Your Account
Manage your account, subscriptions and profile.
MyKomen Health
ShareForCures
In Your Community
In Your Community
View resources and events in your local community.
Change your location:

Susan G. Komen®
One moment can change everything.

Susan G. Komen Blog
Stories about breast cancer that can inspire and inform.
Blog | Newsroom
My Cancer Journey

My Breast Cancer Journey
Hanna-Marie lives in Houston, Texas. She was diagnosed with breast cancer in December 2020. This is her story in her words.
I was diagnosed with a type of breast cancer called triple positive invasive ductal carcinoma on Dec. 15, 2020. I had no family history.
I found a mass in mid-September 2020 that felt like a pencil eraser. During this time, I was having horrible nausea and pelvic pain weeks after my cycle and ovulation period. This was out of the norm for me, even during my cycle. I was one of the lucky ones with no cramps or nausea.
I went to the OBGYN in late September to discuss the nausea and pelvic pain and totally forgot to discuss the mass. I received a pelvic ultrasound and was told there weren’t any abnormalities. My well women’s exam was due in late October, so I waited until then to alert my doctor about the mass. Her saying is, “If you feel something, we without a doubt do a mammogram.” I’m 35 years old, so I had never received a mammogram before.
Due to work schedule and scheduling with the imaging center, I didn’t get the mammogram until November 2020. I received a mammogram and a breast ultrasound. Three masses were discovered that required a biopsy, which I had in early December. A week later the biopsy results revealed:
- Estrogen receptor-positive
- Progesterone receptor-positive
- Her2-positive
The best advice I can give to someone newly diagnosed is to:
- Take it one step at a time. It can be overwhelming to hear you need chemotherapy, surgery, radiation therapy. After treatment, there’s hormone therapy for years. Don’t think about the next step until it’s time.
- Take time to review your health insurance benefits—you would be surprised at what things can be covered with a cancer diagnosis. For instance, acupuncture wasn’t covered with my plan unless there was proof of a chronic illness such as cancer.
- Trust your gut and don’t be forced into something that doesn’t feel right for you.
- Advocate for yourself—no one else will take care of you like you can. Speak out of something isn’t right and remember: closed mouths don’t get fed.
- Don’t be scared to ask questions!
As of August 2021, I am Cancer Free!
Statements and opinions expressed are that of the individual and do not express the views or opinions of Susan G. Komen. This information is being provided for educational purposes only and is not to be construed as medical advice. Persons with breast cancer should consult their healthcare provider with specific questions or concerns about their treatment.
Related Stories


Human Answers to Your Cancer Questions
Welcome to The Patient Story, where you can find hope, guidance, and a supportive community. Explore insights on navigating life after a cancer diagnosis, discover promising treatments, and connect with people who truly understand what you're experiencing. Remember, you're not alone – we're here to help you through this journey.
Welcome to The Patient Story, where you can find hope, guidance, and a supportive community. Explore real patient symptoms, tests, treatments and how to manage treatment side effects.
Remember, you’re not alone – we’re here to help you through this journey.

Ashley’s Stage 4 Rare Adrenal Cancer Story

Samantha’s Cervical Cancer Story

Tracy’s Stage 2B Colorectal Cancer Story

Joe’s Rare Desmoplastic Small Round Cell Tumors (DSRCT) Story
You are not alone.
This time in your life can be overwhelming. Allow us to do some of the work for you. Sign up for our e-newsletter to find out what the cancer journey is really like – from the people who have lived it.

Navigating Your Life with Cancer
Not sure where to begin? We can help. Learn about first symptoms, treatment decisions, questions to ask your doctor, and navigating life with cancer.
Patient Events - Virtual & In-Person
Get your cancer questions answered in real time by leading experts and patients. Explore upcoming and past patient live discussions. Plus, easily sort by cancer type.
Insights by Cancer Type
Detailed stories direct from cancer patients and survivors to help anyone facing a cancer diagnosis of their own, tailored by cancer type.
Share Your Story
Inspire others and join our community today.
Share your cancer journey and make a difference. Whether you’re a cancer survivor, patient, caregiver, or advocate, your story is important and matters. Sharing your story with others can inspire hope, educate and create a lasting impact.
The Patient Story Partners
Join our community.
Get the latest cancer stories, helpful resources, and personalized advice directly to your inbox.
Copyright 2024 © The Patient Story
For cancer patients and caregivers.
Quick Links
Additional Links
Answers. Strength. Confidence. TM
Be ready to take on cancer before, during, and after treatment
Getting screened to help find cancer
Knowing which screenings you need and when to get them can be helpful in finding cancer earlier, before it has spread. See cancer screening recommendations by age
Preparing for cancer surgery
Your doctor may recommend surgery to help treat your cancer, as well as additional treatment before or after surgery. Learn about surgery and how it may fit into your treatment plan
Building your cancer care team
Understand the types of health care providers who may be able to help you through your cancer and treatment journey. Get familiar with what different team members do
Understand your type of cancer
A greater understanding of the different types of common cancers can help you or someone you love manage the journey.
Life with cancer
Sharing your cancer diagnosis.
Cancer is hard to deal with all alone. You have control over if, when, and how much you share about your diagnosis.

Preparing for your first cancer treatment
From Harvard Health Publishing
You can take the edge off your first day of treatment by focusing on stress-relieving techniques and being as comfortable as possible.

How to manage limited energy
Fatigue can be expected with some treatments, but it could also be a serious side effect of your treatment. The first thing you should do is talk with your doctor when you experience fatigue.
Finding a support group
Even if your family and friends are hugely empathetic, a cancer-specific support group may give you even more freedom to discuss your concerns.
Questions to ask your doctor
Use these questions to help prepare for doctor visits throughout your journey.
Sign up for updates
Be the first to know when new information and articles become available.
You are leaving Understand Cancer Together
The link you selected will take you to a site outside of Merck.
Merck does not review or control the content of any non-Merck site. Merck does not endorse and is not responsible for the accuracy, content, practices, or standards of any non-Merck site.
Together we are beating cancer
- Cancer types
- Breast cancer
- Bowel cancer
- Lung cancer
- Prostate cancer
- Cancers in general
- Clinical trials
- Causes of cancer
- Coping with cancer
- Managing symptoms and side effects
- Mental health and cancer
- Money and travel
- Death and dying
- Cancer Chat forum
- Health Professionals
- Cancer Statistics
- Cancer Screening
- Learning and Support
- NICE suspected cancer referral guidelines
- Make a donation
- By cancer type
- Leave a legacy gift
- Donate in Memory
- Find an event
- Race for Life
- Charity runs
- Charity walks
- Search events
- Relay for Life
- Volunteer in our shops
- Help at an event
- Help us raise money
- Campaign for us
- Do your own fundraising
- Fundraising ideas
- Get a fundraising pack
- Return fundraising money
- Fundraise by cancer type
- Set up a Cancer Research UK Giving Page
- Find a shop or superstore
- Become a partner
- Cancer Research UK for Children & Young People
- Our Play Your Part campaign
- Brain tumours
- Skin cancer
- All cancer types
- By cancer topic
- New treatments
- Cancer biology
- Cancer drugs
- All cancer subjects
- All locations
- By Researcher
- Professor Duncan Baird
- Professor Fran Balkwill
- Professor Andrew Biankin
- See all researchers
- Our achievements timeline
- Our research strategy
- Involving animals in research
- Research opportunities
- For discovery researchers
- For clinical researchers
- For population researchers
- In drug discovery & development
- In early detection & diagnosis
- For students & postdocs
- Our funding schemes
- Career Development Fellowship
- Discovery Programme Awards
- Clinical Trial Award
- Biology to Prevention Award
- View all schemes and deadlines
- Applying for funding
- Start your application online
- How to make a successful applicant
- Funding committees
- Successful applicant case studies
- How we deliver research
- Our research infrastructure
- Events and conferences
- Our research partnerships
- Facts & figures about our funding
- Develop your research career
- Recently funded awards
- Manage your research grant
- Notify us of new publications
- Find a shop
- Volunteer in a shop
- Donate goods to a shop
- Our superstores
- Shop online
- Wedding favours
- Cancer Care
- Flower Shop
- Our eBay store
- Shoes and boots
- Bags and purses
- We beat cancer
- We fundraise
- We develop policy
- Our global role
- Our organisation
- Our strategy
- Our Trustees
- CEO and Executive Board
- How we spend your money
- Early careers
- Your development
Cancer News
- For Researchers
- For Supporters
- Press office
- Publications
- Update your contact preferences
- About cancer
- Get involved
- Our research
- Funding for researchers
The latest news, analysis and opinion from Cancer Research UK
- Science & Technology
- Health & Medicine
- Personal Stories
- Policy & Insight
- Charity News
A journey through the cancer pathway
A road to longer, better lives
By Amy Warnock

Nearly 1 in 2 of us will get cancer in our lifetimes.
And that statistic applies to Alex too - our fictional character in this story.
Alex is 47 years old and lives in Sheffield. Alex loves playing tennis, catching up on the latest tv series, and meeting up with friends for a drink and a board game at their local pub.
Like many of us, Alex has had family members affected by cancer and knows first-hand how cancer can impact on someone’s life.
While we have made huge progress on cancer in the past 50 years, we still have a long way to go.
At the moment, the UK lags behind other comparable countries when it comes to cancer survival. And the challenge is only growing.
So let’s follow Alex’s journey through their cancer diagnosis and treatment and look at some of the barriers they encounter along the way.
But while these barriers might exist for now, they can be overcome. So we’ll also look at how government action could transform the cancer pathway and lead to more people living longer, better lives.
Prioritising prevention
As with everyone, Alex’s cancer journey actually starts before their cancer diagnosis. It starts with how Alex goes about living their everyday life.
And that’s because around 4 in 10 UK cancers are preventable.
So, if we can prevent cancers from developing in the first place, we can avoid the need to begin a journey on the cancer pathway.

Image source: Shutterstock/Markus Mainka
The picture now
Let’s take lung cancer as an example. It’s the third most common cancer in the UK, and every year around 49,200 people are diagnosed with the disease.
The majority of lung cancer cases are caused by smoking, which means they are preventable.
And it’s not just lung cancer. Smoking causes at least 15 types of cancer, as well as numerous other health conditions. Around 125,000 people in the UK are killed by tobacco each year - this includes smoking, second-hand smoke and chewing tobacco.
Smoking is also the biggest driver of the difference in life expectancy between the least and most affluent populations in the UK.
Alex has smoked since the age of 17, and like most people who smoke they want to give up. But because of the addictive nicotine in cigarettes, Alex has struggled.
But it’s not just smoking. Obesity and overweight is the second biggest cause of cancer in the UK and is linked to 13 types of cancer. Obesity and overweight prevalence in the UK is increasing, affecting more than 6 in 10 adults.
Drinking alcohol also increases cancer risk and the UK Chief Medical Officer's drinking guidelines advise against regularly exceeding more than 14 units of alcohol spread over a week. But there is no completely safe level of drinking, so the less you drink the better for your health.
The good news is that we can do something about these risk factors. And if we want to reduce the burden of cancer in the UK, that begins with trying to prevent it.

What can change
Put simply. if we can prevent more cancers we can save more lives.
And to do this we need strong government action.
Tackling smoking alone, to ensure that England meets its Smokefree target (that’s 5% or less of the adult population smoking) across all socio-economic groups, would prevent around 26,600 cancer cases by 2040.
And fortunately we could already be on our way to making this a reality. Recently, the UK Government announced that it will introduce legislation to raise the age of sale for tobacco , ensuring no one currently aged 14 or under can ever be legally sold cigarettes or other tobacco products. But we’re not done yet, we need to see this legislation passed, and adequate funding for services to help people stop smoking.
It’s changes like this that could prevent people like Alex ever taking up smoking in the first place, and maybe also prevent their cancer.
But this alone won’t be enough. To prevent even more cancer cases, we need to see more measures introduced to reduce the prevalence of smoking, overweight and obesity, and drinking alcohol above recommended limits in the UK.
Image captions

Image source: Shutterstock/Variety beauty background
Optimising screening
If we can’t prevent cancer, the next best thing is diagnosing it early.
That’s because by diagnosing cancers earlier we can ensure that people have more treatment options and the best chance of survival.
Image source: Shutterstock/Anamaria Meija
The UK has been focusing on early diagnosis for some time, and the NHS have a target of diagnosing 75% of cancer patients early (at stage 1 or 2) by 2028, but it is currently not on track to achieve this.
As it stands, far too many cancers are still diagnosed at stage 4, when there are limited treatment options and prognosis is often poor.
Around 1 in 5 cancer cases in England are diagnosed through emergency routes, which is associated with worse outcomes and worse patient experience. This needs to change.
A key way in which we can diagnose cancers earlier is through screening programmes , where people without symptoms are tested for early signs of cancer. The UK currently has three cancer screening programmes, for bowel, breast and cervical cancer.
But at present only 6% of cancers are diagnosed through screening, so we need to optimise and expand on these programmes to ensure that the screening programmes are working as hard as they can to help save lives.

Image source: Shutterstock/Xdbzxy
We know there isn’t a silver bullet to achieving earlier diagnosis across all cancer types. But there is a big potential for innovation in cancer screening.
The UK breast, cervical and bowel screening programmes save over 5,000 lives every year. But if we increase the uptake of these programmes across England to around 80%, we estimate that we can diagnose an extra 4,000 cases of cancer per year.
And there are also exciting new developments on the horizon.
In June this year, the UK Government announced the roll out of a new targeted lung cancer screening programme for people in England aged 55-74 who either smoke or used to smoke.
By delivering this national lung cancer screening programme we estimate that, with a 50% take up, around 1,900 lives could be saved in the UK each year.
Having smoked for a long time, a screening programme like this could have had a big impact for Alex, as it could have led to their cancer being diagnosed earlier, when there are more treatment options available.
The UK Government now need to ensure that the lung cancer screening programme is quickly implemented across England, and relevant ministers in the devolved nations should also commit to rolling out lung screening in their countries as quickly as possible.

Image credit: Rhoda Baer/National Cancer Institute
Waiting for a diagnosis
Lung cancer screening wasn’t available for Alex yet, so instead their journey to receiving a diagnosis starts when they notice some changes.
Alex first suspects that something isn’t quite right when they notice a new cough that won’t go away. So Alex goes to their GP, who gives them an urgent referral for a chest X ray.
After the X ray, Alex is referred for further tests.
And this is where we run into one of the biggest hurdles on the pathway. Cancer waiting times.

Image credit: National Cancer Institute
Getting an urgent suspected cancer referral is an incredibly stressful time, both for Alex, and their friends and family. So it should be a priority to make sure that this experience is as quick as possible.
But at the moment this isn’t happening. Performance related to cancer waiting times are at a near all-time low.
NHS England has set cancer waiting times targets , but over the past few years, these have consistently been missed.
In England, 85% of patients should start their treatment within 62 days of an urgent cancer referral. But the 62-day standard has been missed since 2015, meaning over 141,000 patients waited longer to start treatment than if the target had been met consistently.
In 2021, the new Faster Diagnosis Standard (FDS) was introduced in England, which stipulates that patients should have their cancer ruled out or receive a diagnosis within 28 days. Although the implemented target of 75% is well below the original target of 95%, this target has still not been met since its introduction.
So what can we do to make sure that people like Alex are diagnosed and treated as quickly as possible?
The main problem facing the NHS when it comes to cancer waiting times is resource, particularly when it comes to diagnosing cancer.
Fixing the cancer workforce isn’t easy, but it’s doable.
The UK Government made a good start this year by publishing their Long-Term Workforce Plan . But they need to build on this plan and commit funding to ensure that it delivers the cancer workforce that the country needs.
Importantly, as well as addressing staff and resource shortages, action needs to be taken to improve NHS workforce retention. There are proven interventions to boost retention, including access to training and professional development opportunities, flexible working and wellbeing support. Using interventions such as these, the UK Government need to fully commit to turning the tide on the numbers of experienced staff leaving the workforce.
If we can improve NHS resource and retention, and begin to meet cancer wait time targets, this could have a huge impact on patients.
By meeting the FDS target at 95%, rather than the current target of 75%, we estimate that around 49,000 extra people per month could receive a cancer diagnosis or have cancer ruled out within the proposed 28-day FDS window. Not only does that mean that cancers can be treated faster, it means less time spent worrying for people and their families.
But it’s not just cancer waits that can be fixed. With new challenges on the horizon, such as an ageing population and more complex treatments, by addressing NHS staffing shortfalls across the cancer workforce, the government can ensure that the UK have a workforce fit for the future of cancer care.

Image source: Shutterstock/Altrendo Images
Innovating new treatments
Because of staff shortages, Alex has had to wait longer than 28 days to receive a diagnosis of lung cancer. And now they are about to begin treatment.
Alex’s treatment plan involves treatment with gefitinib. This is because Alex’s cancer has a mutation in a gene called EGFR, which is involved in helping cells grow and divide.
Gefitinib can specifically target and block EGFR activity in cancer cells
Targeted cancer treatments, such as gefitinib, have made a huge difference to people with cancer over the last 50 years. They work by targeting specific differences between cancer cells and healthy cells which help the cancer to survive and grow. This means they’re less likely to damage healthy tissue.
But the journey of developing new treatments and getting them to patients is a long one.
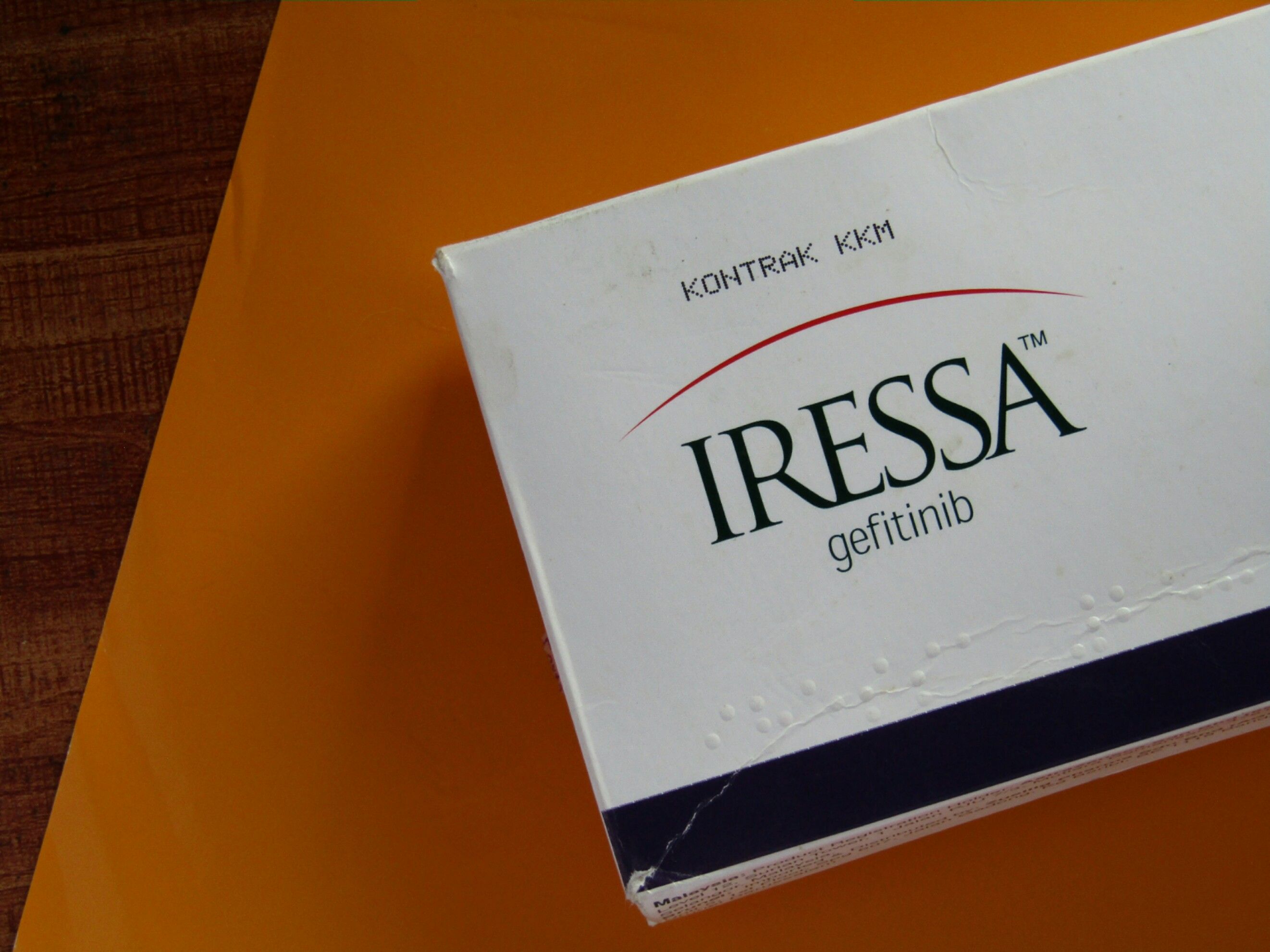
Image source: Shutterstock/Syazwani Pardi
The path to new treatments begins with a strong research workforce. But there are concerns over the sustainability of the biomedical research funding landscape over the next decade.
With current government levels of funding and charity income remaining static, we estimate there will be a shortfall of between £1-2bn in cancer research investment over the next decade.
But it’s not just a problem of research funding. We also need to tackle system-wide issues to ensure that research careers are attractive and accessible for everyone, remove the barriers that may stop international talent coming to the UK to do their research, and build a diverse research community.
We’re also facing barriers when it comes to translation – getting new discoveries from the lab to a place where they can benefit patients. All stages of the UK translation pipeline, from the early stages of clinical research to test safety and effectiveness through to adoption and implementation, need to be strengthened to ensure that patients can see the impact of new tests and treatments.

What can change
Of all publicly funded cancer research in the UK, around 38% comes from the government and around 62% comes from charities.
The US Government funds over 5 times more cancer research per capita than the UK Government...
...and the Norwegian Government funds over 2.5 times more.
The government needs to commit to making research and development (R&D) spending a priority.
The UK can remain at the forefront of cancer research, but it will take sustained, long-term investment across the research sector.
Investment in research not only has huge benefits for patients, but also for our economy. In 2020/21 there was £1.8bn invested into cancer research. This generated more than £5bn of economic impact .
As well as committing to prioritising funding, the government also need to ensure that barriers to cross-border research are minimised, as well as reducing potential barriers, such as high upfront visa costs, to encourage an international and diverse research workforce in the UK. Collaboration across the globe is key to solving cancers biggest problems.
The government also needs to facilitate translation in the UK, streamlining the process of bringing innovations to the health system and encouraging investment to fund the early stages of translation.
With a world-leading research sector, and a streamlined translation process, we can ensure that we continue to make groundbreaking discoveries and develop new cancer treatments for patients just like Alex.

Image source: Shutterstock/Nico El Nino
Leading on cancer
Thanks to getfitinib, Alex is able to live a longer, better life. But that’s not the case for everyone with cancer.
As we can see from Alex’s journey, the cancer pathway for a patient can be long, complex and fraught with obstacles. These obstacles will vary widely depending on the patient, but importantly many of them are fixable.
Fixing them won’t be easy, but it is possible. Cancer survival in the UK has doubled over the last 50 years, and with the right leadership we can make sure that the next 50 years are just as impactful.
The upcoming general election needs to be a turning point for people affected by cancer.
We need to see strong leadership on cancer in the UK, to ensure a long-term focus on cancer. This approach needs to bring together discovery, translation, cancer prevention, detection, diagnosis and treatment, health system investment and reform, to ensure that more of us are able to live longer, better lives.
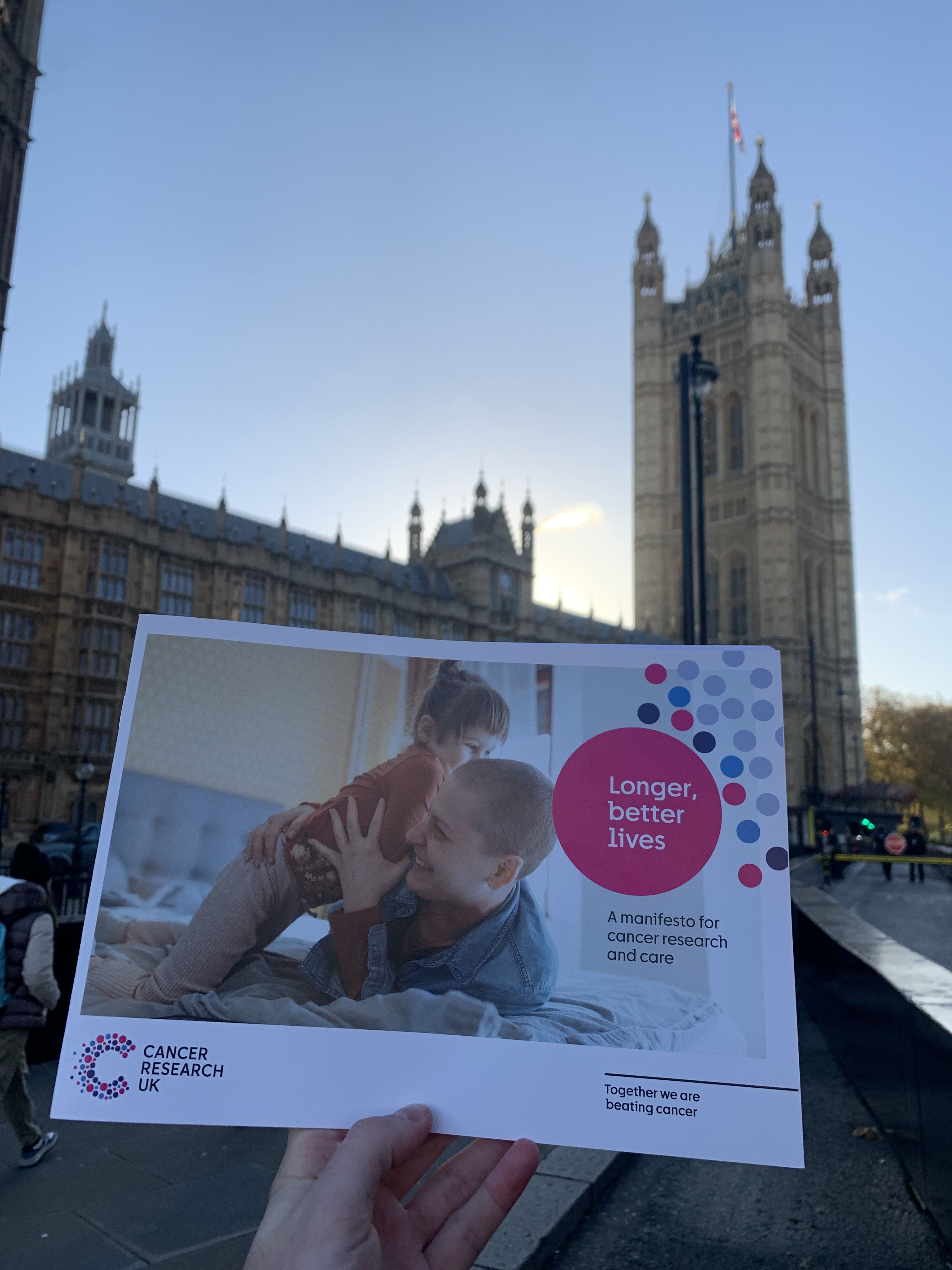
And that’s why we’ve launching Longer, better lives: A manifesto for cancer research and care . Our manifesto outlines the steps the next UK Government must take to make transforming cancer outcomes a reality. And if you agree, you can join us in telling party leaders to back our calls for longer, better lives.

- The Journey
Patients, caregivers and loved ones rely on each other on the path to wellness. The Journey is a blog that addresses the unique hurdles each person faces.
- For Patients
- For Caregivers
- Questions to Ask My Doctor
- 30 Stories in 30 Days™
Read cancer survivors’ stories. Get great advice and inspiration from others on a similar journey.
- Share Your Story
- Just for Kids
Join Hank the Monkey with his friends as they learn about cancer and how they cope with it.
- For Parents
- For Kids & Teens
Recent Posts
- Advice for Patients
- Oral Cancer Awareness
- Thyroid Cancer
- Post Treatment
- Stress Management
- Low-iodine Diet
- Advice for Parents
- Oral Cancer
- After Surgery
- Anxiety & Fear
- Thyroid Cancer Awareness
A curated collection of instructive books.
Download a free cookbook.
Access guides on cancer diagnostics & treatments.
Easily search and match to clinical trials.
Get the definition of cancer-related terms.
Video content with easy-to-digest information.
Browse a list of devices for patients undergoing cancer treatment.
Smartphone apps, online forums & advocacy groups.
Interact with other people who share your journey.
Download the thyroid fact sheet.
Danielle’s Story (Update)
Category: the journey.
Patients and caregivers rely on each other on the path to wellness. The Journey is a blog that addresses the unique hurdles people face on their cancer journey.
How to Decode Your Thyroid Function Tests Now

Is your thyroid healthy? Find out with our complete guide to understanding T3, T4, and TSH tests. Learn more so you can decode your thyroid results today! Continue reading How to Decode Your Thyroid Function Tests Now
- Post date June 6, 2024
- Tags Advice for Patients , Cancer Testing , Diagnosis , Featured , Thyroid Cancer
Your Post-Surgery Guide to a Soft Food or Liquid Diet

Struggling after surgery? Ease your post-surgery recovery with our soft food guide. Discover great diet tips and learn some simple, soothing meal recipes today! Continue reading Your Post-Surgery Guide to a Soft Food or Liquid Diet
- Post date May 23, 2024
- Tags Cancer Recovery , Featured , Post Treatment , Recipes
How to Start a Gratitude Journal as a Healing Exercise

Cancer survivors can cultivate this secret weapon for mental and physical well-being. Learn how to start your gratitude journal now and transform your outlook. Continue reading How to Start a Gratitude Journal as a Healing Exercise
- Post date May 9, 2024
- Tags Advice for Caregivers , Featured , Resources
Spotlight on Cancer Research Month This May

Learn about the research and collaboration driving cancer advancements. Read survivor stories and see how teamwork is transforming treatment options. Continue reading Spotlight on Cancer Research Month This May
- Tags Awareness Month , Cancer Research , Featured
The Role of Caregivers and 14 Amazing Resources to Help Them

Dive into our guide on the vital role of caregivers in the cancer journey. Explore the many resources available to help caregivers along the way. Continue reading The Role of Caregivers and 14 Amazing Resources to Help Them
- Post date February 29, 2024
Surviving Thyroid Cancer: Awesome Celebrity Stories of Hope

Get inspired by courageous stars like Missy Elliott, Sophia Vergara & Sia overcoming thyroid challenges. Their journeys could change your perspective. Continue reading Surviving Thyroid Cancer: Awesome Celebrity Stories of Hope
- Post date February 8, 2024
- Tags Cancer Survivors , Featured , Thyroid Cancer
Boost Your Cancer Fight: Quit Smoking and Alcohol Now!

Did you know you might double your chances of beating cancer by quitting smoking and alcohol today? Explore empowering strategies for a healthier life! Continue reading Boost Your Cancer Fight: Quit Smoking and Alcohol Now!
- Post date February 1, 2024
- Tags Advice for Patients , Resources , Treatment Options
5 Questions: How to Navigate Life After Thyroid Surgery

Navigate your journey through thyroid cancer surgery with confidence! Discover the top 5 questions to ask your doctor for a healthier recovery. Continue reading 5 Questions: How to Navigate Life After Thyroid Surgery
- Post date January 18, 2024
- Tags Advice for Patients , After Surgery , Featured , Post Treatment , Questions to Ask My Doctor , Thyroid Cancer
9 Useful Positive Coping Strategies After a Recent Diagnosis

Boost your quality of life with effective coping strategies for cancer! Discover positive techniques today to enhance recovery and well-being. Continue reading 9 Useful Positive Coping Strategies After a Recent Diagnosis
- Post date January 4, 2024
- Tags Advice for Patients , Communicating , Stress Management
Corporate Supporters

Help us keep this resource free.
Support the THANC Foundation, the creators of this resource.
Make a tax-deductible donation to support the THANC Foundation, the creators of the Thyroid, Head & Neck Cancer Guide.
Check out our blog: The Journey.
A little inspiration can go far.
A little inspiration can go far. Our blog addresses the unique hurdles each person faces.
Learn the Basics of Cancer
Find out things like what treatments are available and what happens if there's a recurrence.
The Cancer Basics section reveals things like how a diagnosis is reached, what treatments are available and what happens if there's a recurrence.
Read our Guide for Parents
Use the tools and advice inside and adapt them for your family.
Children and teenagers have unique interests and learn differently compared to adults. Parents can use the tools and advice inside and adapt them for their family.

Privacy Overview
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
The 5 Emotional Stages of People with Cancer
Common reactions, emotional stages, mental health side effects.
- Helping a Loved One
- When to Seek Care
Frequently Asked Questions
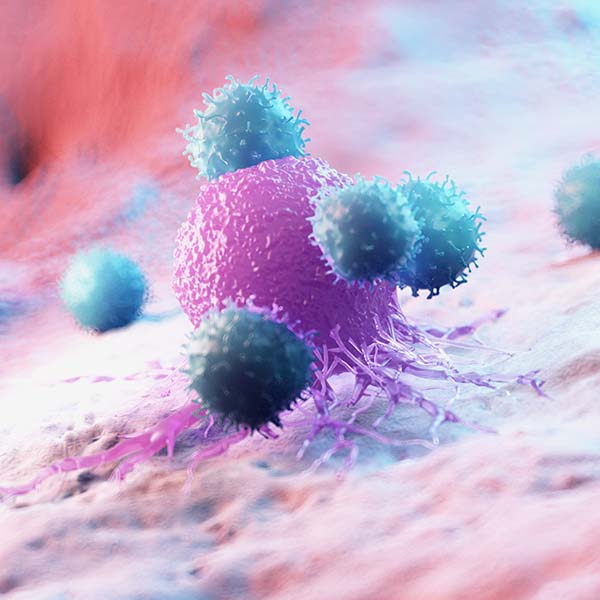
A cancer diagnosis can have a significant impact on the emotional health of you, your family, and your support system. You may experience fear, anxiety, sadness, anger and overwhelm. It’s completely normal to feel a wide range of emotions when facing a cancer diagnosis.
There are over 100 types of cancer, and an estimated 1.9 million people in the United States are diagnosed with cancer each year. Breast cancer, prostate cancer, and colorectal cancers account for nearly 50% of these cases.
FatCamera / Getty Images
When you are living with cancer, it's important to prioritize your emotional and physical health. Studies suggest that addressing the mental health concerns that people with cancer experience may lead to improved treatment outcomes and a better quality of life.
This article discusses the five emotional stages of cancer, how to cope, and how to help a loved one.
You may feel like you’re on an emotional rollercoaster after getting a cancer diagnosis. The range of emotions you feel can change daily, or even hourly.

Cancer Is an Emotional Experience
Though no two people will share the exact same emotions when facing cancer, common reactions to a cancer diagnosis include:
- Loneliness
Intense, varied emotions are common in people living with cancer—not just at the time of diagnosis, but at any point in your cancer treatment. You may grieve the loss of your good health, struggle with changes to your appearance, feel guilt over the impact your diagnosis has on your family, and worry about the future.
Developed by psychiatrist Elisabeth Kubler-Ross in 1969, the five stages of grief—commonly known as DABDA , which stands for "denial," "anger," "bargaining," "depression," and "acceptance"—may reflect the emotions you feel as you navigate your cancer journey. The DABDA model is a good tool to describe the emotional responses of people when they’re facing a life-changing illness or situation.
Although these stages are widely believed to happen in a linear fashion, these emotions can occur at any time, in any order, after a cancer diagnosis.
Getting a cancer diagnosis can be an overwhelming experience. The overwhelm may trigger feelings of disbelief, numbness, or shock. You may want to avoid thinking about it or pretend it isn’t happening. Denial is a common response to life-changing events and is a normal emotion for people with cancer. Denial will fade over time, and you will begin to experience other emotions concerning your diagnosis.
Anger is a natural emotional response to perceived threats. Though often not seen in a positive light, anger can be a good thing. When it comes to a cancer diagnosis, anger can be a vital part of the emotional process. It gives you a way to express your difficult emotions, like anxiety, fear, frustration, and helplessness.
It’s important to allow yourself to feel and express your anger in a healthy way rather than holding it all in. You may find it beneficial to talk about your anger with a trusted family member or friend (without taking it out on them), punch pillows, yell out loud in your car, write in a journal, or do a physical activity (e.g., dancing) to help you process your emotions.
Bargaining
In the bargaining stage, you may feel like your diagnosis is unfair and want to do anything to “fix” it and return to life pre-diagnosis. You may bargain with yourself or a higher power as a way of finding some control over the situation, and think things like, “If I get through this, I will never complain about anything again.” If your loved one has cancer, you may think, “If she survives this cancer, I will never again be angry at her.”
Bargaining and guilt often go hand in hand, and you may find yourself going through countless what-if scenarios, such as: What if I'd never smoked in my 20s? What if I'd never eaten junk food? What if I'd gone to the doctor six months earlier?
If you find yourself in an endless loop of bargaining, it may be helpful to talk through your emotions with a counselor or with peers in a cancer support group.
Depression is a common mental health condition that involves persistent feelings of sadness, loss of pleasure in previously enjoyed activities, and low energy. Depression can lead to changes in your sleeping and eating patterns, difficulty concentrating, and low self-worth.
Depression affects up to 1 in 4 people with cancer. Talk to your healthcare provider if these feelings persist for more than two weeks. They may recommend treatment to help manage your depression such as medication and/or counseling . Studies show that people with cancer who get treated for depression respond better to cancer treatments and have a higher quality of life.
Acceptance
Once you’ve given yourself the space to grieve and feel the emotions that come with a cancer diagnosis, it becomes easier to face your new reality head-on. This doesn’t mean you leave behind any difficult feelings or grief—rather, you learn to accept and find meaning in your current journey.
With acceptance comes hope. And there are plenty of reasons to feel hopeful—millions of people are cancer survivors . While there’s no evidence to suggest that a positive attitude can improve cancer treatment outcomes, there are still benefits to staying hopeful. A hopeful mindset is associated with stress reduction, lower blood pressure, and improved relationships.
Cancer Prognosis
A cancer prognosis is your healthcare provider’s best estimate of how your cancer will respond to treatment, how it will affect you, and what your chances of survival are. The type you have and the stage of cancer you're in, where the cancer is located in your body, your age, and how healthy you were before diagnosis all play a role in your prognosis.
It's important to remember that a prognosis is your cancer specialist's (oncologist) best guess and is not written in stone.
A cancer diagnosis can affect the mental health and well-being of people with cancer, their families, and caregivers.
Many people with cancer experience significant sadness and grieve the life they had before diagnosis. You may feel tired, have a reduced appetite, and find it difficult to get through your daily routine. This is normal, and it may take time for you to work through your feelings and accept your new way of life. Some cancer treatments may change your brain chemistry and increase the likelihood of depression.
Getting support from family members and friends or joining a cancer support group may help you process your emotions. If your feelings of depression persist, ask your healthcare provider about your options for treating depression. This may include medication and counseling.
Up to 45% of adults with cancer experience anxiety. Anxiety is feeling worried, afraid, tense, and/or unable to relax. Physical symptoms include a rapid heart rate, loss of appetite, nausea, dizziness, headaches, muscle pain, tightness in your chest, or changes in your sleep patterns.
It’s completely normal to feel anxious when you or your loved one is facing cancer. If you’re feeling anxious, it’s important to recognize this feeling and take the steps needed to manage how you feel.
Studies show that mindfulness-based activities (e.g., meditation, breathwork) are associated with a reduction of anxiety and depression in adults with cancer. Your doctor may suggest antianxiety medications and/or talk therapy to help manage anxiety.
How to Cope
Coping with cancer and the associated emotional toll is important. Though people cope with their emotions in different ways, you may find these strategies for coping helpful:
- Recognize and be honest about what you’re feeling.
- Talk about your feelings with a trusted loved one.
- Seek out community, such as a cancer support group.
- Eat a balanced, nutritious diet .
- Get plenty of sleep.
- Engage in physical activity (e.g., walking, swimming).
- Try relaxation techniques, such as meditation, mindfulness, breathwork, or yoga
- Write your feelings down in a journal.
- Look for positive experiences—whether that’s with a beloved pet, friends, or a solo activity that brings joy.
- Talk to your healthcare providers if your feelings of depression and/or anxiety persist.
How to Help
If your family member or friend has been diagnosed with cancer, you may be wondering what you can do to help. Here are some ideas on how to support a loved one with cancer :
- Listen : Ask how they’re feeling and provide a listening ear.
- Offer to help : Whether you cook meals, do their laundry, or provide transportation to their appointments, helping with day-to-day tasks is often appreciated.
- Treat them the same : Your loved one is the same person they were before the diagnosis, and treating them as you have in the past is a way to provide normalcy.
- Give them a cancer break : People with cancer often need a break from talking about all things cancer-related. Share interesting stories, some laughs, or sit down for a cozy movie night together.
- Learn about cancer : Taking the initiative to learn about your loved one’s cancer type and treatments is a way to show you care.
- Show up : Stay consistent with your relationship—call, text, or take time for visits to let them know you’re a reliable friend.
Remember that you can’t pour from an empty cup. If you are a caregiver, be sure to carve out time for self-care—being there for a loved one with cancer can take an emotional and physical toll on caregivers, too. Taking care of your own needs can give you the strength you need to continue providing support.
When to See a Healthcare Provider
If your emotions are affecting your day-to-day life or lasting a long time, your cancer care team can help. Ask your healthcare team for mental health support. Your oncologist may refer you to a counselor who can help you learn how to cope with your diagnosis. They may also prescribe medication, such as an antidepressant or antianxiety medications.
Receiving a cancer diagnosis is an emotionally overwhelming experience that can lead you to experience feelings of denial, anger, bargaining, depression, and eventually acceptance. However, the journey is not linear, and not everyone experiences each of these emotions.
That said, receiving a cancer diagnosis or learning your loved one has cancer can contribute to feelings of sadness, anxiety, and hopelessness. It's normal and okay to feel sad, but if you or a loved one is experiencing these emotions for an extended period of time and/or are having trouble coping, it doesn't hurt to ask for help.
A Word From Verywell
Coping with a cancer diagnosis—whether it is your own or a loved one’s—can take a psychological toll. Give yourself the space to acknowledge and express all of your feelings openly and honestly.
If you feel your emotional health is negatively affecting your daily life, talk to your healthcare provider. There is no shame in asking for help—even the strongest, most resilient people need support. Asking for mental health support is one of the best things you can do for yourself as you navigate your cancer journey.
Whether cancer can be cured depends on the type and stage of cancer, how a person responds to treatment, and other factors. A cure means that cancer has gone away with treatment and will never come back. Remission is when cancer has responded to treatment and all signs and symptoms have gone away. If a person remains in remission for five or more years, they may say they are cured.
Most types of cancer have four stages: stage 1, stage 2, stage 3, and stage 4 (sometimes written in Roman numerals as I, II, III, and IV). Some cancers have stage 0. Staging is a way to indicate cancer’s location, size, and whether or not it has spread (metastasized) either locally or farther from the original site. Staging helps doctors determine the best treatment plan (e.g., chemotherapy, surgery).
National Cancer Institute. What is cancer?
National Cancer Institute. Cancer stat facts: common cancer sites.
Mental Health America. Cancer and mental health.
National Cancer Institute. Cancer and feelings.
Stroebe M, Schut H, Boerner K. Cautioning healthcare professionals . Omega (Westport) . 2017;74(4):455-473. doi:10.1177/0030222817691870
Conley CC, Bishop BT, Andersen BL. Emotions and emotion regulation in breast cancer survivorship . Healthcare (Basel) . 2016;4(3):56. doi:10.3390/healthcare4030056
American Society for Clinical Oncology. Coping with anger.
Living Beyond Breast Cancer. Emotional stages of a breast cancer diagnosis.
National Institute of Mental Health. Major depression.
American Cancer Society. Depression.
Smith HR. Depression in cancer patients: Pathogenesis, implications and treatment (review) . Oncol Lett . 2015;9(4):1509-1514. doi:10.3892/ol.2015.2944
National Cancer Institute. Cancer and feelings.
National Cancer Institute. Understanding cancer prognosis .
National Behavioral Health Network. Mental health impacts of a cancer diagnosis.
Zhang MF, Wen YS, Liu WY, Peng LF, Wu XD, Liu QW. Effectiveness of mindfulness-based therapy for reducing anxiety and depression in patients with cancer: a meta-analysis . Medicine (Baltimore) . 2015;94(45):e0897. doi:10.1097/MD.0000000000000897
Canadian Cancer Society. Coping with emotions.
CancerCare. What can I say to a newly diagnosed loved one?
American Society of Clinical Oncology. Counseling .
American Cancer Society. Can cancer be cured?
American Society of Clinical Oncology. Stages of cancer.
By Lindsay Curtis Curtis is a writer with over 20 years of experience focused on mental health, sexual health, cancer care, and spinal health.

Lessons From My Cancer Journey
A personal perspective: hard lessons for a reluctant learner..
Posted August 18, 2022 | Reviewed by Gary Drevitch
After being diagnosed with head and neck cancer in February 2021 and overcoming the shock of what was in store for me, I realized that I had embarked on a journey that I hadn’t planned on taking. The journey would be arduous, comprised of hazardous twists and turns and lessons I hadn’t expected or thought I needed to learn.
I also learned that my cancer was going to be my teacher, and it had no regard for students who displayed a reluctance to learn or whether or not I grew tired from the difficult journey as it would unfold.
My cancer was a harsh and severe teacher; unmerciful, unkind, and unrelenting. Early on, I realized that the metaphor of a war or battle didn’t capture what I was experiencing.
I am writing this about my experience because others can benefit from the lessons I’ve learned. These lessons are especially important for men. Like me, most men are socialized to be stoics: to tough it out when things are hard, to not ask for help even when we desperately need it, and to not seek medical help even when the signs of trouble are clear. As you will see, I learned to reject stoicism and embrace my vulnerability.
I came to think of my cancer as a teacher, one who was a lot like my freshman philosophy professor. He was the quintessential New England Ivy League professor: tweed jacket, wire-rimmed glasses, and a dour expression of judgment permanently on his unfriendly face. Never warm or friendly, he was consistently stern and serious. He approached teaching and his students as if administering a form of punishment in each lecture, and he did so without a hint of compassion.
This professor enjoyed utilizing the Socratic method when teaching. He took special delight in cold-calling on students, especially those who appeared distracted or unprepared. He did not care if his pointed yet thoughtful questions left an uncertain or unprepared student embarrassed or ashamed; that was the point of the questioning. Whether you were prepared, sleepy , distracted, or not, he was there to deliver a set of lessons through a series of probing questions that pushed us to think in ways our young minds were often not ready for.
I found that my cancer lessons were a lot like my experience in freshman philosophy, except I hadn’t chosen to take the course. For some reason, I was required to take this journey and compelled to learn the lessons along the way. Like my professor, my cancer teacher had no patience for unprepared students.
“Why me?” I thought as my cancer journey commenced. I soon came to realize how stupid the question was. My cancer teacher could care less if I felt sorry for myself or if I thought having this disease was unfair. There would be no time for wallowing in self-pity on my cancer journey, and the lessons I would be forced to learn along the way would be taught without patience or compassion. My first lesson was that “why me” was the wrong question.
In her book, Illness as Metaphor (1978), Susan Sontag wrote:
Everyone who is born holds dual citizenship, in the kingdom of the well and in the kingdom of the sick. Although we all prefer to use the good passport, sooner or later each of us is obliged, at least for a spell, to identify ourselves as citizens of that other place.
When I was diagnosed with cancer in February 2021, I began my journey to the kingdom of the sick. I hoped I would merely be a tourist passing through, unlike others I had known who became permanent residents in that horrid and unforgiving land.
According to the Centers for Disease Control and Prevention, six in every 10 adults in the United States have a chronic disease. Four in 10 have two illnesses or more. I had no desire to become a member of this sickly tribe, but here I was.

Pedro Antonio Noguera, Ph.D., is the Emery Stoops and Joyce King Stoops Dean of the Rossier School of Education and a Distinguished Professor of Education at the University of Southern California.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

It’s increasingly common for someone to be diagnosed with a condition such as ADHD or autism as an adult. A diagnosis often brings relief, but it can also come with as many questions as answers.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience

- Adolescent and Young Adult Cancer
- Bile Duct Cancer
- Bladder Cancer
- Brain Cancer
- Breast Cancer
- Cervical Cancer
- Childhood Cancer
- Colorectal Cancer
- Endometrial Cancer
- Esophageal Cancer
- Head and Neck Cancer
- Kidney Cancer
- Liver Cancer
- Lung Cancer
- Mouth Cancer
- Mesothelioma
- Multiple Myeloma
- Neuroendocrine Tumors
- Ovarian Cancer
- Pancreatic Cancer
- Prostate Cancer
- Skin Cancer/Melanoma
- Stomach Cancer
- Testicular Cancer
- Throat Cancer
- Thyroid Cancer
- Prevention and Screening
- Diagnosis and Treatment
- Research and Clinical Trials
- Survivorship

Request an appointment at Mayo Clinic

Integrative oncology: Lifestyle medicine for people with cancer
Share this:.
By Nicole Brudos Ferrara
Integrative medicine combines conventional Western medicine with complementary and alternative treatments that have been researched and proven to be safe and effective in healing. Integrative oncology uses integrative medicine as part of standard cancer care.
"Integrative oncology is a practice where we use lifestyle medicine like dietary modifications, stress reduction, exercise, supplements and mind-body practices," says Stacy D'Andre, M.D., a Mayo Clinic medical and integrative oncologist. "We combine all of these practices to help our cancer patients improve quality of life and hopefully improve treatment outcomes, as well."
Integrative oncology can help people with cancer feel better by reducing the fatigue, nausea, pain, anxiety and other symptoms that can come with cancer and cancer treatment.
If you are living with cancer or caring for someone who is, here's an overview of how integrative oncology can ease the burden of cancer:
Integrative oncology starts with healthy habits.
Integrative oncologists help people develop healthy habits to better cope with the stress of living with cancer. "Lifestyle issues are really the foundation of what we work on. Diet, exercise, stress and sleep — all of these things are the foundation to improving health in general,” says Dr. D'Andre.
Dr. D'Andre says healthy habits during cancer treatment are the same habits everyone should adopt for optimal health:
- Eat a diet rich in fruits and vegetables, and choose whole grains and lean proteins.
- Limit your intake of processed and red meats.
- Exercise regularly. Aim for at least 30 minutes of exercise most days of the week.
- Practice good sleep hygiene to achieve at least seven hours of sleep per night.
- Work to achieve and maintain a healthy weight.
- If you choose to drink alcohol, do so in moderation.
- If you smoke, quit . If you don't smoke, don't start.
- Limit your sun exposure, wear protective clothing and apply sunscreen.
Integrative oncology can help people at each stage of the cancer journey.
Receiving a cancer diagnosis and making decisions about treatment can cause stress. Cancer can cause a long list of signs and symptoms, including fatigue and pain. Conventional treatments for cancer, including surgery, chemotherapy and radiation, also can cause fatigue, pain and stress, as well as nausea, diarrhea or constipation, weight loss and other complications. And some of these complications linger after treatment has ended.
Integrative oncologists counsel people receiving cancer treatment on practices that can help relieve these side effects and improve treatment outcomes. They help cancer patients adopt a healthy lifestyle and lose weight, understand which herbal and dietary supplements are safe to take, and recommend integrative medicine practices that might help manage a person's symptoms.
"We also see people after they've completed cancer treatment to help them cope with lingering symptoms and lifestyle modification," says Dr. D'Andre.
When treatment is not an option as part of palliative care , integrative oncologists also can help people manage their symptoms and quality of life.
Integrative oncology is individualized for each patient.
Integrative oncologists work with patients to determine which integrative medicine practices might work well based on individual needs. Health care professionals can now choose from a range of evidence-based approaches that may help, including:
- Acupuncture and acupressure During acupuncture treatment, a practitioner inserts tiny needles into your skin at precise points. Studies show acupuncture may help relieve nausea caused by chemotherapy. Acupuncture also may help relieve certain types of pain in people with cancer. Acupressure is a technique related to acupuncture where mild pressure is applied to certain areas, such as the wrist, to help relieve nausea.
- Aromatherapy In aromatherapy , fragrant oils are used to provide a calming sensation. Oils, infused with scents such as lavender, can be applied to your skin during a massage, or the oils can be added to bath water. Fragrant oils also can be heated to release their scents into the air. Aromatherapy may help relieve nausea, pain and stress.
- Exercise Adding more movement to your day may help you manage signs and symptoms during and after cancer treatment. Gentle exercise may help relieve fatigue and stress and help you sleep better. Many studies show that an exercise program may help people with cancer live longer and improve their overall quality of life.
- Massage During a massage , your practitioner kneads your skin, muscles and tendons in an effort to relieve muscle tension and stress, and promote relaxation. Studies have found that massage can help relieve pain in people with cancer. It also can help relieve anxiety, fatigue and stress.
- Meditation The practice of meditation involves focusing your mind on one image, sound or idea, such as a positive thought, to reach a state of deep concentration. When meditating, you also might perform deep-breathing or relaxation exercises. Meditation may help people with cancer by relieving anxiety and stress, and improving mood.
- Music therapy During music therapy sessions, you might listen to music, play instruments, sing songs or write lyrics. A trained music therapist may lead you through activities designed to meet your specific needs, or you may participate in music therapy in a group setting. Music therapy may help relieve pain, control nausea and vomiting, and deal with anxiety and stress.
- Relaxation techniques Relaxation techniques focus your attention on calming your mind and relaxing your muscles. They might include visualization exercises or progressive muscle relaxation. Relaxation techniques may help relieve anxiety and fatigue. They also may help people with cancer sleep better.
- Tai chi This form of exercise incorporates gentle movements and deep breathing. Tai chi can be led by an instructor, or you can learn tai chi on your own following books or videos. Practicing tai chi may help relieve stress.
- Yoga This activity combines stretching exercises with deep breathing. During a yoga session, you position your body in various poses that require bending, twisting and stretching. Yoga may provide some stress relief for people with cancer, and it has been shown to improve sleep and reduce fatigue.
Integrative oncology is growing in acceptance and popularity.
Integrative oncology is a new field, and trained integrative oncologists are not yet easy to find, according to Dr. D'Andre. But integrative medicine is now being used at many cancer centers.
"There's a huge patient demand for this. There are integrative medicine practices now at most major academic centers and even in the community, which is different than it has been in the past," says Dr. D'Andre.
If your health care team doesn't have an integrative oncologist on staff, ask if an integrative medicine program in the area can help.
"The great thing about this type of practice is that it really empowers the patient," says Dr. D'Andre. "They're the ones doing the work — working on their diet, doing the exercise — we're just guiding them. These are things they can do and control to improve their health and outcomes."
Watch this "Mayo Clinic Q&A" podcast video to hear Dr. D'Andre explain how integrative oncology helps people with cancer and discuss integrative medicine research underway at Mayo Clinic:
Mayo Clinic's Cancer Education Center offers free virtual classes that explore integrative medicine practices. Learn more .
Also read these articles:
- "7 steps to better nutrition habits for cancer survivors ."
- "Alternative cancer treatments: 11 options to consider ."
- "Integrative health paves road to recovery for young breast cancer patient ."
Online Help
Our 24/7 cancer helpline provides information and answers for people dealing with cancer. We can connect you with trained cancer information specialists who will answer questions about a cancer diagnosis and provide guidance and a compassionate ear.
Chat live online
Select the Live Chat button at the bottom of the page
Call us at 1-800-227-2345
Available any time of day or night
Our highly trained specialists are available 24/7 via phone and on weekdays can assist through online chat. We connect patients, caregivers, and family members with essential services and resources at every step of their cancer journey. Ask us how you can get involved and support the fight against cancer. Some of the topics we can assist with include:
- Referrals to patient-related programs or resources
- Donations, website, or event-related assistance
- Tobacco-related topics
- Volunteer opportunities
- Cancer Information
For medical questions, we encourage you to review our information with your doctor.
Road To Recovery®
Get a free ride to cancer treatment .
The American Cancer Society Road To Recovery® program eases your burden by giving free rides to cancer-related medical appointments. Our trained volunteer drivers are happy to pick you up, take you to your appointment, and drop you off at home. All for free and all to make your days a little easier. Not having a ride shouldn’t stand between you and lifesaving treatment.
Schedule a ride with Road To Recovery®
Connect with us by calling 1-800-227-234 5 . to learn more about Road To Recovery® availability near you and other resources to help you on your cancer journey.
Am I eligible?
Patients must be traveling to a cancer-related medical appointment.
Other eligibility requirements may apply. For example, a caregiver may need to accompany a patient who cannot walk without help, or is under age 18. Contact us to find out what is available in your area, and what the specific requirements are.
It can take several business days to coordinate your ride, so please call us at 1-800-227-2345 well in advance of your appointment date.
How do I become a Road To Recovery® Volunteer?
Volunteering as a Road To Recovery® driver will put you at the heart of the American Cancer Society’s mission and fulfill a critical need for cancer patients. If you own or have regular access to a safe, reliable vehicle, then you’re already on the road to volunteering.
Volunteer drivers must be between the ages of 18 and 84, have a valid driver’s license, pass a background check, and have access to a safe, reliable car.
To learn more about becoming a Road To Recovery® volunteer, please visit our Road To Recovery® volunteer page, linked below.
Our Road To Recovery® program is made possible thanks to generous supporters like you.
Donate today or sign up to volunteer so we can continue our life-changing work.
Help us end cancer as we know it, for everyone.

Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Breast cancer patient experiences through a journey map: A qualitative study
Roles Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Clinical Psychology and Psychobiology Department, Faculty of Psychology, University of Barcelona, Barcelona, Spain
Roles Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing
Affiliation Medical Oncology Department Hospital Universitario Central of Asturias, Oviedo, Spain
Roles Resources, Validation, Writing – review & editing
Affiliation Social Psychology and Quantitative Psychology Department, Faculty of Psychology, University of Barcelona, Barcelona, Spain
Affiliation Medical Oncology Department, Hospital Universitario Clínico San Carlos, Madrid, Spain
Affiliation Medical Oncology Department, Complexo Hospitalario Universitario de Ourense, Ourense, Spain
Affiliation Medical Oncology Department, Hospital Universitario La Paz, Madrid, Spain
Affiliation Medical Oncology Department, Hospital General Universitario de Elche, Elche, Spain
Affiliation Medical Oncology Department, Hospital Universitario Fundación Alcorcón, Madrid, Spain
Roles Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing
- Laura Ciria-Suarez,
- Paula Jiménez-Fonseca,
- María Palacín-Lois,
- Mónica Antoñanzas-Basa,
- Ana Fernández-Montes,
- Aranzazu Manzano-Fernández,
- Beatriz Castelo,
- Elena Asensio-Martínez,
- Susana Hernando-Polo,
- Caterina Calderon

- Published: September 22, 2021
- https://doi.org/10.1371/journal.pone.0257680
- Reader Comments
Registered Report Protocol
21 Dec 2020: Ciria-Suarez L, Jiménez-Fonseca P, Palacín-Lois M, Antoñanzas-Basa M, Férnández-Montes A, et al. (2020) Ascertaining breast cancer patient experiences through a journey map: A qualitative study protocol. PLOS ONE 15(12): e0244355. https://doi.org/10.1371/journal.pone.0244355 View registered report protocol
Breast cancer is one of the most prevalent diseases in women. Prevention and treatments have lowered mortality; nevertheless, the impact of the diagnosis and treatment continue to impact all aspects of patients’ lives (physical, emotional, cognitive, social, and spiritual).
This study seeks to explore the experiences of the different stages women with breast cancer go through by means of a patient journey.
This is a qualitative study in which 21 women with breast cancer or survivors were interviewed. Participants were recruited at 9 large hospitals in Spain and intentional sampling methods were applied. Data were collected using a semi-structured interview that was elaborated with the help of medical oncologists, nurses, and psycho-oncologists. Data were processed by adopting a thematic analysis approach.
The diagnosis and treatment of breast cancer entails a radical change in patients’ day-to-day that linger in the mid-term. Seven stages have been defined that correspond to the different medical processes: diagnosis/unmasking stage, surgery/cleaning out, chemotherapy/loss of identity, radiotherapy/transition to normality, follow-up care/the “new” day-to-day, relapse/starting over, and metastatic/time-limited chronic breast cancer. The most relevant aspects of each are highlighted, as are the various cross-sectional aspects that manifest throughout the entire patient journey.
Conclusions
Comprehending patients’ experiences in depth facilitates the detection of situations of risk and helps to identify key moments when more precise information should be offered. Similarly, preparing the women for the process they must confront and for the sequelae of medical treatments would contribute to decreasing their uncertainty and concern, and to improving their quality-of-life.
Citation: Ciria-Suarez L, Jiménez-Fonseca P, Palacín-Lois M, Antoñanzas-Basa M, Fernández-Montes A, Manzano-Fernández A, et al. (2021) Breast cancer patient experiences through a journey map: A qualitative study. PLoS ONE 16(9): e0257680. https://doi.org/10.1371/journal.pone.0257680
Editor: Erin J. A. Bowles, Kaiser Permanente Washington, UNITED STATES
Received: February 17, 2021; Accepted: September 3, 2021; Published: September 22, 2021
Copyright: © 2021 Ciria-Suarez et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: Relevant anonymized data excerpts from the transcripts are in the main body of the manuscript. They are supported by the supplementary documentation at 10.1371/journal.pone.0244355 .
Funding: This work was funded by the Spanish Society of Medical Oncology (SEOM) in 2018. The sponsor of this research has not participated in the design of research, in writing the report, or in the decision to submit the article for publication.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Breast cancer is the most common cancer and the one that associates the highest mortality rates among Spanish women, with 32,953 new cases estimated to be diagnosed in Spain in 2020 [ 1 ]. Thanks to early diagnosis and therapeutic advances, survival has increased in recent years [ 2 ]. The 5-year survival rate is currently around 85% [ 3 , 4 ].
Though high, this survival rate is achieved at the expense of multiple treatment modalities, such as surgery, chemotherapy, radiotherapy, and hormone therapy, the side effects and sequelae of which can interfere with quality-of-life [ 5 ]. Added to this is the uncertainty surrounding prognosis; likewise, life or existential crises are not uncommon, requiring great effort to adjust and adapt [ 6 ]. This will not only affect the patient psychologically, but will also impact their ability to tolerate treatment and their socio-affective relations [ 7 ].
Several medical tests are performed (ultrasound, mammography, biopsy, CT, etc.) to determine tumor characteristics and extension, and establish prognosis [ 8 ]. Once diagnosed, numerous treatment options exist. Surgery is the treatment of choice for non-advanced breast cancer; chemotherapy, radiotherapy, and hormone therapy are adjuvant treatments with consolidated benefit in diminishing the risk of relapse and improving long-term survival [ 9 ]. Breast cancer treatments prompt changes in a person’s physical appearance, sexuality, and fertility that interfere with their identity, attractiveness, self-esteem, social relationships, and sexual functioning [ 10 ]. Patients also report more fatigue and sleep disturbances [ 11 ]. Treatment side effects, together with prognostic uncertainty cause the woman to suffer negative experiences, such as stress in significant relationships, and emotions, like anxiety, sadness, guilt, and/or fear of death with negative consequences on breast cancer patients’ quality-of-life [ 10 , 12 ]. Once treatment is completed, patients need time to recover their activity, as they report decreased bodily and mental function [ 13 ], fear of relapse [ 14 ], and changes in employment status [ 15 ]. After a time, there is a risk of recurrence influenced by prognostic factors, such as nodal involvement, size, histological grade, hormone receptor status, and treatment of the primary tumor [ 16 ]. Thirty percent (30%) of patients with early breast cancer eventually go on to develop metastases [ 17 ]. There is currently no curative treatment for patients with metastatic breast cancer; consequently, the main objectives are to prolong survival, enhance or maintain quality-of-life, and control symptoms [ 17 , 18 ]. In metastatic stages, women and their families are not only living with uncertainty about the future, the threat of death, and burden of treatment, but also dealing with the existential, social, emotional, and psychological difficulties their situation entails [ 18 , 19 ].
Supporting and accompanying breast cancer patients throughout this process requires a deep understanding of their experiences. To describe the patient’s experiences, including thoughts, emotions, feelings, worries, and concerns, the phrase “patient voice” has been used, which is becoming increasingly common in healthcare [ 20 ]. Insight into this “voice” allows us to delve deeper into the physical, emotional, cognitive, social, and spiritual effects of the patient’s life. This narrative can be portrayed as a “cancer journey", an experiential map of patients’ passage through the different stages of the disease [ 21 ] that captures the path from prevention to early diagnosis, acute care, remission, rehabilitation, possible recurrence, and terminal stages when the disease is incurable and progresses [ 22 ]. The term ‘patient journey’ has been used extensively in the literature [ 23 – 25 ] and is often synonymous with ‘patient pathway’ [ 26 ]. Richter et al. [ 26 ] state that there is no common definition, albeit in some instances the ‘patient journey’ comprises the core concept of the care pathway with greater focus on the individual and their perspective (needs and preferences) and including mechanisms of engagement and empowerment.
While the patient’s role in the course of the disease and in medical decision making is gaining interest, little research has focused on patient experiences [ 27 , 28 ]. Patient-centered care is an essential component of quality care that seeks to improve responsiveness to patients’ needs, values, and predilections and to enhance psychosocial outcomes, such as anxiety, depression, unmet support needs, and quality of life [ 29 ]. Qualitative studies are becoming more and more germane to grasp specific aspects of breast cancer, such as communication [ 27 , 30 ], body image and sexuality [ 31 , 32 ], motherhood [ 33 ], social support [ 34 ], survivors’ reintegration into daily life [ 13 , 15 ], or care for women with incurable, progressive cancer [ 17 ]. Nevertheless, few published studies address the experience of women with breast cancer from diagnosis to follow-up. These include a clinical pathway approach in the United Kingdom in the early 21st century [ 35 ], a breast cancer patient journey in Singapore [ 25 ], a netnography of breast cancer patients in a French specialized forum [ 28 ], a meta-synthesis of Australian women living with breast cancer [ 36 ], and a systematic review blending qualitative studies of the narratives of breast cancer patients from 30 countries [ 37 ]. Sanson-Fisher et al. [ 29 ] concluded that previously published studies had examined limited segments of patients’ experiences of cancer care and emphasized the importance of focusing more on their experiences across multiple components and throughout the continuum of care. Therefore, the aim of this study is to depict the experiences of Spanish breast cancer patients in their journey through all stages of the disease. To the best of our knowledge, there are no studies that examine the experience of women with breast cancer in Spain from diagnosis through treatment to follow-up of survivors and those who suffer a relapse or incurable disease presented as a journey map.
A map of the breast cancer patient’s journey will enable healthcare professionals to learn first-hand about their patients’ personal experiences and needs at each stage of the disease, improve communication and doctor-patient rapport, thereby creating a better, more person-centered environment. Importantly, understanding the transitional phases and having a holistic perspective will allow for a more holistic view of the person. Furthermore, information about the journey can aid in shifting the focus of health care toward those activities most valued by the patient [ 38 ]. This is a valuable and efficient contribution to the relationship between the system, medical team, and patients, as well as to providing resources dedicated to the patient’s needs at any given time, thus improving their quality of life and involving them in all decisions.
Study design and data collection
We conducted a qualitative study to explore the pathway of standard care for women with breast cancer and to develop a schematic map of their journey based on their experiences. A detailed description of the methodology is reported in the published protocol “Ascertaining breast cancer patient experiences through a journey map: A qualitative study protocol” [ 39 ].
An interview guide was created based on breast cancer literature and adapted with the collaboration of two medical oncologists, three nurses (an oncology nurse from the day hospital, a case manager nurse who liaises with the different services and is the ‘named’ point of contact for breast cancer patients for their journey throughout their treatment, and a nurse in charge of explaining postoperative care and treatment), and two psycho-oncologists. The interview covered four main areas. First, sociodemographic and medical information. Second, daily activities, family, and support network. Third, participants were asked about their overall perception of breast cancer and their coping mechanisms. Finally, physical, emotional, cognitive, spiritual, and medical aspects related to diagnosis, treatment, and side effects were probed. Additionally, patients were encouraged to express their thoughts should they want to expand on the subject.
The study was carried out at nine large hospitals located in six geographical areas of Spain. To evaluate the interview process, a pilot test was performed. Interviews were conducted using the interview guide by the principal investigator who had previous experience in qualitative research. Due to the Covid-19 pandemic, all interviews were completed online and video recorded with the consent of the study participants for subsequent transcription. Relevant notes were taken during the interview to document key issues and observations.
Participant selection and recruitment
Inclusion criteria were being female, over 18 years of age, having a diagnosis of histologically-confirmed adenocarcinoma of the breast, and good mental status. To ascertain the reality of women with breast cancer, most of the patients recruited (80%) had been diagnosed in the past 5 years. Patients (20%) were added who had been diagnosed more than 5 years earlier, with the aim of improving the perspective and ascertaining their experience after 5 years.
Medical oncologists and nurses working at the centers helped identify patients who met the inclusion criteria. Participants went to the sites for follow-up between December 2019 and January 2021. Eligible women were informed of the study and invited to participate during an in-person visit by these healthcare professionals. Those who showed interest gave permission to share their contact information (e-mail or telephone number) with the principal investigator, who was the person who conducted all interviews. The principal investigator contacted these women, giving them a more detailed explanation of the study and clarifying any doubts they may have. If the woman agreed to participate, an appointment was made for a videoconference.
A total of 21 women agreed to participate voluntarily in this research. With the objective of accessing several experiences and bolstering the transferability of the findings, selection was controlled with respect to subjects’ stage of cancer, guaranteeing that there would be a proportional number of women with cancer in all stages, as well as with relapses.
Data analysis
The data underwent qualitative content analysis. To assure trustworthiness, analyses were based on the system put forth by Graneheim, and Lundman [ 40 ]. Interviews were transcribed and divided into different content areas; units of meaning were obtained and introduced into each content area; meaning codes were extracted and added; codes were categorized in terms of differences and similarities, and themes were created to link underlying meanings in the categories. All members of the research team (core team, two medical oncologists, three nurses and two psycho-oncologists) reviewed the data and triangulated the outcomes between two sources of data: qualitative data from the interview and non-modifiable information, such as sociodemographic (i.e., age, marital status, having children) and clinical (i.e., cancer stage and surgery type) data. Following this process, we reached saturation of the interview data by the time we had completed 21 interviews.
Ethical considerations
This study was performed in accordance with the ethical standards of the Declaration of Helsinki, and its subsequent amendments. The study was approved by the Research Ethics Committee of University of Barcelona (Institutional Review Board: IRB00003099) and supported by the Bioethics Group of the Spanish Society of Medical Oncology (SEOM) 2018 grant. All participants received a written informed consent form that they signed prior to commencing with the interviews and after receiving information about the study.
Patient baseline characteristics
In total, 21 women with a mean age of 47 years (range, 34 to 61) were interviewed. Most of the study population was married (66.7%), had a college education (66.7%), and had 2 or more children (42.9%). All cancer stages were represented, up to 23.8% tumor recurrence, and most of the primary cancers had been resected (95.2%) (see Table 1 ).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0257680.t001
Description of the breast cancer patient journey
The women diagnosed with breast cancer describe the journey as a process tremendously affected by the different medical stages. Each stage has its own characteristics that condition the experiences, unleashing specific physical, emotional, cognitive, and social processes. Additionally, the patients perceive this entire process as pre-established journey they must undertake to save their life, with its protocols based on the type and stage of cancer.
“ People said to me , ‘What do you think ? ’ and I answered that there was nothing for me to think about because everything is done , I have to go on the journey and follow it and wait to see how it goes” (Patient 6)
Fig 1 displays the various phases of the journey that patients with breast cancer go through; nevertheless, each woman will go through some or others, depending on their type of cancer.
https://doi.org/10.1371/journal.pone.0257680.g001
Throughout the entire patient journey.
Processes of loss and reinterpretation of the new circumstance . What stands out the most in the process these women go through during the diagnosis and treatment of breast cancer is loss; specifically, the loss of health and a reinterpretation of the new circumstance and the new bodily reality. In the most extreme cases, the loss of health emerges with the fear of death that many women report at the time of diagnosis or during treatment, due to the distress generated. The loss of identity seems to be related to the evolutionary (existential) moment in which the woman is; there are patients who report feelings of disability or loss of attractiveness, or fear of not being able to get pregnant in the future, especially the youngest.
I felt a terrifying fear and thought , “You have cancer you tell yourself , you’re going to die tomorrow .” (Patient 6) I feel like after the hysterectomy , as a woman , I no longer have anything , only the physical . Sure , I look great , but I tell myself that it’s just a shell , the shell I inhabit , because as a woman , I only have one breast left . (Patient 6) At that moment , I had to make the decision that I was no longer going to be a mother . (Patient 14)
Personal change . Most of the women report that with the diagnosis of breast cancer, their life stands still and from that point forward, a different journey begins. The sole focus on this journey is the disease and its implications. During all those months, the patients stop working; they focus on their medical treatments, and reflect a lot on their current situation and on life. Most of the participants state, especially those who have already been discharged, that they know themselves better now; they take better care of themselves, and they enjoy their day-to-day and the small moments more, making the most of their time, with more initiatives and fewer trivial complaints.
Clearly , you’re not the same person you were before; I don’t think she’ll ever come back; your mindset changes completely and I have sequelae from all the treatments . (Patient 1) I re-think wasting energy on lost causes; what’s more , I’ve also learnt to say no . If I’m not in the mood to go somewhere , I just say no . (Patient 7) I take much more advantage of the present now , because you realize that things can change on any given day . (Patient 3)
Trust and appreciation for their physician . Most of the interviewees stated that they fully trusted the doctors who care for them, without question or objection to the treatments proposed. They reported that, as they go forward, they discuss the tests and treatments that are going to be performed, as well as possible side effects. Several stated that they are unaware of the stage of their cancer; similarly, most also do not know the benefits expressed in X% of the treatments. A few of the participants claimed that they did talk in detail about the different types of treatments with their oncologists, that they had sought another opinion, and one of them even reported having decided to stop chemotherapy, which was very hard for her, given her physician’s insistence that she continue.
The truth is that the oncologist didn’t say much about percentages; what she told me were the steps that I had to take; I thoroughly trusted her and she gave me a lot of peace of mind . (Patient 5) I told him , “I’m going to do whatever you tell me to . ” It never occurred to me to dispute whatever the oncologist might tell me . I was willing to do whatever was needed . (Patient 8)
Most of the women, at some point during the interview, state that they are grateful for the care they received and that, within the seriousness of their situation, there is a treatment for their condition.
I am super grateful for the treatment I’ve received and with the doctors assigned to me . (Patient 2) I’m very lucky; I’m only on my second line of treatment for metastasis and I’ve got a lot more ahead of me , but I consider myself lucky and I believe things are going very well . (Patient 20)
Role of the woman . We can see that the women adopt a role of care-givers and managers of their surroundings. They worry about the disease negatively affecting the people around them, which is why they make an effort to manage the family’s activity for when they can’t do it and they try to avoid being a physical burden or cause emotional distress to the people around them.
I was very strong ; I made everything easy for people , but making it very easy , doesn’t mean that it was easy for me , but that I made it easy for everyone . (Patient 8) I didn’t want to worry anyone because that’s just the way I am , I push forward and that’s that . (Patient 5)
Support network . In all cases, the family appears to be one of the elements that is most involved in the disease process. Within the family, the partner deserves special mention. The testimonies in this regard reveal a wide spectrum of possibilities that range from the feeling of having had great support to a lack of attention and understanding that, in many situations, causes the relationship to be strained or to end. Friends tend to appear more occasionally.
I can’t complain about my husband; he was up to the challenge , very attentive toward me and he fully understood how I was feeling ; I felt very supported . (Patient 14) We’ve had a period of a lot of arguing; I’ve had to sit down with him and tell him that life had changed for me . (Patient 18) I had a partner I had lived with for five and a half years and he told me , literally , that he looked at me like a little sister , no longer as a woman , and he left me , and that hurt me tremendously . (Patient 6)
On the other hand, many patients commented on the importance of social media, where they have met people in the same situation as them. They report feeling understood and in good company; likewise, they commented on the importance of being able to share their doubts and get to know about other experiences.
It’s a situation that only someone who has gone through can understand; you can have all the good intentions in the world , but if you haven’t gone through it , you can’t even begin to understand . (Patient 8)
Use of complementary treatments . Most patients follow conventional medical treatment. However, many resort to other disciplines that help them improve their quality-of-life, like dietary changes, getting more exercise than usual, visits to a psychologist or physical therapist, or using other integrative therapies, such as acupuncture, yoga, reiki, flowers of Bach, homeopathy, cannabis, or meditation.
I started to read a whole bunch of books to see what I could do to take care of myself in terms of nutrition and exercise ; you consider everything you can do . (Patient 5)
Diagnosis/unmasking.
This phase encompasses the time from when the woman detects some symptom or goes to a check-up until the medical diagnosis is made. For the woman, this is a time of a series of tests and results. We have observed that the procedures, especially the healthcare professionals that deal with the patients, and the timing vary, depending on the medical center where they are being cared for. Emotionally, this is one of the most complicated stages.
Emotional whirlwind . The wait to obtain test results has a huge emotional impact for the women, given that it is a time of great uncertainty and fear.
An entire month with all the anguish of finding out if you have something . (Patient 3) The worst part is waiting 15 days to find out the magnitude of the tragedy , if it’s throughout your entire body or only in your breast; you go through a brutal emotional whirlwind; the wait is horrible because there’s nothing else you can do , so that anguish that you carry inside is dreadful; it was hell for me . (Patient 10)
Additionally, the interviewees described many other emotions that included fear of death, fear of having no time, feeling of unreality, rage, anger, sadness, avoidance, denial…
The first thing I thought was that I was going to die and that I wouldn’t finish watching my children [grow up]; my father had died of lung cancer 25 years ago . (Patient 9) My only aim was to get back to normal , as if there were nothing wrong . (Patient 4) You have a lot of conflicting feelings; you wish this weren’t happening; you want to run away , but you say , “Where am I going to run to ? ” . (Patient 14)
Impact of medical communication . Several women comment that, when given the diagnosis, they dissociate because of the emotional impact and that they don’t listen to all the information that the medical professional is giving them.
I remember that she talked and talked , but I didn’t know what she was saying until she said , “Isabel , you’re going to be cured , okay ?”. (Patient 9)
During the diagnostic testing, the women are highly sensitive to the healthcare professionals’ words and gestures.
I looked at the face of the person who was doing the mammogram and that’s when I started to imagine the worst . (Patient 20) I say to them , “ But , is there a solution to this ? ” , and they say to me , “Don’t worry , I’m sure there is a solution . ” That “sure” is etched in my mind . (Patient 10)
Communication and managing their surroundings . After the diagnosis, the patients feel that they have to tell the people around them about their situation, especially those closest to them, the family. They all agree on how hard it is to share. Normally, the people it’s hardest to tell are their mother and their children. When they do, they try to put the most positive spin on it possible, in an attempt to keep them from worrying.
You no longer think only about yourself , you think , “Good grief , now I’ve got to tell my mother .” It’s hard . (Patient 16) I wanted to tell my kids the way I say things , always trying to look for the upside , and positive , although it was hard , but , anyway , in the end , it went well . When I finished , my husband told me , “You’ve convinced me that it’s no big deal .” (Patient 9) I told my son , “Son , don’t cry , your mom’s going to get over this , this is nothing .” (Patient 1)
During this period, the women contemplate how their situation will affect their surroundings and they try to organize it as much as possible.
I devoted myself to planning everything , to organizing what to do with my daughter , and to thinking about work , too , how I had left things at work . (Patient 4)
Surgery/cleaning out the cancer.
Uncertainty and fear . The participants express that before going into surgery, they are told about the kind of procedure that will be done, but that, depending on what they find and the analysis, it may change. In light of this, they exhibit an enormous feeling of uncertainty and fear. In addition, many voice concern about how the surgery will go.
They tell you conservative surgery , but if we open up and see something we didn’t see on the tests , then everything could change . (Patient 10) Aside from the anesthesia , that I’m terrified of , you spend several hours in surgery and you don’t really know how things will go; when they clean it out , they analyze it , and you go into the operating room and you don’t know what can happen . (Patient 9)
Feeling of loss . Considering that the breast is associated with an intimate, feminine part [of their body], many women experience the operation as a loss. This loss is more acute if the operation is a mastectomy and there is no reconstruction at the same time. The loss also involves a loss of identity, compounded by the side effects of chemotherapy, such as hair loss. The interviewees who had undergone mastectomy say that following surgery, when the bandaging is removed and the scar is revealed, is one of the most critical moments, which is why they express difficulty in managing it and appreciate the caring assistance from the professionals.
It is identification with yourself , you know , it’s what you’ve seen in the mirror , what you think you’re like and , suddenly , you’re no longer like that; there’s an incredible personal crisis because you no longer recognize what you’re seeing . (Patient 11) I closed my eyes and I removed the bandaging and I didn’t dare look … with my eyes , I imagined the worst . (Patient 12)
Acceptance or demand for more aggressive intervention . The patients perceive the surgery as essential to recovering their health, which is why the process is widely accepted. Some patients who demand a more invasive intervention, normally a bilateral mastectomy, do so because that way, they feel safer with respect to a possible relapse, as well as more comfortable esthetically.
If they have to remove my breast , let them take it; what I want is to get better . (Patient 16) They say that I am in full remission , so they only removed the lump , but at first , I said that I wanted my whole [breast] removed ; then they assessed how to do it . (Patient 13) They told me that I had a genetic mutation and more possibilities of developing breast cancer and , since I felt such rejection toward my remaining breast , I decided to get rid of that one , too . (Patient 20)
Chemotherapy/loss of identity.
The chemotherapy phase is one of the phases that affects the women’s lives the most, because of its physical impact and how long it lasts. No differences have been found in how they experience chemotherapy depending on whether it was neoadjuvant or adjuvant.
Negative impact of side effects . Chemotherapy is associated with many side effects that vary from one woman to another. Many indicate that they have suffered physical discomfort, such as fatigue, dysgeusia, pain, nausea and vomiting, mucositis, diarrhea, etc.
One day when I didn’t want to go to bed , I went to bed crying because I had the feeling that I wasn’t going to wake up . That day it was because I felt awful . (Patient 1)
Furthermore, all of the women suffer hair loss, which is one of the most-feared effects. Likewise, their body hair also falls out, especially on their face, and their weight fluctuates. All of these changes lead to a loss of identity that is experienced as taking away from their femininity. It must be remembered that oftentimes, chemotherapy is administered after surgery, further exacerbating this physical change. On top of all that, several women comment having to decide at the beginning of treatment whether to freeze their eggs or not; at that moment, many of them forfeit the possibility of becoming a mother or of becoming a mother again, which also adds to this loss of femininity.
Losing my hair was hard , but when it grew out again , I had an identity crisis . I didn’t recognize myself; people said I was really pretty like that , with my hair so short . I looked at myself in the mirror and I said that I’m not that woman , I can see that that woman is pretty , but it’s just that I don’t recognize myself . That’s not me or , it was like , I looked at myself and I didn’t recognize myself . That’s when I suffered a serious identity crisis , psychologically serious , but also serious because I sobbed because I looked at myself , but it wasn’t me . (Patient 6) Where’s that sexy lady , where is she ?, because you don’t feel good . I didn’t like myself at all . I was several sizes larger and I looked at myself and said , “What a monster . ” I didn’t feel good about myself . (Patient 1)
Many patients say that chemotherapy decreases their libido and dries up their mucous membranes, which is why they prefer not to have sex. For those who live as a couple, this situation can strain the relationship.
Sexually , I just didn’t feel like it , I wasn’t in the mood; not only did I not feel like it , my mucous membranes were dry and , what’s smore , I just couldn’t , I couldn’t , I felt bad for my husband , but he said , “Don’t worry .” (Patient 16)
Finally, some interviewees expressed a feeling of being poisoned by the treatment. These women tend to be highly focused on taking care of their body and have a very natural attitude toward life.
I had to really work my awareness that I was poisoning myself; at night I was at home and I thought that all that red liquid was circulating through my veins … I think I even had nightmares . (Patient 4)
Balance between caring for oneself and caring for others . The patients feel that it is time to take care of themselves, so they prioritize resting when they need it. Moreover, they worry about getting a haircut and, most of the times, they look for turbans and wigs. Some also learn how to put on make-up, which they rate as being very positive. On the other hand, those who have children or another person in their care, try to take care of them as much as they are able.
Around 11 : 00 , I no longer felt good , so I’d go to the armchair to rest and it’s like I had an angel , because I’d wake up a minute before I had to set the table and get lunch for my son who would be coming home from school . (Patient 1) While I was getting chemo , I went with the gadget and I told myself , “I’m going to teach you to apply make-up; for instance , your eyelashes are going to fall out . Make a line like this ” and at that moment when you look in the mirror , and we look like Fester in the Addams family . (Patient 13)
Vulnerability . The women experience great uncertainty and feelings of vulnerability the first times they receive chemotherapy, since they don’t know what side effects they will suffer.
With chemo , I started with a lot of fear and , later on , I became familiar with it little by little until the time comes when you go to the hospital like someone who’s going to pick up a bit of paper . (Patient 9)
In addition, those participants who join a social network or who are more closely tied to the hospital setting, know about the relapses and deaths of people around them diagnosed with breast cancer, which makes them feel highly vulnerable.
There are some people who leave the group because … it’s not like there are a lot of relapses and , geez , I think that it messes with your head . (Patient 13) We were almost always the same people at chemotherapy ; there was one guy who was really yellow who looked terrible and , there was one time when we stopped seeing him and another lady asked and the nurse said that he had died . (Patient 15)
At the same time, given the physical changes, especially those that have to do with body hair, many women feel observed when they leave home.
If I have to go out and take off my scarf because I’m hot or go straight out without any scarf on my head and whoever wants to look… let them ; I think that it’s up to us , the patients , to normalize the situation; unfortunately , there are more and more cases . (Patient 9)
Telling the kids . Since when the chemotherapy stage is going to entail many physical changes, the women look for ways to talk to their children about the treatment. Most of them comment that it is a complicated situation and all of them try to talk to their children in such a way as to protect them as much as possible.
I asked the nurse for help before I started chemotherapy to see if she had any pointers about how to talk about this with the kids and she recommended a story , but when I saw it , I didn’t like it … so , in the end , I decided to do it off the cuff . (Patient 10)
Radiotherapy/transition to normality.
The “last” treatment . When the patient reaches radiotherapy, normally, they have already spent several months undergoing physically aggressive medical procedures, which is why they feel exhausted. There is a physical exhaustion resulting from the previous treatments and made worse by the radiation therapy. Furthermore, many women also report feeling emotionally drained by the entire process. However, this is generally accompanied by joy and relief because they feel that they are in the final stage of treatment.
Emotionally , it’s a marathon that has to end up at some point . (Patient 10) For me , radiotherapy was like a lull in the battle , with a winning mind-set . (Patient 4)
Comparison with chemotherapy . There is a widespread perception that radiotherapy has fewer side effects than chemotherapy, although later, when they receive it, several patients suffer discomfort, above all fatigue and dizziness. Several report that at this point, they are mentally worn out and just want to be done with the process, which is why they have less information than about chemotherapy.
I feel like radiotherapy is unknown , that you think it’s more “light ” and it turns out not to be so light . (Patient 13)
Follow-up care/the “new” day-to-day.
Difficulty in getting back to normal . Once the patients are discharged, many feel that they need some time to recover, that it will be slow, in order to restore a more normalized pace of life. They are still working on their emotional and personal process.
When they tell you that you have cancer , they make it very clear : you have a goal; you have some months of chemo , some months of radio , and when you finish , you say , “And now , what do I do ?”. I say that because now I have to get back to my normal life , but I don’t feel normal . I still don’t feel cured , I’m not 100% . And you’re glad you’ve that you’ve finished it all and you’re alive , but at the same time , you say , “Gosh… this is very odd . ” It was a very strange feeling . (Patient 8)
Most patients report that their quality-of-life has diminished, due to the sequelae from the treatments. Lymphedema is one of the sequelae they name most often, although they also mention other symptoms, like digestive upset, weight issues, eye problems, scar pain, etc. The women who are on hormone therapy also suffer side effects, such as joint and muscle pain.
I have lymphedema and , although I have good mobility , I’m a little bit weak; when I go out for dinner , I generally order fish , because I can’t always cut meat well . (Patient 6)
Several interviewees also express difficulty in their affective-sexual relations. Many of them feel insecure because of all the physical changes; others have sequelae that hinder their relations, and still others are suffering symptoms of early menopause. This can cause problems in the couple and for those who don’t have a partner, suffer many complications when it comes to meeting other people.
I haven’t had sex with my husband for 2 years because , it’s also really complicated to get over; I’ve gone for pelvic physical therapy; I’ve used gels , but nothing works . (Patient 8) It’s taken me many months for me to have a relationship again; it’s been really hard because , even though everyone told me that I looked fine , I didn’t feel fine . My breast cancer had taken away all my attributes as a woman . (Patient 6)
Some women also experience difficulties when it comes to returning to work. Several state that they had been fired when they went back. They also report that when interviewing for a job, it’s complicated for them because they have to explain what happened and they mention the schedule of doctor’s visits that they have. Other women comment that they’ve been given early retirement or disability.
You go to the interview and if you tell them that you’ve had the disease , they look at you like you’re a weirdo . (Patient 13)
Breast reconstruction . How reconstruction is experienced, as well as its timing, are highly contingent upon they type of reconstruction. Each one has its pros and cons, but the opinions collected with respect to the type of reconstruction have been positive.
Although it took 18 months for the entire process to be over , I’m delighted with reconstruction with the expander . (Patient 16)
Some patients state that after the whole process, which has been long and complicated, they prefer not to undergo reconstruction immediately. In these cases, they report having felt a subtle pressure from the outside to undergo reconstruction.
Every time I went for my check-ups , they said , “You’re the only one left [who hasn’t undergone reconstruction]” and in the end , the truth is that I’m really happy because I think I look pretty . (Patient 12)
Check-ups and fear of relapse . Check-ups are one of the times that generate most worry and insecurity. The women remark that, starting a few days before and until they receive the results of the follow-up studies, they are more anxious about the possibility of relapse.
At every check-up my legs start shaking again and my stomach is in knots, although at my last one, everything turned out okay and I’m thrilled. (Patient 6) During the first stage , I did everything I had to do and I got over it , but it’s a lottery . You can do whatever you want , but it’s the luck of the draw and when you start going for check-ups , it’s like going to play Russian roulette . (Patient 8)
Maintenance hormone therapy . Hormone therapy is understood differently depending on age and on the major decision of whether or not to be a mother or to have another child. If the woman does not want to have more children, the treatment is accepted better. The patients who take it also report effects derived from menopause, for instance, joint pain or dry mucous membranes.
I did notice joint pain , but since I exercised , [I felt it] much less than my fellow women , although , for instance , when it comes to getting up from a chair , you get up like an old lady . (Patient 10)
Position of support . Several patients mention that, after discharge, they stay active on social media, they volunteer when they find out about someone or to participate in activities related to breast cancer, with the aim of being able to help other people who are in this situation.
It’s really good to meet other people who are going through the same thing , so , now that I’ve finished , I like it and I always help whenever I can , because I can share what was good for me . (Patient 13)
Relapse/starting over.
Emotional impact . The diagnosis of a relapse is experienced much the same as the initial diagnosis. All of the women report fear, although they also state that they are more familiar with the processes. Other emotions emerge, such as why me, blame, disbelief, etc.
Since they had told me that it wasn’t going to happen again , I believed it , of course , I wanted to believe it and it totally surprised me; I couldn’t stop crying and crying . (Patient 17)
Telling the family again . Patients repeat that telling the family about it again, especially the children and parents, is tough and they try to minimize it in an attempt to protect them emotionally.
On the very same day that I had my mammogram , my mother says that she wants to come a see the kids . We’re in the park , when she arrives , I have to tell her that everything’s fine and when we get home , I tell her everything . My mother’s devastated again and I tell her not to worry , that everything is going to be fine . (Patient 16)
Thinking about whether something could have been done differently . Several women comment that, after their relapse, they think about whether the treatment was enough or there must have been something they could have done to avoid the relapse.
You get furious , because you say , “I wasn’t supposed to get sick , because if , 2 years ago when the first microcalcifications appeared I had had them removed , then I wouldn’t have metastasis , or maybe I would . (Patient 19)
Metastatic breast cancer/time-limited chronic.
Re-interpreting the concept of metastasis . Most of the participants in this stage state that they have had to give new meaning to the word, “metastasis,” since their first perception was directly related to death. In this way, they come to understand that cancer can become chronic, although they now have to take medication and go to the hospital on a regular basis. Nevertheless, they know that their life expectancy may be a few years. The women who are involved in a group point out how hard it is to see their fellow member pass away.
What I now call my “ new normal” consists of lots of visits to the hospital and never going back to work . (Patient18)
They also state that at this stage, they do not identify with the disease generally known socially as “breast cancer”, where there is great emphasis placed on early detection and on their chances of being cured. This causes them to feel more isolated.
These pink ribbon campaigns hurt us because they tend to underscore that everything is going to turn out fine because breast cancer has a very high cure rate; there is huge lack of awareness . (Patient 20)
Physical and emotional discomfort . Most of the women in this stage report side effects from the treatments, although some comment that good quality-of-life can be preserved. On an emotional level, they say that they sometimes feel a certain agony due to not knowing how much longer the treatment will be effective. They live in a state of uncertainty that they try to cope with by focusing on their day-to-day and experience the good times deeply.
When I’m not in pain , I try not to even remember what I have and go out and have fun with my family and live . (Patient 20)
Several women who have children express with regret that they worry about their children enjoying them and remembering them when they were well. They are sad that they won’t be able to grow up in a normal family. Some also comment the impact this diagnosis is having on their partner.
What I don’t want is for them to carry this baggage of having a sick mother . (Patient 18)
A conflict with disability also appears, as many women report their desire to continue working, but feel that they can’t keep up with the pace of work. Additionally, several state that going through the medical board is a strenuous process, given that they look good physically.
It’s hard to deal with , I’m a non-practicing lawyer and I have degrees galore , but I worked the first year and I couldn’t continue . (Patient 21) Every year they call me again for the disability monitoring and they always threaten me . To be honest , the treatment doesn’t make me sick , but I don’t know how long it’s going to be like this . (Patient 19)
Social invisibility . The participants say that they do not have any physical signs of being ill, that they look fine, although they know and feel that inside, they are not well. They say that it is sometimes hard to manage socially, since on occasion, they feel misunderstood and disparaged.
I’m much sicker now , but people think or want to think that I’m fine . When I was doing chemo , it was like wearing a sign that said “cancer . ” (Patient 17)
This study describes the patient journey of women with breast cancer, specifying the different phases with the most relevant aspects of each, as well as the different cross-sectional features they report throughout the entire treatment process.
The results portray breast cancer as a process in which there is a striking feeling of loss of health and self-identity, changes in routines, personal and employment transformation, as well as emotional hardship during and after breast cancer treatment, aspects that are also reported in the literature [ 41 , 42 ]. Earlier studies state that experiencing cancer is highly stressful. It involves a major threat to life or physical integrity, in addition to mental health, interfering with the path, projects, and plans patients have for their life over the short, medium, and, on occasion, long term as well [ 6 ]. Along with reporting adverse physical and psychological impacts, patients also report positive ways in which they have grown psychologically or emotionally from the experience [ 7 , 42 ]. The diagnosis of breast cancer not only impacts the women individually, but also affects their surroundings. As reported in the literature, despite going through a very challenging time, the women struggle to put on a positive face and attempt to conserve the family’s well-being, specifically that of their children [ 7 ]. At the same time, the family is a fundamental source of support and usually provide indispensable support; however, it is not always effective, because family members do not fully understand the stresses involved in living with cancer [ 43 ]. Previous studies also reveal that for some women, their partners are one of their most significant supports; nonetheless, research also suggests that a cancer diagnosis predicts marital breakup more strongly for female survivors than males [ 44 ]. Our results reflect that the women frequently resort to other women in the same situation, possibly because they face significant unmet supportive care needs [ 30 ]. The need for social support may lead patients to seek social support groups consisting of people who are experiencing similar health crises, because such groups allow them to interact with those who best understand their suffering [ 43 ]. Another aspect that appears across the board is the relationship the participants have with the medical team. In this study, we have noted their trust in the medical team and acceptance of the treatments proposed without going into the clinical data of the disease and without needing to know the benefit provided by the treatment. Cancer patients are confronted with a potentially life-threatening [condition], feeling vulnerable, and need to rely heavily on their care providers, expecting the physician to act in their best interests [ 5 ]. Therefore, they need to have a close relationship, as well as comprehensive care [ 30 ]. Patients’ trust in a physician has been associated with a reduction of their fears and anxiety and [increased] satisfaction and adherence to treatment [ 5 , 30 ]. We believe that it would be important to provide patients with accurate information, so as to avoid misunderstandings (such as cancer being synonymous with death, regardless of stage) as several participants in this study have reported, which can lead them to believe that the risk of relapse with and without chemotherapy is much greater than the oncologists estimate [ 45 ]. We believe that in future studies that it would be worthwhile to examine the peculiarities of each kind of patient information with the aim of determining how to break it up and make it both comprehensible and tolerable to promote patients’ well-being.
A breast cancer diagnosis is generally unexpected and practically all patients suffer psychological distress, such as feelings of uncertainty, disbelief, hopelessness, vulnerability, anger, fear, anxiety, and sadness [ 46 , 47 ]. The literature has reported that many women experience peritraumatic distress or dissociation during the medical conversation in which they are given their diagnosis of cancer [ 48 ], which might account for the reactions of the respondents. Given that, when they receive their diagnosis, additional information is generally given to them, such as clinical aspects and preferred treatments. Repeating this information at subsequent appointments could contribute to improving communication with patient, since several participants stated that they found it hard to pay attention to the physician, given the emotional impact. Additionally, breast cancer patients tend to be diagnosed when they are relatively young, and often when they are in the middle furthering their career or raising children [ 12 ]. In spite of everything, the women try to put on as brave a face as they can and focus on maintaining their children’s well-being [ 7 ]. Telling children about their diagnosis is reportedly one of the biggest challenges; parents are usually unsure of how to tell them, because at the same time that they want it to be open and honest and cover their children’s developmental needs, they also want to protect them children [ 49 ].
Once diagnosed, breast cancer patients go through different treatments. The most salient experiences of these phases pertain to the impact of side effects on physical quality-of-life and psychological well-being, which is consistent with the literature [ 11 ]. Moreover, cancer therapy entails physical changes that affect their feminine identity, fertility, self-esteem, sexual functioning, and makes them more vulnerable [ 10 , 50 ]. Women described their inner self as being on an emotional rollercoaster with highs and lows throughout the various phases of treatment [ 7 ]. Given treatment side effects and sequelae, these women are more likely to experience physical symptoms and psychological disorders than patients with other kinds of tumors [ 51 ]. The side effects involve an acute sense of loss of health and quality-of-life, as well as identity and femininity. It would be interesting for future research to explore the therapies used in grief counseling with cancer patients, as understanding and exploring this perspective could comprise an additional clinical aid.
Once the women have completed their treatments, they gradually get back to normal and many contemplate returning to work. However, in line with our results, the literature reveals that even though they want to normalize their lives, female breast cancer survivors feel that they will never return to their baseline status [ 7 ]. A significant number of patients experience difficulties in physical, cognitive, and emotional functioning after their treatment, such as symptoms like lymphedema, fatigue, pain, sleep disorders, cancer-related cognitive impairment, emotional stress, symptoms of depression and anxiety, problems with relationships, reduced sexual identity, fertility problems, and fear of cancer relapse [ 13 , 14 ]. Furthermore, patients with hormone therapy suffer hot flashes, sweats, joint pain, weight gain, decreased libido, and low energy [ 52 ]. A sizeable number of these women also experience changes in employment status which can happen even 5–10 years following diagnosis [ 15 ]. Given that all these changes alter the structure of the woman’s everyday life, personalized care and treatment plans in cancer survivors are highlighted in the literature with extended specialized support being proposed that enables them to make a better psychosocially adjusted transition from treatment to follow-up [ 53 ] and advocating for the patient’s participation in all decisions that affect her during this period [ 54 ]. Further research is needed concerning how to structure the follow-up and support offered to these women during this stage so as to meet their needs and help them adjust to their new reality with the chronic sequelae caused by cancer and its treatment. On the other hand, the personal transformation of the initial stages of the journey are best seen during this phase. The literature shows that women who have had breast cancer report changes in their philosophy of life, such as embarking on a new life path, changing their priorities in life, as well as valuing life in general [ 42 ]. Most of the participants in our study place special emphasis on appreciating life, enjoying it more, and living each day to the fullest. Cancer survivors report being aware of how precarious life is, while also feeling the joy of being alive [ 55 ]. Similarly, they have been found to be more resilient and better able to repair their mood than healthy women [ 56 ].
About 5% of all patients with breast cancer are diagnosed when the disease is metastatic, whereas some 30% have suffered a relapse of an early breast cancer [ 17 ]. We saw that some women suffering a relapse after initial treatment with curative intent tend to wonder if the treatment was sufficient or if they should have done something more to prevent the relapse. Metastatic breast cancer is uncurable, which is why these women’s main psychosocial challenges are not the same as those who are diagnosed in early stages [ 18 ]. Faced with incurability, the women react with shock and fear of imminent death, but this anxiety diminishes once they begin treatment and learn that there are more treatment options [ 17 ]. During this phase, the interviewees reported impaired physical QoL and functioning, being hindered by pain, fatigue, or menopausal symptoms. Emotionally, they report suffering bouts of depression and anxiety, as well as fear because of the spread of their cancer. As for their relational QoL, their children’s welfare is their number one concern, especially for mothers of young children [ 17 , 57 ]. What’s more, these women felt isolated from society in general and, more specifically, from the non-advanced breast cancer community, inasmuch as they feel that nobody understands what they are going through [ 18 ]. A psychosocial approach is especially important in this phase to help these women to continuously adapt to the changes of their individual clinical situation and to the progression of the disease, thereby improving their coping.
Clinical implications
Having first-person information enables us to comprehend in detail the experiences of breast cancer patients, their situation, and emotional state, which favors holistic cancer care for health professionals.
Healthcare professionals should prepare women for a changed life situation, as well as to face prolonged, multimodal treatment (surgery, chemotherapy, hormone therapy, radiotherapy), and to confront physical and psychological sequelae, as well as the fear surrounding an uncertain prognosis. It is important to help them manage their expectations and fears and, to identify and address the issues and concerns that arise at different time points during treatment. The information and support offered should be adjusted to each woman’s individual needs, her life situation, her coping style, and the time and stage of their cancer. This more empathic, understanding outlook can also contribute to improving the physician-patient rapport, promoting communication, understanding, and shared decision-making.
Finally, a comprehensive understanding of the women’s psychosocial support endorses their belonging to groups of women with breast cancer, in which there is a relationship among equals. Further research is needed to specify the type needed so as to decrease both the impact of the death of women in the group, as well as the vast amount of information that they may end up obtaining, without needing it or requesting it.
Limitations
This study was performed with Spanish participants, which is why certain aspects cannot reflect the experiences of breast cancer patients from other countries, given the particularities of both the Spanish healthcare system and Spanish culture. Likewise, the data attained were specific to women with breast cancer, which can scarcely be extrapolated to individuals with other cancers. Moreover, the findings do not reflect men’s experiences with breast cancer and research with this group would enrich the field further. In addition, the age of our participants ranged from 34 to 61 years; hence the results should be interpreted for a middle-aged population and do not reflect the experiences of women diagnosed at very early or very old ages. Finally, we believe that there may be a bias regarding the women who agree to participate, as this group has probably accepted their condition more, as well as having worked on it more.
Despite these limitations, we hope that our findings can contribute to better understanding the experiences of women with breast cancer.
Acknowledgments
The authors are grateful to the investigators of the Neoetic study and the Bioetic Group of the Spanish Society of Medical Oncology (SEOM) for their contribution to this study. We would like to thank all the women who generously shared their experiences with us, the support of HealthyOnco ( www.healthyonco.com ), and Priscilla Chase Duran for editing and translating the manuscript.
- View Article
- Google Scholar
- PubMed/NCBI
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Med Internet Res
- v.17(5); 2015 May

The Cancer Experience Map: An Approach to Including the Patient Voice in Supportive Care Solutions
Leslie kelly hall.
1 Healthwise, Boise, ID, United States
Breanne F Kunz
Elizabeth v davis, rose i dawson, ryan s powers.
The perspective of the patient, also called the “patient voice”, is an essential element in materials created for cancer supportive care. Identifying that voice, however, can be a challenge for researchers and developers. A multidisciplinary team at a health information company tasked with addressing this issue created a representational model they call the “cancer experience map”. This map, designed as a tool for content developers, offers a window into the complex perspectives inside the cancer experience. Informed by actual patient quotes, the map shows common overall themes for cancer patients, concerns at key treatment points, strategies for patient engagement, and targeted behavioral goals. In this article, the team members share the process by which they created the map as well as its first use as a resource for cancer support videos. The article also addresses the broader policy implications of including the patient voice in supportive cancer content, particularly with regard to mHealth apps.
Introduction
“Patient voice” is a term that has become more common in health care contexts. It is often used to describe a compilation of many patients’ expressed feelings, concerns, and experiences during an illness. While “patient voice” sounds singular—as if all of these voices had somehow reached a consensus and blended into one voice—it is plural in that this “voice” reflects a span as wide as the vastness of human experience and response. For the purpose of this article, “patient voice” is defined as the perspective of a cancer patient, and acknowledging the voice of the cancer patient is synonymous with having a deep understanding of how cancer affects a person as a human being, including in physical, emotional, psychosocial, and spiritual ways.
When our team, consisting of a medical writer, an oncology content specialist, and two user experience researchers, set out to concretely represent the voice of the cancer patient, our goal was to build a tool for our company’s content developers. We call this new patient-voice model a “cancer experience map”. We believe that, in this time when technology makes very little seem impossible, the usefulness and long-term, proven success of mobile health apps (mHealth apps) will depend on the app developers’ willingness and ability to tailor their apps to the cancer patient. Here, we offer the cancer experience map as a new tool for mHealth app developers.
Mobile Health Apps: Benefits and Barriers
Mobile health apps (mHealth apps) not only can be a source of support for people who have cancer but also can improve their quality of life. During cancer treatment, this support can help a cancer patient manage health-related issues and promote better patient-provider communication, collaboration, and shared decision making [ 1 ]. After cancer treatment, an mHealth app can ease this transition by helping him or her deal with lingering side effects, such as insomnia, or make health behavior changes, such as trying a new exercise routine [ 2 ]. Also, mHealth apps that are online coaching programs can benefit family or friends who are caring for a person with cancer—lightening their burden, increasing their coping skills, and improving their mood [ 3 ].
Amidst all this promise, there are some real-world limitations. A systematic review of mobile phone apps found that while there are hundreds of apps covering a range of cancer-related support, there is a lack of evidence on how they are used and how effective and safe they are [ 4 ]. There is no index or repository where a person can go to see what apps are available, nor is there a standard rating system that includes reviews by cancer patients who have tried these apps. In addition, mHealth apps in the United States are subject to legal implications, so health care providers and app developers need guidance to comply with regulations [ 5 ].
Many barriers have been identified. A recent review of mobile phone apps for breast cancer noted as a barrier the lack of consumer confidence in these apps and pointed out the need for a robust framework for identifying high-quality cancer supportive care apps that could be used by patients and their medical providers [ 6 ]. The technology limitations of mobile devices pose another barrier, and app developers are advised to use cancer patients to test their apps and then implement the design and functionality features recommended by these patients [ 1 ]. The unmet supportive care needs of cancer survivors after treatment are also a barrier that is becoming increasingly more evident [ 7 ].
Capturing the Cancer Patient Voice
How can researchers and others who are interested in building mHealth apps for cancer supportive care know what cancer patients need the most? It may seem obvious that the first step would be to ask cancer patients what they need and want. But, surprisingly, the voice of the cancer patient is often absent from the conversations that lead to the design of supportive-care programs for this very population.
Some developers have invited cancer patients into their app development process, such as the researcher who created a real-time tracking tool for breast cancer patients and had patients try it out [ 8 ]. Others have created apps and then had cancer patients try them out, such as the researcher who made revisions after getting feedback from the adolescent cancer patients who tried out her game-type app for managing pain [ 9 ].
While the actual use and testing of mHealth apps with cancer patients during development and afterwards is essential, what about the initial steps in developing an app? A key starting point is a “rigorous evaluation of the consumer’s needs” [ 10 ]. Understanding “the nature and magnitude of the impact of cancer” is essential in planning supportive care [ 7 ].
Looking to gain entry into the mindset of cancer patients, our small team found ourselves at this very point when assigned the task of creating a suite of cancer support videos. In this paper, we share how we developed a representational model to reflect the cancer patient voice and how we used this model in our product development process. We also briefly discuss the broader concerns of the patient voice and recent steps that have been taken to represent that voice in health care public policy in the United States. The aim of this paper is to offer our process and the resulting cancer experience map as a resource for designers of mHealth apps specifically for this population. Our deepest hope is that ultimately cancer patients will benefit from the sharing of this story.
The Oncology Content Specialist: Hearing the Patient Voice
When our health information company decided to create supportive cancer content, an early assignment came to the oncology content specialist and the user experience researchers. Our task was to create a representational model to support script development for cancer support videos and for future cancer content development.
As the oncology content specialist, I was responsible for providing information, resources, and insight about cancer and cancer patients to the team. For over 6 years, I had followed the medical news on cancer and had been tracking the “consumer experience” of cancer patients online in blogs and forums as well as in other media. While my work often involved reviewing oncology content for medical accuracy with an eye to the patient perspective, my initial meeting with the user experience researchers was the first time I was part of a project where the scope of the discussion was the entire range of the cancer experience. Two questions were paramount in the conversation: Who is the person with cancer? And what does a person with cancer experience?
I remember the day that they diagnosed me. I left the hospital, and I couldn’t find my car. It was in a parking garage. I literally was bumping into cars. I was so broken up. I couldn’t see where I was walking. It was just like, ‘Oh, my God. This can’t be happening to me’. [ 11 ]
Emotionally, you don’t drop to the bottom; you get thrown to the bottom. [ 11 ]
When asked to summarize my informal observations, I talked about the patient interview I had recently read in which a man described losing his car in the hospital parking lot shortly after finding out he had cancer. This story brought up the striking contrast between reading research about people who had cancer and reading what was written by cancer patients about their experiences. It had to do with hearing the voice of the cancer patient. Having cancer isn’t like having another kind of illness but is an experience that only those who have had cancer seem to truly understand. There is also a considerable gap in perspective that appears to exist between people who have cancer and those who don’t. Sometimes it seems as if people with cancer are members, albeit unwilling members, of an exclusive club, and those outside—those who haven’t been “thrown to the bottom”—are left wondering what is happening.
It is hard to describe how unsafe, angry, depressed, and betrayed by my own body I felt when first diagnosed with cancer. [ 12 ]
It was also fairly apparent from reading the stories of cancer patients that people don’t have uniform or parallel responses to having cancer. Individuals at one end of the spectrum experience empowering personality changes, while at the other end there are fiercely private individuals who are determined not to say anything about their cancer, who hope no one will find out.
A few weeks before my meeting with the user experience researchers, the medical writer [RSP] and I had talked about our hope that the cancer support videos would feature patients relating their experiences rather than actors reading a script. While our company’s process was underway for creating the necessary legal paperwork, we soon learned that the permission forms wouldn’t be ready in time for our project. With this change in plans, we now needed a representational model more than ever.
I was trying to find information about what treatments are available and things like that, but I kept on finding that every person is different. [ 13 ]
I can’t be the only person who fought cancer and will never say ‘Well, in the end, it was a gift’. [ 14 ]
The User Experience Researchers: Building the Cancer Experience Map
From the start of developing our cancer support videos, we planned to work with the oncology content specialist to develop personas to represent our target users. A persona is an archetype that is based on user research and that communicates user requirements [ 15 ]. Using a persona during product design helps writers and developers understand the information needs as well as the goals, challenges, motivations, hopes, and fears of their target audience.
Researching the Persona
While personas are very common in product development, most companies treat them as proprietary internal collateral and don’t share them outside the company. We suspect that many cancer personas exist, but we located only a few limited cancer personas online. It seemed clear that approaching something as complex as cancer would need a wider view than the view that our established persona process provided. A cancer patient’s needs and experience change dramatically over the course of time. We felt that our traditional single-point-in-time persona format would not be enough. A point-in-time persona, even brilliantly rendered, could not adequately represent the cancer patient’s experience.
To gain insight into an approach that would inform our team and fit both immediate and longer-term needs, we engaged friends and coworkers to chart their perceptions of their personal cancer journeys. These exercises reinforced the complexity of the cancer journey and hinted at common points of experience. We decided that the similarities in the experiences of different kinds of cancer warranted our pursuing a universal cancer experience map.
The hardest part was the waiting. I wasn't sure what it was going to do—if it was going to rapidly expand or slow down . . . If you’re not sure what's going on in your body, it's hard to sit down and think about anything that's going on around you. [ 16 ]
After I got my cancer-free diagnosis, that's when I got depressed . . . Disease-free is the moment—it doesn't mean you're going to stay that way. Everyone around me was celebrating; they were happy, life was good, and I became completely depressed. [ 17 ]
We noticed that the timeline created from the discovered common points followed a clinical path. This wasn’t surprising, given that the experience of cancer is often closely tied to what is happening clinically—for example, getting a diagnosis or making treatment decisions.
With the stages in the timeline identified, we again teamed up with the oncology content specialist to collaborate on how we could keep the patient voice in the forefront. In addition to talking to cancer patients, we had found that actual patient quotes seemed to be our best option for accurately capturing the patient voice, and our preference was to get this information first-hand, rather than as told by a clinician or other third party. So we combed the research sent to us by the oncology content specialist, pulled out the patient quotes, reviewed open-ended interviews our company had previously conducted with cancer survivors, and conducted additional literature reviews, as needed, to have patient quotes from across the stages of the timeline.
I experienced overwhelming distress at my cancer’s recurrence with metastatic disease. I cried buckets of tears with my husband, family, and friends. However, the support of those who love me enough to supply companionship and food helped me realize that I wasn’t dying today. [ 18 ]
People say, ‘You have to be positive. You have to fight this.’ You’re sitting there, depressed, ill, and you just feel like saying, ‘I don’t feel positive.’ Then you feel guilty, ‘I should be positive to be healthy, but I don’t feel positive.’ There’s this whole Catch-22. [ 19 ]
We also identified a variety of sources, including national cancer websites such as the LiveStrong Foundation and the American Cancer Society, articles from magazines like “Coping with Cancer”, and newspapers, including “The New York Times”. Our criteria for choosing an article or patient story was simply that it had to contain actual patient quotes. We also limited our selection to quotes in which a cancer patient described his or her own experiences. In addition, we sought out patient quotes from research articles that included the recorded comments of cancer patients who otherwise might not have spoken out.
My spouse, and most of my family and friends are supportive, but they don’t seem to really understand the constant lifetime struggle of my cancer walk. … I feel my best when I’m around other cancer survivors. [ 20 ]
Initially . . . I couldn't put on earrings, hold a pencil, or button my pants with grace and dignity. Now, seven months out, I have full functionality but my fingertips feel waterlogged, like I've been swimming or hot-tubbing for too long. My doctor says that whatever you feel after a year will likely be permanent. [ 21 ]
We followed a process for affinity sorting, as outlined in Mental Models: Aligning Design Strategy with Human Behavior [ 22 ]. The affinity of the quotes was validated by a team of three user experience researchers. Strong parallels across cancer types were evident, including shock at hearing the diagnosis, difficulty choosing from conflicting treatment options, the waiting and uncertainty inherent in treatment, pressure to be positive, and the benefits of connecting with others who have experienced cancer. The map summarizes those common experiences.
Insights from our research led us to propose actionable strategies for writers and developers. With the assistance of the oncology content specialist, a family medicine physician, and a behavioral health psychologist, we identified the single most important behavior for each stage. For example, “Getting needed information and support” is the behavior for the treatment decisions stage. Because research supporting how best to move this behavior is cited, the map is not only a summary of user research but a resource for content or product development.
Translating research into user-centered mHealth apps is not an easy task. Multidisciplinary teams are composed of individuals with varying familiarity of the topic, varying understanding of user-centered design, and different geographical locations. Development proceeds on many parts separately. Tight timelines are the norm. The voice of the patient can easily lose prominence. We created the cancer experience map in part to bridge these gaps.
The Cancer Experience Map
The cancer experience map represents the complexity of the cancer experience while capturing the common points of change and transition throughout. Based on direct quotes from cancer patients, the map provides design guidelines and identifies one behavioral factor for each stage. We found this combination to be an effective user-centered design strategy. The map is a tangible representation of the cancer patient voice, a solid and trustworthy resource for writers and developers tasked with creating supportive care materials for cancer patients. See Figure 1 and Multimedia Appendix 1 .

Cancer experience map (see Multimedia Appendix 1 ).
The Parts of the Map
The main part of the map (in shaded columns) is the experience timeline, which documents the continuum of stages from initial cancer diagnoses to possible recurrence.
Each stage is further broken down under the headings of Pain Points, Research Findings, Strategies, and Behavioral Factors.
- The Pain Points segment describes the very common situational stressors that someone in each stage is experiencing. For example, in the Diagnosis stage, people feel shock, fear of incapacitation and death, feel betrayed by their bodies, and wonder how to tell others about the diagnosis. In the Treatment Decisions stage, people grapple with conflicting treatment recommendations, get overwhelmed by frightening information, wonder whether a given treatment will work, and have a hard time finding relevant information to make an informed treatment choice. By referring to the pain points in a given stage, writers and developers can approach their work with a more holistic understanding of what the audience or end user is dealing with. Effective developers will keep in mind what is going on during the stage at which their product is aimed.
- The Research Findings segment lists cited information that supports our choice of pain points for each stage.
- The Strategies segment proposes best practices for addressing needs. For example, in the Diagnosis stage, shock and crisis are major stressors, yet research shows that only about 15% of testicular cancer patients report receiving information about common stress and crisis reactions [ 23 ]. This is clearly a gap, an unmet need for cancer patients. One of the strategies described, therefore, is to inform about common stress and crisis reactions and to empathize with emotional turbulence. Strategies are specific, actionable approaches to be considered by the developer of a solution for a given stage. The strategies vary significantly across the journey, just as the patient’s experience and needs evolve.
- The Behavioral Factors segment identifies the primary objective at each stage. These designations are based on expertise from our in-house behavioral health psychologists. For example, in the Diagnosis stage, the most important behavioral factor to influence is acceptance—moving from shock toward an acceptance of reality. Validating emotions and reminding someone to focus on what they can control are listed as ideas for moving a person in that direction.
Patterns that are not stage-specific and that show up throughout the journey include relationship stress, loss of control, and uncertainty. These journey-spanning patterns are represented by the colored circles at the top of the timeline.
The top right of the map includes a data table with cancer statistics, including a breakdown for the four most prevalent cancers: breast, colon, prostate, and lung. This macro research is included as a reference to complement the detailed experience timeline.
How to Use the Map
A writer or developer creating materials or apps for cancer patients can refer to the map and see what a person is likely dealing with at each stage. Understanding stressors from the patient perspective, having research-based strategies, and knowing what behaviors to focus on: all of these help the writer or developer build effective products.
The Medical Writer: Using the Map to Inform Cancer Support Videos
Knowing your audience is fundamental to writing good content. By listening to the words—the voices—of real people, developers can gain a better understanding of the audience they’re trying to reach. The cancer experience map—and the research that informed its development—helped give us insight into a large, diverse audience that would have otherwise been hard to represent.
The cancer experience map proved to be valuable for developing cancer support videos. The videos needed to be very short—at most three minutes—so we had to make hard decisions about what information to cut out or include to capture people’s experiences with cancer and to address cancer’s inherently difficult issues. The cancer experience map—and the verbatim quotes on which it is based—helped us decide what to focus on. The map helped to validate the choices we made about what would be most relevant to the most people.
Not everyone’s experience with cancer is the same. While there are commonalities, people tend to approach cancer in different ways, face different struggles, and find different ways of coping. Essentially, the map helped us answer the question: How can we make the videos more relatable—and helpful—to a greater number of people?
By reflecting both concerns and coping strategies relevant to each stage of the experience, the map helped us create more targeted, tailored videos that could speak to a person’s experience during different periods of time. The data also provided useful information on topics that aren’t as prevalent in evidence-based research, such as the role of spirituality.
After battling cancer, I have a real appreciation for trees, chipmunks, our dog, shrubs, flowers, clouds, people, thunderstorms, the stars at night and life itself—all these things seem more intense to me now. [ 24 ]
We also looked at various themes that emerged in the research, which were summarized in the map or, in many cases, represented by the actual patient quotes. They included the fear of the unknown, the pressure to act positive, the obligation to be strong for the sake of others, the importance of support from friends and family, ways of coping with difficult emotions, strength in one’s faith, and an appreciation for the small things in life. We were able to address many of these themes in the videos.
We approached these issues through personal stories. Through short vignettes, we were able to convey concepts—for example, focusing on what gives you strength—in a way that would resonate more with users. The details of the cancer experience map helped us make these stories richer and more nuanced and to capture the right emotional tone.
I am a firm believer in prayer. It calms me and gives me peace in times that I am spinning with emotions. It gives me someone to tell everything – however I want to say it – rather than picking the things that are appropriate for the person I’m talking to or working to say what I mean without seeming ungrateful or selfish or rude. [ 25 ]
The cancer experience map was a reliable guide for our approach to a difficult, complex subject. Our resulting set of 11 cancer support videos includes Cancer: When You First Find Out, Cancer: Finding Your Strength , and Cancer: Life After Treatment.
We want our cancer support videos to represent the patient voice as effectively as possible. And we want them to be shared with as many patients as possible. We are encouraged, knowing that policy can help make this happen.
The Policy Advisor: Promoting the Patient Voice Through Health Care Policy
The imperative to include the patient voice in cancer supportive care content, whether through the use of the cancer experience map or other patient voice approaches, resonates as well upstream in the realm of health for all patients, that is, in health care policy.
Health care in the United States is in a time of great change and opportunity. At the heart of it, amidst all the swirl that accompanies a transition of this magnitude, is the patient. Many policy leaders, providers, payers, and other health care stakeholders who are active participants in this change agree that patient involvement is critical to the progress of health care. A noted thought leader blogged, “If patient engagement were a drug, it would be the blockbuster drug of the century and malpractice not to use it” [ 26 ].
While the goal is full participation by patients, where does it all begin? Perhaps the first step is with the relationship between a patient and his or her health care provider. Respect, mutual trust, and empathy all play a role in creating a relationship of professional intimacy, where shared decisions can be made.
The consequences for a patient can be significant when the provider and a patient do not share common understanding, goals, values, and assumptions—or said in another way, when the patient’s voice is not considered. Such a disconnect has negative consequences for both patient and provider, and ultimately, for the health care system at large, undermining whatever benefit, care, or healing is being sought or otherwise may be possible.
How can the importance of patient voice affect policy? The patient voice is a key to effective care, to systems that support that care, and to policy that enforces care. And the patient voice has already informed some policy in the United States. The Health and Human Services, Office of the National Coordinator (ONC) Health Information Standards Committee’s Consumer/Patient Engagement Power Team brought a group of patients and advocates together and asked them what they would want from Health Information Technology (HIT). This was the result—a goal to “ensure that pending regulatory requirements and standards meet current opportunities for engaging patients and their families in their care, and anticipate future policy and technology that encourages further engagement” [ 27 ].
This group made recommendations that will enable patients to participate as partners in their care. Their work has subsequently informed policy and standards work, specifically within the ONC for Health Information Technology Meaningful Use criteria. This includes patients’ access to medical records to view, download, or transmit (Blue Button); secure messaging; patient-generated data; patient-specific education in English and other languages; and further clarity on privacy and security for patients/consumers in the Health Insurance Portability and Accountability Act (HIPAA) omnibus rule.
Policy-focused groups (such as the ONC team) that represent the patient/consumer voice will continue to put pressure on access, design, education, quality, and care. This will affect innovative mHealth apps being created to provide cancer supportive care. Why is this important? The patient voice must be heard. The cancer experience map is an example of a guide, a design tool to help mHealth apps succeed.
We have described the development of the cancer experience map, which has value as a resource for mHealth app developers who are looking to include the voice and concerns of the cancer patient in the creation, development, and delivery of apps for cancer supportive care.
Cancer supportive care is an ideal focus for the development of mHealth apps. Cancer patients are a population of people who have been through a life-threatening and life-altering experience. In the United States, an estimated 14 million people live with a history of cancer. Many issues affect people who are in active treatment—hearing the diagnosis, making treatment decisions, dealing with side effects. Then another related but separate set of concerns arises after treatment: fear of recurrence, long-lasting or permanent effects from treatment, and the emotional and psychological consequences of going through such an experience. The transition in care from active treatment under an oncology care team back to a person’s former general practitioner can also be difficult for both patient and provider. Through all these stages, mHealth apps could offer seamless methods for patients to connect with their providers and vice versa. Issues such as how often checkups are needed or what symptoms are common or expected could be handled simply and quickly, and reassurance could replace worry or unneeded health care calls or office visits.
A major limitation to the current work is the lack of user-testing data thus far. User testing is important to find out if products are effective.
In our case, the cancer experience map was put to the test while the ink was still wet, so to speak. As the map was being assembled, our writer used parts of it in the scripts he wrote for the first six videos on coping with cancer. He then was able to use the entire cancer experience map for the next five scripts. However, the videos are still too recent to have accumulated enough user feedback to get a good sense of how they are perceived by viewers. Having sufficient user feedback will be key to knowing if we were successful in identifying commonalities in the cancer experience and addressing points of concern. We look forward to gathering this additional data.
Another limitation we encountered is that projects like the cancer experience map are ordinarily featured in product development materials rather than professional research journals; consequently, this article lacks a systematic literature review.
While the cancer experience map reflects the experience of Americans with cancer, it is likely that some of these traits are universal. Further research is needed to discover what those similarities and differences are and to see how our work compares with similar research projects in other parts of the world.
The cancer experience map presented in this paper is one way mHealth app developers can consider and include the voice of the cancer patient in their design, creation, testing, and utilization of apps for cancer supportive care. This is an exciting time for mHealth app developers, as rapid developments in technology are moving beyond those that seemed so novel just yesterday, and apps that offered limited fitness data or diet information are giving way to wearable motion sensor detectors and programs that seamlessly integrate mHealth apps with electronic health records systems. It is only a matter of time before current obstacles, such as security concerns and certification criteria, are resolved. With this article, we offer a contribution—the cancer experience map—to help developers create cancer supportive care apps that will assure patients that their voice is being heard.
Acknowledgments
This paper had its genesis in the presentation “The Patient Voice and Experience Matters” by Leslie Kelly Hall (one of the authors of this paper) at the Bucconi Conference in Milan, Italy, in April 2014, on mHealth for improving quality of life and enhancing cancer supportive care.
The authors would like to thank associate editor Pat Truman for her copyediting, medical librarian Liisa Rogers for her research, and senior content manager Katy Magee for her editorial work.
Abbreviations
Multimedia appendix 1.
Cancer experience map.
Conflicts of Interest: None declared.

IMAGES
VIDEO
COMMENTS
Navigating your way through a cancer journey can be tough. It can be hard to find time to care for your body, spirit and mind. Journaling is one way patients can care for themselves. Writing down your thoughts gives you an opportunity to work out your feelings and emotions, which may help you relax and find reasons to be happier and more ...
My Cancer Journey
What to expect when caring for someone with cancer
Your Cancer Road Map is the guide that every cancer patient needs to relieve the stress of diagnosis and provide guidance and companionship throughout the cancer journey. Lidia Schapira, MD, FASCO Director of the Cancer Survivorship Program at the Stanford Comprehensive Cancer Institute
Here are five ways patient navigators can help you through your cancer journey: 1. Bridge cultural gaps that can affect your cancer care. The health care experience is different across geographic locations and cultures, and learning the complexities of health care in the U.S. isn't easy. If you are from another country or part of a diverse ...
OncoPilot: Navigating the Cancer Journey. This guide has been developed to give you suggestions on ways to make a new diagnosis of cancer easier and to help you make the best decisions during this emotional time. It is important for the patient to become an active member of his or her healthcare team.
The Patient Story: Human Answers to Your Cancer Questions
Lessons from my cancer journey. As a child, I played a game with my friends that involved crawling through drain pipes underneath the streets. Of course, my mother had no idea of where we were or ...
Love yourself, even when you feel unworthy. My doctor warned me that I was beginning to feel worse as the treatments came to an end and for several weeks after they were over. He was right, and ...
Understand Cancer Together is an educational website brought to you by Merck. Merck has selected information on this website from various organizations that are experts in cancer to help guide you through your journey and make more informed decisions with your doctor.
Cancer survivorship is the longest part of the cancer journey. Acknowledging that recovery will take time, setting boundaries, moving your body, and making an appointment with your primary- care ...
2. Once treatment stops the patient will still need help. One of the first steps after being told someone has cancer will be learning about the diagnosis. This will help the caregiver and other family members understand the disease process and get an idea of what lies ahead.
Life After Cancer | When Cancer Treatment Ends
As we can see from Alex's journey, the cancer pathway for a patient can be long, complex and fraught with obstacles. These obstacles will vary widely depending on the patient, but importantly many of them are fixable. Fixing them won't be easy, but it is possible. Cancer survival in the UK has doubled over the last 50 years, and with the ...
The Journey. Patients and caregivers rely on each other on the path to wellness. The Journey is a blog that addresses the unique hurdles people face on their cancer journey. The Journey.
Introduction. Cancer is a leading cause of morbidity and mortality worldwide. In 2013, there were ∼1,660,290 new cancer cases and 580,350 cancer deaths in the United States. 1 A diagnosis of cancer is still very stressful and frightening for the majority of patients and families 2-4 although the number of patients living with cancer has increased threefold since 1971. 5 According to the ...
A cancer diagnosis can shake you to your core and affect every aspect of your life. It can also leave you feeling overwhelmed with emotion and at a loss for words. During this complex and difficult journey, many patients say that they find solace and strength in documenting their experiences.
Anxiety. Up to 45% of adults with cancer experience anxiety. Anxiety is feeling worried, afraid, tense, and/or unable to relax. Physical symptoms include a rapid heart rate, loss of appetite, nausea, dizziness, headaches, muscle pain, tightness in your chest, or changes in your sleep patterns.
My cancer teacher could care less if I felt sorry for myself or if I thought having this disease was unfair. There would be no time for wallowing in self-pity on my cancer journey, and the lessons ...
Integrative oncology: Lifestyle medicine for people with ...
Road To Recovery
Breast cancer is the most common cancer and the one that associates the highest mortality rates among Spanish women, with 32,953 new cases estimated to be diagnosed in Spain in 2020 [1]. Thanks to early diagnosis and therapeutic advances, survival has increased in recent years [2]. The 5-year survival rate is currently around 85% [3, 4].
These exercises reinforced the complexity of the cancer journey and hinted at common points of experience. We decided that the similarities in the experiences of different kinds of cancer warranted our pursuing a universal cancer experience map. The hardest part was the waiting. I wasn't sure what it was going to do—if it was going to rapidly ...