November 17, 2020

The human skull can be grossly divided into a movable and an immovable part. The movable part is formed by the lower jaw called the mandible. The rest of the skull forms the immovable portion. These two parts of the skull are connected by a joint near the ear. This joint is the temporomandibular joint (TMJ).
The TMJ has three main parts. A temporal part, that is the part of the immovable portion of the skull. The temporal bone is a depression that receives the condyle. The condyle is a part of the mandible that makes the primary movements of the lower jaw. A disc located between the temporal bone and the condyle helps in the range of movements. The smooth movements of the articular disk are possible because of a fluid called the synovial fluid. This fluid acts as a lubricant, as a result of which our lower jaw can move freely during speech, chewing, etc.
The movements produced by the TMJ are protrusion (moving the lower jaw forward), retrusion (moving the lower jaw backward), elevation (mouth closure), depression (mouth opening), lateral excursion (side to side). In this article, we would be focusing on lateral excursion.
Simply put, lateral excursion is when the mandible moves to one side. But the mechanism behind this is not as simple as it sounds. The mandible is capable of two movements if we take the condyle as the hinge: rotation and translation. Imagine a vertical and horizontal axis passing through the condyles. The movement of the mandible with respect to the vertical axis is called rotation and with respect to the horizontal axis it is translation.
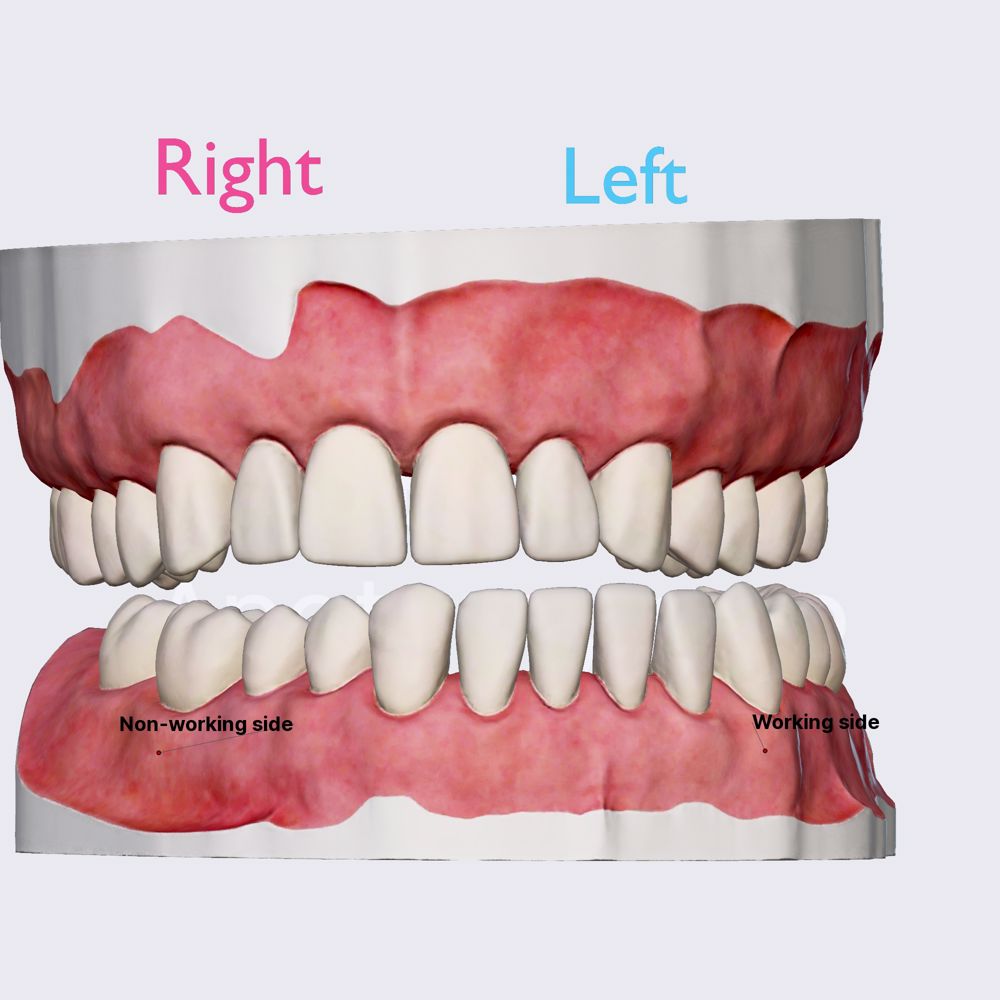
The forward movement of the mandible is a translatory motion. The sideways movement is a rotational motion. In lateral excursion, both these motions take place simultaneously. Let us understand this movement with an example. Imagine you want to move your lower jaw to the left side. This means that both the condyles would have to move towards the left. Since the jaw has to be moved to the left, the left condyle will rotate in the desired direction. In our case, the left side is the working side. The mandible is a single bone, if the left condyle moves, the right condyle will be also stretched towards the left. However, since there are many structures that limit this movement of the right condyle, it will simply move forward in translation. Hence, the right side in our example would be the non-working side.
The working and the non-working side function in conjunction to produce the desired movement. However, lateral excursion is not simply a movement attributed to the condyles. A key role is played by the muscles that are attached to the mandible. These are the muscles that find their origin in the immovable part of the skull are terminate their fibres in the moving mandible. The four muscles are lateral pterygoid, medial pterygoid, temporalis and masseter. Each of these muscles help the mandible to glide forwards, downwards and sideways to make the lateral excursion.
Lateral excursion is one of the key functional movements that helps in chewing. It ensures that we humans do not simply chop down the food by simply opening and closing the mouth but also grind it to make a proper bolus for effective digestion. Lateral excursion is the second key step when we chew our food. Once the mouth opens and the food enters the oral cavity, the jaw moves sideways and grinds the food, closes gradually and finally the teeth meet each other before the mouth comes back in a state of rest.
Lateral excursion might be hampered due to problems in the gnathic system. A locked jaw, tumour, traumatic injury, muscle pain, disk injuries, congenital disorders may contribute to improper or no lateral excursion movement. While some of these disturbances need surgical intervention or pharmacological cover, minor disturbances can be corrected with home techniques focusing on physiotherapy.
Prosthetic treatments that involve fabrication of complete dentures give notable emphasis on lateral excursion. During the fabrication of dentures, the upper and lower canines are made to touch each other as the sideway movement occurs. When they glide over each other, the back teeth are no longer in contact which ensures proper lateral excursion. This is also called canine guidance .
Thus, lateral excursion is one of the vital movements that the mandible can perform considering how the entire surrounding musculature comes into picture for normal functioning.

Partners and Sponsors

- Advertising with DentaGama
- Terms and Conditions
- Privacy Policy
- Cookies Policy
- Reviews Policy
© 2023 DentaGama All rights reserved
- Media Library
- Encyclopedia
- Universities
Unlock with Premium
- Dynamic occlusion: lateral excursion
The dynamic occlusion is the contact that teeth make during movements of the mandible - when the jaw moves side to side, forward, backward or at an angle. In dynamic occlusion, the contacts of the teeth are not points as in static occlusion, but they are described with lines.
- Dental occlusion
- Occlusal relationship
- Temporomandibular joint (TMJ)
- Joint capsule and ligaments of TMJ
- Movements of TMJ
- Static occlusion: centric occlusion
- Occlusion concepts: centric relation
- Angle's classification
- Angle's classification: Class I
- Angle’s classification: Class II, Division 1
- Angle's classification: Class II, Division 2
- Angle's classification: Class III
- Dynamic occlusion: canine guidance
- Dynamic occlussion: protrusion
- Curve of Spee
- Curve of Wilson
- Sphere of Monson
What Is Occlusion?
- First Online: 04 June 2022
Cite this chapter

- Stephen Davies 2
Part of the book series: BDJ Clinician’s Guides ((BDJCG))
The aim of this book is to explore the role of Occlusion in Dental Practice.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as EPUB and PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Smith BGN. Occlusion: 1. General considerations. Dent Update. 1991;18:141–5.
Google Scholar
O’Carroll EO, Leung A, Fine PD, Boniface D, Louca C. The teaching of occlusion in undergraduate dental schools in the UK and Ireland. Brit Dent J. 2019;227:512–7.
Article Google Scholar
Oxford University Press. Shorter Oxford English dictionary. Oxford: Oxford University Press; 1973.
Greenfield S, editor. The private life of the brain: emotions, consciousness, and the secret of self. London: Penguin Books. ISBN-13 978-0-141-00720-5.
Ash MM, Ramfjord SP. Occlusion. 4th ed. Philadelphia: Saunders; 1995. p. 76.
Horner GQ. The effects of positioning variations in transcranial radiographs of the temporomandibular joint: a laboratory study. Br J Oralmaxillofac Surg. 1991;29:241–2.
Posselt UOA. Studies in the mobility of the human mandible. Acta Odontol Scand. 1952;10:19.
Ramfjord SP, Ash MM. Occlusion. 2nd ed. Philadelphia: Saunders; 1971. p. 178.
Ash MM, Ramfjord SP. Occlusion. 4th ed. Philadelphia: Saunders; 1995. p. 84–5.
Davies SJ. Malocclusion—a term in need of dropping or redefinition? Br Dent J. 2007;202:12.
Gremillion HA. Relationship between TMD and occlusion. J Evid Base Dent Pract. 2006;6:43–7.
Moufti MA, Lilico JT, Wassell R. How to make a well-fitting stabilization splint. Dent Update. 2007;34:398–408.
Wise M. Occlusion and restorative dentistry for the general dental practitioner. Br Dent J. 1982;152:319–20.
Davies SJ. Occlusion in restorative dentistry: conformative, re-organised or unorganised. Dent Update. 2004;31:334.
Davies SJ, et al. Occlusion: is there a third way? A discussion paper. Br Dent J. 2021;321:160–2.
Download references
Author information
Authors and affiliations.
Specialist in Restorative Dentistry, Lecturer in Occlusal and Temporomandibular Studies, Division of Dentistry, Faculty of Biology, Medicine and Health, University of Manchester, A Lead Clinician, Temporomandibular Disorder Clinic, University Dental Hospital of Manchester, Manchester, UK
Stephen Davies
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Stephen Davies .
Rights and permissions
Reprints and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Davies, S. (2022). What Is Occlusion?. In: A Guide to Good Occlusal Practice. BDJ Clinician’s Guides. Springer, Cham. https://doi.org/10.1007/978-3-030-79225-1_1
Download citation
DOI : https://doi.org/10.1007/978-3-030-79225-1_1
Published : 04 June 2022
Publisher Name : Springer, Cham
Print ISBN : 978-3-030-79224-4
Online ISBN : 978-3-030-79225-1
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Angle Orthod
- v.80(1); 2010 Jan

Functional Occlusal Patterns and Their Relationship to Static Occlusion
Kazem s. al-nimri.
a Associate Professor, Department of Orthodontics, School of Dentistry, Jordan University of Science and Technology, Irbid-Jordan
Anwar B. Bataineh
b Professor, Department of Oral and Maxillo-Facial Surgery, School of Dentistry, Jordan University of Science and Technology, Irbid-Jordan
Sawsan Abo-Farha
c Postgraduate student, Department of Orthodontics, School of Dentistry, Jordan University of Science and Technology, Irbid-Jordan
Objectives:
To test the hypothesis that there is no relationship between static occlusion and dynamic occlusion.
Materials and Methods:
The relationship between static and dynamic occlusion was investigated in a sample of 94 dental students (39 males and 55 females) with an age range of 21–30 years. Static occlusion was determined by intraoral examination. Dynamic occlusion was determined in regulated lateral (0.5 mm and 3 mm lateral to the intercuspal position) and protrusive movements of the mandible by intraoral examination with the aid of shimstock.
At the 0.5 mm lateral excursion, 24.5% had bilateral group function and 12.7% had bilateral canine guidance. At the 3 mm positions, the guidance pattern changed to a predominantly canine guidance. Fifty percent of subjects had bilateral canine guidance, and only 8.8% had bilateral group function. In terms of the anterior guidance pattern, a predominant anterior contact with posterior disocclusion (77.5%) was noted. Examination of the relationship between static and dynamic occlusions revealed that at the 0.5 mm position, the pattern of dynamic occlusion was different in relation to various static occlusion features but without reaching a significant level. While at the 3 mm position, the pattern of dynamic occlusion was significantly affected by incisor relationship. The distribution of protrusive excursion patterns was significantly influenced by incisor, canine, and molar relationships.
Conclusions:
The hypothesis is rejected. An association exists between dynamic occlusion and different aspects of static occlusion.
INTRODUCTION
Dental treatment has the capacity to fundamentally change static and dynamic occlusal relationships, while aiming for achieving as near “ideal” occlusion as possible. Accepted criteria for the “ideal” static occlusion were established based on the work of Angle, 1 who is credited with making the profession most aware of occlusion by presenting standards whereby a malocclusion could be compared with normal occlusion, and the work of Andrews, 2 who presented six keys that gave a well-delineated prescription for an ideal intercuspation of teeth. Conversely, the features that constitute “ideal” dynamic occlusion continue to be subject to great debate and have not, to date, been conclusively established.
There are three main concepts regarding tooth contact during the lateral excursion of mandibular movement: (1) balanced occlusion, which was developed from the work of Bonwill, 3 (2) canine guidance, described by D'Amico, 4 and (3) group function, as discussed by Beyron. 5
The relationship between static and dynamic occlusion is one of the aspects of the study of functional occlusion that has received little attention. Few studies have explored the possibility of an association but conflicting results have been reported. Scaife and Holt 6 found canine protected occlusion to be associated with Class II then Class I, and least associated with Class III, malocclusion. The above mentioned findings were confirmed by Al-Hiyasat and Abu-Alhaija 7 in a study of 447 school children, aged 14–17 years. Other studies found that most Class I Angle occlusion cases were associated with balanced occlusion. 8 – 10 On the other hand, Tipton and Rinchuse 11 found no significant association between static and dynamic occlusion.
A number of limitations can be noted in the above mentioned studies: No reference was made to the location of the canine in terms of its relationship to the line of the arch nor to the degree of attrition of the canine, which is of particular importance in examining the assumption that attrition could lead from one type of contact during lateral movement to another. 12 Moreover, the position at which the occlusal contact pattern was recorded (cusp to cusp) is not representative of the functional range of the lateral excursion of mandibular movement.
Another fact for consideration is that changes occurring during occlusal development could influence the occlusal contact pattern; Heikinheimo et al 13 reported an increase in occlusal interferences between the ages of 12 and 15 years in 167 Finns; other studies found a decreasing prevalence with increasing age. 14 , 15 Although the results of these studies are contradictory, they suggest that changes occur during occlusal development that must not be overlooked in sample selection; samples that are beyond the adolescent years would be more representative of a population as it avoids the effects of age and occlusal development on the results of research.
Based on the above mentioned facts, we thought it warranted to further investigate whether a relationship exists between static occlusion and dynamic occlusion, and, if such a relationship exists, which type of dynamic occlusion is associated with which type of static occlusion.
MATERIALS AND METHODS
The population for this study consisted of 94 dental students at Jordan University of Science and Technology (39 males and 55 females). The age of subjects ranged from 21–30 years, with a mean age of 23.1 (±1.44) years. Subjects who met the following criteria were selected:
- No previous or current orthodontic treatment.
- The presence of fully permanent dentition except for the third molars
- No previous occlusal adjustments
- No large restorations involving the incisal edge or a cusp tip
- No crowns or bridges
- No apparent pathologic periodontal problems
- Upper and lower canines in the line of the arch
- No tooth showing attrition into the dentine
The static occlusion of each subject was assessed by intraoral examination on a dental chair under direct vision. The following static occlusal features were recorded:
- Incisor relationship classified according to the British Standard Institute 16
- Canine relationship classified according to Houston et al 16
- Molar relationship classified according to Angle's criteria 1
Dynamic occlusion was determined with the aid of shimstock (Almore shimstock, 8 mm wide, 8 µm thick, Hanel, Langenau, Germany) to confirm tooth contact. The examination was carried out with subjects seated in an upright position in a dental chair with the Frankfort plane parallel to the floor. All recordings were made by the same operator in the same period of the day (morning hours) to avoid possible diurnal variation. 17
For the lateral excursion, occlusal contacts were recorded on the working and the nonworking side at ½ mm and at 3 mm lateral to the habitual centric occlusion. To regulate each lateral position, marks were made on the maxillary central incisor with a water-resistant pencil to mark the intercuspal position at 0.5 mm and 3 mm positions for both right and left sides. Subjects were asked to perform the movements with the aid of a handheld mirror. The shimstock was placed on the occlusal surfaces of teeth from the canine backward; the subject was then asked to close his/her mandible into maximum intercuspation. Gliding movement was performed to the right or the left while the examiner maintained a constant pulling force on the shimstock; on reaching the 0.5 mm position, the teeth holding the shimstock were recorded as working side contacts. The subject was asked to repeat the movement with the shimstock placed on the opposite side to record nonworking side contact. The same procedure was carried out to record occlusal contact at 3 mm lateral to the habitual centric occlusion.
Occlusal contacts at the protrusive excursion of mandibular movement were recorded at the edge-to-edge position. The shimstock was placed on the occlusal surfaces of the anterior teeth; the subject was asked to close into maximum intercuspation and then slide to the edge-to-edge protrusive position while the examiner maintained a constant pulling pressure. Once the teeth were at the edge-to-edge position, teeth holding the shimstock were considered to be in contact and were recorded. The shimstock was then placed on the occlusal surfaces of post teeth, and the subject was asked to repeat the same movement to check for the presence of posterior teeth contact.
In the lateral excursion, the guidance pattern was considered as one of the following:
- Bilateral canine protected occlusion
- Bilateral group function occlusion
- Mixed canine protected and group function
- Bilateral balanced occlusion
- Mixed balanced and group function
- Mixed group function and single tooth contact
- Others (this category included bilateral mediotrusive interference, mixed laterotrusive and canine, bilateral laterotrusive interference, mixed mediotrusive and group, mixed canine guidance, and laterotrusive interference)
In the protrusive excursion, the guidance pattern was considered as one of the following:
- Anterior contact with posterior disocclusion
- Anterior contact with unilateral posterior contact
- Anterior contact with bilateral posterior contact
- No anterior contact with unilateral posterior contact
- No anterior contact with bilateral posterior contact
Ten subjects were reexamined at 2 months following the initial clinical examination to determine intraexaminer reliability. The Kappa ranged from (0.8–1), indicating a reliable examination.
Statistical Analysis
Data were analyzed using the Statistical Package for the Social Sciences (SPSS), version 11 (SPSS Inc, Chicago, Ill). The Chi-square test was used to examine the relationship between the different variables included in this study. P values less than .05 were considered statistically significant.
Dynamic Occlusion
In the total sample at 0.5 mm lateral guidance, 24.5% of subjects had bilateral group function and 18.1% had mixed canine guidance and group function. While at the 3 mm positions, the guidance pattern changed to a predominantly canine guidance. Fifty percent of subjects had bilateral canine guidance, and only 8.5% had bilateral group function ( Table 1 ).
Distribution (%) of Dynamic Occlusion at 0.5 mm and 3 mm Lateral Excursion and Incisor Classification a

In the protrusive guidance patterns, a predominant anterior contact with posterior disocclusion (77.5%) was followed by anterior contact with unilateral posterior contact (12.7%). Anterior contact with bilateral posterior contact was found in 4% of subjects. The remaining 5.8% had no anterior contact with unilateral or bilateral posterior contact.
Static Occlusion
The incisor relationship was Class I in 49 subjects, Class II/1 in 10 subjects, Class II/2 in 17 subjects, and Class III in 18 subjects. The molar and canine relationships are reported in Tables 2 and and3 3 .
Distribution (%) of Dynamic Occlusion at 0.5 mm and 3 mm Lateral Excursion and Canine Classification a

Distribution (%) of Dynamic Occlusion at 0.5 mm and 3 mm Lateral Excursion and Molar Classification a

No statistically significant differences were found between males and females in the various aspects of static occlusion or in the guidance pattern in lateral or protrusive excursions. Therefore, male and female subjects were pooled together in the analysis.
Relationship Between Static and Dynamic Occlusion
The type of guidance at the 0.5 mm position was not significantly associated with the incisor ( Table 1 ), canine ( Table 2 ), or molar classification ( Table 3 ). However, it should be noted that at 0.5 mm lateral excursion, bilateral canine protected occlusion was observed only in subjects with Class I incisor, canine, or molar relationships
As can be seen in Table 1 , 70% of subjects with Class II div 1 and Class II div 2 incisor relationships have bilateral canine protected occlusion at 3 mm lateral guidance, compared with 53% in Class I and 11% in Class III. This difference was statistically significant ( P = .047). On the other hand, no significant association was noted between the type of lateral guidance at the 3 mm positions and the canine relationship ( Table 2 ) or the molar relationship ( Table 3 ).
The pattern of guidance in protrusive mandibular excursions was significantly associated with incisor classification ( P < .0001; Table 4 ), canine classification ( P < .0001; Table 5 ), and molar classification ( P = .031; Table 6 ), with less anterior contact with posterior disocclusion observed in Class III subjects.
Distribution (%) of the Pattern of Guidance in Protrusive Mandibular Excursion and Incisor Classification a

Distribution (%) of the Pattern of Guidance in Protrusive Mandibular Excursion and Canine Classification a

Distribution (%) of the Pattern of Guidance in Protrusive Mandibular Excursion and Molar Classification a

The criteria set for selecting subjects for this study were chosen to ensure the presence of a natural dentition. The absence of apparent pathologic periodontal problems was used as a criterion because the neuromuscular control of occlusion stability and masticatory muscles is influenced by the periodontal afferent. 18 , 19 The fact that the sample was composed of subjects aged 21 to 30 years was chosen because the changes occurring during occlusal development could influence the occlusal contact pattern. Cases with marked attrition were excluded based on the assumption made by McAdam 20 and Woda et al 12 that canine guidance and group function appear to correspond to two successive states of the evolving dentition under the effect of attrition.
Static occlusion was assessed by intraoral examination by direct vision with the aid of a dental mirror, as was done in previous investigations. 7 , 11 Ovsenik et al 21 reported that intraexaminer and inter-examiner malocclusion assessment recorded and measured intraorally is reliable and therefore is proposed as the method of choice to be used not only in epidemiologic studies and screenings, but also in clinical orthodontic assessments.
Occlusal contacts for both lateral and protrusive excursions of the mandible were determined by intraoral examination with the aid of shimstock to confirm the contact between the teeth, as was done in previous investigations. 7 , 22 – 24 Shimstock has been shown to have greater interexaminer reliability than articulating film 25 and high intraexaminer reliability. 7 The chosen thickness of the shimstock was 8 µm, which is below the range of reported thresholds for dental proprioception. This method allows identification of contacting teeth without disturbing this delicate mechanism; a system of measurement that disrupts proprioception may alter mandibular position and consequently tooth contact. 26
For the lateral excursion of the mandible, occlusal contacts were recorded at two positions: ½ mm and 3 mm lateral to the habitual centric. These two positions were selected based on the findings of Ogawa and coworkers, 23 who conducted a study in which tooth contacts were recorded at 0.5, 1, 2, and 3 mm lateral to the maximum intercuspation. They concluded that the occlusal contact patterns during lateral movement varied greatly with mandibular position. The occlusal contact pattern in the 3 mm position predicted the presence or absence of the occlusal contact in the 1 and 2 mm positions (sensitivity >0.7) but not in the 0.5 mm position (sensitivity <0.6). Finally, they suggest that the 0.5 mm position could be used to evaluate occlusal contact in a position close to maximum intercuspation in the functional range, and that the 3 mm position could be used to assess occlusal contact in an edge-to-edge position in the parafunctional range. 24
The orthodontic picture of “ideal occlusion” places considerable emphasis on the static occlusal relationship in assessing the quality of completed orthodontic treatment, with less emphasis on the importance of the dynamic occlusion. In fact, none of the available orthodontic indices for the assessment of treatment outcome contains any functional components! One could argue that this is caused by the absence of consensus regarding what constitutes an “ideal” dynamic occlusion. This, nonetheless, should not lead to a practice of disregarding basic functional principles during orthodontic treatment. As Clark and Evans 27 argue, the gradual adaptation of muscles and joints that occurs during the slow development of a specific occlusion during growth may not occur following the much quicker change related to orthodontic treatment. Other possible consequences of occlusal interference, such as tooth wear and relapse of tooth position, may become apparent only some time after completion of orthodontic treatment, but nevertheless may be attributable to interferences introduced during appliance therapy.
Based on all of the above, we found it particularly interesting to explore the relationship between static and dynamic occlusion. At 0.5 mm lateral excursion, canine protected occlusion was more dominant in Class I incisor, canine, and molar relationships; at 3 mm lateral excursion, canine protected occlusion was dominant in Class II occlusion. Our findings at the 3 mm position compare favorably with those of Al-Hiyasat and Abu-Alhaija, 7 who reported that canine guidance was more dominant in Class II followed by Class I; and those of Scaife and Holt, 6 who found canine protected occlusion to be associated with Class II then Class I and least associated with Class III. However, these results do not agree with other studies, in which investigators found most of Class I Angle occlusion to be associated with balanced occlusion 8 – 10 ; neither do they agree with the findings of Tipton and Rinchuse, 11 who found no significant association between static and dynamic occlusion.
This lack of agreement may be attributed to the different registration materials utilized. Registration material has a significant influence on the number of contacts recorded; some materials tend to record “near contact” as actual contact resulting in differences in the occlusal contact pattern registered. 28 Diurnal difference in occlusal contacts, 17 differences in the criteria used for sample selection, and differences in the classification system are additional factors that contribute to the observed differences.
Anterior guidance with posterior distocclusion was associated with Class II div 2 incisors, followed by Class I and Class II div 1; Class II canines followed by Class I; and Class II molars followed by Class I. These associations explain the high prevalence of posterior contact in protrusion observed in Class III cases and the high prevalence of anterior contact with posterior distocclusion in Class II div 2 cases.
These observations are consistent with those of Al-Hiyasat and Abu-Alhaija, 7 who reported that anterior guidance with posterior distocclusion was associated with Class II div 2 incisors, then Class I and Class II div 1. The prevalence of posterior contact in protrusion was dominantly associated with Class III incisor and molar relationships (50% and 33%, respectively).
Although an association between static and dynamic occlusion was found, it is very difficult to establish a definitive association between them. Therefore, it is necessary to evaluate dynamic occlusion with the aspects of length and inclination of the occlusal guidance of each tooth used as functional indicators.
CONCLUSIONS
- The distribution of lateral guidance is different at the 0.5 mm and 3 mm positions.
- At 0.5 mm lateral excursion, bilateral canine protected occlusion was observed only in subjects with Class I incisor relationships or subjects with unilateral or bilateral Class I molar or canine relationships.
- At 3 mm lateral excursion, bilateral canine protected occlusion was predominant in subjects with Class II incisor, canine, and molar relationships.
- Anterior guidance with posterior disocclusion was observed most often in subjects with Class II div 2 occlusion and was least observed in subjects with Class III occlusion.

- No menu assigned!
Complete Dentures Occlusal Schemes - Anatomic and Semi-Anatomic Occlusion
Complete Dentures»
Complete Dentures – Occlusal Schemes – Anatomic and Semiamatomic Occlusion — Course Transcript
- 1. 17. Occlusal Schemes – Anatomic and Semi-anatomic John Beumer III, DDS, MS and Michael Hamada DDS Division of Advanced Prosthodontics, Biomaterials and Hospital Dentistry UCLA School of Dentistry This program of instruction is protected by copyright ©. No portion of this program of instruction may be reproduced, recorded or transferred by any means electronic, digital, photographic, mechanical etc., or by any information storage or retrieval system, without prior permission.
- 2. Semi-anatomic Denture Teeth Begin by positioning the appropriate protrusive insert, and check to ensure that the incisal guide pin is set at zero and in contact with the incisal guide table. Protrusive insert Protrusive Inserts Zero setting
- 3. Background – Balanced occlusion Our objective in setting anatomic or semi-anatomic posterior teeth is to create a balanced occlusion. We wish to insure that all the posterior teeth as well as the anterior teeth maintain contact in lateral excursions. To ensure bilateral balance we place an anterior-posterior curve in the arch, called a compensating curve, which is analogous to the curve of Spee in natural dentition. In addition , we place a curve from side to side, the so called curve of Wilson. Semi-anatomic Denture Teeth
- 4. Mark the casts indicating midline, crest of the ridge, and the retromolar pad . These landmarks will be used to check your denture setup. Maxilla Midline Anterior land Mandible Ridge Retromolar pad Cast Landmarks
- 5. Anterior land Cast Landmarks – Maxilla Midline Incisive papilla
- 6. Lines indicating the crest of the ridge Cast Landmarks -Mandible Midpoint of retromolar pad Land Mark on land indicating the midpoint of the retromolar pad
- 7. As previously mentioned (13c, 1a), the wax rim is ideally contoured on the patient and used to mount the upper cast with a facebow transfer record. When the lower cast is mounted on the articulator with a centric relation record the plane of occlusion is readily seen. The three landmarks used to identify the plane of occlusion are: The midpoint of the retromolar pads bilaterally as previously marked on the mandibular cast. The incisal edge of the maxillary central incisors Setting the Maxillary Anterior Teeth
- 8. To set the remaining maxillary anterior teeth a clear glass or plastic slab is positioned on the mandibular record base to represent the plane of occlusion. When setting anatomic posterior teeth we recommend setting the maxillary posterior teeth before the mandibular posterior teeth. To aid in positioning the maxillary teeth, a line is inscribed on the slab indicating the crest of the mandibular ridge. Setting the Maxillary Anterior Teeth Mark indicating midpoint of the retromolar pad
- 9. Setting the Maxillary Anterior Teeth These two lines, inscribed on the plastic plane, indicate the crest of the alveolar ridge. These lines will be used to position the maxillary posterior denture teeth to insure that the mandibular posterior teeth are centered over the ridge. The lingual cusp tips of the posterior maxillary teeth should contact these lines. Lines indicating the crest of the ridge
- 10. Setting the Maxillary Anterior Teeth Soften some baseplate wax and attach some to the ridge lap portion of the other maxillary central incisor and attach it to the record base as shown. Set the lateral incisors and cuspids as shown previously (Section 13c, 1a Lingualized occlusion).
- 11. Setting the Maxillary Anterior Teeth Note the angulations of the anterior teeth in relation to the occlusal plane when viewed in profile. Occlusal plane
- 12. Setting the Maxillary Anterior Teeth “ Toed-in” Position Note how the cervical and incisal edges of the cuspid are aligned vertically (yellow line). The facial surface of the cuspid however, is canted inward and appears “toed in” (red line) due to the prominence of the cervical area of the tooth (yellow arrow). The centrals and laterals are inclined slightly towards the distal.
- 13. The long axis of the premolars should be perpendicular to the occlusal plane and the buccal and lingual cusp tips should touch the occlusal plane. Arranging the premolars in this way insures that the adjacent marginal ridges will be on the same level. This is an important factor when setting the opposing premolars. Setting the Maxillary Posterior Teeth Occlusal plane
- 14. The Maxillary Premolars Setting the Maxillary Posterior Teeth Both the buccal and lingual cusp tips of the maxillary premolars should contact the plane of occlusion. The lingual cusp tips should also contact the line inscribed on the plastic plane indicating the crest of the mandibular ridge. This will ensure that when the opposing mandibular denture teeth are properly positioned and in occlusion, their central fossae will be centered over the mandibular ridge.
- 15. Setting the Maxillary Posterior Teeth The curve of Wilson and the curve of Spee begin in the molar region. The mesial lingual cusp tip of the 1 st molar contacts the occlusal plane but the buccal cusp tips and the distal lingual cusp are elevated about .5mm off the occlusal plane (yellow line) . The Maxillary 1 st Molar
- 16. The Maxillary 2 nd Molar Setting the Maxillary Posterior Teeth The set up viewed in profile. Note that the mesial lingual cusp tip touches the plane of occlusion along with the buccal and lingual cusps of the premolars. The curve of Spee begins at the 1 st molar.
- 17. The Maxillary 2 nd Molar Setting the Maxillary Posterior Teeth The curve of Spee is continued by elevating the 2 nd molar off the plane of occlusion as shown. The 2 nd molar is elevated to an even greater degree than the 1 st molar, about 15 degrees in the average patient. When viewed from the distal it is set, like the 1 st molar, with a slight curve of Wilson. Occlusal plane
- 18. Setting the Mandibular Posterior Teeth Note that with this particular posterior tooth form, the mandibular cusps tips are designed to engage the embrasures of the opposing maxillary teeth. This true of almost all anatomic tooth forms designed for bilateral balance except the Ivoclar Ortholingual. Completed set up Centric
- 19. The Mandibular 1st Molar Setting the Mandibular Posterior Teeth Begin by positioning the mandibular 1 st molar. The mesial buccal cusp tip should engage the embrasure between the 1 st molar and 2 nd premolar. Therefore adjacent marginal ridges of the maxillary premolar and molar must be at the same level for the lower molar to properly engage them.
- 20. The Mandibular 1st Molar Setting the Mandibular Posterior Teeth Check the relationship from the lingual side. Make sure that the maxillary lingual cusp tips engage the the central fossa of the mandibular molar.
- 21. The Mandibular 1st Molar Setting the Mandibular Posterior Teeth Using a clear plastic ruler and the marks made on the cast check to insure that the 1 st molar is perfectly centered over the ridge. Make sure the central fossa of the molar is properly aligned over the ridge. If the central fossa is either buccal or lingual to the ridge make the appropriate adjustments. It is apparent that the molar is positioned too far to the buccal.
- 22. The Mandibular 1st Molar Setting the Mandibular Posterior Teeth Note the alignment of the central fossa.The molar is positioned too far to the buccal and should be moved towards to the lingual . If the remaining mandibular posterior teeth are arranged on this line the denture will be prone to tipping and its stability will be impaired. Line indicating the crest of the ridge After repositioning this tooth focus your attention on the maxillary posterior teeth and reposition them lingually so that the maxillary 1 st molar and 2 nd premolar properly occlude with the mandibular 1 st molar. Do not forget to move the 1 st premolar as well.
- 23. The Mandibular 1st Molar Setting the Mandibular Posterior Teeth The molar is twisted and positioned too far to the lingual. If the remaining posterior mandibular teeth are arranged along this line the space for the tongue will likely be insufficient. The molar must be moved slightly to the buccal and twisted clockwise so that the central fossa is parallel to the ridge line. Line indicating the crest of the ridge After repositioning this tooth the posterior maxillary teeth should be moved to the buccal so that they properly occlude with the mandibular molar and permit positioning the remaining mandibular posterior teeth over the ridge.
- 24. The Mandibular Premolars – Centric Setting the Mandibular Posterior Teeth Position the mandibular premolars. The buccal cusp of the 2 nd premolar should occlude with the the adjacent marginal ridges of the maxillary 1 st and 2 nd premolars.
- 25. The Mandibular Premolars – Centric Setting the Mandibular Posterior Teeth The buccal cusp of the mandibular 1 st premolar should engage the mesial marginal ridge of the opposing 1 st premolar. There should be a space between the 1 st premolar and the cuspid.
- 26. The Mandibular Premolars – Centric Setting the Mandibular Posterior Teeth Verify that the premolars are in solid centric occlusion. If lingual centric contacts are lacking, contacts in balancing position will be lacking.
- 27. The Mandibular Premolars – Working Setting the Mandibular Posterior Teeth When there is a lack of working side contacts at this stage of the setup check for the following discrepancies in the following order: Verify buccal centric Check for balancing interferences on the opposite side Slightly increase the curve of Wilson without compromising lingual centric
- 28. The Mandibular Premolars – Working Complete Denture Occlusion During the lateral excursion into working, with this cusp form, when the teeth are properly arranged, there should be no lingual cusp contacts between the maxillary and mandibular teeth.
- 29. The Mandibular Molars – Balancing Setting the Mandibular Posterior Teeth When you lack balancing side contacts at this stage of the setup, check for the following discrepancies in the following order. Verify lingual centric Check for working interferences on the opposite side
- 30. The Mandibular 2 nd Molar – Centric Setting the Posterior Mandibular Teeth Position the 2 nd molars in centric. Inappropriate positioning and angulation of the 2 nd molars can cause significant discrepancies in working, balancing and protrusive, and so you again must check the excursions carefully.
- 31. The Mandibular 2 nd Molar – Centric Setting the Mandibular Posterior Teeth Check lingual centric. Make sure that the lingual cusps of the maxillary 2 nd molar properly occludes with the central fossa of the mandibular 2 nd molar as shown.
- 32. Verify contacts in working excursions Setting the Mandibular Posterior Teeth Lack of working side contacts may be the result of: Poor buccal centric Insufficient curve of Wilson Working interferences in the 2 nd molar region Balancing interferences on the opposite side * Check these in the order cited .
- 33. Verify contacts in during balancing excursion Setting the Mandibular Posterior Teeth Lack of balancing side contacts may be the result of: Poor lingual centric Working interferences on the opposite side, particularly in the 2 nd molar region
- 34. The Central Incisors Setting the Mandibular Anterior Teeth Begin by setting the central incisors. The mesial surfaces should be on the midline.
- 35. Setting the Mandibular Central Incisors In most patients the labial surface of the mandibular incisors should be roughly perpendicular to the occlusal plane. Occlusal plane The Central Incisors
- 36. Determining the Amount of Vertical and Horizontal Overlap Setting the Mandibular Anterior Teeth The articulator is placed in the working and protrusive position, and the position of the central incisors adjusted to permit passive contact during lateral excursions. Working Protrusive
- 37. Setting the Mandibular Anterior Teeth Horizontal overlap This practice will idealize the amount of horizontal and vertical overlap and ensure that anterior guidance is not introduced into the setup. Horizontal overlap Vertical overlap
- 38. The Lateral Incisors and the Cuspids Setting the Mandibular Anterior Teeth Position the lateral incisors and cuspids in the same fashion as the central incisors. Take care not to introduce anterior guidance into the set up. The anterior teeth should be in only passive contact during lateral excursions. Working Protrusive
- 39. The Lateral Incisors and the Cuspids Setting the Mandibular Anterior Teeth Upon completion, the amount of vertical and horizontal overlap will be idealized and anterior guidance has not been introduced into the setup. Bilateral balance has been maintained.
- 40. Semi-anatomic Denture Teeth Check to ensure you have retained appropriate contacts in working, balancing and protrusive. Balancing Working Protrusive Completed set up Centric
- 41. Anatomic Denture Teeth (30 degree)
- 42. Anatomic Denture Teeth (30 degree) These teeth are arranged in the same fashion as the semi-anatomic teeth shown previously. Use the same sequence of steps as we have just shown.
- 43. Anatomic Denture Teeth (30 degree) Begin by positioning the appropriate protrusive insert, and check to ensure that the incisal guide pin is set at zero and in contact with the incisal guide table. Protrusive insert Protrusive Inserts Zero setting
- 44. Setting Anatomic Teeth (30 degree) When you are finished check to see that the posterior teeth are on plane and the posterior teeth centered over the mandibular ridge. Make corrections as necessary.
- 45. Setting Anatomic Teeth (30 degree) Check buccal and lingual centric.
- 46. Setting Anatomic Teeth (30 degree) Check to ensure you have retained appropriate contacts in working, balancing and protrusive. Balancing Protrusive Working
- 47. Trouble shooting Anatomic and Semi-anatomic Denture Teeth Lack of working side contacts Verify buccal centric. Restore centric contacts as necessary. Increase the curve of Wilson Eliminate any anterior guidance present on the working side. Check for balancing interferences on the opposite side and make adjustments as necessary.
- 48. Trouble shooting Anatomic and Semi-anatomic Denture Teeth Lack of balancing side contacts Verify lingual centric. Restore missing contacts as necessary. Eliminate any anterior guidance present on the opposite or working side. Check for working interferences on the opposite side particularly in the 2 nd molar region.
Most Viewed this Month
Sorry. No data so far.
New Lectures

Internal Links
- Maxillofacial Rehabilitation
- Oral Cancer Foundation
- Quintessence Publishing
- The Weintraub Center
Lecture Topics
- COMPLETE DENTURES
- FIXED PROSTHODONTICS
- IMPLANT DENTISTRY
- MAXILLOFACIAL PROSTHETICS
- REMOVABLE PARTIAL DENTURES
© 2024 Foundation for Oral-facial Rehabilitation. FFOFR is a tax-exempt public charity under 501 (3)(c)
- 汉语 – Lectures in Chinese
- Lectures in Spanish
- Sao Paulo, Brazil 2019
- Sponsorship
Pocket Dentistry
Fastest clinical dentistry insight engine.
- Dental Hygiene
- Dental Materials
- Dental Nursing and Assisting
- Dental Technology
- Endodontics
- Esthetic Dentristry
- General Dentistry
- Implantology
- Operative Dentistry
- Oral and Maxillofacial Pathology
- Oral and Maxillofacial Radiology
- Oral and Maxillofacial Surgery
- Orthodontics
- Pedodontics
- Periodontics
- Prosthodontics
- Gold Member
- Terms and Condition
Occlusion and malocclusion
1 Occlusion and malocclusion
Orthodontics is the speciality of dentistry concerned with the management and treatment of malocclusion. In the majority of cases, a malocclusion does not in itself represent a disease state, but rather a variation from what is considered ideal. It is therefore important for the orthodontist to have a clear definition of ideal occlusion, as this will form a basis for diagnosis and treatment planning.
Ideal occlusion
The ideal relationship of the teeth can be defined in terms of static (or morphological) and functional occlusion. Edward Angle ( Box 1.1 ) felt the key to normal occlusion was the relative anteroposterior position of the first permanent molars, which he used to define the dental arch relationship. He also recognized the importance of good cuspal interdigitation to provide mutual support for the teeth in function ( Angle, 1899 ). Almost one hundred years after Angle, Lawrence Andrews redefined the concept of an ideal static occlusion by describing it in terms of six individual keys, including an updated ideal relationship for the first molars ( Andrews, 1972 ) ( Box 1.2 ).
Box 1.1 Edward Hartley Angle
Edward Angle was an American dentist born in 1855. Originally trained as a prosthodontist, he developed an interest in occlusion and was instrumental in developing orthodontics as a specialty of dentistry. Amongst his many achievements, including developing the principles upon which most modern fixed appliances are based, Angle proposed a classification of malocclusion that is still relevant today. He suggested that normal occlusion was based fundamentally around the position of the first permanent molar teeth. If these teeth were in the correct relationship and the remaining teeth occupied a smoothly curved line of occlusion, a normal occlusion would result. Angle’s molar classification is still used today but it is now realized that first molar position is not immutable and the position these teeth come to occupy in the dental arch can be influenced by the environment.
Box 1.2 Andrews Six Keys of Occlusion
Orthodontists have traditionally based their treatment upon these static goals, with little consideration for the dynamics of occlusion or temporomandibular joints and associated musculature that forms the masticatory system. However, over the past few decades there has been a greater interest in the principles of gnathology and aspects of an occlusion in function ( Table 1.1 ). Much has been written about what constitutes an ideal functional occlusion and why it is important ( Box 1.3 ); however, an essential concept is one of mutual protection, whereby teeth of the anterior and posterior dentitions protect each other in function. Mutual protection is thought to be achieved in the presence of:
Table 1.1 Occlusal definitions
Box 1.3 How important is an ideal functional occlusion?
Advocates of an ideal functional occlusion claim it is necessary to avoid temporomandibular dysfunction, periodontal breakdown and long-term occlusal instability. Indeed, it has been suggested that orthodontic treatment is indicated in all young adults in whom the occlusion is not functionally optimal. These criteria would mean treating most of the population, as an ideal functional occlusion is not very common. For example, as many as 75% of subjects have been described as having non-working side contacts ( Tipton & Rinchuse, 1991 ), whilst a difference of greater than 2 mm has been reported between RCP and ICP for up to 40% of orthodontic patients ( Hidaka et al., 2002 ). So does this matter? Whilst artificially creating non-working side interferences can increase the signs and symptoms of temporomandibular dysfunction ( Christensen and Rassouli, 1995 ), the results of occlusal equilibration, when an idealized functional occlusion is created, are equivocal. Canine guidance has been reported to reduce electromyographic (EMG) activity of the muscles of mastication ( Christensen and Rassouli, 1995 ) but the reproducibility of EMG is open to question ( Cecere et al., 1996 ). There does appear to be a relationship between temporomandibular dysfunction and large slides from RCP into ICP ( Solberg et al., 1979 ) although the correlations between other traits of malocclusion and temporomandibular dysfunction are generally weak ( Egermark-Eriksson et al., 1981 ). So by treating to an ideal functional occlusion does it eliminate or reduce temporomandibular dysfunction? Unfortunately, there is a lack of evidence to support this, or the claim that it results in greater long-term stability ( Luther, 2007a, b ). Therefore, while any treatment should aim for an ideal functional occlusion, if it is not achieved, there do not appear to be long-term serious consequences to the patient.
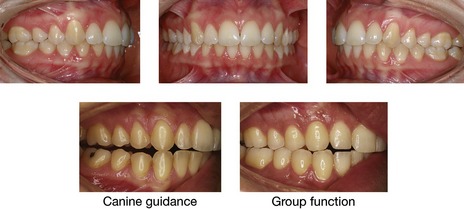
Figure 1.1 Ideal untreated occlusion.
The incisor, canine and molar relationship are class I, the dental arches are well aligned and there are no transverse discrepancies. In lateral excursion there should be either canine guidance or group function.
In reality, an ideal static or functional occlusion is rarely found in Western societies ( Fig. 1.1 ), which have a high occurrence of various traits of malocclusion.
Classification of malocclusion
Malocclusion can be defined as an appreciable deviation from the ideal that may be considered aesthetically or functionally unsatisfactory. Malocclusion has been described in numerous ways, ranging from specific classifications to indices of treatment need and outcome. Unlike a disease process, when the presence of specific features classifies the disease, a wide range of occlusal traits can constitute a malocclusion. However, within this spectrum, certain features can be identified for the purpose of classification, which allows communication and a basis for diagnosis. For any classification to be of use it needs to be simple, objective and reliable.
Molar classification
Angle classified occlusion according to the molar relationship and this remains the most internationally recognized classification of malocclusion. When looking at ideal occlusion, Angle found that the mesiobuccal cusp of the upper first permanent molar should occlude with the sulcus between the mesial and distal buccal cusps of the lower first permanent molar ( Fig. 1.2 ). He therefore based his classification of occlusion on this relative mesiodistal position:
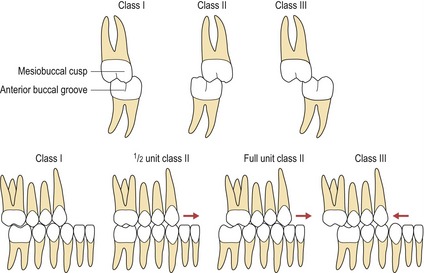
Figure 1.2 The Angle molar classification.
The buccal segment occlusion can be further defined in relation to the degree of mesial or distal occlusion and this is usually measured in units of tooth space.
In clinical practice, it is common to describe molar relationships in terms of half or even a third of a tooth unit of a class II or class III relationship ( Fig. 1.2 ). However, a basic premise of the Angle classification is that the first permanent molars hold a fixed position within the dental arch, which is not necessarily the case. Early loss of deciduous teeth can influence their position and distort the molar relationship and this classification can also be difficult to apply when there is an asymmetric molar relationship. These problems can lead to low levels of inter-examiner agreement ( Gravely and Johnson, 1974 ).
Canine classification
The canine relationship also provides a useful anteroposterior occlusal classification:
Similarly to the molar relationship, the severity of the canine relationship can also be described in terms of tooth units and can be inappropriately influenced by local factors such as crowding ( Fig. 1.2 ).
Incisor classification
A more clinically relevant method of classifying malocclusion is based upon the relationship of the maxillary and mandibular incisors. This represents a truer reflection of the underlying skeletal base relationship and also highlights what is often of most concern to the patient. It is essentially the Angle classification, as applied to the incisor teeth, and is defined upon the relationship of the mandibular incisor tip to the cingulum plateau of the maxillary central incisors ( Fig. 1.3 ), being included in the British Standards Institute’s Glossary of Dental Terms :
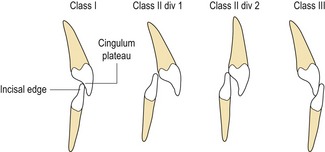
Figure 1.3 British Standards Institute incisor classification.
Confusion can arise when the upper incisors are upright or retroclined, but with an increased overjet. This has led to the introduction of a class II intermediate classification ( Williams and Stephens, 1992 ):
In reality, an increased overjet with retroclined upper incisors is within the descriptive range of class II division 2.
Prevalence of malocclusion
Malocclusion has been described as a disease of Western societies, and certainly within developed polygenic societies, certain occlusal traits such as crowding are more common. Indeed, from data generated by population studies, the presence of one or more traits of malocclusion is very common. In the USA, noticeable incisor irregularity is present in the majority of adults, with only 34% having well-aligned mandibular incisors and 45% well-aligned maxillary incisors. In addition, about 20% of the American population has a marked deviation from the ideal sagittal jaw relationship, with 2% of these being disfiguring and at the limit for orthodontic correction ( Proffit et al, 1998 ). Within the UK, the last Child Dental Health Survey found around 35% of 12 year olds with a definite need for orthodontic treatment on dental health or aesthetic grounds, which increased to 43% when those already in treatment were included ( Chestnutt et al, 2006 ).
Ethnicity also has a significant bearing on malocclusion. Class II problems are commoner in white populations of northern European descent, whilst class III malocclusion is a common trait amongst Chinese and Japanese societies. Amongst African-Caribbean populations, anterior open bite is more common than in Caucasians who, in turn, have a greater proportion of increased overbite.
Aetiology of malocclusion
A malocclusion should be regarded as a developmental condition and does not represent a single entity. Rather, it is the sum of a number of complex occlusal traits, which demonstrate multifactorial inheritance. Although in certain cases specific factors and pathologies can be identified as the cause of a malocclusion; in the majority, the aetiology is less clear. In each individual there is a close interaction between genetics and the environment during development and growth of both the jaws and dentition; it is at this interface that the aetiology of malocclusion lies ( Box 1.4 ).
Box 1.4 Nature versus nurture?
How much a malocclusion is due to the genetic makeup of an individual or the environmental influence upon growth and dental development is the key to understanding the aetiology of malocclusion. The forefathers of modern orthodontics thought that malocclusion was a disease of civilization and that by re-establishing normal jaw function and occlusion; a stable treatment result would be achieved. With a greater understanding of genetics and inheritance, as well as the introduction of cephalometric radiography, it was thought that malocclusion resulted from inherited factors. Therefore, treatment became directed at correcting malocclusion within the existing facial skeleton and soft tissue envelope; both cephalometric and clinical treatment goals were developed, often based around the position of the mandibular incisor teeth. More recently, as science has moved away from simple Mendelian genetics, there has been a shift back to examining the environmental causes of malocclusion. This has also led to renewed interest in treatments that attempt to modify jaw growth.
Evolutionary trends
Comparison of large population studies with archaeological records confirms that malocclusion has become more common over the past 1000 years. In fact, epidemiological data show that the increase in human occlusal variation has been rapid, taking place within a couple of generations, occasionally even from one generation to the next ( Weiland et al, 1997 ). A rapid change such as this would imply a significant contribution from a changing environment, such as has occurred with increasingly urbanized and industrialized societies ( Corruccini, 1984 ). It has been hypothesized that dietary changes in modern societies, with increased consumption of soft, energy-rich food, has resulted in less interproximal wear between the teeth. Research on aboriginal and stone aged populations has demonstrated this lack of attrition as a possible cause of malocclusion, particularly crowding ( Begg, 1954 ). However, it has been shown that the amount of tooth material lost in each quadrant by interproximal wear is not more than 2 to 3-mm ( Fig. 1.4 ).

Figure 1.4 Well-interdigitated class I dentition showing diet-related occlusal interproximal wear.
A soft diet may also result in underdevelopment of the jaws and a lack of arch space, leading to crowding. According to this hypothesis, hard diet requires vigorous mastication, stimulating the growth of facial bones, particularly in the transverse dimension of the maxilla and mandible. Tooth wear is merely a by-product, brought about by diet-related attrition and high masticatory activity, and has only a minor effect on tooth alignment. Experimental studies have shown that dietary consistency and masticatory activity affect not only the masticatory muscles, but also many aspects of bone growth, including bone size and mass, internal bone structure, and craniofacial size and morphology ( Varrela, 2006 ).
Genetic influences
Genetically homogenous societies exhibit low levels of malocclusion compared to heterogeneous societies and a significant genetic component appears to exist for many individual dental and occlusal anomalies. Early animal experiments initially put forward a compelling argument for a genetic component to malocclusion, based upon inbreeding of dogs, culminating in gross facial deformity. It later emerged that these studies were flawed, merely segregating mutations for specific traits such as achondroplasia, which are present in many breeds of small dog, but rare in humans.
Until recently, most information on the relative contribution of genetic factors to malocclusion has been gained from family studies and the twin method. Monozygotic twins are genetically identical, whereas dizygotic twins only share 50% of their genetic makeup. Therefore, by comparing the differences in occlusal traits between pairs in both groups, some indication of the genetic influence on a particular trait is given; the larger the difference, the greater the genetic effect ( Corruccini et al, 1990 ). This assumes that the environmental effects are similar for both groups.
Many developmental dental anomalies have been shown to occur together and have a strong familial trend. An example of this is development of a palatally impacted maxillary canine, which is more common in females and certain ethnic groups and is often associated with microdont or absent lateral incisors ( Peck et al, 1994 ). Similarly, jaw growth appears to be mostly genetically determined. A higher correlation has been shown between patients and immediate family than in unrelated subjects for class II division 1 malocclusion, which supports a polygenetic inheritance, particularly in relation to mandibular retrognathia. However, environmental factors, such as lower lip position and digit sucking, can also play a part. Mandibular prognathism, found in class III malocclusions, seems to have a high genetic predisposition, as demonstrated by the high familial inheritance and variation amongst different ethnic groups. More robust evidence for this exists from studies of siblings and first degree relatives ( Litton et al, 1970 ; Watanabe et al, 2005 ).
Dental arch size and form seems to be more subject to environmental influences ( Cassidy et al, 1998 ). Dental crowding represents a discrepancy between the size of the teeth and the size of the dental arch. Tooth development, including the size, form and presence of teeth within a dentition, is under strong genetic influence. However, the main aetiological factor in crowding appears to be arch size as opposed to tooth size ( Howe et al, 1983 ).
Large population studies have also investigated the influence of population admixture and inbreeding on malocclusion. Generally, the results of these epidemiological studies have shown a greater genetic influence on skeletal relations and arch size and a lower heritability of dental variables such as overbite, molar relationships and crowding, suggesting a greater environmental influence. The importance of hereditary factors also appears to increase with severity of the malocclusion. Although craniofacial form and growth may be under genetic control, the reason that siblings often present with similar malocclusions is probably related to their similar responses to environmental influences. Therefore, while malocclusion appears to be acquired, the underlying genetic control of craniofacial form will tend to divert siblings into similar physiological responses, resulting in the development of similar malocclusions ( King et al, 1993 ).
These studies have also shown that malocclusion does not follow simple Mendelian inheritance, but rather polygenetic or epigenetic transmission, when the interaction of genes with each other and the environment during development determine the phenotypic variation of the trait. Therefore, each would have an additive effect, showing variation along a continuous scale for traits of a malocclusion, which is exactly what happens. Theoretically, in genetically isolated communities, alleles for these traits may be expressed more frequently, giving an indication which have a greater genetic component. Island studies investigating the effects of inbreeding on malocclusion support this polygenetic theory of transmission for certain traits such as overjet and overbite ( Lauc et al, 2003 ).
Environmental factors
The developing dentition is under the influence of resting soft tissue pressure form, and function: lying in a position of muscular balance or equilibrium ( Proffit, 1978 ). Teeth erupt under the influence of the lips and cheeks on one side and the tongue on the other. Abnormal soft tissue patterns seen in those with persistent digit-sucking habits or lip incompetence, with the lower lip trapped behind the upper incisors in function, may predispose to an increased overjet. An alteration in tooth position can also arise when there is a change in this balance of force. Possible causes may be physiological, habitual or pathological and may impact on the lips, cheeks, tongue and periodontal tissues.
Physiological factors
A physiological adaptation can take place in the presence of a skeletal base discrepancy. When teeth erupt, they do so under the influence of soft tissue pressure from the lips, cheeks and tongue. There is a tendency, most notably in the labial segments, for them to upright or procline towards teeth in the opposing arch. This is most often seen in class III skeletal cases, with proclination of the upper incisors and retroclination of the lowers ( Fig. 1.5 ).

Figure 1.5 Class III malocclusion showing incisor dentoalveolar compensation.
The mandibular incisors have retroclined in an attempt to achieve a class I incisor relationship in the presence of a class III skeletal base.
Soft tissue envelope
The zone of balance between the lips and cheeks and tongue can in part dictate where the teeth sit. If the forces are imbalanced it can result in tooth movement. Many children have lip incompetence:

Figure 1.6 Lip trap contributing to an increase in overjet.

Figure 1.7 Strap-like lower lip.
Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
Related posts:
- Prenatal development of the craniofacial region
- Development of the dentition
- Management of the developing dentition
- Adult orthodontics
- Cleft lip and palate, and syndromes affecting the craniofacial region
- The orthodontic patient: examination and diagnosis
Stay updated, free dental videos. Join our Telegram channel
Comments are closed for this page.

VIDEdental - Online dental courses

- Email: [email protected]

- Periobasics A Textbook of Periodontics and Implantology
- Text Book of Basic Sciences for MDS Students
Occlusal adjustment / harmonization in periodontics
Introduction to occlusal trauma.
Occlusal trauma is detrimental to periodontal health. It may act as a cofactor which can increase the rate of progression of an existing periodontal disease. Thus, elimination of occlusal trauma is essential to achieve complete periodontal health. The first and foremost principle for the initial treatment of patients diagnosed with periodontitis with slow, moderate or rapid rate of disease progression in which the etiologic factors are both bacterial plaque and occlusal factors, is to eliminate and control first the plaque and then the occlusal factors, except where delay may unfavorably influence treatment of occlusal abnormalities, or cause discomfort to the patient. The end point of the occlusal therapy should be to achieve stable occlusion with the least interference to plaque control and periodontal maintenance. The following treatment modalities can be used to treat the occlusal abnormalities as a part of periodontal treatment,
- Orthodontic treatment.
- Restorative treatment.
- Occlusal adjustment.
Orthodontic treatment
It is an established fact that there is no significant relationship between malocclusion and severity of the periodontal disease. So, orthodontic treatment should not be considered as a routine treatment for preventing or treating periodontitis. However, there are specific situations where orthodontic treatment is essential to achieve optimal results of periodontal therapy. In the following situations, orthodontic treatment becomes essential to achieve periodontal health,
- Impinging overbite where trauma to gingival tissue is causing gingival recession. In extreme cases, a combination of orthodontic and surgical procedures may be required.
- Lack of lip seal and mouth breather’s gingivitis may indicate the need for orthodontic treatment.
- Up-righting of tipped teeth helps in reducing periodontal pocket depth as well as facilitate restorative treatment and plaque control.
- Presence of anterior cross-bite is an important indication for orthodontic treatment. It is accompanied by an unstable jiggling type of occlusion, which seems to aggravate periodontitis.
- Extensive open bite with contacts only on the last molars often has associated periodontal problems and orthodontic treatment may be beneficial.
- Correction of severely malpositioned teeth improves the long-term prognosis of the dentition.
- Orthodontic intrusion of anterior teeth with advanced periodontal destruction may help in improving their periodontal support.
It must be noted here that, orthodontic treatment should be done only when inflammation in periodontal tissues has subsided following scaling and root planing and the patient is maintaining good oral hygiene. Tooth movement in the presence of gingival inflammation may be detrimental.
It is a procedure by which the resistance of a tooth to the occlusal forces is increased by joining a neighboring tooth or teeth. It is a well-accepted treatment used to control irreversible tooth mobility through mechanical stabilization. It stabilizes the mobile teeth by forming a firm unit, thus minimizing tooth mobility and greatly improving the occlusal function of teeth. It not only ensures the retention of the periodontally compromised teeth, but also positively affects their longevity in the oral cavity. Splinting may be done for short term or long term. The primary objective of splinting is to ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book……..

Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
Buy with Instamojo
International Users:
Buy with PayPal
Restorative treatment
Restorative treatment is sometimes essential to achieve periodontal health. Food impaction, impinging overbite or various forms of unstable occlusion require restorative treatment. Permanent splints are also a component of restorative treatment. It should be noted here that permanent splinting of teeth should be considered only after other forms of occlusal therapy have been ruled out as being inadequate.
Occlusal adjustments
In order to have a healthy masticatory system, periodontal trauma because of faulty occlusion should be treated. A successful adjustment in the occlusal abnormalities results in occlusal stability. Occlusal adjustment may also eliminate food impaction and gingival impingement in some instances. It should be remembered that because occlusal adjustment involves removal of tooth structure and is an irreversible treatment, it should be carried out only after a definite diagnosis has been made regarding the presence of a traumatic lesion rather than the presence of any occlusal interferences, which may be ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book……..
Indications for occlusal adjustment
It must be remembered that occlusal adjustments result in changes in occlusal scheme. It is an irreversible treatment so should only be planned with great care. Even minor mistakes made during the occlusal adjustment may result in worsening of the situation. Following are the indications for occlusal adjustment,
- The presence of parafunctional habits in conjunction with occlusal disharmony.
- Signs of occlusal trauma, excessive occlusal attrition, and/or TMJ dysfunction.
- The presence of multiple restorations on posterior or anterior teeth, which require occlusal adjustment to achieve a harmonious occlusion.
- To eliminate occlusal interferences after the orthodontic treatment is finished.
- Some clinicians also recommend prophylactic occlusal adjustments in the absence of any periodontal or TMJ symptom to prevent future problems.

Evaluation of TMJ and occlusion
A precise occlusal history should be recorded before any occlusal examination is done. The details of the history depend on the type of occlusal symptoms and their severity. The patient’s problems and their duration should be recorded in a chronological order. The patients usually cannot relate the occlusal problems with their symptoms. So, appropriate questions should be asked to establish any relation between the patient’s symptoms and occlusal abnormalities. Para-functional habits are the most common cause of occlusal problems. So, the patient should be asked questions about the history of pain in teeth, periodontium or TMJ and associated musculature.
The patient should be asked questions like: “Do you have your teeth in tight contact when you wake up? Do you feel tiredness in the jaws on waking up?” Any positive answer indicates parafunctional habit. The patients usually do not know about night grinding. So, any other person sleeping with the patient should be asked about ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book……..
Extra-oral examination
The patient should be made to sit in a semi-recline position with head slightly tipped back. The head should be supported by the headrest. Any facial asymmetry should be noted and the cause of abnormality should be detected. The patient should be asked to open and close the mouth slowly. Any deviation during mouth opening or closing should be noted. The TMJ examination should be done by lateral palpation of the joint and auscultation of the joint should be done (For more detail, “Art of history taking in periodontics” ). The muscles of mastication should be palpated for any tenderness.
Intra-oral examination
The intra-oral examination of the patient should be done to identify any occlusal interference. It must be emphasized here that any single positive sign should not be considered as diagnostic of the occlusal problem, but should be related carefully to other findings. The following steps are followed while recording functional occlusion,
- The static relation between maxillary and mandibular teeth i.e., centric occlusion (CO) position should be determined first.
- Overjet, overbite and freeway space should be determined.
- Any occlusal variation in the occlusion plane, cross-bite, open bite, extrusion etc. should be recorded.
- Wear facets and their distribution should be recorded. It should be remembered that the presence of wear facets is related to patient’s age.
- The presence of wear facets is not always pathognomonic of traumatic occlusion. So, it must be correlated with other findings.
- Tooth/teeth with increased mobility should be identified. Along with increased tooth mobility, increased tooth sensitivity to thermal changes and to percussion should also be checked because these findings can also be due to occlusal trauma.
- Any tooth migration should be recorded. Tooth migration associated with an occlusal abnormality is usually associated with wear facet.
- Tooth migration without wear facets is usually associated with abnormal tongue habits or atypical swallowing habits.
- Radiographic examination of teeth with mobility or migration should be done. Loss of bone support or changes in periodontal ligament space are indicative of trauma from occlusion.
Diagnosis of occlusal interferences
An “occlusal interference” is any tooth contact that inhibits the remaining occluding surfaces from achieving stable and harmonious contacts 15 . Very small interferences up to 15 µm can trigger an untoward response such as tooth pain or mobility 16, 17 . Hence, these interferences must be eliminated to achieve a stable and harmonious occlusion. In a harmonious occlusion without any interference, the occlusal contact time simultaneity, by definition implies that a time of 0 seconds elapses between the first and the last occlusal contact 18 . In other words, we can say that all the occluding surfaces of the mandibular teeth come in contact with the maxillary teeth at the same instant during the mandibular closure.
There are four types of occlusal interferences:
- Non-working.
- Protrusive.
Armamentarium required for diagnosing and correcting occlusal interferences
The armamentarium used to record functional occlusion includes occlusal indicators (described below), cotton rolls, dental mirror, hand mirror, abrasive disks and wheels, cutting and abrasive burs, polishing burs and rubber polishing cones. The findings of the occlusal examination should be recorded on a chart which consists of columns for recording all the significant occlusal parameters.
Occlusal indicators are essential components of recording functional occlusion. Occlusal indicators can be divided as qualitative and quantitative indicators. The primary difference between the qualitative and quantitative indicators is that quantitative indicators are capable of recording the tooth contact events.
Qualitative indicators:
- Articulating paper.
- Articulating silk.
- Articulating film.
- Metallic shim stock film.
- High spot indicator.
Quantitative indicators
- T-Scan occlusal analysis system.
- Virtual dental patient.
Qualitative indicators
Articulating papers:.
Articulating papers are the most commonly used occlusal indicators. These consist of a coloring agent and a bonding agent between the two layers of the film. On making tooth contact, the coloring agent is expelled from the film and the bonding agent binds it onto the tooth surface. In areas with heavy contact, the dye spreads peripheral to the actual location of the occlusal contact making a central area that is devoid of the colorant surrounded by a peripheral rim of the dye. The central area of the contact indicates interference and requires correction. Articulating papers are available with different width, thickness and ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book……..

Articulating silk:
A better way to avoid pseudo-markings is to use an articulating silk. It is made up of micronized color pigment, embedded in a wax-oil emulsion. However, it should be remembered that its marking capability is lost if the staining components are dried. Secondly, contamination of the field by saliva spoils the markings. Hence, it should be used in a dry field and should be stored in a cool and closed environment. It can be used on highly polished surfaces which is its important advantage over articulating papers.
Articulating films:
These are made up of emulsion ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book……..
Thin sheets of dark-colored wax are available which can be placed over the occlusal surfaces of the teeth in one arch. The opposing teeth are tapped gently into the wax until it perforates. The perforation represents interfering contacts. These are then marked with pencil and reduced. Waxes are very useful in identifying interferences on sharp line angles.
Metallic shim stock films:
These contain metallic surface on one side and coloring agent on the other side of the film. These are primarily used to accurately mark the contacts on the soft splint.
High spot indicators:
These are also used in the laboratory to check the proximal contacts of crowns, inlays, onlays, telescopic crowns and clasps. These are supplied in the form of a liquid which is applied over the proximal areas where it forms a thickness of 3 µm.
Quantitative indicators:
T-scan occlusal analysis system:.
This is a quantitative indicator which provides contact sequence in 0.01 second increments. The main advantage of this scan is that it identifies time magnitude along with the distribution of the occlusal contacts. The device consists of a piezoelectric foil sensor, a sensor handle and software and hardware to record the data. The foil sensor is placed between the maxillary and mandibular arches and an arch support is placed between the maxillary central incisors of the patient. After the recording button is pressed, the patient is asked to close his/her mouth slowly in the maximum intercuspation position without making any lateral movement.
The sequence of ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book……..
Virtual dental patient:
This is a recently introduced technology wherein patient’s dentition casts are scanned and a three-dimensional virtual occlusion is established. The functional movements on this virtual model provide us the quantitative information regarding the occlusal interferences. Similar to the T-scan, the sequence of the occlusal contacts, enables us to eliminate the initial contacts and hence the interferences.
Determination and recording of CR and CO position
The patient should be seated in a reclined and comfortable position in the dental chair with the head properly supported by the headrest. The patient should be asked to take a deep breath and relax the body as much as possible. The patient is asked to look in front and to keep the head stable during manipulation of the lower jaw.
Now, the little finger is placed slightly behind the angle of the jaw and remaining three fingers on the border of the mandible. The thumb is placed over the notch over the sym-physis. The patient is asked to open and close the mouth and the hinge movement of the mandible is felt. A firm pressure is then applied with fingers in an upward direction and with the thumb in a downward and backward direction to position the condyle of the mandible in terminal hinge position. It must be made sure that the manipulation of the mandible in the terminal hinge position should be totally free of any muscular influence. The position is then again verified by repeating the procedure. While the terminal hinge position is verified repeatedly, the patient is asked to gently close the mouth.
Sometimes, the patient complains of pain or discomfort while positioning the mandible in terminal hinge position. It indicates that the condyle meniscus assembly has not been braced against the bone. In such a situation repositioning of the mandible is done by placing cotton rolls between anterior teeth or by placing Hawley’s bite plane.
Once the CR position is well established, an articulating paper (preferably blue) is placed with the help of Miller’s forceps between the occlusal surfaces of teeth on the side making initial contacts. To avoid pseudo markings, thin articulating paper such as GHM occlusion foil (Hanel-GMH Dental GMBH, Nurtingen, Germany) which has 19 μm thickness should be used. The patient is then asked to slowly close the mouth to make contact of maxillary and mandibular teeth. The pair of teeth, making initial ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book……..
Registration of lateral and protrusive excursions
The lateral excursive movements are preferably recorded with a different color (such as red) than used for recording CR and CO. A dental tape is placed between the teeth of the patient on the right side and with the help of hand pressure mandible is moved to the right. Teeth with red marks are recorded on the occlusal chart. A similar procedure is then repeated on the left side and markings are recorded on the occlusal chart. A hand mirror can be given to the patient if he/she faces difficulty in performing lateral excursions. The protrusive excursion movements are recorded by gliding the teeth forward from the CO position without any lateral movement.
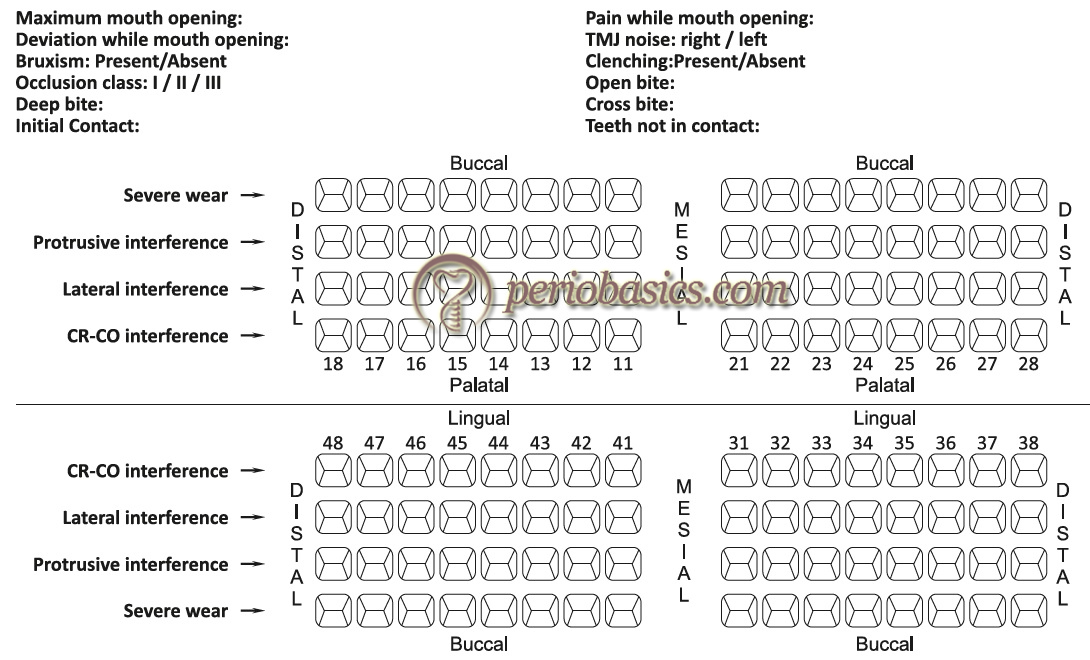
Now, the dental tape used to record CO and CR position is placed between the teeth and the patient is asked to bring teeth in CO position. The CO points of contact will superimpose on the lateral and protrusive contacts. The CO contact points (blue) can be differentiated from the lateral contacts (red) by their color difference.
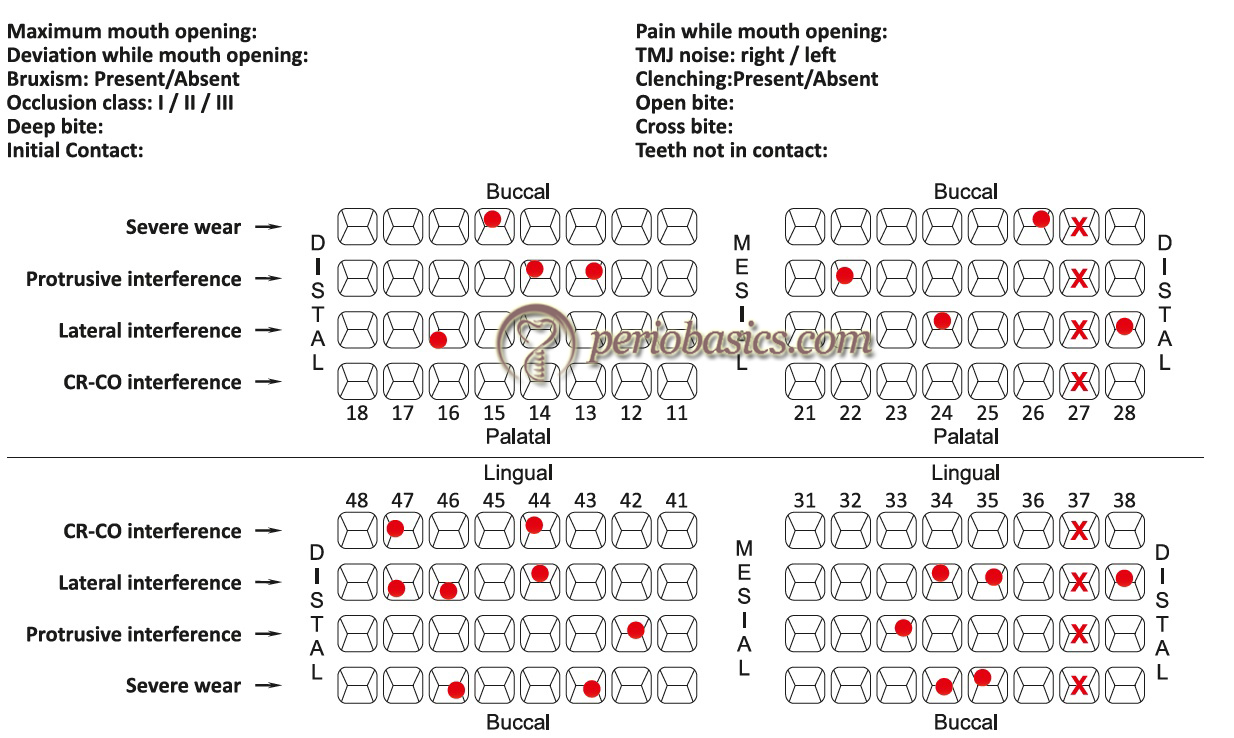
Impression making and articulator analysis
Although the information gathered from contact point markings in CR, CO, lateral and protrusive positions are sufficient to identify the occlusal interferences; but for accurate diagnosis and treatment planning, the impressions are ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book……..
Types of occlusal therapy
Occlusal therapy is any treatment that alters a patient’s occlusal condition. It can be used to improve the function of the masticatory system through the influence of occlusal contact patterns and by altering the functional jaw position. Occlusal therapy can be reversible or irreversible. Reversible therapy temporarily alters the occlusal condition, the joint position, or both. The example of this therapy is occlusal splints. The disadvantage of reversible occlusal therapy is that the original condition might return after the therapy is discontinued. On the other hand, irreversible therapy permanently alters the occlusal condition so that the original condition cannot be recovered. The examples of irreversible occlusal therapy include selective grinding, fixed prosthetic procedures, and orthodontic therapy. In the following sections, we shall discuss in detail the irreversible occlusal therapy (selective occlusal grinding).
Principles of selective grinding
The clinical procedure to eliminate occlusal interferences consists of three procedures, namely grooving, spheroiding and pointing 19. Grooving is done to re-establish the depth of developmental grooves. Spheroiding is done to restore the original tooth contour in areas with supra-contacts. Once the supra-contacts have been identified, the burs are applied with a paint brush like manner over the markings and reshaping is done up to 2-3 mm mesially and distally from the marking and 2-3 mm apical to the marking. The cusp height should be maintained during this procedure. In situations where ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book……..
Steps in the correction of occlusal interferences
Once the occlusal interferences have been identified, the clinician must determine the extent of occlusal adjustments required. As already stated, these adjustments should be first performed on the articulated casts and then should be duplicated on the patient. Another important factor to be considered while doing occlusal adjustment is the age of the patient. In younger patients, usually conservative approach is adopted because they have a developing dentition which may have many unpredictable mechanisms for occlusal harmonization. Only minor occlusal adjustment, interceptive in nature is adopted in these patients. On the other hand, in older patients extensive occlusal adjustment can be planned.
Basic principles followed to eliminate occlusal interferences
The selective occlusal grinding is done to eliminate the occlusal interferences in a stepwise manner. These are,
Step 1: Elimination of retrusive supra-contacts and deflective occlusal interferences from CR to CO. Step 2: Adjust CO to achieve stable, simultaneous, multi-pointed, widely distributed contacts. The unbalanced cuspal inclines and contacts should be eliminated to maintain or move the force vectors along the long axis of the tooth. Step 3: Test for excessive contact (fremitus) on the incisal teeth. Step 4: Remove posterior protrusive supra-contacts and establish contacts that are bilaterally distributed on the anterior teeth. Step 5: Remove all interferences to lateral excursions. Step 6: Eliminate gross occlusal disharmonies. Improve the occlusal anatomy by maintaining the cusp form, by creating correct marginal ridge relationships, cusp-fossa relationships, elimination of broad facets and narrow occlusal tables. Step 7: Re-check tooth contact relationships. Step 8: Polish all rough tooth surfaces.
Following is the detailed description of these steps,
The first step in the elimination of occlusal interferences is to remove these interferences in retrusive and CR to CO position. The primary objective here is to remove the supra-contacts and remove interferences that interfere with posterior border closure of the mandible to a stable bilateral RCP. The clinician should try to achieve following objectives by removing these interferences,
- A maximum number of centric holding contacts are achieved in CR position.
- Vertical dimension in CR should be same or a little more than in CO position.
- Removal of interferences from CR to CO position, thereby facilitating smooth gliding movement in the horizontal plane from CR to CO.
The interferences are identified by placing blue marking tape between the teeth and asking the patient to “Squeeze” once the initial contact is made. Most commonly the mesial inclines of the maxillary lingual cusps and their opposing tooth surfaces are typical sites for supra-contacts. The mesial inner incline of the lingual cusp of the maxillary first premolars is the most common initial supra-contact at the RCP.

The second step is to achieve stable centric contacts in CO position. The occlusal contacts in the CO position should be planned in such a way that maximum stability of occlusion in this position is achieved. The primary objectives of clinician during this step are,
- Achieving a cusp to fossa relationship wherever possible as compared to cusp to marginal relationship. The cusp should contact, preferably at the center of the fossae so that occlusal forces are directed along the long axis of the tooth. However, it should be remembered that in unworn teeth (young patients), the cusp tips do not reach the base of the fossa. In such situation, multiple contacts on the inclined planes are considered as stable centric holding contacts.
- There should be no cusp contacts with the inclined planes except for the lingual surfaces of the maxillary anterior teeth.
The patient is asked to tap the teeth together on both sides at the same time. This is CO position where the maxillary and mandibular teeth are in maximum contact. Now, the wax is placed ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book……..
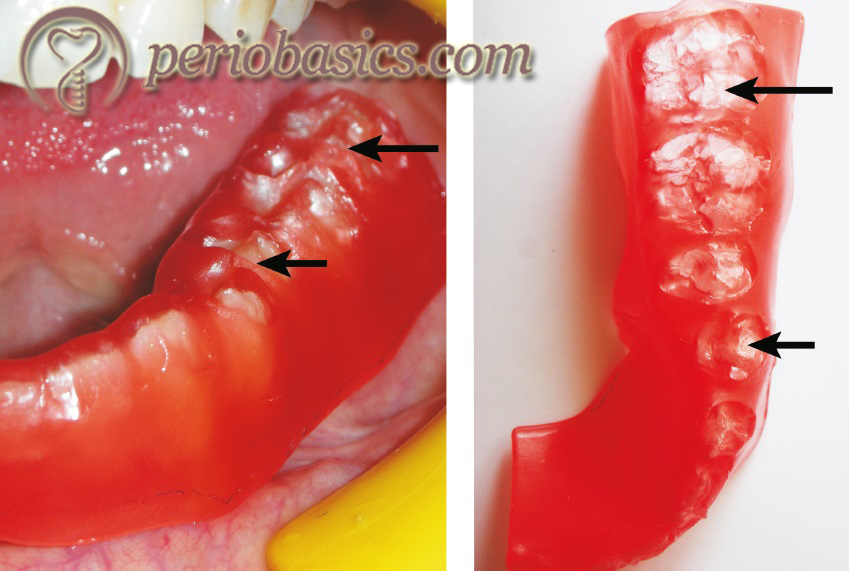
The third step is to remove excessive contacts from incisal surfaces. The objectives of this step are,
- Making the incisors slightly out of contact or in light contact over the maximum number of teeth.
- Eliminating supra-contact and hence trauma from occlusion on anterior teeth.
The firmness of the occlusal contact can be detected by placing a Mylar occlusal strip between the maxillary and mandibular anterior teeth held with a hemostat. The strip should just ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book……..
Protrusive excursion refers to the path of the mandible as it moves anteriorly between the CO and the edge to edge relationship of the anterior teeth (Figure 34.8). In this step, adjustment in protrusive excursions is done. The primary objectives of the dentist during this step are,
- Even distribution of contacts during protrusive excursions over as many teeth as possible. During the protrusive excursion, there should be no contact between the posterior teeth, except between the mesial slope of the buccal cusp of mandibular first premolar and the distal slope of maxillary cuspid.
- Reduction of the incisal edges of the extruded anterior teeth if they are interfering with the smooth protrusive excursion.
- Elimination of deep overbite by reduction of crown length of the anterior teeth. However, it must be remembered that it does not eliminate the requirement of orthodontic treatment. Only slight overbite can be eliminated by selective grinding. Moderate to severe cases require orthodontic treatment for deep bite correction.
The patient is asked to protrude the mandible slowly from CO position to edge to edge position of anterior teeth. Ideally, there should be bilateral contacts between maxillary and mandibular anterior teeth during this movement with little or no deviation of the mandible. The deviation usually is caused by a ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book……..

However, it should be preferred that wherever possible the adjustment is confined to the maxillary teeth to protect mandibular functional cusp height. Mandibular incisors should be ground only when the limit of grinding of the maxillary teeth has been reached because of pain, proximity to the pulp, or esthetic reasons. Following selective grinding, all the marks are removed and the patient is again asked to perform the protrusive movement. If posterior teeth are interfering with the protrusive movement, tooth structure is removed from the offending cusps until all articulating contacts between the posterior teeth have been eliminated.
This step deals with the removal or lessening of all interferences in lateral excursions. The mediotrusive interferences usually manifest as oblique facets on the first and second molar teeth on the inner inclines of the mandibular buccal cusps and the inner inclines of maxillary lingual cusps. The objectives of the dentist while eliminating lateral interferences are,
- A slight cuspid mediated disocclusion of the posterior teeth during the lateral excursion except in situations where cuspid is already worn and group function occlusion is present or cuspid is malposed and adjustment to group function of posterior teeth is necessary.
- Elimination of interferences on working side and balancing side.
- Elimination of interferences on central and lateral incisors which hinder the cuspid function during the lateral excursion except when both central and lateral incisors are in group function with cuspid and show no sign of trauma from occlusion.
While registering the lateral interferences, both habitual and passive (border) manipulation of the mandible is employed. A two-color method is used here in which the centric contact in CO are registered as blue and lateral supra-contacts are recorded in red color. For registering interferences on the working side, red ribbon is placed between the teeth in quadrant under question. Now, hold the mandible in CR position and ask the patient to close with moderate pressure. The patient is now asked to slide the mandible towards the right or left side, depending upon the side that has to be checked for working interferences. The red marks show interferences on the working side. Now, place a blue ribbon and without disturbing the red marks, establish the centric holding marks in CO position. To remove interferences, only undesirable red marks are removed. The inner inclines of maxillary buccal cusps or lingual surfaces of the upper anterior teeth are adjusted.

For registering interferences on the balancing side, a strip of adhesive occlusal registration wax is placed over the mandibular quadrant in question and another strip of folded occlusal registration wax is given to the patient that is placed on the opposite side and the patient is asked to chew this wax bolus up to five times. If there are ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book……..
It should be remembered that while adjusting interferences on lateral excursion, reshape the inner inclines of the maxillary buccal cusps and mandibular lingual cusps. This is because grinding of the mandibular buccal cusps jeopardizes the functional cusps in CO position. Grinding should not result in the formation of flat surfaces and vertical stops should be preserved during the procedure.
This step deals with the elimination of undesirable gross occlusal features. Once all the interferences have been removed, there may be some remaining gross undesirable occlusal features which are harmful to the periodontal structures, and require modification. These include,
Extruded teeth:
These teeth are reduced to the level of the occlusal plane by grinding and reshaping within the limits permitted by proximity to the pulp.
Plunger cusps:
Plunger cusps are responsible for wedging of food in the interdental areas. Distolingual cusps of maxillary molars often are plunger cusps. These cusps should be rounded off and reshaped to eliminate food impaction.
Uneven adjacent marginal ridges:
These may also cause food impaction and should be corrected by either reducing the height of a comparatively high marginal ridge or increasing the height of a lower one with a restoration.
Rotated malposed and tilted teeth:
The most preferred treatment for rotated teeth is orthodontic de-rotation. However, minor rotations which interfere with the functional movement of the mandible or are causing food accumulation and impaction can be re-shaped by selective grinding.
The wear facets are the result of the tooth to tooth wear. These can be easily detected by drying the tooth surface and viewing under a regular dental chair lamp. These should be corrected because the periphery of these facets may produce lateral or tipping forces which are deleterious to the periodontium.
Flat occlusal wear:
Sometimes excessive wear of the occlusal surfaces of the posterior teeth results in the formation of the flat occlusal surface. Similar to facets, the margins of the occlusal wear creates force component which causes lateral and tipping forces deleterious to the periodontium. The anatomy of the occlusal surfaces should be restored by selective grinding.
All the occlusal adjustments done are re-investigated in this step. All possible movements are done to check retrusive, protrusive and lateralotrusive interferences. In cases where occlusal equilibration can be better achieved by prosthodontic, restorative or orthodontic treatment, these treatments should be considered.
All the surfaces which have been selectively reduced are then polished to achieve smooth tooth surfaces and patient is instructed regarding the maintenance of teeth.
Correction of occlusal discrepancies prior to restorative procedures
Prior to restorative treatment, the present status of patient’s functional occlusion should be carefully evaluated. The occlusal corrections, if required, should be done prior to the restorative treatment. Dentition that requires multiple occlusal restorations either immediately or in future should be corrected for occlusal abnormalities. Following types of discrepancies are commonly observed and should be corrected prior to restorative treatment,
Marginal ridge discrepancies:
Marginal ridges of the posterior teeth that do not direct the food into the fossae promote food impaction in the inter-proximal region. Before restoring these teeth, opposing marginal ridge should be ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book……..
Tooth extrusion is observed in the case where there is a massive coronal breakdown of the opposing tooth, or more frequently, if the opposite arch is edentulous. The extruded tooth should be corrected in conjunction with the restoration of the carious tooth or rehabilitation of the edentulous areas. It can be done by grinding or reshaping if the extrusion is slight or by installing a crown if the extrusion is excessive. If the extrusion is allowed to remain, it may result in functional disorders caused by occlusal interferences. Orthodontic treatment may be done to intrude the extruded tooth if extrusion is minor. However, it is difficult to intrude molars where extrusion is commonly seen. Sometimes, extrusion is so severe that intentional endodontic treatment of the extruded tooth followed by crown placement is required.
Plunger centric holding cusps commonly result because of tipping and extrusion into a grossly carious opposing occlusal surface. The correction of the plunger cusps must be done prior to the restoration of the carious tooth. Simply reducing the height of the plunging cusp would be insufficient and would result in an excessively flattened cusp. The centric holding areas should be ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book ……. Contents available in the book……..
Broad opposing wear facets:
Broad wear facets should be eliminated by reshaping to permit the establishment of minimal centric contact areas. However, while reshaping the surface, stable centric stops must be preserved.
Wide occlusal tables:
The wide occlusal tables are usually a symptom of excessive occlusal wear. They should be narrowed to achieve stable centric holding areas by reshaping the cusp tips.
Rotated teeth:
If possible, the rotated teeth should be treated by orthodontic treatment. Orthodontic de-rotation brings the tooth in a proper position. If orthodontic treatment is not possible, moderate reshaping of the rotated tooth may improve the occlusion.
Our primary aim of the restorative treatment is not only to restore the decayed tooth or to replace the missing tooth, but also to provide a harmonious occlusion to the patient which functions smoothly without causing any discomfort to the patient. The understanding of the basic principles of occlusion is essential to achieve this goal. It should be remembered that occlusal adjustments should be well planned because an improper treatment my worsen the existing problems of the patient.
A comprehensive TMJ and occlusal examination is an inseparable part of the complete periodontal examination. The neuromuscular harmony is the prime requirement for appropriate TMJ function and functional mandibular movements. However, it should be remembered that a thorough knowledge of occlusion is required to treat the condition otherwise the situation may worsen after the treatment. Therefore, clinical examination, which consists of the examination of the TMJ, teeth, soft tissue as well as the periodontium, should be carried out before the commencement of dental treatment. The occlusal examination and identification of the interferences should be done and in a stepwise manner, all the interferences should be eliminated.
References are available in the hard-copy of the website.
Suggested reading
- Gher ME. Changing concepts. The effects of occlusion on periodontitis. Dental Clinics of North America. 1998 Apr;42(2):285-99.
- De Boever JA, Carlsson GE, Klineberg IJ. Need for occlusal therapy and prosthodontic treatment in the management of temporomandibular disorders. Part I. Occlusal interferences and occlusal adjustment. Journal of oral rehabilitation. 2000 May;27(5):367-79.
- Rothner JT. Occlusal equilibration—A part of orthodontic treatment. American Journal of Orthodontics. 1952 Jul 1;38(7):530-7.
- McKenzie JS. Mutual problems of the periodontist and prosthodontist. Journal of Prosthetic Dentistry. 1955 Jan 1;5(1):37-42.
- Becker IM. Comprehensive occlusal concepts in clinical practice. John Wiley & Sons; 2010 Dec 20.
- Popa1a ST, Popescu2b SM, Constantinescu3c MV. OCCLUSAL EQUILIBRATION BETWEEN OPTION AND CLINICAL REALITY.
- Recent Posts
- Periodontal vaccine
- Can connective tissue attachment occurs over restorative surfaces like GIC/composite/ceramic?
- What are the oral and periodontal manifestations of Ehlers-Danlos syndrome (Type IV, VIII)?
- Periodontitis as an autoimmune disease
- Subversion of the host response in periodontitis
- Basic Periodontology
- Basic Sciences
- Clinical Periodontology
- Implantology
- Recent Research
Submit Your Query or Question. Will be Back to You Soon with an Answer
Occlusal contact area of mandibular teeth during lateral excursion
Affiliation.
- 1 Section of Pediatric Dentistry, Division of Oral Health, Growth & Development, Faculty of Dental Science, Kyushu University, Fukuoka, Japan. [email protected]
- PMID: 15008236
Purpose: This study observed occlusal contacts and determined their areas on the mandibular teeth, especially the molars, during voluntary lateral excursions.
Materials and methods: Occlusal contact areas were estimated with a measurement system combining 3-D tracking of mandibular movements with 3-D digitization of tooth shape. Sixteen women with sound permanent dentitions participated.
Results: At the intercuspal position, estimated occlusal contact areas of the first and second mandibular molars were on average 12.6 mm2 and 9.0 mm2, respectively. However, after 3.0 mm of lateral excursion, their areas were sharply reduced to 2.2 mm2 and 1.5 mm2 on the working side, and 0.4 mm2 and 1.1 mm2 on the nonworking side, respectively.
Conclusion: These results suggest that the occlusal contact areas on working- and nonworking-side molars differ from each other as lateral excursion proceeds.
Publication types
- Research Support, Non-U.S. Gov't
- Bicuspid / anatomy & histology
- Cuspid / anatomy & histology
- Dental Occlusion*
- Dental Occlusion, Balanced
- Dental Occlusion, Centric
- Imaging, Three-Dimensional
- Incisor / anatomy & histology
- Jaw Relation Record / instrumentation
- Molar / anatomy & histology
- Tooth / anatomy & histology*
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 08 September 2021
Development of a biomechanical model for dynamic occlusal stress analysis
- Zheng Duanmu 1 ,
- Qi Deng 2 ,
- Yuanyuan Ren 2 &
- Meiqing Wang ORCID: orcid.org/0000-0002-7373-385X 2
International Journal of Oral Science volume 13 , Article number: 29 ( 2021 ) Cite this article
2706 Accesses
6 Citations
Metrics details
- Biomedical engineering
- Bone quality and biomechanics
The use of traditional finite element method (FEM) in occlusal stress analysis is limited due to the complexity of musculature simulation. The present purpose was to develop a displacement boundary condition (DBC)-FEM, which evaded the muscle factor, to predict the dynamic occlusal stress. The geometry of the DBC-FEM was developed based on the scanned plastic casts obtained from a volunteer. The electrognathographic and video recorded jaw positional messages were adopted to analyze the dynamic occlusal stress. The volunteer exhibited asymmetrical lateral movements, so that the occlusal stress was further analyzed by using the parameters obtained from the right-side eccentric movement, which was 6.9 mm long, in the stress task of the left-side eccentric movement, which was 4.1 mm long. Further, virtual occlusion modification was performed by using the carving tool software aiming to improve the occlusal morphology at the loading sites. T-Scan Occlusal System was used as a control of the in vivo detection for the location and strength of the occlusal contacts. Data obtained from the calculation using the present developed DBC-FEM indicated that the stress distribution on the dental surface changed dynamically with the occlusal contacts. Consistent with the T-Scan recordings, the right-side molars always showed contacts and higher levels of stress. Replacing the left-side eccentric movement trace by the right-side one enhanced the simulated stress on the right-side molars while modification of the right-side molars reduced the simulated stress. The present DBC-FEM offers a creative approach for pragmatic occlusion stress prediction.
Similar content being viewed by others

Dynamic changes in tooth displacement and bone morphometry induced by orthodontic force

An accurate and efficient method for occlusal tooth wear assessment using 3D digital dental models

Periodontal ligament and alveolar bone remodeling during long orthodontic tooth movement analyzed by a novel user-independent 3D-methodology
Introduction.
Occlusion is defined as: (i) the act or process of closure or of being closed or shut off; (ii) the static relationship between the incising, masticating surfaces of the maxillary or mandibular teeth or tooth analogues. 1 The primary function of occlusion is to chew up foods with exact tooth contacts and large forces of food-crushing. 2 Overloading may lead to tooth wear, 3 , 4 , 5 fatigue, 6 , 7 , 8 , 9 cervical lesions, 10 , 11 , 12 and cracks from the contact zone at the occlusal surface of the nature teeth. 13 , 14 Hence, dental stress under occlusal loading has been largely reported, especially in the field of restorations’ design. 15 , 16 , 17 Researches indicated that food stiffness has a slight impact on the stress distribution of the restored and sound teeth because the stress distribution does not differ particularly in the same geometrical configuration of cavity with varying stiffness of food. 18 The impact of dental geometry is then of significance because it determines the occlusion contact areas where the mastication force is focused. 19 , 20 The contact between tooth surface and food bolus alter dynamically during chewing, meaning that the masticatory forces on dentition constantly change in direction, intensity, and point of application. 21 The uneven occlusal contact surface divides the loading following the principles of force decomposition that can be transferred to roots and then the periodontal tissues. 22 The loading messages are picked up by periodontal mechanoreceptors. By activating the periodontal-trigeminal mesencephalic nucleus-trigeminal motor nucleus circuit, occlusion modifies the jaw muscles’ activity. 23 About 85% of the muscular activity necessary to chew is peripherally induced, that means, the contact stress message of the uneven occlusion takes a pivotal role in feedback controlling of the jaw muscles activity during chewing function. 24 Obviously, dental stress during simulated centric and eccentric clenching is meaningful in view of function and dysfunction of masticatory system, yet the stressing regularity during centric and eccentric clenching remains undetermined.
There are the largest contacts in the maximum intercuspal occlusion situation, while there are fewer contacts in the protrusion and lateral excursive occlusion. 25 Dynamic occlusal contacts had been discussed greatly in literatures for its interferential role. 26 , 27 , 28 The posterior contacts during protrusion and the balancing side contacts during lateral excursion had been proposed as the interferences because they might be the causes of temporomandibular disorders (TMD). 28 However, diverse reports are documented regarding the view point that the balancing interferences are harmful to oral function. Some researchers indicated no differences in the frequency of the interferences between the TMD patients and healthy peoples. 29 , 30 , 31 The limited strength information of the interferential contacts might be one of the explanations for that inconsistency. In literature, efforts had made to describe the contact features of the occlusion with strength message. For example, T-Scan system provides locational loading information with time-dependent strength relative values. An inserted transducer recorded the detection procedure of dentitions. Even though thin to 60 μm, the transducer affects the test accuracy. 32 Further, the uniformity of the transducer thickness prevents the T-scan from a real contact provider.
Direct measurements of tooth contacts and forces are difficult. Biomechanical models are better for understanding the relationship between occlusion and function. 2 In literature, the virtual simulation tool of finite element method has been widely used in mandibular lever analysis, most often on tooth or TMJ condyles. 19 , 33 , 34 , 35 , 36 In the reported finite element models (FEM), the stress analysis based on the muscle force simulation is often simplified as specific concentrate forces at particular bite locations. The jaw movements are relatively small and directional perplexing that are under fine neural control. 37 For example, muscles with a generally vertical orientation are responsible for fine horizontal regulation of movement and stabilization. 38 That means each muscle can influence more than one degree of freedom. The schematic representation of a single line of action is incomplete, so more realistic loadings are then required for bite simulation. 39
It is indicated that stress analysis can be performed based on muscle liked concentrated force and the defined displacement boundary condition. 40 Using the recorded mandibular displacement as the boundary condition, a reformative FEM, termed the displacement boundary condition finite element model (DBC-FEM) 41 could be developed where the muscular forces are no longer necessary to analyze occlusal stress. The DBC-FEM model is an explicit scheme that efficiently solves highly nonlinear problems, especially when dealing with complex contacts and large deformations. 42 Giving a uniform linear motion, the larger a contact size is, the smaller the contact stress will be. When a tooth exposes its different sites to have occlusal contacts with the opposing tooth, various stresses came out according to the contact size of the sites. Then, the stress at the contact sites could be obtained based on the contact size following the penalty algorithms 43 , 44 as DBC-FEM provides.
This paper developed a DBC-FEM by using the jaw kinematic three-dimensional movement recordings. The location and size of the dynamic occlusion contact were computed, and the derived occlusal stress was analyzed. The purpose was to explore a creative approach for occlusion stress prediction without either interrupting nature behaviors of dental occlusion or simulation of muscles force.
The data from EGN recordings are presented in Fig. 4c and Supplemental Tables 1 – 4 . The volunteer showed asymmetrical lateral excursive movements, more prominent on the right side than the left side, which were 6.9 and 4.1 mm, respectively.
Occlusion stress in the simulated centric and eccentric movements—obtaining from the tasks in section 1
The DBC-FEM model successfully revealed the shear and vertical stress at different stages of each task. Generally, the stress value changed when the contact size increased or decreased in the dynamic tasks. Three images representing the occlusal maximum stress value at the lowest, middle, and largest level in each task are presented in Fig. 1 .
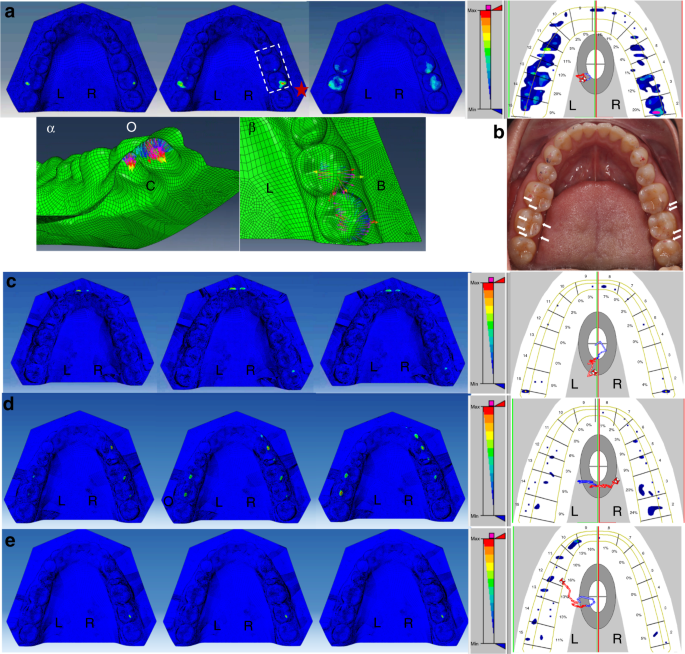
The occlusion stress representation at initial (left), middle (middle), and end (right) stage of the simulated contact and the representative T-scan occlusion recordings of the four defined dynamic tasks. The typical locations of the maximum stress are marked with red stars in each panel. a Centric closing; the image of the local sites with the highest values of the maximum stress were squared and magnified in panels α the bottom view, and β the top view. b the articulating papers measurements in centric occlusion. The occlusal imprints are scatter in distribution and slight in strength although the voluntary maximal effect was required. The blue and red imprints merged well as the arrows indicate. c The centric to protrusion; d Right-side lateral extension; e Left-side lateral extension. O, occlusion side; C, bottom side; L, lingual side; B, buccal side
The centric closing task (Fig. 1 a )
The highest maximum stress value was 117 GPa, located at the right-side second molar. All the maximum stress values were increased when the mandibular dentition was simulated closing to the maxillary dentition from the early to the later closing stage. Similarity was noticed when the red and blue articulating papers (Tianjin Shengshili Dental Materials Factory, Tianjin, China) were used separately during the maximal voluntary biting in centric occlusion. The two records merged well (Fig. 1b ), although no speckle occlusal imprints were obtained after several times attempts. The T-Scan graph presented the contacts that were located at the bilateral molar regions, coincidental with the simulation in the DBC-FEM model.
The centric to protrusion task (Fig. 1 c )
The maximum stress was initially located at the bilateral molar regions but gradually at the region of the central incisors during the protruding task. In the end stage of protrusion, the stress concentration was noticed at the right-side third molar. The highest value of the maximum stress was 110 GPa, which appeared at the end stage of protrusion, located at the incisors. The T-Scan graph showed similarities and the contacts displayed at bilateral incisor and molar regions. The contact at higher level strength appeared at the right-side third molar in T-Scan, identical with simulation in the DBC-FEM model.
The centric to lateral extension task (Fig. 1d, e )
When simulating the mandible to excurse to the right side, the maximum stress was observed on not only the right-side canine, the premolars, and the first molar, but also on the left-side first and second molars at the late stage of the task. The highest value of the maximum stress was 53.3 GPa, which appeared at the end stage of the right-side lateral excursion, located at the left-side second molar. The T-Scan graph showed quite a similarity. The contacts appeared at the canine, premolar, and molar region of the right side and the molar region of the left side. When the mandible was simulated to excurse to the left side, the maximum stress was observed only at the right-side second molar. No maximum stress was observable at the left-side arch. The highest value of the maximum stress was 5.48 GPa, which appeared at the end stage of the left-side excursion, located at the right-side second molar. However, the T-Scan graph showed contacts at the left-side arch and at the right-side molar.
Occlusion stress in the simulated symmetrical lateral excursive movements—obtaining from the tasks in section 2
Recordings from EGN demonstrated that the volunteer had a shorter left-side excursive range, which was 4.1 mm leftward and 1.9 mm downward, than the right-side excursive range, which was 6.9 mm rightward and 6.6 mm downward. When simulating the left-side excursion task according to the right-side lateral excursion recordings, the maximum stress on the right-side first and second molars turned more significant (Fig. 2a ). There was maximum stress on the left-side first molar at the middle stage. The maximum stress happened on the left-side canine and the first premolar at the end stage. The values of the maximum stress from the initial stage to the end stage are shown in Fig. 2b . The highest value of the maximum stress was on the right-side second molar, which was 40.7 GPa. The normal and shear stress of that site were 5 and 0.5 GPa, respectively (Fig. 2c, d ). When simulating the right-side excursion task according to the left-side lateral excursion recordings, no maximum stress showed on the whole arch.
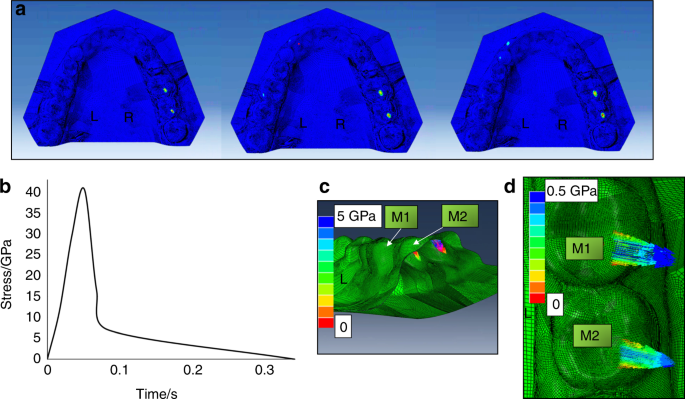
The occlusion stress representation for the simulated left-side lateral excursion movement according to the right-side lateral excursion recording. a The stress distribution at the initial (left), middle (middle), and end (right) stage of the simulated left-side lateral excursion movement; b The time–stress curve of the maximum stress at the right-side second molar. c The vertical stress. d The shear stress. M1 the right-side first molar, M2 the right-side second molar
Occlusion stress after the virtual tooth morphological modification—obtaining from the tasks in section 3
Virtual teeth morphological modification was performed on the lingual ridge of the distal buccal cusps of the right-side mandibular first molar and second molar (Fig. 3c ). There were contacts during the left-side lateral excursion (Fig. 1 ) and the simulated symmetrical left-side lateral excursion (Fig. 2 ). After the virtual morphological modification, the maximum stress in the simulated centric task was distributed with more symmetry, wider, and broader on the arch (Fig. 3c ). There was maximum stress located at the premolar region, which was not the case before modification (Figs. 3 d, 1a ). The highest value of the maximum stress was 66.8 GPa, located at the left second molar after virtual modification.
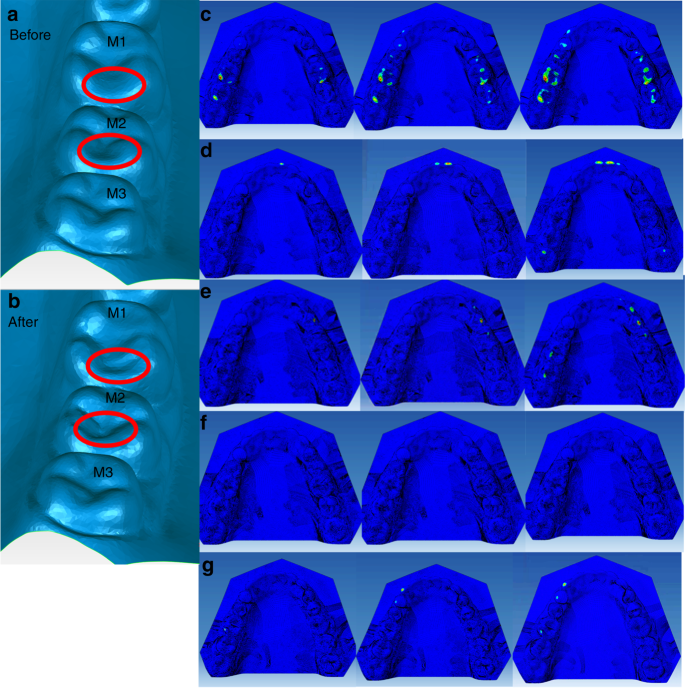
The geometry of the right-side molars (M1-3) before ( a ) and after ( b ) the virtual tooth morphological modification, and the occlusion stress distributions after in the virtual tooth modification in the tasks of Section 1, i.e., centric closing ( c ), the protrusion ( d ), the right-side excursion ( e ) and left-side excursion ( f ), and in the task of Section 2 ( g )
In the centric to protrusion task, there was still maximum stress at the central incisors region and the right third molars. Unexpectedly, there appeared contact on the left-side third molar at the end stage of the task (Fig. 3e ). In the centric to right-side lateral extension task, there was still maximum stress on the right-side canine and the first and second premolars, and also on the left-side first and second molars, but no more on the right-side first molar (Fig. 3e ). However, in the centric to left-side lateral extension task, no maximum stress was observed (Fig. 3f ). When simulating the left-side excursion task according to the right-side lateral excursion recordings, the maximum stress occurred on the left-side canine and the first premolar region (Fig. 3g ).
Biomechanics analysis helps understand the structure and function of biological systems and the forces on and displacements of the dental occlusion. 2 In this work, we developed a method to create a DBC-FEM that makes it possible to analyze the dynamic occlusal stress at the real sense contact sites according to the EGN and video recordings. Taking the recorded kinematical data as the boundary condition makes it unnecessary to simulate the complex muscular forces. The penalty formulation with finite sliding could prevent the unlimited permeated contacts, which is impossible in real conditions. With this DBC-FEM, we analyzed occlusion stress on the fluctuation surface of the mandibular dentition during nature closing, protrusive, and eccentric movements. In line with the lateral literature, 36 , 45 the highest maximum value of stress was in terms of GPa unit. Our present DBC-FEM model provides a new approach to evaluate occlusal stress and virtual occlusal correction in daily clinical practices or research, which helps correct clinical misperceptions and hopefully inform better patient care.
Functional studies considering the kinematics of teeth are essential to understand biomechanics and interpret morphological adaptation of teeth. 35 The present volunteer did not know that she has a problem excursing her mandible to the left side as precisely as what she did for the right side until she attended the present test. In the test process of the left-side excursion task, she tried her best to make the left-side teeth in contact with experimental requirements. By using her DBC-FEM for analyzing the occlusal stress, we revealed that the highest value of the maximum stress was located on her right-side molars when performing the left-side lateral excursion. It should be those right-side contacts, or the balance side interference, that prevented the teeth of the left side or the working side from contact. We performed the left-side lateral excursive movement simulation with the mirror trace of the right side. The result showed that the right-side interference contacts got heavier (Fig. 2 ). Such heavy contacts should be harmful to the masticatory organs. The potential harmfulness of the serious contacts should be why she moved to the left side with a larger vertical dimension but shorter lateral extension than moving to the right side. Such a successful protective compensation in the mandibular movement explains, at least partially, her free of disordered symptoms. Avoidance of heavy occlusion contact via alteration of mandibular movement pattern is, thus, an important design of the masticatory system. With such mechanisms, the masticatory system is adapted to complex changes in the dental occlusion and exhibits a high level of damage tolerance. 2
The biomechanical effects of occlusal loads on teeth during clenching and mastication and the transfer of occlusal forces have been primarily reported in the literature. 46 , 47 In a chewing simulation study, occlusal contact stiffness was the key point substantially affecting maximum contact force. 48 Clenching of molars and masticating morsels of high elastic moduli evoke considerable stress concentrations in the occlusal enamel of these teeth. While masticating a morsel of low elastic modulus, which conforms to the occlusal surfaces of teeth, creates considerable stresses in the cervical portion of the lingual wall of the mandibular molar. 47 Even though, the dental stress distribution patterns are more likely to be affected by loading direction and position. 35 Loads oriented normal to the tooth axis, such as that in subjects with balanced occlusion, are better distributed to the supporting tissues, thus was believed capable of avoiding tooth bending and stress concentrations. 12 Instable occlusion, on the other hand, is linked with tooth-damage-inducible occlusal forces. With many masticatory cycles, the unstable occlusion could be damage-inducible and cause tooth fracture. 49 A compelling feature of the splitting load relation is its explicit dependence on key geometrical dimensions. 50 Some anatomic occlusion forms have a higher fracture potential, such as the nonfunctional cusps versus functional cusps due to the wedging effect of the cusp–fossa. 13 Grooves and fissures on the occlusal surface had been taken as critical locations of cracks because tensile stresses on a FEM model were concentrated at these features. 35 It is then essential in clinical practice to identify the contact areas to estimate how the chewing force is distributed in the tooth and in the supporting structure 51 to provide an optimal occlusion load to ensure the long-term success of dental treatment.
In addition to dental healthy, occlusion has an impact on temporomandibular joints (TMJs), jaw muscles 2 and even cervical and trunk muscles. 52 Experimental occlusal interference in animals could cause jaw muscle damage, fatigue, and pain. 53 , 54 , 55 During the mastication process, the occlusion and the TMJs suffer the loading from jaw muscles’ contraction, which is originally active to chew up foods. The periodontal proprioceptors will pick up the message of occlusion loadings and then modify the jaw muscles activity via periodontal-muscle reflex mechanisms. The dynamic occlusal stress is then worth recording and measuring. However, as far as our extension, in literature, there are still no dynamic occlusal stress evaluation devices or systems in view of oral function and dysfunction. 56 Clinical measurements like laser scanner, occlusal stress detector, electromyograph, and mandibular movement recorder are generally used in an independent pattern for diagnosing occlusal functions. 57 None of them directly provide the stress information. The clinical loading assessment relies primarily on the doctor’s personal experience and strong empirical operation by using a single bite size evaluation to the stress tester, which lacks quantitative indicators. 58 Our DBC-FEM method brings about a new insight for dynamic occlusion stress assessment. With our developed method, the occlusion stress can be analyzed, and the virtual occlusion modification could be performed to achieve satisfactory occlusion function.
As far as our extension, this work is the first one in the literature that describes the movements setting in three directions and combined using dimensions and rotations based on the EGN and video recordings. The EGN and videos were not synchronously recorded due to the limitations of the recording technique. We segmented the EGN and videos recordings by time so that the video angle measurements could match the ENG displacement measurements. Even though the system errors existed, which contributed, at least partially, to the minor differences of the present DBC-FEM data from T-Scan recordings. However, the minor differences may also come from the T-Scan transducer’s obstacle interferences, which were more predominant during protrusion and lateral excursions. The even thickness of the transducer prevented the freedom of the dynamic tasks and increased the possibility of systemic errors. The system errors have to be taken into account, especially when aiming for occlusal correction. More complex composite three-dimensional solid structure and nonlinear material models are expected to develop. The high simulation model studies are expected to be conducted, for example, the kinematics of the simulated chewing tasks and linear shell element structure for occlusal simulation.
In summary, taking the mandibular kinematical parameters as the boundary condition, the present contact derived from DBC-FEM brings about a creative approach for occlusion stress prediction. Importantly, our DBC-FEM makes it practical to correct occlusion biomechanics through virtual morphological modification. It will be helpful in occlusion-related operations such as computer aided design and computer aided manufacturing (CAD/CAM) for denture processing.
Materials and methods
This study collected information from a 32-years-old Chinese female volunteer. She had no symptoms of oral dysfunction, such as that observed in patients with temporomandibular disorders (TMDs). She declared no known bruxism. She had no tooth surface lesions such as severe tooth wear, cervical lesions, and caries, and her periodontal condition was healthy as examined by one of the authors (MQ). She understood the task well because she is a dental nurse. She had 30 permanent teeth arranged in morphological normal. The measurements were performed by one of the authors (DQ). All the procedures were conducted according to established ethical guidelines with written consent. This study was approved by the Human Experiment Committee, College of Stomatology, the Fourth Military Medical University (Ethics Certificate No: IRB-REV-2015031).
Dentition reconstruction
Plastic casts were obtained and then scanned using a dental scanner (3Shape R750, 3Shape, Denmark). The 3D digital model was created using 3Shape software (3Shape ScanItManagerTM, 1.7.1.0, 3Shape, Denmark) and smoothed by using Model Preparation software (3Shape OrthoAnalyzerTM, 1.7.1.0, 3Shape, Denmark). The static and dynamic noises were removed through mean filtering from raw data. The noise was further removed utilizing the gray histogram analysis and the threshold value. The entire dentition models were reconstructed with upper 589 and lower 509 pieces curved surfaces after smoothing (Fig. 4a ).
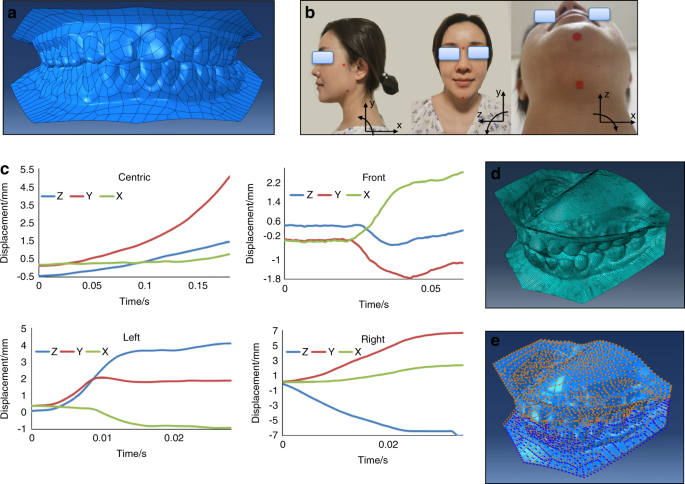
Development and application of the displacement boundary condition finite element model (DBC-FEM) and the jaw rotation movements recording methods. a The full reconstructed 3D dentition surface models positioned at centric occlusion. b Diagram for jaw rotation video recording. The pogonion, gonion, nasion, hyoid bone, and root of zygomatic process (RZP), as indicated by red spots, were taken as the osteological landmarks. Video of the jaw rotation movements was recorded in sagittal ( x- and y -axis), frontal ( y - and z -axis), and horizontal ( x - and z -axis) planes, separately. c The mandibular movements of three plane decomposition originated from ENG recordings. d The dentitions mesh elements. e The displacement boundary conditions. The blue arrows represent rotational loadings, and the orange ones represent displacement loadings
Electrognathograph (EGN)
The volunteer was trained before testing. The mandibular movements were recorded by EGN and BioPAK system software (both by Bioresearch Associates, Inc., Milwaukee, WI, USA). 41 Briefly, a magnet was attached to the labial surface of the mandibular central incisors without interfering with any movements of the mandible. The sensor array was fixed on the subject’s head, as we previously reported. 36 The measurements recorded the nature close from the rest position to the centric occlusion position in three dimensions. Followed by protrusion and the right- and left-side lateral excursion movement. All of the movements were started from the intercuspal position (ICP). During the processes of the movements, the maxillary and mandibular teeth were required to be kept in touch. The sampling frequency was 1 000 Hz. The displacing amplitudes were automatically calculated and displayed by the software (BioPAK software Version 8.1, BioResearch Associates, Inc., Milwaukee, WI, USA). During the whole testing process, the subject sat upright in a chair, keeping the eyes on a point at eye level two meters away as required.
Video of the jaw rotation movements
The rotation of the jaw during centric and eccentric movements were recorded by a video camera (Canon EOS 6D, Canon Inc., USA). The locations of the osteological landmarks were pogonion, gonion, nasion, hyoid bone, and root of the zygomatic process (RZP) (Fig. 4b ). When the mandibular rotational messages were extracted from the video recordings for the 3D motion coordinates deposition, different pairs of markers were used. One of the markers in each pair was fixed and the other was movable. RZP was taken as the fixed and gonion as the movable for saggital view, nasion as fixed and pogonion as movable for frontal view, and hyoid bone as fixed and pogonion as movable for horizontal view. By taking the video of the centric and eccentric movements, the 3D motion coordinates can be deposited into sagittal (with RZP and gonion), frontal (with nasion and pogonion), and horizontal (with hyoid bone and pogonion) planes, each with two directions displacements and one rotation. The displacement curves of different occlusions are shown in Fig. 4c . The rotated angles of each plane are shown in Table 1 .
DBC-FEM modeling
The material property of this research was assumed to be homogeneous, isotropic, and linear elastic. The whole dentition is processing as enamel shell elements. The elastic modulus for enamel was defined as 84 GPa with a Poisson’s ratio of 0.3. 36 The total 3D occlusion model was meshed in Abaqus software (Version 14.0, Dassault Systemes, Co., Velizy-Villacoublay, FRANCE) with 60 345 nodes and 60,309 elements, which include 943 linear triangles and 59 336 linear quadrilaterals (Fig. 4d ). The displacement and angle recordings were used as merged data by taking the initial centric occlusion position as the common reference frames. The accuracy of the two recordings were different, more precise in ENG recordings than video recordings. We segmented the recordings by time scales, and the data from the same segment was merged. The merged datasets, containing 18, 61, 29, and 35 segments separately for the four tasks of the centric closing, protrusion and left-side and right-side lateral excursion, were delivered to the DBC-FEM model for dynamic stress analysis.
The boundary condition for the stress analysis using DBC-FEM
The mandibular dentition was simulated to move under the fixed maxillary dentition. The movement was set as three directional displacements and rotations based on the EGN and video recordings (Fig. 4e ). The displacements can be captured by tracing a magnetic point in the ENG, and the rotational angles can be captured by tracing the markers in the video recordings. The volunteer first kept in the initial occlusal gesture with mouth closed, and then was required to start the four moving tasks. The displacements data from EGN and video derived from the same task were matched by time scales. The displacement and angle data were merging analyzed by taking the initial gesture as the common reference frames. The accuracy of ENG was higher than video, but with the time scales as labels, the system errors were diminished to minimal. The contacts between the pairs of the maxillary and mandibular dentitions were set with friction coefficient 0.1 and no elastic slip on the interactions. 59 The contact stress was calculated proportionally according to the occlusal contact areas at each material point of the model following penalty algorithms.
The simulated tasks
In total three sets of tasks were simulated.
Section 1: Four simulated tasks were centric movement, which was the nature closing to the centric occlusion position, and eccentric movement, which included protrusion from the centric position to the edge-to-edge relation, and lateral excursion from the centric position to the right and left side, separately, with the mandibular buccal cusps directly under the maxillary buccal cusps of the molars.
Section 2: Applying the mirror trace of the right-side lateral excursion movement to the left-side lateral excursion movement to achieve complete symmetrical lateral tasks. The left-side lateral excursion movement was also applied to the right side for reference.
Section 3: Applying a virtual removal of the lateral balance interferential contacts on the right-side first and second molars. Then the rehabilitated model was applied with the four simulated tasks as that in section 1 and the mirror simulated task as in section 2.
Stress analysis
The dynamic contact sizes were calculated to obtain the contact derived from maximum principal stress on the mandibular dentition. The stress was analyzed based on the decomposed normal and shear components in the environment of the Abaqus software (Version 14.0, Dassault Systemes, Co., Velizy-Villacoublay, FRANCE). The locations and the values of the maximum stress in each task were presented.
The location and strength of the occlusion contacts recorded with the T-Scan III occlusion analysis system (Tekscan, Inc., Boston, MA, USA) 34 were taken as contrasts. The thickness of the sensor was 60 μm. The time-dependent number and relative strength level of occlusal contacts were displayed as color contour images. The system set the force threshold before testing according to the instrumental introduction.
Aidsman, I. K. Glossary of prosthodontic terms. J. Prosthet. Dent. 38 , 66–109 (1977).
Article Google Scholar
Peck, C. Biomechanics of occlusion—implications for oral rehabilitation. J. Oral. Rehabil. 43 , 205–214 (2016).
Article PubMed Google Scholar
Ghazal, M., Yang, B., Ludwig, K. & Kern, M. Two-body wear of resin and ceramic denture teeth in comparison to human enamel. Dent. Mater. 24 , 502–507 (2008).
Lambrechts, P., Debels, E. Van Landuyt, K., Peumans, M. & Van Meerbeek, B. How to simulate wear?: overview of existing methods. Dent. Mater. 22 , 693–701 (2006).
Stober, T., Lutz, T., Gilde, H. & Rammelsberg, P. Wear of resin denture teeth by two-body contact. Dent. Mater. 22 , 243–249 (2006).
Blatz, M. B., Oppes, S., Chiche, G., Holst, S. & Sadan, A. Influence of cementation technique on fracture strength and leakage of alumina all-ceramic crowns after cyclic loading. Quintessence international 39.1 (2008).
Naumann, M. et al. Influence of test parameters on in vitro fracture resistance of post‐endodontic restorations: a structured review. J. Oral. Rehabil. 36 , 299–312 (2009).
Ohlmann, B. et al. Fracture-load values of all-ceramic cantilevered FPDs with different framework designs. Int. J. Prosthodont. 22 .1 (2009).
Zhang, Y., Sailer, I. & Lawn, B. R. Fatigue of dental ceramics. J. Dent. 41 , 1135–1147 (2013).
Dejak, B., Mlotkowski, A. & Romanowicz, M. Finite element analysis of mechanism of cervical lesion formation in simulated molars during mastication and parafunction. J. Prosthet. Dent. 94 , 520–529 (2005).
Takehara, J., Takano, T., Akhter, R. & Morita, M. Correlations of noncarious cervical lesions and occlusal factors determined by using pressure-detecting sheet. J. Dent. 36 , 774–779 (2008).
Guimarães, J. C. et al. Stress amplifications in dental non-carious cervical lesions. J. Biomech. 47 , 410–416 (2014).
Lubisich, E. B., Hilton, T. J. & Ferracane, J. Cracked teeth: a review of the literature. J. Esthet. Restor. Dent. 22 , 158–167 (2010).
Sailer, I., Gottner, J., Känel, S. & Franz Hämmerle, C. H. Randomized controlled clinical trial of zirconia-ceramic and metal-ceramic posterior fixed dental prostheses: a 3-year follow-up. Int. J. Prosthodont. 22 , 553 (2009).
PubMed Google Scholar
Dejak, B. & Młotkowski, A. A comparison of stresses in molar teeth restored with inlays and direct restorations, including polymerization shrinkage of composite resin and tooth loading during mastication. Dent. Mater. 31 , e77–e87 (2015).
Ausiello, P. et al. Mechanical behavior of bulk direct composite versus block composite and lithium disilicate indirect Class II restorations by CAD-FEM modeling. Dent. Mater. 33 , 690–701 (2017).
Soliman, S. et al. Influence of cavity margin design and restorative material on marginal quality and seal of extended class II resin composite restorations in vitro. J. Adhes. Dent. 18 , 7–16 (2016).
Ausiello, P. et al. The effects of cavity-margin-angles and bolus stiffness on the mechanical behavior of indirect resin composite class II restorations. Dent. Mater. 33 , e39–e47 (2017).
Pascalea, A., Rugeb, S., Hauthc, S., Kordaßd, B. & Linsene, L. Chewing simulation with a physically accurate deformable model Kausimulation mit einem physikalisch exakten verformbaren Modell. Int. J. Comput. Dent. 18 , 237–258 (2015).
Google Scholar
Gibbs, C. H. et al. Occlusal forces during chewing and swallowing as measured by sound transmission. J. Prosthet. Dent. 46 , 443–449 (1981).
Desai, P. D. & Das, U. K. Comparison of fracture resistance of teeth restored with ceramic inlay and resin composite: An in vitro study. Indian J. Dent. Res. 22 , 877 (2011).
Wang, M. & Mehta, N. A possible biomechanical role of occlusal cusp–fossa contact relationships. J. Oral. Rehabil. 40 , 69–79 (2013).
Liu, X. et al. Proprioceptive mechanisms in occlusion‐stimulated masseter hypercontraction. Eur. J. Oral. Sci. 125 , 127–134 (2017).
Lund, J. P. & Kolta, A. Generation of the central masticatory pattern and its modification by sensory feedback. Dysphagia 21 , 167–174 (2006).
Wang, X. R., Zhang, Y., Xing, N., Xu, Y. F. & Wang, M. Q. Stable tooth contacts in intercuspal occlusion makes for utilities of the jaw elevators during maximal voluntary clenching. J. Oral. Rehabil. 40 , 319–328 (2013).
Sharma, A. et al. History of materials used for recording static and dynamic occlusal contact marks: a literature review. J. Clin. Exp. Dent. 5 , e48 (2013).
Article PubMed PubMed Central Google Scholar
WANG, Y. L. et al. Patterns and forces of occlusal contacts during lateral excursions recorded by the T‐Scan II system in young Chinese adults with normal occlusions. J. Oral. Rehabil. 38 , 571–578 (2011).
Al-Nimri, K. S., Bataineh, A. B. & Abo-Farha, S. Functional occlusal patterns and their relationship to static occlusion. Angle Orthod. 80 , 65–71 (2010).
Weissman-Fogel, I. et al. Abnormal cortical activity in patients with temporomandibular disorder evoked by cognitive and emotional tasks. Pain 152 , 384–396 (2011).
Tröltzsch, M., Cronin, R., Brodine, A., Frankenberger, R. & Messlinger, K. Prevalence and association of headaches, temporomandibular joint disorders, and occlusal interferences. J. Prosthet. Dent. 105 , 410–417 (2011).
Fujii, T. The relationship between the occlusal interference side and the symptomatic side in temporomandibular disorders. J. Oral. Rehabil. 30 , 295–300 (2003).
Shiga, H., Kobayashi, Y., Arakawa, I., Yokoyama, M. & Tanaka, A. Relationship between pattern of masticatory path and state of lateral occlusal contact. J. Oral. Rehabil. 36 , 250–256 (2009).
Zhang, Y.-R., Du, W., Zhou, X.-D. & Yu, H.-Y. Review of research on the mechanical properties of the human tooth. Int. J. Oral. Sci. 6 , 61–69 (2014).
Oladapo, B. I., Zahedi, S. A., Vahidnia, F., Ikumapayi, O. & Farooq, M. U. Three-dimensional finite element analysis of a porcelain crowned tooth. Beni Suef Univ. J. Basic Appl. Sci. 7 , 461–464 (2018).
Benazzi, S., Kullmer, O., Grosse, I. R. & Weber, G. W. Using occlusal wear information and finite element analysis to investigate stress distributions in human molars. J. Anat. 219 , 259–272 (2011).
Zhang, H., Cui, J. W., Lu, X. & Wang, M. Q. Finite element analysis on tooth and periodontal stress under simulated occlusal loads. J. Oral. Rehabil. 44 , 526–536 (2017).
Phanachet, I. et al. Functional heterogeneity in the superior head of the human lateral pterygoid. J. Dent. Res. 82 , 106–111 (2003).
Chen, H., Whittle, T., Gal, J., Murray, G. & Klineberg, I. The medial pterygoid muscle: a stabiliser of horizontal jaw movement. J. Oral. Rehabil. 44 , 779–790 (2017).
Benazzi, S., Kullmer, O., Grosse, I. R. & Weber, G. W. Brief communication: comparing loading scenarios in lower first molar supporting bone structure using 3D finite element analysis. Am. J. Phys. Anthropol. 147 , 128–134 (2012).
Mesnard, M. et al. Biomechanical analysis comparing natural and alloplastic temporomandibular joint replacement using a finite element model. J. Oral. Maxillofac. Surg. 69 , 1008–1017 (2011).
Guo, S. et al. Interferential effect of the over-erupted third molar on chewing movement. Arch. Oral. Biol. 82 , 147–152 (2017).
Lafontaine, N., Rossi, R., Cervera, M. & Chiumenti, M. Explicit mixed strain-displacement finite element for dynamic geometrically non-linear solid mechanics. Comput. Mech. 55 , 543–559 (2015).
Ortega, R., Orden, J. C. G., Cruchaga, M. & García, C. Energy-consistent simulation of frictional contact in rigid multibody systems using implicit surfaces and penalty method. Multibody Syst. Dyn. 41 , 275–295 (2017).
Bhattacharya, P., Betts, D. & van Lenthe, G. H. A novel contact interaction formulation for voxel‐based micro‐finite‐element models of bone. Int. J. Numer. Methods Eng. 115 , 411–426 (2018).
Saini, H. et al. Occlusal load modelling significantly impacts the predicted tooth stress response during biting: a simulation study. Computer Methods Biomech. Biomed. Eng. 23 , 261–270 (2020).
Palamara, D., Palamara, J., Tyas, M. & Messer, H. Strain patterns in cervical enamel of teeth subjected to occlusal loading. Dent. Mater. 16 , 412–419 (2000).
Dejak, B., Młotkowski, A. & Romanowicz, M. Finite element analysis of stresses in molars during clenching and mastication. J. Prosthet. Dent. 90 , 591–597 (2003).
Rues, S., Huber, G., Rammelsberg, P. & Stober, T. Effect of impact velocity and specimen stiffness on contact forces in a weight-controlled chewing simulator. Dent. Mater. 27 , 1267–1272 (2011).
Mamoun, J. S. & Napoletano, D. Cracked tooth diagnosis and treatment: an alternative paradigm. Eur. J. Dent. 9 , 293 (2015).
Barani, A., Chai, H., Lawn, B. R. & Bush, M. B. Mechanics analysis of molar tooth splitting. Acta Biomater. 15 , 237–243 (2015).
DeLong, R. Intra-oral restorative materials wear: rethinking the current approaches: how to measure wear. Dent. Mater. 22 , 702–711 (2006).
Julià-Sánchez, S., Álvarez-Herms, J., Cirer-Sastre, R., Corbi, F. & Burtscher, M. The influence of dental occlusion on dynamic balance and muscular tone. Front. Physiol. 10 , 1626 (2020).
Wu, D. & Liu, J. Occlusal interference induces oxidative stress and increases the expression of UCP3 in the masseter muscle: a rat model. Arch. Oral. Biol. 102 , 249–255 (2019).
Zhang, H.-Y. et al. Masseter response to long-term experimentally induced anterior crossbite in Sprague-Dawley rats. Arch. Oral. Biol. 122 , 104985 (2021).
Zhang, H.-Y. et al. Injury responses of Sprague-Dawley rat jaw muscles to an experimental unilateral anterior crossbite prosthesis. Arch. Oral. Biol. 109 , 104588 (2020).
Achour, T., Merdji, A., Bouiadjra, B. B., Serier, B. & Djebbar, N. Stress distribution in dental implant with elastomeric stress barrier. Mater. Des. 32 , 282–290 (2011).
Liu, C.-W., Chang, Y.-M., Shen, Y.-F. & Hong, H.-H. Using the T-scan III system to analyze occlusal function in mandibular reconstruction patients: a pilot study. Biomed. J. 38 , 1 (2015).
Becker, I. M. Comprehensive Occlusal Concepts in Clinical Practice (John Wiley & Sons, 2010).
Mulvihill, D. M., Kartal, M. E., Nowell, D. & Hills, D. A. An elastic–plastic asperity interaction model for sliding friction. Tribology Int. 44 , 1679–1694 (2011).
Download references
Acknowledgements
This work was supported by the National Natural Science Foundation of China (No. 81530033, 81920108013).
Author information
Authors and affiliations.
Key Laboratory of the Ministry of Education for Optoelectronic Measurement Technology and Instrument, Beijing Information Science and Technology University, Beijing, China
Zheng Duanmu
Department of Oral Anatomy and Physiology and TMD, School of Stomatology, Air Force Medical University, Xi’an, China
Lu Liu, Qi Deng, Yuanyuan Ren & Meiqing Wang
You can also search for this author in PubMed Google Scholar
Contributions
M.W. and Z.D. conceptualized and designed the study, interpreted the data, and composed the manuscript. Z.D. developed the model. L.L. and Q.D. helped with measuring the clinical experiment and collecting data. Y.R. provided her experiment data. All authors gave approval for the final version of this manuscript to be published and agreed to be accountable for all aspects of the work.
Corresponding author
Correspondence to Meiqing Wang .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Supplementary information
Supplemental table+1-4, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Duanmu, Z., Liu, L., Deng, Q. et al. Development of a biomechanical model for dynamic occlusal stress analysis. Int J Oral Sci 13 , 29 (2021). https://doi.org/10.1038/s41368-021-00133-5
Download citation
Received : 15 February 2021
Accepted : 06 July 2021
Published : 08 September 2021
DOI : https://doi.org/10.1038/s41368-021-00133-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

IMAGES
VIDEO
COMMENTS
Jaw teeth lateral excursion is a sideways movement to left or right of your mandible (lower jaw) until disoccluding the top and bottom dental arch. Business Login. Login. ... Lateral excursion might be hampered due to problems in the gnathic system. A locked jaw, tumour, traumatic injury, muscle pain, disk injuries, congenital disorders may ...
Lateral excursion. Lateral excursions are a form of dynamic occlusion which occurs when the mandible moves left or right with teeth in contact. They can be described as: Canine guidance: canine protected articulation. The canines on the working side are the only occluding teeth whilst all other teeth become discluded when carrying out lateral ...
A demonstration of the lateral excursion and an explanation of when and why lateral excursion adjustment is necessary. Orig. air date: AUG 14 74This is part...
Dynamic occlusion: lateral excursion The dynamic occlusion is the contact that teeth make during movements of the mandible - when the jaw moves side to side, forward, backward or at an angle. In dynamic occlusion, the contacts of the teeth are not points as in static occlusion, but they are described with lines. ...
Canine guidance - this means during lateral excursion of the mandible the canines are the teeth which guide the mandibles movement and the last to disclude ; Group function - this means during lateral excursion of the mandible, the tooth contact which guides the movement is shared between multiple teeth on the working side.
Correct tooth restoration means reproducing the original shape of the tooth, taking into account the functional aspect of dental morphology and its occlusal relationships. ... sagittal, vertical. During lateral excursion we can distinguish a working side, which is the side toward which the mandible moves, and a balancing side, or the side away ...
mandible moves towards during lateral excursions (WS) ... several teeth on the working side during lateral excursions. 2. TMJ - this is the hinge that allows contacts between the teeth, to
Non-working Side - side of the mandible that moves towards the midline during lateral excursion (NWS) Interferences - tooth contact that hinders mandibular movement, can be on the WS or NWS.
During a lateral excursion of the mandible, the principle movement within the TMJs is on the non-working side (NWS). The head of the condyle on the non-working side moves: forwards, downwards and ...
A 'Non-Working Side Interference' is an anterior guidance on the back teeth on the non-working side during lateral excursion. During a Lateral Excursion. Non-Working Side: The side on which the head of the condyle does translate downwards, forwards and medially. Working Side:
Right lateral excursion (RLE) Note the guidance teeth and interferences on the working and non-working sides. Left lateral excursion (LLE) As for RLE. Protrusion. Note the guidance teeth: interferences are usually on the posterior teeth. Loss of vertical dimension. Where indicated, measure occlusal and rest vertical dimensions
The current study primarily investigated the hypothesis that reducing excursive occlusal loads on a tooth in lateral excursion would lead to a reduction in the rate of progression of abfraction lesions. The study was carried out in a primary care setting, in this case, a predominantly private general dental practice, with most of the subjects ...
There are clinical signs of a molar rise with a lateral excursion on the patient's working (chewing) side, and also a balancing side contact on the same tooth with the opposite lateral excursion. In addition, the tooth is slightly mobile and the periodontal tissues are tender and bleed upon probing.
Canine guidance during right lateral excursions (Institute of Dentistry University of Aberdeen) Canine Guidance. Dynamic occlusion that occurs on the canines (on the working side) during lateral excursions of the mandible. These teeth are best suited to accept horizontal forces in eccentric movements due to their long roots and good crown/root ...
There are three main concepts regarding tooth contact during the lateral excursion of mandibular movement: (1) balanced occlusion, which was developed from the work of Bonwill, 3 (2) canine guidance, described by D'Amico, 4 and (3) group function, as discussed by Beyron. 5. The relationship between static and dynamic occlusion is one of the ...
The anterior teeth should be in only passive contact during lateral excursions. Working Protrusive; 39. The Lateral Incisors and the Cuspids Setting the Mandibular Anterior Teeth Upon completion, the amount of vertical and horizontal overlap will be idealized and anterior guidance has not been introduced into the setup.
• An immediate and permanent posterior disclusion in lateral and protrusive contact with no associated non-working side interferences (tooth contacts); this is achieved by the presence of canine guidance or group function in lateral excursion and incisal guidance in protrusion. Thus, the anterior teeth protect the posteriors;
Disclusion of the posterior teeth, upon lateral and protrusive mandibular movements. ... with even centric stops in CO and posterior disclusion on protrusion and lateral excursions.
Posterior teeth should be arranged to encourage the envelope of motion through a true lateral excursion. 8. Lateral anterior guidance should permit positive contacts of the posterior teeth during rotations through lateral excursions. Lateral-protrusive anterior guidances should prevent them. 9. Posterior teeth with cusps, fossae and grooves are ...
If posterior teeth are interfering with the protrusive movement, tooth structure is removed from the offending cusps until all articulating contacts between the posterior teeth have been eliminated. Step 5: This step deals with the removal or lessening of all interferences in lateral excursions.
Cross-tooth contact negates centralization of forces on the mandibular posterior teeth, and increases the likelihood of lateral displacement. As a result, the arrangement does not satisfy the objectives of a lingualized occlusion. ... Accomplish corrective adjustment procedures for right lateral and left lateral excursions. Ensure sustained ...
Purpose: This study observed occlusal contacts and determined their areas on the mandibular teeth, especially the molars, during voluntary lateral excursions. Materials and methods: Occlusal contact areas were estimated with a measurement system combining 3-D tracking of mandibular movements with 3-D digitization of tooth shape. . Sixteen women with sound permanent dentitions partic
The occlusion stress representation for the simulated left-side lateral excursion movement according to the right-side lateral excursion recording.
Muscles of head & Neck -Facial expression: originate on the surface of skull, insert to skin (dermis) o Zygomaticus major: smile -Mastication (chewing): move mandible at temporomandibular joint (TMJ) o Masseter: strongest jaw muscle o Temporalis: elevate mandible, you can feel this around zygomatic arch o Pterygoid: elevate, depress, protract mandible; slide from side to side (lateral ...