- Open access
- Published: 04 September 2021

Journey mapping as a novel approach to healthcare: a qualitative mixed methods study in palliative care
- Stephanie Ly 1 ,
- Fiona Runacres 1 , 2 , 3 &
- Peter Poon 1 , 2
BMC Health Services Research volume 21 , Article number: 915 ( 2021 ) Cite this article
12k Accesses
16 Citations
6 Altmetric
Metrics details
Journey mapping involves the creation of visual narrative timelines depicting the multidimensional relationship between a consumer and a service. The use of journey maps in medical research is a novel and innovative approach to understanding patient healthcare encounters.
To determine possible applications of journey mapping in medical research and the clinical setting. Specialist palliative care services were selected as the model to evaluate this paradigm, as there are numerous evidence gaps and inconsistencies in the delivery of care that may be addressed using this tool.
A purposive convenience sample of specialist palliative care providers from the Supportive and Palliative Care unit of a major Australian tertiary health service were invited to evaluate journey maps illustrating the final year of life of inpatient palliative care patients. Sixteen maps were purposively selected from a sample of 104 consecutive patients. This study utilised a qualitative mixed-methods approach, incorporating a modified Delphi technique and thematic analysis in an online questionnaire.
Our thematic and Delphi analyses were congruent, with consensus findings consistent with emerging themes. Journey maps provided a holistic patient-centred perspective of care that characterised healthcare interactions within a longitudinal trajectory. Through these journey maps, participants were able to identify barriers to effective palliative care and opportunities to improve care delivery by observing patterns of patient function and healthcare encounters over multiple settings.
Conclusions
This unique qualitative study noted many promising applications of the journey mapping suitable for extrapolation outside of the palliative care setting as a review and audit tool, or a mechanism for providing proactive patient-centred care. This is particularly significant as machine learning and big data is increasingly applied to healthcare.
Peer Review reports
Introduction
Patterns of healthcare utilisation are evolving in response to the ageing population and increasing burden of chronic disease. There is an urgent need to ensure timely proactive medical care, effective and efficient resource deployment, while averting unnecessary, often distressing, emergency department (ED) presentations, admissions and conveyor belt medicine. A key area of medicine able to address these issues is palliative care.
Central to optimal delivery of palliative care is timely initiation [ 1 , 2 , 3 ]. However, differing patient, illness trajectory and clinical factors have resulted in inconsistencies in the degree of care provided [ 4 , 5 ]. This has subsequently translated into significant variability in palliative care research and limitations in applying international evidence to clinical practice [ 6 ]. The utilisation of journey mapping has the potential to address these inconsistencies and to our knowledge, this research is the first of its kind.
Journey mapping is a relatively new approach in medical research that has been adapted from customer service and marketing research [ 7 ]. It is gaining increasing recognition for its ability to organise complex multifaceted data from numerous sources and explore interactions across care settings and over time. Medical journey mapping involves creating narrative timelines, by incorporating markers of the patient experience with healthcare service encounters. Integrating diverse components of the patient healthcare journey provides a holistic perspective of the relationships between the different elements that may guide directions for change and service improvement. As medical journey mapping is still in its infancy, there is an absence of literature exploring implementation. Of the existing literature, journey mapping techniques are described mainly in process papers, outlining their potential utility in observing healthcare delivery and patient outcomes [ 8 , 9 , 10 , 11 , 12 ]. However journey mapping paradigms have broader significance across healthcare, especially in an environment for which machine learning, big data and artificial intelligence is maturing.
We aimed to determine whether journey mapping could contribute to the improvement of patient-centred medical research in a palliative care setting and provide new insight into possible “pivot-points” or moments of care that could be altered to improve care delivery. Specifically, we sought to determine whether journey maps were able to assist in capturing a holistic, longitudinal and more integrative patient history whilst outlining healthcare provision and identifying gaps in care.
Study design
We performed a qualitative mixed-methods analysis of a journey mapping tool. The tool was purpose-developed and sample journey maps were derived from the scanned medical records of palliative care patients. A panel of specialist palliative care providers were then involved in an online questionnaire combining a modified Delphi approach with inductive thematic analysis. Figure 1 depicts a flow diagram of the methodology.
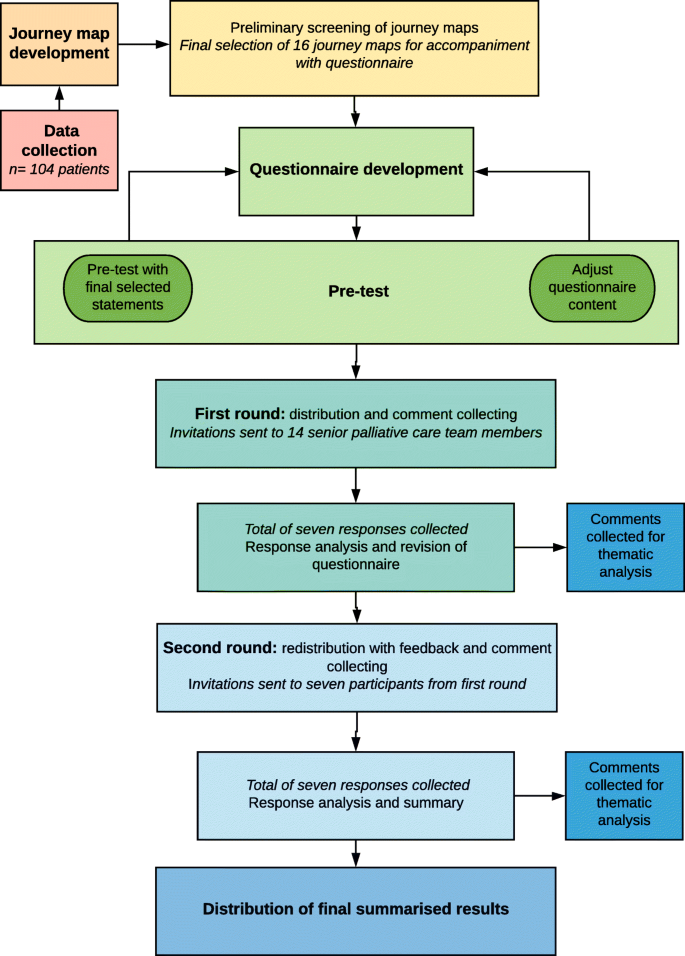
Flow chart detailing data collection, journey map development and analysis. This figure illustrates the phases and processes of this study. Data was collected from a retrospective cohort of 104 palliative care patients and journey maps were subsequently developed. Preliminary screening of the journey maps was performed to obtain a purposive sample that best highlighted the breadth of information and healthcare encounters captured within the journey maps. A total of 16 maps were selected for further analysis. Following questionnaire development and pre-test, questionnaires were distributed, and responses collected and analysed over two rounds to obtain consensus. Free-text comments from both rounds were collected for thematic analysis
All methods were carried out and reported in accordance with Standards for Reporting Qualitative Research (SRQR) guidelines and Consolidated criteria for Reporting Qualitative research (COREQ) criteria for reporting qualitative studies.
Ethics approval for this study was obtained from Monash Health Human Research Ethics Committee Monash Health Ref: RES-29-0000-071Q) and Monash University Human Research Ethics Committee (Project ID: 18,853).
Data was collected from a retrospective cohort of 104 consecutive palliative care patients from a major tertiary hospital network in Melbourne, Australia. Inclusion criteria were patients greater than 18 years of age who had died in hospital between the 1st of August 2018 and 31st of October 2018, had at least one inpatient palliative care admission in their last year of life and scanned medical records data spanning at least three months’ duration. This sample size was considered sufficient to incorporate a varied and representative sample of palliative care patients encountered in the tertiary hospital.
Following data collection, a Python Software-based code was designed to extract de-identified data and create journey map visuals. All 104 journey maps were independently screened by two investigators (PP and FR) and a purposive sample of 16 maps was selected for analysis based on seven criteria for informative value. The criteria that the 104 maps were assessed on included their ability to provide insight into the initiation, triggers, delivery and barriers of palliative care, SPICT scores, pivot points and disease trajectories.
Modified Delphi approach and thematic analysis
A qualitative mixed-methods approach involving thematic analysis and a modified Delphi technique was utilised as an explorative analysis of expert opinion. The consensus agreement was used to reinforce and confirm the patterns of significance identified through thematic analysis. In combining these two approaches, there was greater flexibility in responses and additional structure to support analysis.
The modified Delphi approach used in this study was adapted from the enhanced Delphi method described by Yang et al. [ 13 ] and consisted of a questionnaire pre-test and two rounds of questionnaire distribution. A total of 14 email invitations were sent to a purposive sample of seven senior palliative care physicians and seven palliative care nurse consultants across two palliative care inpatient units within a major tertiary hospital network in Melbourne, Australia. The emails contained an explanatory statement, a questionnaire link and the file containing the 16 de-identified journey maps.
The questionnaires consisted of 16 statements per journey map, covering eight palliative care domains: palliative care triggers, initiation, delivery, outcomes, barriers, pivot-points, needs assessment (using the Supportive and Palliative Care Indicators Tool, SPICT) and the utility of advanced care plans. An additional nine statements assessed the utility of the journey map approach (see Table 2 ). All statements were ranked using Likert scales. A four-point Likert scale including the options: insufficient information, disagree, neither agree nor disagree and agree was used to assess individual journey maps. A five-point Likert scale including options: strongly disagree, somewhat disagree, neither agree nor disagree, somewhat agree and strongly agree was used to assess the journey mapping approach. For analysis of consensus, the results were categorised to reflect overall agreement by using a three-point scale consisting of disagree, neutral and agree . Consensus was defined as agreement of greater than 70 % of respondents in any one of these three categories. Following the first round, all consensus statements were determined and participants were sent a second questionnaire containing anonymous feedback from the first round and statements which did not reach consensus for re-evaluation using the condensed three-point Likert scale.
Following each palliative care domain, free-text fields were included to collect comments and provide data for inductive thematic analysis. Analysis of the free-text comments from both rounds was guided by Braun and Clarke’s phases of thematic analysis [ 14 ]. The codes and themes were derived from the data using NVivo 12 Plus software to generate nodes, initial codes and preliminary subthemes. Candidate themes were reviewed by two additional investigators (PP and FR) to ensure consistency and the final themes were defined. Providing participants with the opportunity to review de-identified feedback through the Delphi questionnaire enabled discussion, reflection and clarification of comments, thus achieving thematic saturation with a smaller group of participants.
Additional steps were taken to increase trustworthiness of the qualitative data per Lincoln and Guba’s criteria for credibility, transferability, dependability and confirmability across all phases of analysis [ 15 , 16 , 17 ]. Triangulation of the methods, researchers and analysts aimed to increase consistency and accuracy, whilst reducing interpretation errors and the effects of bias. Thorough audit trails and reflexive journaling were maintained. The use of the online questionnaire with free-text fields for thematic data collection limited the role of the researcher and the potential for associated bias.
While this study also produced findings relevant to current issues of palliative care delivery, we will for the purpose of this paper, present results specific to the clinical utility of journey maps.
The journey maps
Figure 2 depicts one of the 16-sample journey maps analysed by participants and illustrates the key elements of a map. While journey maps are interactive visualisations with options for providing additional information summarising patient healthcare encounters, we are unable to fully convey the dynamic functions of the mapping tool in this paper. The journey map in Fig. 2 illustrates the final year of life of a 73 year old male patient with diffuse large B-cell lymphoma.
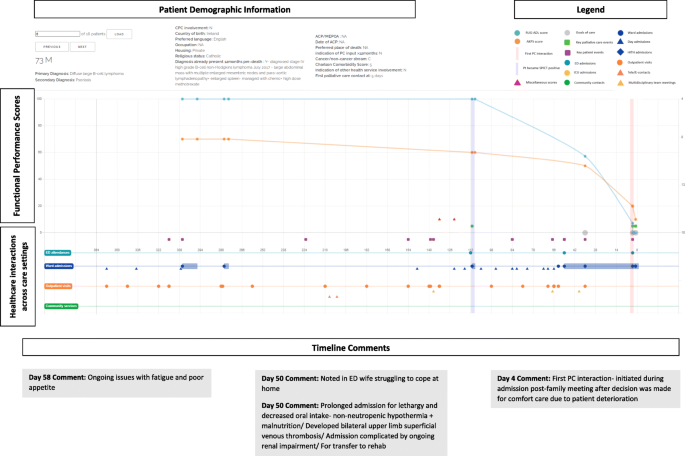
Screen capture of Journey Map 6. A screen capture of one of the 16 interactive journey maps that was analysed by the Delphi panel. The lower segment of the map depicts healthcare interactions that occurred in hospital and in the community. Delphi participants are able to hover over specific health service touch points to obtain more information about the specific interaction that occurred. The upper segment represents functional performance scores using two different tools- the Australian Karnofsky Performance Scale (AKPS) and the Resource Utilisation Groups-Activities of Daily Living (RUG-ADL). The orange vertical line indicates when palliative care needs first presented using the SPICT screening tool. The vertical purple line indicates when specialist palliative care was initiated. Delphi participants were able to analyse the maps and respond to statements on the palliative care provided
The map reveals that at day 112 prior to death, palliative care needs were noted using the SPICT screening tool. It is also at this point that the patient’s functional performance scores began to decline, with patient notes from day admissions and clinic visits also documenting poor tolerance of chemotherapy side effects, fatigue, anorexia and weight loss. In response to this pattern of decline, participants noted that there was an opportunistic role for community palliative care support that was missed and could have potentially negated the need for the final ED admission.
“Onc (sic)(oncology) outpatient notes describing symptoms, deterioration, carer distress… Community pall care (sic)(palliative care) could have been helpful” – Participant 2, Journey Map (JM) 6.
Another major pivot-point occurred during the patient’s admission to ED on day 50 when notes indicated that the patient’s wife was struggling to cope with care at home. Given the nature of the prolonged admission with multiple complications that followed, Delphi participants questioned the suitability of the transfer to the rehabilitation ward.
“Symptoms and functional decline appear to be related to lymphoma and not an acute illness. More appropriate for pall care (sic) than rehab (sic)(rehabilitation).” – Participant 6, JM6.
Additionally, the decision to initiate palliative care only four days prior to death was delayed and there was a role for earlier palliative care involvement.
“Clearly PC (sic)(palliative care) involvement inadequate and was a later referral for terminal care only” – Participant 1, JM6.
“Pt (sic)(patient) would have benefitted from earlier palliative care referral” – Participant 7, JM6.
Through the maps, participants were able to observe patterns of deterioration with a broader view of continuity of care and determine pivot-points, where the involvement of specialist palliative care had the potential to improve the patient experience.
Modified Delphi
The two Delphi rounds were conducted over 31 days with the first round taking 13 days and the second round spanning 18 days. A total of seven responses were collected from the first round of the online Delphi questionnaire. Six members of the medical staff and one member of the nursing team responded, representing a 50 % response rate. All seven participants completed the questionnaire in full. For the second round, all first round participants were re-contacted and invited to participate. All seven participants from the first round agreed to participate, attributing to a 100 % second round response rate and 100 % questionnaire completion rate. Participant characteristics have been described in Table 1 . All participants are senior palliative care team members.
The statements assessing journey map utility are shown in Table 2 . As there was a strong overall consensus following the first round of the Delphi questionnaire, these statements were not rechallenged in a second round. However free-text fields were included to allow participants to provide any further comments.
Thematic analysis
Following analysis of all free-text comments, the following themes were derived regarding the applications of the journey mapping tool: (1) design and information, (2) longitudinal care and the patient trajectory and (3) opportunities for care improvement. These are discussed with supporting quotations listed in Table 3 .
Theme 1: tool design and information
A large determinant of the practicality of the tool relates to its design. Participants provided feedback regarding the design and informational elements of the journey mapping tool used in this study.
Aspects of the interface
Participants found that there were certain elements of the journey maps that limited functionality of the tool, however these were associated with the specific design of the tool interface, rather than the actual components underlying the journey mapping approach. Participants responded well to the concept of a visual representation of patient information and the timeline view of care that was constructed.
Catering information needs
Given the palliative care specific focus on patient care presented in these maps, participants found that at times there was an excess of unnecessary information and insufficient palliative care appropriate information. The absence of objective measures of quality of life also restricted the ability of participants to determine whether outcomes were improved as a result of interventions.
Theme 2: Longitudinal care and the patient trajectory
The benefits of conveying patient information and healthcare encounters in the form of journey maps were also recognised. Journey maps provided a patient-centred focus of care that characterises patient healthcare interactions within a longitudinal trajectory rather than individual care episodes as is standard in conventional medical records. In doing so, patterns of the disease trajectory and also patient decline can be mapped to provide more proactive patient care.
Theme 3: Opportunities for care improvement
The benefits of having the journey mapping tool and its utility if incorporated into patient care were also explored, with participants noting numerous possible applications and opportunities to improve patient care.
Identifying barriers and missed opportunities for care
By framing the patient healthcare experience as a longitudinal and continuous journey, participants were able to recognise missed opportunities to address barriers and initiate more timely palliative care.
Clinical applications
Participants also noted that journey maps were a useful tool for identifying gaps in care provision and underlying barriers to initiation and delivery. This could assist clinicians with recognition of pivot-points and opportunities to enhance care by pre-emptively managing issues. Additionally, journey maps presented possible applications as a review or screening tool to evaluate patient care needs and enable better patient-centred care practices both in the clinical and research setting.
Findings from both the modified Delphi and thematic analysis appeared congruent, with the consensus consistent with emerging themes.
Journey mapping is a novel approach to reviewing patient healthcare interactions over time and across care settings to identify potential pivot points, which in turn can facilitate timely healthcare and promote proactive delivery of patient-centred care. Our research has focused on palliative care as the model to explore this approach, especially given its importance in an ageing population and considering many aspects of care are ubiquitous to this cohort.
Variation and inconsistencies in palliative care initiation and delivery have limited the applicability and role of research in informing evidence-based practice [ 6 ]. A journey map approach may provide one solution to address these challenges. The journey mapping tool used in this study was found to enable a patient-centred focus to the clinician’s perspective, increasing opportunities to pro-actively identify pivot-points and deliver more effective patient care.
In comparison to conventional medical records, journey maps link patient healthcare encounters longitudinally, promoting continuity and a holistic understanding of care across settings and over time. As described in conceptual studies, journey maps offer a perspective that takes into account the more dynamic and multidimensional aspects of healthcare interactions to facilitate enhanced insight into the patient experience within medical research [ 10 , 18 ]. This enables a more integrated interpretation and awareness of individual episodes of care and how these contribute to a patient’s overall health and their interaction with health services. Our participants also noted that journey mapping enabled greater emphasis on particular patient outcomes that may be difficult to observe or measure using conventional research methods. The journey mapping tool was also able to highlight gaps in care and facilitate recognition of patterns of disease progression and deterioration with a greater emphasis on patient needs and experiences.
The use of the journey mapping approach has further enabled identification of barriers and potential biases to providing effective care. This study confirms that journey mapping as a tool is effective at identifying specific barriers and trends in care provision and increase opportunities for care providers to pro-actively and appropriately address these.
Journey maps have traditionally been used in research to review and analyse the consumer experience and provide feedback on avenues for development [ 7 ]. Our panel consensus affirmed that journey mapping had applications as a clinical audit tool to identify gaps in care and opportunities for improvement when used to assess retrospective patient experiences. This is consistent with known utilities of previous journey mapping tools. Other identified benefits included potential to achieve better collaboration between healthcare providers, enabling smoother transitions of care and improving communication between healthcare providers and patients.
Limitations of this study include the design and interface of the journey mapping tool. Following a thorough search, pre-existing journey mapping software and tools were considered inappropriate for this study as they were oversimplified, unable to convey complex information appropriately and not designed for use in a medical setting. Consequently, self-designing a tool was considered the most suitable approach. The technical limitations identified did not reflect the utility of the journey mapping paradigm.
The retrospective nature of this study prohibits direct patient feedback. Consequently, the patient and caregiver perspective, including quality of life and symptom burden experienced were not well represented. Future research utilising a prospective approach with patient and caregiver involvement is needed to address these research gaps.
The response rate to the initial Delphi questionnaire was only 50 % due to time constraints and limited ability to accommodate delayed responses, however the response rate to the second Delphi questionnaire was 100 %. While this does limit the diversity of responses, it suggests good retention and engagement of involved participants with meaningful contributions.
The size of the Delphi panel in this study was seven. Studies have noted that smaller panels are still able to provide effective and reliable results and a minimum panel size of seven is considered suitable in most cases [ 19 , 20 ]. Our modified approach complied with this. Despite being a single institution study, the participants come from a diverse clinical background covering multiple domains of specialty palliative care, henceforth reducing potential bias. This study demonstrates that there is a role for journey mapping in clinical practice, however, considerations must be made for future design. Given the volume of patient data available, the amount of information presented needs to be appropriately moderated to provide clarity and best utilisation of the resources available. With the gradual transition of most health services from paper medical records to electronic medical records, the inclusion of a journey mapping tool into clinical practice is becoming more feasible. As medical technology continues to grow, the potential for incorporation of artificial intelligence, machine learning and big data into journey maps could be the key to providing pro-active, holistic patient-centred care that pre-emptively anticipates patient needs.
This study is one of the first to use a journey mapping tool in clinical practice to explore the healthcare journey and patient experience on a larger scale. The maps were used to depict a more fluid and continuous interpretation of the patient healthcare experience which enabled a more holistic and patient-centred analysis of palliative care provision. Furthermore, this is one of the first medical journey mapping studies to consider and propose potential pivot-points and opportunities for changes in the delivery of care. The use of journey maps can enhance the holistic patient healthcare experience and enable better patient-centred care not only in the palliative care setting, but also more broadly across healthcare from both a research and clinical practice perspective. Further application studies in other contexts are required.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due to the confidential nature of the patient data, but are available from the corresponding author on reasonable request.
Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010;363(8):733–42.
Article CAS Google Scholar
Bakitas MA, Tosteson TD, Li Z, et al. Early versus delayed initiation of concurrent palliative oncology care: patient outcomes in the ENABLE III randomized controlled trial. J Clin Oncol. 2015;33(13):1438–45.
Article Google Scholar
King JD, Eickhoff J, Traynor A, Campbell TC. Integrated onco-palliative care associated with prolonged survival compared to standard care for patients with advanced lung cancer: a retrospective review. J Pain Symptom Manage. 2016;51(6):1027–32.
Hawley P. Barriers to access to palliative care. Palliative Care. 2017;10:1178224216688887.
PubMed PubMed Central Google Scholar
Rodriguez KL, Barnato AE, Arnold RM. Perceptions and utilization of palliative care services in acute care hospitals. J Palliat Med. 2007;10(1):99–110.
Evans CJ, Harding R, Higginson IJ. Morecare. ‘Best practice’ in developing and evaluating palliative and end-of-life care services: a meta-synthesis of research methods for the MORECare project. Palliat Med. 2013;27(10):885–98.
Gibbons S. Journey Mapping 101. 2018; https://www.nngroup.com/articles/journey-mapping-101/ .
Crunkilton DD. Staff and client perspectives on the Journey Mapping online evaluation tool in a drug court program. Eval Program Plan. 2009;32(2):119–28.
Westbrook JI, Coiera EW, Sophie Gosling A, Braithwaite J. Critical incidents and journey mapping as techniques to evaluate the impact of online evidence retrieval systems on health care delivery and patient outcomes. Int J Med Inform. 2007;76(2–3):234–45.
McCarthy S, O’Raghallaigh P, Woodworth S, Lim YL, Kenny LC, Adam F. An integrated patient journey mapping tool for embedding quality in healthcare service reform. J Decision Syst. 2016;25(sup1):354–68.
Hide E, Pickles J, Maher L. Experience based design: a practical method of working with patients to redesign services. Clin Gov. 2008;13(1):51–8.
Trebble TM, Hansi N, Hydes T, Smith MA, Baker M. Process mapping the patient journey: an introduction. BMJ. 2010;341:c4078.
Yang T-H. Case study: application of enhanced Delphi method for software development and evaluation in medical institutes. Kybernetes. 2016;45(4):637–49.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis: striving to meet the trustworthiness criteria. Int J Qual Methods. 2017;16(1):1609406917733847.
Lincoln YS, Guba EG. Naturalistic Inquiry. Newbury Park: Sage Publications; 1985.
Book Google Scholar
Cohen D, Crabtree B. Qualitative Research Guidelines Project. 2006; http://www.qualres.org/HomeRefl-3703.html .
Ben-Tovim DI, Dougherty ML, O’Connell TJ, McGrath KM. Patient journeys: the process of clinical redesign. Med J Aust. 2008;188(S6):S14–7.
PubMed Google Scholar
Linstone H. The Delphi technique. Handbook of Futures Research. Westport: Greenwood; 1978.
Google Scholar
Akins RB, Tolson H, Cole BR. Stability of response characteristics of a Delphi panel: application of bootstrap data expansion. BMC Med Res Methodol. 2005;5:37–37.
Download references
Acknowledgements
We would like to acknowledge and extend our thanks to Kevin Shi who contributed to the Python code used for the journey map visuals.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
Faculty of Medicine Nursing and Health Sciences, Monash University, Clayton, VIC, Australia
Stephanie Ly, Fiona Runacres & Peter Poon
Supportive & Palliative Care Department, McCulloch House, Monash Medical Centre, 246 Clayton Road, VIC, 3168, Clayton, Australia
Fiona Runacres & Peter Poon
Calvary Health Care Bethlehem, Parkdale, VIC, Australia
Fiona Runacres
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualisation PP. Methodology: PP, FR, SL. Formal analysis PP, FR, SL. Investigation: PP, FR, SL. Writing –original draft: SL. Writing- Review and Editing: PP, FR. Supervision : PP, FR. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Peter Poon .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval for this study was obtained from Monash Health Human Research Ethics Committee Monash Health Ref: RES-29-0000-071Q) and Monash University Human Research Ethics Committee (Project ID: 18853). Informed consent from patients was not required as this was a retrospective audit of pre-existing available data which was de-identified prior to analysis. All participants of the Delphi questionnaire were provided with an explanatory statement and by completing and returning the questionnaires, consent was implied.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ly, S., Runacres, F. & Poon, P. Journey mapping as a novel approach to healthcare: a qualitative mixed methods study in palliative care. BMC Health Serv Res 21 , 915 (2021). https://doi.org/10.1186/s12913-021-06934-y
Download citation
Received : 10 April 2021
Accepted : 24 August 2021
Published : 04 September 2021
DOI : https://doi.org/10.1186/s12913-021-06934-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Patient journey mapping
- Health services research
- Palliative care
- Illness trajectory
- Proactive healthcare
- Medical informatics
- Patient-centred care
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Breast cancer patient experiences through a journey map: A qualitative study
Roles Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Clinical Psychology and Psychobiology Department, Faculty of Psychology, University of Barcelona, Barcelona, Spain
Roles Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing
Affiliation Medical Oncology Department Hospital Universitario Central of Asturias, Oviedo, Spain
Roles Resources, Validation, Writing – review & editing
Affiliation Social Psychology and Quantitative Psychology Department, Faculty of Psychology, University of Barcelona, Barcelona, Spain
Affiliation Medical Oncology Department, Hospital Universitario Clínico San Carlos, Madrid, Spain
Affiliation Medical Oncology Department, Complexo Hospitalario Universitario de Ourense, Ourense, Spain
Affiliation Medical Oncology Department, Hospital Universitario La Paz, Madrid, Spain
Affiliation Medical Oncology Department, Hospital General Universitario de Elche, Elche, Spain
Affiliation Medical Oncology Department, Hospital Universitario Fundación Alcorcón, Madrid, Spain
Roles Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing
- Laura Ciria-Suarez,
- Paula Jiménez-Fonseca,
- María Palacín-Lois,
- Mónica Antoñanzas-Basa,
- Ana Fernández-Montes,
- Aranzazu Manzano-Fernández,
- Beatriz Castelo,
- Elena Asensio-Martínez,
- Susana Hernando-Polo,
- Caterina Calderon

- Published: September 22, 2021
- https://doi.org/10.1371/journal.pone.0257680
- Reader Comments
Registered Report Protocol
21 Dec 2020: Ciria-Suarez L, Jiménez-Fonseca P, Palacín-Lois M, Antoñanzas-Basa M, Férnández-Montes A, et al. (2020) Ascertaining breast cancer patient experiences through a journey map: A qualitative study protocol. PLOS ONE 15(12): e0244355. https://doi.org/10.1371/journal.pone.0244355 View registered report protocol
Breast cancer is one of the most prevalent diseases in women. Prevention and treatments have lowered mortality; nevertheless, the impact of the diagnosis and treatment continue to impact all aspects of patients’ lives (physical, emotional, cognitive, social, and spiritual).
This study seeks to explore the experiences of the different stages women with breast cancer go through by means of a patient journey.
This is a qualitative study in which 21 women with breast cancer or survivors were interviewed. Participants were recruited at 9 large hospitals in Spain and intentional sampling methods were applied. Data were collected using a semi-structured interview that was elaborated with the help of medical oncologists, nurses, and psycho-oncologists. Data were processed by adopting a thematic analysis approach.
The diagnosis and treatment of breast cancer entails a radical change in patients’ day-to-day that linger in the mid-term. Seven stages have been defined that correspond to the different medical processes: diagnosis/unmasking stage, surgery/cleaning out, chemotherapy/loss of identity, radiotherapy/transition to normality, follow-up care/the “new” day-to-day, relapse/starting over, and metastatic/time-limited chronic breast cancer. The most relevant aspects of each are highlighted, as are the various cross-sectional aspects that manifest throughout the entire patient journey.
Conclusions
Comprehending patients’ experiences in depth facilitates the detection of situations of risk and helps to identify key moments when more precise information should be offered. Similarly, preparing the women for the process they must confront and for the sequelae of medical treatments would contribute to decreasing their uncertainty and concern, and to improving their quality-of-life.
Citation: Ciria-Suarez L, Jiménez-Fonseca P, Palacín-Lois M, Antoñanzas-Basa M, Fernández-Montes A, Manzano-Fernández A, et al. (2021) Breast cancer patient experiences through a journey map: A qualitative study. PLoS ONE 16(9): e0257680. https://doi.org/10.1371/journal.pone.0257680
Editor: Erin J. A. Bowles, Kaiser Permanente Washington, UNITED STATES
Received: February 17, 2021; Accepted: September 3, 2021; Published: September 22, 2021
Copyright: © 2021 Ciria-Suarez et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: Relevant anonymized data excerpts from the transcripts are in the main body of the manuscript. They are supported by the supplementary documentation at 10.1371/journal.pone.0244355 .
Funding: This work was funded by the Spanish Society of Medical Oncology (SEOM) in 2018. The sponsor of this research has not participated in the design of research, in writing the report, or in the decision to submit the article for publication.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Breast cancer is the most common cancer and the one that associates the highest mortality rates among Spanish women, with 32,953 new cases estimated to be diagnosed in Spain in 2020 [ 1 ]. Thanks to early diagnosis and therapeutic advances, survival has increased in recent years [ 2 ]. The 5-year survival rate is currently around 85% [ 3 , 4 ].
Though high, this survival rate is achieved at the expense of multiple treatment modalities, such as surgery, chemotherapy, radiotherapy, and hormone therapy, the side effects and sequelae of which can interfere with quality-of-life [ 5 ]. Added to this is the uncertainty surrounding prognosis; likewise, life or existential crises are not uncommon, requiring great effort to adjust and adapt [ 6 ]. This will not only affect the patient psychologically, but will also impact their ability to tolerate treatment and their socio-affective relations [ 7 ].
Several medical tests are performed (ultrasound, mammography, biopsy, CT, etc.) to determine tumor characteristics and extension, and establish prognosis [ 8 ]. Once diagnosed, numerous treatment options exist. Surgery is the treatment of choice for non-advanced breast cancer; chemotherapy, radiotherapy, and hormone therapy are adjuvant treatments with consolidated benefit in diminishing the risk of relapse and improving long-term survival [ 9 ]. Breast cancer treatments prompt changes in a person’s physical appearance, sexuality, and fertility that interfere with their identity, attractiveness, self-esteem, social relationships, and sexual functioning [ 10 ]. Patients also report more fatigue and sleep disturbances [ 11 ]. Treatment side effects, together with prognostic uncertainty cause the woman to suffer negative experiences, such as stress in significant relationships, and emotions, like anxiety, sadness, guilt, and/or fear of death with negative consequences on breast cancer patients’ quality-of-life [ 10 , 12 ]. Once treatment is completed, patients need time to recover their activity, as they report decreased bodily and mental function [ 13 ], fear of relapse [ 14 ], and changes in employment status [ 15 ]. After a time, there is a risk of recurrence influenced by prognostic factors, such as nodal involvement, size, histological grade, hormone receptor status, and treatment of the primary tumor [ 16 ]. Thirty percent (30%) of patients with early breast cancer eventually go on to develop metastases [ 17 ]. There is currently no curative treatment for patients with metastatic breast cancer; consequently, the main objectives are to prolong survival, enhance or maintain quality-of-life, and control symptoms [ 17 , 18 ]. In metastatic stages, women and their families are not only living with uncertainty about the future, the threat of death, and burden of treatment, but also dealing with the existential, social, emotional, and psychological difficulties their situation entails [ 18 , 19 ].
Supporting and accompanying breast cancer patients throughout this process requires a deep understanding of their experiences. To describe the patient’s experiences, including thoughts, emotions, feelings, worries, and concerns, the phrase “patient voice” has been used, which is becoming increasingly common in healthcare [ 20 ]. Insight into this “voice” allows us to delve deeper into the physical, emotional, cognitive, social, and spiritual effects of the patient’s life. This narrative can be portrayed as a “cancer journey", an experiential map of patients’ passage through the different stages of the disease [ 21 ] that captures the path from prevention to early diagnosis, acute care, remission, rehabilitation, possible recurrence, and terminal stages when the disease is incurable and progresses [ 22 ]. The term ‘patient journey’ has been used extensively in the literature [ 23 – 25 ] and is often synonymous with ‘patient pathway’ [ 26 ]. Richter et al. [ 26 ] state that there is no common definition, albeit in some instances the ‘patient journey’ comprises the core concept of the care pathway with greater focus on the individual and their perspective (needs and preferences) and including mechanisms of engagement and empowerment.
While the patient’s role in the course of the disease and in medical decision making is gaining interest, little research has focused on patient experiences [ 27 , 28 ]. Patient-centered care is an essential component of quality care that seeks to improve responsiveness to patients’ needs, values, and predilections and to enhance psychosocial outcomes, such as anxiety, depression, unmet support needs, and quality of life [ 29 ]. Qualitative studies are becoming more and more germane to grasp specific aspects of breast cancer, such as communication [ 27 , 30 ], body image and sexuality [ 31 , 32 ], motherhood [ 33 ], social support [ 34 ], survivors’ reintegration into daily life [ 13 , 15 ], or care for women with incurable, progressive cancer [ 17 ]. Nevertheless, few published studies address the experience of women with breast cancer from diagnosis to follow-up. These include a clinical pathway approach in the United Kingdom in the early 21st century [ 35 ], a breast cancer patient journey in Singapore [ 25 ], a netnography of breast cancer patients in a French specialized forum [ 28 ], a meta-synthesis of Australian women living with breast cancer [ 36 ], and a systematic review blending qualitative studies of the narratives of breast cancer patients from 30 countries [ 37 ]. Sanson-Fisher et al. [ 29 ] concluded that previously published studies had examined limited segments of patients’ experiences of cancer care and emphasized the importance of focusing more on their experiences across multiple components and throughout the continuum of care. Therefore, the aim of this study is to depict the experiences of Spanish breast cancer patients in their journey through all stages of the disease. To the best of our knowledge, there are no studies that examine the experience of women with breast cancer in Spain from diagnosis through treatment to follow-up of survivors and those who suffer a relapse or incurable disease presented as a journey map.
A map of the breast cancer patient’s journey will enable healthcare professionals to learn first-hand about their patients’ personal experiences and needs at each stage of the disease, improve communication and doctor-patient rapport, thereby creating a better, more person-centered environment. Importantly, understanding the transitional phases and having a holistic perspective will allow for a more holistic view of the person. Furthermore, information about the journey can aid in shifting the focus of health care toward those activities most valued by the patient [ 38 ]. This is a valuable and efficient contribution to the relationship between the system, medical team, and patients, as well as to providing resources dedicated to the patient’s needs at any given time, thus improving their quality of life and involving them in all decisions.
Study design and data collection
We conducted a qualitative study to explore the pathway of standard care for women with breast cancer and to develop a schematic map of their journey based on their experiences. A detailed description of the methodology is reported in the published protocol “Ascertaining breast cancer patient experiences through a journey map: A qualitative study protocol” [ 39 ].
An interview guide was created based on breast cancer literature and adapted with the collaboration of two medical oncologists, three nurses (an oncology nurse from the day hospital, a case manager nurse who liaises with the different services and is the ‘named’ point of contact for breast cancer patients for their journey throughout their treatment, and a nurse in charge of explaining postoperative care and treatment), and two psycho-oncologists. The interview covered four main areas. First, sociodemographic and medical information. Second, daily activities, family, and support network. Third, participants were asked about their overall perception of breast cancer and their coping mechanisms. Finally, physical, emotional, cognitive, spiritual, and medical aspects related to diagnosis, treatment, and side effects were probed. Additionally, patients were encouraged to express their thoughts should they want to expand on the subject.
The study was carried out at nine large hospitals located in six geographical areas of Spain. To evaluate the interview process, a pilot test was performed. Interviews were conducted using the interview guide by the principal investigator who had previous experience in qualitative research. Due to the Covid-19 pandemic, all interviews were completed online and video recorded with the consent of the study participants for subsequent transcription. Relevant notes were taken during the interview to document key issues and observations.
Participant selection and recruitment
Inclusion criteria were being female, over 18 years of age, having a diagnosis of histologically-confirmed adenocarcinoma of the breast, and good mental status. To ascertain the reality of women with breast cancer, most of the patients recruited (80%) had been diagnosed in the past 5 years. Patients (20%) were added who had been diagnosed more than 5 years earlier, with the aim of improving the perspective and ascertaining their experience after 5 years.
Medical oncologists and nurses working at the centers helped identify patients who met the inclusion criteria. Participants went to the sites for follow-up between December 2019 and January 2021. Eligible women were informed of the study and invited to participate during an in-person visit by these healthcare professionals. Those who showed interest gave permission to share their contact information (e-mail or telephone number) with the principal investigator, who was the person who conducted all interviews. The principal investigator contacted these women, giving them a more detailed explanation of the study and clarifying any doubts they may have. If the woman agreed to participate, an appointment was made for a videoconference.
A total of 21 women agreed to participate voluntarily in this research. With the objective of accessing several experiences and bolstering the transferability of the findings, selection was controlled with respect to subjects’ stage of cancer, guaranteeing that there would be a proportional number of women with cancer in all stages, as well as with relapses.
Data analysis
The data underwent qualitative content analysis. To assure trustworthiness, analyses were based on the system put forth by Graneheim, and Lundman [ 40 ]. Interviews were transcribed and divided into different content areas; units of meaning were obtained and introduced into each content area; meaning codes were extracted and added; codes were categorized in terms of differences and similarities, and themes were created to link underlying meanings in the categories. All members of the research team (core team, two medical oncologists, three nurses and two psycho-oncologists) reviewed the data and triangulated the outcomes between two sources of data: qualitative data from the interview and non-modifiable information, such as sociodemographic (i.e., age, marital status, having children) and clinical (i.e., cancer stage and surgery type) data. Following this process, we reached saturation of the interview data by the time we had completed 21 interviews.
Ethical considerations
This study was performed in accordance with the ethical standards of the Declaration of Helsinki, and its subsequent amendments. The study was approved by the Research Ethics Committee of University of Barcelona (Institutional Review Board: IRB00003099) and supported by the Bioethics Group of the Spanish Society of Medical Oncology (SEOM) 2018 grant. All participants received a written informed consent form that they signed prior to commencing with the interviews and after receiving information about the study.
Patient baseline characteristics
In total, 21 women with a mean age of 47 years (range, 34 to 61) were interviewed. Most of the study population was married (66.7%), had a college education (66.7%), and had 2 or more children (42.9%). All cancer stages were represented, up to 23.8% tumor recurrence, and most of the primary cancers had been resected (95.2%) (see Table 1 ).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0257680.t001
Description of the breast cancer patient journey
The women diagnosed with breast cancer describe the journey as a process tremendously affected by the different medical stages. Each stage has its own characteristics that condition the experiences, unleashing specific physical, emotional, cognitive, and social processes. Additionally, the patients perceive this entire process as pre-established journey they must undertake to save their life, with its protocols based on the type and stage of cancer.
“ People said to me , ‘What do you think ? ’ and I answered that there was nothing for me to think about because everything is done , I have to go on the journey and follow it and wait to see how it goes” (Patient 6)
Fig 1 displays the various phases of the journey that patients with breast cancer go through; nevertheless, each woman will go through some or others, depending on their type of cancer.
https://doi.org/10.1371/journal.pone.0257680.g001
Throughout the entire patient journey.
Processes of loss and reinterpretation of the new circumstance . What stands out the most in the process these women go through during the diagnosis and treatment of breast cancer is loss; specifically, the loss of health and a reinterpretation of the new circumstance and the new bodily reality. In the most extreme cases, the loss of health emerges with the fear of death that many women report at the time of diagnosis or during treatment, due to the distress generated. The loss of identity seems to be related to the evolutionary (existential) moment in which the woman is; there are patients who report feelings of disability or loss of attractiveness, or fear of not being able to get pregnant in the future, especially the youngest.
I felt a terrifying fear and thought , “You have cancer you tell yourself , you’re going to die tomorrow .” (Patient 6) I feel like after the hysterectomy , as a woman , I no longer have anything , only the physical . Sure , I look great , but I tell myself that it’s just a shell , the shell I inhabit , because as a woman , I only have one breast left . (Patient 6) At that moment , I had to make the decision that I was no longer going to be a mother . (Patient 14)
Personal change . Most of the women report that with the diagnosis of breast cancer, their life stands still and from that point forward, a different journey begins. The sole focus on this journey is the disease and its implications. During all those months, the patients stop working; they focus on their medical treatments, and reflect a lot on their current situation and on life. Most of the participants state, especially those who have already been discharged, that they know themselves better now; they take better care of themselves, and they enjoy their day-to-day and the small moments more, making the most of their time, with more initiatives and fewer trivial complaints.
Clearly , you’re not the same person you were before; I don’t think she’ll ever come back; your mindset changes completely and I have sequelae from all the treatments . (Patient 1) I re-think wasting energy on lost causes; what’s more , I’ve also learnt to say no . If I’m not in the mood to go somewhere , I just say no . (Patient 7) I take much more advantage of the present now , because you realize that things can change on any given day . (Patient 3)
Trust and appreciation for their physician . Most of the interviewees stated that they fully trusted the doctors who care for them, without question or objection to the treatments proposed. They reported that, as they go forward, they discuss the tests and treatments that are going to be performed, as well as possible side effects. Several stated that they are unaware of the stage of their cancer; similarly, most also do not know the benefits expressed in X% of the treatments. A few of the participants claimed that they did talk in detail about the different types of treatments with their oncologists, that they had sought another opinion, and one of them even reported having decided to stop chemotherapy, which was very hard for her, given her physician’s insistence that she continue.
The truth is that the oncologist didn’t say much about percentages; what she told me were the steps that I had to take; I thoroughly trusted her and she gave me a lot of peace of mind . (Patient 5) I told him , “I’m going to do whatever you tell me to . ” It never occurred to me to dispute whatever the oncologist might tell me . I was willing to do whatever was needed . (Patient 8)
Most of the women, at some point during the interview, state that they are grateful for the care they received and that, within the seriousness of their situation, there is a treatment for their condition.
I am super grateful for the treatment I’ve received and with the doctors assigned to me . (Patient 2) I’m very lucky; I’m only on my second line of treatment for metastasis and I’ve got a lot more ahead of me , but I consider myself lucky and I believe things are going very well . (Patient 20)
Role of the woman . We can see that the women adopt a role of care-givers and managers of their surroundings. They worry about the disease negatively affecting the people around them, which is why they make an effort to manage the family’s activity for when they can’t do it and they try to avoid being a physical burden or cause emotional distress to the people around them.
I was very strong ; I made everything easy for people , but making it very easy , doesn’t mean that it was easy for me , but that I made it easy for everyone . (Patient 8) I didn’t want to worry anyone because that’s just the way I am , I push forward and that’s that . (Patient 5)
Support network . In all cases, the family appears to be one of the elements that is most involved in the disease process. Within the family, the partner deserves special mention. The testimonies in this regard reveal a wide spectrum of possibilities that range from the feeling of having had great support to a lack of attention and understanding that, in many situations, causes the relationship to be strained or to end. Friends tend to appear more occasionally.
I can’t complain about my husband; he was up to the challenge , very attentive toward me and he fully understood how I was feeling ; I felt very supported . (Patient 14) We’ve had a period of a lot of arguing; I’ve had to sit down with him and tell him that life had changed for me . (Patient 18) I had a partner I had lived with for five and a half years and he told me , literally , that he looked at me like a little sister , no longer as a woman , and he left me , and that hurt me tremendously . (Patient 6)
On the other hand, many patients commented on the importance of social media, where they have met people in the same situation as them. They report feeling understood and in good company; likewise, they commented on the importance of being able to share their doubts and get to know about other experiences.
It’s a situation that only someone who has gone through can understand; you can have all the good intentions in the world , but if you haven’t gone through it , you can’t even begin to understand . (Patient 8)
Use of complementary treatments . Most patients follow conventional medical treatment. However, many resort to other disciplines that help them improve their quality-of-life, like dietary changes, getting more exercise than usual, visits to a psychologist or physical therapist, or using other integrative therapies, such as acupuncture, yoga, reiki, flowers of Bach, homeopathy, cannabis, or meditation.
I started to read a whole bunch of books to see what I could do to take care of myself in terms of nutrition and exercise ; you consider everything you can do . (Patient 5)
Diagnosis/unmasking.
This phase encompasses the time from when the woman detects some symptom or goes to a check-up until the medical diagnosis is made. For the woman, this is a time of a series of tests and results. We have observed that the procedures, especially the healthcare professionals that deal with the patients, and the timing vary, depending on the medical center where they are being cared for. Emotionally, this is one of the most complicated stages.
Emotional whirlwind . The wait to obtain test results has a huge emotional impact for the women, given that it is a time of great uncertainty and fear.
An entire month with all the anguish of finding out if you have something . (Patient 3) The worst part is waiting 15 days to find out the magnitude of the tragedy , if it’s throughout your entire body or only in your breast; you go through a brutal emotional whirlwind; the wait is horrible because there’s nothing else you can do , so that anguish that you carry inside is dreadful; it was hell for me . (Patient 10)
Additionally, the interviewees described many other emotions that included fear of death, fear of having no time, feeling of unreality, rage, anger, sadness, avoidance, denial…
The first thing I thought was that I was going to die and that I wouldn’t finish watching my children [grow up]; my father had died of lung cancer 25 years ago . (Patient 9) My only aim was to get back to normal , as if there were nothing wrong . (Patient 4) You have a lot of conflicting feelings; you wish this weren’t happening; you want to run away , but you say , “Where am I going to run to ? ” . (Patient 14)
Impact of medical communication . Several women comment that, when given the diagnosis, they dissociate because of the emotional impact and that they don’t listen to all the information that the medical professional is giving them.
I remember that she talked and talked , but I didn’t know what she was saying until she said , “Isabel , you’re going to be cured , okay ?”. (Patient 9)
During the diagnostic testing, the women are highly sensitive to the healthcare professionals’ words and gestures.
I looked at the face of the person who was doing the mammogram and that’s when I started to imagine the worst . (Patient 20) I say to them , “ But , is there a solution to this ? ” , and they say to me , “Don’t worry , I’m sure there is a solution . ” That “sure” is etched in my mind . (Patient 10)
Communication and managing their surroundings . After the diagnosis, the patients feel that they have to tell the people around them about their situation, especially those closest to them, the family. They all agree on how hard it is to share. Normally, the people it’s hardest to tell are their mother and their children. When they do, they try to put the most positive spin on it possible, in an attempt to keep them from worrying.
You no longer think only about yourself , you think , “Good grief , now I’ve got to tell my mother .” It’s hard . (Patient 16) I wanted to tell my kids the way I say things , always trying to look for the upside , and positive , although it was hard , but , anyway , in the end , it went well . When I finished , my husband told me , “You’ve convinced me that it’s no big deal .” (Patient 9) I told my son , “Son , don’t cry , your mom’s going to get over this , this is nothing .” (Patient 1)
During this period, the women contemplate how their situation will affect their surroundings and they try to organize it as much as possible.
I devoted myself to planning everything , to organizing what to do with my daughter , and to thinking about work , too , how I had left things at work . (Patient 4)
Surgery/cleaning out the cancer.
Uncertainty and fear . The participants express that before going into surgery, they are told about the kind of procedure that will be done, but that, depending on what they find and the analysis, it may change. In light of this, they exhibit an enormous feeling of uncertainty and fear. In addition, many voice concern about how the surgery will go.
They tell you conservative surgery , but if we open up and see something we didn’t see on the tests , then everything could change . (Patient 10) Aside from the anesthesia , that I’m terrified of , you spend several hours in surgery and you don’t really know how things will go; when they clean it out , they analyze it , and you go into the operating room and you don’t know what can happen . (Patient 9)
Feeling of loss . Considering that the breast is associated with an intimate, feminine part [of their body], many women experience the operation as a loss. This loss is more acute if the operation is a mastectomy and there is no reconstruction at the same time. The loss also involves a loss of identity, compounded by the side effects of chemotherapy, such as hair loss. The interviewees who had undergone mastectomy say that following surgery, when the bandaging is removed and the scar is revealed, is one of the most critical moments, which is why they express difficulty in managing it and appreciate the caring assistance from the professionals.
It is identification with yourself , you know , it’s what you’ve seen in the mirror , what you think you’re like and , suddenly , you’re no longer like that; there’s an incredible personal crisis because you no longer recognize what you’re seeing . (Patient 11) I closed my eyes and I removed the bandaging and I didn’t dare look … with my eyes , I imagined the worst . (Patient 12)
Acceptance or demand for more aggressive intervention . The patients perceive the surgery as essential to recovering their health, which is why the process is widely accepted. Some patients who demand a more invasive intervention, normally a bilateral mastectomy, do so because that way, they feel safer with respect to a possible relapse, as well as more comfortable esthetically.
If they have to remove my breast , let them take it; what I want is to get better . (Patient 16) They say that I am in full remission , so they only removed the lump , but at first , I said that I wanted my whole [breast] removed ; then they assessed how to do it . (Patient 13) They told me that I had a genetic mutation and more possibilities of developing breast cancer and , since I felt such rejection toward my remaining breast , I decided to get rid of that one , too . (Patient 20)
Chemotherapy/loss of identity.
The chemotherapy phase is one of the phases that affects the women’s lives the most, because of its physical impact and how long it lasts. No differences have been found in how they experience chemotherapy depending on whether it was neoadjuvant or adjuvant.
Negative impact of side effects . Chemotherapy is associated with many side effects that vary from one woman to another. Many indicate that they have suffered physical discomfort, such as fatigue, dysgeusia, pain, nausea and vomiting, mucositis, diarrhea, etc.
One day when I didn’t want to go to bed , I went to bed crying because I had the feeling that I wasn’t going to wake up . That day it was because I felt awful . (Patient 1)
Furthermore, all of the women suffer hair loss, which is one of the most-feared effects. Likewise, their body hair also falls out, especially on their face, and their weight fluctuates. All of these changes lead to a loss of identity that is experienced as taking away from their femininity. It must be remembered that oftentimes, chemotherapy is administered after surgery, further exacerbating this physical change. On top of all that, several women comment having to decide at the beginning of treatment whether to freeze their eggs or not; at that moment, many of them forfeit the possibility of becoming a mother or of becoming a mother again, which also adds to this loss of femininity.
Losing my hair was hard , but when it grew out again , I had an identity crisis . I didn’t recognize myself; people said I was really pretty like that , with my hair so short . I looked at myself in the mirror and I said that I’m not that woman , I can see that that woman is pretty , but it’s just that I don’t recognize myself . That’s not me or , it was like , I looked at myself and I didn’t recognize myself . That’s when I suffered a serious identity crisis , psychologically serious , but also serious because I sobbed because I looked at myself , but it wasn’t me . (Patient 6) Where’s that sexy lady , where is she ?, because you don’t feel good . I didn’t like myself at all . I was several sizes larger and I looked at myself and said , “What a monster . ” I didn’t feel good about myself . (Patient 1)
Many patients say that chemotherapy decreases their libido and dries up their mucous membranes, which is why they prefer not to have sex. For those who live as a couple, this situation can strain the relationship.
Sexually , I just didn’t feel like it , I wasn’t in the mood; not only did I not feel like it , my mucous membranes were dry and , what’s smore , I just couldn’t , I couldn’t , I felt bad for my husband , but he said , “Don’t worry .” (Patient 16)
Finally, some interviewees expressed a feeling of being poisoned by the treatment. These women tend to be highly focused on taking care of their body and have a very natural attitude toward life.
I had to really work my awareness that I was poisoning myself; at night I was at home and I thought that all that red liquid was circulating through my veins … I think I even had nightmares . (Patient 4)
Balance between caring for oneself and caring for others . The patients feel that it is time to take care of themselves, so they prioritize resting when they need it. Moreover, they worry about getting a haircut and, most of the times, they look for turbans and wigs. Some also learn how to put on make-up, which they rate as being very positive. On the other hand, those who have children or another person in their care, try to take care of them as much as they are able.
Around 11 : 00 , I no longer felt good , so I’d go to the armchair to rest and it’s like I had an angel , because I’d wake up a minute before I had to set the table and get lunch for my son who would be coming home from school . (Patient 1) While I was getting chemo , I went with the gadget and I told myself , “I’m going to teach you to apply make-up; for instance , your eyelashes are going to fall out . Make a line like this ” and at that moment when you look in the mirror , and we look like Fester in the Addams family . (Patient 13)
Vulnerability . The women experience great uncertainty and feelings of vulnerability the first times they receive chemotherapy, since they don’t know what side effects they will suffer.
With chemo , I started with a lot of fear and , later on , I became familiar with it little by little until the time comes when you go to the hospital like someone who’s going to pick up a bit of paper . (Patient 9)
In addition, those participants who join a social network or who are more closely tied to the hospital setting, know about the relapses and deaths of people around them diagnosed with breast cancer, which makes them feel highly vulnerable.
There are some people who leave the group because … it’s not like there are a lot of relapses and , geez , I think that it messes with your head . (Patient 13) We were almost always the same people at chemotherapy ; there was one guy who was really yellow who looked terrible and , there was one time when we stopped seeing him and another lady asked and the nurse said that he had died . (Patient 15)
At the same time, given the physical changes, especially those that have to do with body hair, many women feel observed when they leave home.
If I have to go out and take off my scarf because I’m hot or go straight out without any scarf on my head and whoever wants to look… let them ; I think that it’s up to us , the patients , to normalize the situation; unfortunately , there are more and more cases . (Patient 9)
Telling the kids . Since when the chemotherapy stage is going to entail many physical changes, the women look for ways to talk to their children about the treatment. Most of them comment that it is a complicated situation and all of them try to talk to their children in such a way as to protect them as much as possible.
I asked the nurse for help before I started chemotherapy to see if she had any pointers about how to talk about this with the kids and she recommended a story , but when I saw it , I didn’t like it … so , in the end , I decided to do it off the cuff . (Patient 10)
Radiotherapy/transition to normality.
The “last” treatment . When the patient reaches radiotherapy, normally, they have already spent several months undergoing physically aggressive medical procedures, which is why they feel exhausted. There is a physical exhaustion resulting from the previous treatments and made worse by the radiation therapy. Furthermore, many women also report feeling emotionally drained by the entire process. However, this is generally accompanied by joy and relief because they feel that they are in the final stage of treatment.
Emotionally , it’s a marathon that has to end up at some point . (Patient 10) For me , radiotherapy was like a lull in the battle , with a winning mind-set . (Patient 4)
Comparison with chemotherapy . There is a widespread perception that radiotherapy has fewer side effects than chemotherapy, although later, when they receive it, several patients suffer discomfort, above all fatigue and dizziness. Several report that at this point, they are mentally worn out and just want to be done with the process, which is why they have less information than about chemotherapy.
I feel like radiotherapy is unknown , that you think it’s more “light ” and it turns out not to be so light . (Patient 13)
Follow-up care/the “new” day-to-day.
Difficulty in getting back to normal . Once the patients are discharged, many feel that they need some time to recover, that it will be slow, in order to restore a more normalized pace of life. They are still working on their emotional and personal process.
When they tell you that you have cancer , they make it very clear : you have a goal; you have some months of chemo , some months of radio , and when you finish , you say , “And now , what do I do ?”. I say that because now I have to get back to my normal life , but I don’t feel normal . I still don’t feel cured , I’m not 100% . And you’re glad you’ve that you’ve finished it all and you’re alive , but at the same time , you say , “Gosh… this is very odd . ” It was a very strange feeling . (Patient 8)
Most patients report that their quality-of-life has diminished, due to the sequelae from the treatments. Lymphedema is one of the sequelae they name most often, although they also mention other symptoms, like digestive upset, weight issues, eye problems, scar pain, etc. The women who are on hormone therapy also suffer side effects, such as joint and muscle pain.
I have lymphedema and , although I have good mobility , I’m a little bit weak; when I go out for dinner , I generally order fish , because I can’t always cut meat well . (Patient 6)
Several interviewees also express difficulty in their affective-sexual relations. Many of them feel insecure because of all the physical changes; others have sequelae that hinder their relations, and still others are suffering symptoms of early menopause. This can cause problems in the couple and for those who don’t have a partner, suffer many complications when it comes to meeting other people.
I haven’t had sex with my husband for 2 years because , it’s also really complicated to get over; I’ve gone for pelvic physical therapy; I’ve used gels , but nothing works . (Patient 8) It’s taken me many months for me to have a relationship again; it’s been really hard because , even though everyone told me that I looked fine , I didn’t feel fine . My breast cancer had taken away all my attributes as a woman . (Patient 6)
Some women also experience difficulties when it comes to returning to work. Several state that they had been fired when they went back. They also report that when interviewing for a job, it’s complicated for them because they have to explain what happened and they mention the schedule of doctor’s visits that they have. Other women comment that they’ve been given early retirement or disability.
You go to the interview and if you tell them that you’ve had the disease , they look at you like you’re a weirdo . (Patient 13)
Breast reconstruction . How reconstruction is experienced, as well as its timing, are highly contingent upon they type of reconstruction. Each one has its pros and cons, but the opinions collected with respect to the type of reconstruction have been positive.
Although it took 18 months for the entire process to be over , I’m delighted with reconstruction with the expander . (Patient 16)
Some patients state that after the whole process, which has been long and complicated, they prefer not to undergo reconstruction immediately. In these cases, they report having felt a subtle pressure from the outside to undergo reconstruction.
Every time I went for my check-ups , they said , “You’re the only one left [who hasn’t undergone reconstruction]” and in the end , the truth is that I’m really happy because I think I look pretty . (Patient 12)
Check-ups and fear of relapse . Check-ups are one of the times that generate most worry and insecurity. The women remark that, starting a few days before and until they receive the results of the follow-up studies, they are more anxious about the possibility of relapse.
At every check-up my legs start shaking again and my stomach is in knots, although at my last one, everything turned out okay and I’m thrilled. (Patient 6) During the first stage , I did everything I had to do and I got over it , but it’s a lottery . You can do whatever you want , but it’s the luck of the draw and when you start going for check-ups , it’s like going to play Russian roulette . (Patient 8)
Maintenance hormone therapy . Hormone therapy is understood differently depending on age and on the major decision of whether or not to be a mother or to have another child. If the woman does not want to have more children, the treatment is accepted better. The patients who take it also report effects derived from menopause, for instance, joint pain or dry mucous membranes.
I did notice joint pain , but since I exercised , [I felt it] much less than my fellow women , although , for instance , when it comes to getting up from a chair , you get up like an old lady . (Patient 10)
Position of support . Several patients mention that, after discharge, they stay active on social media, they volunteer when they find out about someone or to participate in activities related to breast cancer, with the aim of being able to help other people who are in this situation.
It’s really good to meet other people who are going through the same thing , so , now that I’ve finished , I like it and I always help whenever I can , because I can share what was good for me . (Patient 13)
Relapse/starting over.
Emotional impact . The diagnosis of a relapse is experienced much the same as the initial diagnosis. All of the women report fear, although they also state that they are more familiar with the processes. Other emotions emerge, such as why me, blame, disbelief, etc.
Since they had told me that it wasn’t going to happen again , I believed it , of course , I wanted to believe it and it totally surprised me; I couldn’t stop crying and crying . (Patient 17)
Telling the family again . Patients repeat that telling the family about it again, especially the children and parents, is tough and they try to minimize it in an attempt to protect them emotionally.
On the very same day that I had my mammogram , my mother says that she wants to come a see the kids . We’re in the park , when she arrives , I have to tell her that everything’s fine and when we get home , I tell her everything . My mother’s devastated again and I tell her not to worry , that everything is going to be fine . (Patient 16)
Thinking about whether something could have been done differently . Several women comment that, after their relapse, they think about whether the treatment was enough or there must have been something they could have done to avoid the relapse.
You get furious , because you say , “I wasn’t supposed to get sick , because if , 2 years ago when the first microcalcifications appeared I had had them removed , then I wouldn’t have metastasis , or maybe I would . (Patient 19)
Metastatic breast cancer/time-limited chronic.
Re-interpreting the concept of metastasis . Most of the participants in this stage state that they have had to give new meaning to the word, “metastasis,” since their first perception was directly related to death. In this way, they come to understand that cancer can become chronic, although they now have to take medication and go to the hospital on a regular basis. Nevertheless, they know that their life expectancy may be a few years. The women who are involved in a group point out how hard it is to see their fellow member pass away.
What I now call my “ new normal” consists of lots of visits to the hospital and never going back to work . (Patient18)
They also state that at this stage, they do not identify with the disease generally known socially as “breast cancer”, where there is great emphasis placed on early detection and on their chances of being cured. This causes them to feel more isolated.
These pink ribbon campaigns hurt us because they tend to underscore that everything is going to turn out fine because breast cancer has a very high cure rate; there is huge lack of awareness . (Patient 20)
Physical and emotional discomfort . Most of the women in this stage report side effects from the treatments, although some comment that good quality-of-life can be preserved. On an emotional level, they say that they sometimes feel a certain agony due to not knowing how much longer the treatment will be effective. They live in a state of uncertainty that they try to cope with by focusing on their day-to-day and experience the good times deeply.
When I’m not in pain , I try not to even remember what I have and go out and have fun with my family and live . (Patient 20)
Several women who have children express with regret that they worry about their children enjoying them and remembering them when they were well. They are sad that they won’t be able to grow up in a normal family. Some also comment the impact this diagnosis is having on their partner.
What I don’t want is for them to carry this baggage of having a sick mother . (Patient 18)
A conflict with disability also appears, as many women report their desire to continue working, but feel that they can’t keep up with the pace of work. Additionally, several state that going through the medical board is a strenuous process, given that they look good physically.
It’s hard to deal with , I’m a non-practicing lawyer and I have degrees galore , but I worked the first year and I couldn’t continue . (Patient 21) Every year they call me again for the disability monitoring and they always threaten me . To be honest , the treatment doesn’t make me sick , but I don’t know how long it’s going to be like this . (Patient 19)
Social invisibility . The participants say that they do not have any physical signs of being ill, that they look fine, although they know and feel that inside, they are not well. They say that it is sometimes hard to manage socially, since on occasion, they feel misunderstood and disparaged.
I’m much sicker now , but people think or want to think that I’m fine . When I was doing chemo , it was like wearing a sign that said “cancer . ” (Patient 17)
This study describes the patient journey of women with breast cancer, specifying the different phases with the most relevant aspects of each, as well as the different cross-sectional features they report throughout the entire treatment process.
The results portray breast cancer as a process in which there is a striking feeling of loss of health and self-identity, changes in routines, personal and employment transformation, as well as emotional hardship during and after breast cancer treatment, aspects that are also reported in the literature [ 41 , 42 ]. Earlier studies state that experiencing cancer is highly stressful. It involves a major threat to life or physical integrity, in addition to mental health, interfering with the path, projects, and plans patients have for their life over the short, medium, and, on occasion, long term as well [ 6 ]. Along with reporting adverse physical and psychological impacts, patients also report positive ways in which they have grown psychologically or emotionally from the experience [ 7 , 42 ]. The diagnosis of breast cancer not only impacts the women individually, but also affects their surroundings. As reported in the literature, despite going through a very challenging time, the women struggle to put on a positive face and attempt to conserve the family’s well-being, specifically that of their children [ 7 ]. At the same time, the family is a fundamental source of support and usually provide indispensable support; however, it is not always effective, because family members do not fully understand the stresses involved in living with cancer [ 43 ]. Previous studies also reveal that for some women, their partners are one of their most significant supports; nonetheless, research also suggests that a cancer diagnosis predicts marital breakup more strongly for female survivors than males [ 44 ]. Our results reflect that the women frequently resort to other women in the same situation, possibly because they face significant unmet supportive care needs [ 30 ]. The need for social support may lead patients to seek social support groups consisting of people who are experiencing similar health crises, because such groups allow them to interact with those who best understand their suffering [ 43 ]. Another aspect that appears across the board is the relationship the participants have with the medical team. In this study, we have noted their trust in the medical team and acceptance of the treatments proposed without going into the clinical data of the disease and without needing to know the benefit provided by the treatment. Cancer patients are confronted with a potentially life-threatening [condition], feeling vulnerable, and need to rely heavily on their care providers, expecting the physician to act in their best interests [ 5 ]. Therefore, they need to have a close relationship, as well as comprehensive care [ 30 ]. Patients’ trust in a physician has been associated with a reduction of their fears and anxiety and [increased] satisfaction and adherence to treatment [ 5 , 30 ]. We believe that it would be important to provide patients with accurate information, so as to avoid misunderstandings (such as cancer being synonymous with death, regardless of stage) as several participants in this study have reported, which can lead them to believe that the risk of relapse with and without chemotherapy is much greater than the oncologists estimate [ 45 ]. We believe that in future studies that it would be worthwhile to examine the peculiarities of each kind of patient information with the aim of determining how to break it up and make it both comprehensible and tolerable to promote patients’ well-being.
A breast cancer diagnosis is generally unexpected and practically all patients suffer psychological distress, such as feelings of uncertainty, disbelief, hopelessness, vulnerability, anger, fear, anxiety, and sadness [ 46 , 47 ]. The literature has reported that many women experience peritraumatic distress or dissociation during the medical conversation in which they are given their diagnosis of cancer [ 48 ], which might account for the reactions of the respondents. Given that, when they receive their diagnosis, additional information is generally given to them, such as clinical aspects and preferred treatments. Repeating this information at subsequent appointments could contribute to improving communication with patient, since several participants stated that they found it hard to pay attention to the physician, given the emotional impact. Additionally, breast cancer patients tend to be diagnosed when they are relatively young, and often when they are in the middle furthering their career or raising children [ 12 ]. In spite of everything, the women try to put on as brave a face as they can and focus on maintaining their children’s well-being [ 7 ]. Telling children about their diagnosis is reportedly one of the biggest challenges; parents are usually unsure of how to tell them, because at the same time that they want it to be open and honest and cover their children’s developmental needs, they also want to protect them children [ 49 ].
Once diagnosed, breast cancer patients go through different treatments. The most salient experiences of these phases pertain to the impact of side effects on physical quality-of-life and psychological well-being, which is consistent with the literature [ 11 ]. Moreover, cancer therapy entails physical changes that affect their feminine identity, fertility, self-esteem, sexual functioning, and makes them more vulnerable [ 10 , 50 ]. Women described their inner self as being on an emotional rollercoaster with highs and lows throughout the various phases of treatment [ 7 ]. Given treatment side effects and sequelae, these women are more likely to experience physical symptoms and psychological disorders than patients with other kinds of tumors [ 51 ]. The side effects involve an acute sense of loss of health and quality-of-life, as well as identity and femininity. It would be interesting for future research to explore the therapies used in grief counseling with cancer patients, as understanding and exploring this perspective could comprise an additional clinical aid.
Once the women have completed their treatments, they gradually get back to normal and many contemplate returning to work. However, in line with our results, the literature reveals that even though they want to normalize their lives, female breast cancer survivors feel that they will never return to their baseline status [ 7 ]. A significant number of patients experience difficulties in physical, cognitive, and emotional functioning after their treatment, such as symptoms like lymphedema, fatigue, pain, sleep disorders, cancer-related cognitive impairment, emotional stress, symptoms of depression and anxiety, problems with relationships, reduced sexual identity, fertility problems, and fear of cancer relapse [ 13 , 14 ]. Furthermore, patients with hormone therapy suffer hot flashes, sweats, joint pain, weight gain, decreased libido, and low energy [ 52 ]. A sizeable number of these women also experience changes in employment status which can happen even 5–10 years following diagnosis [ 15 ]. Given that all these changes alter the structure of the woman’s everyday life, personalized care and treatment plans in cancer survivors are highlighted in the literature with extended specialized support being proposed that enables them to make a better psychosocially adjusted transition from treatment to follow-up [ 53 ] and advocating for the patient’s participation in all decisions that affect her during this period [ 54 ]. Further research is needed concerning how to structure the follow-up and support offered to these women during this stage so as to meet their needs and help them adjust to their new reality with the chronic sequelae caused by cancer and its treatment. On the other hand, the personal transformation of the initial stages of the journey are best seen during this phase. The literature shows that women who have had breast cancer report changes in their philosophy of life, such as embarking on a new life path, changing their priorities in life, as well as valuing life in general [ 42 ]. Most of the participants in our study place special emphasis on appreciating life, enjoying it more, and living each day to the fullest. Cancer survivors report being aware of how precarious life is, while also feeling the joy of being alive [ 55 ]. Similarly, they have been found to be more resilient and better able to repair their mood than healthy women [ 56 ].
About 5% of all patients with breast cancer are diagnosed when the disease is metastatic, whereas some 30% have suffered a relapse of an early breast cancer [ 17 ]. We saw that some women suffering a relapse after initial treatment with curative intent tend to wonder if the treatment was sufficient or if they should have done something more to prevent the relapse. Metastatic breast cancer is uncurable, which is why these women’s main psychosocial challenges are not the same as those who are diagnosed in early stages [ 18 ]. Faced with incurability, the women react with shock and fear of imminent death, but this anxiety diminishes once they begin treatment and learn that there are more treatment options [ 17 ]. During this phase, the interviewees reported impaired physical QoL and functioning, being hindered by pain, fatigue, or menopausal symptoms. Emotionally, they report suffering bouts of depression and anxiety, as well as fear because of the spread of their cancer. As for their relational QoL, their children’s welfare is their number one concern, especially for mothers of young children [ 17 , 57 ]. What’s more, these women felt isolated from society in general and, more specifically, from the non-advanced breast cancer community, inasmuch as they feel that nobody understands what they are going through [ 18 ]. A psychosocial approach is especially important in this phase to help these women to continuously adapt to the changes of their individual clinical situation and to the progression of the disease, thereby improving their coping.
Clinical implications
Having first-person information enables us to comprehend in detail the experiences of breast cancer patients, their situation, and emotional state, which favors holistic cancer care for health professionals.
Healthcare professionals should prepare women for a changed life situation, as well as to face prolonged, multimodal treatment (surgery, chemotherapy, hormone therapy, radiotherapy), and to confront physical and psychological sequelae, as well as the fear surrounding an uncertain prognosis. It is important to help them manage their expectations and fears and, to identify and address the issues and concerns that arise at different time points during treatment. The information and support offered should be adjusted to each woman’s individual needs, her life situation, her coping style, and the time and stage of their cancer. This more empathic, understanding outlook can also contribute to improving the physician-patient rapport, promoting communication, understanding, and shared decision-making.
Finally, a comprehensive understanding of the women’s psychosocial support endorses their belonging to groups of women with breast cancer, in which there is a relationship among equals. Further research is needed to specify the type needed so as to decrease both the impact of the death of women in the group, as well as the vast amount of information that they may end up obtaining, without needing it or requesting it.
Limitations
This study was performed with Spanish participants, which is why certain aspects cannot reflect the experiences of breast cancer patients from other countries, given the particularities of both the Spanish healthcare system and Spanish culture. Likewise, the data attained were specific to women with breast cancer, which can scarcely be extrapolated to individuals with other cancers. Moreover, the findings do not reflect men’s experiences with breast cancer and research with this group would enrich the field further. In addition, the age of our participants ranged from 34 to 61 years; hence the results should be interpreted for a middle-aged population and do not reflect the experiences of women diagnosed at very early or very old ages. Finally, we believe that there may be a bias regarding the women who agree to participate, as this group has probably accepted their condition more, as well as having worked on it more.
Despite these limitations, we hope that our findings can contribute to better understanding the experiences of women with breast cancer.
Acknowledgments
The authors are grateful to the investigators of the Neoetic study and the Bioetic Group of the Spanish Society of Medical Oncology (SEOM) for their contribution to this study. We would like to thank all the women who generously shared their experiences with us, the support of HealthyOnco ( www.healthyonco.com ), and Priscilla Chase Duran for editing and translating the manuscript.
- View Article
- Google Scholar
- PubMed/NCBI
Journey mapping as a novel approach to healthcare: a qualitative mixed methods study in palliative care
Affiliations.
- 1 Faculty of Medicine Nursing and Health Sciences, Monash University, Clayton, VIC, Australia.
- 2 Supportive & Palliative Care Department, McCulloch House, Monash Medical Centre, 246 Clayton Road, VIC, 3168, Clayton, Australia.
- 3 Calvary Health Care Bethlehem, Parkdale, VIC, Australia.
- 4 Faculty of Medicine Nursing and Health Sciences, Monash University, Clayton, VIC, Australia. [email protected].
- 5 Supportive & Palliative Care Department, McCulloch House, Monash Medical Centre, 246 Clayton Road, VIC, 3168, Clayton, Australia. [email protected].
- PMID: 34479541
- PMCID: PMC8417950
- DOI: 10.1186/s12913-021-06934-y
Background: Journey mapping involves the creation of visual narrative timelines depicting the multidimensional relationship between a consumer and a service. The use of journey maps in medical research is a novel and innovative approach to understanding patient healthcare encounters.
Objectives: To determine possible applications of journey mapping in medical research and the clinical setting. Specialist palliative care services were selected as the model to evaluate this paradigm, as there are numerous evidence gaps and inconsistencies in the delivery of care that may be addressed using this tool.
Methods: A purposive convenience sample of specialist palliative care providers from the Supportive and Palliative Care unit of a major Australian tertiary health service were invited to evaluate journey maps illustrating the final year of life of inpatient palliative care patients. Sixteen maps were purposively selected from a sample of 104 consecutive patients. This study utilised a qualitative mixed-methods approach, incorporating a modified Delphi technique and thematic analysis in an online questionnaire.
Results: Our thematic and Delphi analyses were congruent, with consensus findings consistent with emerging themes. Journey maps provided a holistic patient-centred perspective of care that characterised healthcare interactions within a longitudinal trajectory. Through these journey maps, participants were able to identify barriers to effective palliative care and opportunities to improve care delivery by observing patterns of patient function and healthcare encounters over multiple settings.
Conclusions: This unique qualitative study noted many promising applications of the journey mapping suitable for extrapolation outside of the palliative care setting as a review and audit tool, or a mechanism for providing proactive patient-centred care. This is particularly significant as machine learning and big data is increasingly applied to healthcare.
Keywords: Health services research; Illness trajectory; Medical informatics; Palliative care; Patient journey mapping; Patient-centred care; Proactive healthcare.
© 2021. The Author(s).
- Delivery of Health Care
- Hospice and Palliative Care Nursing*
- Palliative Care*
- Qualitative Research
- Search Menu
Sign in through your institution
- Browse content in Arts and Humanities
- Browse content in Architecture
- Theory of Architecture
- Browse content in History
- History of Education
- Regional and National History
- Browse content in Philosophy
- Feminist Philosophy
- Philosophy of Language
- Browse content in Religion
- Religious Studies
- Browse content in Society and Culture
- Cultural Studies
- Ethical Issues and Debates
- Technology and Society
- Browse content in Law
- Comparative Law
- Criminal Law
- Environment and Energy Law
- Human Rights and Immigration
- Browse content in International Law
- Public International Law
- Legal System and Practice
- Medical and Healthcare Law
- Browse content in Medicine and Health
- Browse content in Public Health and Epidemiology
- Public Health
- Browse content in Science and Mathematics
- Browse content in Earth Sciences and Geography
- Environmental Geography
- Urban Geography
- Environmental Science
- Browse content in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Browse content in Business and Management
- Business Ethics
- Business History
- Corporate Governance
- Corporate Social Responsibility
- Human Resource Management
- Industry Studies
- Information and Communication Technologies
- Knowledge Management
- Criminology and Criminal Justice
- Browse content in Economics
- Behavioural Economics and Neuroeconomics
- Economic History
- Economic Systems
- Economic Development and Growth
- Financial Markets
- History of Economic Thought
- International Economics
- Public Economics
- Browse content in Education
- Educational Strategies and Policy
- Higher and Further Education
- Philosophy and Theory of Education
- Browse content in Human Geography
- Political Geography
- Browse content in Politics
- Asian Politics
- Comparative Politics
- Conflict Politics
- Environmental Politics
- European Union
- Indian Politics
- International Relations
- Middle Eastern Politics
- Political Economy
- Political Sociology
- Political Theory
- Public Policy
- Russian Politics
- Security Studies
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- Asian Studies
- Browse content in Social Work
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Developmental and Physical Disabilities Social Work
- Direct Practice and Clinical Social Work
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Urban and Rural Studies
- Reviews and Awards
- Journals on Oxford Academic
- Books on Oxford Academic

- < Previous chapter
- Next chapter >
14 Journey mapping as a method to make sense of participation
- Published: March 2021
- Cite Icon Cite
- Permissions Icon Permissions
This chapter explores how journey mapping as a qualitative research method allows young people on the edge of society to reflect upon and make sense of their engagement in different youth projects. The method provides the young people with the time, space and means to explore the participatory activities they engage in and to map the multiple ways they play into the often messy, multi-sensual and frictional youth life on the edge of society. This approach to journey mapping is inspired by cultural researcher Roz Stewart-Hall, who developed the method along with other participatory-driven visual methods in a critique of how project evaluation seldom carried any meaningful insights into what makes a difference to the participants in different projects as well as in broader explorations of what it means to be a young person on the edge of society (Hall, 2005; Hall, 2015).
Signed in as
Institutional accounts.
- Google Scholar Indexing
- GoogleCrawler [DO NOT DELETE]
Personal account
- Sign in with email/username & password
- Get email alerts
- Save searches
- Purchase content
- Activate your purchase/trial code
- Add your ORCID iD
Institutional access
Sign in with a library card.
- Sign in with username/password
- Recommend to your librarian
- Institutional account management
- Get help with access
Access to content on Oxford Academic is often provided through institutional subscriptions and purchases. If you are a member of an institution with an active account, you may be able to access content in one of the following ways:
IP based access
Typically, access is provided across an institutional network to a range of IP addresses. This authentication occurs automatically, and it is not possible to sign out of an IP authenticated account.
Choose this option to get remote access when outside your institution. Shibboleth/Open Athens technology is used to provide single sign-on between your institution’s website and Oxford Academic.
- Click Sign in through your institution.
- Select your institution from the list provided, which will take you to your institution's website to sign in.
- When on the institution site, please use the credentials provided by your institution. Do not use an Oxford Academic personal account.
- Following successful sign in, you will be returned to Oxford Academic.
If your institution is not listed or you cannot sign in to your institution’s website, please contact your librarian or administrator.
Enter your library card number to sign in. If you cannot sign in, please contact your librarian.
Society Members
Society member access to a journal is achieved in one of the following ways:
Sign in through society site
Many societies offer single sign-on between the society website and Oxford Academic. If you see ‘Sign in through society site’ in the sign in pane within a journal:
- Click Sign in through society site.
- When on the society site, please use the credentials provided by that society. Do not use an Oxford Academic personal account.
If you do not have a society account or have forgotten your username or password, please contact your society.
Sign in using a personal account
Some societies use Oxford Academic personal accounts to provide access to their members. See below.
A personal account can be used to get email alerts, save searches, purchase content, and activate subscriptions.
Some societies use Oxford Academic personal accounts to provide access to their members.
Viewing your signed in accounts
Click the account icon in the top right to:
- View your signed in personal account and access account management features.
- View the institutional accounts that are providing access.
Signed in but can't access content
Oxford Academic is home to a wide variety of products. The institutional subscription may not cover the content that you are trying to access. If you believe you should have access to that content, please contact your librarian.
For librarians and administrators, your personal account also provides access to institutional account management. Here you will find options to view and activate subscriptions, manage institutional settings and access options, access usage statistics, and more.
Our books are available by subscription or purchase to libraries and institutions.
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Rights and permissions
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Help & FAQ
Journey mapping as a novel approach to healthcare: a qualitative mixed methods study in palliative care
- Medicine Monash Health
Research output : Contribution to journal › Article › Research › peer-review
Background: Journey mapping involves the creation of visual narrative timelines depicting the multidimensional relationship between a consumer and a service. The use of journey maps in medical research is a novel and innovative approach to understanding patient healthcare encounters. Objectives: To determine possible applications of journey mapping in medical research and the clinical setting. Specialist palliative care services were selected as the model to evaluate this paradigm, as there are numerous evidence gaps and inconsistencies in the delivery of care that may be addressed using this tool. Methods: A purposive convenience sample of specialist palliative care providers from the Supportive and Palliative Care unit of a major Australian tertiary health service were invited to evaluate journey maps illustrating the final year of life of inpatient palliative care patients. Sixteen maps were purposively selected from a sample of 104 consecutive patients. This study utilised a qualitative mixed-methods approach, incorporating a modified Delphi technique and thematic analysis in an online questionnaire. Results: Our thematic and Delphi analyses were congruent, with consensus findings consistent with emerging themes. Journey maps provided a holistic patient-centred perspective of care that characterised healthcare interactions within a longitudinal trajectory. Through these journey maps, participants were able to identify barriers to effective palliative care and opportunities to improve care delivery by observing patterns of patient function and healthcare encounters over multiple settings. Conclusions: This unique qualitative study noted many promising applications of the journey mapping suitable for extrapolation outside of the palliative care setting as a review and audit tool, or a mechanism for providing proactive patient-centred care. This is particularly significant as machine learning and big data is increasingly applied to healthcare.
- Health services research
- Illness trajectory
- Medical informatics
- Palliative care
- Patient journey mapping
- Patient-centred care
- Proactive healthcare
This output contributes to the following UN Sustainable Development Goals (SDGs)
Access to Document
- 10.1186/s12913-021-06934-y Licence: CC BY
Other files and links
- Link to publication in Scopus
T1 - Journey mapping as a novel approach to healthcare
T2 - a qualitative mixed methods study in palliative care
AU - Ly, Stephanie
AU - Runacres, Fiona
AU - Poon, Peter
N1 - Funding Information: We would like to acknowledge and extend our thanks to Kevin Shi who contributed to the Python code used for the journey map visuals. Publisher Copyright: © 2021, The Author(s). Copyright: Copyright 2021 Elsevier B.V., All rights reserved.
PY - 2021/12
Y1 - 2021/12
N2 - Background: Journey mapping involves the creation of visual narrative timelines depicting the multidimensional relationship between a consumer and a service. The use of journey maps in medical research is a novel and innovative approach to understanding patient healthcare encounters. Objectives: To determine possible applications of journey mapping in medical research and the clinical setting. Specialist palliative care services were selected as the model to evaluate this paradigm, as there are numerous evidence gaps and inconsistencies in the delivery of care that may be addressed using this tool. Methods: A purposive convenience sample of specialist palliative care providers from the Supportive and Palliative Care unit of a major Australian tertiary health service were invited to evaluate journey maps illustrating the final year of life of inpatient palliative care patients. Sixteen maps were purposively selected from a sample of 104 consecutive patients. This study utilised a qualitative mixed-methods approach, incorporating a modified Delphi technique and thematic analysis in an online questionnaire. Results: Our thematic and Delphi analyses were congruent, with consensus findings consistent with emerging themes. Journey maps provided a holistic patient-centred perspective of care that characterised healthcare interactions within a longitudinal trajectory. Through these journey maps, participants were able to identify barriers to effective palliative care and opportunities to improve care delivery by observing patterns of patient function and healthcare encounters over multiple settings. Conclusions: This unique qualitative study noted many promising applications of the journey mapping suitable for extrapolation outside of the palliative care setting as a review and audit tool, or a mechanism for providing proactive patient-centred care. This is particularly significant as machine learning and big data is increasingly applied to healthcare.
AB - Background: Journey mapping involves the creation of visual narrative timelines depicting the multidimensional relationship between a consumer and a service. The use of journey maps in medical research is a novel and innovative approach to understanding patient healthcare encounters. Objectives: To determine possible applications of journey mapping in medical research and the clinical setting. Specialist palliative care services were selected as the model to evaluate this paradigm, as there are numerous evidence gaps and inconsistencies in the delivery of care that may be addressed using this tool. Methods: A purposive convenience sample of specialist palliative care providers from the Supportive and Palliative Care unit of a major Australian tertiary health service were invited to evaluate journey maps illustrating the final year of life of inpatient palliative care patients. Sixteen maps were purposively selected from a sample of 104 consecutive patients. This study utilised a qualitative mixed-methods approach, incorporating a modified Delphi technique and thematic analysis in an online questionnaire. Results: Our thematic and Delphi analyses were congruent, with consensus findings consistent with emerging themes. Journey maps provided a holistic patient-centred perspective of care that characterised healthcare interactions within a longitudinal trajectory. Through these journey maps, participants were able to identify barriers to effective palliative care and opportunities to improve care delivery by observing patterns of patient function and healthcare encounters over multiple settings. Conclusions: This unique qualitative study noted many promising applications of the journey mapping suitable for extrapolation outside of the palliative care setting as a review and audit tool, or a mechanism for providing proactive patient-centred care. This is particularly significant as machine learning and big data is increasingly applied to healthcare.
KW - Health services research
KW - Illness trajectory
KW - Medical informatics
KW - Palliative care
KW - Patient journey mapping
KW - Patient-centred care
KW - Proactive healthcare
UR - http://www.scopus.com/inward/record.url?scp=85114358544&partnerID=8YFLogxK
U2 - 10.1186/s12913-021-06934-y
DO - 10.1186/s12913-021-06934-y
M3 - Article
C2 - 34479541
AN - SCOPUS:85114358544
SN - 1472-6963
JO - BMC Health Services Research
JF - BMC Health Services Research
- Architecture and Design
- Asian and Pacific Studies
- Business and Economics
- Classical and Ancient Near Eastern Studies
- Computer Sciences
- Cultural Studies
- Engineering
- General Interest
- Geosciences
- Industrial Chemistry
- Islamic and Middle Eastern Studies
- Jewish Studies
- Library and Information Science, Book Studies
- Life Sciences
- Linguistics and Semiotics
- Literary Studies
- Materials Sciences
- Mathematics
- Social Sciences
- Sports and Recreation
- Theology and Religion
- Publish your article
- The role of authors
- Promoting your article
- Abstracting & indexing
- Publishing Ethics
- Why publish with De Gruyter
- How to publish with De Gruyter
- Our book series
- Our subject areas
- Your digital product at De Gruyter
- Contribute to our reference works
- Product information
- Tools & resources
- Product Information
- Promotional Materials
- Orders and Inquiries
- FAQ for Library Suppliers and Book Sellers
- Repository Policy
- Free access policy
- Open Access agreements
- Database portals
- For Authors
- Customer service
- People + Culture
- Journal Management
- How to join us
- Working at De Gruyter
- Mission & Vision
- De Gruyter Foundation
- De Gruyter Ebound
- Our Responsibility
- Partner publishers

Your purchase has been completed. Your documents are now available to view.

Journey mapping as a method to make sense of participation
From the book young people’s participation.
- Anne Mette W. Nielsen and Maria Bruselius-Jensen
This chapter explores how journey mapping as a qualitative research method allows young people on the edge of society to reflect on and make sense of their engagement in different youth projects. The method provides young people with the time, space and means to explore the participatory activities they engage in and to map the multiple ways they interact with the often messy, multi-sensual and frictional youth life on the edge of society. This approach to journey mapping is inspired by cultural researcher Roz Stewart-Hall (hereafter and in the References quoted as Hall). She developed the method to address a critique of how project evaluations seldom carried any meaningful insights into what makes a difference to the participants as well as in broader explorations of what it means to be a young person on the edge of society (Hall, 2005).
Journey mapping is a way to invite young people on the edge of society to (re)define and negotiate that which makes sense to them when they engage in participatory activities.
The method emphasises the significance of a space for young people on the edge of society to reflect on their engagement and participation in adult-led programmes.
The method promotes a multiplicity of insights into youth lives on the edge of society rather than a unifying overview.
The method argues that this multiplicity can lead to new questions and understandings of what matters, when young people on the edge of society engage in participatory activities.
The method can easily be employed in arenas other than research, in order to increase and strengthen knowledge exchanges between professionals and young people on the edge of society.
- X / Twitter
Supplementary Materials
Please login or register with De Gruyter to order this product.
Chapters in this book (23)
Learn / Guides / Customer journey mapping (CJM) guide
Back to guides
The 7 best research methods for customer journey mapping
Getting authentic insights from customers is essential to effectively map out their journey. And understanding how users really interact with your product is the best way to provide tailored experiences that fit your customers’ diverse needs.
But it’s often hard to know where to begin the customer journey mapping research process and which methods to use.
Last updated
Reading time.

This article outlines the seven most effective research methods for customer journey mapping. Use our guide to prioritize the right qualitative and quantitative research processes for your needs—and implement them right away.
Use product experience insights to map your customer journey
Hotjar helps you understand your users by combining observational data with voice-of-the-customer (VoC) insights
7 effective customer journey mapping research methods
A customer journey map is a visual representation of how your users engage with your brand, from initial discovery—like searching online for a solution to their problem—to browsing your site, trying out your product, making a purchase—and beyond.
Make sure your customer journey maps are informed by user-centric research rather than assumptions and guesswork.
Carry out both qualitative and quantitative research using the methods below to create a map that accurately represents your users' product experience (PX):
Qualitative research methods
Quantitative research methods are essential for effective customer journey mapping: they provide hard data that’s easy to track and compare over time. But qualitative methods uncover the how and the why behind the numbers, helping you deeply understand your customers' experience.
Hotjar Product Designer Iga Gawronska stresses the importance of diving into customer emotions in research:
"I think it’s important to map out the actions, and also the emotions and thoughts of the people that perform the actions, your users."
Use the following four qualitative research methods to get an in-depth understanding of how customers engage with your brand online.
1. Customer interviews
Customer interviews are one-on-one conversations with people who actually use your product or service. Conducting them in-person often yields the best results because it’s easier to pick up on non-verbal cues and the interview can flow more naturally—but video conferencing with tools like Zoom is a good secondary option.
By engaging in an open-ended conversation with customers, you’ll get unexpected insights and granular details about your customer’s journey, which helps you empathize with the user experience (UX).
Structuring your user interviews in different stages can help get the conversation going. Start with a warm-up that establishes trust and builds rapport, then home in on your core questions, and end with more informal, concluding thoughts from both parties.
Input your results into a user research repository as you go, so you don’t get overwhelmed at the end of the interview process. Some researchers make simple spreadsheets in Google Sheets or Excel, while others use dedicated tools like EnjoyHQ or Dovetail .
Once you’ve aggregated your interview data, you’ll start to notice trends and commonalities between interviewees and understand how they’re engaging with key touchpoints in your customer journey and what’s most important to them.
Pro tip : use a transcription tool like Otter.ai to stay focused on conducting your interview without having to take detailed notes. Having a written record of interviews at your fingertips also speeds up your data organization and analysis later.
2. Remote observation
Remote observation lets researchers see how users are behaving using online tools like video calling and screen recordings.
Remote research is convenient for both researchers and participants—neither party has to leave the comfort of their home or workspace and they can do what they need to do when it suits their schedule. Using remote research gives you insights into how your customers interact with key touchpoints on the customer journey in their everyday environment and context.
Here are two effective ways to observe your customers’ journey remotely:
Use a video conferencing tool like Zoom or Google Meet and ask users to share their screen with you while they’re interacting with your site, app, or product. Draw on the data you gather to inform your customer journey map.
Use a product experience insights tool like Hotjar Session Recordings and watch playbacks of real users interacting with your site or product across an entire session, as you observe how they scroll, what attracts attention, and where they backtrack or bounce.
Recordings are particularly valuable tools to understand the customer journey because they let researchers observe users remotely without them feeling ‘watched’ and behaving differently than usual.
Filter your Hotjar Recordings to show certain user sessions based on referrer URL, the landing page they visited, whether they’re a new or returning customer, their session, the specific action they take, their location, and u-turns. This helps you spot trends, understand behavior patterns for different user personas , and dig deeper into the customer journey.
3. Lab observation
In lab observation, the researcher observes the participant in person, either in a formal ‘lab’ setting or another professional, controlled environment.
Lab observation can be complicated to carry out because of the cost and logistics involved, and it’s often more time-consuming than remote methods. But it’s a valuable research technique, with a reduced risk of technical difficulties and a great opportunity to build a friendly rapport with participants.
If you op for lab observation, record your conversations with participants or use a note-taking tool like Notion or Evernote to write down your observations while the participant is interacting with the site or product, so it’s easy to find the data later. As the participant explores key customer journey touchpoints , take the opportunity to ask follow-up questions to understand why your test customers are making certain choices.
4. Qualitative surveys
Qualitative surveys usually involve asking open-ended questions that prompt detailed, long-form user responses. They give you great customer insights to inform your journey map, are easy to put together, inexpensive, and work well with large numbers of participants.
The success of your survey depends on the UX research questions you ask .
It’s important not to (knowingly or unknowingly) ask leading questions, as you’ll likely get biased responses from your participants, which won’t help you in accurately mapping out your customers’ journey. Let’s imagine you ask a research participant the following survey question:
“Did our ‘sign up for a free trial’ button catch your attention on our homepage? Why?”
This doesn’t work because the participant can’t really answer your question freely: you’re implying that your homepage CTA button should have caught their attention, so they’re more likely to answer ‘yes.’
Instead, you should ask:
“What site element attracts your attention most on our homepage? Why?”
Or, if they’ve already converted:
“What made you decide to click the ‘sign up for a free trial’ button on the homepage?’
Here, you’re letting the research participant fill in the blanks on their own, which will get you a more accurate picture of their user experience.
Pro tip: use Hotjar’s Survey tool and s urvey templates to quickly and easily create your own qualitative surveys and get all the details about your customers’ journey—in their own words. Filter responses and set up automations for your team to receive alerts when you get certain survey responses to uncover trends in your user data all in one place.
Use Hotjar Surveys to connect with customers and hear about all the stages in their journey with your brand.
Quantitative research methods to complement qualitative data
While qualitative research is the best way to build empathy with your customers and get a holistic view of their product experience, you also need quantitative data to get an objective, granular understanding of key moments in the customer journey.
Use these three quantitative research methods to gather precise information about your customers’ digital journey with your product:
5. Website analytics
Because website analytics show you hard data about how people are interacting with your site, they’re a great resource for customer journey mapping research. Investigate these key metrics to better understand how your users move across touchpoints:
Traffic source: are customers searching for your site on Google, clicking on a landing page, or visiting from a social media channel?
Bounce rate : do visitors arrive on your site and navigate away soon after? Or do they stay for a while, browse, and take a conversion action, like making a purchase?
New vs. returning customers: how many users are new leads and how many are existing customers?
Session duration: how long do customers spend engaging with your site on average?
While website analytics don’t explain why your users are taking certain actions, they clearly show what customers are doing on your site —and how they got there .
For best results, use a PX insights platform like Hotjar to fill in the gaps between the numbers with rich qualitative insights.
Matthew Nixon, managing director of Molzana , illustrates how teams can combine website analytics and qualitative research tools for optimal customer journey mapping:
"Using tools like Hotjar adds color to our quantitative analysis. Before, events like button clicks, scroll rate, and video plays might not have been tagged. This is where Hotjar comes in; click and scroll maps allow us to quantify user behavior in a much more granular way, which complements the trend data we collect from web analytics."
Google Analytics is a great option for quantitative website or app data: it’s both powerful and relatively easy to set up and navigate. Use Hotjar’s Google Analytics integration to go deeper and gather both qualitative and quantitative insights to inform your customer journey map .
6. Quantitative surveys
Quantitative surveys ask customers closed-ended questions that can be answered quickly—by checking yes or no, typing in one word, or selecting a multiple-choice answer.
Quantitative surveys can take a bit longer to put together, but they’re quick and easy for customers to fill out. With Hotjar, you can quickly create quantitative surveys by modifying questions from our question bank, and build surveys your users can address in a click or two, without disrupting their experience.
While quantitative surveys don’t give you the same level of in-depth information as qualitative, open-ended questions, they’re helpful to get a statistical overview on the customer journey, or if you’ve already identified a potential problem and want to better understand the issue.
Imagine you've discovered, through qualitative research, that several customers report difficulties browsing your website. Place a quantitative survey on key web or product pages to get more details about the exact issues they’re experiencing with questions like:
Did you experience friction when browsing our website?
What was the biggest problem you experienced when browsing our website:
Difficult to navigate on mobile
Bugs or glitches
Confusing navigation menu
Pages loaded slowly or incorrectly
I had trouble finding what I wanted
Collecting enough responses to quantitative questions helps you prioritize the most important elements of the customer experience to map out an improved user journey.
7. Customer satisfaction scores
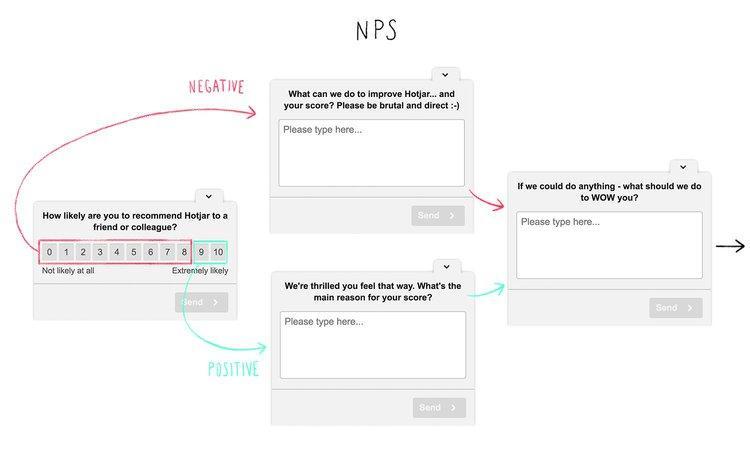
Measuring customer satisfaction is important to understand which touchpoints are working well for your users, and which you need to improve. In particular, Net Promoter Score® (NPS) is a great indicator of overall customer loyalty and satisfaction.
Researchers calculate this metric by asking existing customers how likely they are to recommend your product to their network on a scale of 1 to 10. Their ratings help you understand overall customer satisfaction levels, and also split users up into specific groups:
Promoters (9-10): your biggest fans. They’re highly likely to stay loyal to your company and recommend you far and wide.
Passives (7-8): middle of the road. These customers are more or less satisfied with your brand but would consider jumping ship to a competitor who meets their needs better.
Detractors (0-6): these users may have had a negative experience with your company that’s made them unlikely to return—they may even write negative reviews or testimonials about your product or services. However, negative feedback is also useful as it helps you understand which parts of your customer journey you need to focus on and fix.
While NPS scores give you an idea of how well your brand is serving your customers, they don’t tell you why customers are so loyal they regularly recommend your company. That’s why it’s a good idea to ask a couple of quick follow-up questions in your NPS survey , like “What can we do to improve your score?”
Use Hotjar’s non-intrusive Feedback widgets and Survey tools to get NPS survey responses from customers while they’re navigating your site.
Once you’ve calculated your NPS score, use your findings to identify how you can improve the customer experience and where the customer journey needs updating. For example, if many customers complained about friction in the checkout process, that’s a good indication you should focus on optimizing that part of your on-site customer journey.
Deep customer knowledge makes for easy journey mapping
Thorough research is the best way to build a customer journey map that lets you truly understand your customers and their user experience. It’s essential to use a mix of qualitative and quantitative research methods to dig deep into how customers are behaving on your site and understand why and how they’re carrying out certain actions.
Combine these methods to understand your customers’ experiences from different perspectives and prioritize creating a stellar user journey.
Hotjar helps you understand your users by combining observational data with voice-of-the-customer (VoC) insights.
FAQs about customer journey mapping research
Why is customer journey mapping research important.
Customer journey mapping is important because it helps teams understand how customers interact with their brand in the wild. Customer journey mapping research makes sure your maps are based on accurate user data rather than guesswork and assumptions. By doing research, teams dig deep into the customer experience, uncover the touchpoints that are most impactful, and optimize their products or services accordingly.
What methods are good for customer journey mapping research?
Use a mix of qualitative and quantitative methods to get a full picture of how customers experience brand touchpoints and engage in strong customer journey mapping research. Here’s what we recommend:
Qualitative methods: customer interviews, remote observation, lab observation, and qualitative surveys
Quantitative methods: website analytics, customer satisfaction scores like Net Promoter Scores®, and quantitative surveys
Is quantitative or qualitative research better for customer journey mapping?
Neither quantitative nor qualitative research is better for customer journey mapping—both approaches complement each other and should be used together to get a full picture of how customers are behaving—and why they’re behaving that way. While qualitative research excels in uncovering genuine customer feelings and emotions, quantitative research is valuable because it gives research teams hard data that’s easily measurable and useful for analytics and spotting trends.
CJM examples
Previous chapter
CJM B2B stages
Next chapter
- Login to Survey Tool Review Center
Journey Mapping
Our process.
If you are coming from the user experience (UX) world, you are probably familiar with customer journey mapping. If you are coming from the customer experience (CX) or voice of the customer world, then you may be hearing more and more about journey mapping. This is the link between both worlds as more companies realize that the user experience is not limited to the usage of products, and the customer experience is not just about what happens when customers call customer service.
There are three main categories in journey mapping:
- Customer Journey Mapping: Focuses on the interactions a customer/user has with a company when trying to accomplish a goal (e.g. learn, try, buy, maintain, etc.)
- Human Experience Mapping: Focuses on an individual’s general experience within a particular product or service category without referring to a specific company (e.g. how consumers buy auto parts)
- Service Blueprint: Focuses on the alignment of customer-facing and back-end actions of the service process (e.g. customers’ use of hotel reservation systems and the company processes and resources to support them)
Why You Should Do It
In the current experience economy, it is important to understand the journey potential and current journeys customers take as they navigate a product/service category and interact with your company. It is also crucial for your organization’s processes to be aligned with the actions users take as they interact with your company.
You will win customers if you master this knowledge, but you will lose them if you don’t. Knowing your customer touchpoints and pain points will provide you with actionable insights to improve the customer experience. However, more important than that is the journey they take across those touchpoints.
Depending on how your organization is structured, and the nature of your products and services, your customers will have different journeys when they interact with your products and services. Some customers will have more pain points than others, therefore, you need to know which problems your customers are facing before you can fix them.
Mapping the customer experience either through customer journey mapping, human experience mapping or service blueprint mapping will allow your business to grow if you are willing to implement the insights you will gain from it.
The Approach
Journey mapping is conducted mainly through qualitative research. It requires the involvement of both key stakeholders in the organization and customers/users, particularly for customer journey mapping. The development of journey maps is often conducted in different phases and includes meeting with stakeholders, gathering available internal research and conducting external research with users for validation purposes.
In the case of customer journey mapping, it is important to understand the types of customers for which the experience is being mapped. Customer types are often described as “personas” who are involved in typical scenarios a particular customer segment may find itself in. If no persona research or customer segmentation has been conducted before journey mapping, we strongly recommend doing it. Without a clear idea of who the customer is, the journey mapping research is unlikely to provide useful insights.
Qualitative research methods we can use for journey mapping include:
- In-depth interviews (phone, online, and in-person)
- Diary studies
- Direct observation
- Contextual inquiry
- Competitive analysis (users use competitive products/services)
Target Audience Recruitment
Relevant Insights can recruit qualified B2C and B2B participants through our sample provider partners for both qualitative and quantitative research. Relevant Insights can also recruit participants from your customer database and will implement procedures to protect any identifiable personable information.
Another option is for you to recruit directly from your own customer database if data privacy restrictions don’t allow for customer data sharing. In this case, we will provide the necessary data collection tools or work with existing data collection tools (i.e. survey tools) if the data is required to remain in the account.
After a discussion with your team, we determine the sample parameters and assist with developing screeners. We also manage participant incentives.
Implementation
In direct collaboration with the client team, relevant insights will:.
- Conduct internal meetings with key stakeholder groups.
- Gather and synthesize internal research available (e.g. surveys, customer support logs, voice of the customer feedback, etc.) in hypothetical maps.
- Recommend the most appropriate qualitative research data collection method for the target sample.
- Develop a discussion guide to uncover the journey being mapped.
- Conduct qualitative research with customers/users (e.g. interviews, observations, etc.).
- Discuss recommendations for sample size and sample sources. Sample size requirements will depend on the product category, target audience, and incidence rates, among other factors.
- Monitor the field and provide daily reports on its progress and any issues that may arise.
- Rent facilities or online platforms as needed.
Analytical Plan
Depending on the type of journey mapping, you the map may include.
- Journey phases.
- Interactions and behaviors.
- Touchpoints.
- Customer-interface actions.
- Backstage actions.
- Business opportunities for improvement.
Relevant insights can provide different reporting options, which can be chosen based on budget and time constraints:
- Summary of internal stakeholder meetings.
- Short summary report with key findings for external research.
- Full, detailed report with analysis, charts, tables, quotes, and graphics in an appealing format for external research.
- Graphic representation of the journey map(s).
Typical Project Duration
Six to eight weeks.
Factors that can affect project duration include:
- The incidence rate of the target sample: The lower the incidence rate, the longer we need to stay in the field to gather the required data.
- Client team responsiveness: A delayed response to requests for feedback at different steps of the project, will stall a project and affect the delivery date.
- Timeline for stakeholder meetings.
The cost will vary depending on:
- Sample specifications and sample size.
- Reporting requirements.
- The number of stakeholder meetings/interviews.

- Privacy Overview
- Strictly Necessary Cookies
This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
Strictly Necessary Cookie should be enabled at all times so that we can save your preferences for cookie settings.
If you disable this cookie, we will not be able to save your preferences. This means that every time you visit this website you will need to enable or disable cookies again.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Glob Adv Integr Med Health
- v.12; Jan-Dec 2023

Journey Mapping Healthcare Worker Experience With Heart Rhythm Meditation
Logan t murry.
1 Department of Pharmacy Practice, The University of Iowa College of Pharmacy, Iowa City, IA, USA
Lisa Wilhelm
2 Penn State Health Milton S Hershey Medical Center, Hershey, PA, USA
John Corrigan
3 Journimap, Iowa City, IA, USA
Matthew J Witry
Levels of stress and burnout continue to rise amongst healthcare workers. In addition to systemic and institution-level changes to healthcare practice environments, well-being interventions, resources, and support to assist healthcare providers are necessary. Meditation practices like Heart Rhythm Meditation (HRM) may provide benefits to healthcare workers, but healthcare worker experiences with HRM are not well understood.
To explore healthcare worker experiences with HRM using a journey mapping approach.
An exploratory cross-sectional online survey was administered between May and July of 2020 to a purposeful sample of 25 healthcare workers currently practicing HRM. Surveys consisted of 5 open-ended and 36 multiple-choice items mapped to five journey mapping domains: Discover, Search, Assess, Decide, Assist. Descriptive statistics for survey items were generated in addition to a visual representation of a Persona and associated journey map for HRM. Content analysis was performed on open-ended responses using a general inductive approach to code responses and identify representative quotes.
Twenty surveys were completed for a response rate of 80%. The majority of respondents identified as women (n = 14). From the journey mapping output, the overall emotional experience score was an 8.2/10, suggesting respondents had positive experiences with HRM. Open-ended comments suggest that HRM provides important benefits to the personal and professional lives of healthcare workers. A small number of participants reported challenges like feeling difficult emotions during HRM practice.
Mapping the healthcare worker journey with HRM identified generally positive experiences with personal and professional benefits. While experiences were largely positive, HRM elicited difficult emotions from some individuals, suggesting that appropriate resources and support are required when considering HRM and other meditation forms.
Burnout is a psychological syndrome emerging as a prolonged response to chronic stressors experienced in one’s work environment which have not been successfully managed. 1 , 2 Burnout is characterized by three dimensions: physical and emotional exhaustion, increased mental distance from one’s job, and reduced professional efficacy. 3 High levels of stress and burnout are prevalent among healthcare workers, with existing studies indicating that approximately 50% of clinicians (physicians, nurses, pharmacists, and other professionals) report feeling burned out. 4
A large body of research has emphasized and evaluated self-care activities as potential coping-strategies for burnout, with considerable focus on mindfulness, meditation, and meditative practices. 5 - 9 Meditation, as defined by the National Institutes of Health Center on Complementary and Alternative Medicine, is “a mind and body practice that has a long history of use for increasing calmness and physical relaxation, improving psychological balance, coping with illness and enhancing overall health and well-being.” 10 Meditation has been shown to have a number of benefits, including improvements in perceived stress and burnout. 11 - 19 Further, mindfulness meditation may have positive effects on patient safety, with studies demonstrating a reduction in preventable errors. 12 , 20 - 23 While numerous studies have focused on mindfulness and loving-kindness meditation practices, exploring additional forms of meditation practice used by health care workers like Heart Rhythm Meditation (HRM) may provide new insights.
Heart Rhythm Meditation (HRM) is a form of meditation that coordinates the fundamental rhythms of the heartbeat and breath, with the basic steps of HRM include sitting upright, concentrating on breathing full slow breaths, and observing ones heartbeat or pulse by using a finger on an artery or feeling the heartbeat through proprioception and counting heartbeats and pulse. Once the heartbeat is identified, the heartbeat and counting are used to balance breathing, making inhalation and exhalation equal in length with the intent of slowing down both the heartbeat and breathe. While empirical evidence of HRM benefits are limited, heart and breath-related meditative practice have the potential to promote conscious breathing, improve heart rate variability (HRV) and vagal tone, which are correlated with improvements in brain function, self-regulation, performance, health, and well-being. 16 , 24 - 27 Pharmacists, pharmacy students, and a myriad of additional healthcare workers have reported engaging in, and benefiting from meditative practices, including HRM. Despite the increase in meditation amongst this population, the experiences of healthcare providers discovering, establishing, and maintaining a meditative practice are not well understood. 6 One way to understand these experiences is through the processes of journey mapping.
Journey mapping is a research methodology focused on the user experience and is typically employed to better understand consumer behavior, preferences, and experiences with products or services. 28 , 29 Journey mapping enables visualization of the overall experience of an individual from their perspective, including feelings, motivations, and attitudes, as they move through various interactions or “touch points.” 30 For the present evaluation, we focus on the journey of healthcare workers who have engaged in and developed a HRM practice. By using research methods purposefully focused on gaining empathy for the individual experience and collecting data on the entirety of the experience, journey mapping has the potential to convey deeper and more nuanced insights than other evaluation techniques. These insights may subsequently be used to identify potential targets to develop and implement formal resources and programs designed to support healthcare workers’ well - being and mitigate burnout. The objectives of this study were to 1) create a healthcare provider journey map depicting the experience of discovering, developing, and maintaining a HRM practice and 2) to explore the self-reported effects and experiences of healthcare worker HRM practices.
This exploratory study was conducted between May and July 2020. A purposeful convenience sample of 25 healthcare workers with HRM experience were recruited to complete online, journey map surveys. The sample was comprised of pharmacists, certified pharmacy technicians, physicians, registered nurses (RNs), certified registered nurse practitioners (CRNPs), opticians, therapists, chaplains, and dentists and were identified by a study author (LW) as having experience with HRM.
The study author (LW) who identified participants is a Medication Safety and Compliance Specialist trained in HRM and is a Certified HRM Instructor who currently offers virtual drop-in meditation sessions at their institution. While some individuals identified to complete the journey map surveys had participated in the drop-in meditation sessions, others were recruited from outside the institution who had familiarity with the study author providing HRM sessions and had experience with HRM outside of and/or in addition to the drop-in sessions. While some study participants had participated in HRM instruction provided at the institution, the anonymous nature of the survey prevented those individuals from being identified. The drop-in meditation sessions consisted of weekly classes, taught by a certified HRM teacher (LW), where the fundamental steps of HRM were practiced, any questions or difficulties surrounding HRM were resolved, and individuals were prepared for an established regular HRM practice moving forward. The study was reviewed by the Institutional Review Board and received an exempt status.
Survey questions were informed by standardized items within the online journey mapping platform (Journimap, Iowa City, IA) and were adapted for HRM. The journey mapping survey consisted of 5 open-ended and 36 multiple choice items, collecting data from five journey domains: Discover, Search, Assess, Decide, and Assist. These domains were identified from existing human-centered design research, focused on collecting information related to multiple phases which provide a holistic reflection and visualization of an individual experience. 30 , 31 Additionally, the journey mapping survey was informed by remote ethnography principles. 32 Ethnography is a methodological tool that “gets close” to a particular group and/or sub-group to uncover cultural phenomena, offering exploratory researchers an opportunity to uncover their social realities. 33 , 34 Ultimately, the journey mapping survey was specifically designed to collect and visualize the dynamic experience of healthcare workers currently practicing HRM and to uncover specific components of the experience related to the practice.
The online journey mapping platform maps multiple-choice survey response items to each experiential domain ( Discover , Search , Assess , Decide , Assist) and uses an algorithm to produce a visual journey map which is an aggregate representation of all respondents’ experience with HRM, titled: Persona , E mpathy , and Current Journey . The Persona outputs can be described as an avatar representing an aggregate of all responses, providing generalized characteristics of the survey group based on median responses. The Empathy outputs are a visual depiction of four emotion domains: Think & Feel , Hear & See , Pain , Gains , which are common experiential domains within journey mapping work. 28 , 29 , 35 While these domains within the Empathy output are specific to the journey mapping platform, they were designed to capture emotions experienced throughout the process of discovering and practicing HRM while facilitating empathetic understanding of the participant experience. The Think & Feel and Hear & See domains reflected participant emotions surrounding discovery and practice of HRM. The Pain and Gains domains captured participant emotions reflecting general difficulties and positive outcomes or benefits associated with HRM experience. The domain outputs were informed by the 35-items of the journey map survey and were generated by median scores for items in each of the five decision-making domains. The Empathy output also procured an overall emotional experience score, quantifying the overall experience based on the range of emotions felt in learning HRM. Scores may range in values from 0 to 10, with larger values associated with better or more positive experiences. The Current Journey outputs provide a visual depiction of the HRM process, progression through the five journey map domains. The Current Journey outputs mapped Good and Bad Experiences within the healthcare worker’s experience with HRM.
Descriptive statistics for survey items were generated in addition to a visual representation of journey mapping results. Content analysis was performed by two authors using a general inductive and manifest analysis approach to categorize open-ended responses and identify areas of salience and divergence. 36 , 37 The manifest analysis approach to content analysis focuses on what the informants actually say and is well-suited to descriptively assess participants experience with HRM. 38 To encourage quality in qualitative research and to triangulate findings, initial open codes were assigned to open-ended response text by two study authors (LTM and MJW). The two study authors then met to group open-ended responses which reflected similar concepts, identifying similarities and differences in HRM experience and discussing the interpretation of responses. The two study authors developed a narrative which reflected the experiences of healthcare workers practicing HRM, which was reviewed by a third study author who was a certified HRM instructor and was providing drop-in HRM sessions (LW). Finally, all study authors met to discuss journey map results and identified themes.
Quantitative Journey Map Survey Responses
In total, 20 surveys were completed for a response rate of 80%. Of the received responses, 70% identified as women (14) with 85% (17) of respondents identifying as white. The most frequent response categories for education level and annual household income were “Advanced Graduate Work or PhD” and “Over $100,000,” respectively. The journey map Persona output ( Appendix 1 ) provides an avatar representing the mean age and most frequent responses from the sample.
From the Empathy output ( Appendix 2 ), the overall emotional experience score was an 8.2 out of a possible 10, which suggests that the sample had overall positive experiences with HRM. Individuals overall had initially heard good things about HRM, felt good about their experiences, and looked forward to engaging with HRM. No salient pain points were identified across participants, but individuals appeared to have difficulties comparing HRM to other forms of meditation or well-being practices and understanding what HRM had to offer related to benefits or practice alternatives. Further, the decision to initiate and continue an HRM practice and the associated discomfort associated with the difficulty of these decisions varied across respondents. Descriptive statistics for items comprising each journey map domain are included in Table 1 .
Descriptive Statistics for Journey Map Items. a
a the total number of responses for all items was 20, with Likert-type items reported as 0 = Strongly Disagree to 4 = Strongly Agree.
b indicates a negative-worded item.
From the Current Journey output, healthcare workers appeared to have the most difficult time in the Search and Decide journey map domains. The Current Journey output is included in Figure 1 .

Current journey output: Healthcare workers experience with HRM.
Qualitative Journey Map Open-Ended Responses
The process of discovering and engaging with HRM. Healthcare (HC) respondents were referred to HRM through different processes including personal invitations from colleagues and friends, or from an advertisement by the health system or health system wellness programming. Individuals had a wide range of HRM practice experience, which varied from 3.5 to 20 years. Additional quotations and their associated domain can be found in Table 2 .
Through a physician at work that had attended the school. About 5 years ago. [HC9]
From a friend. 20 Years ago. [HC4]
Easy decision, I trusted the person who told me about it. [HC14]
Journey Mapping Domains and Quotes. a
a (+) and (−) denote positive and negative comments within the healthcare provider HRM journey as determined during the coding process.
Respondents varied in their process for initially evaluating and discerning their engagement with HRM. Some found the premise for HRM intuitive and that it “felt right” [HC4] and appreciated the physiological basis for HRM. Others, however, wanted more explicit research supporting the HRM practice.
It was new and exciting form of meditation and based on science seemed to make sense. [HC9]
There is not any research in referenced journals about HRM. [HC16]
There are some materials in the teaching [session], but when it comes to more detailed or scientific-based information, it was difficult to get or find. [HC6]
Some participants had experience with other forms of mindfulness-oriented meditation and preferred HRM because of the flexibility, openness, and spiritual but not religious nature of the approach.
HRM helped me focus more than mindfulness. [HC9]
Most enjoyable was connecting my breath with my heartbeat--this felt like I was home. [HC3]
At first, it felt almost like work since I was used to just doing mindful meditating. But once I worked up to it… the benefits of breathing really seemed to have more benefits than mindfulness. [HC11]
Positive Experiences with HRM practice. Most individuals appreciated that HRM was practiced as a group with trained instructors guiding the weekly session. Many found community with their fellow meditators and instructors.
I loved the small group sharing. [HC8]
Feeling accepted by a group of like-minded people. [HC10]
Most enjoyable was the connection to the teachers and students. [HC4]
Many of the healthcare workers also reported benefits to individual growth which they attributed to their HRM practice including improving awareness, gaining confidence, being present, improving relationships, and better engaging with patients and the world.
Daily regular practice that benefited my well-being. [HC11]
Yes. improve relationship capacity and manner, self-trust, regulation of physical health. [HC2]
Deep and vivid experience of my emotions; clarity to negotiate higher salary; ability to authentically connect with and serve my patients. [HC14]
My benefits were strengthening my nervous system, getting self-worth, decision making got easier, there came more clarity into my thoughts and feelings, less fear for everything that is needed to do, more joy, better relationships. [HC4]
Negative Experiences With HRM Practice
While not a common sentiment, a small number reported challenges and frustration with HRM practice, especially early on as they were gaining experience. Some were initially hard on themselves for not doing HRM properly and comparing themselves to the experiences and abilities of others. Additionally, some individuals noted that it was difficult to establish a daily practice. Lastly, a few respondents shared they had experienced difficulty breathing and uncomfortable emotions, especially when practicing HRM on their own.
Least enjoyable was comparing myself to others in my meditation class that knew more and had deeper experiences than myself. [HC3]
Least enjoyable was to find a daily rhythm and establish a daily practice. Further to go to the deepest emotions as anger, fear, guilt, and breath through it. [HC4]
Initially I felt very incompetent. I went through a period of 4 months where I was drenched in sweat by the end of every 20 min. session -- it was most unpleasant, but I persisted…,[HC20]
The ONLY time I can count on it being pleasant is in a group setting. It is still extremely unpleasant at times -- a kind of nameless anxiety comes over me that I can barely stand. [HC20]
That inner voice that comes and goes that… I’m not progressing properly. [HC2]
Trying to control breathing, it felt unnatural and caused hyperventilation. [HC17]
Overall, the healthcare worker journey with HRM was positive, with an aggregate emotional experience score of 8.2 without salient pain points. Some participants, however, expressed strong emotional reactions at different points in the process and expressed multiple difficulties in their HRM practice. There was variation in how healthcare workers gained an understanding of HRM and making the decision to continue an HRM practice. Other key findings were the importance of group practice and the personal and professional benefits to HRM.
Respondents shared a range of positive sentiments in their open-ended comments including the benefits of the practice on individual growth, self-management, and their ability to engage with patients. This provides some support that meditation practices such as HRM may be especially beneficial in the study population, as the majority of participants had completed advanced graduate work and were practicing clinicians, a population is especially susceptible to burnout. 39 , 40 In the existing literature, institutions supporting meditation and mindfulness-based interventions while providing guided meditation and training resources appears to provide individual benefit. 8 , 9 , 41 , 42 More specifically, a study on the effects of “Heartfulness Meditation,” a heart-based meditation practice, found that a 12-week program resulted in significant improvements in professional burnout and emotional wellness in residents, faculty physicians, and nurses at a large community teaching hospital. 5
Additionally, the group nature of HRM sessions that some individuals participated in appeared to provide considerable benefit and may be a key attribute to initial and sustained practice. A recent study by Hanley et al suggests that group meditation may be especially beneficial in producing states of mindfulness and improving feelings of social connectivity compared to a solitary meditation practice. 43 Other interventions commonly offered in group-settings, such as Yoga, have shown positive effects on healthcare worker stress and burnout. 44 Further, social support appears to mediate the effect of burnout in health-professionals, providing additional support that group-based interventions facilitating social support and connectedness may improve healthcare worker well-being. 1 A recent study by Halimi et. al. identified that peer and organizational support, and resilience-fostering programs, supported professional resilience in early career pharmacists. 45 As such, additional research is needed to explore and understand the moderating effects of group-based interventions, such as meditation, on participate experience and outcomes associated with interventions designed to improve healthcare worker well-being.
In addition to the reported benefits of HRM, qualitative responses suggested several challenges which may be useful to incorporate into the development of HRM programs, specifically related to developing a sustainable practice and the need for support. A number of participants reported difficulties establishing a daily practice and experienced negative thoughts, emotions, and physical responses to HRM. Studies have highlighted that negative emotions amongst healthcare workers with the initiation of meditative practice are not uncommon. 46 Further, long practices, emerging negative thoughts, and becoming self-critical were factors identified as key barriers to healthcare workers engaging in a self-help mindfulness-based intervention. 47 When considering the development and provision of meditation interventions, education and interpersonal support may help to improve the initial and sustained practice of meditation and facilitate the development and provision of meditation self-care activities. 48
Recommendations for Health Systems and Healthcare Workers
This exploratory study found generally positive experiences for HRM both in the areas of personal and professional growth, but also for community building when people meditate as a group. Health system investment in well-being programs and initiatives like group meditation sessions may help build connectedness and resiliency while potentially mitigating burnout. When encouraging healthcare workers to participate in self-care activities, organizations and institutions may benefit from considering how to support employees to engage in these activities, providing the necessary time and support to have positive experiences, outcomes, and develop sustainable meditation practices. In the instance of healthcare workers HRM practice, providing dedicated work time and access to licensed meditation instructors and other mental-health professionals may contribute to promoting meditation as a self-care activity.
While HRM and other meditation practices may be a potentially beneficial self-care activity promoting well-being and helping individuals cope with burnout, meditation is not a substitute for structural changes and organizational support for employees at a system level to address burnout and employee well-being. 48 , 49 Additional workplace and organizational level changes are likely needed to prevent burnout and support employee well-being, in addition to the development and provision of evidence-based strategies to promote the health, development, and well-being of healthcare workers. 2
Limitations
The study should be considered exploratory, as a small, purposeful sample of healthcare workers were surveyed who already were enrolled in the HRM program. Further, the sample consisted of predominately women and individuals who had completed advanced graduate work, which may limit transferability of findings to other groups. Additionally, many individuals have established long-term HRM practices, and their experiences may differ from individuals with more recent familiarity with HRM. As journey mapping is designed to explore and understand individual experience, no control group (eg those who did not use HRM) was included in the study. Participants who initiated HRM practice but have been unable to sustain practice likely have different journeys and experiences. The survey also may be subject to recall bias as some participants made the decision to practice HRM years before completing the survey, with varying durations of practice, practice setting, and current practice having the potential to impact perceptions and experiences with HRM.
Conclusions
Overall, healthcare workers practicing HRM had generally positive experiences and reported a number of benefits from their meditative practice, including an increased connection with patients and colleagues. Care should be exercised in administering these programs as a small fraction of individuals reported difficult emotions and discomfort in their early experiences with HRM. Most healthcare workers practicing HRM persisted in their HRM practice, even when experiencing difficult emotions and perceived long-term benefits.
Appendix 1. Persona output from journey map, depicting a general summary persona based on demographics and characteristics of all respondents.

Appendix 2. Empathy output from journey map, depicting the experienced emotions and overall emotion score.

The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: JC is the founder and CEO of Journimap, Iowa City, IA.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Logan T Murry https://orcid.org/0000-0003-0345-6997

Journey Mapping – A Visual Way to Get Closer to Your Consumers and Their Needs
Filed Under: Shopper , Consumer Empathy

Kat Figatner
Senior Vice President, In-Person Qualitative Research
Journey Mapping has been getting a lot of buzz lately. At C+R, we’ve been seeing the frequency of requests for this type of project growing over the years from clients across all industries. But you may ask, “what is a journey map and what’s so special about it?”
A journey map visualizes the needs, actions, mindset, and emotions a customer experiences as they engage with a product, service, or brand.
- The scope of the journey may span across the entire lifespan of a customer’s experiences – from awareness, through consideration, purchase, and loyalty or abandonment.
- It may be tighter in scope – to hone-in on a specific type of interaction or experience, such as the consumer shopper journey or the onboarding or learning curve within the initial usage stage of the product or service post-purchase.
Often with a journey mapping project, the key component is the specific output of the research – a highly visualized and succinct 1-page map to represent the journey.
- This visualization tells the story tightly and clearly to help build empathy for your consumers, identify how to engage with them, and optimize their experiences at the various touchpoints throughout the journey.

At C+R, we have a framework for approaching journey mapping, but as a custom consumer and market insights firm, it’s not a black box solution. Instead, we work with our clients to craft the research program that meets their specific needs.
- Typically, we start with a qualitative exploration to identify and illuminate consumers’ different paths and steps throughout their journey.
- This qual approach, which may include digital assignments, live conversations, or a combination of both, allows us to probe and understand their emotional highs and lows through the process: understanding triggers, key points of influence, and frustrations and roadblocks along the way.
We typically have a good sense of the journey from the qual research and may transition from there into the mapping process, or we may pause to validate what we learned through a quantitative survey.
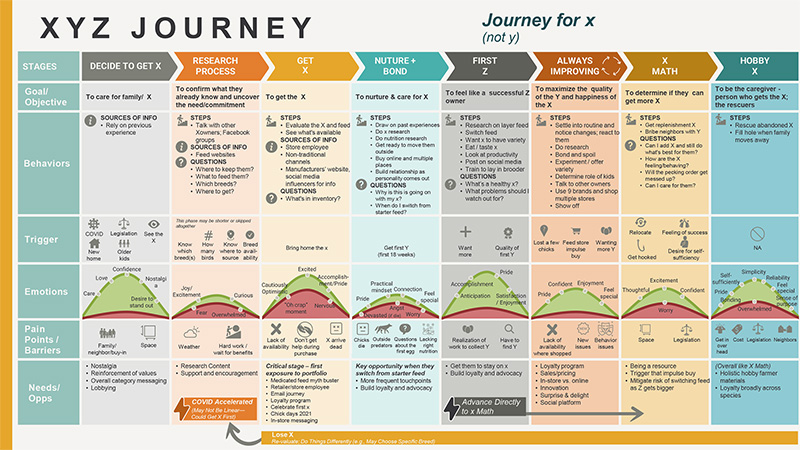
Example: Consumer Journey Map
Regardless, at the end of the research, we move onto the journey mapping phase of the initiative. This process typically involves two steps:
- We do this by holding an in-person workshop or series of virtual work sessions with the client team.
- We first prep a “strawman” or working draft of the map, then review each component in-depth with the client team.
- This collaboration allows us to add our client’s internal knowledge and previous consumer and market insights into the map, creating a more robust deliverable.
- We also use the time together to brainstorm on the implications and opportunities–what the client can do at each phase to address needs and pain points, and enhance their customers’ experiences.
- This process turns an otherwise boring grid into something more visually pleasing and easily digestible through graphics, icons, and other visual cues. This phase usually involves some back-and-forth collaboration to get the map’s look just right.
Sometimes the process ends there; other times, we go through it again, in a streamlined manner, if there are multiple maps to create based on different categories or consumer cohorts.
Journey mapping is a valuable final deliverable to sum up the consumer insights, and building one is useful to bring the client team closer to their consumers and their needs. Read how we helped our client understand the journey of the consumer sales consultant team in order to identify opportunities to support the consultants on their sales journey. Reach out to us at C+R if you want to learn more or see how we’d recommend tackling your consumer journey research mapping needs.
explore featured Case studies
Unlocking the power of product display pages for…, assessing the physical and digital shopper journey to…, helping a retailer organize its departments to meet….

Hey, get our newsletter
Join 5,000+ market research professionals who “emerge smarter” with our insights, what’s new & coming up, smartpulse: our neuroscience tool for assessing experiences, shopper segmentation.
Discover how our Shopper Segmentation can help understand shoppers’ mindsets.
WEBINAR NOW On-Demand
Empowering Your Strategies with Shopper Segmentation
Hear from our shopper insights expert, Kathleen Blum as she unveils our new proprietary Shopper Segmentation. Gain valuable insights into shoppers’ thoughts, needs, and behaviors in the food, beverage, and household categories. In this webinar:
- Learn the difference between a shopper and a consumer segmentation.
- Meet some of the shopper segments and gain a deeper understanding of their mindset, preferences, and motivations.
- Learn how our typing tool can be incorporated in targeted shopper projects and custom consumer segmentations for a comprehensive view of how your consumer and shopper segments intertwine.
- Discover how our shopper segmentation can help inform decisions about your product offerings, marketing strategies, and customer engagement initiatives.
Register Now
Search this site
Skip navigation

World Leaders in Research-Based User Experience
Journey mapping 101.

December 9, 2018 2018-12-09
- Email article
- Share on LinkedIn
- Share on Twitter
Journey maps are a common UX tool. They come in all shapes, sizes, and formats. Depending on the context, they can be used in a variety of ways. This article covers the basics: what a journey map is (and is not), related terminology, common variations, and how we can use journey maps.
In This Article:
Definition of a journey map, key components of a journey map, journey-map variations, why use journey maps.
Definition: A journey map is a visualization of the process that a person goes through in order to accomplish a goal.
In its most basic form, journey mapping starts by compiling a series of user actions into a timeline. Next, the timeline is fleshed out with user thoughts and emotions in order to create a narrative. This narrative is condensed and polished, ultimately leading to a visualization.
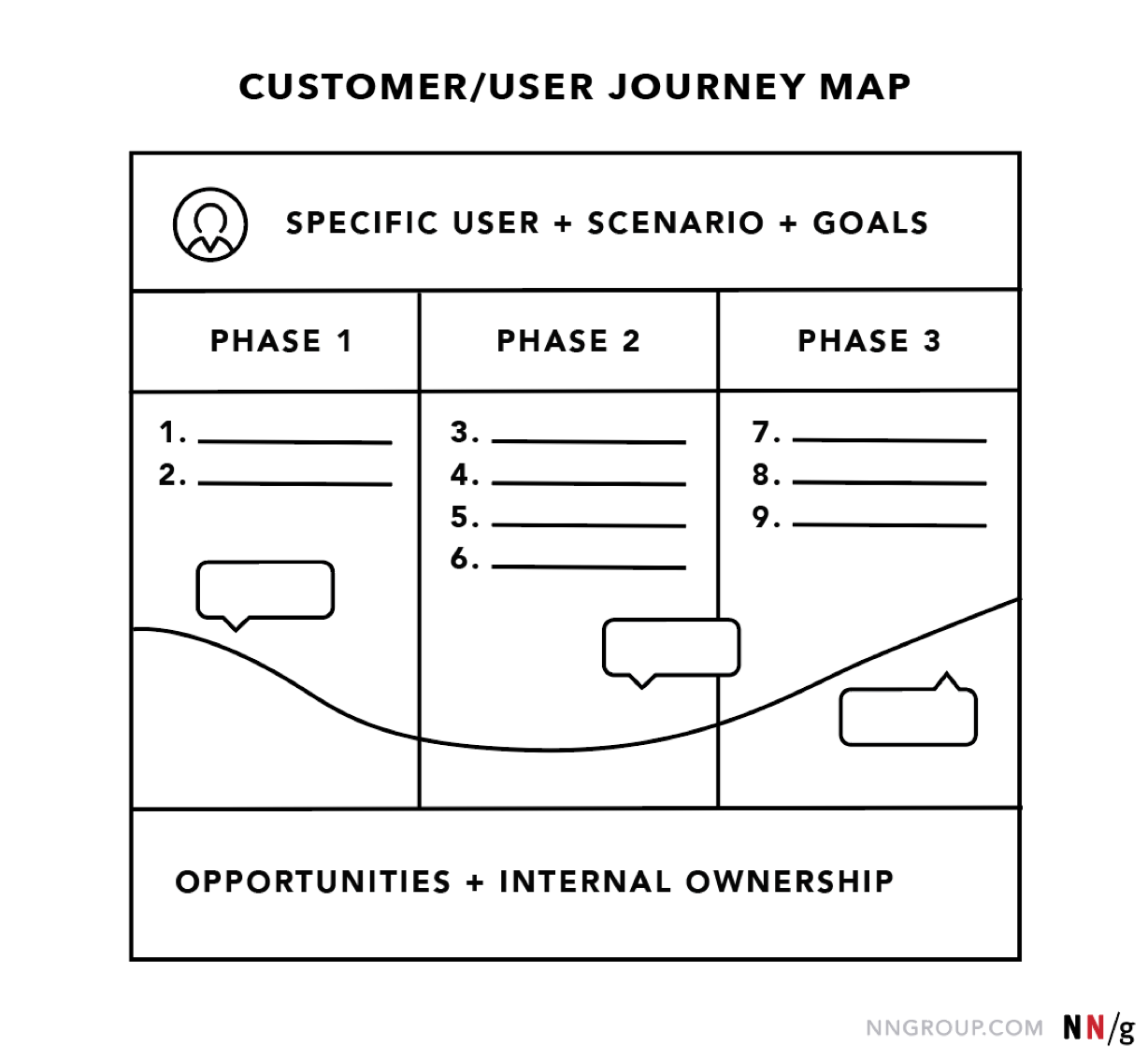
The terms ‘user journey map’ and ‘customer journey map’ can be used interchangeably. Both reference a visualization of a person using your product or service.
While the argument can be made that the term ‘customer’ does a disservice to the method (because, especially for certain business-to-business products, not all of end users are technically customers, i.e., product buyers), alignment on what you call the map is far less important than alignment on the content within the map.
Journey maps come in all shapes and sizes. Regardless of how they look, journey maps have the following 5 key elements in common:
Scenario + Expectations
Journey phases, actions, mindsets, and emotions, opportunities.
The actor is the persona or user who experiences the journey. The actor is who the journey map is about — a point of view. Actors usually align with personas and their actions in the map are rooted in data.
Provide one point of view per map in order to build a strong, clear narrative. For example, a university might choose either a student or a faculty member as actor — each would result in different journeys. (To capture both viewpoints, the university will need to build two separate maps, one for each of the two user types.)
The scenario describes the situation that the journey map addresses and is associated with an actor’s goal or need and specific expectations. For example, one scenario could be switching mobile plans to save money, and expectations for it include to easily find all the information needed to make a decision.
Scenarios can be real (for existing products and services) or anticipated — for products that are yet in the design stage.
Journey maps are best for scenarios that involve a sequence of events (such as shopping or taking a trip), describe a process (thus involve a set of transitions over time), or might involve multiple channels .
Journey phases are the different high-level stages in the journey. They provide organization for the rest of the information in the journey map (actions, thoughts, and emotions). The stages will vary from scenario to scenario; each organization will usually have data to help it determine what these phases are for a given scenario.
Here are some examples:
- For an ecommerce scenario (like buying Bluetooth speakers), the stages can be discover, try, buy, use, seek support.
- For big (or luxury) purchases (like buying a car), the stages can be engagement, education, research, evaluation, justification.
- For a business-to-business scenario (like rolling out an internal tool), the stages could be purchase, adoption, retention, expansion, advocacy.
These are behaviors, thoughts, and feelings the actor has throughout the journey and that are mapped within each of the journey phases.
Actions are the actual behaviors and steps taken by users. This component is not meant to be a granular step-by-step log of every discrete interaction. Rather, it is a narrative of the steps the actor takes during that phase.
Mindsets correspond to users’ thoughts, questions, motivations, and information needs at different stages in the journey. Ideally, these are customer verbatims from research.
Emotions are plotted as single line across the journey phases, literally signaling the emotional “ups” and “downs” of the experience. Think of this line as a contextual layer of emotion that tells us where the user is delighted versus frustrated.
Opportunities (along with additional context such as ownership and metrics) are insights gained from mapping; they speak to how the user experience can be optimized. Insights and opportunities help the team draw knowledge from the map:
- What needs to be done with this knowledge?
- Who owns what change?
- Where are the biggest opportunities?
- How are we going to measure improvements we implement?
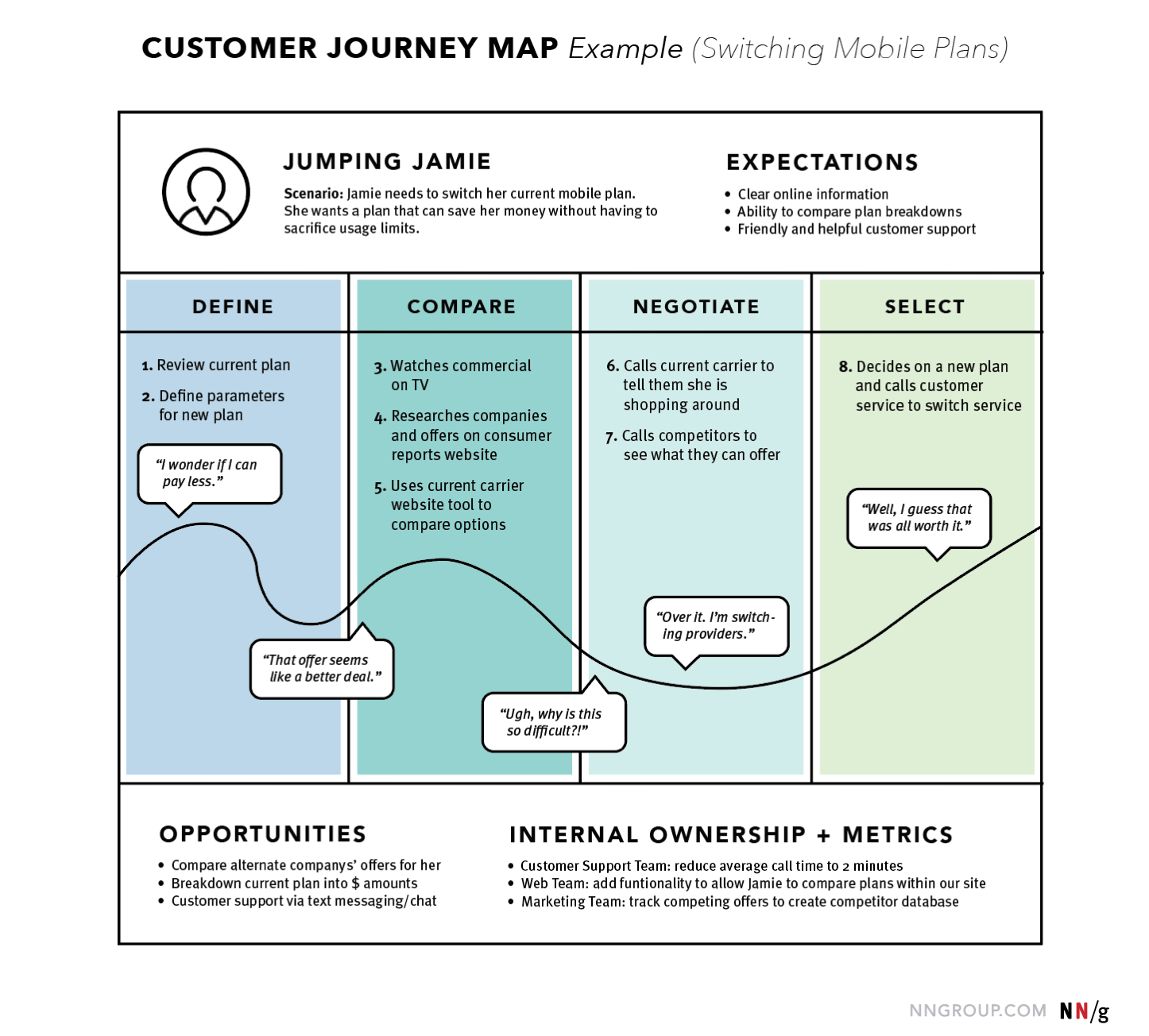
There are several concepts closely related and thus easily confused with journey maps.
It is important to note that this section is only meant to help your personal understanding and clarification of these terms. It is not advised to debate or attempt to shift a whole organization’s language to abide by the definitions stated here. Instead, use these definitions to guide you towards aspects of another method that your team has not previously considered.
Journey Map vs. Experience Map
Think of an experience map as a parent to a journey map. A journey map has a specific actor (a singular customer or user of a product) and specific scenario (of a product or service), while an experience map is broader on both accounts — a generic human undergoing a general human experience.
The experience map is agnostic of a specific business or product. It’s used for understanding a general human behavior; in contrast, a customer journey map is specific and focused on a particular business or product.
For example, imagine the world before the ridesharing market existed (Uber, Lyft, Bird, or Limebike, to name a few). If we were to create an experience map of how a person gets from one place to another, the map would likely include walking, biking, driving, riding with a friend, public transportation, or calling a taxi. Using that experience map we could then isolate pain points: unknown fares, bad weather, unpredictable timing, paying in cash, and so on. Using these pain points, we would then create a future journey map for specific product: how does a particular type of user call a car using the Lyft app?
Journey Map vs. Service Blueprint
If journey maps are the children to experience maps, then service blueprints are the grandchildren. They visualize the relationships between different service components (such as people or processes) at various touchpoints in a specific customer journey.
Think of service blueprints as a part two to customer journey maps. They are extensions of journey maps, but instead of being focused on the user (and taking the user’s viewpoint), they are focused on the business (and take its perspective).
For the Lyft scenario above, we would take the journey map and expand it with what Lyft does internally to support that customer journey. The blueprint could include matching the user to a driver, contacting the driver, calculating fares, and so on.
Journey Map vs. User Story Map
User stories are used in Agile to plan features or functionalities. Each feature is condensed down to a deliberately brief description from a user’s point of view; the description focuses on what the user wants to do, and how that feature will help. The typical format of a user story is a single sentence: “As a [type of user], I want to [goal], so that [benefit].” For example, “As a checking account holder, I want to deposit checks with my mobile device, so that I don’t have to go to the bank.”
A user story map is a visual version of a user story. For example, take the user story above (“As a checking account holder, I want to deposit checks with my mobile device, so that I don’t have to go to the bank.”) and imagine writing out the different steps that the team plans for the user to take when using that functionality. These steps could be: logging in, beginning deposit, taking picture of check, and entering transaction details. For each step, we can document required features: enabling camera access, scanning check and auto filling numbers, and authorizing signature. In a user story map, these features are written on sticky notes, then arranged based on the product release that each functionality will be added to.
While, at a glance, a user story map may look like a journey map, journey maps are meant for discovery and understanding (think big picture), while user story maps are for planning and implementation (think little picture).
Although a journey map and user story map may contain some of the same pieces, they are used at different points of the process. For example, imagine our journey map for Lyft indicated that a pain point appeared when the user was in a large group. To address it, the team may introduce a multicar-call option. We could create a user story map to break this feature (multicar call) into smaller pieces, so a product-development team could plan release cycles and corresponding tasks.
The benefits of journey maps (and most other UX mappings ) are two-fold. First, the process of creating a map forces conversation and an aligned mental model for the whole team. Fragmented understanding is a widespread problem in organizations because success metrics are siloed; it is no one’s responsibility to look at the entire experience from the user’s standpoint. This shared vision is a critical goal of journey mapping, because, without it, agreement on how to improve customer experience would never take place.
Second, the shared artifact resulting from the mapping can be used to communicate an understanding of your user or service to all involved. Journey maps are effective mechanisms for conveying information in a way that is memorable, concise, and that creates a shared vision. The maps can also become the basis for decision making as the team moves forward.
Journey mapping is a process that provides a holistic view of the customer experience by uncovering moments of both frustration and delight throughout a series of interactions. Done successfully, it reveals opportunities to address customers’ pain points, alleviate fragmentation, and, ultimately, create a better experience for your users.
Additional articles are available, discussing:
- When to create customer journey maps
- The 5-step process
- Journey mapping in real life
Free Downloads
Related courses, journey mapping to understand customer needs.
Capture and communicate UX insights across complex interactions
Omnichannel Journeys and Customer Experience
Create a usable and cohesive cross-channel experience by following guidelines to resolve common user pain points in a multi-channel landscape
Interaction
Generating Big Ideas with Design Thinking
Unearthing user pain points to drive breakthrough design concepts
Related Topics
- Customer Journeys Customer Journeys
- Design Process
Learn More:
Please accept marketing cookies to view the embedded video. https://www.youtube.com/watch?v=2W13ext26kQ
Customer Journey Mapping 101

Interactive UX Maps 101
Megan Brown · 4 min

Journey Mapping: 2 Decisions to Make Before You Begin
Kate Kaplan · 3 min

Scenario Mapping for Design Exploration
Kim Salazar · 3 min
Related Articles:
The 5 Steps of Successful Customer Journey Mapping
Kate Kaplan · 6 min
Parking Lots in UX Meetings and Workshops
Sarah Gibbons · 5 min
When and How to Create Customer Journey Maps
User Experience vs. Customer Experience: What’s The Difference?
Kim Salazar · 5 min
Journey Mapping: 9 Frequently Asked Questions
Alita Joyce and Kate Kaplan · 7 min
Luxury Shopping User Groups and Journeys
Kate Moran · 14 min

IMAGES
VIDEO
COMMENTS
Journey mapping involves the creation of visual narrative timelines depicting the multidimensional relationship between a consumer and a service. The use of journey maps in medical research is a novel and innovative approach to understanding patient healthcare encounters. To determine possible applications of journey mapping in medical research and the clinical setting.
An acceleration of patient journey mapping research was observed, with 76.5% (n = 62) of articles published since 2015. Diverse mapping approaches were identified. ... Consolidated criteria for reporting qualitative research (COREQ): A 32‐itm checklist for interviews and focus groups. International Journal for Quality in Health Care, ...
Complement Qualitative Research with Quantitative Data. Aside from highlighting potential problem areas to help shape qualitative research efforts at the onset of a customer-journey mapping initiative, quantitative data can also add another layer of evidence to your insights to make your narrative even more compelling.
Breast cancer is the most common cancer and the one that associates the highest mortality rates among Spanish women, with 32,953 new cases estimated to be diagnosed in Spain in 2020 [ 1 ]. Thanks to early diagnosis and therapeutic advances, survival has increased in recent years [ 2 ]. The 5-year survival rate is currently around 85% [ 3, 4 ].
The use of journey maps in medical research is a novel and innovative approach to understanding patient healthcare encounters. Objectives: To determine possible applications of journey mapping in medical research and the clinical setting. Specialist palliative care services were selected as the model to evaluate this paradigm, as there are ...
This chapter explores how journey mapping as a qualitative research method allows young people on the edge of society to reflect upon and make sense of their engagement in different youth projects. The method provides the young people with the time, space and means to explore the participatory activities they engage in and to map the multiple ...
This unique qualitative study noted many promising applications of the journey mapping suitable for extrapolation outside of the palliative care setting as a review and audit tool, or a mechanism for providing proactive patient-centred care. Background Journey mapping involves the creation of visual narrative timelines depicting the multidimensional relationship between a consumer and a service.
Conclusions: This unique qualitative study noted many promising applications of the journey mapping suitable for extrapolation outside of the palliative care setting as a review and audit tool, or a mechanism for providing proactive patient-centred care. ... Objectives: To determine possible applications of journey mapping in medical research ...
This chapter explores how journey mapping as a qualitative research method allows young people on the edge of society to reflect on and make sense of their engagement in different youth projects. The method provides young people with the time, space and means to explore the participatory activities they engage in and to map the multiple ways ...
Google Analytics is a great option for quantitative website or app data: it's both powerful and relatively easy to set up and navigate. Use Hotjar's Google Analytics integration to go deeper and gather both qualitative and quantitative insights to inform your customer journey map. 6. Quantitative surveys.
Journey mapping requires qualitative research and your visualization should be based on real data. You need to observe customers' real behavior and hear from them first hand. Usability methods like contextual inquiry, interviews, and diary studies are great for collecting the insights needed for mapping customer journeys.
The utilisation of journey mapping has the potential to address these inconsistencies and to our knowledge, this research is the first of its kind. Journey mapping is a relatively new approach in medical research that has been adapted from customer service and marketing research . It is gaining increasing recognition for its ability to organise ...
Journey mapping is a research methodology focused on the user experience and is typically employed to better understand consumer behavior, ... actually say and is well-suited to descriptively assess participants experience with HRM. 38 To encourage quality in qualitative research and to triangulate findings, initial open codes were assigned to ...
An acceleration of patient journey mapping research was observed, with 76.5% (n = 62) of articles published since 2015. Diverse mapping approaches were identified. ... 8.3%) used or identified specific reporting guidelines, including the Standards for Reporting Qualitative Research (Rushton et al., 2020), the COREQ guidelines (Fennelly et al., ...
At the heart of a journey map's narrative is what the user is doing, thinking, and feeling during the journey. These data points should be based on qualitative research, such as field studies, contextual inquiry, and diary studies. The granularity of representation can vary based on the purpose of the map.
RESEARCH Open Access Journey mapping as a novel approach to healthcare: a qualitative mixed methods study in palliative care Stephanie Ly1, Fiona Runacres1,2,3 and Peter Poon1,2* Abstract Background: Journey mapping involves the creation of visual narrative timelines depicting the multidimensional relationship between a consumer and a service.
Cork, T23 T2VY, Ireland. +1 888 917 7480. Hours. As demand for Journey Mapping continues to grow, discovery / exploratory research tools like Indeemo offer UX researchers and Designers the ability to leverage remote research methods such as Digital Ethnography to surface context rich, in-the-moment experience insights.
Qualitative research is the go-to standard for product development, brand insights and user testing, as well as my favorite use: developing consumer journey maps. There is simply no other way to ...
The Approach. Journey mapping is conducted mainly through qualitative research. It requires the involvement of both key stakeholders in the organization and customers/users, particularly for customer journey mapping. The development of journey maps is often conducted in different phases and includes meeting with stakeholders, gathering ...
Surveys consisted of 5 open-ended and 36 multiple-choice items mapped to five journey mapping domains: Discover, Search, Assess, Decide, Assist. Descriptive statistics for survey items were generated in addition to a visual representation of a Persona and associated journey map for HRM. Content analysis was performed on open-ended responses ...
Journey mapping is a research methodology focused on the user experience and is typically employed to better understand consumer behavior, preferences, and experiences with products or services. 28,29 Journey mapping enables visualization of the overall experience of an individual from their perspective, including feelings, motivations, and ...
Often with a journey mapping project, the key component is the specific output of the research - a highly visualized and succinct 1-page map to represent the journey. This visualization tells the story tightly and clearly to help build empathy for your consumers, identify how to engage with them, and optimize their experiences at the various ...
Definition: A journey map is a visualization of the process that a person goes through in order to accomplish a goal. In its most basic form, journey mapping starts by compiling a series of user actions into a timeline. Next, the timeline is fleshed out with user thoughts and emotions in order to create a narrative.