Explore prestigious scientific journals and award and funding opportunities to advance your research.
Access practice-improvement tools, including guidelines, measures, and practice management resources.
Learn to effectively advocate on behalf of neurologists and their patients, and access AAN position and policy statements.
Loading... please wait
We’re experiencing unusually high levels of traffic. Thank you for your patience.

Billing and Coding
Practice management.
To be indispensable to its members, the AAN provides resources to help them with coding and reimbursement. This includes resources about the Current Procedural Terminology (CPT) code set, staying current on Evaluation and Management (E/M) coding and documentation guidelines, and understanding how Medicare and other payers reimburse.*
Change Healthcare Outage
CMS issued guidance concerning advanced payments in response to the Change Healthcare Cyberattack. Read more using these links:
- CMS FAQs on Advanced Payments
- MIPS EUC Exception Application
- AMA Change Healthcare Updates
- UHC Change Healthcare Cyber Response
Evaluation and Management (E/M)
Stay current on Evaluation and Management (E/M) coding and documentation guidelines.
CPT and Coding Resources
Learn about the CPT process and ensure you are coding accurately.
Model Coverage Policies
Review model coverage policies developed by the AAN that can be used as examples of appropriate coverage and coding.
Understand ICD-10 CM, the system used by US physicians to classify and code diagnosis and symptoms.
Find answers to your most common coding questions.
*The billing and coding information provided by the American Academy of Neurology and its affiliates (collectively, “Academy”) are assessments of clinical information provided as an educational service. The information (1) is not clinical advice; (2) does not account for how private payers cover and reimburse procedures or services*; (3) is not continually updated and may not reflect the most current clinical information (new clinical information may emerge between the time information is developed and when it is published or read); and (4) is not a substitute for the independent professional judgment of the treating provider, who is responsible for correctly coding procedures and services.
Using this information is voluntary. The Academy is providing the information on an “as is” basis and makes no warranty, expressed or implied, regarding the information. The Academy specifically disclaims any warranties of merchantability or fitness for a particular use or purpose. The Academy assumes no responsibility for any injury or damage to persons or property arising out of or related to any use of this information or for any errors or omissions.
*The Academy recommends always checking private payer policies before rendering procedures or services
Qway Health Care
A Premium Revenue Cycle Partner
(609) 905-7929
Home Blog Articles Specialty Coding Neurology Billing and Coding: ...
Neurology Billing and Coding: A Comprehensive Guide
Providing quality neurology services to patients requires not only expertise in the field but also a solid understanding of the complex world of neurology billing and coding. Efficiently managing the financial aspect of a neurology practice necessitates familiarity with the intricacies of submitting claims, adhering to regulations, and staying up to date with the ever-evolving billing codes. Within this exhaustive guide, we navigate the intricate world of neurology billing and coding, shedding light on the obstacles faced by healthcare providers and presenting pivotal strategies to triumph over them.
Understanding Neurology Billing and Coding
Neurology billing encompasses the process of submitting claims to insurance companies or payers to seek reimbursement for the services rendered by neurology healthcare providers. Central to this process are the neurology billing codes, which identify the specific procedures and treatments provided. These codes are based on the widely recognized Current Procedural Terminology (CPT) system, maintained by the esteemed American Medical Association ( AMA ). Being well-versed in the codes of various neurological procedures like lumbar punctures, treatment for dementia, movement disorders, headaches, epilepsy, sleep disorders, chronic pain management, and multiple sclerosis or neuromuscular diseases; management of bipolar disorder and schizophrenia; psychiatric procedures is crucial to ensure accurate billing and maximize reimbursement.
According to NCBI, for hospitalists and other hospital providers, services are coded under the Current Procedural Terminology (CPT) Evaluation and Management (E/M) guidelines. These codes are based on either the level of medical complexity or on time spent on care. When coding on medical complexity, each E/M service encounter has 3 major components: the history, examination, and the complexity of medical decision-making (MDM). MDM is further divided into the number of diagnostic considerations or management options, the amount and intensity of data review, and risk. MDM level is determined by the highest of 2 of the 3 categories. Depending on the type of encounter, i.e., an initial or subsequent visit, inpatient or outpatient, there are specific requirements within those 3 components that must be included in order to achieve a certain billing code level.
Related Post : Peripheral Neuropathy ICD 10 Codes
Commonly used icd-10 and cpt codes for neurology billing and coding:.
ICD-10 Codes for Some Common Neurology Conditions
- F90.9 Attention-Deficit Hyperactivity Disorder, Unspecified Type
- F03.90 Unspecified Dementia Without Behavioral Disturbance
- G30.9 Alzheimer’s Disease, Unspecified
- R47.01 Aphasia
- R48.1 Agnosia
- R48.2 Apraxia
- G45.9 Transient Cerebral Ischemic Attack, Unspecified
- I63.9 Cerebral Infarction, Unspecified
- G52.9 Cranial Nerve Disorder, Unspecified
- E72.01 Cystinuria
- F72 Severe Intellectual Disabilities
- F84.0 Autistic Disorder
- F84.5 Asperger’s Syndrome
- R62.0 Delayed Milestone In Childhood
- E70.0 Classical Phenylketonuria
- E70.1 Other Hyperphenylalaninemias
- E72.04 Cystinosis
- E75.02 Tay-Sachs Disease
- G43.001 Migraine Without Aura, Not Intractable, With Status Migrainosus
- G43.101 Migraine With Aura, Not Intractable, With Status Migrainosus
- G43.821 Menstrual Migraine, Not Intractable, With Status Migrainosus G43.C1 Periodic Headache Syndromes In Child Or Adult, Intractable
- G43.D0 Abdominal Migraine, Not Intractable
- G03.9 Meningitis, Unspecified
- G04.90 Encephalitis And Encephalomyelitis, Unspecified
- G04.91 Myelitis, Unspecified
- C71.6 Malignant Neoplasm Of Cerebellum
- G12.21 Amyotrophic Lateral Sclerosis
- G12.29 Other Motor Neuron Disease
- F95.2 Tourette’s Disorder
- F95.9 Tic Disorder, Unspecified
- G10 Huntington’s Disease
- G20 Parkinson’s Disease
- G71.0 Muscular Dystrophy
- G0.61 Intraspinal Abscess And Granuloma
- G11.1 Early-Onset Cerebellar Ataxia
- G12.9 Spinal Muscular Atrophy, Unspecified
- G50.0 Trigeminal Neuralgia
- G51.0 Bell’s Palsy
- G40.101 Localization-Related (Focal) (Partial) Symptomatic Epilepsy And Epileptic Syndromes With Simple Partial Seizures, Not Intractable, With Status Epilepticus
- G40.109 Localization-Related (Focal) (Partial) Symptomatic Epilepsy And Epileptic Syndromes With Simple Partial Seizures, Not Intractable, Without Status Epilepticus
- G25.81 Restless Legs Syndrome
- G47.00 Insomnia, Unspecified
- G47.20 Circadian Rhythm Sleep Disorder, Unspecified Type
- G47.30 Sleep Apnea, Unspecified
- D89.89 Other Specified Disorders Involving The Immune Mechanism, Not Elsewhere Classified
- E11.42 Type 2 Diabetes Mellitus With Diabetic Polyneuropathy
- F32.9 Major Depressive Disorder, Single Episode, Unspecified
- G11.8 Other Hereditary Ataxias
- G12.8 Other Spinal Muscular Atrophies And Related Syndromes
- H02.409 Unspecified Ptosis Of Unspecified Eyelid
- H46.9 Unspecified Optic Neuritis
- H47.20 Unspecified Optic Atrophy
- M54.10 Radiculopathy, Site Unspecified
- M54.2 Cervicalgia
- M54.5 Low Back Pain
- M60.9 Myositis, Unspecified
- M62.50 Muscle Wasting And Atrophy, Not Elsewhere Classified, Unspecified Site
- M79.1 Myalgia
- M79.2 Neuralgia And Neuritis, Unspecified
- M79.609 Pain In Unspecified Limb
- R13.10 Dysphagia, Unspecified
- R25.2 Cramp And Spasm
- R41.2 Retrograde Amnesia
CPT codes for neurology and neuromuscular procedures
The CPT code range for neurology and neuromuscular procedures includes:
- 95700-95811 Sleep Medicine Testing and Long-term EEG Procedures
- 95812-95830 Routine Electroencephalography (EEG) Procedures
- 95829-95836 Electrocorticography
- 95851-95857 Range of Motion Testing
- 95860-95872 Electromyography Procedures
- 95873-95887 Ischemic Muscle Testing Procedures and Guidance Procedures for Chemo denervation
- 95905-95913 Nerve Conduction Tests
- 95919-95924 Autonomic Function Testing Procedures
- 95925-95937 Evoked Potentials and Reflex Testing Procedures
- 95938-95941 Intraoperative Neurophysiology Procedure
- 95954-95726 Special EEG Testing Procedures
- 95970-95984 Neurostimulators Analysis-Programming Procedures
- 95990-95999 Other Neurology and Neuromuscular Procedures
- 96000-96004 Motion Analysis Procedures
- 96020-96020 Functional Brain Mapping
Challenges in Neurology Billing and Coding
Neurology billing presents a unique set of challenges for healthcare providers. Staying compliant with the rules and regulations set forth by insurance companies and government agencies, such as the Centers for Medicare and Medicaid Services ( CMS ), is of utmost importance. Non-compliance can lead to denials, delayed payments, and potential legal repercussions. Keeping up with the ever-changing landscape of neurology billing codes is another hurdle, requiring ongoing education and training to prevent errors and optimize revenue cycle management.
- Complexity of neurological disorders: Neurology is a complex medical specialty, and the disorders that neurologists treat can be very challenging to diagnose and code. This can lead to errors in coding, which can result in claim denials or delayed payments.
- Intricacy of documentation requirements: Neurology billing and coding is highly dependent on accurate and detailed documentation. This documentation must be compliant with the Health Insurance Portability and Accountability Act ( HIPAA ) and other regulations. Failure to meet documentation requirements can lead to claim denials.
- Regulatory compliance: The healthcare industry is constantly changing, and the regulations governing billing and coding are no exception. Neurologists must stay up-to-date on the latest regulations in order to ensure that their claims are compliant. Failure to comply with regulations can result in fines or penalties.
Strategies for tackling the challenges: For effective neurology billing and coding healthcare providers can adopt several key strategies:
- Expertise and Training : Investing in specialized training and continuous education for the billing and coding staff ensures a deep understanding of neurology-specific codes and regulations. This expertise minimizes errors, optimizes reimbursement, and mitigates compliance risks.
- Technology Integration : Implementing robust billing software and electronic health record (EHR) systems streamlines the neurology billing process. Automated coding, claims submission, and comprehensive reporting improve accuracy, efficiency, and overall revenue cycle management.
- Documentation Excellence : Thorough and accurate documentation is vital for successful neurology billing. Healthcare providers should emphasize comprehensive patient records, including detailed descriptions of diagnoses, treatments, and procedures. This documentation provides the foundation for precise coding and supports successful claims submission.
- Continuous Auditing and Monitoring : Regular internal audits and ongoing monitoring of billing processes are critical to identifying potential errors, compliance issues, and areas for improvement. Proactive measures ensure early detection and resolution of discrepancies, enhancing overall financial performance.
- Partnering with Experts : Collaborating with professional medical billing and coding services specializing in neurology can alleviate the burden on healthcare providers. These experts possess the knowledge, experience, and resources to navigate the complex billing landscape effectively, enabling medical practices to focus on patient care while ensuring optimal reimbursement.
Mastering the art of neurology billing and coding is indispensable for healthcare providers striving to provide exceptional neurology services while maintaining financial stability. By understanding the nuances of neurology billing codes, embracing compliance, and implementing efficient processes, medical practices can overcome challenges, optimize revenue, and ensure a seamless experience for both patients and providers.
Related Blog Posts
We all know how important is medical billing and coding for specialties when it comes…

Pediatricians have a lot on their plates. They need to provide excellent care to their…
Are you new to medical billing outsourcing companies in Australia? Then you must probably be…
Is spine surgery billing and coding critical for various clinical specialties like Neurology, Radiology, Orthopedics,…
Comments are closed.

Simplified guidelines for coding and documenting evaluation and management office visits are coming next year. Learn how to apply the guidelines to some common visit types.
CAROL SELF, CPPM, CPC, EMT, KENT MOORE, AND SAMUEL L. CHURCH, MD, MPH, CPC, FAAFP
Fam Pract Manag. 2020;27(6):6-11
Author disclosures: no relevant financial affiliations disclosed.
Editor's note: In its 2021 Medicare Physician Fee Schedule, CMS released new guidance regarding coding for prolonged E/M services. This article has been updated accordingly.

The American Medical Association (AMA) has established new coding and documentation guidelines for office visit/outpatient evaluation and management (E/M) services, effective Jan. 1, 2021. The changes are designed to simplify code selection and allow physicians to spend less time documenting and more time caring for patients. Physicians and other qualified health professionals (QHPs) will be able to select the level of office visit using either medical decision making (MDM) alone or total time (excluding staff time) on the date of service. In addition, the history and physical exam will be eliminated as components of code selection, and code 99201 will be deleted (code 99211 will not change). (See “ E/M coding changes summary .”)
To follow up on the previous FPM article detailing these changes (see “ Countdown to the E/M Coding Changes ,” FPM , September/October 2020), we have applied the 2021 guidelines to some common types of family medicine visits, and we explain below how documentation using a typical SOAP (Subjective, Objective, Assessment, and Plan) note can support the chosen level of service.
In each vignette, we've arrived at a code based only on the documentation included in the note. It's possible that a more extensive note could support a higher level of service by further clarifying the physician's decision making. But we've analyzed each case through an auditor's lens and tried not to make any assumptions that aren't explicitly supported by the note.
Starting in January, physicians and other qualified health professionals will be able to select the level of office visit using either medical decision making alone or total time (excluding staff time) on the date of service.
Medical decision making is made up of three factors: problems addressed, data reviewed, and the patient's risk. The highest level reached by at least two out of three determines the overall level of the office visit.
If the visit was time-consuming, but the medical decision making did not rise to a high level, the physician or qualified health professional may want to code based on total time instead.
MEDICAL DECISION MAKING (MDM)
Starting in January, physicians will be able to select the level of visit using only medical decision making, with a revised MDM table. (See the table at https://www.ama-assn.org/system/files/2019-06/cpt-revised-mdm-grid.pdf .)
The four levels of MDM (straightforward, low, moderate, and high) will be maintained but will no longer be based on checkboxes or bullet points. The level of service will be determined by the number and complexity of problems addressed at the encounter, the amount and complexity of data reviewed and analyzed, and the patient's risk of complications and morbidity or mortality.
Here's what that looks like in practice:
STRAIGHTFORWARD MDM VIGNETTE
An established patient presents for evaluation of eye matting. The documentation is as follows:
Subjective: 16 y/o female presents with a 2-day history of bilateral eye irritation. She denies any fever or sick contacts. She started having a slight runny nose and cough this morning. She thinks the matting is a little better than yesterday. She wears daily disposable contacts but hasn't used them since her eyes have been bothering her. Her younger sibling has had similar symptoms for a few days.
Objective: Temperature 98.8, BP 105/60, P 58.
General: No distress. Does not appear ill.
HEENT: Mild bilateral conjunctival erythema without discharge. No tenderness over eye sockets. EOMI, PERRL.
Neck: No cervical lymph nodes palpated.
Lungs: Clear to auscultation.
Assessment: Viral conjunctivitis.
Plan: Reviewed likely viral nature of symptoms. Supportive and conservative treatment options reviewed, including eye cleaning instructions and contact lens precautions. Call the office if symptoms persist or worsen. Avoid use of contacts until symptoms resolve.
CPT code: 99212.
Explanation: Under the 2021 guidelines, straightforward MDM involves at least two of the following:
Minimal number and complexity of problems addressed at the encounter,
Minimal (in amount and complexity) or no data to be reviewed and analyzed,
Minimal risk of morbidity from additional diagnostic testing or treatment.
This is the lowest level of MDM and the lowest level of service physicians are likely to report if they evaluate the patient themselves (code 99211 will still be available for visits of established patients that may not require the presence of a physician).
In this fairly common scenario, the assessment and plan make it clear that the physician addressed a single, self-limited problem (“minimal” in number and complexity, per the 2021 MDM guidelines) for which no additional data was needed or ordered, and which involved minimal risk of morbidity.
Per the 2021 CPT guidelines, “For the purposes of medical decision making, level of risk is based upon consequences of the problem(s) addressed at the encounter when appropriately treated.” In this case, there is little risk of morbidity to this patient from the viral infection diagnosed by the physician.
It's possible the physician considered prescribing an antibiotic in this case, but decided against it. Options considered but not selected can be used as an element for “risk of complications,” but they should be appropriate and documented. There is no documentation in this note to indicate the physician made that decision. The documentation provided, therefore, does not support a higher level of service using MDM. But if the physician did make that decision and the ensuing conversation with the patient was time-consuming, the physician always retains the option to choose the level of service based on time instead.
LOW LEVEL OF MDM VIGNETTE
An established patient presents for follow-up for stable fatty liver. The documentation is as follows:
Subjective: 62 y/o female presents for follow-up of nonalcoholic fatty liver. She has no other complaints today and no other chronic conditions. She denies any fever, weight gain, swelling, or skin color changes. She also denies any confusion. She continues to work at her regular job and reports no difficulties there. She denies any unusual bleeding or bruising. Energy is good. Diagnosis was made three years ago, incidentally, on an ultrasound. Condition has been stable since the initial full evaluation.
Objective: BP 124/70, P 76, Temperature 98.7, BMI 26.
General: Well-appearing. Alert and oriented x 3.
Eyes: Sclera nonicteric.
Heart: Regular rate and rhythm; trace pretibial edema.
Abdomen: Soft, nontender, no ascites, liver margin not palpable.
Skin: No bruising.
Labs reviewed and analyzed: CBC normal, CMP with elevated AST (62 IU/ml) and ALT (50 IU/ml), PT/PTT normal.
Last ultrasound was 3 years ago.
Assessment: Nonalcoholic steatohepatitis, stable.
Plan: LFTs continue to be improved since initial diagnosis and 30-pound intentional weight reduction. Continue monitoring appropriate labs at 6-month intervals. Follow up in 6 months, or sooner if swelling, bruising, or confusion. Avoid alcohol. Continue weight maintenance. She is reassured her condition is stable and has no other questions or concerns, especially in light of her prior extensive education on the topic. I am arranging for hepatitis A and B vaccination. Discussed OTC medications, including vitamin E, and for now will avoid them.
CPT code: 99213
Explanation: Under the 2021 guidelines, low-level MDM involves at least two of the following:
Low number and complexity of problems addressed at the encounter,
Limited amount and/or complexity of data to be reviewed and analyzed,
Low risk of morbidity from additional diagnostic testing or treatment.
In this vignette, the patient has one stable chronic illness, which is an example of an encounter for problems low in number and complexity. The risk of complications from treatment is also low. The “Objective” section indicates review of three lab tests, which qualifies as a moderate amount and/or complexity of data reviewed and analyzed. However, the level of MDM requires meeting two of the three bullets above, so the overall level remains low for this vignette.
MODERATE LEVEL OF MDM VIGNETTE
An established patient with obesity and diabetes presents with new onset right lower quadrant pain. The documentation is as follows:
Subjective: 42 y/o female presents for evaluation of 2 days of abdominal pain. She has a history of Type 2 diabetes, controlled. Pain is moderate, 6/10 currently, and 10/10 at worst. The pain is intermittent. The pain is located in the back and right lower quadrant, mostly. She denies diarrhea or vomiting but does note some nausea. She denies fever. She denies painful or frequent urination. She is sexually active with her spouse. She has had a hysterectomy due to severe dysfunctional bleeding. She has not tried any medication for relief. No position seems to affect her pain. She has not had symptoms like this before. Home glucose checks have been in the 140s fasting. Her last A1C was 6.9% two months ago. Family history: Sister with a history of kidney stones.
Objective: BP 160/95, P 110, BMI 36.1.
General: Appears to be in mild to moderate pain. Frequently repositioning on exam table.
HEENT: Moist oral mucosa.
Abdomen: Mild right-sided tenderness. No focal or rebound tenderness. Normal bowel sounds. No CVA tenderness. No suprapubic tenderness. No guarding.
UA with microscopy: 3 + blood, no LE, 50–100 RBCs, 5–10 WBCs.
CBC, CMP, CT stone study ordered stat.
Assessment: Abdominal pain – suspect renal stone. Also consider cholecystitis, gastroparesis, gastroenteritis, appendicitis, and early small bowel obstruction.
Diabetes, type 2, controlled.
Obesity – this is a risk factor for gall-bladder problems, but still favor renal stone.
Plan: Ketorolac 60 mg given in office for pain relief. Hydrocodone/APAP prescription for pain relief. Discussed at length suspicion of renal stone. Will plan lab work and pain control and await CT stone study. Urine sent to reference lab for microscopy. Drink plenty of fluids. Urine strainer provided. Call the office if worsening or persistent symptoms. Await labs/CT for next steps of treatment plan. Will follow up with her if urology referral is indicated.
CPT code: 99214
Explanation: Under the 2021 guidelines, moderate level MDM involves at least two of the following:
Moderate number and complexity of problems addressed at the encounter,
Moderate amount and/or complexity of data to be reviewed and analyzed,
Moderate risk of morbidity from additional diagnostic testing or treatment.
In this vignette, the patient has one undiagnosed new problem with uncertain prognosis (abdominal pain) and two stable chronic conditions (diabetes and obesity). Either one (the new problem with uncertain prognosis or two stable chronic conditions) meets the definition of a moderate number and complexity of problems under the 2021 MDM guidelines. But they do not meet the threshold of a high number and complexity of problems, even when combined.
The physician reviews or orders a total of four tests, which again exceeds the requirements for a moderate amount and/or complexity of data, but doesn't meet the requirements for the high category.
The prescription drug management is an example of moderate risk of morbidity. One might argue that the risk of morbidity is high because renal failure could result from a major kidney stone obstruction. But even then the overall MDM would still remain moderate, because of the number and complexity of problems addressed and the amount and/or complexity of data involved.
HIGH LEVEL OF MDM VIGNETTE
An established patient with a new lung mass and probable lung cancer presents with a desire to initiate hospice services and forgo curative treatment attempts. The documentation is as follows:
Subjective: 92-year-old male presents for follow-up of hemoptysis, fatigue, and weight loss, along with review of his recent chest CT. He reports moderate mid-back pain, new since last week. Appetite is fair. He denies fever. He continues to have occasional cough with mixed blood in the produced sputum.
Objective: BP 135/80, P 95, Weight down 5 pounds from 2 weeks ago, BMI 18.5, O2 sat 94% on RA.
General: Frail-appearing elderly male. No distress or shortness of breath. Able to speak in full sentences.
HEENT: No palpable lymph nodes.
Lungs: Frequent coughing and diffuse coarse breath sounds.
Heart: Regular rate and rhythm.
Ext: No extremity swelling.
MSK: Moderate tenderness over multiple thoracic vertebrae.
CT shows large right-sided lung mass suspicious for malignancy, along with a moderate left-sided effusion. Lytic lesions seen in T6-8.
Assessment: Lung mass, suspect malignancy with bone metastasis.
Plan: After extensive review of the findings, the patient was informed of the likely poor prognosis of the suspected lung cancer. We reviewed his living will, and he reiterated that he did not desire life-prolonging measures and would prefer to allow the disease to run its natural course. He also declines additional testing for diagnosis/prognosis. A shared decision was made to initiate hospice services. Specifically, we discussed need for oxygen and pain control. He declines pain medications for now, but will let us know. He and his son who was accompanying him voiced agreement and understanding of the plan.
CPT code: 99215
Explanation: Under the 2021 guidelines, high level MDM involves at least two of the following:
High number and complexity of problems addressed at the encounter,
Extensive amount and/or complexity of data to be reviewed and analyzed,
High risk of morbidity from additional diagnostic testing or treatment.
In this vignette, the patient has one acute or chronic illness or injury (suspected lung cancer) that poses a threat to life or bodily function. This is an example of a high complexity problem in the 2021 MDM guidelines. The physician reviewed one test (CT), so the amount and/or complexity of data is minimal. A decision not to resuscitate, or to de-escalate care, because of poor prognosis is an example of high risk of morbidity, and the physician has clearly documented that in the plan portion of the note. Consequently, even though the amount and/or complexity of data is minimal, the overall MDM remains high because of the problem addressed and the risk involved.
Under the new guidelines, total time means all time (face-to-face and non-face-to-face) the physician or other QHP personally spends on the visit on the date of service. Examples include time spent reviewing labs or reports, obtaining or reviewing history, ordering tests and medications, and documenting clinical information in the EHR.
The AMA has also created a new add-on code, 99417, for prolonged services. It can be used when the total time exceeds that of a level 5 visit – 99205 or 99215. (See “ Total time plus prolonged services template .”)
TIME-BASED CODING VIGNETTE
An established patient presents with a three-month history of fatigue, weight loss, and intermittent fever, and new diffuse adenopathy and splenomegaly. The documentation is as follows:
Subjective: 30-year-old healthy male with no significant PMH presents with a three-month history of fatigue, weight loss, and intermittent fever. He travels for work and has been evaluated in several urgent care centers and reassured that he likely had a viral syndrome. Fevers have been as high as 101, but usually around 100.5, typically in the afternoons. Testing for flu and acute mono has been negative. He denies high-risk sexual behavior and IV drug use. He denies any sick contacts. He has not had vomiting or diarrhea. He has not had any pain. He denies cough.
Objective: BP 125/80, P 92, BMI 27.4.
General: Well-nourished male, no distress.
HEENT: No abnormal findings.
Lungs: Clear.
Heart: No murmurs. Regular rate and rhythm.
Abdomen: Soft, non-tender, moderate splenomegaly.
Skin: Multiple petechia noted.
Lymph: Multiple cervical, axillary, and inguinal lymph nodes that are enlarged, mobile, and non-tender.
Assessment: Weight loss, lymphadenopathy, and splenomegaly
Plan: Prior to the visit, I spent 15 minutes reviewing the medical records related to his recent symptoms and various urgent care visits. We reviewed the differential at length to include infectious disease and acute myelodysplastic condition. I have ordered stat blood cultures, TB test, EBV titers, echo, and CBC. The pathologist called to report concerning findings on the CBC for likely acute leukemia. I called the patient to inform him of his results and need for additional testing. I also discussed the patient with oncology and arranged a follow-up visit for tomorrow. I spent a total of 92 minutes with record review, exam, and communication with the patient, communication with other providers, and documentation of this encounter.
CPT Codes: 99215 and 99417 x 3.
Explanation: In this instance, the physician has chosen to code based on time rather than MDM. The physician has documented 92 minutes associated with the visit on the date of service, including time not spent with the patient (e.g., time spent talking with the pathologist and time spent in documentation). According to the 2021 CPT code descriptors, 40–54 minutes of total time spent on the date of the encounter represents a 99215 for an established patient.
The 2021 CPT code set also notes that for services of 55 minutes or longer, you should use the prolonged services code, 99417, which can be reported for each 15 minutes beyond the minimum total time of the primary service (99215). The difference between the 92 minutes spent by the physician and the 40-minute minimum for 99215 is 52 minutes. There are three full 15-minute units of 99417 in those 52 minutes, so the physician may report three units of 99417 in addition to 99215. CPT 2021 instructs you to not report 99417 for any time unit less than 15 minutes, so the seven remaining minutes of prolonged service is unreportable.
Note that if this had been a new patient, the physician would only be able to report two units of 99417 in addition to 99205. Though the elements of MDM do not differ between new and established patients, the total time thresholds do. The range for a level 5 new patient is 60–74 minutes.
FINAL THOUGHTS
CPT does not dictate how physicians document their patient encounters. As illustrated above, a standard SOAP note can be used to support levels of MDM (and thus levels of service) under the 2021 guidelines.
Physicians who want to further solidify their documentation in case of an audit may choose to make the elements of MDM more explicit in their documentation. This could be particularly helpful for documenting the level of risk, which is the least clearly defined part of the MDM table and potentially most problematic because of its inherent subjectivity. Stating the level of risk and giving a rationale when possible allows a physician to articulate in the note the qualifying criteria for the submitted code. For example, going back to our vignette of moderate MDM, the physician could note in the chart, “This condition poses a threat to bodily function if not addressed, due to acute kidney injury for an obstructive stone.”
It is also worth noting that much of the note in each case is for purposes other than documenting the level of service. For instance, with history and physical exam no longer required, the subjective and objective portions of the note are recorded primarily for continuity or quality of care rather than to justify the level of service. This provides some administrative simplification. What's in the note will become more about what is needed for medical care and less about payment justification under the new guidelines. That's a plus for primary care.
We hope these examples are helpful as you prepare to implement the 2021 CPT changes. You can also visit https://www.aafp.org/emcoding for more resources and information.
Continue Reading
More in FPM
More in pubmed.
Copyright © 2020 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
Free Inquiry (631) 652-3106 | Request a quote
CPT Coding Reimbursement for Neurology Medical Billing
- Medical Billing and Coding Learning
Touseef Riaz
May 24, 2023.

- ucontrolbilling
CPT coding is an essential medical billing component. In addition, it plays a critical role in neurology medical billing. In neurology medical billing, CPT codes describe various neurological services. It includes diagnostic tests, consultation services, procedures, and follow-up visits. So, accurate CPT coding is crucial for neurology medical billing. In addition, it ensures that healthcare providers are reimbursed for their services. This guide will provide an overview of CPT coding reimbursement in neurology medical billing .

Standard CPT coding reimbursement in Neurology Medical Billing
Neurology medical billing involves using CPT codes to describe various diagnostic tests. Accurate coding of these tests is essential for proper reimbursement. Besides, it helps to avoid any potential billing errors or denials. Here are some commonly used CPT codes for diagnostic tests in neurology medical billing.
Office or another outpatient visit to check and manage a new patient. The session lasts for 30 minutes. The consultation involves a comprehensive evaluation of the patient’s medical history. It also includes a physical examination. The neurologist will also provide a detailed report of the talk.
This code reports outpatient visits to evaluate and manage an established patient. It lasts for 15 minutes.
Muscle testing, manual (separate procedure) with the report. This test diagnoses conditions such as muscular dystrophy, neuropathy, and myasthenia gravis.
Nerve conduction studies, 1-2 studies.
Spinal cords neurostimulator’s electronic analysis of implanted neurostimulator pulse generator/transmitter.
Neuromuscular junction testing (repetitive stimulation, paired stimuli), each nerve, any one method.
Neurobehavioral status examination.
Neuropsychological testing (e.g., Halstead-Reitan Neuropsychological Battery).
Therapeutic, prophylactic, or diagnostic injection (specify substance or drug). The injection can be subcutaneous or intramuscular.
Mechanical traction is applied to single or several regions.
This code is used to describe the nerve conduction study. It is a diagnostic test that evaluates the electrical activity of nerves. This test diagnoses peripheral neuropathy, carpal tunnel syndrome, and radiculopathy.
Neuromuscular junction testing (repetitive stimulation, paired stimuli), each nerve, any one method. This code describes the diagnostic testing of the location where muscles and nerves converge. It is known as the neuromuscular junction connection. This test is used to diagnose conditions such as myasthenia gravis.
Neurobehavioral status examination. This code describes the diagnostic testing of cognitive and behavioral functions. This test diagnoses conditions such as dementia and traumatic brain injury.
Office visits for a brand-new or current patient typically last 40 minutes. This code describes an office consultation for a new or established patient.
Office visits for a brand-new or current patient typically last 60 minutes. This code describes an extended office consultation for a new or established patient. The neurologist will also provide a detailed report of the consultation.
What are the Reimbursement Challenges with CPT Codes for Neurology Procedures?
Neurology medical billing can present various reimbursement challenges because of the intricate and specific procedures and services involved. Here are some of the common CPT coding reimbursement challenges with CPT codes for neurology procedures:
Lack of Specificity in Codes
Some CPT codes used for neurology procedures may need more specificity. Thus, it can lead to billing errors and denials. This is especially true for systems that are similar but require different coding. For instance, electromyography (EMG) and nerve conduction studies (NCS) are separate procedures. Therefore, these procedures need different coding. But they are sometimes coded together, leading to claim denials.
Unbundling refers to billing different CPT codes for components of a procedure. Unbundling can result in billing errors and denials. In addition, it can raise fraud and abuse concerns.
Documentation Requirements
Proper documentation is essential for accurate coding and billing, especially for neurology procedures. Only incomplete documentation can result in coding errors, denials, and compliance issues.
Insurance Coverage
Insurance coverage for specific neurology procedures and services may vary. It depends on the payer. So it is challenging to determine appropriate billing codes and reimbursement rates.
Medicare Policies
Medicare policies and reimbursement rates for neurology procedures may also pose challenges. Especially given the complex nature of some functions and services.
How to Maximize Reimbursement with CPT Codes for Neurology Follow-Up Visits?
In neurology medical billing, follow-up visits are essential. Maximizing CPT coding reimbursemen t for these visits requires accurate and appropriate use of CPT codes. Here are some tips for maximizing reimbursement with CPT codes for neurology follow-up visits:
Accurately document the Visit
Proper documentation of the follow-up visit is essential for accurate coding and billing. The documentation should include the reason for the visit and the patient’s medical history. It must also include a physical examination and any tests or procedures performed. This documentation should support the use of the appropriate CPT code.
Use the Appropriate CPT Code
There are different CPT codes for follow-up visits. It depends on the level of complexity and time spent with the patient. The appropriate CPT code should be selected based on the patient’s condition.
Use Modifier Codes When Appropriate
Modifier codes can provide additional information about the visit. Such as whether it was a telehealth visit or a procedure performed during the visit. Proper use of modifier codes can help ensure accurate reimbursement.
Stay Updated with Coding Changes
The coding and billing regulations for neurology follow-up visits may change over time. Staying current with these changes can help ensure appropriate codes are used.
Ensure Compliance with Payer Policies
Different payers may have different policies and requirements for neurology follow-up visits. Ensuring compliance with these policies can help avoid billing errors and denials .
What is the Importance of Accurate CPT Coding for Neurology Telehealth Services?
Telehealth services have become increasingly important in neurology, especially during the COVID-19 pandemic. Accurate CPT coding for neurology telehealth services is critical to medical billing. Thus, it helps to ensure that patients receive the care they need. Here are some reasons why accurate CPT coding reimbursement is essential for neurology telehealth services:
Reimbursement
Accurate CPT coding for neurology telehealth services is essential for a proper refund. Incorrect or incomplete coding can lead to billing errors and denials. In addition, it can impact healthcare providers’ financial health and limit patient care access.
It is also essential for compliance with regulatory requirements. Therefore, improper coding can result in compliance issues and potential legal liabilities.
Quality of Care
It is essential for ensuring the quality of care provided to patients. In addition, proper coding helps to ensure that the appropriate services are billed and that patients receive the necessary care for their neurological conditions.
Patient Satisfaction
Accurate coding for neurology telehealth services can also impact patient satisfaction. Proper coding helps ensure that patients receive the care they need and that their insurance covers the services provided.

Transparency
It promotes transparency and accountability in the healthcare system. Proper coding ensures that payers and patients understand the services provided. They also know about the associated costs.
What is a Joint Neurodynamics CPT Coding and Reimbursement?
Neurodynamics is a technique used in neurology to assess the function of the nervous system. It diagnoses neurological disorders. Here are some standard CPT codes used for neurodynamic testing. These codes are also considered for reimbursement:
95905 -Nerve Conduction Studies
This code reports motor and sensory nerve conduction studies. Neurologists perform NCS on one or more nerves. This code can be used for the upper or lower extremities, trunk, and head.
95907 – Nerve Conduction Studies, Each Limb
This code reports motor and sensory nerve conduction studies performed in each limb.
95886 – Needle Electromyography
This code reports the needle electrode insertion into a muscle to record. It analyzes the electrical activity in power.
95885 – Needle Electromyography, Limited Study
This code reports a little needle electromyography study, typically involving a single muscle.
95904 – Autonomic Nervous System Testing
This code reports tests that evaluate the autonomic nervous system’s function—for example, heart rate variability and sudomotor testing.
95860 – EMG, One Extremity with or without Related Paraspinal Areas
This code reports an electromyography test performed on a spine.
CPT coding reimbursement for neurodynamic testing will depend on many factors. It includes specific CPT codes used, the payer, and the patient’s insurance coverage. Therefore, healthcare providers and medical billers must stay updated with the latest coding and billing regulations. Proper documentation and precise coding are essential for an appropriate refund for neurodynamic testing.
What is Vascular Surgery: 2020 CPT Coding and Reimbursement Update?
In 2020, there were several updates to the CPT codes and the reimbursement rates for vascular surgery procedures. Here are some of the fundamental changes:
New codes for endovascular repair of iliac artery:
Two new codes were added for endovascular repair of iliac artery aneurysms. It was previously reported with unlisted codes. The new regulations are 34713 for unilateral repair and 34714 for bilateral repair.
Reimbursement rates for endovascular repair of abdominal aortic aneurysms:
The reimbursement rates for endovascular repair of abdominal aortic aneurysms were included in 2020.
How do you find CPT Coding Reimbursement Lookup?
There are several ways to look up CPT code reimbursement rates, including:
Through means of the Centers for Medicare and Medicaid Services (CMS). The CMS Physician Fee Schedule is a publicly available database. It provides reimbursement rates for CPT codes for Medicare beneficiaries. Healthcare providers can use this database to determine reimbursement rates for specific CPT codes.
What is a CPT Coding Reimbursement?
A CPT code reimbursement is the amount of money an insurance payer pays a healthcare provider. The payer can be Medicare or a private insurance company. The patient gets reimbursements for a specific medical procedure or service.
Several third-party resources are available that provide information on CPT code reimbursement rates, such as the American Medical Association (AMA). Besides, commercial databases such as EncoderPro and Find-A-Code. These resources may require a subscription or fee to access.
Where Can I Get a List of CPT Codes?
The american medical association (ama) website.
The AMA website lists all CPT codes along with their descriptions, guidelines, and coding changes. You can access the list for free but may need to create an account.
The Centers for Medicare and Medicaid Services (CMS) Website.
The CMS website lists all CPT codes, descriptions, and payment rates for Medicare beneficiaries. You can access the list for free but may need to create an account.
Commercial Coding Databases
Several commercial coding databases, such as EncoderPro and Find-A-Code, comprehensively lists CPT codes, descriptions, and coding guidelines. These databases may need a subscription or fee to access.
How do CPT Codes drive Reimbursement?
CPT coding reimbursement provides a standardized way to identify and bill for medical procedures. It includes all evaluation, management, and diagnostic services. Each CPT code is associated with a specific reimbursement rate. Insurance payers like Medicare or private insurance companies determine this rate.
How do I Find my CPT Code Reimbursement?
To find your CPT code reimbursement, you can follow these steps:
- Identify the CPT code(s) for the medical procedure(s) or service(s) provided. You can also find it by contacting your healthcare provider.
- Determine the insurance payer for the service. This could be Medicare or a private insurance company.
- Check the insurance payer’s fee schedule or reimbursement policy. It will help to find the reimbursement rate for the specific CPT code. This information can typically be found on the payer’s website or by contacting their customer service department.
- Multiply the reimbursement rate by the number of units or time associated with the service provided. Some CPT codes have specific unit or time requirements, which can affect the reimbursement amount.
What are the highest reimbursed CPT Codes?
The highest reimbursed CPT codes can vary depending on geographic location, insurance payer, and the specific procedure or service performed. However, some of the highest reimbursed CPT codes in general include:
- 69990 – Neurostimulator analysis, programming, and reprogramming: This code is used for programming and analyzing neurostimulators, devices used to treat chronic pain and other neurological conditions.
- 93229 – Implantable cardioverter-defibrillator (ICD) programming: This code is used for programming and analyzing ICDs, devices used to treat irregular heart rhythms.
- 96372 – Therapeutic, prophylactic, or diagnostic injection: This code injects medications or other substances, such as vaccines.
- 43239 – Upper gastrointestinal endoscopy with biopsy: This code is used for a diagnostic procedure that examines the upper gastrointestinal tract and includes taking tissue samples for biopsy.
- 32557 – Removal of thoracic duct: This code removes the thoracic duct, a major vessel in the lymphatic system.
Accurate and efficient CPT coding reimbursement is crucial for neurology medical billing. It is essential to stay up-to-date with the latest coding guidelines and regulations. Healthcare providers can streamline billing processes and optimize financial performance with the right tools and expertise. U Control Billing helps reduce administrative workload, maximizing revenue through accurate billing and coding.

A couple of years ago, I executed the effective plan of creating a Medical billing and Coding company named U Control Billing. The company aims to bring revolutionary advancements to foster medical billing and coding revenues. As an official member of HIA-LI and MGMA, I feel honored in providing networking opportunities, problem-solving, and improving the revenue management cycle.
- Awards and Recognition
- Billing Specialist Duties
- Commercial Insurance
- Free Medical Billing
- Medical Billing
- Medical Billing Software
- Medical Billling Services
- Medical Coding
- Telemedicine
- Uncategorized
Recent Posts
- Streamlining Abdominoplasty Medical Billing Services: A Comprehensive Guide May 29, 2024
- What are the Medical Billing Time Limits by State? May 22, 2024
- What is the CPT Code for Ear Wax Removal Bilateral? May 16, 2024
- Navigating Medical Bills for Terminally Ill Patients: Understanding the Financial Challenges May 10, 2024
- Medical Billing for Motor Vehicle Accidents: Navigating the Complexities May 1, 2024
You May Also Like…

Streamlining Abdominoplasty Medical Billing Services: A Comprehensive Guide
by Touseef Riaz
Abdominoplasty, commonly referred to as a tummy tuck, is a surgical...

What are the Medical Billing Time Limits by State?
Medical billing time limits by state plays a crucial role in the...

What is the CPT Code for Ear Wax Removal Bilateral?
The correct Current Procedural Terminology code is crucial for...
Ready To Get Started?
Pin it on pinterest.
Diseases & Diagnoses
Issue Index
- Case Reports
Columns | May 2022
Practice Management: Botulinum Toxin Billing & Coding Update
What neurologists need to know to earn appropriate reimbursement in 2022..
Martin Taylor, DO, PhD; Laxman Bahroo, DO, FAAN; and Carrie Dougherty, MD, FAHS
As the number of conditions treated with botulinum toxin (BTX) increases, so does the importance of clinicians understanding the intricacies of billing and coding for this therapeutic agent. Unfortunately, even after a clinician feels comfortable with neurotoxin injection technique, the process of authorization, billing, and coding may still seem daunting. Clinicians need to be familiar with the purchase and storage of BTX, prior authorization requirements across insurers, and appropriate documentation of indications and procedures. Correct coding, using current procedural terminology (CPT) and International Statistical Classification of Diseases, 10th revision (ICD-10), linkage is critical for successful integration of BTX therapy into clinical practice (Box 1). 1
BOX 1. Tips For Initiating Therapy With Botulinum Toxin
- need for botulinum toxin (BTX),
- prior treatment failures, and
- injection plan.
- preferred toxin,
- ICD-10 diagnosis codes,
- prior treatment failures,
- requested number of vials,
- CPT procedure codes, and
- guidance procedure code.
- Schedule patients with traditional Medicare/Medicaid as soon as possible because prior authorization is not required.
- verify benefits and obtain prior authorization;
- receive BTX from a specialty pharmacy if required; and
- avoid multiple calls from patients inquiring about status.
- Obtain consent at time of scheduling from patients with private insurance or Medicare/Medicaid HMO if a prior authorization service may be utilized.
Prior Authorization
Medicare, Medicaid, and private insurances cover BTX treatment for on- and off-label uses considered medically necessary. Uses for many off-label conditions (eg, oromandibular dystonia or limb dystonia) are considered standard of care and are commonly approved. Medicare policies can vary from state to state, but private insurance policies are typically universal. Being familiar with the policies in your state can save time and frustration when submitting prior authorization.
With traditional Medicare or Medicaid, no prior authorization is needed for BTX. Payment will occur if the procedure is covered by your state’s policy and if the proper linkage between ICD-10 code and CPT code is documented. Prior authorization for BTX, including for on-label uses, should be obtained for all patients with private insurances or Medicaid/Medicare health maintenance organization (HMO) and Medicare/Medicaid. Prior authorization can be requested by contacting the insurance company directly or by using the BTX manufacturer’s prior authorization services, which can expedite approvals and save staff time. Patients must give written consent to allow the company to contact their insurance provider. An office note justifying the reasoning for BTX treatment and discussing failed treatment along with a letter of medical necessity should always be included with the prior authorization request (Box 1).
Benefit verification is first performed to ensure the patient’s insurance policy is current and covers injectable treatments such as BTX. Benefit verification does not equal preapproval or medical necessity. Prior authorization must be performed to increase the probability of proper payment. Most insurance companies will grant prior authorization for 6 to 12 months or for 2 to 4 treatments. Injections need to be performed within this authorization window or payment could be denied. Authorization results typically include approved dates of service and approved CPT codes. The allowable number of toxin units and how to obtain the drug (ie, the buy-and-bill process vs using a specialty pharmacy) are also reported.
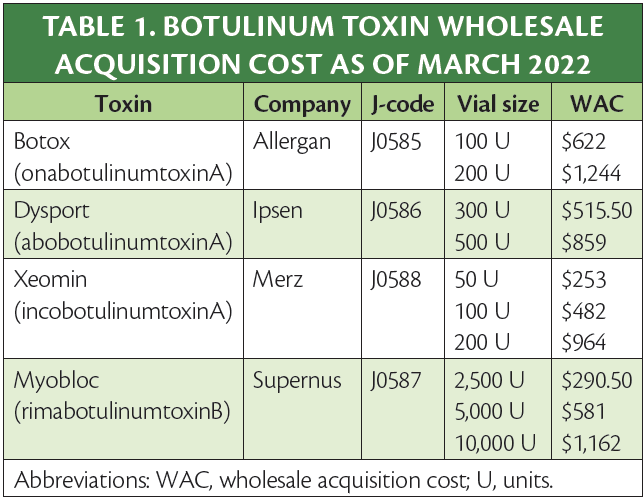
Ordering, Storing, and Billing for BTX
BTX procurement options include buy-and-bill by the practice or provided by a specialty pharmacy. Traditional Medicare and some private insurance companies require practices buy-and-bill the drug. Many private insurers require the use of a third-party specialty pharmacy. The use of a specialty pharmacy may limit risk of lost funds from insurance denials; however, it also reduces total reimbursement. If clinicians obtain BTX and bill from their stock, a margin above the cost of the drug is reimbursed. For Medicare, the margin is up to 6% above the average wholesale cost, making buy and bill minimally profitable. Margins for private carriers or workers’ compensation benefits may be much larger, making buying and billing more attractive. Your billing staff should be able to provide an expected margin per unit for each major insurance carrier. OnabotulinumtoxinA (Botox; Allergan, Madison, NJ) and incobotulinumtoxinA (Xeomin; Merz, Raleigh, NC) are billed by the single unit, abobotulinumtoxinA (Dysport; Ipsen, Cambridge, MA) per 5 units, and rimabotulinumtoxinB (Myobloc; Supernus, Rockville, MD) per 100 units. Remember that both the amount of drug used for injection and the drug wasted should be charged. For example, if a 200-unit vial of onabotulinumtoxinA is mixed to inject a person being treated for chronic migraine with 155 units, the 45 units wasted are also billed. When billing waste, add a JW modifier (Table 1).
Click to view larger
Availability of toxin samples, discounts, and patient assistant programs varies among companies. Check with your local BTX manufacturer’s representative for such programs. Each toxin can be ordered directly from the manufacturer with expected next day arrival. Avoid placing orders that could arrive on the weekend for toxins that require refrigeration. It is recommended that all of the toxins be stored together in a locked refrigerator between 2°C and 8°C with a temperature alarm. In the case of specialty pharmacies, have the drug sent directly to your office rather than the patient’s home to ensure proper storage. A separate log for drugs obtained by the practice and another for drugs obtained from specialty pharmacies is recommended, with documentation of lot numbers. Regular reconciliation of inventory on a weekly or monthly basis is also suggested.
Procedure Coding, Documentation, and Billing
Proper documentation is essential for correct payments (Box 2). A procedure note should be detailed and include diagnosis, site, injection location, dilution, electrophysiologic/ultrasound guidance, provider of medication (buy-and-bill vs specialty pharmacy), amount of BTX used, amount wasted, approval dates, and prior authorization number. Although not essential, insurance companies like to see a written procedure note with a diagram of the areas injected and an outline of the specific dosages injected at each site. From a clinical perspective, this makes reproducing injections in the future easier. For ongoing treatment, response to therapy should also be clearly documented. A real-time inventory log is suggested with the date of service, amount, and source of BTX (practice stock vs specialty pharmacy), along with the patient’s name/medical record number, and lot number in case of an unexpected side effect or drug recall. This can be performed using an inventory management system or by creating a spreadsheet.
BOX 2. Botulinum Toxin Billing And Coding Pearls
- Be aware of which insurance carriers in your area allow for injections to be performed every 12 weeks (84 days) vs every 90 days or 13 weeks, to ensure payment.
- Medicare requires the proper CPT code linked with the approved ICD-10 code for reimbursement.
- Medicare may not pay for buy-and-bill of the toxin if the patient is in a nursing home.
- record temperature daily and
- link the thermostat to your alarm system to prevent loss of the drug in case of faulty refrigerator or power outage.
- Keep separate inventory logs of stock drug with lot number, date received/injected, and whether from buy-and-bill or specialty pharmacy.
- Consider collecting the patient’s expected coinsurance amount before scheduled injection, similar to what is commonly done for surgical procedures.
CPT Codes for Chemodenervation
Specific chemodenervation codes for BTX are based on the appropriate anatomic location site injected (Table 2). 2-5 The Centers for Medicare and Medicaid Services (CMS) will allow payment for 1 injection per site, regardless of the number of injections made into the site. 6 For injection into bilateral parotid and/or submandibular glands for sialorrhea use CPT 64611 only once with no modifier. Any injection in the cranium (64612) including corrugator, frontalis, temporalis, occipitalis, facial muscles, and masseter are considered head/face. This code can be used bilaterally using the right (RT), left (LT), or bilateral (50) modifiers. All injections within the chronic migraine paradigm are considered 1 site (64515) even though injections are performed in the head/face, cervical paraspinals, and trapezii, and no modifiers are permitted.
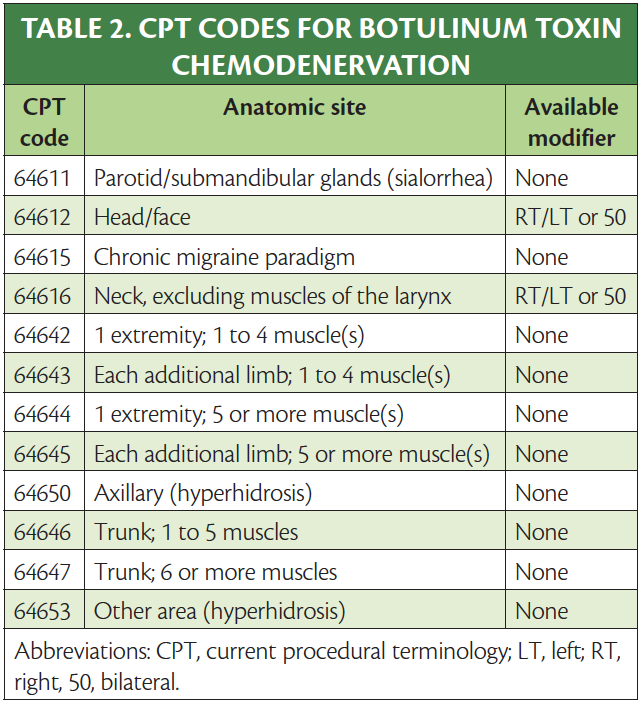
Both axillae are considered 1 site (64640 chemodenervation of eccrine glands) and can only be used once per session. When injecting for hyperhidrosis in other sites (eg, scalp, face, or extremities), use 64643, chemodenervation of eccrine glands; other area(s). For injections of neck muscles for conditions (eg, cervical dystonia) use code 64616 (chemodenervation of neck muscle(s) excluding muscles of the larynx), which can be used bilaterally using RT, LT, or 50 modifiers.
Chemodenervation of 1 or more extremities involves the use of several different CPT codes. The first code is known as the base code and should represent the limb with the most muscles injected. Pick code 64642 chemodenervation of 1 extremity; 1 to 4 muscle(s) or 64644 chemodenervation of 1 extremity; 5 or more muscle(s). Further limb injections can be billed using add-on codes based on the number of muscles injected in each limb. No modifiers are necessary. For each additional extremity, 1 to 4 muscle(s) injected, use +64643 and for each additional limb injected, 5 or more muscles, use +64645.
Trunk muscles are an independent region that includes the erector spinae/paraspinal muscles and rectus abdominis/obliques. Use CPT code 64646 when injecting 1 to 5 muscles and 64647 for 6 or more. Each code can only be used once per session. Based on the site definition above, muscles such as the trapezius/levator scapulae (below C7), rhomboid, gluteus, and piriformis are considered limb/limb girdle muscles.
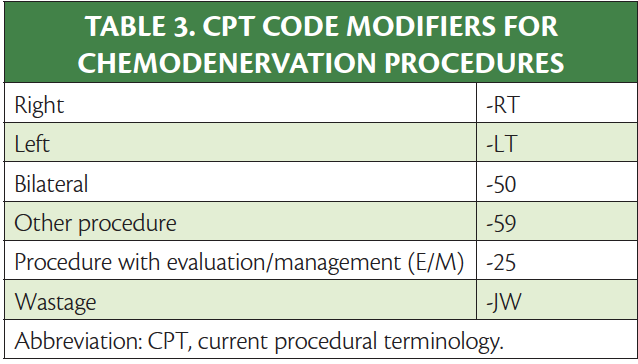
Insurance companies allow the addition of modifiers RT, LT, or 50. Check with your local carriers to determine when to bill with a modifier and which modifier is appropriate (Table 3). Typically, if a code is listed a second time on the billing sheet without a modifier, it is automatically kicked out as a duplicate. Some codes such as 64611 and 64615 can be used only once per injection session and, therefore, modifiers will not apply.
The use of an evaluation and management (E/M) code along with a BTX procedure is discouraged. This coding is only appropriate if a separate identifiable medical service is provided for a different diagnosis than the one used for BTX. For example, if a patient with Parkinson disease (PD) is seen for medical management of PD and also receives treatment with BTX for sialorrhea, an E/M could be used with a -25 modifier. It is imperative that the medical diagnosis is linked to the E/M and that the other diagnosis (in this case sialorrhea) is linked to the CPT code to ensure proper reimbursement.
Anatomic Guidance
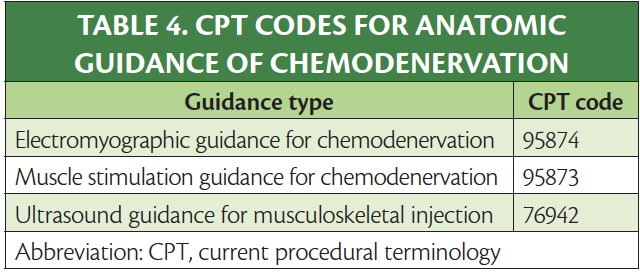
To ensure efficacy and safety, electrophysiologic or visual guidance is suggested for many injection locations. Electromyography, muscle stimulation, and ultrasound can be used independently or together based on clinical necessity. Medicare, for instance, allows for electromyography or electric stimulation to be performed with ultrasound guidance. Use of these techniques maximizes clinical efficacy, decreases potential side effects, and is reimbursable. Table 4 reviews the CPT codes for BTX injections under anatomic guidance. Each code can be used once per date of service.
Reimbursement and Collections
Be familiar with your major regional insurance policies for BTX to help reduce delays in payment and even denials. Review each claim before the patient’s next injection cycle to ensure the procedure, anatomic guidance, and drug have all been paid in accordance with your payer contract. Commonly, the carrier may only pay for procedures that are considered medically necessary. If a particular code is paid bilaterally by a payer, reimbursement for the second side is typically reduced by half. Each toxin company has reimbursement specialists that can assist in billing and coding, insurance verification, local coverage policy support, and claims denials and appeals. Consider requesting an analysis every 6 to 12 months to avoid loss of revenue and repetitive billing errors.
1. American Medical Association. CPT Standard - Current Procedural Terminology (Standard Edition). 1st ed. American Medical Association; 2013.
2. Botox. Prescribing information. Allergan Inc; 2021.
3. Dysport. Prescribing information. Ipsen Biopharm Ltd; 2020.
4. Myobloc. Prescribing information. Solstice Neurosciences, LLC; 2019.
5. Xeomin. Prescribing information. Merz Pharmaceuticals, LLC; 2021.
6. Centers for Medicaid & Medicare Service. 2022 ASP Drug Pricing Files. Updated March 9, 2022. Accessed March 14, 2022. https://www.cms.gov/medicare/medicare-part-b-drug-average-sales-price/2022-asp-drug-pricing-files
MT is on the speaker’s bureau and serves as a consultant to Abbvie and Biohaven and has received grants from Abbvie, Neurocrine, Ipsen, and Aeon LB is on the speaker’s bureau and serves as a consultant to Abbvie, Acadia, Acorda, Amneal, Ipsen, Jazz, Kyowa Kirin, Neurocrine, Sunovion, Supernus, and Teva CD is a consultant for Abbvie, Biohaven, Impel, Eli Lilly, Lundbeck, Novartis, Theranica, and Regeneron and has received clinical trial grants from Abbvie, Eli Lilly, Amgen, and Axsome

Martin Taylor, DO, PhD
Clinical Associate Professor Ohio University, College of Osteopathic Medicine Chief of Neurology, Orthoneuro Columbus, OH

Laxman Bahroo, DO, FAAN
Vice Chair of Finance Associate Professor & Residency Director Neurology Director, Botulinum Toxin Clinic Medstar Georgetown University Hospital Washington, DC

Carrie Dougherty, MD, FAHS
Program Director, Headache Medicine Fellowship Associate Professor of Neurology Medstar Georgetown University Hospital Washington, DC
About the Cover Artist
Epilepsy Essentials: VideoEEG Analysis
Jacqui-Lyn Saw, MBBS; and Elson L. So, MD
This Month's Issue
Lex Denysenko, MD, FACLP; and Deena Kuruvilla, MD, FAHS
Stewart J. Tepper, MD; Peter McAllister, MD, FAAN; and Teshamae Monteith, MD
Gustavo Dalto Barroso Machado, MD, MSc; David Pasquale, MD; and José Biller, MD, FACP, FAAN, FANA, FAHA

Related Articles
Swati Pradeep, DO; and Jaime M. Hatcher-Martin, MD, PhD
Richa Tripathi, MD, MS; J. Lucas McKay, PhD, MSCR; and Christine D. Esper, MD, FAAN
Sign up to receive new issue alerts and news updates from Practical Neurology®.
Related News
Jump to content

Chobanian & Avedisian School of Medicine/CCE
Bookmark/search this post.

You are here
E&m coding and documentation in 2024.
Course Instructor: Megan Priore, CPC, PCA , Senior Auditor and Clinician Educator
Updating new providers and current providers of the coding changes since 1/1/2021
What drives the code choices
Office Level visit Decision Making
Understanding Patient and Visit Types
Medical Decision Making
- 1.00 AAPA Category I CME
Boston University Chobanian & Avedisian School of Medicine designates this Enduring activity for a maximum of 1.00 AMA PRA Category 1 Credit™ . Physicians should claim only the credit commensurate with the extent of their participation in the activity.

IMAGES
VIDEO
COMMENTS
Billing and Coding. To be indispensable to its members, the AAN provides resources to help them with coding and reimbursement. This includes resources about the Current Procedural Terminology (CPT) code set, staying current on Evaluation and Management (E/M) coding and documentation guidelines, and understanding how Medicare and other payers ...
of neurology procedure codes include: Electroencephalogram (EEG): CPT codes 95812, 95813, 95816, and 95819; Electromyography (EMG): CPT codes 95860, 95861, 95863, and 95864; Nerve conduction studies: CPT codes 95905, 95906, 95907, and 95908. It is important to note that coding guidelines and rules may vary depending on the specific
INTRODUCTION. The changes to 2021 Evaluation and Management (E/M) coding involve only outpatient codes for new patient visits and follow-up visits described by Current Procedural Terminology (CPT) codes 99202-99205 and 99211-99215. 1 Knowing the history of the development of these codes and the rationale for the code changes is key to understanding the improvements that align code structure ...
Step 1: Total time. Think time first. If your total time spent on a visit appropriately credits you for level 3, 4, or 5 work, then document that time, code the visit, and be done with it. But if ...
These code descriptors do not apply until 2021 — you will not find these code descriptors in your 2020 CPT® code book. CPT® code 99201 Office or other outpatient visit for the evaluation and management of a new patient, which requires these 3 key components: A problem focused history; A problem focused examination; Straightforward medical ...
R41.2 Retrograde Amnesia. CPT codes for neurology and neuromuscular procedures. The CPT code range for neurology and neuromuscular procedures includes: 95700-95811 Sleep Medicine Testing and Long-term EEG Procedures. 95812-95830 Routine Electroencephalography (EEG) Procedures.
Neurosurgery/ Neurology A comprehensive illustrated guide to coding and reimbursement 2022 optum360coding.com CODING COMPANION ATNN_ATNN21_CVR_Final.indd 1 5/7/2020 11:44:12 AM
The American Medical Association (AMA) has established new coding and documentation guidelines for office visit/outpatient evaluation and management (E/M) services, effective Jan. 1, 2021. The ...
The following is a list of standard codes used on bills for neurology consultations: CPT code 95700-95700 is used for long-term EEG setup. CPT code 95700-95700, Sleep medicine testing procedure. CPT code 95705-95726, extended-term EEG monitoring. CPT code 95812-95836, Routine electroencephalography. CPT code 95851-95857, Range of Motion testing ...
CPT® code 99213: Established patient office or other outpatient visit, 20-29 minutes. As the authority on the CPT® code set, the AMA is providing the top-searched codes to help remove obstacles and burdens that interfere with patient care. These codes, among the rest of the CPT code set, are clinically valid and updated on a regular basis to ...
Pay parity for phone services was agreed to by CMS with respect to evaluation and management (E/M) visits, matching levels 2 to 4 established outpatient visits based on time, retroactive to March 1, 2020. 6,7 There are 238 codes listed under Medicare telehealth services, with 135 codes temporarily added for the PHE for the COVID-19 pandemic. 8
Neurology and Neuromuscular Procedures. 95700-95811. Sleep Medicine Testing and Long-term EEG Procedures. 95812-95830. Routine Electroencephalography (EEG) Procedures. 95829-95836. Electrocorticography. 95836-95857. Range of Motion Testing.
99214. High Complexity. 99245. 99205. 99215. The above lists the most commonly used E/M codes in outpatient neurology: levels 3, 4 and 5 (low, moderate and high complexity, respectively). For levels 1 and 2, click here. Alternative E/M Coding: Using Time.
ICD-10-CM Diagnostic Codes. ICD-10-CM diagnostic codes listed are common diagnoses or reasons the procedure may be necessary. This list in most cases is inclusive to the specialty. Some ICD-10-CM codes are further identified with the following icons: 8 Newborn: 0 9 Pediatric: 0-17 x Maternity: 9-64 y Adult: 15-124.
May 24, 2023. CPT coding is an essential medical billing component. In addition, it plays a critical role in neurology medical billing. In neurology medical billing, CPT codes describe various neurological services. It includes diagnostic tests, consultation services, procedures, and follow-up visits. So, accurate CPT coding is crucial for ...
Effective January 1, 2021. Shorter prolonged services code to capture each 15 minutes of critical physician/other QHP work beyond the time captured by the office or other outpatient service E/M code. Used only when the office/other outpatient code is selected using time. For use only with 99205, 99215.
OFFICE VISIT PROCEDURAL CODING. Procedural coding in a behavioral neurology encounter is typically composed of standard E/M codes plus CPT code 96111 for developmental testing and CPT code 96116 for a separately reported neurobehavioral status examination. Modifier 25 is used with the E/M code to identify it as separate and distinct from the neurobehavioral or developmental testing.
In this case, codes for the physician's work for an initial day hospital visit (99222), 3 daily inpatient follow-up visits (99232), a discharge-day note (99238), and 5 video-EEG monitoring days (95720) would be coded. The technical codes are the set-up code on day 1 (95700), and 5 units of (95716). Those physician and technical video-EEG CPT ...
This can be performed using an inventory management system or by creating a spreadsheet. BOX 2. Botulinum Toxin Billing And Coding Pearls. Be aware of which insurance carriers in your area allow for injections to be performed every 12 weeks (84 days) vs every 90 days or 13 weeks, to ensure payment.
Updating new providers and current providers of the coding changes since 1/1/2021. What drives the code choices Office Level visit Decision Making. Understanding Patient and Visit Types. Medical Decision Making. Session date: 05/24/2024 - 10:00am to 11:00am EDT. 1.00 AAPA Category I CME;