights. It does not apply between Canada and Sierra Leone.
If your child was wrongfully taken to, or is being held in Sierra Leone by an abducting parent:
- act as quickly as you can
- consult a lawyer in Canada and in Sierra Leone to explore all the legal options for the return of your child
- report the situation to the nearest Canadian government office abroad or to the Vulnerable Children’s Consular Unit at Global Affairs Canada by calling the Emergency Watch and Response Centre
If your child was removed from a country other than Canada, consult a lawyer to determine if The Hague Convention applies.
Be aware that Canadian consular officials cannot interfere in private legal matters or in another country’s judicial affairs.
- International Child Abduction: A Guidebook for Left-Behind Parents
- Travelling with children
- Canadian embassies and consulates by destination
- Emergency Watch and Response Centre
Dress and behaviour
You should respect religious and social traditions to avoid offending local sensitivities. Exercise common sense and discretion in dress and behaviour.
The currency is the leone (SLL).
The economy is cash-based and strict rules limit the import of foreign currency in the form of cash.
Credit and debit cards are not widely accepted.
There are very few ATMs in Freetown. You should exchange foreign currency at banks or official foreign exchange offices only. The U.S. dollar and the Euro are the best currencies for exchange.
Rainy seaon
The rainy season extends from May to November. Seasonal flooding can hamper overland travel and reduce the provision of essential services. Roads may become impassable due to mudslides and landslides.
- Monitor local media for the latest updates, including road conditions
- Stay away from flooded areas
- Monitor weather reports
- Follow instructions from local authorities, including evacuation orders
Local services
In case of emergency, dial:
- police: 112
- medical assistance: 999
- firefighters: 033 / 300 / 301
Consular assistance
Sierra Leone, Togo
For emergency consular assistance, call the High Commission of Canada in Ghana, in Accra, and follow the instructions. At any time, you may also contact the Emergency Watch and Response Centre in Ottawa.
The decision to travel is your choice and you are responsible for your personal safety abroad. We take the safety and security of Canadians abroad very seriously and provide credible and timely information in our Travel Advice to enable you to make well-informed decisions regarding your travel abroad.
The content on this page is provided for information only. While we make every effort to give you correct information, it is provided on an "as is" basis without warranty of any kind, expressed or implied. The Government of Canada does not assume responsibility and will not be liable for any damages in connection to the information provided.
If you need consular assistance while abroad, we will make every effort to help you. However, there may be constraints that will limit the ability of the Government of Canada to provide services.
Learn more about consular services .
Risk Levels
take normal security precautions.
Take similar precautions to those you would take in Canada.
Exercise a high degree of caution
There are certain safety and security concerns or the situation could change quickly. Be very cautious at all times, monitor local media and follow the instructions of local authorities.
IMPORTANT: The two levels below are official Government of Canada Travel Advisories and are issued when the safety and security of Canadians travelling or living in the country or region may be at risk.
Avoid non-essential travel
Your safety and security could be at risk. You should think about your need to travel to this country, territory or region based on family or business requirements, knowledge of or familiarity with the region, and other factors. If you are already there, think about whether you really need to be there. If you do not need to be there, you should think about leaving.
Avoid all travel
You should not travel to this country, territory or region. Your personal safety and security are at great risk. If you are already there, you should think about leaving if it is safe to do so.
You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.
- Section 2 - Interactions Between Travel Vaccines & Drugs
- Section 2 - Travelers’ Diarrhea
Yellow Fever Vaccine & Malaria Prevention Information, by Country
Cdc yellow book 2024.
Author(s): Mark Gershman, Rhett Stoney (Yellow Fever) Holly Biggs, Kathrine Tan (Malaria)
The following pages present country-specific information on yellow fever (YF) vaccine requirements and recommendations, and malaria transmission information and prevention recommendations. Country-specific maps are included to aid in interpreting the information. The information in this chapter was accurate at the time of publication; however, it is subject to change at any time due to changes in disease transmission or, in the case of YF, changing entry requirements for travelers. Updated information reflecting changes since publication can be found in the online version of this book and on the Centers for Disease Control and Prevention (CDC) Travelers’ Health website. Recommendations for prevention of other travel-associated illnesses can also be found on the CDC Travelers’ Health website .
Yellow Fever Vaccine
Entry requirements.
Entry requirements for proof of YF vaccination under the International Health Regulations (IHR) differ from CDC’s YF vaccination recommendations. Under the IHR, countries are permitted to establish YF vaccine entry requirements to prevent the importation and transmission of YF virus within their boundaries. Certain countries require proof of vaccination from travelers arriving from all countries ( Table 5-25 ); some countries require proof of vaccination only for travelers above a certain age coming from countries with risk for YF virus transmission. The World Health Organization (WHO) defines areas with risk for YF virus transmission as countries or areas where YF virus activity has been reported currently or in the past, and where vectors and animal reservoirs exist.
Unless issued a medical waiver by a yellow fever vaccine provider, travelers must comply with entry requirements for proof of vaccination against YF.
WHO publishes a list of YF vaccine country entry requirements and recommendations for international travelers approximately annually. But because entry requirements are subject to change at any time, health care professionals and travelers should refer to the online version of this book and the CDC Travelers’ Health website for any updates before departure.
CDC Recommendations
CDC’s YF vaccine recommendations are guidance intended to protect travelers from acquiring YF virus infections during international travel. These recommendations are based on a classification system for destination-specific risk for YF virus transmission: endemic, transitional, low potential for exposure, and no risk ( Table 2-08 ). CDC recommends YF vaccination for travel to areas classified as having endemic or transitional risk (Maps 5-10 and 5-11 ). Because of changes in YF virus circulation, however, recommendations can change; therefore, before departure, travelers and clinicians should check CDC’s destination pages for up-to-date YF vaccine information.
Duration of Protection
In 2015, the US Advisory Committee on Immunization Practices published a recommendation that 1 dose of YF vaccine provides long-lasting protection and is adequate for most travelers. The recommendation also identifies specific groups of travelers who should receive additional doses, and others for whom additional doses should be considered (see Sec. 5, Part 2, Ch. 26, Yellow Fever ). In July 2016, WHO officially amended the IHR to stipulate that a completed International Certificate of Vaccination or Prophylaxis is valid for the lifetime of the vaccinee, and YF vaccine booster doses are not necessary. Moreover, countries cannot require proof of revaccination (booster) against YF as a condition of entry, even if the traveler’s last vaccination was >10 years ago.
Ultimately, when deciding whether to vaccinate travelers, clinicians should take into account destination-specific risks for YF virus infection, and individual risk factors (e.g., age, immune status) for serious YF vaccine–associated adverse events, in the context of the entry requirements. See Sec. 5, Part 2, Ch. 26, Yellow Fever , for a full discussion of YF disease and vaccination guidance.
Table 2-08 Yellow fever (YF) vaccine recommendation categories 1
Malaria prevention.
The following recommendations to protect travelers from malaria were developed using the best available data from multiple sources. Countries are not required to submit malaria surveillance data to CDC. On an ongoing basis, CDC actively solicits data from multiple sources, including WHO (main and regional offices); national malaria control programs; international organizations; CDC overseas offices; US military; academic, research, and aid organizations; and the published scientific literature. The reliability and accuracy of those data are also assessed.
If the information is available, trends in malaria incidence and other data are considered in the context of malaria control activities within a given country or other mitigating factors (e.g., natural disasters, wars, the coronavirus disease 2019 pandemic) that can affect the ability to control malaria or accurately count and report it. Factors such as the volume of travel to that country and the number of acquired cases reported in the US surveillance system are also examined. In developing its recommendations, CDC considers areas within countries where malaria transmission occurs, substantial occurrences of antimalarial drug resistance, the proportions of species present, and the available malaria prophylaxis options.
Clinicians should use these recommendations in conjunction with an individual risk assessment and consider not only the destination but also the detailed itinerary, including specific cities, types of accommodations, season, and style of travel, as well as special health conditions (e.g., pregnancy). Several medications are available for malaria prophylaxis. When deciding which drug to use, consider the itinerary and length of trip, travelers’ previous adverse reactions to antimalarials, drug allergies, medical history, and drug costs. For a thorough discussion of malaria and guidance for prophylaxis, see Sec. 5, Part 3, Ch. 16, Malaria .
Sierra Leone
Entry requirements : Required for all arriving travelers.
CDC recommendations : Recommended for all travelers ≥9 months old.
- Chloroquine
- P. falciparum (primarily)
- P. malariae , P. ovale , and P. vivax (less commonly)
- Atovaquone-proguanil, doxycycline, mefloquine, tafenoquine 3
Other Vaccines to Consider
See Health Information for Travelers to Sierra Leone .
1 Current as of November 2022. This is an update of the 2010 map created by the Informal WHO Working Group on the Geographic Risk of Yellow Fever.
2 Refers to Plasmodium falciparum malaria, unless otherwise noted.
3 Tafenoquine can cause potentially life-threatening hemolysis in people with glucose-6-phosphate-dehydrogenase (G6PD) deficiency. Rule out G6PD deficiency with a quantitative laboratory test before prescribing tafenoquine to patients.
4 Mosquito avoidance includes applying topical mosquito repellant, sleeping under an insecticide-treated mosquito net, and wearing protective clothing (e.g., long pants and socks, long-sleeve shirt). For additional details on insect bite precautions, see Sec. 4, Ch. 6, Mosquitoes, Ticks & Other Arthropods.
5 Primaquine can cause potentially life-threatening hemolysis in people with G6PD deficiency. Rule out G6PD deficiency with a quantitative laboratory test before prescribing primaquine to patients.
6 P. knowlesi is a malaria species with a simian (macaque) host. Human cases have been reported from most countries in Southwest Asia and are associated with activities in forest or forest-fringe areas. P. knowlesi has no known resistance to antimalarials.
Yellow Fever Maps
2 In 2017, the Centers for Disease Control and Prevention (CDC) expanded its YF vaccination recommendations for travelers going to Brazil because of a large YF outbreak in multiple states in that country. Please refer to the CDC Travelers’ Health website for more information and updated recommendations.
3 YF vaccination is generally not recommended for travel to areas where the potential for YF virus exposure is low. Vaccination might be considered, however, for a small subset of travelers going to these areas who are at increased risk for exposure to YF virus due to prolonged travel, heavy exposure to mosquitoes, or inability to avoid mosquito bites. Factors to consider when deciding whether to vaccinate a traveler include destination-specific and travel-associated risks for YF virus infection; individual, underlying risk factors for having a serious YF vaccine–associated adverse event; and destination entry requirements.
The following authors contributed to the previous version of this chapter: Mark D. Gershman, Emily S. Jentes, Rhett J. Stoney (Yellow Fever) Kathrine R. Tan, Paul M. Arguin (Malaria)
File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.

Request an appointment
Vaccinations for sierra leone.

Yellow Fever is a viral disease transmitted by mosquitoes. This live vaccine is given on one occasion at least 10 days before travel (if at all possible) and provides life long cover in the majority of patients.
Find out more about Yellow Fever
All Travellers
Poliomyelitis is a viral disease transmitted through oral/faecal contamination and the respiratory route. The vaccine is combined with cover against Tetanus and Diphtheria. Most travellers who have completed their primary course of childhood vaccines will only require a single booster dose to provide cover . Once completed it is expected that cover should last for 10 years.
Find out more about Poliomyelitis
Tetanus is contracted through contaminated cuts, bites and breaks in the skin. The vaccination provides cover for approximately 10 years in the majority of patients. It is frequently combined with cover against other diseases such as Poliomyelitis , Diphtheria and/or Pertussis .
Find out more about Tetanus
Hepatitis A is a common disease in many of the hotter regions of the world and usually contracted through contaminated food and water. Cover against Hepatitis A can be given alone or combined with protection against Hepatitis B. Once completed, the Hepatitis A vaccination ( given on two occasions 6 to 12 months apart ) provides cover for approximately 25 years in the majority of patients.
Find out more about Hepatitis A
Typhoid is a bacterial disease contracted through contaminated food and water. Once completed, the Typhoid vaccination given on one occasion provides cover for between 2 to 3 years in the majority of patients
Find out more about Typhoid
Meningococcal Meningitis is a bacterial disease which is usually transmitted through the respiratory route. The vaccine is given on one occasion and provides cover against four of the main forms of this disease. Once a course is completed the vaccination provides for over 10 years in the majority of patients.
Find out more about Meningococcal Meningitis
Hepatitis B is a viral disease which is usually transmitted in a very similar fashion to HIV/AIDS through contact with infected body fluids (eg blood exposure and sexually). This vaccine can be combined with cover against Hepatitis A. The standard schedule for Hepatitis B is to administer the vaccine on days 0, 28 and 180. A more rapid schedule can be used in cases where cover is needed more urgently and this is administered on days 0, 7, 21 to 28 and also 365. Following either course (and not before completion) a blood test can be taken to confirm sufficient antibody protection. Where the correct level of antibodies are showing (>10iu) the vaccination is recognised to provide cover for life .
Find out more about Hepatitis B
Rabies is a viral disease which is usually transmitted through the bite, the lick or the scratch of any infected warm blooded animal. As per the current WHO guidance, the vaccine is usually administered on days 0 and between 7 and 28 . Once a course is completed, the vaccination provides life long ‘immune memory’ in the majority of patients BUT after any possible exposure the individual always needs further vaccination to boost antibody production
Find out more about Rabies
Cholera / E coli are both food / water borne diseases. This oral vaccine is given on two occasions between 1 to 6 weeks apart before travel. The second dose (frequently given one week after the initial one) should be administered 7 days before potential exposure . Once completed the cover against Cholera is expected to be for about 2 years . The cover against E coli is shorter and thought to be effective for between 3 to 4 months . In travellers who have completed an initial primary course within the past 2 years a single further dose is sufficient to maintain this cover.
Find out more about Cholera
Cookies on GOV.UK
We use some essential cookies to make this website work.
We’d like to set additional cookies to understand how you use GOV.UK, remember your settings and improve government services.
We also use cookies set by other sites to help us deliver content from their services.
You have accepted additional cookies. You can change your cookie settings at any time.
You have rejected additional cookies. You can change your cookie settings at any time.
Register to vote Register by 18 June to vote in the General Election on 4 July.
- Passports, travel and living abroad
- Travel abroad
- Foreign travel advice
Sierra Leone
Warnings and insurance.
The Foreign, Commonwealth & Development Office ( FCDO ) provides advice about risks of travel to help British nationals make informed decisions. Find out more about FCDO travel advice .
Before you travel
No travel can be guaranteed safe. Read all the advice in this guide and any specific travel advice that applies to you:
- women travellers
- disabled travellers
- LGBT+ travellers
- solo and independent travel
- volunteering and adventure travel
Follow and contact FCDO travel on Twitter , Facebook and Instagram . You can also sign up to get email notifications when this advice is updated.
Travel insurance
If you choose to travel, research your destinations and get appropriate travel insurance . Insurance should cover your itinerary, planned activities and expenses in an emergency.
Related content
Is this page useful.
- Yes this page is useful
- No this page is not useful
Help us improve GOV.UK
Don’t include personal or financial information like your National Insurance number or credit card details.
To help us improve GOV.UK, we’d like to know more about your visit today. Please fill in this survey (opens in a new tab) .
Mobile teams bring COVID-19 vaccines to rural villages in Sierra Leone
COVID-19 vaccination rates remain low in many African countries, often because providing access to vaccines is difficult in remote areas. A new international research project showed that intervention with mobile vaccination teams in Sierra Leone is an effective way of reaching rural populations to increase vaccination uptake.
Madison Levine, a doctoral student in the Department of Agricultural and Consumer Economics (ACE), part of the College of Agricultural, Consumer and Environmental Sciences (ACES) at the University of Illinois Urbana-Champaign, participated in the project as a field research assistant. She is a co-author on the research paper, which is published in Nature, and she shared her experiences overseeing the project implementation.
"I was organizing the fieldwork, coordinating communications, and training everybody. Everything was approved by the principal investigators, of course, but I was making field plans and ensuring every route would work within the time frame we had. I assisted if there were any problems, and I was in as many villages as possible," Levine said.
"It was challenging because we were going to very remote areas. We had a car for the project, but there were places you couldn't go by car, so there was a lot of traveling on motorbikes, and sometimes we had to take a boat to get across an area of water. The health staff who were going with us carried the vaccines in ice boxes."
Levine holds a master's degree in international development economics from the University of San Francisco and she worked in Sierra Leone for several years before implementing the COVID-19 project. At Illinois, her advisors are ACE professors Hope Michelson and Sarah Janzen.
The research was conducted by a collaborative team from the International Growth Centre, University of Oxford, Yale University, and Wageningen University in cooperation with the Sierra Leone Ministry of Health and Sanitation (MoHS) and the international non-governmental organization Concern Worldwide. The Sierra Leone MoHS operates a network of peripheral health units, but many Sierra Leoneans live far away from these units, and people have to travel an average of 3.5 hours each way to reach a vaccination center.
The study included 150 rural villages in Sierra Leone that were located more than 5 miles from any health unit, and the intervention took place over several days.
"First, a team of community mobilizers would talk to the village leaders. Once the leaders approved, the team would hold a public meeting where they would talk about what the vaccine does and address any concerns. The next day, they would put up a small clinic with a couple of tables that held the medical supplies, and people would line up to get vaccinated. The MoHS assisted in providing trained nurses and medical staff for each place. All teams included local people who spoke the language of the village, which helped to build trust," Levine said.
"The majority of the communities welcomed our team. These very small villages are used to being surpassed by bigger cities, so they were happy we were coming out to them. Only two villages declined to participate, and we had to respect that."
The study found that immunization rates increased by about 26% in the trial villages. In addition, people who were traveling nearby would also stop to get vaccinated, further increasing the uptake. On average, the cost was about $33 per person, making it a very cost-effective intervention.
While there is some misinformation and vaccine hesitancy, by far the biggest obstacle is vaccine access, Levine said. "This project clearly shows you can make it cost-effective to reach people, even in very remote areas. For instance, the COVID-19 vaccine was received for free, so there needs to be a process in place to distribute it. It has to be budgeted properly and organized well, which people are highly capable of doing. This project shows it can be done, and hopefully, it opens doors for future global health interventions."
The paper, "Last-mile delivery increases vaccine uptake in Sierra Leone," is published in Nature.
- Health Policy
- COVID and SARS
- Today's Healthcare
- Education and Employment
- Social Issues
- Public Health
- Urbanization
- Vaccination
- MMR vaccine
- Search and rescue
- Mobile phone radiation and health
- Social inequality
Story Source:
Materials provided by University of Illinois College of Agricultural, Consumer and Environmental Sciences . Original written by Marianne Stein. Note: Content may be edited for style and length.
Journal Reference :
- Niccolò F. Meriggi, Maarten Voors, Madison Levine, Vasudha Ramakrishna, Desmond Maada Kangbai, Michael Rozelle, Ella Tyler, Sellu Kallon, Junisa Nabieu, Sarah Cundy, Ahmed Mushfiq Mobarak. Last-mile delivery increases vaccine uptake in Sierra Leone . Nature , 2024; 627 (8004): 612 DOI: 10.1038/s41586-024-07158-w
Cite This Page :
Explore More
- How Statin Therapy May Prevent Cancer
- Origins of 'Welsh Dragons' Exposed
- Resting Brain: Neurons Rehearse for Future
- Observing Single Molecules
- A Greener, More Effective Way to Kill Termites
- One Bright Spot Among Melting Glaciers
- Martian Meteorites Inform Red Planet's Structure
- Volcanic Events On Jupiter's Moon Io: High Res
- What Negative Adjectives Mean to Your Brain
- 'Living Bioelectronics' Can Sense and Heal Skin
Trending Topics
Strange & offbeat.
Bridging the gap to accelerate malaria vaccination rollout in Africa through experience sharing.
Africa is gradually making strides in fighting malaria across the continent through the Accelerating Malaria Vaccine Introduction and Rollout in Africa (AMVIRA) initiative.
As Burundi, Chad, Central African Republic (CAR), Democratic Republic of Congo (DRC), and Niger are gearing up for the introduction and rollout of the malaria vaccines, the World Health Organization (WHO) with funding from PATH and partners convened stakeholders from these countries to learn from Benin, Ghana, Cameroon, Burkina Faso, Liberia, and Sierra Leone’s malaria vaccination experience and ensure adequate preparation towards new introductions and rollout across these countries.
In addition, the intercountry peer learning is building capacities on the vaccines RTS, S, R21, and its monitoring tools to enhance readiness for successful vaccine rollout following the high interest and preparation for its introduction in about 20 more African countries.
“The vaccines are important for reducing malaria in young children, providing an important new tool to combat malaria. There is huge interest as we have seen, and PATH timely support is significantly appreciated”. Dr Konan Kouame Jean, WHO Representative Benin underscored.
Participants gained insights into vaccine introduction, digitalization of data management, vaccine risk communication, readiness monitoring, and supervision, among others. Additionally, a field visit to malaria vaccination centres was organized to provide participants with firsthand experience in Benin’s vaccination process.
“ PATH is committed to health equity and the inter-country learning platform is creating a network of experts in accelerating the malaria vaccinations in countries”, Mr John Bawa, Director of malaria Vaccines Implementation, PATH expressed.
As Africa continues to shoulder 94% of the global malaria burden, WHO and its partners including UNICEF and Gavi are strengthening malaria control efforts with vaccines being the latest in the control toolbox. In January 2024, the WHO Regional Office for Africa established the Accelerating Malaria Vaccine Introduction and Rollout in Africa (AMVIRA).
This initiative aims to strengthen the provision of technical support to Member States in their efforts to introduce and roll out malaria vaccines while strengthening partners’ coordination at national, regional, and global levels effectively and efficiently.
So far, African countries including Benin, Burkina Faso, Cameroon, Liberia, and Sierra Leone are rolling out the malaria vaccine into routine immunization. Since 2019, Ghana, Malawi, and Kenya have been rolling out the malaria vaccine as part of a pilot programme, reaching 2.5 million children as of December 2023.
WHO and partners also leveraged the workshop to address information gaps and share lessons and best practices to ensure successful scale-up of vaccine introduction and rollout in countries. Participants expressed sincere appreciation for the workshop, highlighting the significance and the knowledge gained which will help shape their strategies towards effective malaria vaccine rollout.
“One of the key lessons we picked in Benin, is the effective use of risk communications and consistent information sharing all through the rollout. We also picked other lessons from Ghana and Sierra Leone’s implementation including the use of data management and monitoring tools to accelerate the vaccine rollout”. Jean Crispin Mukendi, Deputy Manager for the Expanded Program on Immunization in the Democratic Republic of Congo noted.
In addition to facilitating the cross-learning, WHO through AMVIRA have deployed experts in immunization, data management, risk communication, and external communication to assist 5 countries in efficiently planning and delivering the vaccines.
Dr Joseph Biey, Country Support and Operation Pillar Lead for AMVIRA emphasized: “With more investment, we can together beat malaria in Africa”.
Communications Officer WHO Country Office, United Republic of Tanzania Tel: +255 744377899 (Phone) Email: adjeidum [at] who.int
Chargée de Communication OMS Bénin Email: akomatsria [at] who.int

IMAGES
VIDEO
COMMENTS
All international travelers should be fully vaccinated against measles with the measles-mumps-rubella (MMR) vaccine, including an early dose for infants 6-11 months, according to CDC's measles vaccination recommendations for international travel. In Sierra Leone poliovirus has been identified in the past year.
Proof of yellow fever vaccination is required for entry to Sierra Leone.. The CDC also says that the Zika virus is a risk in Sierra Leone. This virus can cause serious birth defects. It is recommended that pregnant women, or women planning to become pregnant, should not travel to Sierra Leone.
Call us in Washington, D.C. at 1-888-407-4747 (toll-free in the United States and Canada) or 1-202-501-4444 (from all other countries) from 8:00 a.m. to 8:00 p.m., Eastern Standard Time, Monday through Friday (except U.S. federal holidays). See the State Department's travel website for the Worldwide Caution and Travel Advisories.
Proof of yellow fever vaccination is required for entry to Sierra Leone. The NaTHNaC also says that the Zika virus is a risk in Sierra Leone. This virus can cause serious birth defects. It is recommended that pregnant women, or women planning to become pregnant, should not travel to Sierra Leone. Ebola struck Sierra Leone in July of 2014.
The White House announced that vaccines will be required for international travelers coming into the United States, with an effective date of November 8, 2021. For purposes of entry into the United States, vaccines accepted will include FDA approved or authorized and WHO Emergency Use Listing vaccines. More information is available here.
Find continuously updated travel restrictions for Sierra Leone such as border, vaccination, COVID-19 testing, and quarantine requirements. Flights. Hotels. Cars. Packages. Travel Guides. ... Most visitors from the United States, regardless of vaccination status, can enter Sierra Leone.
Health insurance card (your regular plan and/or supplemental travel health insurance plan) and copies of claim forms; Proof of yellow fever vaccination If required for your trip, take your completed International Certificate of Vaccination or Prophylaxis card or medical waiver; Copies of all prescriptions Make sure prescriptions include generic ...
Travel.Gov.Sl is Sierra Leone's official travel registration portal for passengers arriving at or departing from Freetown International Airport. The ICT Covid-19 Response PIllar manages the site which processes travel authorisation and assists the Surveillance Pillar with contact tracing during the COVID-19 pandemic. The Government of Sierra ...
FCDO travel advice for Sierra Leone. Includes safety and security, insurance, entry requirements and legal differences. ... At least 8 weeks before you travel, check how to get vaccines and ...
The 200,000 Pfizer vaccines donated March 17 and the 302,200 Johnson & Johnson vaccines donated March 15 are part of the over 800,000 vaccines to donated to Sierra Leone by the United States since last year. As of December 2021, the Pfizer vaccine has been approved for children in Sierra Leone as young as 12 years old.
For more details about medical entry requirements and recommended vaccinations, see TravelHealthPro's Sierra Leone guide. Airport security fee All passengers must pay a 25 US dollar airport ...
Last-mile delivery increases vaccine uptake in Sierra Leone. Nature 627 , 612-619 ( 2024) Cite this article. Less than 30% of people in Africa received a dose of the COVID-19 vaccine even 18 ...
The World Bank approved an $8.5 million grant in additional financing to support affordable and equitable access to COVID-19 vaccines in Sierra Leone. The funds will provide upfront financing to help purchase and deploy coronavirus vaccines, and to strengthen relevant health systems necessary for a successful deployment and to prepare for future pandemic outbreaks.
Current travel vaccine advice and how to prevent infections when travelling to Sierra Leone. The recommendations and advice on this page can never replace a medical consultation. To get the best effect from the vaccines, you should begin vaccination well before departure.
In Sierra Leone 60% of the rural population live on less than US$1.25 a day. Getting to a clinic would cost more than one week's wages. Health workers and vaccines packed in a solar-powered ...
While Sierra Leone was one of the first western African nations to receive COVID-19 vaccines—beginning its vaccine rollout in March 2021—by March 2022, Sierra Leone had only 14 percent of its population vaccinated. That was up from five percent two months previous. On the strength (12 mass vaccination campaigns in 2022 and three in 2021 ...
The laws of Sierra Leone prohibit sexual acts between individuals of the same sex. 2SLGBTQI+ travellers should carefully consider the risks of travelling to Sierra Leone. Travel and your sexual orientation, gender identity, gender expression and sex characteristics. Driving. Carry your identification and vehicular documentation with you.
Avoid travel if unwell with influenza-like symptoms; ... Yellow fever vaccine recommendation map for Sierra Leone. Click on map to open in a new window; Some travellers. The vaccines in this section are recommended for some travellers visiting this country. Information on when these vaccines should be considered can be found by clicking on the ...
Advice for All Destinations COVID-19. Read the information on the COVID-19: Health Considerations for Travel page for advice on travelling during the COVID-19 pandemic.. Vaccinations and malaria risk. Review both the Vaccination and Malaria sections on this page to find out if you may need vaccines and/or a malaria risk assessment before you travel to this country.
CDC recommends YF vaccination for travel to areas classified as having endemic or transitional risk (Maps 5-10 and 5-11). Because of changes in YF virus circulation, ... See Health Information for Travelers to Sierra Leone. Footnotes Yellow Fever Vaccine. 1 Current as of November 2022. This is an update of the 2010 map created by the Informal ...
Vaccinations for Sierra Leone 13:12 Sat 1st Jun, 2024. Required. Yellow Fever. Yellow Fever is a viral disease transmitted by mosquitoes. ... Since then it has expanded greatly and today TMB is the largest travel vaccination organisation in Ireland with over 20 clinics nationwide. As medical director, Dr Fry plays a pivotal role in the ...
Warnings and insurance. Still current at: 29 May 2024. Updated: 9 February 2024. Latest update: This travel advice has been rewritten to make it easier to read and understand. The Foreign ...
The Sierra Leone MoHS operates a network of peripheral health units, but many Sierra Leoneans live far away from these units, and people have to travel an average of 3.5 hours each way to reach a ...
So far, African countries including Benin, Burkina Faso, Cameroon, Liberia, and Sierra Leone are rolling out the malaria vaccine into routine immunization. Since 2019, Ghana, Malawi, and Kenya have been rolling out the malaria vaccine as part of a pilot programme, reaching 2.5 million children as of December 2023.
Ethiopian Airlines, the largest network operating airline in Africa, is pleased to announce the commencement of its thrice weekly passenger services to Freetown, Sierra Leone via Ouagadougou ...